RADIOLOGY OF RESPIRATORY SYSTEM Weizhong Cheng Dept Radiology






























- Slides: 90

RADIOLOGY OF RESPIRATORY SYSTEM Weizhong Cheng Dept. Radiology, Zhongshan Hospital Institute of Medical Imaging, Shanghai
AIMS • Basics • Best exam results • Appreciate the role radiology plays • ? Instill an interest in radiology

BEFORE CLASS: Textbook Reference Literature book Internet Apps Teacher & classmate Histology and Embryology Anatomy Pathology Internal Medicine Surgery Gynecology Pediatrics Neurology 。。。 Everything。。。U need to know

METHODS X-ray CT MR DSA US Nuclear Medicine PET/CT Radionuclide ventilation perfusion imaging

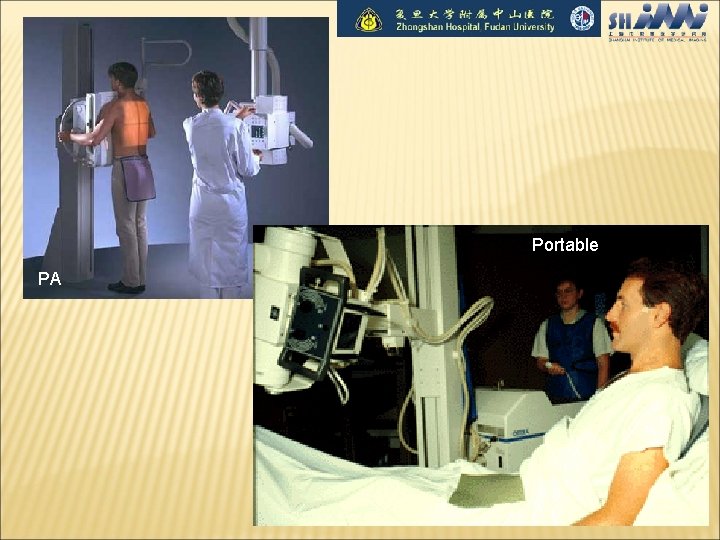
X-RAY TECHNIQUES PA (posteroanterior) & Lateral More information Two views Standardized Distance Pt needs to be stable Portable Quick Anywhere One shot No standardization
Portable PA
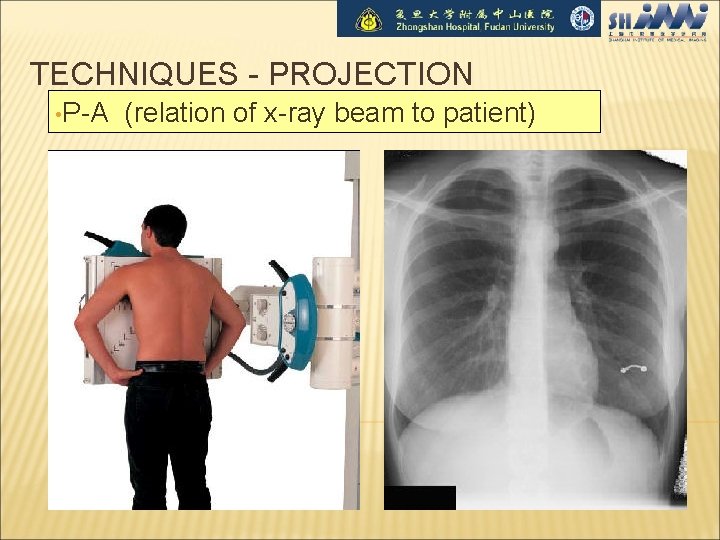
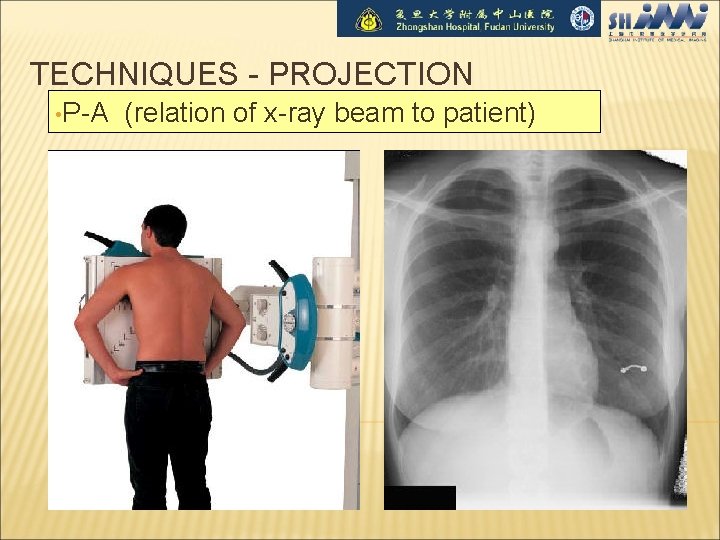
TECHNIQUES - PROJECTION • P-A (relation of x-ray beam to patient)
TECHNIQUES - PROJECTION (CONTINUED) • A-P Supine/Erect
TECHNIQUES - PROJECTION (CONTINUED) • Lateral
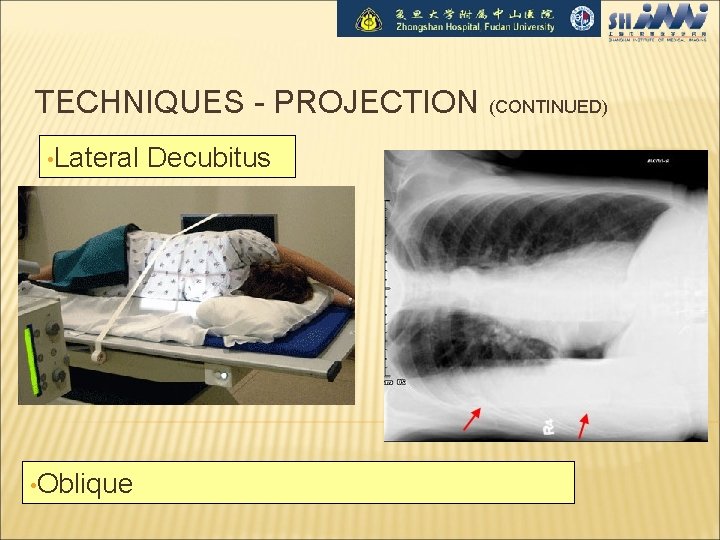
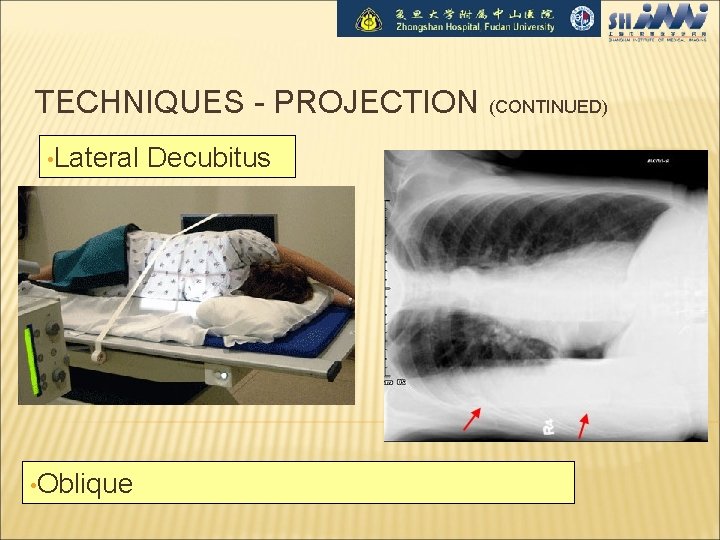
TECHNIQUES - PROJECTION (CONTINUED) • Lateral • Oblique Decubitus
TECHNICAL DETAILS • Type • Orientation • Rotation • Inspiration/expiration • Penetration
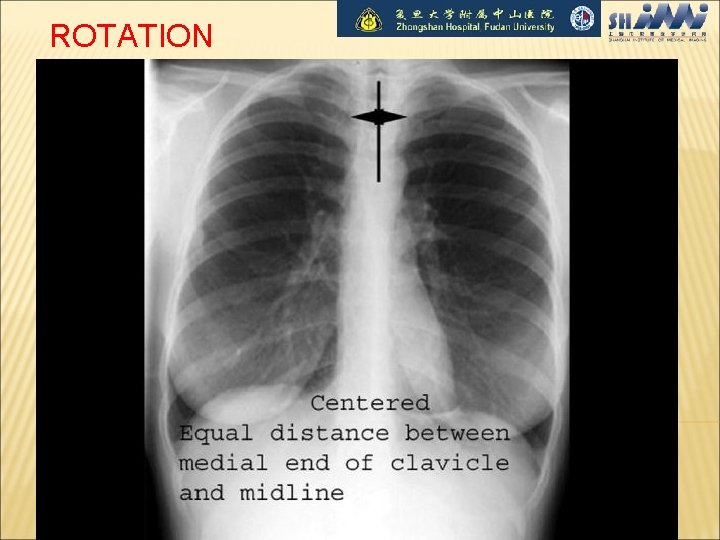
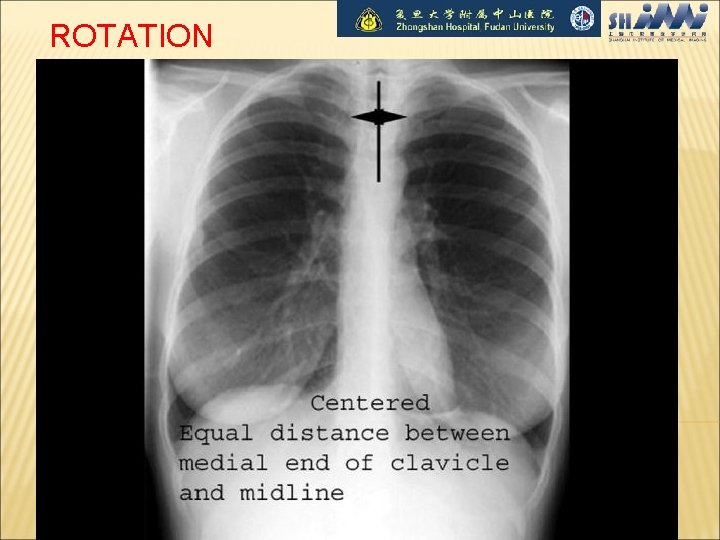
ROTATION

ROTATION (CONTINUED)

PENETRATION
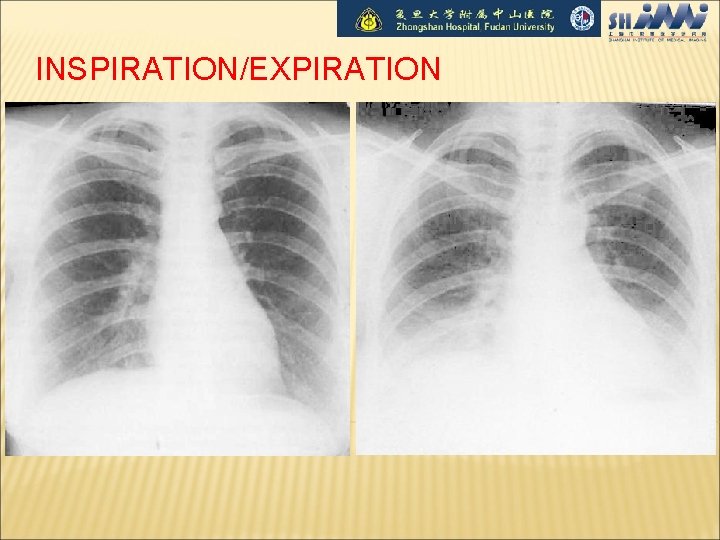
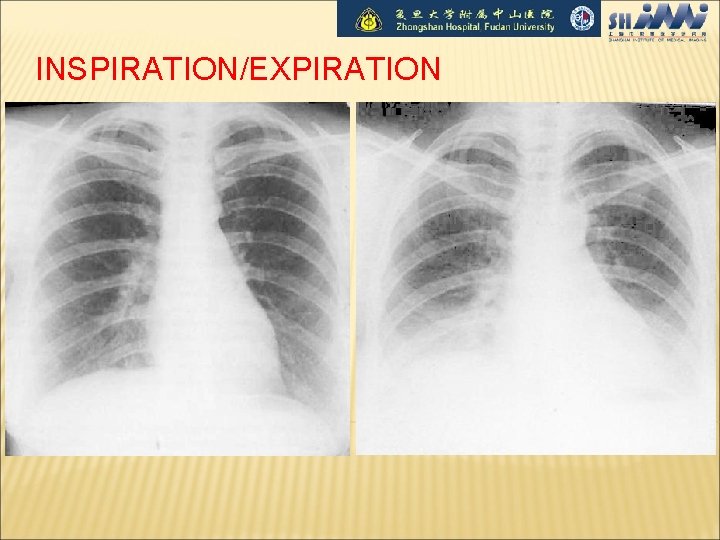
INSPIRATION/EXPIRATION
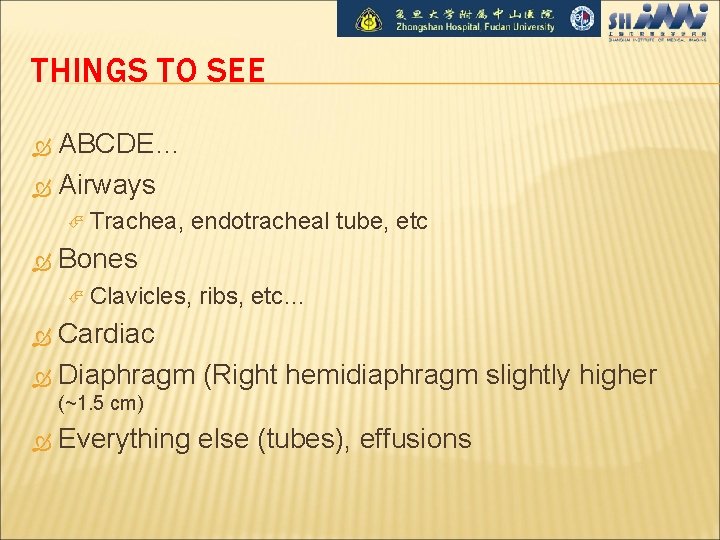
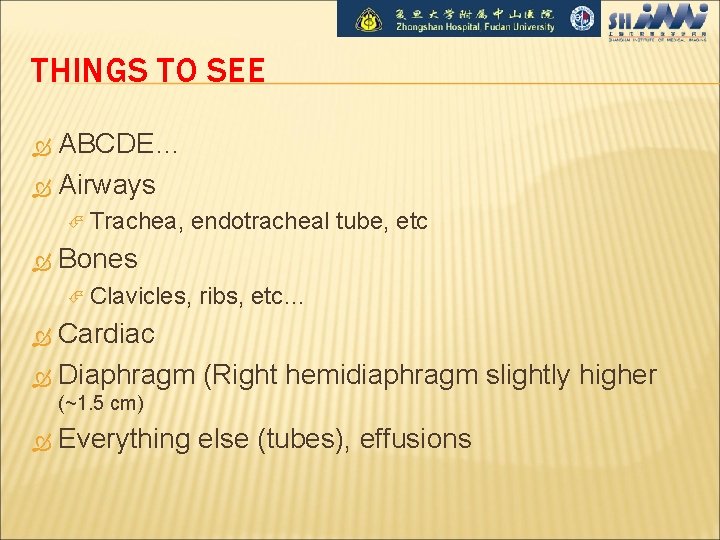
THINGS TO SEE ABCDE… Airways Trachea, endotracheal tube, etc Bones Clavicles, ribs, etc… Cardiac Diaphragm (Right hemidiaphragm slightly higher (~1. 5 cm) Everything else (tubes), effusions




DENSITIES The big two densities are: (1) WHITE - Bone (2) BLACK - Air The others are: (3) DARK GREY- Fat (4) GREY- Soft tissue/water And if anything Man-made is on the film, it is: (5) BRIGHT WHITE - Man-made
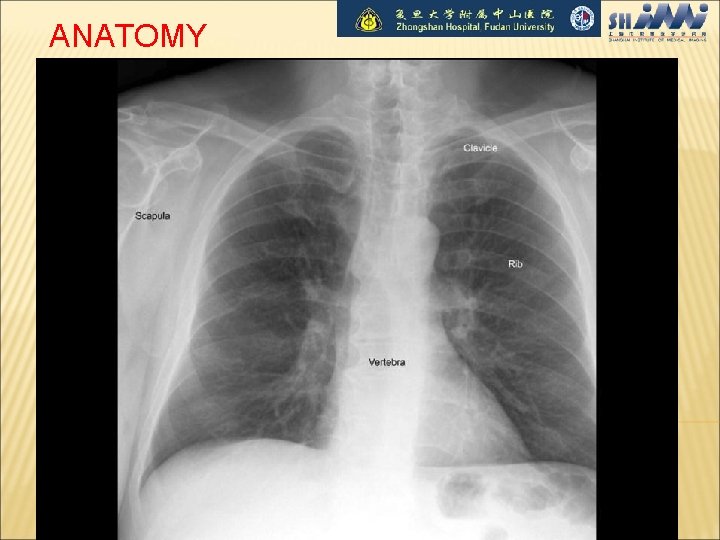
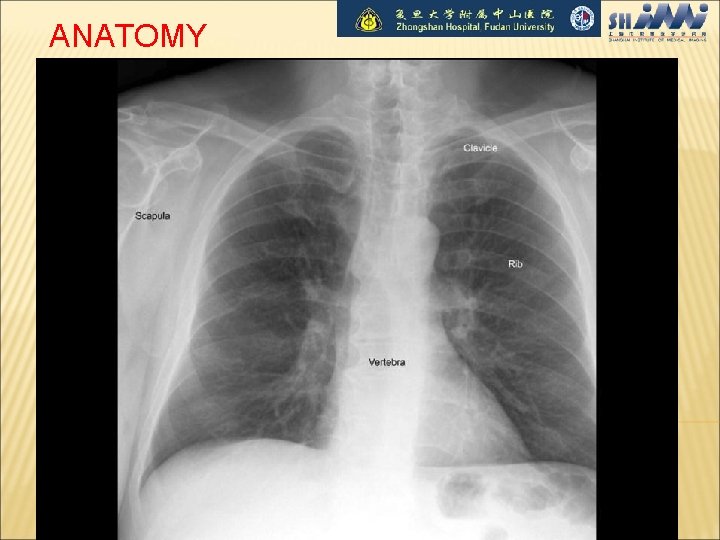
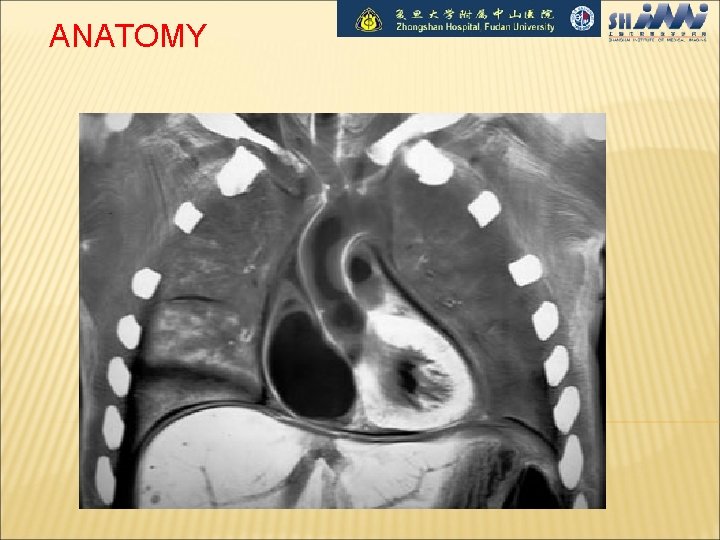
ANATOMY
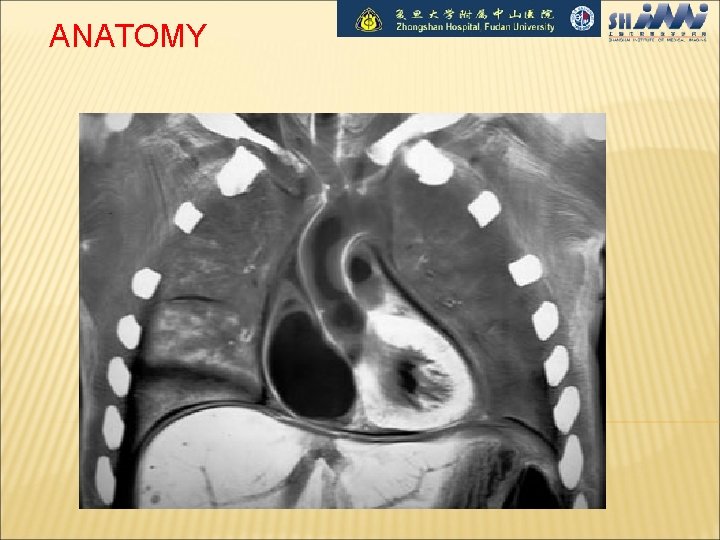
ANATOMY
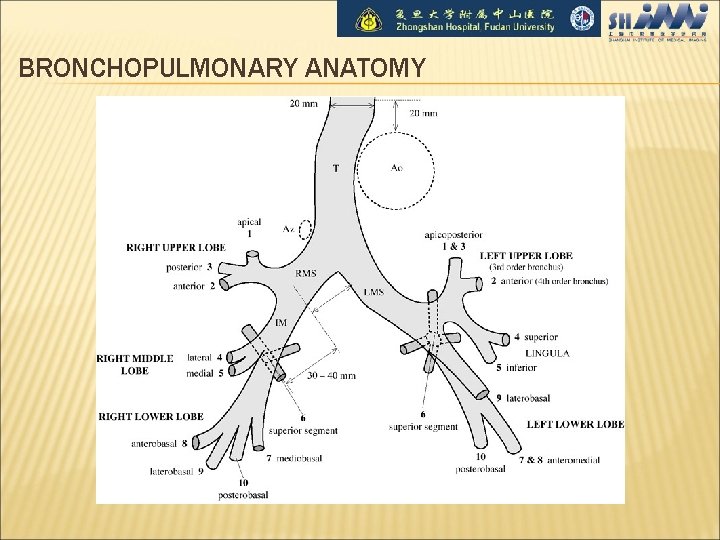
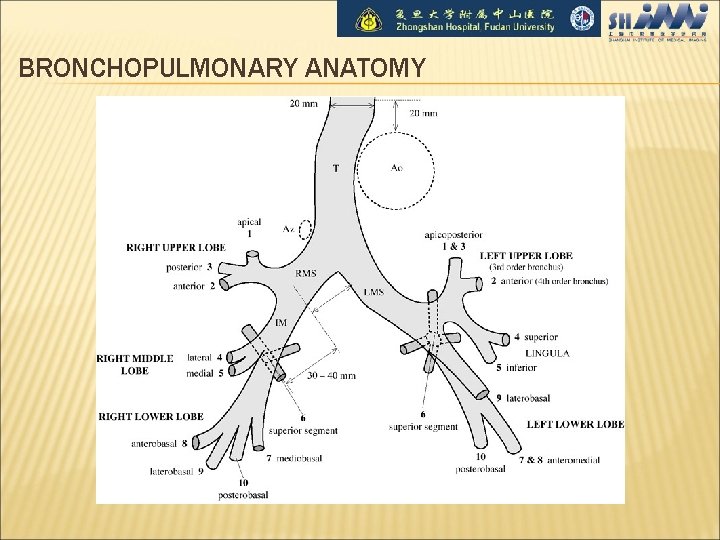
BRONCHOPULMONARY ANATOMY
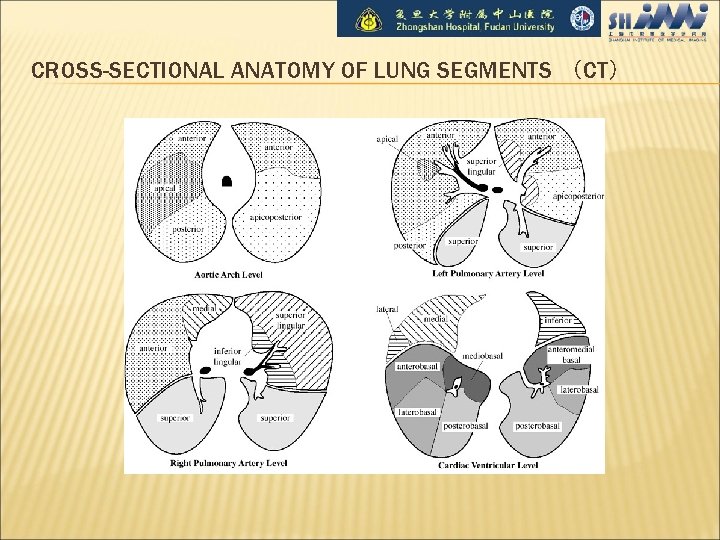
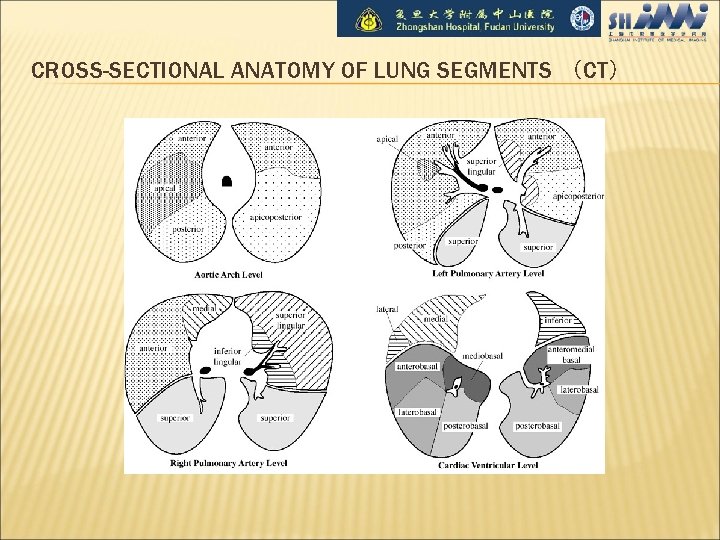
CROSS-SECTIONAL ANATOMY OF LUNG SEGMENTS (CT)

LOBES • Right upper lobe:
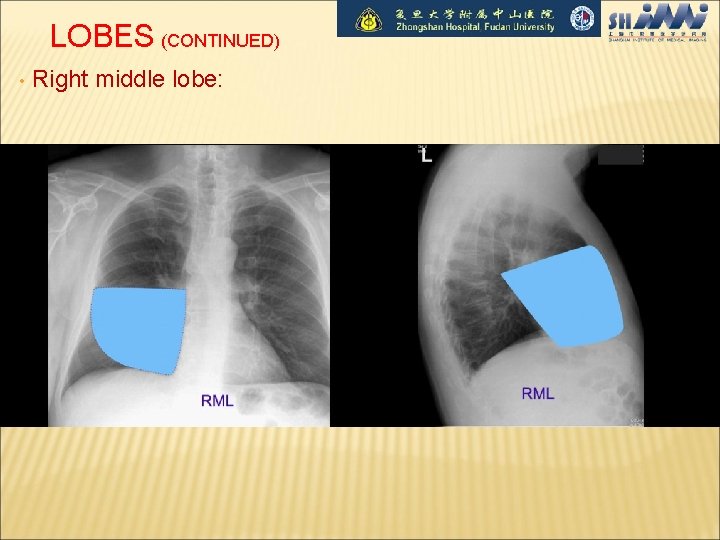
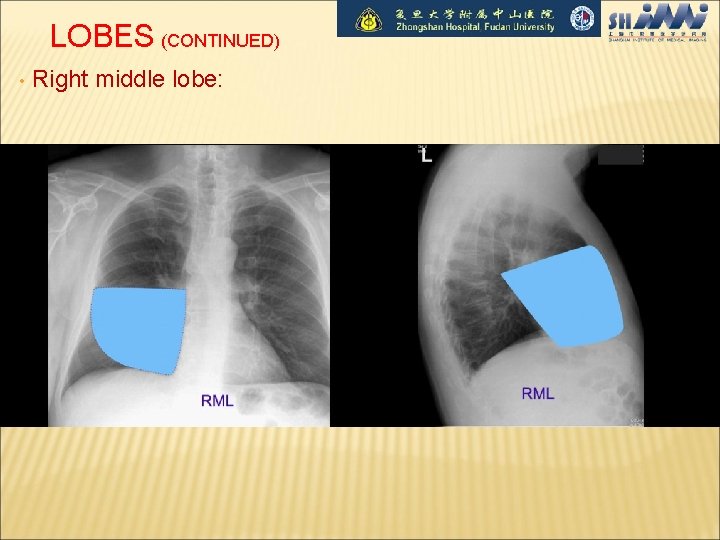
LOBES (CONTINUED) • Right middle lobe:
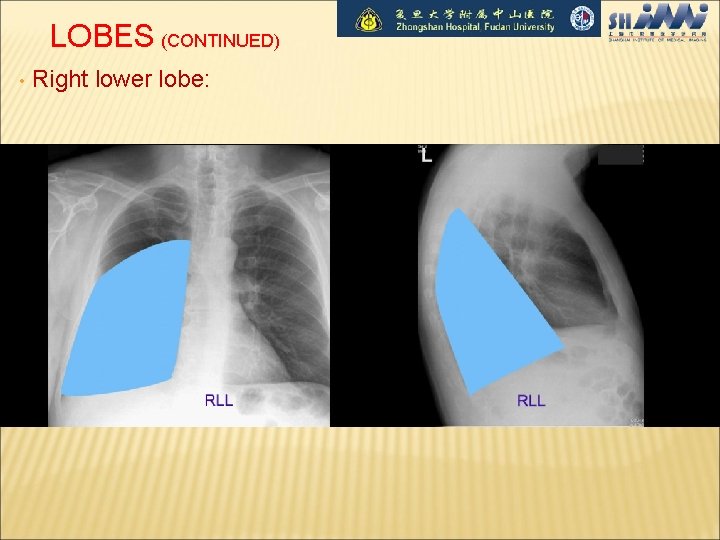
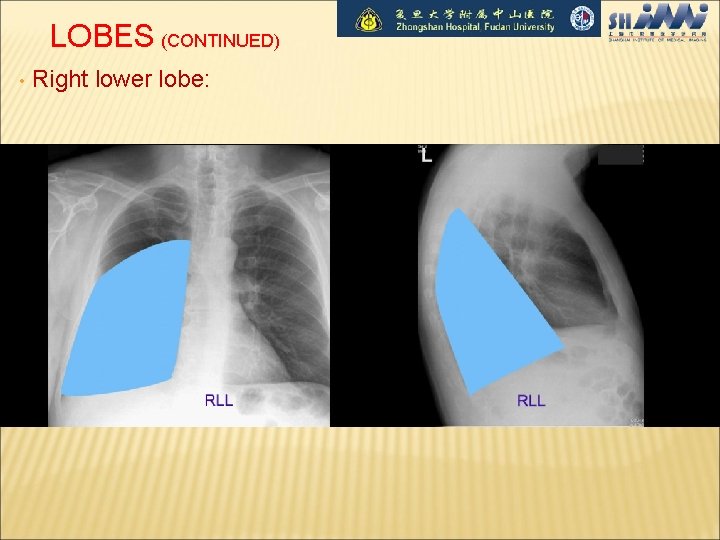
LOBES (CONTINUED) • Right lower lobe:
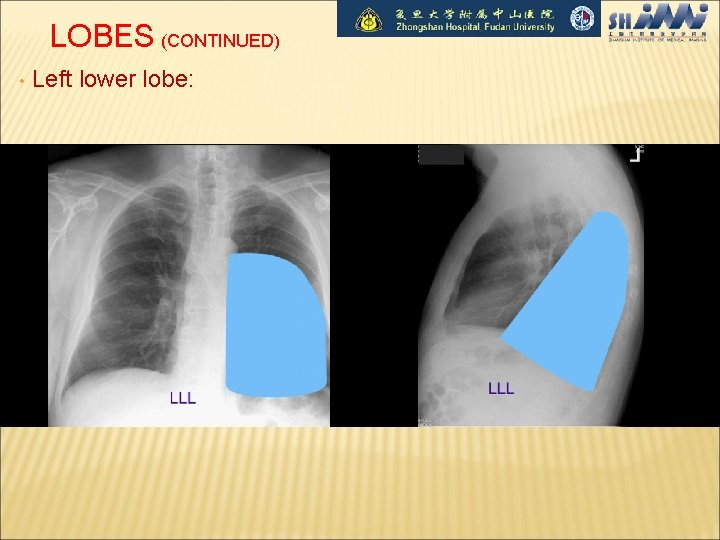
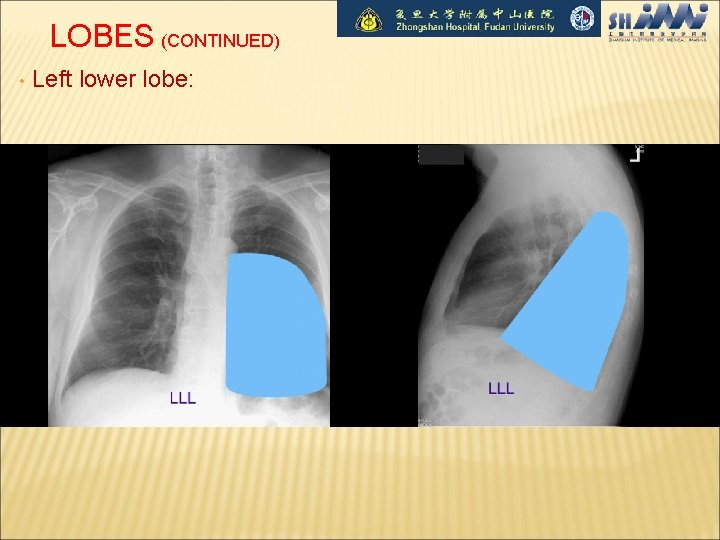
LOBES (CONTINUED) • Left lower lobe:
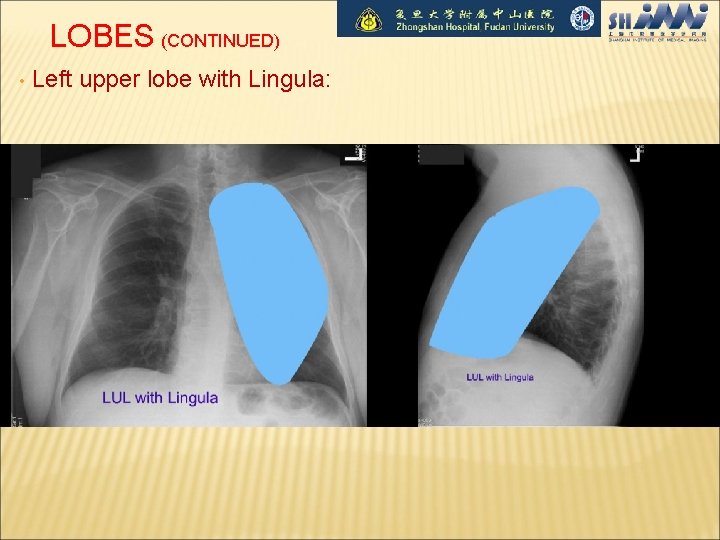
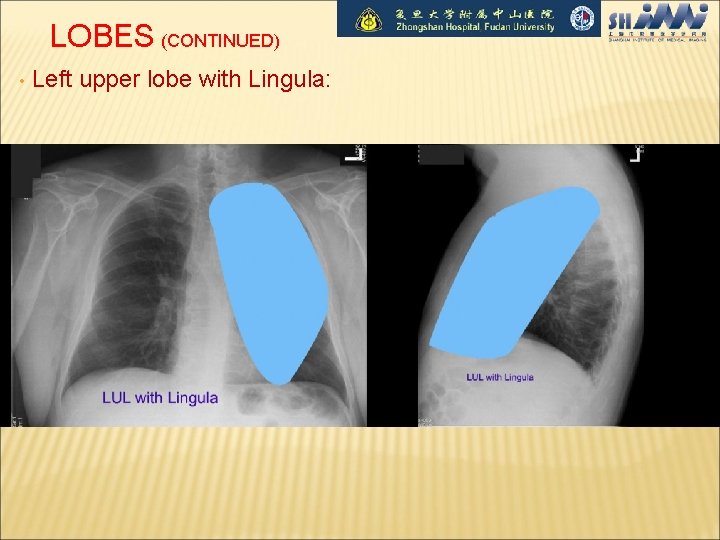
LOBES (CONTINUED) • Left upper lobe with Lingula:
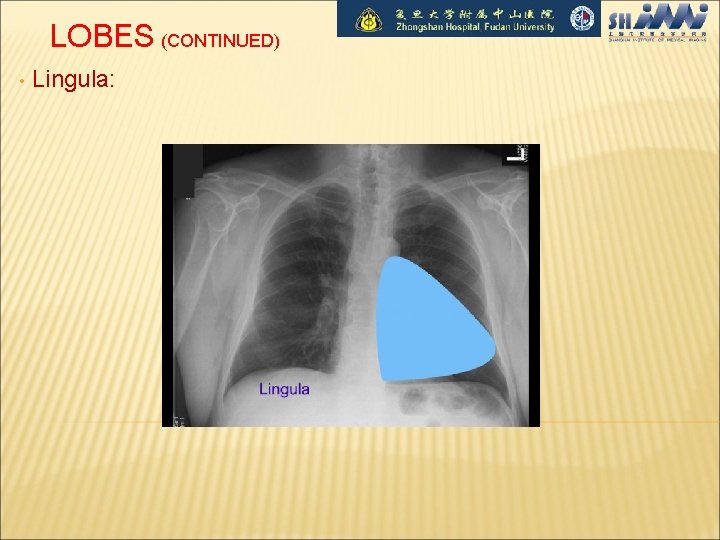
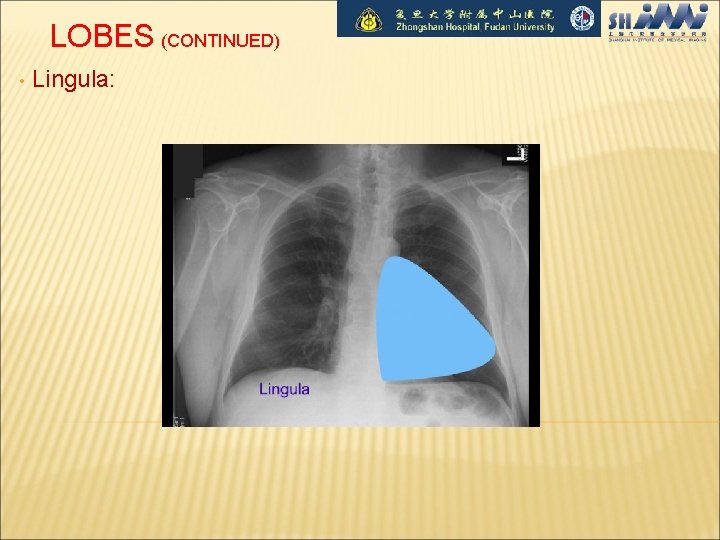
LOBES (CONTINUED) • Lingula:
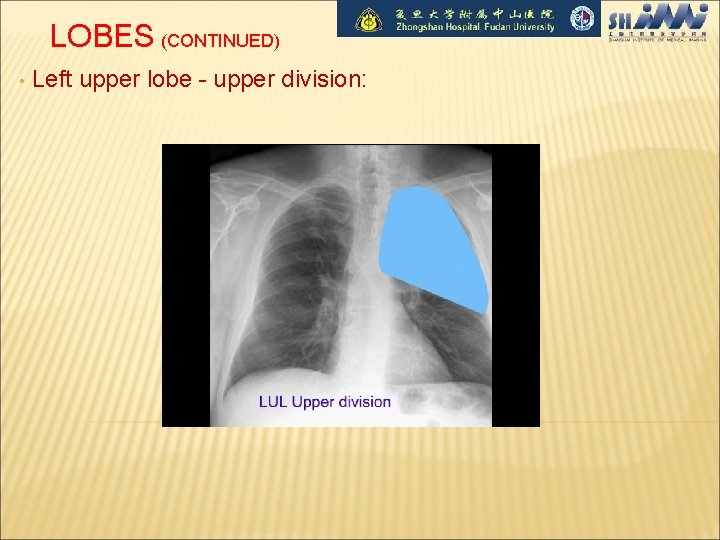
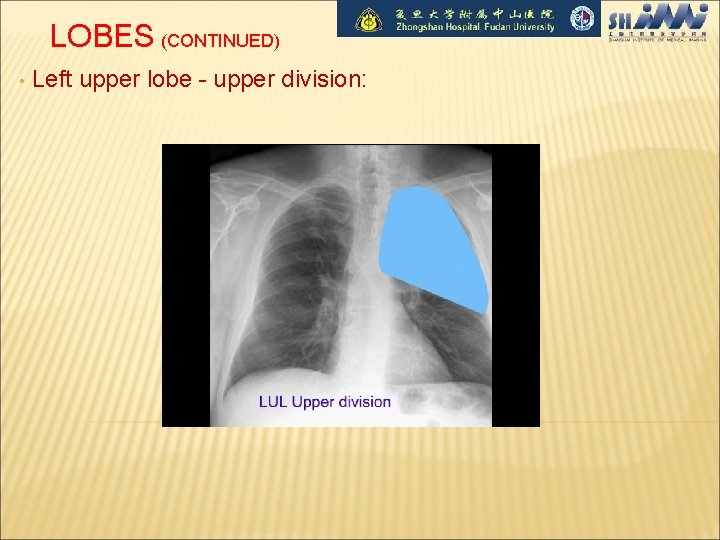
LOBES (CONTINUED) • Left upper lobe - upper division:
HEART Right border: Edge of (r) Atrium 3. Left border: (l) Ventricle + Atrium 4. Posterior border: Reft Ventricle 5. Anterior border: Right Ventricle

HEART (CONTINUED 。。。。)
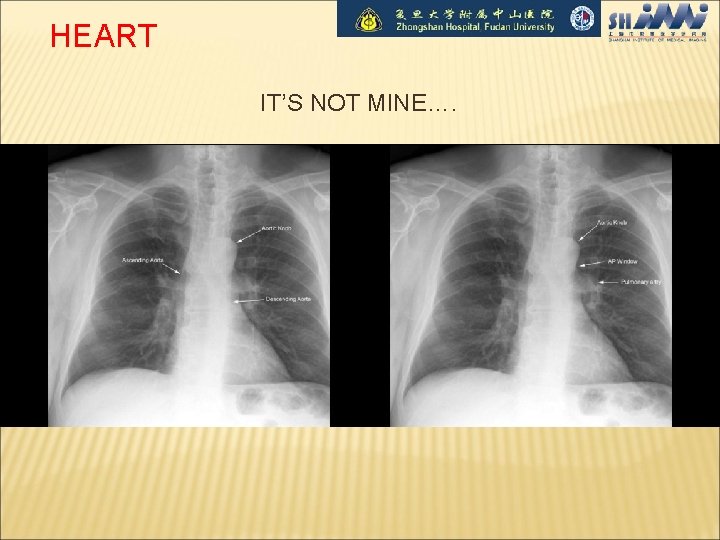
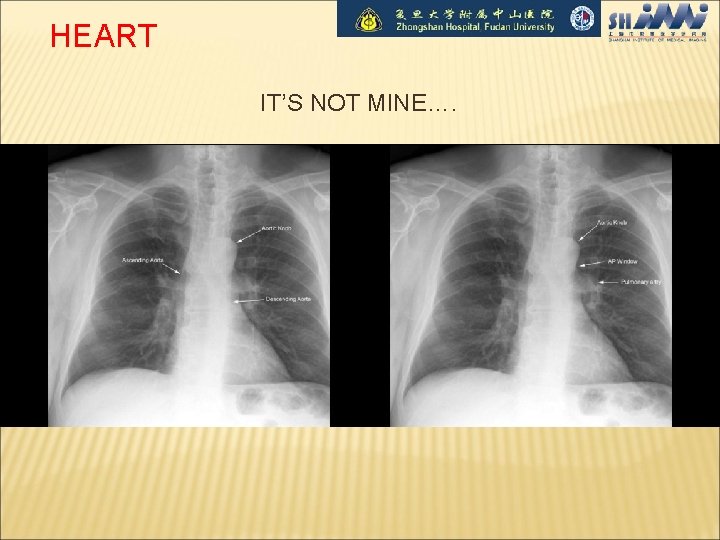
HEART IT’S NOT MINE….
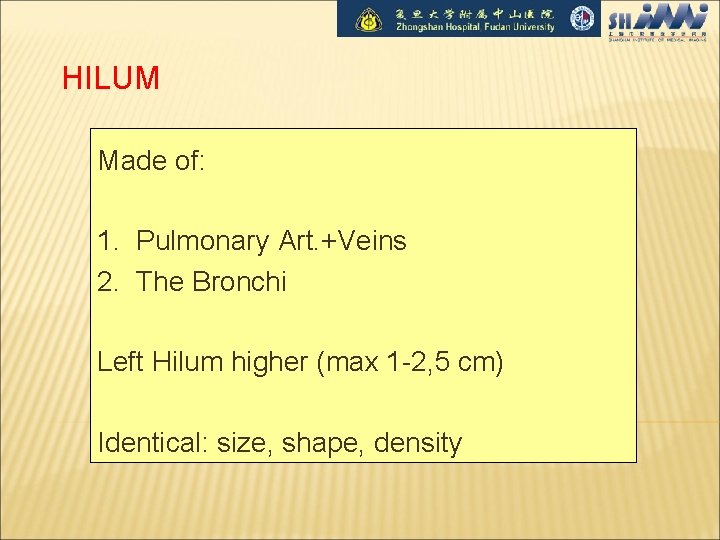
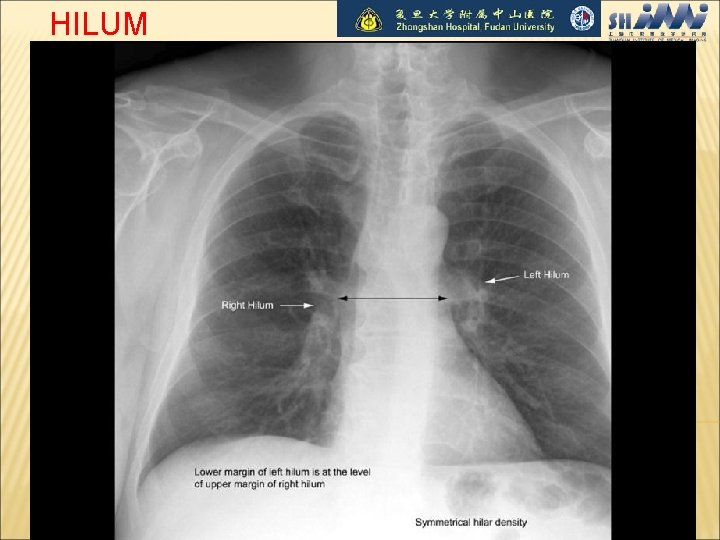
HILUM Made of: 1. Pulmonary Art. +Veins 2. The Bronchi Left Hilum higher (max 1 -2, 5 cm) Identical: size, shape, density
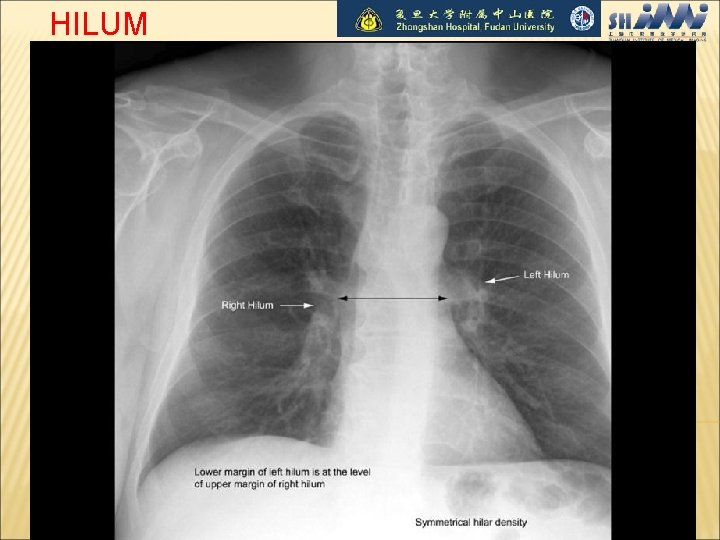
HILUM
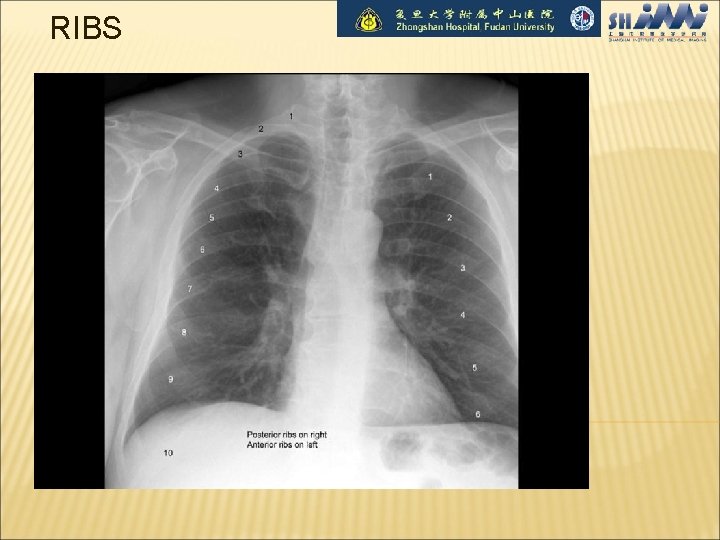
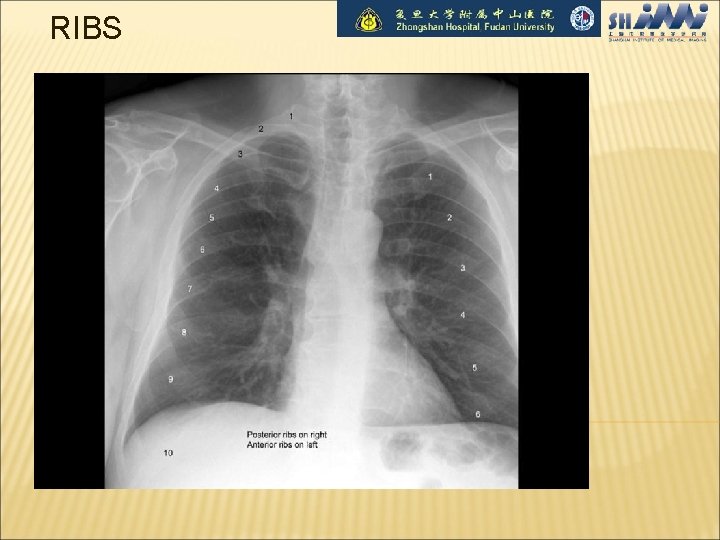
RIBS
REVIEW AREAS: Apices • Behind the heart • Costophrenic angle (CPA) • Below the diaphragm • Soft tissues ( breast, surgical emphysema) • Ribs & clavicle • Vertebrae •
ABNORMALS
LUNG FINDINGS Darker areas Lighter areas radiolucent Opacities Pneumothorax Atelectasis Cysts/bulla “infiltrates” Air bronchograms Blood Pus Water Nodules or mass
OPACITIES Lobar or not…. Pneumonia Pulmonary Edema “fluffy, ” diffuse, “bat wing” distribution Hemorrhage Can’t tell by x-ray, need bronch

RML pneumonia Opacities
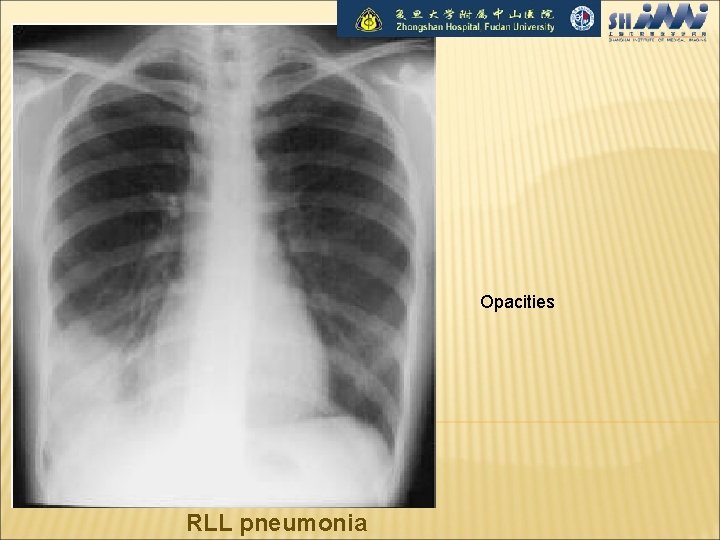
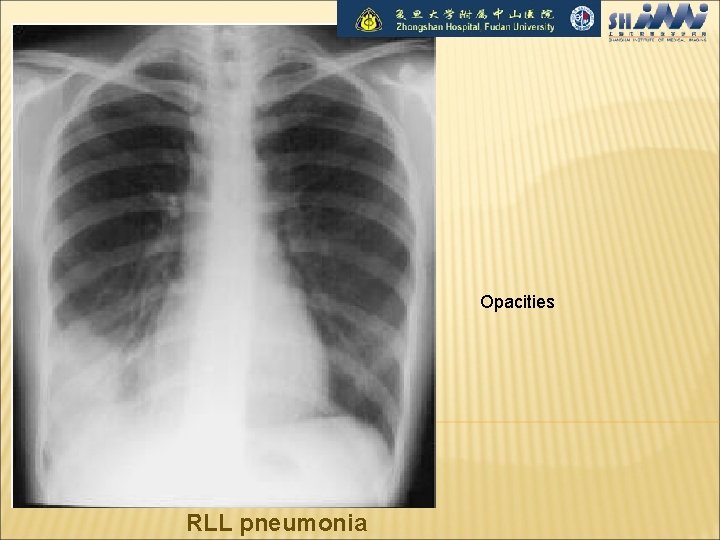
Opacities RLL pneumonia
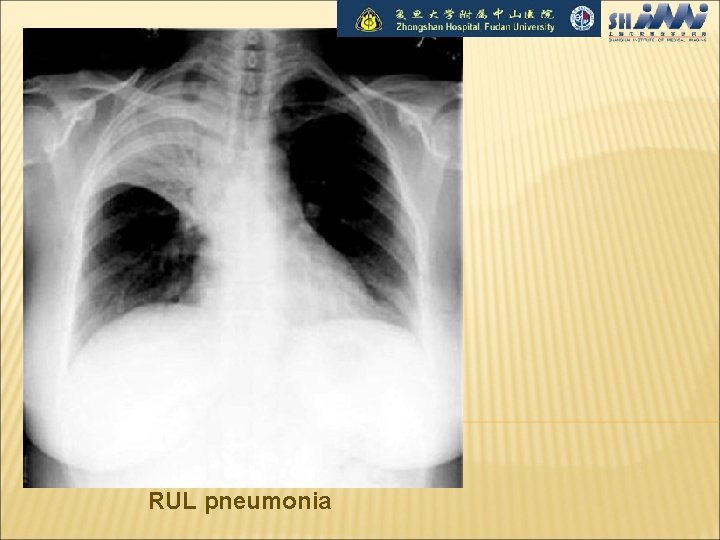
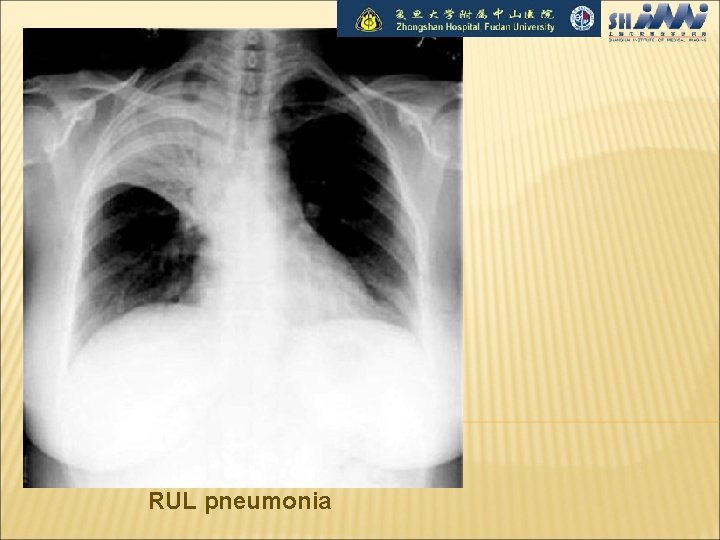
RUL pneumonia

LLL pneumonia
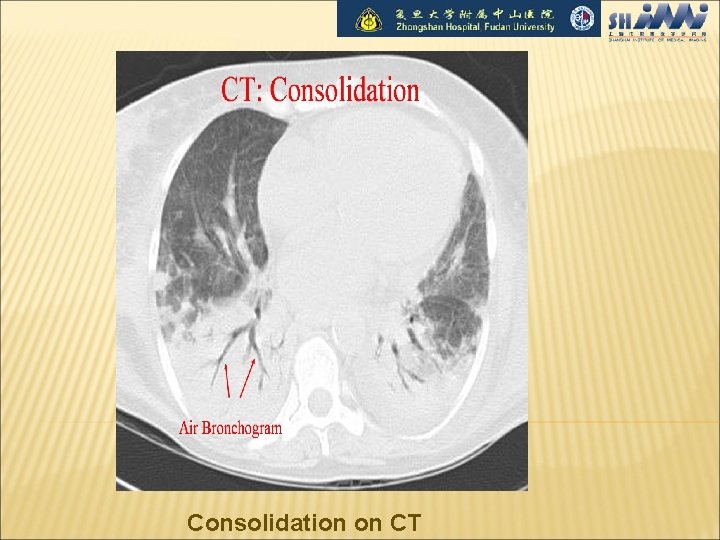
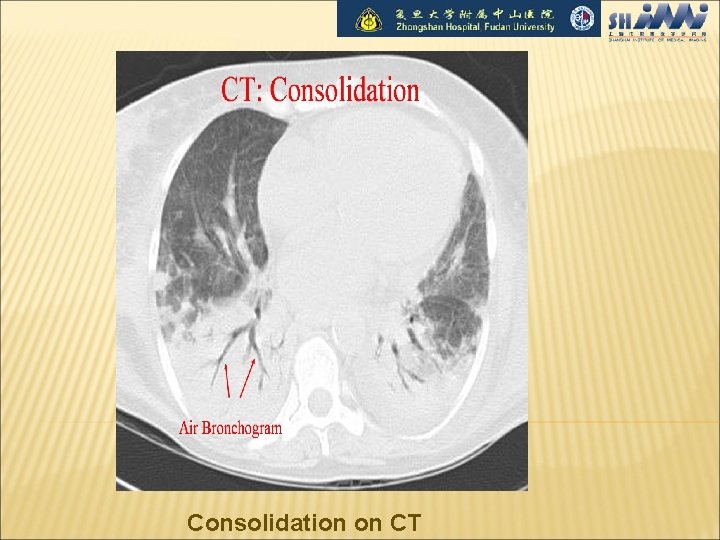
Consolidation on CT
THE ENLARGED HILA Causes: 1. Adenopathies (neoplasia, infection) 2. Primary Tumor 3. Vascular 4. Sarcoidosis

Mass

Hilar Lymphadenopathy - BL
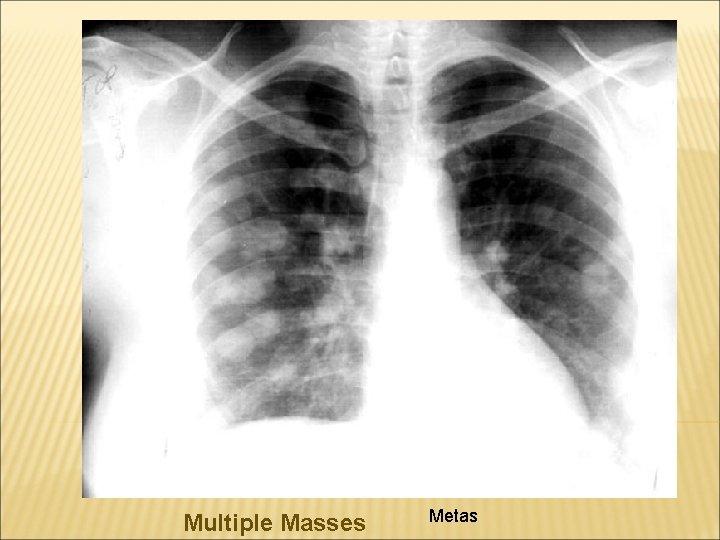
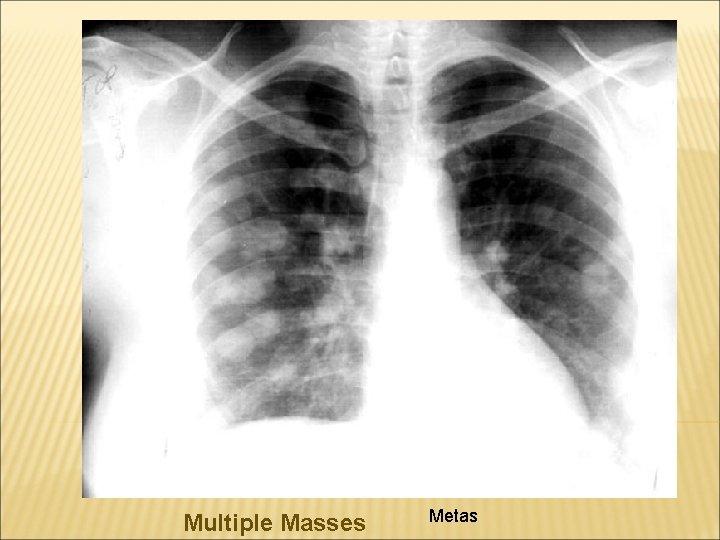
Multiple Masses Metas

Pleural Effusion

Pulmonary Fibrosis
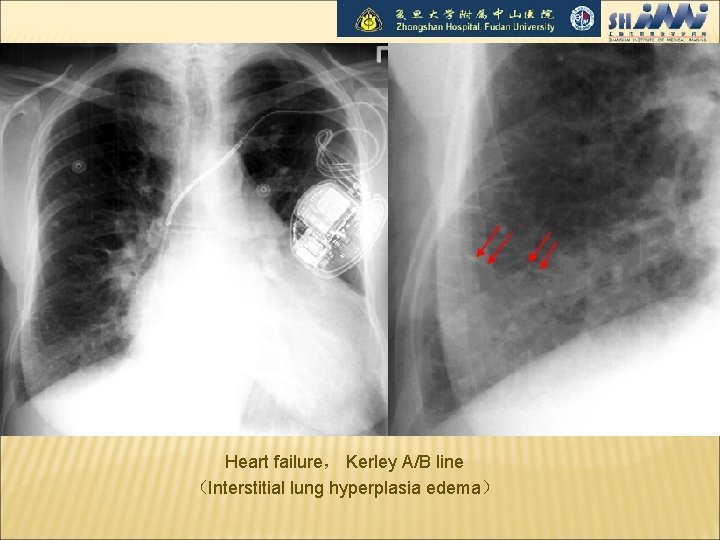
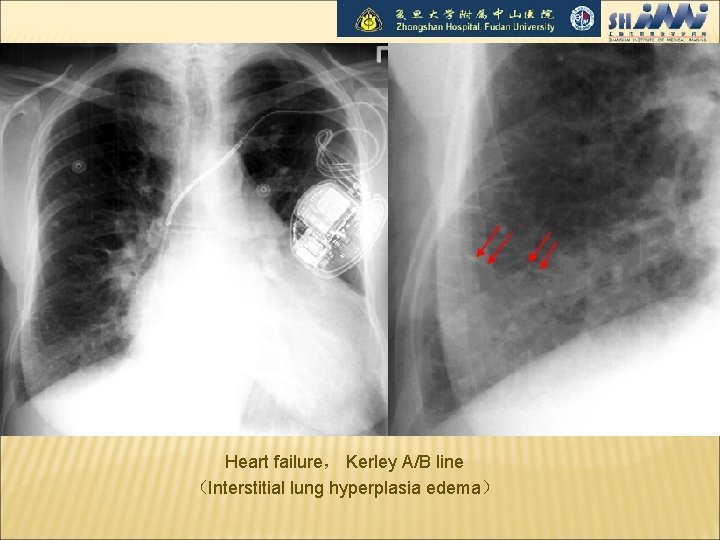
Heart failure, Kerley A/B line (Interstitial lung hyperplasia edema)

Heart failure

Pneumothorax
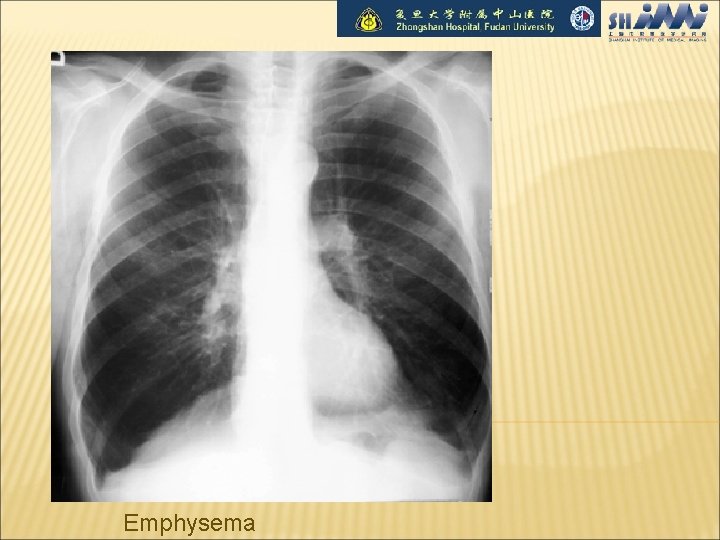
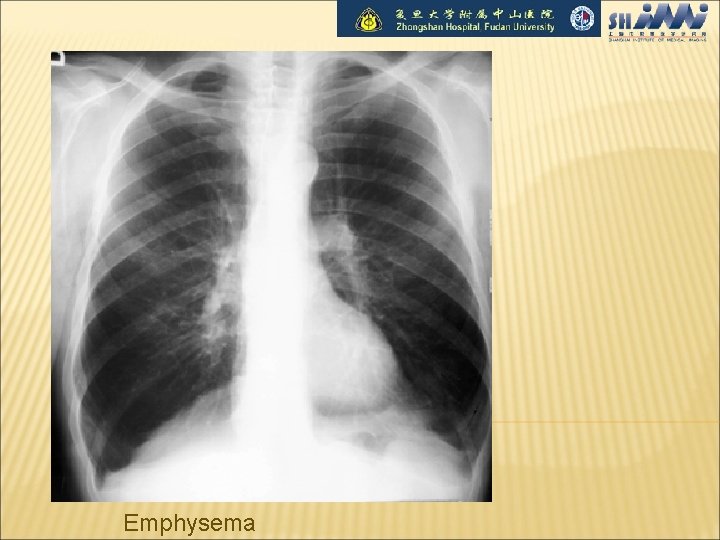
Emphysema
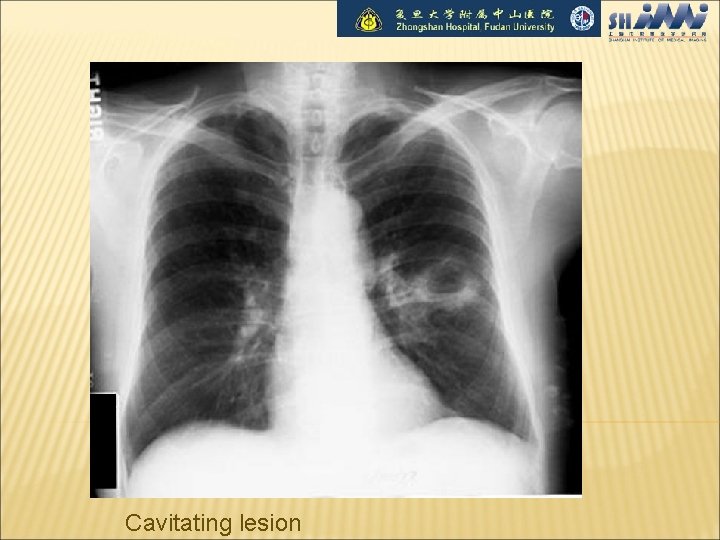
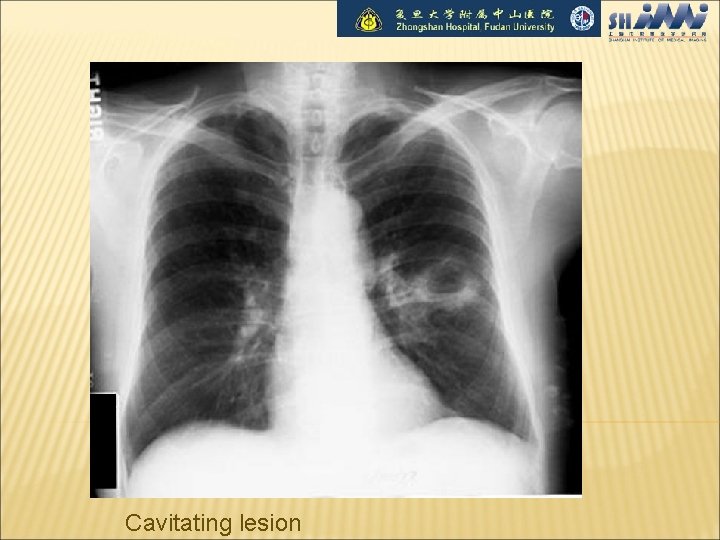
Cavitating lesion

Thin-walled Cavitating lesion 3 mm Thick-walled Cavitating lesion

Bronchiectasis
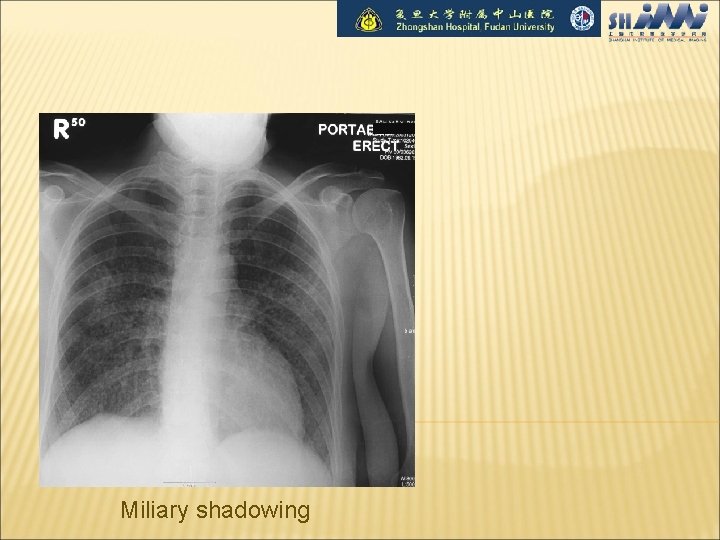
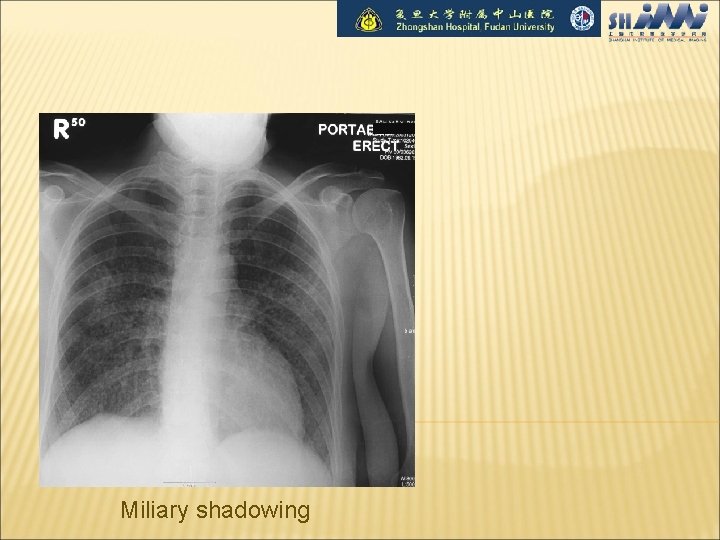
Miliary shadowing

CALCIFICATION Benign Patterns of Calcification Within a Solitary Pulmonary Nodule

Chest Tube, NG Tube, Pulm. artery cath
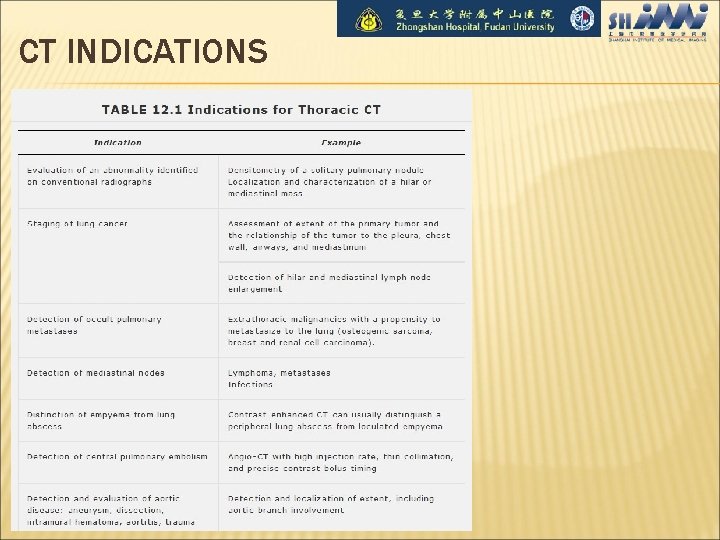
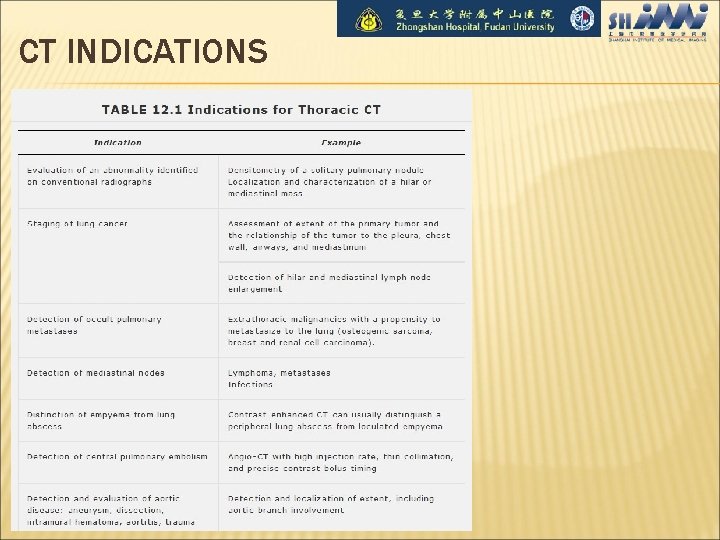
CT INDICATIONS
KEY Clinical Factors Growth Pattern Size Margin (Border) Characteristics Density Contrast-Enhanced CT Other findings

PULMONARY INFECTION dense multifocal segmental airspace opacification pneumonia air bronchograms

lung abscess Pneumonia finding Lobar/segmental consolidation cavitation
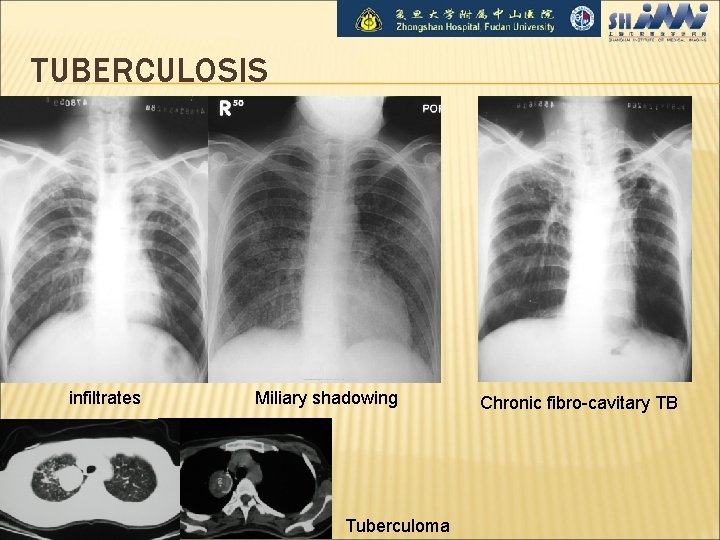
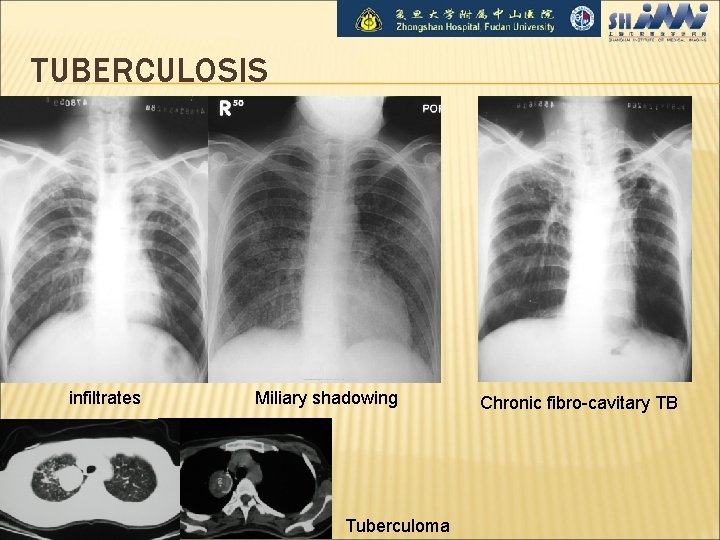
TUBERCULOSIS infiltrates Miliary shadowing Tuberculoma Chronic fibro-cavitary TB
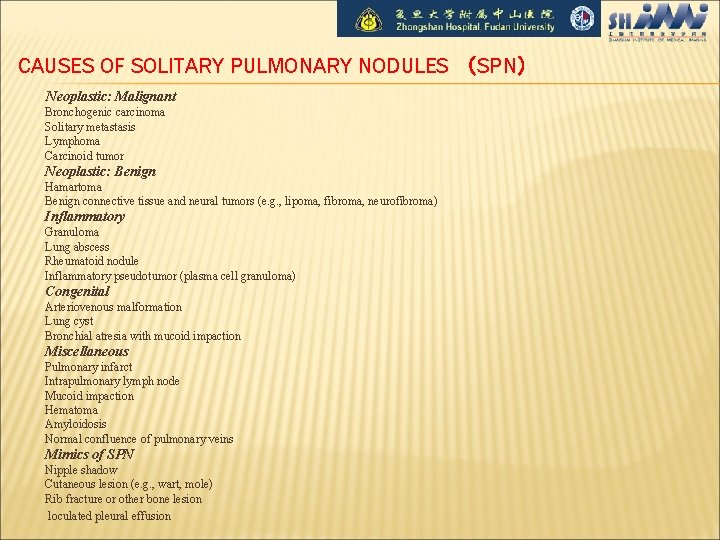
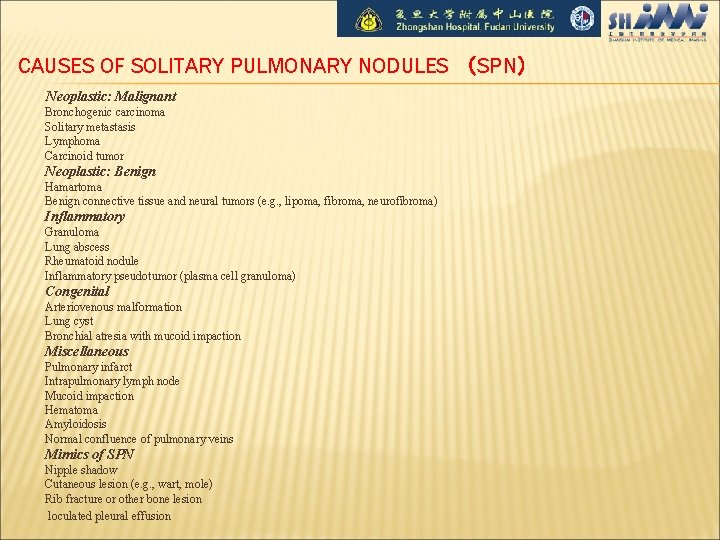
CAUSES OF SOLITARY PULMONARY NODULES (SPN) Neoplastic: Malignant Bronchogenic carcinoma Solitary metastasis Lymphoma Carcinoid tumor Neoplastic: Benign Hamartoma Benign connective tissue and neural tumors (e. g. , lipoma, fibroma, neurofibroma) Inflammatory Granuloma Lung abscess Rheumatoid nodule Inflammatory pseudotumor (plasma cell granuloma) Congenital Arteriovenous malformation Lung cyst Bronchial atresia with mucoid impaction Miscellaneous Pulmonary infarct Intrapulmonary lymph node Mucoid impaction Hematoma Amyloidosis Normal confluence of pulmonary veins Mimics of SPN Nipple shadow Cutaneous lesion (e. g. , wart, mole) Rib fracture or other bone lesion loculated pleural effusion
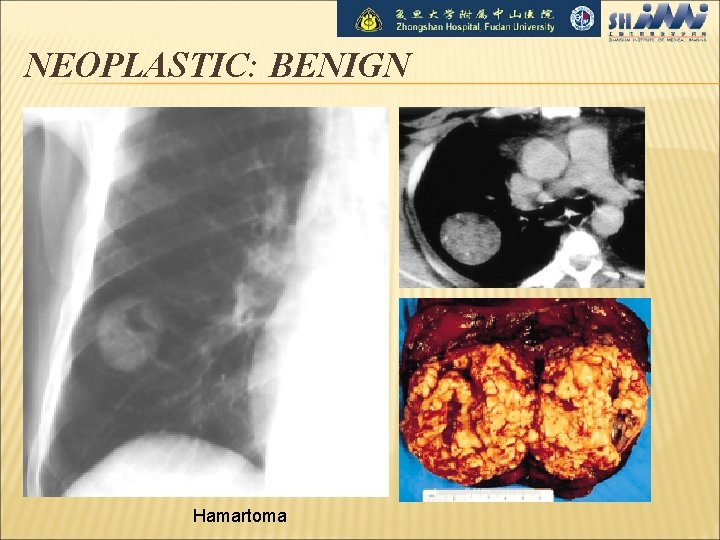
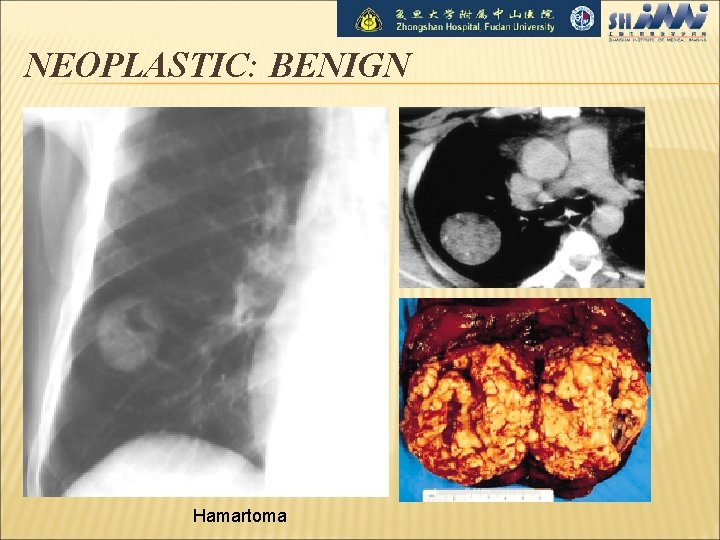
NEOPLASTIC: BENIGN Hamartoma
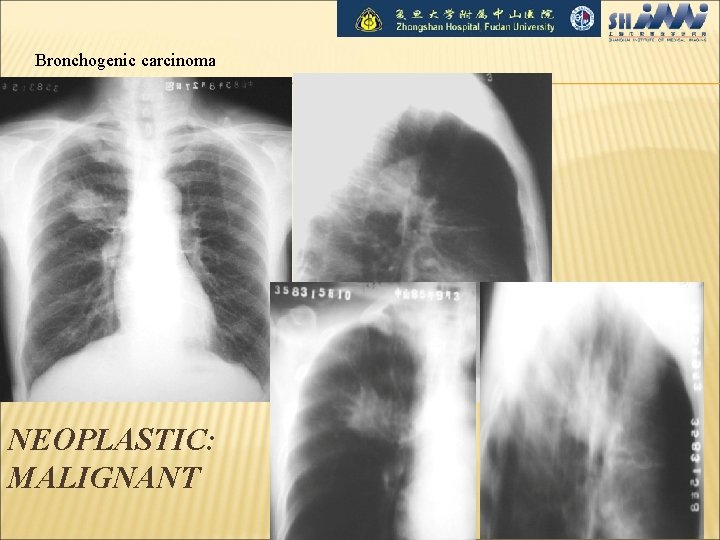
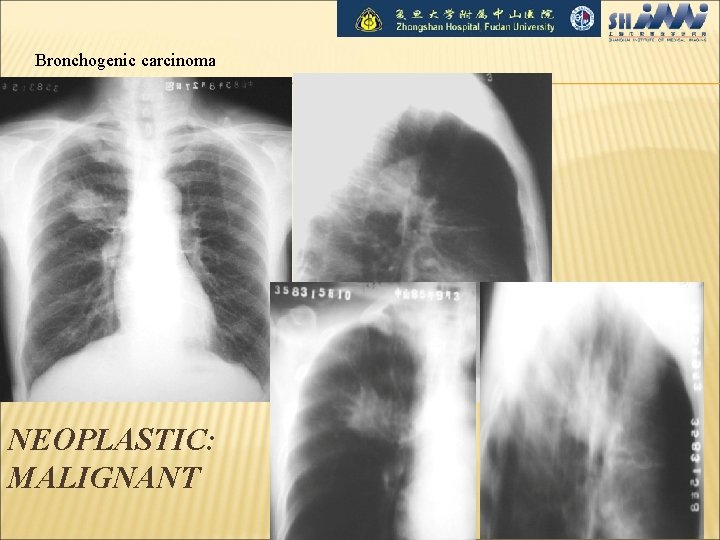
Bronchogenic carcinoma NEOPLASTIC: MALIGNANT
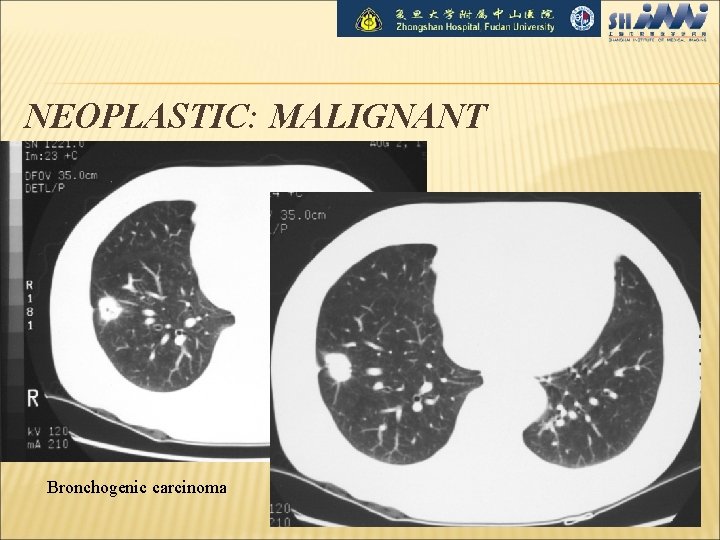
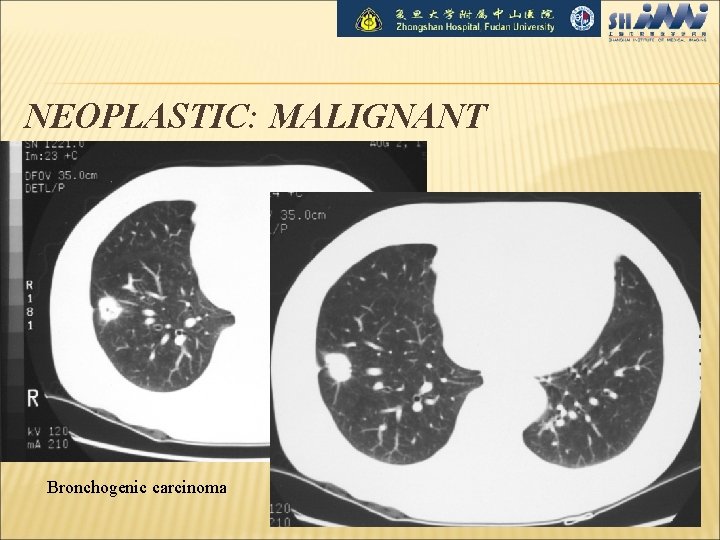
NEOPLASTIC: MALIGNANT Bronchogenic carcinoma
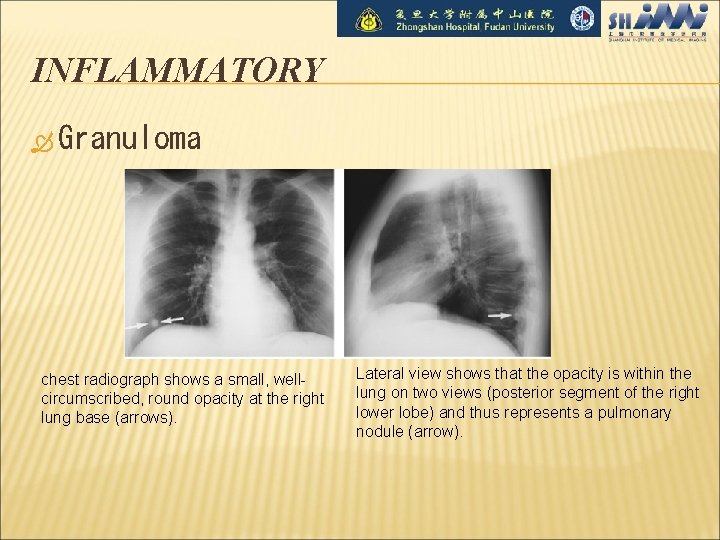
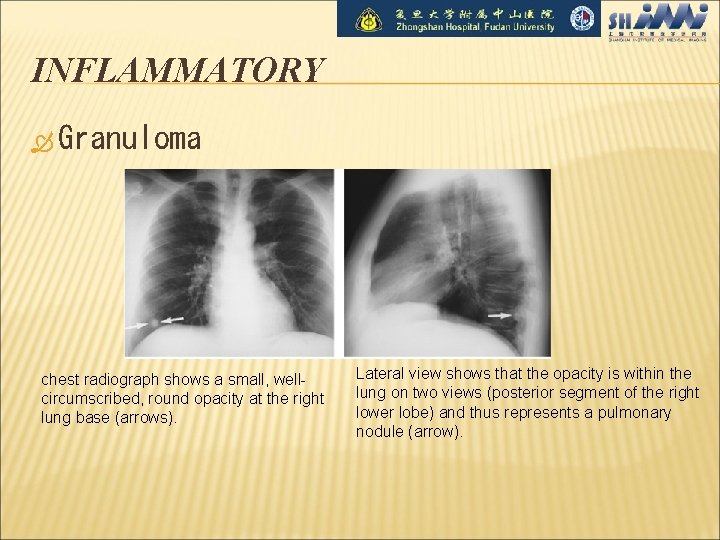
INFLAMMATORY Granuloma chest radiograph shows a small, wellcircumscribed, round opacity at the right lung base (arrows). Lateral view shows that the opacity is within the lung on two views (posterior segment of the right lower lobe) and thus represents a pulmonary nodule (arrow).
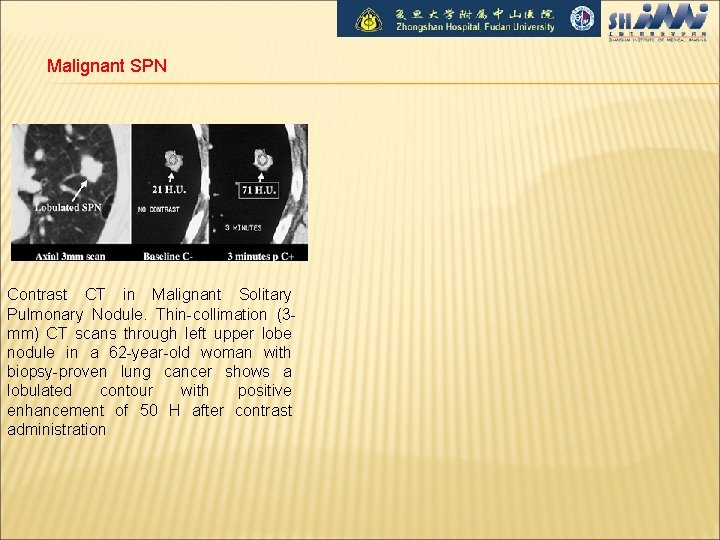
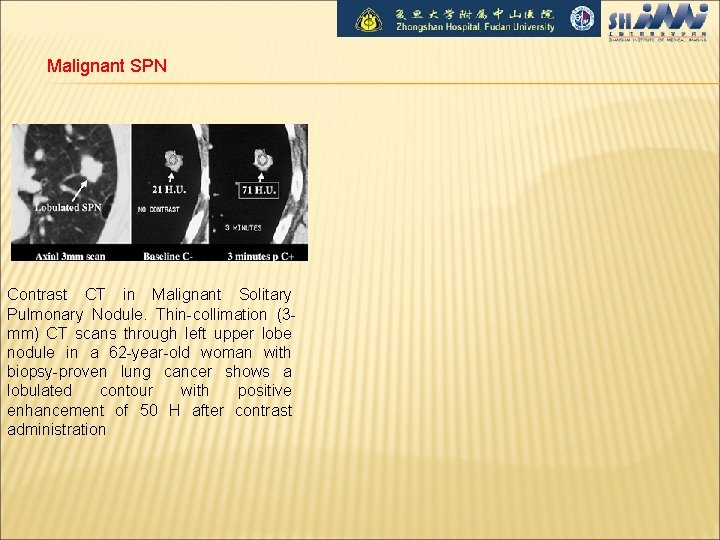
Malignant SPN Contrast CT in Malignant Solitary Pulmonary Nodule. Thin-collimation (3 mm) CT scans through left upper lobe nodule in a 62 -year-old woman with biopsy-proven lung cancer shows a lobulated contour with positive enhancement of 50 H after contrast administration

BRONCHOGENIC CARCINOMA(CLINICAL) Age at diagnosis: 55 -60 years (range 40 -80 years); M: F = 1. 4: 1 asymptomatic (10 -50%) usually with peripheral tumors symptoms of central tumors: cough (75%), wheezing, pneumonia hemoptysis (50%), dysphagia (2%) symptoms of peripheral tumors: pleuritic/local chest pain, dyspnea, cough Pancoast syndrome, superior vena cava syndrome hoarseness symptoms of metastatic disease (CNS, bone, liver, adrenal gland) paraneoplastic syndromes: cachexia of malignancy clubbing + hypertrophic osteoarthropathy nonbacterial thrombotic endocarditis migratory thrombophlebitis ectopic hormone production: hypercalcemia, syndrome of inappropriate secretion of antidiuretic hormone, Cushing syndrome, gynecomastia, acromegaly

RISK FACTORS Cigarette smoking (squamous cell carcinoma + small cell carcinoma) 鈥搑elated to number of cigarettes smoked, depth of inhalation, age at which smoking began 85% of lung cancer deaths are attributable to cigarette smoking! Passive smoking may account for 25% of lung cancers in nonsmokers! Radon gas: may be the 2 nd leading cause for lung cancer with up to 20, 000 deaths per year Industrial exposure: asbestos, uranium, arsenic, chlormethyl ether Concomitant disease: chronic pulmonary scar + pulmonary fibrosis Scar carcinoma 45% of all peripheral cancers originate in scars! Incidence: 7% of lung tumors; 1% of autopsies Origin: related to infarcts (>50%), tuberculosis scar (<25%) Histo: adenocarcinoma (72%), squamous cell carcinoma (18%) Location: upper lobes (75%)
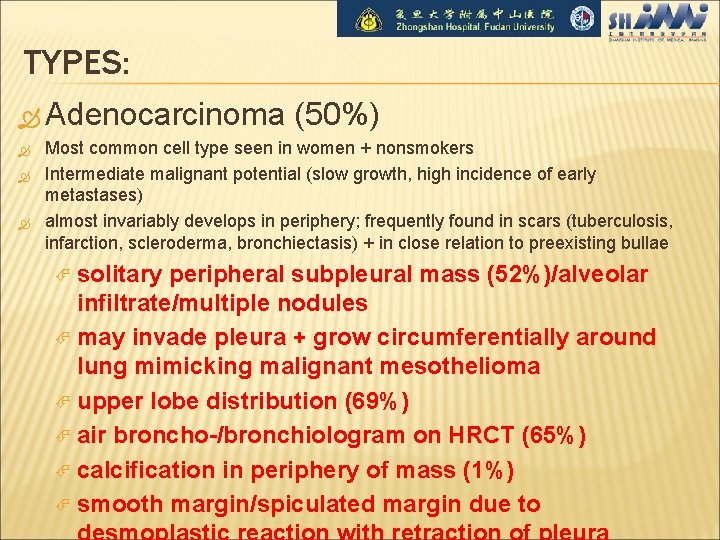
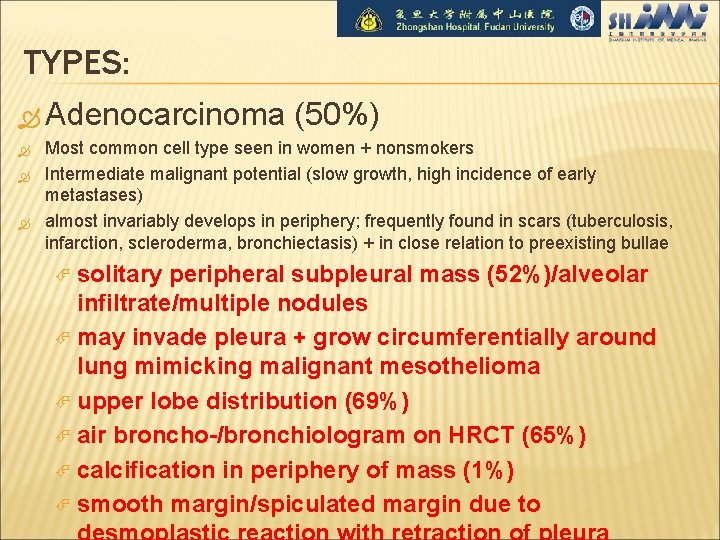
TYPES: Adenocarcinoma (50%) Most common cell type seen in women + nonsmokers Intermediate malignant potential (slow growth, high incidence of early metastases) almost invariably develops in periphery; frequently found in scars (tuberculosis, infarction, scleroderma, bronchiectasis) + in close relation to preexisting bullae solitary peripheral subpleural mass (52%)/alveolar infiltrate/multiple nodules may invade pleura + grow circumferentially around lung mimicking malignant mesothelioma upper lobe distribution (69%) air broncho-/bronchiologram on HRCT (65%) calcification in periphery of mass (1%) smooth margin/spiculated margin due to
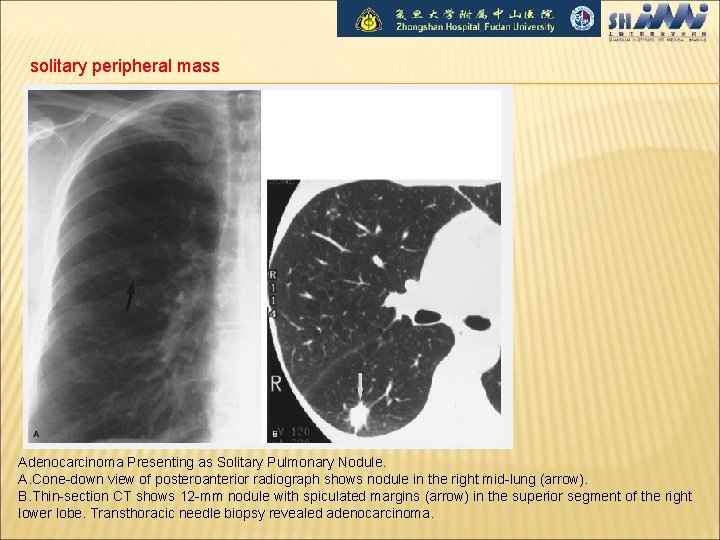
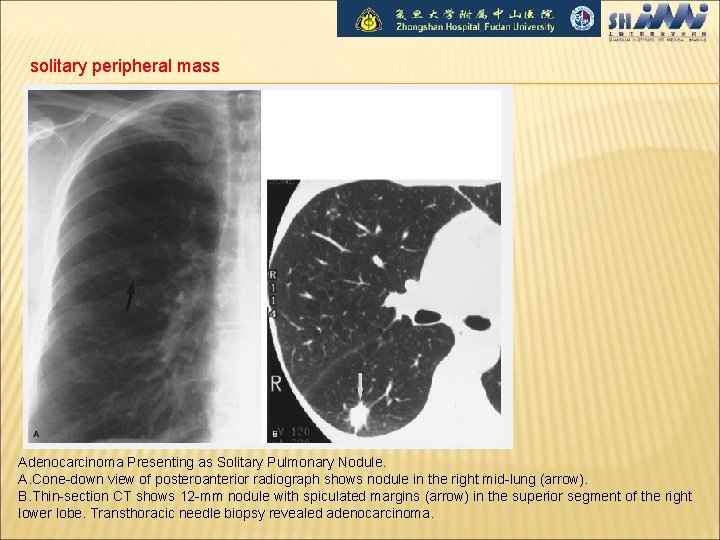
solitary peripheral mass Adenocarcinoma Presenting as Solitary Pulmonary Nodule. A. Cone-down view of posteroanterior radiograph shows nodule in the right mid-lung (arrow). B. Thin-section CT shows 12 -mm nodule with spiculated margins (arrow) in the superior segment of the right lower lobe. Transthoracic needle biopsy revealed adenocarcinoma.
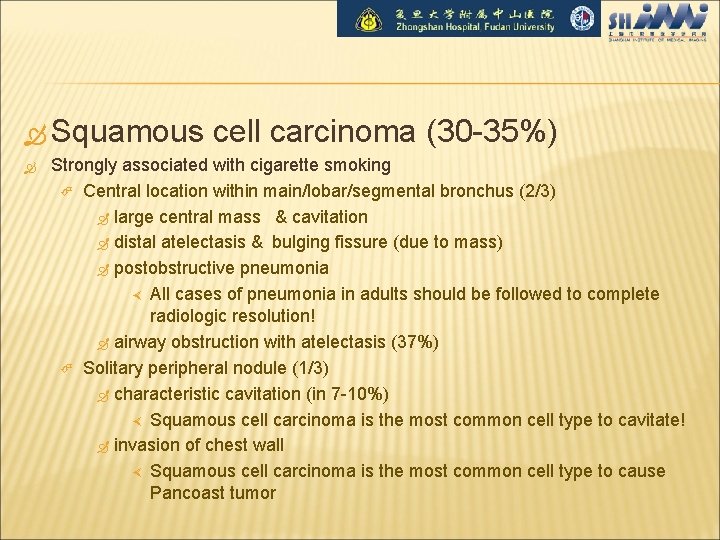
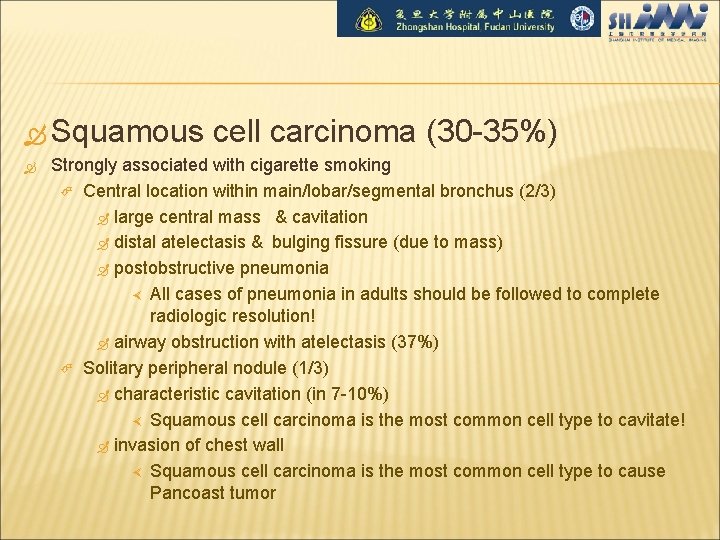
Squamous cell carcinoma (30 -35%) Strongly associated with cigarette smoking Central location within main/lobar/segmental bronchus (2/3) large central mass & cavitation distal atelectasis & bulging fissure (due to mass) postobstructive pneumonia All cases of pneumonia in adults should be followed to complete radiologic resolution! airway obstruction with atelectasis (37%) Solitary peripheral nodule (1/3) characteristic cavitation (in 7 -10%) Squamous cell carcinoma is the most common cell type to cavitate! invasion of chest wall Squamous cell carcinoma is the most common cell type to cause Pancoast tumor
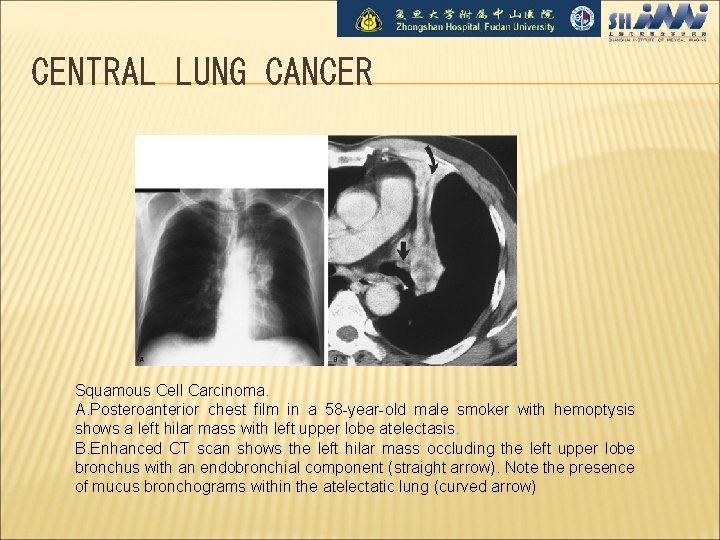
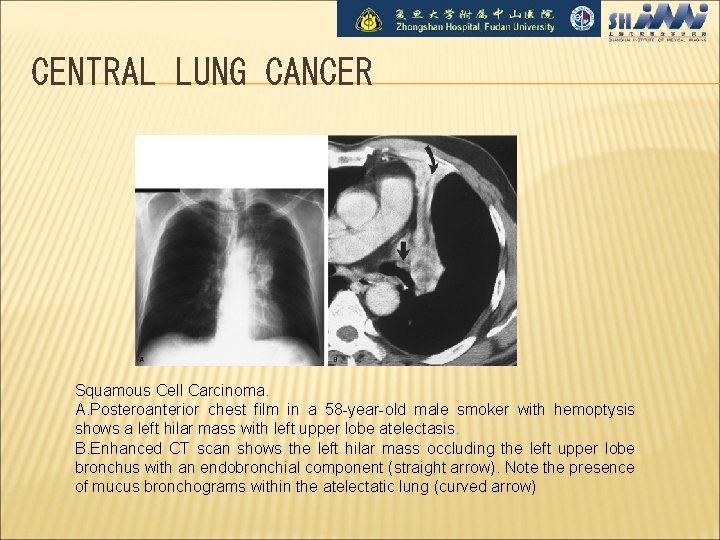
CENTRAL LUNG CANCER Squamous Cell Carcinoma. A. Posteroanterior chest film in a 58 -year-old male smoker with hemoptysis shows a left hilar mass with left upper lobe atelectasis. B. Enhanced CT scan shows the left hilar mass occluding the left upper lobe bronchus with an endobronchial component (straight arrow). Note the presence of mucus bronchograms within the atelectatic lung (curved arrow)

Squamous Cell Carcinoma
Small cell undifferentiated carcinoma (15%) Strongly associated with cigarette smoking Rapid growth + high metastatic potential typically large hilar/perihilar mass often associated with mediastinal widening (from adenopathy) extensive necrosis + hemorrhage small lung lesion (rare)
Large undifferentiated cell carcinoma (<5%) Strongly associated with smoking large bulky usually peripheral mass >6 cm (50%) large area of necrosis pleural involvement large bronchus involved in central lesion (50%)
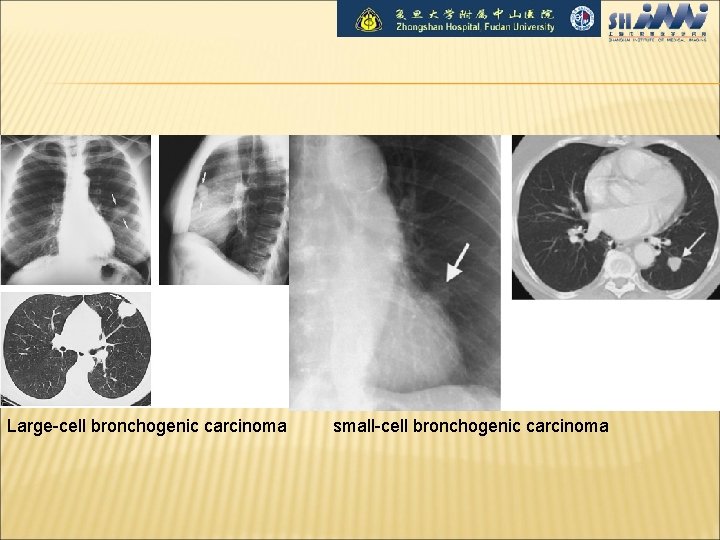
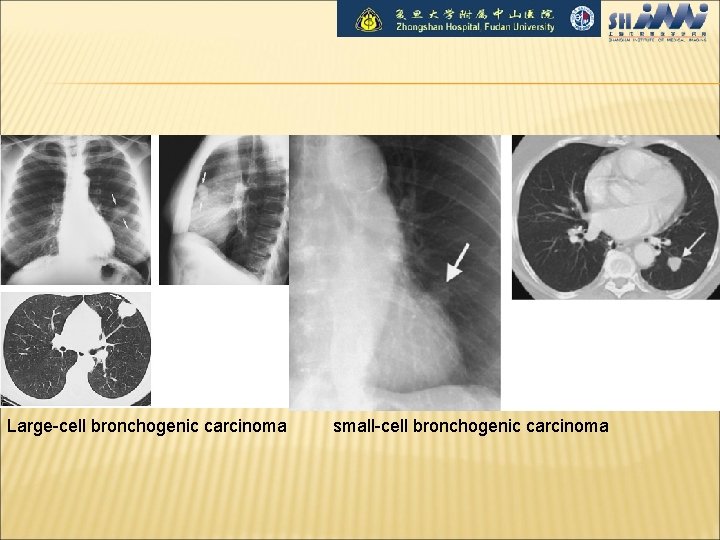
Large-cell bronchogenic carcinoma small-cell bronchogenic carcinoma
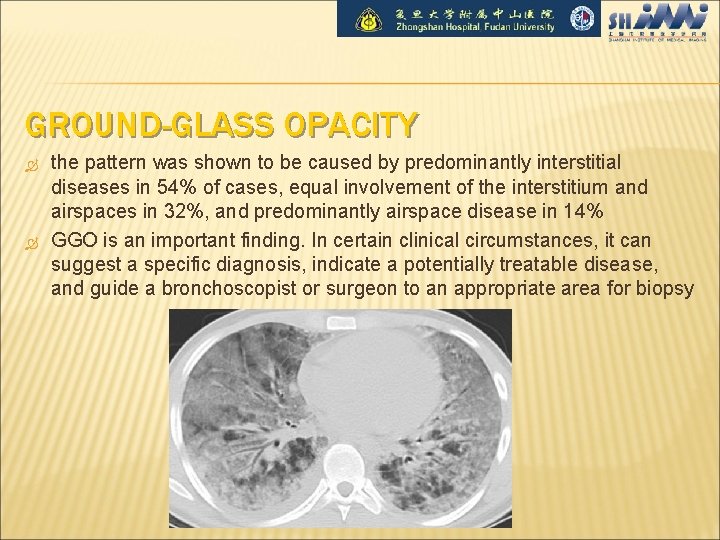
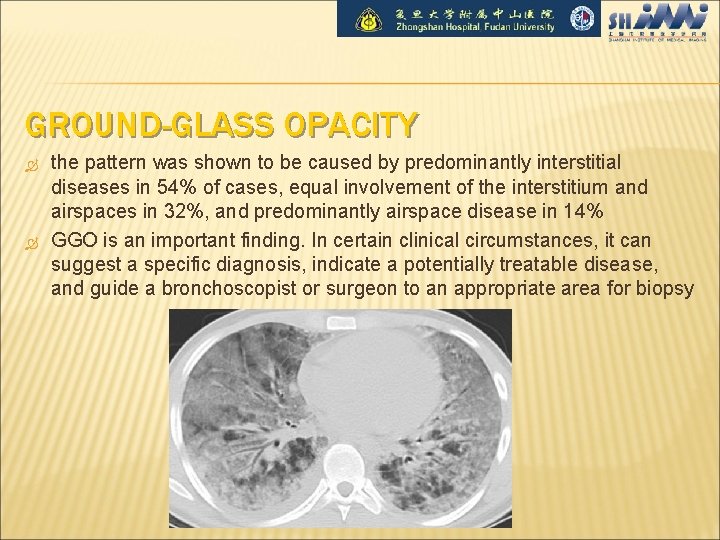
GROUND-GLASS OPACITY the pattern was shown to be caused by predominantly interstitial diseases in 54% of cases, equal involvement of the interstitium and airspaces in 32%, and predominantly airspace disease in 14% GGO is an important finding. In certain clinical circumstances, it can suggest a specific diagnosis, indicate a potentially treatable disease, and guide a bronchoscopist or surgeon to an appropriate area for biopsy

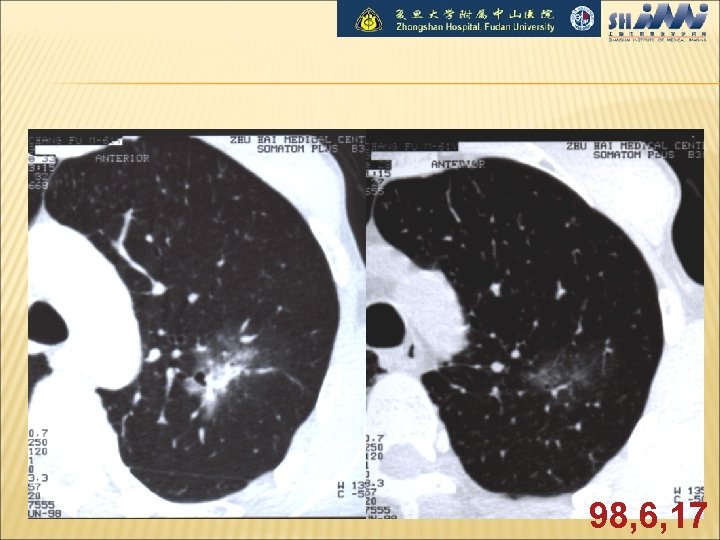
Pure GGO( Ground-glass Opacity) Early stage
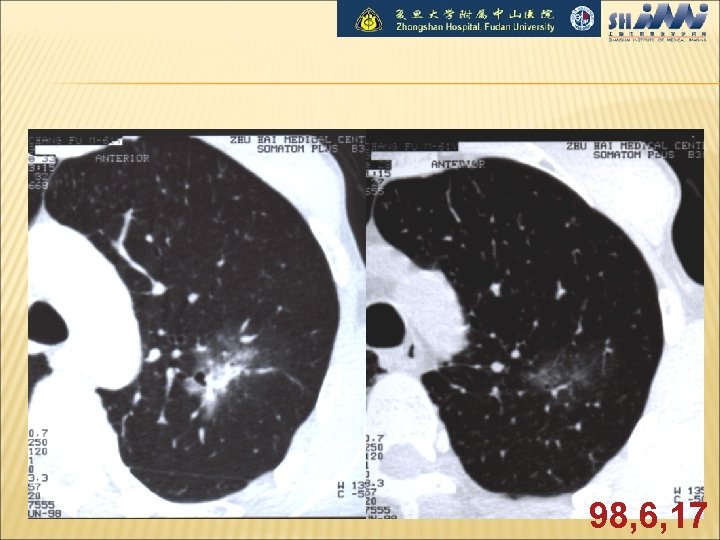
98, 6, 17
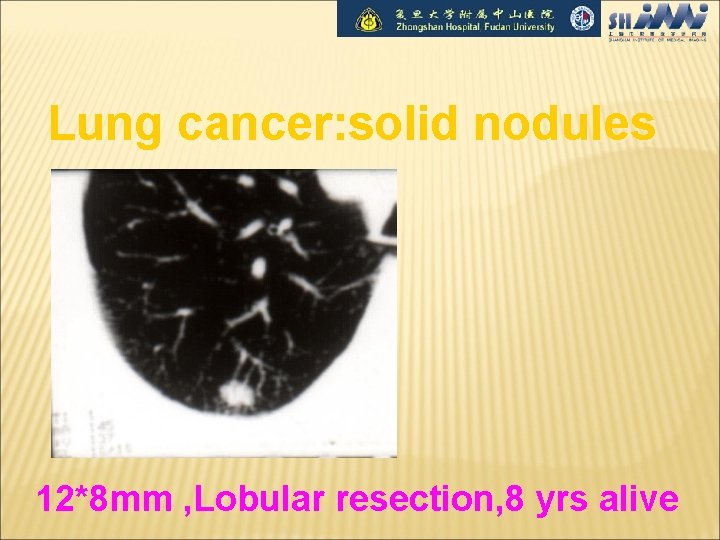
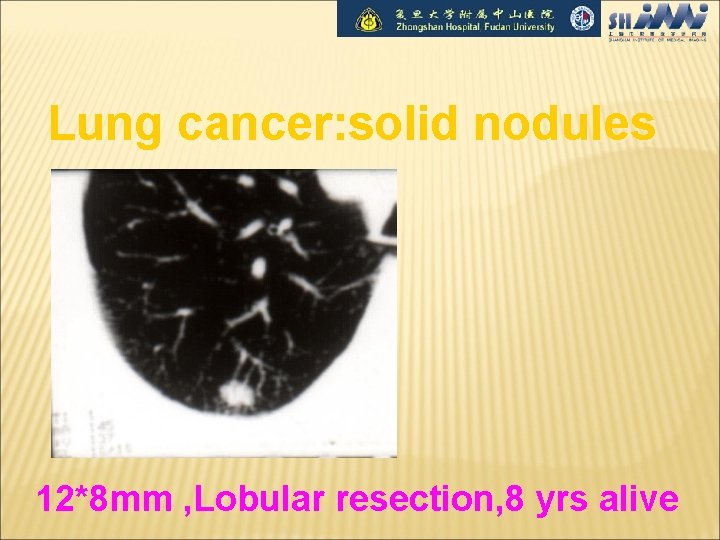
Lung cancer: solid nodules 12*8 mm , Lobular resection, 8 yrs alive
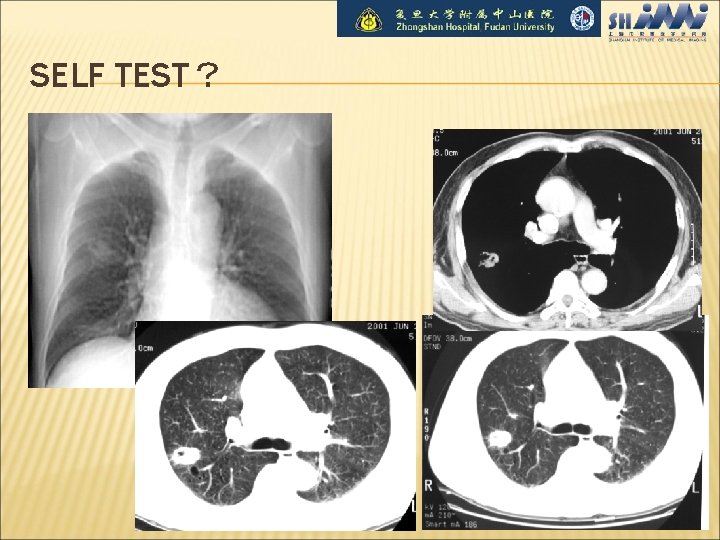
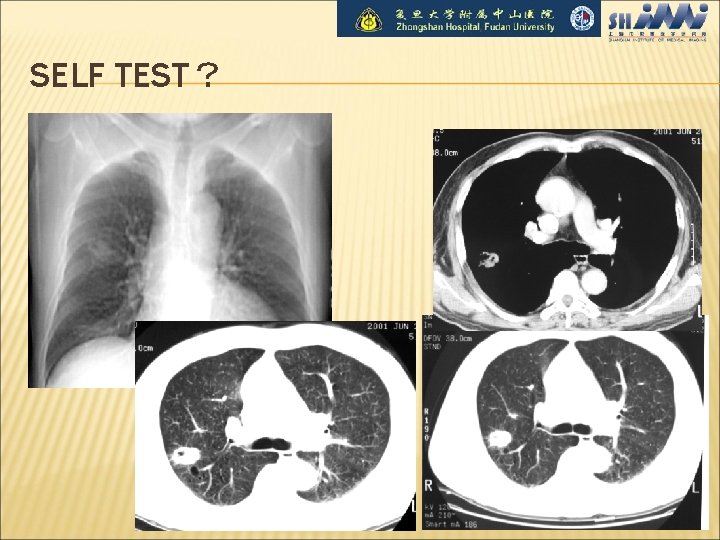
SELF TEST?
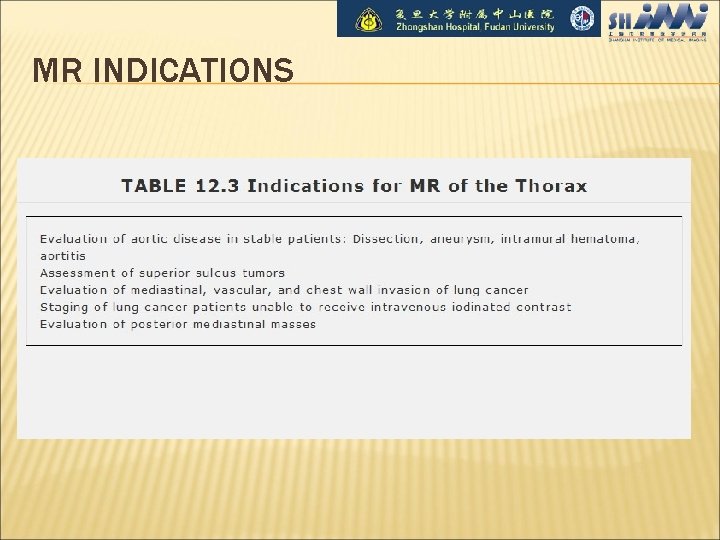
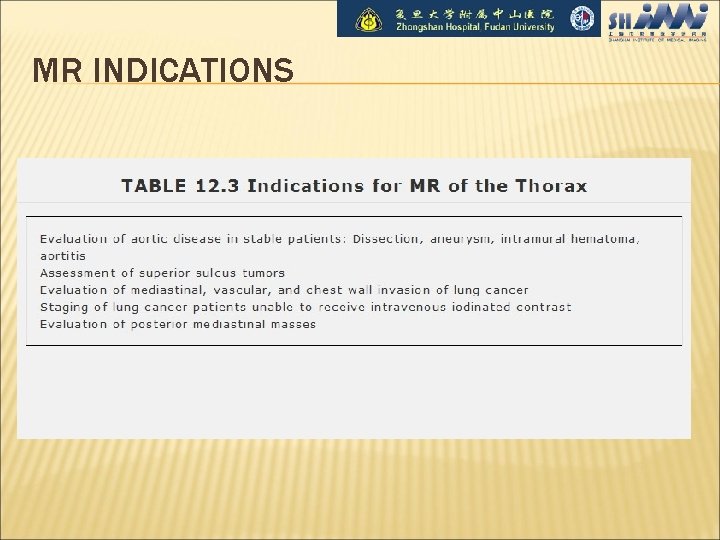
MR INDICATIONS
NEVER STOP LOOKING, CARRY ON WITH YOUR SYSTEMATIC APPROACH!!
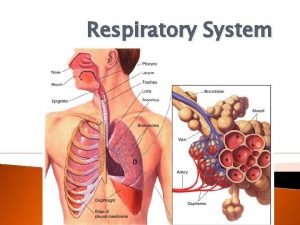
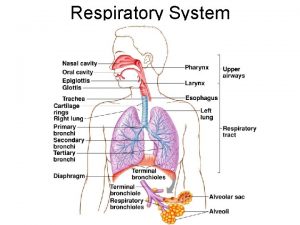
 Conducting zone respiratory
Conducting zone respiratory Respiratory digestive and circulatory system
Respiratory digestive and circulatory system Tiny air sacs at the end of the bronchioles
Tiny air sacs at the end of the bronchioles Circulatory system and respiratory system work together
Circulatory system and respiratory system work together Dept nmr spectroscopy
Dept nmr spectroscopy Department of agriculture consumer services
Department of agriculture consumer services Finance dept structure
Finance dept structure City of worcester inspectional services
City of worcester inspectional services Dept. name of organization
Dept. name of organization Mn dept of education
Mn dept of education Dept of finance and administration
Dept of finance and administration Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) Ohio dept of dd
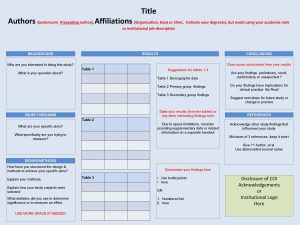
Ohio dept of dd Affiliation poster presentation
Affiliation poster presentation Vaginal dept
Vaginal dept Gome dept
Gome dept Gome dept
Gome dept Gome dept
Gome dept Gome dept
Gome dept Hoe dept
Hoe dept Firefighter interview tips
Firefighter interview tips Oviposition
Oviposition Dept of education
Dept of education Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Dept a
Dept a Central islip fire department
Central islip fire department Rowan county medicaid transportation
Rowan county medicaid transportation Dept of education
Dept of education Dept c13 nmr
Dept c13 nmr Pt dept logistik
Pt dept logistik Nys dept of homeland security
Nys dept of homeland security Affiliate disclodures
Affiliate disclodures Geaux biz login
Geaux biz login Oxford dept of continuing education
Oxford dept of continuing education Nebraska dept of agriculture
Nebraska dept of agriculture Iit
Iit Dept ind onegov
Dept ind onegov Albany county dept of social services
Albany county dept of social services Radiology alert system
Radiology alert system Disappeared boey kim cheng
Disappeared boey kim cheng John cheng md
John cheng md Entity types
Entity types Cheng field and wave electromagnetics
Cheng field and wave electromagnetics Antony cheng
Antony cheng King cheng of zhou
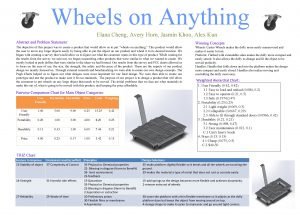
King cheng of zhou Avery cheng
Avery cheng The planners by boey kim cheng
The planners by boey kim cheng Cheng
Cheng Ck cheng ucsd
Ck cheng ucsd Wei cheng lee
Wei cheng lee Mktg 303
Mktg 303 Cheng xiang zhai
Cheng xiang zhai Myelopathy vs radiculopathy
Myelopathy vs radiculopathy Yizong cheng
Yizong cheng Cheng
Cheng Lou cheng
Lou cheng Boey kim cheng
Boey kim cheng Kung fu panda chi
Kung fu panda chi Chung-kuan cheng
Chung-kuan cheng Cheng xiang zhai
Cheng xiang zhai Chia liang cheng
Chia liang cheng Cheng xiang zhai
Cheng xiang zhai Sophia cheng accident
Sophia cheng accident Cheng xiang zhai
Cheng xiang zhai Cheng xiang zhai
Cheng xiang zhai Cheng-few lee
Cheng-few lee Morrp
Morrp Cheng xiang zhai
Cheng xiang zhai Kiddonet games
Kiddonet games Morrp
Morrp Judy cheng hopkins
Judy cheng hopkins Luke daemen
Luke daemen Ismael herrera
Ismael herrera Cộc cách tùng cheng
Cộc cách tùng cheng Pauline cheng
Pauline cheng Wayne cheng loma linda
Wayne cheng loma linda Sega cheng
Sega cheng Respiratory system bozeman
Respiratory system bozeman Unit 9 respiratory system
Unit 9 respiratory system Diagnostic test of respiratory system
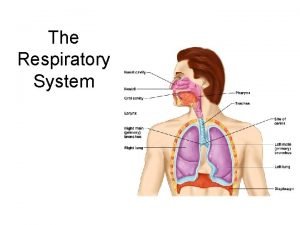
Diagnostic test of respiratory system What is the respiratory system
What is the respiratory system Voice box in respiratory system
Voice box in respiratory system Respiratory system coloring page
Respiratory system coloring page Respiratory system purpose
Respiratory system purpose Conclusion for respiratory system
Conclusion for respiratory system The energy-releasing process that is fueled by oxygen
The energy-releasing process that is fueled by oxygen Chapter 7:10 respiratory system
Chapter 7:10 respiratory system Bronchide
Bronchide Perfusion respiratory system
Perfusion respiratory system Interesting facts about respiratory system
Interesting facts about respiratory system