INTERSTITIAL LUNG DISEASE SARCOIDOSIS Dr Ishraq Elshamli Respiratory



- Slides: 84
INTERSTITIAL LUNG DISEASE & SARCOIDOSIS Dr. Ishraq Elshamli Respiratory Unit Tripoli Medical Center
What is interstitial lung disease : Accounts for : n 15% of the cases seen by pulmonologists. n Includes more than 130 disorders Similar symptoms, signs, radiological changes and pulmonary function tests. 9/12/2021 2
Different Causes and Pathological process Involving interstitial alveolar structures thus Therapy and Prognosis 9/12/2021 3
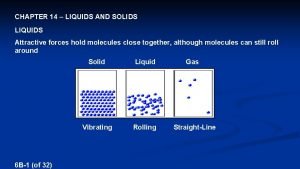
Interstitial Lung Diseases are Characterized by : n Abnormal accumulation of inflammatory cells and/or non cellular material (exudate) within the walls of the alveoli of the lungs results in Thickening and stiffness of the normally elastic tissues of the lung, ( stiff lung) 1. 9/12/2021 4
2. Loss of normal alveolar capillary gas exchange ( Ventilation / Perfusion mismatch) Interferes with normal breathing DYSPNEA 9/12/2021 5
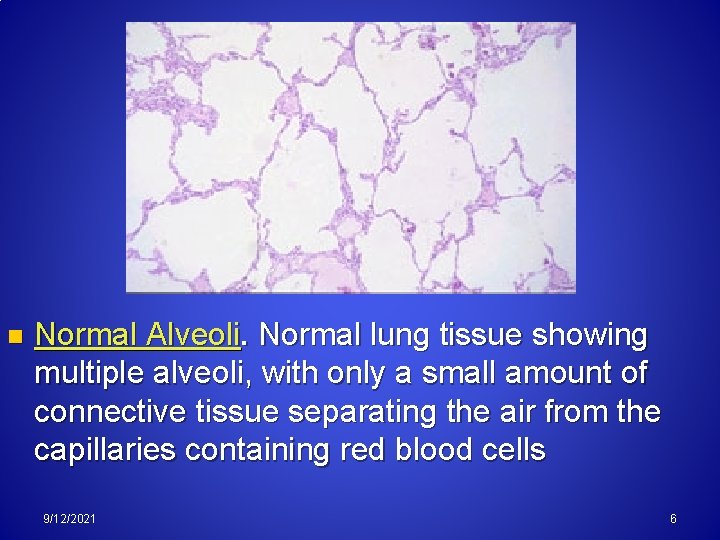
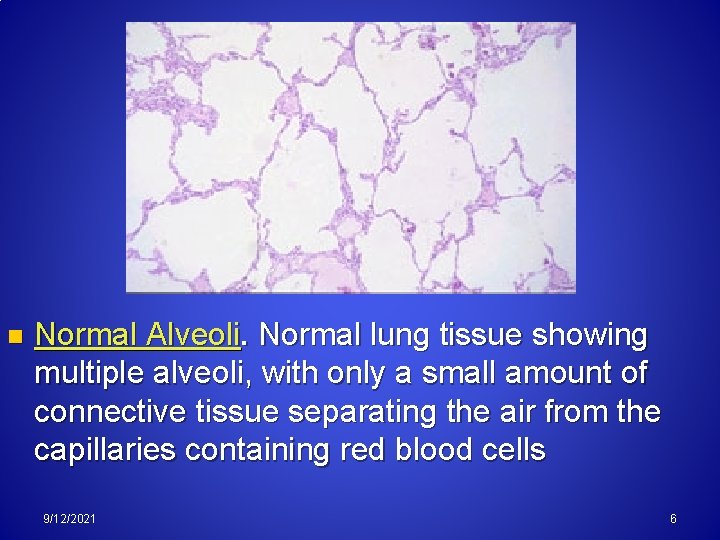
n Normal Alveoli. Normal lung tissue showing multiple alveoli, with only a small amount of connective tissue separating the air from the capillaries containing red blood cells 9/12/2021 6
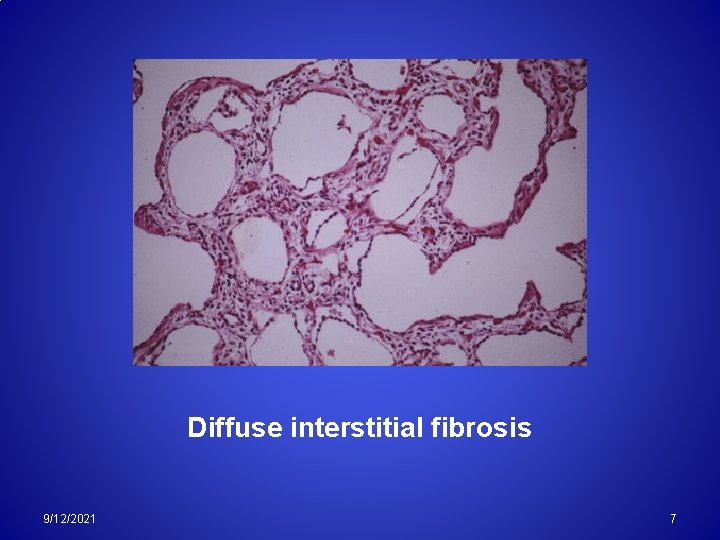
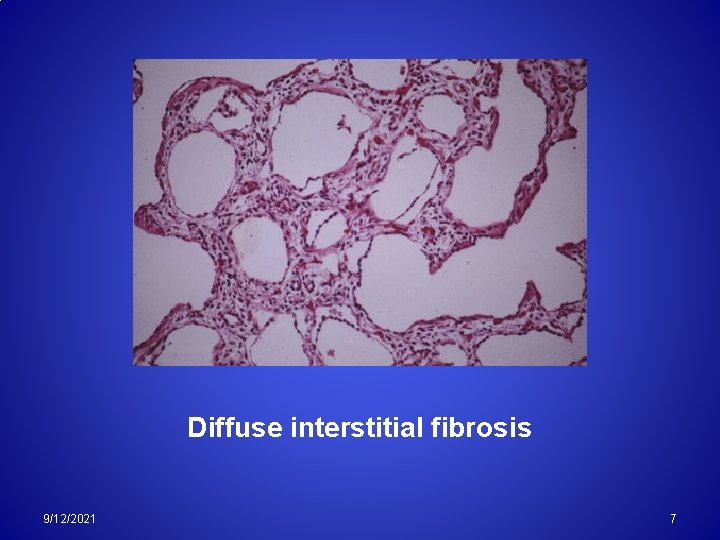
Diffuse interstitial fibrosis 9/12/2021 7
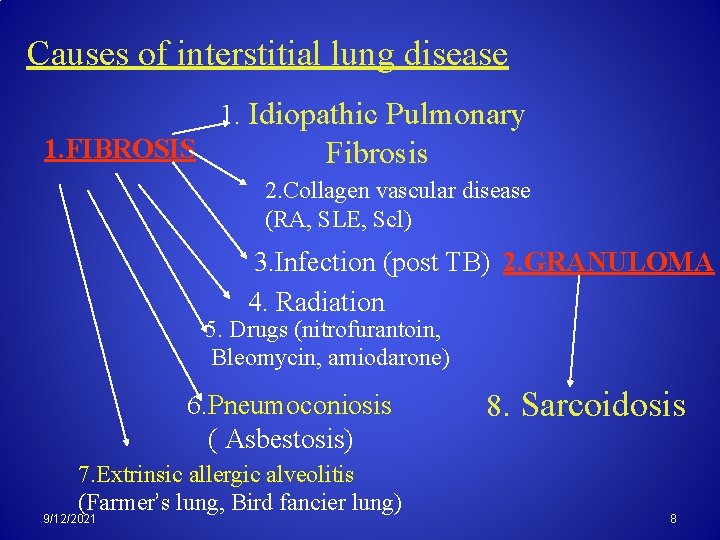
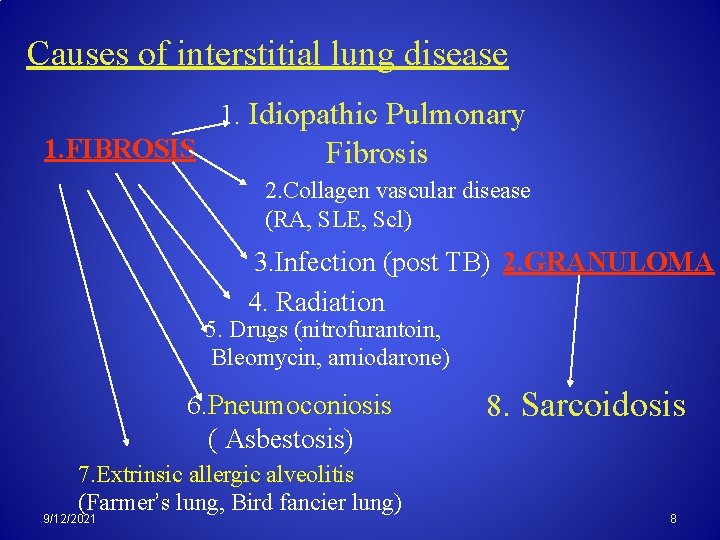
Causes of interstitial lung disease 1. Idiopathic Pulmonary 1. FIBROSIS Fibrosis 2. Collagen vascular disease (RA, SLE, Scl) 3. Infection (post TB) 2. GRANULOMA 4. Radiation 5. Drugs (nitrofurantoin, Bleomycin, amiodarone) 6. Pneumoconiosis ( Asbestosis) 7. Extrinsic allergic alveolitis (Farmer’s lung, Bird fancier lung) 9/12/2021 8. Sarcoidosis 8

3. Unclassified diseases may include: 1. Pulmonary histiocytosis X 2. LAM. 3. Pulmonary vasculitis. 4. Alveolar proteinosis. 5. Eosinophilic pneumonia. 6. BOOP. 9/12/2021 9
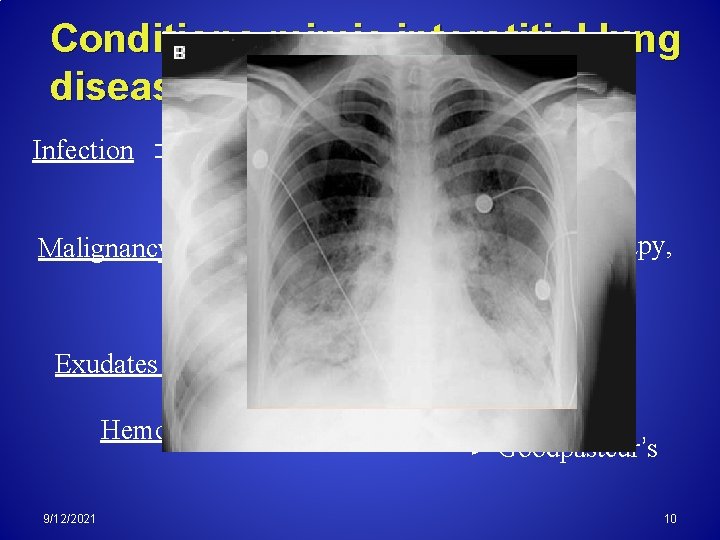
Conditions mimic interstitial lung disease Viral Pneumonia Pneumocystis Pneumonia Infection Malignancy Leukemia, Lymphoma, Radiotherapy, Lymphangitis carcinomatosa Exudates (Edema) Hemorrhage 9/12/2021 ARDS Goodpasteur’s 10
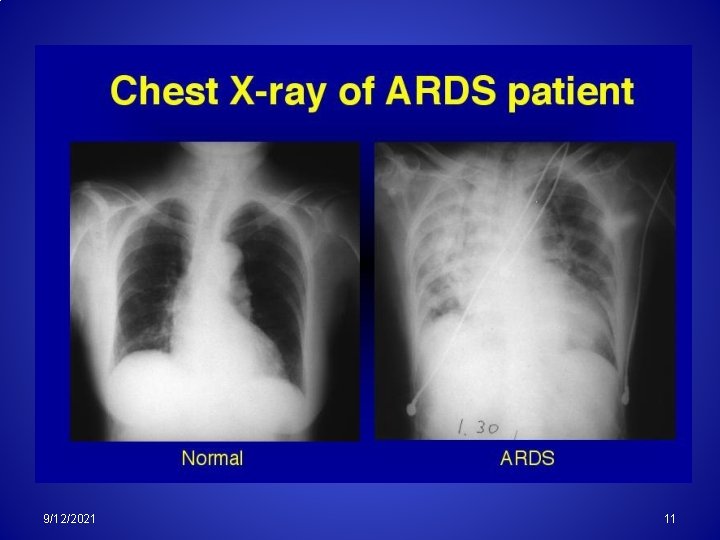
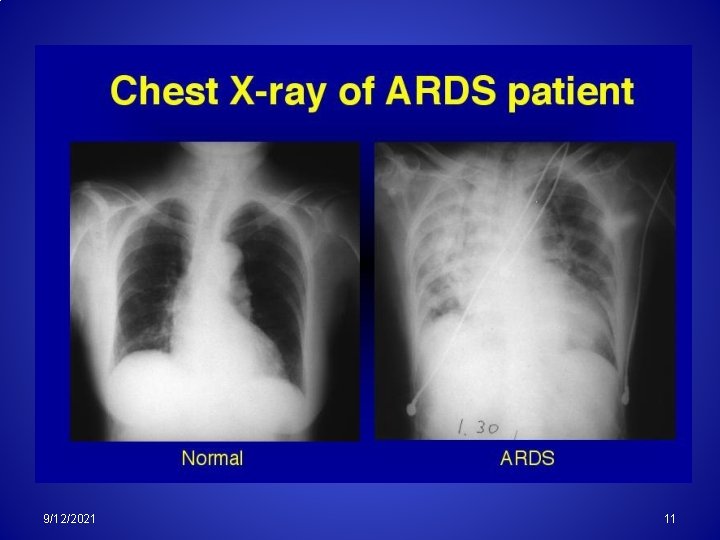
9/12/2021 11
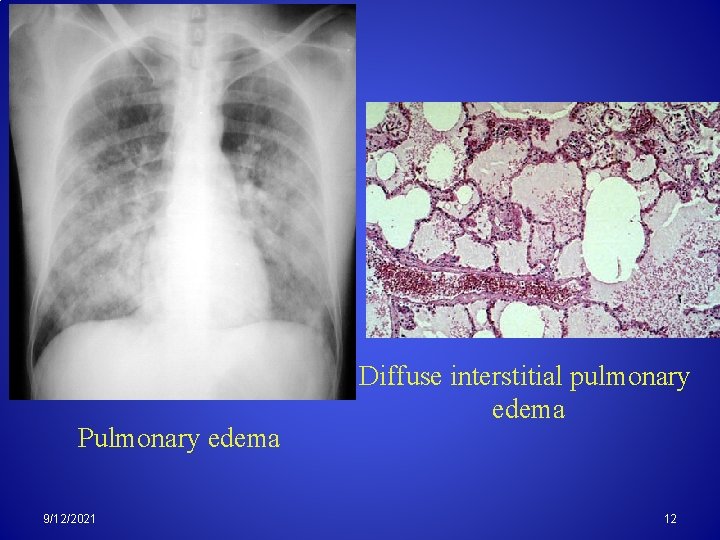
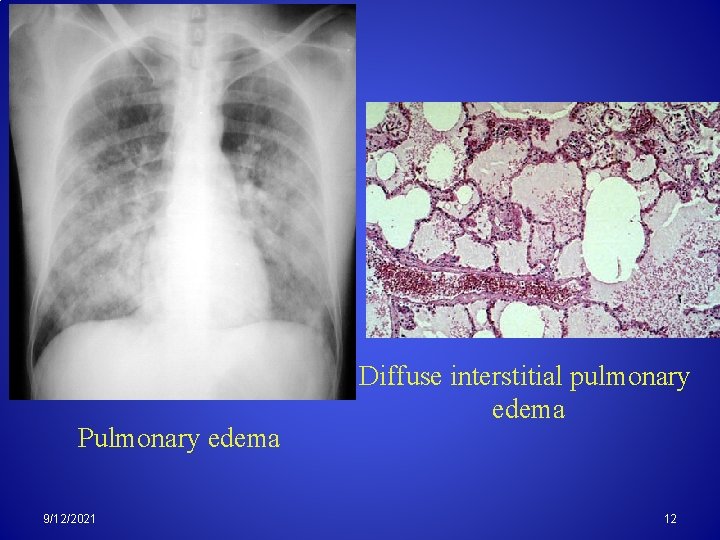
Pulmonary edema 9/12/2021 Diffuse interstitial pulmonary edema 12
The variable underlying etiology imply different therapy and prognosis 9/12/2021 13
Idiopathic pulmonary fibrosis (Cryptogenic Fibrosing Alveolitis)
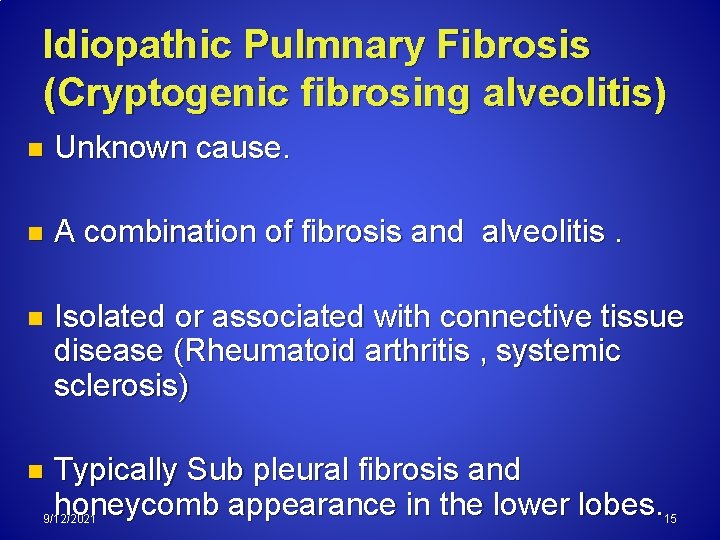
Idiopathic Pulmnary Fibrosis (Cryptogenic fibrosing alveolitis) n Unknown cause. n A combination of fibrosis and alveolitis. n Isolated or associated with connective tissue disease (Rheumatoid arthritis , systemic sclerosis) n Typically Sub pleural fibrosis and honeycomb appearance in the lower lobes. 9/12/2021 15
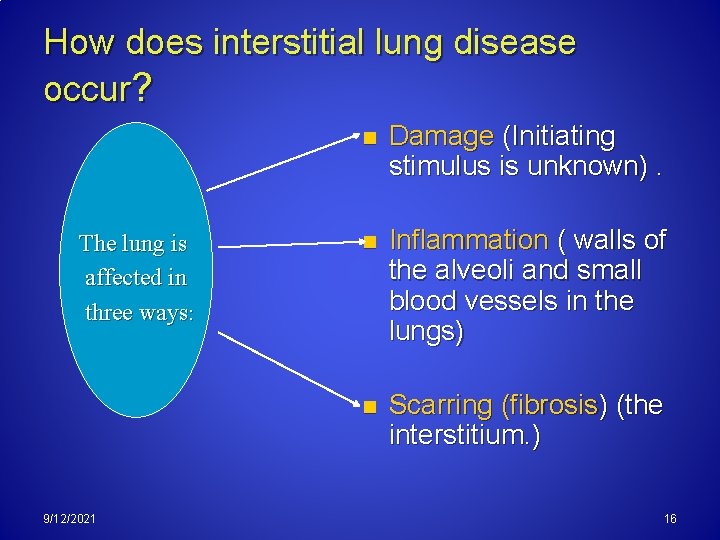
How does interstitial lung disease occur? The lung is affected in three ways: 9/12/2021 n Damage (Initiating stimulus is unknown). n Inflammation ( walls of the alveoli and small blood vessels in the lungs) n Scarring (fibrosis) (the interstitium. ) 16
Inflammation and scarring of the interstitium disrupts this tissue and leads to a decrease in the ability of the lungs to extract oxygen from the air.
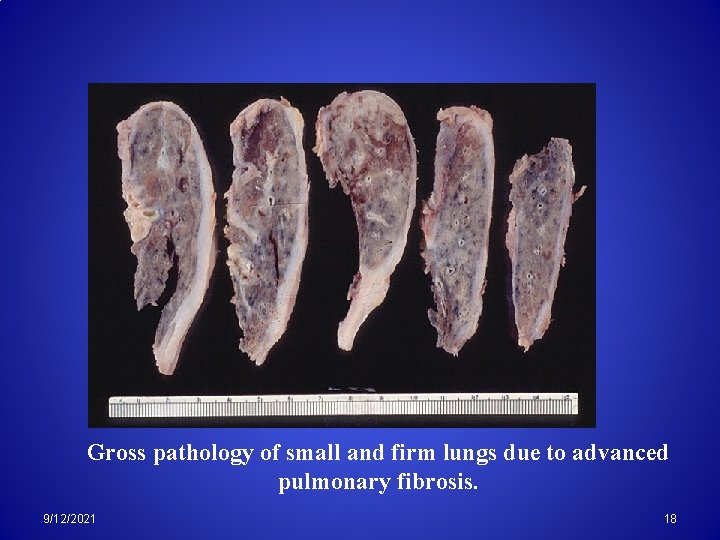
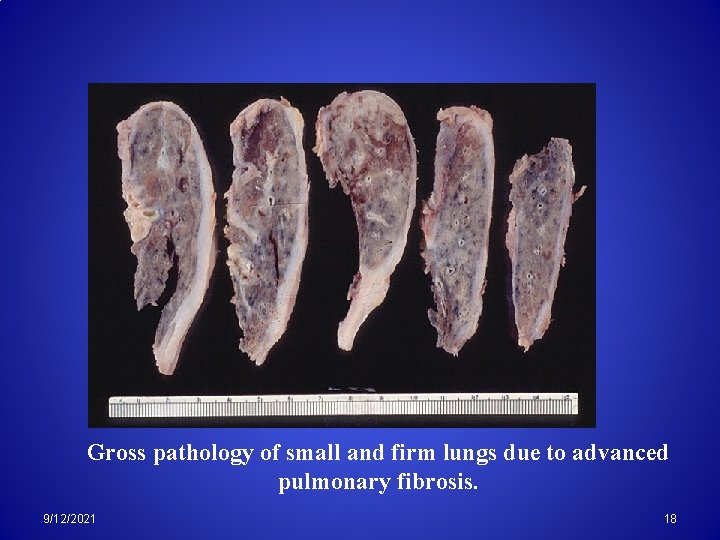
Gross pathology of small and firm lungs due to advanced pulmonary fibrosis. 9/12/2021 18
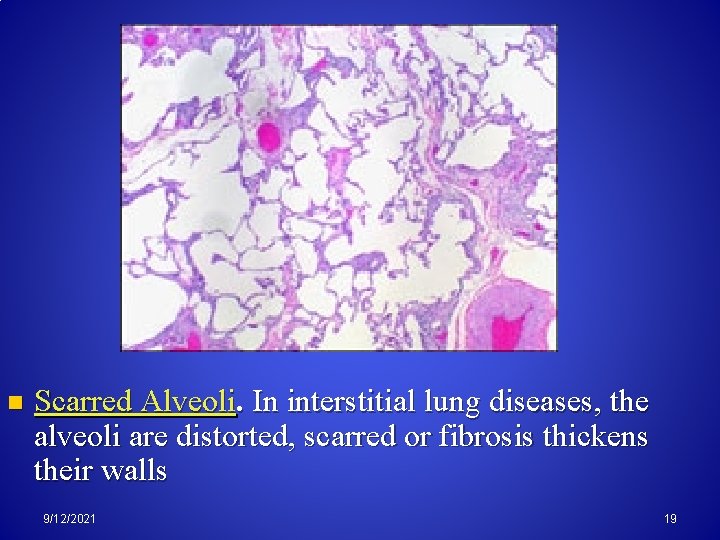
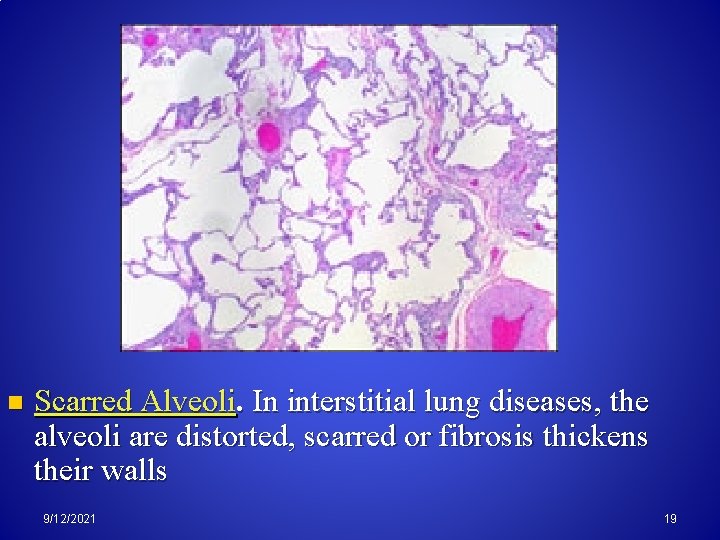
n Scarred Alveoli. In interstitial lung diseases, the alveoli are distorted, scarred or fibrosis thickens their walls 9/12/2021 19
The course of ILDs is unpredictable n The diseases may run a gradual or rapid course. n Varied symptoms from very mild to moderate to very severe. n The condition may remain the same for long periods of time or it may change quickly. 9/12/2021 20
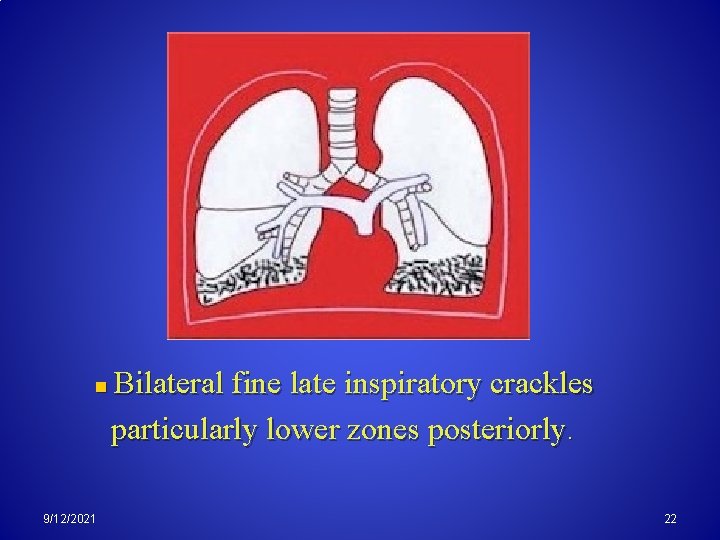
Clinical Features: Predominently a disease of the elderly >60 ys. n Progressive exertional dyspnea. n Dry cough, and digital clubbing. n Poor chest expansion, with bilateral end inspiratory crackles particularly lower zones posteriorly. n 9/12/2021 21
n 9/12/2021 Bilateral fine late inspiratory crackles particularly lower zones posteriorly. 22

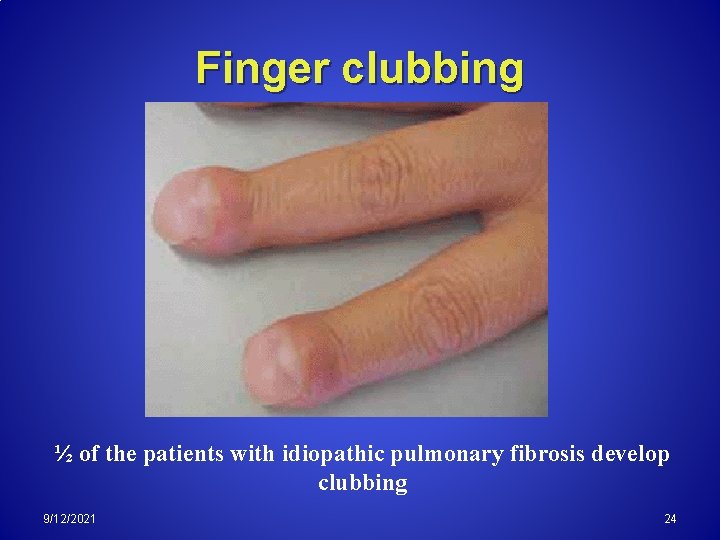
Central cyanosis and digital clubbing 9/12/2021 23
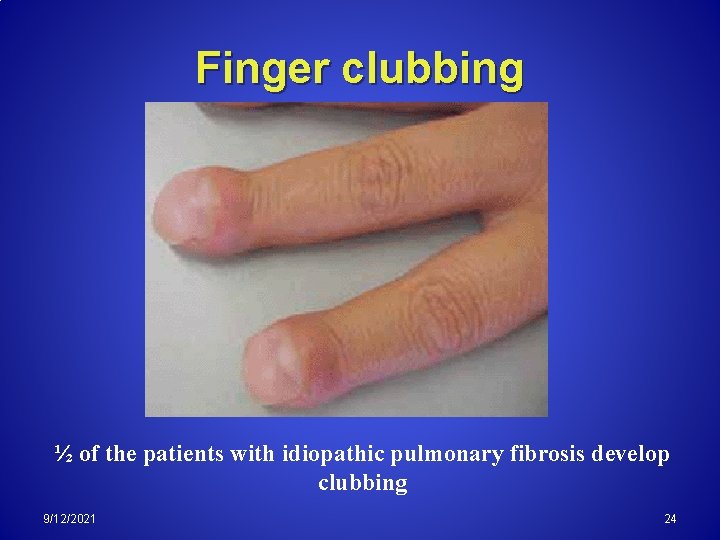
Finger clubbing ½ of the patients with idiopathic pulmonary fibrosis develop clubbing 9/12/2021 24
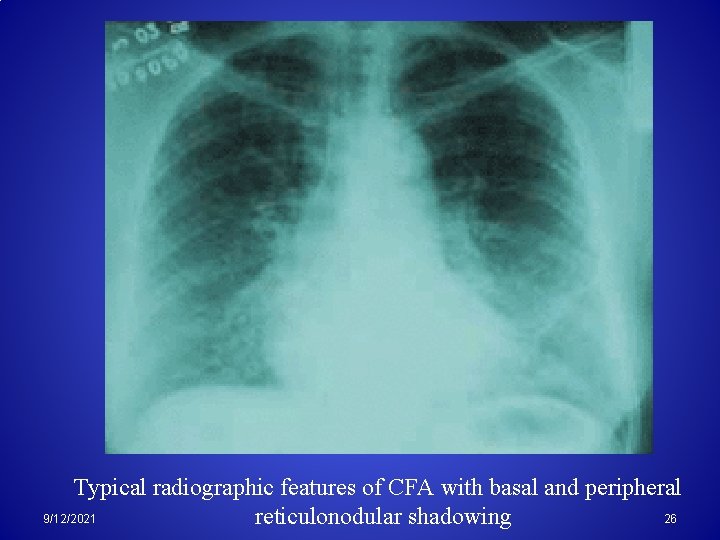
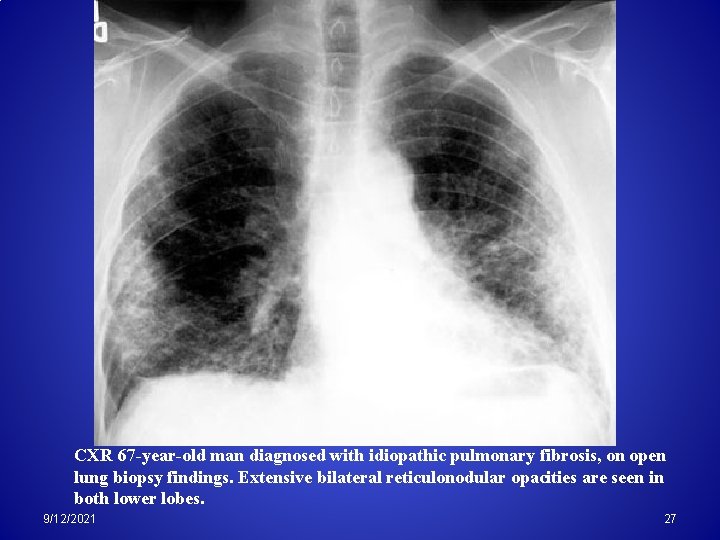
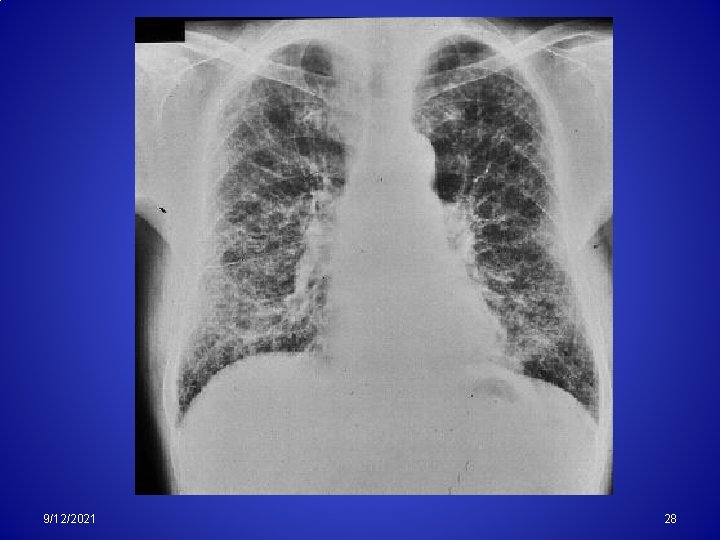
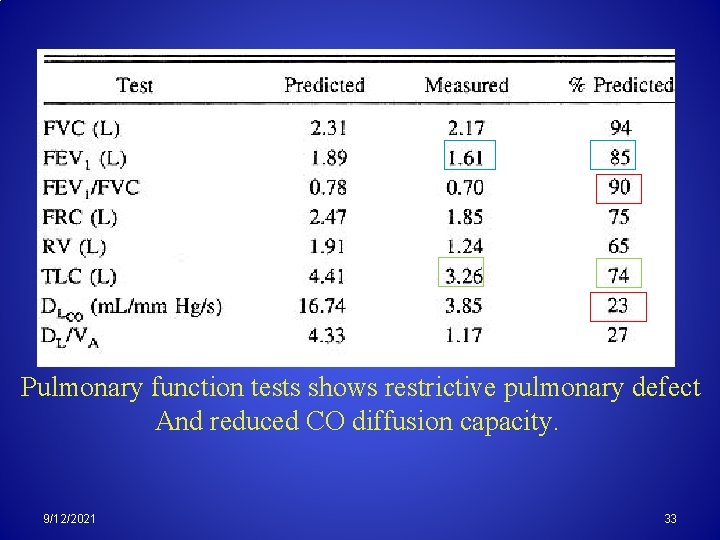
Investigations Rheumatoid factor and ANA (+)ive in 30 50% of cases. n ESR is n Chest X ray shows diffuse lower zone opacities, Honeycomb appearance in advanced lung disease. n Pulmonary function tests shows restrictive pulmonary defect. n 9/12/2021 25
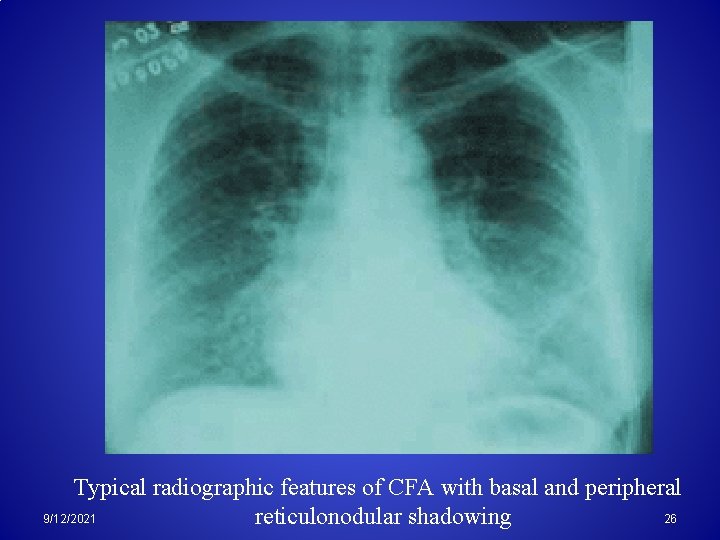
Typical radiographic features of CFA with basal and peripheral 26 9/12/2021 reticulonodular shadowing
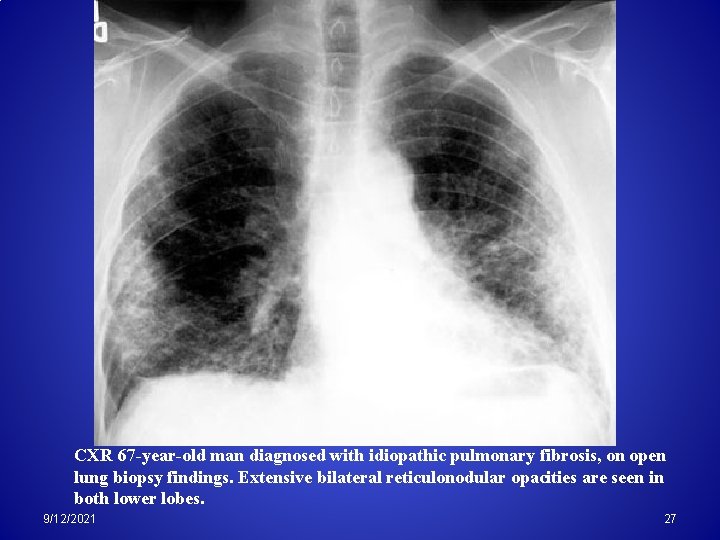
CXR 67 -year-old man diagnosed with idiopathic pulmonary fibrosis, on open lung biopsy findings. Extensive bilateral reticulonodular opacities are seen in both lower lobes. 9/12/2021 27
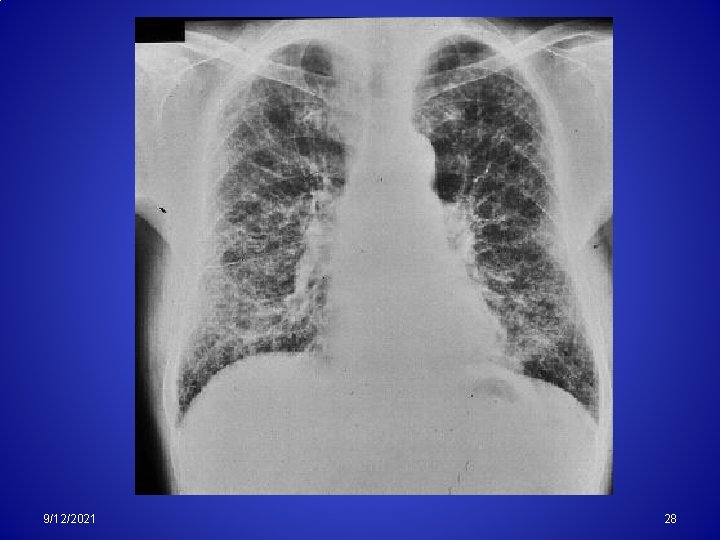
9/12/2021 28
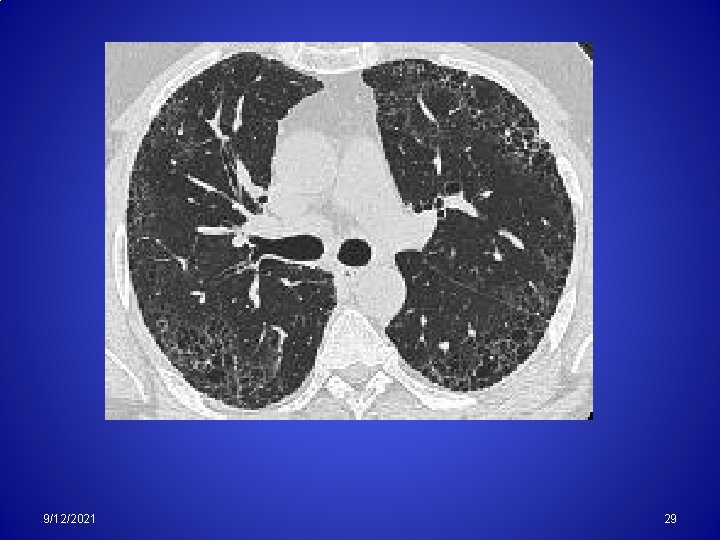
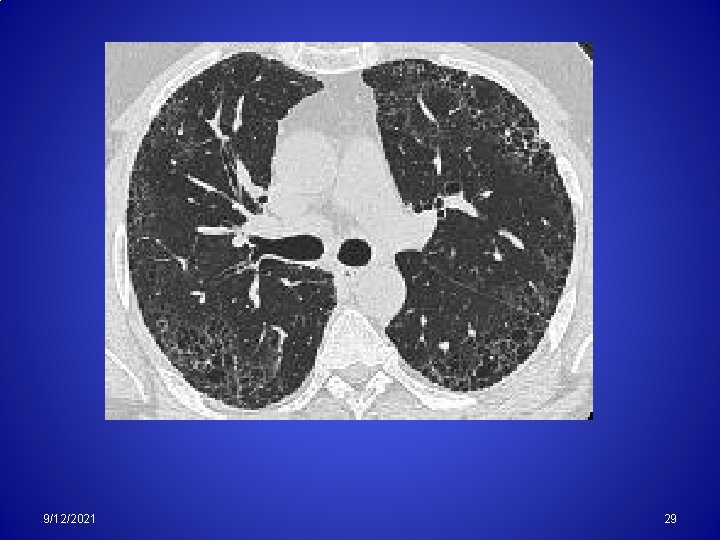
9/12/2021 29
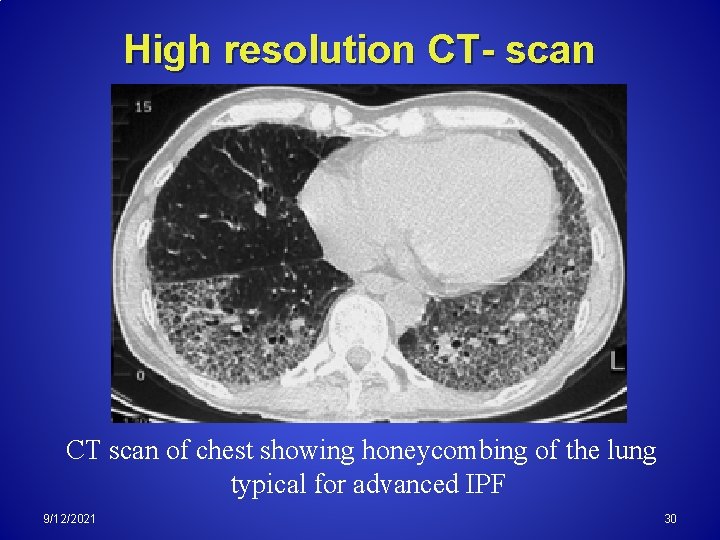
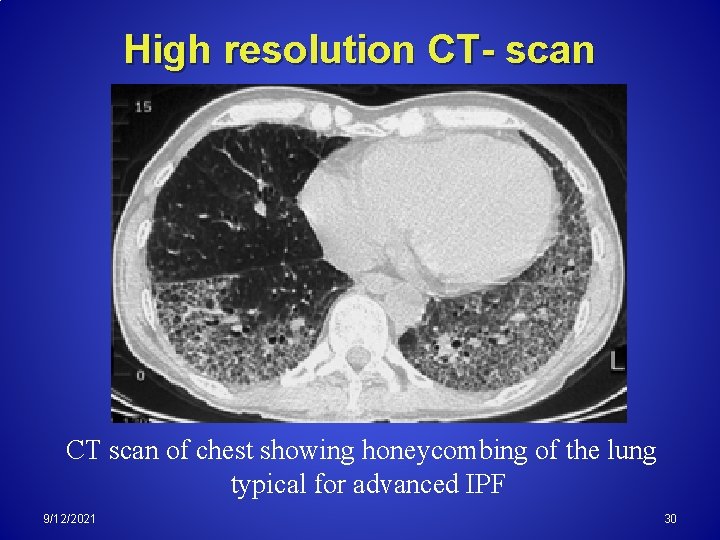
High resolution CT- scan CT scan of chest showing honeycombing of the lung typical for advanced IPF 9/12/2021 30
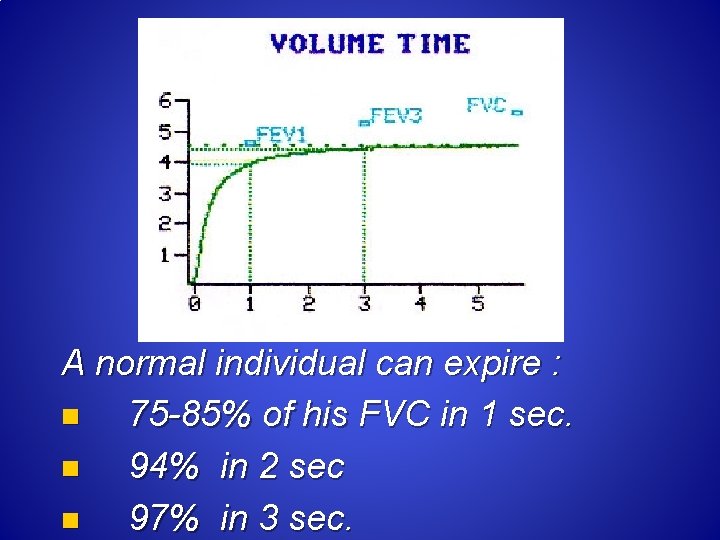
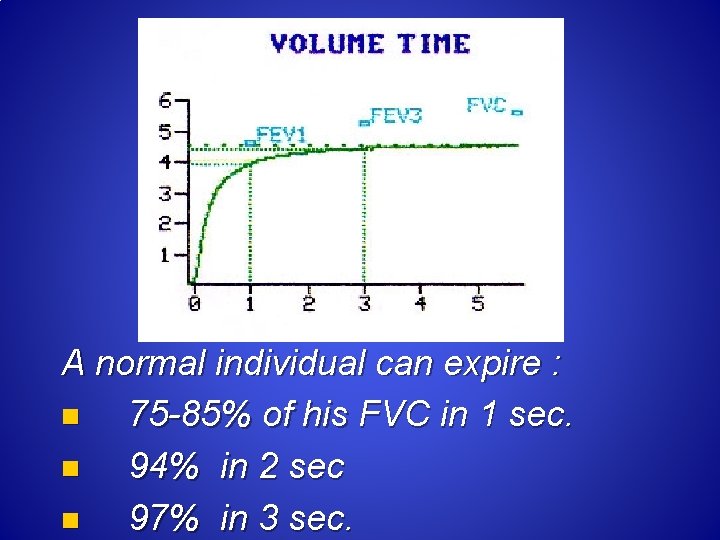
A normal individual can expire : n 75 -85% of his FVC in 1 sec. n 94% in 2 sec n 97% in 3 sec.
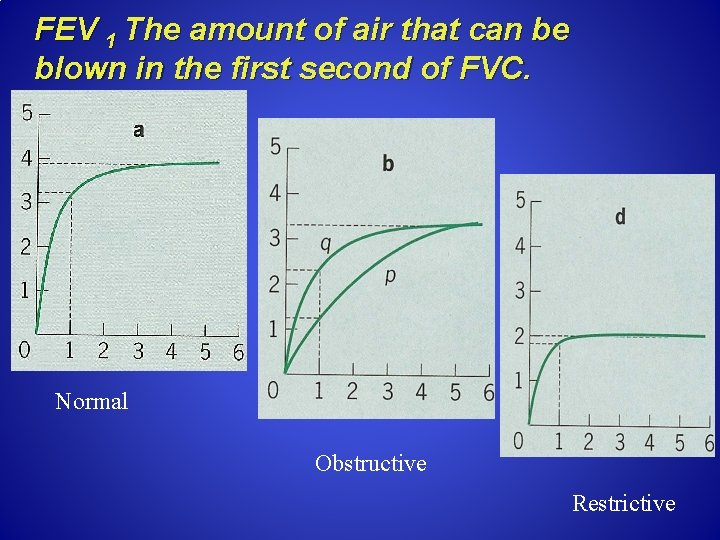
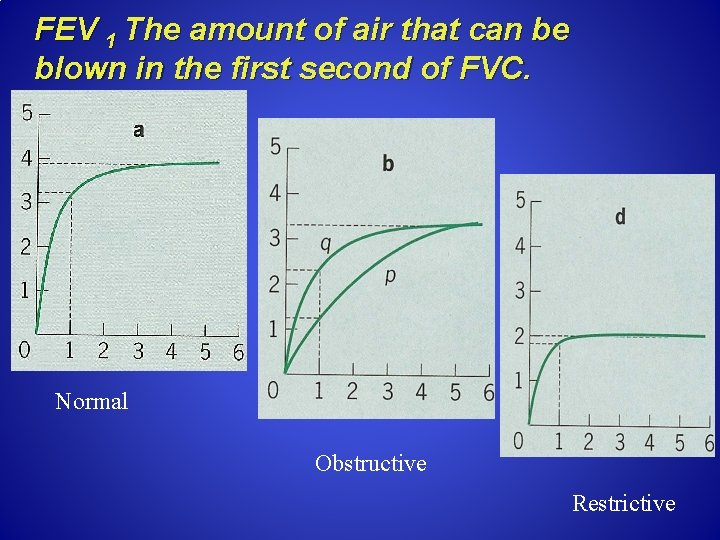
FEV 1 The amount of air that can be blown in the first second of FVC. Normal Obstructive Restrictive
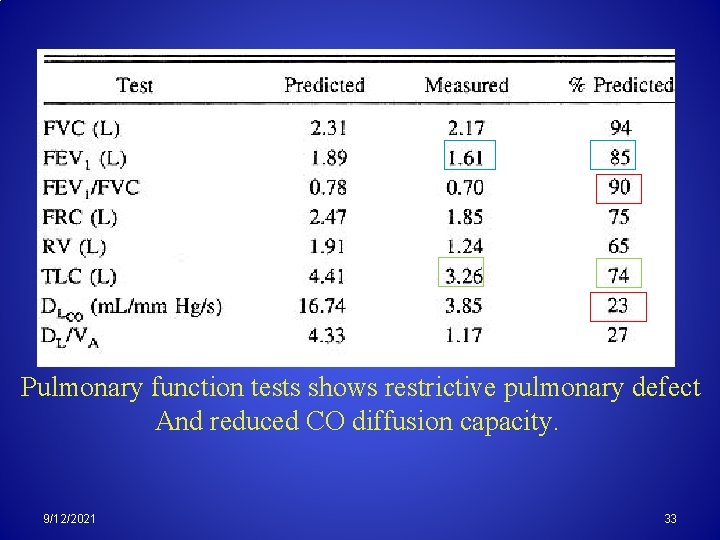
Pulmonary function tests shows restrictive pulmonary defect And reduced CO diffusion capacity. 9/12/2021 33
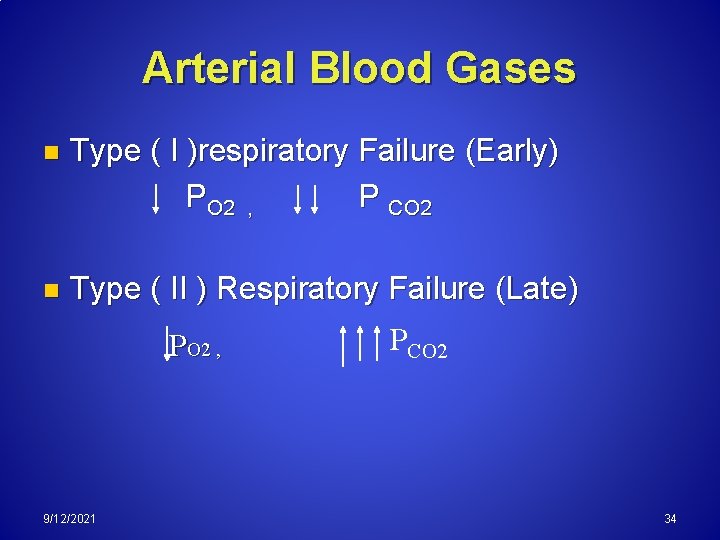
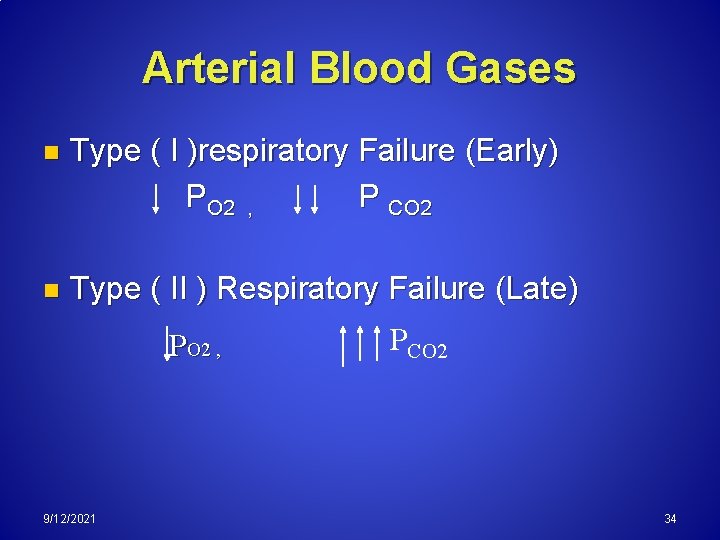
Arterial Blood Gases n Type ( I )respiratory Failure (Early) PO 2 , P CO 2 n Type ( II ) Respiratory Failure (Late) PO 2 , 9/12/2021 PCO 2 34
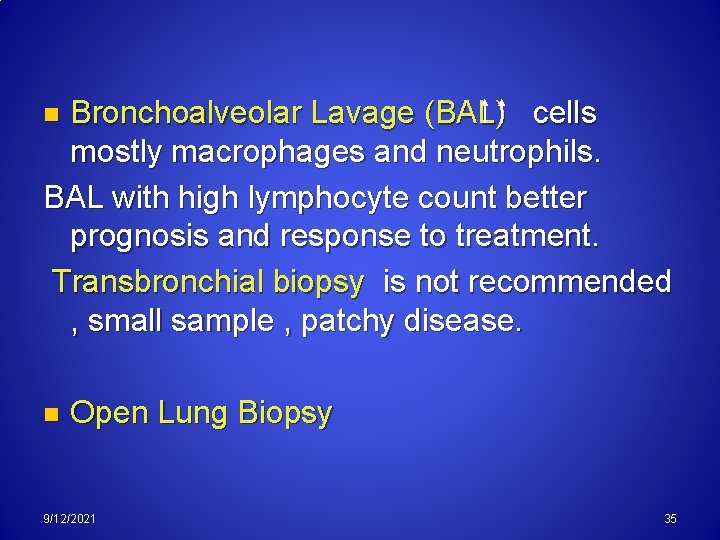
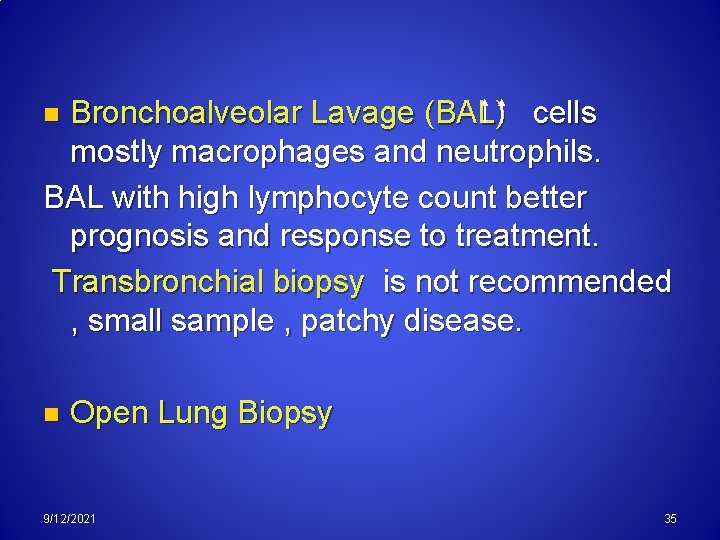
Bronchoalveolar Lavage (BAL) cells mostly macrophages and neutrophils. BAL with high lymphocyte count better prognosis and response to treatment. Transbronchial biopsy is not recommended , small sample , patchy disease. n n Open Lung Biopsy 9/12/2021 35
Complications 1. 2. 3. Hypoxemia & Respiratory failure. Pulmonary hypertension. Right-sided heart failure (cor pulmonale). 9/12/2021 36
Management of Interstitial (ILD) and Fibrotic Lung Disease
Disease Progression 50% will die within 5 ys. n 75% die of respiratory problems. n Increased incidence of Bronchogenic carcinoma which is the cause of death in 10%of cases. n Treatment should be started early and monitored carefully 9/12/2021 38
The goals of treatment are: n Decrease inflammation and prevent further lung scarring. n Remove the source of the problem, when possible. n Minimize and manage potential complications of ILD. n Improve or prevent deterioration in a patients quality of life 9/12/2021 39
Treatment Corticosteroids n 50% improvement in symptoms n 25% improvement in lung function tests 9/12/2021 40
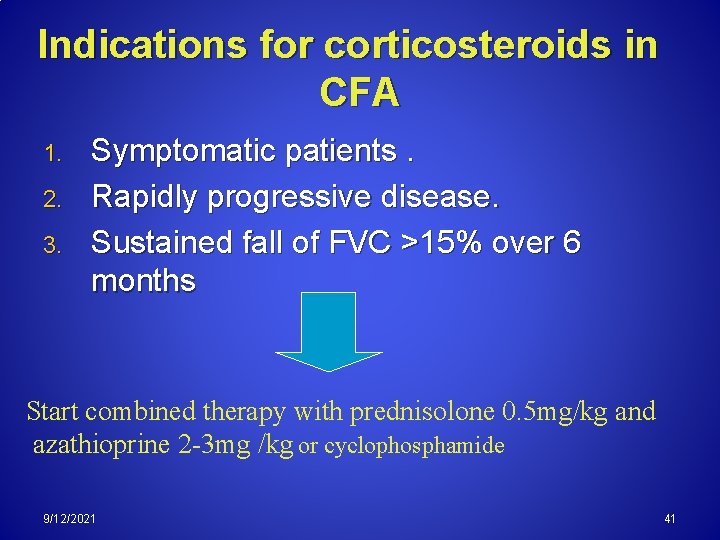
Indications for corticosteroids in CFA 1. 2. 3. Symptomatic patients. Rapidly progressive disease. Sustained fall of FVC >15% over 6 months Start combined therapy with prednisolone 0. 5 mg/kg and azathioprine 2 -3 mg /kg or cyclophosphamide 9/12/2021 41
OTHER: 1. n 2. Antifibrotics colchicine and D-penicillamine have failed to show significant benefit !!. Pirfenidone, a unique, investigational antifibrotic agent, was recently shown to have some potential benefit ? ? IFN-gamma ? ? ? 9/12/2021 42
Otherapies? Oxygen Therapy n Oxygen therapy help relieve strain on the heart and lungs and improve symptoms of shortness of breath and fatigue. Pulmonary Rehabilitation n Helps patients to achieve their highest possible level of functioning includes: education, exercise, breathing techniques, energy saving techniques, nutritional counseling and psychosocial support. 9/12/2021 43
Lung Transplantation Lung transplantation in selected patients is an option for some advanced cases to improve quality of life and prolong survival. n Indicated in: 1. Previously fit , < 60 ys, 2. Rapidly progressive disease. unresponsive to therapy. 9/12/2021 44
SARCOIDOSIS
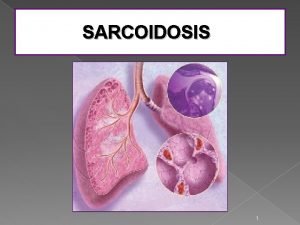
Sarcoidosis Introduction: A chronic non caseating granulomatous disease of unknown etiology that affects many organs and tissues, most commonly the lungs n The etiology is unknown. n High mortality in patients with extensive organ involvment. n 9/12/2021 46
Race: The disease affects all races. n High incidence among american black than white persons 10 20: 1. Sex: n Females are affected more often than males. Age: n Most commonly affect 20 40 ys old n 9/12/2021 47
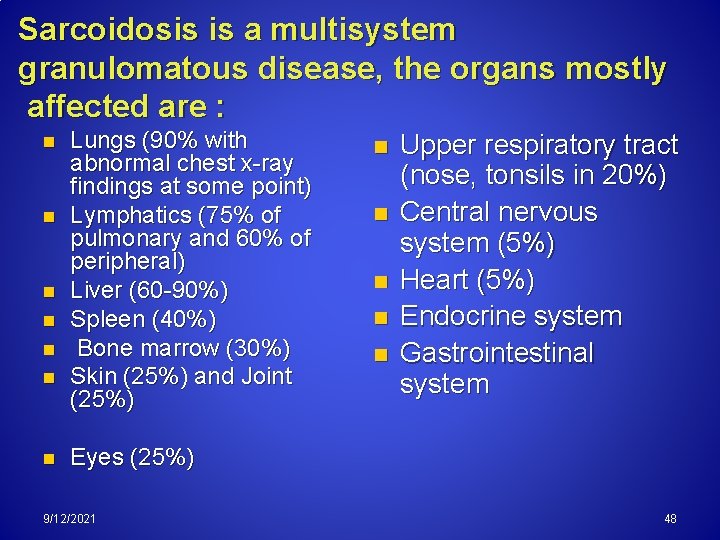
Sarcoidosis is a multisystem granulomatous disease, the organs mostly affected are : n n n n Lungs (90% with abnormal chest x ray findings at some point) Lymphatics (75% of pulmonary and 60% of peripheral) Liver (60 90%) Spleen (40%) Bone marrow (30%) Skin (25%) and Joint (25%) n n n Upper respiratory tract (nose, tonsils in 20%) Central nervous system (5%) Heart (5%) Endocrine system Gastrointestinal system Eyes (25%) 9/12/2021 48
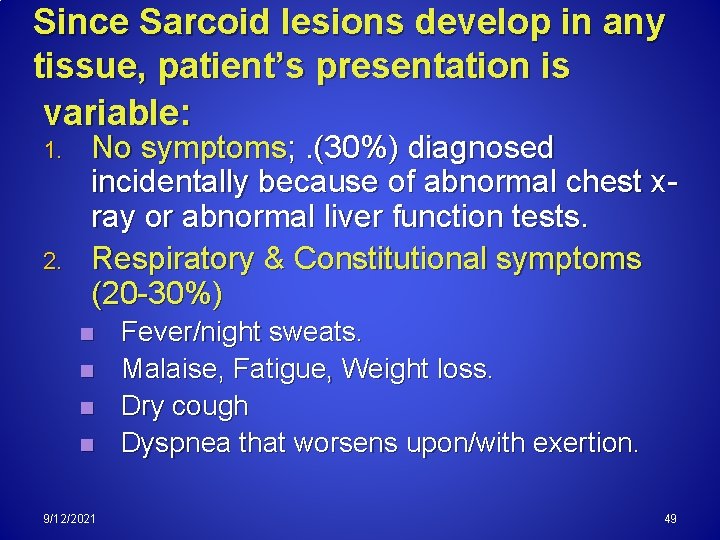
Since Sarcoid lesions develop in any tissue, patient’s presentation is variable: 1. 2. No symptoms; . (30%) diagnosed incidentally because of abnormal chest x ray or abnormal liver function tests. Respiratory & Constitutional symptoms (20 30%) n n 9/12/2021 Fever/night sweats. Malaise, Fatigue, Weight loss. Dry cough Dyspnea that worsens upon/with exertion. 49
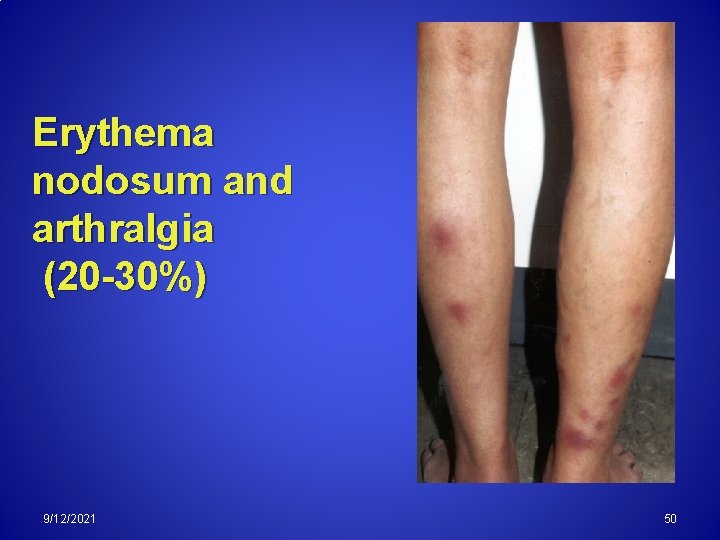
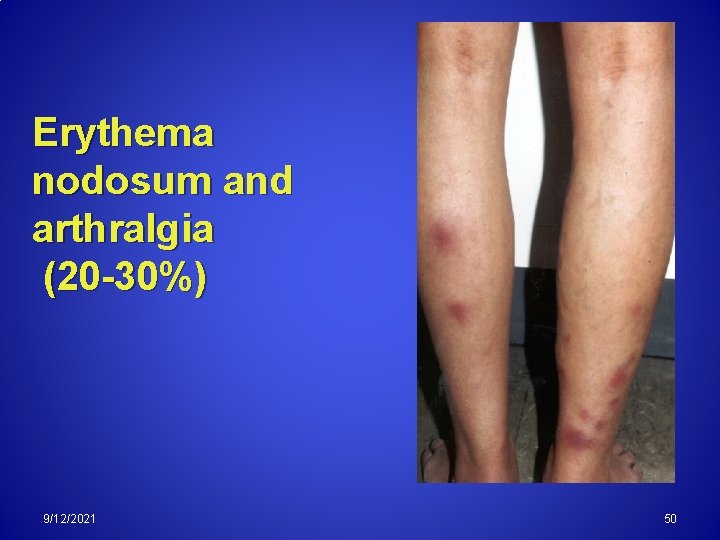
Erythema nodosum and arthralgia (20 -30%) 9/12/2021 50
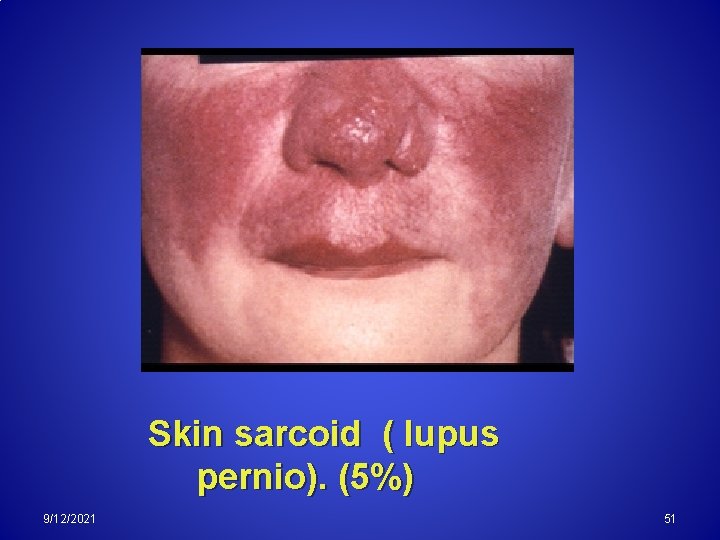
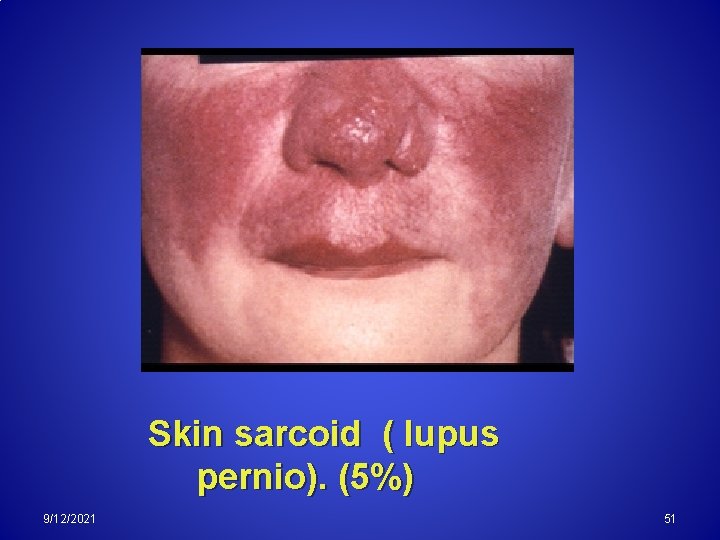
Skin sarcoid ( lupus pernio). (5%) 9/12/2021 51
3. 4. 5. Ocular symptoms (ant. uveitis & sicca syndrome). Superficial lymphadenopathy. (5%) Other, ( Hypercalcemia, diabetes isipidus, cranial nerve palsies, cardiac arrhythmias, and nephrocalcinosis). 9/12/2021 52
90% have an abnormal chest xray finding at some stage of the disease; 10% have pulmonary fibrosis.
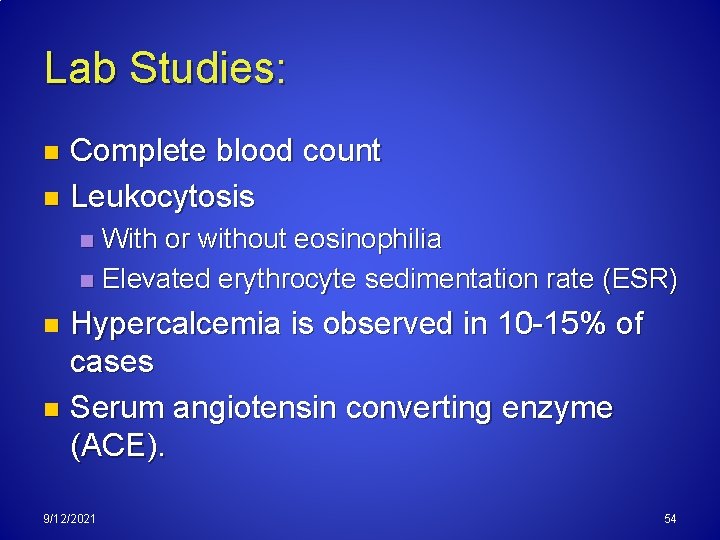
Lab Studies: Complete blood count n Leukocytosis n With or without eosinophilia n Elevated erythrocyte sedimentation rate (ESR) n Hypercalcemia is observed in 10 15% of cases n Serum angiotensin converting enzyme (ACE). n 9/12/2021 54
Imaging Studies: 1. Chest x-ray For diagnosis and staging. Stage O : No findings 9/12/2021 55
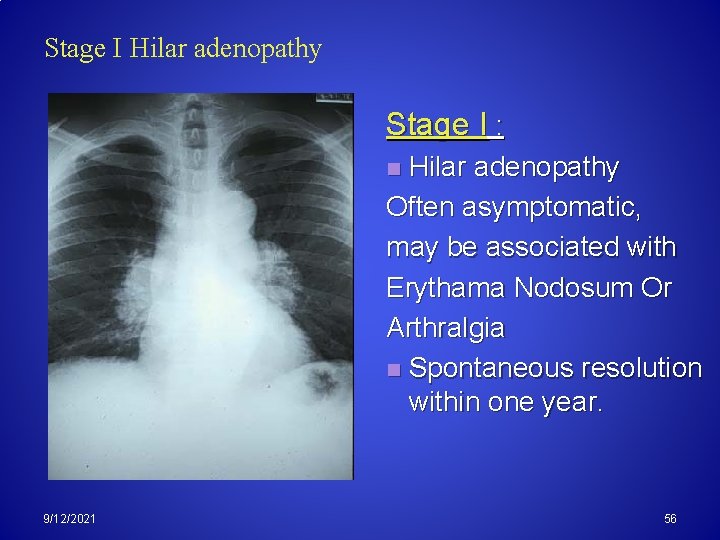
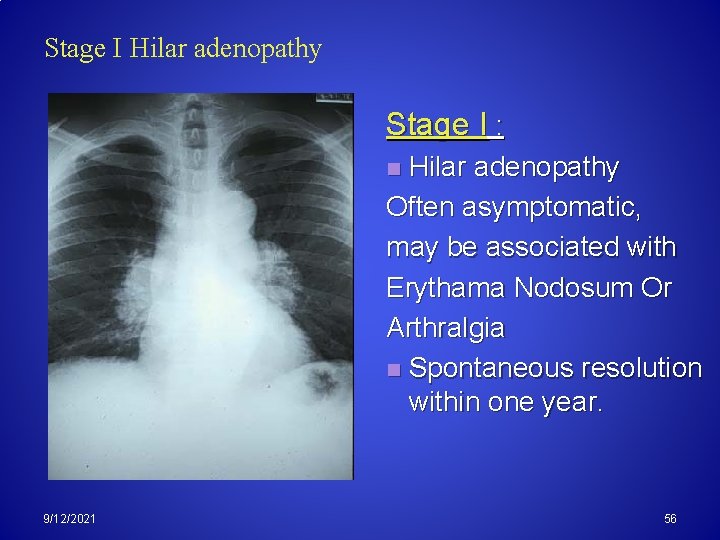
Stage I Hilar adenopathy Stage I : Hilar adenopathy Often asymptomatic, may be associated with Erythama Nodosum Or Arthralgia n Spontaneous resolution within one year. n 9/12/2021 56
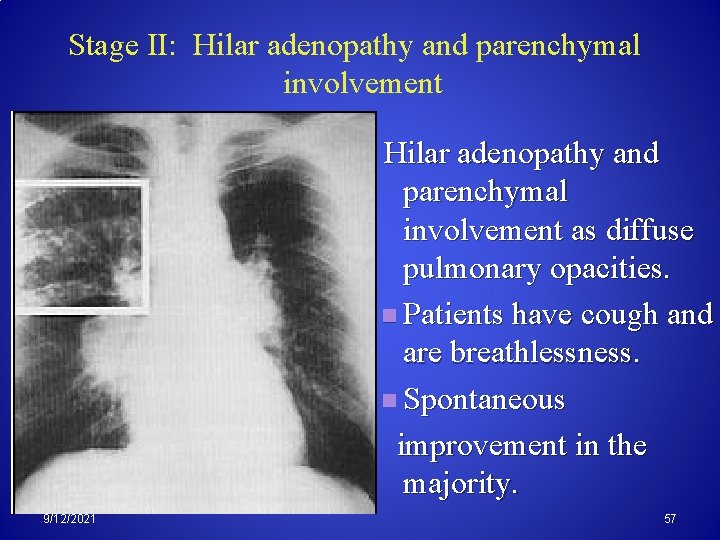
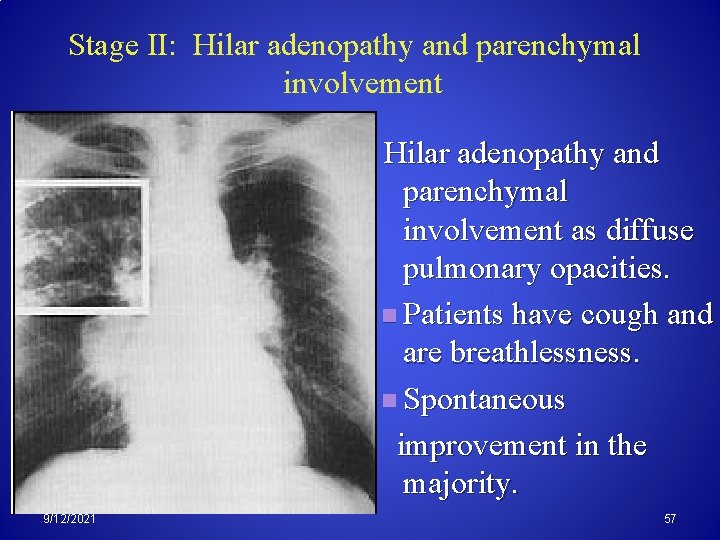
Stage II: Hilar adenopathy and parenchymal involvement as diffuse pulmonary opacities. n Patients have cough and are breathlessness. n Spontaneous improvement in the majority. 9/12/2021 57
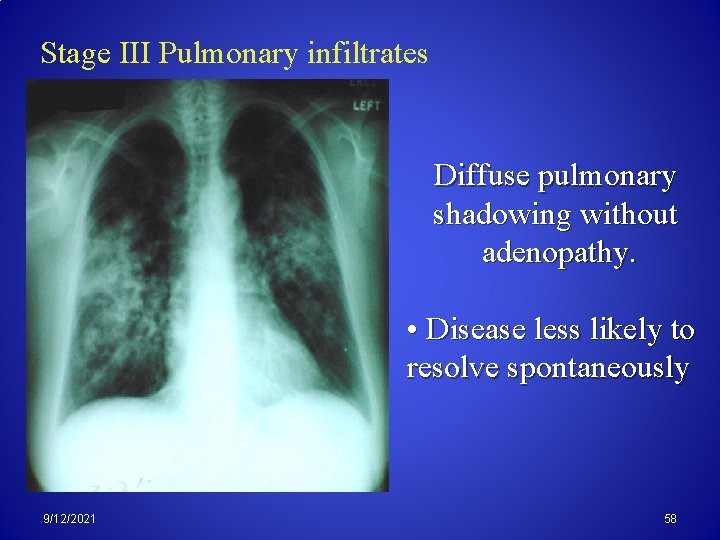
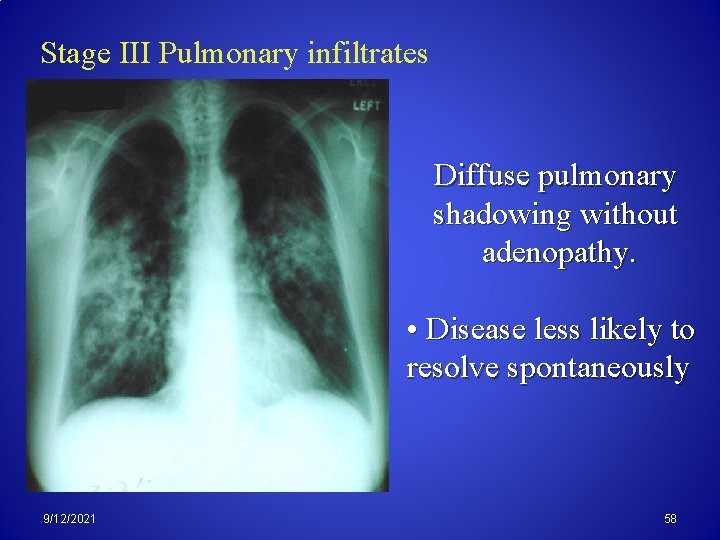
Stage III Pulmonary infiltrates Diffuse pulmonary shadowing without adenopathy. • Disease less likely to resolve spontaneously 9/12/2021 58
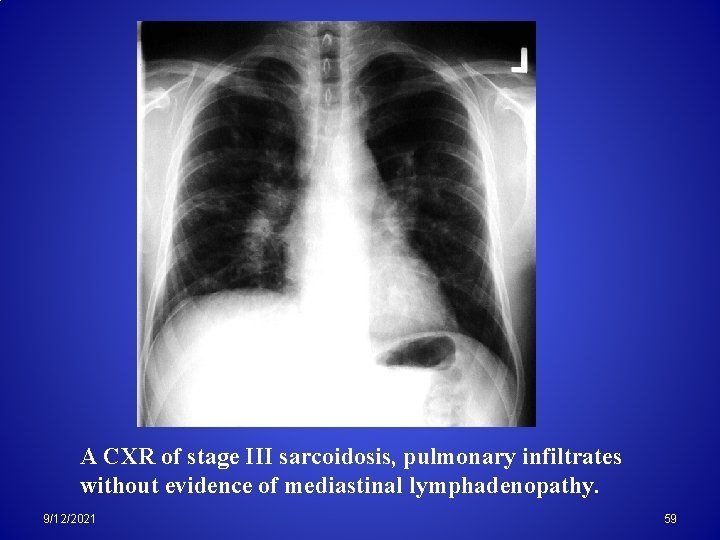
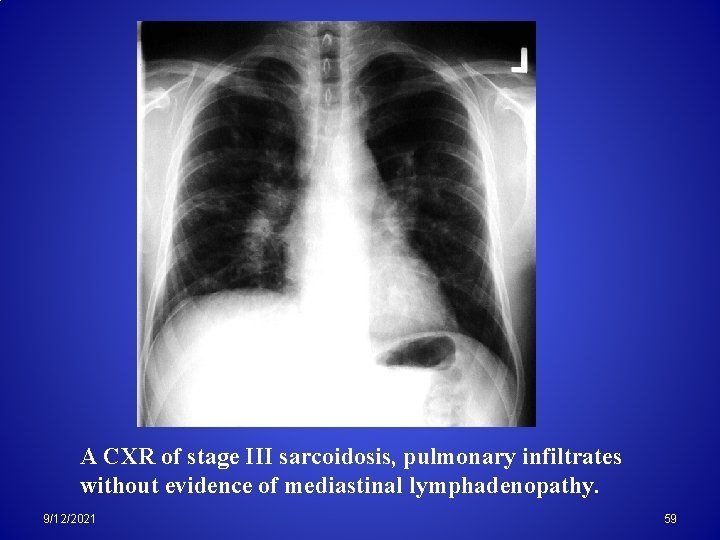
A CXR of stage III sarcoidosis, pulmonary infiltrates without evidence of mediastinal lymphadenopathy. 9/12/2021 59
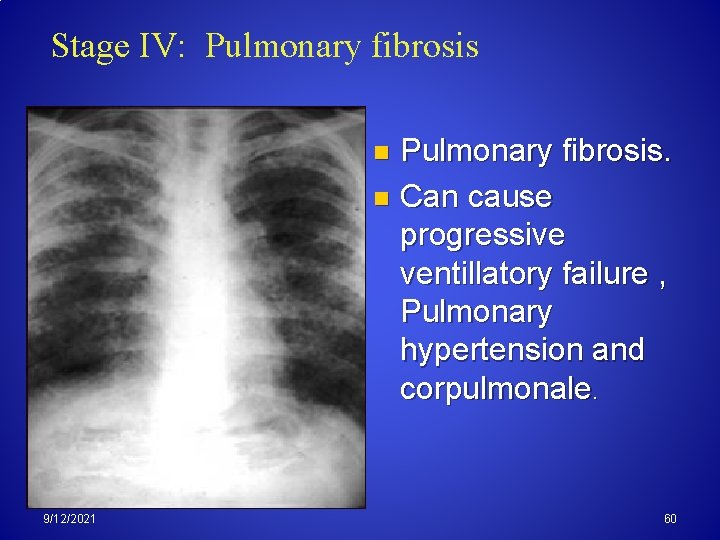
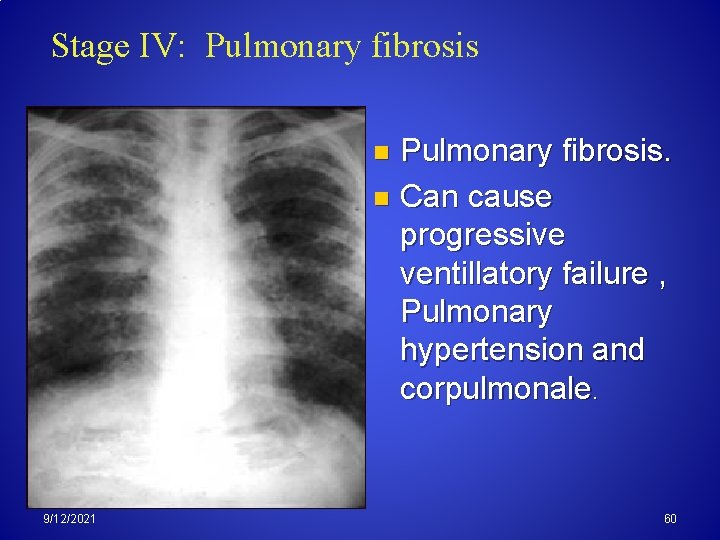
Stage IV: Pulmonary fibrosis. n Can cause progressive ventillatory failure , Pulmonary hypertension and corpulmonale. n 9/12/2021 60
Gallium 67 scanning n n Used for staging of disease and to detect extrapulmonary sarcoidosis. Gallium bound by inflammatory tissue and not by fibrotic tissue Distinguish areas of fibrosis from inflammation. 9/12/2021 61
Other Tests: Skin anergy with PPD ( Tuberculin Test) is common in sarcoidosis patients but obviously not specific. n Kveim test n A suspension from the spleen or a lymph node of a patient with a confirmed diagnosis of sarcoidosis is injected intradermaly into a patient suspected to be affected by the disease. n Test results are considered positive if a nodule appears within 2 7 weeks. n The nodule is then biopsied to find similarities 62 9/12/2021 to sarcoid granuloma n
Bronchoalveolar lavage A bronchoalveolar lavage (BAL) shows increases in the CD 4/CD 8 ratio, lymphocytes, and cytokines. n Biopsy is an integral part of the diagnosis and is of very high yield. n n n The site of biopsy is dictated by clinical presentation of the organ involved. . Pulmonary function tests (PFTs) findings consistent with restrictive lung disease. 9/12/2021 63

TREATMENT
STAGE I&II n Resolve spontaneously. . usually no treatment required. n Persistent erythema nodosum, pyrexia, arthralgia NSAID n Hypercalcemia and ant uveitis short course corticosteroids. 9/12/2021 65
STAGE III n Symptomatic pulmonary and sarcoid involving the eyes or vital organ as heart or brain Corticosteroids starting at 40 60 mg /day tapered after 6 months by 5 mg per month. and maintained on 10 mg /day for years. n Methotrexate and hydroxychloroquin are effective steroid sparing drugs. (2 nd line) 9/12/2021 66
n Extrapulmonary Sarcoidosis The heart can manifest with mechanical (CHF) and/or conduction defects (arrhythmia). Diuretics and inotropics n CNS or peripheral neuropathy systemic steroids. n Eye involvement uveitis or conjunctivitis. Topical steroids and or systemic steroids. n 9/12/2021 67
Hypercalcemia is generally responsive to IV hydration and systemic steroids. . n Skin manifestations are treated with topical or systemic steroids. n Arthritis generally is treated with NSAIDs. Steroids and occasionally colchicine are reserved for severe cases. n Asymptomatic elevation of LFTs does not require treatment n 9/12/2021 68
Lung Disease Due To Organic Dust
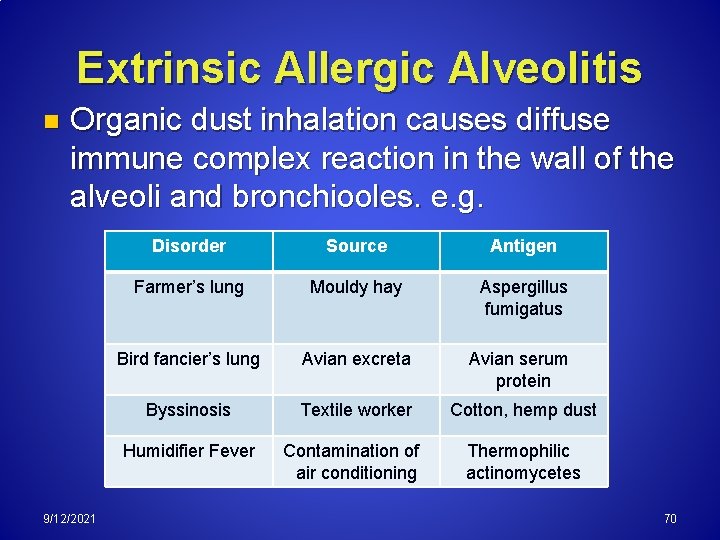
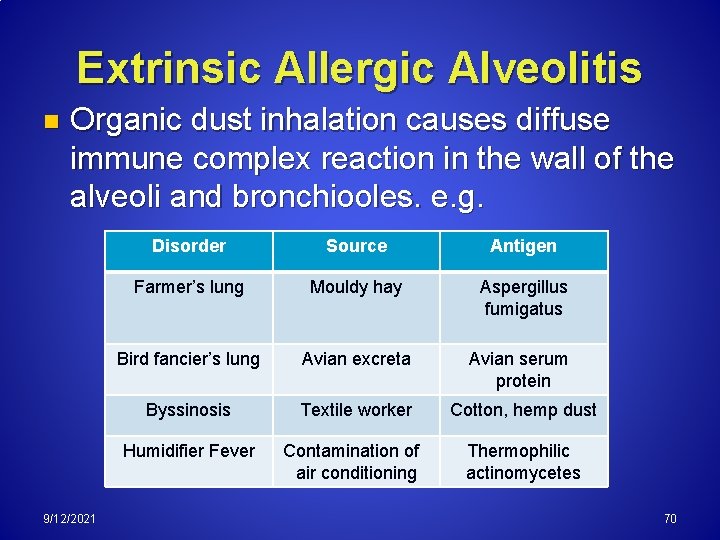
Extrinsic Allergic Alveolitis n Organic dust inhalation causes diffuse immune complex reaction in the wall of the alveoli and bronchiooles. e. g. 9/12/2021 Disorder Source Antigen Farmer’s lung Mouldy hay Aspergillus fumigatus Bird fancier’s lung Avian excreta Avian serum protein Byssinosis Textile worker Cotton, hemp dust Humidifier Fever Contamination of air conditioning Thermophilic actinomycetes 70
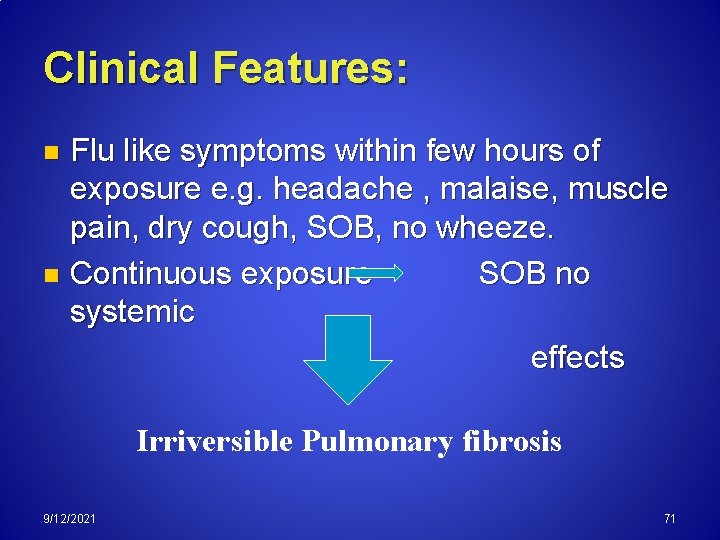
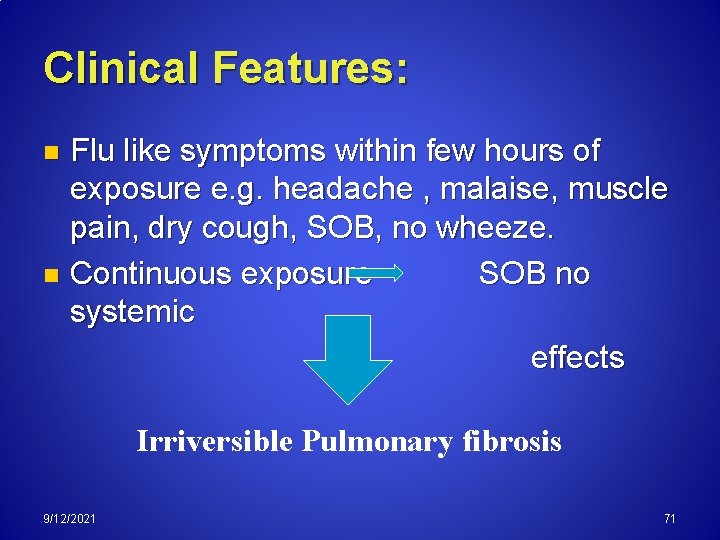
Clinical Features: Flu like symptoms within few hours of exposure e. g. headache , malaise, muscle pain, dry cough, SOB, no wheeze. n Continuous exposure SOB no systemic effects n Irriversible Pulmonary fibrosis 9/12/2021 71
Lung Disease Due To Inorganic Dust Exposure 9/12/2021 72
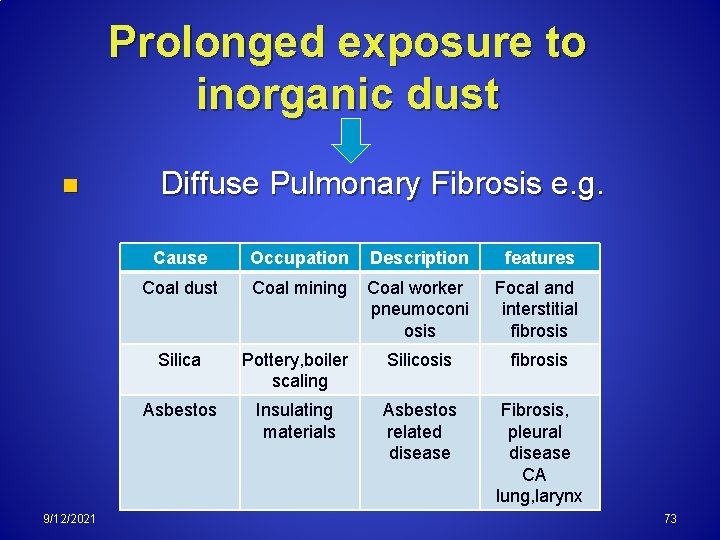
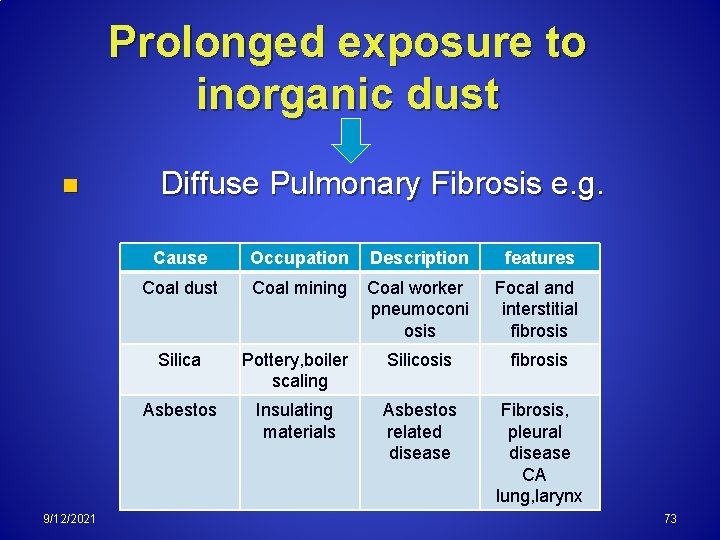
Prolonged exposure to inorganic dust n 9/12/2021 Diffuse Pulmonary Fibrosis e. g. Cause Occupation Description features Coal dust Coal mining Coal worker pneumoconi osis Focal and interstitial fibrosis Silica Pottery, boiler scaling Silicosis fibrosis Asbestos Insulating materials Asbestos related disease Fibrosis, pleural disease CA lung, larynx 73
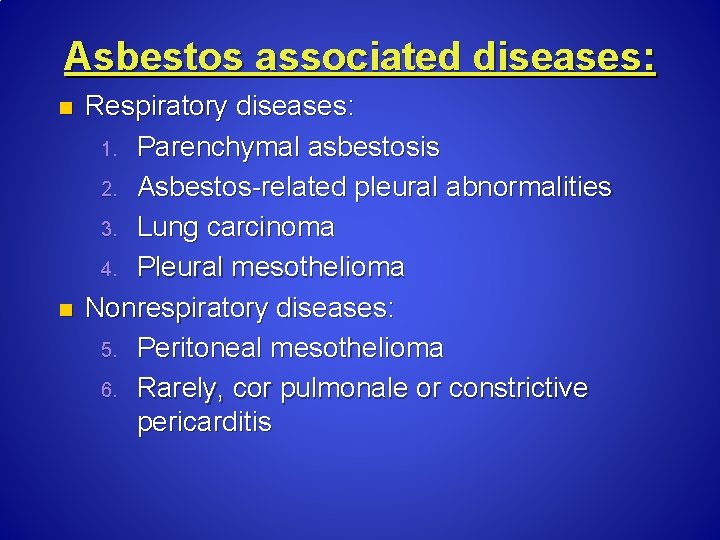
Asbestos associated diseases: n n Respiratory diseases: 1. Parenchymal asbestosis 2. Asbestos related pleural abnormalities 3. Lung carcinoma 4. Pleural mesothelioma Nonrespiratory diseases: 5. Peritoneal mesothelioma 6. Rarely, cor pulmonale or constrictive pericarditis
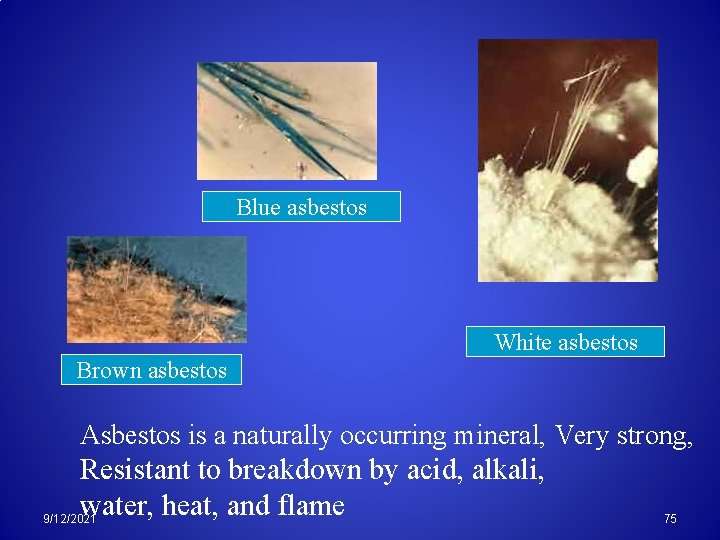
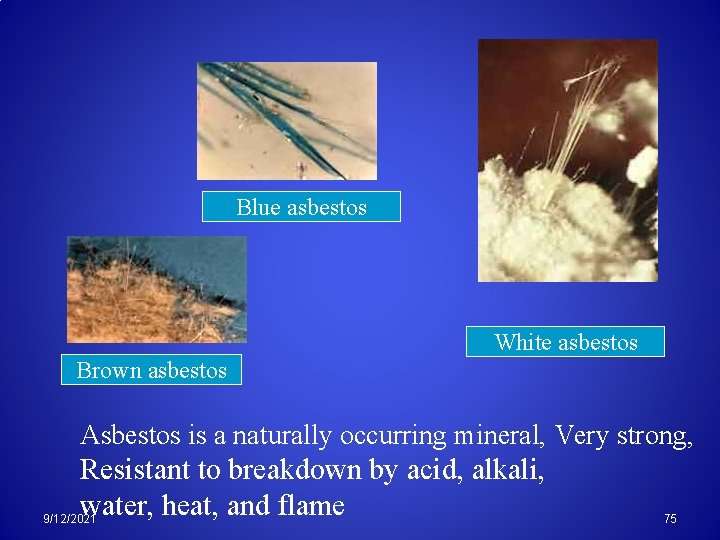
Blue asbestos White asbestos Brown asbestos Asbestos is a naturally occurring mineral, Very strong, Resistant to breakdown by acid, alkali, water, heat, and flame 9/12/2021 75
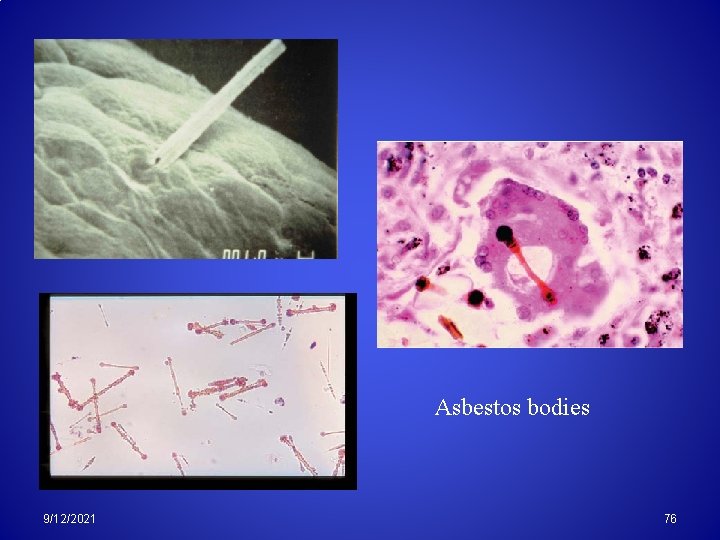
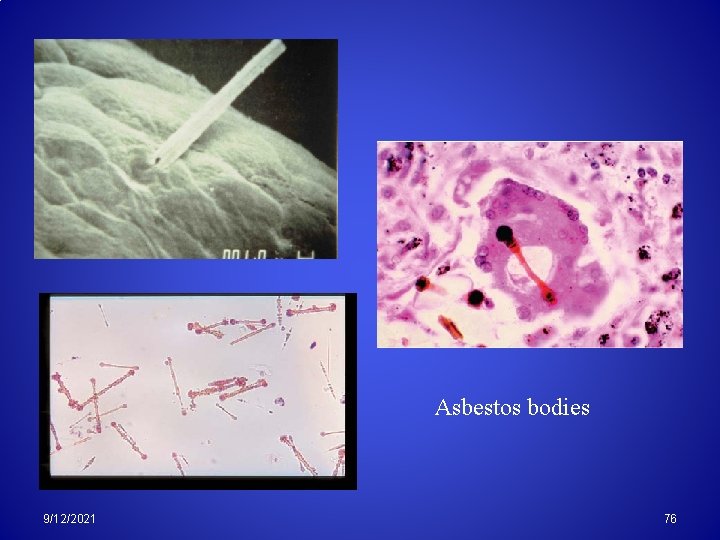
Asbestos bodies 9/12/2021 76
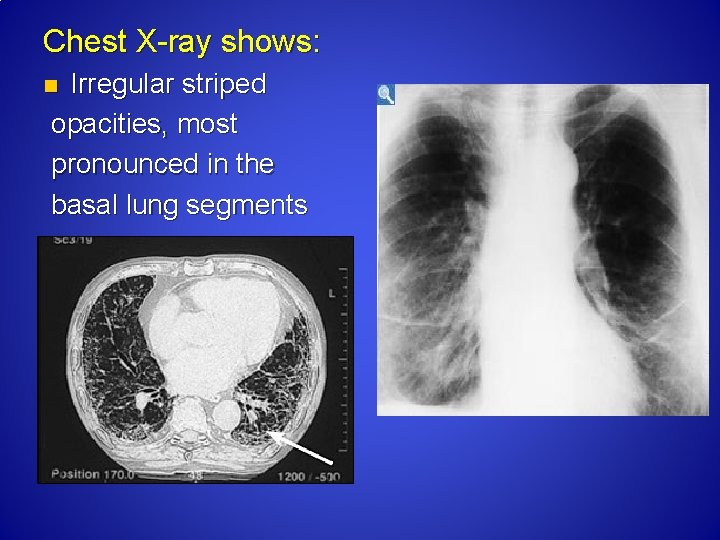
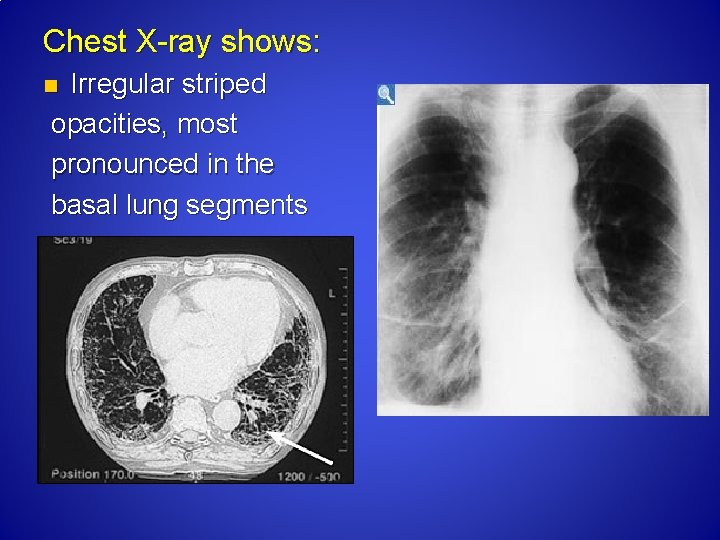
Chest X ray shows: Irregular striped opacities, most pronounced in the basal lung segments n
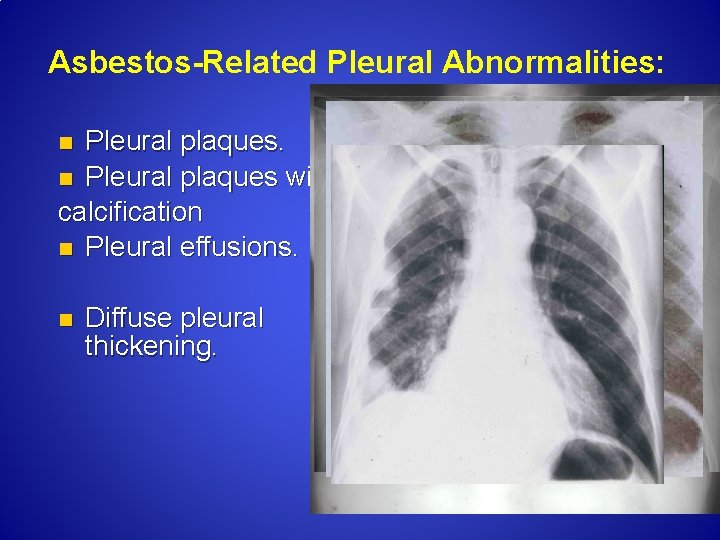
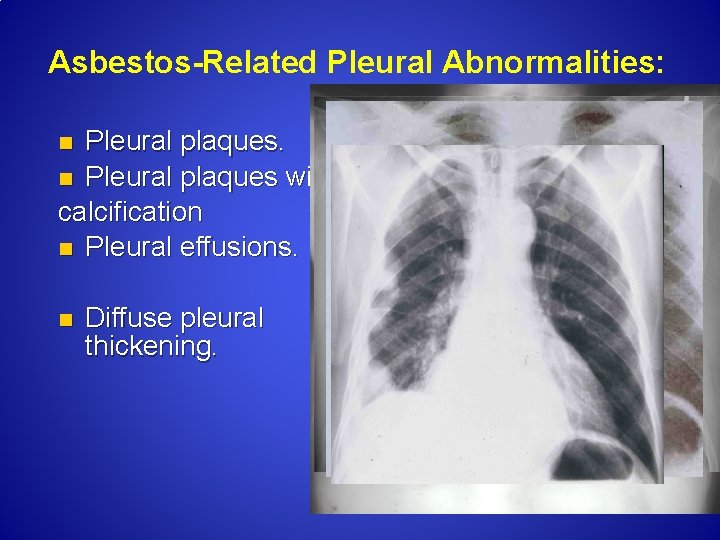
Asbestos-Related Pleural Abnormalities: Pleural plaques. n Pleural plaques with calcification n Pleural effusions. n n Diffuse pleural thickening.
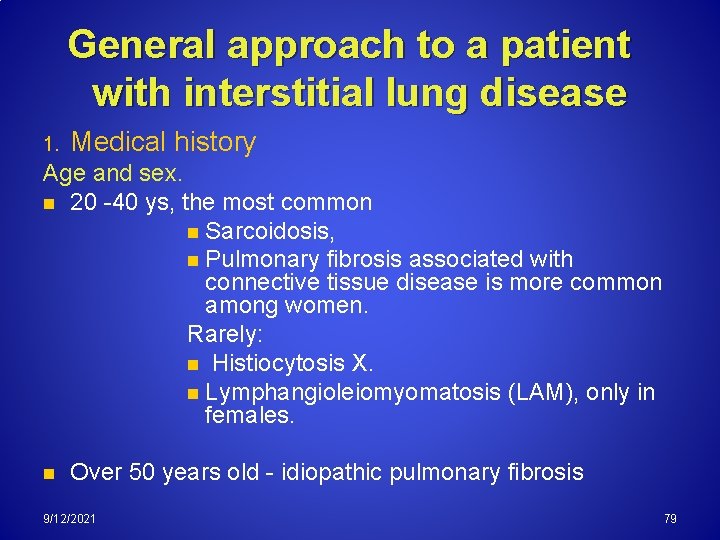
General approach to a patient with interstitial lung disease 1. Medical history Age and sex. n 20 40 ys, the most common n Sarcoidosis, n Pulmonary fibrosis associated with connective tissue disease is more common among women. Rarely: n Histiocytosis X. n Lymphangioleiomyomatosis (LAM), only in females. n Over 50 years old idiopathic pulmonary fibrosis 9/12/2021 79
Family history: This can provide very useful information. n Patients with IPF disease (familial pulmonary fibrosis). n Sarcoidosis. Smoking Certain types of ILD primarily affect smokers e. g. desquamative intersitial pneumonia (DIP), respiratory bronchiolitis-associated interstitial lung disease (RB-ILD). Sarcoidosis and EAA, occur more frequently in nonsmokers 9/12/2021 80
Occupational and work history. A complete occupational history should be recorded with details of work activities and any possible exposure to inorganic dust. EAA is caused by exposure to organic agents, and Pneumoconiosis by exposure to inorganic dust Drug history. all current and past medications taken by the patient should be noted, including details of the dose and duration of treatment. Radiotherapy. A history of chest radiation therapy could be the cause of DILD. Systemic diseases. Identify and investigate ( rash, joint pain…) 9/12/2021 81
Diagnostic Tests That May Be Used to Identify Pulmonary Fibrosis or Interstitial Lung Disease 1. 2. 3. 4. 5. 6. 7. Blood Tests Pulmonary Function Tests Chest X ray CT Scan Bronchoscopy Bronchoalveolar Lavage Lung Biopsy 9/12/2021 82
CONCLUSION Current therapy remains with uncertain outcome and is not thought to reverse scarring that has already taken place. Early diagnosis as well as identifying and removal of occupational or environmental exposure is essential still Hope For An Effective And Safe Medications In The Future
THANK YOU
 Interstial
Interstial Sacrodiosis
Sacrodiosis Sarcoidosis
Sarcoidosis Caseating granuloma vs noncaseating
Caseating granuloma vs noncaseating Giulio rossi anatomia patologica
Giulio rossi anatomia patologica Respiratory failure types
Respiratory failure types Dr rajesh babu
Dr rajesh babu Septae
Septae Emphysème
Emphysème Farmer's lung disease
Farmer's lung disease Obstructive vs restrictive
Obstructive vs restrictive Difference between obstructive and restrictive lung disease
Difference between obstructive and restrictive lung disease What is a restrictive lung disease
What is a restrictive lung disease Dpld lung disease
Dpld lung disease Restrictive lung disease
Restrictive lung disease Difference between obstructive and restrictive lung disease
Difference between obstructive and restrictive lung disease Restrictive lung disease
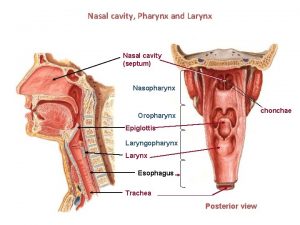
Restrictive lung disease What is the conducting zone of the respiratory system
What is the conducting zone of the respiratory system Disease respiratory
Disease respiratory Communicable disease and non communicable disease
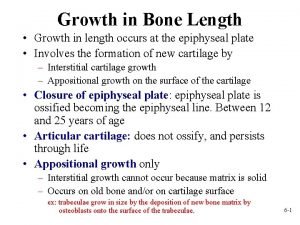
Communicable disease and non communicable disease Interstitial cartilage
Interstitial cartilage Ecf icf and interstitial fluid
Ecf icf and interstitial fluid Interstitial and appositional growth of cartilage
Interstitial and appositional growth of cartilage Vacancy defect and interstitial defect
Vacancy defect and interstitial defect Ecf icf and interstitial fluid
Ecf icf and interstitial fluid Steel interstitial alloy
Steel interstitial alloy Movement of body fluids
Movement of body fluids Particle arrangement of solid
Particle arrangement of solid Interstitial velocity
Interstitial velocity Acute interstitial nephritis urine findings
Acute interstitial nephritis urine findings An atypical accumulation of fluid in the interstitial space
An atypical accumulation of fluid in the interstitial space Interstitial pattern
Interstitial pattern Interstitial velocity
Interstitial velocity Interstitial impurity atom
Interstitial impurity atom Solid
Solid Periosteum and endosteum of bone
Periosteum and endosteum of bone Interstitial condensation
Interstitial condensation An atypical accumulation of fluid in the interstitial space
An atypical accumulation of fluid in the interstitial space Colloid osmotic pressure vs hydrostatic pressure
Colloid osmotic pressure vs hydrostatic pressure Interstitial vs intracellular
Interstitial vs intracellular Haustrum
Haustrum Blood vessels
Blood vessels Interstitial ceilings
Interstitial ceilings Hydrostatic vs osmotic pressure
Hydrostatic vs osmotic pressure Dr. amy ford
Dr. amy ford Static compliance formula
Static compliance formula Iron lung
Iron lung Chest expansion palpation
Chest expansion palpation Acinus
Acinus Superior sulcus lung anatomy
Superior sulcus lung anatomy Sacii pulmonari
Sacii pulmonari Dynamic compliance formula
Dynamic compliance formula Lung acinus
Lung acinus Lung capacity
Lung capacity Breathstacking
Breathstacking Rhonchi
Rhonchi Identify the epithelium.
Identify the epithelium. Trachea histology labeled
Trachea histology labeled Right middle lobe pneumonia
Right middle lobe pneumonia Lung cancer location
Lung cancer location 3 types of lung receptors
3 types of lung receptors Exudative pleural effusion
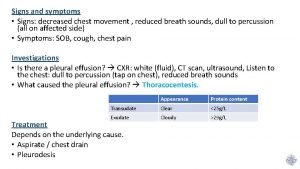
Exudative pleural effusion Caroline liqui lung
Caroline liqui lung Hilum of lung
Hilum of lung Posterior intercostal arteries
Posterior intercostal arteries X ray of asthma patient
X ray of asthma patient Lung histology identification points
Lung histology identification points Fremitus lungs
Fremitus lungs Cel mai scurt verset din biblie
Cel mai scurt verset din biblie Primary bronchi
Primary bronchi Necrosis
Necrosis Alveoli function
Alveoli function Pleura
Pleura Root of lung anatomy
Root of lung anatomy Pneumonia lung sound
Pneumonia lung sound Bronchial artery
Bronchial artery 3 lobes of lung
3 lobes of lung Mammalian lung diagram
Mammalian lung diagram Compliance and elastic recoil
Compliance and elastic recoil Right marginal artery
Right marginal artery Increase tactile fremitus
Increase tactile fremitus Lung buds
Lung buds Lung tissue
Lung tissue Spirogram diagram
Spirogram diagram Spontaneous pneumothorax
Spontaneous pneumothorax