RADIODIAGNOSIS AND NUCLEARTHERAPY FOR THYROID DISEASE Hesti Gunarti









- Slides: 51
RADIODIAGNOSIS AND NUCLEARTHERAPY FOR THYROID DISEASE Hesti Gunarti Departemen Radiologi FK UGM/RSUP DR Sardjito
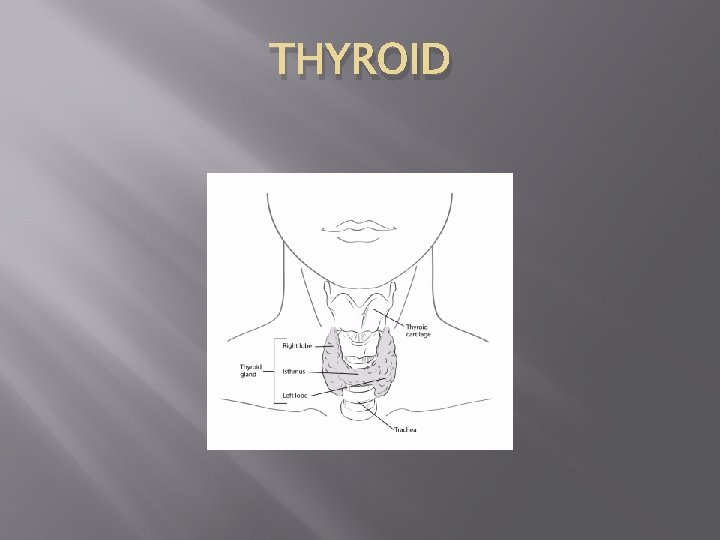
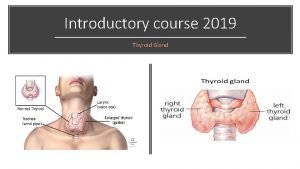
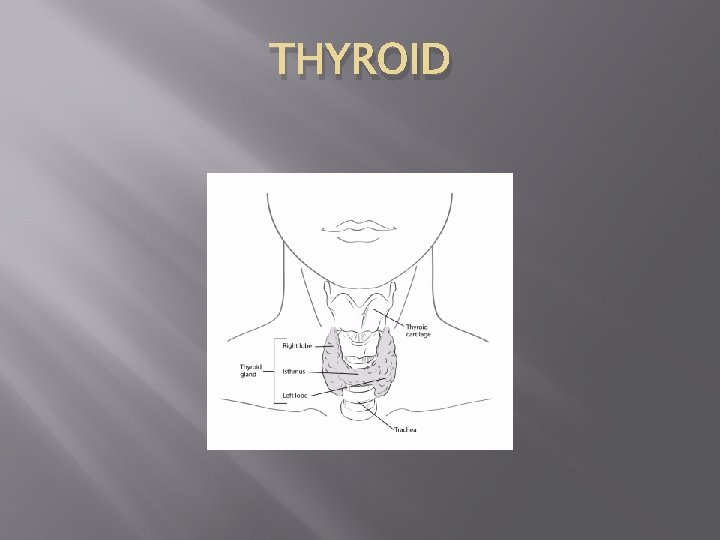
THYROID
Radiodiagnosis for Thyroid Disease 1. 2. 3. 4. Ultrasonography CT Scan MRI Thyroid scintigraphy
1. Ultrasonography (USG) � � Gray scale, color Doppler Transducer : linear frekuensi tinggi (7. 5 -15. 0 MHz)
� � Ukuran normal kelenjar thyroid orang dewasa Indonesia : 4 -4, 8 cm x 1, 0 -1, 8 cm x 0, 8 -1, 6 cm. Berat normal : neonatus 2 -3 gram. Orang dewasa 18 -20 gram
� Normal thyroid parenchyma has a homogeneous, medium-level to high-level echogenicity that makes detection of focal cystic or hypoechoic thyroid lesions relatively easy in most cases.
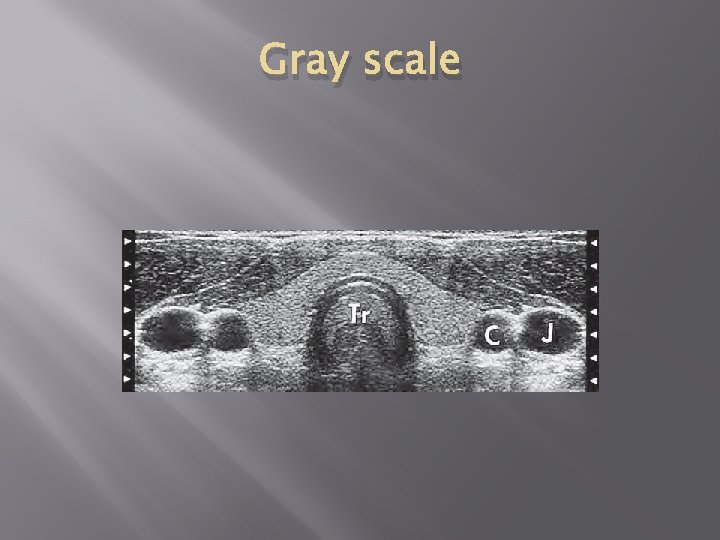
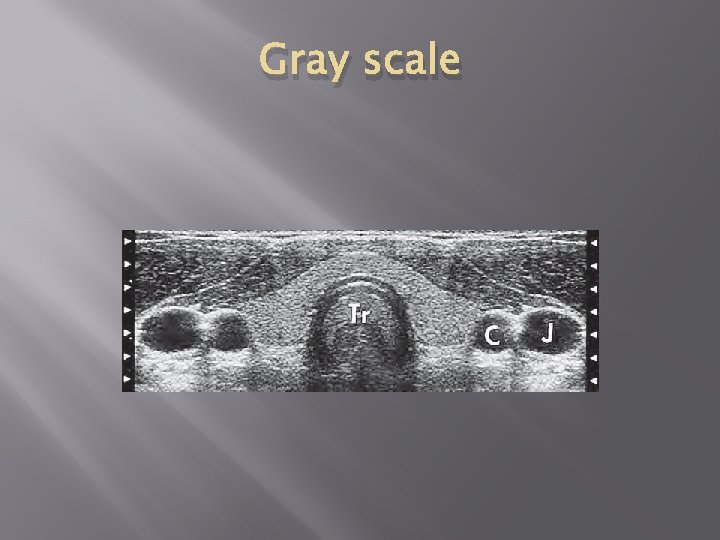
Gray scale


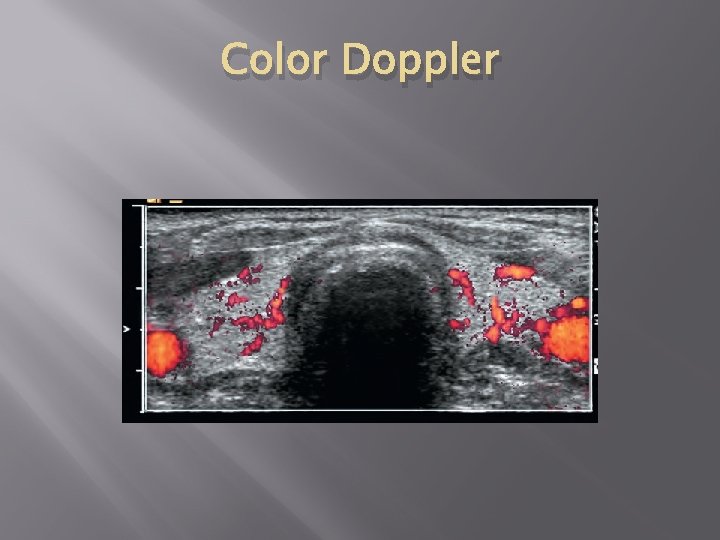
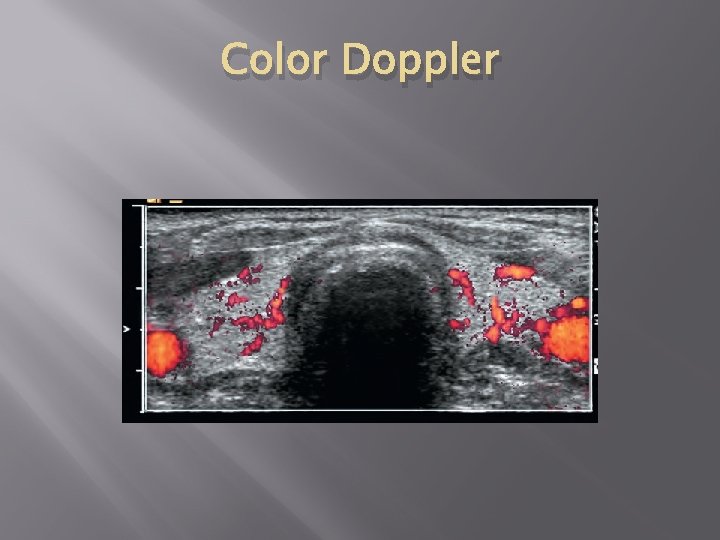
Color Doppler

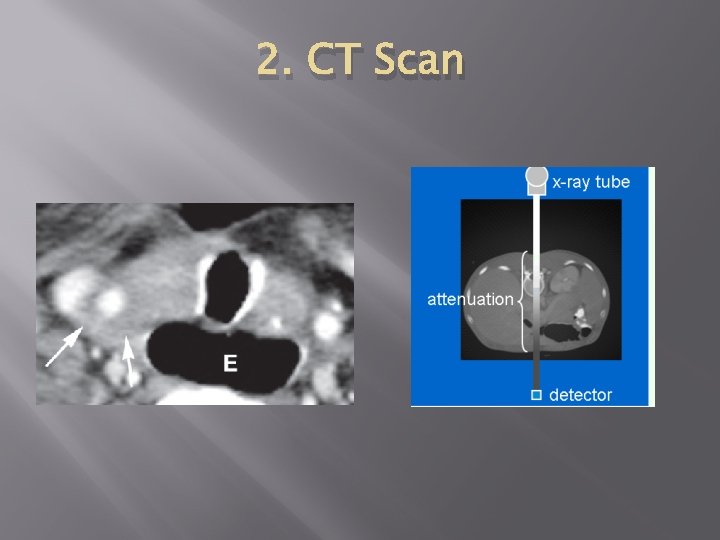
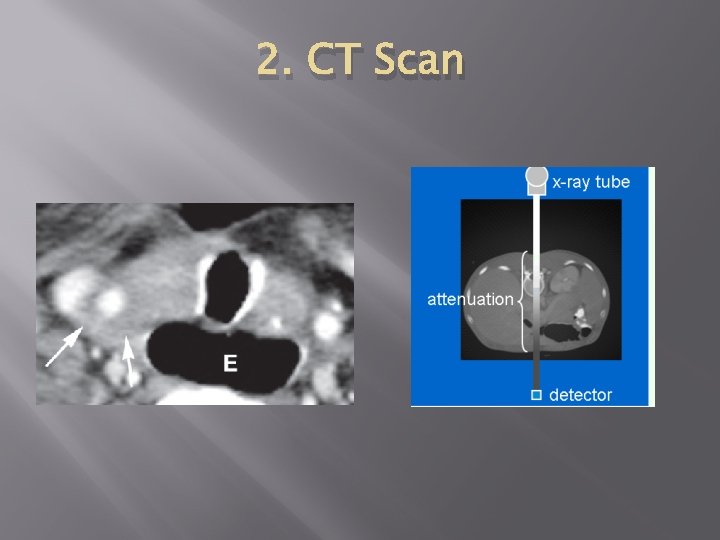
2. CT Scan
3. MRI � Jarang dikerjakan
4. Thyroid scintigraphy


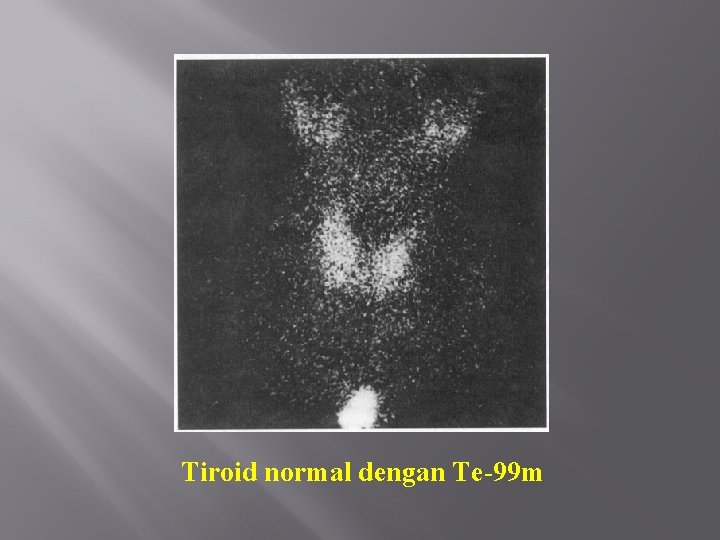
PEMERIKSAAN TIROID SKENING Radiofarmaka 1. Tc-99 m Pertechnetate 2. I-131 Pengambilan citra 1. Dinamik 2. Statik 3. Total body
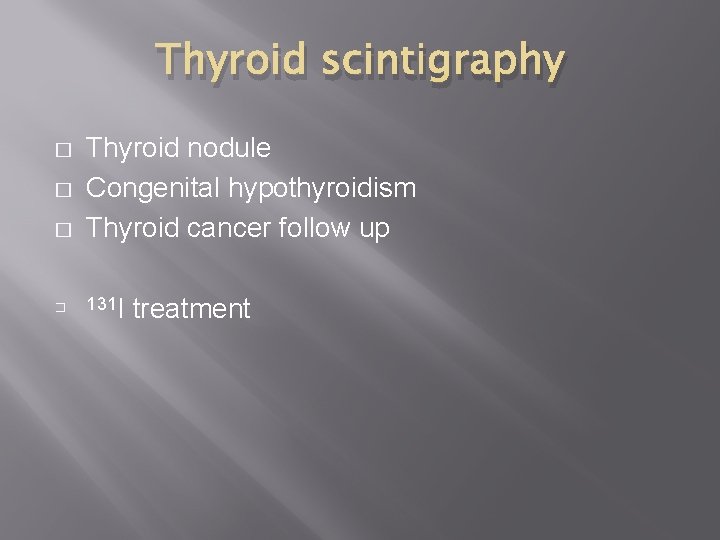
Thyroid scintigraphy � � Thyroid nodule Congenital hypothyroidism Thyroid cancer follow up 131 I treatment
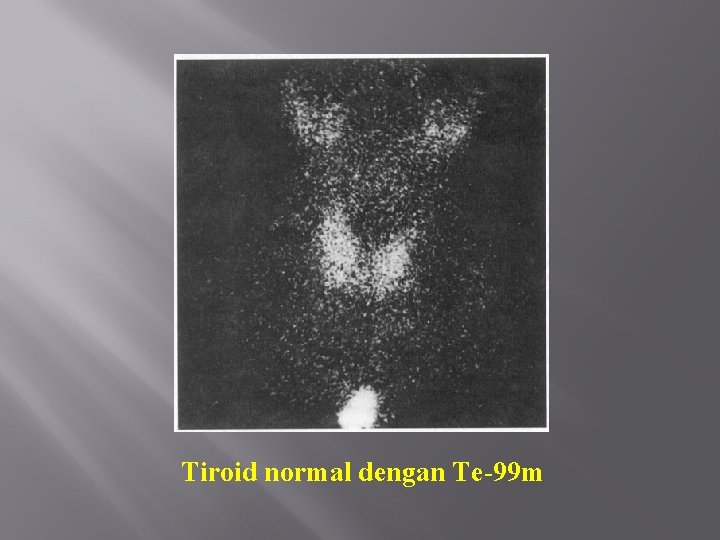
Tiroid normal dengan Te-99 m


Struma multinoduler
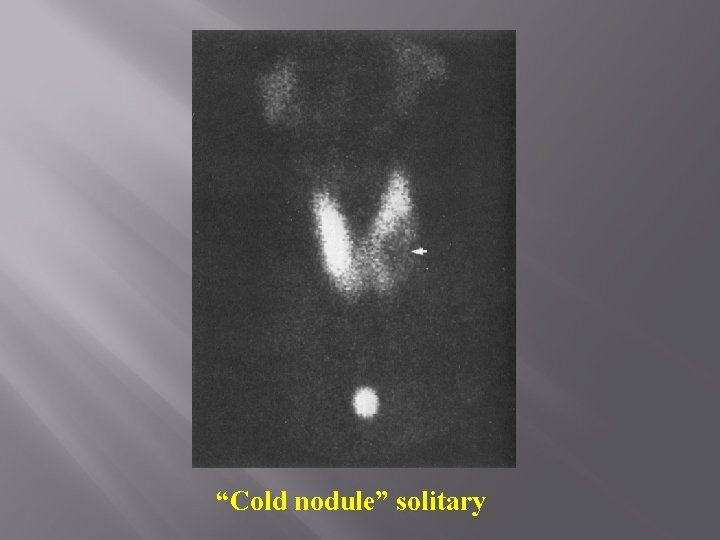
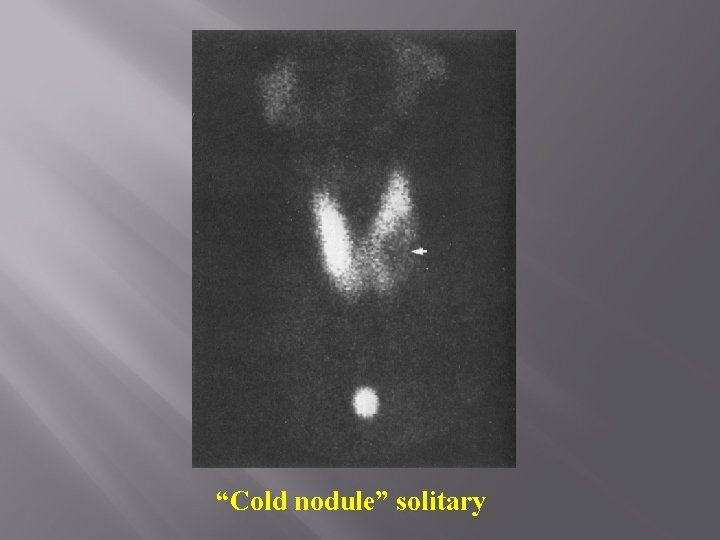
“Cold nodule” solitary
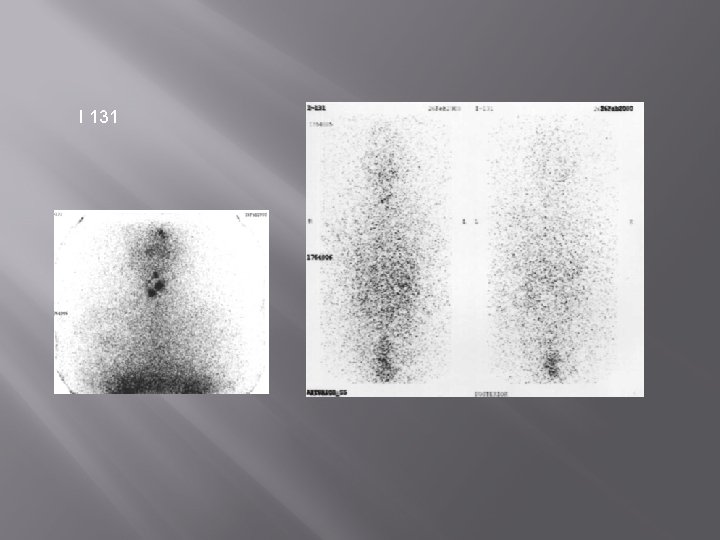
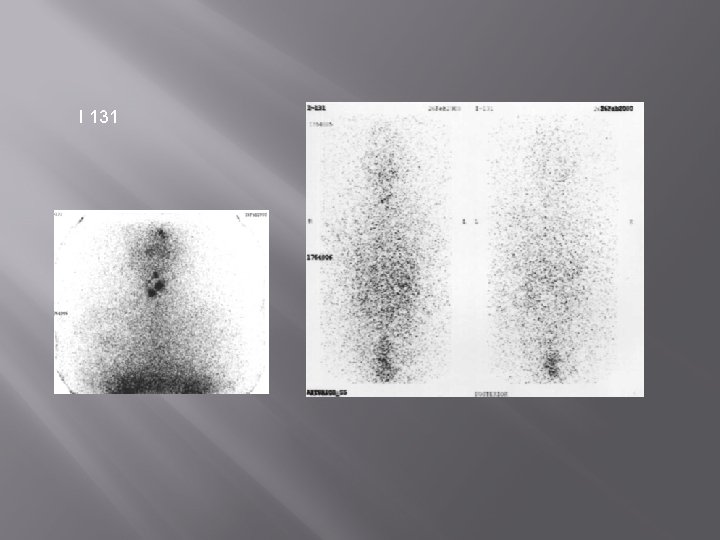
I 131

NUCLEARTHERAPY FOR THYROID DISEASE � Radioisotop : Iodine (I) 131
IODINE (I)-131 THERAPY FOR: 1. 2. Hyperthyroid ( Thyrotoxicosis) Thyroid cancer: 1. Papillary 2. Follicular 3. Mixed papillary and follicular
HYPERTHYROIDISM � � � Toxic diffuse goiter (Graves’ disease) – autoimmune Toxic adenoma – more common in elderly Toxic multinodular goiter- more common in elderly Painful subacute thyroiditis – viral infection Excessive iodine intake – too much hormone production Excessive thyroid hormone replacement therapy
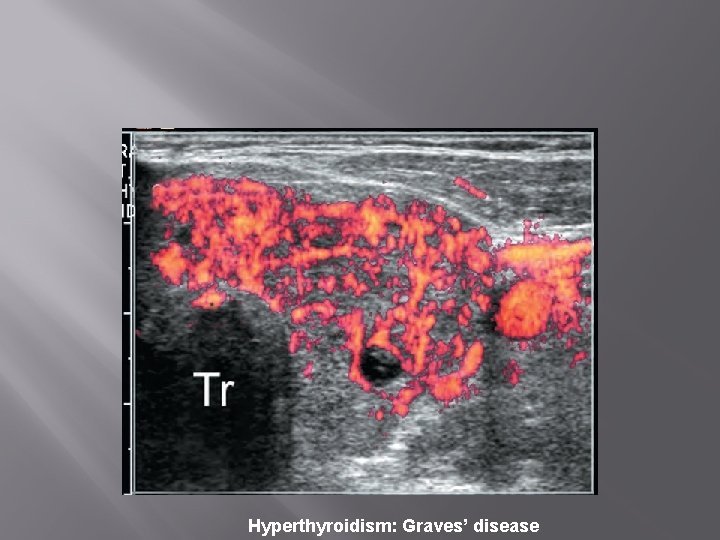
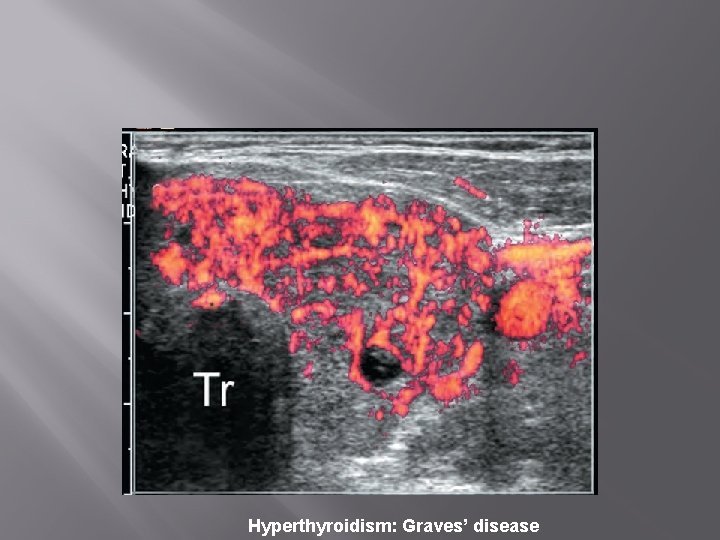
Hyperthyroidism: Graves’ disease
Diagnosis � � � Clinical history and physical examination Routine thyroid hormone function test FT 4, T 4; T 3, FT 3. Thyroid autoantibodies, antithyroid peroxidase, antithyroglobuline antibodies. Radioactive iodine uptake Radioactive thyroid scan Tc-99 m and/or I-131
SIGN AND SYMPTOMS 1. 2. 3. 4. 5. 6. 7. Central nervous system Eye, ear, nose, and throat Musculoskeletal Skin / hair Cardiac Gastrointestinal Genitourinary
The criteria for establishing the diagnosis 1. 2. 3. Subtle symptoms and sign of hyperthyroidism A normal FT 4 level A suppressed serum TSH level
THERAPY General therapy 1. 2. Surgical Intervention Anti thyroid drugs Specific therapy Radioactive iodine (I)-131 is the most common form of therapy in USA. It is used if the general therapy is not response or not possible to be done
INDICATION Treatment of choice: Graves’ disease • Toxic nodular goiter • 25% pt will become hypothyroid 1 year later and will continue to increase yearly • If smaller doses are used, there is a higher incidence of recurrences of hyperthyroidism •

CONTRAINDICATION � � Pregnancy Breastfeeding
DOSES � � 185 – 553 MBq atau 5 – 15 m. Ci
COMPLICATION � � Permanent hypothyroidism Prevalence rises at a rate of 2 -3% per year
� � The success rate of I-131 therapy: �May vary from 75% - 100% Side effect: �Life long hypothyroidism (Radioiodine treatment of hyperthyroidism: prognostic factors for outcome. J Clin Endocrinol Metab. 2001. Aug; 86 (8): 3611 -7)
THYROID CANCER � � Incidence: varies 1 -4/100. 000/year Histological types: � Papillary(paling � Follicular � Anaplastic sering/most case)
THYROID CANCER Papillary: The most common, usually affects women of child bearing age (CBA) Follicular: 30% of all cases, greater rate of recurance and metastasis Medullary: Familial, the symptoms similar to Chushing’s Syndrome Anaplastic: Giant and Spindle Cell Cancer, the most malignant form, does not response to radioiodine therapy, quickly metastasis, invades nearby structures i. e trachea, causing compression, breathing difficulties
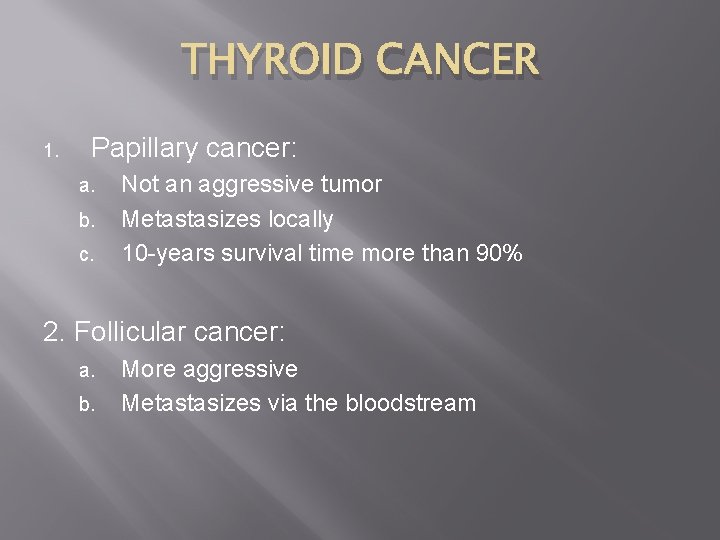
THYROID CANCER 1. Papillary cancer: a. b. c. Not an aggressive tumor Metastasizes locally 10 -years survival time more than 90% 2. Follicular cancer: a. b. More aggressive Metastasizes via the bloodstream
PREVENTION NO KNOWN PREVENTION
SYMPTOMS � � � Enlargement of thyroid gland or neck swelling Hoarseness or changing voice Cough or cough with bleeding Diarhea or constipation Very depending on the type of thyroid cancer
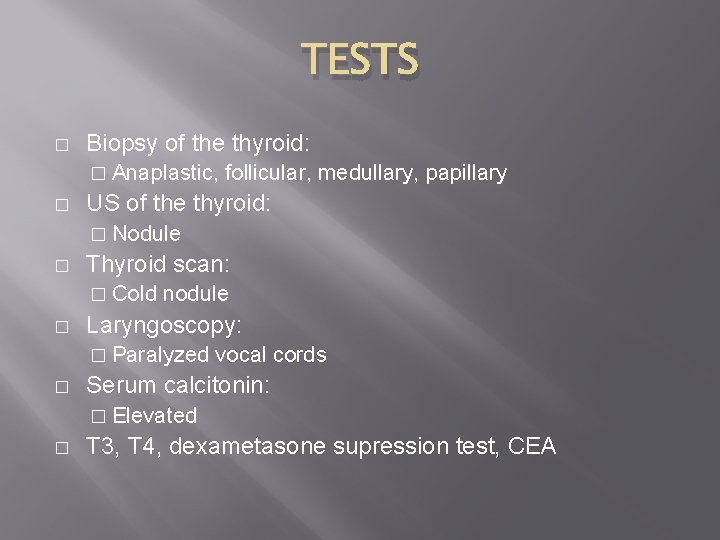
TESTS � Biopsy of the thyroid: � Anaplastic, � follicular, medullary, papillary US of the thyroid: � Nodule � Thyroid scan: � Cold � nodule Laryngoscopy: � Paralyzed � vocal cords Serum calcitonin: � Elevated � T 3, T 4, dexametasone supression test, CEA
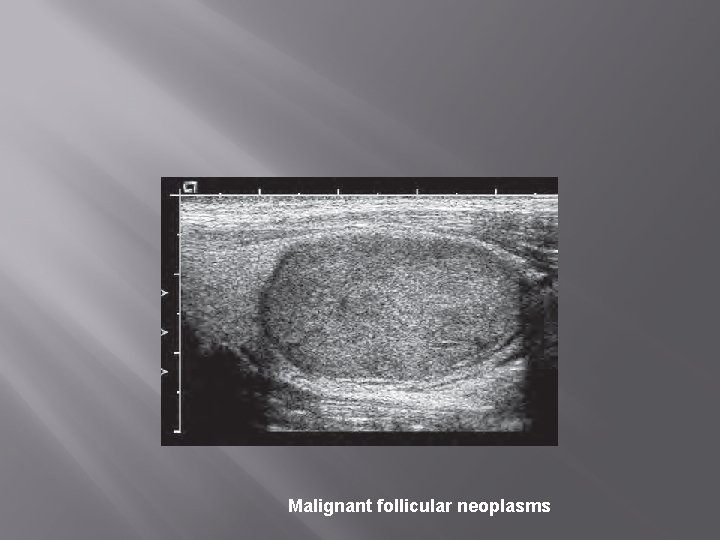
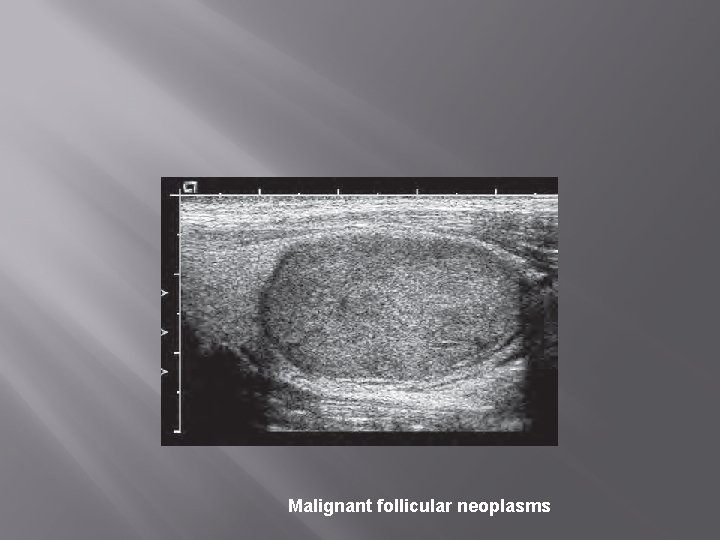
Malignant follicular neoplasms
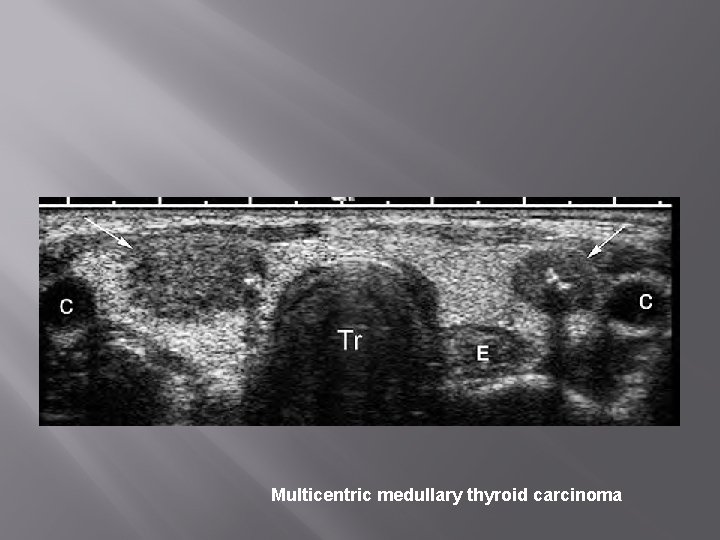
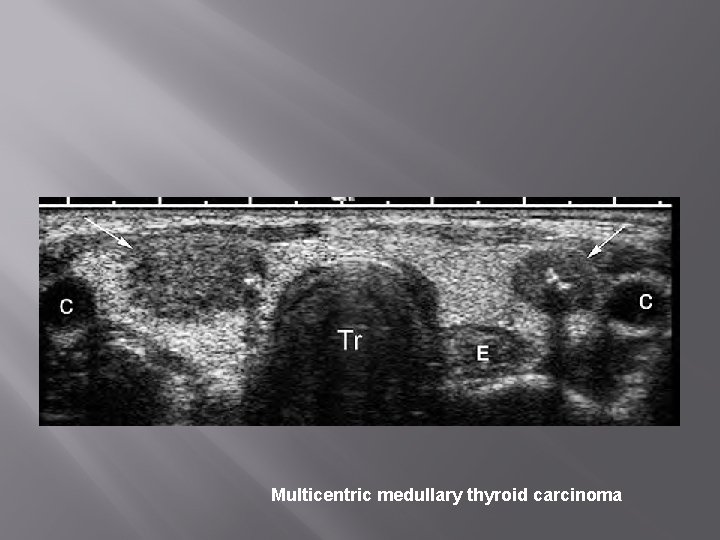
Multicentric medullary thyroid carcinoma
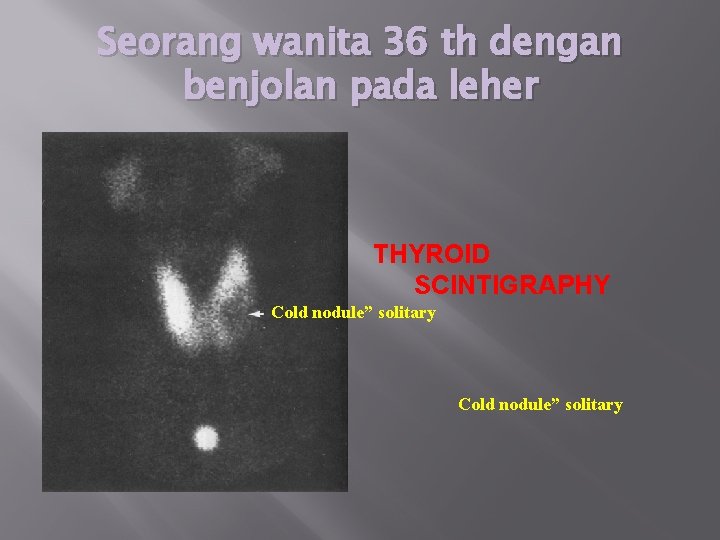
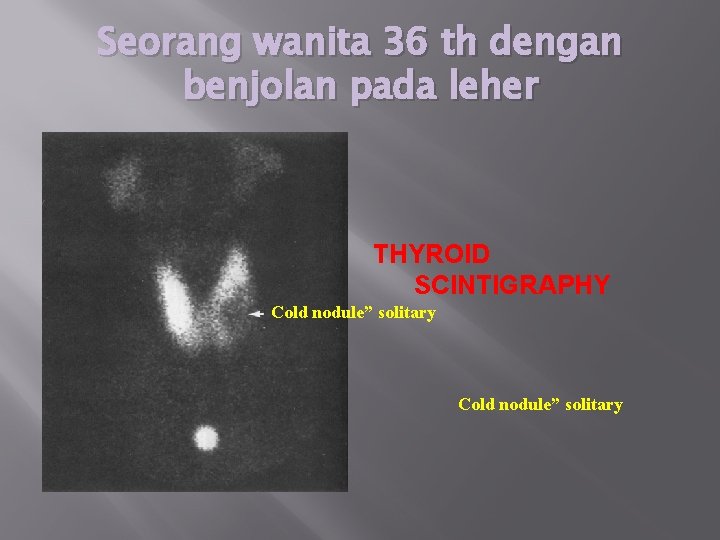
Seorang wanita 36 th dengan benjolan pada leher THYROID SCINTIGRAPHY Cold nodule” solitary
THERAPY OF DIFFERENTIATED THYROID CANCER � � SURGICAL RESECTION RADIOTHERAPY IN MANY CASES (RADIATION THERAPY WITH I-131)
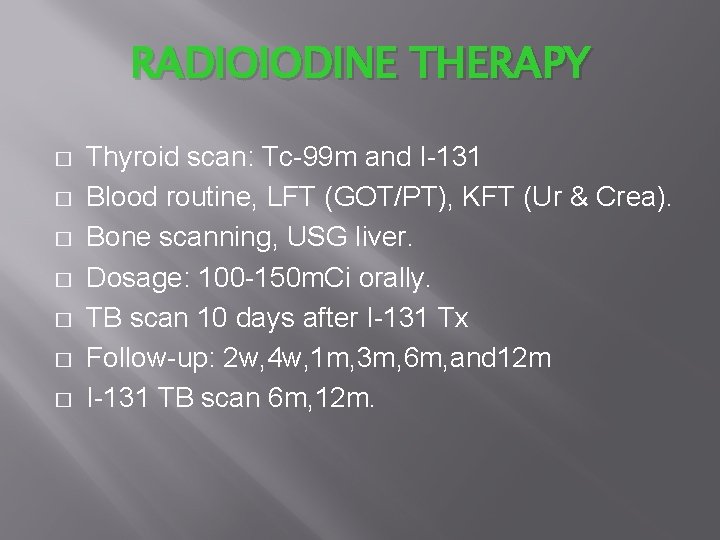
RADIOIODINE THERAPY � � � � Thyroid scan: Tc-99 m and I-131 Blood routine, LFT (GOT/PT), KFT (Ur & Crea). Bone scanning, USG liver. Dosage: 100 -150 m. Ci orally. TB scan 10 days after I-131 Tx Follow-up: 2 w, 4 w, 1 m, 3 m, 6 m, and 12 m I-131 TB scan 6 m, 12 m.
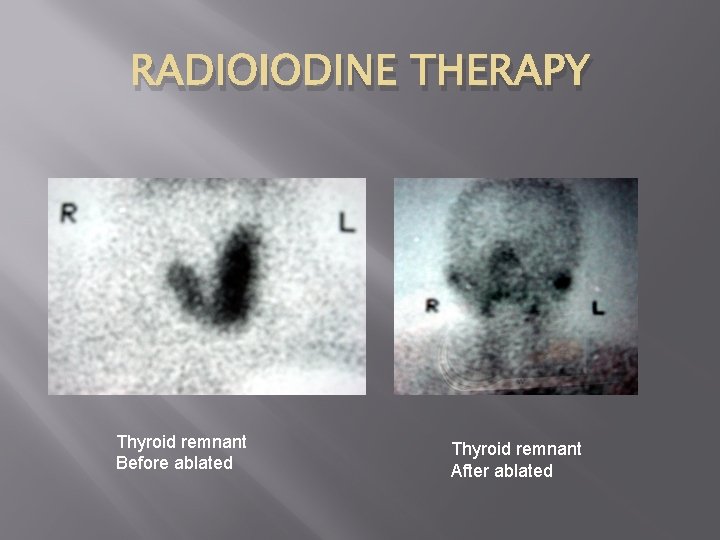
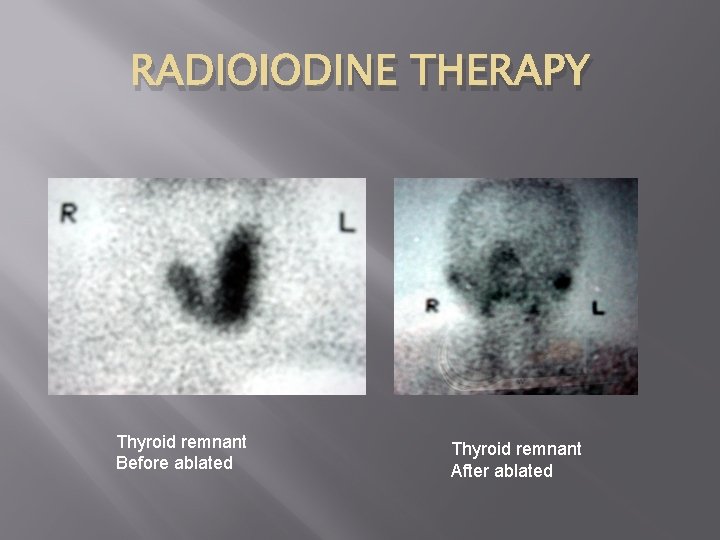
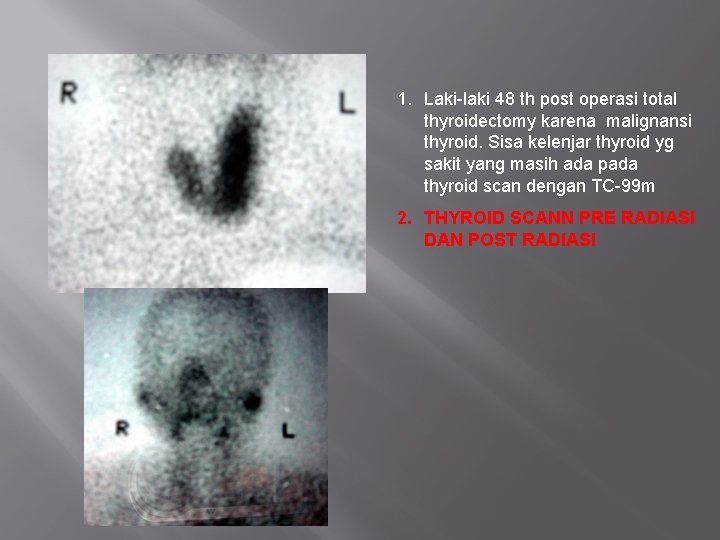
RADIOIODINE THERAPY Thyroid remnant Before ablated Thyroid remnant After ablated
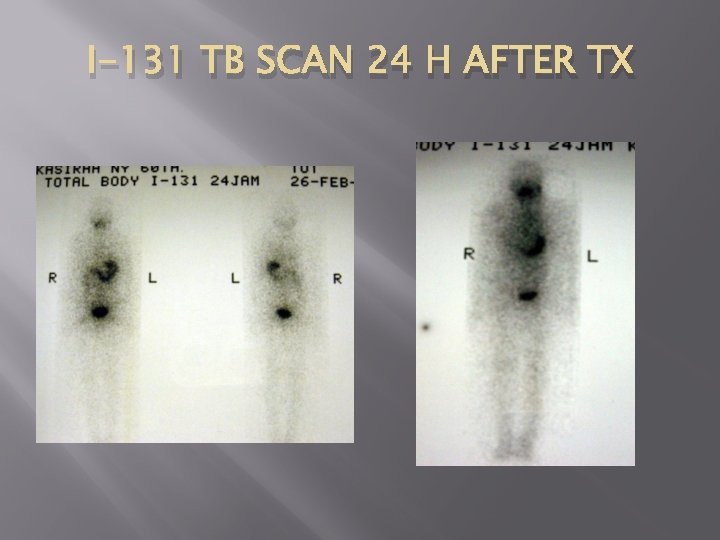
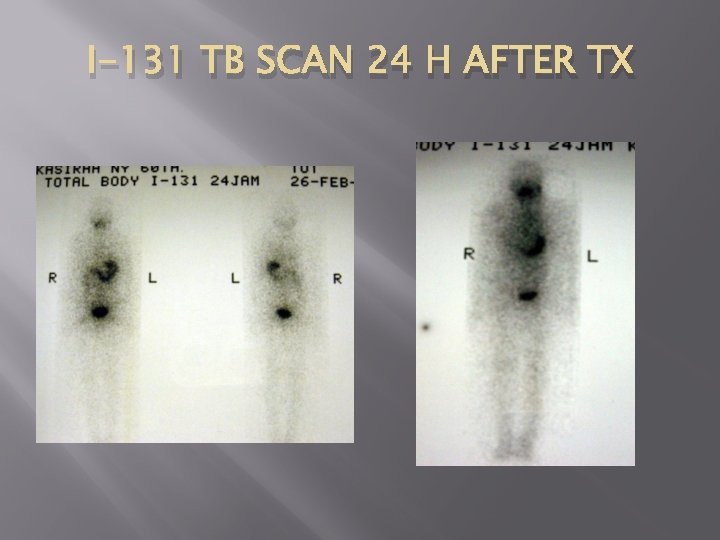
I-131 TB SCAN 24 H AFTER TX
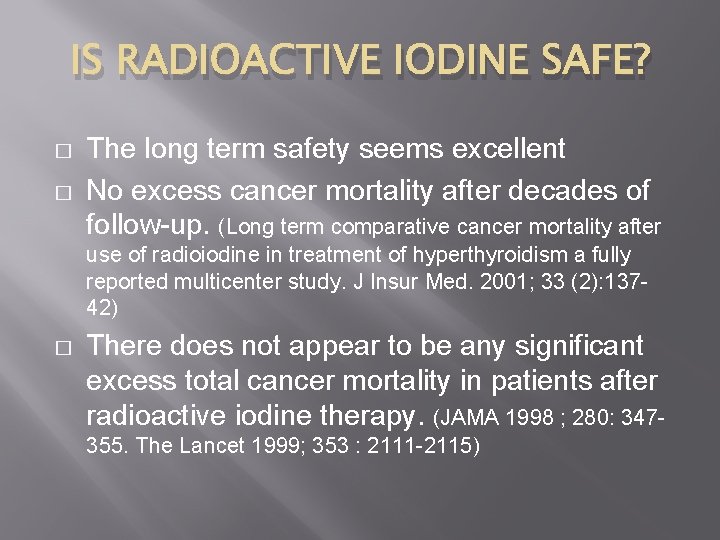
IS RADIOACTIVE IODINE SAFE? � � The long term safety seems excellent No excess cancer mortality after decades of follow-up. (Long term comparative cancer mortality after use of radioiodine in treatment of hyperthyroidism a fully reported multicenter study. J Insur Med. 2001; 33 (2): 13742) � There does not appear to be any significant excess total cancer mortality in patients after radioactive iodine therapy. (JAMA 1998 ; 280: 347355. The Lancet 1999; 353 : 2111 -2115)
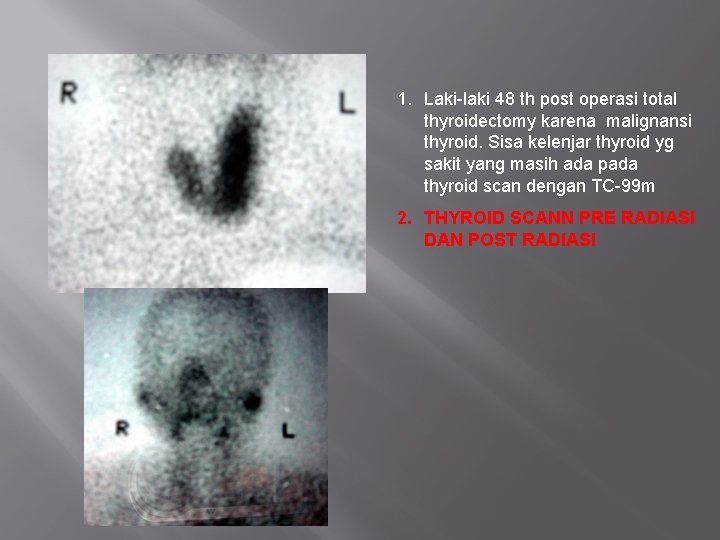
1. Laki-laki 48 th post operasi total thyroidectomy karena malignansi thyroid. Sisa kelenjar thyroid yg sakit yang masih ada pada thyroid scan dengan TC-99 m 2. THYROID SCANN PRE RADIASI DAN POST RADIASI
 Thyroid eye disease
Thyroid eye disease Infection
Infection Neurofibromatosus
Neurofibromatosus Thyroid eye disease
Thyroid eye disease Lid lag
Lid lag Bharathi viswanathan
Bharathi viswanathan Kontinuitetshantering
Kontinuitetshantering Typiska novell drag
Typiska novell drag Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Ekologiskt fotavtryck
Ekologiskt fotavtryck Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Särskild löneskatt för pensionskostnader
Särskild löneskatt för pensionskostnader Vilotidsbok
Vilotidsbok Sura för anatom
Sura för anatom Densitet vatten
Densitet vatten Datorkunskap för nybörjare
Datorkunskap för nybörjare Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Debatt mall
Debatt mall Magnetsjukhus
Magnetsjukhus Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Vätsketryck formel
Vätsketryck formel Publik sektor
Publik sektor Lyckans minut erik lindorm analys
Lyckans minut erik lindorm analys Presentera för publik crossboss
Presentera för publik crossboss Argument för teckenspråk som minoritetsspråk
Argument för teckenspråk som minoritetsspråk Vem räknas som jude
Vem räknas som jude Treserva lathund
Treserva lathund Mjälthilus
Mjälthilus Bästa kameran för astrofoto
Bästa kameran för astrofoto Cks
Cks Byggprocessen steg för steg
Byggprocessen steg för steg Mat för idrottare
Mat för idrottare Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Rutin för avvikelsehantering
Rutin för avvikelsehantering Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Tack för att ni har lyssnat
Tack för att ni har lyssnat Referatmarkering
Referatmarkering Redogör för vad psykologi är
Redogör för vad psykologi är Stål för stötfångarsystem
Stål för stötfångarsystem Atmosfr
Atmosfr Borra hål för knoppar
Borra hål för knoppar Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Hur räknar man standardavvikelse
Hur räknar man standardavvikelse Tack för att ni har lyssnat
Tack för att ni har lyssnat Steg för steg rita
Steg för steg rita Verksamhetsanalys exempel
Verksamhetsanalys exempel Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Toppslätskivling dos
Toppslätskivling dos Handledning reflektionsmodellen
Handledning reflektionsmodellen