Neonatal Jaundice Dr Kalpana Malla MD Pediatrics Manipal








- Slides: 81
Neonatal Jaundice Dr. Kalpana Malla MD Pediatrics Manipal Teaching Hospital Download more documents and slide shows on The Medical Post [ www. themedicalpost. net ]
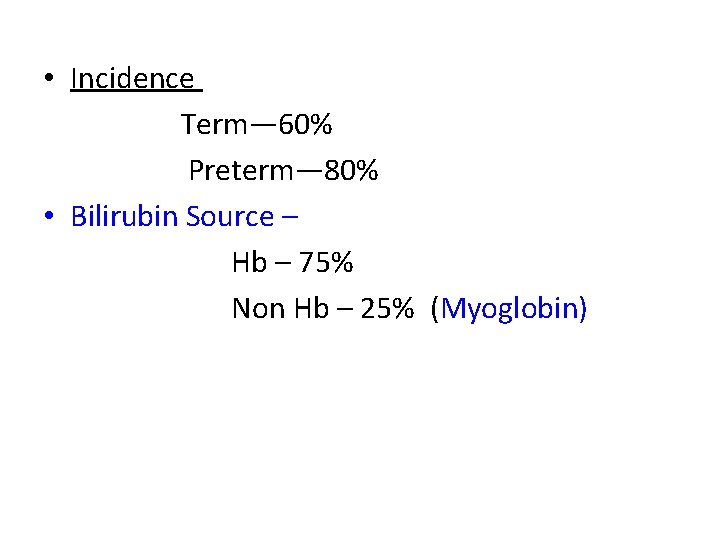
• Incidence Term— 60% Preterm— 80% • Bilirubin Source – Hb – 75% Non Hb – 25% (Myoglobin)
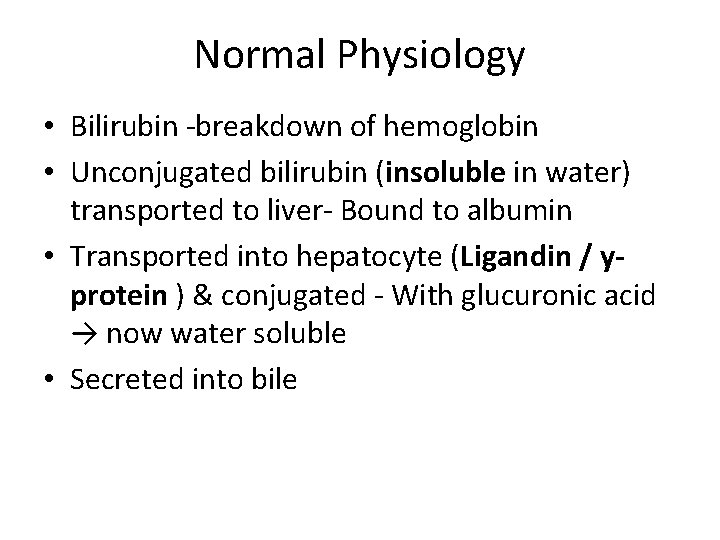
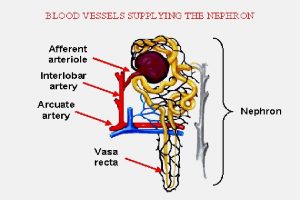
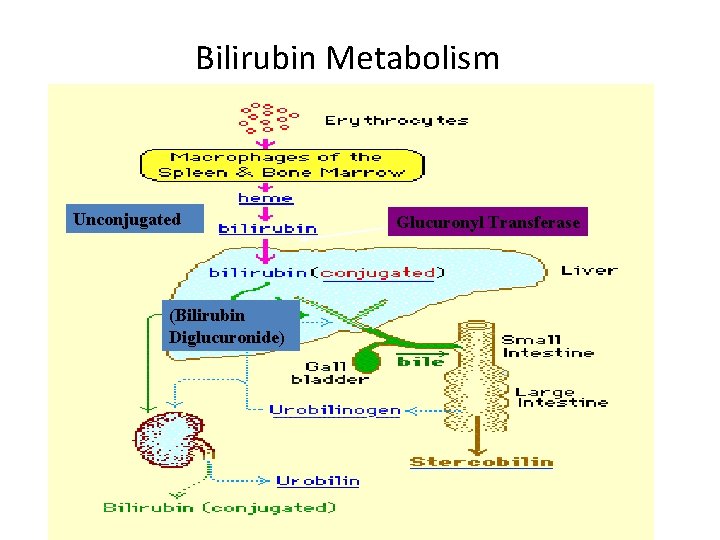
Normal Physiology • Bilirubin -breakdown of hemoglobin • Unconjugated bilirubin (insoluble in water) transported to liver- Bound to albumin • Transported into hepatocyte (Ligandin / yprotein ) & conjugated - With glucuronic acid → now water soluble • Secreted into bile
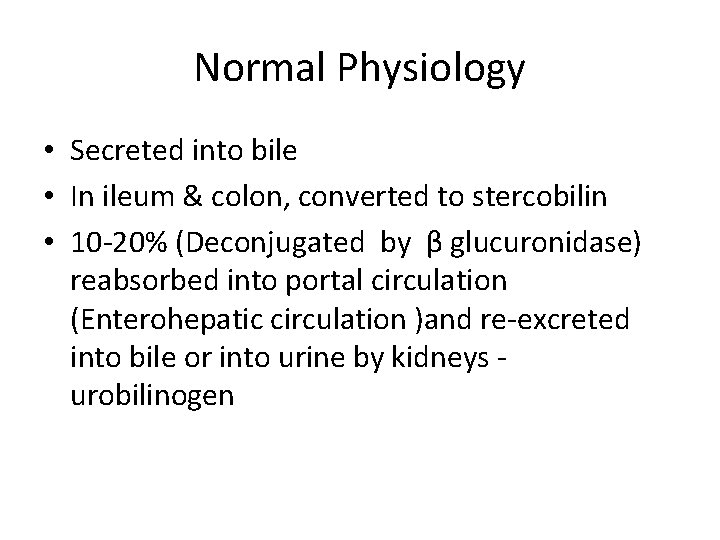
Normal Physiology • Secreted into bile • In ileum & colon, converted to stercobilin • 10 -20% (Deconjugated by β glucuronidase) reabsorbed into portal circulation (Enterohepatic circulation )and re-excreted into bile or into urine by kidneys urobilinogen
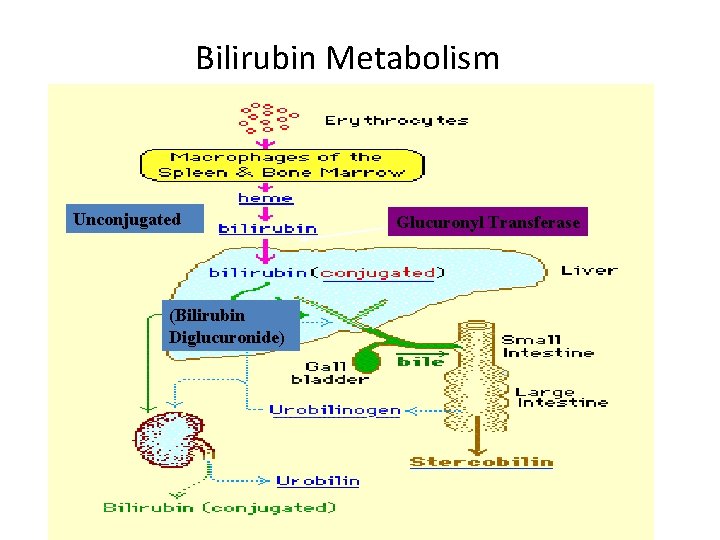
Bilirubin Metabolism Unconjugated (Bilirubin Diglucuronide) Glucuronyl Transferase
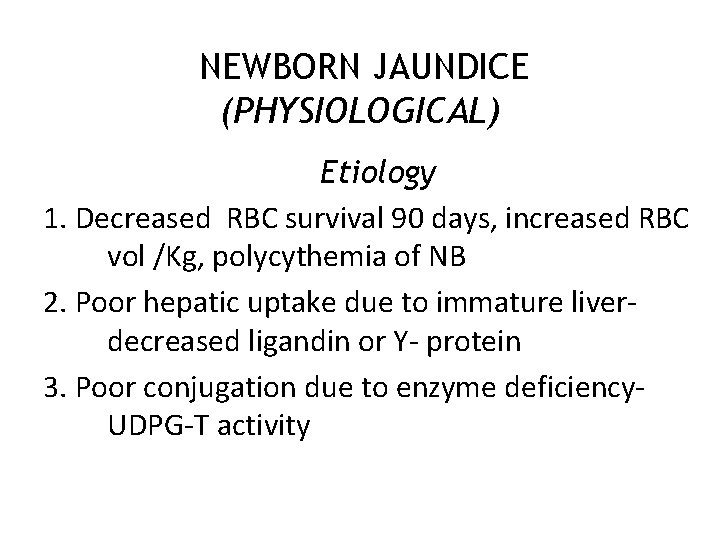
NEWBORN JAUNDICE (PHYSIOLOGICAL) Etiology 1. Decreased RBC survival 90 days, increased RBC vol /Kg, polycythemia of NB 2. Poor hepatic uptake due to immature liverdecreased ligandin or Y- protein 3. Poor conjugation due to enzyme deficiency. UDPG-T activity
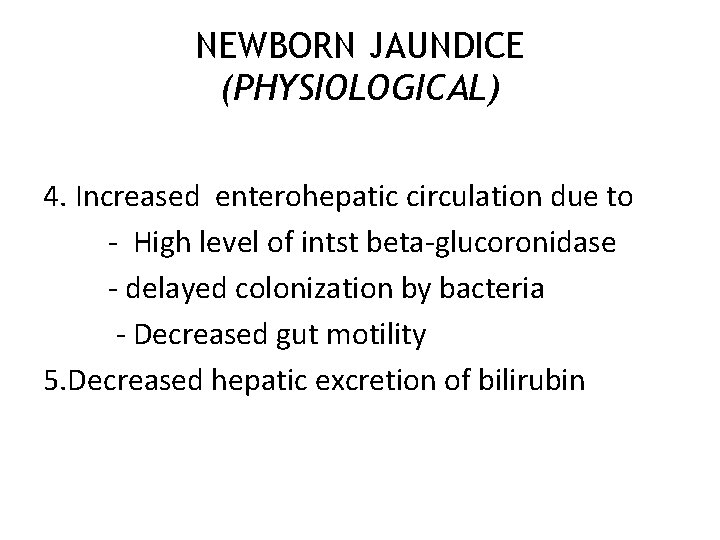
NEWBORN JAUNDICE (PHYSIOLOGICAL) 4. Increased enterohepatic circulation due to - High level of intst beta-glucoronidase - delayed colonization by bacteria - Decreased gut motility 5. Decreased hepatic excretion of bilirubin
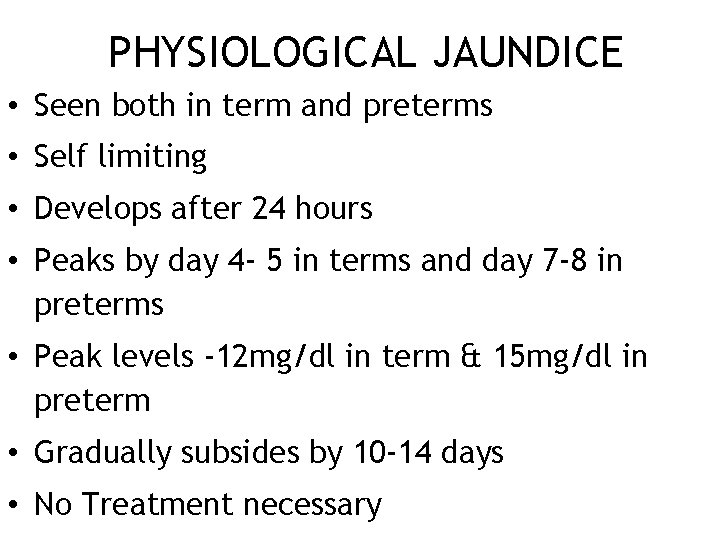
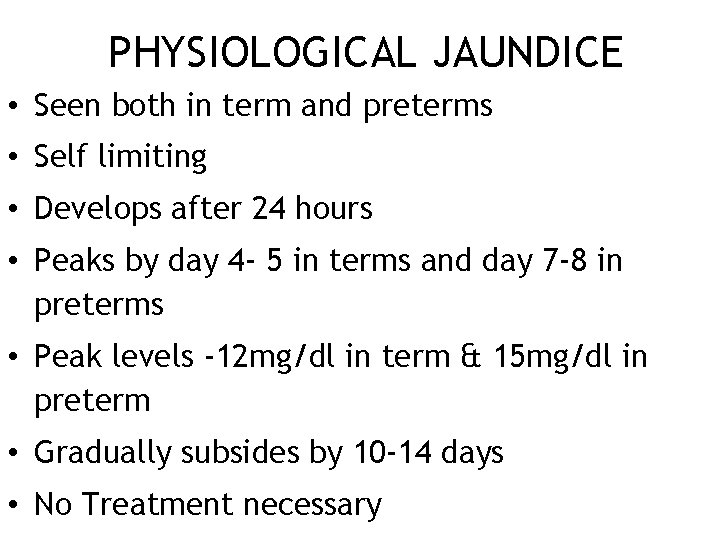
PHYSIOLOGICAL JAUNDICE • Seen both in term and preterms • Self limiting • Develops after 24 hours • Peaks by day 4 - 5 in terms and day 7 -8 in preterms • Peak levels -12 mg/dl in term & 15 mg/dl in preterm • Gradually subsides by 10 -14 days • No Treatment necessary
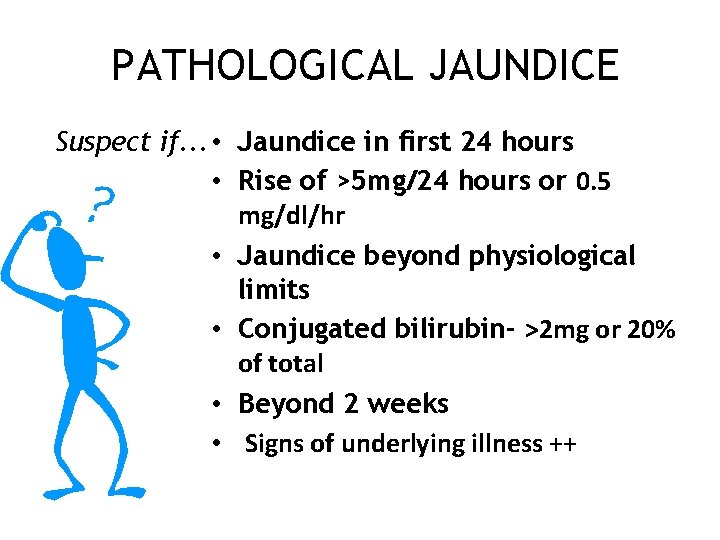
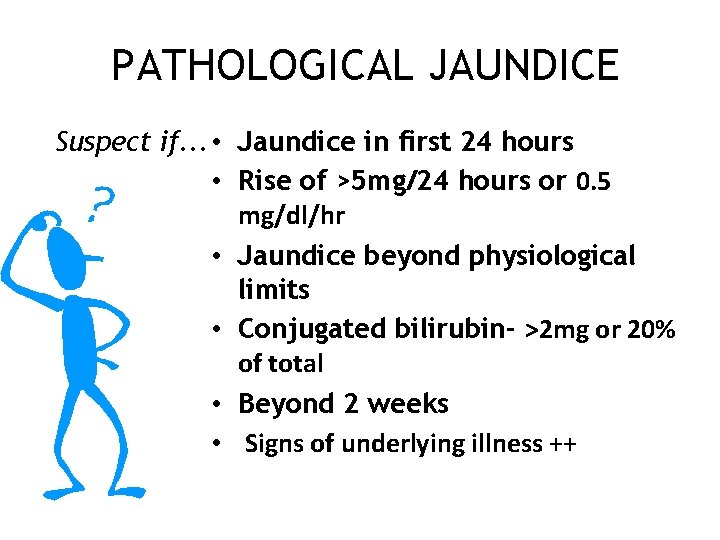
PATHOLOGICAL JAUNDICE Suspect if. . . • Jaundice in first 24 hours • Rise of >5 mg/24 hours or 0. 5 mg/dl/hr • Jaundice beyond physiological limits • Conjugated bilirubin- >2 mg or 20% of total • Beyond 2 weeks • Signs of underlying illness ++
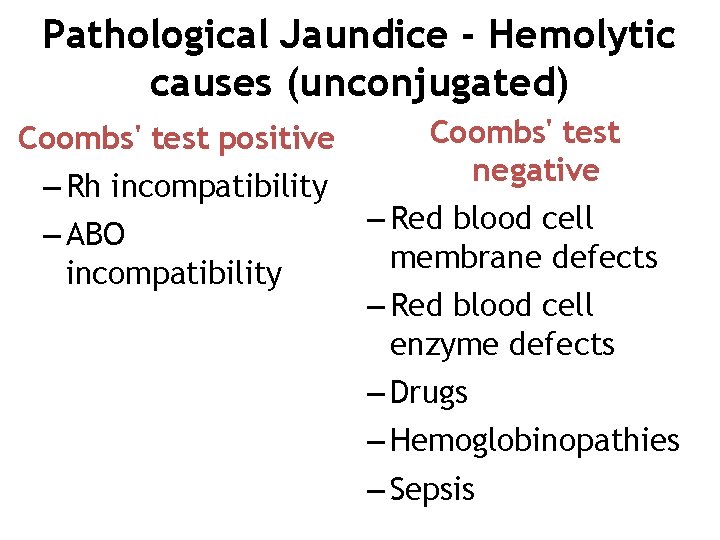
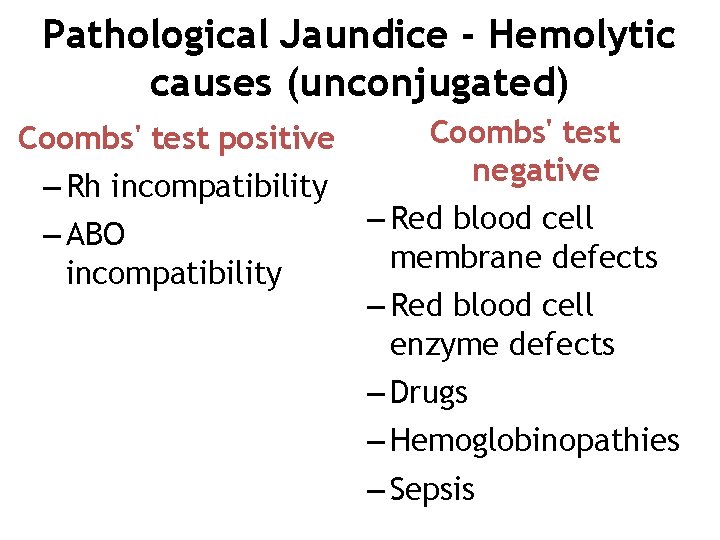
Pathological Jaundice - Hemolytic causes (unconjugated) Coombs' test positive – Rh incompatibility – ABO incompatibility Coombs' test negative – Red blood cell membrane defects – Red blood cell enzyme defects – Drugs – Hemoglobinopathies – Sepsis
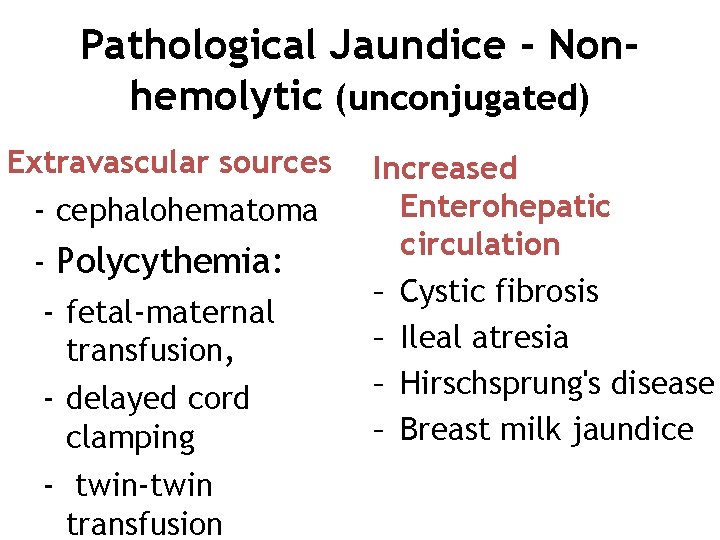
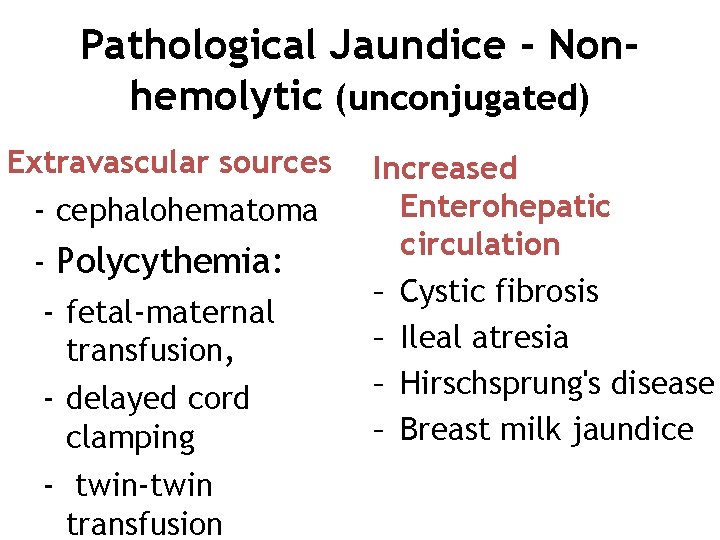
Pathological Jaundice - Nonhemolytic (unconjugated) Extravascular sources - cephalohematoma - Polycythemia: - fetal-maternal transfusion, - delayed cord clamping - twin-twin transfusion Increased Enterohepatic circulation – Cystic fibrosis – Ileal atresia – Hirschsprung's disease – Breast milk jaundice
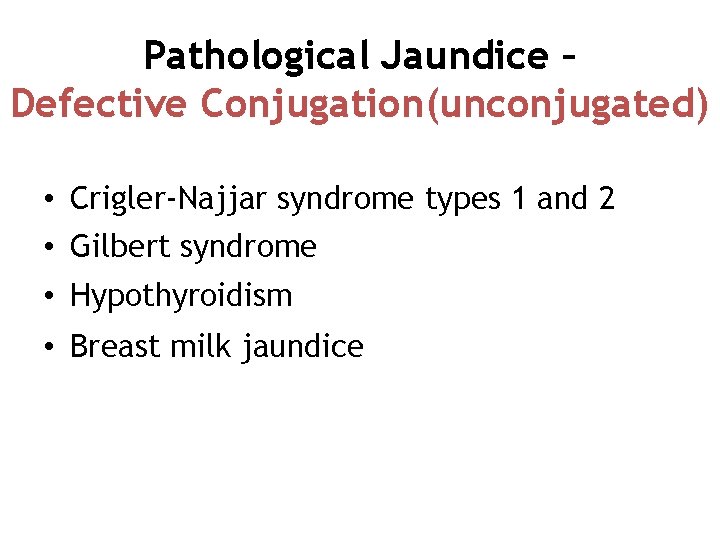
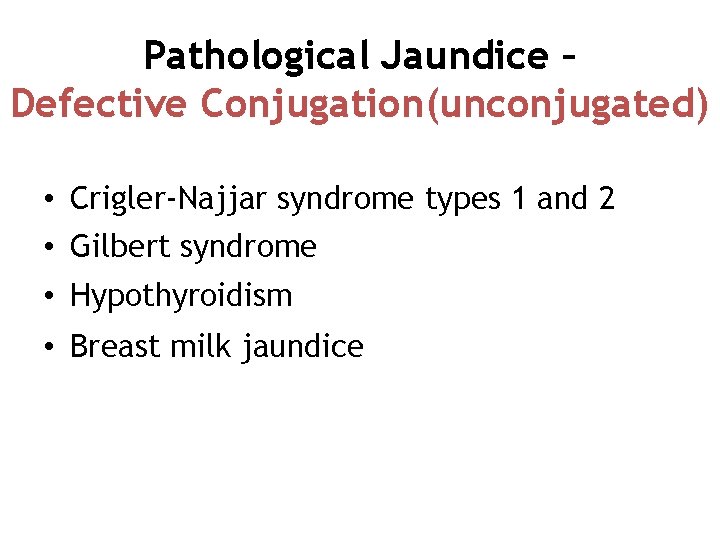
Pathological Jaundice – Defective Conjugation(unconjugated) • Crigler-Najjar syndrome types 1 and 2 • Gilbert syndrome • Hypothyroidism • Breast milk jaundice
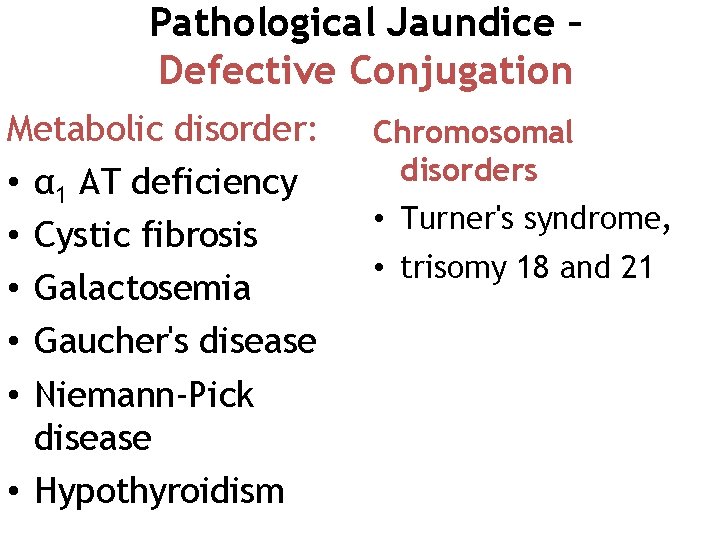
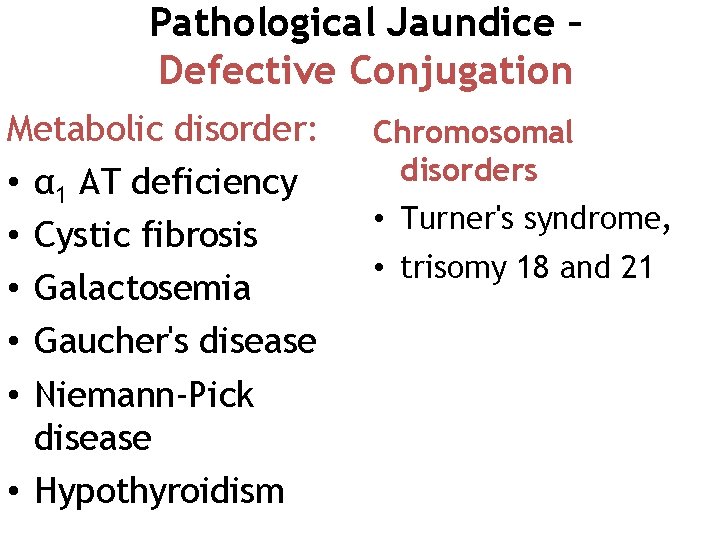
Pathological Jaundice – Defective Conjugation Metabolic disorder: • α 1 AT deficiency • Cystic fibrosis • Galactosemia • Gaucher's disease • Niemann-Pick disease • Hypothyroidism Chromosomal disorders • Turner's syndrome, • trisomy 18 and 21
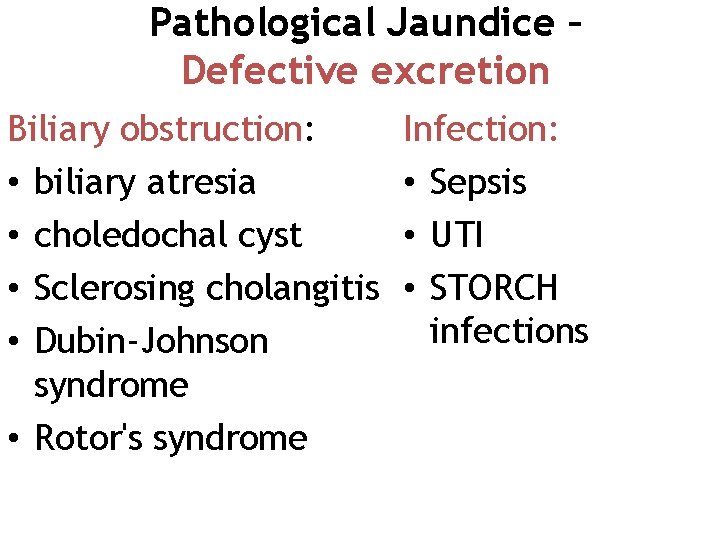
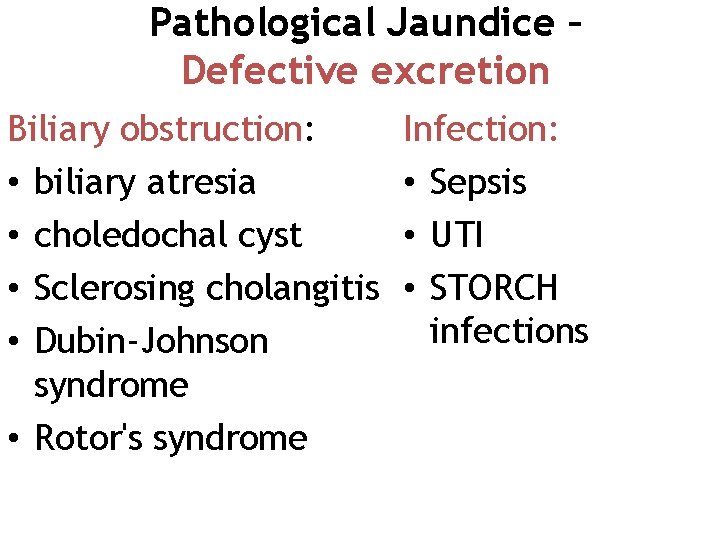
Pathological Jaundice – Defective excretion Biliary obstruction: • biliary atresia • choledochal cyst • Sclerosing cholangitis • Dubin-Johnson syndrome • Rotor's syndrome Infection: • Sepsis • UTI • STORCH infections
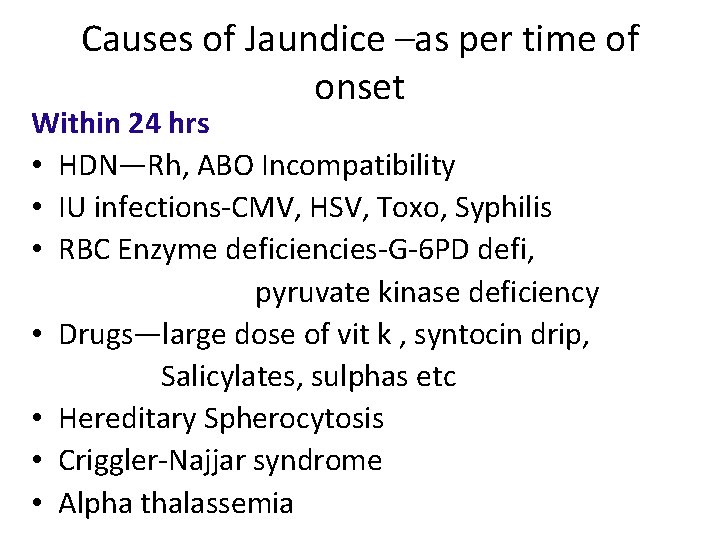
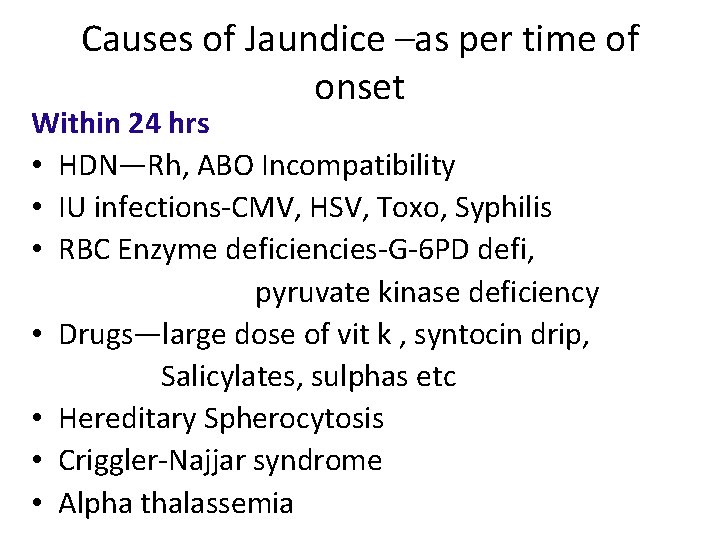
Causes of Jaundice –as per time of onset Within 24 hrs • HDN—Rh, ABO Incompatibility • IU infections-CMV, HSV, Toxo, Syphilis • RBC Enzyme deficiencies-G-6 PD defi, pyruvate kinase deficiency • Drugs—large dose of vit k , syntocin drip, Salicylates, sulphas etc • Hereditary Spherocytosis • Criggler-Najjar syndrome • Alpha thalassemia
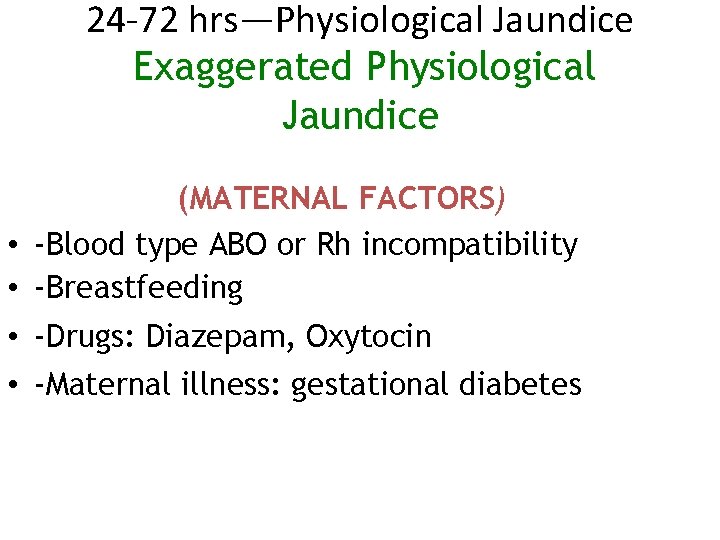
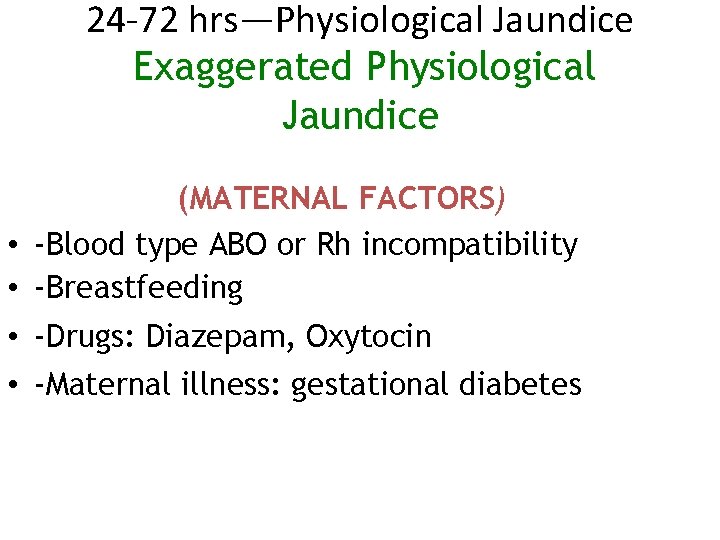
24 -72 hrs—Physiological Jaundice Exaggerated Physiological Jaundice (MATERNAL FACTORS) • -Blood type ABO or Rh incompatibility • -Breastfeeding • -Drugs: Diazepam, Oxytocin • -Maternal illness: gestational diabetes
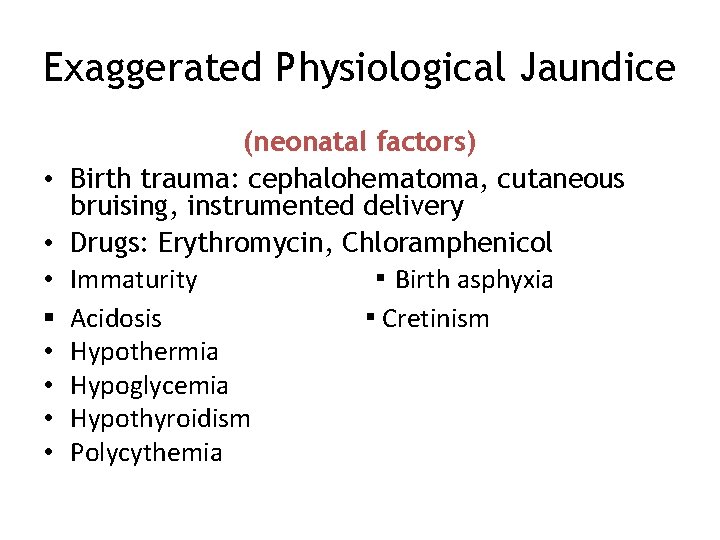
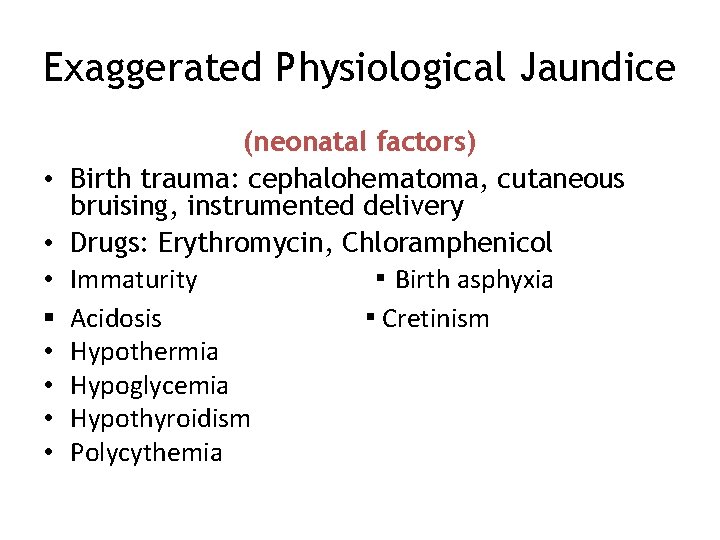
Exaggerated Physiological Jaundice • • • § • • (neonatal factors) Birth trauma: cephalohematoma, cutaneous bruising, instrumented delivery Drugs: Erythromycin, Chloramphenicol Immaturity ▪ Birth asphyxia Acidosis ▪ Cretinism Hypothermia Hypoglycemia Hypothyroidism Polycythemia
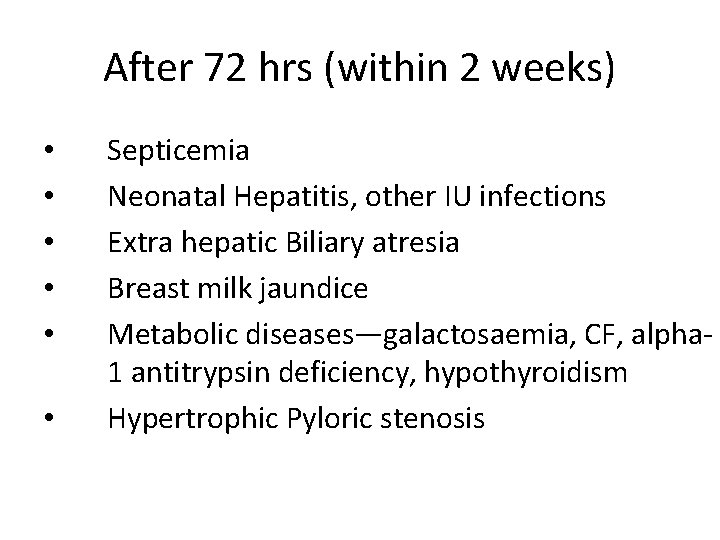
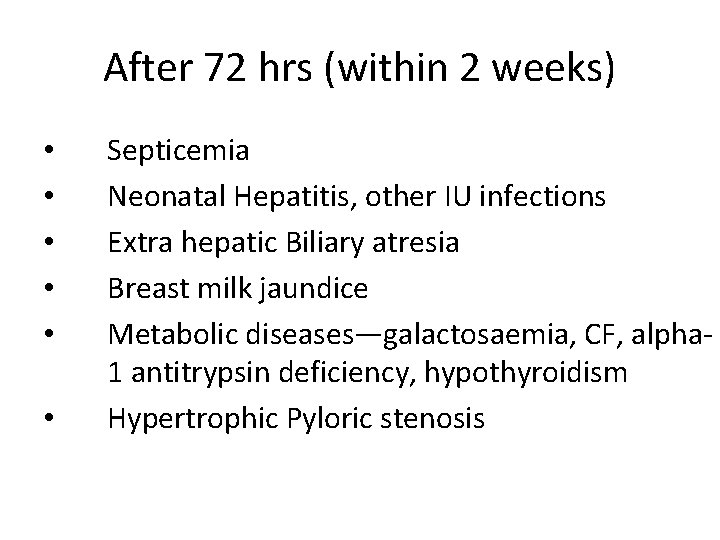
After 72 hrs (within 2 weeks) • • • Septicemia Neonatal Hepatitis, other IU infections Extra hepatic Biliary atresia Breast milk jaundice Metabolic diseases—galactosaemia, CF, alpha 1 antitrypsin deficiency, hypothyroidism Hypertrophic Pyloric stenosis


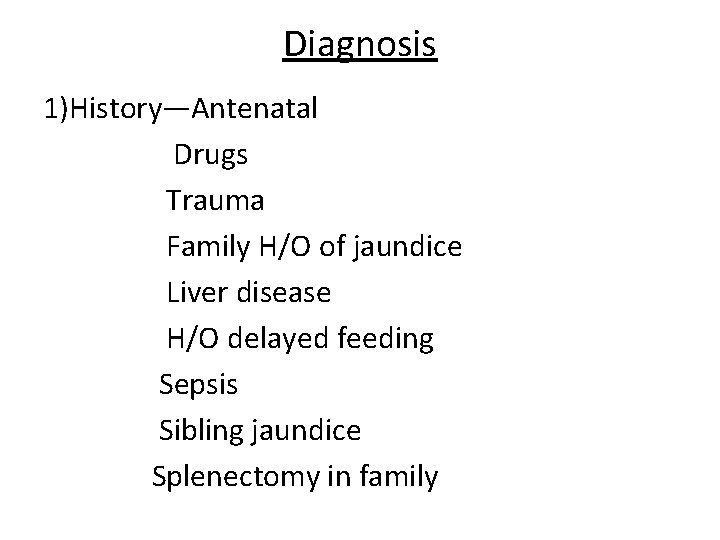
Diagnosis 1)History—Antenatal Drugs Trauma Family H/O of jaundice Liver disease H/O delayed feeding Sepsis Sibling jaundice Splenectomy in family
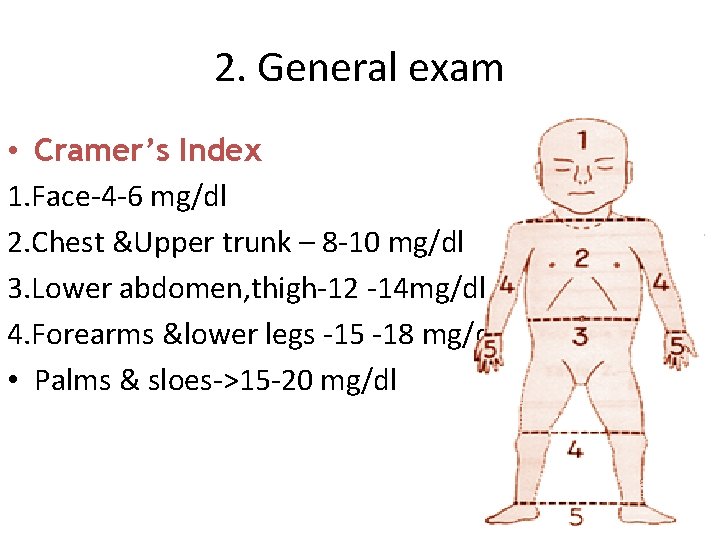
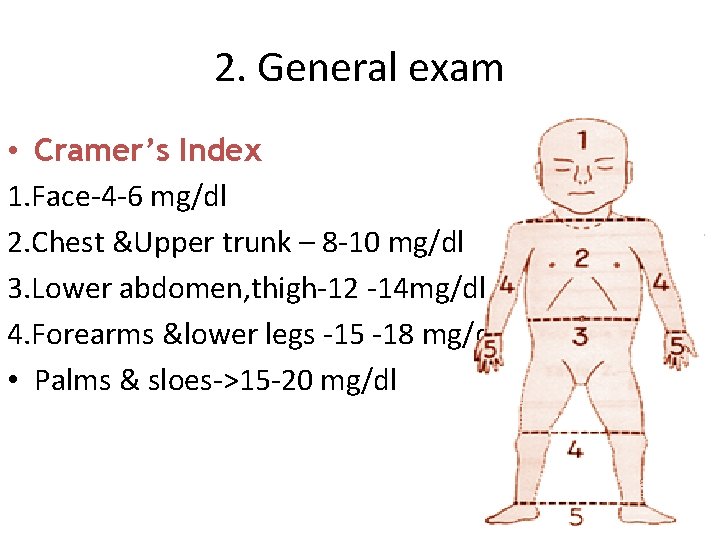
2. General exam • Cramer’s Index 1. Face-4 -6 mg/dl 2. Chest &Upper trunk – 8 -10 mg/dl 3. Lower abdomen, thigh-12 -14 mg/dl 4. Forearms &lower legs -15 -18 mg/dl • Palms & sloes->15 -20 mg/dl
Examine Gestation age-preterm, IUGR Cephalhematoma, bruising Pallor-hemolytic anemia Patechiea -sepsis, erythroblastosis, cong infections • HSM-hemolytic anemia, cong infections • Evidence of hypothyroidism, cong infections • •
3) Lab investigations 1. Hemoglobin, PCV with peripheral smear 2. Total Bilirubin (Total / Direct & Indirect) - >12 mg /<24 hr - <12 mg/ >24 hr 3. Bilirubin level –Special tests – – TORCH titres – Metabolic work up – USG / X ray abdomen - Thyroid function tests - Sepsis screen • Blood group and Rh typing • Reticulocyte count
Investigations in RH incompatibility • Antenatal - (mother Rh-ve, previous baby Rh + ve, father Rh +ve. 1) H/o of abortion, H/o having taken Anti D gammaglobulin 2) USG for baby maturation , HSM, ascites, hydrominos, gen. anasraca
Investigations in RH incompatibility • Antenatal - Blood grp (ABO & Rh) of father , earlier baby - Indirect Coomb’s test – to detect antibodies in mother’s serum Ig. G Anti body Titre to D TO be estimated at 12 -16, 2832 and 36 weeks. If anti D antibody Titre 1: 16 it should be tested serially - Ab titre in mother’s blood ->1: 64 dignostic of HDNTO CONSIDER TERMINATION OF PREGNANCY.
Investigations in RH incompatibility • Anmiocentesis: - Look for lecithin sphingomyelin ratio to suggest maturity. - Shake test for 15 sec. with equal vol etanol 95%allowed to stand-ring of buble at the disc - Optical density-by spectrophotometer OD. >0. 15 denotes maturity of lungs - Alpha feto protein level increased –rh issoimun - Fetal bloob grp prenatally – amniocentesis
POSTNATAL INVESTIGATION BABY Cord blood—all babies of Rh-ve mothers, all Unknown blood groups, all with prior h/o jaundice in earlier babies Blood group-both mother and baby - For evidence of hemolysis – Direct Coombs test Reticulocyte count - >10 suggest hemolysis. Hemoglobin cord Peripheral smear -RBC morphology Bilirubin
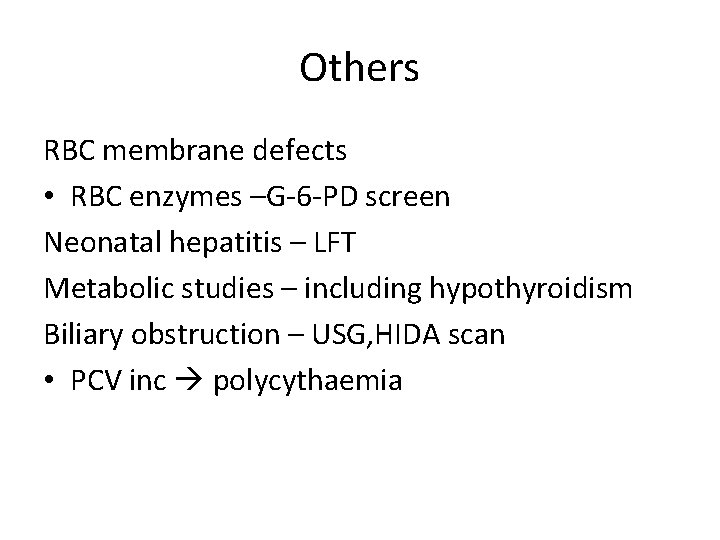
Others RBC membrane defects • RBC enzymes –G-6 -PD screen Neonatal hepatitis – LFT Metabolic studies – including hypothyroidism Biliary obstruction – USG, HIDA scan • PCV inc polycythaemia
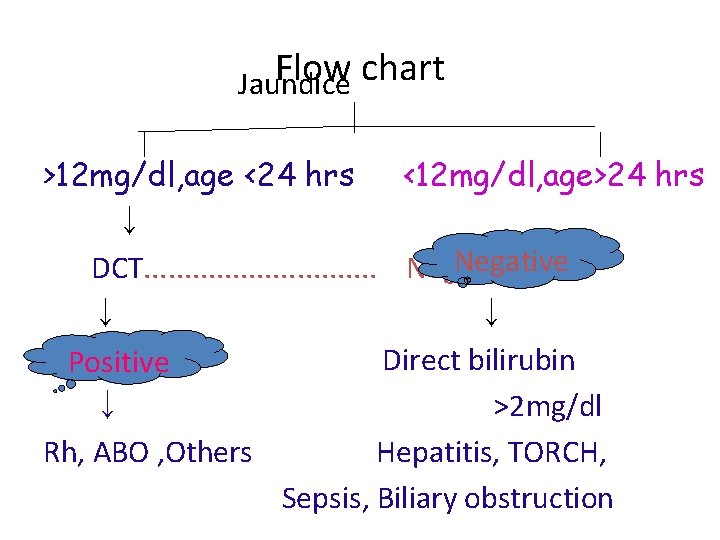
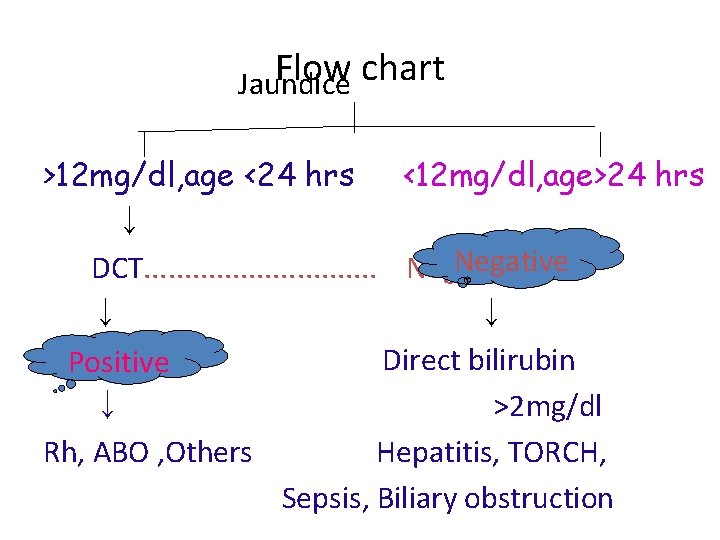
Flow chart Jaundice >12 mg/dl, age <24 hrs <12 mg/dl, age>24 hrs ↓ Negative DCT. . . . Negative ↓ ↓ Positive Direct bilirubin Positive ↓ >2 mg/dl Rh, ABO , Others Hepatitis, TORCH, Sepsis, Biliary obstruction
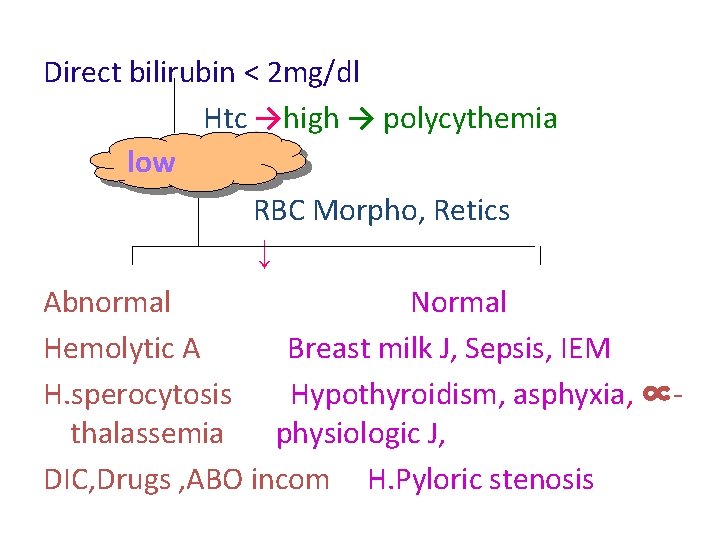
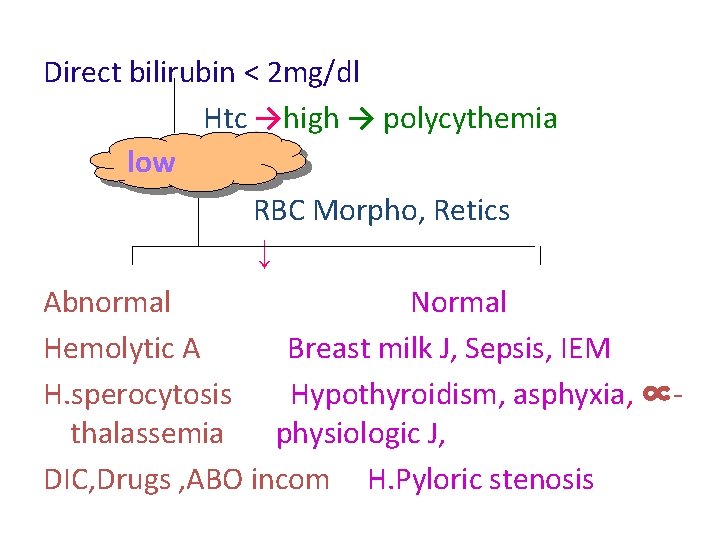
Direct bilirubin < 2 mg/dl Htc →high → polycythemia low RBC Morpho, Retics ↓ Abnormal Normal Hemolytic A Breast milk J, Sepsis, IEM H. sperocytosis Hypothyroidism, asphyxia, ∝thalassemia physiologic J, DIC, Drugs , ABO incom H. Pyloric stenosis
MANAGEMENT • Phototherapy • Drugs • Exchange transfusion
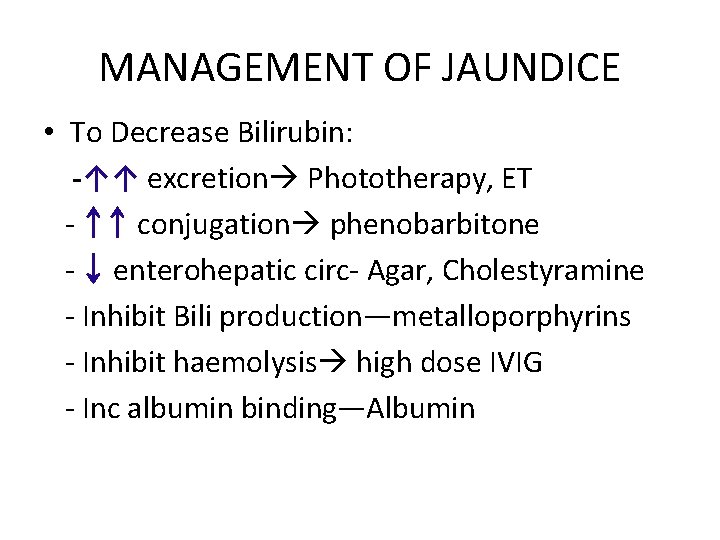
MANAGEMENT OF JAUNDICE • To Decrease Bilirubin: -↑↑ excretion Phototherapy, ET - ↑↑ conjugation phenobarbitone - ↓ enterohepatic circ- Agar, Cholestyramine - Inhibit Bili production—metalloporphyrins - Inhibit haemolysis high dose IVIG - Inc albumin binding—Albumin

PHOTOTHERAPY
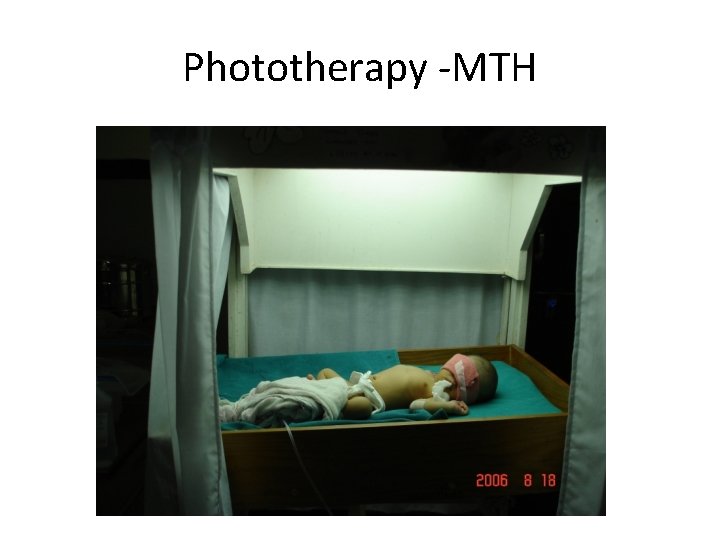
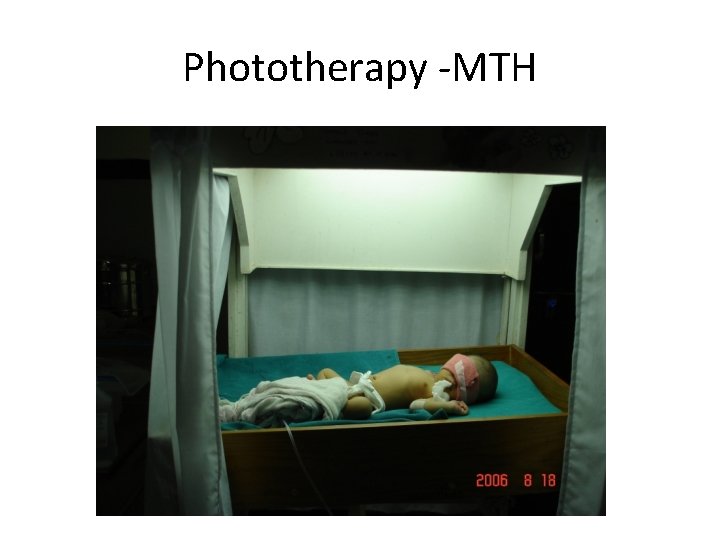
Phototherapy -MTH

Phototherapy -MTH


Phototherapy • Safe and effective method for treatment of neonatal jaundice • Bilirubin absorbs light maximum at 420 -460 nm
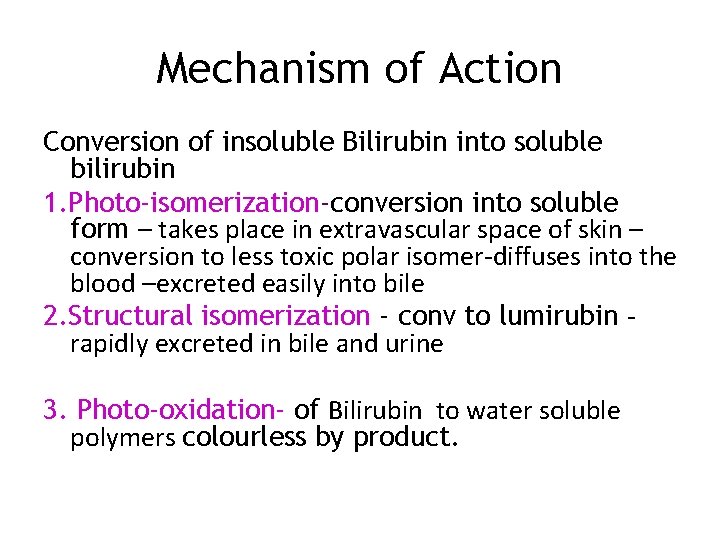
Mechanism of Action Conversion of insoluble Bilirubin into soluble bilirubin 1. Photo-isomerization-conversion into soluble form – takes place in extravascular space of skin – conversion to less toxic polar isomer-diffuses into the blood –excreted easily into bile 2. Structural isomerization - conv to lumirubin rapidly excreted in bile and urine 3. Photo-oxidation- of Bilirubin to water soluble polymers colourless by product.
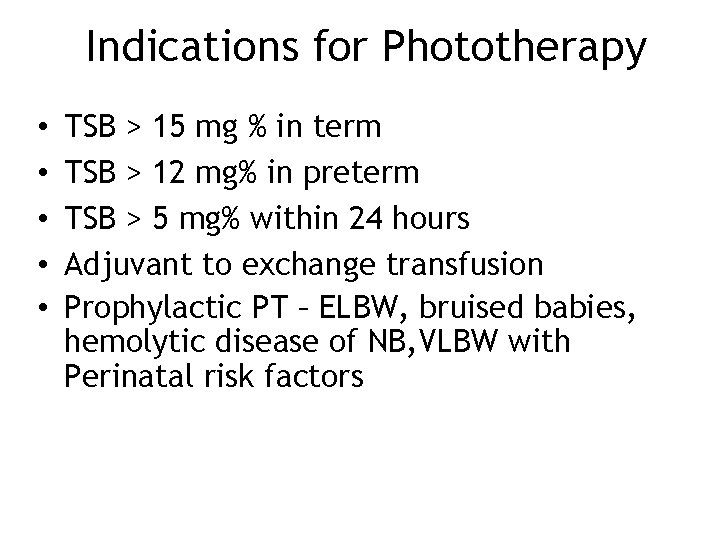
Indications for Phototherapy • • • TSB > 15 mg % in term TSB > 12 mg% in preterm TSB > 5 mg% within 24 hours Adjuvant to exchange transfusion Prophylactic PT – ELBW, bruised babies, hemolytic disease of NB, VLBW with Perinatal risk factors
Indications • Precautions – Cover the eyes and Genitals – Supplemental hydration – Watch for side effects

Procedure • Best is narrow spectral blue lights (425475 nm) • White lamps (380 -700 nm) • Distance from skin – 45 cm • Intensive PT – 15 -20 cm • Shield eyes & genitalia • Space of 5 -8 cm between phototherapy unit & incubator
• Double surface PT – can be given by fiber-optic blankets (biliblankets) • Change position once in every 2 -4 hrs • Skin bleached by PT • Level to be checked every 10 -20 hrs • Frequent temperature monitoring & daily weight check
Side Effects • Immediate – – Loose stools – Dehydration, – Hyperthermia, – ‘Bronze baby’ syndrome, – Rashes, – Upsets maternal infant interactions (bond)
• Late – – Risk of skin malignancies – Damage to intracellular DNA – Retinal damage – Disturbance in circadian rhythm Testicular damage

Home phototherapy Biliblanket or glow-worm ?
DRUGS • Phenobarbitone – increase y and z ligands -induces liver ezymes - ↑↑ conjugation phenobarbitone • Metalloporphyrins (tin and zinc porphyrins and meso prophyrins) -inhibits heme oxygenase
• IVIG - Inhibit haemolysis • Oral agar, Cholestyramine-↓ enterohepatic circ • Albumin infusions Inc albumin binding
• Exchange blood transfusion -- changing the babies blood with the other blood. • Usually in hemolytic disease of newborn. • It removes partially hemolysed antibody coated RBCs and also billirubin
Methods of exchange • Single volume exchange- 80 ml/kg • Double volume exchange- 160 ml/kg (87% of infant blood volume exchanged with new blood) • Triple volume exchange.
Partial exchange transfusion • • Polycythemia Chronic anemia with heart failure Hydrops fetalis. Observed pcv - desired pcv X 100 / observed pcv.
Exchange Transfusion Indications: • Rh and ABO incompatibility • Unconjugated billirubin > 20 -25 mg/dl in term, >15 -18 mg/dl preterm babies. Sick neonates exchange at lower level • Septicemia /DIC/ sclerema • Neonatal ITP • Severe anemia due to any cause with HF
Exchange Transfusion (Indications) • • Early Kernicterus Cong H Sperocytosis G-6 - PD deficiency Hepatic coma
In Hemolytic disease of the newborn (ABO / Rh) • • • H/O previous severely affected infant Cord Hb <10 gm% & bilirubin > 5 mg/dl Rate of rise of bilirubun > 0. 5 mg/100 ml/hr Jaundice in first 24 hrs of life Signs of hemolysis-clinical or lab Maternal ab titer > 1 in 64 Positive DCT Preterm LBW with hyperbilirubinemia Reticulocyte >10
Rh incompatibility • Due to Rh D-Ag • < 1 m. L of Rh-positive fetal blood is sufficient to sensitize the mother • 90% sensitization during delivery/abortion • So , most first born infants are not affected due to the short period of exposure which is insufficient to produce a significant maternal Ig G antibody response.
Rh incompatibility • Sensitized mother produces Ab –Ig. G types— crosses placenta • Once sensitized –small doses of Ag stimulate high Ab titer. • So, risk and severity of sensitization response increases with each subsequent pregnancy with Rh-positive blood fetus
ABO incompatibility • Mother is type O and the baby is either type A or B. • O +ve Mothers makes antibodies which are Ig. M & (Ig. G) types - Ig. G types crosses the placenta • No effects if the mother & baby have same blood group or baby is grp O, as there is nothing to make antibodies against.
ABO incompatibility • If mother - type A or B Makes antibodies (Ig. M) type so does not cross the placenta So, even if baby has a different blood type no effect
Selection of blood • Blood group O – no antigen Ab –anti -A, anti-B • Blood group A – antigen A Ab - Anti-B • Blood group B –antigen B Ab – anti -A
Blood for exchange transfusion • Fresh CPD blood • Rh HDN • ABO incompatibility -
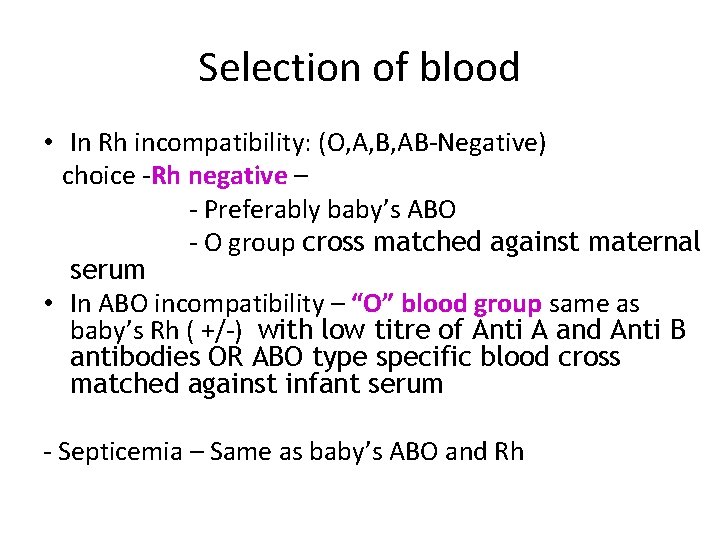
Selection of blood • In Rh incompatibility: (O, A, B, AB-Negative) choice -Rh negative – - Preferably baby’s ABO - O group cross matched against maternal serum • In ABO incompatibility – “O” blood group same as baby’s Rh ( +/-) with low titre of Anti A and Anti B antibodies OR ABO type specific blood cross matched against infant serum - Septicemia – Same as baby’s ABO and Rh
Investigations • Pre exchange: Hb%, PCV, billirubin, glucose K+, Ca+. • Post exchange: Hb%, PCV, billirubin, glucose, Calcium, K+, culture.
Procedure • IN NICU OR OT • Radiant warmer, Monitor HR, BP and other vitals, infants arms and legs are restrained. • Assistant to record volume in & out, to check vitals. • Blood pre warmed to 37 c • Dried umbilical cord soaked with wet gauze. • Canulation of umbilical vein- 12 o’clock
• Catheter inserted till free flow of blood or SHOULDER UMBILICAL LENGTH. • Small aliquots of blood removed 5 to 10 ml -PUSH PULL method. • Blood in the bag gently mixed. • Procedure over 1 to 2 hr. • Tie around the cord for 1 hr, or hold tightly at the end of procedure.
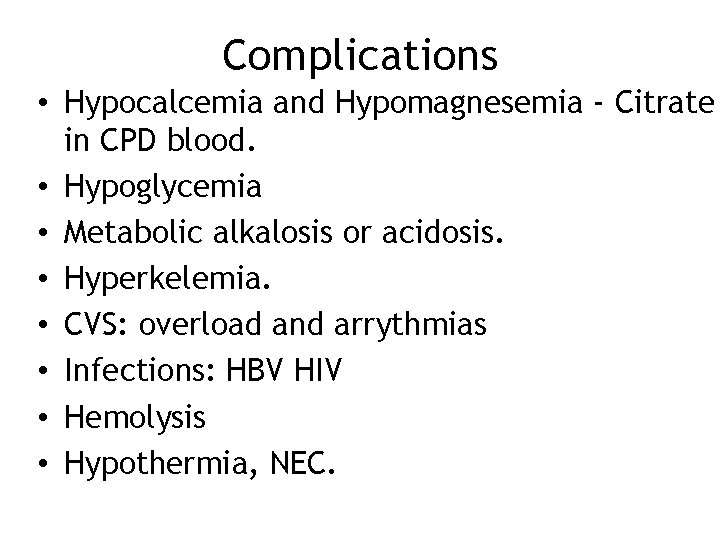
Complications • Hypocalcemia and Hypomagnesemia - Citrate in CPD blood. • Hypoglycemia • Metabolic alkalosis or acidosis. • Hyperkelemia. • CVS: overload and arrythmias • Infections: HBV HIV • Hemolysis • Hypothermia, NEC.
Other roots for exchange • Umbilical vein cut down- incision above umbilicus in midline. • Femoral vein canulation with radial artery canulation.
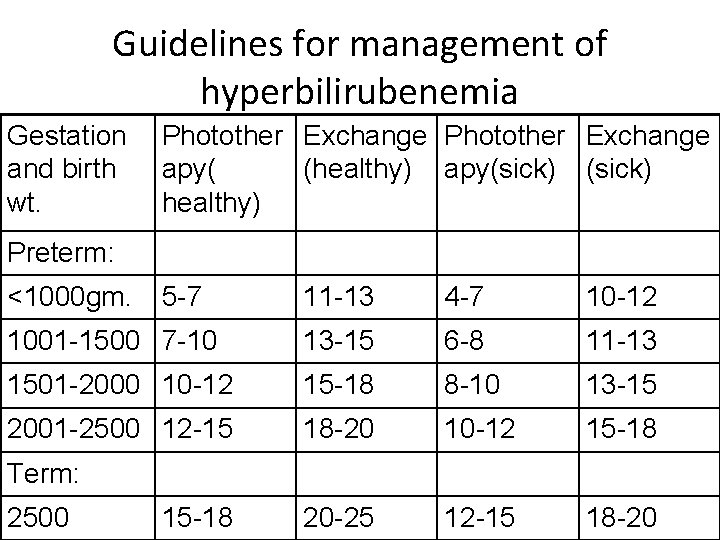
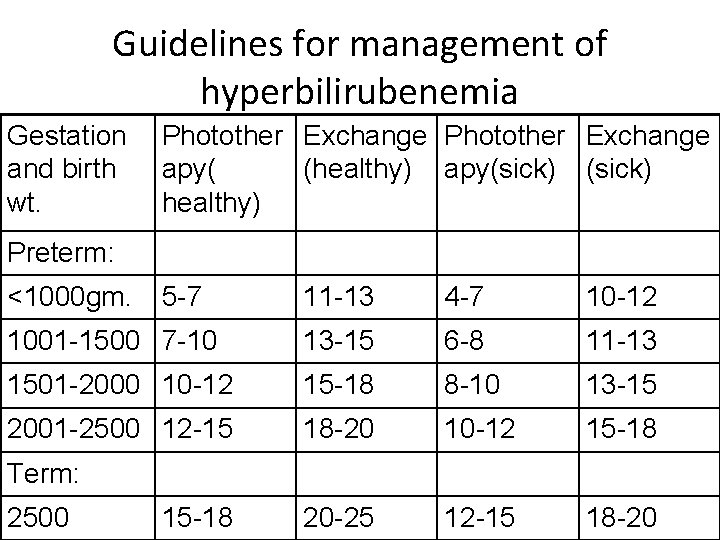
Guidelines for management of hyperbilirubenemia Gestation and birth wt. Photother Exchange apy( (healthy) apy(sick) healthy) Preterm: <1000 gm. 5 -7 11 -13 4 -7 10 -12 1001 -1500 7 -10 13 -15 6 -8 11 -13 1501 -2000 10 -12 15 -18 8 -10 13 -15 2001 -2500 12 -15 18 -20 10 -12 15 -18 20 -25 12 -15 18 -20 Term: 2500 15 -18
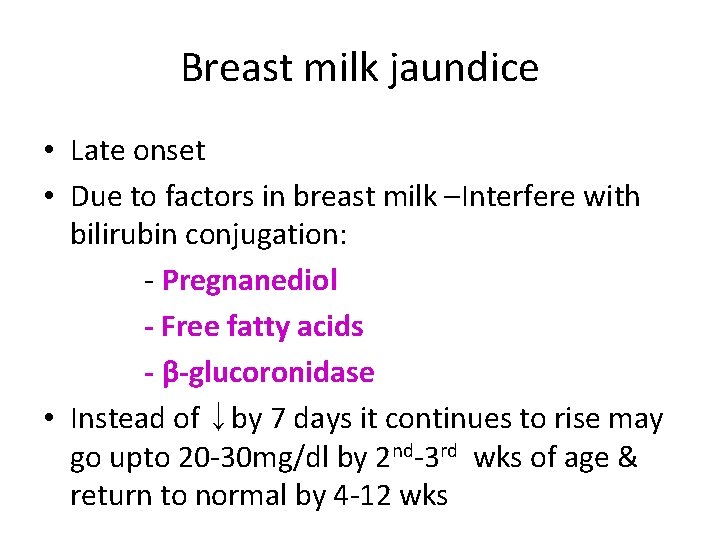
Breast milk jaundice • Late onset • Due to factors in breast milk –Interfere with bilirubin conjugation: - Pregnanediol - Free fatty acids - β-glucoronidase • Instead of ↓by 7 days it continues to rise may go upto 20 -30 mg/dl by 2 nd-3 rd wks of age & return to normal by 4 -12 wks
Management • Stop breast feeding -48 hrs • Again resume it, bilirubin may rise again but not reach previous high level
Breast feeding jaundice • Decreased intake of milk leads to increased enterohepatic circulation • Higher levels on day 4 compared to formula fed babies due decreased intake of milk
Prevention 1. Anti D to be given to the mother after delivery of the baby-within 48 hrs. Also can be given to all unsensitized mothers at 28 -32 weeks of gestation 2. Amniocentesis and IU transfusion to severely affected babies 3. Preterm delivery of severely affected babies 4. Cord blood studies-followed by Phototherapy 5. Exchange transfusion
KERNICTERUS • Entry of unbound bilirubin into brain as free or albumin bound bilirubin • Acidosis affects bilirubin solubility • Hyperosmolarity, anoxia and hypercarbia disrupt BBB
• Yellow staining of brain assc with neuronal injury • Affects basal ganglia, cranial nerve nuclei, brain stem nuclei, hippocampus and AHC of spinal cord (cortex usually spared) • Necrosis, neuronal loss and gliosis …pathological findings
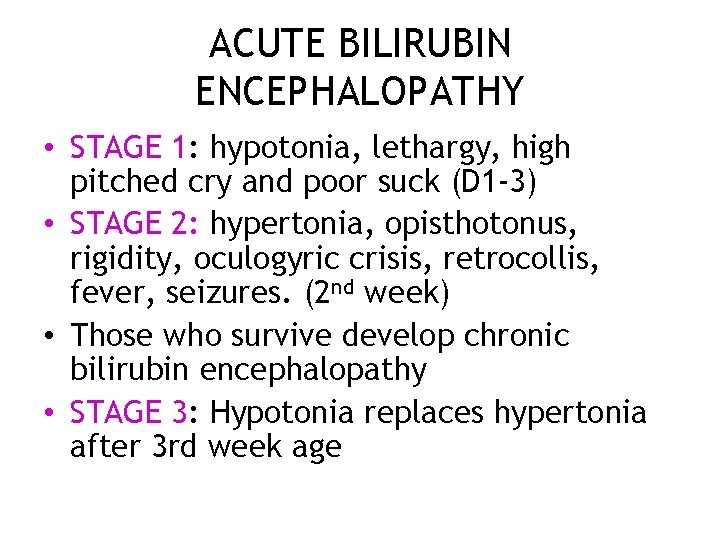
ACUTE BILIRUBIN ENCEPHALOPATHY • STAGE 1: hypotonia, lethargy, high pitched cry and poor suck (D 1 -3) • STAGE 2: hypertonia, opisthotonus, rigidity, oculogyric crisis, retrocollis, fever, seizures. (2 nd week) • Those who survive develop chronic bilirubin encephalopathy • STAGE 3: Hypotonia replaces hypertonia after 3 rd week age
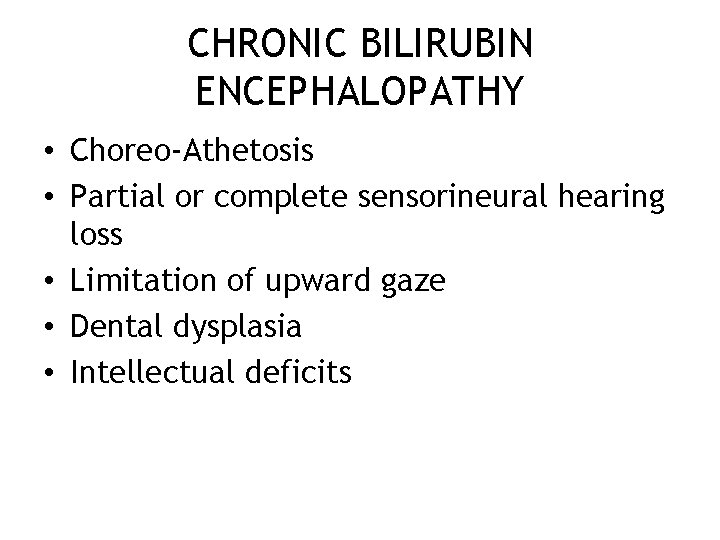
CHRONIC BILIRUBIN ENCEPHALOPATHY • Choreo-Athetosis • Partial or complete sensorineural hearing loss • Limitation of upward gaze • Dental dysplasia • Intellectual deficits
LOW BILIRUBIN KERNICTERUS • • In LBW babies, preterms Overt changes not seen Other factors: IVH, drugs, benzyl alcohol More likely to suffer from anoxia, hypercarbia and sepsis
TREATMENT • • • Phototherapy Exchange transfusion Albumin infusion Anticonvulsants: phenobarbitone BERA at follow up
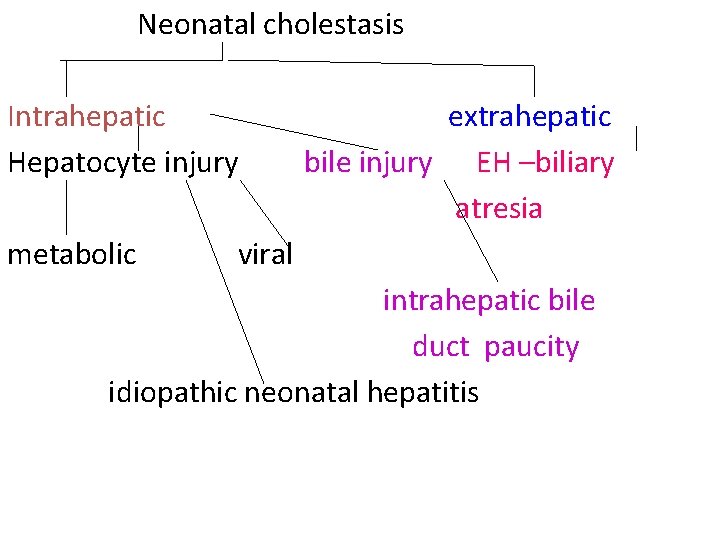
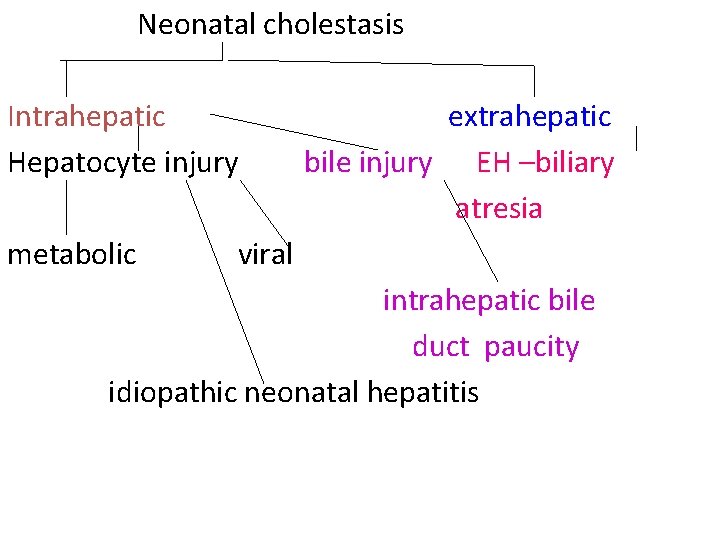
Neonatal cholestasis Intrahepatic Hepatocyte injury metabolic extrahepatic bile injury EH –biliary atresia viral intrahepatic bile duct paucity idiopathic neonatal hepatitis
Thank you Download more documents and slide shows on The Medical Post [ www. themedicalpost. net ]
 Nec diagnosis
Nec diagnosis Classification of jaundice
Classification of jaundice Jaundice physical examination
Jaundice physical examination Phototherapy machine working principle
Phototherapy machine working principle Neonatal jaundice
Neonatal jaundice Nursing diagnosis for neonatal jaundice
Nursing diagnosis for neonatal jaundice Clinical manifestation of hepatitis
Clinical manifestation of hepatitis Dd jaundice
Dd jaundice Kalpana satellite images
Kalpana satellite images Kalpana rajgopalan
Kalpana rajgopalan Kalpana had encyclopaedic knowledge means
Kalpana had encyclopaedic knowledge means Manipal university bhubaneswar
Manipal university bhubaneswar Manipal university
Manipal university Manipal university chemistry department
Manipal university chemistry department Ezproxy manipal
Ezproxy manipal Malla curricular inicial
Malla curricular inicial Malla
Malla Malla curricular preescolar 2012
Malla curricular preescolar 2012 Malla bestur
Malla bestur Malla curricular contaduria publica ucr
Malla curricular contaduria publica ucr Institut torre de malla
Institut torre de malla Malla receptora de información design thinking
Malla receptora de información design thinking Malla curricular preescolar 2012
Malla curricular preescolar 2012 Malla bestur
Malla bestur Nodo circuitos
Nodo circuitos Ins torre de malla gestin
Ins torre de malla gestin Malla receptora
Malla receptora Malla rantanen
Malla rantanen Malla circuito
Malla circuito Ins torre de malla gestin
Ins torre de malla gestin Modern concept of child care ppt
Modern concept of child care ppt Vital signs normal range for pediatrics
Vital signs normal range for pediatrics Nn pediatrics
Nn pediatrics Vital sign ped
Vital sign ped Randall neustaedter
Randall neustaedter Im injection sites and volumes pediatrics
Im injection sites and volumes pediatrics 11yo
11yo Normal vital signs for adults
Normal vital signs for adults Nelson pediatria
Nelson pediatria Himalaya vigorcare benefits
Himalaya vigorcare benefits Nbme shelf percentiles 2021
Nbme shelf percentiles 2021 Abdominal restraint procedure
Abdominal restraint procedure Mummy restraint in pediatrics
Mummy restraint in pediatrics River valley pediatrics
River valley pediatrics Vancouver clinic pediatrics
Vancouver clinic pediatrics New trends in pediatric nursing
New trends in pediatric nursing N-pass pain scale
N-pass pain scale Introduction to pediatrics
Introduction to pediatrics Nelson pediatrics
Nelson pediatrics Nelson pediatrics
Nelson pediatrics Chest pain in pediatrics
Chest pain in pediatrics What is a buretrol
What is a buretrol Carrie tingley pediatrics
Carrie tingley pediatrics Warm chain in pediatrics
Warm chain in pediatrics Equipment used in pediatrics
Equipment used in pediatrics Duke pediatrics durham nc
Duke pediatrics durham nc Trends in pediatric nursing
Trends in pediatric nursing Normal vital signs of newborn
Normal vital signs of newborn Tlc pediatrics flint
Tlc pediatrics flint Combivent syrup
Combivent syrup Practical approach pediatrics
Practical approach pediatrics Bristol pediatrics
Bristol pediatrics Stabbing pain in chest
Stabbing pain in chest Xxx
Xxx Lsuhsc pediatrics
Lsuhsc pediatrics Organization of neonatal unit
Organization of neonatal unit Halo de oxigeno
Halo de oxigeno Newborn reflexes
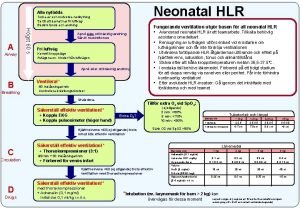
Newborn reflexes Neonatal hlr
Neonatal hlr Tamiz neonatal
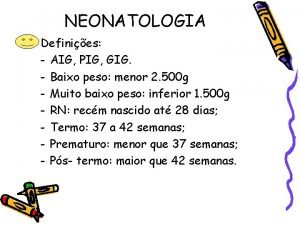
Tamiz neonatal Aig neonatologia
Aig neonatologia Neonatal liver failure
Neonatal liver failure Neonatal sepsis
Neonatal sepsis Hipoglicemia neonatal sequelas
Hipoglicemia neonatal sequelas Poliglobulia
Poliglobulia Neonatal energy triangle
Neonatal energy triangle Sepsis neonatal temprana y tardía
Sepsis neonatal temprana y tardía Neonatal progeria
Neonatal progeria Hepatocytolyse
Hepatocytolyse Lenticuloestriado
Lenticuloestriado Grading murmurs
Grading murmurs Curva bilirrubina fototerapia
Curva bilirrubina fototerapia