Pathophysiology of respiration External respiration is a set






- Slides: 124
Pathophysiology of respiration
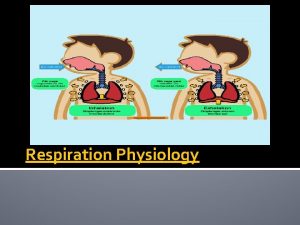
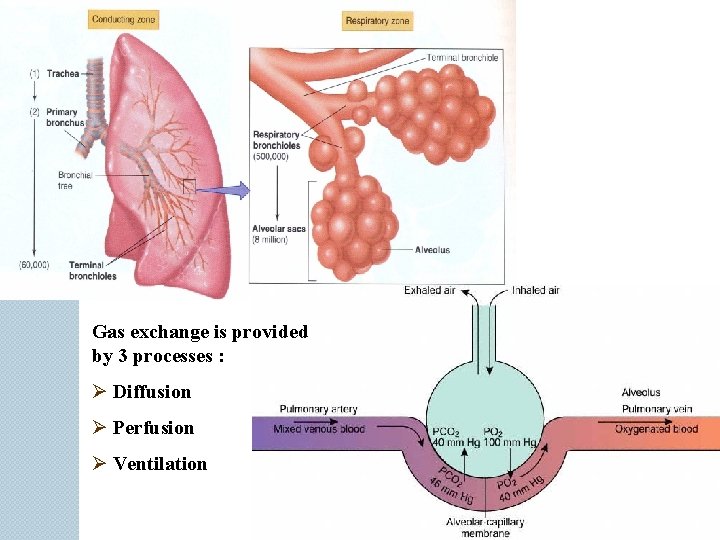
External respiration is a set of processes occurring in lungs and providing normal contents of O 2 and CO 2 in blood. Three primary processes take place in the lungs: ventilation of alveoli, diffusion of O 2 and CO 2 through the alveolar-capillary membrane, perfusion (passing of appropriate amount of blood through the lung capillaries). Strict interconnection of all these processes ensures normal gas composition of blood.
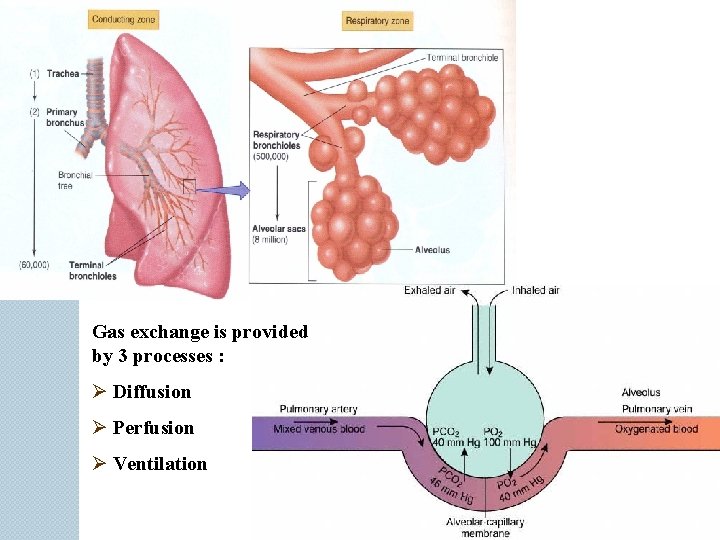
Gas exchange is provided by 3 processes : Ø Diffusion Ø Perfusion Ø Ventilation
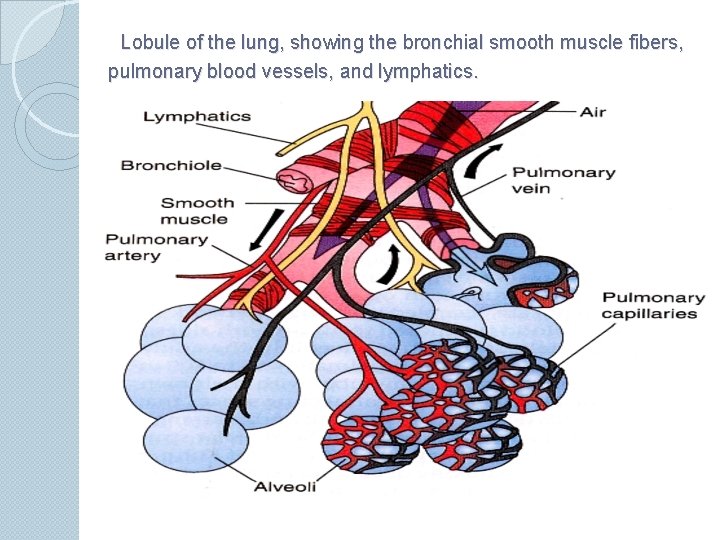
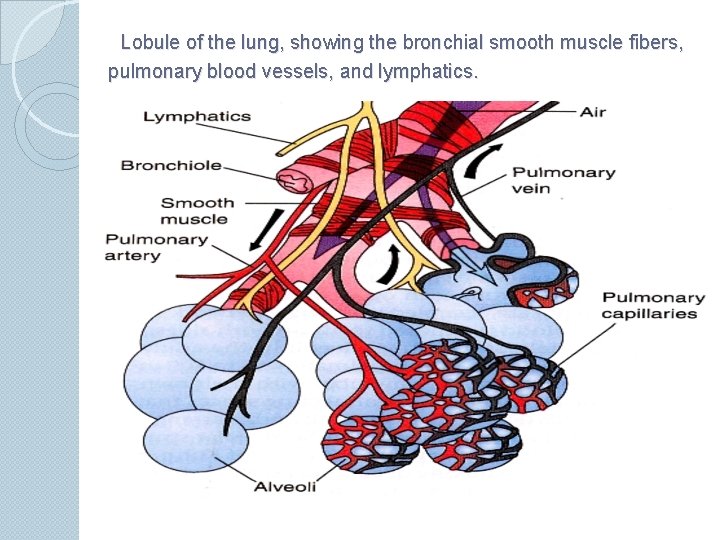
Lobule of the lung, showing the bronchial smooth muscle fibers, pulmonary blood vessels, and lymphatics.
The pressures of oxygen and carbon dioxide in arterial blood are closely controlled. In a normal adult at rest: The pulmonary blood flow of 5 L/min carries 11 mmol/min (250 m. L/min) of oxygen from the lungs to the tissues. Ventilation at about 6 L/min carries 9 mmol/min (200 m. L/min) of carbon dioxide out of the body. Alveolar ventilation at about 4 L/min The normal pressure of O 2 in arterial blood (Pa. O 2) is 12 -13 k. Pa (90 and 98 mm. Hg). The normal pressure of CO 2 in arterial blood (Pa. CO 2) is 4. 8 -6. 0 k. Pa (36 -45 mm. Hg).
Any disease developing in respiratory system may lead to disturbances of one of these processes, decrease in efficacy of respiration and development of respiratory failure. Respiratory failure is a pathological process resulting from impairment of gas exchange between ambient air and circulating blood and leading to inequality of blood gas composition to an organism oxygen demand in rest or in physical loads.
Impaired intrapulmonary gas exchange usually results in primarily hypoxemia (decreased p. O 2 in arterial blood at normal levels of 90 -100 mm Hg), because the diffusing capacity of CO 2 is approximately 25 times grater than that of O 2 and because regional zones of hypoventilation (inadequate alveolar ventilation) with poor CO 2 removal can be compensated for by increased ventilation of normal lung units.
The process of moving gases in and out of the lungs may be inadequate (global or generalized hypoventilation), producing primarily hypercapnia (increased p. CO 2 in arterial blood at normal levels of 45 mm Hg), although hypoxemia occurs as well.
Many pathological processes cause simultaneous failure of both of these function and development of total respiratory failure, but selective or disproportionate impairment of one or the over with development of partial respiratory failure.
Classifications Total respiratory failure – hypoxemia with hypercapnia Partial respiratory failure – hypoxemia without hypercapnia Compensative Decompensative
The clinical symptoms and signs of respiratory failure are nonspecific. The primary physical signs of ventilatory fatigue are Ø vigorous use of accessory ventilatory muscles, Ø tachypnea, Ø tachycardia, Ø declining tidal volume, Ø irregular or gasping breathing patterns, and paradoxal abdominal motion.
Acute hypoxemia may cause diverse problems, including cardiac arrhythmia and coma. Alveolar hypoxia can induce pulmonary arteriolar vasoconstriction and increase pulmonary vascular resistance (Eiler-Lilestrand’s reflex), leading over weeks to months, to pulmonary hypertension, right ventricular hypertrophy (“cor pulmonale”), and eventual right ventricular failure.
Hypercapnia may produce acidemia. Acute CO 2 retention causes acidemia, which when severe (p. H < 7. 3), contributes to: Ø pulmonary arterial vasoconstriction, Ø systemic vascular dilatation, Ø reduced myocardial contractility, Ø hyperkalemia, Ø hypotension, and Ø cardiac irritability, with the potential for life-threatening arrhythmias.
Diffusion is gas exchange across alveolar-capillary membrane. Alveolarcapillary barrier consists of six zones: 1) a fluid layer containing surfactant, 2) the alveolar epithelium; 3) a fluid-filled interstitial space; 4) the capillary endothelium with basement membrane; 5) the blood plasma; 6) the erythrocyte membrane.
Disorders of diffusion Etiology: 1) Increase thickness of the alveolarcapillary membrane (Normal 7 -9 mcm) ◦ in chronic lung disease (sclerosis, fibrosis) ◦ edema of alveolar-capillary membrane (pneumonia, congestion) ◦ adult and newborn respiratory distress syndrome (shock, embolus, DIC-syndrome). 2) Decrease of alveolar-capillary membrane area (emphysema, abscess, lung resection).
Pathogenesis: Ø Diffusion of oxygen through alveolarcapillary membrane in 20 -25 times worse, than for CO 2. Ø If the thickness of the membrane increase, diffusion of O 2 decrease, but diffusion of CO 2 don’t changes. Development partial respiratory failure. Ø Compensation by hyperventilation.
Perfusion is lung blood flow, delivering venous blood to alveoli and arterial blood to left heart. The right ventricle pumps, on average, the same amount of blood through the lungs as the left ventricle sends through the entire systemic circulation. Ignoring the small amount of blood reaching the lungs via the bronchial arteries, the mean pulmonary blood flow or perfusion (Q) equals the cardiac output (5 l/min at rest).
Disorders of perfusion Hyperperfusion and hypoperfusion leads for decrease gas exchange in the lungs. Hyperperfusion Etiology: Asphyxia, stress (total hyperperfusion) Inflammation, atelectasis (local hyperperfusion)
Pathogenesis: For normal O 2 exchange erythrocytes need from 0, 3 to 0, 5 sec for moving through the alveolar capillary. If the speed of blood increase, erythrocytes have not enough time for normal gas exchange. Development hypoxemia. Because diffusion of CO 2 in 20 -25 times better hypercapnia is not developed (partial respiratory failure). In clinics this pathology name functional shunt. Compensation by hyperventilation.
Hypoperfusion Etiology: Pathology of the heart (heart failure, shock, valves dysfunction) Pathology of the vessels (atherosclerosis, tromboembolism).
Pathogenesis has three different variants: Decrease minute volume and hypotension because heart failure development. Opening of shunts between arterials and veins of pulmonary circulation. In this case blood quicker come to the left ventricle and compensate stroke volume, but have not normal oxygenation. In clinics this pathology name anatomical shunt.
If blood flow blocks in some vessels of pulmonary circulation (embolism, sclerosis) development pulmonary hypertension and increase blood flow in working vessels. In this vessels development hyperperfussion. All three cases lead for partial respiratory failure.
If for patients give air with high concentration of oxygen, in hyperperfussion with functional shunt hypoxemia is decrease or disappear, but in hypoperfussion with anatomical shunt hypoxemia don’t change.
Disorders of ventilation Ventilation provides optimal composition of alveolar air necessary for maintenance of gas partial pressure gradients between alveolus and venous blood. In a healthy person alveolar ventilation is typically about 4 liters/minute, and cardiac output averages about 5 liters/minute, for an overall ventilation-perfusion ratio (VPR) of 0. 8. If VPR less than 0, 8 – hypoventilation, if VPR more than 0, 8 – hyperventilation.
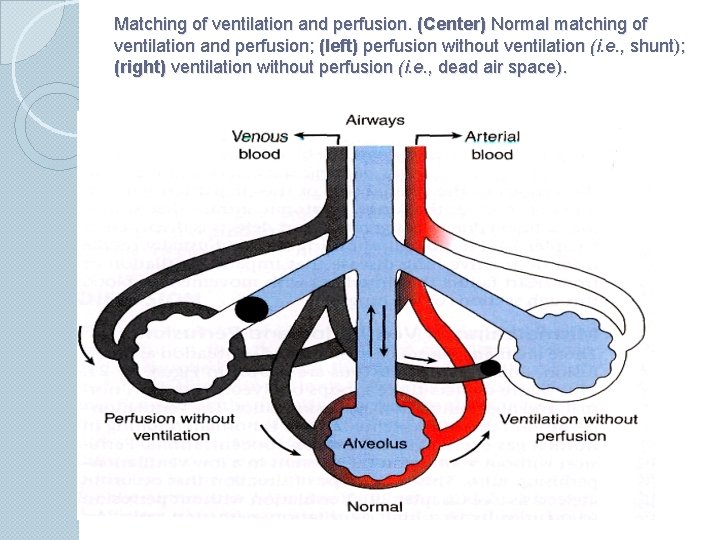
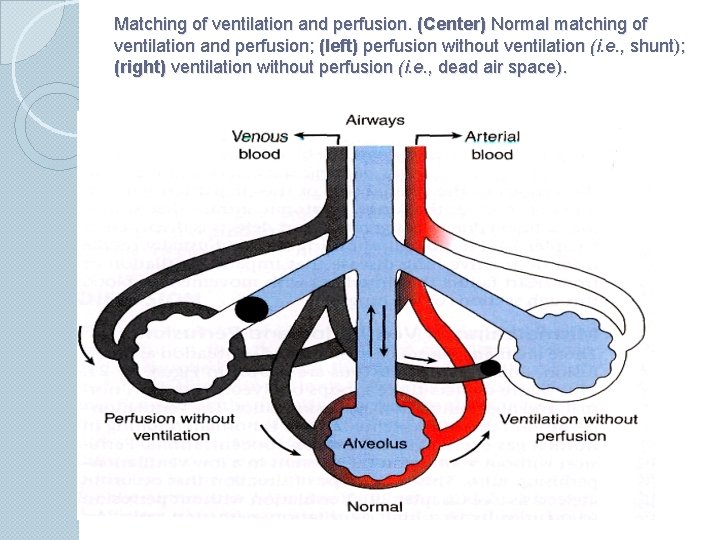
Matching of ventilation and perfusion. (Center) Normal matching of ventilation and perfusion; (left) perfusion without ventilation (i. e. , shunt); (right) ventilation without perfusion (i. e. , dead air space).
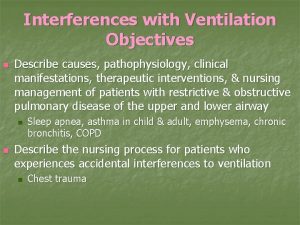
Hypoventilation Etiology: Øpathology of lungs (obstructive and restrictive disorders) Øpathology of respiratory center Øpathology of chest Central, neuromuscular and thoracodiaphragmal disturbances of ventilation: Disorders of functions of respiratory center. Dysfunctions of motoneurons of spinal cord. Dysfunctions of neuromuscular apparatus. Disorders of thorax motility. Damage of integrity of thorax and pleural cavity.
Pathogenesis: Hypoxemia, hypercapnia, gas acidosis, total respiratory failure. Pulmonary hypertension, right ventricular hypertrophy (cor pulmonale), and eventual right ventricular failure (Eiler-Lilestrand’s reflex).
Hyperventilation Etiology: ◦ stimulation of respiratory center ◦ compensation in hemodynamic disorders Pathogenesis: Normoxemia, alkalosis. hypocapnia, gas
Basic clinical manifestations of respiratory failure Dyspnea is an unpleasant sensation of difficulty in breathing. Hyperpnea is an increase in depth and frequency of respiratory movements. Bradypnea is a decrease in frequency of respiratory movements. Tachypnea is a frequent and shallow respiration.
Accordingly to structure of act of respiration it is possibly to distinguish two types of dyspnea: expiratory (difficulties in exhalation) and inspiratory (difficulties in inhalation) ones. Inspiratory dyspnea is observed in case of excitement of respiratory center and restrictive disorders of ventilation. Expiratory dyspnea is characteristic for obstructive disorders.
Pathological types of respiration: (1) Periodical respiration (Cheyne-Stokes’ respiration and Biot’s respiration) is characterized by interchange of the stop of breathing (apnea) with resuming of the respiratory activity. In case of the Cheyne-Stokes’ respiration the cease of respiration is preceded by the gradual decrease in amplitude of respiratory movements. Periods of apnea interchanging with period of resuming of breathing without significant changes in amplitude of respiratory movements are characteristic for Biot’s respiration.
(2) Kussmaul’s respiration (“big”, “noisy” respiration) is characterized by vigorous inhalation and active exhalation with forced contraction of expiratory muscles. (3) Stenotic respiration and gasping respiration; (4) Dissociated respiration (Grocco’s respiration) manifests with non-synchronous contractions of different groups of respiratory muscles (e. g. intracostal muscles constrict and diaphragm relaxes).

Diffuse pulmonary diseases can be classified in two categories: (1) obstructive disease (airway disease), characterized by limitation of airflow usually resulting from an increase in resistance due to partial or complete obstruction at any level; (2) restrictive disease, characterized by reduced expansion of lung parenchyma accompanied by decreased total lung capacity.
Obstructive airway disorders are caused by disorders that limit expiratory air flow. Bronchial asthma represents a reversible form of airway disease caused by narrowing of airways due to bronchospasm, inflammation, and increased airway secretions. Chronic obstructive airway disease can be caused by a variety of airway diseases, including chronic bronchitis, emphysema, bronchiectasis, and cystic fibrosis.
The term chronic obstructive pulmonary disease encompasses two types of obstructive airway disease: emphysema, with enlargement of air spaces and destruction of lung tissue, chronic obstructive bronchitis, with obstruction of small airways.
Asthma
Introduction Chronic inflammatory disease of the airways Most common childhood chronic disease Affects ~4. 8 million >100 million days of restricted activity 470, 000 hospitalizations/yr
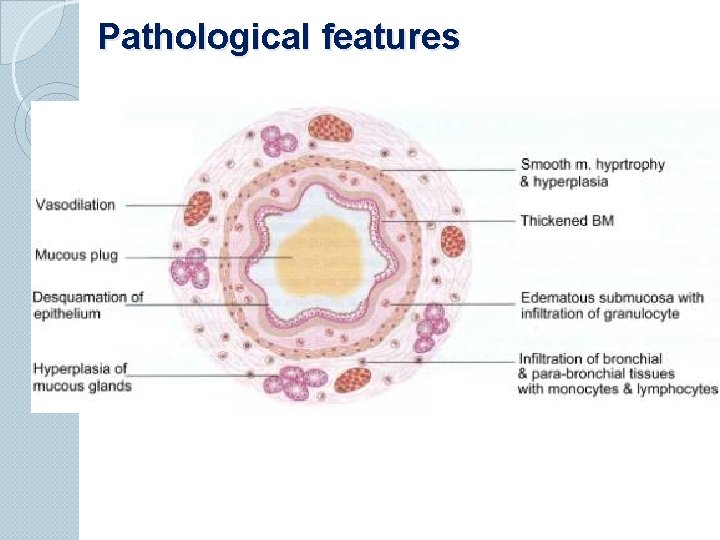
Pathogenesis and Definition Key points ◦ Chronic inflammatory disorder of the airways ◦ Immunohistopathologic features denudation of airway epithelium collagen deposition beneath basement membrane edema mast cell activation
◦ Immunohistopathologic features inflammatory cell infiltration Neutrophils (sudden, fatal asthma) Eosinophils Lymphocytes Airway inflammation (AI) contributes to hyperresponsiveness, airflow limitation, symptoms & chronicity AI causes types of airflow limitation: ◦ Bronchoconstriction, edema, mucus plug formation, airway wall remodeling Atopy is strongest predisposing factor for developing asthma
Working definition of asthma Ø Asthma is a chronic inflammatory disorder of the airways in which many cells & cellular elements play a role (mast cells, eosinophils, T lymphocytes, macrophages, neutrophils, & epithelial cells). Ø In susceptible individuals , inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night/early morning. These episodes are associated with variable airflow obstruction often reversible spontaneously/treatment
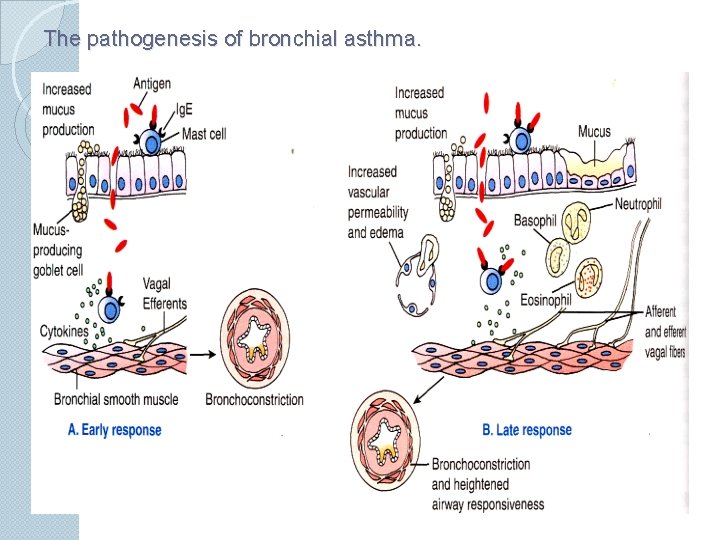
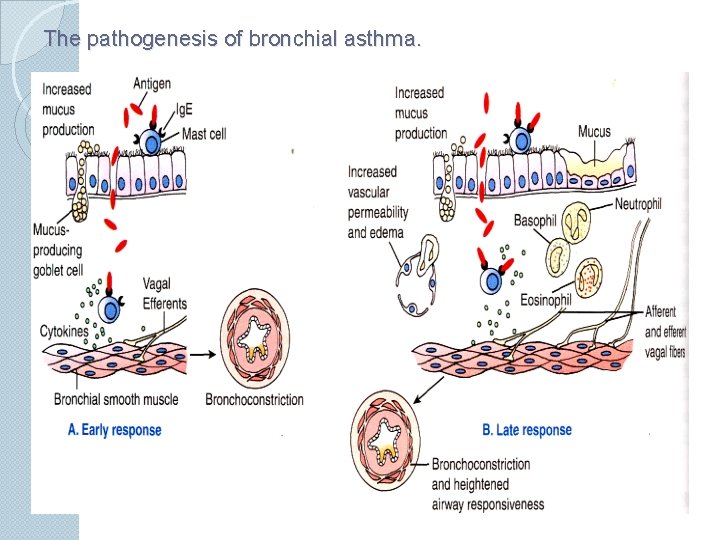
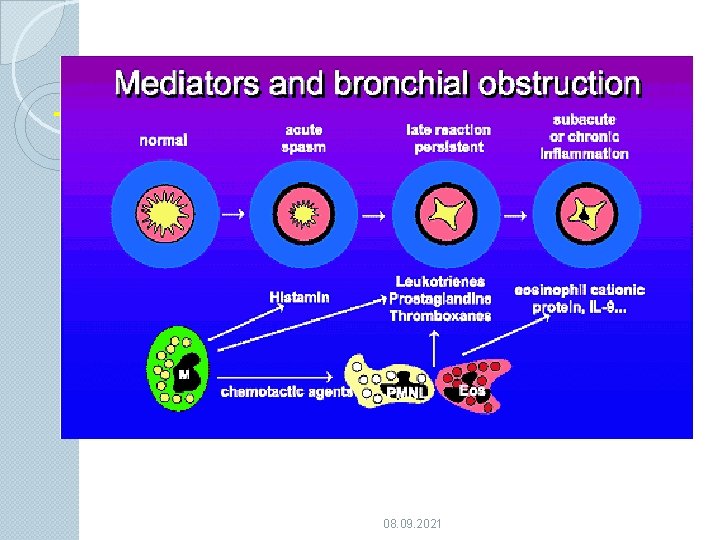
The pathogenesis of bronchial asthma.
08. 09. 2021
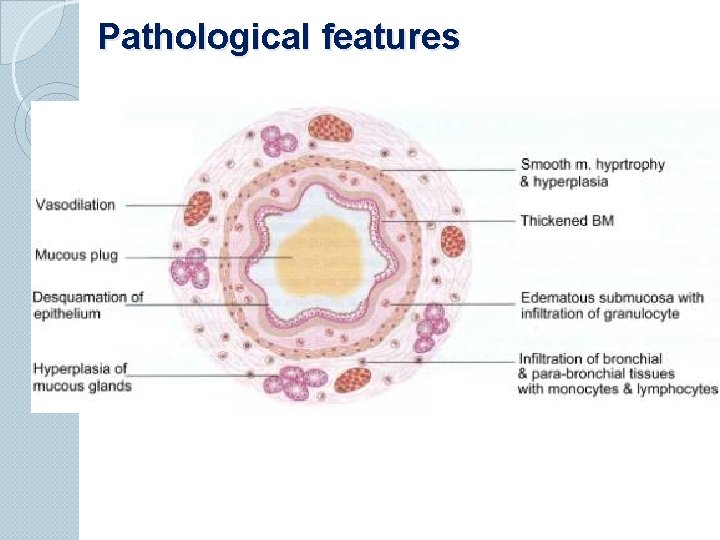
Pathological features
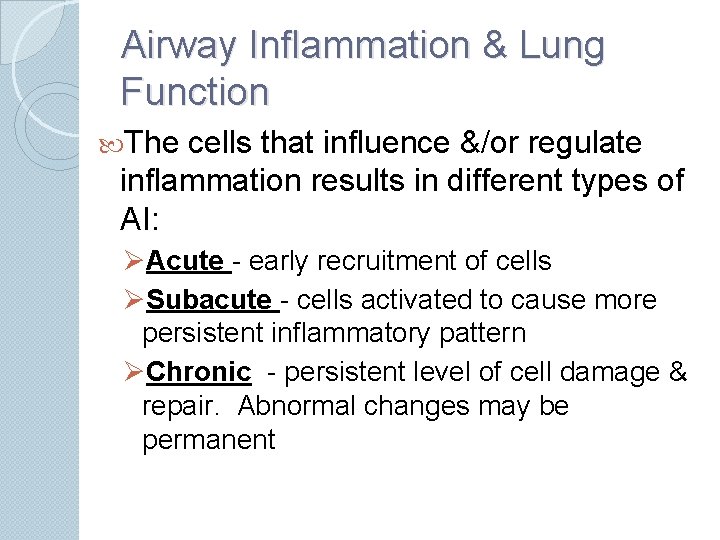
Airway Inflammation & Lung Function The cells that influence &/or regulate inflammation results in different types of AI: ØAcute - early recruitment of cells ØSubacute - cells activated to cause more persistent inflammatory pattern ØChronic - persistent level of cell damage & repair. Abnormal changes may be permanent
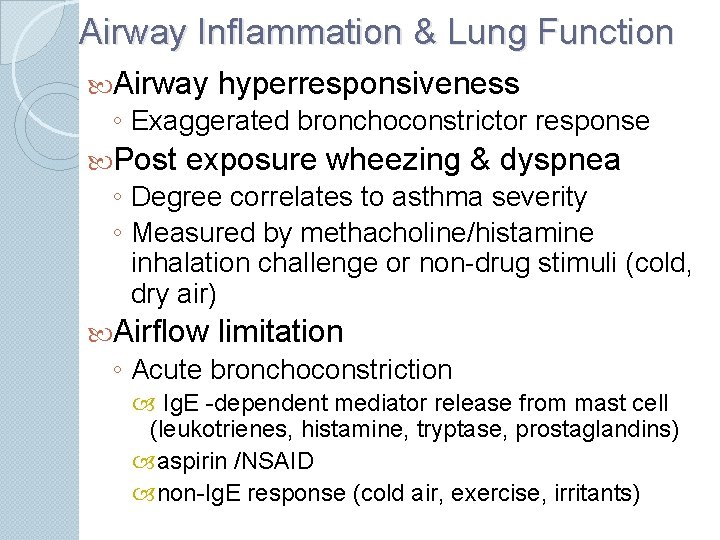
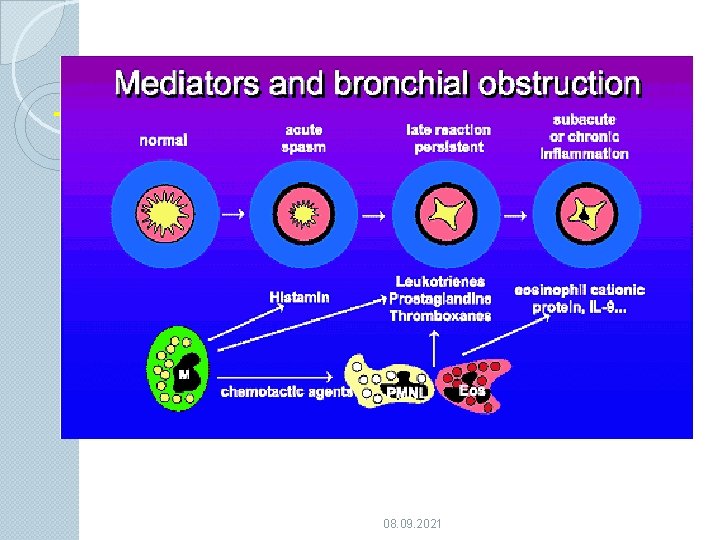
Airway Inflammation & Lung Function Airway hyperresponsiveness ◦ Exaggerated bronchoconstrictor response Post exposure wheezing & dyspnea ◦ Degree correlates to asthma severity ◦ Measured by methacholine/histamine inhalation challenge or non-drug stimuli (cold, dry air) Airflow limitation ◦ Acute bronchoconstriction Ig. E -dependent mediator release from mast cell (leukotrienes, histamine, tryptase, prostaglandins) aspirin /NSAID non-Ig. E response (cold air, exercise, irritants)
Airflow limitation ◦ Acute bronchoconstriction stress - mechanisms ? ? Airway edema mediators increase microvascular permeability/ leakage mucosal thickening & airway swelling airway rigidity Airflow limitation ◦ Chronic mucus plug formation secretions & inspissated plugs persistent airflow limitation in severe intractable asthma ◦ Airway remodeling irreversible component of airflow limitation secondary to structural airway matrix changes attributed to chronic, severe airway inflammation early intervention with anti-inflammatory therapy suggests prevention of permanent airflow limitation
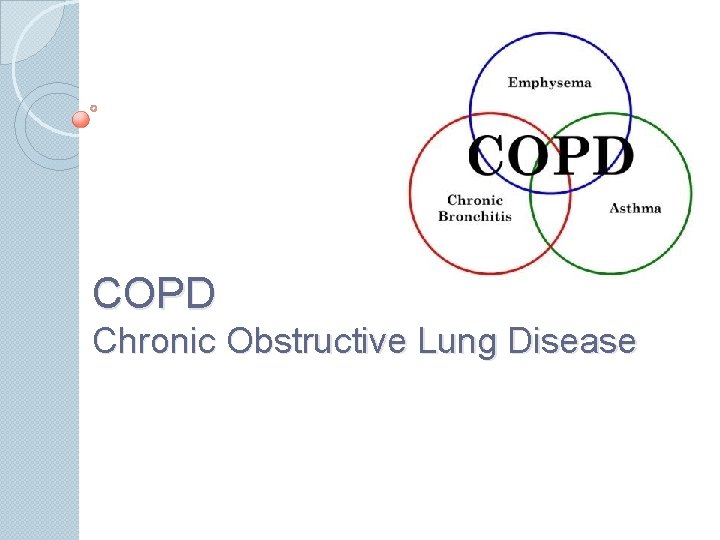
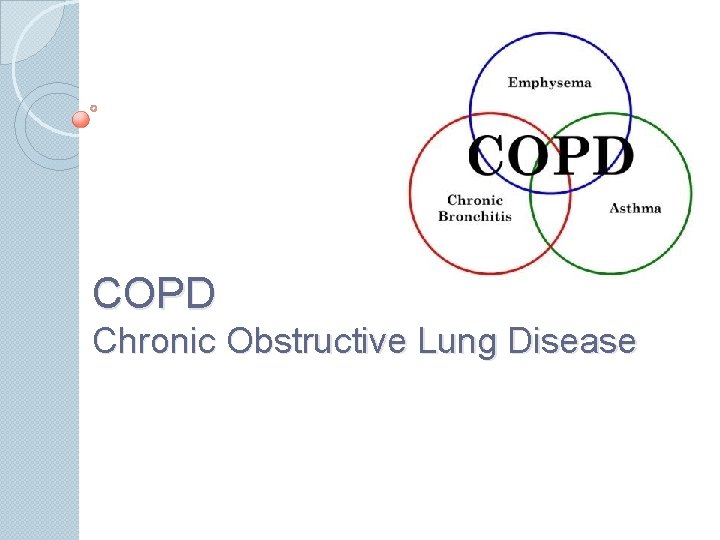
COPD Chronic Obstructive Lung Disease
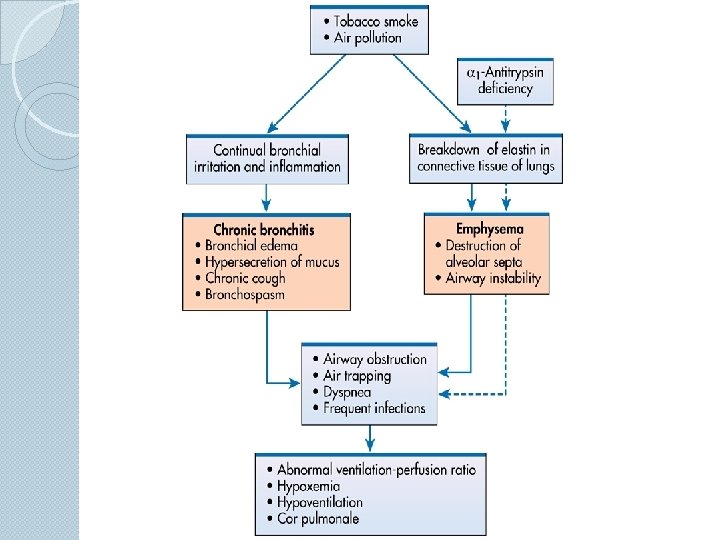
COPD Description Ø Characterized by presence of airflow obstruction Ø Caused by emphysema or chronic bronchitis Ø Generally progressive Ø May be accompanied by airway hyperreactivity Ø May be partially reversible
Emphysema Description Ø Abnormal permanent enlargement of the air space distal to the terminal bronchioles Ø Accompanied bronchioles by destruction of
Chronic Bronchitis Description Ø Presence of chronic productive cough for 3 or more months in each of 2 successive years in a patient whom other causes of chronic cough have been excluded
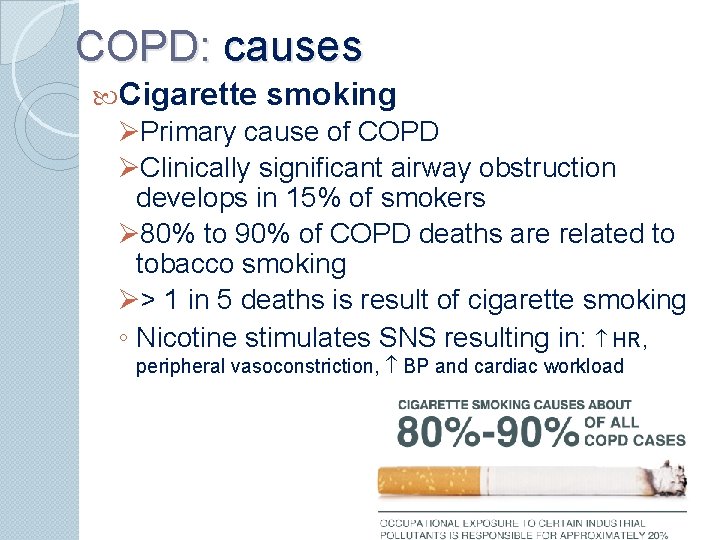
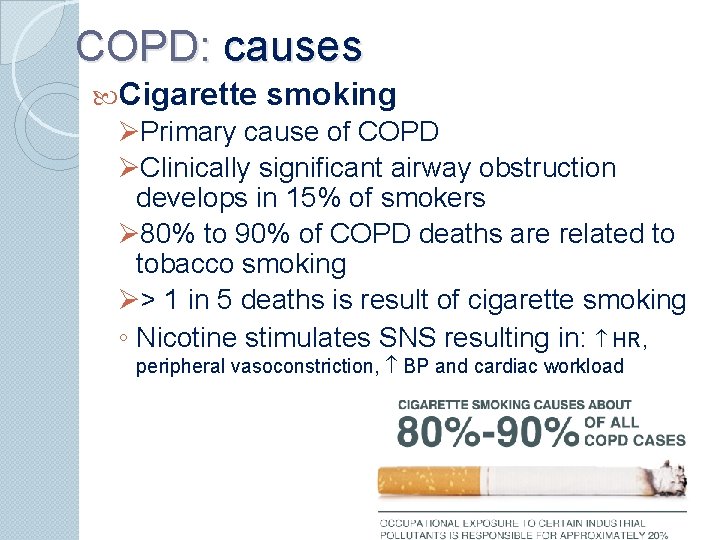
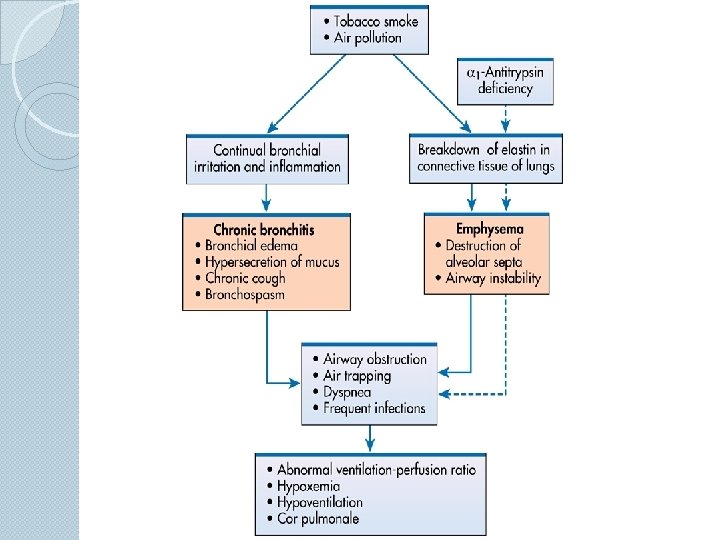
COPD: causes Cigarette smoking ØPrimary cause of COPD ØClinically significant airway obstruction develops in 15% of smokers Ø 80% to 90% of COPD deaths are related to tobacco smoking Ø> 1 in 5 deaths is result of cigarette smoking ◦ Nicotine stimulates SNS resulting in: HR, peripheral vasoconstriction, BP and cardiac workload
Cigarette smoking ◦ Compounds problems in a person with Coronary Artery Disease ◦ Ciliary activity ◦ Possible loss of ciliated cells ◦ Abnormal dilation of the distal air space ◦ Alveolar wall destruction ◦ Carbon monoxide O 2 carrying capacity Impairs psychomotor performance and judgment ◦ Cellular hyperplasia Production of mucus Reduction in airway diameter Increased difficulty in clearing secretions
Secondhand smoke exposure Associated with: ◦ Pulmonary function ◦ Risk of lung cancer ◦ Mortality rates from ischemic heart disease
COPD: causes Prolonged exposures to harmful particles and gases from: ◦ ◦ Second-hand smoke, Industrial smoke, Chemical gases, vapors, mists & fumes Dusts from grains, minerals & other materials Infection ◦ Major contributing factor to the aggravation and progression of COPD Heredity ◦ -Antitrypsin (AAT) deficiency (produced by liver and found in lungs); accounts for < 1% of COPD cases Emphysema results from lysis of lung tissues by proteolytic enzymes from neutrophils and macrophages
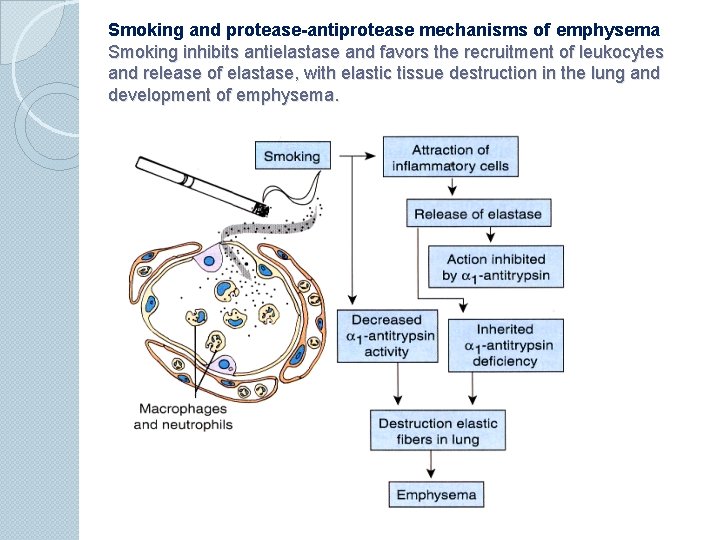
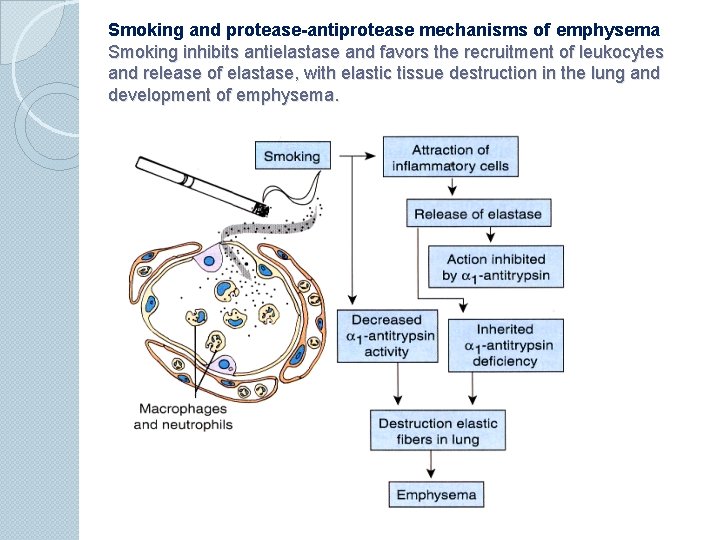
Smoking and protease-antiprotease mechanisms of emphysema Smoking inhibits antielastase and favors the recruitment of leukocytes and release of elastase, with elastic tissue destruction in the lung and development of emphysema.
Emphysema: pathophysiology ØDestruction of alveolar walls ØDestruction of alveolar capillary membrane ØNarrowed airways ØLoss of lung elasticity Two types: Centrilobular (central part of lobule) Most common Panlobular (destruction of whole lobule) Usually associated with AAT deficiency
Emphysema: pathophysiology ◦ Small bronchioles become obstructed as a result of Mucus Smooth muscle spasm Inflammatory process Collapse of bronchiolar walls ◦ Recurrent infections → production /stimulation of neutrophils and macrophages →release proteolytic enzymes→alveolar destruction→ inflammation, exudate, and edema ◦ Elastin and collagen are destroyed ◦ Air goes into the lungs but is unable to come out on its own and remains in the lung Causes bronchioles to collapse

Emphysema: pathophysiology ØTrapped air hyperinflation and overdistention ØAs more alveoli coalesce, blebs and bullae may develop ØDestruction of alveolar walls and capillaries reduced surface area for O 2 diffusion ØCompensation is done by increasing respiratory rate to increase alveolar ventilation ØHypoxemia usually develops late in disease
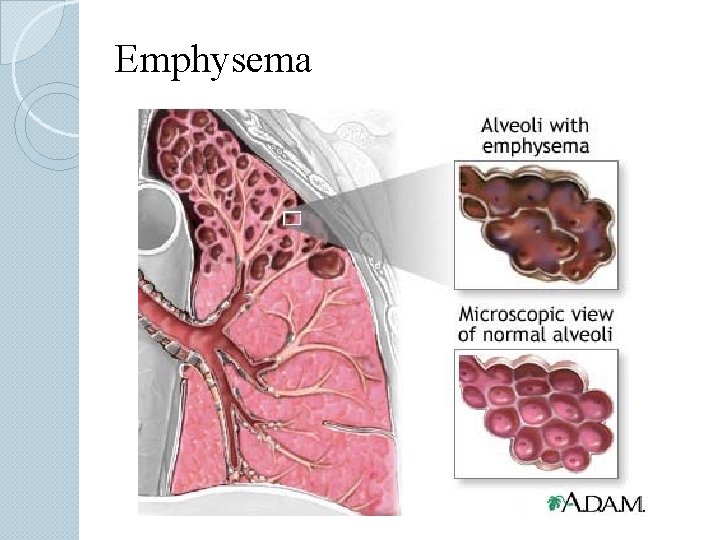
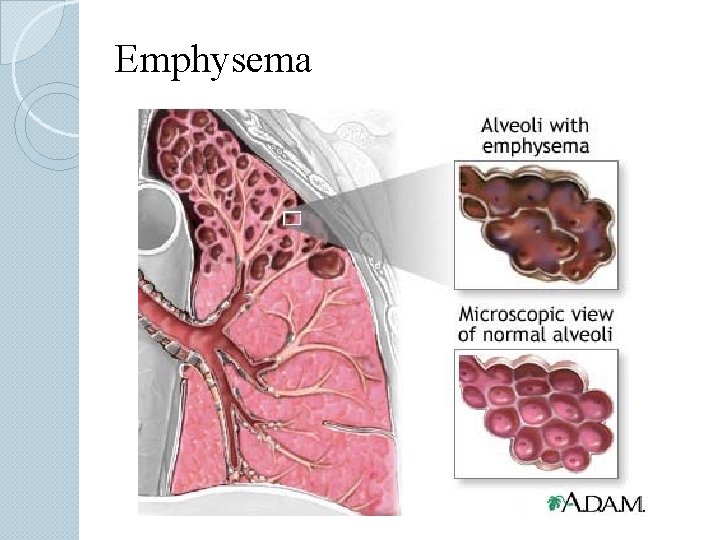
Emphysema
Emphysema: manifestations ◦ Dyspnea ØProgresses in severity ØPatient will first complain of dyspnea on exertion and progress to interfering with ADLs and rest ◦ Minimal coughing with no to small amounts of sputum ◦ Overdistention of alveoli causes diaphragm to flatten ◦ Patient becomes chest breather, relying on accessory muscles Ribs become fixed in inspiratory position Patient is underweight (despite adequate calorie intake)
Chronic Bronchitis Pathophysiology Pathologic lung changes are: üHyperplasia of mucus-secreting glands in trachea and bronchi üIncrease in goblet cells üDisappearance of cilia üChronic inflammatory changes and narrrowing of small airways üAltered fxn of alveolar macrophages → infections
Chronic Bronchitis: pathophysiology ◦ Bronchioles are clogged with mucus and pose a physical barrier to ventilation ◦ Greater resistance to airflow increases work of breathing ◦ Hypoxemia and hypercapnia develop more frequently in chronic bronchitis (lack of ventilation and O 2 diffusion) than emphysema ◦ Hypoxemia and hypercapnia; retain CO 2 ◦ Cough is ineffective to remove secretions because the person cannot breathe deeply enough ◦ Bronchospasm frequently develops More common with history of smoking or asthma
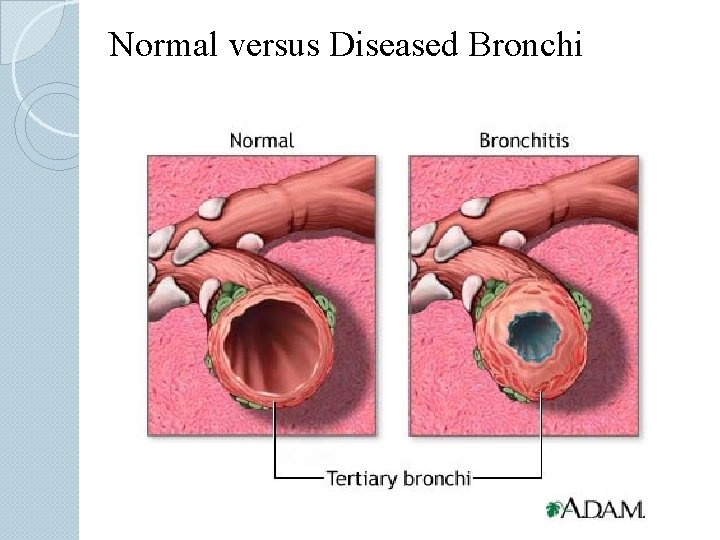
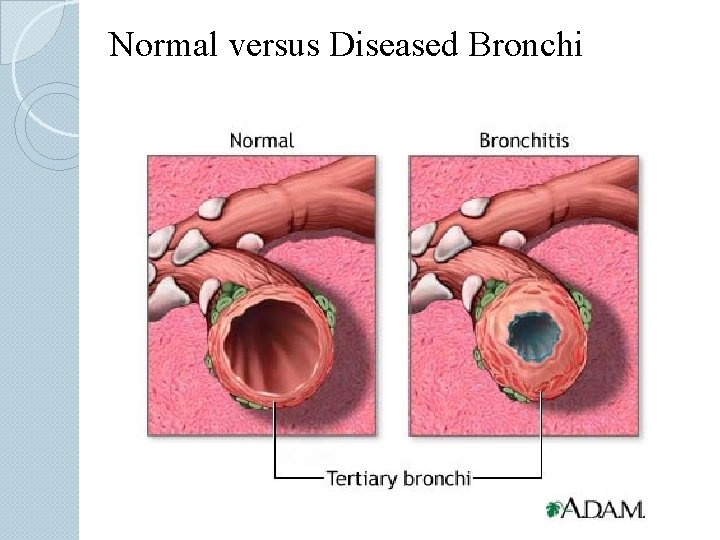
Normal versus Diseased Bronchi
Chronic Bronchitis: manifestations ◦ Earliest symptoms: Frequent, productive cough during winter Frequent respiratory infections ◦ Bronchospasm at end of paroxysms of coughing ◦ Dyspnea on exertion ◦ History of smoking ◦ Ruddy (bluish-red) appearance polycythemia (due to chronic hypoxemia) cyanosis ◦ Hypoxemia and hypercapnia Results from hypoventilation and airway resistance + problems with alveolar gas exchange
Summary Chronic Bronchitis is characterized by ◦ Chronic inflammation and excess mucus production ◦ Presence of chronic productive cough Emphysema is characterized by ◦ Damage to the small, sac-like units of the lung that deliver oxygen into the lung and remove the carbon dioxide ◦ Chronic dyspnea
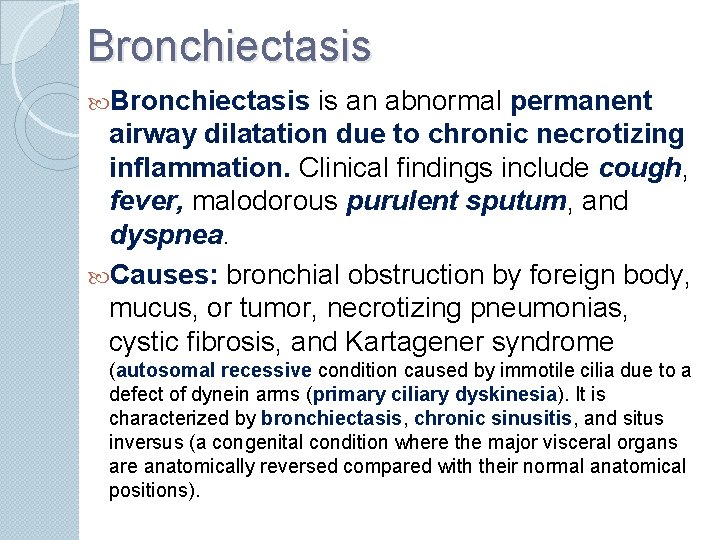
Bronchiectasis is an abnormal permanent airway dilatation due to chronic necrotizing inflammation. Clinical findings include cough, fever, malodorous purulent sputum, and dyspnea. Causes: bronchial obstruction by foreign body, mucus, or tumor, necrotizing pneumonias, cystic fibrosis, and Kartagener syndrome (autosomal recessive condition caused by immotile cilia due to a defect of dynein arms (primary ciliary dyskinesia). It is characterized by bronchiectasis, chronic sinusitis, and situs inversus (a congenital condition where the major visceral organs are anatomically reversed compared with their normal anatomical positions).
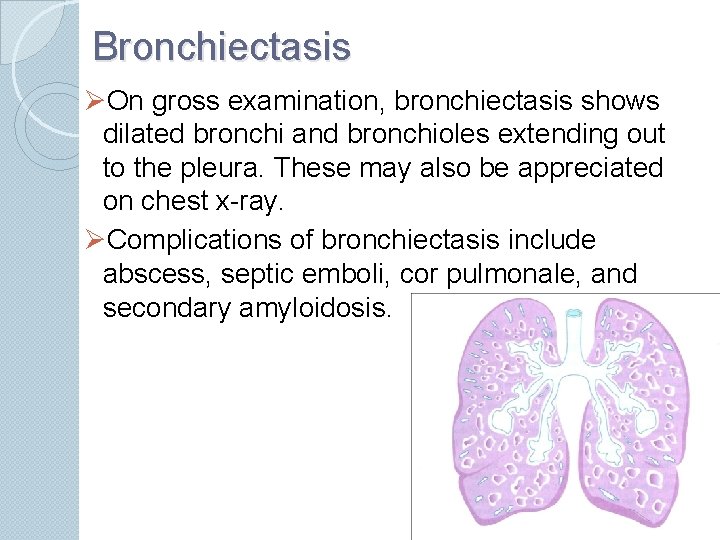
Bronchiectasis ØOn gross examination, bronchiectasis shows dilated bronchi and bronchioles extending out to the pleura. These may also be appreciated on chest x-ray. ØComplications of bronchiectasis include abscess, septic emboli, cor pulmonale, and secondary amyloidosis.
Restrictive Lung Diseases
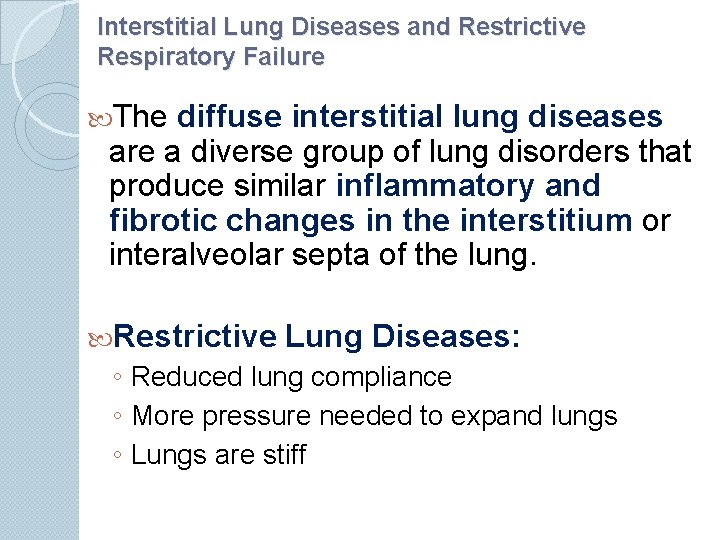
Interstitial Lung Diseases and Restrictive Respiratory Failure The diffuse interstitial lung diseases are a diverse group of lung disorders that produce similar inflammatory and fibrotic changes in the interstitium or interalveolar septa of the lung. Restrictive Lung Diseases: ◦ Reduced lung compliance ◦ More pressure needed to expand lungs ◦ Lungs are stiff
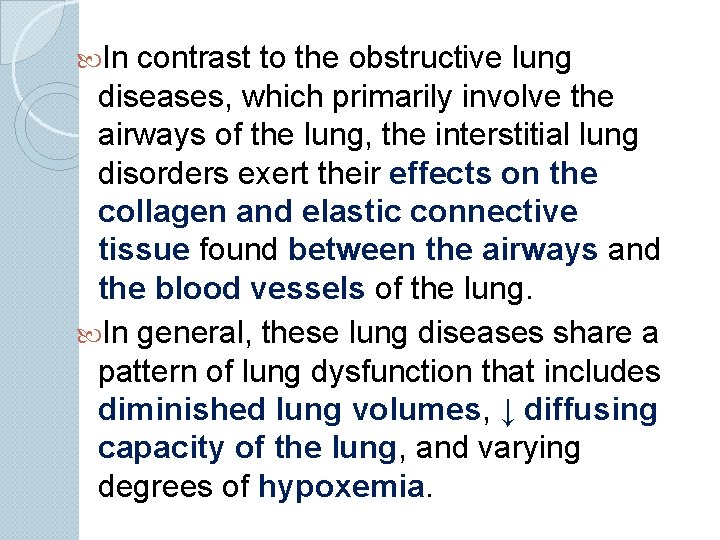
In contrast to the obstructive lung diseases, which primarily involve the airways of the lung, the interstitial lung disorders exert their effects on the collagen and elastic connective tissue found between the airways and the blood vessels of the lung. In general, these lung diseases share a pattern of lung dysfunction that includes diminished lung volumes, ↓ diffusing capacity of the lung, and varying degrees of hypoxemia.
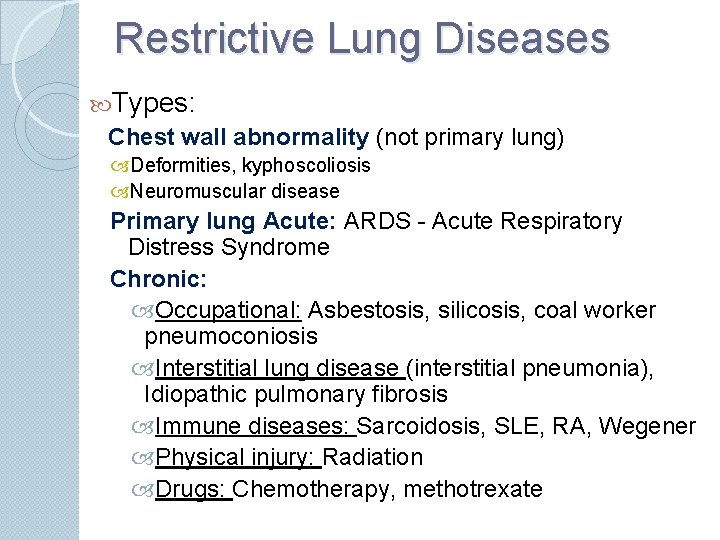
Restrictive Lung Diseases Types: Chest wall abnormality (not primary lung) Deformities, kyphoscoliosis Neuromuscular disease Primary lung Acute: ARDS - Acute Respiratory Distress Syndrome Chronic: Occupational: Asbestosis, silicosis, coal worker pneumoconiosis Interstitial lung disease (interstitial pneumonia), Idiopathic pulmonary fibrosis Immune diseases: Sarcoidosis, SLE, RA, Wegener Physical injury: Radiation Drugs: Chemotherapy, methotrexate
Restrictive Lung Diseases Gas exchange barrier: Ø Ø Basement membrane Interstitial tissue Endothelial cell Epithelial cell
Restrictive Lung Diseases Initial injury to cells: endothelial, epithelial This is followed by reaction that end by interstitial fibrosis – stiff lung – dyspnea Damage to epithelium and vessels – abnormal ventilation-perfusion – Hypoxia – cyanosis Pulmonary hypertension – cor pulmonale
Acute Lung Injury – Acute Respiratory Distress Syndrome ARDS
ARDS Can be caused by many conditions: 1. Direct injury to lung: Pneumonia, aspiration, pulmonary contusion (trauma), fat embolism, near-drowning, inhalation injury, post-lung transplant 2. Indirect Lung injury: Sepsis, severe trauma with shock, cadiopulmonary bypass, acute pancreatitis, transfusion, uremia
ARDS: pathogenesis ◦ Epithelial or endothelial injury ◦ Inflammation: increased vascular permeability, edema, fluid in alveoli, loss of diffusion capacity, loss of surfactant, damage of type II pneumocytes ◦ Proinflammatory cytokines>> Anti-inflammatory cytokines ◦ Cytokines: IL-8: Chemotaxis of neutrophils IL-1, TNF ◦ Neutrophils: Oxidative damage Attract other inflmmatory cells Fibrosis/Repair: transforming growth factor (TGF)alpha, platelet-derived growth factor (PDGF)
ARDS: morphology Diffuse alveolar damage Exudative phase (0 -7 days) Lung is dark, red, firm: capillary congestion Necrosis of epithelial cells; interstitial, alveolar edema, Collection of neutrophils Alveolar collapse (loss of surfactant) Hyaline membrane lining alveolar ducts Proliferative phase (1 -3 weeks) Proliferation of type II pneumocytes Macrophages, removing cell debris Fibrotic phase Resolution with minimal fibrosis Repair/Fibrosis, thick alveolar walls Progressive fibrosis (honeycomb lung) Rare
ARDS Clinical: ◦ ◦ ◦ Mortality was 100% Now 30 -40% with good ICU support Poor prognosis: old age, multisystem failure Characterized by progressive respiratory failure: ◦ ◦ Acute onset dyspnea Decreased arterial oxygen pressure (hypoxemia) Bilateral pulmonary infiltrates (edema) Absence of evidence of left-sided heart failure Most common cause of non-cardiogenic pulmonary edema

Chronic Restrictive Lung Diseases
Chronic Restrictive Lung Diseases Group of different diseases Similar clinical, pulmonary function test and pathological findings Represent 15% of non-infectious diseases of lungs End-stage: diffuse interstitial pulmonary fibrosis (Honeycomb lung)
Idiopathic Pulmonary Fibrosis Cryptogenic fibrosing alveolitis ◦ Unknown etiology ◦ Diffuse interstitial fibrosis ◦ Sever hypoxemia, and cyanosis ◦ Male>Female, 60 y ◦ Diagnosis of exclusion
Idiopathic Pulmonary Fibrosis Pathogenesis: ◦ Alveolar wall injury ◦ Alveolitis: inflammation, edema ◦ Neutrophil, macrophages, lymphocytes ◦ Interstitial Fibrosis ◦ ? Immune disorder: association with immune diseases: RA, SLE, Sjogren…. ◦ Macrophages: IL-8, FGF, TGF-beta, PDGF
Idiopathic Pulmonary Fibrosis Clinical: ◦ Gradual, non-productive cough ◦ Progressive Dyspnea, cyanosis ◦ Finger clubbing ◦ Mean survival 2 -4 years
Sarcoidosis Multisystem disease Unknown etiology Non-caseating granuloma in many tissues and organs Diagnosis of exclusion
Sarcoidosis Presenting Picture: ◦ Bilateral hilar lymphadenopathy ◦ Lung involvement, lung nodules ◦ Other organs: skin, eye, any tissue ◦ Adult, younger than <40 y ◦ Common in US blacks ◦ Higher in non-smokers
Sarcoidosis Pathogenesis ◦ Unknown cause ◦ Immunologic factors Activated CD 4 T cells Increase number of CD 4 Tcells High level f IL-2, Interferon-gamma, IL-8, TNF ◦ Genetic factors: Familial, racial clustering Association with HLA-A 1, HLA-B 8 ◦ Environmental factors ? Viral infection
Sarcoidosis Clinical: ◦ Asymptomatic in many ◦ Lymphadenopathy, skin, eye lesion ◦ Respiratory disease: dyspnea, dry cough ◦ Fever, fatigue, wt. loss ◦ Unpredictable course ◦ Progressive or relapsing remitting disease ◦ 10% develop progressive fibrosis

Hypersensitivity Pneumonitis Immune mediated disease Type III and type IV hypersensitivity Inflammatory disease Affect alveoli (mainly) (Allergic Alveolitis) Occupational disease Restrictive disease
Wegener Granulomatosis Necrotizing vasculitis Affect both upper and lower respiratory tract Parenchymal necrotizing granuloma URT: sinusitis, epistaxis, nasal perforation LRT: cough, hemoptysis, chest pain
Pneumonia
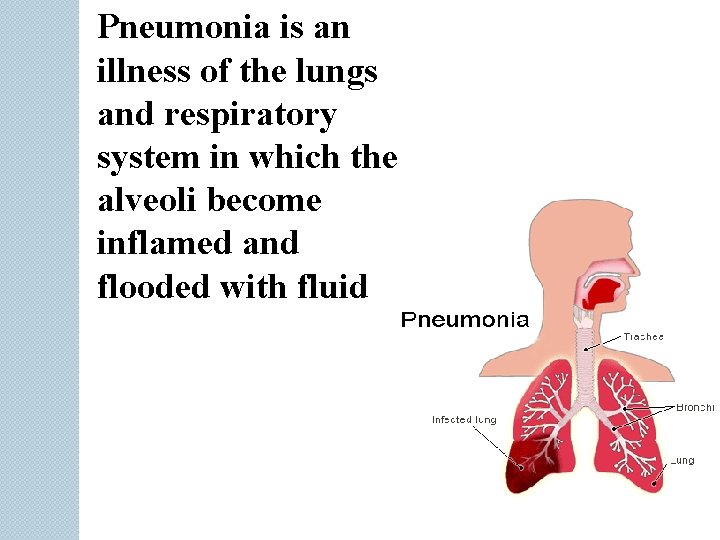
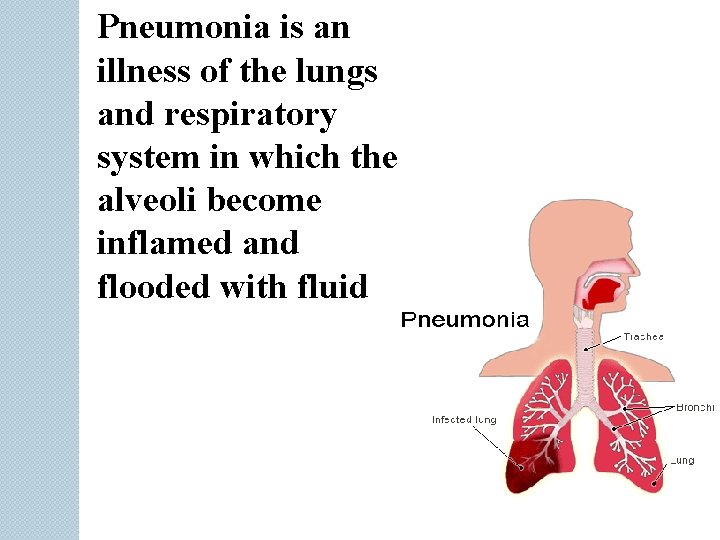
Pneumonia is an illness of the lungs and respiratory system in which the alveoli become inflamed and flooded with fluid
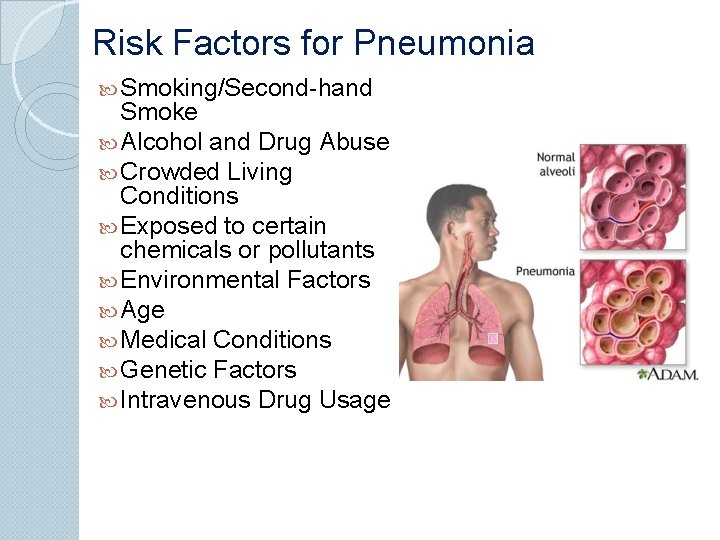
Risk Factors for Pneumonia Smoking/Second-hand Smoke Alcohol and Drug Abuse Crowded Living Conditions Exposed to certain chemicals or pollutants Environmental Factors Age Medical Conditions Genetic Factors Intravenous Drug Usage
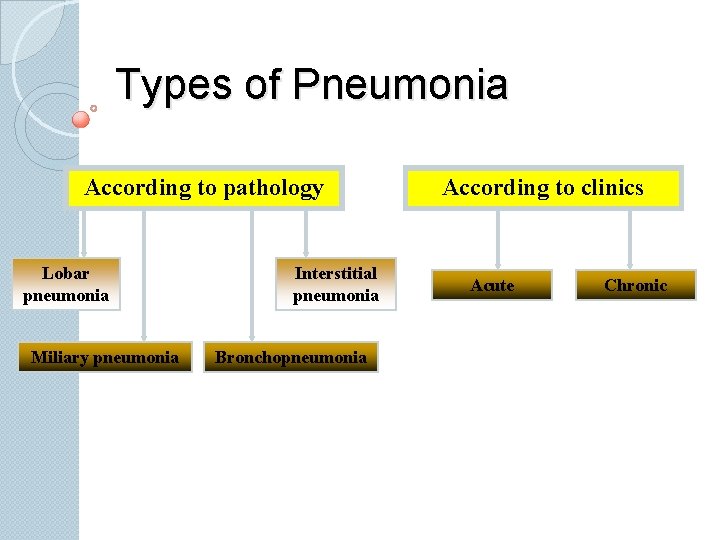
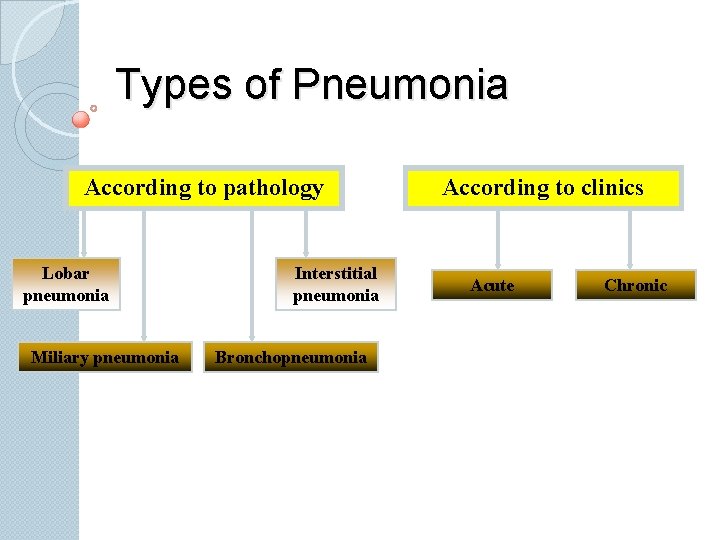
Types of Pneumonia According to pathology Lobar pneumonia Miliary pneumonia Interstitial pneumonia Bronchopneumonia According to clinics Acute Chronic
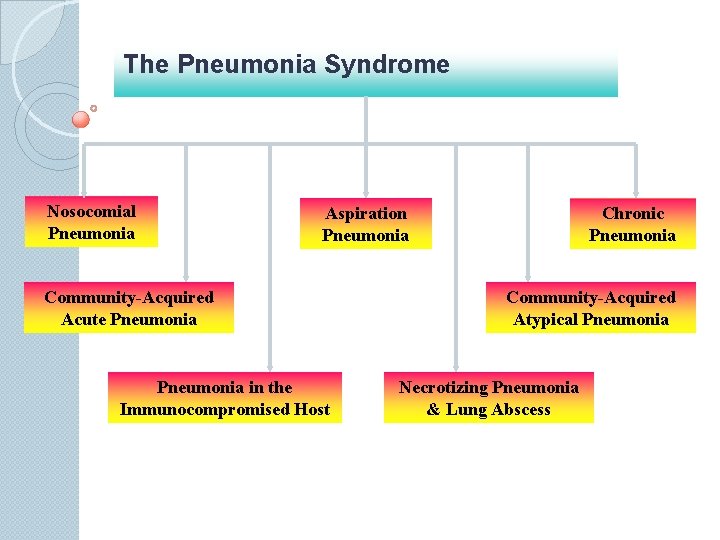
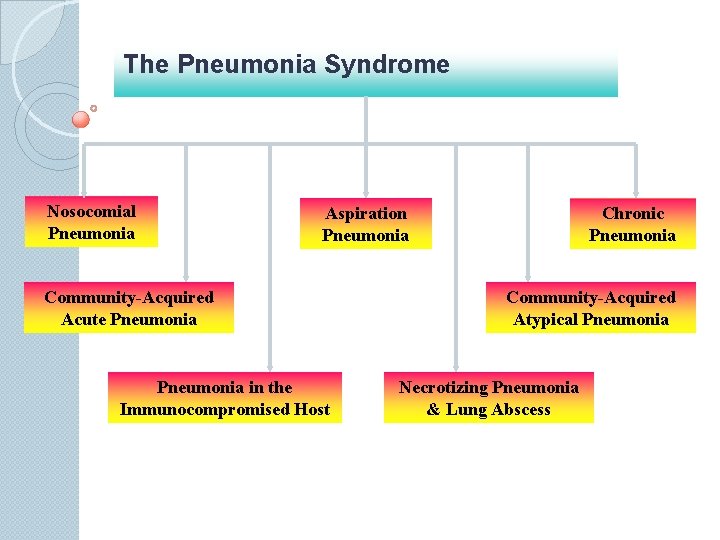
The Pneumonia Syndrome Nosocomial Pneumonia Aspiration Pneumonia Community-Acquired Acute Pneumonia in the Immunocompromised Host Chronic Pneumonia Community-Acquired Atypical Pneumonia Necrotizing Pneumonia & Lung Abscess

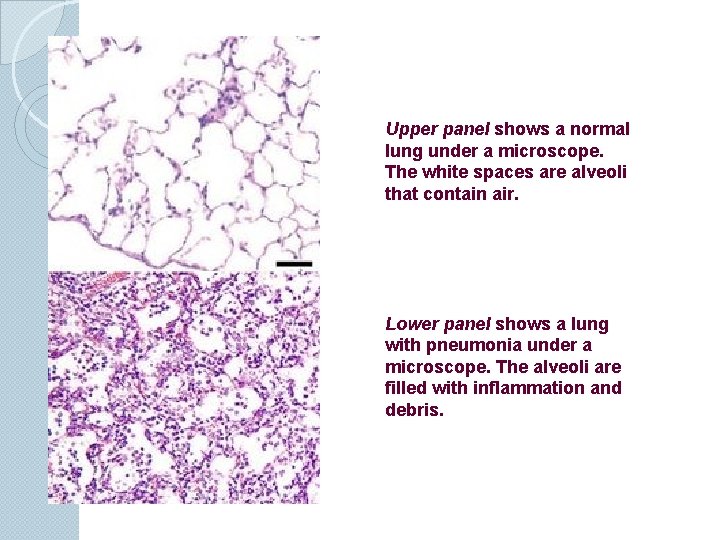
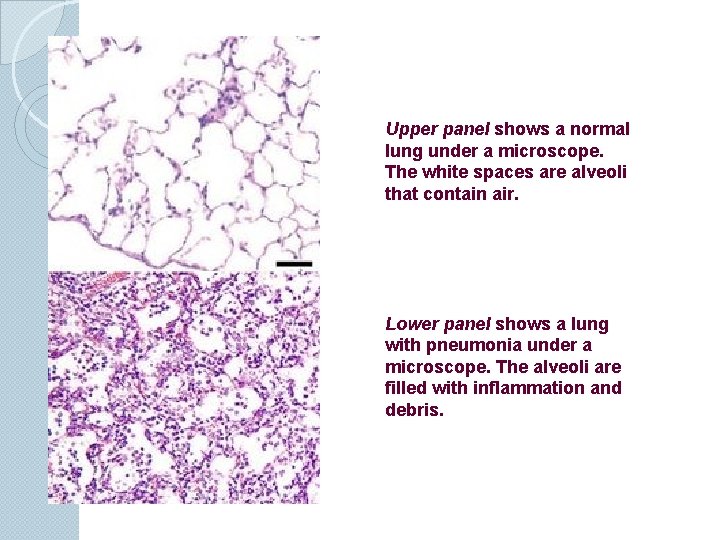
Upper panel shows a normal lung under a microscope. The white spaces are alveoli that contain air. Lower panel shows a lung with pneumonia under a microscope. The alveoli are filled with inflammation and debris.
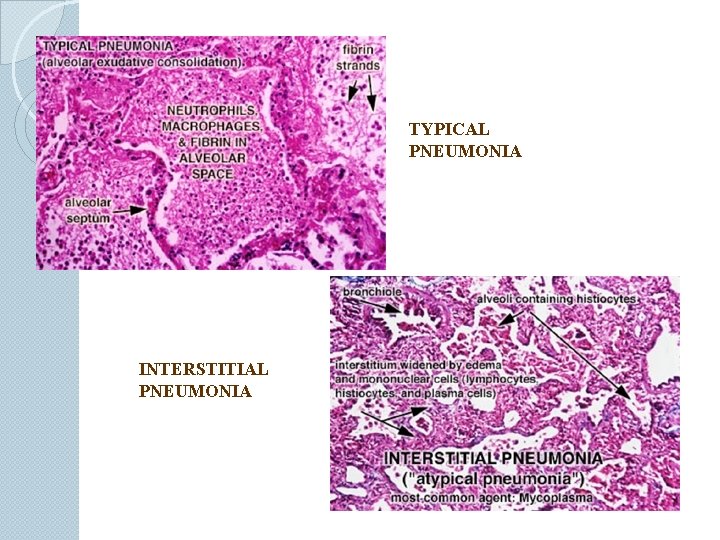
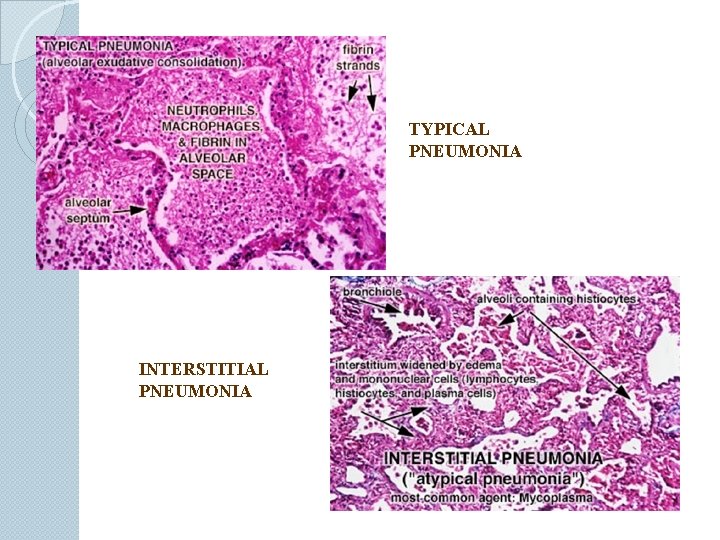
TYPICAL PNEUMONIA INTERSTITIAL PNEUMONIA
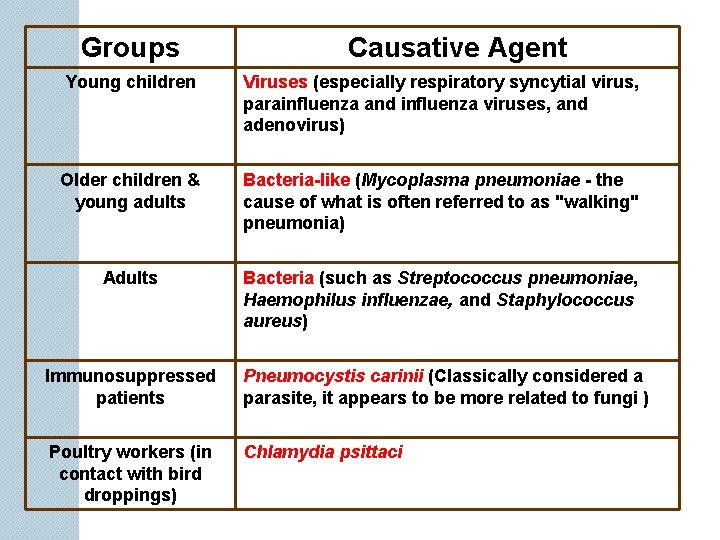
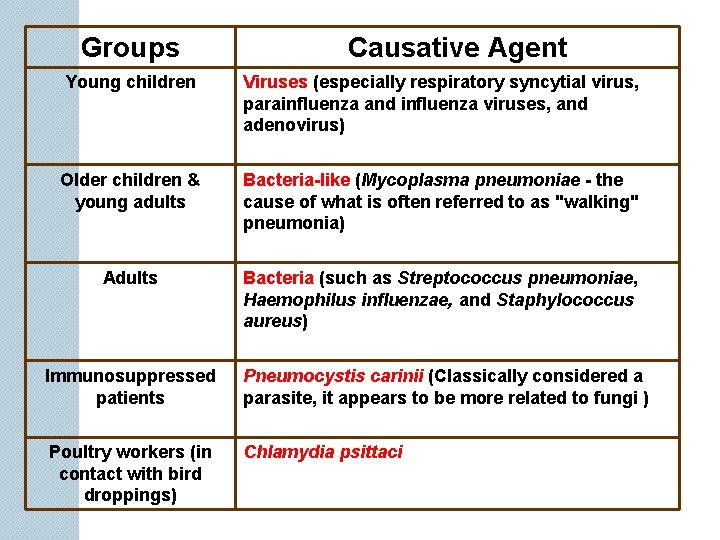
Groups Causative Agent Young children Viruses (especially respiratory syncytial virus, parainfluenza and influenza viruses, and adenovirus) Older children & young adults Bacteria-like (Mycoplasma pneumoniae - the cause of what is often referred to as "walking" pneumonia) Adults Bacteria (such as Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus) Immunosuppressed patients Pneumocystis carinii (Classically considered a parasite, it appears to be more related to fungi ) Poultry workers (in contact with bird droppings) Chlamydia psittaci
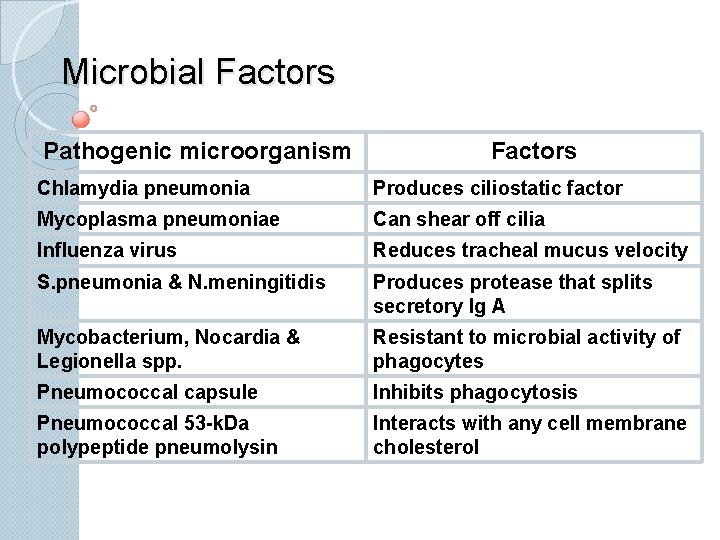
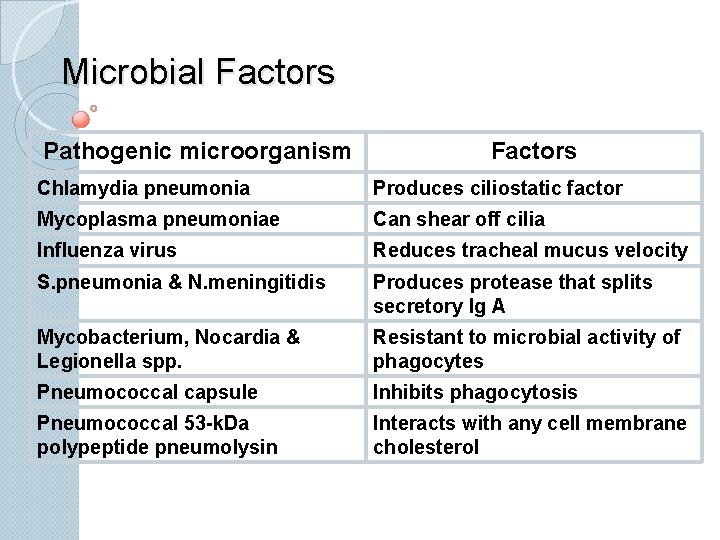
Microbial Factors Pathogenic microorganism Factors Chlamydia pneumonia Produces ciliostatic factor Mycoplasma pneumoniae Can shear off cilia Influenza virus Reduces tracheal mucus velocity S. pneumonia & N. meningitidis Produces protease that splits secretory Ig A Mycobacterium, Nocardia & Legionella spp. Resistant to microbial activity of phagocytes Pneumococcal capsule Inhibits phagocytosis Pneumococcal 53 -k. Da polypeptide pneumolysin Interacts with any cell membrane cholesterol
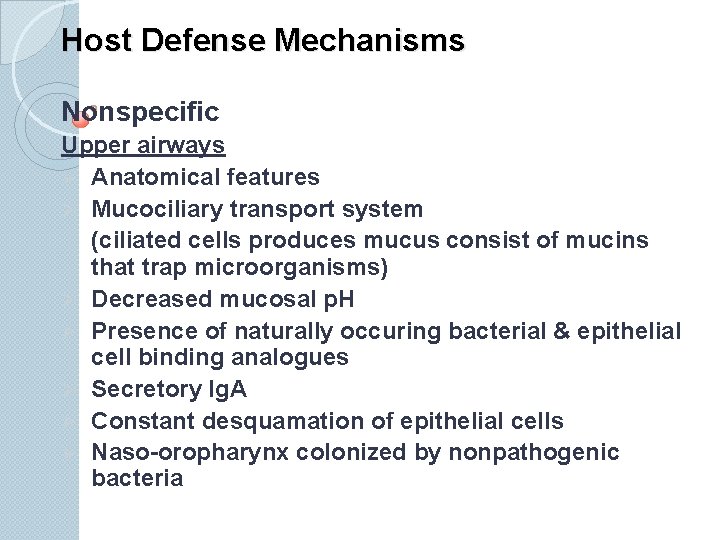
Host Defense Mechanisms Nonspecific Upper airways Ø Anatomical features Ø Mucociliary transport system (ciliated cells produces mucus consist of mucins that trap microorganisms) Ø Decreased mucosal p. H Ø Presence of naturally occuring bacterial & epithelial cell binding analogues Ø Secretory Ig. A Ø Constant desquamation of epithelial cells Ø Naso-oropharynx colonized by nonpathogenic bacteria
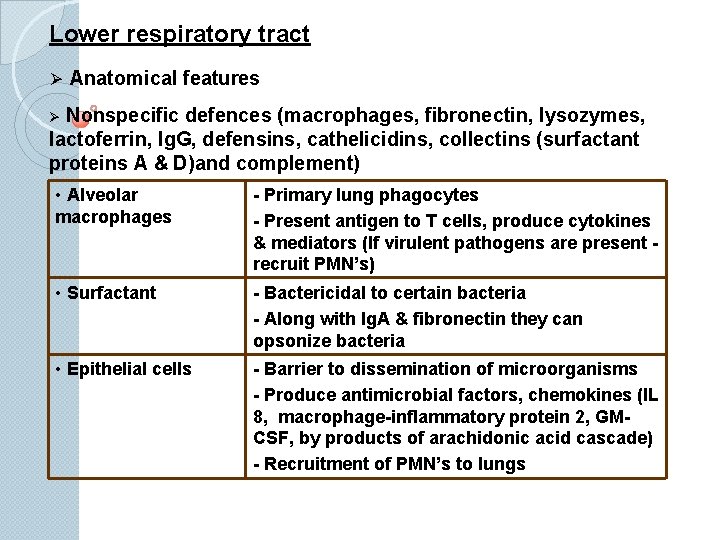
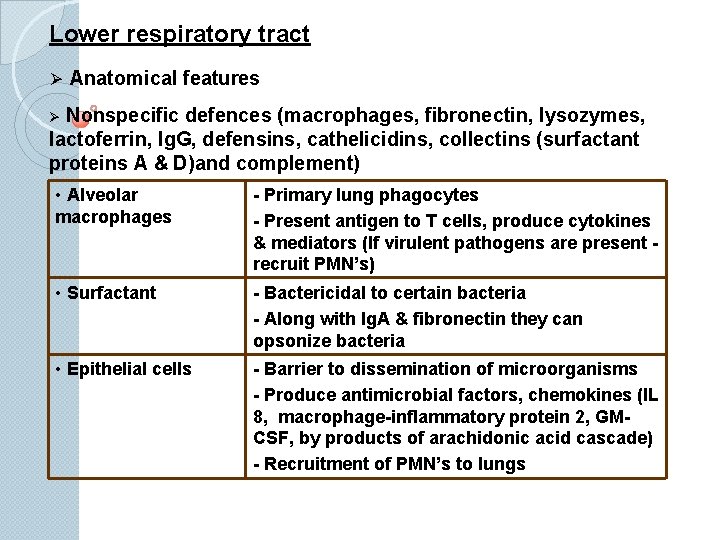
Lower respiratory tract Ø Anatomical features Nonspecific defences (macrophages, fibronectin, lysozymes, lactoferrin, Ig. G, defensins, cathelicidins, collectins (surfactant proteins A & D)and complement) Ø • Alveolar macrophages - Primary lung phagocytes - Present antigen to T cells, produce cytokines & mediators (If virulent pathogens are present recruit PMN’s) • Surfactant - Bactericidal to certain bacteria - Along with Ig. A & fibronectin they can opsonize bacteria • Epithelial cells - Barrier to dissemination of microorganisms - Produce antimicrobial factors, chemokines (IL 8, macrophage-inflammatory protein 2, GMCSF, by products of arachidonic acid cascade) - Recruitment of PMN’s to lungs
How can the pulmonary defense mechanisms be impaired ? v Loss or suppression of the cough reflex v Injury to the mucociliary apparatus v Interference with the phagocytic or bactericidal action of alveolar macrophages v Pulmonary congestion & edema v Accumulation of secretions in conditions such as cystic fibrosis & bronchial obstruction
v Hypogammaglobulinemia v Defects in phagocytosis or ciliary function v Neutropenia v Functional or anatomical asplenia v Reduction in CD 4+ T lymphocyte counts v Viral infection of alveolar macrophages v Anatomical defects such as obstructed bronchus, bronchiectasis, or sequestration of a pulmonary segment all lead to recurrent pneumonia. v Polymorphisms in or near TNF-alpha gene causes variability in TNF-alpha production and with outcomes in pneumonia.
Pathophysiology of pneumonia has 2 main components. . . v cellular v exudative
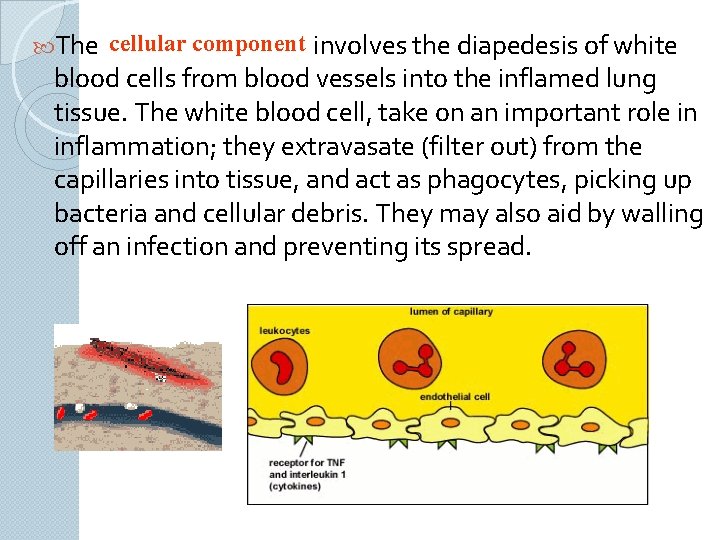
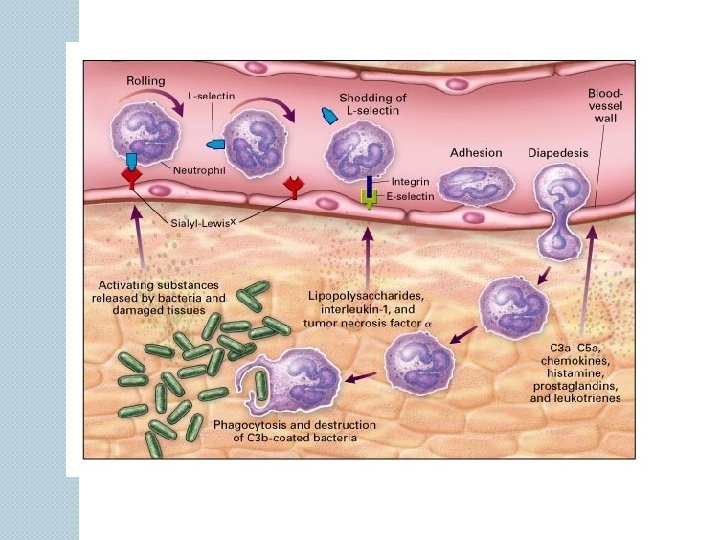
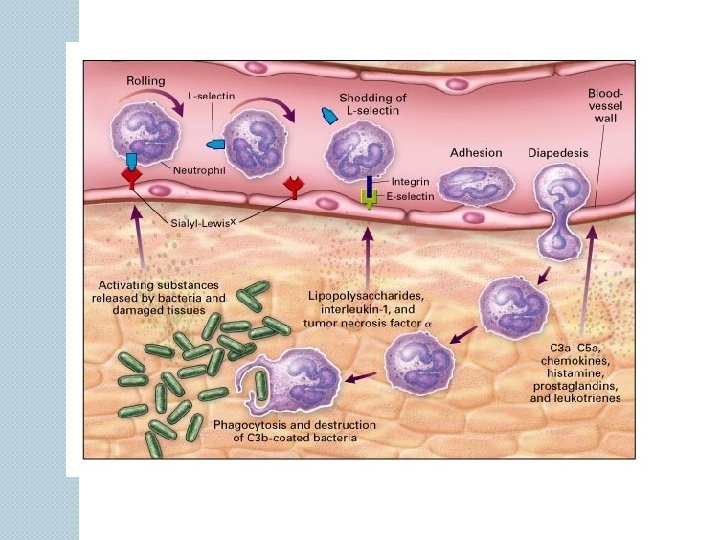
The cellular component involves the diapedesis of white blood cells from blood vessels into the inflamed lung tissue. The white blood cell, take on an important role in inflammation; they extravasate (filter out) from the capillaries into tissue, and act as phagocytes, picking up bacteria and cellular debris. They may also aid by walling off an infection and preventing its spread.
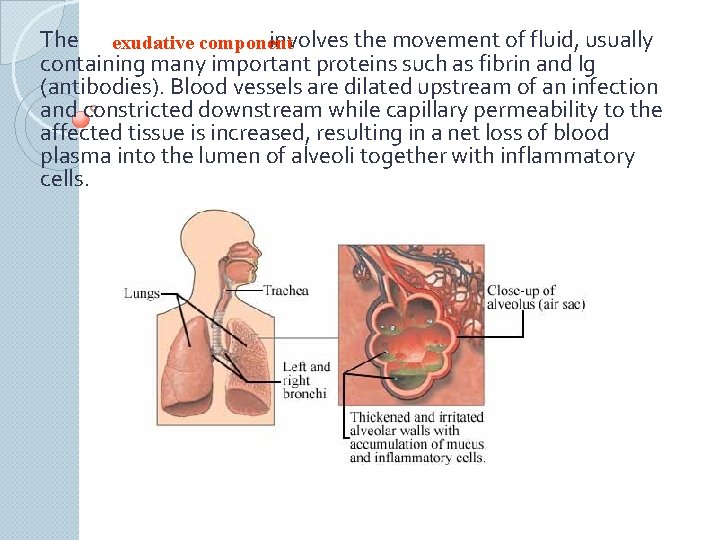
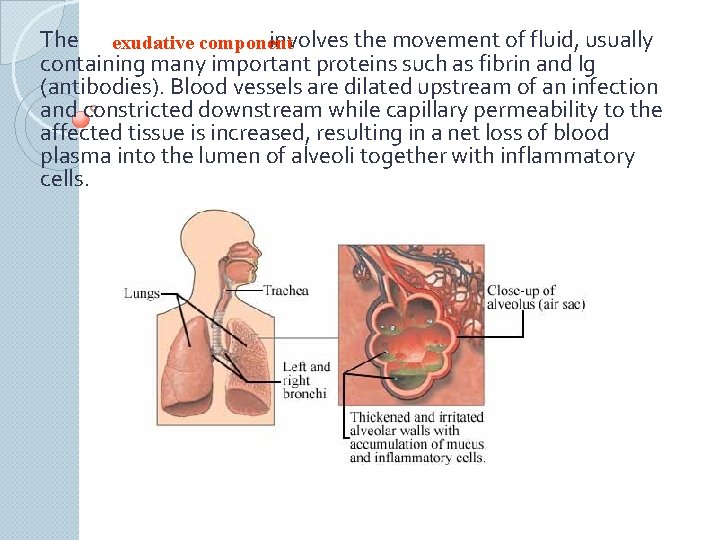
The exudative component involves the movement of fluid, usually containing many important proteins such as fibrin and Ig (antibodies). Blood vessels are dilated upstream of an infection and constricted downstream while capillary permeability to the affected tissue is increased, resulting in a net loss of blood plasma into the lumen of alveoli together with inflammatory cells.
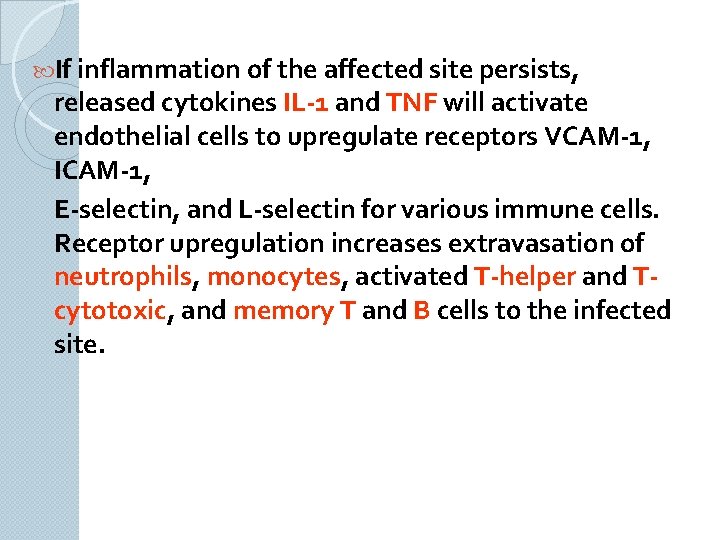
If inflammation of the affected site persists, released cytokines IL-1 and TNF will activate endothelial cells to upregulate receptors VCAM-1, ICAM-1, E-selectin, and L-selectin for various immune cells. Receptor upregulation increases extravasation of neutrophils, monocytes, activated T-helper and Tcytotoxic, and memory T and B cells to the infected site.
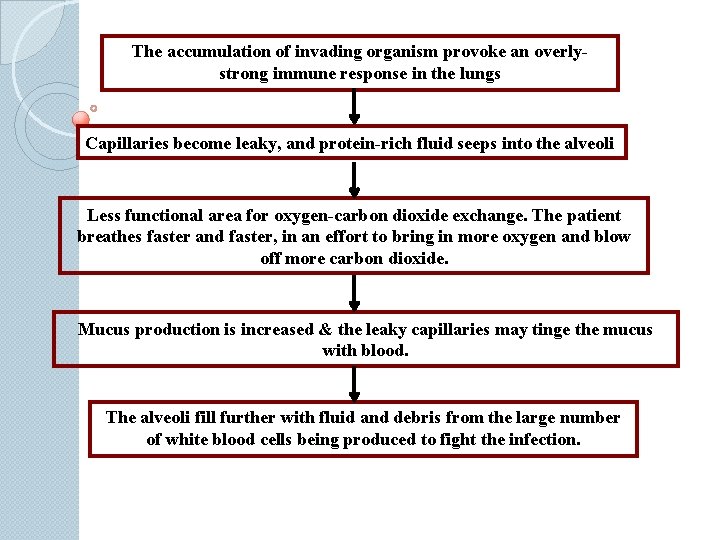
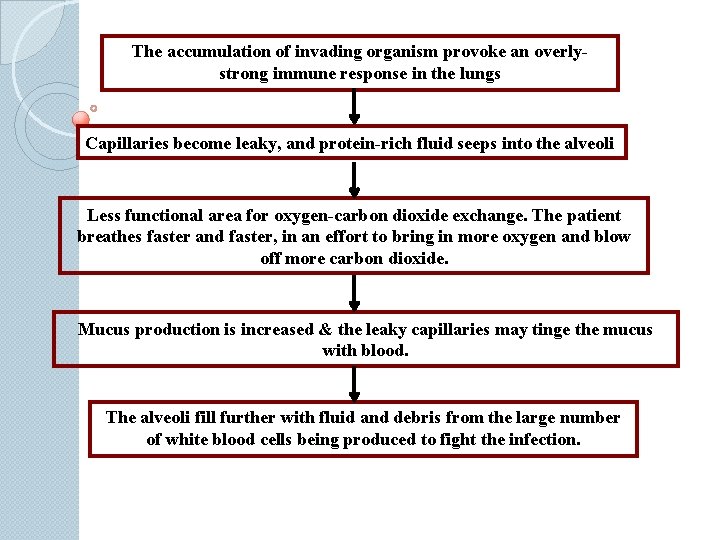
The accumulation of invading organism provoke an overlystrong immune response in the lungs Capillaries become leaky, and protein-rich fluid seeps into the alveoli Less functional area for oxygen-carbon dioxide exchange. The patient breathes faster and faster, in an effort to bring in more oxygen and blow off more carbon dioxide. Mucus production is increased & the leaky capillaries may tinge the mucus with blood. The alveoli fill further with fluid and debris from the large number of white blood cells being produced to fight the infection.

Acute respiratory distress syndrome (ARDS) is a devastating syndrome of acute lung injury. The disorder is the final common pathway through which many serious localized and systemic disorders produce diffuse injury to the alveolarcapillary membrane.
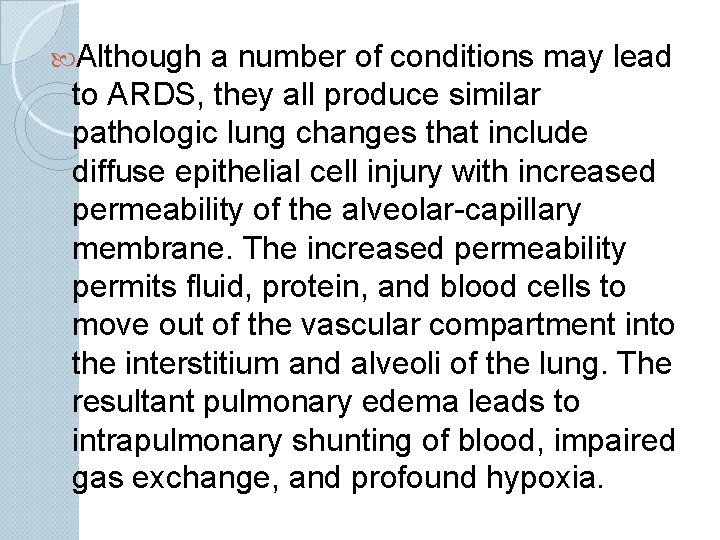
Although a number of conditions may lead to ARDS, they all produce similar pathologic lung changes that include diffuse epithelial cell injury with increased permeability of the alveolar-capillary membrane. The increased permeability permits fluid, protein, and blood cells to move out of the vascular compartment into the interstitium and alveoli of the lung. The resultant pulmonary edema leads to intrapulmonary shunting of blood, impaired gas exchange, and profound hypoxia.
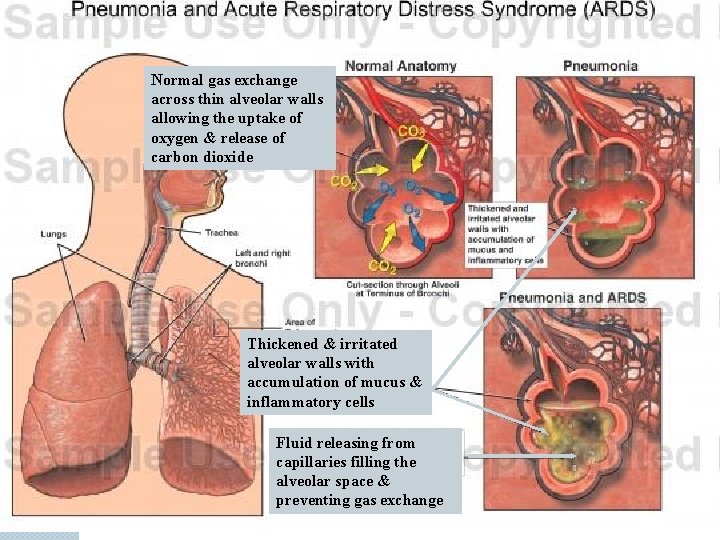
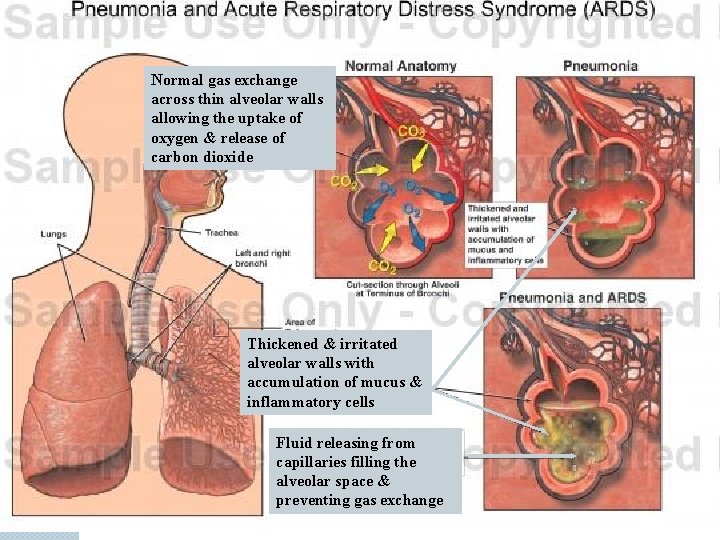
Normal gas exchange across thin alveolar walls allowing the uptake of oxygen & release of carbon dioxide Thickened & irritated alveolar walls with accumulation of mucus & inflammatory cells Fluid releasing from capillaries filling the alveolar space & preventing gas exchange
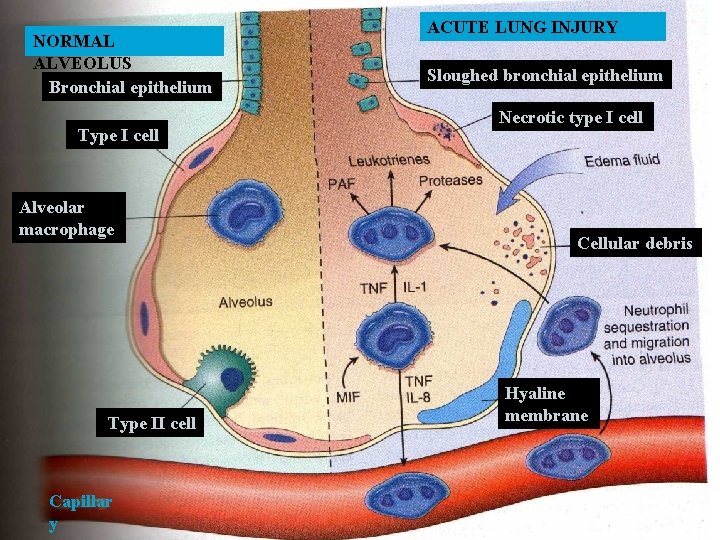
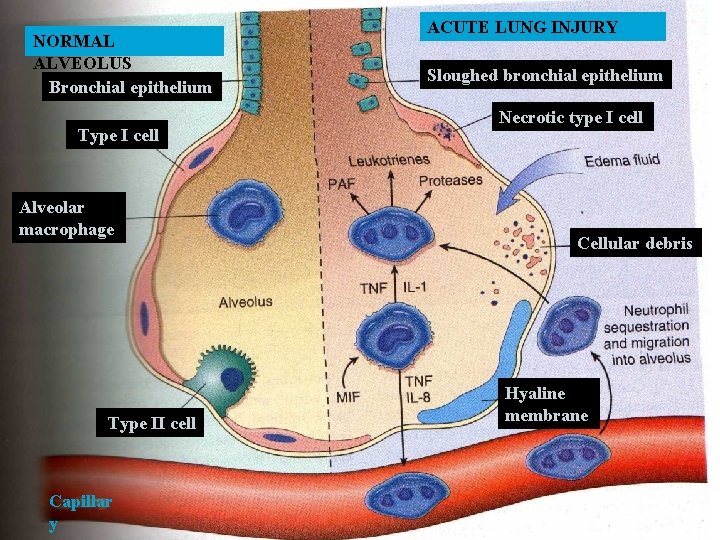
NORMAL ALVEOLUS Bronchial epithelium Type I cell Alveolar macrophage Type II cell Capillar y ACUTE LUNG INJURY Sloughed bronchial epithelium Necrotic type I cell Cellular debris Hyaline membrane
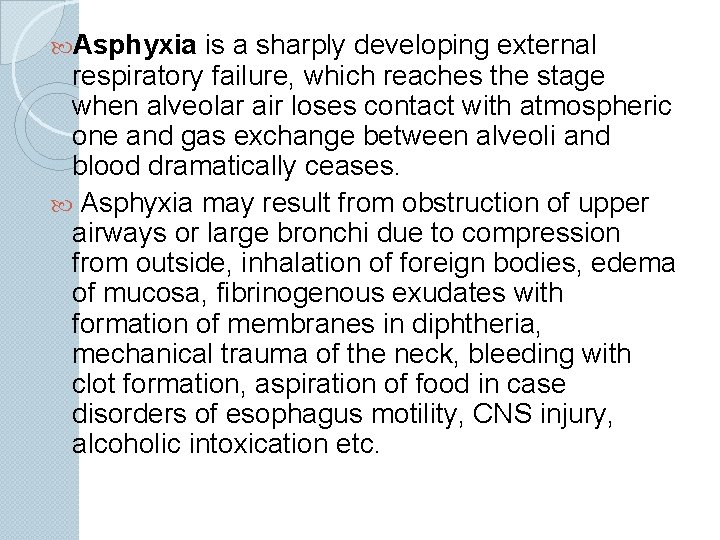
Asphyxia is a sharply developing external respiratory failure, which reaches the stage when alveolar air loses contact with atmospheric one and gas exchange between alveoli and blood dramatically ceases. Asphyxia may result from obstruction of upper airways or large bronchi due to compression from outside, inhalation of foreign bodies, edema of mucosa, fibrinogenous exudates with formation of membranes in diphtheria, mechanical trauma of the neck, bleeding with clot formation, aspiration of food in case disorders of esophagus motility, CNS injury, alcoholic intoxication etc.
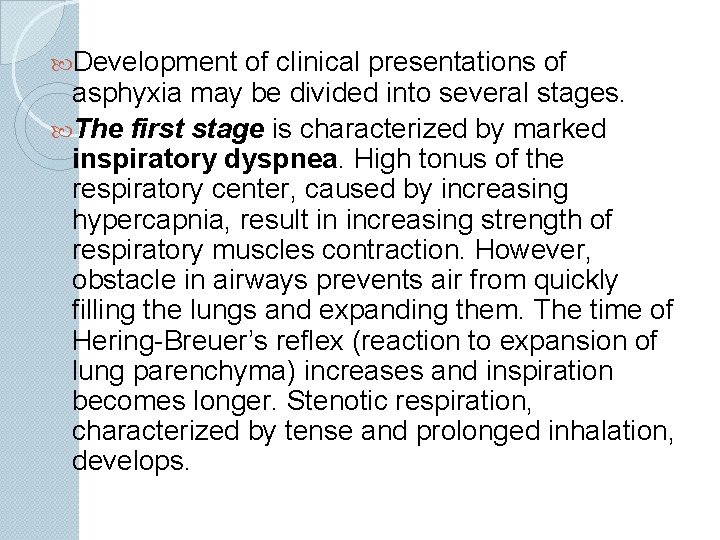
Development of clinical presentations of asphyxia may be divided into several stages. The first stage is characterized by marked inspiratory dyspnea. High tonus of the respiratory center, caused by increasing hypercapnia, result in increasing strength of respiratory muscles contraction. However, obstacle in airways prevents air from quickly filling the lungs and expanding them. The time of Hering-Breuer’s reflex (reaction to expansion of lung parenchyma) increases and inspiration becomes longer. Stenotic respiration, characterized by tense and prolonged inhalation, develops.
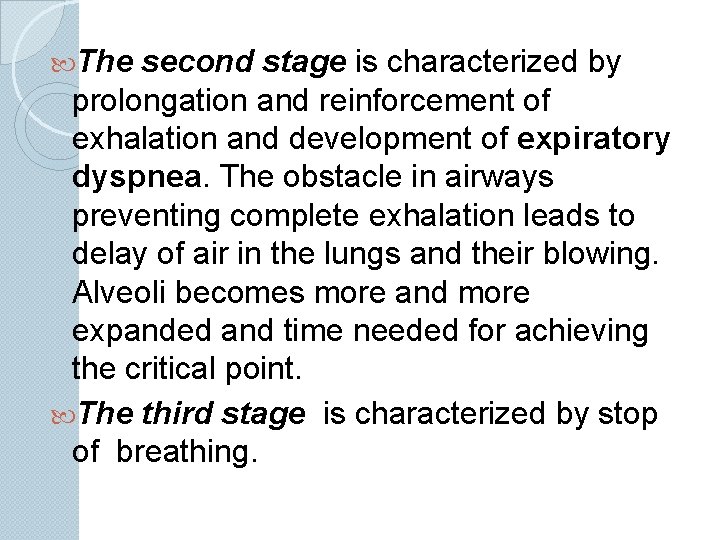
The second stage is characterized by prolongation and reinforcement of exhalation and development of expiratory dyspnea. The obstacle in airways preventing complete exhalation leads to delay of air in the lungs and their blowing. Alveoli becomes more and more expanded and time needed for achieving the critical point. The third stage is characterized by stop of breathing.
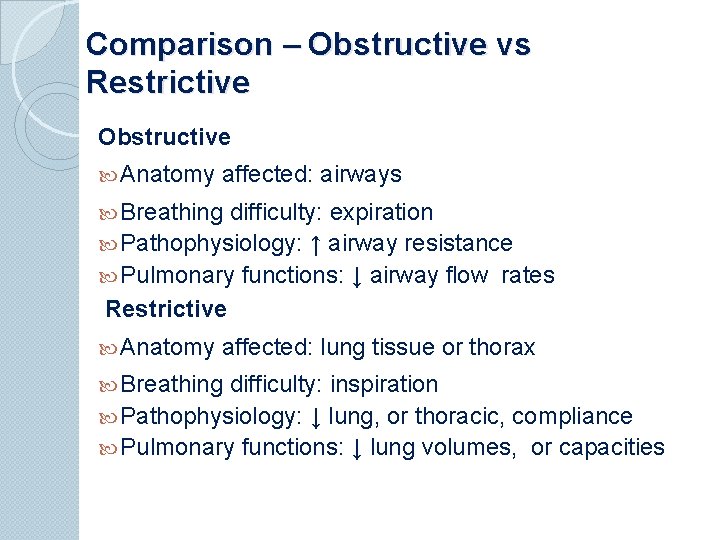
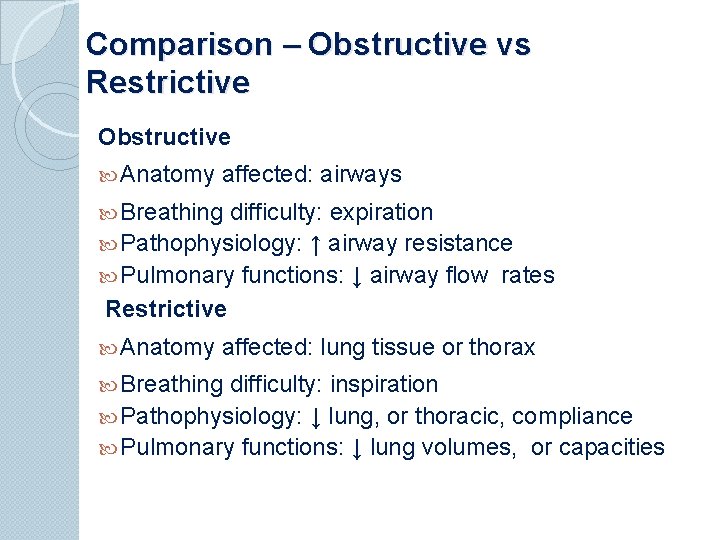
Comparison – Obstructive vs Restrictive Obstructive Anatomy affected: airways Breathing difficulty: expiration Pathophysiology: ↑ airway resistance Pulmonary functions: ↓ airway flow rates Restrictive Anatomy affected: lung tissue or thorax Breathing difficulty: inspiration Pathophysiology: ↓ lung, or thoracic, compliance Pulmonary functions: ↓ lung volumes, or capacities
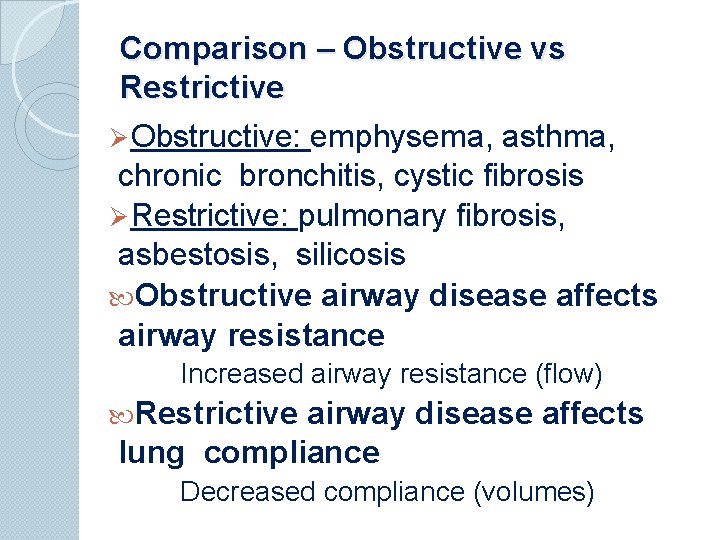
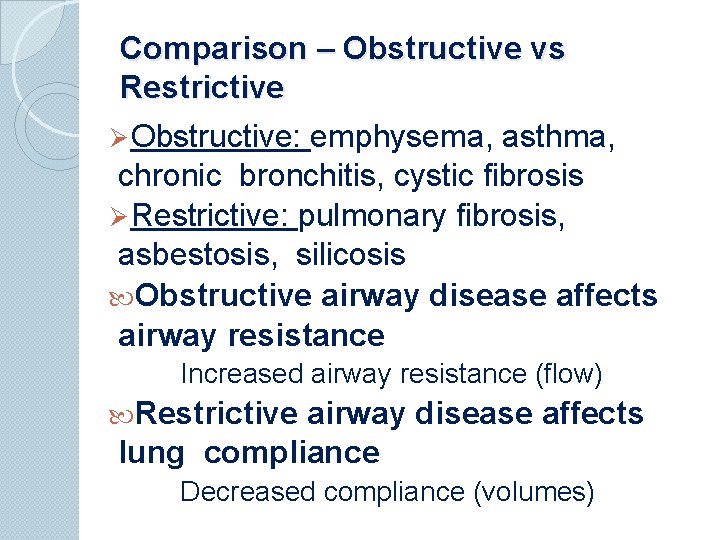
Comparison – Obstructive vs Restrictive Ø Obstructive: emphysema, asthma, chronic bronchitis, cystic fibrosis Ø Restrictive: pulmonary fibrosis, asbestosis, silicosis Obstructive airway disease affects airway resistance Increased airway resistance (flow) Restrictive airway disease affects lung compliance Decreased compliance (volumes)
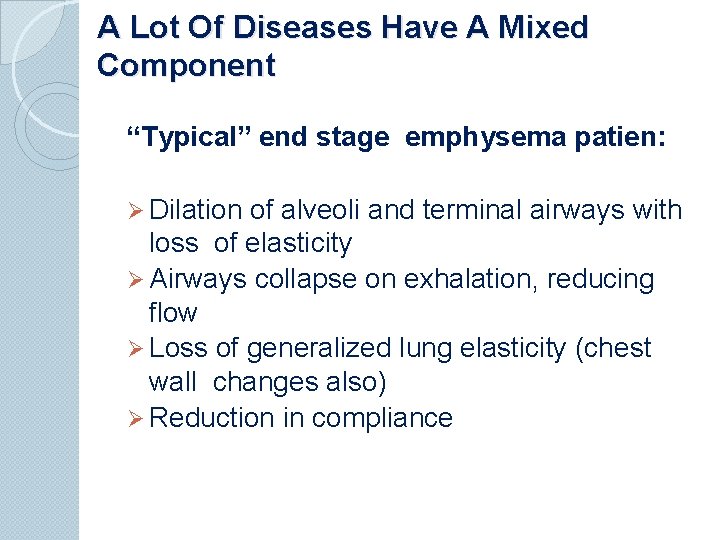
A Lot Of Diseases Have A Mixed Component “Typical” end stage emphysema patien: Ø Dilation of alveoli and terminal airways with loss of elasticity Ø Airways collapse on exhalation, reducing flow Ø Loss of generalized lung elasticity (chest wall changes also) Ø Reduction in compliance
 External respiration
External respiration The nose serves all the following functions except
The nose serves all the following functions except Total set awareness set consideration set
Total set awareness set consideration set Training set validation set test set
Training set validation set test set External respiration
External respiration Meaning of cellular respiration
Meaning of cellular respiration Internal vs external respiration
Internal vs external respiration External vs internal respiration
External vs internal respiration Nasal flaring
Nasal flaring Labled
Labled Mechanism of breathing
Mechanism of breathing Internal vs external respiration
Internal vs external respiration Cellular respiration reactants
Cellular respiration reactants Internal respiration
Internal respiration External respiration steps
External respiration steps Differentiate between external and internal respiration
Differentiate between external and internal respiration Classification of respiration
Classification of respiration Internal respiration
Internal respiration External-external trips
External-external trips Bounded set vs centered set
Bounded set vs centered set What is the overlap of data set 1 and data set 2?
What is the overlap of data set 1 and data set 2? Fuzzy logic
Fuzzy logic The function from set a to set b is
The function from set a to set b is Crisp set vs fuzzy set
Crisp set vs fuzzy set Crisp set vs fuzzy set
Crisp set vs fuzzy set Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pathophysiology ankylosing spondylitis
Pathophysiology ankylosing spondylitis Intestinal obstruction pathophysiology
Intestinal obstruction pathophysiology Nursing interventions for thyroid storm
Nursing interventions for thyroid storm Patent ductus arteriosus pathophysiology
Patent ductus arteriosus pathophysiology Dumping syndrome pathophysiology
Dumping syndrome pathophysiology Otosclerosis pathophysiology ppt
Otosclerosis pathophysiology ppt Preductal vs postductal
Preductal vs postductal Renal vein thrombosis pathophysiology
Renal vein thrombosis pathophysiology 4th stage renal failure
4th stage renal failure Chickenpox pathophysiology
Chickenpox pathophysiology Methimazole dosing guidelines
Methimazole dosing guidelines Zuzana 6357
Zuzana 6357 X ray of asthma patient
X ray of asthma patient Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Hypothyriodism
Hypothyriodism Mixoedema
Mixoedema Pathophysiology of cirrhosis of liver
Pathophysiology of cirrhosis of liver Pathophysiology of anemia diagram
Pathophysiology of anemia diagram Pathophysiology signs and symptoms
Pathophysiology signs and symptoms Vagal maneuvers
Vagal maneuvers What is pathophysiology
What is pathophysiology Pancreatitis film
Pancreatitis film Excecerbate
Excecerbate Neurogenic shock pathophysiology
Neurogenic shock pathophysiology Pathophysiology of appendicitis
Pathophysiology of appendicitis Homocystinuria pathophysiology
Homocystinuria pathophysiology Disseminated intravascular coagulation pathophysiology
Disseminated intravascular coagulation pathophysiology Lund browder chart adults
Lund browder chart adults Why “avoid chocolate” after nissen fundoplication
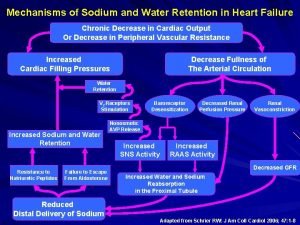
Why “avoid chocolate” after nissen fundoplication Pathophysiology of sodium and water retention
Pathophysiology of sodium and water retention Burn injury pathophysiology of burns
Burn injury pathophysiology of burns Lymphocytosis
Lymphocytosis Pathophysiology of tuberculosis flow chart
Pathophysiology of tuberculosis flow chart Thyroglossal cyst pathophysiology
Thyroglossal cyst pathophysiology Mitral regurgitation symptoms
Mitral regurgitation symptoms Woodruffs plexus
Woodruffs plexus Di vs siadh
Di vs siadh Hypertensive emergency definition
Hypertensive emergency definition Stages of appendicitis
Stages of appendicitis Otosclerosis nursing management
Otosclerosis nursing management Diarrhea plan a
Diarrhea plan a Status asthmaticus pathophysiology
Status asthmaticus pathophysiology Examples of pathophysiology
Examples of pathophysiology Pathophysiology of hirschsprung disease
Pathophysiology of hirschsprung disease Pathophysiology of pulmonary hypertension
Pathophysiology of pulmonary hypertension Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Osteopern
Osteopern Pathophysiology of jaundice
Pathophysiology of jaundice Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Pain pathophysiology
Pain pathophysiology Sinusoids liver
Sinusoids liver Patent ductus arteriosus pathophysiology
Patent ductus arteriosus pathophysiology Rds pathophysiology
Rds pathophysiology Pathophysiology of aplastic anemia
Pathophysiology of aplastic anemia Pathophysiology of thrombosis ppt
Pathophysiology of thrombosis ppt Jihan nezir
Jihan nezir Pathophysiology of asthm
Pathophysiology of asthm Pathophysiology of aortic aneurysm ppt
Pathophysiology of aortic aneurysm ppt Taxis maneuver hernia
Taxis maneuver hernia Morphology of peptic ulcer
Morphology of peptic ulcer Pinched and blue facies
Pinched and blue facies Pathophysiology of intestinal obstruction
Pathophysiology of intestinal obstruction Myxedema crisis treatment
Myxedema crisis treatment Site:slidetodoc.com
Site:slidetodoc.com Pathophysiology of tonsillitis
Pathophysiology of tonsillitis Case mysteries in pathophysiology (doc or html) file
Case mysteries in pathophysiology (doc or html) file Asthma pathophysiology
Asthma pathophysiology Reactive arthritis pathophysiology
Reactive arthritis pathophysiology Asthma pathophysiology
Asthma pathophysiology Egfr formula
Egfr formula Uterine bleeding
Uterine bleeding Cardiogenic shock
Cardiogenic shock Nursing management of chronic pancreatitis
Nursing management of chronic pancreatitis Hellp syndrome meaning
Hellp syndrome meaning Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pathophysiology of migraine
Pathophysiology of migraine Cholecystitis pathophysiology
Cholecystitis pathophysiology Hyperkalemia pathophysiology
Hyperkalemia pathophysiology Joffroys sign
Joffroys sign Peripheral sensitization
Peripheral sensitization Perinephric abscess symptoms
Perinephric abscess symptoms Denitrogenation atelectasis
Denitrogenation atelectasis Emphysema
Emphysema Prepartum haemorrhage
Prepartum haemorrhage Who is this
Who is this Acute dystonia pathophysiology
Acute dystonia pathophysiology Cholecystitis pathogenesis
Cholecystitis pathogenesis Pathophysiology of hemophilia ppt
Pathophysiology of hemophilia ppt Atopic dermatitis pathophysiology
Atopic dermatitis pathophysiology Multinodular goiter pathophysiology
Multinodular goiter pathophysiology Scarred gallbladder
Scarred gallbladder Tanda ruptur bulbi
Tanda ruptur bulbi Pathophysiology of angina
Pathophysiology of angina Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Type 1 diabetes pathophysiology
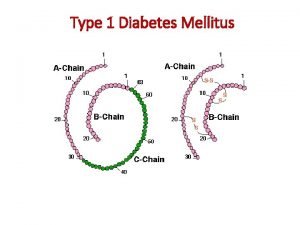
Type 1 diabetes pathophysiology Hepatic encephalopathy pathophysiology
Hepatic encephalopathy pathophysiology Asthma pathophysiology
Asthma pathophysiology Stages of pneumonia
Stages of pneumonia Pathophysiology of appendicitis
Pathophysiology of appendicitis