SEPSIS WITH MULTI ORGAN FAILURE DR SUDHA RANI





- Slides: 82
SEPSIS WITH MULTI ORGAN FAILURE DR. SUDHA RANI PANEM MODERATOR: DR. B. S. K. PRUSTI
� Sepsis, a syndrome of physiologic, pathologic, and biochemical abnormalities induced by infection, is a major public health concern. � A 1991 consensus conference developed initial definitions that focused on thenprevailing view that sepsis resulted from a host’s systemic inflammatory response syndrome (SIRS) to infection.
� 1. Inflammatory response starts with recognition of pathogen molecular components by receptors on cells of the innate immune system. � 2. Innate immune cell members consist of neutrophils, macrophages, monocytes, basophils, e osinophils, natural killer cells, mast cells, dendritic cells and platelets. � 3. Pathogen-inducing components capable of triggering an immune response are numerous and include lipopolysaccharides(LPS)from gram – negative bacteria; lipoteicoic acid from grampositive bacteria , and flagellin.
� INFECTION � 1. Sepsis is an overwhelming and complicated proinflammatory response to infection. � 2. Inciting organisms have changed in time. Change is connected to drug resistance. � 3. Gram negative and Gram positive organisms are each separately linked to 25% of sepsisrelated infections. � 4. Mixed Gram negative and Gram positive infections account for about 15% of causative infections. � 5. Fungi associated with 5%to 10% of infections.
1. TLRs are cell membrane protiens that exist to specifically recognise a variety of pathogen and tissue damage associated components. 2. TLRs –key element to initiate immune response which along with other protiens comprise a cadre known as a protien recognition receptors. 3. Activaion of TLRs leads to initiation of inflammatory cascade. This includes activation of critical trancription factor. NF-Kb. Ongoing respose is host dependent and variable.
� 1. Activation of the inflammatory cascade leads release of mediators. � 2. These encompass cytokines including interleukin-1(IL-1), IL-6, IL-8 and tumor necrosis factor. TNF-alpha. � 3. High mobility (HMGB-1)is a unique cytokine to provoke a lethal proinflammatory response. � 4. Additional mediators-patelet activating factor PAF, bradikinine, nitricoxide, and elements of complement system.
� Include vasodilatation and altered perfusion, microvascular permeability and thrombosis, myocardial depression, mitochondrial dysfunction, maladaptive use of cellular nutrients, and cellular apoptosis.
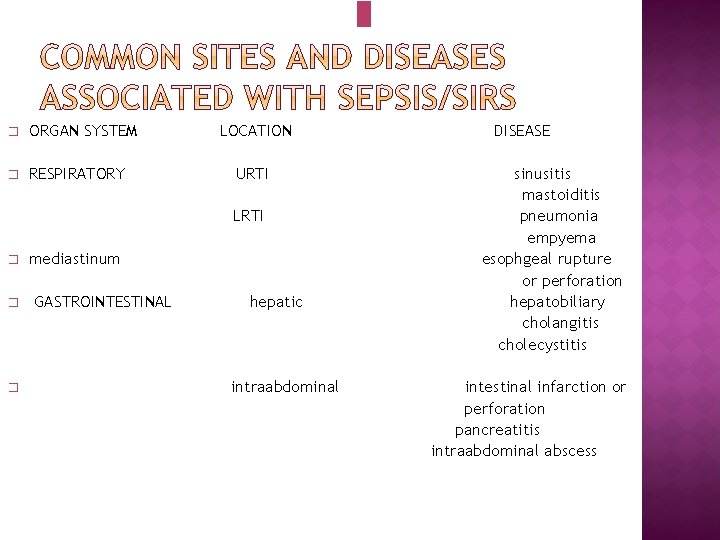
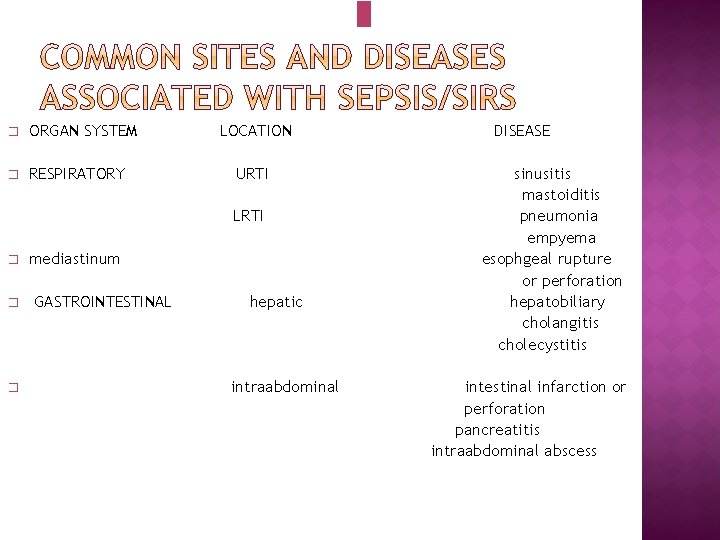
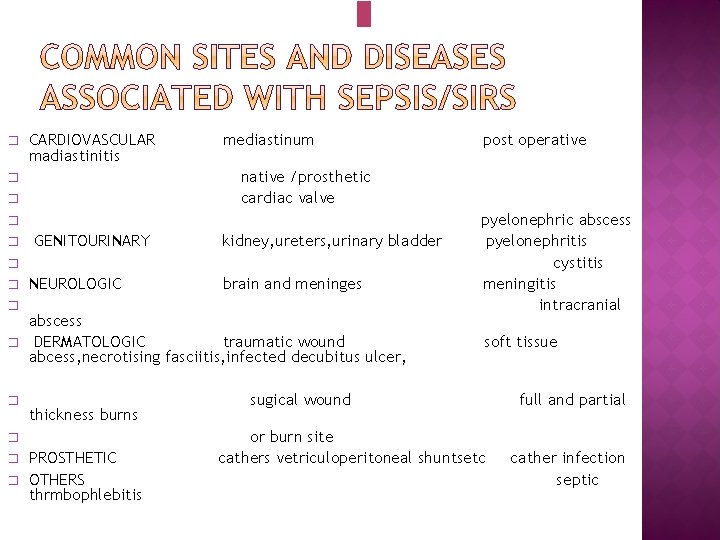
� ORGAN SYSTEM � RESPIRATORY LOCATION URTI LRTI � � � mediastinum GASTROINTESTINAL hepatic intraabdominal DISEASE sinusitis mastoiditis pneumonia empyema esophgeal rupture or perforation hepatobiliary cholangitis cholecystitis intestinal infarction or perforation pancreatitis intraabdominal abscess
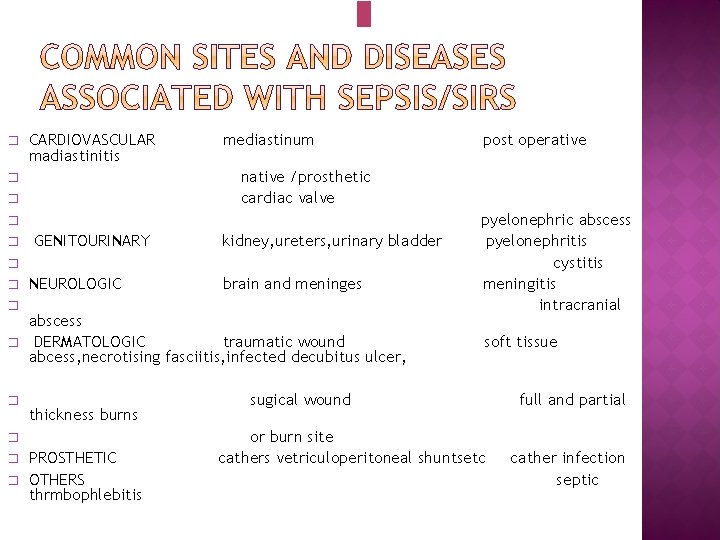
� CARDIOVASCULAR madiastinitis mediastinum native /prosthetic cardiac valve � � GENITOURINARY kidney, ureters, urinary bladder � � � NEUROLOGIC � brain and meninges abscess DERMATOLOGIC traumatic wound abcess, necrotising fasciitis, infected decubitus ulcer, thickness burns � � post operative PROSTHETIC OTHERS thrmbophlebitis pyelonephric abscess pyelonephritis cystitis meningitis intracranial soft tissue sugical wound or burn site cathers vetriculoperitoneal shuntsetc full and partial cather infection septic

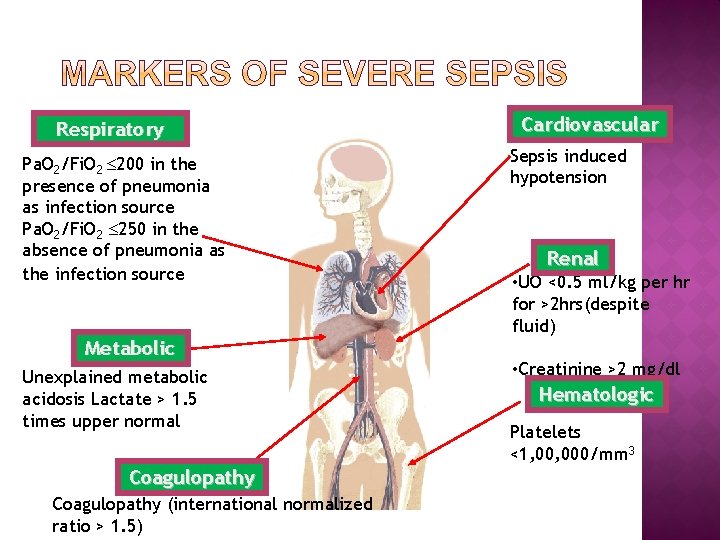
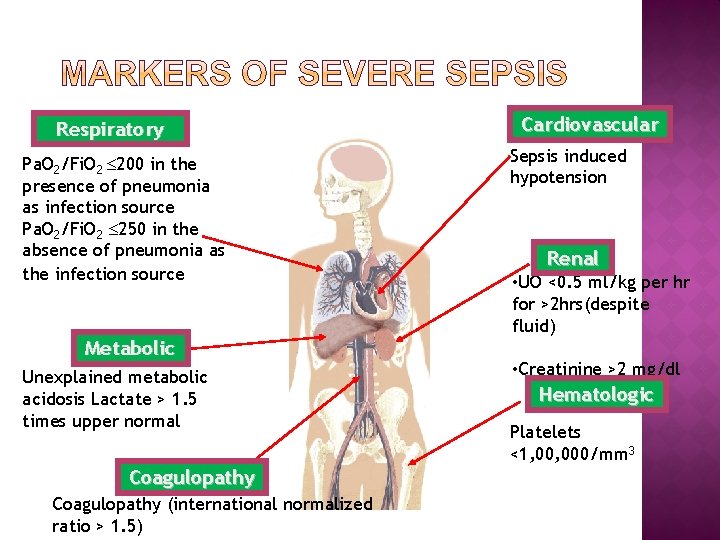
Respiratory Pa. O 2/Fi. O 2 200 in the presence of pneumonia as infection source Pa. O 2/Fi. O 2 250 in the absence of pneumonia as the infection source Metabolic Unexplained metabolic acidosis Lactate > 1. 5 times upper normal Coagulopathy (international normalized ratio > 1. 5) Cardiovascular Sepsis induced hypotension Renal • UO <0. 5 ml/kg per hr for >2 hrs(despite fluid) • Creatinine >2 mg/dl Hematologic Platelets <1, 000/mm 3
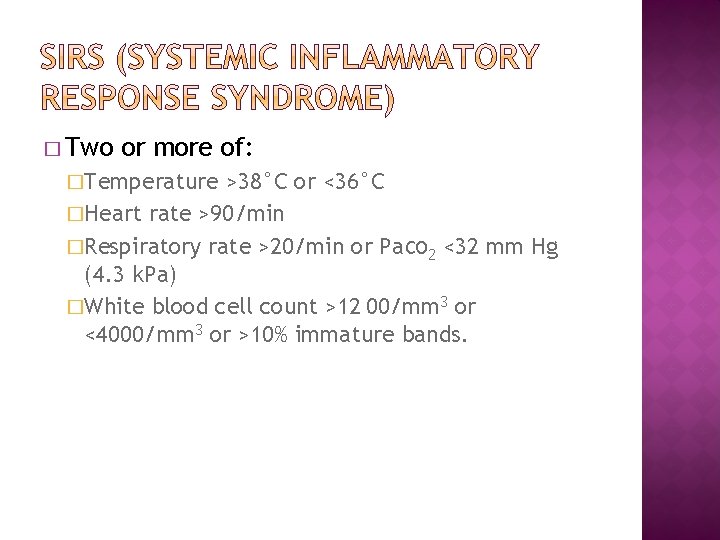
� Two or more of: �Temperature >38°C or <36°C �Heart rate >90/min �Respiratory rate >20/min or Pa. CO 2 <32 mm Hg (4. 3 k. Pa) �White blood cell count >12 00/mm 3 or <4000/mm 3 or >10% immature bands.
Sepsis complicated by organ dysfunction was termed severe sepsis, which could progress to septic shock, defined as “sepsis-induced hypotension persisting despite adequate fluid resuscitation. � A 2001 task force, recognizing limitations with these definitions, expanded the list of diagnostic criteria but did not offer alternatives because of the lack of supporting evidence. � In effect, the definitions of sepsis, septic shock, and organ dysfunction have remained largely unchanged for more than 2 decades. �
� Recognizing the need to reexamine the current definitions, 11 the European Society of Intensive Care Medicine and the Society of Critical Care Medicine convened a task force of 19 critical care, infectious disease, surgical, and pulmonary specialists in January 2014. � An expert consensus process, based on a current understanding of sepsis-induced changes in organ function, morphology, cell biology, biochemistry, immunology, and circulation (collectively referred to as pathobiology), forged agreement on updated definition(s) and the criteria to be tested in the clinical arena (content validity).
The task force recognized that sepsis is a syndrome without, at present, a validated criterion standard diagnostic test. There is currently no process to operationalize the definitions of sepsis and septic shock, a key deficit that has led to major variations in reported incidence and mortality rates. � The task force determined that there was an important need for features that can be identified and measured in individual patients and sought to provide such criteria to offer uniformity. Ideally, these clinical criteria should identify all the elements of sepsis (infection, host response, and organ dysfunction), be simple to obtain, and be available promptly and at a reasonable cost or burden. �
Furthermore, it should be possible to test the validity of these criteria with available large clinical data sets and, ultimately, prospectively. � In addition, clinical criteria should be available to provide practitioners in out-of-hospital, emergency department, and hospital ward settings with the capacity to better identify patients with suspected infection likely to progress to a life-threatening state. Such early recognition is particularly important because prompt management of septic patients may improve outcomes. 4 �
� In addition, to provide a more consistent and reproducible picture of sepsis incidence and outcomes, the task force sought to integrate the biology and clinical identification of sepsis with its epidemiology and coding.
� Improved Understanding of Sepsis Pathobiology � Sepsis is now recognized to involve early activation of both pro- and anti-inflammatory responses, along with major modifications in nonimmunologic pathways such as cardiovascular, neuronal, autonomic, hormonal, bioenergetic, metabolic, and coagulation, all of which have prognostic significance. Organ dysfunction, even when severe, is not associated with substantial cell death.
� Multichannel molecular signatures (eg, transcriptomic, metabolomic, proteomic) will likely lead to better characterization of specific population subsets. Such signatures may also help to differentiate sepsis from noninfectious insults such as trauma or pancreatitis, in which a similar biological and clinical host response may be triggered by endogenous factors.
� • Sepsis is a syndrome shaped by pathogen factors and host factors (eg, sex, race and other genetic determinants, age, comorbidities, environment) with characteristics that evolve over time. What differentiates sepsis from infection is an aberrant or dysregulated host response and the presence of organ dysfunction. � • Sepsis-induced organ dysfunction may be occult; therefore, its presence should be considered in any patient presenting with infection. Conversely, unrecognized infection may be the cause of new-onset organ dysfunction. Any unexplained organ dysfunction should thus raise the possibility of underlying infection.
� • The clinical and biological phenotype of sepsis can be modified by preexisting acute illness, long-standing comorbidities, medication, and interventions. � • Specific infections may result in local organ dysfunction without generating a dysregulated systemic host response.
Sepsis: The current use of 2 or more SIRS criteria to identify sepsis was unanimously considered by the task force to be unhelpful. Changes in white blood cell count, temperature, and heart rate reflect inflammation, the host response to “danger” in the form of infection or other insults. The SIRS criteria do not necessarily indicate a dysregulated, lifethreatening response.
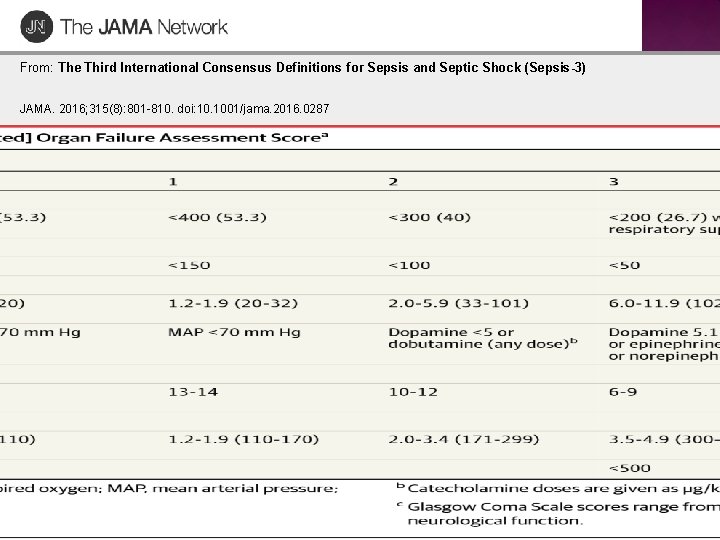
� Organ � Dysfunction or Failure The predominant score in current use is the Sequential Organ Failure Assessment (SOFA) (originally the Sepsis-related Organ Failure Assessment). �A higher SOFA score is associated with an increased probability of mortality.
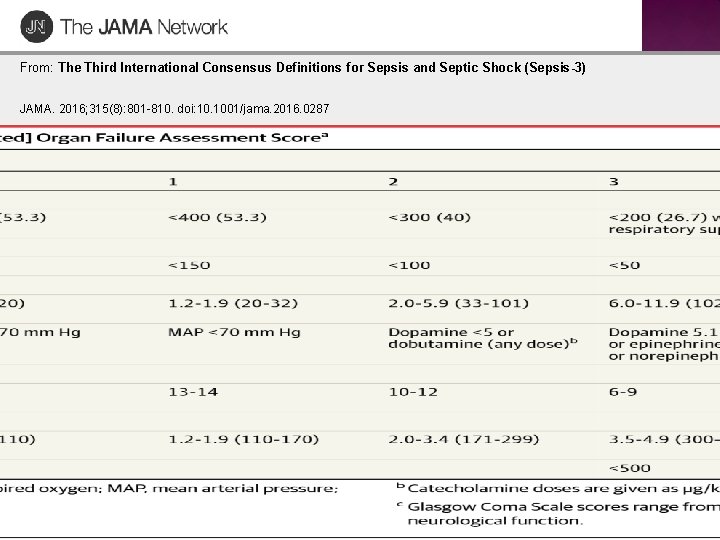
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287 Table Title: Sequential [Sepsis-Related] Organ Failure Assessment Scorea Date of download: 8/13/2016 Copyright © 2016 American Medical Association. All rights reserved.
� Assessing the Validity of Definitions When There Is No Gold Standard. � Because no gold standard diagnostic test exists, the task force sought definitions and supporting clinical criteria that were clear and fulfilled multiple domains of usefulness and validity.
� Septic Shock Multiple definitions for septic shock are currently in use. � A systematic review of the operationalization of current definitions highlights significant heterogeneity in reported mortality. This heterogeneity resulted from differences in the clinical variables chosen (varying cutoffs for systolic or mean blood pressure ± diverse levels of hyperlactatemia ± vasopressor use ± concurrent new organ dysfunction ± defined fluid resuscitation volume/targets), the data source and coding methods, and enrollment dates. �
� Despite its worldwide importance, 6, 7 public awareness of sepsis is poor. 29 Furthermore, the various manifestations of sepsis make diagnosis difficult, even for experienced clinicians. � The public needs an understandable definition of sepsis, whereas health care practitioners require improved clinical prompts and diagnostic approaches to facilitate earlier identification and an accurate quantification of the burden of sepsis.
� Definition of Sepsis � Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection. This new definition emphasizes the primacy of the nonhomeostatic host response to infection, the potential lethality that is considerably in excess of a straightforward infection, and the need for urgent recognition.
� Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection. � Organ dysfunction can be identified as an acute change in total SOFA score ≥ 2 points consequent to the infection. � The baseline SOFA score can be assumed to be zero in patients not known to have preexisting organ dysfunction. � A SOFA score ≥ 2 reflects an overall mortality risk of approximately 10% in a general hospital population with suspected infection. Even patients presenting with modest dysfunction can deteriorate further, emphasizing the seriousness of this condition and the need for prompt and appropriate intervention, if not already being instituted.
� � In lay terms, sepsis is a life-threatening condition that arises when the body’s response to an infection injures its own tissues and organs. Patients with suspected infection who are likely to have a prolonged ICU stay or to die in the hospital can be promptly identified at the bedside with q. SOFA, ie, alteration in mental status, systolic blood pressure ≤ 100 mm Hg, or respiratory rate ≥ 22/min. Septic shock is a subset of sepsis in which underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality. Patients with septic shock can be identified with a clinical construct of sepsis with persisting hypotension requiring vasopressors to maintain MAP ≥ 65 mm Hg and having a serum lactate level >2 mmol/L (18 mg/d. L) despite adequate volume resuscitation. With these criteria, hospital mortality is in excess of 40%.
The Delphi process assessed agreements on descriptions of terms such as “hypotension, ” “need for vasopressor therapy, ” “raised lactate, ” and “adequate fluid resuscitation” for inclusion within the new clinical criteria. A majority (11/17; 64. 7%) of the task force agreed, whereas 2 (11. 8%) disagreed, that an elevated lactate level is reflective of cellular dysfunction in sepsis, albeit recognizing that multiple factors, such as insufficient tissue oxygen delivery, impaired aerobic respiration, accelerated aerobic glycolysis, and reduced hepatic clearance, also contribute. Hyperlactatemia is, however, a reasonable marker of illness severity, with higher levels predictive of higher mortality.
Criteria for “adequate fluid resuscitation” or “need for vasopressor therapy” could not be explicitly specified because these are highly user dependent, relying on variable monitoring modalities and hemodynamic targets for treatment. � Other aspects of management, such as sedation and volume status assessment, are also potential confounders in the hypotension -vasopressor relationship. �
� The task force has generated new definitions that incorporate an up-to-date understanding of sepsis biology, including organ dysfunction. � To assist the bedside clinician, and perhaps prompt an escalation of care if not already instituted, simple clinical criteria (q. SOFA) that identify patients with suspected infection who are likely to have poor outcomes, that is, a prolonged ICU course and death, have been developed and validated.
Barcelona Declaration: “to reduce global mortality from severe sepsis by 25% in 5 years”
� In response to the European Society of Intensive Care Medicine’s and the Society of Critical Care Medicine’s Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3), 1– 3 the Surviving Sepsis Campaign (SSC) offers clarification on the implications of the new definition statements and guidance for hospitals and practitioners. Many organizations, including regulatory agencies and hospitals, are focused on sepsis quality improvement programs
� Step 1: Screening and Management of Infection: � The appropriate first step in screening should be identification of infection. Hospitals should continue to use signs and symptoms of infection to promote the early identification of patients with suspected or confirmed infection. In those patients identified as having infection, management should begin by obtaining blood and other cultures as indicated, administering tailored antibiotics as appropriate, and simultaneously obtaining laboratory results to evaluate the patient for infection-related organ dysfunction
� Step 2: Screening for Organ Dysfunction and Management of Sepsis (formerly called Severe Sepsis): � Patients with sepsis (formerly called severe sepsis) should still be identified by the same organ dysfunction criteria (including lactate level greater than 2 mmol/L).
� If organ dysfunction is identified, ensuring that the three-hour bundle elements have been initiated continues to be a priority. For instance, patients with organ dysfunction require blood cultures if only non-blood cultures had previously been obtained and administration of broad-spectrum antibiotics if only narrow-spectrum antibiotics had previously been administered
� Step 3: Identification and Management of Initial Hypotension: � In those patients who have infection and hypotension or a lactate level greater than or equal to 4 mmol/L, providing 30 m. L/kg crystalloid with reassessment of volume responsiveness or tissue perfusion should be implemented. The six-hour elements of care should be completed. For the six-hour bundle, repeat lactate level is also recommended if initial lactate level was greater than 2 mmol/L.
� Prepare for Change : � As always, hospitals should prepare for major changes that can alter fiscal considerations. Hospitals should develop detailed plans and educate their physician and nursing staff and their coding departments to ensure that their coders accurately capture the sense of the new definitions.
� Conclusion : � Once hospitals have adequately prepared for change, sepsis team leaders should reinforce the message that the new definitions do not change the primary focus of early sepsis identification and initiation of timely treatment in the management of this vulnerable patient population.
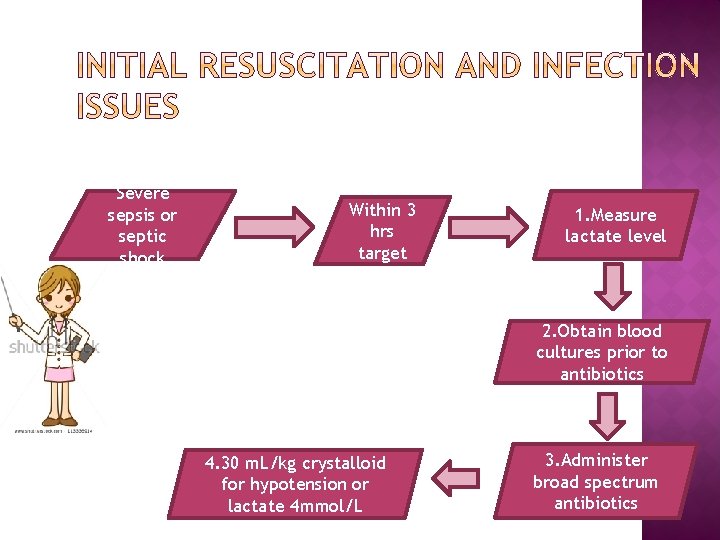
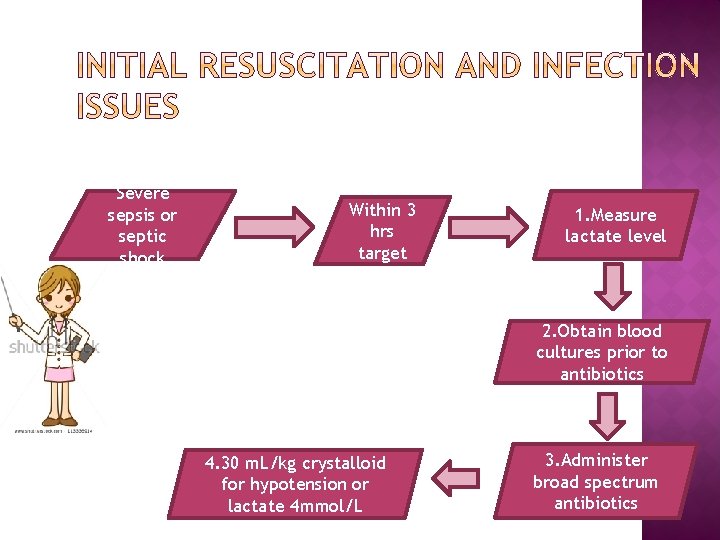
Severe sepsis or septic shock Within 3 hrs target 1. Measure lactate level 2. Obtain blood cultures prior to antibiotics 4. 30 m. L/kg crystalloid for hypotension or lactate 4 mmol/L 3. Administer broad spectrum antibiotics
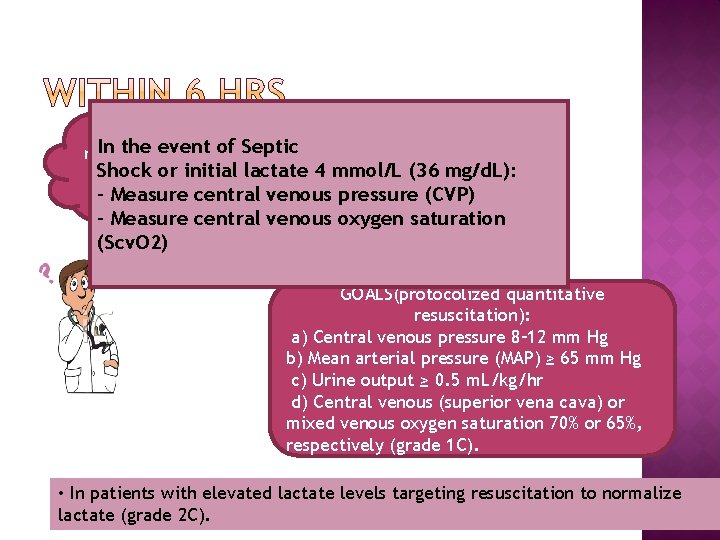
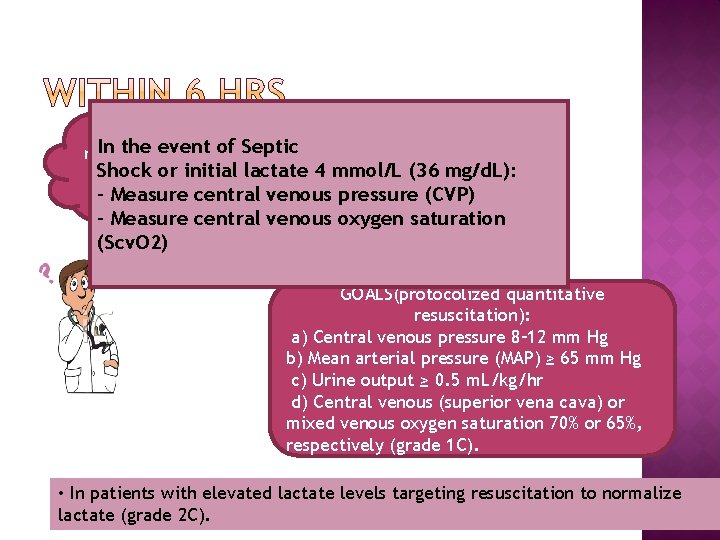
hypotension Apply vasopressors In responding the event of Septic not SEPTIC → target →mean Shock or initial lactate 4 mmol/L (36 mg/d. L): to initial fluid SHOCK arterial pressure - Measure central venous pressure resuscitation (MAP) (CVP) 65 mm Hg - Measure central venous oxygen saturation (Scv. O 2) GOALS(protocolized quantitative resuscitation): a) Central venous pressure 8– 12 mm Hg b) Mean arterial pressure (MAP) ≥ 65 mm Hg c) Urine output ≥ 0. 5 m. L/kg/hr d) Central venous (superior vena cava) or mixed venous oxygen saturation 70% or 65%, respectively (grade 1 C). • In patients with elevated lactate levels targeting resuscitation to normalize lactate (grade 2 C).
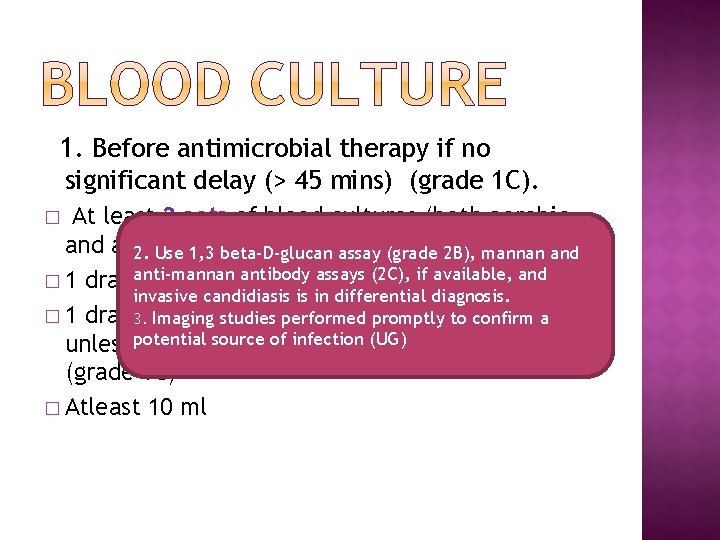
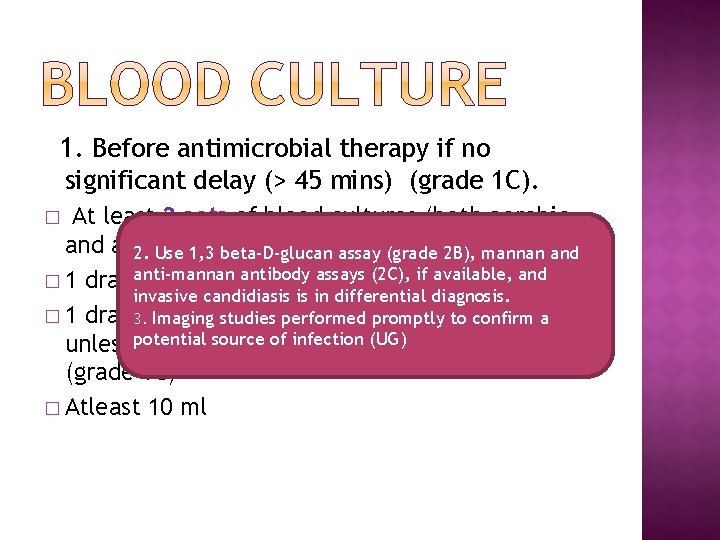
1. Before antimicrobial therapy if no significant delay (> 45 mins) (grade 1 C). At least 2 sets of blood cultures (both aerobic and anaerobic bottles) assay (grade 2 B), mannan and 2. Use 1, 3 beta-D-glucan anti-mannan antibody assays (2 C), if available, and � 1 drawn percutaneously invasive candidiasis is in differential diagnosis. � 1 drawn through each vascular access device, 3. Imaging studies performed promptly to confirm a sourcewas of infection (UG)(<48 hrs) inserted unless potential the device recently (grade 1 C) � Atleast 10 ml �
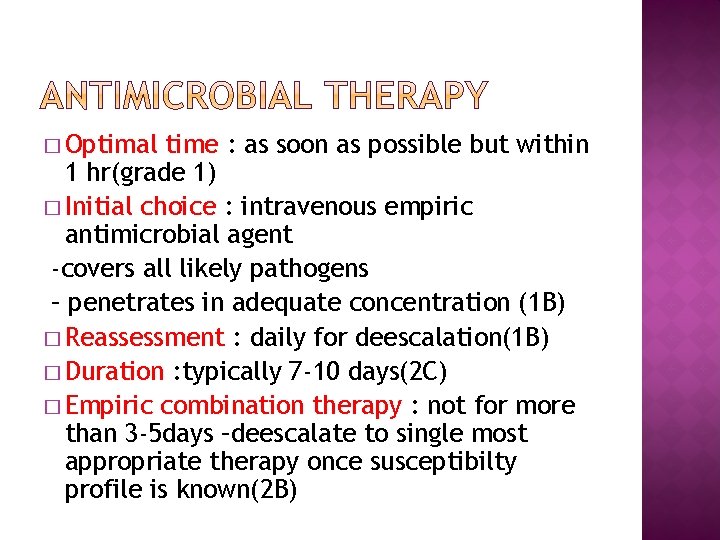
� Optimal time : as soon as possible but within 1 hr(grade 1) � Initial choice : intravenous empiric antimicrobial agent -covers all likely pathogens – penetrates in adequate concentration (1 B) � Reassessment : daily for deescalation(1 B) � Duration : typically 7 -10 days(2 C) � Empiric combination therapy : not for more than 3 -5 days –deescalate to single most appropriate therapy once susceptibilty profile is known(2 B)
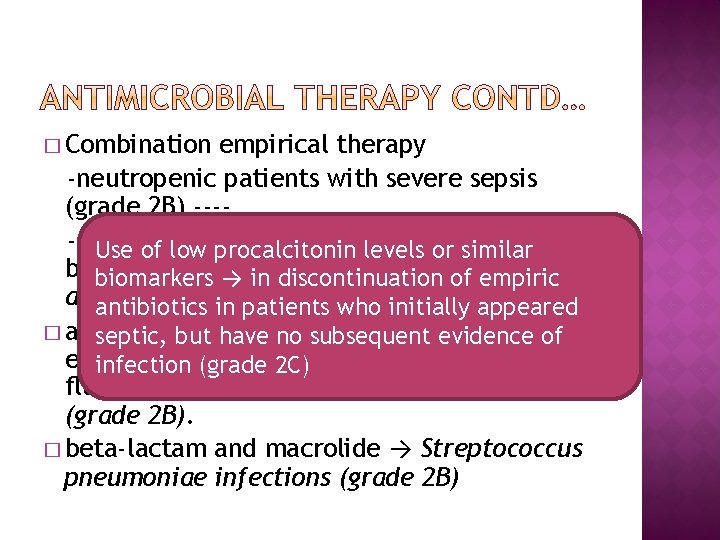
� Combination empirical therapy -neutropenic patients with severe sepsis (grade 2 B) ----difficult-to-treat, multidrug-resistant Use of low procalcitonin levels or similar bacterial pathogens such as Acinetobacter biomarkers → in discontinuation of empiric andantibiotics Pseudomonas spp. (grade 2 B) appeared in patients who initially � an septic, extended beta-lactam and of but spectrum have no subsequent evidence either an aminoglycoside or a infection (grade 2 C) fluoroquinolone → P. aeruginosa bacteremia (grade 2 B). � beta-lactam and macrolide → Streptococcus pneumoniae infections (grade 2 B)
� Antiviral therapy initiated as early as possible in patients with severe sepsis or septic shock of viral origin (grade 2 C)
� Specific anatomical diagnosis requiring emergent source control be sought and diagnosed or excluded as rapidly as possible and intervention undertaken for source control within the first 12 hr after diagnosis, if feasible (grade 1 C) � Exception Peripancreatic necrosis → intervention delayed until adequate demarcation of viable and nonviable tissues.
� Use effective intervention associated with the least physiologic insult(eg, percutaneous rather than surgical drainage of an abscess) (UG). � If intravascular access devices → possible source → removed promptly after other vascular access has been established (UG).
� Selective oral decontamination and selective digestive decontamination→ introduced and investigated as a method to reduce ventilator -associated pneumonia; this infection control measure can then be instituted in health care settings and regions where this methodology is found to be effective (grade 2 B). � Oral chlorhexidine gluconate for oropharyngeal decontamination to reduce the risk of ventilator-associated pneumonia (grade 2 B).

Crystalloids → initial fluid of choice(1 B) � Against the use of hydroxyethyl starches (1 B) � Albumin in the fluid resuscitation when substantial amounts of crystalloids are required(2 C) � Initial fluid challenge sepsis induced hypoperfusion minimum of 30 m. L/kg of crystalloids (a portion of this may be albumin equivalent) (1 C) � Rapid and greater amounts in some � continued as long as hemodynamic improvement. (UG) �
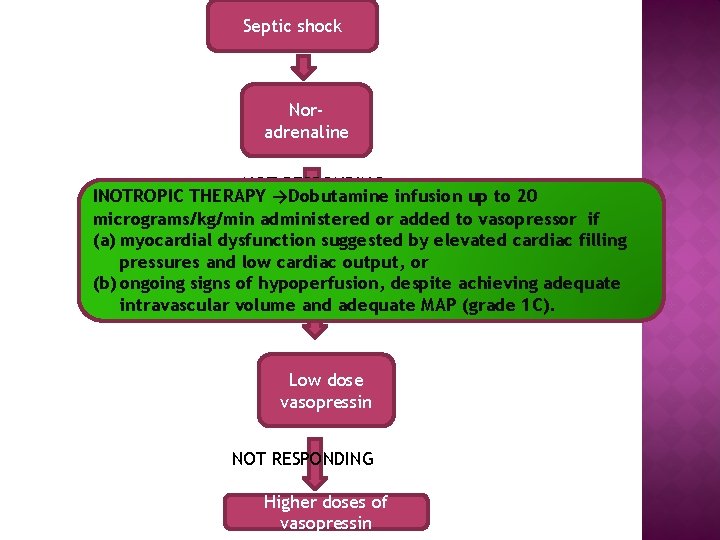
� � � � Target → mean arterial pressure (MAP) of 65 mm Hg (1 C). Norepinephrine → first choice vasopressor (1 B) Epinephrine(added or alternative to NE) →when an additional agent is needed (2 B). ᴺᵉᵂ Vasopressin 0. 03 units/minute added to norepinephrine (NE) to raise MAP or decrease NE dosage (UG). ᴺᵉᵂ Low dose vasopressin → not recommended as the single initial vasopressor (UG) ᴺᵉᵂ vasopressin doses higher than 0. 03 -0. 04 units/minute reserved for salvage therapy (failure to achieve adequate MAP with other vasopressor agents) (UG). ᴺᵉᵂ Dopamine as an alternative vasopressor agent to norepinephrine only in highly selected patients (eg, patients with low risk of tachyarrhythmias and absolute or relative bradycardia) (grade 2 C).
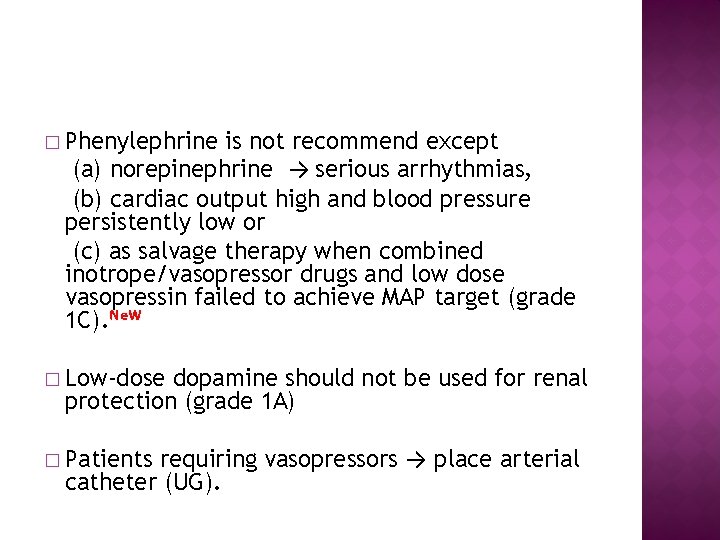
� Phenylephrine is not recommend except (a) norepinephrine → serious arrhythmias, (b) cardiac output high and blood pressure persistently low or (c) as salvage therapy when combined inotrope/vasopressor drugs and low dose vasopressin failed to achieve MAP target (grade 1 C). ᴺᵉᵂ � Low-dose dopamine should not be used for renal protection (grade 1 A) requiring vasopressors → place arterial catheter (UG). � Patients
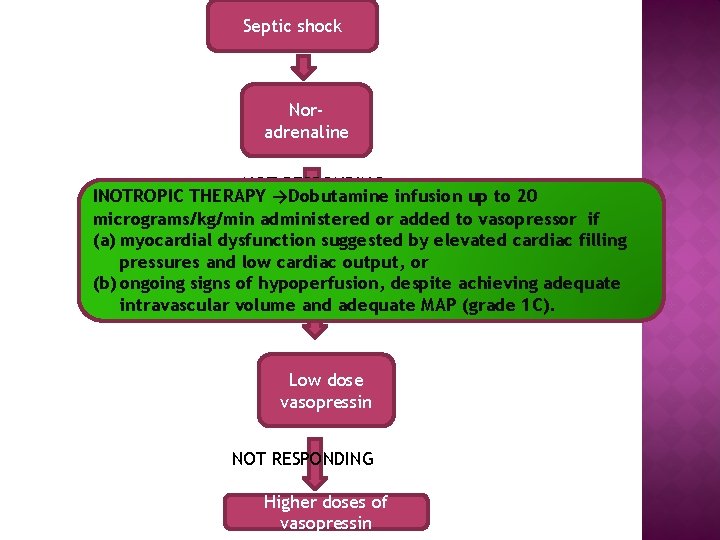
Septic shock Noradrenaline NOT RESPONDING INOTROPIC THERAPY →Dobutamine infusion up to 20 micrograms/kg/min administered or added to vasopressor if (a) myocardial dysfunction suggested by elevated cardiac filling adrenaline pressures and low cardiac output, or (b) ongoing signs of hypoperfusion, despite achieving adequate intravascular volume and adequate MAP (grade 1 C). NOT RESPONDING Low dose vasopressin NOT RESPONDING Higher doses of vasopressin
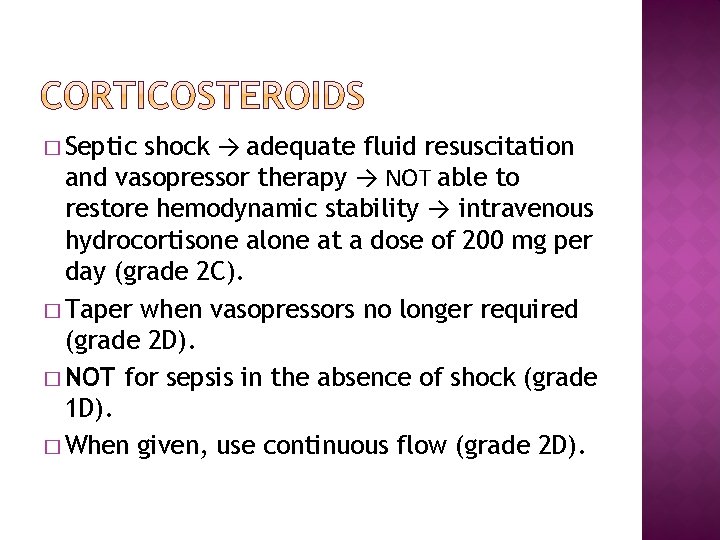
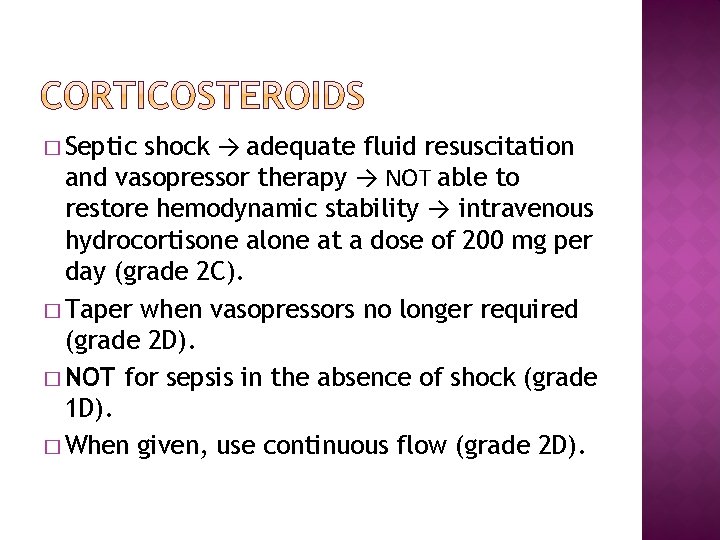
shock → adequate fluid resuscitation and vasopressor therapy → NOT able to restore hemodynamic stability → intravenous hydrocortisone alone at a dose of 200 mg per day (grade 2 C). � Taper when vasopressors no longer required (grade 2 D). � NOT for sepsis in the absence of shock (grade 1 D). � When given, use continuous flow (grade 2 D). � Septic
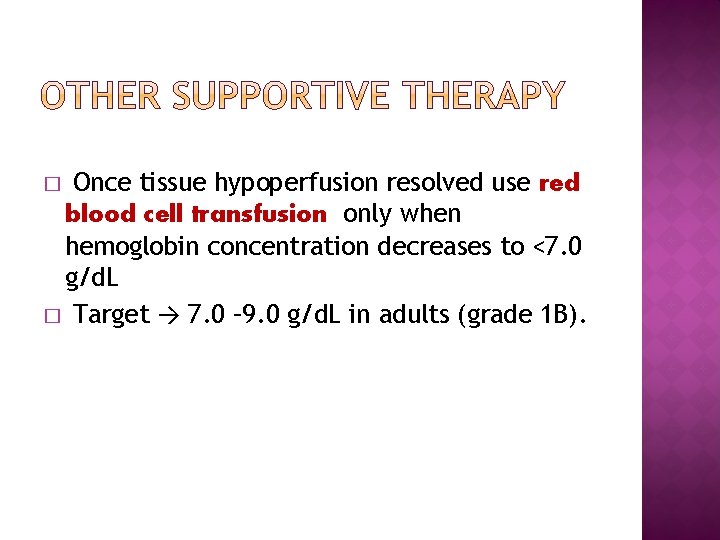
Once tissue hypoperfusion resolved use red blood cell transfusion only when hemoglobin concentration decreases to <7. 0 g/d. L � Target → 7. 0 – 9. 0 g/d. L in adults (grade 1 B). �
� Prophylactic Platelet transfusion when 1. Severe sepsis with counts < 10, 000 2. Significant risk of bleeding and a count of <20, 000 � Maintain >50, 000 if 1. Active bleeding present 2. Pt planned for surgery or invasive procedure
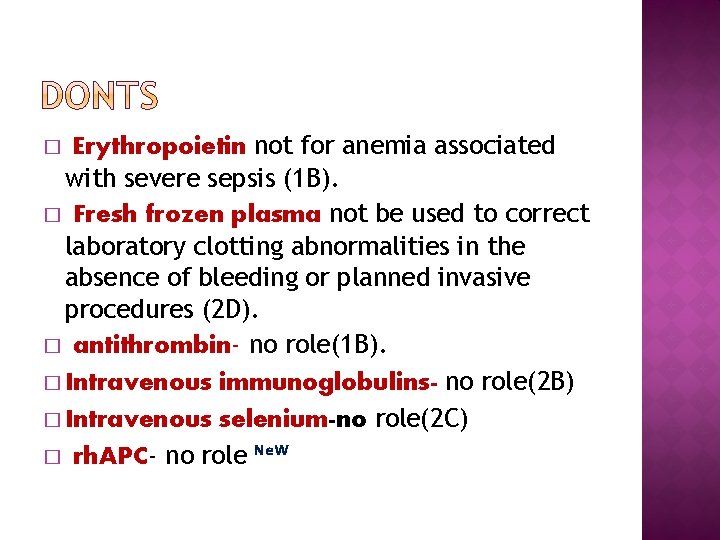
Erythropoietin not for anemia associated with severe sepsis (1 B). � Fresh frozen plasma not be used to correct laboratory clotting abnormalities in the absence of bleeding or planned invasive procedures (2 D). � antithrombin- no role(1 B). � Intravenous immunoglobulins- no role(2 B) � Intravenous selenium-no role(2 C) � rh. APC- no role ᴺᵉᵂ �
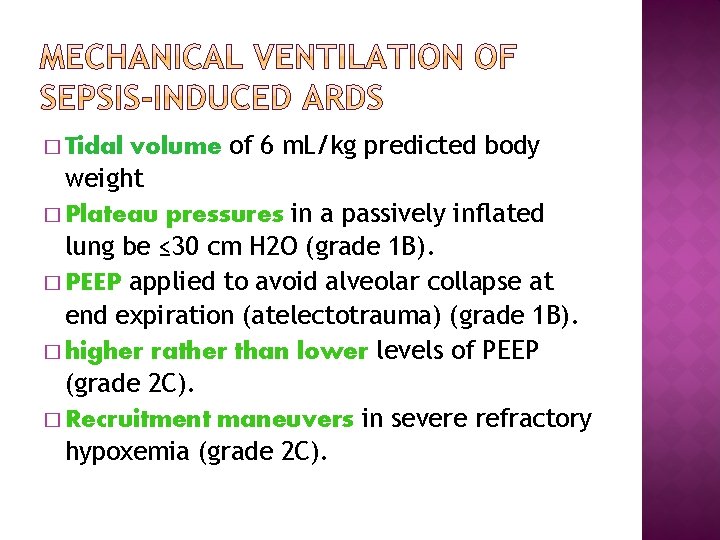
volume of 6 m. L/kg predicted body weight � Plateau pressures in a passively inflated lung be ≤ 30 cm H 2 O (grade 1 B). � PEEP applied to avoid alveolar collapse at end expiration (atelectotrauma) (grade 1 B). � higher rather than lower levels of PEEP (grade 2 C). � Recruitment maneuvers in severe refractory hypoxemia (grade 2 C). � Tidal

positioning when Pao 2/Fio 2 ratio ≤ 100 mm Hg in facilities with experience in such practices (grade 2 B). � Head end elevation to 30 -45 degrees to limit aspiration risk and to preventilator -associated pneumonia (grade 1 B). � Noninvasive mask ventilation (NIV) used in minority in whom benefits carefully considered and thought to outweigh the risks (grade 2 B). � Prone
protocol be in place and patients undergo spontaneous breathing trials regularly to discontinue mechanical ventilation when they satisfy the following : a) arousable; b) hemodynamically stable (without vasopressor agents); c) no new potentially serious conditions; d) low ventilatory and end-expiratory pressure requirements; and e) low Fio 2 requirements which can be met safely delivered with a face mask or nasal cannula. If trial successful→ considerextubation (grade 1 A). � weaning •
Continuous or intermittent sedation be minimized in mechanically ventilated sepsis patients, targeting specific titration endpoints (grade 1 B). ᴺᵉᵂ � Neuromuscular blocking agents (NMBAs) be avoided if possible in the septic patient without ARDS due to the risk of prolonged neuromuscular blockade following discontinuation. If NMBAs must be maintained, either intermittent bolus as required or continuous infusion with train-of-four monitoring of the depth of blockade should be used (grade 1 C). � A short course of NMBA of not greater than 48 hours for patients with early sepsis-induced ARDS and a Pao 2/Fio 2 < 150 mm Hg (grade 2 C). �
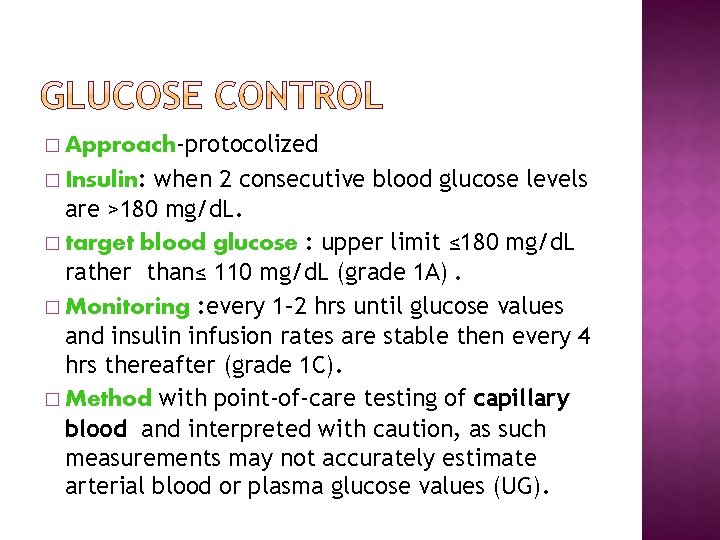
� Approach-protocolized when 2 consecutive blood glucose levels are >180 mg/d. L. � target blood glucose : upper limit ≤ 180 mg/d. L rather than≤ 110 mg/d. L (grade 1 A). � Monitoring : every 1– 2 hrs until glucose values and insulin infusion rates are stable then every 4 hrs thereafter (grade 1 C). � Method with point-of-care testing of capillary blood and interpreted with caution, as such measurements may not accurately estimate arterial blood or plasma glucose values (UG). � Insulin:
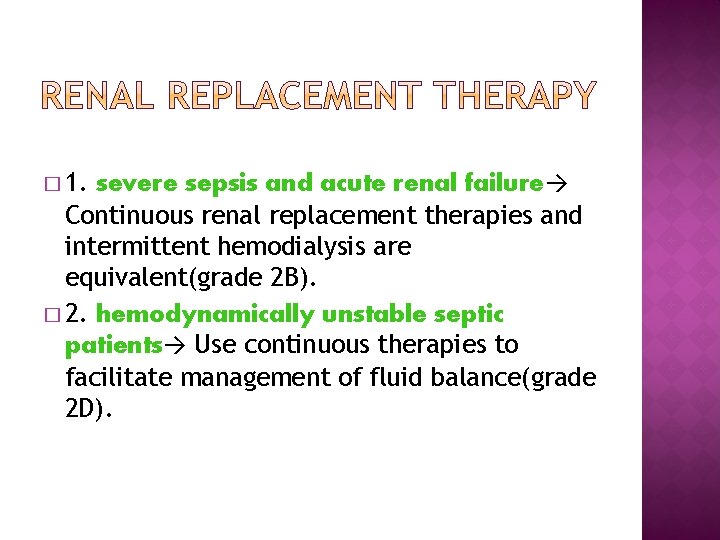
� 1. severe sepsis and acute renal failure→ Continuous renal replacement therapies and intermittent hemodialysis are equivalent(grade 2 B). � 2. hemodynamically unstable septic patients→ Use continuous therapies to facilitate management of fluid balance(grade 2 D).
� Not using sodium bicarbonate therapy for the purpose of improving hemodynamics or reducing vasopressor requirements in patients with hypoperfusion-induced lactic acidemia with p. H ≥ 7. 15 (grade 2 B).
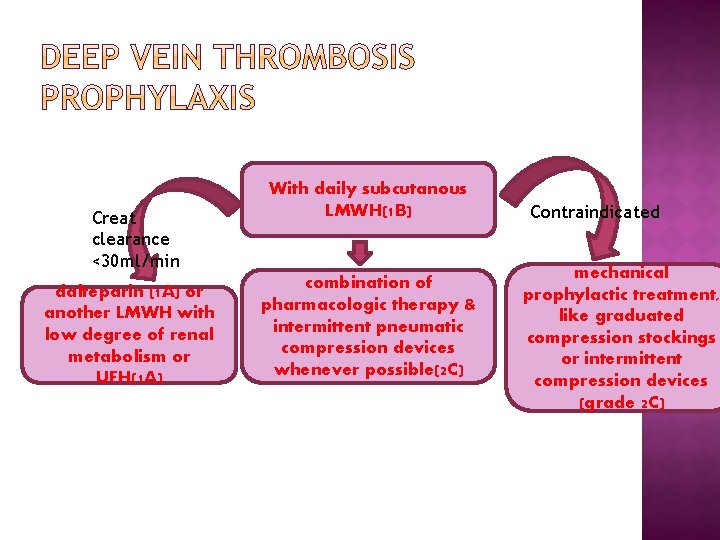
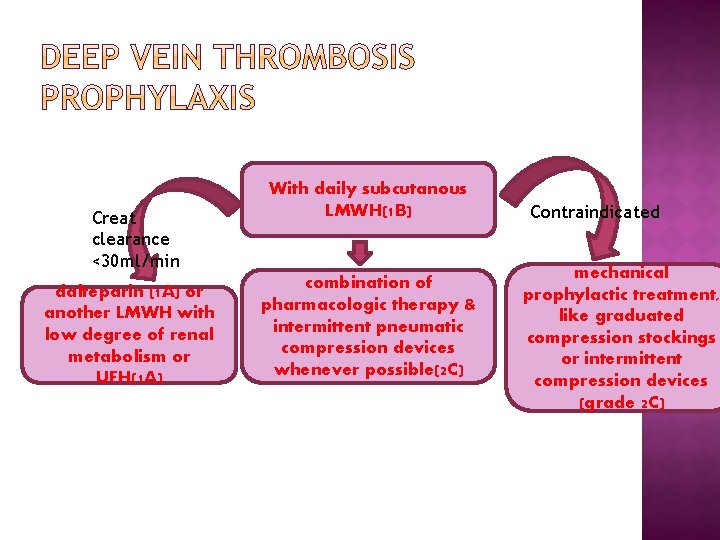
Creat clearance <30 ml/min dalteparin (1 A) or another LMWH with low degree of renal metabolism or UFH(1 A) With daily subcutanous LMWH(1 B) combination of pharmacologic therapy & intermittent pneumatic compression devices whenever possible(2 C) Contraindicated mechanical prophylactic treatment, like graduated compression stockings or intermittent compression devices (grade 2 C)
� Stress ulcer prophylaxis using H 2 blocker or proton pump inhibitor to patients who have bleeding risk factors (grade 1 B). � Proton pump inhibitors > H 2 RA (grade 2 D) � Patients without risk factors do not receive prophylaxis (grade 2 B).
� � 1. Administer oral or enteral (if necessary) feedings, as tolerated, rather than either complete fasting or provision of only intravenous glucose within the first 48 hours after a diagnosis of severe sepsis/septic shock (grade 2 C). 2. Avoid mandatory full caloric feeding in the first week but rather suggest low dose feeding (eg, up to 500 calories per day), advancing only as tolerated (grade 2 B). 3. Use intravenous glucose and enteral nutrition rather than total parenteral nutrition (TPN) alone or parenteral nutrition in conjunction with enteral feeding in the first 7 days after a diagnosis of severe sepsis/septic shock (grade 2 B). 4. Use nutrition with no specific immunomodulating supplementation rather than nutrition providing specific immunomodulating supplementation in patients with severe sepsis (grade 2 C).
� 1. Discuss goals of care and prognosis with patients and families (grade 1 B). � 2. Incorporate goals of care into treatment and end-of-life care planning, utilizing palliative care principles where appropriate (grade 1 B). � 3. Address goals of care as early as feasible, but no later than within 72 hours of ICU admission (grade 2 C).
WHAT IS A BUNDLE? “A bundle is a structured way of improving the processes of care and patient outcomes: a small, straightforward set of evidence-based practices generally three to five - that, when performed collectively and reliably, have been proven to improve patient outcomes. ” - IHI. org Goal of 25 percent reduction in mortality


� Step 2: Screening for Organ Dysfunction and Management of Sepsis (formerly called Severe Sepsis): � Patients with sepsis (formerly called severe sepsis) should still be identified by the same organ dysfunction criteria (including lactate level greater than 2 mmol/L).
� Organ dysfunction may also be identified in the future using the quick Sepsis-Related Organ Failure Assessment (q. SOFA)
� Importantly, evidence of two out of three q. SOFA elements (altered mental status, respiratory rate greater than or equal to 22 breaths/min and systolic blood pressure less than or equal to 100 mm Hg) in patients who have screened positive for infection may be used as a secondary screen to identify patients at risk for clinical deterioration. These three q. SOFA elements were determined through analysis of a data-driven model to predict deterioration. Practitioners should strongly consider closer monitoring of these at-risk patients.
� If organ dysfunction is identified, ensuring that the three-hour bundle elements have been initiated continues to be a priority. For instance, patients with organ dysfunction require blood cultures if only non-blood cultures had previously been obtained and administration of broad-spectrum antibiotics if only narrow-spectrum antibiotics had previously been administered
� Step 3: Identification and Management of Initial Hypotension: � In those patients who have infection and hypotension or a lactate level greater than or equal to 4 mmol/L, providing 30 m. L/kg crystalloid with reassessment of volume responsiveness or tissue perfusion should be implemented. The six-hour elements of care should be completed. For the six-hour bundle, repeat lactate level is also recommended if initial lactate level was greater than 2 mmol/L.
� Quick SOFA Clarification for the Practitioner: � Sepsis-3 introduces q. SOFA as a tool for identifying patients at risk of sepsis with a higher risk of hospital death or prolonged intensive care unit (ICU) stay both inside and outside critical care units.
� �q. SOFA does not define sepsis (but the presence of two q. SOFA criteria is a predictor of both increased mortality and ICU stays of more than three days in non-ICU patients) � �The new sepsis definitions recommend using a change in baseline of the total SOFA score of two or more points to represent organ dysfunction.
� Prepare for Change : � As always, hospitals should prepare for major changes that can alter fiscal considerations. Hospitals should develop detailed plans and educate their physician and nursing staff and their coding departments to ensure that their coders accurately capture the sense of the new definitions.
� Conclusion : � Once hospitals have adequately prepared for change, sepsis team leaders should reinforce the message that the new definitions do not change the primary focus of early sepsis identification and initiation of timely treatment in the management of this vulnerable patient population.
 Quick sofa escala
Quick sofa escala Ventricular escape rhythm
Ventricular escape rhythm Vvi pacemaker
Vvi pacemaker Ductile vs brittle fracture
Ductile vs brittle fracture Sudha chandran smoking
Sudha chandran smoking Sudha yalamanchili
Sudha yalamanchili Sudha balla
Sudha balla Dr sudha gupta
Dr sudha gupta Cell tissue organ organ system organism
Cell tissue organ organ system organism Tractus respiratorius
Tractus respiratorius Tissues group together to form
Tissues group together to form Keratomalasi
Keratomalasi Organ penyusun sistem gerak pada manusia adalah
Organ penyusun sistem gerak pada manusia adalah Organ and organ system
Organ and organ system Multi loop pid controller regolatore pid multi loop
Multi loop pid controller regolatore pid multi loop Waiting line management
Waiting line management Rani toersilaningsih
Rani toersilaningsih Mahila samman kosh up
Mahila samman kosh up Dean and rani enterprise
Dean and rani enterprise Anita rani feet
Anita rani feet Binita rani
Binita rani Antigona tema
Antigona tema Rani elkon
Rani elkon Tansen became a good singer after *
Tansen became a good singer after * Rani chandran
Rani chandran Raj rani vs prem adib case summary
Raj rani vs prem adib case summary Räni orgaaniline polümeer
Räni orgaaniline polümeer Jane fiemeyer
Jane fiemeyer Binita rani
Binita rani Mistress seema rani
Mistress seema rani How do you get sepsis
How do you get sepsis Driver diagram template
Driver diagram template Sepsis hour 1 bundle
Sepsis hour 1 bundle Gdp sepsis decision support tool
Gdp sepsis decision support tool Sepsis care near palo alto
Sepsis care near palo alto Dental sepsis
Dental sepsis Sepsis
Sepsis Indication for exploratory laparotomy
Indication for exploratory laparotomy Dr ali hieatt
Dr ali hieatt Prevention of puerperal sepsis
Prevention of puerperal sepsis Stages of sepsis
Stages of sepsis Accefluid
Accefluid Surviving sepsis definition
Surviving sepsis definition Vertical y horizontal
Vertical y horizontal Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Sepsis einkenni
Sepsis einkenni Quick sofa
Quick sofa Hoja de balance hidrico en enfermeria
Hoja de balance hidrico en enfermeria Indometacia
Indometacia Sepsis
Sepsis Puerperal sepsis
Puerperal sepsis Sepsis pp respiratorio
Sepsis pp respiratorio Give 3 take 3 sepsis
Give 3 take 3 sepsis Maternal sepsis
Maternal sepsis Riesgo de sepsis nanda
Riesgo de sepsis nanda Criterios sepsis
Criterios sepsis Sepsis bundle
Sepsis bundle Sepsis dietary management
Sepsis dietary management Hora de oro en sepsis
Hora de oro en sepsis Sepsis
Sepsis David howe ent
David howe ent What is hypotensis
What is hypotensis Neonatal sepsis symptoms
Neonatal sepsis symptoms Sepsis hour 1 bundle
Sepsis hour 1 bundle Neonatal sepsis
Neonatal sepsis Pengertian market failure
Pengertian market failure Double angle section
Double angle section Failure to fire pacemaker
Failure to fire pacemaker Heart failure complications
Heart failure complications Failure to give care that is normally expected
Failure to give care that is normally expected Slope failure
Slope failure Role of government in correcting market failure
Role of government in correcting market failure Partial failure
Partial failure Types of failure in distributed database system
Types of failure in distributed database system Schools without failure
Schools without failure Failure point analysis
Failure point analysis Hepatic encephalopathy staging
Hepatic encephalopathy staging Expectation failure
Expectation failure Agile failure stories
Agile failure stories Sod table in fmea
Sod table in fmea Common hazard in market
Common hazard in market Daniel mahzonni
Daniel mahzonni What is failure demand
What is failure demand