Respiratory Failure Respiration external respiration pulmonary ventilation and
- Slides: 40
Respiratory Failure
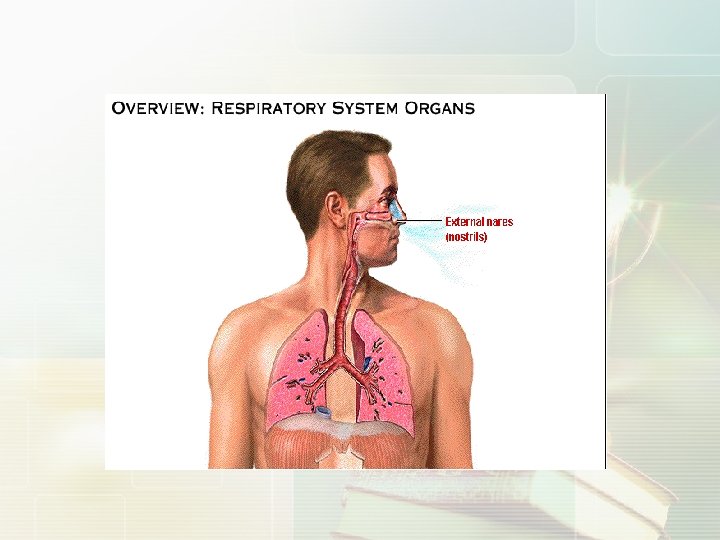
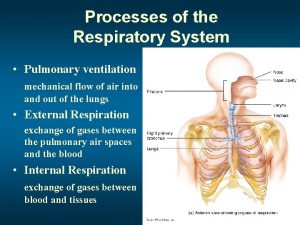
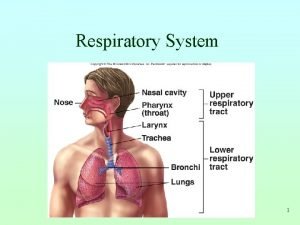
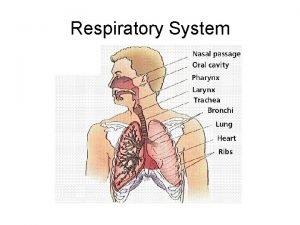
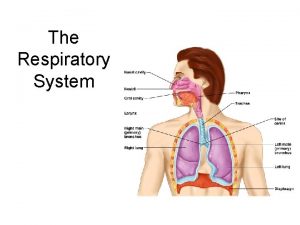
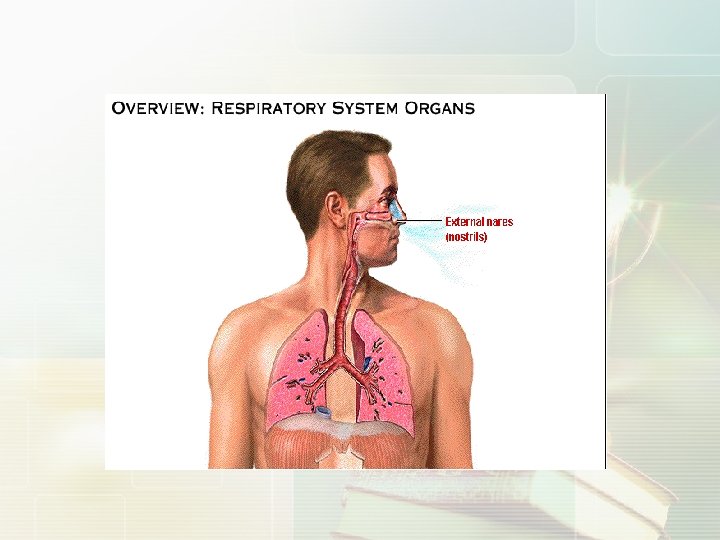
Respiration Ø external respiration( pulmonary ventilation and gas exchange in lung) Ø transport of gas Ø internal respiration
concept and classification
respiratory insufficienc The condition in which the lungs can not take in sufficient oxygen or expel sufficient carbon dioxide to meet the needs of the cells of the body. Also called pulmonary insufficiency.
respiratory failure Respiratory failure is a syndrome in which the respiratory system fails in one or both of its gas exchange functions: oxygenation and carbon dioxide elimination. In practice, respiratory failure is defined as a Pa. O 2 value of less than 60 mm Hg while breathing air or a Pa. CO 2 of more than 50 mm Hg.
respiratory failure normal reference values : Pa. O 2 < 60 mm. Hg(8 k. Pa) RFI =or. Pa. O without 2/Fi. OPa. CO 2 ≤ 300 2 > 50 mm. Hg(6. 67 k. Pa)
classification (1)according to Pa. CO 2 ■ hypoxemic (Group Ⅰ) respiratory failure a Pa. O 2 of less than 60 mm. Hg with a normal or low Pa. CO 2. Cause of: Edema, Vascular disease, Chest Wall. ■ hypercapnic (Group Ⅱ ) respiratory failure a Pa. O 2 low 60 mm. Hg and Pa. CO 2 of more than 50 mm. Hg. Cause of: Airway obstruction, Neuromuscular disease.
(2)according to pathogenic mechanism ventilatory disorders gas exchange disorders
(3)according to primary site ■ central respiratory failure ■ peripheral respiratory failure
(4)according to duration ■ acute respiratory failure ■ chronic respiratory failure
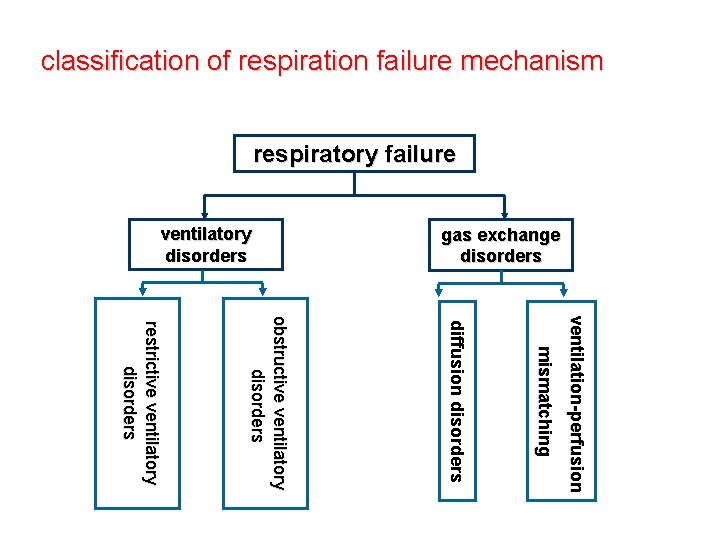
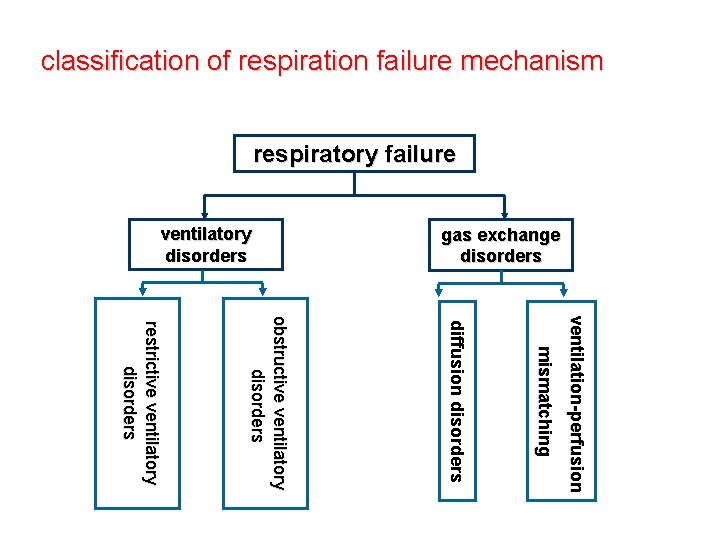
classification of respiration failure mechanism respiratory failure gas exchange disorders ventilatory disorders v e n ti l a ti o n -p e r fu s i o n m i s m a tc h i n g d i ffu s i o n d i s o r d e r s obstructive ventilatory disorders restrictive ventilatory disorders
Ⅰ. ventilatory disorders 1. restrictive ventilatory disorders Restrictive hypoventilation is caused by the diseases that affect the distensibility of the alveolar.
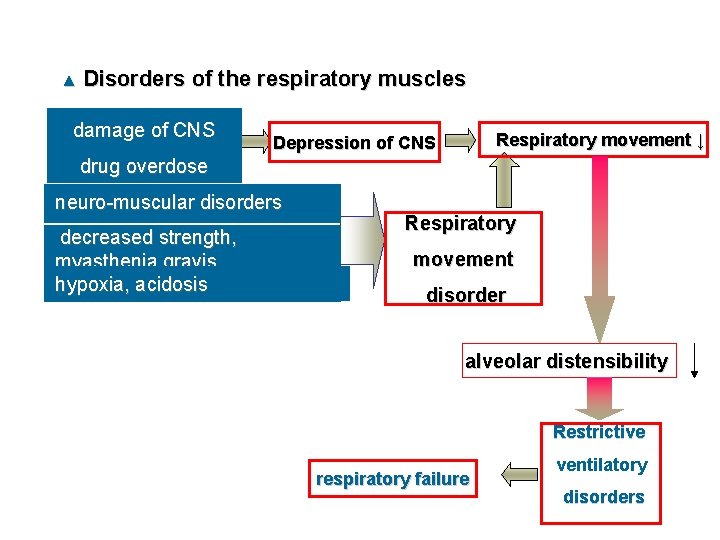
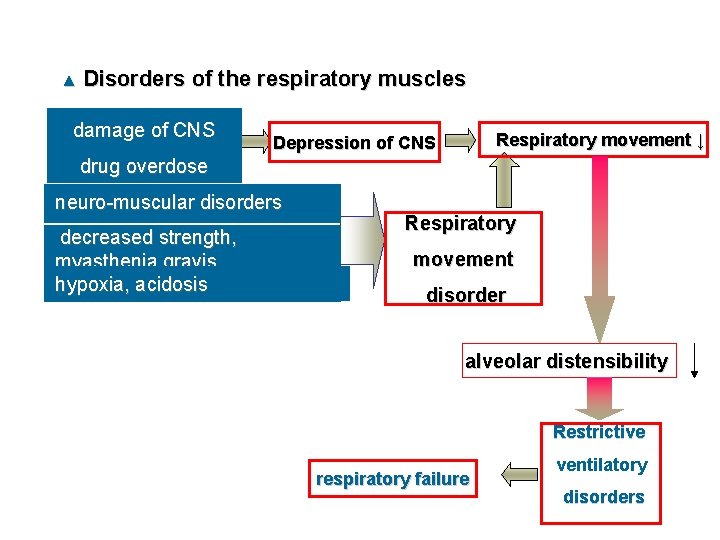
▲ Disorders of the respiratory muscles damage of CNS Respiratory movement ↓ Depression of CNS drug overdose neuro-muscular disorders decreased strength, myasthenia gravis hypoxia, acidosis Respiratory movement disorder alveolar distensibility Restrictive respiratory failure ventilatory disorders
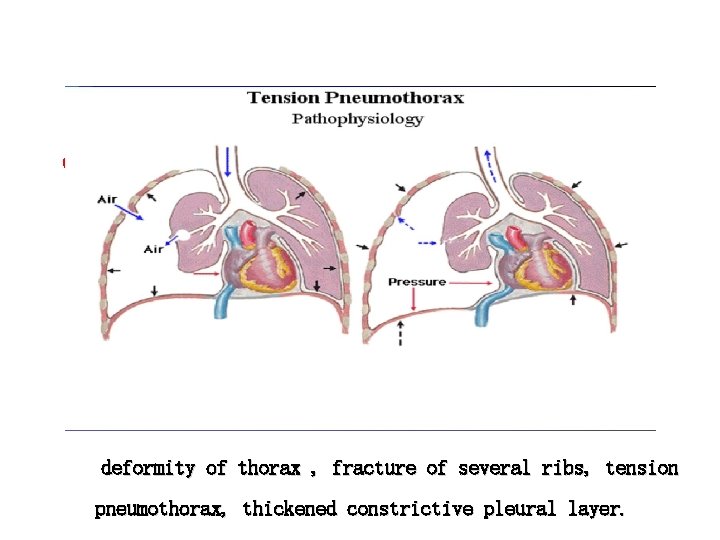
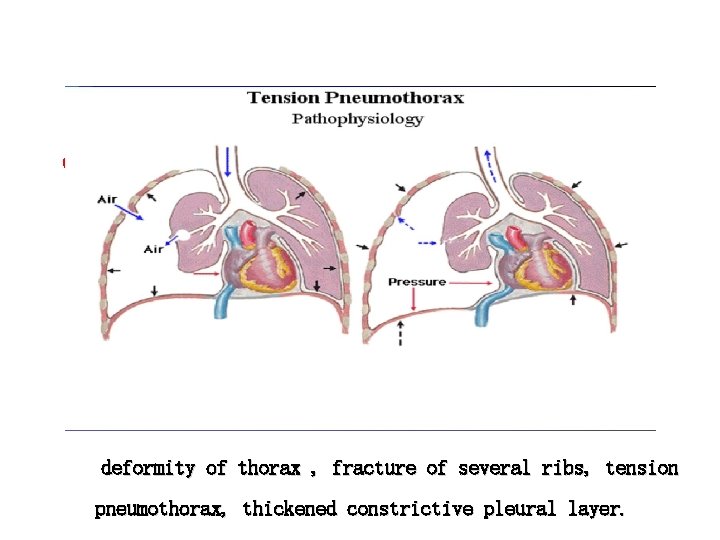
▲ ● decreased lung compliance decrease of pulmonary surfactants and increase of surface tension force ● diffuse interstitial fibrosis ▲ decreased thoracic compliance of lung deformity of thorax , fracture of several ribs, tension pneumothorax, thickened constrictive pleural layer.
2. obstructive ventilatory disorders are caused by the diseases which share the common characterestic of causing enough narrowing within the tracheobronchial tree to ■ increase resistance to the flow of air. ■ etiology asthma, emphysema, chronic bronchitis, and bronchiectasis.
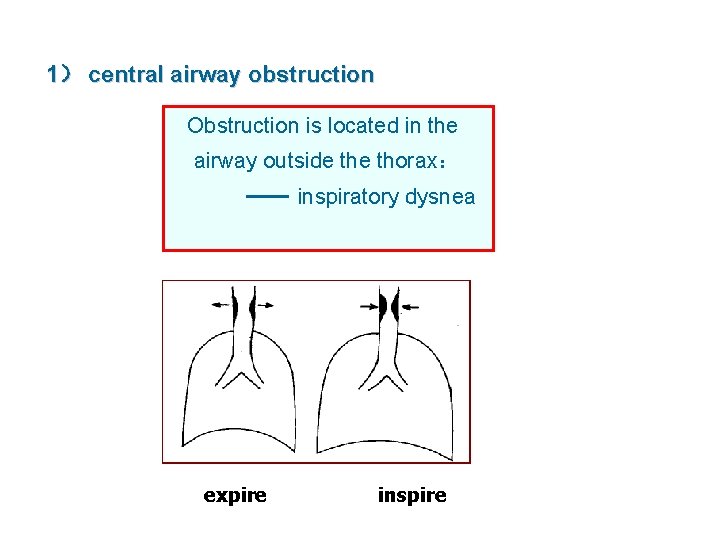
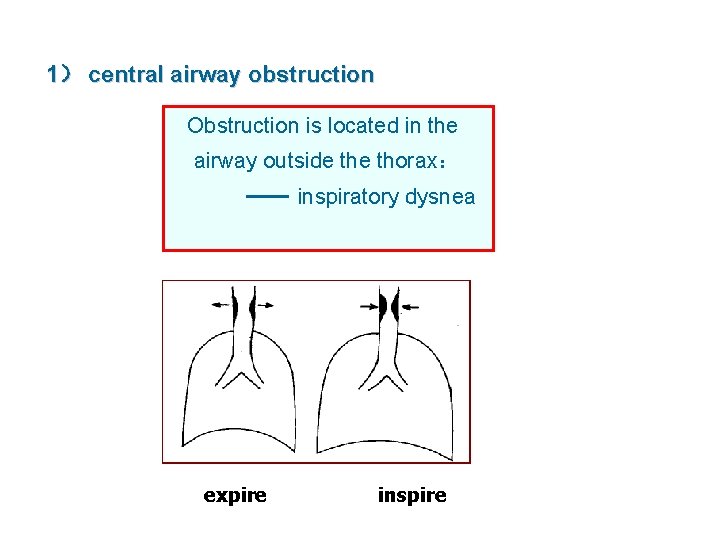
1) central airway obstruction Obstruction is located in the airway outside thorax: inspiratory dysnea expire inspire +
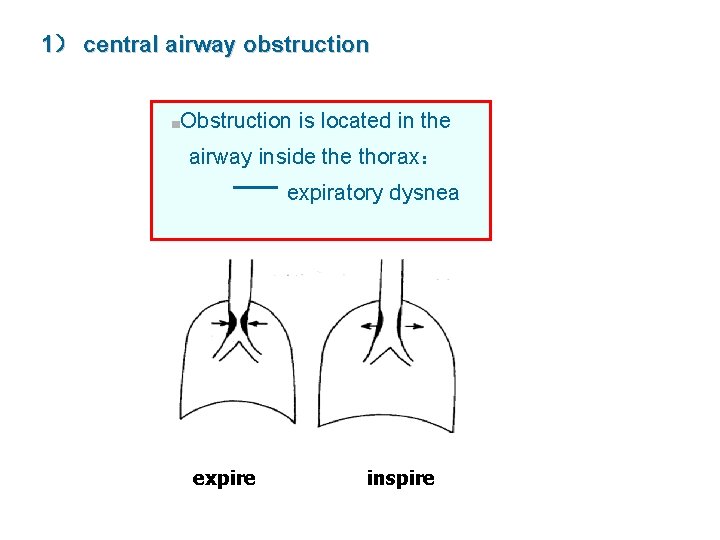
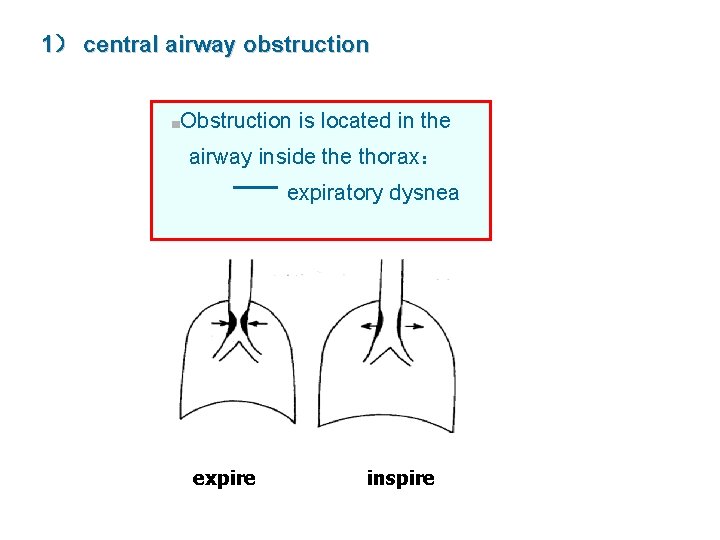
1) central airway obstruction ■Obstruction is located in the airway inside thorax: expiratory dysnea expire inspire +
2) peripheral airway obstruction smaller airways less than 2 mm in diameter. Determinants of airway closure are the intrinsic caliber of peripheral airways.
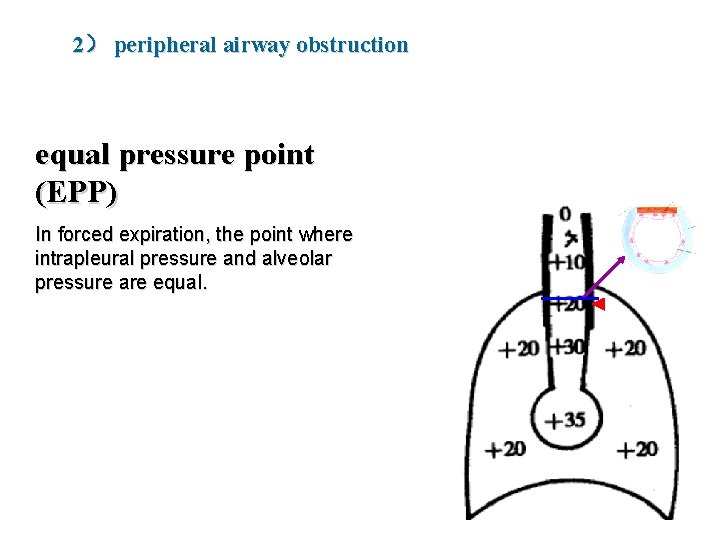
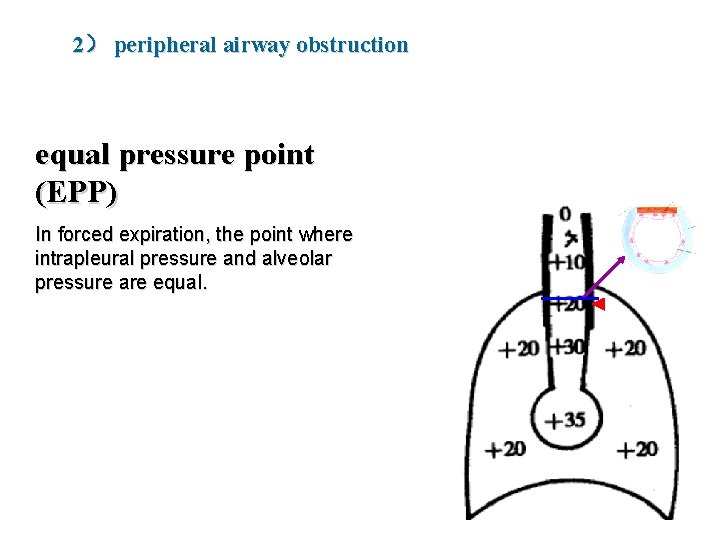
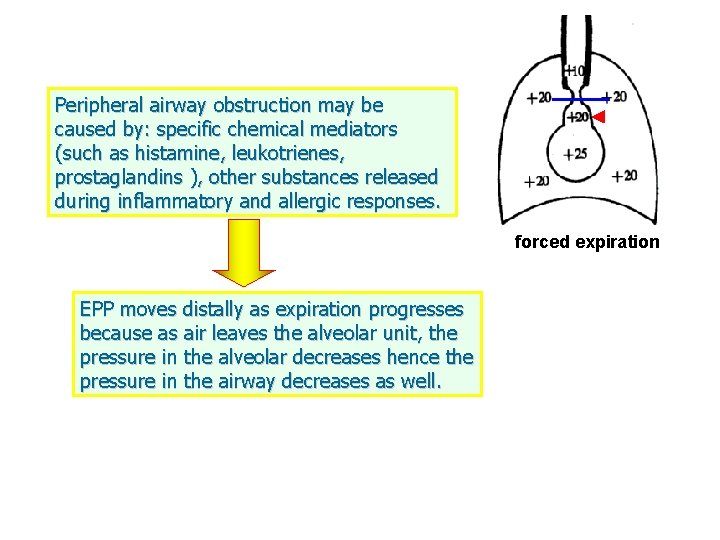
2) peripheral airway obstruction equal pressure point (EPP) In forced expiration, the point where intrapleural pressure and alveolar pressure are equal.
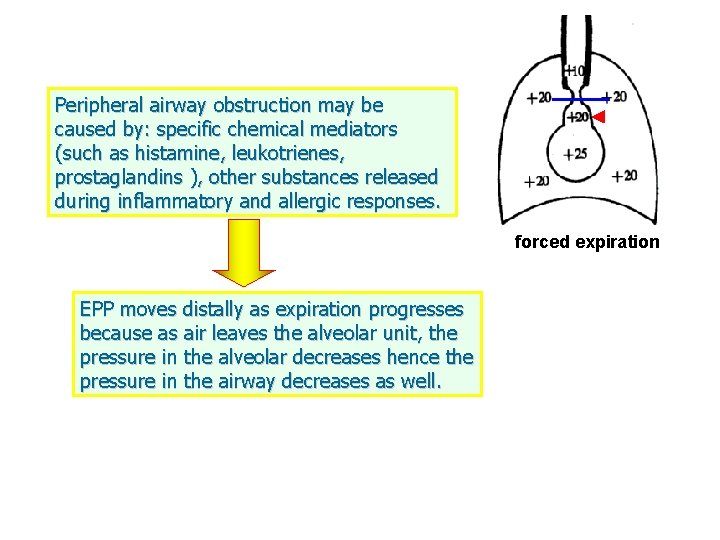
Peripheral airway obstruction may be caused by: specific chemical mediators (such as histamine, leukotrienes, prostaglandins ), other substances released during inflammatory and allergic responses. forced expiration EPP moves distally as expiration progresses because as air leaves the alveolar unit, the pressure in the alveolar decreases hence the pressure in the airway decreases as well.
forced expiration
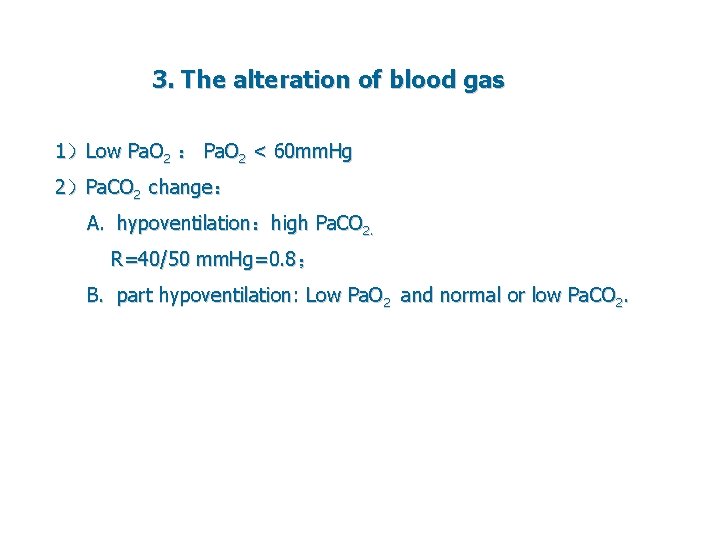
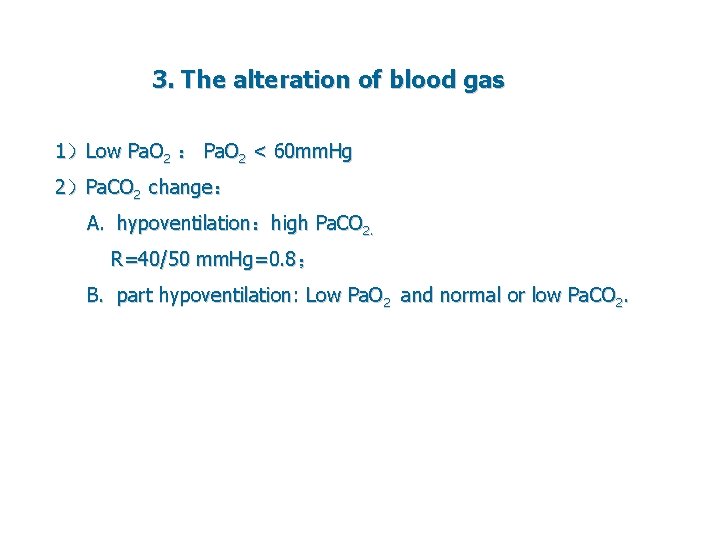
3. The alteration of blood gas 1)Low Pa. O 2 : Pa. O 2 < 60 mm. Hg 2)Pa. CO 2 change: A. hypoventilation:high Pa. CO 2. R=40/50 mm. Hg=0. 8; B. part hypoventilation: Low Pa. O 2 and normal or low Pa. CO 2.
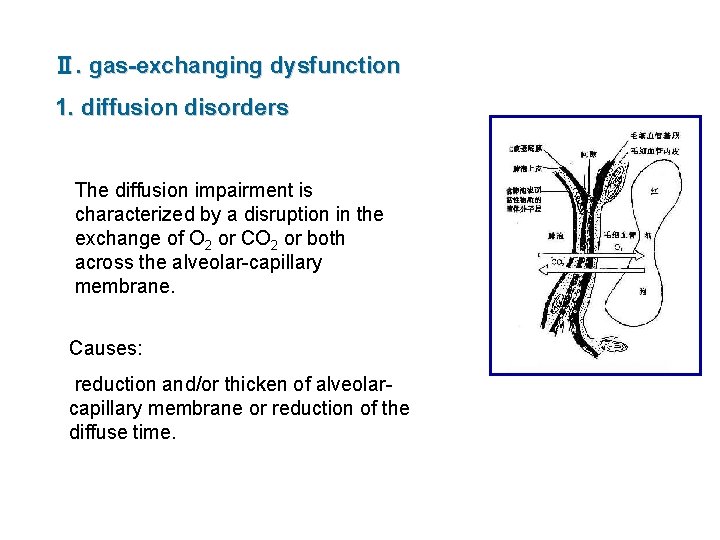
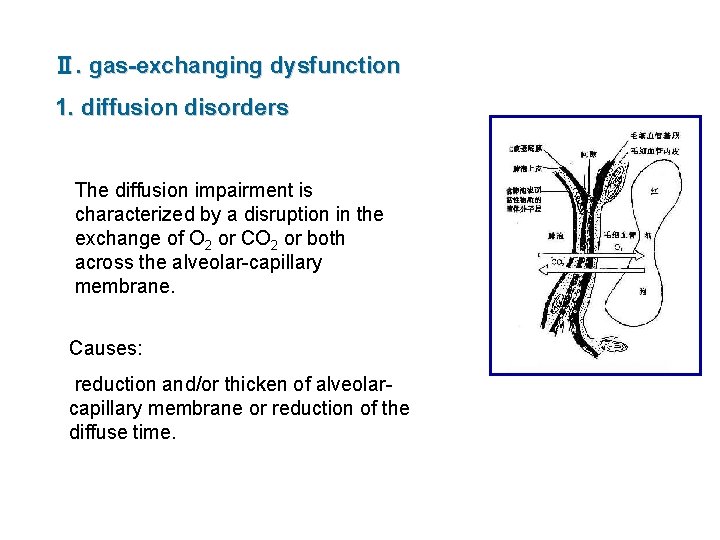
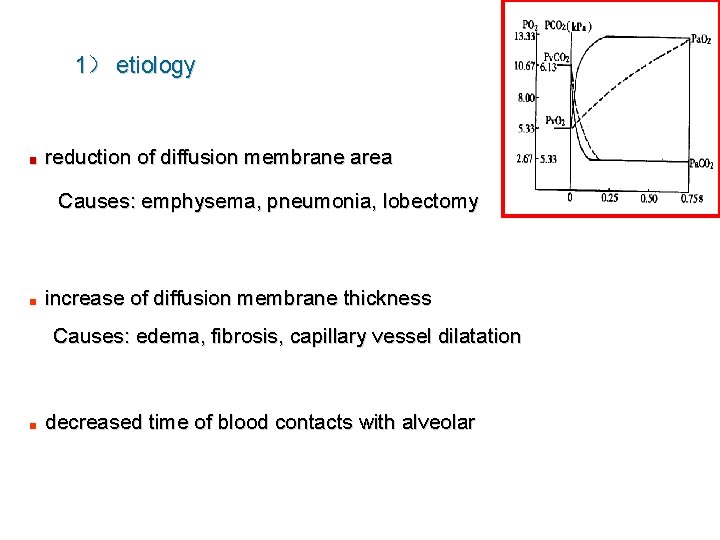
Ⅱ. gas-exchanging dysfunction 1. diffusion disorders The diffusion impairment is characterized by a disruption in the exchange of O 2 or CO 2 or both across the alveolar-capillary membrane. Causes: reduction and/or thicken of alveolarcapillary membrane or reduction of the diffuse time.
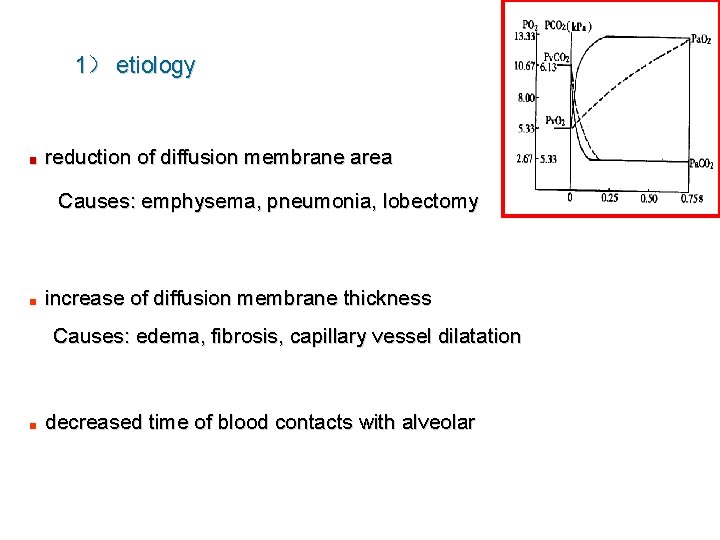
1) etiology ■ reduction of diffusion membrane area Causes: emphysema, pneumonia, lobectomy ■ increase of diffusion membrane thickness Causes: edema, fibrosis, capillary vessel dilatation ■ decreased time of blood contacts with alveolar
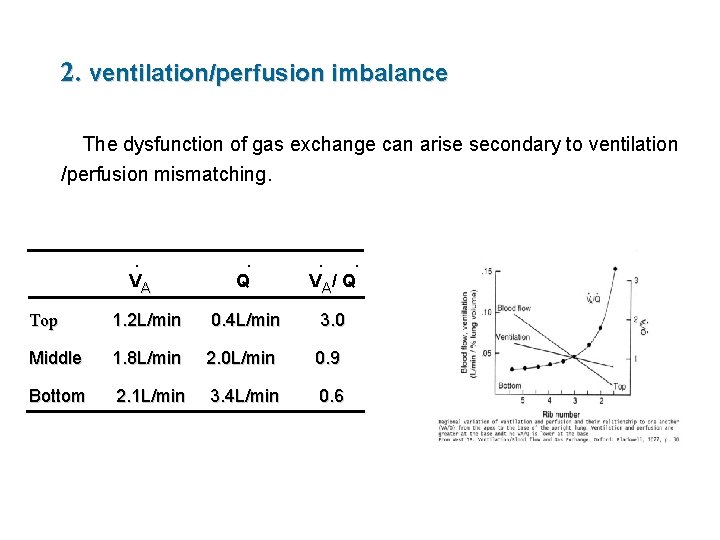
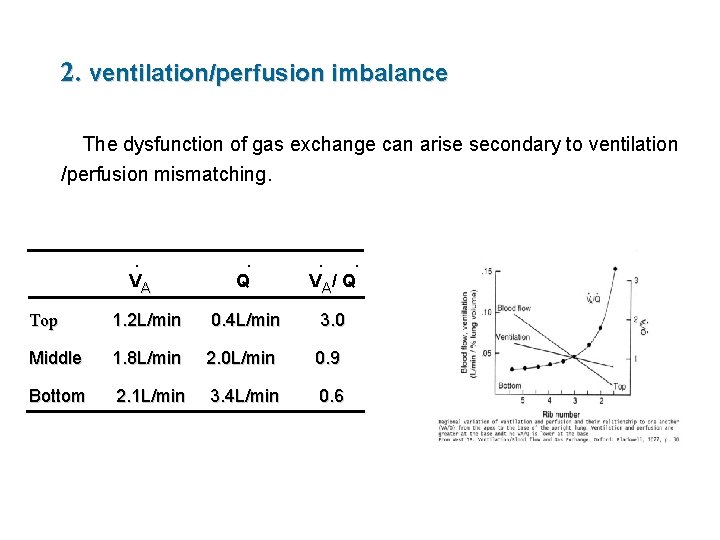
2. ventilation/perfusion imbalance The dysfunction of gas exchange can arise secondary to ventilation /perfusion mismatching. · VA · · · Q V A/ Q Top 1. 2 L/min 0. 4 L/min 3. 0 Middle 1. 8 L/min 2. 0 L/min 0. 9 Bottom 2. 1 L/min 3. 4 L/min 0. 6
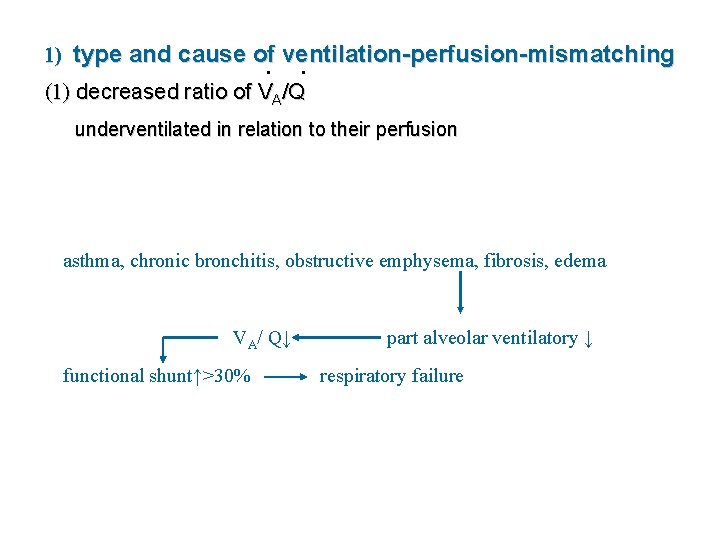
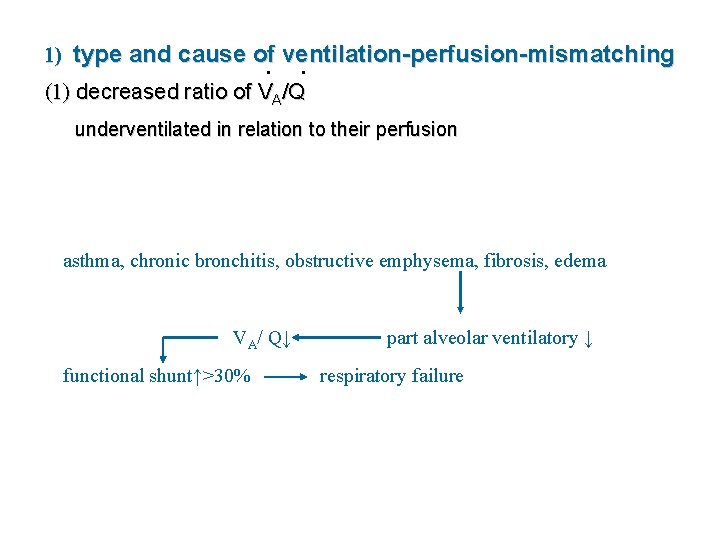
1) type and cause of ventilation-perfusion-mismatching · · (1) decreased ratio of V /Q (1) decreased ratio of VA /Q underventilated in relation to their perfusion asthma, chronic bronchitis, obstructive emphysema, fibrosis, edema · · VA/ Q↓ functional shunt↑>30% part alveolar ventilatory ↓ respiratory failure
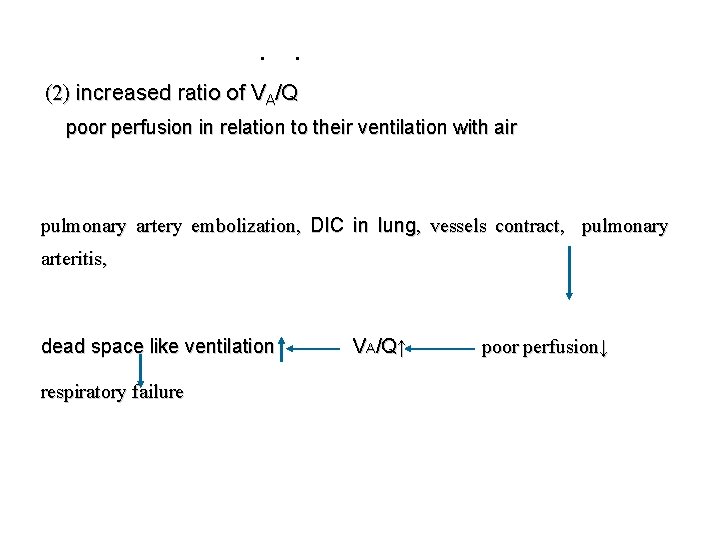
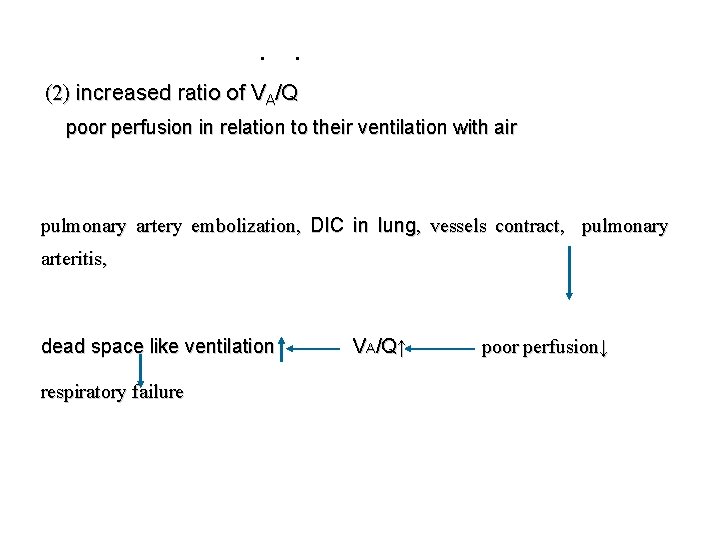
· · (2) increased ratio of VA/Q poor perfusion in relation to their ventilation with air pulmonary artery embolization, DIC in lung, vessels contract, pulmonary arteritis, dead space like ventilation respiratory failure VA/Q↑ poor perfusion↓
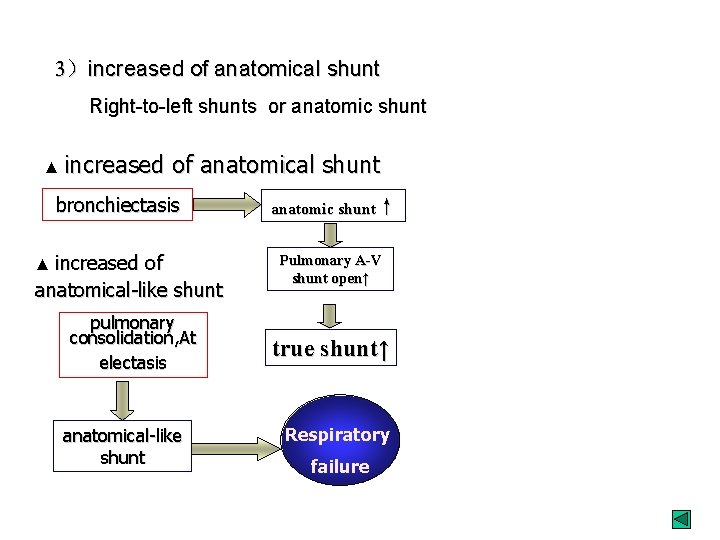
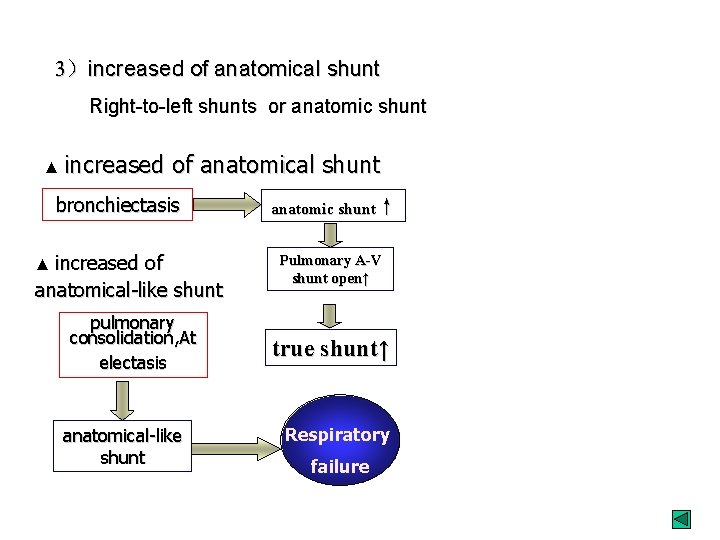
3)increased of anatomical shunt Right-to-left shunts or anatomic shunt ▲ increased of anatomical shunt bronchiectasis ▲ increased anatomic shunt↑ of anatomical-like shunt Pulmonary A-V shunt open↑ pulmonary consolidation, At electasis true shunt↑ anatomical-like shunt Respiratory failure
Effects of respiratory failure 1. Acid-base disturbances disorders of electrolyte balance
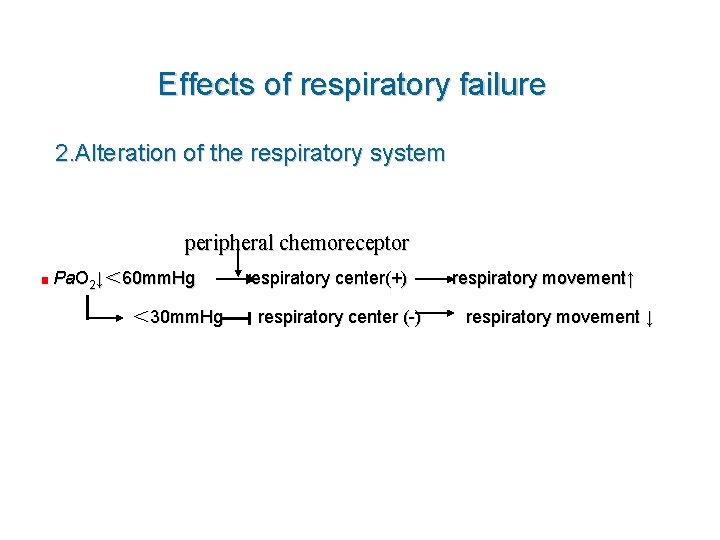
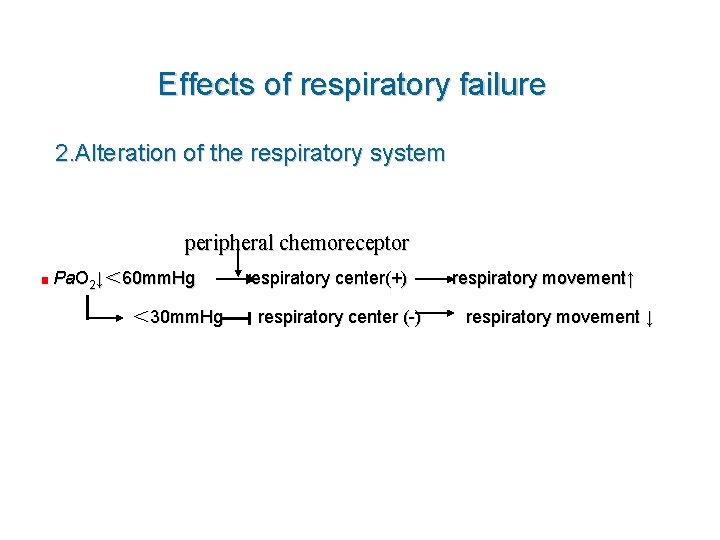
Effects of respiratory failure 2. Alteration of the respiratory system peripheral chemoreceptor ■ Pa. O 2↓< 60 mm. Hg < 30 mm. Hg respiratory center(+) respiratory center (-) respiratory movement↑ respiratory movement ↓
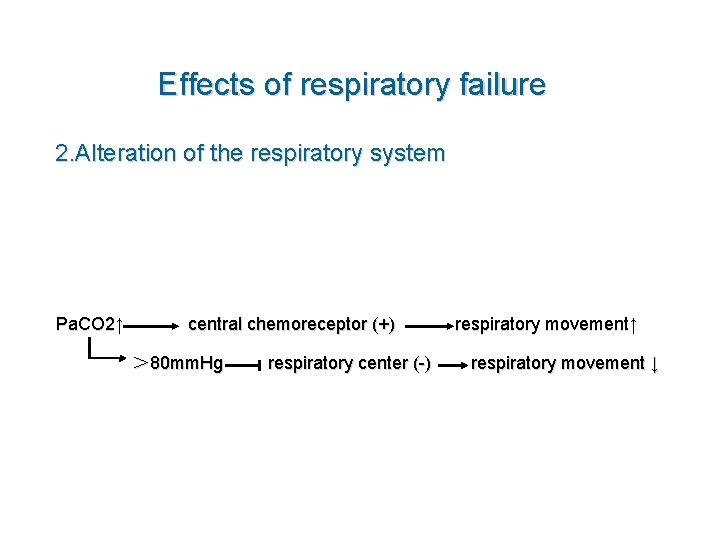
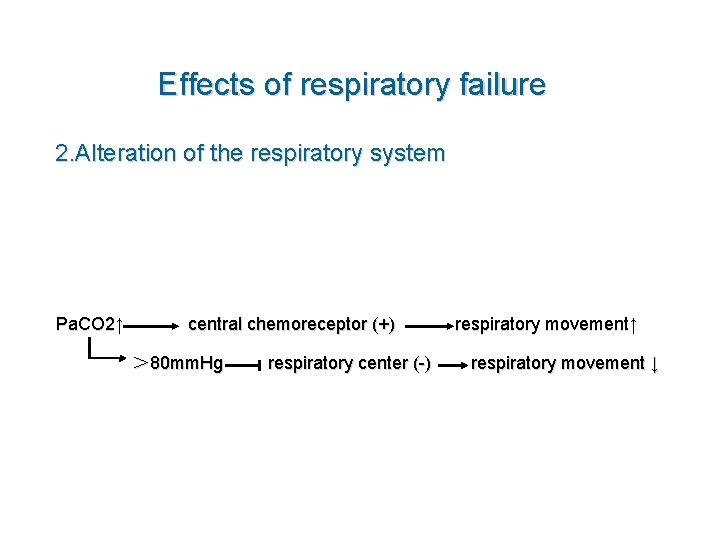
Effects of respiratory failure 2. Alteration of the respiratory system Pa. CO 2↑ central chemoreceptor (+) > 80 mm. Hg respiratory center (-) respiratory movement↑ respiratory movement ↓
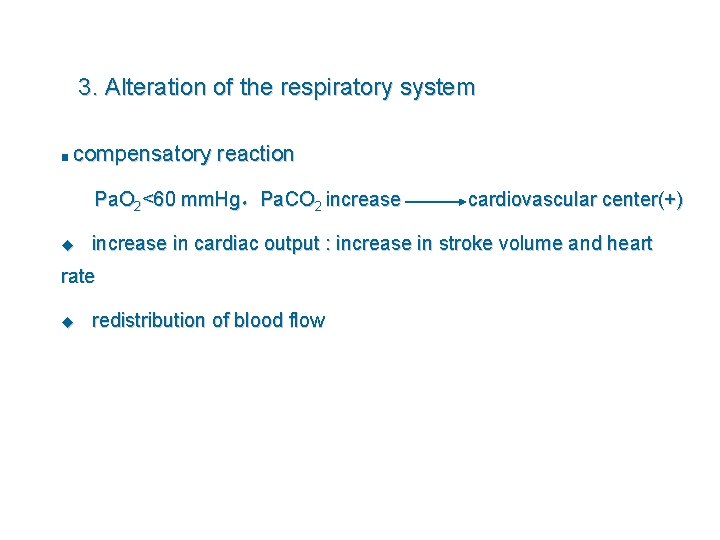
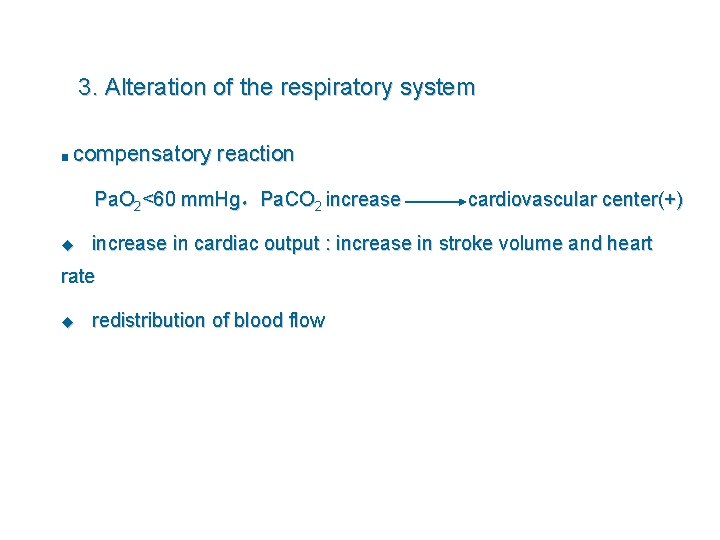
3. Alteration of the respiratory system ■ compensatory reaction Pa. O 2<60 mm. Hg,Pa. CO 2 increase u increase in cardiac output : increase in stroke volume and heart rate u cardiovascular center(+) redistribution of blood flow
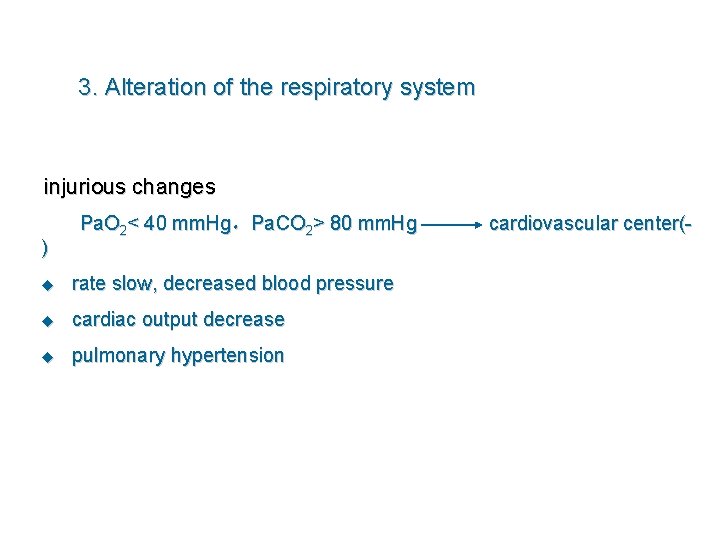
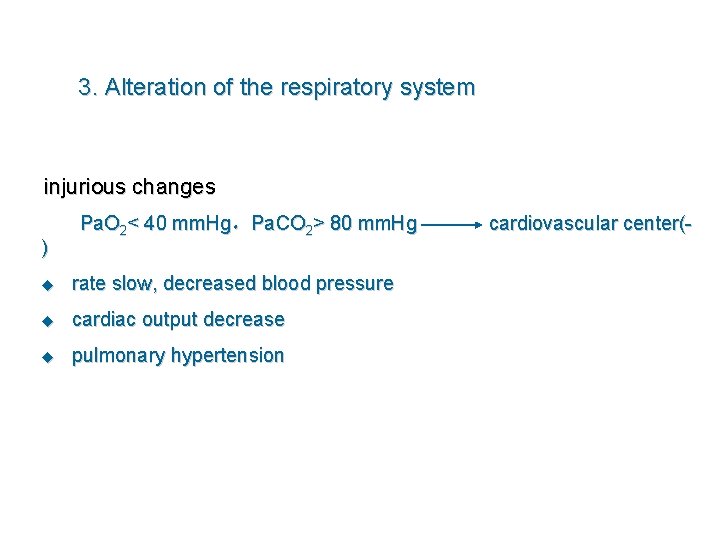
3. Alteration of the respiratory system injurious changes ) Pa. O 2< 40 mm. Hg,Pa. CO 2> 80 mm. Hg u rate slow, decreased blood pressure u cardiac output decrease u pulmonary hypertension cardiovascular center(-
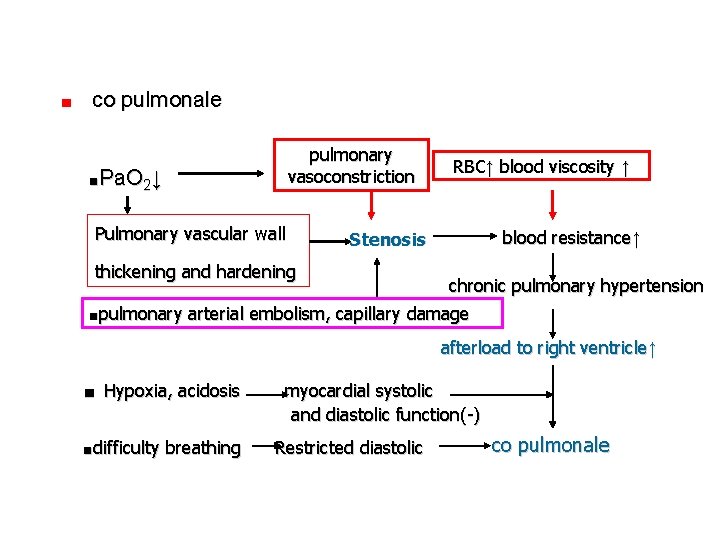
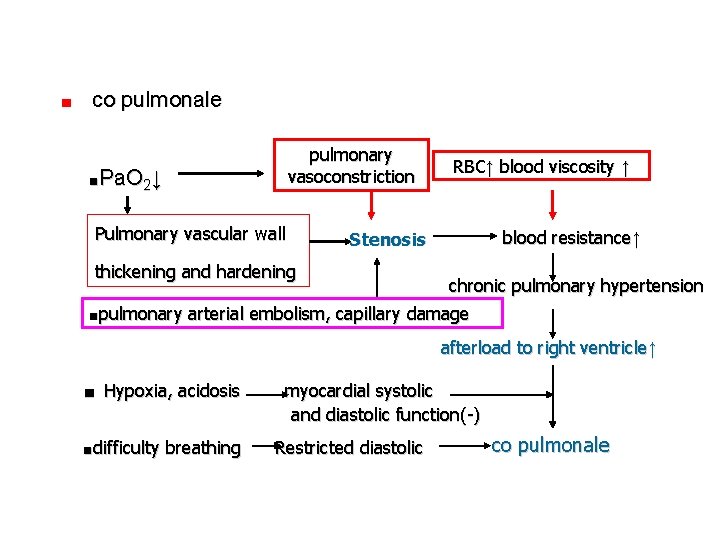
■ co pulmonale pulmonary vasoconstriction ■Pa. O 2↓ Pulmonary vascular wall RBC↑ blood viscosity ↑ blood resistance↑ Stenosis thickening and hardening chronic pulmonary hypertension ■pulmonary arterial embolism, capillary damage afterload to right ventricle↑ ■ Hypoxia, acidosis ■difficulty breathing myocardial systolic and diastolic function(-) Restricted diastolic co pulmonale
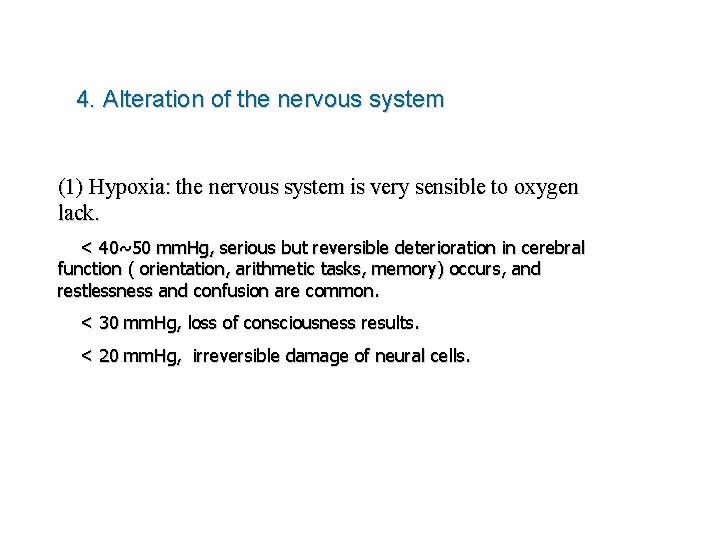
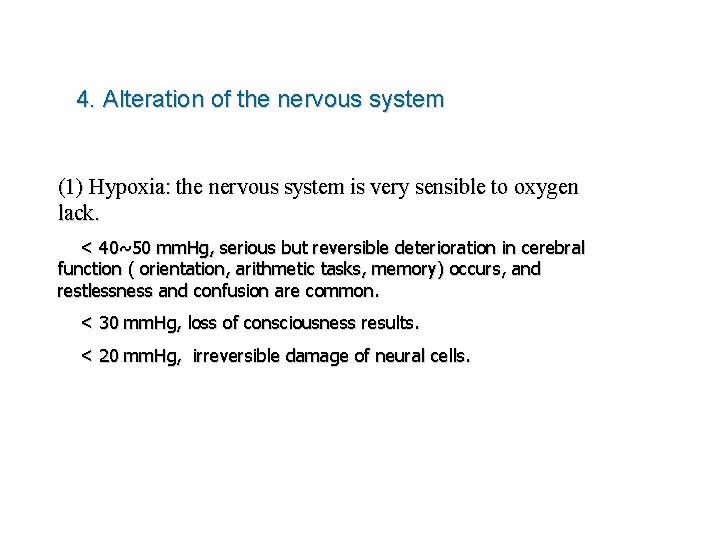
4. Alteration of the nervous system (1) Hypoxia: the nervous system is very sensible to oxygen lack. < 40~50 mm. Hg, serious but reversible deterioration in cerebral function ( orientation, arithmetic tasks, memory) occurs, and restlessness and confusion are common. < 30 mm. Hg, loss of consciousness results. < 20 mm. Hg, irreversible damage of neural cells.
4. Alteration of the nervous system (2) Hypercapnia: CO 2 nacosis. a condition of confusion, tremors, convulsions, and possible coma that may occur if blood levels of carbon dioxide increase to 80 mm Hg or higher.
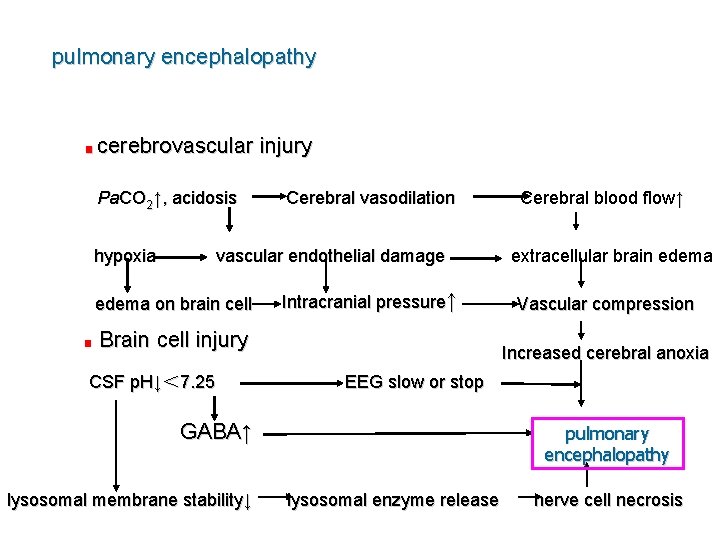
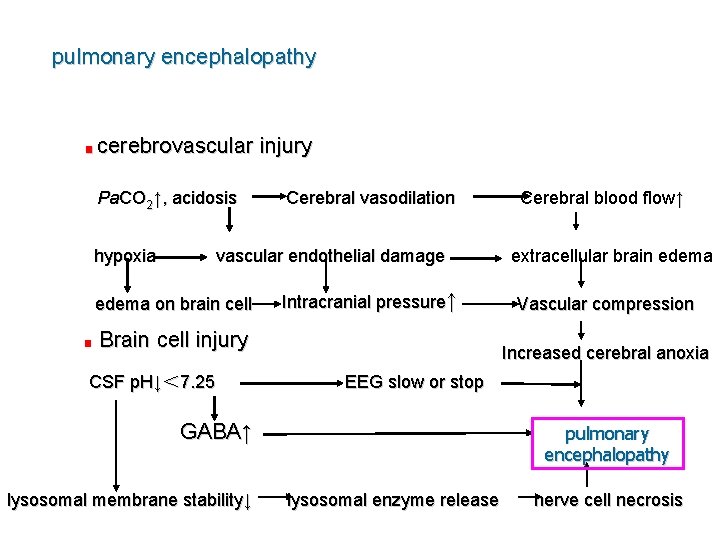
pulmonary encephalopathy ■ cerebrovascular Pa. CO 2↑, acidosis hypoxia Cerebral vasodilation vascular endothelial damage edema on brain cell ■ injury Intracranial pressure↑ Brain cell injury CSF p. H↓< 7. 25 extracellular brain edema Vascular compression Increased cerebral anoxia EEG slow or stop GABA↑ lysosomal membrane stability↓ Cerebral blood flow↑ pulmonary encephalopathy lysosomal enzyme release nerve cell necrosis
4. Alteration of the renal function 5. Alteration of the digestive system
Thanks
 Pulmonary ventilation consists of two cyclic phases, , and
Pulmonary ventilation consists of two cyclic phases, , and External vs internal respiration
External vs internal respiration External respiration
External respiration Windpipe cells
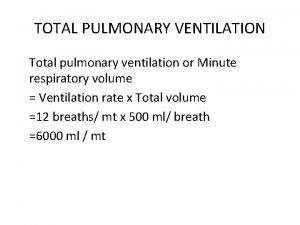
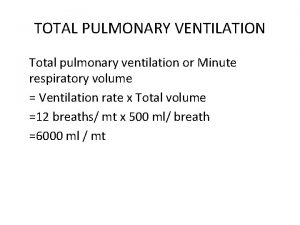
Windpipe cells Total pulmonary ventilation
Total pulmonary ventilation Respiratory physiology
Respiratory physiology Types of respiration
Types of respiration Pulmonary ventilation
Pulmonary ventilation Ventilation modes
Ventilation modes Failure to sense
Failure to sense Failure to pace vs failure to capture
Failure to pace vs failure to capture Ductile vs brittle fracture surface
Ductile vs brittle fracture surface Allergic granulomatous angiitis
Allergic granulomatous angiitis Pink puffer
Pink puffer Hypercapnic respiratory failure causes
Hypercapnic respiratory failure causes Pulmonary toilet
Pulmonary toilet Types of respiratory failure
Types of respiratory failure Complications of respiratory failure
Complications of respiratory failure Respiration vs ventilation
Respiration vs ventilation Conducting zone of the respiratory system
Conducting zone of the respiratory system Stimulus for breathing
Stimulus for breathing Differentiate between external and internal respiration
Differentiate between external and internal respiration Labled
Labled Internal and external respiration
Internal and external respiration How are internal and external respiration alike
How are internal and external respiration alike Alveoli and capillaries
Alveoli and capillaries Internal vs external respiration
Internal vs external respiration Meaning of cellular respiration
Meaning of cellular respiration External respiration
External respiration External respiration
External respiration Bird respiratory system
Bird respiratory system Air path through the respiratory system
Air path through the respiratory system External respiration steps
External respiration steps External respiration
External respiration External respiration
External respiration External-external trips
External-external trips Pulmonary gas exchange and transport diagram
Pulmonary gas exchange and transport diagram Pulmonary artery and aorta
Pulmonary artery and aorta Bronchioles
Bronchioles Pmi
Pmi Aorta and pulmonary artery
Aorta and pulmonary artery