UNC Hospitals Sepsis Mortality Reduction Initiative Code Sepsis









- Slides: 40
UNC Hospitals Sepsis Mortality Reduction Initiative Code Sepsis Core Adult Patient Sepsis Training Slides
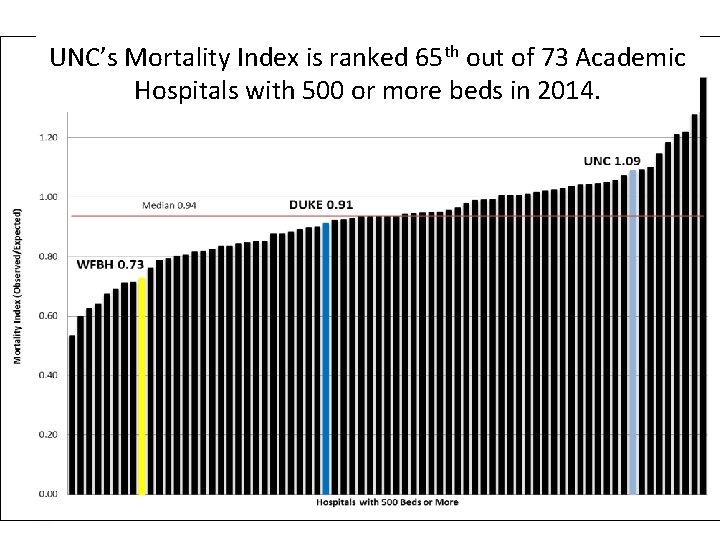
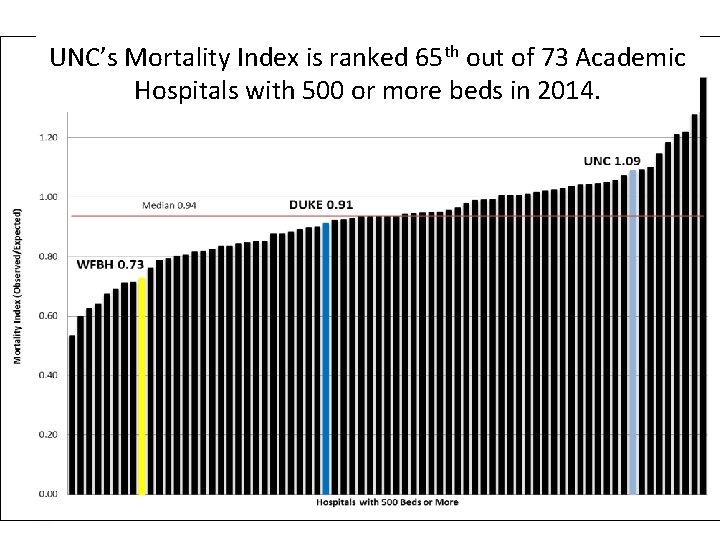
UNC’s Mortality Index is ranked 65 th out of 73 Academic Hospitals with 500 or more beds in 2014.
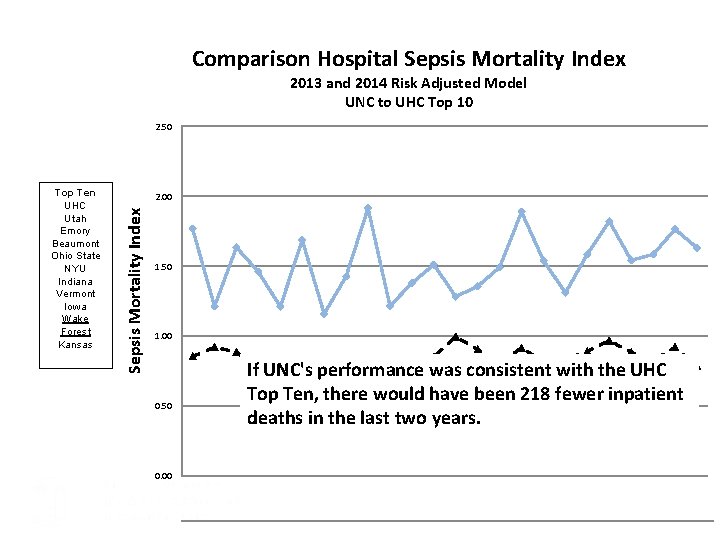
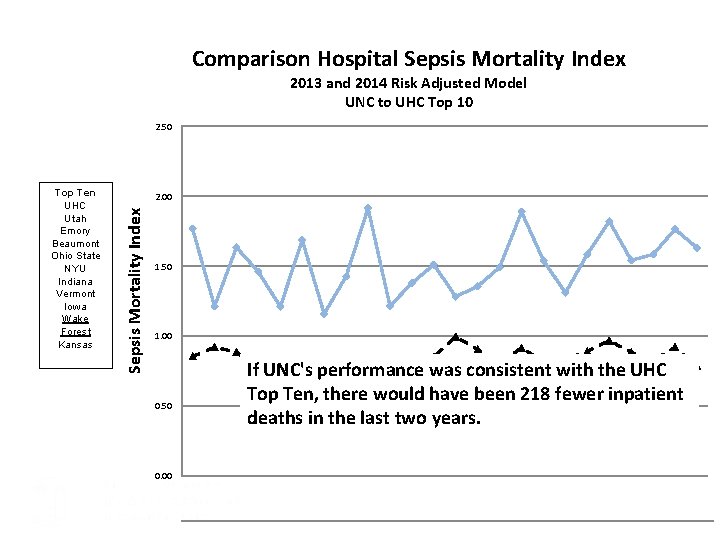
Comparison Hospital Sepsis Mortality Index 2013 and 2014 Risk Adjusted Model UNC to UHC Top 10 2. 50 2. 00 Sepsis Mortality Index Top Ten UHC Utah Emory Beaumont Ohio State NYU Indiana Vermont Iowa Wake Forest Kansas 1. 50 1. 00 0. 50 If UNC's performance was consistent with the UHC Top Ten, there would have been 218 fewer inpatient deaths in the last two years. 0. 00 UNC Sepsis Mortality Index 1. 77 1. 21 1. 63 1. 46 1. 21 1. 69 1. 16 1. 43 1. 91 1. 21 1. 38 1. 51 1. 28 1. 36 1. 49 1. 89 1. 54 1. 31 1. 59 1. 82 1. 54 1. 58 1. 76 1. 63
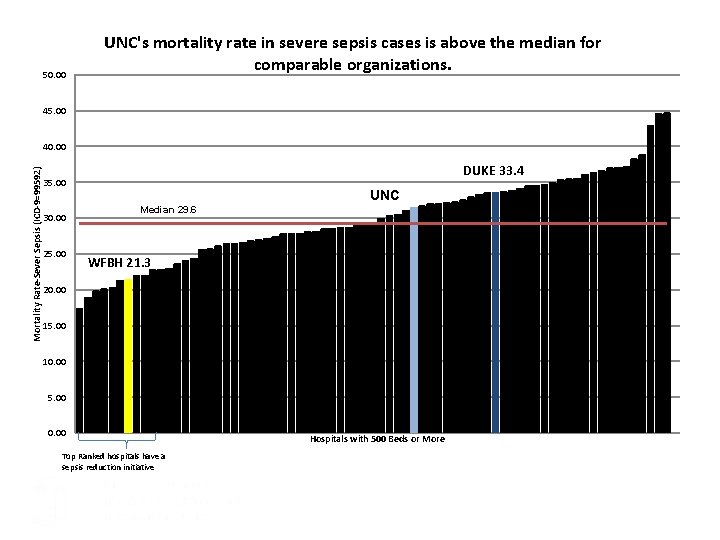
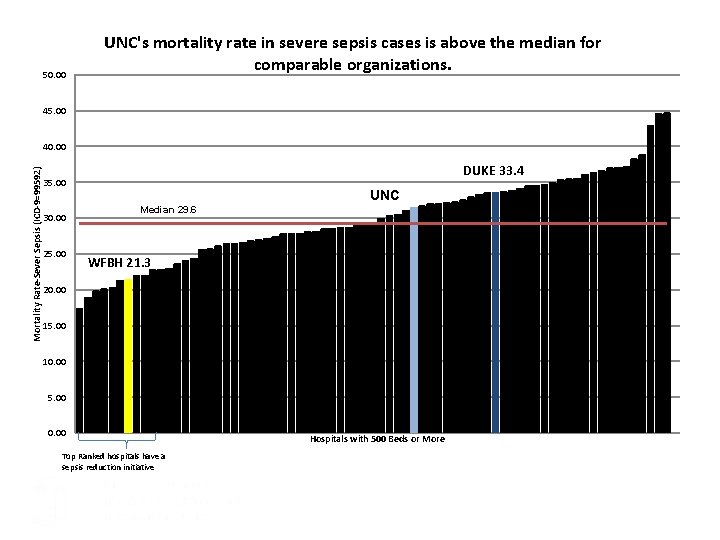
50. 00 UNC's mortality rate in severe sepsis cases is above the median for comparable organizations. 45. 00 Mortality Rate-Sever Sepsis (ICD-9=99592) 40. 00 DUKE 33. 4 35. 00 30. 00 25. 00 UNC Median 29. 6 WFBH 21. 3 20. 00 15. 00 10. 00 5. 00 0. 00 Top Ranked hospitals have a sepsis reduction initiative Hospitals with 500 Beds or More
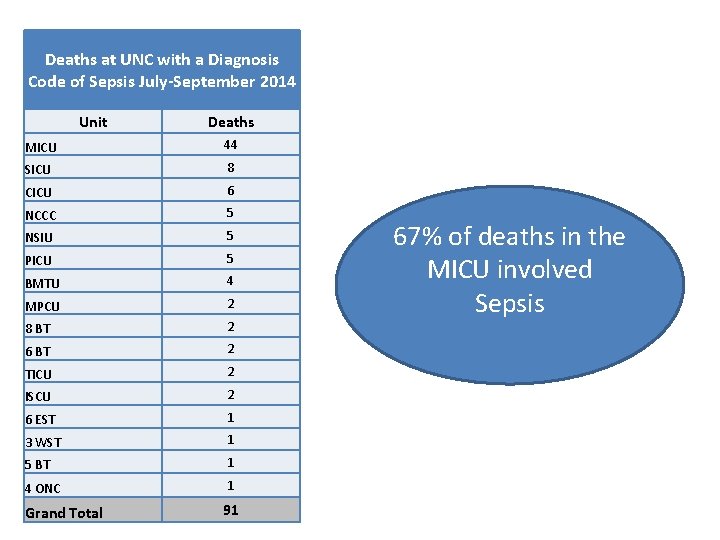
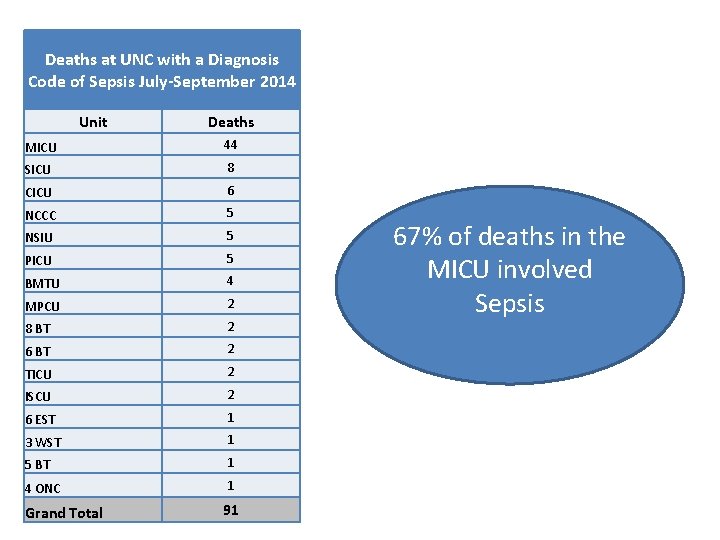
Deaths at UNC with a Diagnosis Code of Sepsis July-September 2014 Unit Deaths MICU 44 SICU 8 CICU 6 NCCC 5 NSIU 5 PICU 5 BMTU 4 MPCU 2 8 BT 2 6 BT 2 TICU 2 ISCU 2 6 EST 1 3 WST 1 5 BT 1 4 ONC 1 Grand Total 91 67% of deaths in the MICU involved Sepsis
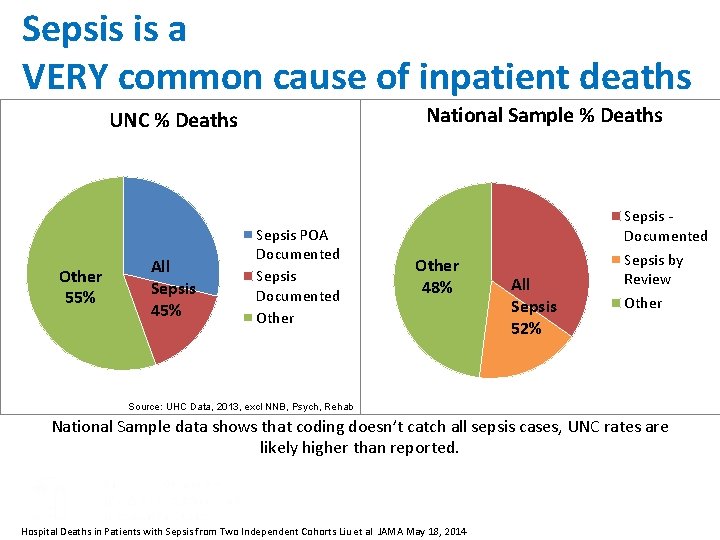
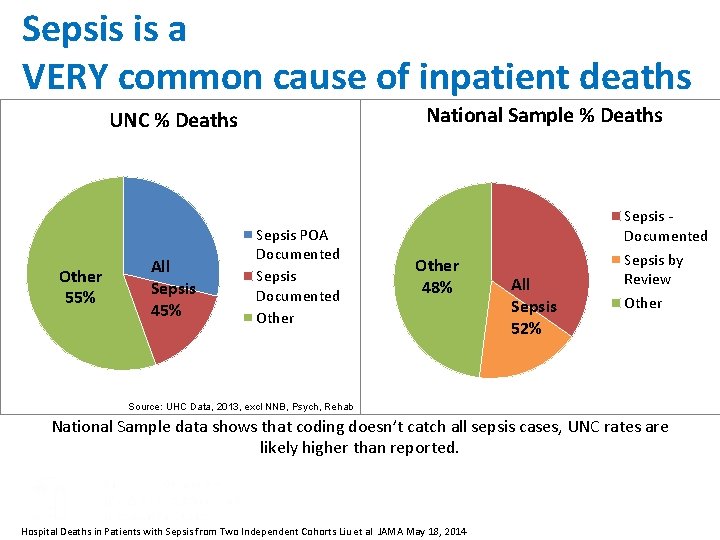
Sepsis is a VERY common cause of inpatient deaths National Sample % Deaths UNC % Deaths Other 55% All Sepsis 45% Sepsis POA Documented Sepsis Documented Other Sepsis - Documented Other 48% All Sepsis 52% Sepsis by Review Other Source: UHC Data, 2013, excl NNB, Psych, Rehab National Sample data shows that coding doesn’t catch all sepsis cases, UNC rates are likely higher than reported. Hospital Deaths in Patients with Sepsis from Two Independent Cohorts Liu et al JAMA May 18, 2014

Other Organizations with successful sepsis reduction programs • • • Wake Forest Baptist Nation of Scotland Penn State Long Island Jewish Health System Many more

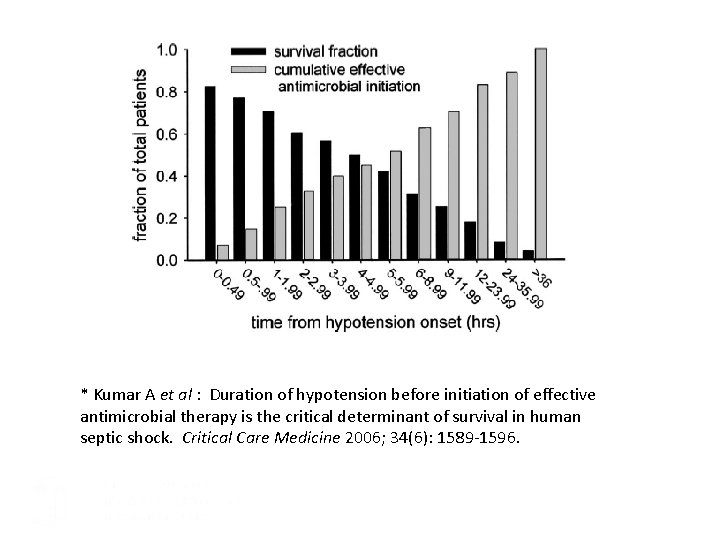
Wake Forest reduced their time to first antibiotic significantly. Time to Antibiotic Administration Is the Most Important Predictor of Survival in Septic Shock* 0. 9 WFBMC Code Sepsis average time is 53 0. 8 Survival Fraction 0. 7 6 hours considered “Early” Sepsis management 0. 6 0. 5 0. 4 0. 3 0. 2 0. 1 0 0. 5 1 2 3 4 5 6 Hours 7 to 9 10 to 12 13 to 24 25 to 35 >36 *Kumar A et al : Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Critical Care Medicine 2006; 34(6): 1589 -1596.

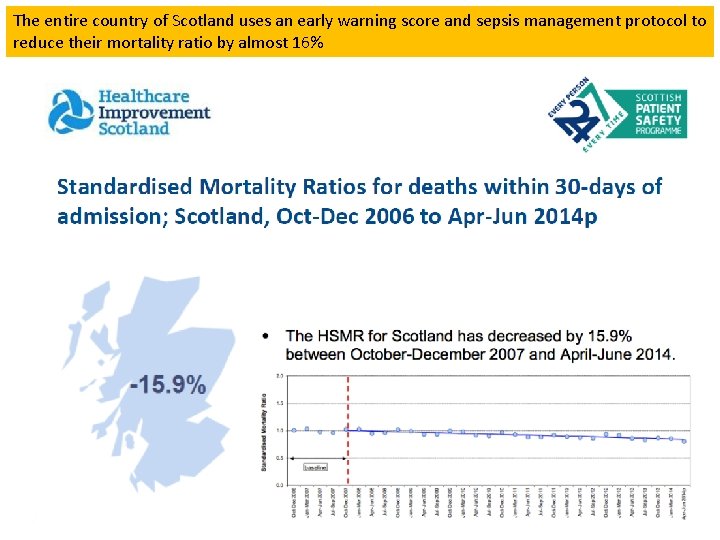
Scotland is using an Early Warning Score, an advanced sepsis screen, and a one hour bundle.
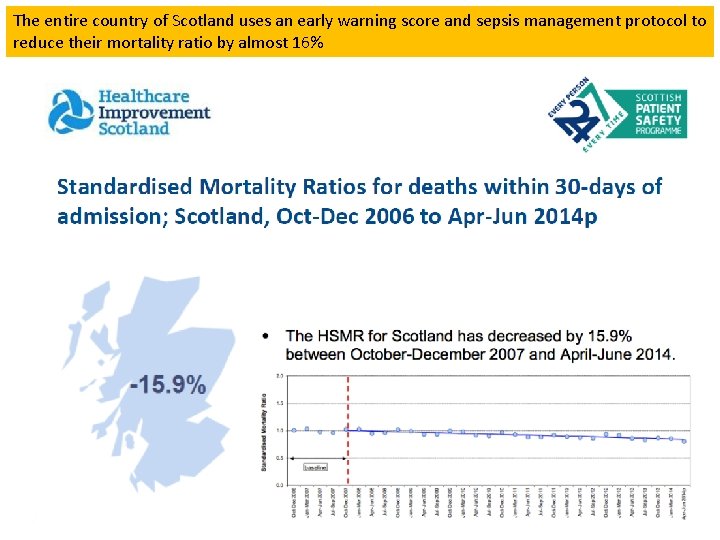
The entire country of Scotland uses an early warning score and sepsis management protocol to reduce their mortality ratio by almost 16%

North Shore University Hospital in Long Island Jewish system reduced ALOS and Mortality.
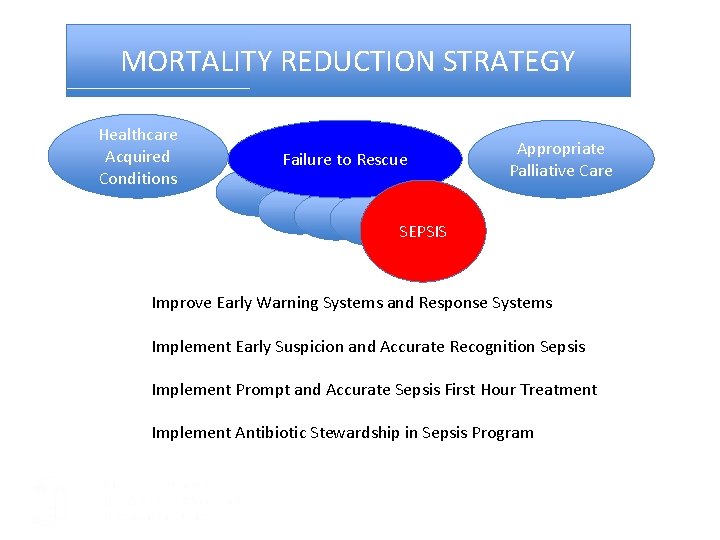
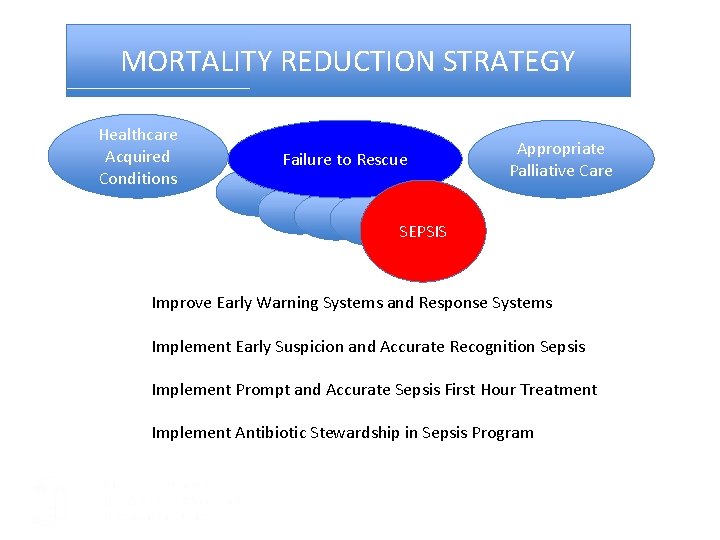
MORTALITY REDUCTION STRATEGY Healthcare Acquired Conditions Failure to Rescue Appropriate Palliative Care SEPSIS Improve Early Warning Systems and Response Systems Implement Early Suspicion and Accurate Recognition Sepsis Implement Prompt and Accurate Sepsis First Hour Treatment Implement Antibiotic Stewardship in Sepsis Program
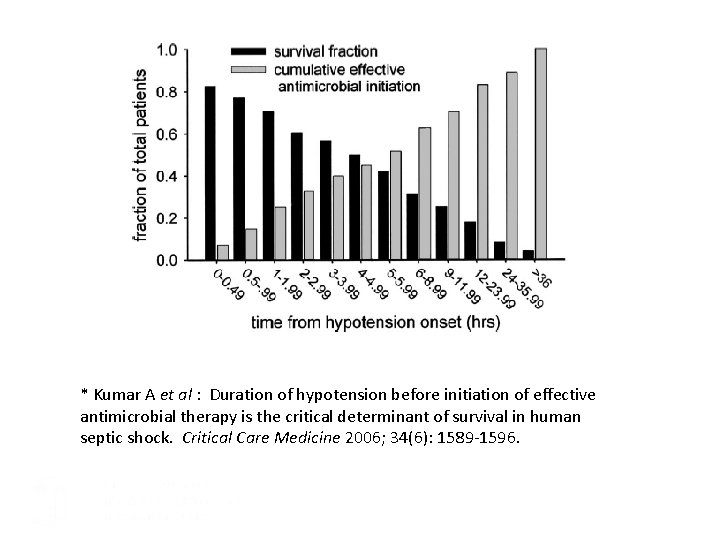
* Kumar A et al : Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Critical Care Medicine 2006; 34(6): 1589 -1596.
Sepsis Program Overview • Triage and Screening System for rapid recognition • Rapid treatment with antibiotics and fluid resuscitation, lactate, CBC, and blood cultures • Each area will have representation on implementation teams • Adaptation of best practices from centers of excellence
Complacency, Education & Trying Harder isn’t enough
3 Recent Large Randomized Control Trials: Although advanced severe sepsis therapies (such as central line placement, SVO 2 goals, etc) did not show improved outcomes, all were randomized after early recognition and standard therapies including antibiotics and fluid resuscitation which are the goals of UNC Code Sepsis
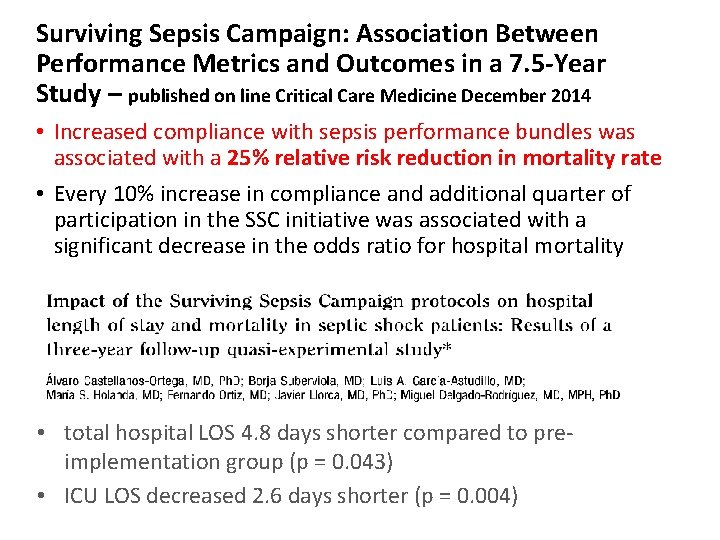
Surviving Sepsis Campaign: Association Between Performance Metrics and Outcomes in a 7. 5 -Year Study – published on line Critical Care Medicine December 2014 • Increased compliance with sepsis performance bundles was associated with a 25% relative risk reduction in mortality rate • Every 10% increase in compliance and additional quarter of participation in the SSC initiative was associated with a significant decrease in the odds ratio for hospital mortality • total hospital LOS 4. 8 days shorter compared to preimplementation group (p = 0. 043) • ICU LOS decreased 2. 6 days shorter (p = 0. 004)
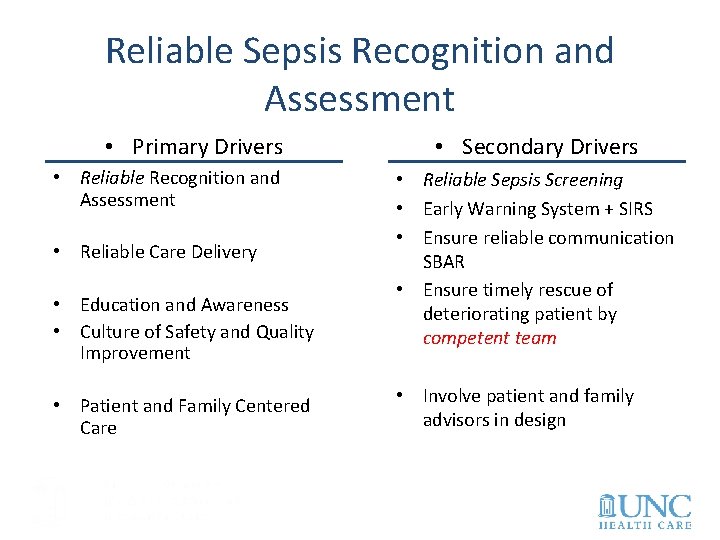
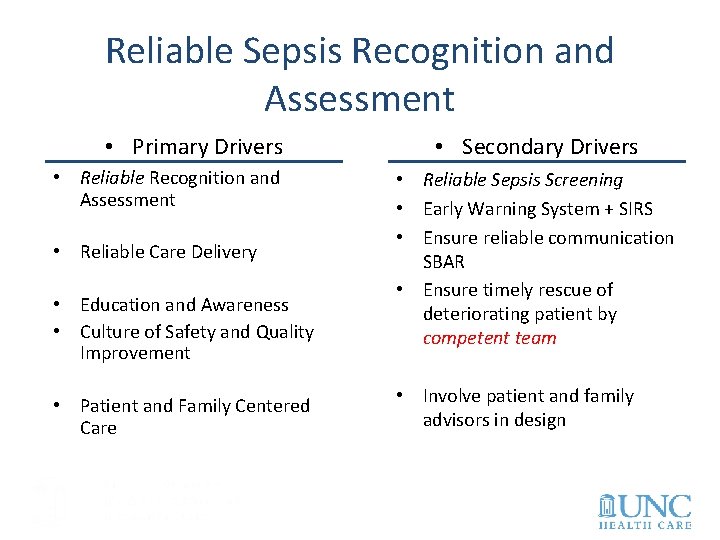
Reliable Sepsis Recognition and Assessment • Primary Drivers • Reliable Recognition and Assessment • Reliable Care Delivery • Education and Awareness • Culture of Safety and Quality Improvement • Patient and Family Centered Care • Secondary Drivers • Reliable Sepsis Screening • Early Warning System + SIRS • Ensure reliable communication SBAR • Ensure timely rescue of deteriorating patient by competent team • Involve patient and family advisors in design
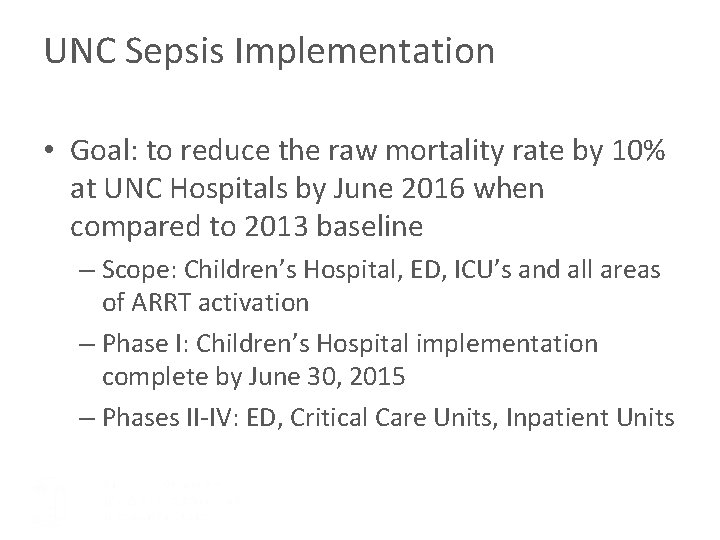
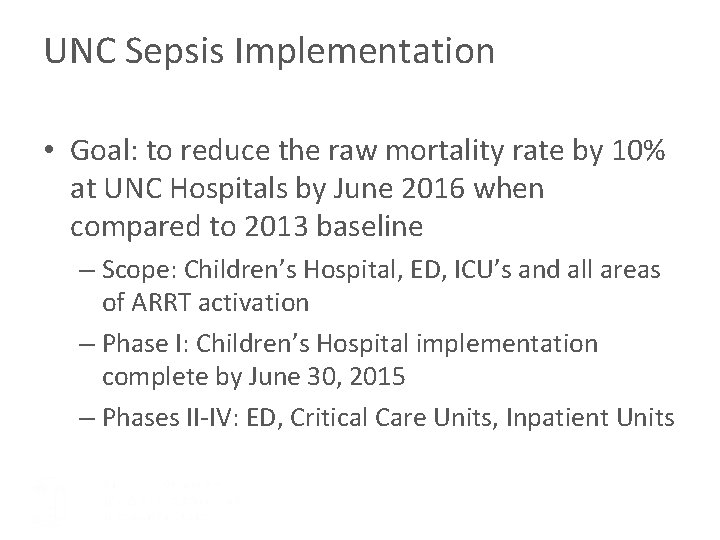
UNC Sepsis Implementation • Goal: to reduce the raw mortality rate by 10% at UNC Hospitals by June 2016 when compared to 2013 baseline – Scope: Children’s Hospital, ED, ICU’s and all areas of ARRT activation – Phase I: Children’s Hospital implementation complete by June 30, 2015 – Phases II-IV: ED, Critical Care Units, Inpatient Units

Project Updates

UNC Children’s Hospital Working Timeline Sep-14 Oct-14 Nov-14 Dec-14 Jan-15 Feb-15 Mar-15 Apr-15 May-15 Jun-15 Jul-15 Aug-15 Sep-15 Peds ED implementation Peds Acute Care Screening Implementaion Peds Clinics Screening Implementation NCCC standardized protocol NBN Screening Implementation Measurement Administration Educational Spread Plan Go Live PRRT Training and Response Soft Start Expert Panel Recommendations
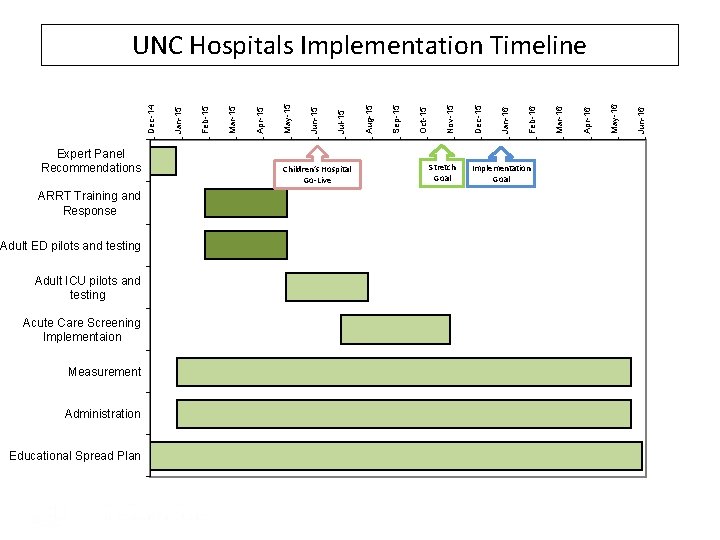
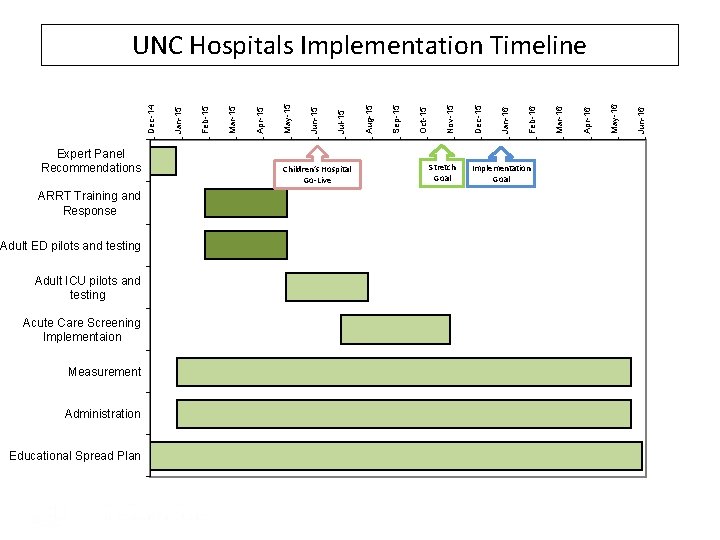
Expert Panel Recommendations ARRT Training and Response Adult ED pilots and testing Adult ICU pilots and testing Acute Care Screening Implementaion Measurement Administration Educational Spread Plan Children’s Hospital Go-Live Stretch Goal Implementation Goal Jun-16 May-16 Apr-16 Mar-16 Feb-16 Jan-16 Dec-15 Nov-15 Oct-15 Sep-15 Aug-15 Jul-15 Jun-15 May-15 Apr-15 Mar-15 Feb-15 Jan-15 Dec-14 UNC Hospitals Implementation Timeline
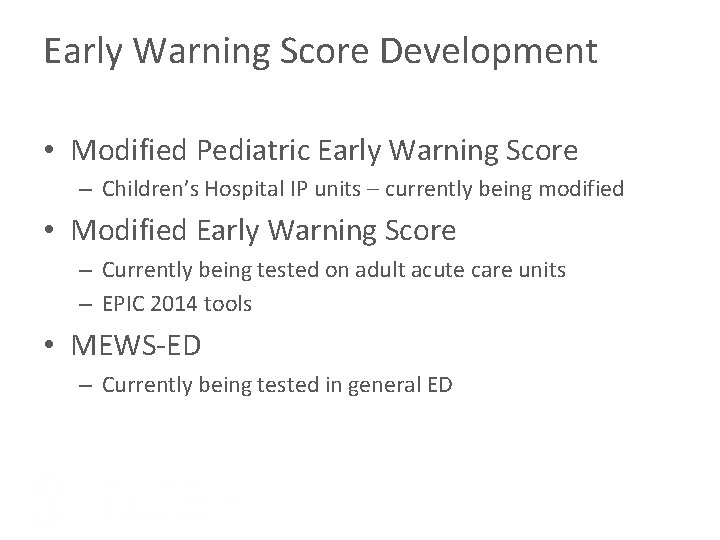
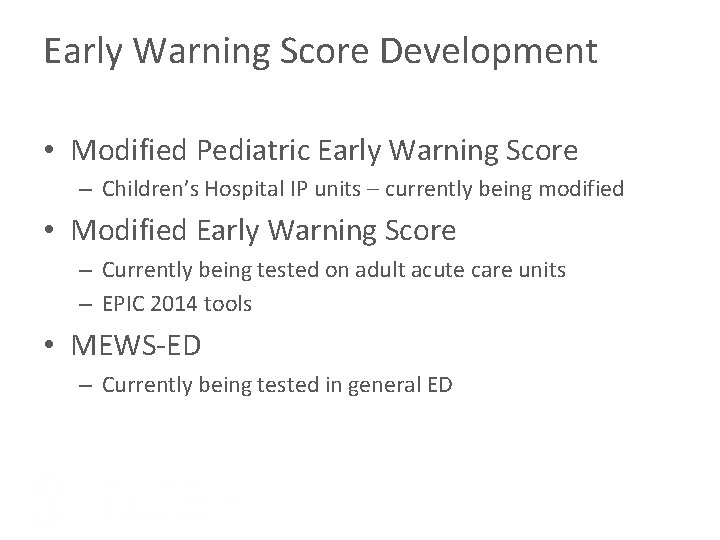
Early Warning Score Development • Modified Pediatric Early Warning Score – Children’s Hospital IP units – currently being modified • Modified Early Warning Score – Currently being tested on adult acute care units – EPIC 2014 tools • MEWS-ED – Currently being tested in general ED
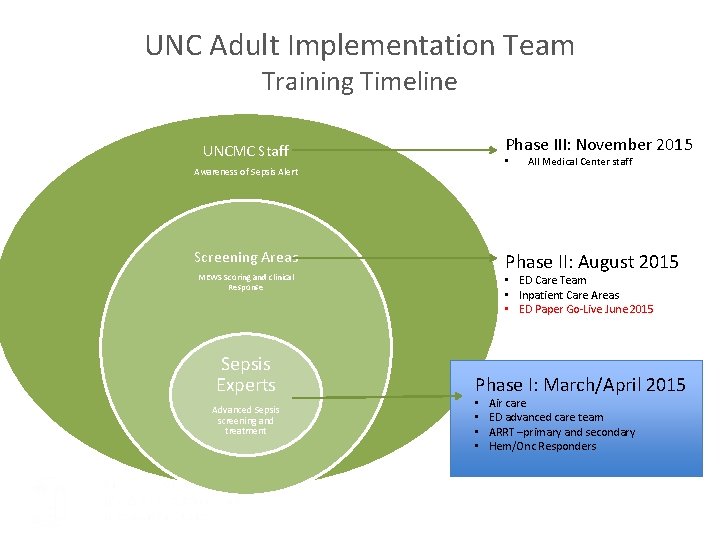
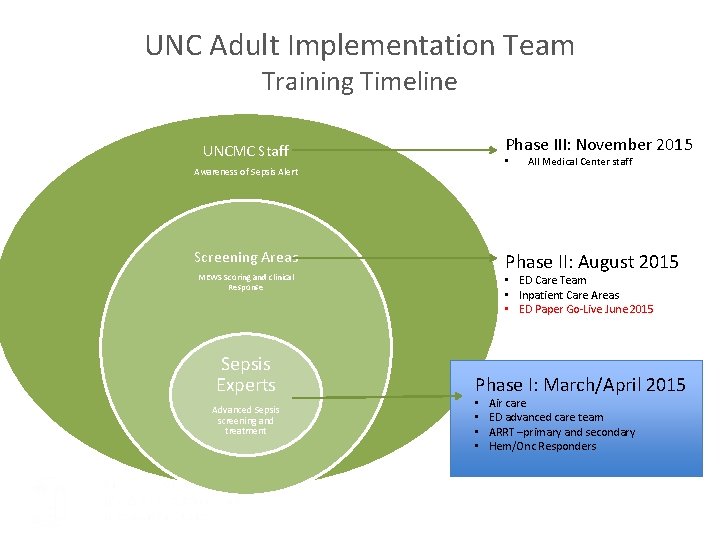
UNC Adult Implementation Team Training Timeline Phase III: November 2015 UNCMC Staff • Awareness of Sepsis Alert Screening Areas Phase II: August 2015 MEWS Scoring and clinical Response Sepsis Experts Advanced Sepsis screening and treatment All Medical Center staff • ED Care Team • Inpatient Care Areas • ED Paper Go-Live June 2015 Phase I: March/April 2015 • • Air care ED advanced care team ARRT –primary and secondary Hem/Onc Responders
Working Adult Patient Bundle
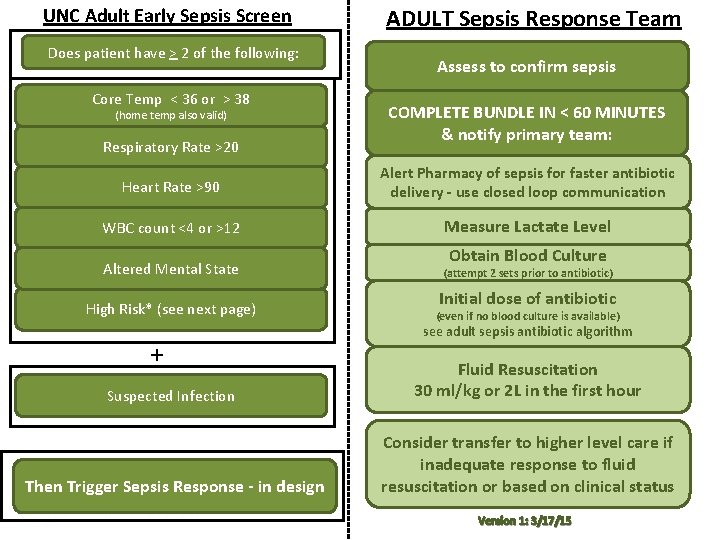
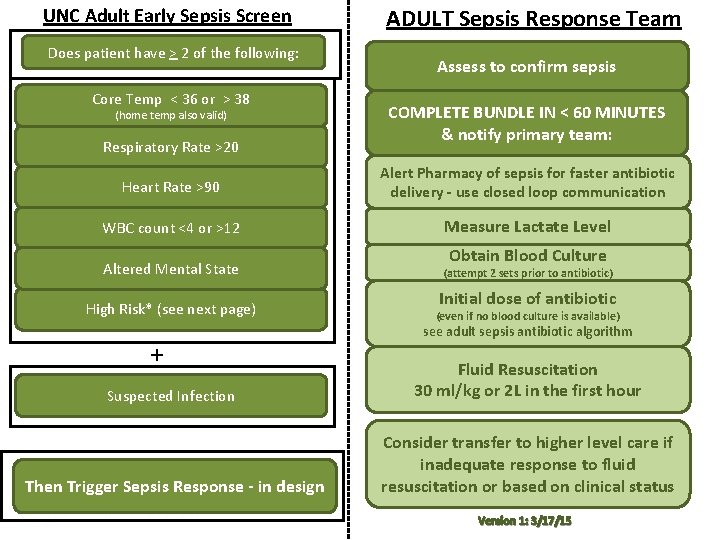
UNC Adult Early Sepsis Screen Does patient have > 2 of the following: Core Temp < 36 or > 38 (home temp also valid) Respiratory Rate >20 ADULT Sepsis Response Team Assess to confirm sepsis COMPLETE BUNDLE IN < 60 MINUTES & notify primary team: Heart Rate >90 Alert Pharmacy of sepsis for faster antibiotic delivery - use closed loop communication WBC count <4 or >12 Measure Lactate Level Obtain Blood Culture Altered Mental State (attempt 2 sets prior to antibiotic) High Risk* (see next page) (even if no blood culture is available) + Initial dose of antibiotic see adult sepsis antibiotic algorithm Suspected Infection Fluid Resuscitation 30 ml/kg or 2 L in the first hour Then Trigger Sepsis Response - in design Consider transfer to higher level care if inadequate response to fluid resuscitation or based on clinical status Version 1: 3/17/15
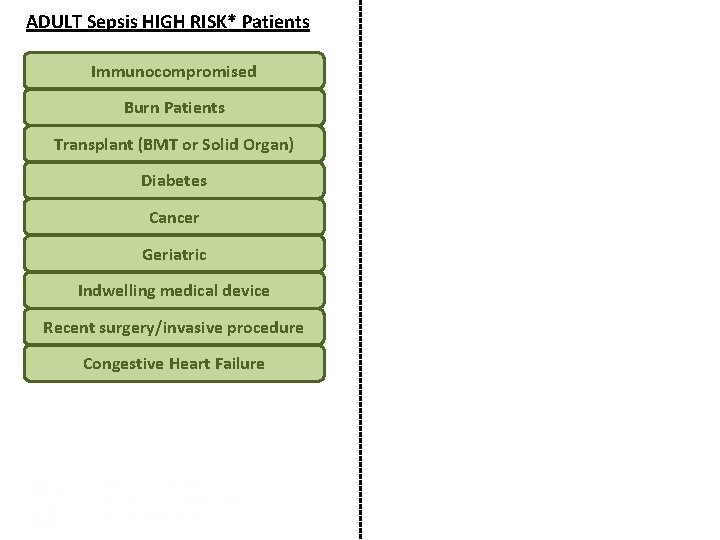
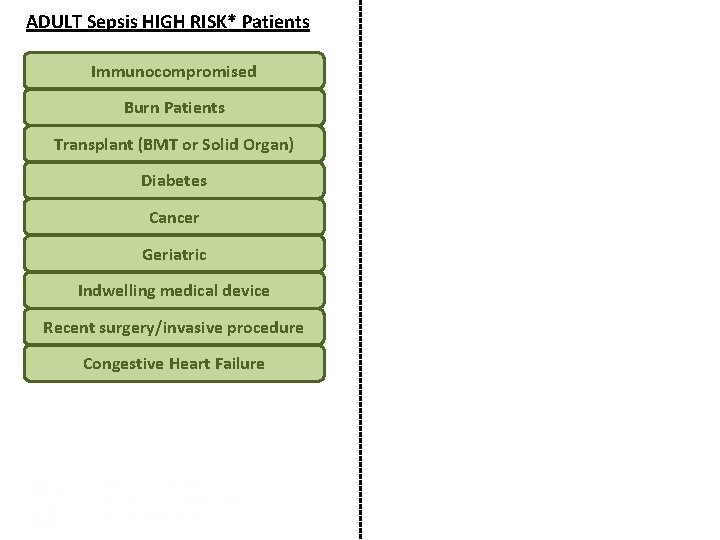
ADULT Sepsis HIGH RISK* Patients Immunocompromised Burn Patients Transplant (BMT or Solid Organ) Diabetes Cancer Geriatric Indwelling medical device Recent surgery/invasive procedure Congestive Heart Failure
When in doubt… • Think to yourself first, “This is sepsis!” • Then ask, “Why isn’t this sepsis? ” • When no other reason found, then conclude, “Oh wait, it is sepsis. ”

Placeholder Adult Patient Sepsis Antibiotic Guidelines
Sepsis Case Reviews
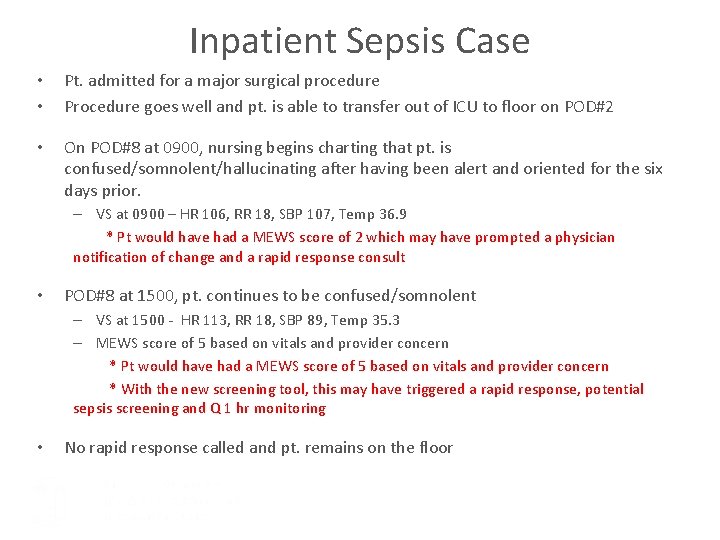
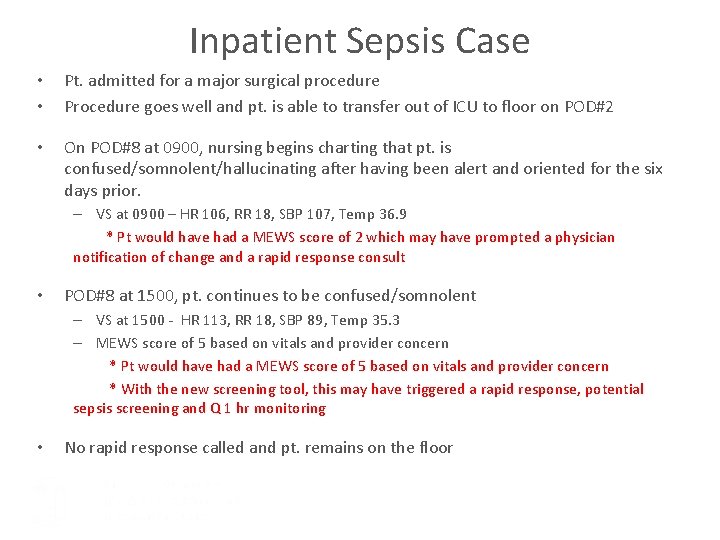
Inpatient Sepsis Case • • Pt. admitted for a major surgical procedure Procedure goes well and pt. is able to transfer out of ICU to floor on POD#2 • On POD#8 at 0900, nursing begins charting that pt. is confused/somnolent/hallucinating after having been alert and oriented for the six days prior. – VS at 0900 – HR 106, RR 18, SBP 107, Temp 36. 9 * Pt would have had a MEWS score of 2 which may have prompted a physician notification of change and a rapid response consult • POD#8 at 1500, pt. continues to be confused/somnolent – VS at 1500 - HR 113, RR 18, SBP 89, Temp 35. 3 – MEWS score of 5 based on vitals and provider concern * Pt would have had a MEWS score of 5 based on vitals and provider concern * With the new screening tool, this may have triggered a rapid response, potential sepsis screening and Q 1 hr monitoring • No rapid response called and pt. remains on the floor

Inpatient Sepsis Case • 20 hrs later, at 1100 on POD#9, nurse charts that pt. was extremely confused and hallucinating – VS at 1100 – HR 120, RR 18, SBP 81, Temp 35. 6 – No urine output since POD#8 at 2200 • POD#9 MD note states that sepsis suspected – Blood culture ordered at 1210 – 2250 ml of Albumin 5% given between 1225 and 1809 • Pt. weighed 81. 6 kg – Zosyn ordered and first dose given at 1326 – Vanc ordered and first dose given at 1830 • • • First lactate not drawn until POD#10 at 1530 Pt. transferred to SICU at 1458 on POD#9 Pt. eventually passed away 1 month post procedure
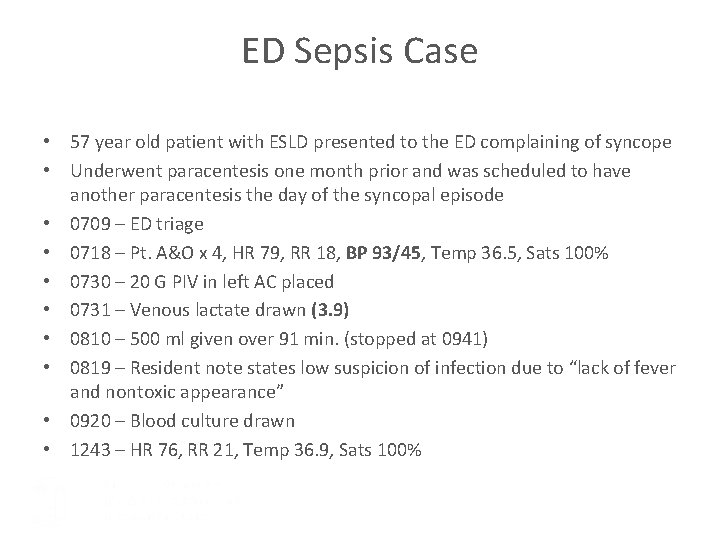
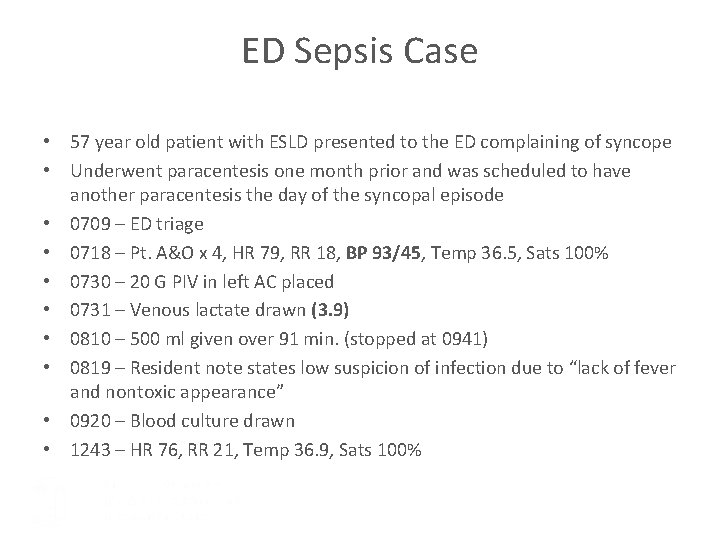
ED Sepsis Case • 57 year old patient with ESLD presented to the ED complaining of syncope • Underwent paracentesis one month prior and was scheduled to have another paracentesis the day of the syncopal episode • 0709 – ED triage • 0718 – Pt. A&O x 4, HR 79, RR 18, BP 93/45, Temp 36. 5, Sats 100% • 0730 – 20 G PIV in left AC placed • 0731 – Venous lactate drawn (3. 9) • 0810 – 500 ml given over 91 min. (stopped at 0941) • 0819 – Resident note states low suspicion of infection due to “lack of fever and nontoxic appearance” • 0920 – Blood culture drawn • 1243 – HR 76, RR 21, Temp 36. 9, Sats 100%
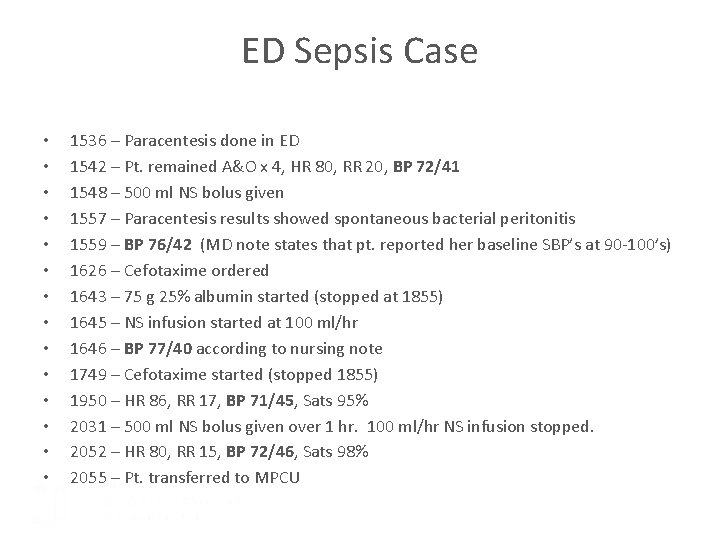
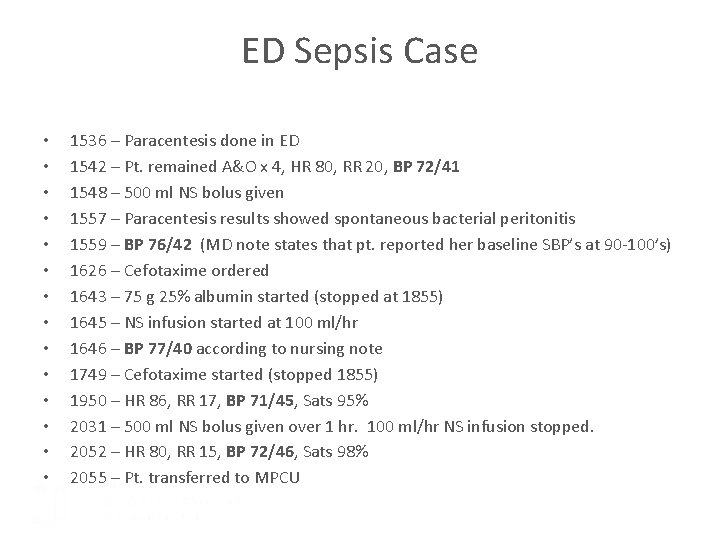
ED Sepsis Case • • • • 1536 – Paracentesis done in ED 1542 – Pt. remained A&O x 4, HR 80, RR 20, BP 72/41 1548 – 500 ml NS bolus given 1557 – Paracentesis results showed spontaneous bacterial peritonitis 1559 – BP 76/42 (MD note states that pt. reported her baseline SBP’s at 90 -100’s) 1626 – Cefotaxime ordered 1643 – 75 g 25% albumin started (stopped at 1855) 1645 – NS infusion started at 100 ml/hr 1646 – BP 77/40 according to nursing note 1749 – Cefotaxime started (stopped 1855) 1950 – HR 86, RR 17, BP 71/45, Sats 95% 2031 – 500 ml NS bolus given over 1 hr. 100 ml/hr NS infusion stopped. 2052 – HR 80, RR 15, BP 72/46, Sats 98% 2055 – Pt. transferred to MPCU
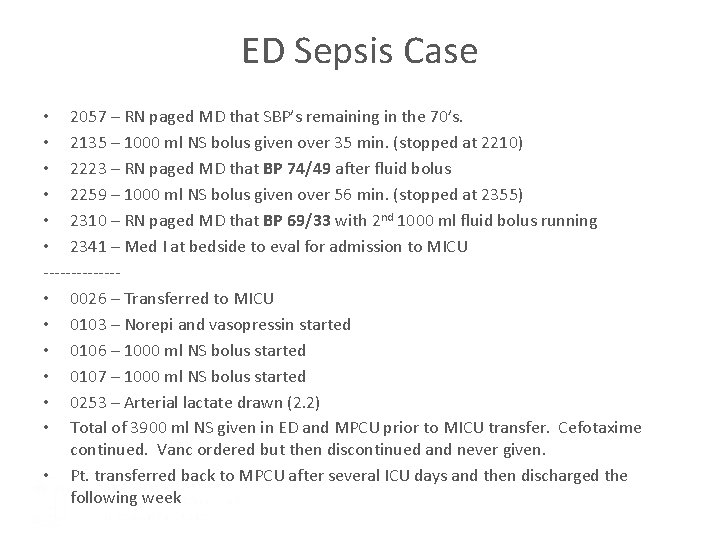
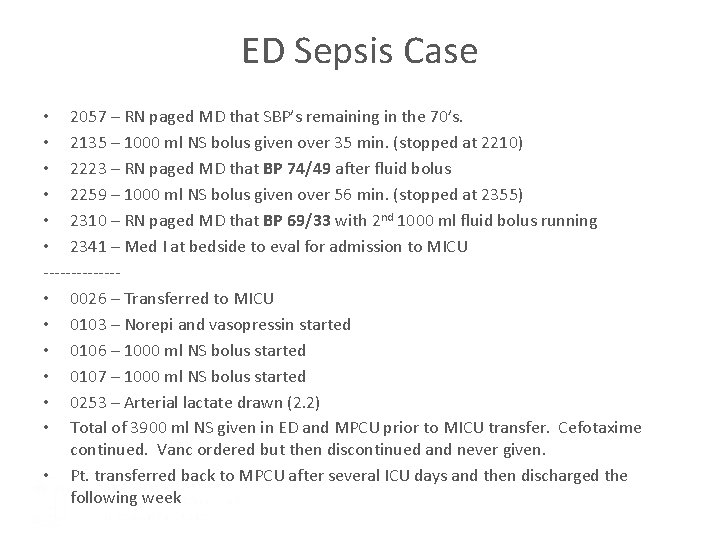
ED Sepsis Case • 2057 – RN paged MD that SBP’s remaining in the 70’s. • 2135 – 1000 ml NS bolus given over 35 min. (stopped at 2210) • 2223 – RN paged MD that BP 74/49 after fluid bolus • 2259 – 1000 ml NS bolus given over 56 min. (stopped at 2355) • 2310 – RN paged MD that BP 69/33 with 2 nd 1000 ml fluid bolus running • 2341 – Med I at bedside to eval for admission to MICU ------- • 0026 – Transferred to MICU • 0103 – Norepi and vasopressin started • 0106 – 1000 ml NS bolus started • 0107 – 1000 ml NS bolus started • 0253 – Arterial lactate drawn (2. 2) • Total of 3900 ml NS given in ED and MPCU prior to MICU transfer. Cefotaxime continued. Vanc ordered but then discontinued and never given. • Pt. transferred back to MPCU after several ICU days and then discharged the following week
Placeholder Area Screening and Treatment Plan
Take Home Points • This new system is still in design and will be different in the coming months when we “go live” • Septic Shock may be more subtle than you think • Call sepsis team (RRT for inpatient units – triggered ED response in ED) for rapid IV access, fluid administration, antibiotic arrival, and lab studies – all bundle elements • Patients can worsen rapidly • If you want to help us in the development or have feedback please contact the Sepsis Program Team: sepsisfeedbackunch@unchealth. unc. edu

Communication Tools
Intranet Site Resources>Performance Improvement and Patient Safety>Sepsis Program Content: Background Resources Sepsis Toolkit FAQs Need Help?