Histology of the Skin Kelli A Hutchens MD
- Slides: 23
Histology of the Skin Kelli A. Hutchens, MD, FCAP Director of Dermatopathology Assistant Professor Loyola University Medical Center Assistant Director of Mechanisms of Human Disease Loyola Stritch School of Medicine
• • Objectives Identify the epidermis, and subcutis of the skin Name and label the layers five layers of the epidermis Compare and contrast the anatomic and histologic differences between thick and thin skin Identify (when possible) / or know the location of the following cells: – – • Describe the general function and location of the following components of the dermal epidermal junction and intercellular space. – – – • • Keratinocyte Melanoycte Merkel cell Langerhan cell Hemidesmosomes Basement membrane Basal layer keratinocytes Anchoring fibrils Desmosomes Name and identify the two regions of the dermis Identify and classify the following: – Eccrine gland – Sebaceous gland – Apocrine gland • Compare and contrast the histologic appearance, function, and location of Pacinian corpuscles versus Meissner’s corpuscles.
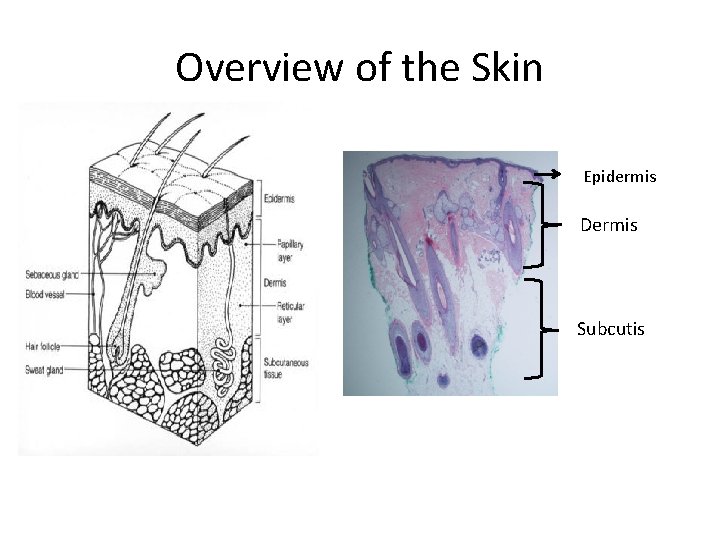
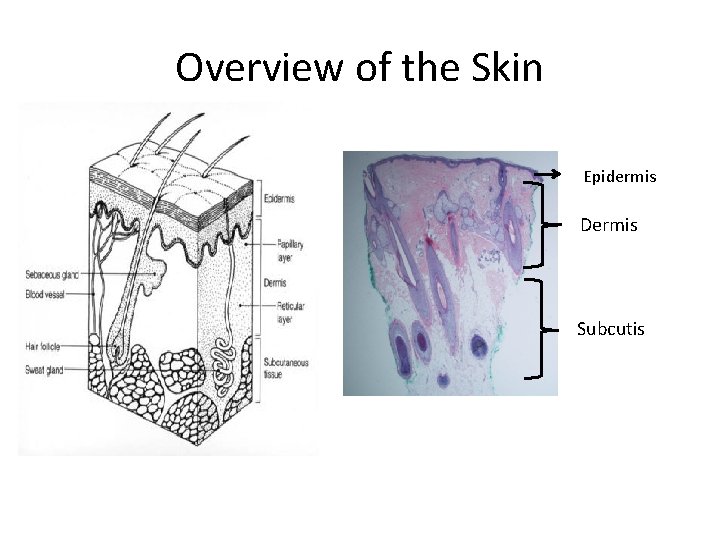
Overview of the Skin Epidermis Dermis Subcutis
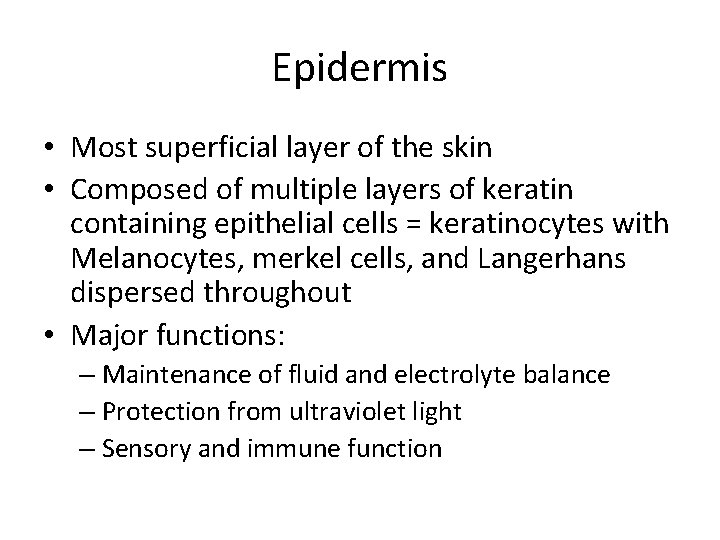
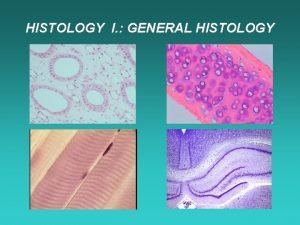
Epidermis • Most superficial layer of the skin • Composed of multiple layers of keratin containing epithelial cells = keratinocytes with Melanocytes, merkel cells, and Langerhans dispersed throughout • Major functions: – Maintenance of fluid and electrolyte balance – Protection from ultraviolet light – Sensory and immune function
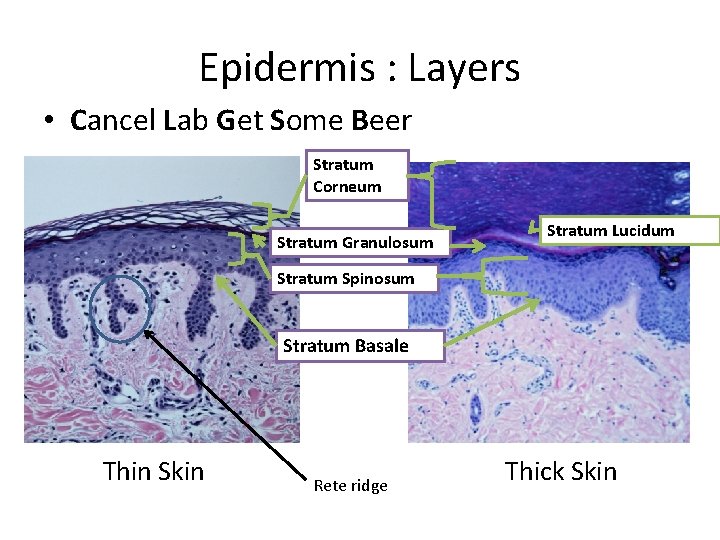
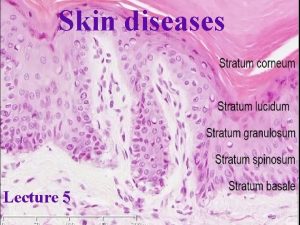
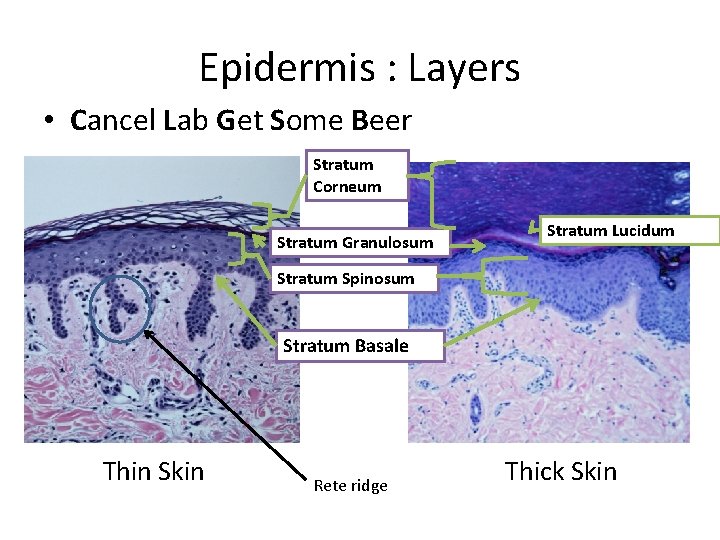
Epidermis : Layers • Cancel Lab Get Some Beer Stratum Corneum Stratum Granulosum Stratum Lucidum Stratum Spinosum Stratum Basale Thin Skin Rete ridge Thick Skin
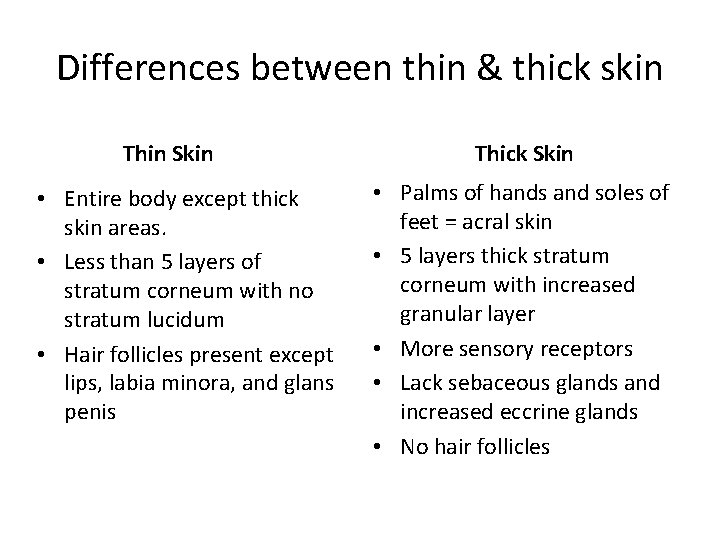
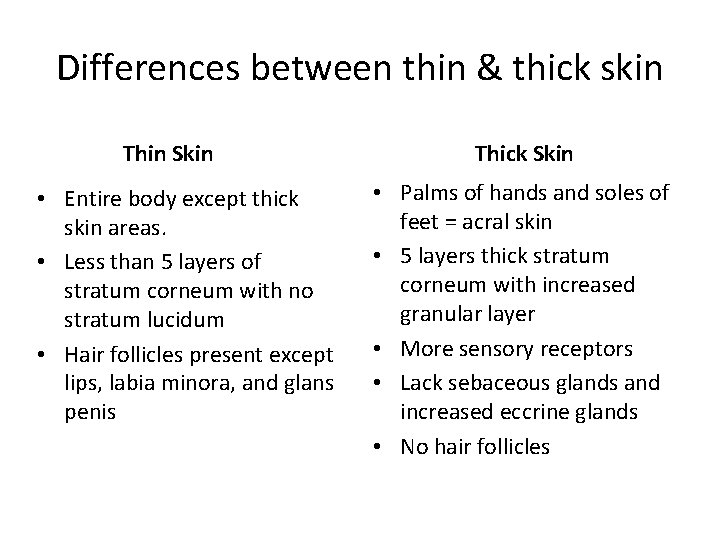
Differences between thin & thick skin Thin Skin • Entire body except thick skin areas. • Less than 5 layers of stratum corneum with no stratum lucidum • Hair follicles present except lips, labia minora, and glans penis Thick Skin • Palms of hands and soles of feet = acral skin • 5 layers thick stratum corneum with increased granular layer • More sensory receptors • Lack sebaceous glands and increased eccrine glands • No hair follicles
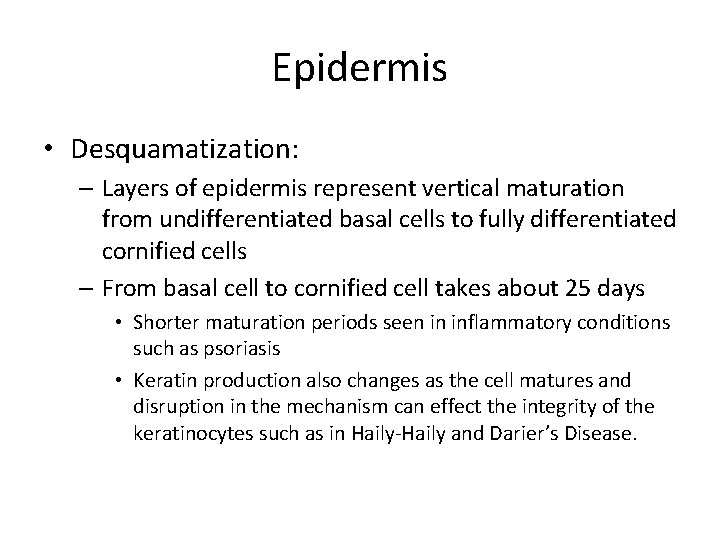
Epidermis • Desquamatization: – Layers of epidermis represent vertical maturation from undifferentiated basal cells to fully differentiated cornified cells – From basal cell to cornified cell takes about 25 days • Shorter maturation periods seen in inflammatory conditions such as psoriasis • Keratin production also changes as the cell matures and disruption in the mechanism can effect the integrity of the keratinocytes such as in Haily-Haily and Darier’s Disease.
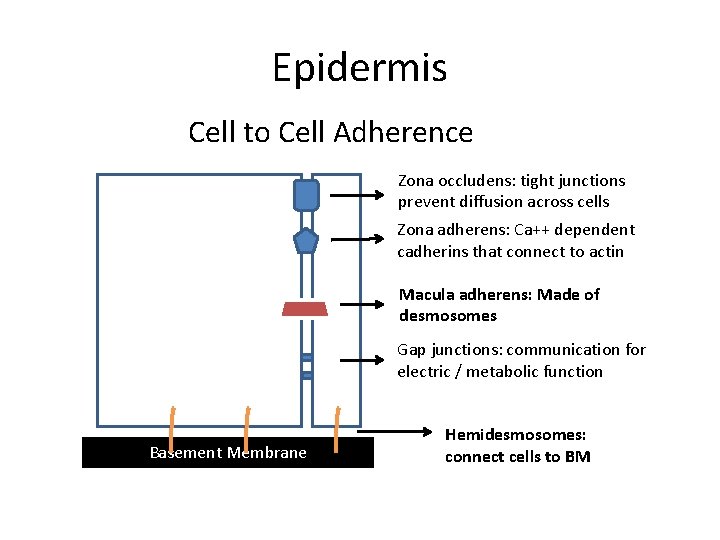
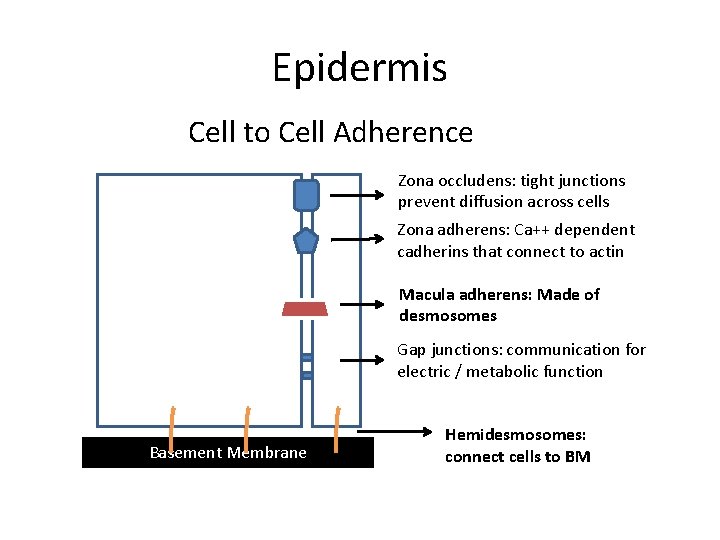
Epidermis Cell to Cell Adherence Zona occludens: tight junctions prevent diffusion across cells Zona adherens: Ca++ dependent cadherins that connect to actin Macula adherens: Made of desmosomes Gap junctions: communication for electric / metabolic function Basement Membrane Hemidesmosomes: connect cells to BM
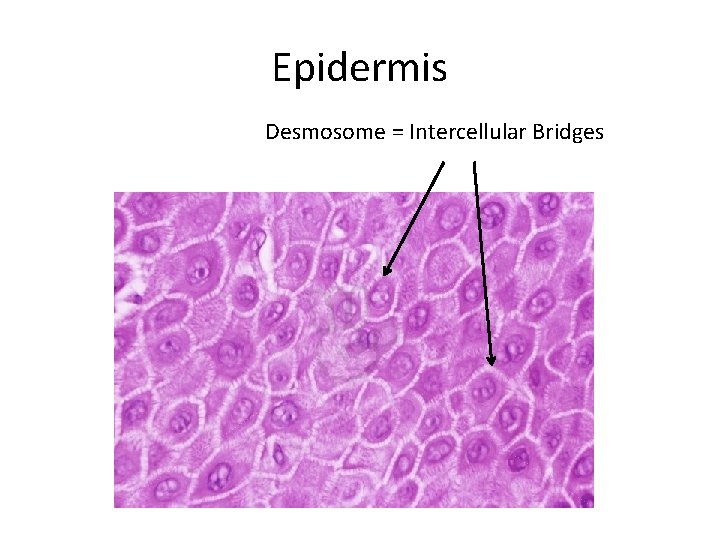
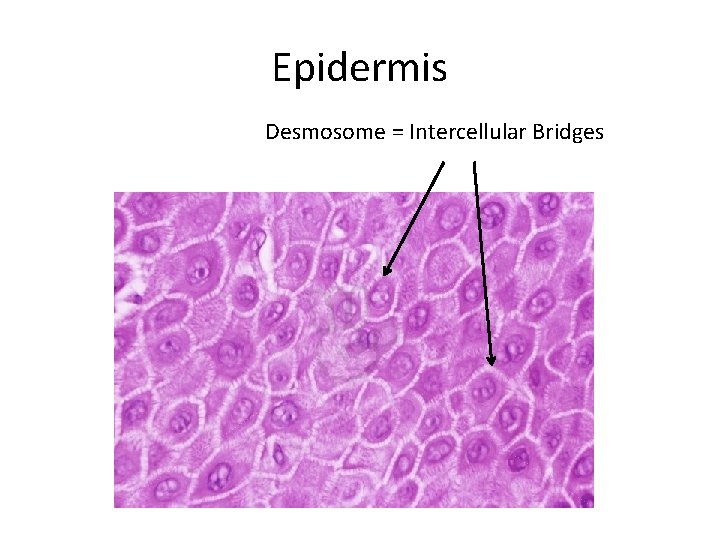
Epidermis Desmosome = Intercellular Bridges
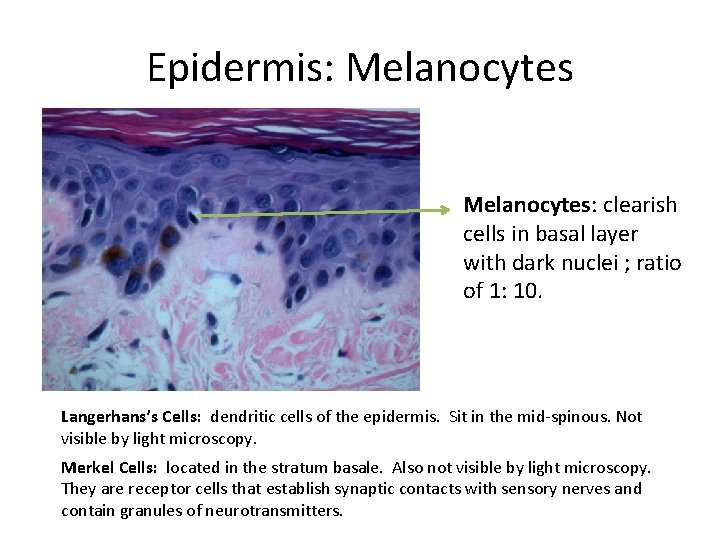
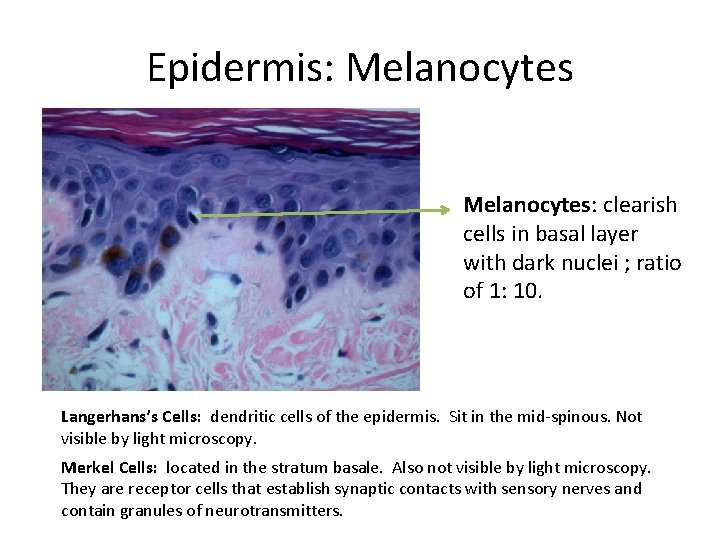
Epidermis: Melanocytes: clearish cells in basal layer with dark nuclei ; ratio of 1: 10. Langerhans’s Cells: dendritic cells of the epidermis. Sit in the mid-spinous. Not visible by light microscopy. Merkel Cells: located in the stratum basale. Also not visible by light microscopy. They are receptor cells that establish synaptic contacts with sensory nerves and contain granules of neurotransmitters.
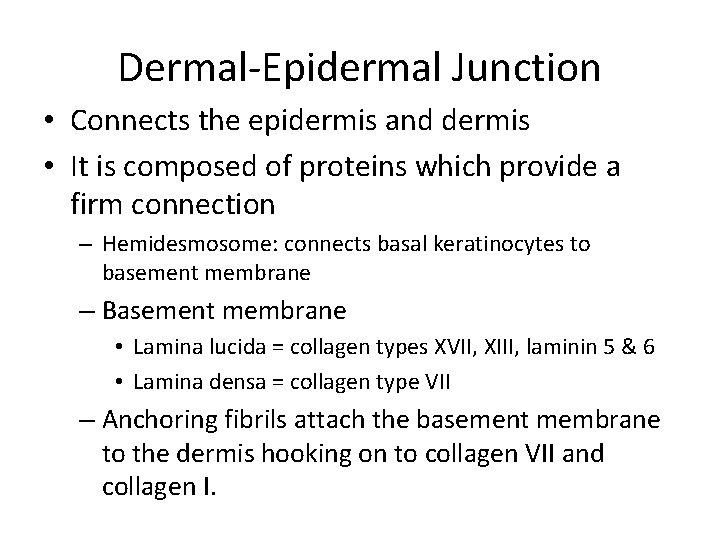
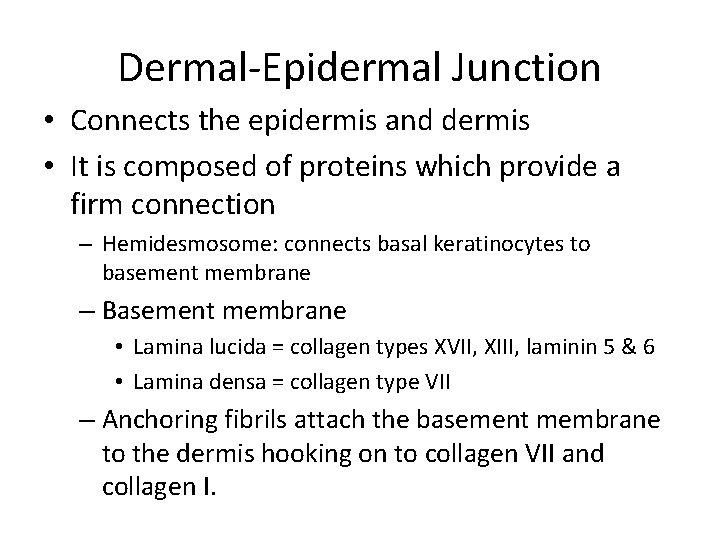
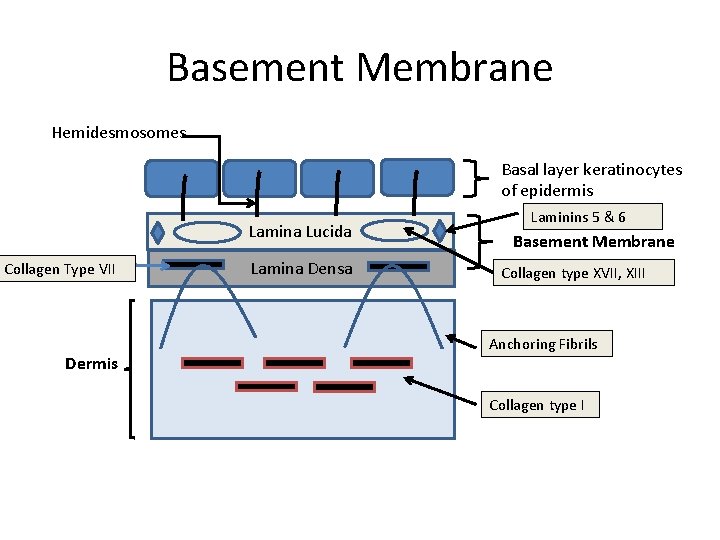
Dermal-Epidermal Junction • Connects the epidermis and dermis • It is composed of proteins which provide a firm connection – Hemidesmosome: connects basal keratinocytes to basement membrane – Basement membrane • Lamina lucida = collagen types XVII, XIII, laminin 5 & 6 • Lamina densa = collagen type VII – Anchoring fibrils attach the basement membrane to the dermis hooking on to collagen VII and collagen I.
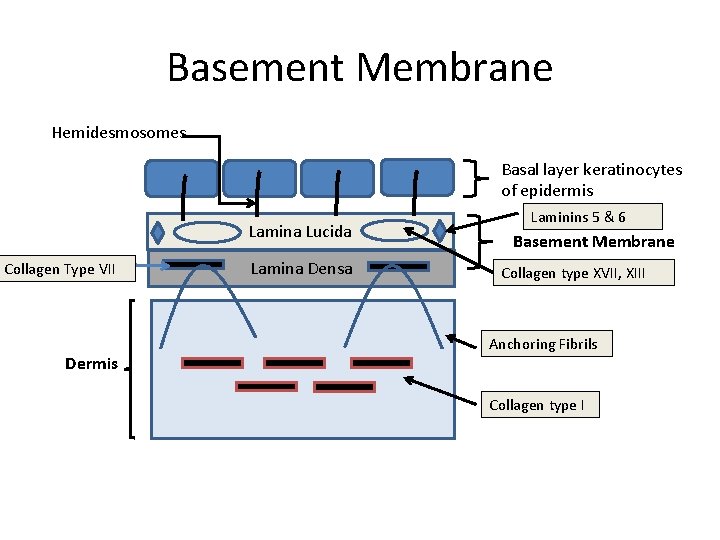
Basement Membrane Hemidesmosomes Basal layer keratinocytes of epidermis Lamina Lucida Collagen Type VII Dermis Lamina Densa Laminins 5 & 6 Basement Membrane Collagen type XVII, XIII Anchoring Fibrils Collagen type I
Dermis • Everything below the dermal epidermal junction / basement membrane – Connective tissue layer with contains blood vessels, nerves, sensory receptors, adnexal structures
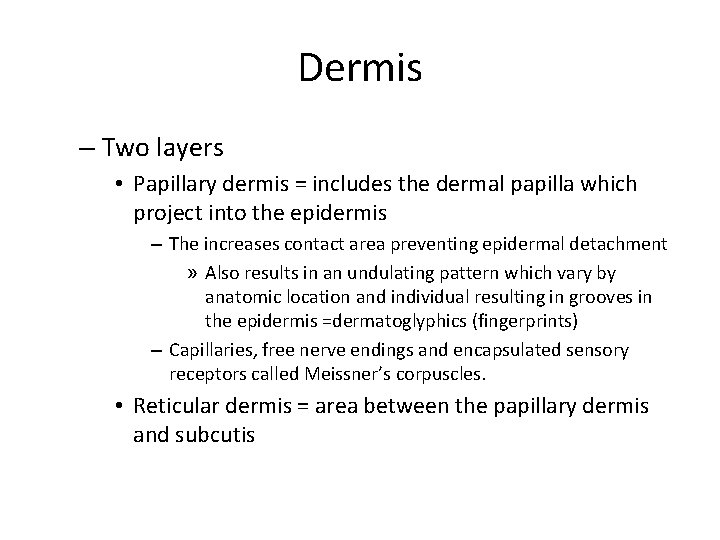
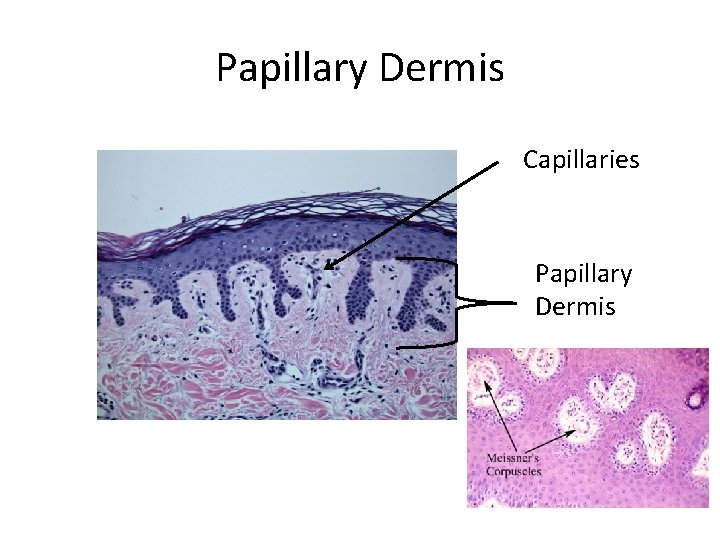
Dermis – Two layers • Papillary dermis = includes the dermal papilla which project into the epidermis – The increases contact area preventing epidermal detachment » Also results in an undulating pattern which vary by anatomic location and individual resulting in grooves in the epidermis =dermatoglyphics (fingerprints) – Capillaries, free nerve endings and encapsulated sensory receptors called Meissner’s corpuscles. • Reticular dermis = area between the papillary dermis and subcutis
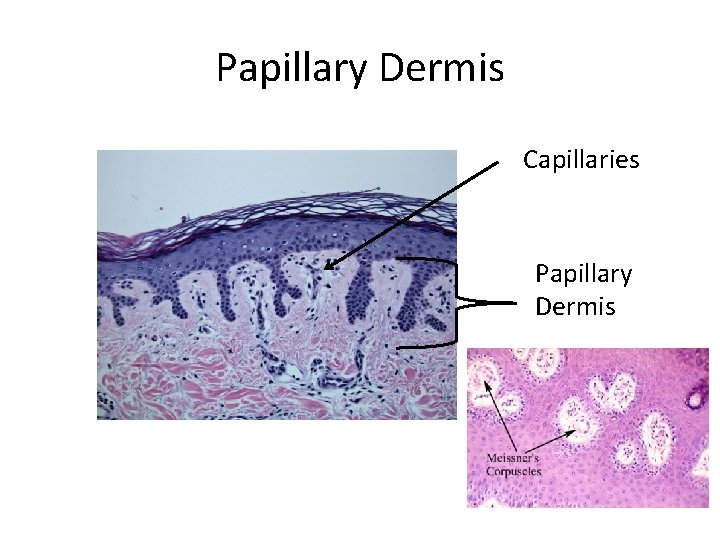
Papillary Dermis Capillaries Papillary Dermis
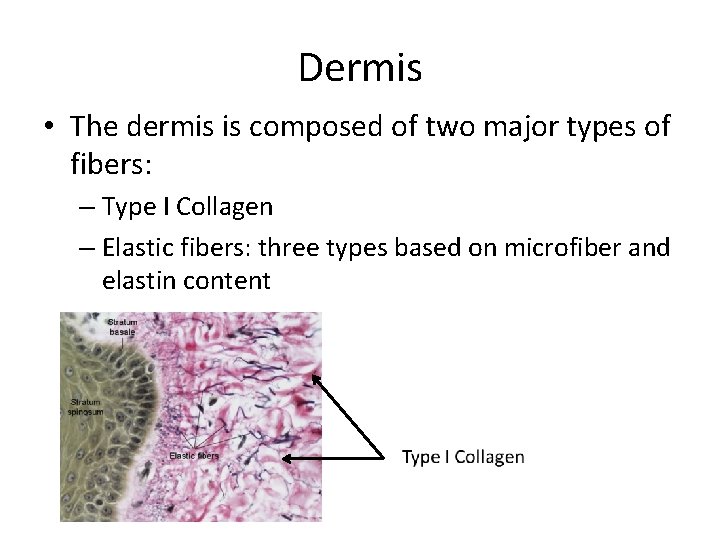
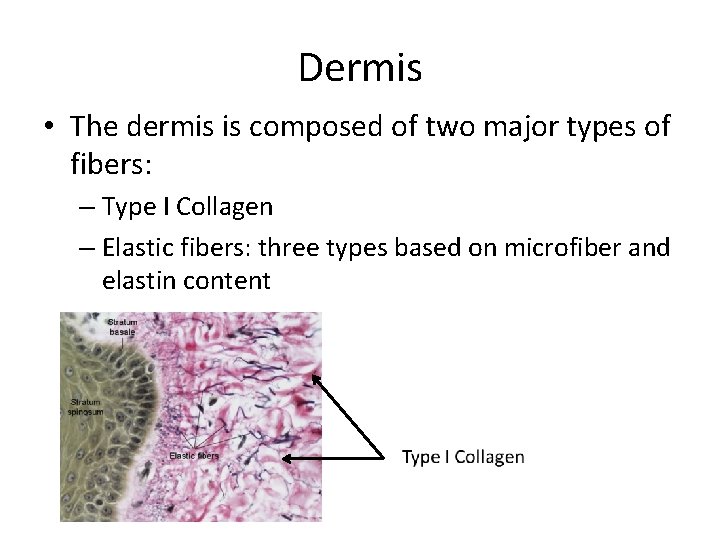
Dermis • The dermis is composed of two major types of fibers: – Type I Collagen – Elastic fibers: three types based on microfiber and elastin content
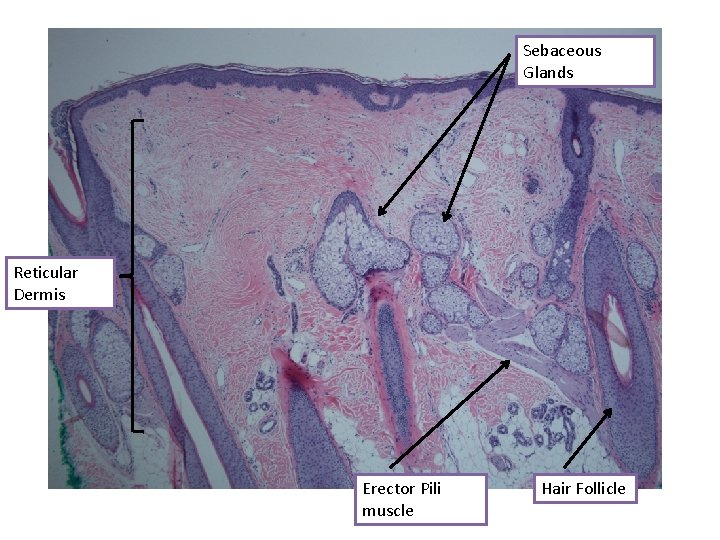
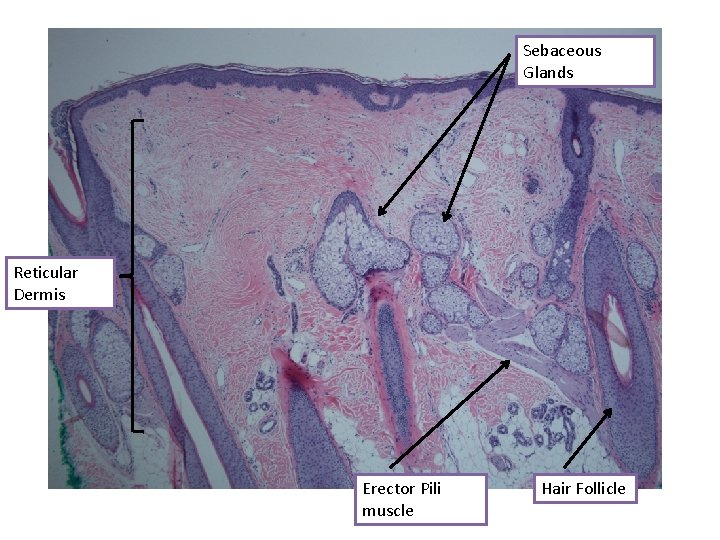
Sebaceous Glands Reticular Dermis Erector Pili muscle Hair Follicle
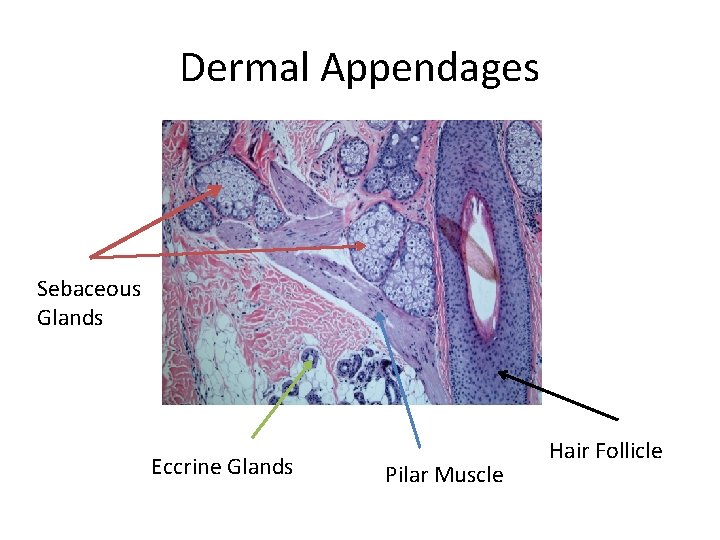
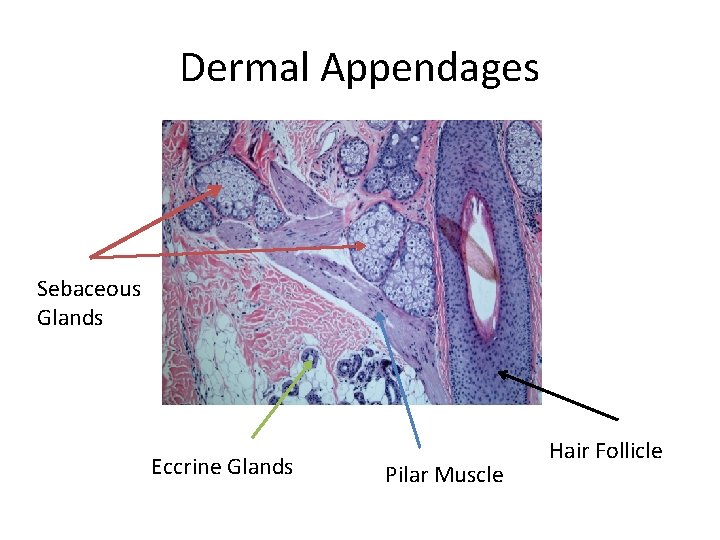
Dermal Appendages Sebaceous Glands Eccrine Glands Pilar Muscle Hair Follicle
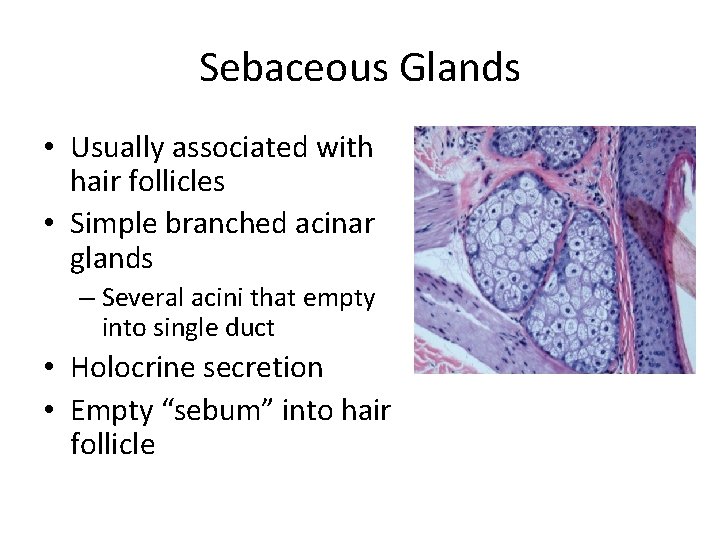
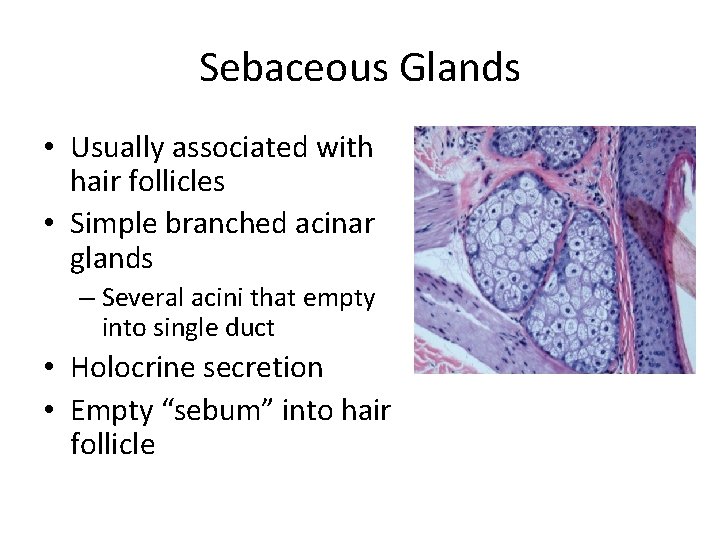
Sebaceous Glands • Usually associated with hair follicles • Simple branched acinar glands – Several acini that empty into single duct • Holocrine secretion • Empty “sebum” into hair follicle
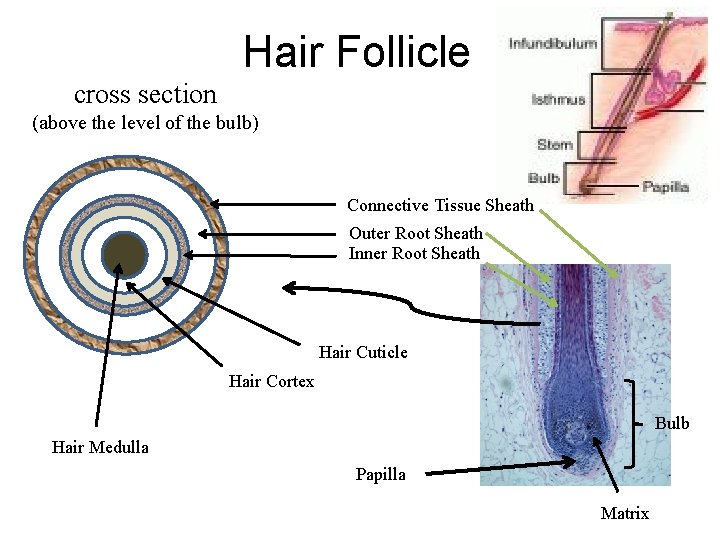
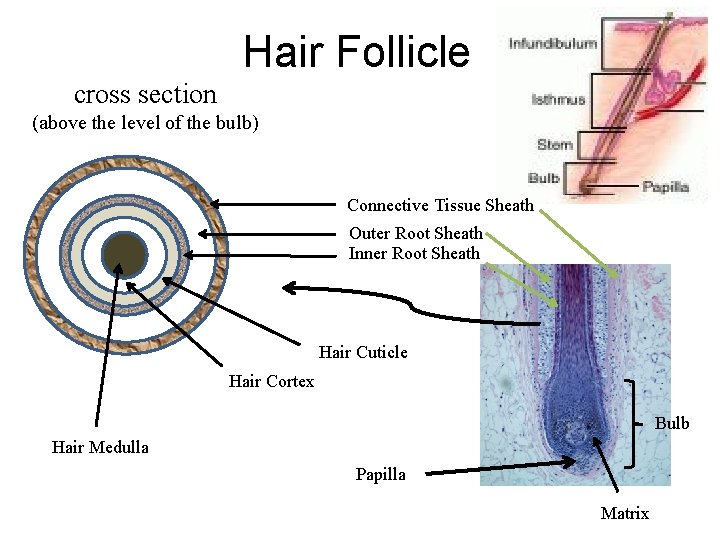
Hair Follicle cross section (above the level of the bulb) Connective Tissue Sheath Outer Root Sheath Inner Root Sheath Hair Cuticle Hair Cortex Bulb Hair Medulla Papilla Matrix
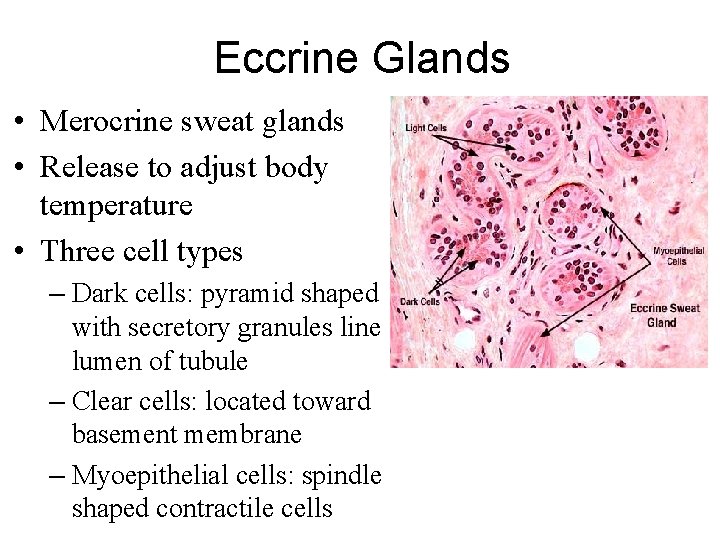
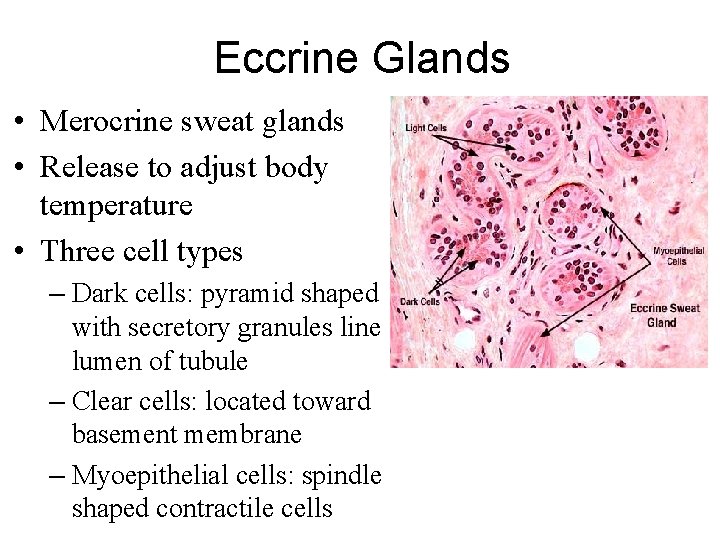
Eccrine Glands • Merocrine sweat glands • Release to adjust body temperature • Three cell types – Dark cells: pyramid shaped with secretory granules line lumen of tubule – Clear cells: located toward basement membrane – Myoepithelial cells: spindle shaped contractile cells
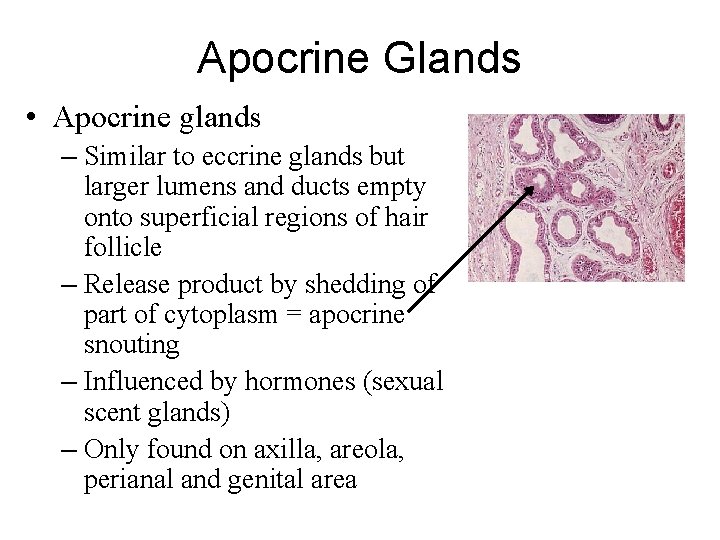
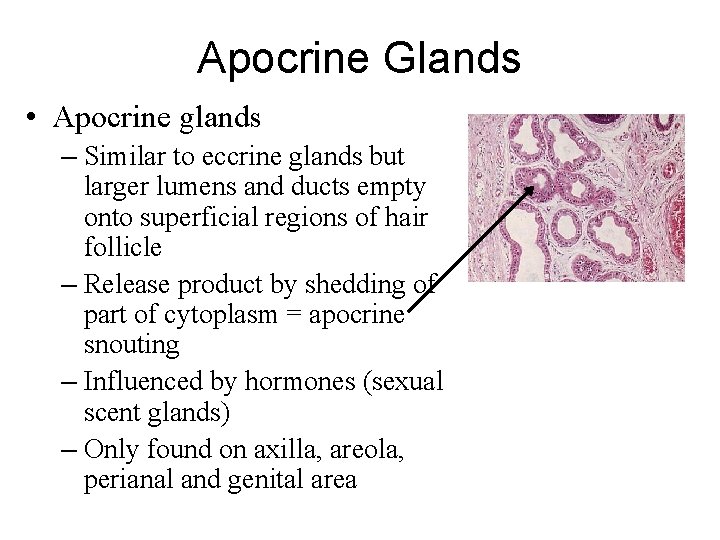
Apocrine Glands • Apocrine glands – Similar to eccrine glands but larger lumens and ducts empty onto superficial regions of hair follicle – Release product by shedding of part of cytoplasm = apocrine snouting – Influenced by hormones (sexual scent glands) – Only found on axilla, areola, perianal and genital area
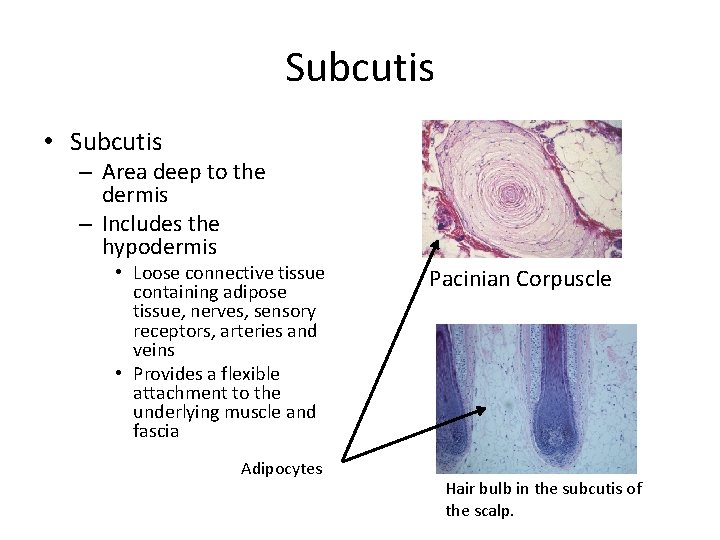
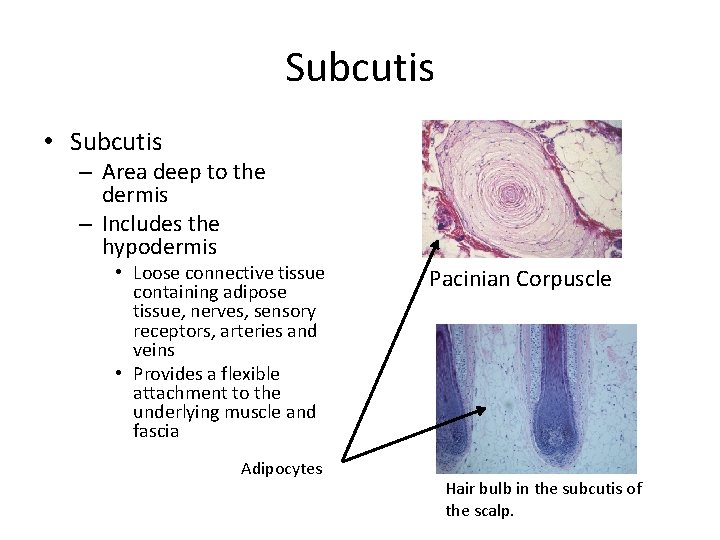
Subcutis • Subcutis – Area deep to the dermis – Includes the hypodermis • Loose connective tissue containing adipose tissue, nerves, sensory receptors, arteries and veins • Provides a flexible attachment to the underlying muscle and fascia Adipocytes Pacinian Corpuscle Hair bulb in the subcutis of the scalp.
 Troy hutchens
Troy hutchens Hal hutchens
Hal hutchens Which is the largest organ in our body? *
Which is the largest organ in our body? * Thin skin histology
Thin skin histology Kelli kiipus
Kelli kiipus Kelli lehto
Kelli lehto Kelli lehto
Kelli lehto Taavi lehto
Taavi lehto Cuinvolved
Cuinvolved Noortegarantii tugisüsteem
Noortegarantii tugisüsteem Kelli phillips pictures
Kelli phillips pictures Thin skin vs thick skin
Thin skin vs thick skin Chapter 23 milady pdf
Chapter 23 milady pdf Stratum lucidum
Stratum lucidum Vẽ hình chiếu vuông góc của vật thể sau
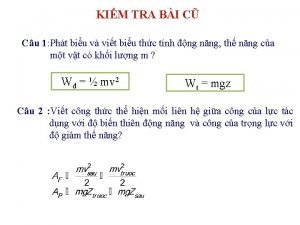
Vẽ hình chiếu vuông góc của vật thể sau Công của trọng lực
Công của trọng lực Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể độ dài liên kết
độ dài liên kết Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ