National Optimal Lung Pathway Amy Ford Medical Oncologist
- Slides: 35
National Optimal Lung Pathway Amy Ford - Medical Oncologist, UHMBT Lisa Flanagan – Project Manager, Pathway Redesign, Lancashire and South Cumbria Cancer Alliance
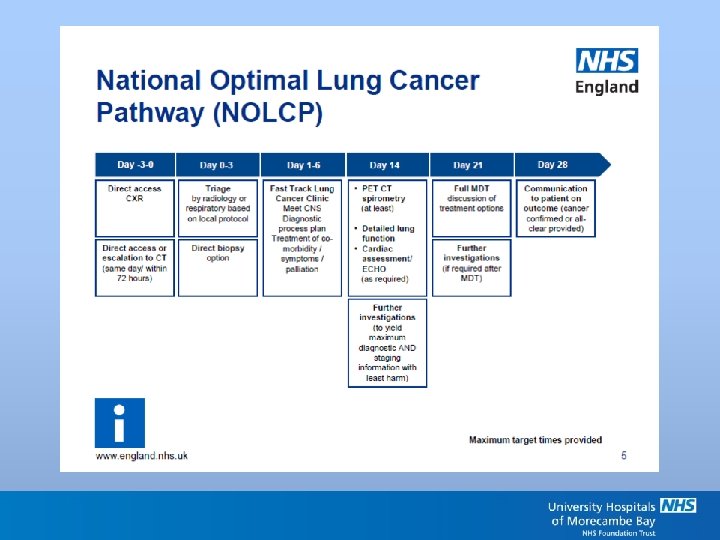
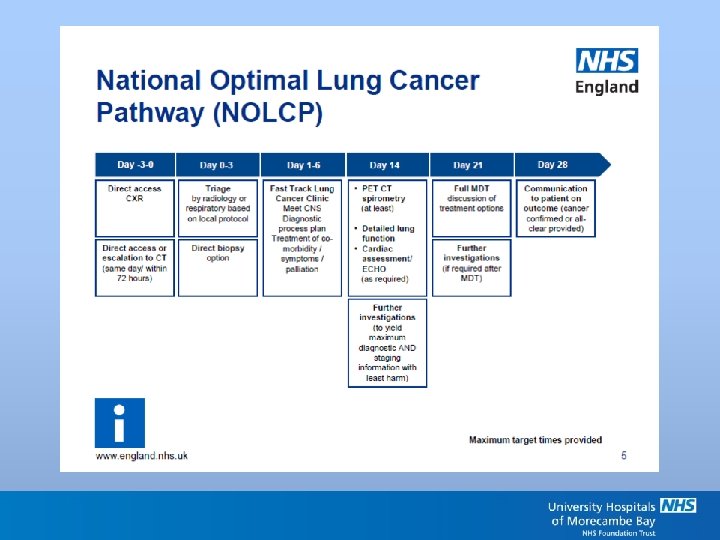
Implementation of the National Optimal Lung Pathway (NOLP) • In a nutshell; • Currently – definitive treatment to be achieved by day 62 • Future – diagnosis by day 28, treatment by day 49
Why?
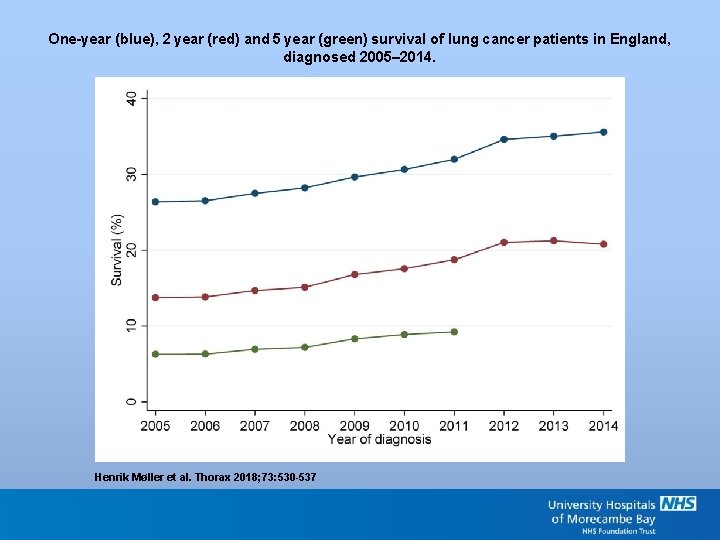
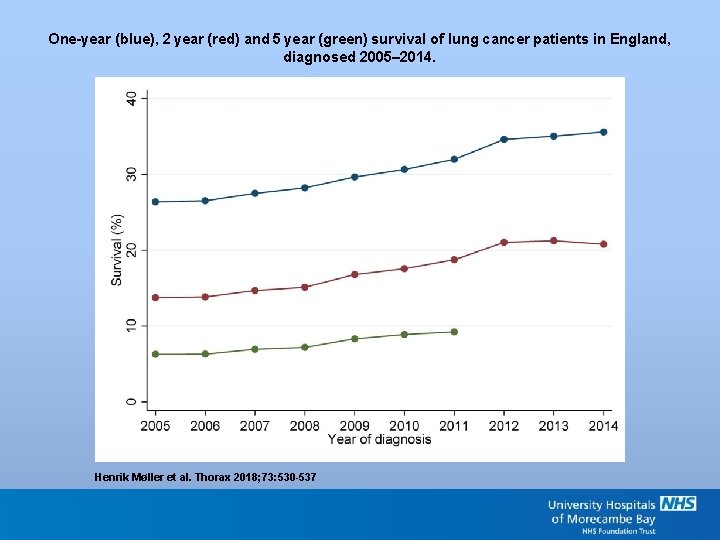
One-year (blue), 2 year (red) and 5 year (green) survival of lung cancer patients in England, diagnosed 2005– 2014. Henrik Møller et al. Thorax 2018; 73: 530 -537 Copyright © BMJ Publishing Group Ltd & British Thoracic Society. All rights reserved.
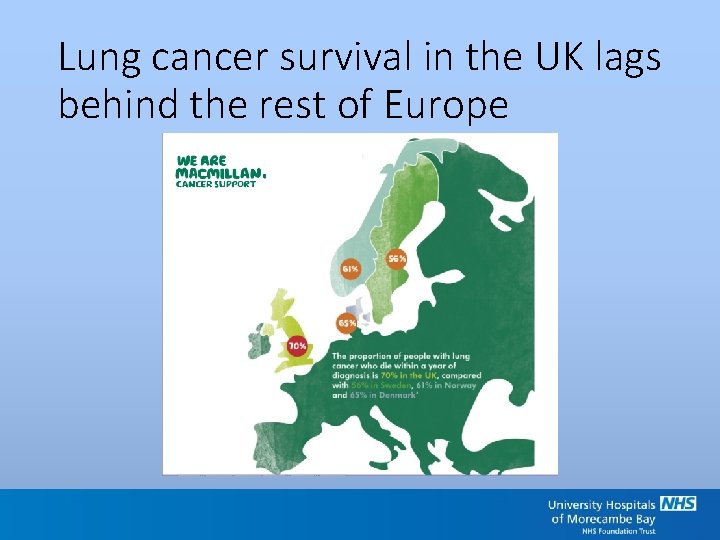
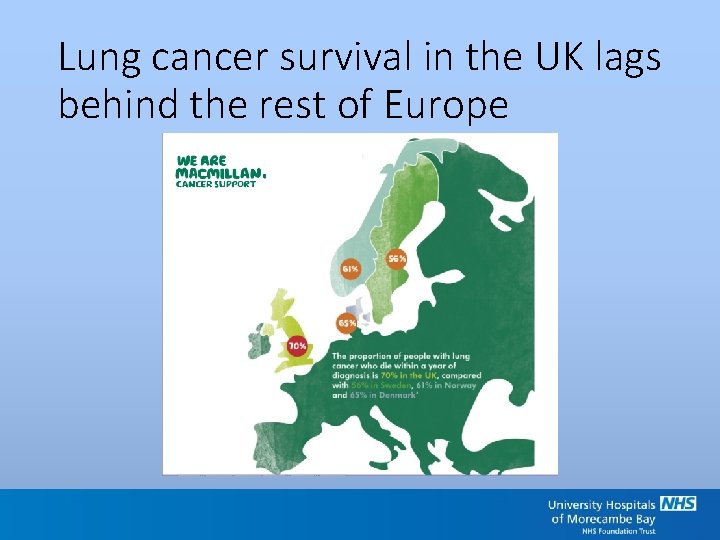
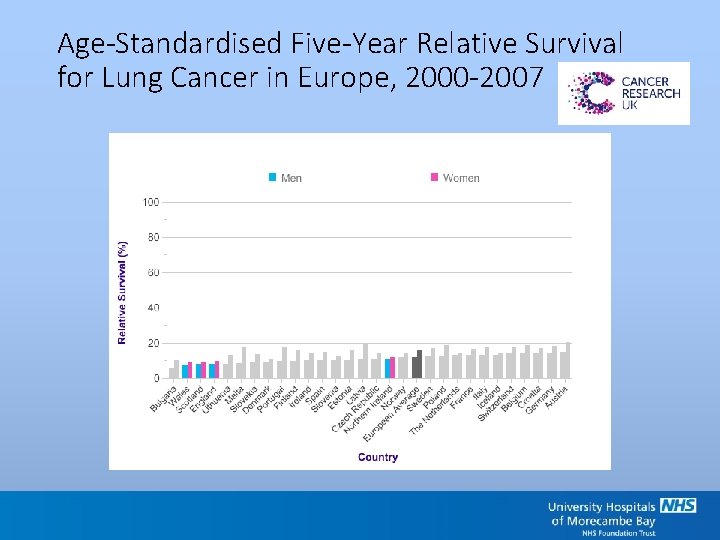
Lung cancer survival in the UK lags behind the rest of Europe
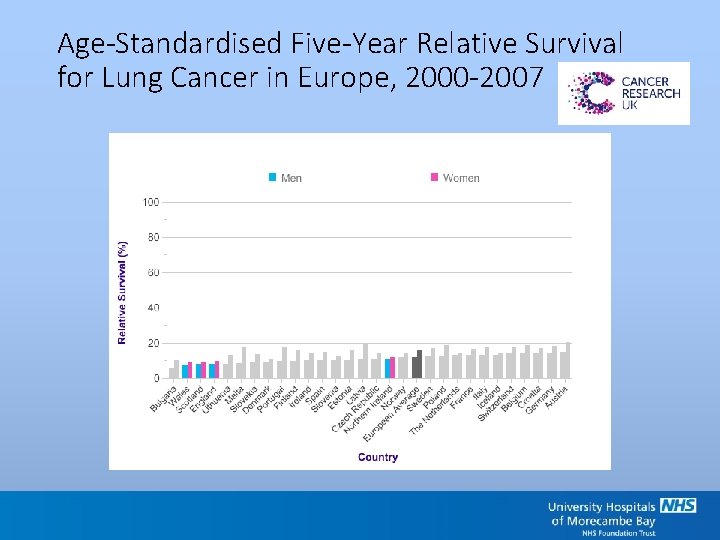
Age-Standardised Five-Year Relative Survival for Lung Cancer in Europe, 2000 -2007
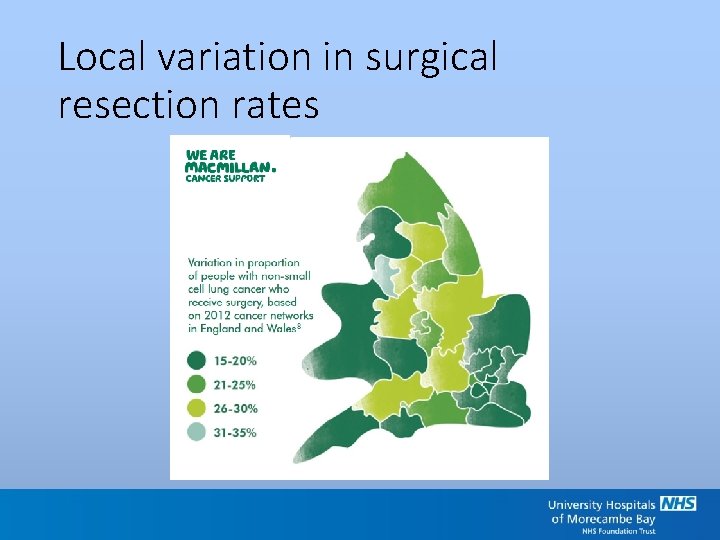
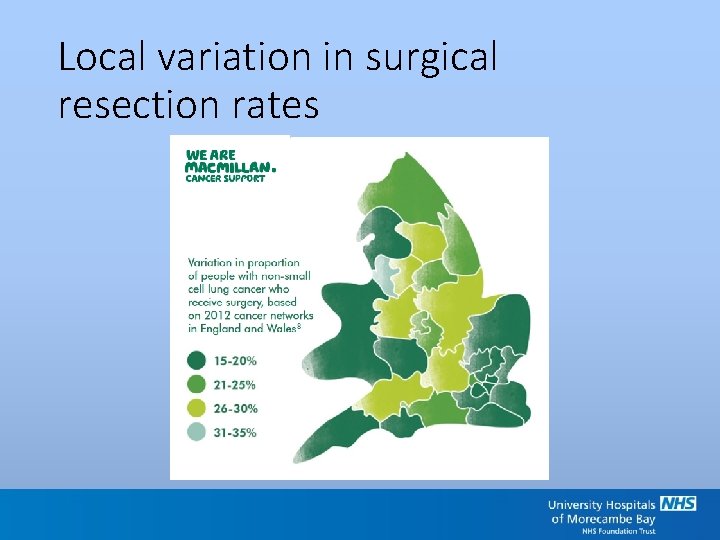
Local variation in surgical resection rates
Local variation in radiotherapy and systemic treatment rates
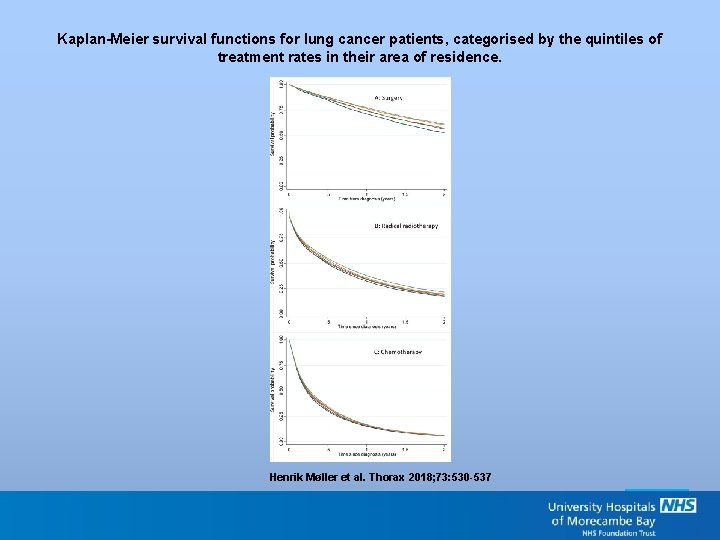
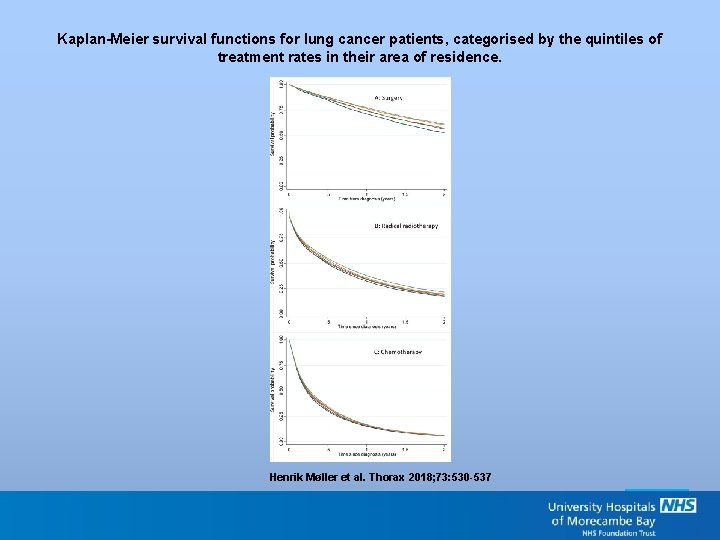
Kaplan-Meier survival functions for lung cancer patients, categorised by the quintiles of treatment rates in their area of residence. Henrik Møller et al. Thorax 2018; 73: 530 -537 Copyright © BMJ Publishing Group Ltd & British Thoracic Society. All rights reserved.
Why do we need a National Optimal Lung Pathway? • Lung cancer survival lags behind the rest of Europe • Local variation in surgical resection rates, radiotherapy and systemic treatment • High proportion of lung cancers still present late, as an emergency
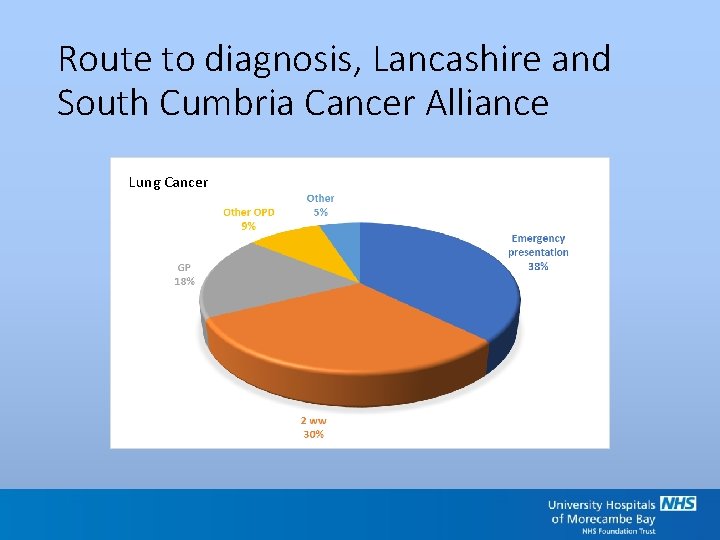
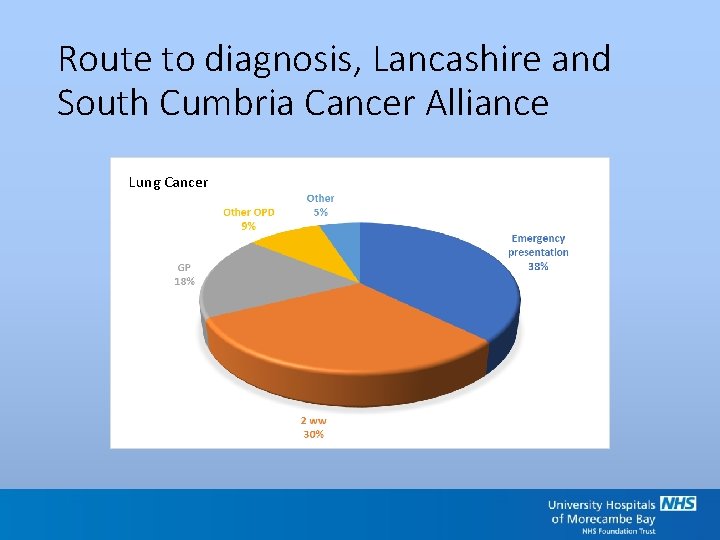
Route to diagnosis, Lancashire and South Cumbria Cancer Alliance Lung Cancer
Current target; Definitive lung cancer treatment to be started by day 62 for 85 % of patients.
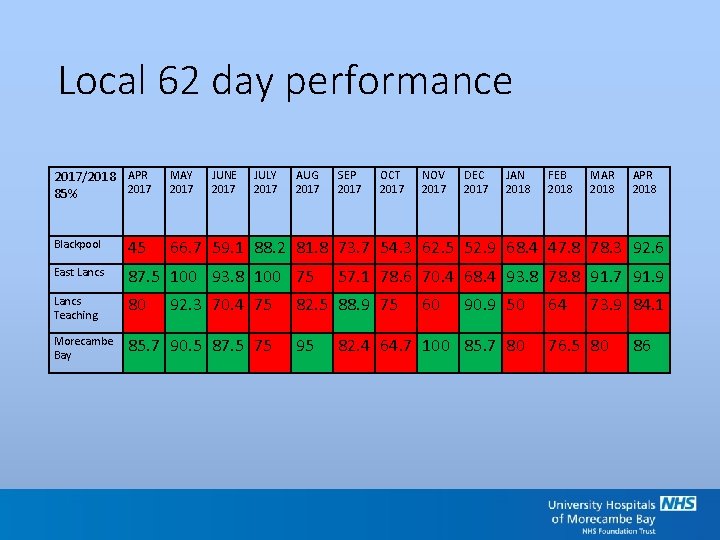
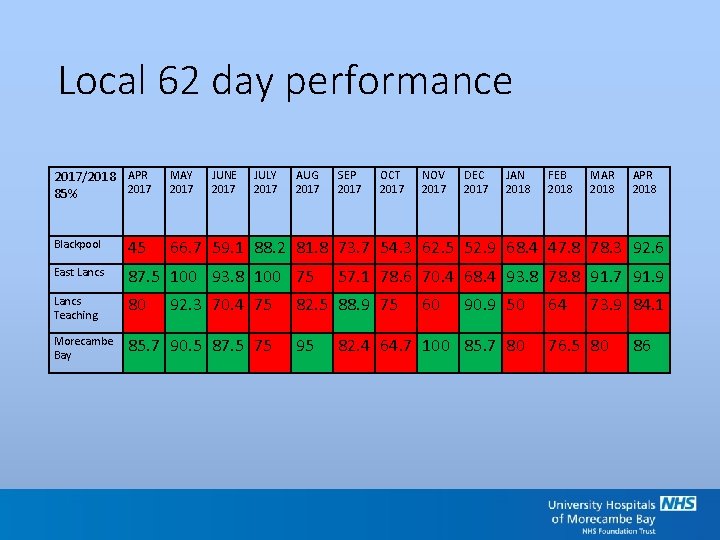
Local 62 day performance 2017/2018 APR 2017 85% MAY 2017 JUNE 2017 JULY 2017 AUG 2017 Blackpool 45 East Lancs 87. 5 100 93. 8 100 75 Lancs Teaching 80 Morecambe Bay 85. 7 90. 5 87. 5 75 SEP 2017 OCT 2017 NOV 2017 DEC 2017 JAN 2018 FEB 2018 MAR 2018 APR 2018 66. 7 59. 1 88. 2 81. 8 73. 7 54. 3 62. 5 52. 9 68. 4 47. 8 78. 3 92. 6 92. 3 70. 4 75 57. 1 78. 6 70. 4 68. 4 93. 8 78. 8 91. 7 91. 9 82. 5 88. 9 75 95 60 90. 9 50 82. 4 64. 7 100 85. 7 80 64 73. 9 84. 1 76. 5 80 86
Achieving World Class Cancer Outcome Target - 2020 Diagnosis by day 28 Treatment by day 49 ‘Shadow’ monitoring of this target from April 2018 Will the National Optimal Lung Pathway (NOLP) make a difference?
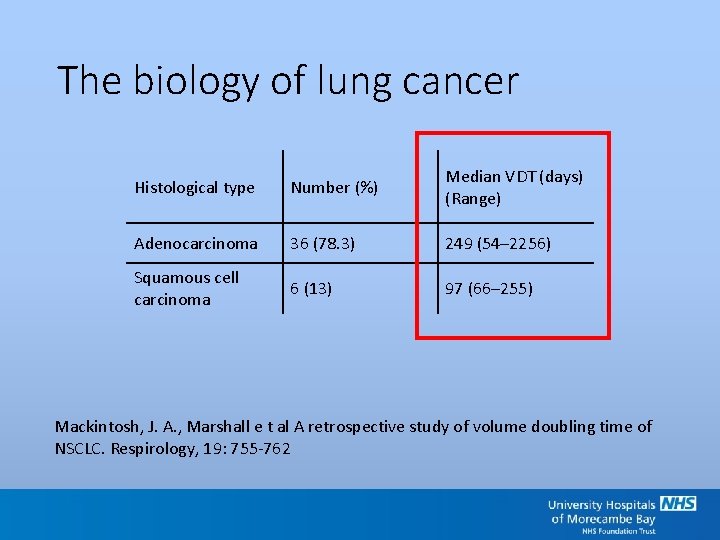
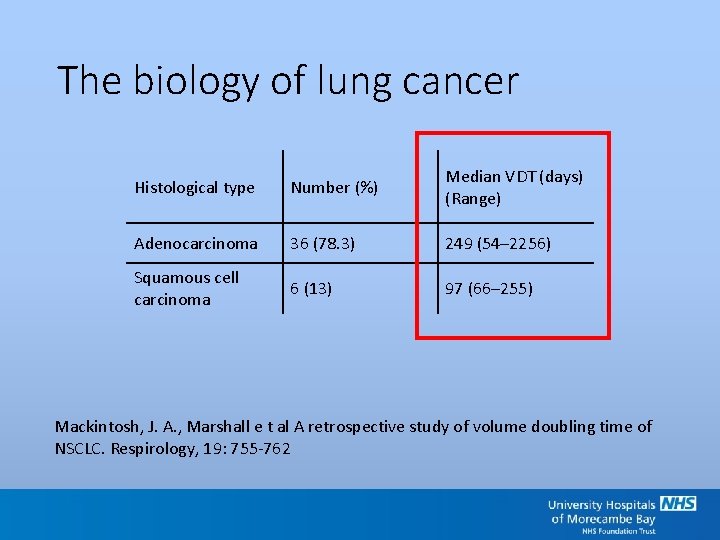
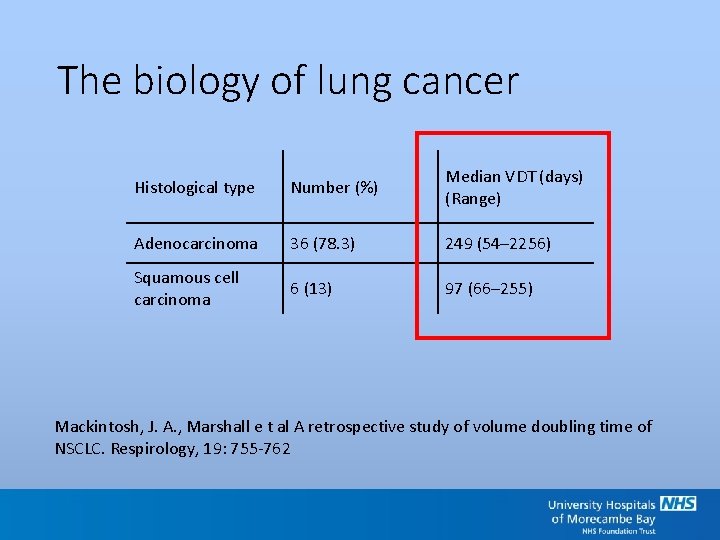
The biology of lung cancer Histological type Number (%) Median VDT (days) (Range) Adenocarcinoma 36 (78. 3) 249 (54– 2256) Squamous cell carcinoma 6 (13) 97 (66– 255) Mackintosh, J. A. , Marshall e t al A retrospective study of volume doubling time of NSCLC. Respirology, 19: 755 -762
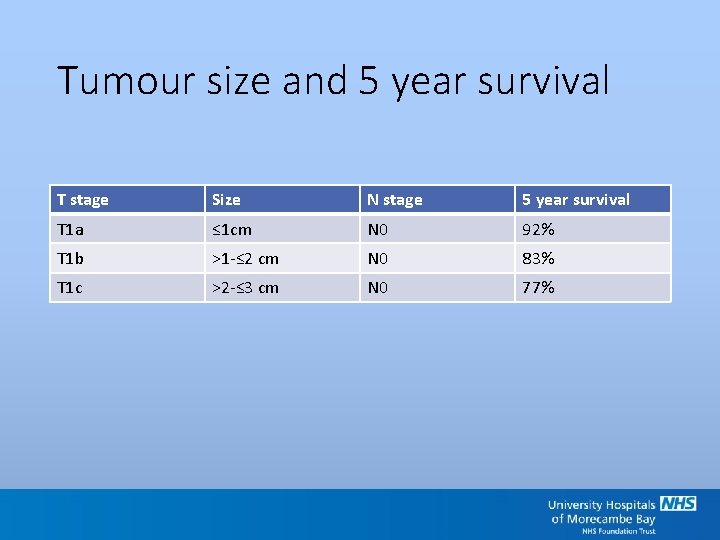
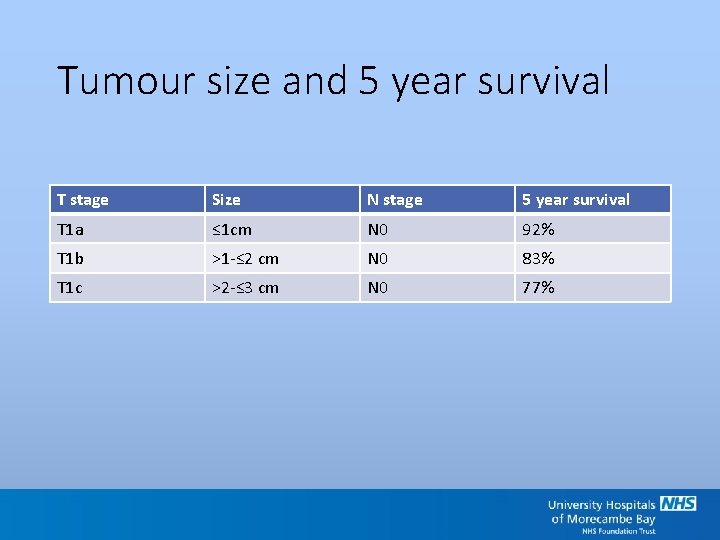
Tumour size and 5 year survival T stage Size N stage 5 year survival T 1 a ≤ 1 cm N 0 92% T 1 b >1 -≤ 2 cm N 0 83% T 1 c >2 -≤ 3 cm N 0 77%
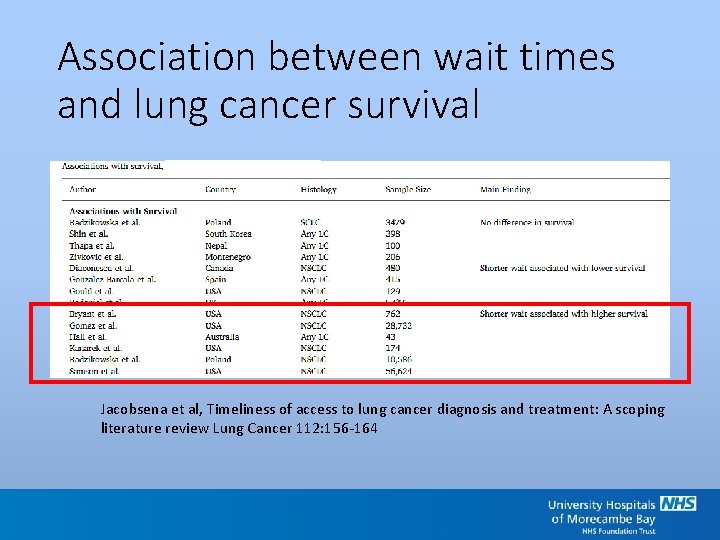
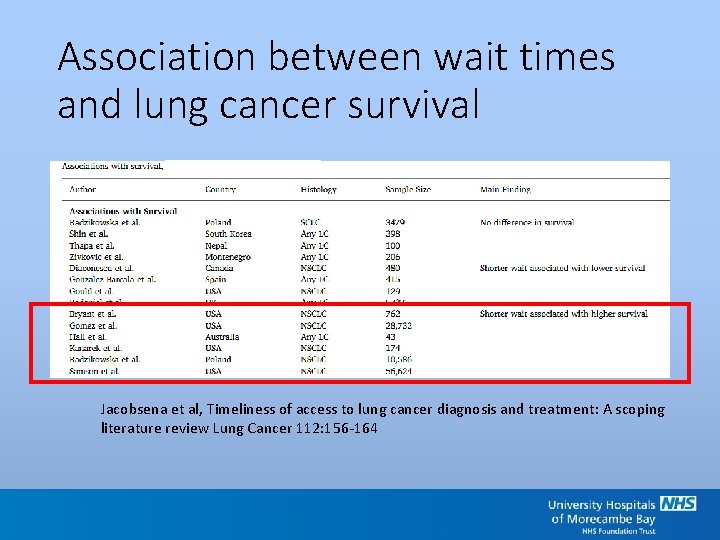
Association between wait times and lung cancer survival Jacobsena et al, Timeliness of access to lung cancer diagnosis and treatment: A scoping literature review Lung Cancer 112: 156 -164
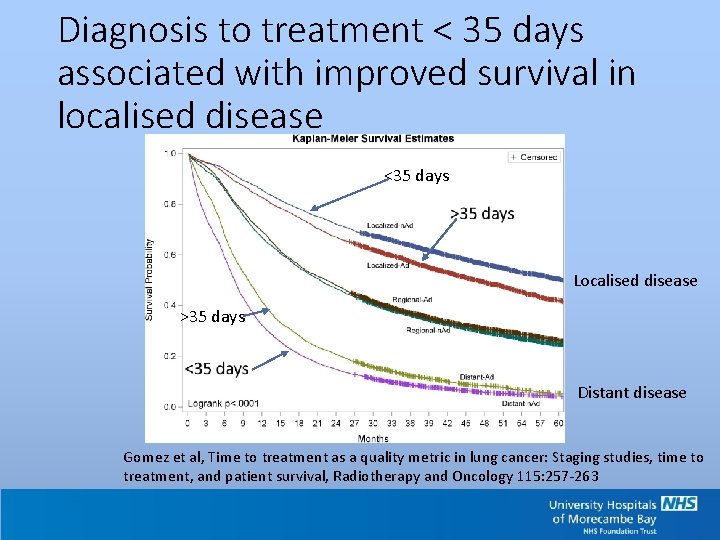
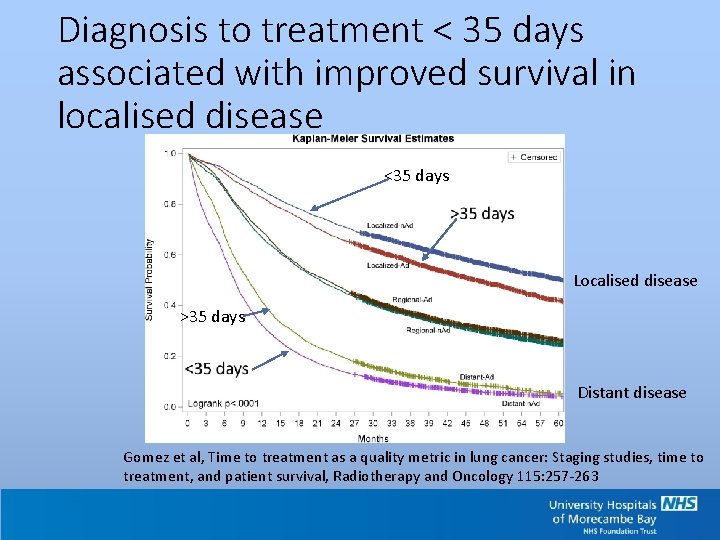
Diagnosis to treatment < 35 days associated with improved survival in localised disease <35 days Localised disease >35 days Distant disease Gomez et al, Time to treatment as a quality metric in lung cancer: Staging studies, time to treatment, and patient survival, Radiotherapy and Oncology 115: 257 -263
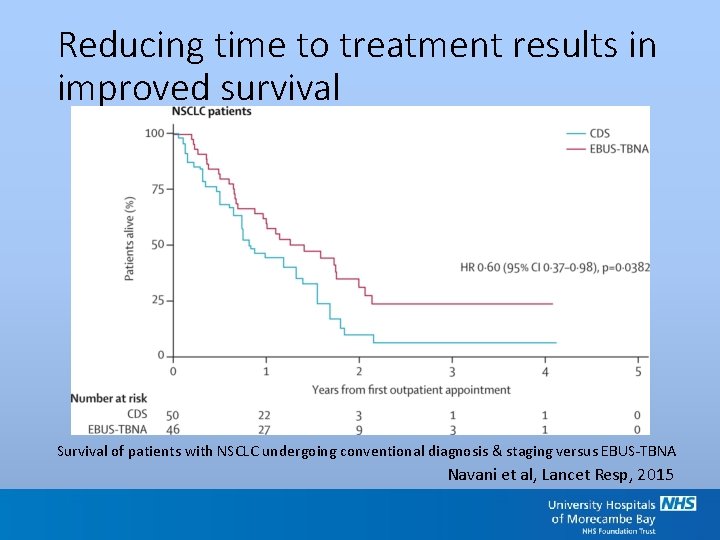
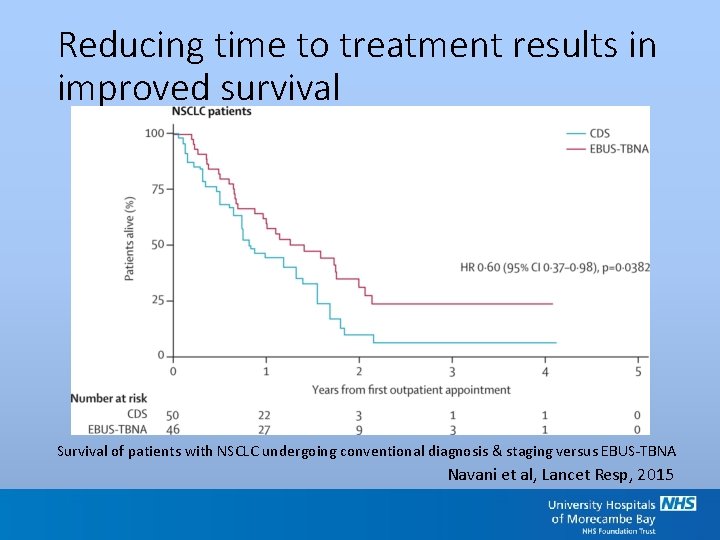
Reducing time to treatment results in improved survival Survival of patients with NSCLC undergoing conventional diagnosis & staging versus EBUS-TBNA Navani et al, Lancet Resp, 2015
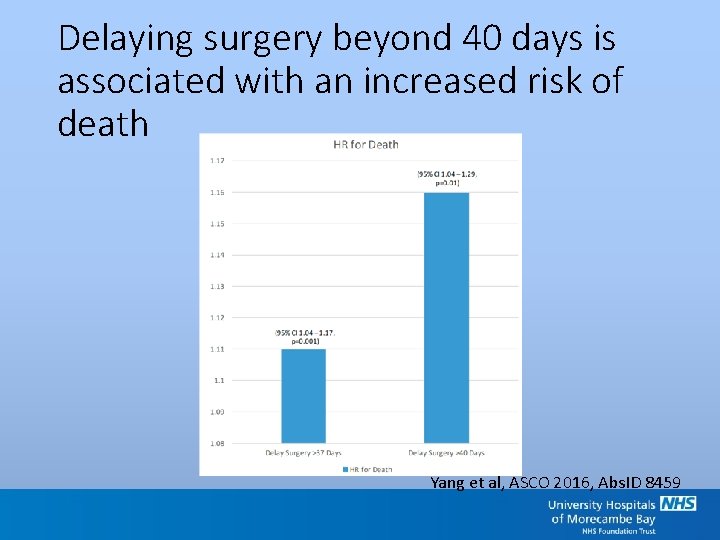
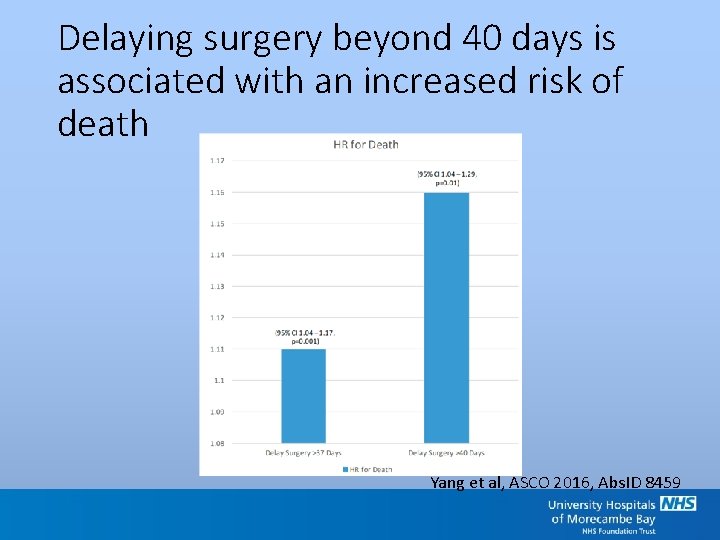
Delaying surgery beyond 40 days is associated with an increased risk of death Yang et al, ASCO 2016, Abs. ID 8459
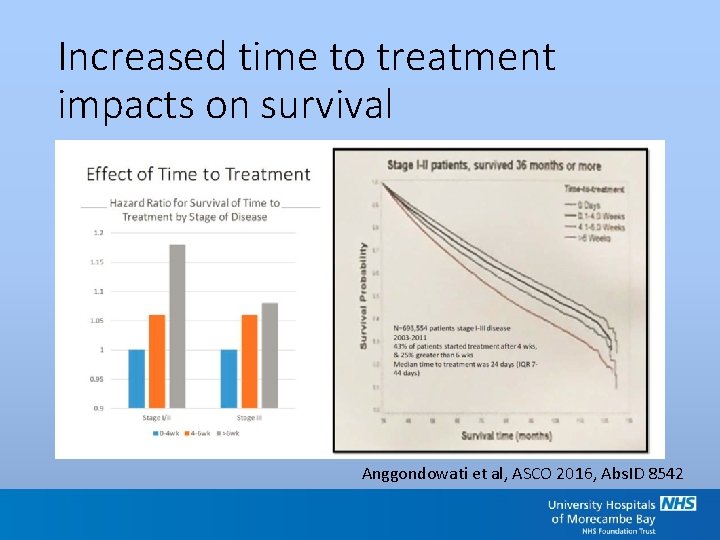
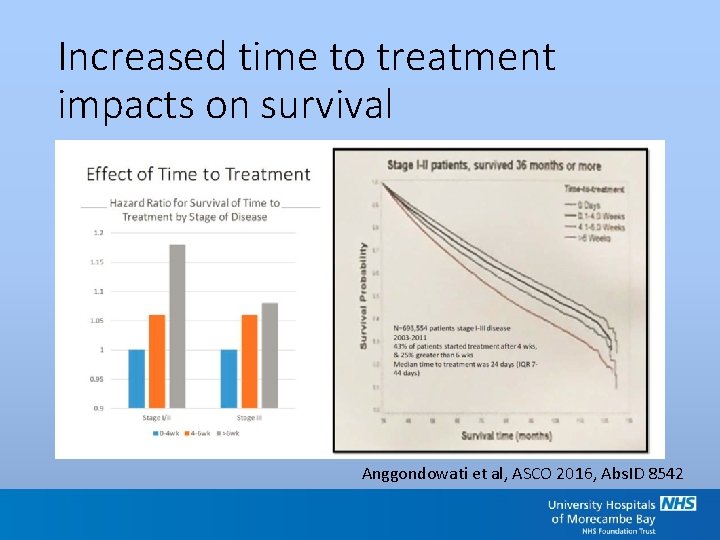
Increased time to treatment impacts on survival Anggondowati et al, ASCO 2016, Abs. ID 8542
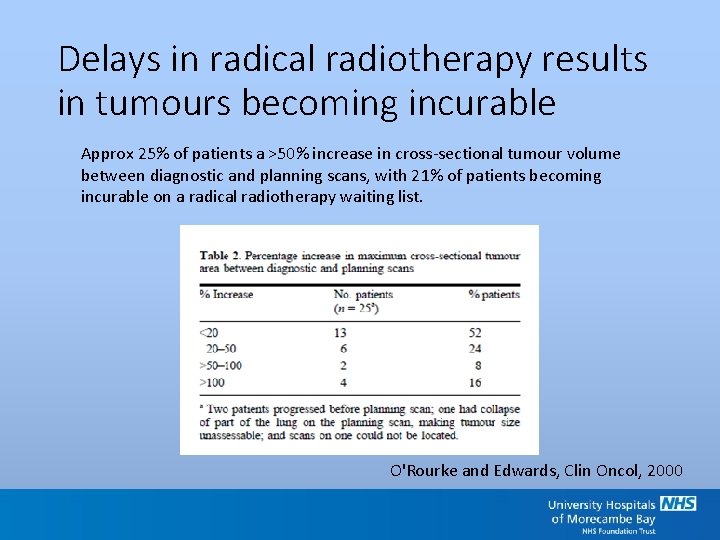
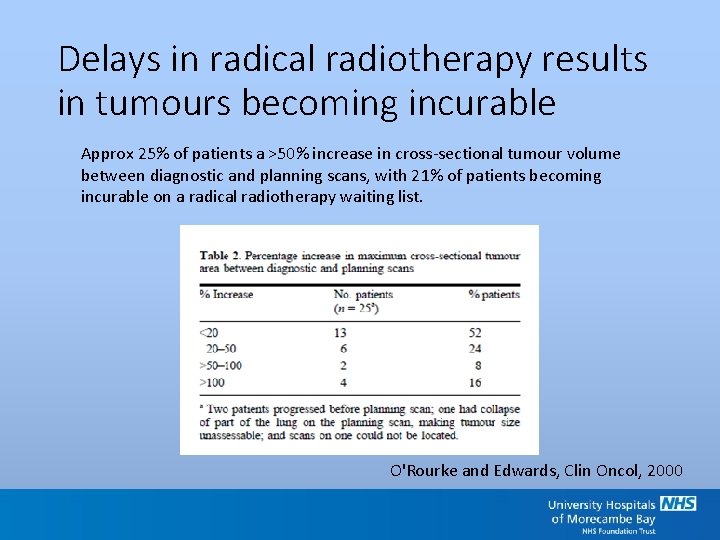
Delays in radical radiotherapy results in tumours becoming incurable Approx 25% of patients a >50% increase in cross-sectional tumour volume between diagnostic and planning scans, with 21% of patients becoming incurable on a radical radiotherapy waiting list. O'Rourke and Edwards, Clin Oncol, 2000
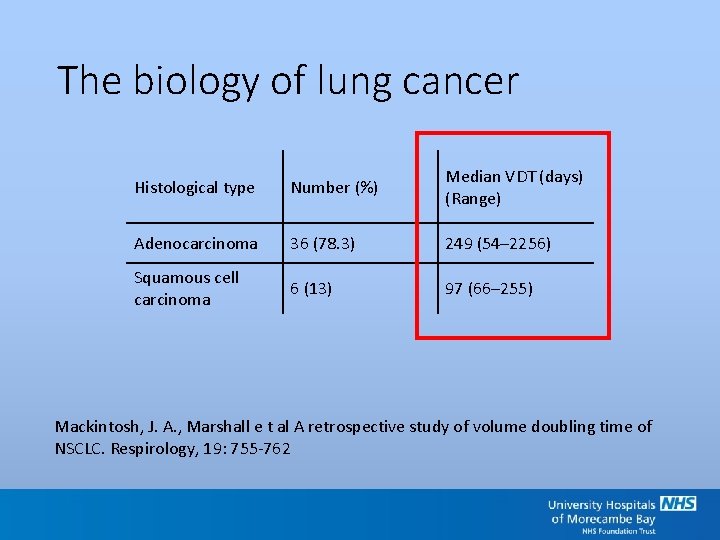
The biology of lung cancer Histological type Number (%) Median VDT (days) (Range) Adenocarcinoma 36 (78. 3) 249 (54– 2256) Squamous cell carcinoma 6 (13) 97 (66– 255) Mackintosh, J. A. , Marshall e t al A retrospective study of volume doubling time of NSCLC. Respirology, 19: 755 -762
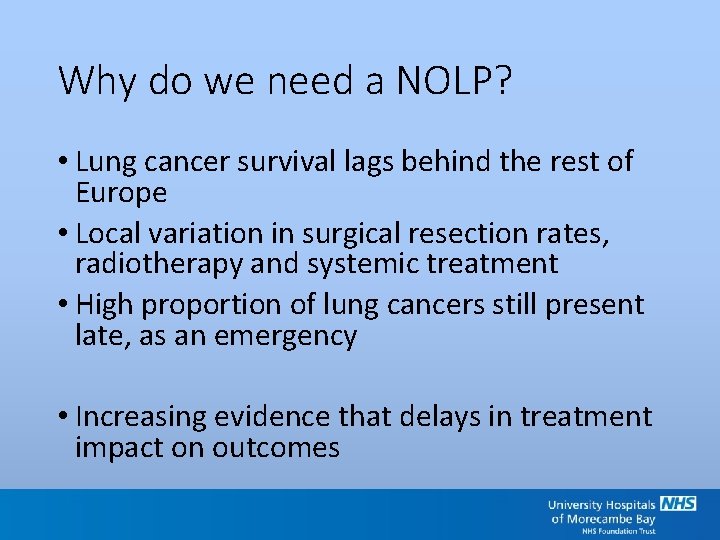
Why do we need a NOLP? • Lung cancer survival lags behind the rest of Europe • Local variation in surgical resection rates, radiotherapy and systemic treatment • High proportion of lung cancers still present late, as an emergency • Increasing evidence that delays in treatment impact on outcomes
Current pathway (UMBHT)
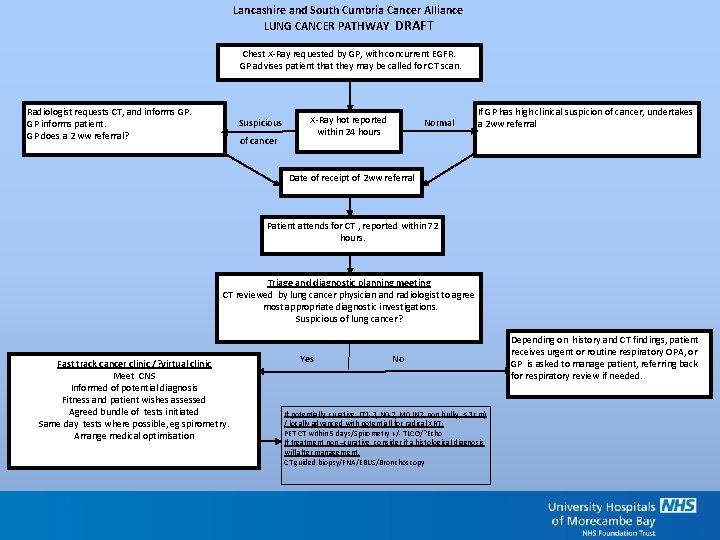
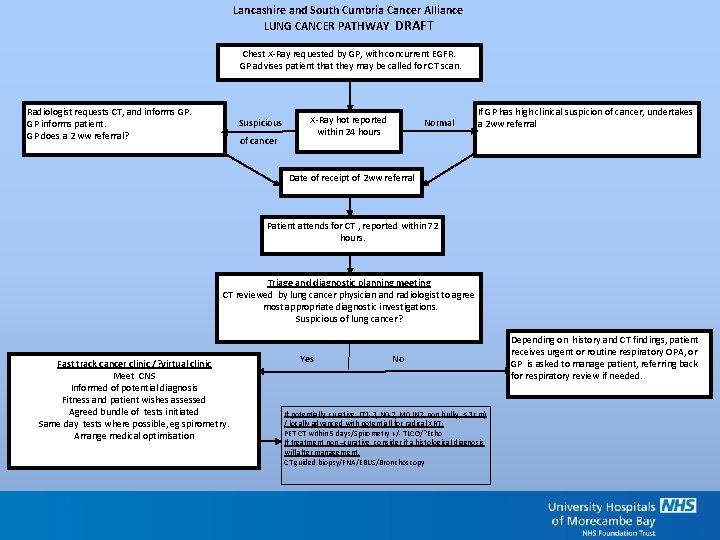
Lancashire and South Cumbria Cancer Alliance LUNG CANCER PATHWAY DRAFT Chest X-Ray requested by GP, with concurrent EGFR. GP advises patient that they may be called for CT scan. Radiologist requests CT, and informs GP. GP informs patient. GP does a 2 ww referral? Suspicious of cancer X-Ray hot reported within 24 hours Normal If GP has high clinical suspicion of cancer, undertakes a 2 ww referral Date of receipt of 2 ww referral Patient attends for CT , reported within 72 hours. Triage and diagnostic planning meeting CT reviewed by lung cancer physician and radiologist to agree most appropriate diagnostic investigations. Suspicious of lung cancer? Fast track cancer clinic /? virtual clinic Meet CNS Informed of potential diagnosis Fitness and patient wishes assessed Agreed bundle of tests initiated Same day tests where possible, eg spirometry. Arrange medical optimisation Yes No If potentially curative (T 1 -3, N 0 -2, M 0 (N 2 non bulky, < 3 cm) / locally advanced with potentiall for radical XRT; PET CT within 5 days/Spirometry +/- TLCO/? Echo If treatment non –curative, consider if a histological diagnosis will alter management. CT guided biopsy/FNA/EBUS/Bronchoscopy Depending on history and CT findings, patient receives urgent or routine respiratory OPA, or GP is asked to manage patient, referring back for respiratory review if needed.
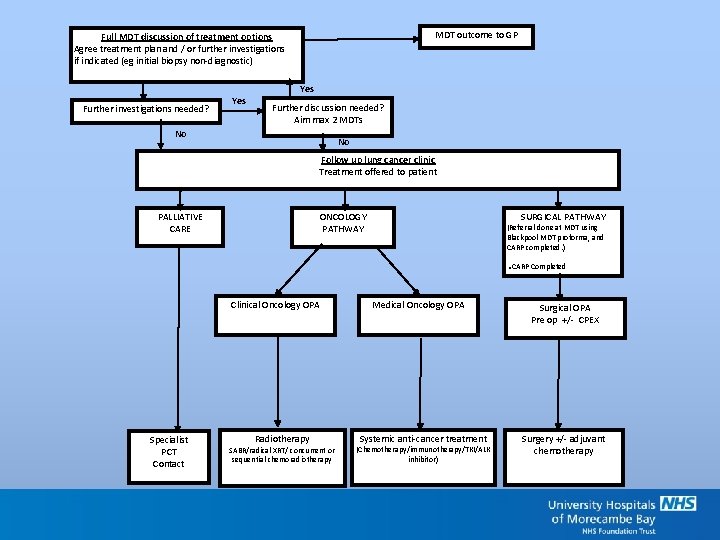
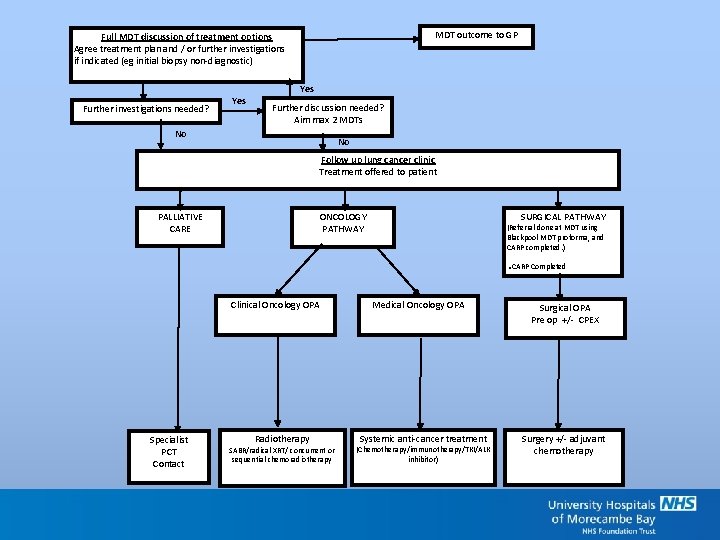
MDT outcome to GP Full MDT discussion of treatment options Agree treatment plan and / or further investigations if indicated (eg initial biopsy non-diagnostic) Further investigations needed? Yes Further discussion needed? Aim max 2 MDTs No No Follow up lung cancer clinic Treatment offered to patient ONCOLOGY PATHWAY PALLIATIVE CARE SURGICAL PATHWAY (Referral done at MDT using Blackpool MDT proforma, and CARP completed. ) . CARP Completed Clinical Oncology OPA Specialist PCT Contact Radiotherapy SABR/radical XRT/ concurrent or sequential chemoradiotherapy Medical Oncology OPA Systemic anti-cancer treatment (Chemotherapy/immunotherapy/TKI/ALK inhibitor) Surgical OPA Pre op +/- CPEX Surgery +/- adjuvant chemotherapy
Challenges
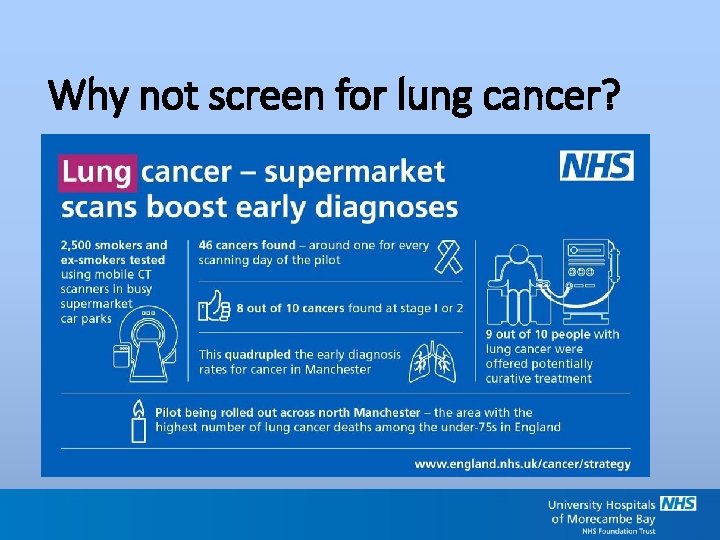
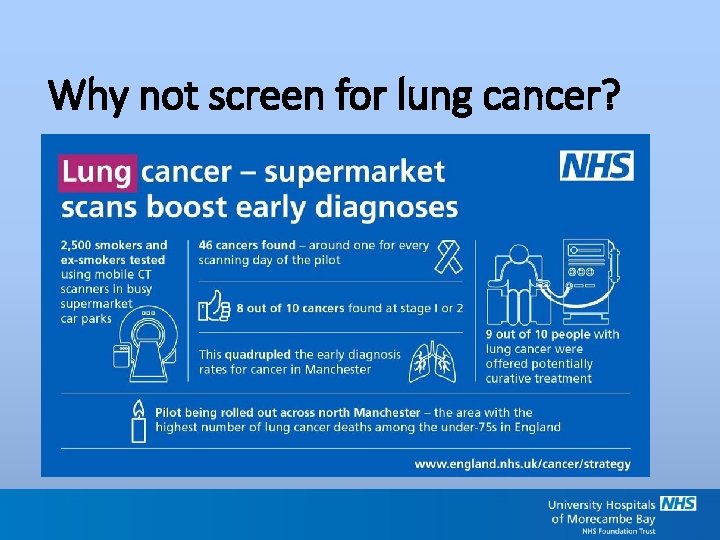
Why not screen for lung cancer?
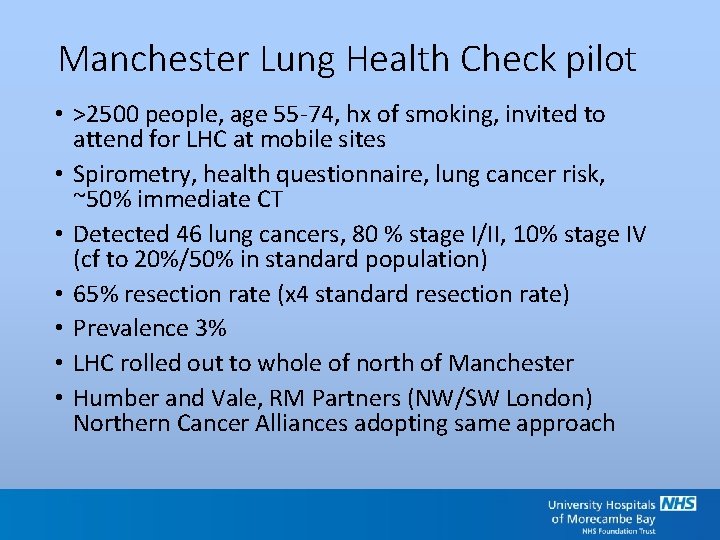
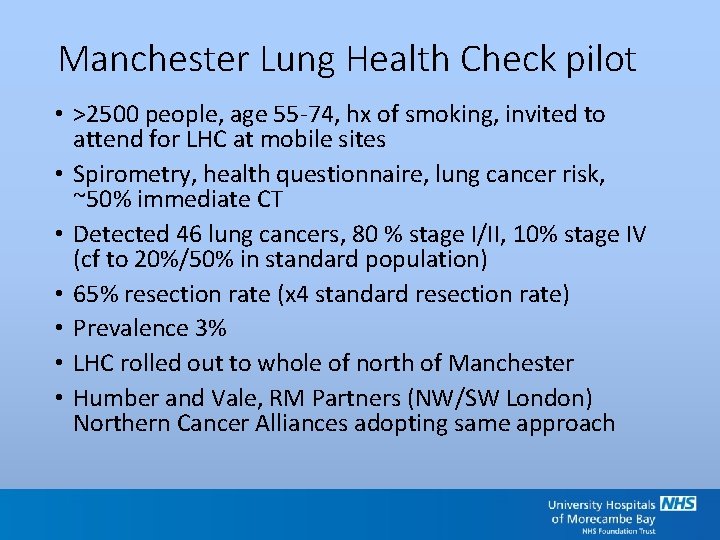
Manchester Lung Health Check pilot • >2500 people, age 55 -74, hx of smoking, invited to attend for LHC at mobile sites • Spirometry, health questionnaire, lung cancer risk, ~50% immediate CT • Detected 46 lung cancers, 80 % stage I/II, 10% stage IV (cf to 20%/50% in standard population) • 65% resection rate (x 4 standard resection rate) • Prevalence 3% • LHC rolled out to whole of north of Manchester • Humber and Vale, RM Partners (NW/SW London) Northern Cancer Alliances adopting same approach
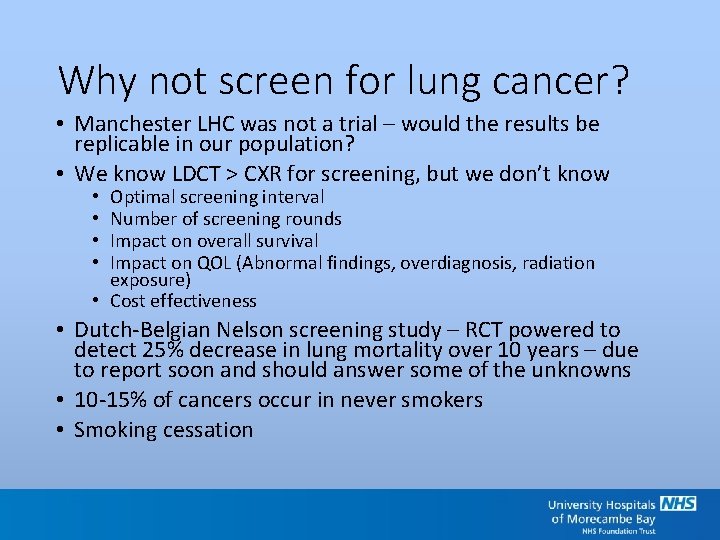
Why not screen for lung cancer? • Manchester LHC was not a trial – would the results be replicable in our population? • We know LDCT > CXR for screening, but we don’t know Optimal screening interval Number of screening rounds Impact on overall survival Impact on QOL (Abnormal findings, overdiagnosis, radiation exposure) • Cost effectiveness • • • Dutch-Belgian Nelson screening study – RCT powered to detect 25% decrease in lung mortality over 10 years – due to report soon and should answer some of the unknowns • 10 -15% of cancers occur in never smokers • Smoking cessation
Questions/comments? Amy. ford@mbht. nhs. uk
 Dr. amy ford
Dr. amy ford Optimal lung cancer pathway
Optimal lung cancer pathway A dermatologist and an oncologist both provide
A dermatologist and an oncologist both provide Sarah slater md
Sarah slater md Dr. dalia kamel
Dr. dalia kamel California medical license application
California medical license application Gbmc medical records
Gbmc medical records Difference between medical report and medical certificate
Difference between medical report and medical certificate Torrance memorial lab manhattan beach
Torrance memorial lab manhattan beach Cartersville medical center medical records
Cartersville medical center medical records National board of certified medical interpreters
National board of certified medical interpreters National ambulatory medical care survey
National ambulatory medical care survey Abu ali sina university peshawar
Abu ali sina university peshawar M.gorky donetsk national medical university
M.gorky donetsk national medical university Seoul national university history
Seoul national university history Mongolian national university of medical sciences
Mongolian national university of medical sciences National unification and the national state
National unification and the national state Socially optimal quantity
Socially optimal quantity Optimal arousal theory
Optimal arousal theory What is optimal policy in reinforcement learning
What is optimal policy in reinforcement learning Optimal arousal theory
Optimal arousal theory Post optimal
Post optimal Product availability is a measure of
Product availability is a measure of Contoh soal anggaran modal optimal
Contoh soal anggaran modal optimal Fifo page replacement calculator
Fifo page replacement calculator Contoh portofolio optimal
Contoh portofolio optimal 300 är optimal
300 är optimal Optimal risky portfolio formula
Optimal risky portfolio formula Cost of capital
Cost of capital Nutritional status assessment
Nutritional status assessment Hunger games hierarchy
Hunger games hierarchy Kriteria penjadualan yang optimal terdiri dari ?
Kriteria penjadualan yang optimal terdiri dari ? Saldo kas optimal model baumol
Saldo kas optimal model baumol Optimum inventory level
Optimum inventory level Wwu optimal resume
Wwu optimal resume Pareto-optimal
Pareto-optimal