UNC Hospitals Sepsis Mortality Reduction Initiative Code Sepsis



- Slides: 67
UNC Hospitals Sepsis Mortality Reduction Initiative Code Sepsis Emergency Medicine Sepsis Training Updated 3. 23. 16
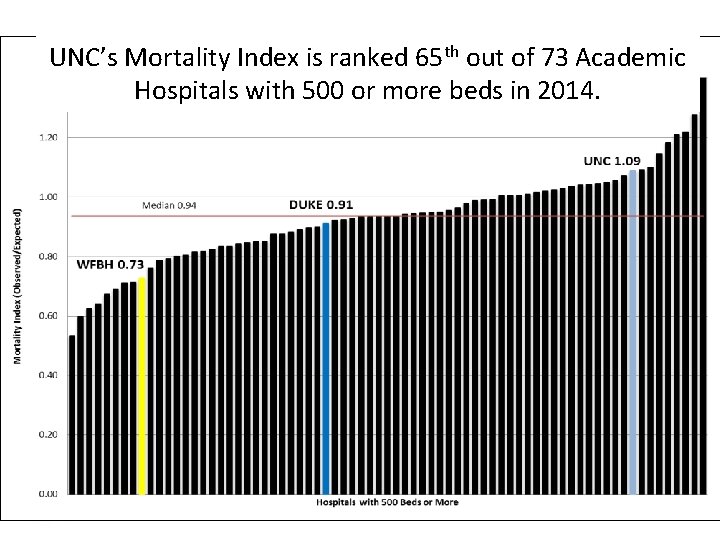
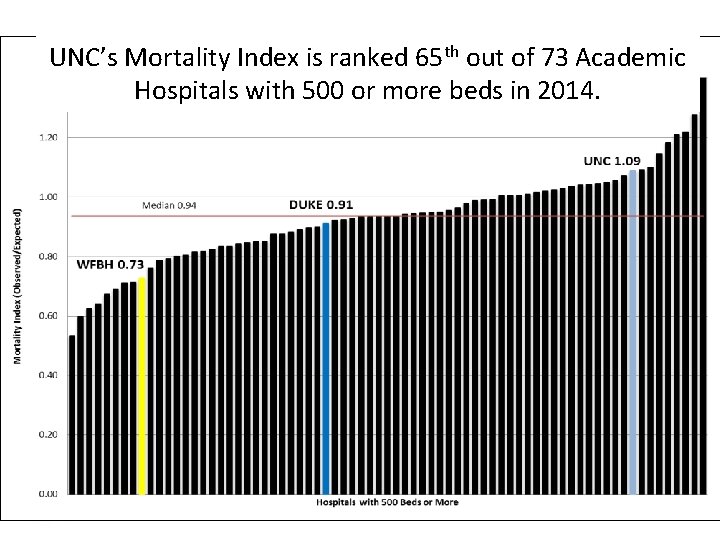
UNC’s Mortality Index is ranked 65 th out of 73 Academic Hospitals with 500 or more beds in 2014.
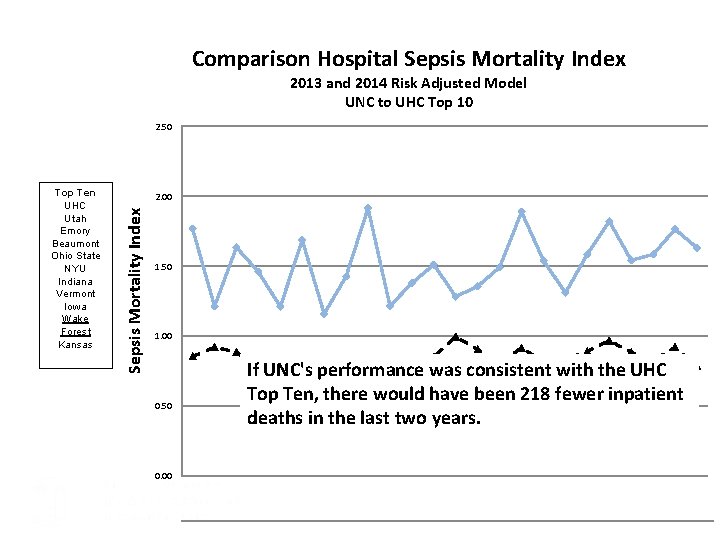
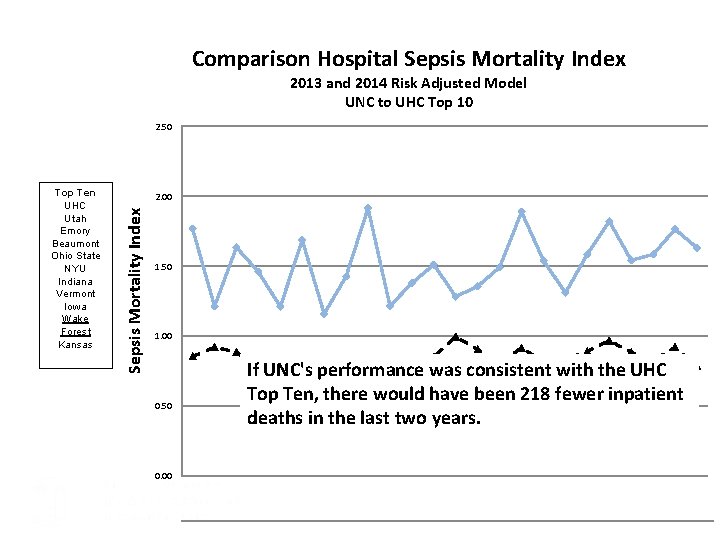
Comparison Hospital Sepsis Mortality Index 2013 and 2014 Risk Adjusted Model UNC to UHC Top 10 2. 50 2. 00 Sepsis Mortality Index Top Ten UHC Utah Emory Beaumont Ohio State NYU Indiana Vermont Iowa Wake Forest Kansas 1. 50 1. 00 0. 50 If UNC's performance was consistent with the UHC Top Ten, there would have been 218 fewer inpatient deaths in the last two years. 0. 00 UNC Sepsis Mortality Index 1. 77 1. 21 1. 63 1. 46 1. 21 1. 69 1. 16 1. 43 1. 91 1. 21 1. 38 1. 51 1. 28 1. 36 1. 49 1. 89 1. 54 1. 31 1. 59 1. 82 1. 54 1. 58 1. 76 1. 63
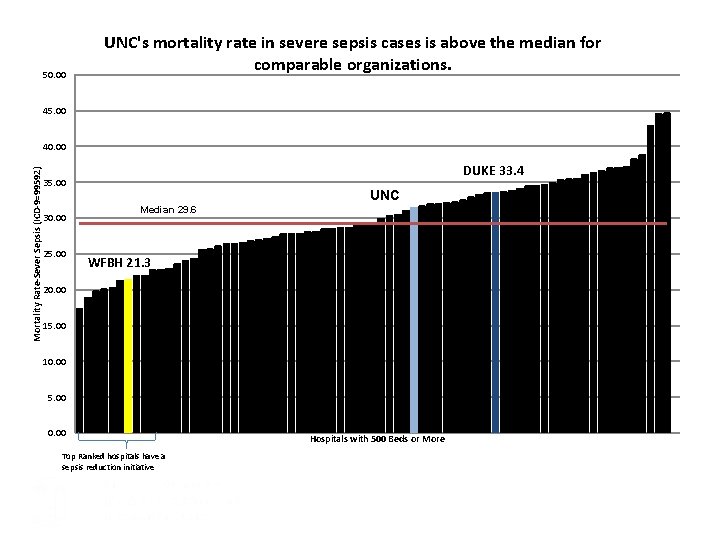
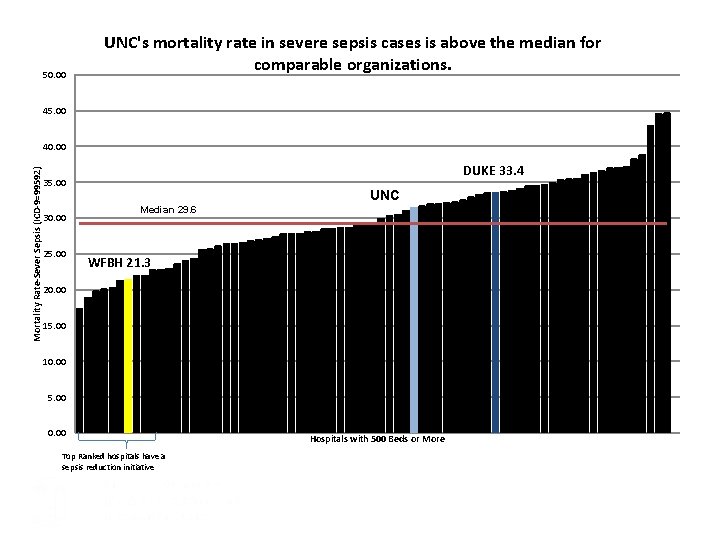
50. 00 UNC's mortality rate in severe sepsis cases is above the median for comparable organizations. 45. 00 Mortality Rate-Sever Sepsis (ICD-9=99592) 40. 00 DUKE 33. 4 35. 00 30. 00 25. 00 UNC Median 29. 6 WFBH 21. 3 20. 00 15. 00 10. 00 5. 00 0. 00 Top Ranked hospitals have a sepsis reduction initiative Hospitals with 500 Beds or More
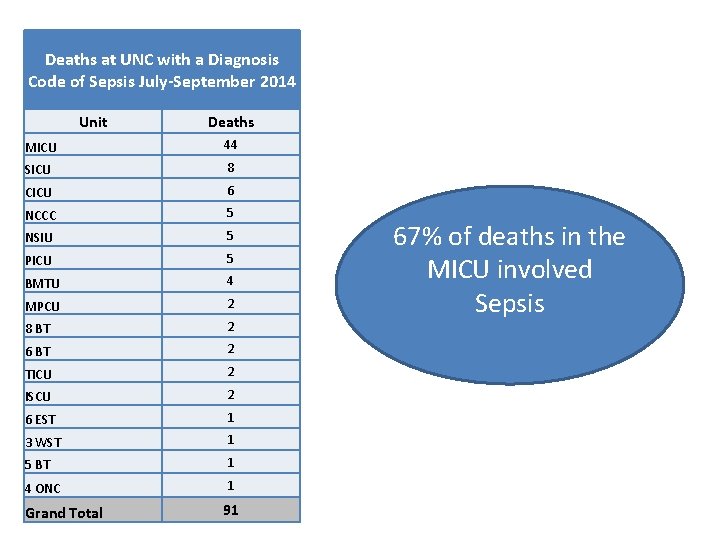
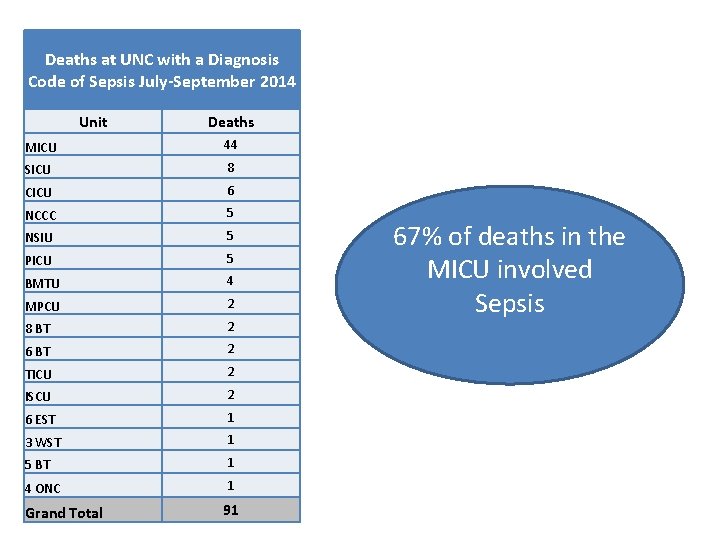
Deaths at UNC with a Diagnosis Code of Sepsis July-September 2014 Unit Deaths MICU 44 SICU 8 CICU 6 NCCC 5 NSIU 5 PICU 5 BMTU 4 MPCU 2 8 BT 2 6 BT 2 TICU 2 ISCU 2 6 EST 1 3 WST 1 5 BT 1 4 ONC 1 Grand Total 91 67% of deaths in the MICU involved Sepsis
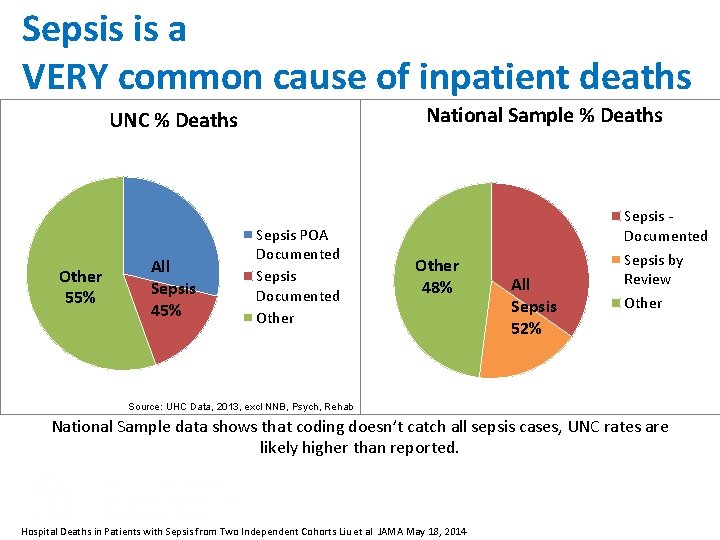
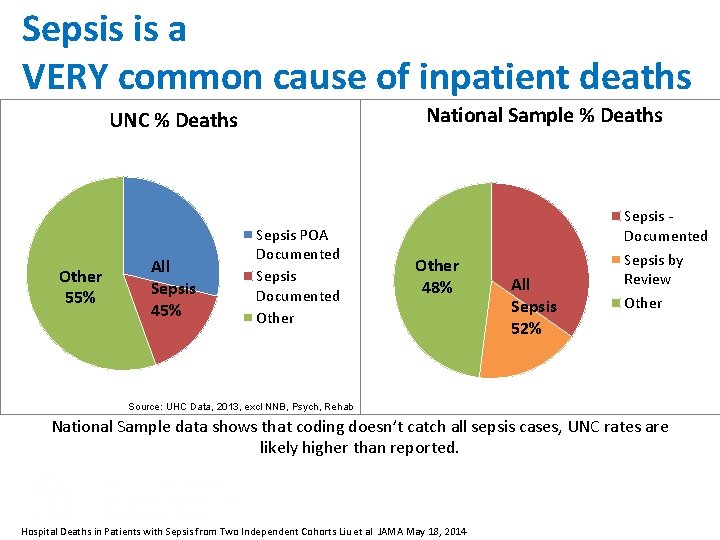
Sepsis is a VERY common cause of inpatient deaths National Sample % Deaths UNC % Deaths Other 55% All Sepsis 45% Sepsis POA Documented Sepsis Documented Other 48% All Sepsis 52% Sepsis by Review Other Source: UHC Data, 2013, excl NNB, Psych, Rehab National Sample data shows that coding doesn’t catch all sepsis cases, UNC rates are likely higher than reported. Hospital Deaths in Patients with Sepsis from Two Independent Cohorts Liu et al JAMA May 18, 2014
Other Organizations with successful sepsis reduction programs • • • Wake Forest Baptist Nation of Scotland Penn State Long Island Jewish Health System Many more
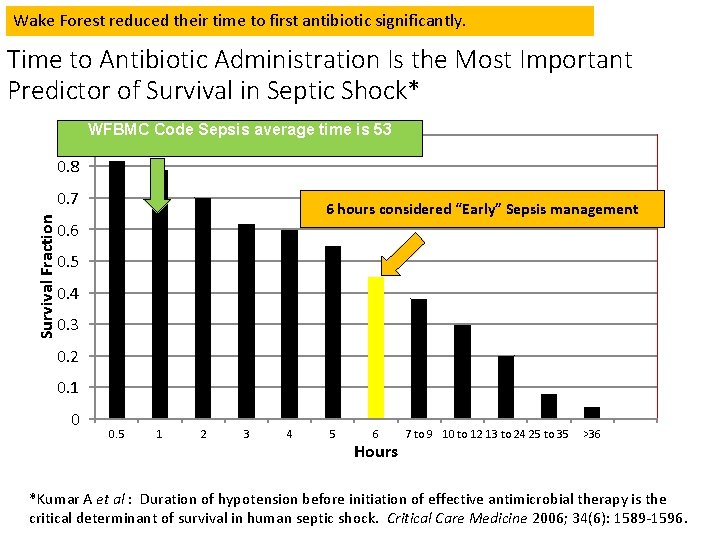
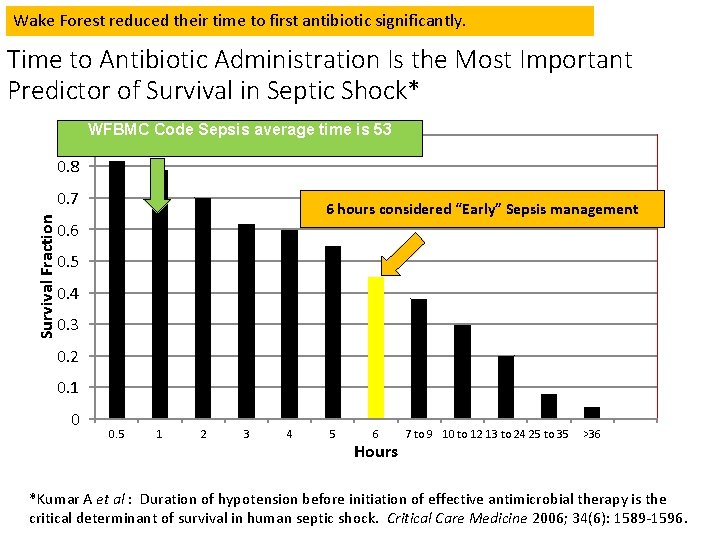
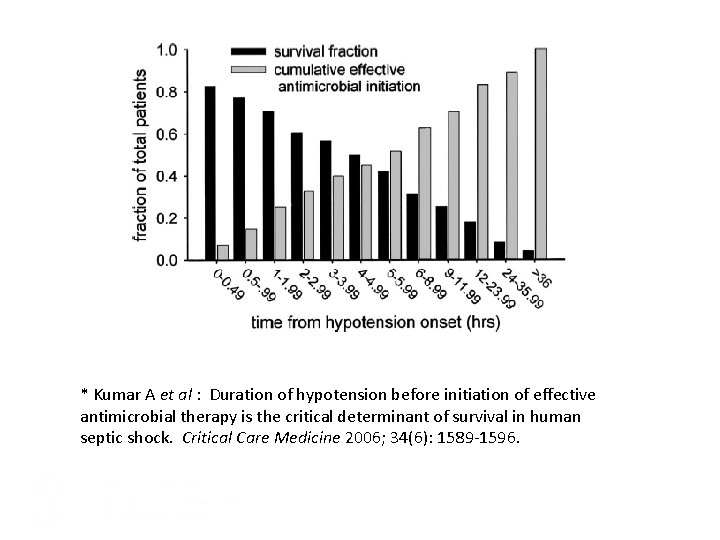
Wake Forest reduced their time to first antibiotic significantly. Time to Antibiotic Administration Is the Most Important Predictor of Survival in Septic Shock* 0. 9 WFBMC Code Sepsis average time is 53 0. 8 Survival Fraction 0. 7 6 hours considered “Early” Sepsis management 0. 6 0. 5 0. 4 0. 3 0. 2 0. 1 0 0. 5 1 2 3 4 5 6 Hours 7 to 9 10 to 12 13 to 24 25 to 35 >36 *Kumar A et al : Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Critical Care Medicine 2006; 34(6): 1589 -1596.
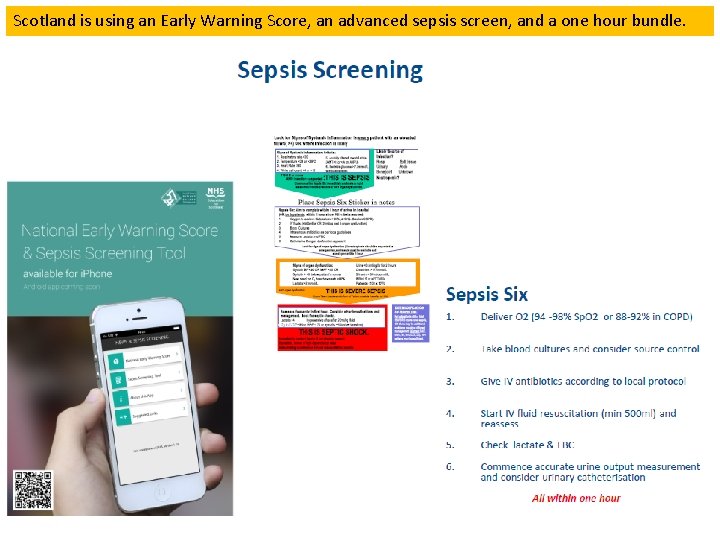
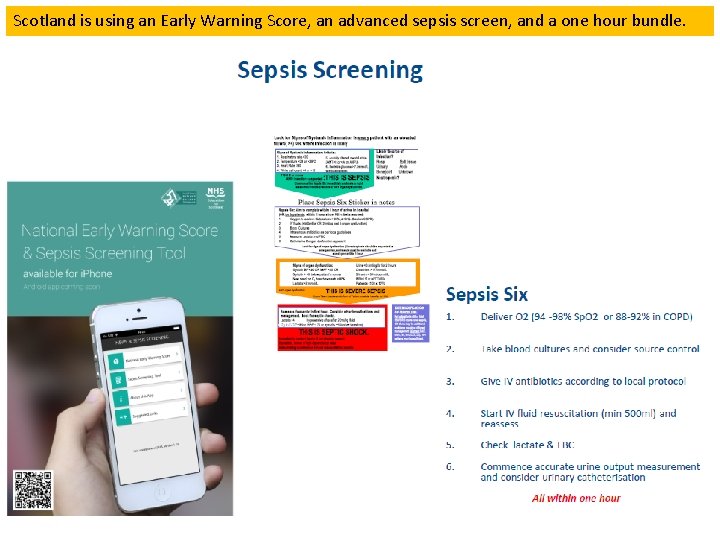
Scotland is using an Early Warning Score, an advanced sepsis screen, and a one hour bundle.
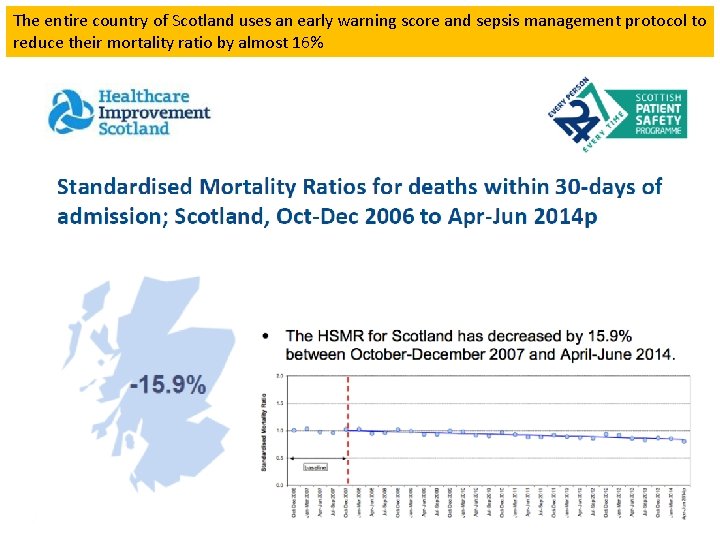
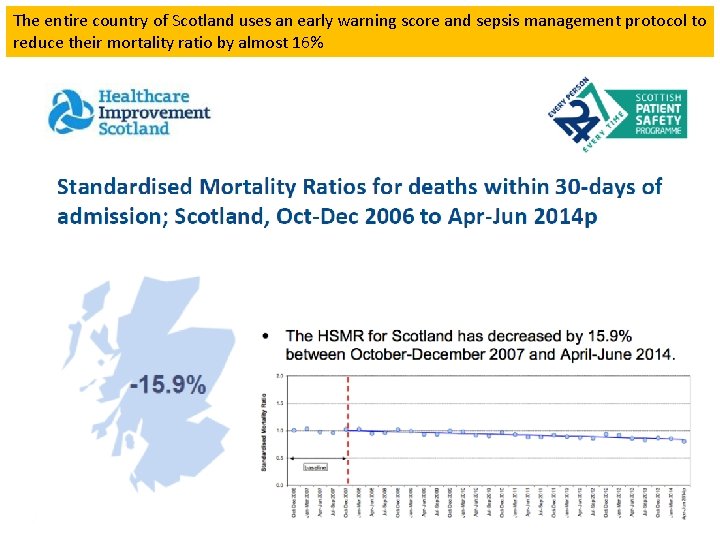
The entire country of Scotland uses an early warning score and sepsis management protocol to reduce their mortality ratio by almost 16%
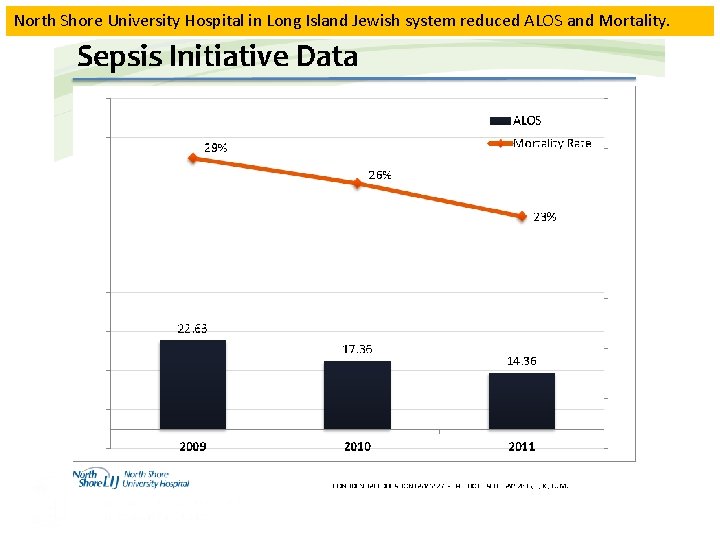
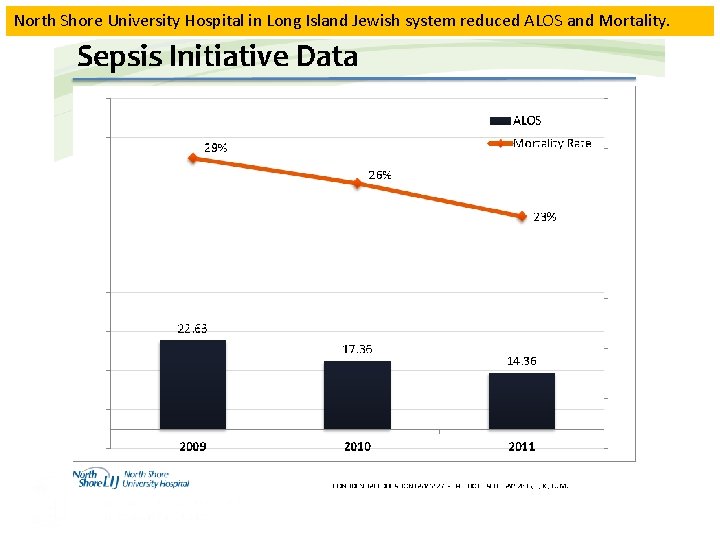
North Shore University Hospital in Long Island Jewish system reduced ALOS and Mortality.
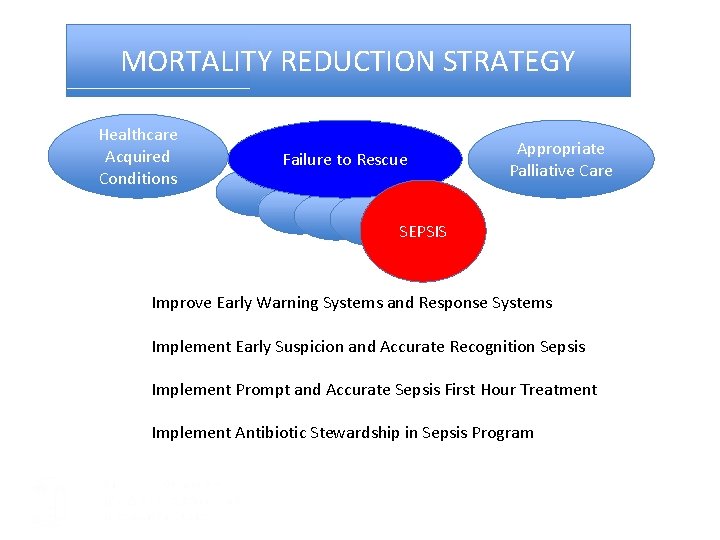
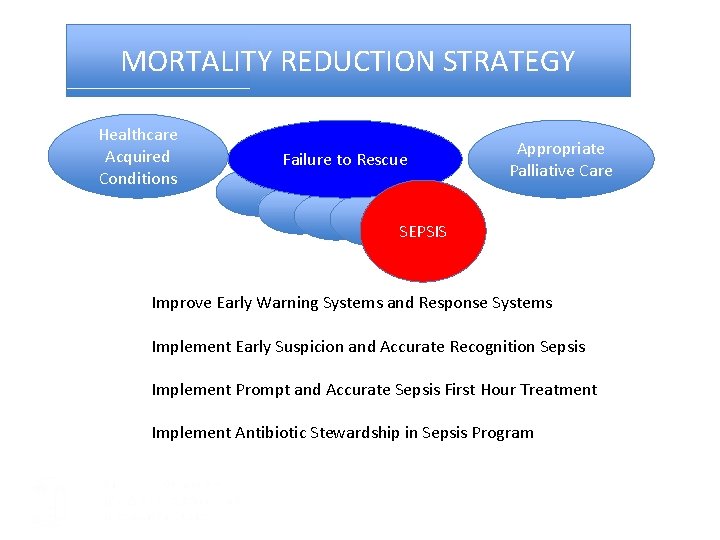
MORTALITY REDUCTION STRATEGY Healthcare Acquired Conditions Failure to Rescue Appropriate Palliative Care SEPSIS Improve Early Warning Systems and Response Systems Implement Early Suspicion and Accurate Recognition Sepsis Implement Prompt and Accurate Sepsis First Hour Treatment Implement Antibiotic Stewardship in Sepsis Program
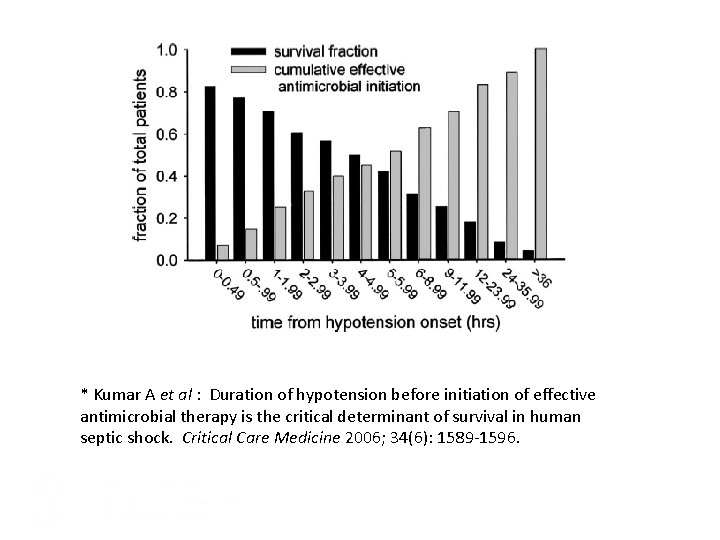
* Kumar A et al : Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Critical Care Medicine 2006; 34(6): 1589 -1596.
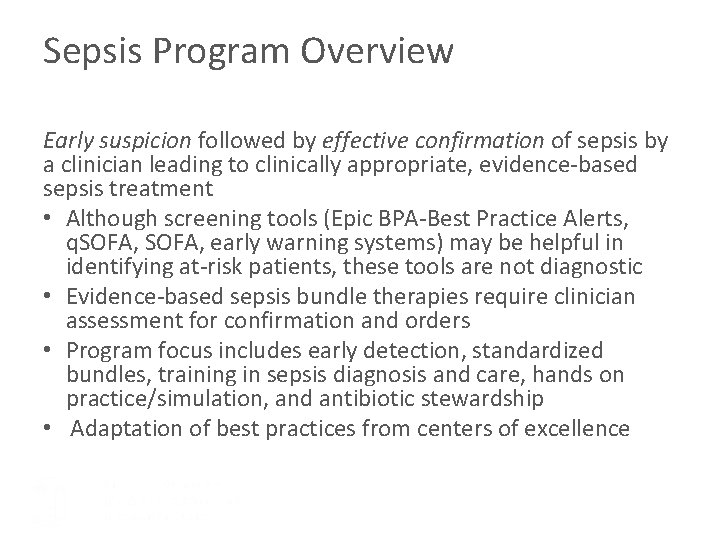
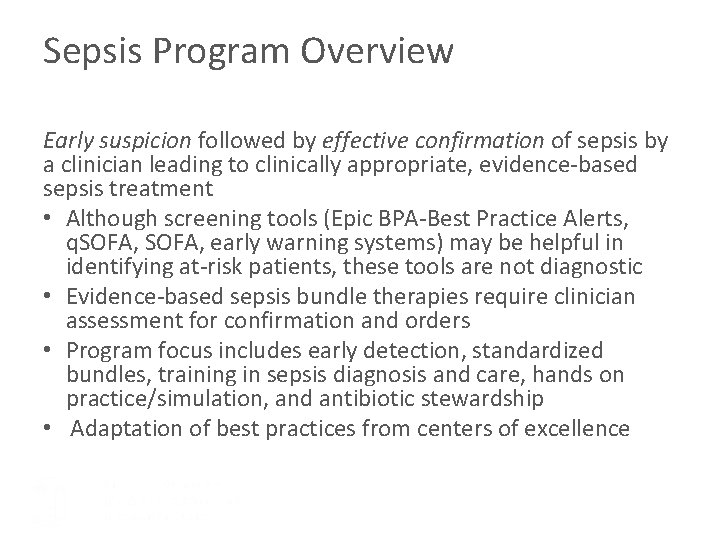
Sepsis Program Overview Early suspicion followed by effective confirmation of sepsis by a clinician leading to clinically appropriate, evidence-based sepsis treatment • Although screening tools (Epic BPA-Best Practice Alerts, q. SOFA, early warning systems) may be helpful in identifying at-risk patients, these tools are not diagnostic • Evidence-based sepsis bundle therapies require clinician assessment for confirmation and orders • Program focus includes early detection, standardized bundles, training in sepsis diagnosis and care, hands on practice/simulation, and antibiotic stewardship • Adaptation of best practices from centers of excellence
Complacency, Education & Trying Harder isn’t enough
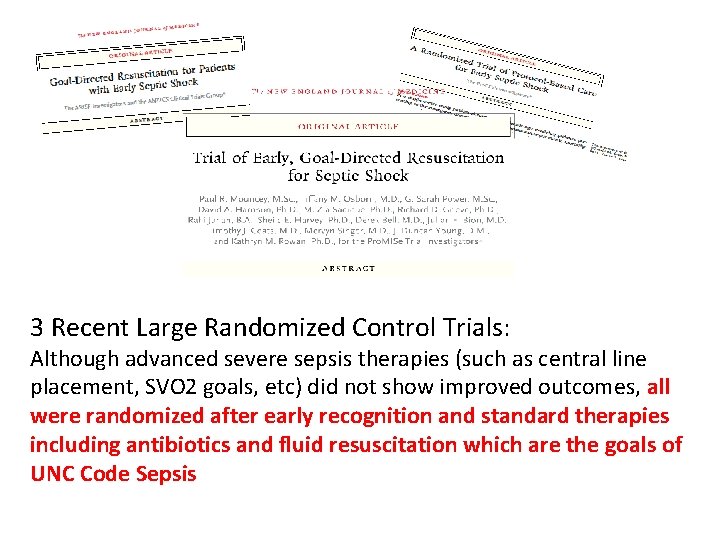
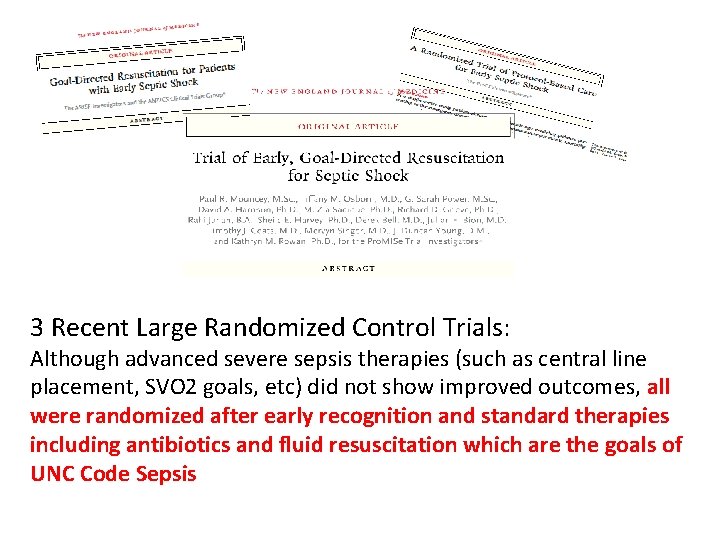
3 Recent Large Randomized Control Trials: Although advanced severe sepsis therapies (such as central line placement, SVO 2 goals, etc) did not show improved outcomes, all were randomized after early recognition and standard therapies including antibiotics and fluid resuscitation which are the goals of UNC Code Sepsis
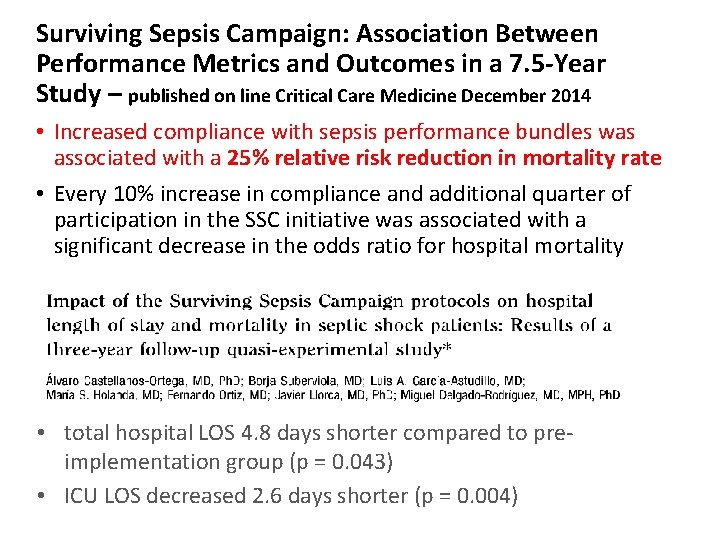
Surviving Sepsis Campaign: Association Between Performance Metrics and Outcomes in a 7. 5 -Year Study – published on line Critical Care Medicine December 2014 • Increased compliance with sepsis performance bundles was associated with a 25% relative risk reduction in mortality rate • Every 10% increase in compliance and additional quarter of participation in the SSC initiative was associated with a significant decrease in the odds ratio for hospital mortality • total hospital LOS 4. 8 days shorter compared to preimplementation group (p = 0. 043) • ICU LOS decreased 2. 6 days shorter (p = 0. 004)
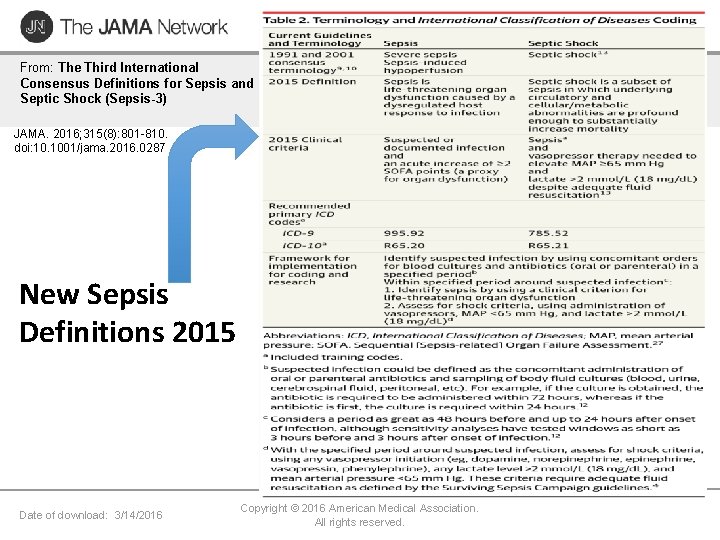
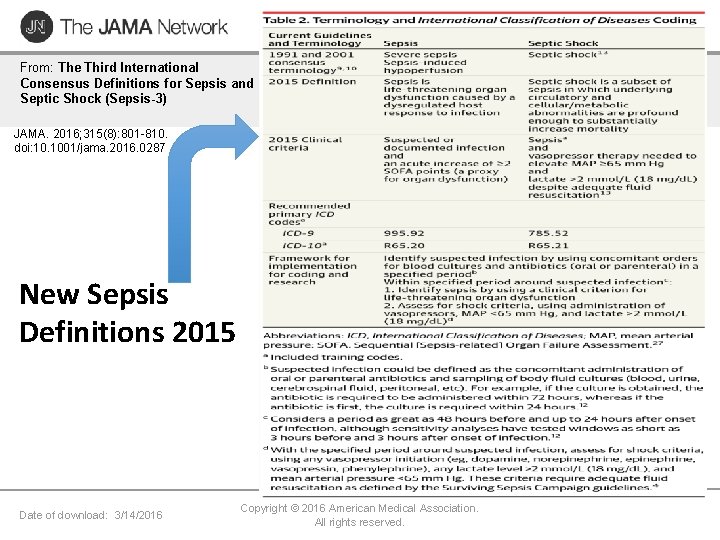
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287 New Sepsis Definitions 2015 Date of download: 3/14/2016 Copyright © 2016 American Medical Association. All rights reserved.
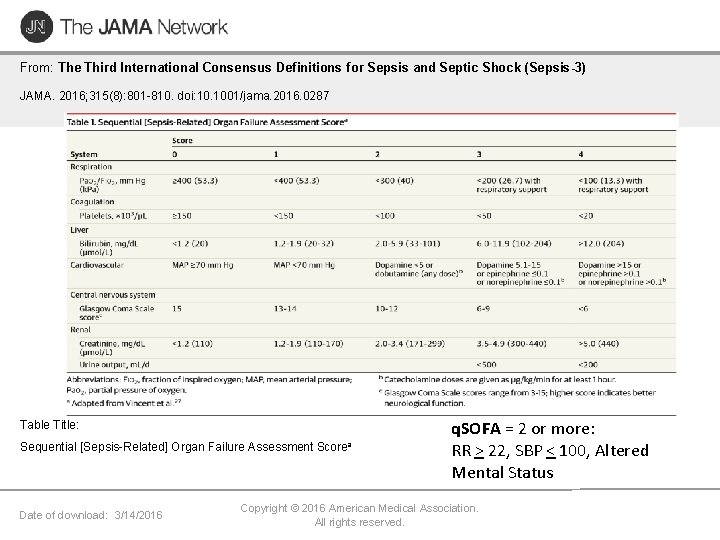
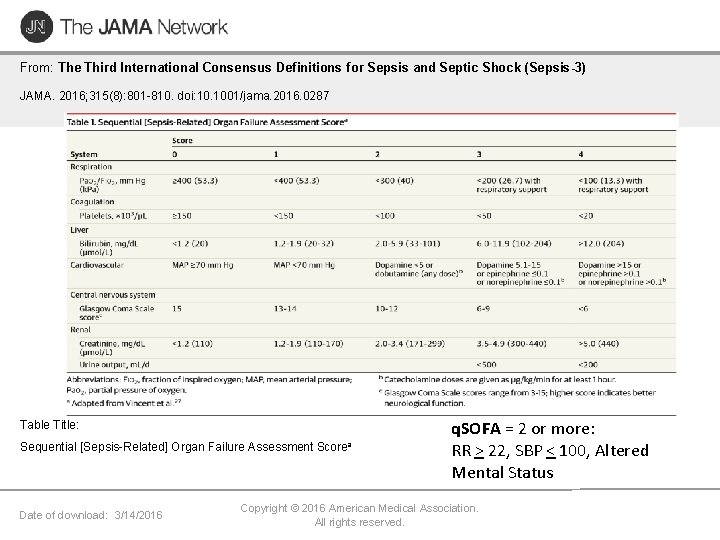
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287 Table Title: Sequential [Sepsis-Related] Organ Failure Assessment Date of download: 3/14/2016 Scorea q. SOFA = 2 or more: RR > 22, SBP < 100, Altered Mental Status Copyright © 2016 American Medical Association. All rights reserved.
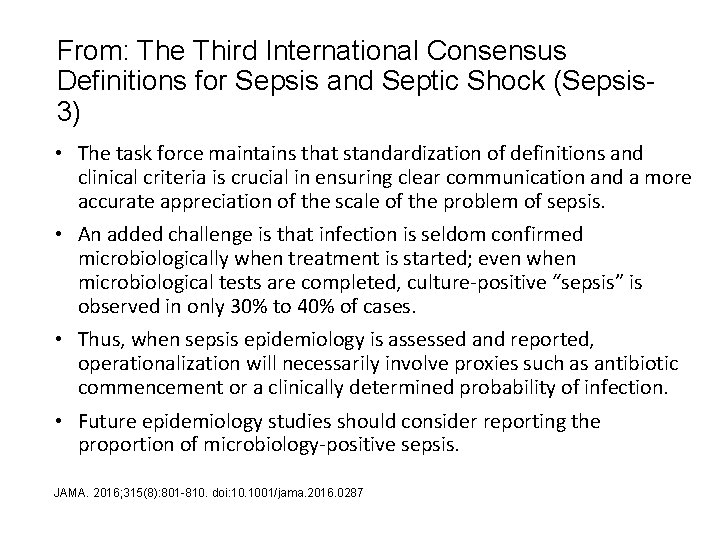
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis 3) • The task force maintains that standardization of definitions and clinical criteria is crucial in ensuring clear communication and a more accurate appreciation of the scale of the problem of sepsis. • An added challenge is that infection is seldom confirmed microbiologically when treatment is started; even when microbiological tests are completed, culture-positive “sepsis” is observed in only 30% to 40% of cases. • Thus, when sepsis epidemiology is assessed and reported, operationalization will necessarily involve proxies such as antibiotic commencement or a clinically determined probability of infection. • Future epidemiology studies should consider reporting the proportion of microbiology-positive sepsis. JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287
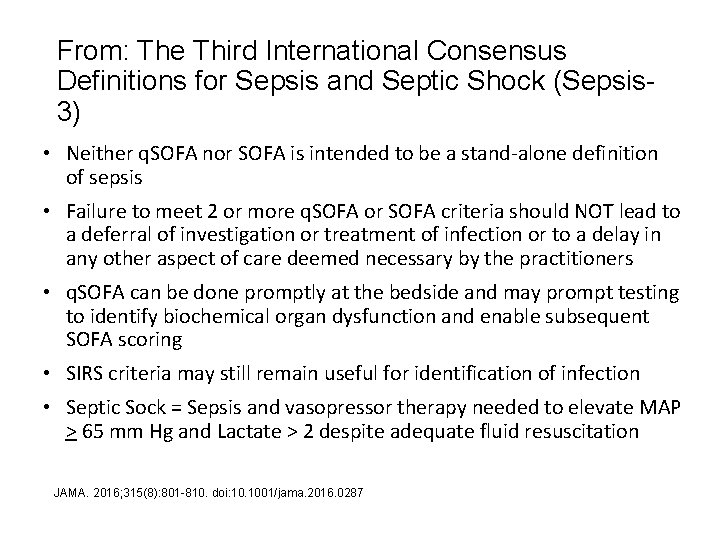
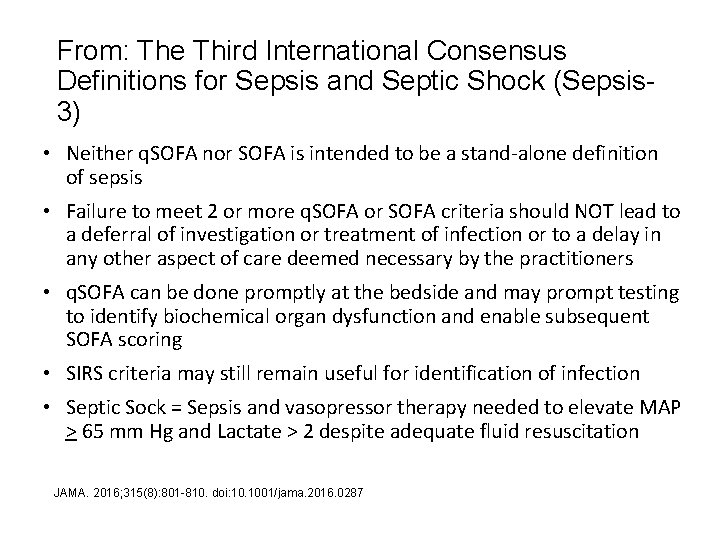
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis 3) • Neither q. SOFA nor SOFA is intended to be a stand-alone definition of sepsis • Failure to meet 2 or more q. SOFA or SOFA criteria should NOT lead to a deferral of investigation or treatment of infection or to a delay in any other aspect of care deemed necessary by the practitioners • q. SOFA can be done promptly at the bedside and may prompt testing to identify biochemical organ dysfunction and enable subsequent SOFA scoring • SIRS criteria may still remain useful for identification of infection • Septic Sock = Sepsis and vasopressor therapy needed to elevate MAP > 65 mm Hg and Lactate > 2 despite adequate fluid resuscitation JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287
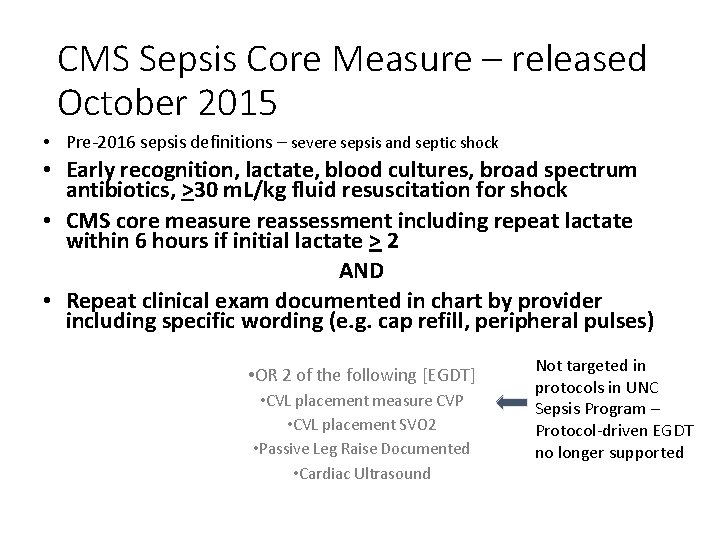
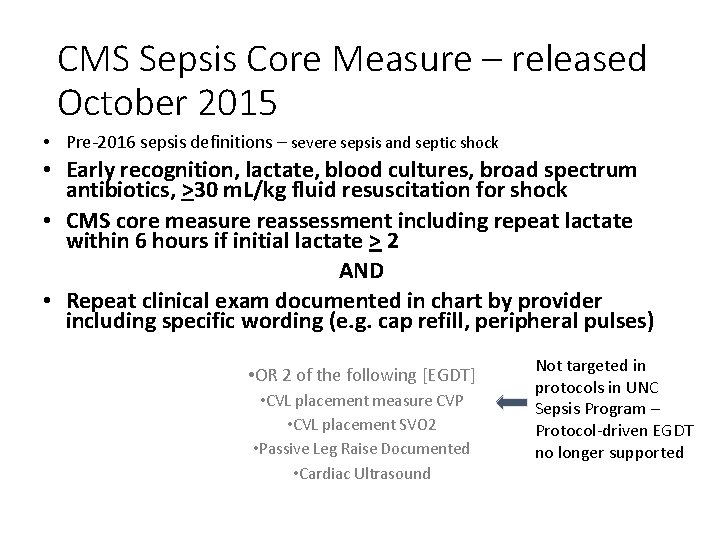
CMS Sepsis Core Measure – released October 2015 • Pre-2016 sepsis definitions – severe sepsis and septic shock • Early recognition, lactate, blood cultures, broad spectrum antibiotics, >30 m. L/kg fluid resuscitation for shock • CMS core measure reassessment including repeat lactate within 6 hours if initial lactate > 2 AND • Repeat clinical exam documented in chart by provider including specific wording (e. g. cap refill, peripheral pulses) • OR 2 of the following [EGDT] • CVL placement measure CVP • CVL placement SVO 2 • Passive Leg Raise Documented • Cardiac Ultrasound Not targeted in protocols in UNC Sepsis Program – Protocol-driven EGDT no longer supported

Current Pilot Test Tools
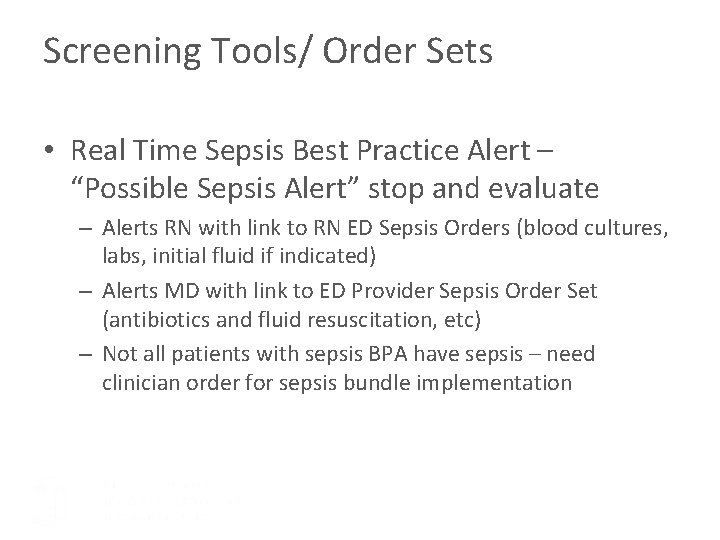
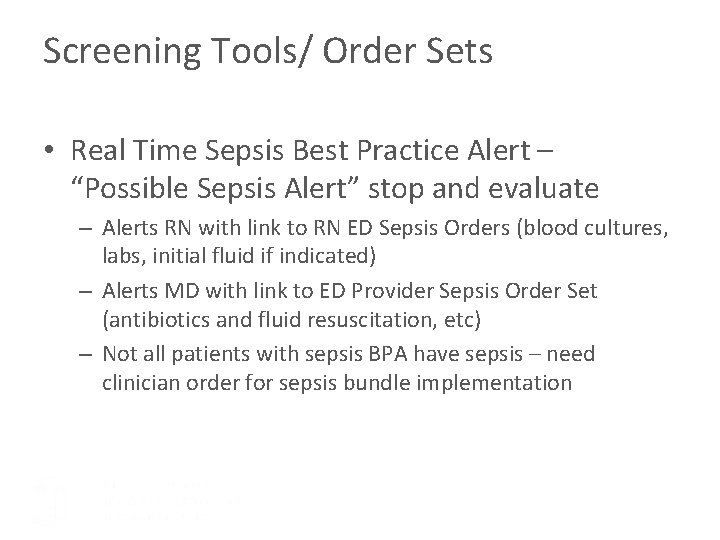
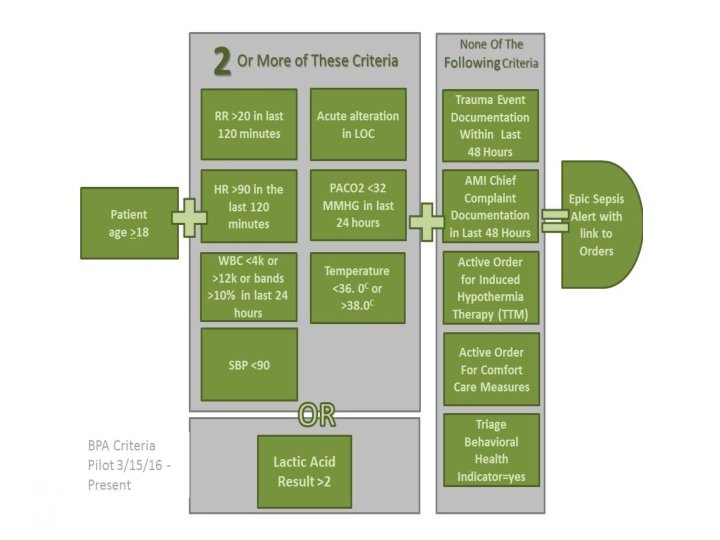
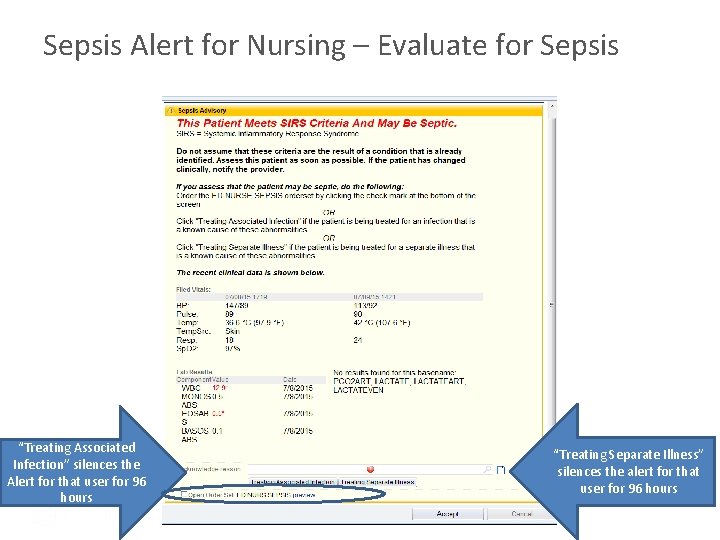
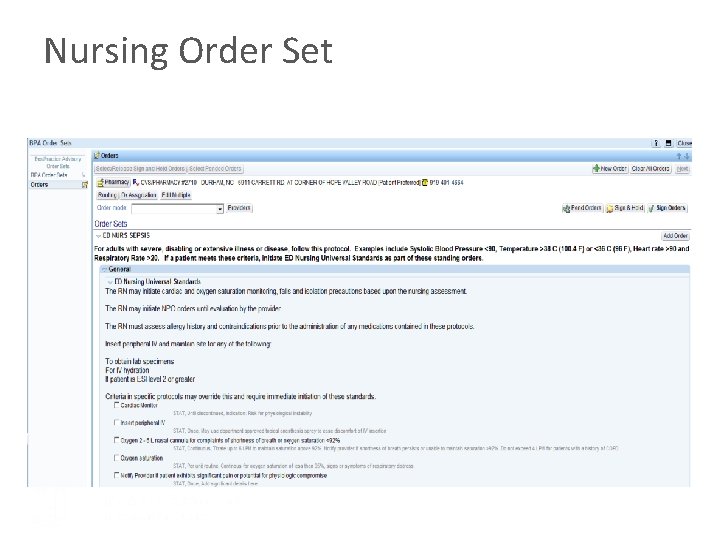
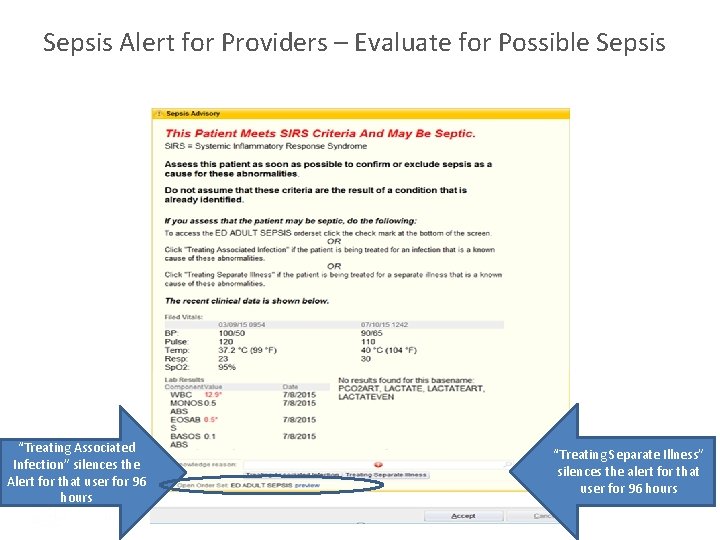
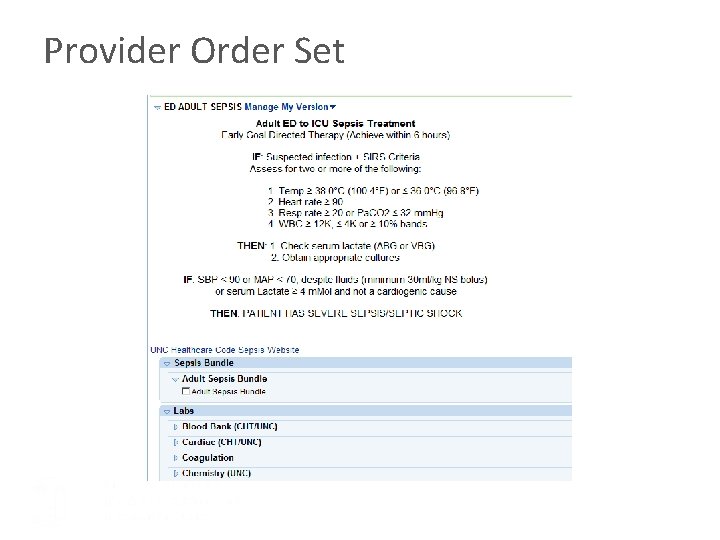
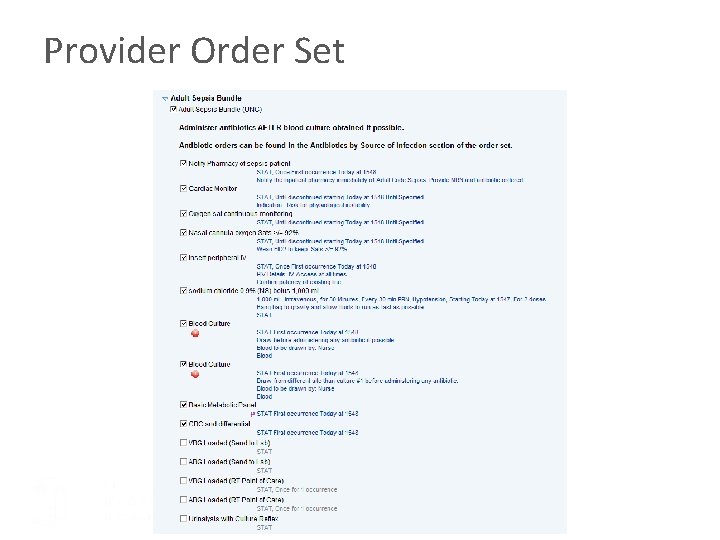
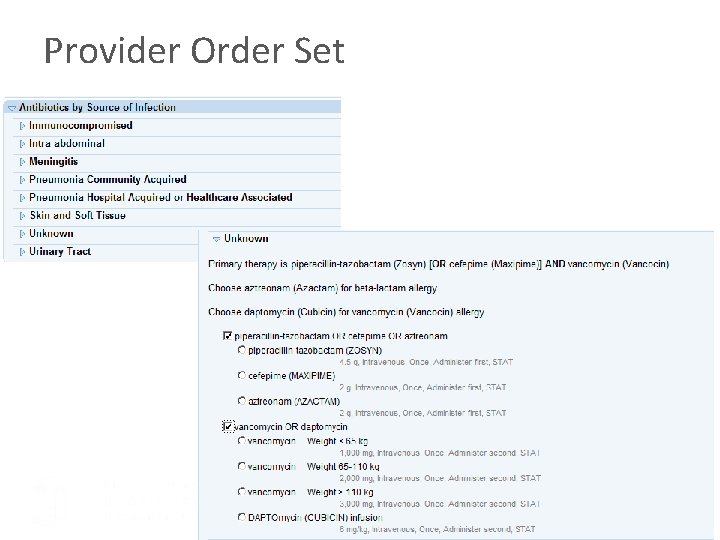
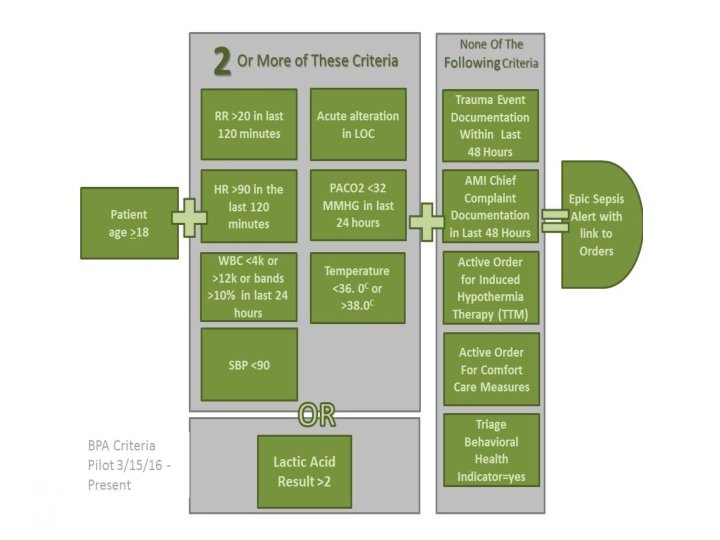
Screening Tools/ Order Sets • Real Time Sepsis Best Practice Alert – “Possible Sepsis Alert” stop and evaluate – Alerts RN with link to RN ED Sepsis Orders (blood cultures, labs, initial fluid if indicated) – Alerts MD with link to ED Provider Sepsis Order Set (antibiotics and fluid resuscitation, etc) – Not all patients with sepsis BPA have sepsis – need clinician order for sepsis bundle implementation
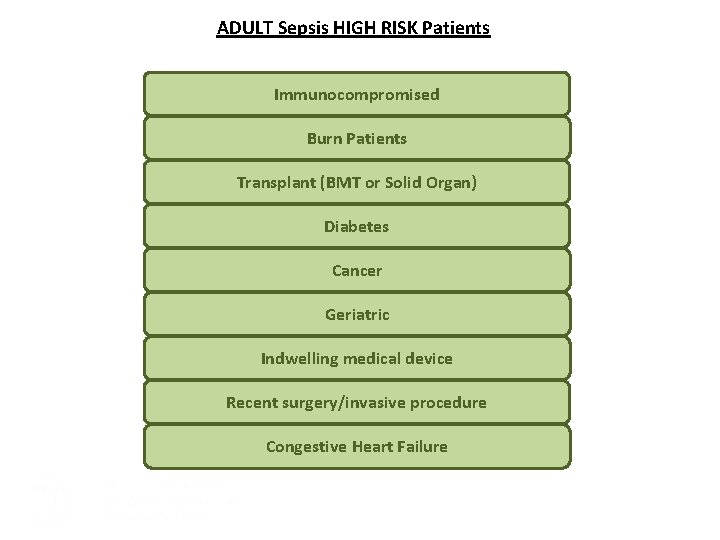
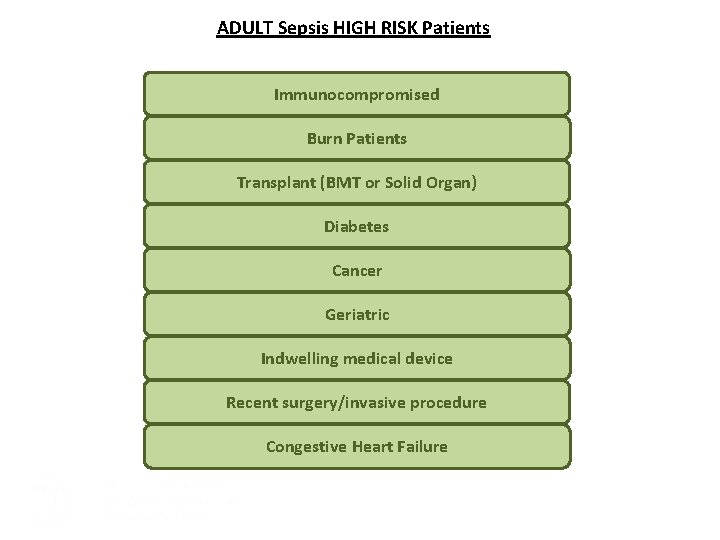
ADULT Sepsis HIGH RISK Patients Immunocompromised Burn Patients Transplant (BMT or Solid Organ) Diabetes Cancer Geriatric Indwelling medical device Recent surgery/invasive procedure Congestive Heart Failure
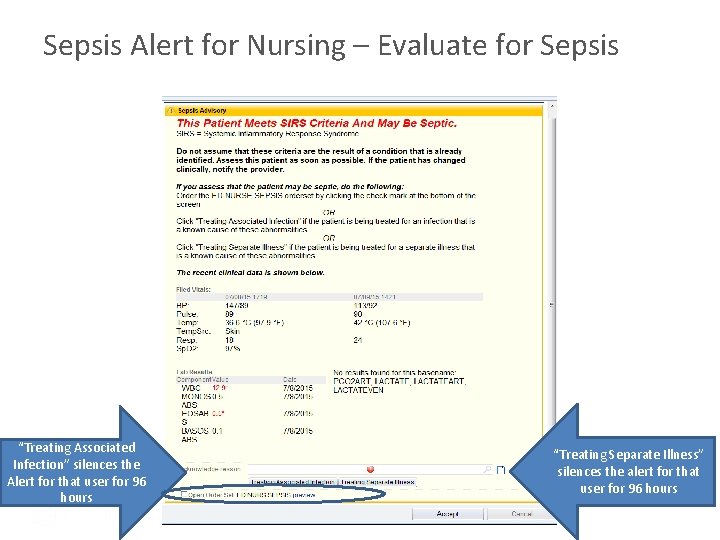
Sepsis Alert for Nursing – Evaluate for Sepsis “Treating Associated Infection” silences the Alert for that user for 96 hours “Treating Separate Illness” silences the alert for that user for 96 hours
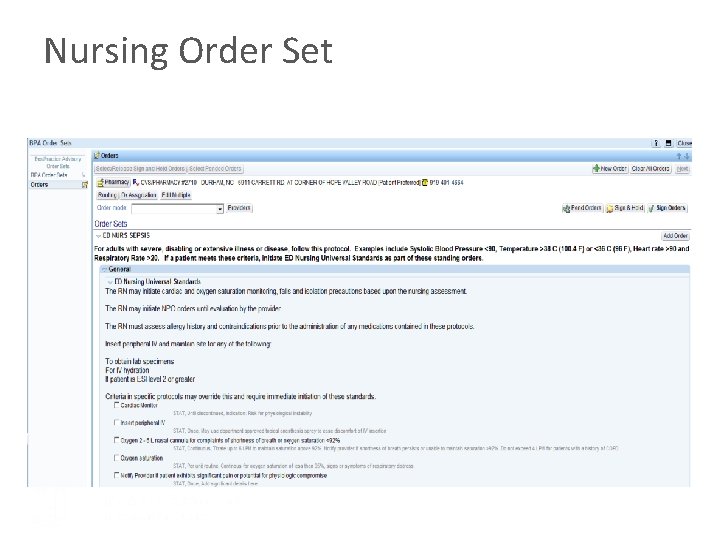
Nursing Order Set
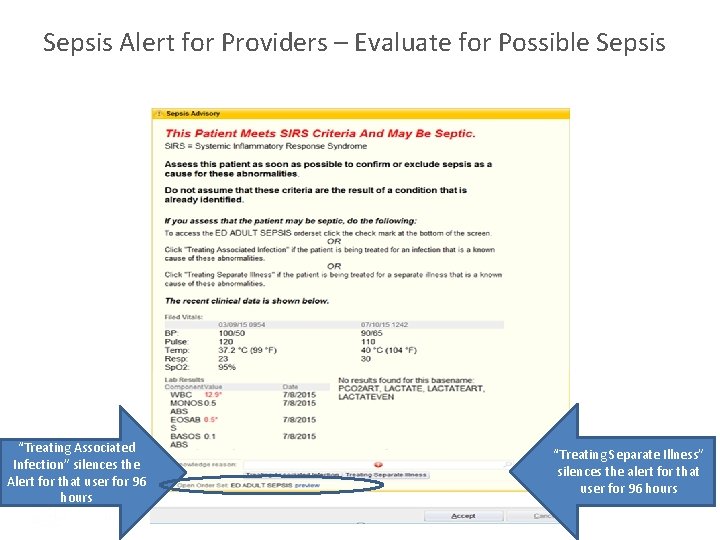
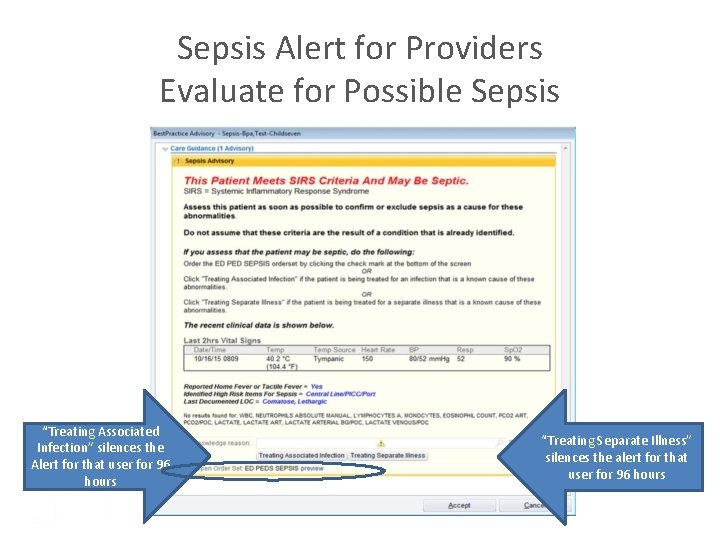
Sepsis Alert for Providers – Evaluate for Possible Sepsis “Treating Associated Infection” silences the Alert for that user for 96 hours “Treating Separate Illness” silences the alert for that user for 96 hours
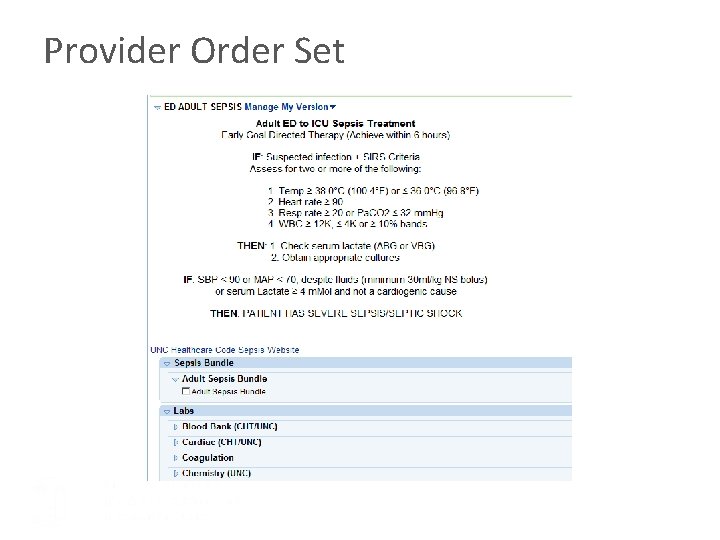
Provider Order Set
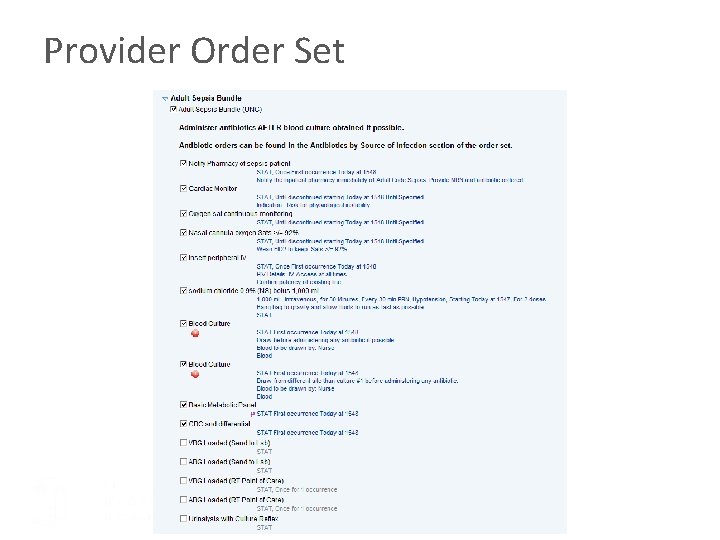
Provider Order Set
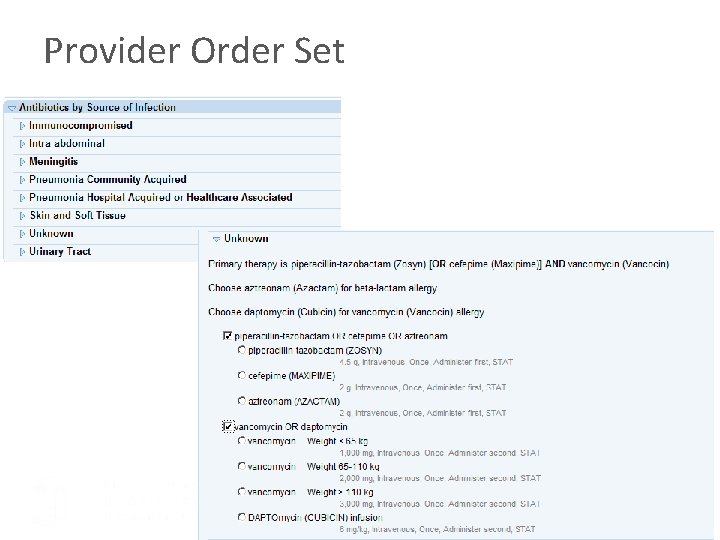
Provider Order Set
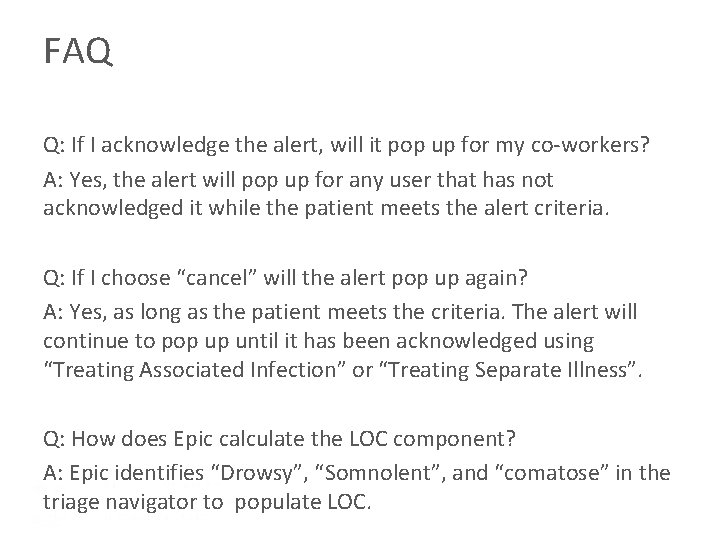
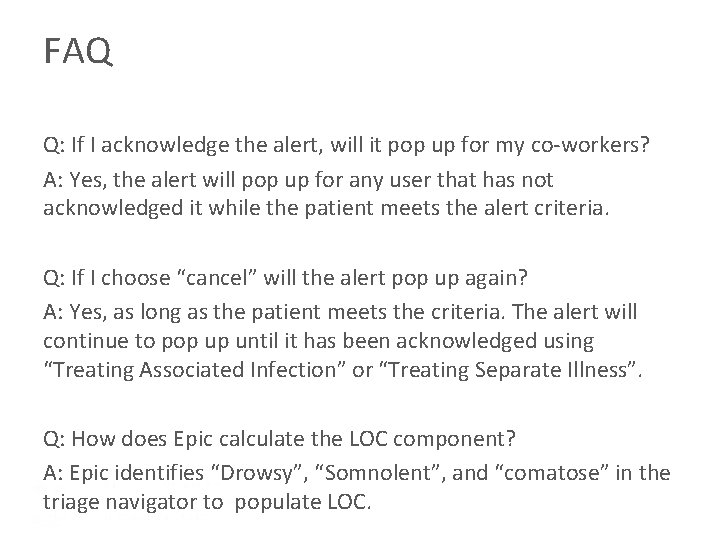
FAQ Q: If I acknowledge the alert, will it pop up for my co-workers? A: Yes, the alert will pop up for any user that has not acknowledged it while the patient meets the alert criteria. Q: If I choose “cancel” will the alert pop up again? A: Yes, as long as the patient meets the criteria. The alert will continue to pop up until it has been acknowledged using “Treating Associated Infection” or “Treating Separate Illness”. Q: How does Epic calculate the LOC component? A: Epic identifies “Drowsy”, “Somnolent”, and “comatose” in the triage navigator to populate LOC.
Q: If my patient’s condition improves, will the alert stop? A: Yes Q: Should I always utilize the order set when the alert pops up? A: No, the alert is designed to be sensitive rather than specific. Use your clinical judgment to determine whether or not the patient is showing signs and symptoms of sepsis.
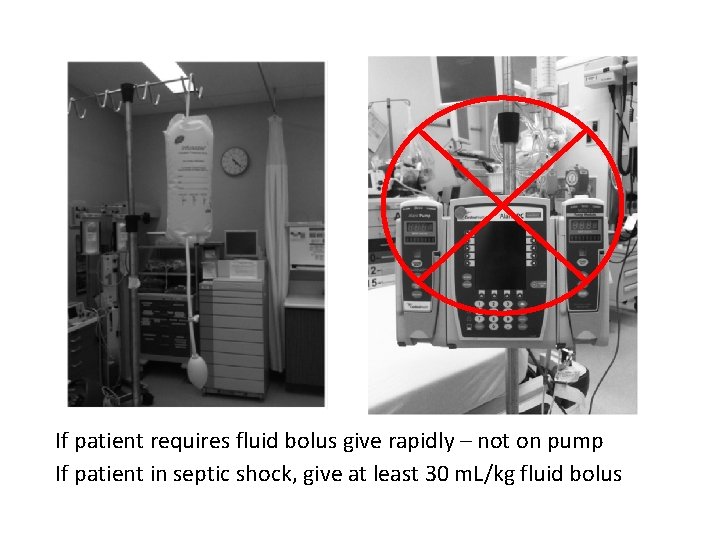
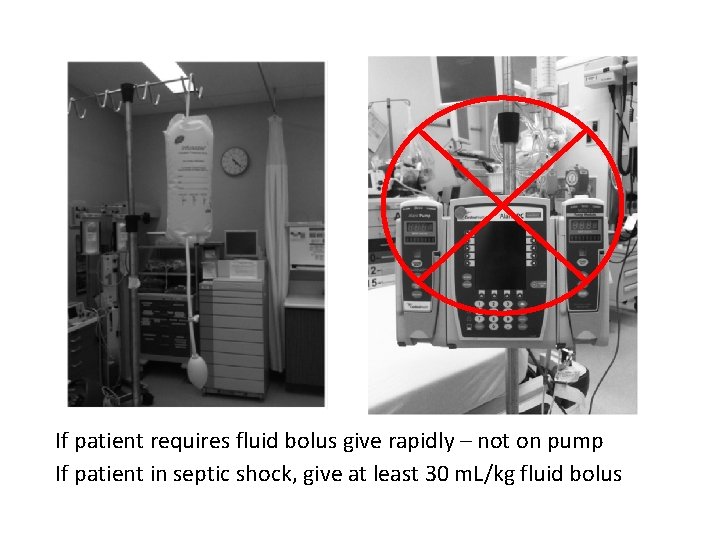
If patient requires fluid bolus give rapidly – not on pump If patient in septic shock, give at least 30 m. L/kg fluid bolus
Reassessment • Patients with sepsis can progress to shock rapidly • Reassess patients with documented repeat exam within the first few hours of sepsis development • Repeat lactate within 4 hours of the first lactate if septic patient’s initial lactate is >2
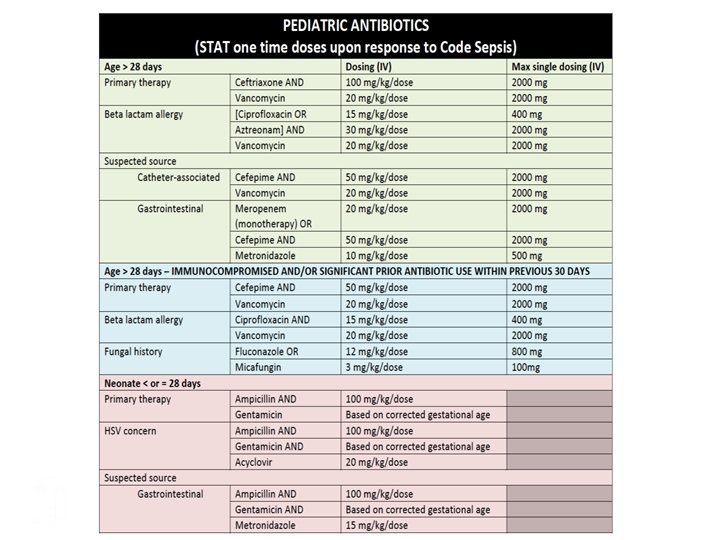
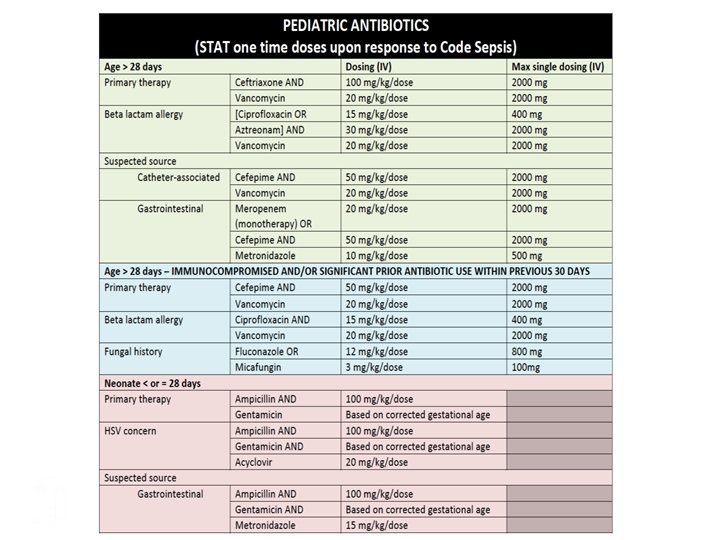
Pediatric Patient Specifics
Initial Management of Pediatric Shock • 20 ml/kg bolus fluid (crystalloid) in repeated doses as needed to treat shock even if BP normal • Common errors of pediatric resuscitation – Failure to open airway – Failure to provide appropriate fluid resuscitation – Failure to recognize and treat internal bleeding *Pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; 122: S 876 –S 908.
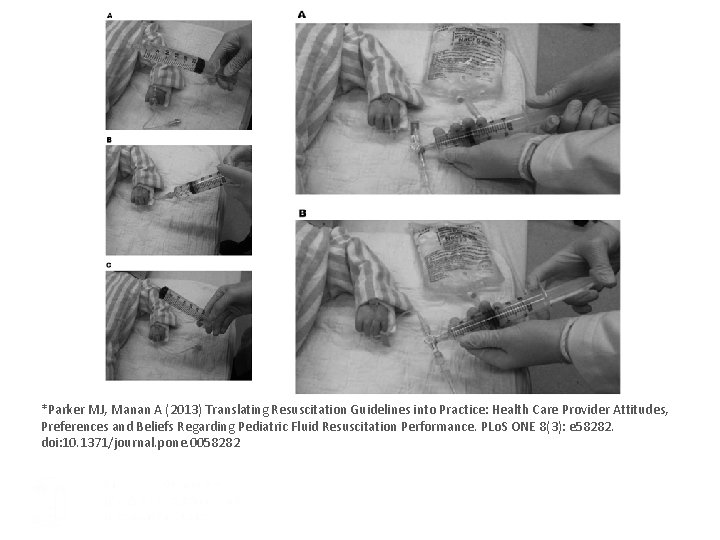
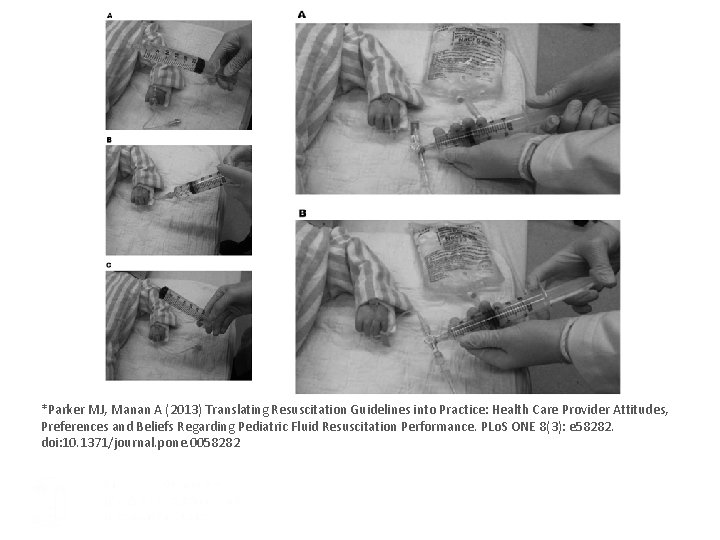
*Parker MJ, Manan A (2013) Translating Resuscitation Guidelines into Practice: Health Care Provider Attitudes, Preferences and Beliefs Regarding Pediatric Fluid Resuscitation Performance. PLo. S ONE 8(3): e 58282. doi: 10. 1371/journal. pone. 0058282
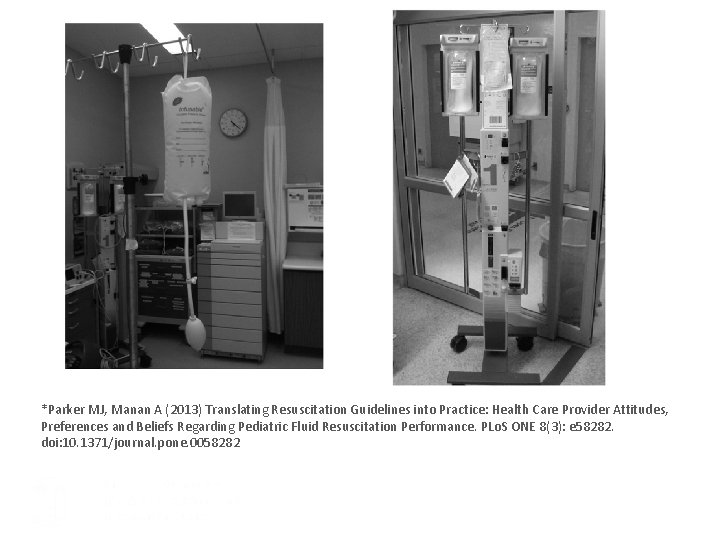
*Parker MJ, Manan A (2013) Translating Resuscitation Guidelines into Practice: Health Care Provider Attitudes, Preferences and Beliefs Regarding Pediatric Fluid Resuscitation Performance. PLo. S ONE 8(3): e 58282. doi: 10. 1371/journal. pone. 0058282
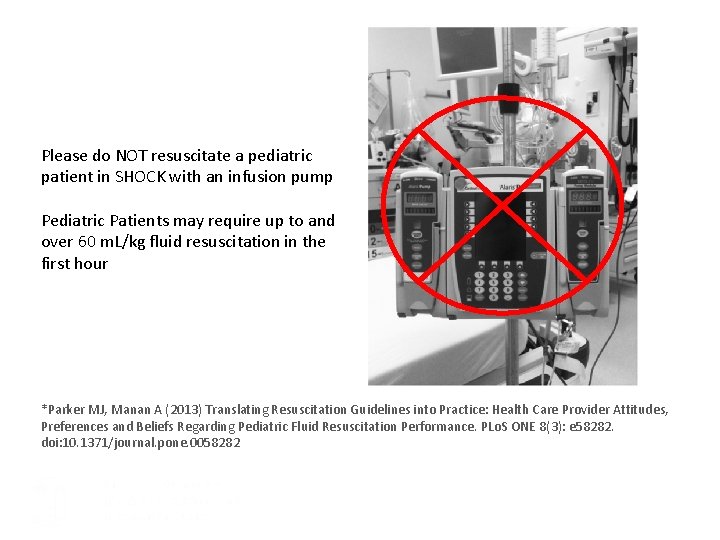
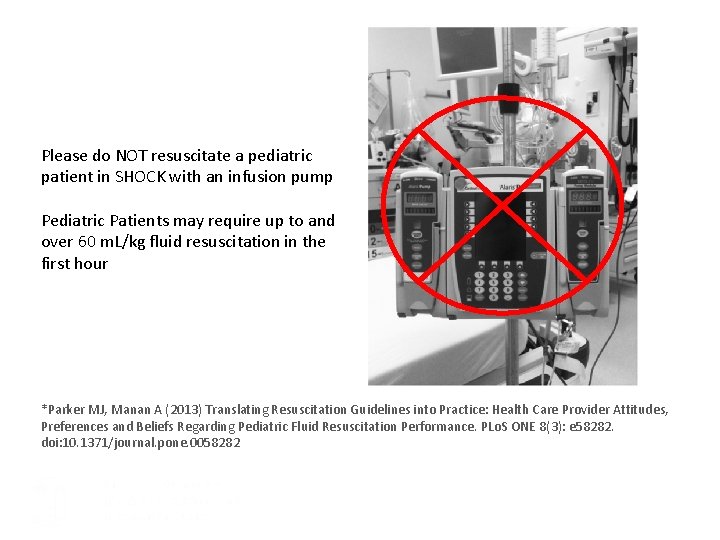
Please do NOT resuscitate a pediatric patient in SHOCK with an infusion pump Pediatric Patients may require up to and over 60 m. L/kg fluid resuscitation in the first hour *Parker MJ, Manan A (2013) Translating Resuscitation Guidelines into Practice: Health Care Provider Attitudes, Preferences and Beliefs Regarding Pediatric Fluid Resuscitation Performance. PLo. S ONE 8(3): e 58282. doi: 10. 1371/journal. pone. 0058282
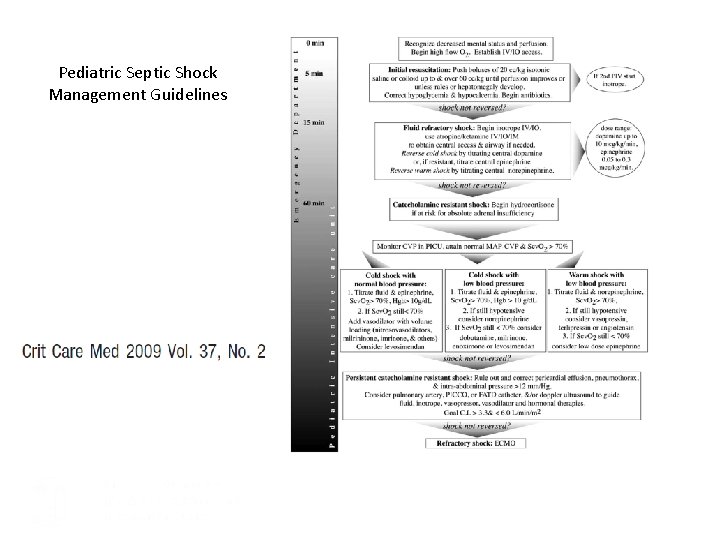
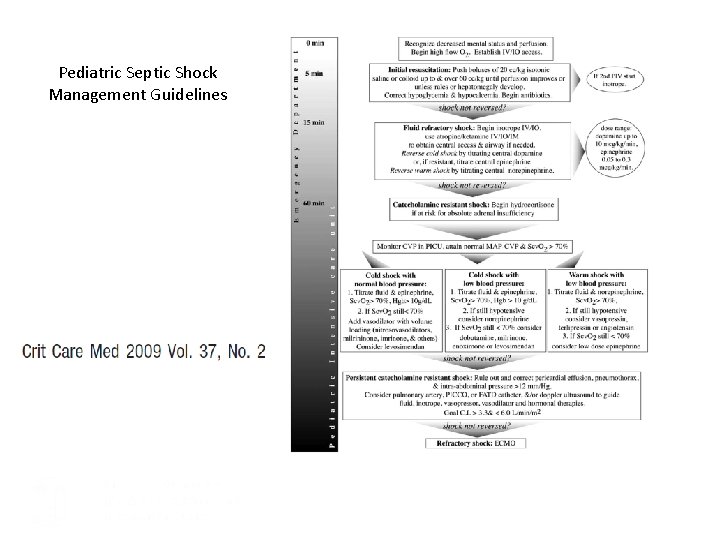
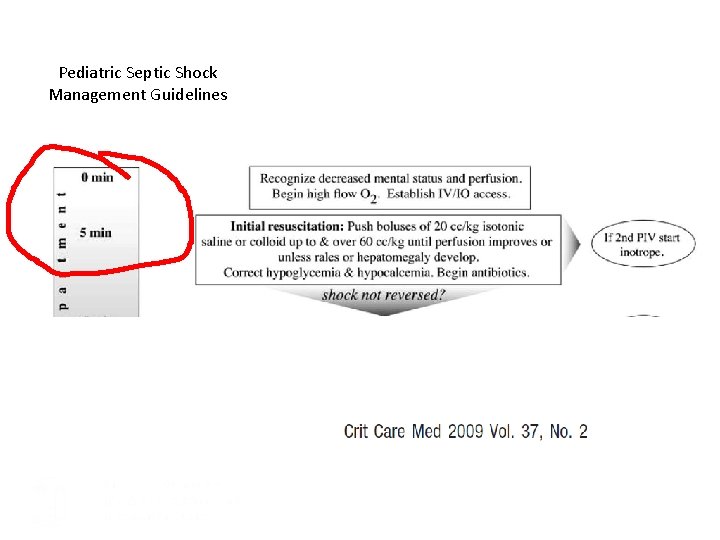
Pediatric Septic Shock Management Guidelines

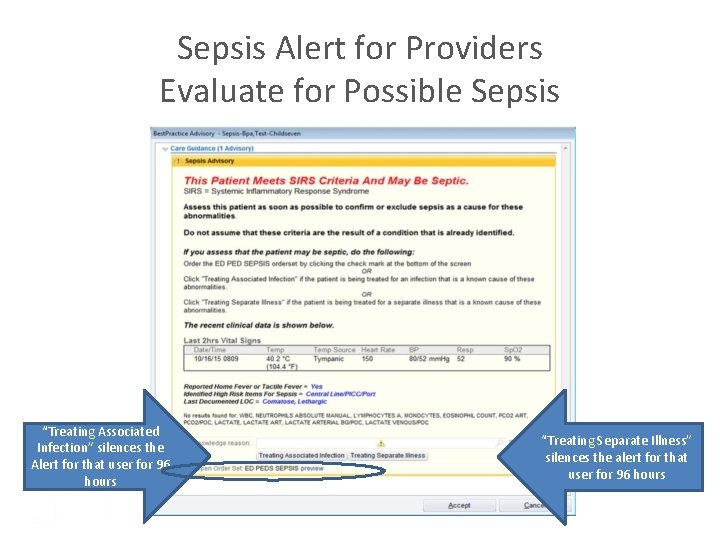
Sepsis Alert for Providers Evaluate for Possible Sepsis “Treating Associated Infection” silences the Alert for that user for 96 hours “Treating Separate Illness” silences the alert for that user for 96 hours
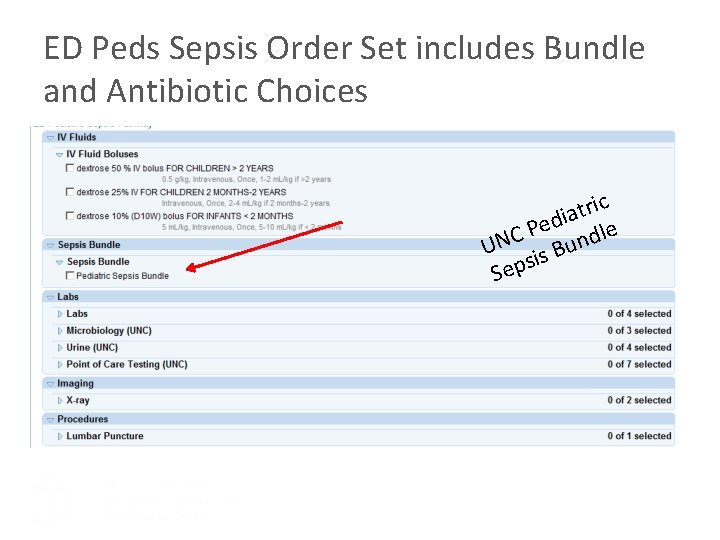
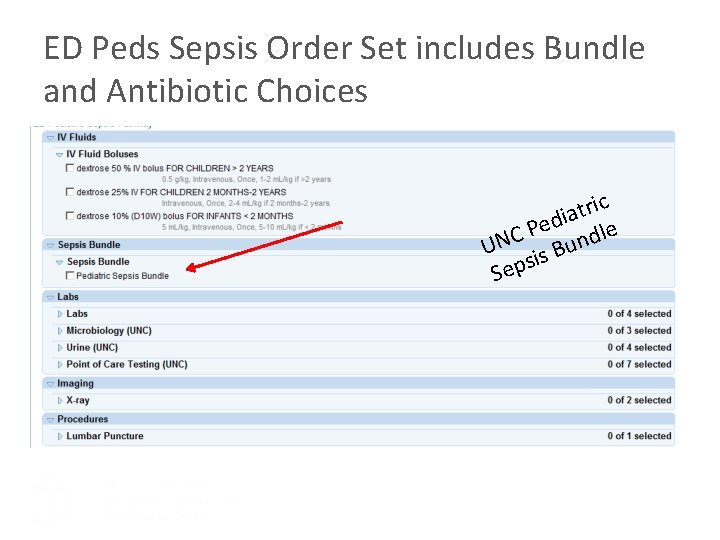
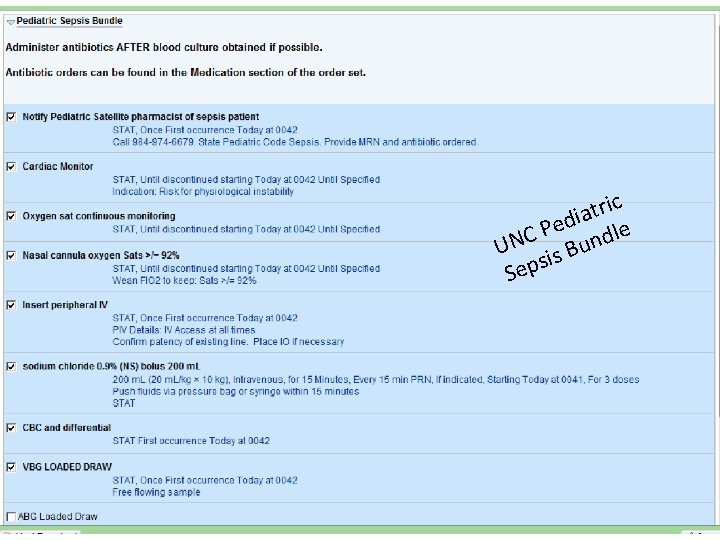
ED Peds Sepsis Order Set includes Bundle and Antibiotic Choices c i r t a di le e P UNC is Bund s Sep
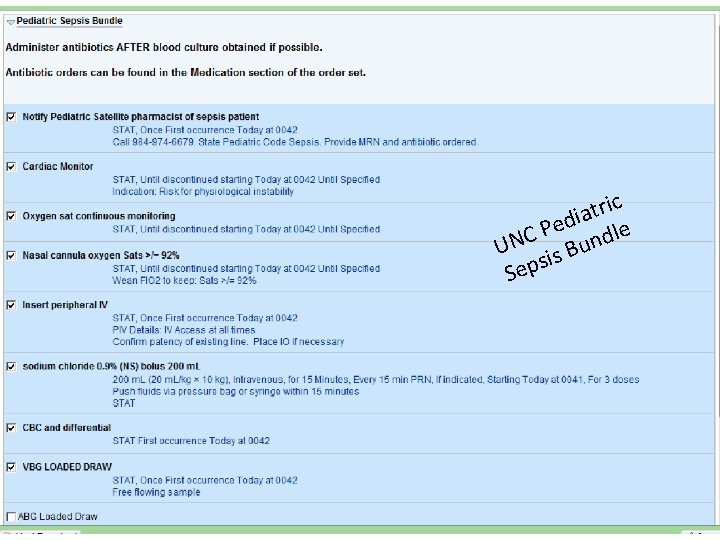
c i r t a di le e P UNC is Bund s Sep
Additional Information ED Peds Sepsis • Document the result of your sepsis assessment using the phrase. SEPSISPEDS • The BPA, and sepsis screening process, for patients 18 years and older follows the adult process • The BPA collects lab results from all patient encounters within the prior 24 hours • The BPA includes the vital sign data collected most recently
Additional Information ED Peds Sepsis • Anytime the patient meets 2+ criteria and the chart is opened it will fire for the person that opened the chart • It will constantly update with new information as it is entered and pop up accordingly • The only exception is if a user has utilized the buttons that silence the alert • The Positive Sepsis Screen result is documented on the timeline • The Sepsis Screen section also is available on the ED Nurse Narrator
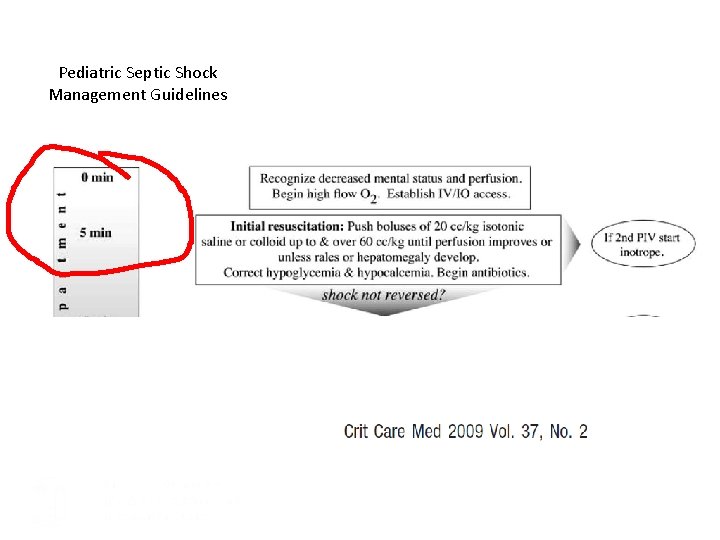
Pediatric Septic Shock Management Guidelines
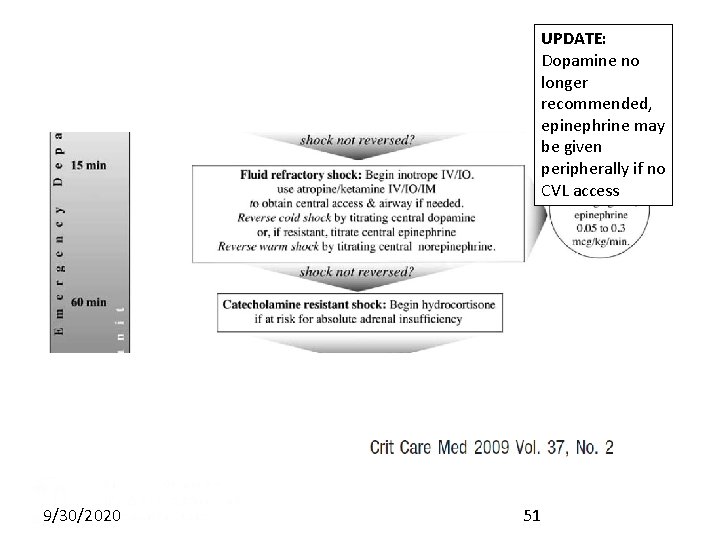
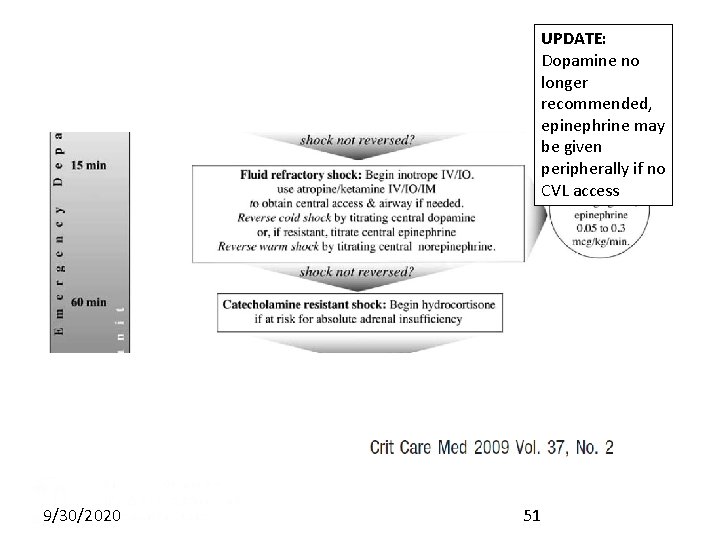
UPDATE: Dopamine no longer recommended, epinephrine may be given peripherally if no CVL access 9/30/2020 51
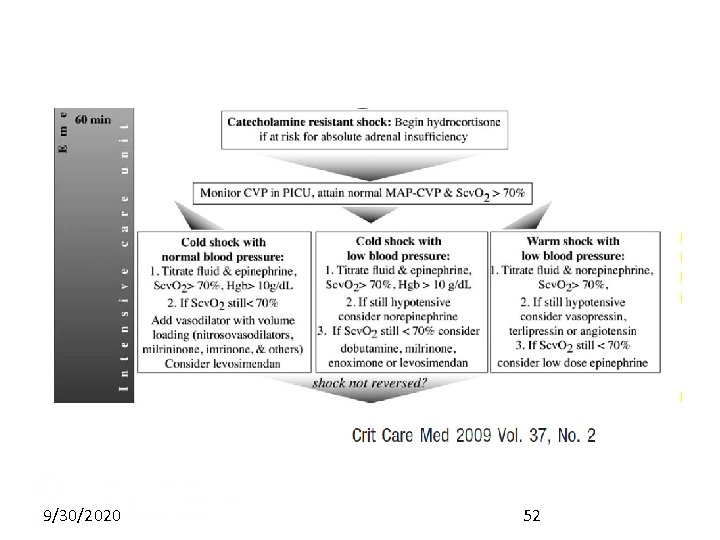
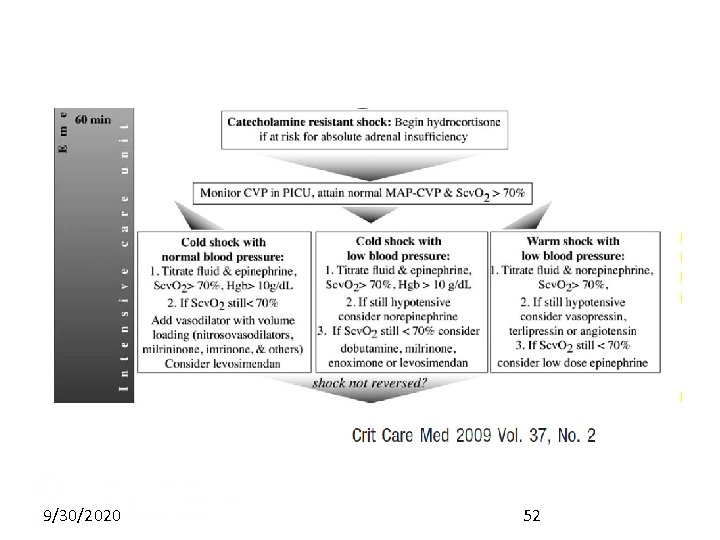
9/30/2020 52
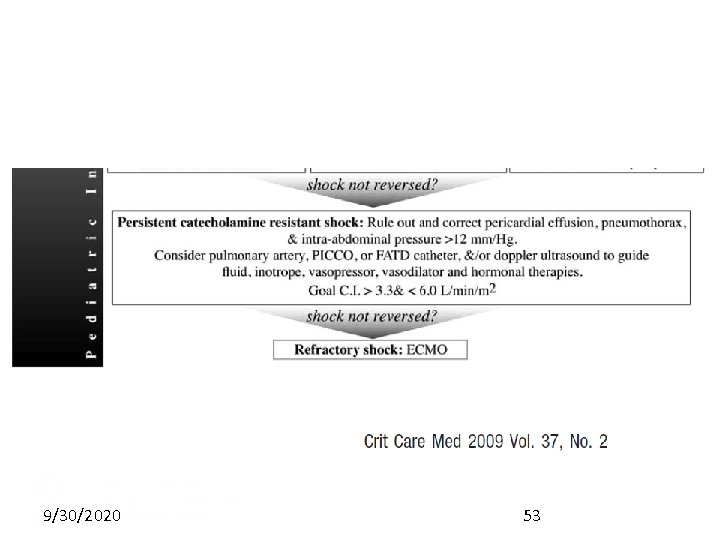
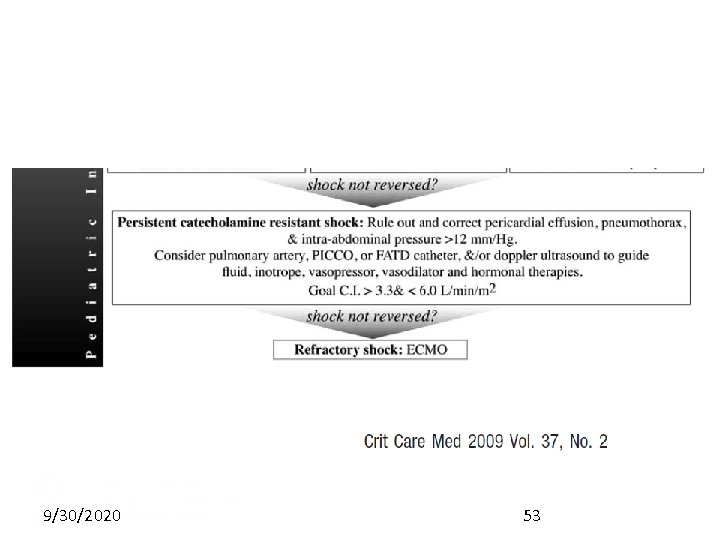
9/30/2020 53
Sepsis Case Reviews
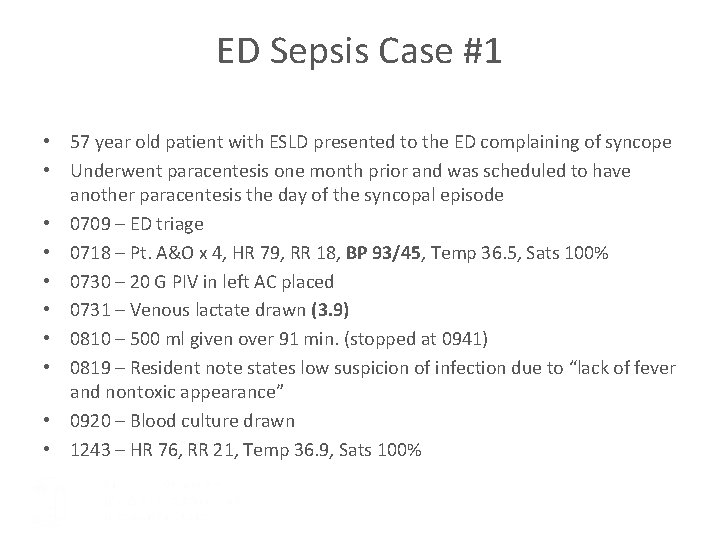
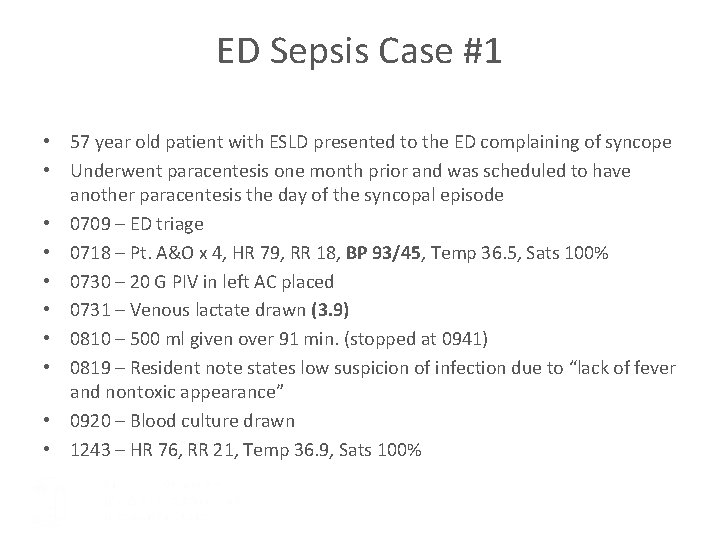
ED Sepsis Case #1 • 57 year old patient with ESLD presented to the ED complaining of syncope • Underwent paracentesis one month prior and was scheduled to have another paracentesis the day of the syncopal episode • 0709 – ED triage • 0718 – Pt. A&O x 4, HR 79, RR 18, BP 93/45, Temp 36. 5, Sats 100% • 0730 – 20 G PIV in left AC placed • 0731 – Venous lactate drawn (3. 9) • 0810 – 500 ml given over 91 min. (stopped at 0941) • 0819 – Resident note states low suspicion of infection due to “lack of fever and nontoxic appearance” • 0920 – Blood culture drawn • 1243 – HR 76, RR 21, Temp 36. 9, Sats 100%
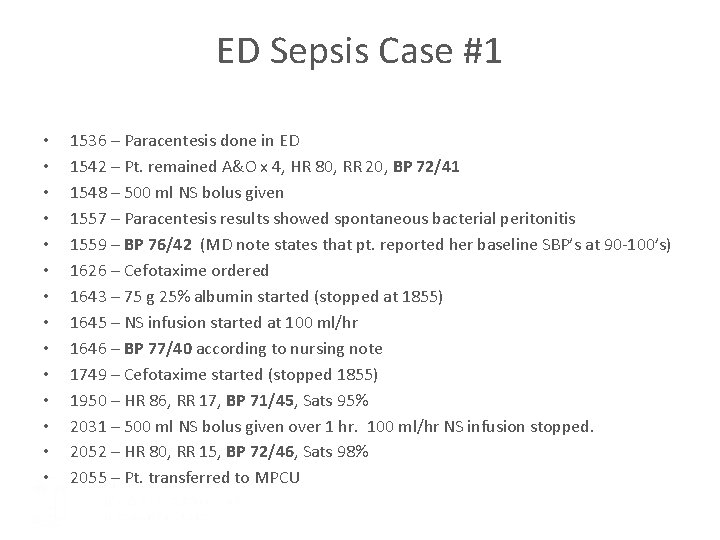
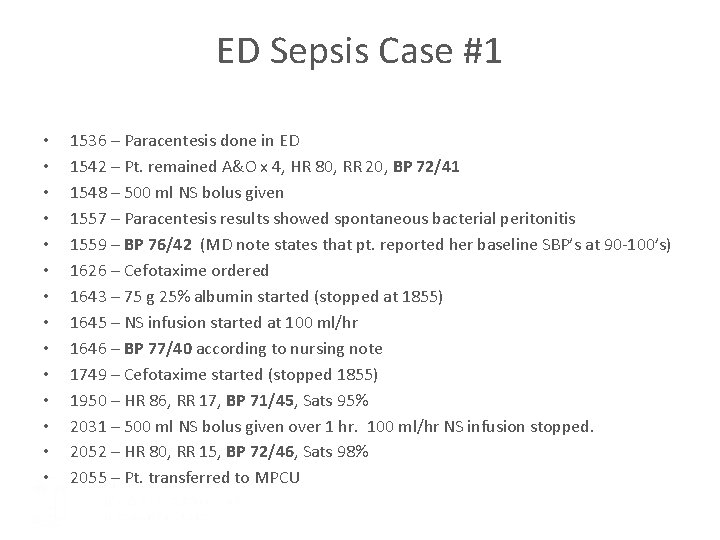
ED Sepsis Case #1 • • • • 1536 – Paracentesis done in ED 1542 – Pt. remained A&O x 4, HR 80, RR 20, BP 72/41 1548 – 500 ml NS bolus given 1557 – Paracentesis results showed spontaneous bacterial peritonitis 1559 – BP 76/42 (MD note states that pt. reported her baseline SBP’s at 90 -100’s) 1626 – Cefotaxime ordered 1643 – 75 g 25% albumin started (stopped at 1855) 1645 – NS infusion started at 100 ml/hr 1646 – BP 77/40 according to nursing note 1749 – Cefotaxime started (stopped 1855) 1950 – HR 86, RR 17, BP 71/45, Sats 95% 2031 – 500 ml NS bolus given over 1 hr. 100 ml/hr NS infusion stopped. 2052 – HR 80, RR 15, BP 72/46, Sats 98% 2055 – Pt. transferred to MPCU
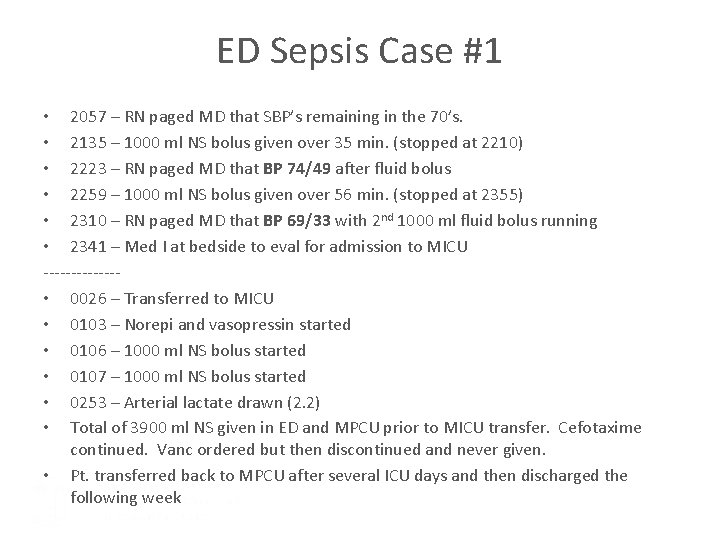
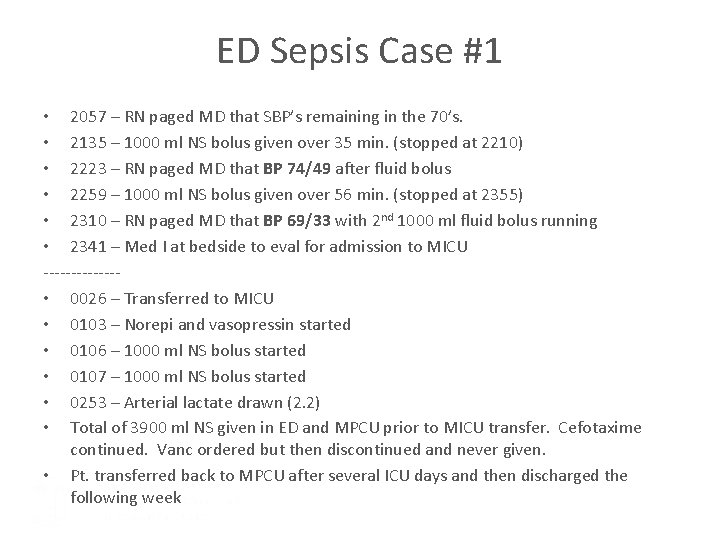
ED Sepsis Case #1 • 2057 – RN paged MD that SBP’s remaining in the 70’s. • 2135 – 1000 ml NS bolus given over 35 min. (stopped at 2210) • 2223 – RN paged MD that BP 74/49 after fluid bolus • 2259 – 1000 ml NS bolus given over 56 min. (stopped at 2355) • 2310 – RN paged MD that BP 69/33 with 2 nd 1000 ml fluid bolus running • 2341 – Med I at bedside to eval for admission to MICU ------- • 0026 – Transferred to MICU • 0103 – Norepi and vasopressin started • 0106 – 1000 ml NS bolus started • 0107 – 1000 ml NS bolus started • 0253 – Arterial lactate drawn (2. 2) • Total of 3900 ml NS given in ED and MPCU prior to MICU transfer. Cefotaxime continued. Vanc ordered but then discontinued and never given. • Pt. transferred back to MPCU after several ICU days and then discharged the following week
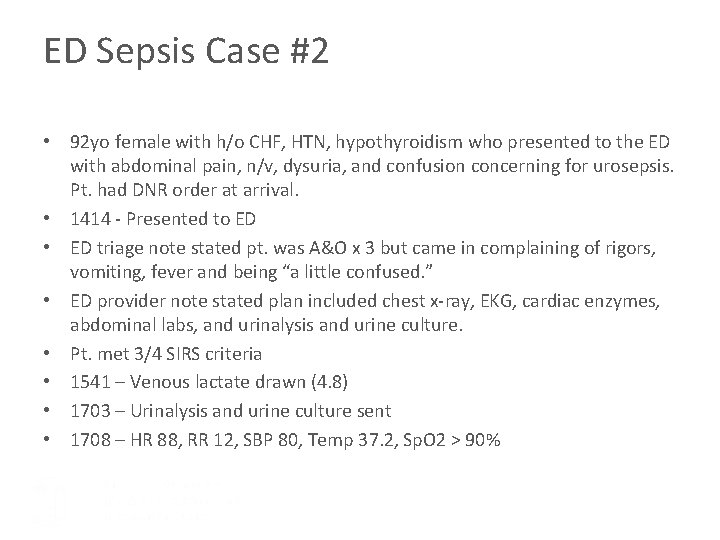
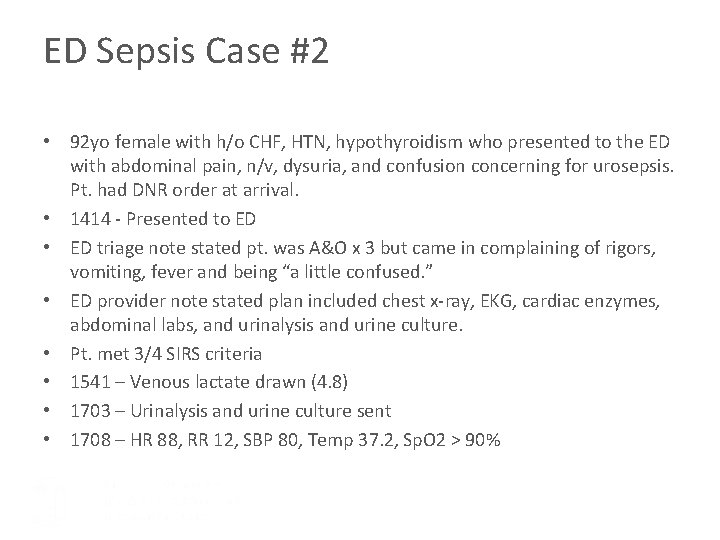
ED Sepsis Case #2 • 92 yo female with h/o CHF, HTN, hypothyroidism who presented to the ED with abdominal pain, n/v, dysuria, and confusion concerning for urosepsis. Pt. had DNR order at arrival. • 1414 - Presented to ED • ED triage note stated pt. was A&O x 3 but came in complaining of rigors, vomiting, fever and being “a little confused. ” • ED provider note stated plan included chest x-ray, EKG, cardiac enzymes, abdominal labs, and urinalysis and urine culture. • Pt. met 3/4 SIRS criteria • 1541 – Venous lactate drawn (4. 8) • 1703 – Urinalysis and urine culture sent • 1708 – HR 88, RR 12, SBP 80, Temp 37. 2, Sp. O 2 > 90%

ED Sepsis Case #2 • • • 1713 – 1000 ml NS bolus (given over 2 hrs) Pt. had one 22 g PIV in rt. forearm placed in ED Repeat vitals not recorded after bolus 2039 – Admitted to MPCU 2045 – HR 80, RR 20, SBP 77, Temp 36. 9, Sp. O 2 > 90% 2050 – IV ceftriaxone ordered 2108 – Blood culture drawn (positive for E coli) 2110 – HR 78, RR 16, SBP 57, Temp 36. 9, Sp. O 2 > 90% Pt. confused 2118 – Rapid Response called 2118 – IV vanc, metrodnidazole, and cefepime ordered 2118 – 1000 ml NS bolus given via pressure bag
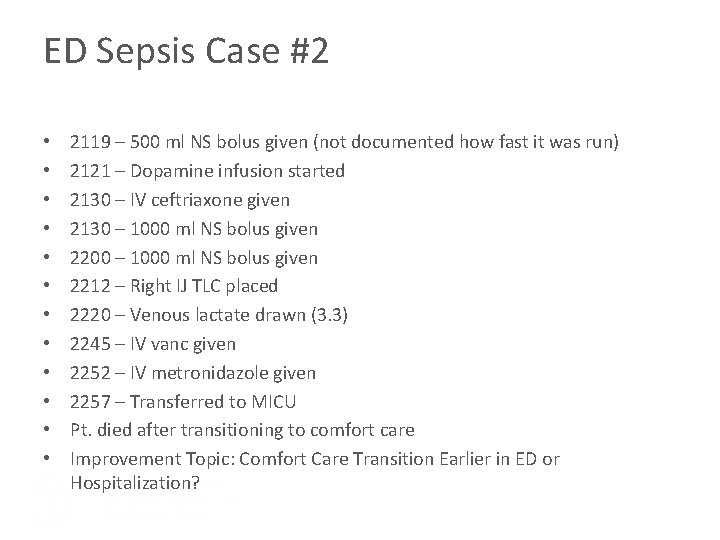
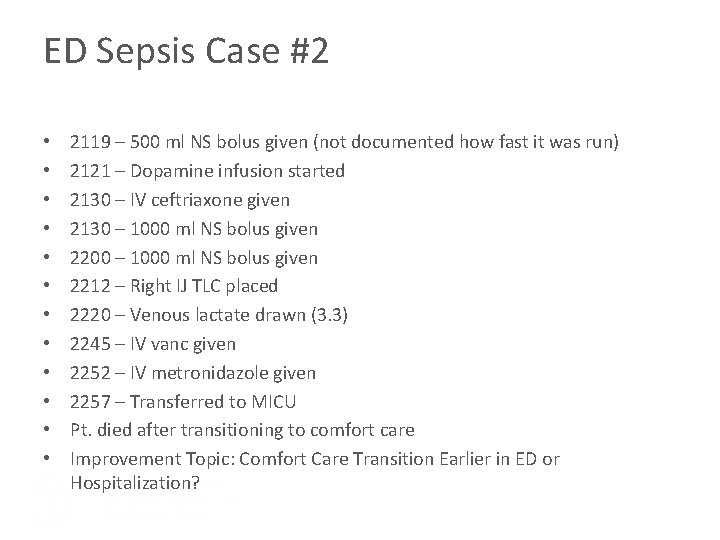
ED Sepsis Case #2 • • • 2119 – 500 ml NS bolus given (not documented how fast it was run) 2121 – Dopamine infusion started 2130 – IV ceftriaxone given 2130 – 1000 ml NS bolus given 2200 – 1000 ml NS bolus given 2212 – Right IJ TLC placed 2220 – Venous lactate drawn (3. 3) 2245 – IV vanc given 2252 – IV metronidazole given 2257 – Transferred to MICU Pt. died after transitioning to comfort care Improvement Topic: Comfort Care Transition Earlier in ED or Hospitalization?
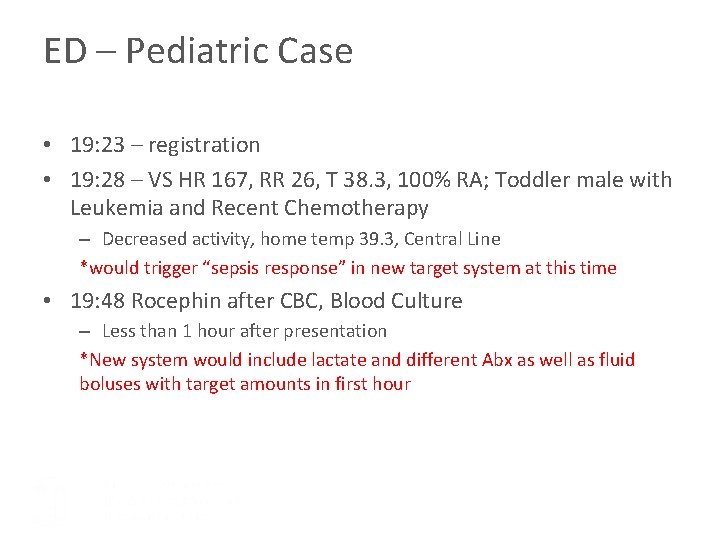
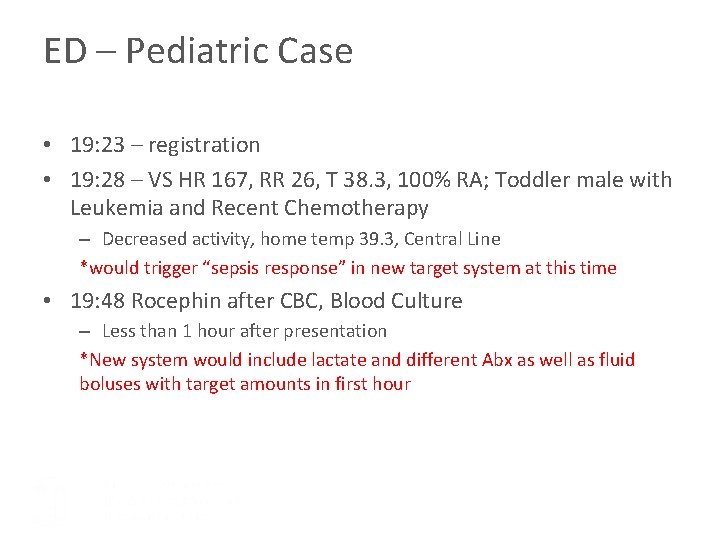
ED – Pediatric Case • 19: 23 – registration • 19: 28 – VS HR 167, RR 26, T 38. 3, 100% RA; Toddler male with Leukemia and Recent Chemotherapy – Decreased activity, home temp 39. 3, Central Line *would trigger “sepsis response” in new target system at this time • 19: 48 Rocephin after CBC, Blood Culture – Less than 1 hour after presentation *New system would include lactate and different Abx as well as fluid boluses with target amounts in first hour
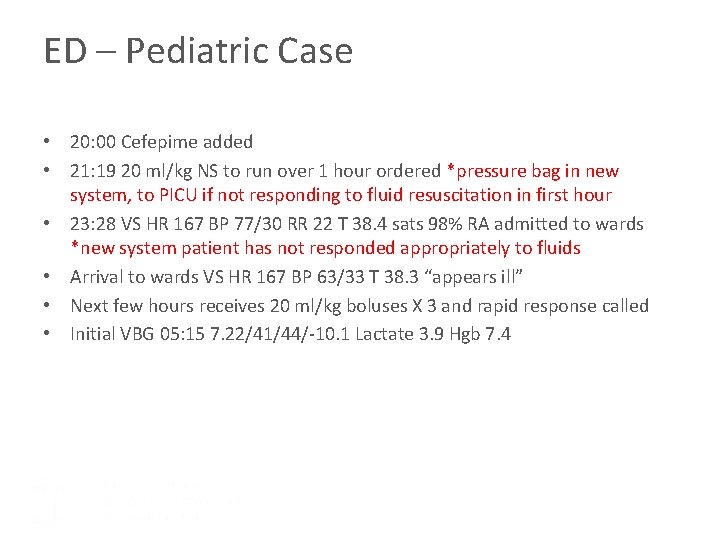
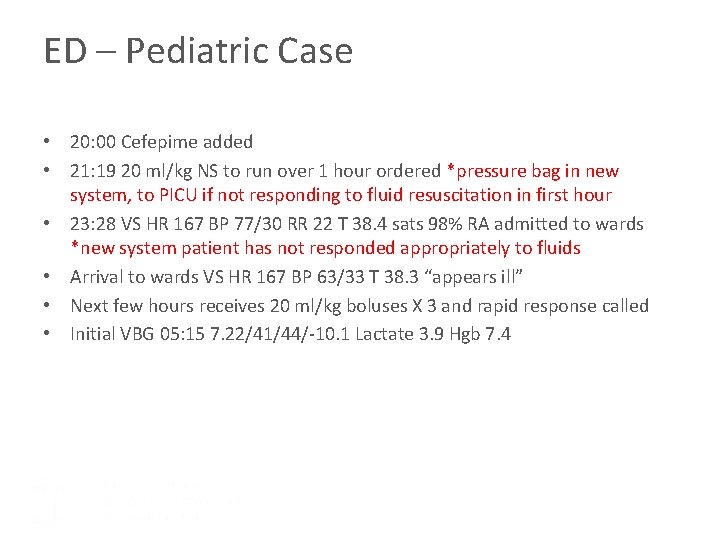
ED – Pediatric Case • 20: 00 Cefepime added • 21: 19 20 ml/kg NS to run over 1 hour ordered *pressure bag in new system, to PICU if not responding to fluid resuscitation in first hour • 23: 28 VS HR 167 BP 77/30 RR 22 T 38. 4 sats 98% RA admitted to wards *new system patient has not responded appropriately to fluids • Arrival to wards VS HR 167 BP 63/33 T 38. 3 “appears ill” • Next few hours receives 20 ml/kg boluses X 3 and rapid response called • Initial VBG 05: 15 7. 22/41/44/-10. 1 Lactate 3. 9 Hgb 7. 4
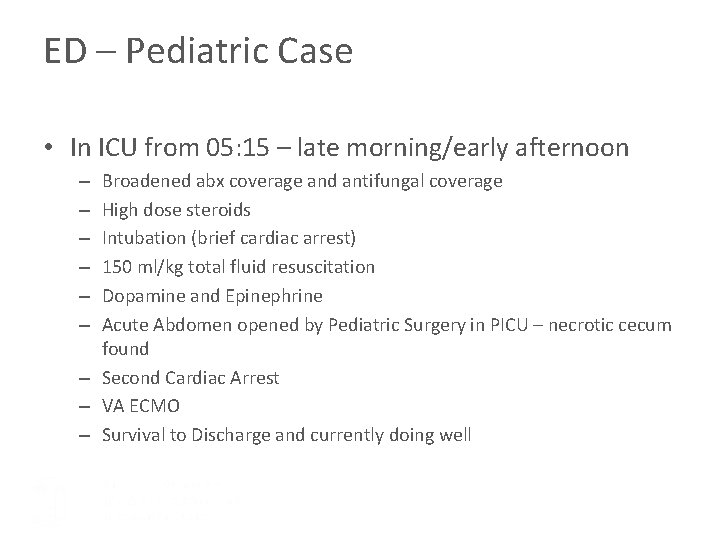
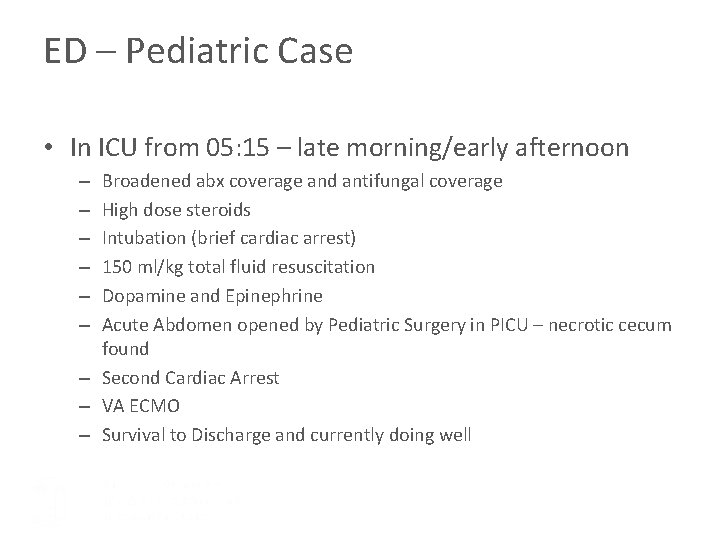
ED – Pediatric Case • In ICU from 05: 15 – late morning/early afternoon Broadened abx coverage and antifungal coverage High dose steroids Intubation (brief cardiac arrest) 150 ml/kg total fluid resuscitation Dopamine and Epinephrine Acute Abdomen opened by Pediatric Surgery in PICU – necrotic cecum found – Second Cardiac Arrest – VA ECMO – Survival to Discharge and currently doing well – – –
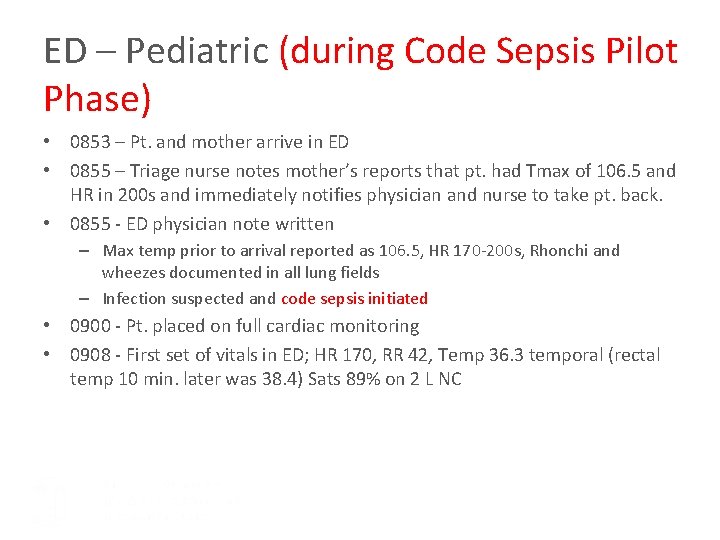
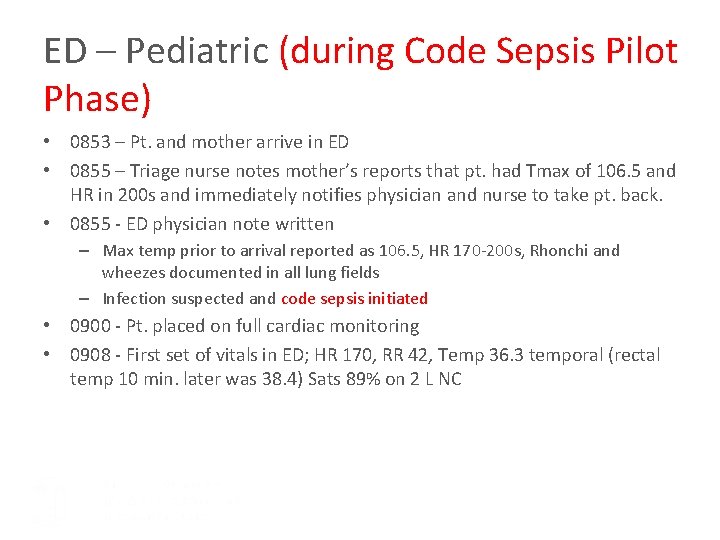
ED – Pediatric (during Code Sepsis Pilot Phase) • 0853 – Pt. and mother arrive in ED • 0855 – Triage nurse notes mother’s reports that pt. had Tmax of 106. 5 and HR in 200 s and immediately notifies physician and nurse to take pt. back. • 0855 - ED physician note written – Max temp prior to arrival reported as 106. 5, HR 170 -200 s, Rhonchi and wheezes documented in all lung fields – Infection suspected and code sepsis initiated • 0900 - Pt. placed on full cardiac monitoring • 0908 - First set of vitals in ED; HR 170, RR 42, Temp 36. 3 temporal (rectal temp 10 min. later was 38. 4) Sats 89% on 2 L NC
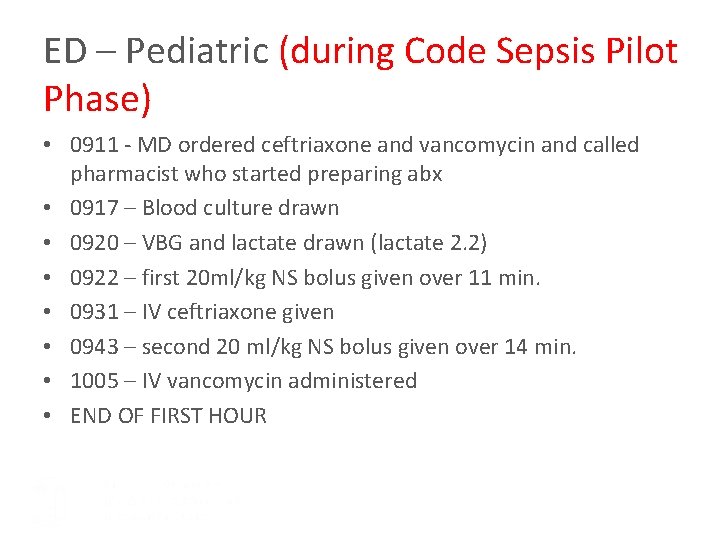
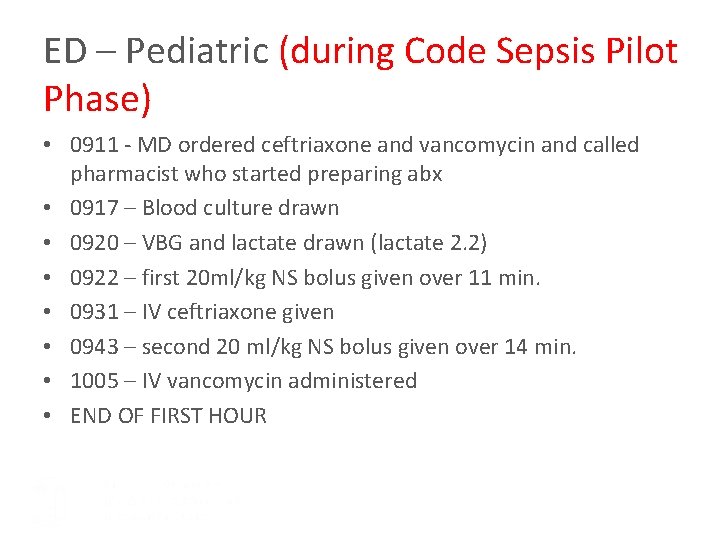
ED – Pediatric (during Code Sepsis Pilot Phase) • 0911 - MD ordered ceftriaxone and vancomycin and called pharmacist who started preparing abx • 0917 – Blood culture drawn • 0920 – VBG and lactate drawn (lactate 2. 2) • 0922 – first 20 ml/kg NS bolus given over 11 min. • 0931 – IV ceftriaxone given • 0943 – second 20 ml/kg NS bolus given over 14 min. • 1005 – IV vancomycin administered • END OF FIRST HOUR
Public UNC Code Sepsis Website Resources>Performance Improvement and Patient Safety>Sepsis Program Content: Background Resources Sepsis Toolkit FAQs Need Help? Or just Google “UNC Code Sepsis”
Take Home Points • This new system is an iterative process and will be different in the coming months • Septic Shock may be more subtle than you think • Process is a team event (RRT for inpatient units – triggered ED response in ED) for rapid IV access, fluid administration, antibiotic arrival, and lab studies – all bundle elements • Patients can worsen rapidly • If you want to help us in the development or have feedback please contact the Sepsis Program Team: sepsisfeedbackunch@unchealth. unc. edu