THE SKIN COLOUR DISORDERS OF PIGMENTATION Skin Colour










- Slides: 45
THE SKIN COLOUR & DISORDERS OF PIGMENTATION
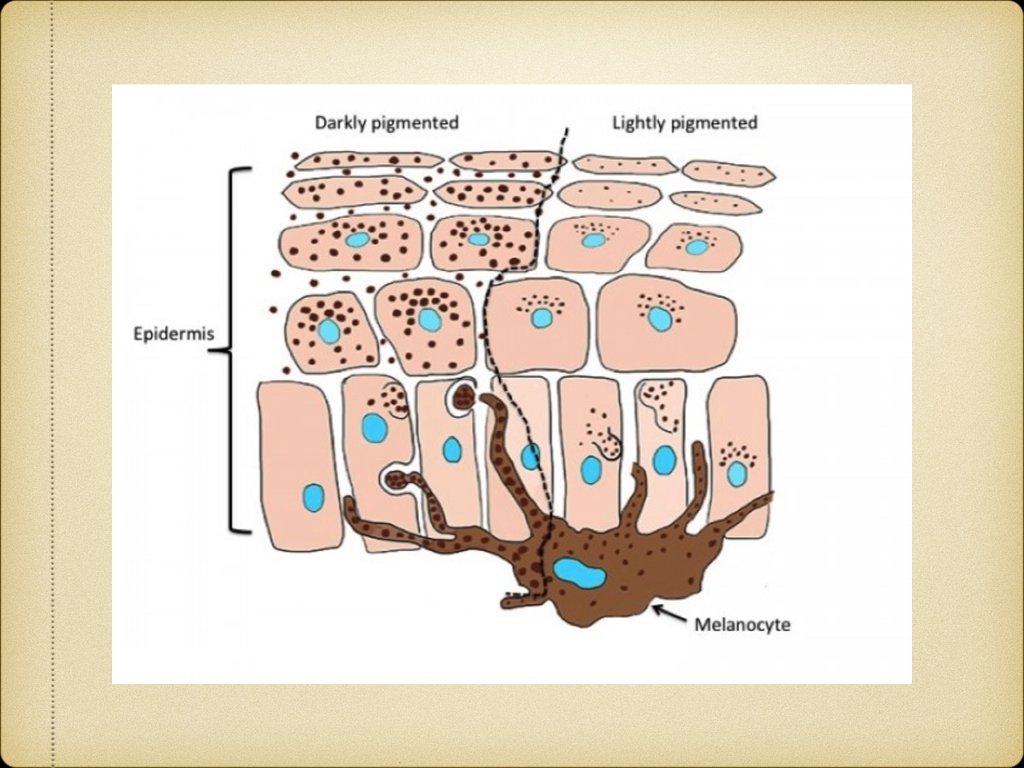
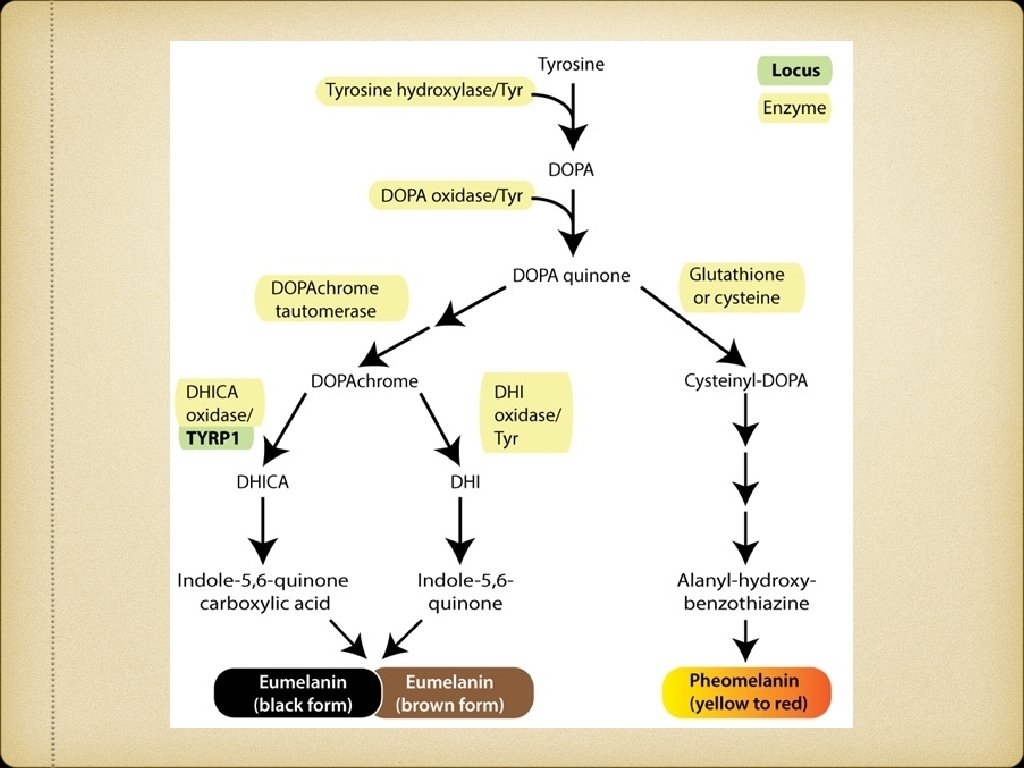
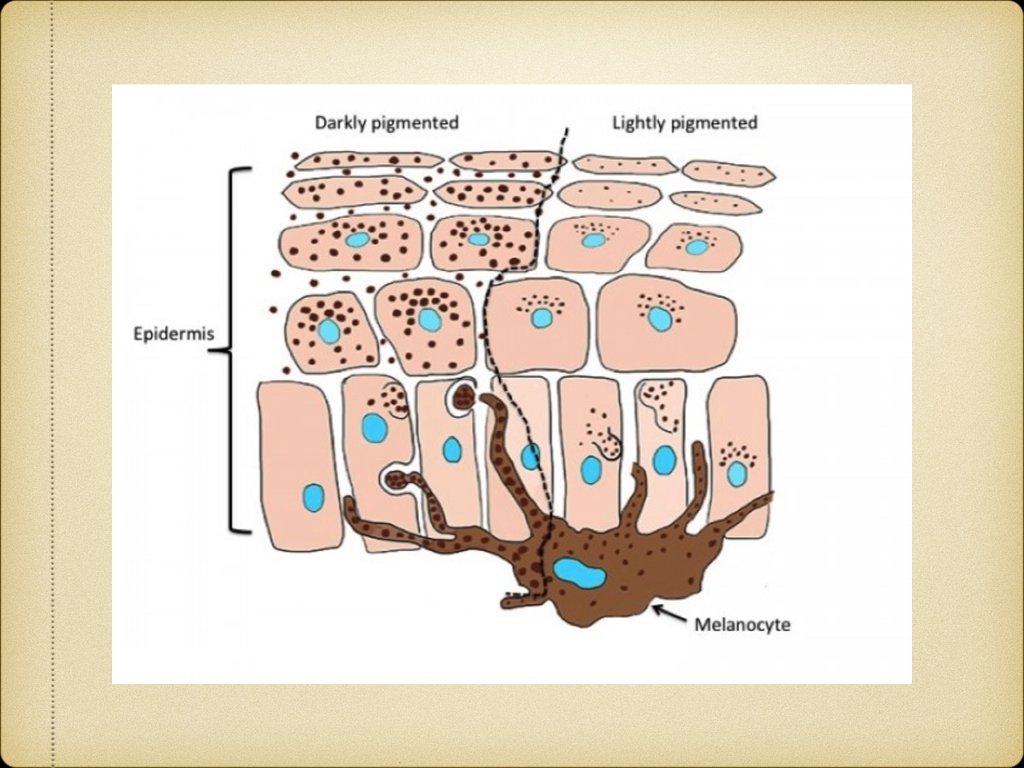
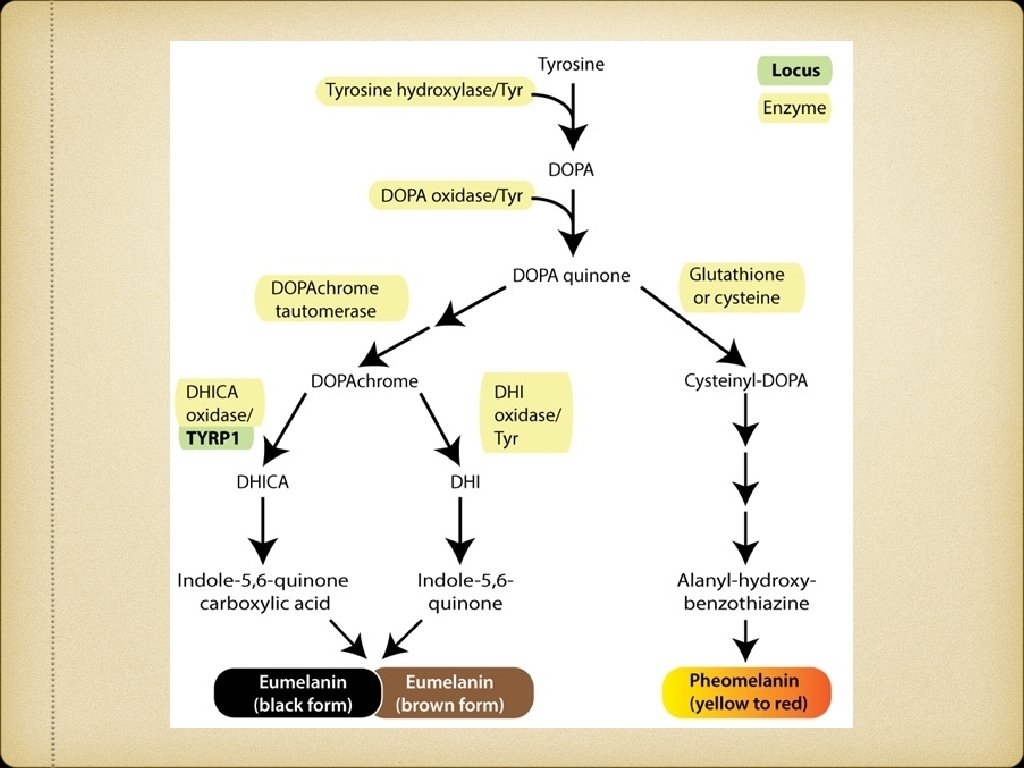
Skin Colour Determined by 1. Melanin 2. Hemoglobin 3. Carotenoids Constitutive skin colour Facultative skin colour
HYPOMELANOTIC DISEASES CLASSIFICATIONS: Congenital/Acquired Diffuse/Focal Hypopigmented/Depigmented Melanopenic/Melanocytopenic Etiological classification
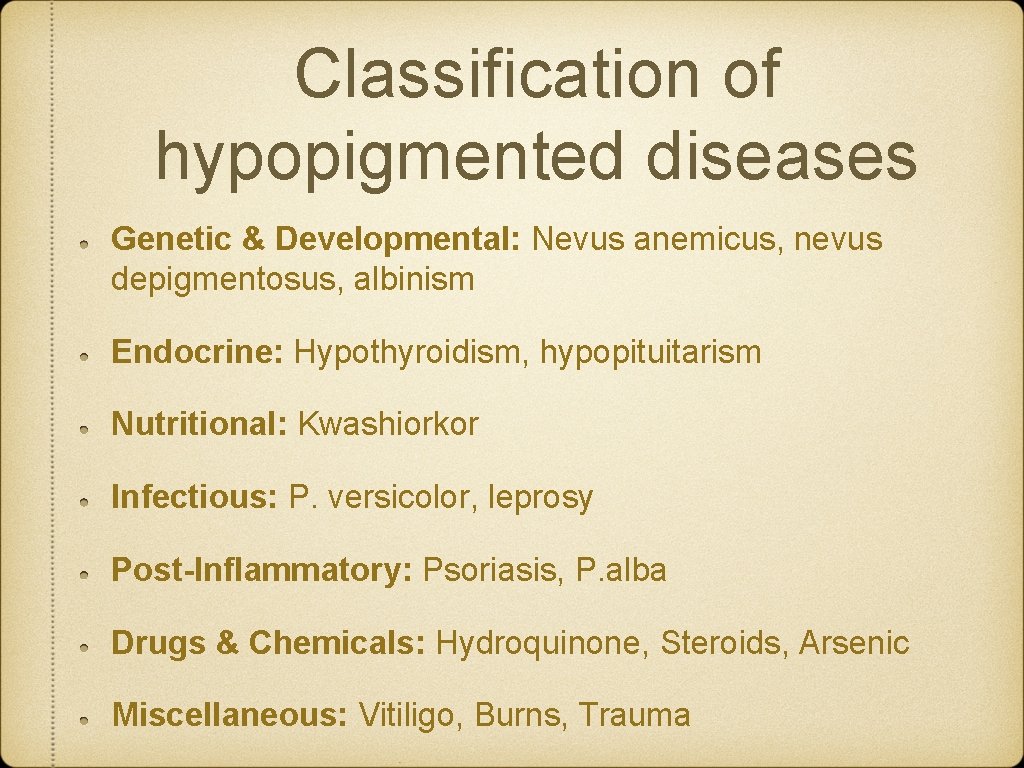
Classification of hypopigmented diseases Genetic & Developmental: Nevus anemicus, nevus depigmentosus, albinism Endocrine: Hypothyroidism, hypopituitarism Nutritional: Kwashiorkor Infectious: P. versicolor, leprosy Post-Inflammatory: Psoriasis, P. alba Drugs & Chemicals: Hydroquinone, Steroids, Arsenic Miscellaneous: Vitiligo, Burns, Trauma
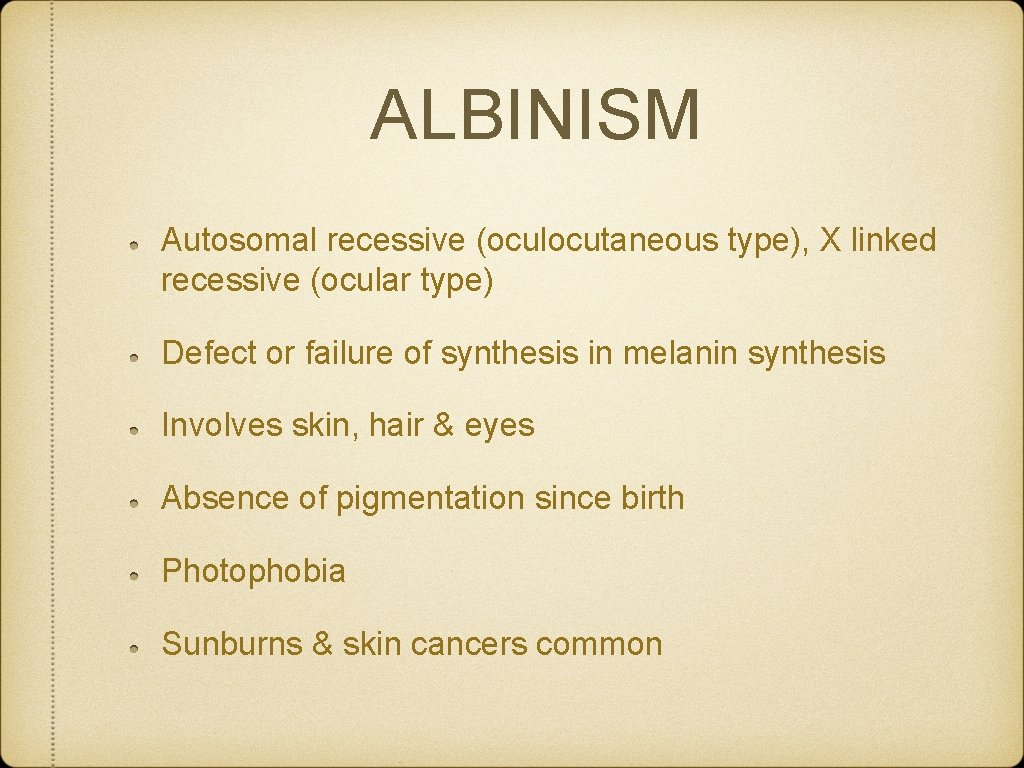
ALBINISM Autosomal recessive (oculocutaneous type), X linked recessive (ocular type) Defect or failure of synthesis in melanin synthesis Involves skin, hair & eyes Absence of pigmentation since birth Photophobia Sunburns & skin cancers common

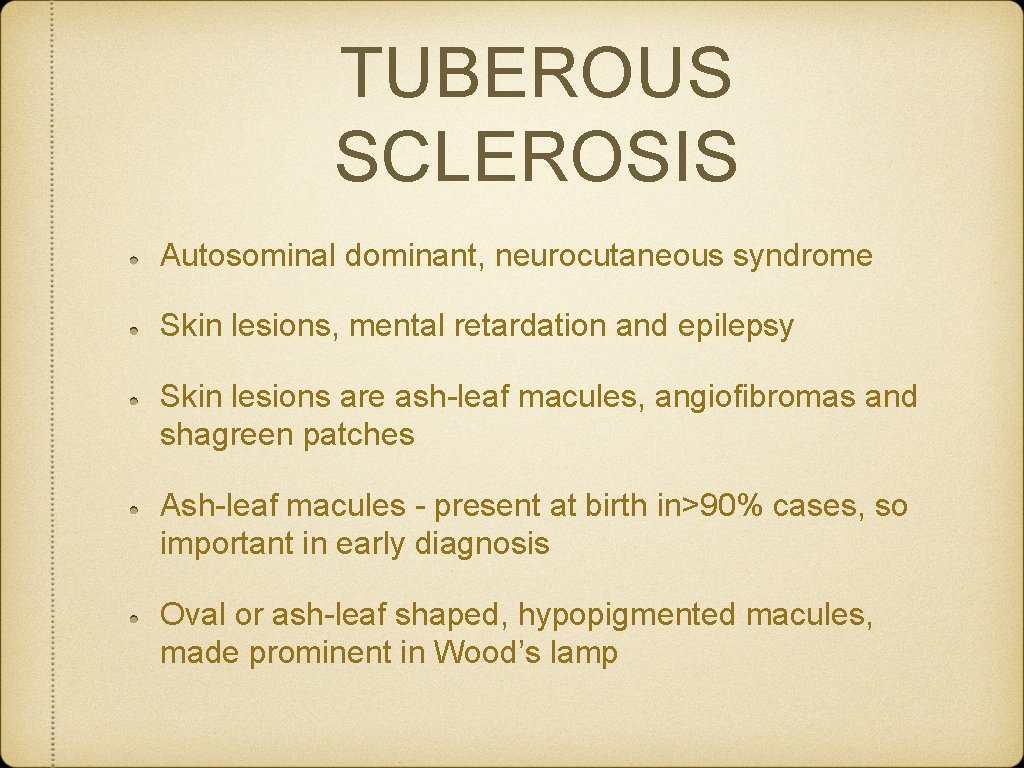
TUBEROUS SCLEROSIS Autosominal dominant, neurocutaneous syndrome Skin lesions, mental retardation and epilepsy Skin lesions are ash-leaf macules, angiofibromas and shagreen patches Ash-leaf macules - present at birth in>90% cases, so important in early diagnosis Oval or ash-leaf shaped, hypopigmented macules, made prominent in Wood’s lamp


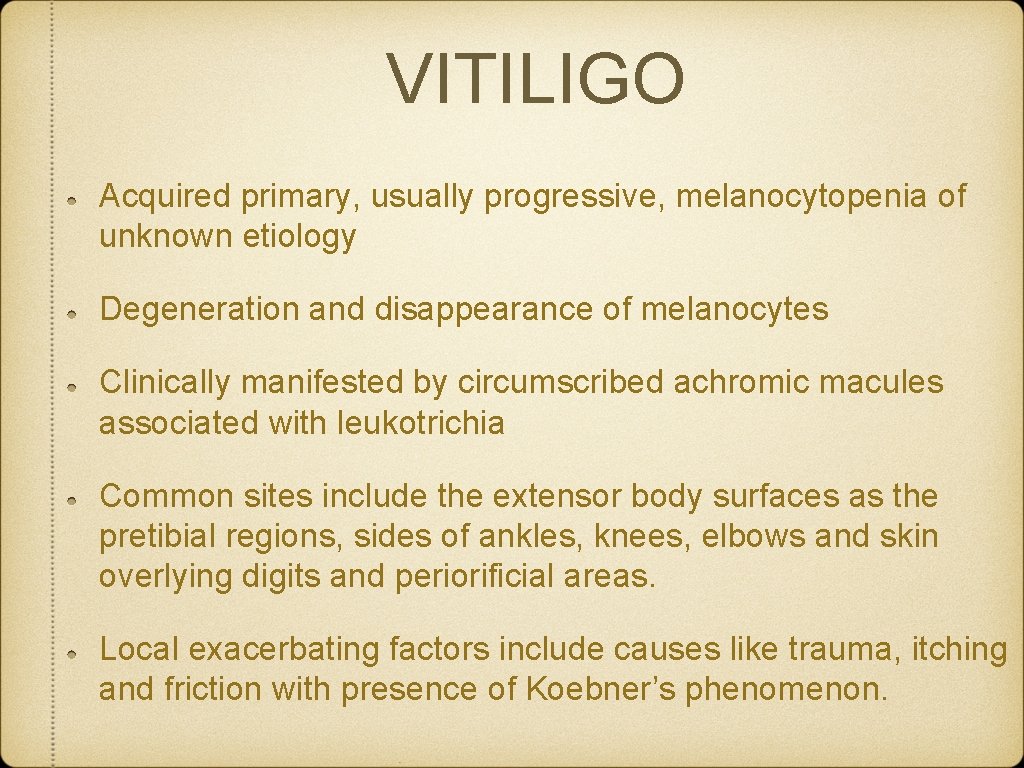
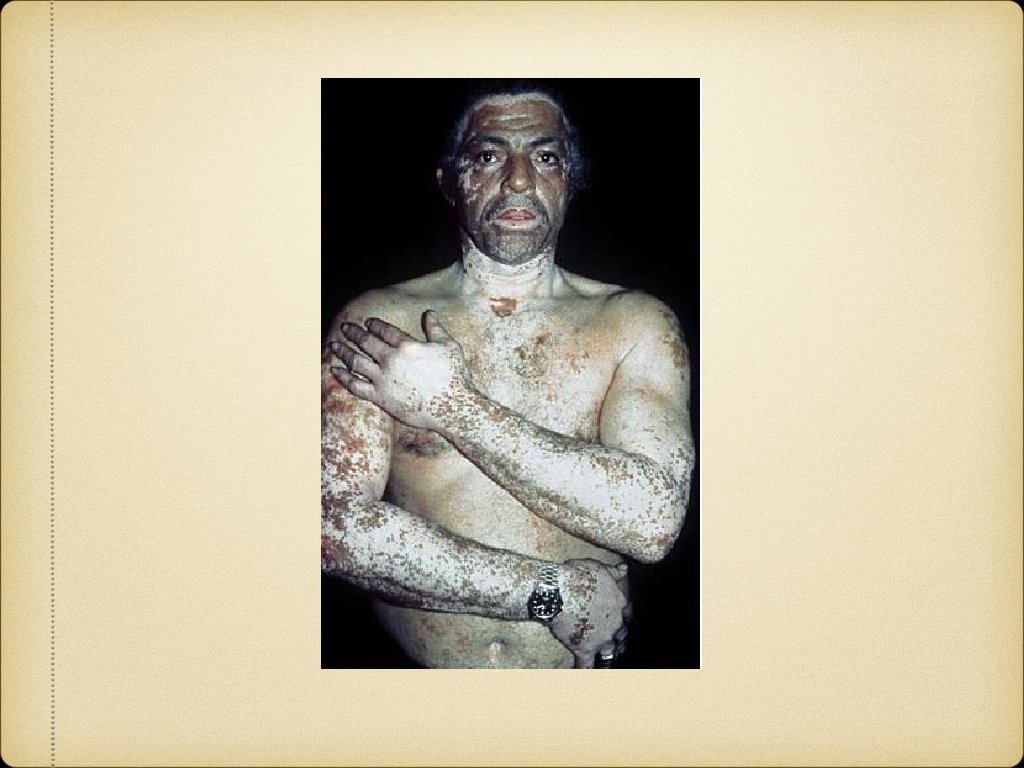
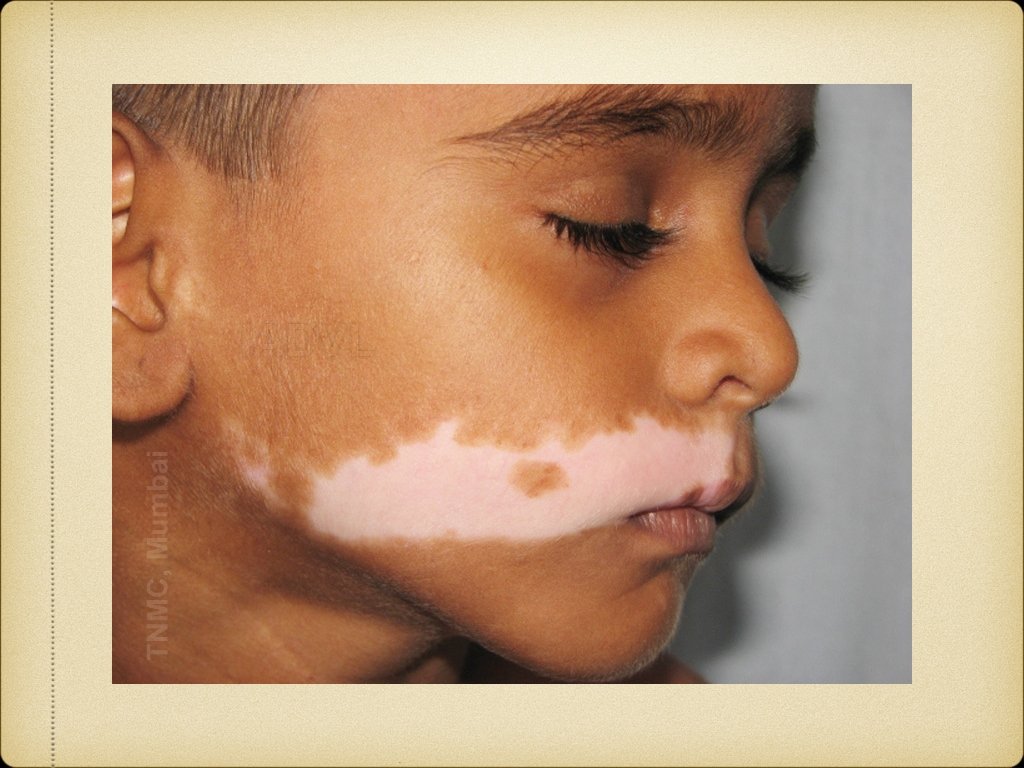
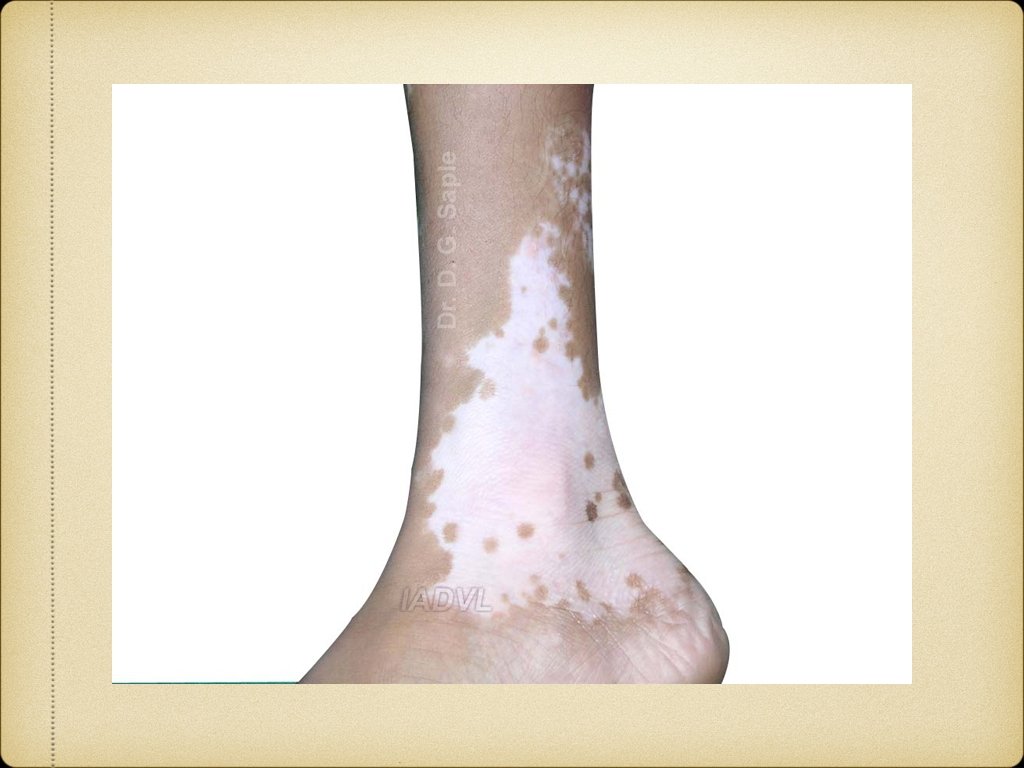
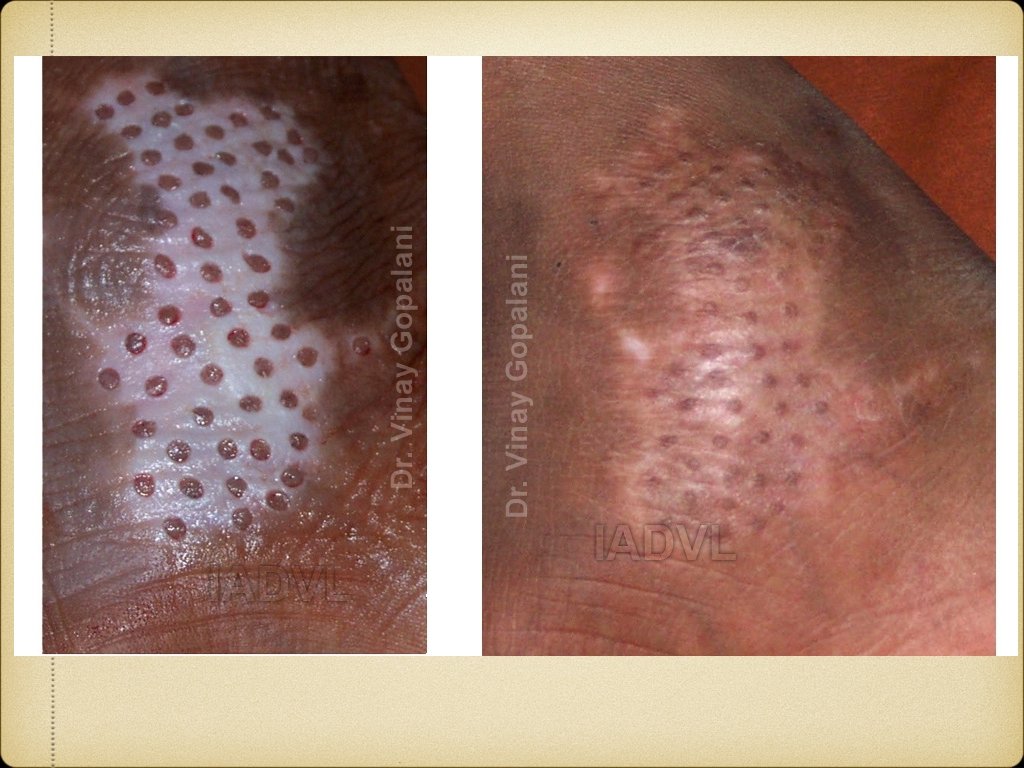
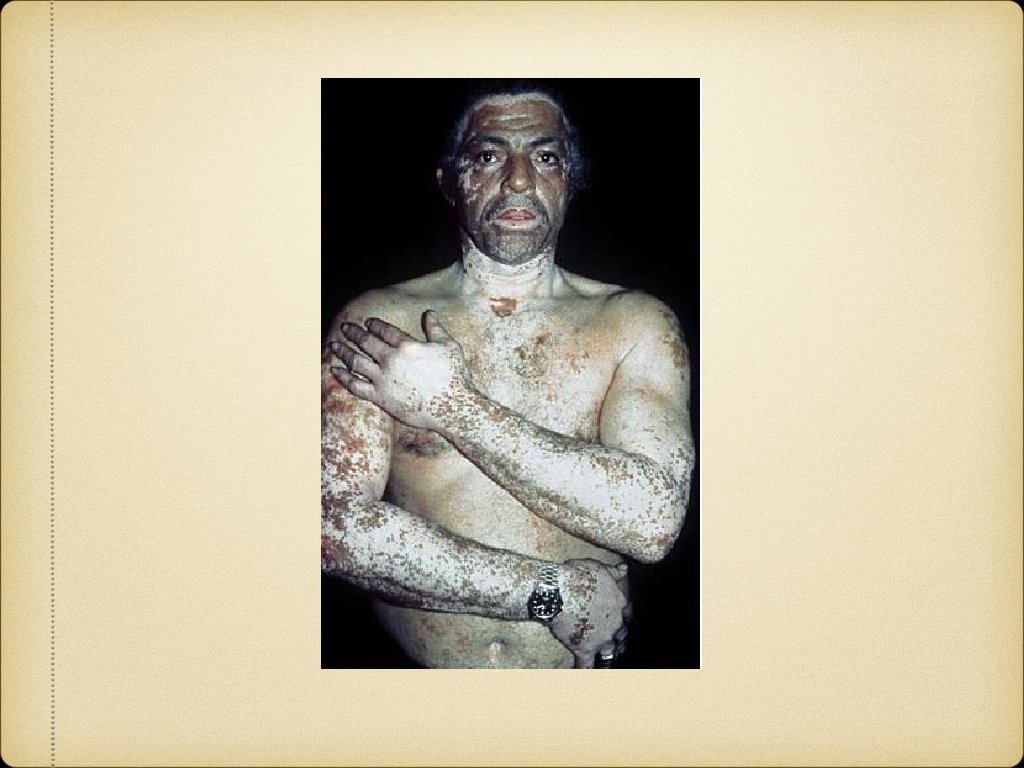
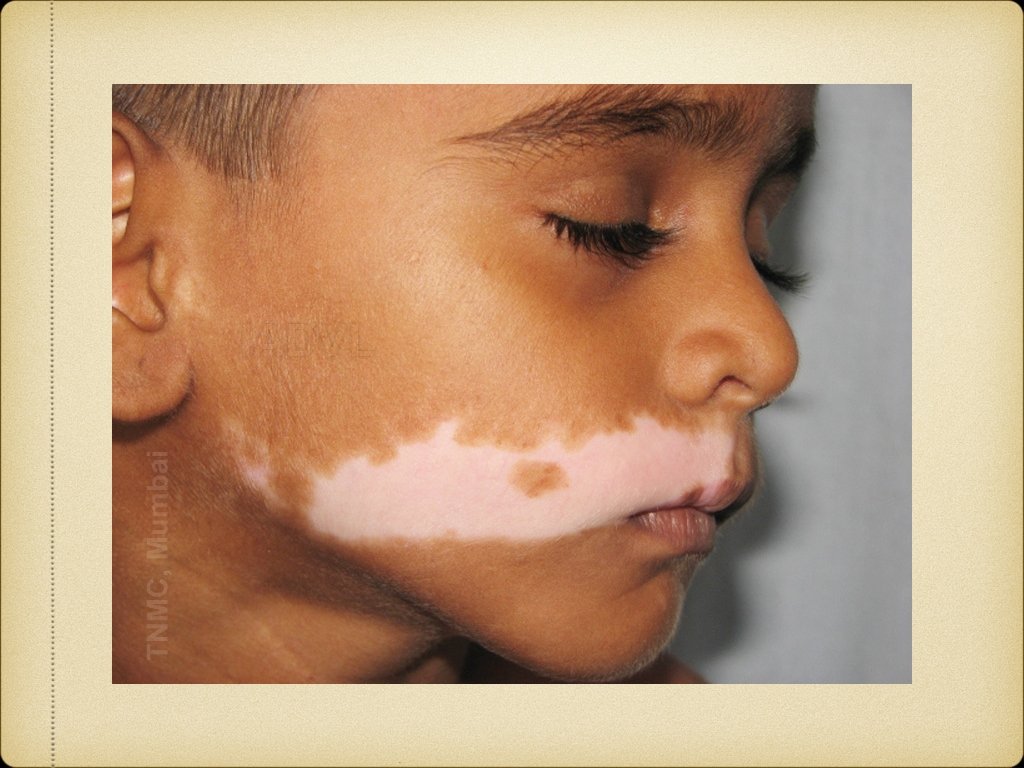
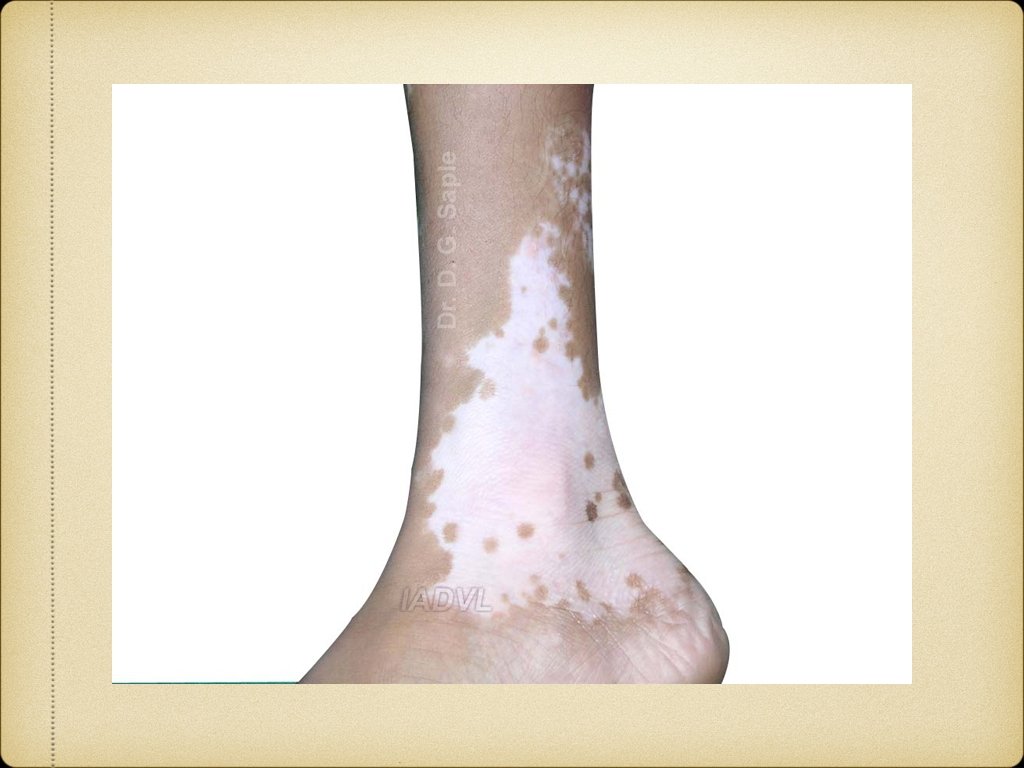
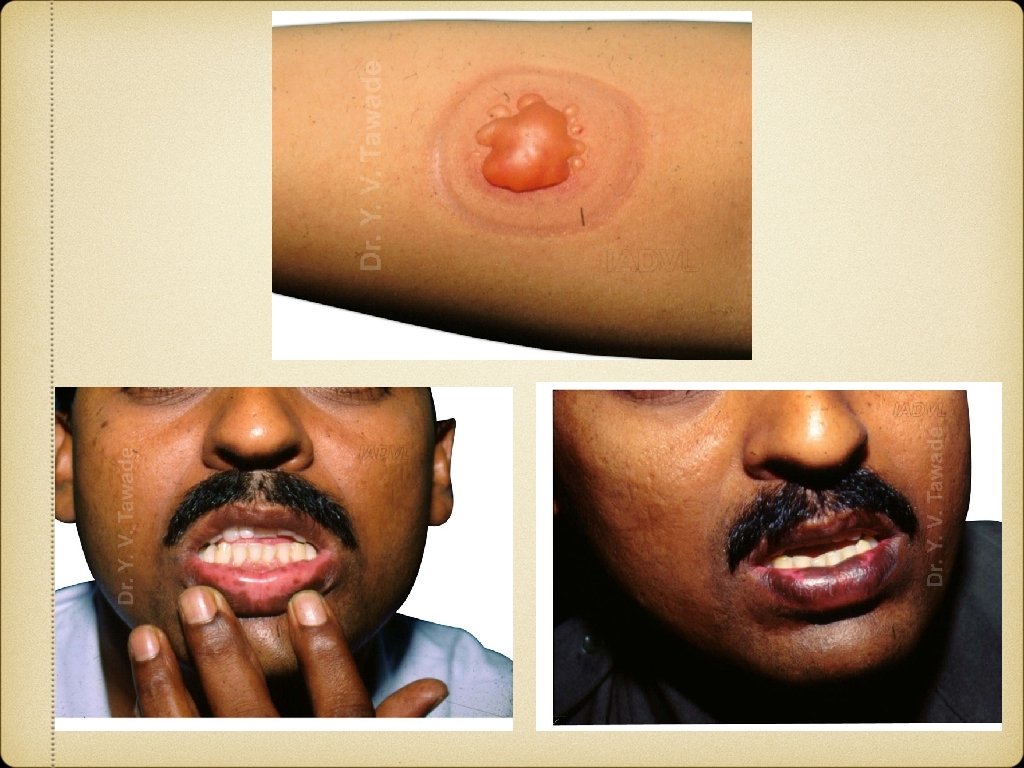
VITILIGO Acquired primary, usually progressive, melanocytopenia of unknown etiology Degeneration and disappearance of melanocytes Clinically manifested by circumscribed achromic macules associated with leukotrichia Common sites include the extensor body surfaces as the pretibial regions, sides of ankles, knees, elbows and skin overlying digits and periorificial areas. Local exacerbating factors include causes like trauma, itching and friction with presence of Koebner’s phenomenon.
Etiopathogenesis of Vitiligo Autoimmune hypothesis Neural hypothesis Free radical hypothesis Antioxidant reduction hypothesis Composite hypothesis
Classification 1. Generalized Vitiligo vulgaris Vitiligo universalis 2. Localised Focal Segmental Acrofacial Mucosal


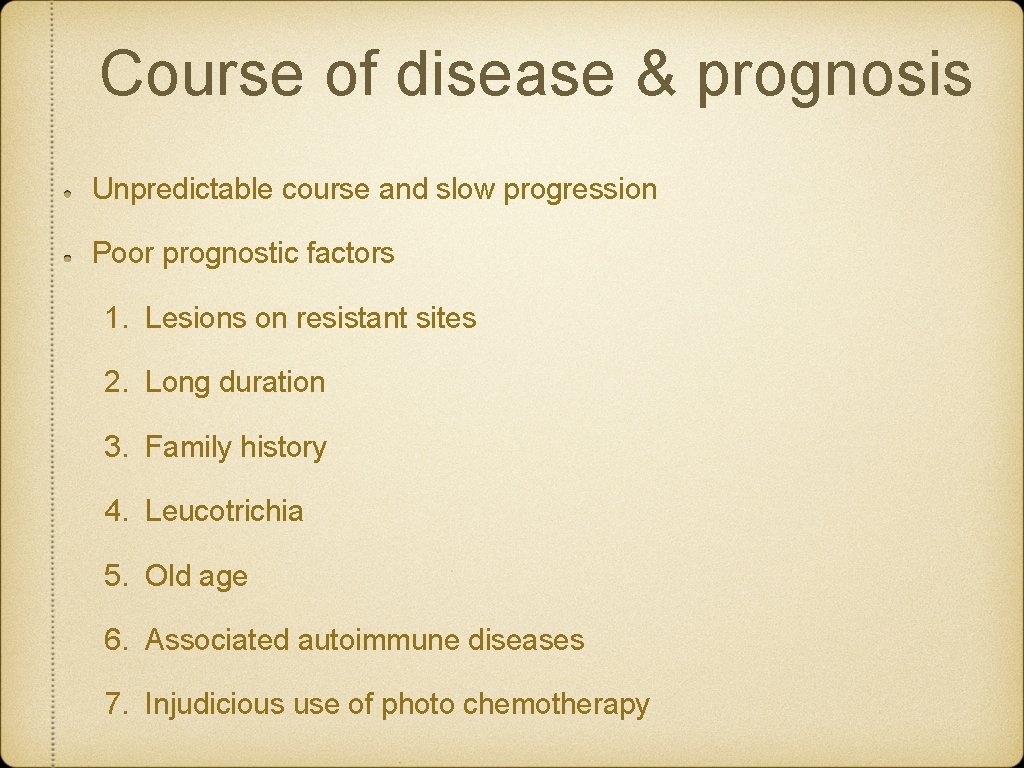
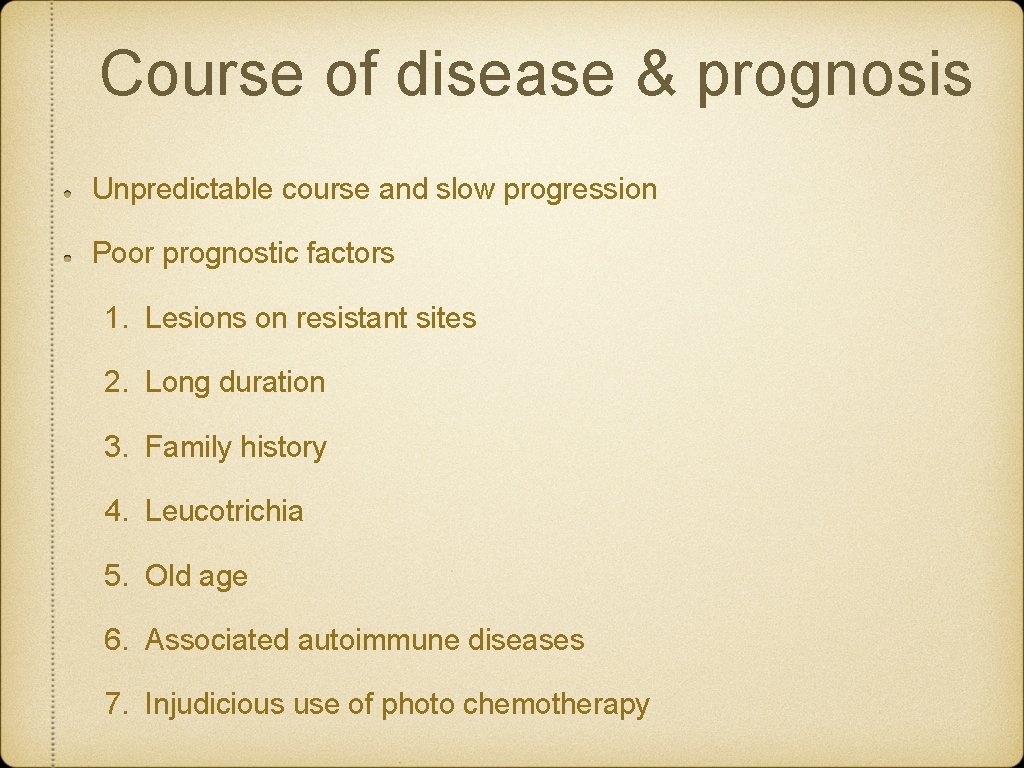
Course of disease & prognosis Unpredictable course and slow progression Poor prognostic factors 1. Lesions on resistant sites 2. Long duration 3. Family history 4. Leucotrichia 5. Old age 6. Associated autoimmune diseases 7. Injudicious use of photo chemotherapy
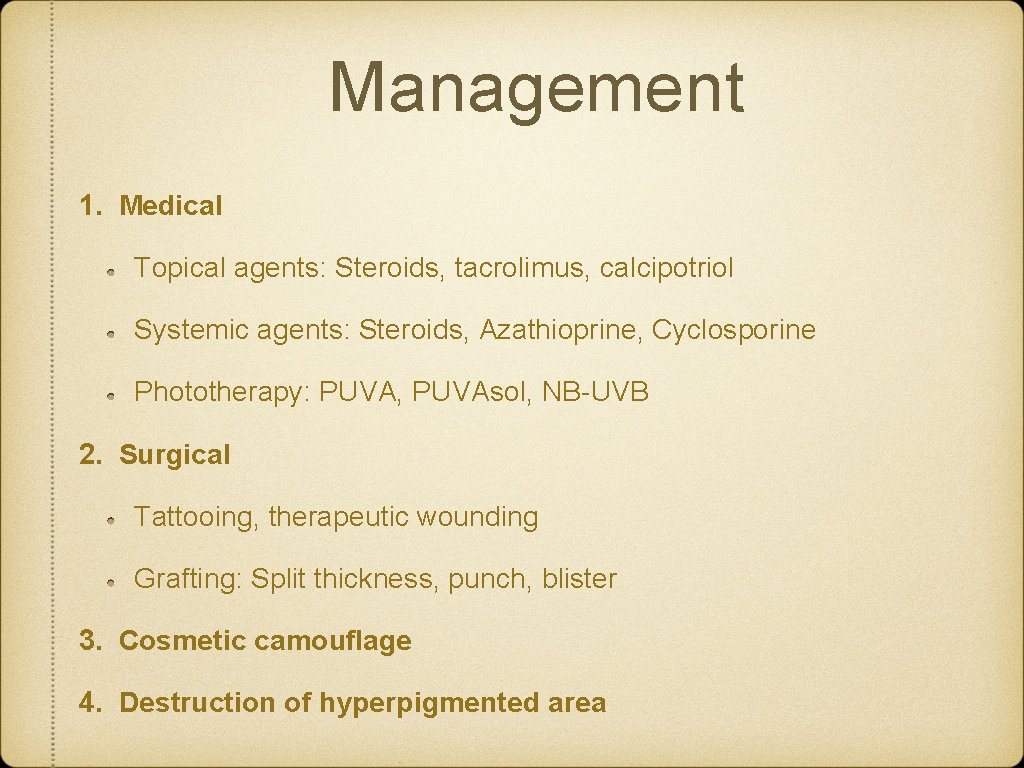
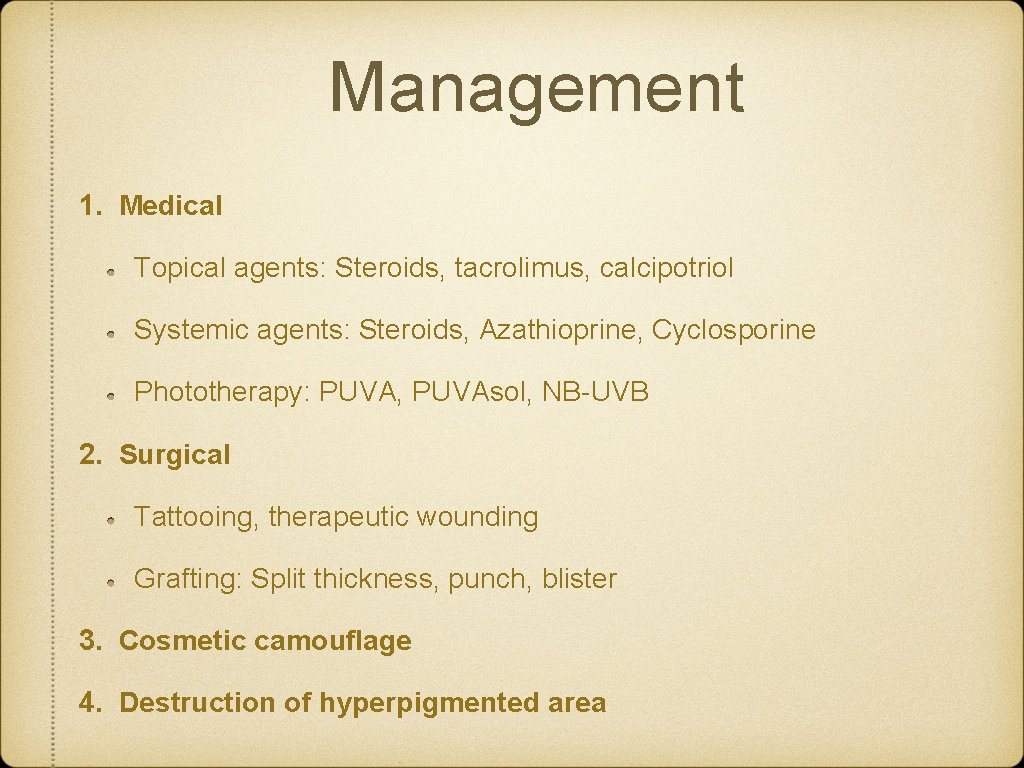
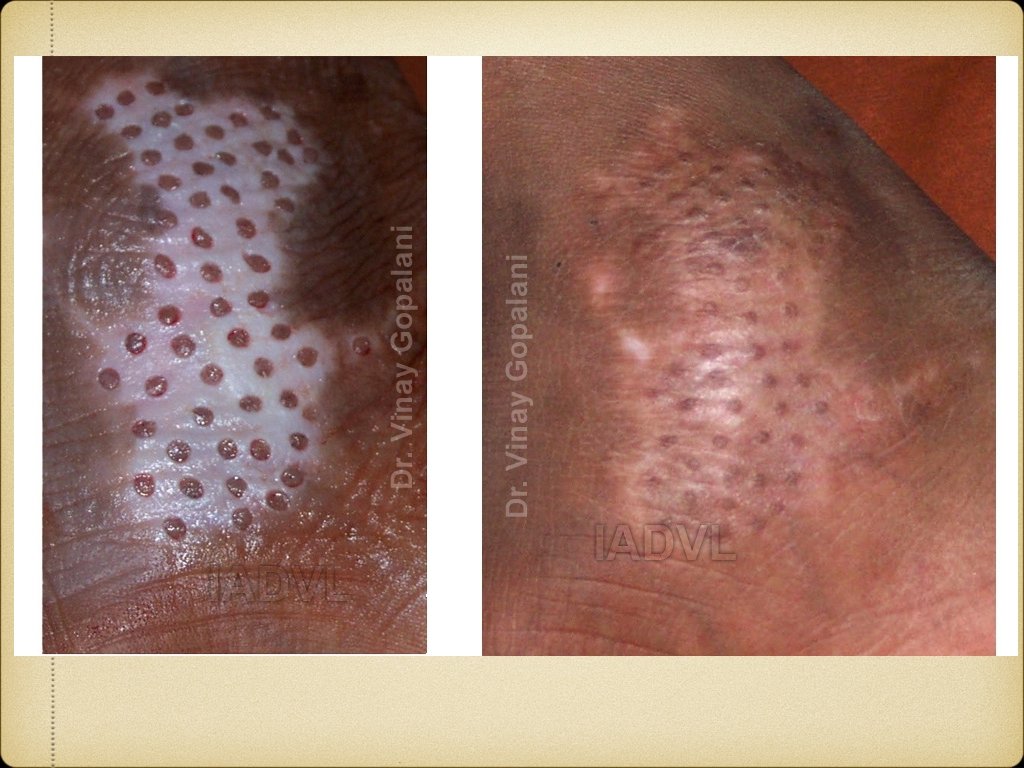
Management 1. Medical Topical agents: Steroids, tacrolimus, calcipotriol Systemic agents: Steroids, Azathioprine, Cyclosporine Phototherapy: PUVA, PUVAsol, NB-UVB 2. Surgical Tattooing, therapeutic wounding Grafting: Split thickness, punch, blister 3. Cosmetic camouflage 4. Destruction of hyperpigmented area



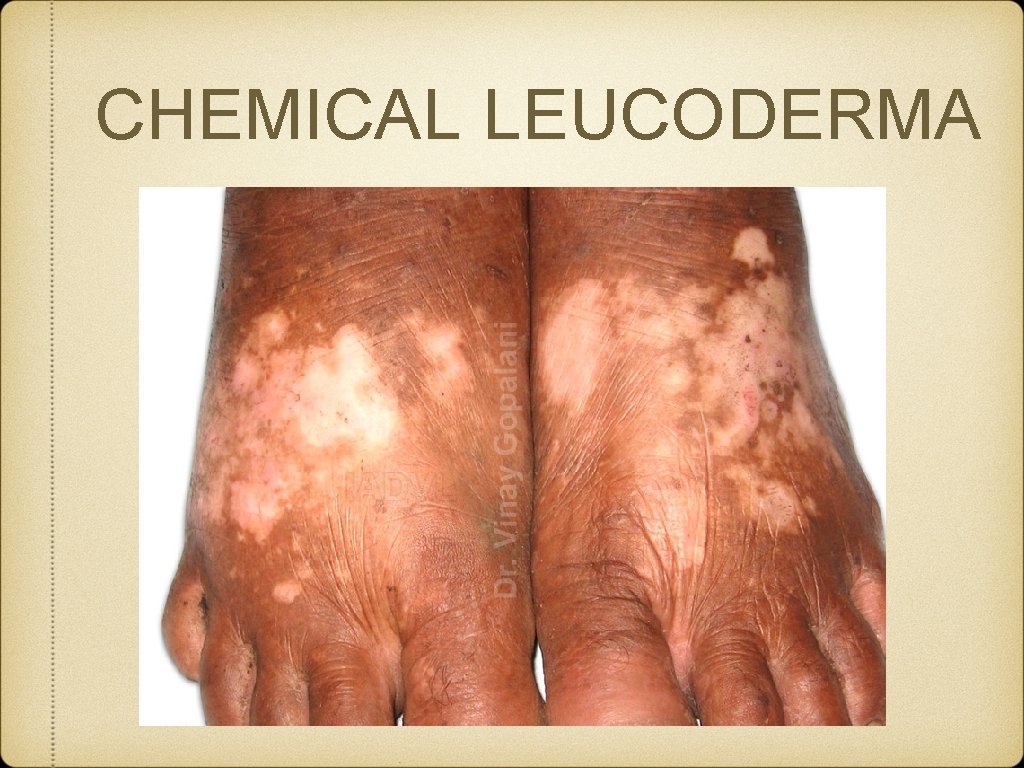
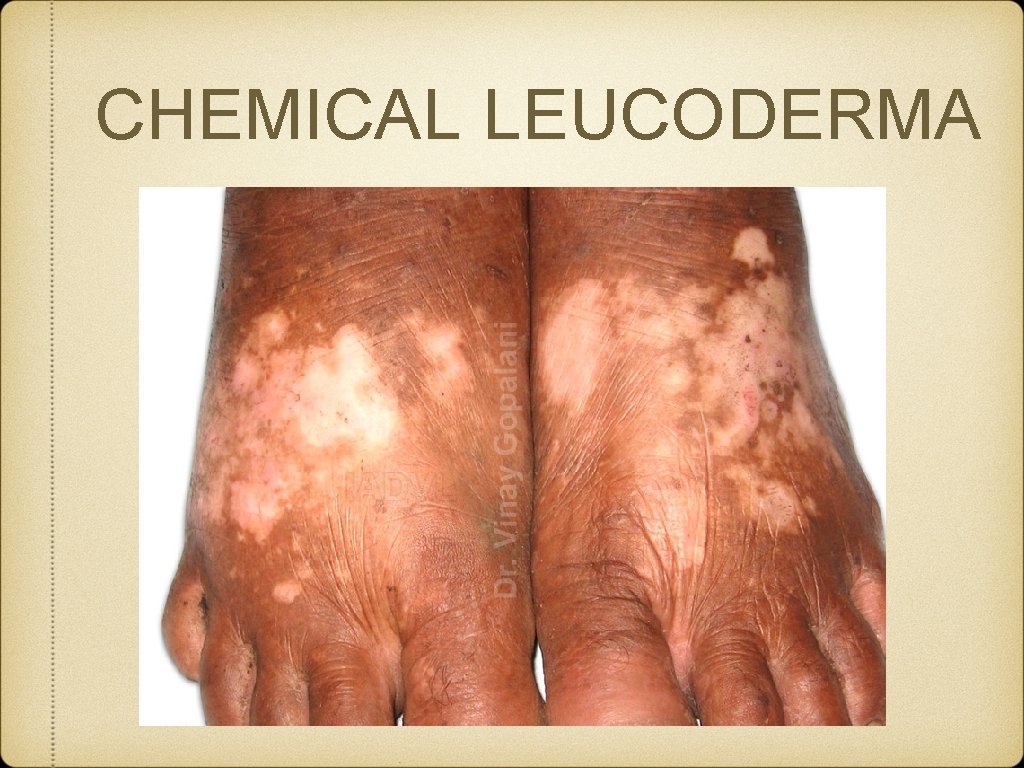
CHEMICAL LEUCODERMA
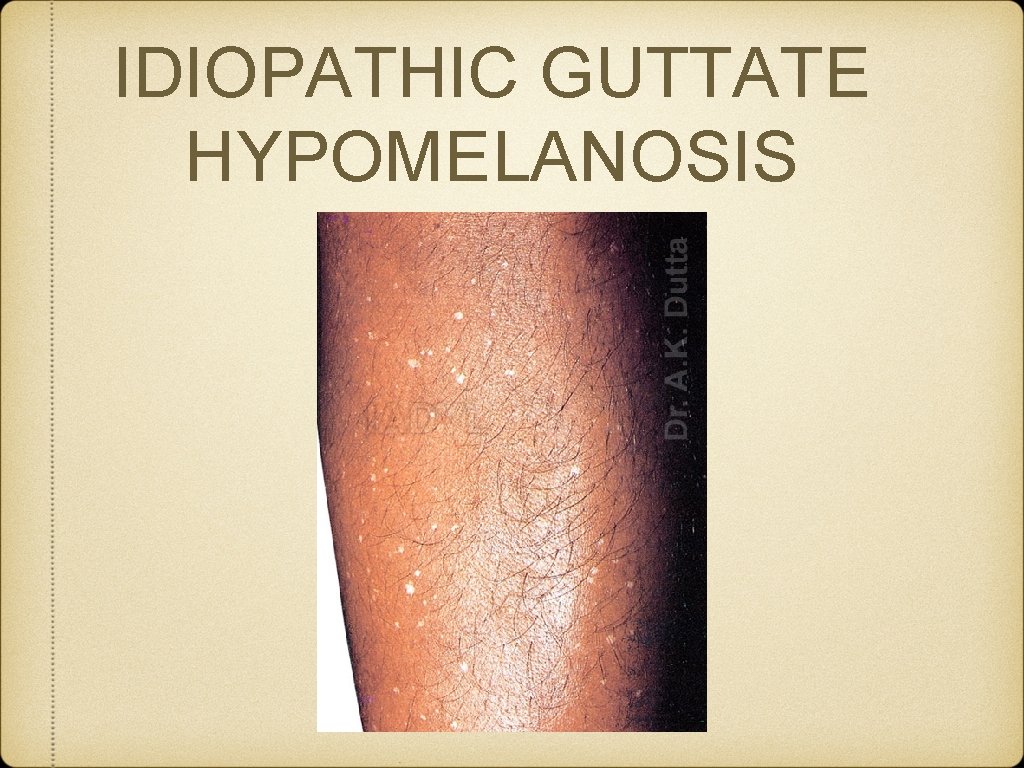
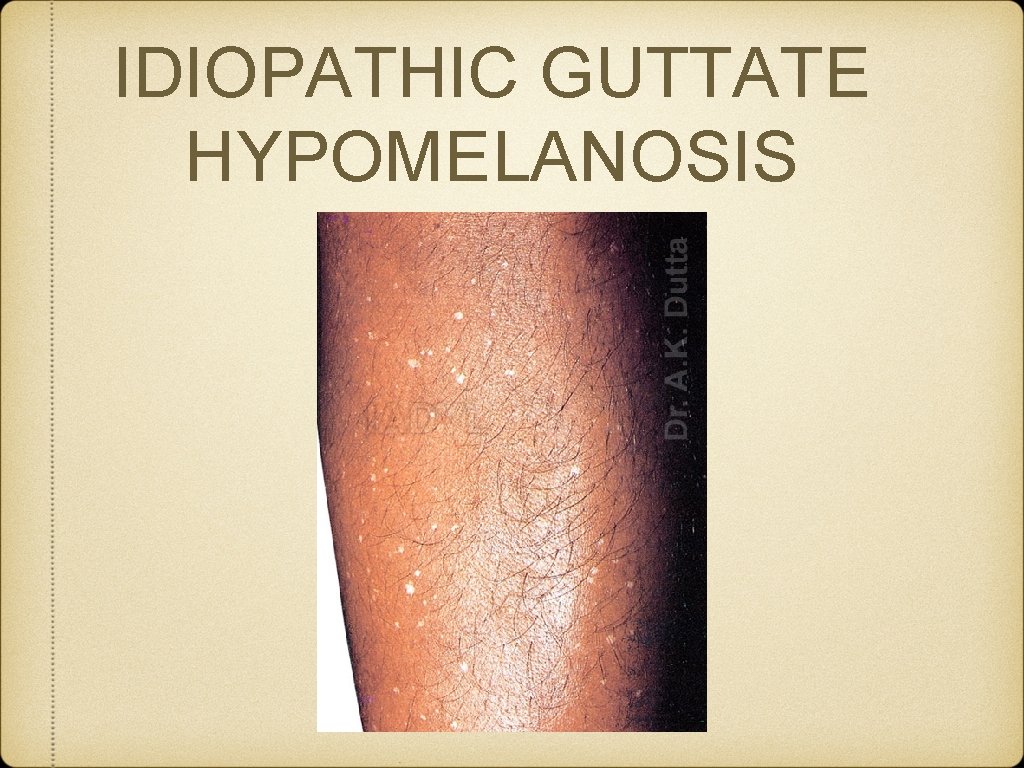
IDIOPATHIC GUTTATE HYPOMELANOSIS
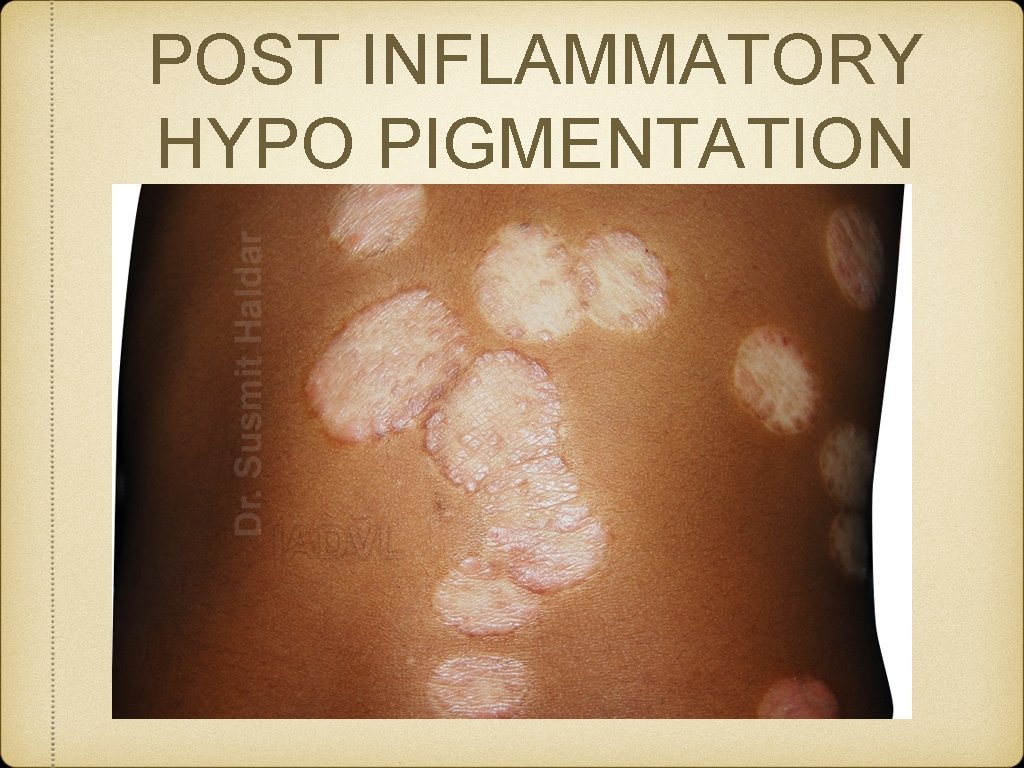
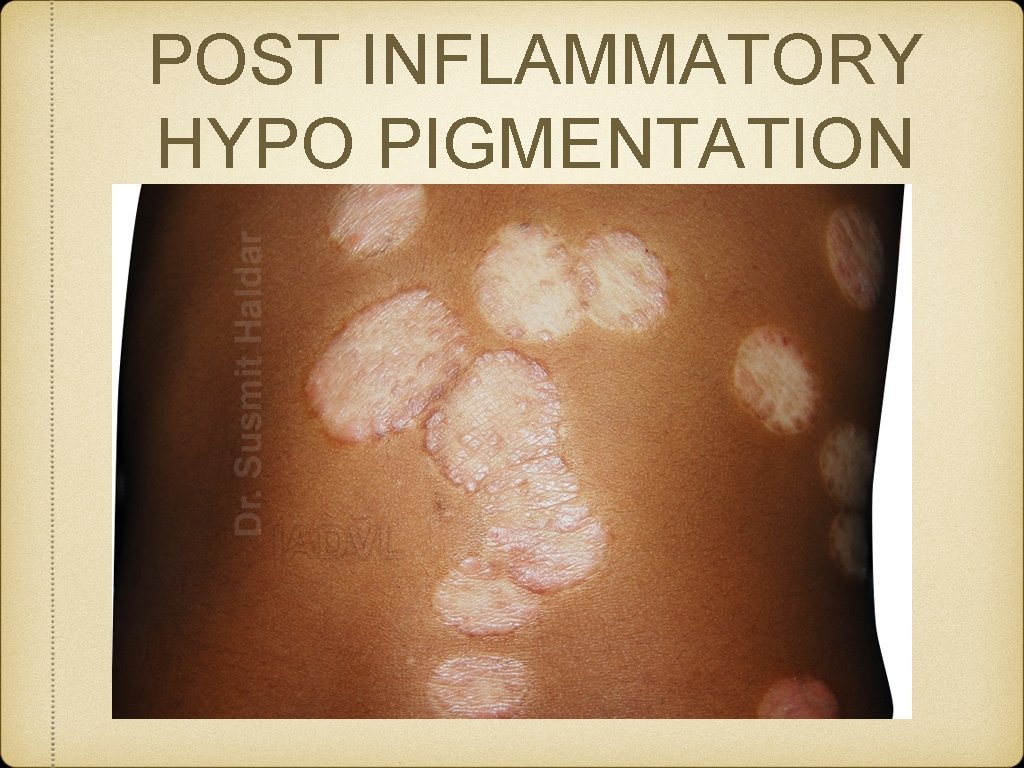
POST INFLAMMATORY HYPO PIGMENTATION
DISORDERS OF HYPERPIGMENTATION Epidermal: dark brown Increase in melanin Increase in melanocyte Dermal: blue-grey Epidermal melanin in dermis Melanin from dermal melanocytes
Epidermal pigmentation Physiological: Tanning Genetic & Developmental: Melanocytic nevus, Lentigines, Ephelides, Xerodermal pigementosum Post inflammatory: LP, Psoriasis Infection: P. versicolor Nutritional: Pellagra, Vit B 12 deficiency Endocrine: Addison’s disease, Melasma, Acromegaly Neoplastic: Melanoma, Pigmented BCC Physical: Trauma, Radiodermatitis
Dermal pigmentation Genetic & Developmental: Mongolian spots, Nevus of Ota Inflammatory: Fixed drug eruption Drugs & Chemicals: Minocycline, OCPs, Clofazamine Endocrine: Melasma Infections: Syphilis Neoplastic: melanoma mets Physical: Post traumatic, burns Metabolic: Amyloidosis Miscellaneous: Chronic nutritional deficiency
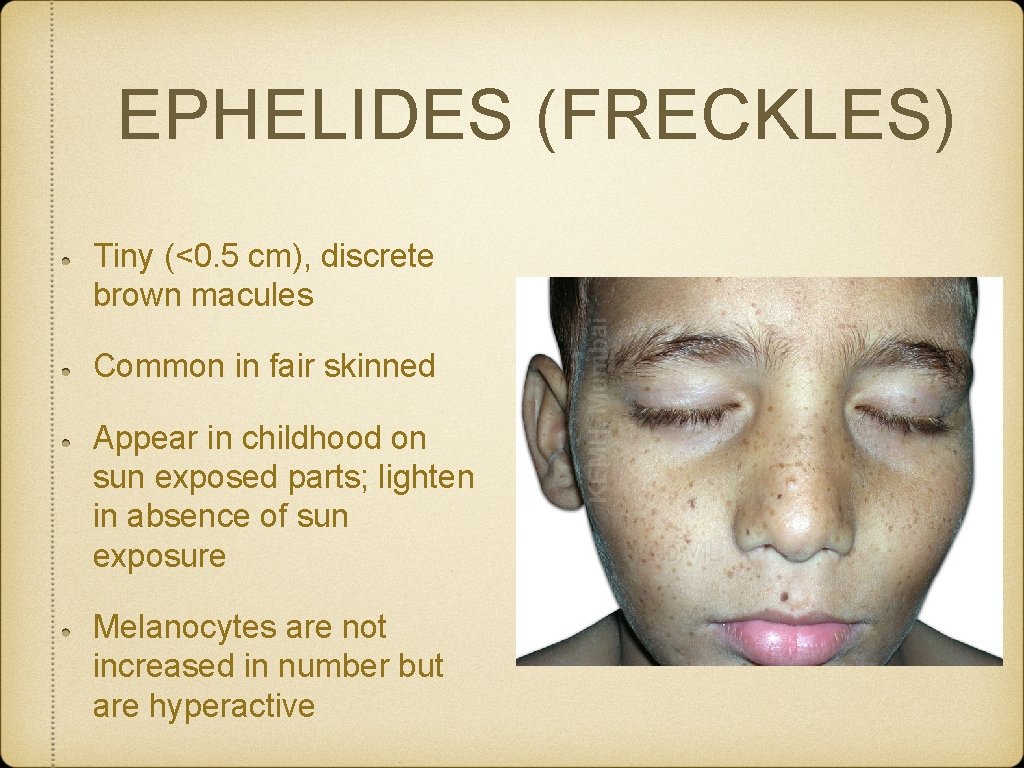
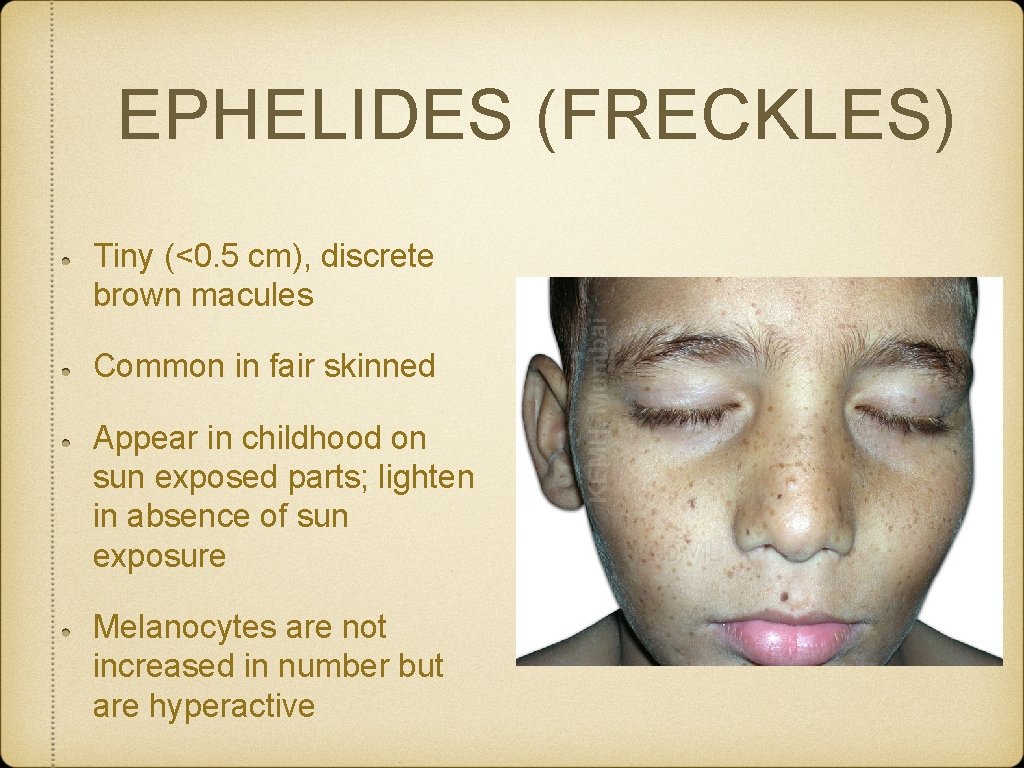
EPHELIDES (FRECKLES) Tiny (<0. 5 cm), discrete brown macules Common in fair skinned Appear in childhood on sun exposed parts; lighten in absence of sun exposure Melanocytes are not increased in number but are hyperactive
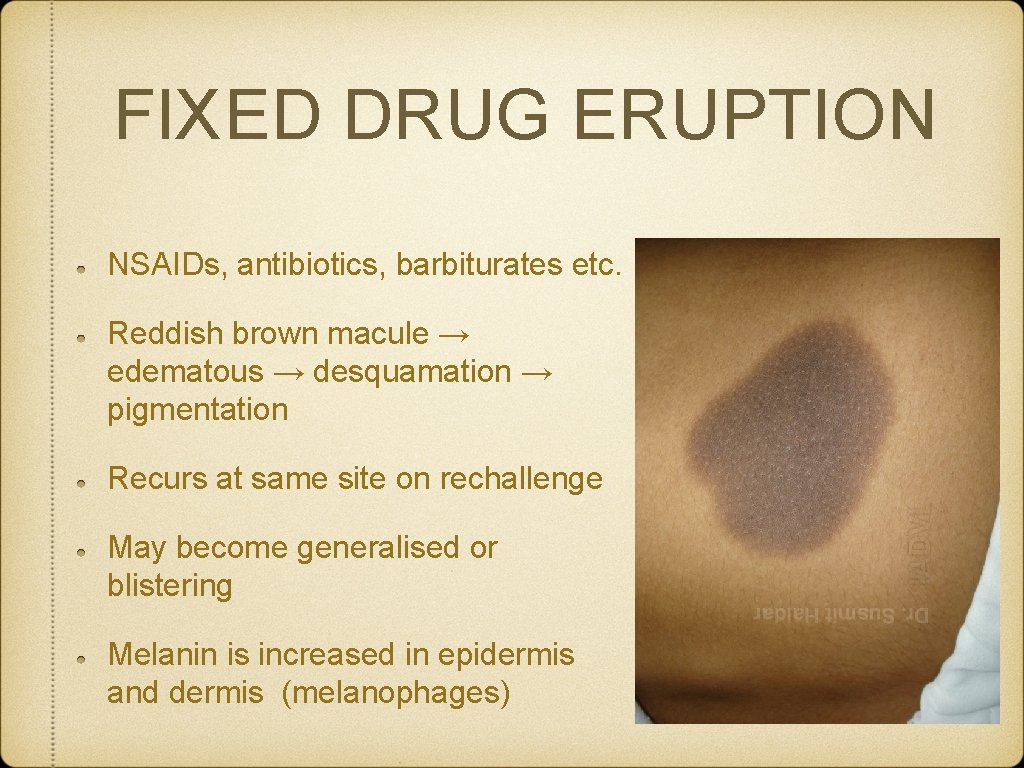
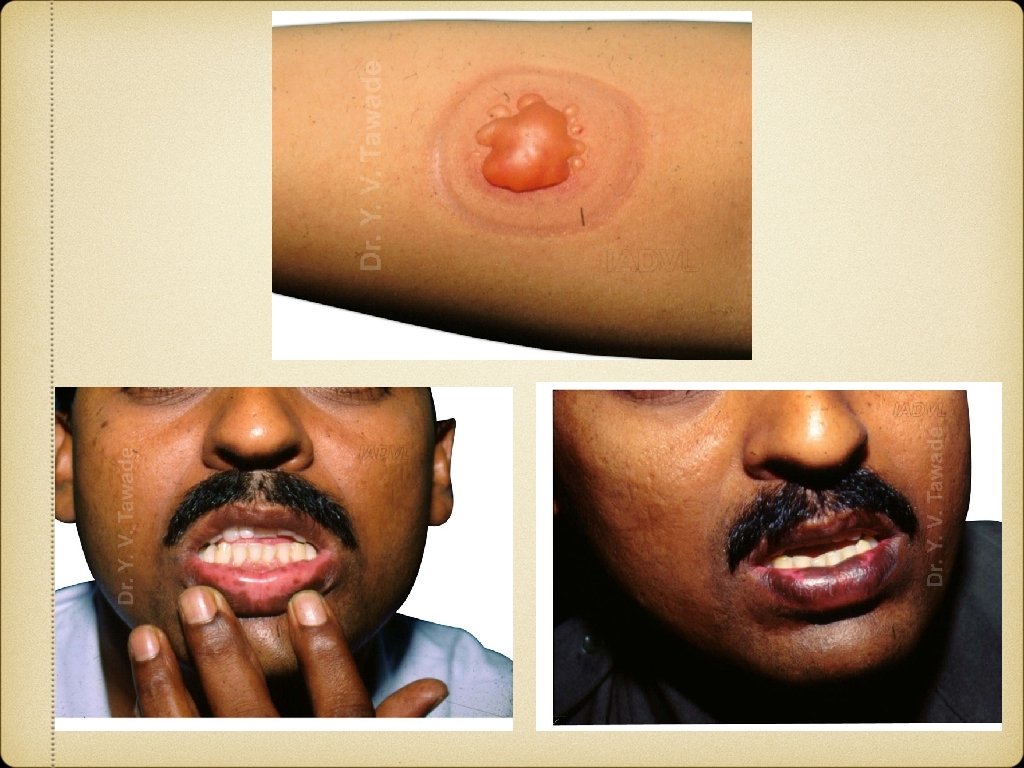
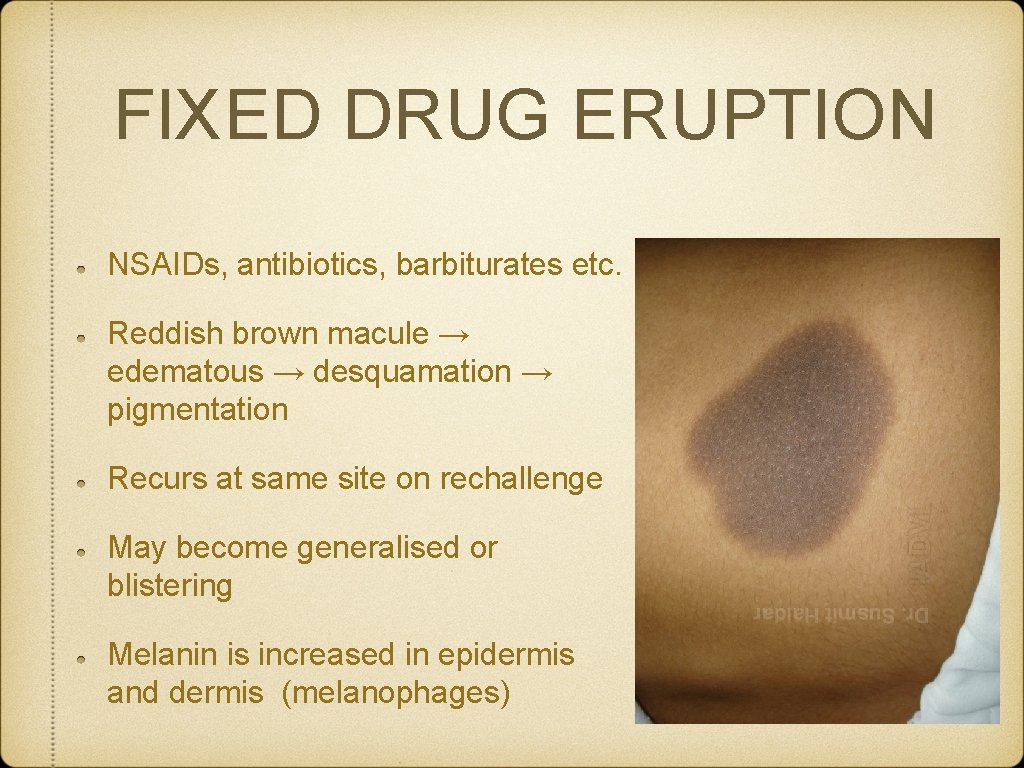
FIXED DRUG ERUPTION NSAIDs, antibiotics, barbiturates etc. Reddish brown macule → edematous → desquamation → pigmentation Recurs at same site on rechallenge May become generalised or blistering Melanin is increased in epidermis and dermis (melanophages)
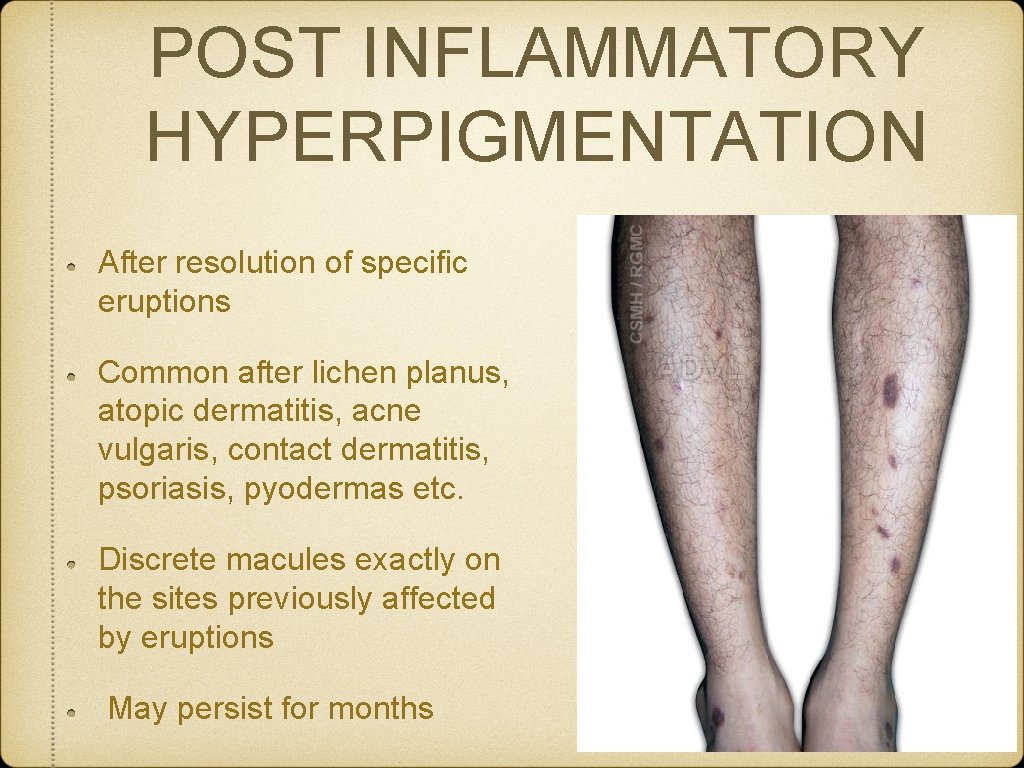
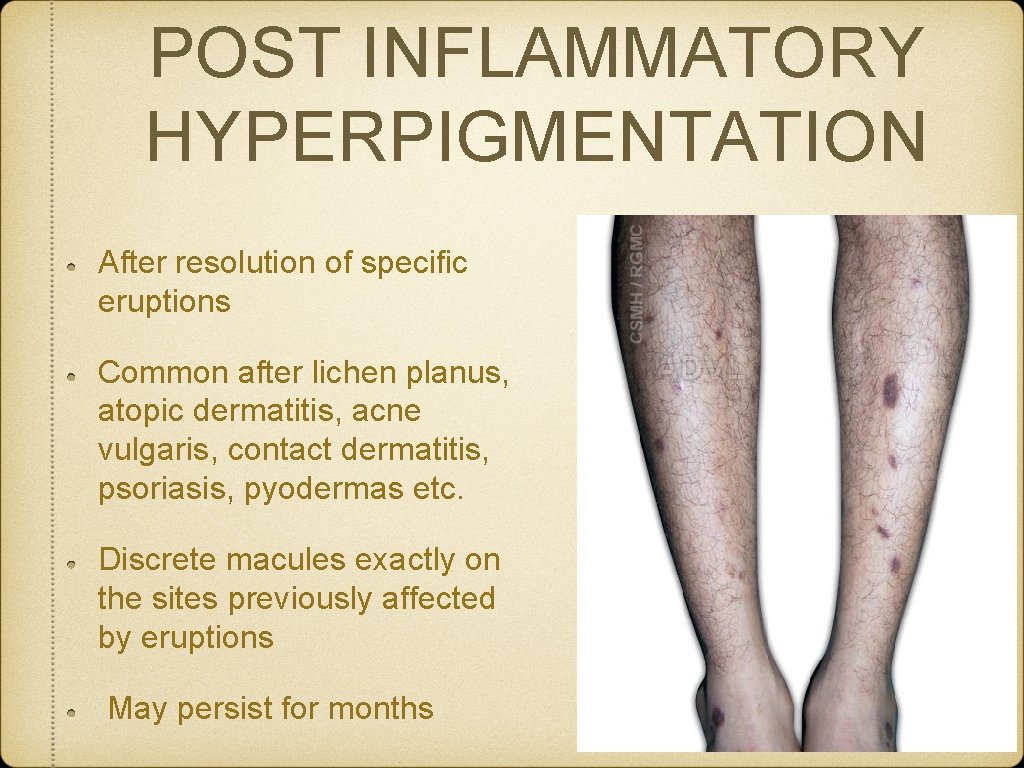
POST INFLAMMATORY HYPERPIGMENTATION After resolution of specific eruptions Common after lichen planus, atopic dermatitis, acne vulgaris, contact dermatitis, psoriasis, pyodermas etc. Discrete macules exactly on the sites previously affected by eruptions May persist for months

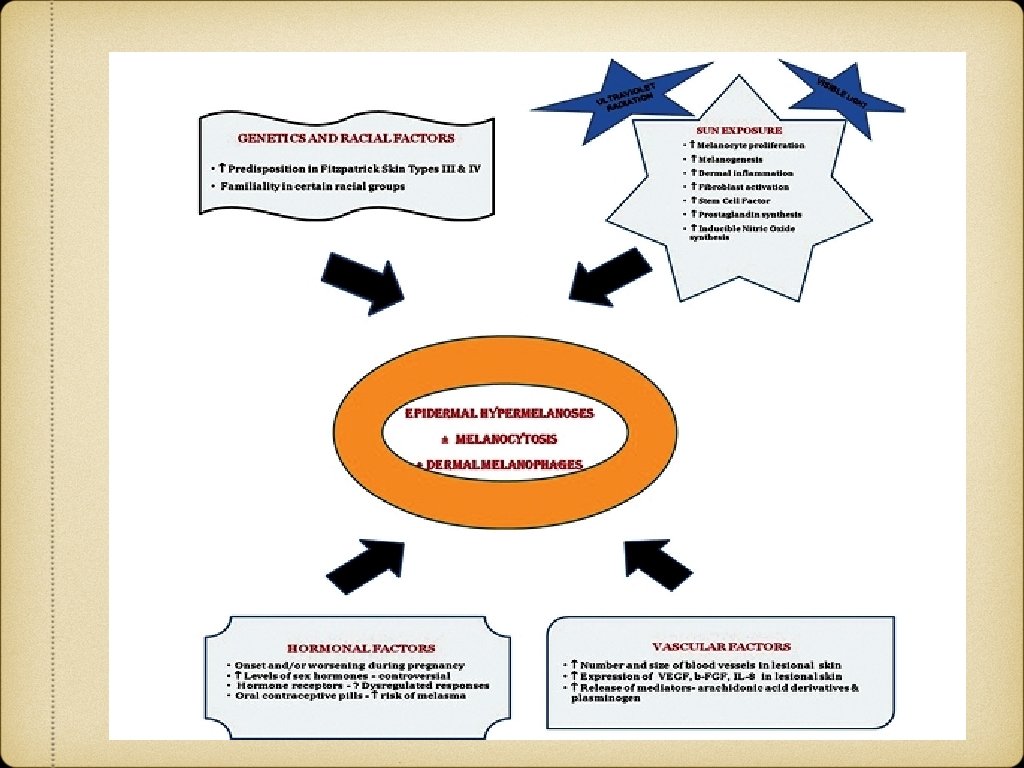
MELASMA Greek “melas” = black, “chloazein” (green). Acquired hypermelanosis of the sun exposed skin. M: F=1: 9 Much more common in constitutionally darker skin types Most common pigmentary disorder among Indians
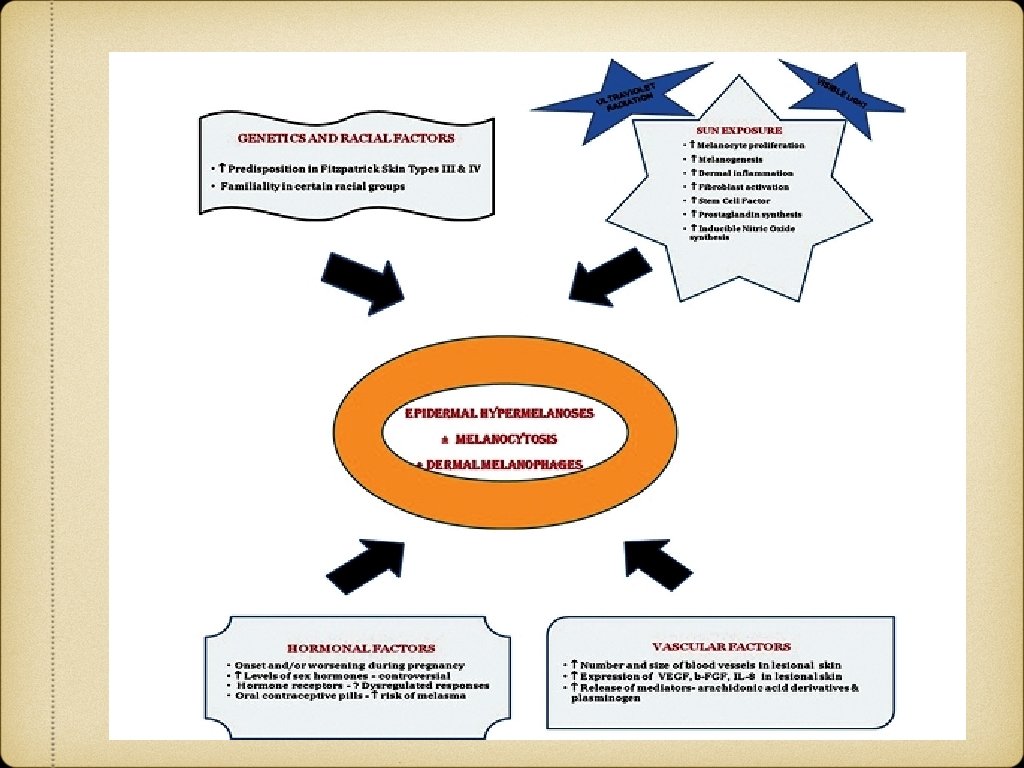
Clinical Features Presents as symmetric, hyperpigmented macules having irregular, serrated, and geographic borders. Distribution: Centrofacial (63%), Malar (21%), Mandibular (16%) Woods lamp examination: Epidermal, Dermal, Mixed and Indeterminate. Natural history: Transient, Permanent

Treatment Sun protection Topicals: Hydroquinone, Retinoids, Steroids, Glycolic acid, Kojic acid, Arbutin etc Systemic agents: Glutathione, Tranexemic acid, Vitamin A, C, E Chemical peels Lasers
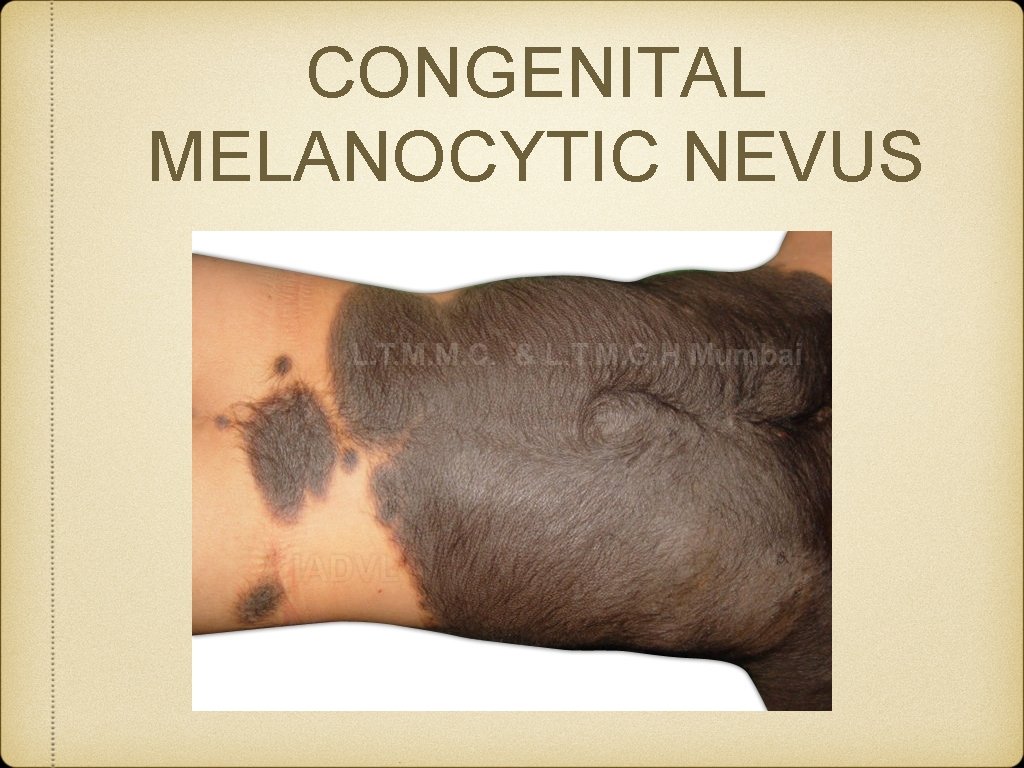
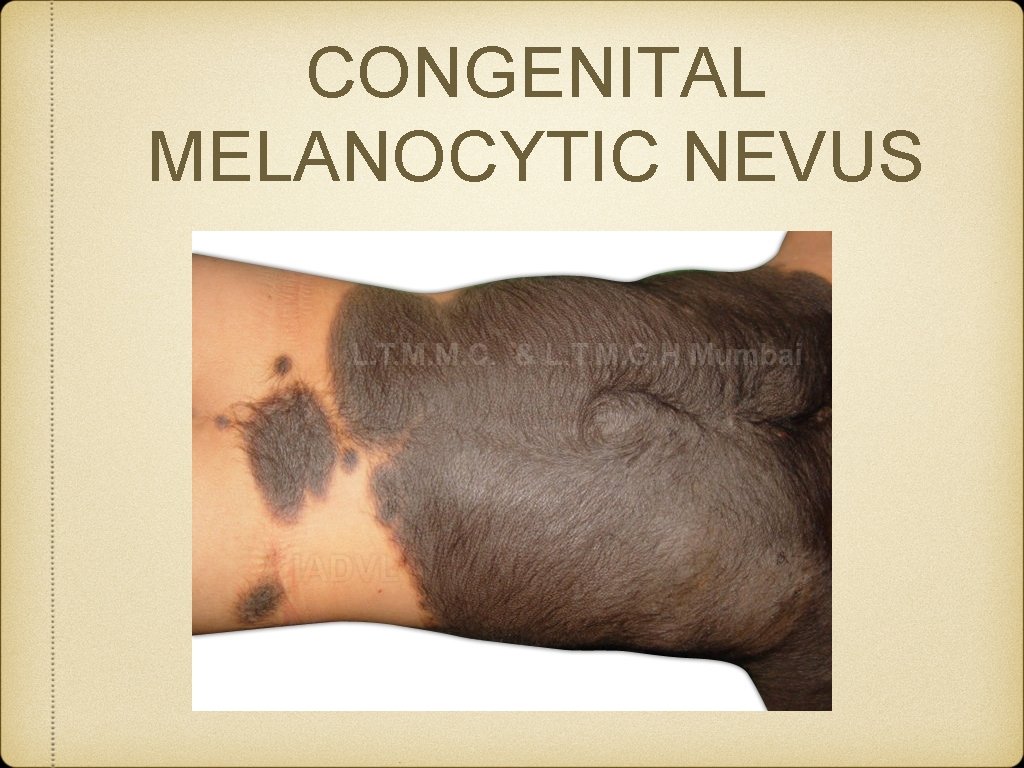
CONGENITAL MELANOCYTIC NEVUS
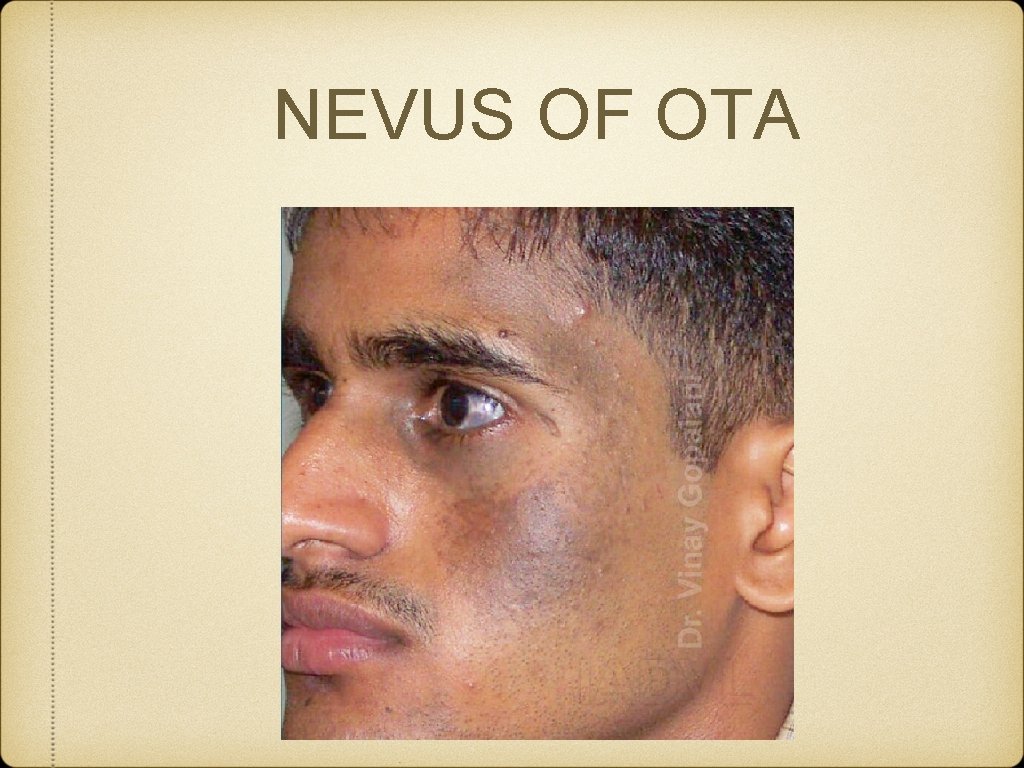
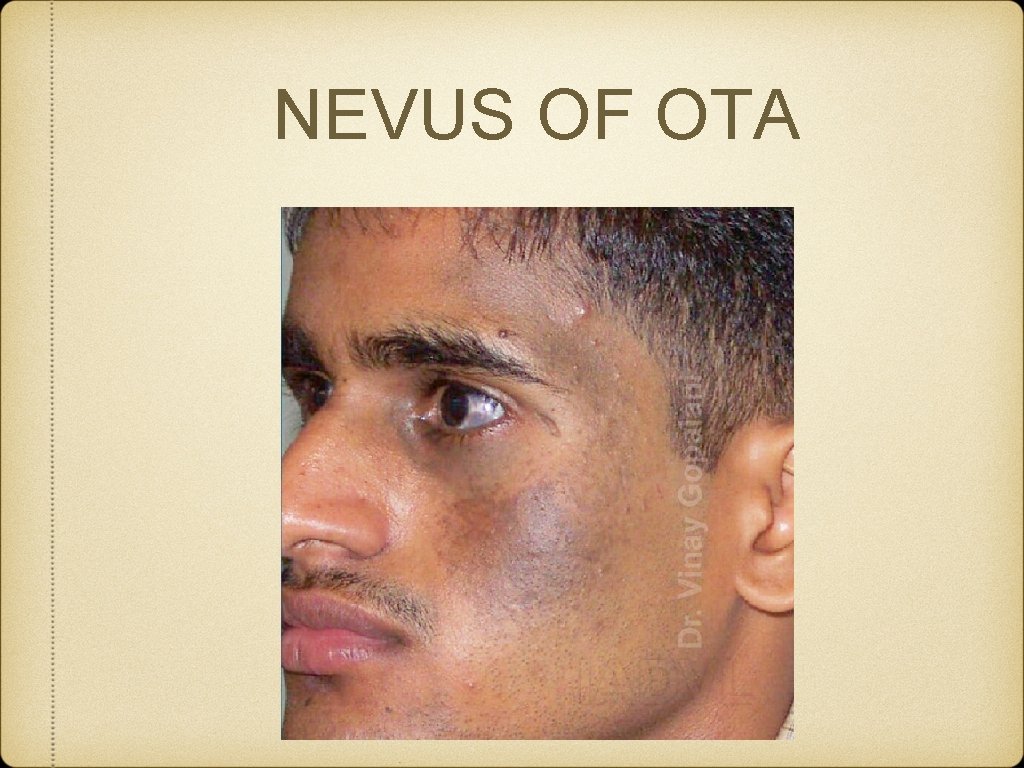
NEVUS OF OTA
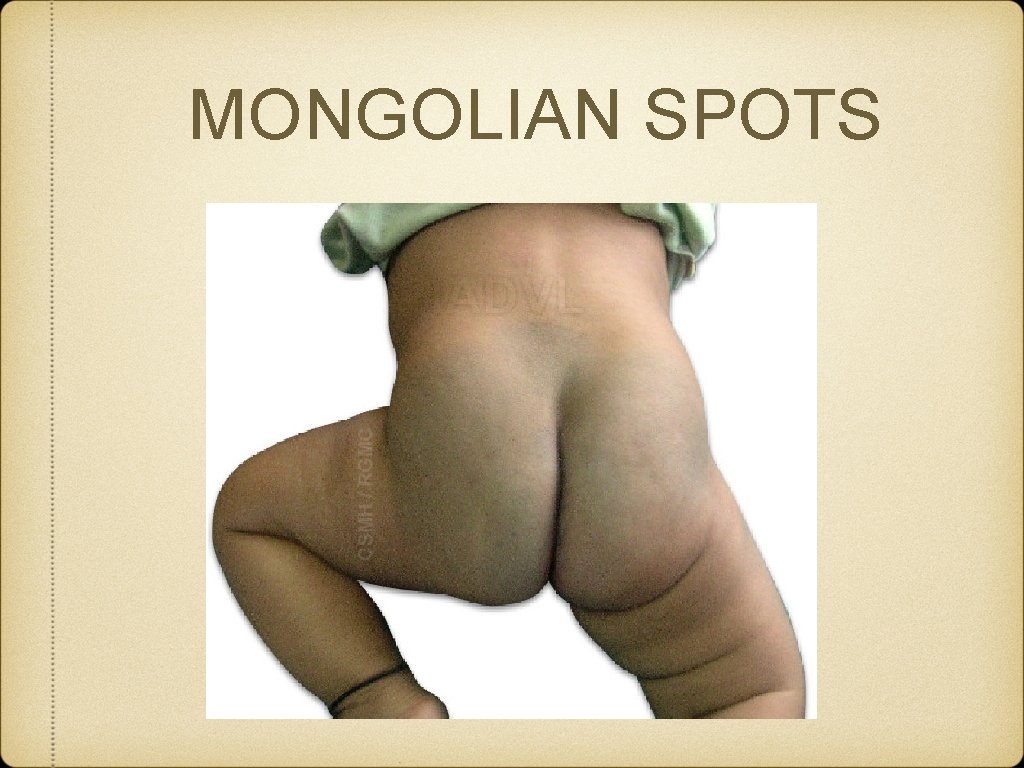
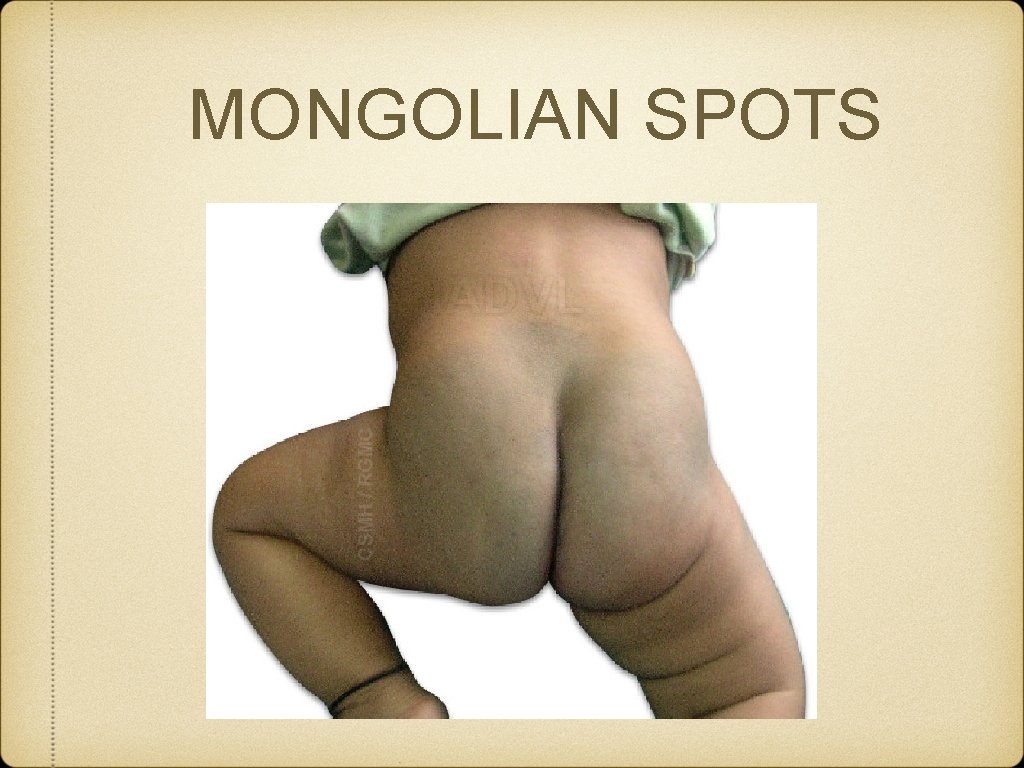
MONGOLIAN SPOTS
 Skin pigmentation
Skin pigmentation Elsevier
Elsevier Contoh soal kkpmt
Contoh soal kkpmt Define a primary skin lesion and list three types
Define a primary skin lesion and list three types Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Kode icd 10 iritasi mata
Kode icd 10 iritasi mata Stratum granulosum
Stratum granulosum Thin skin vs thick skin
Thin skin vs thick skin Chapter 23 milady pdf
Chapter 23 milady pdf Incomplete dominance traits in humans
Incomplete dominance traits in humans Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Hệ hô hấp
Hệ hô hấp Tư thế ngồi viết
Tư thế ngồi viết Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Tư thế worm breton là gì
Tư thế worm breton là gì ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Thẻ vin
Thẻ vin Gấu đi như thế nào
Gấu đi như thế nào Thể thơ truyền thống
Thể thơ truyền thống Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Thế nào là giọng cùng tên
Thế nào là giọng cùng tên 101012 bằng
101012 bằng Chúa sống lại
Chúa sống lại Lời thề hippocrates
Lời thề hippocrates Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Bổ thể
Bổ thể Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể độ dài liên kết
độ dài liên kết Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi điện thế nghỉ
điện thế nghỉ Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ