Interstitial lung disease Paul Swift What the 1














- Slides: 47
Interstitial lung disease Paul Swift

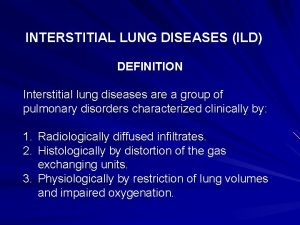
What the? 1. Extrinsic Allergic alveolitis 2. Idiopathic pulmonary fibrosis 3. Industrial dust disease 4. Organic dust disease 5. Sarcoidosis

What’s important Pathophysiology Clinical features Investigation Management Prognosis
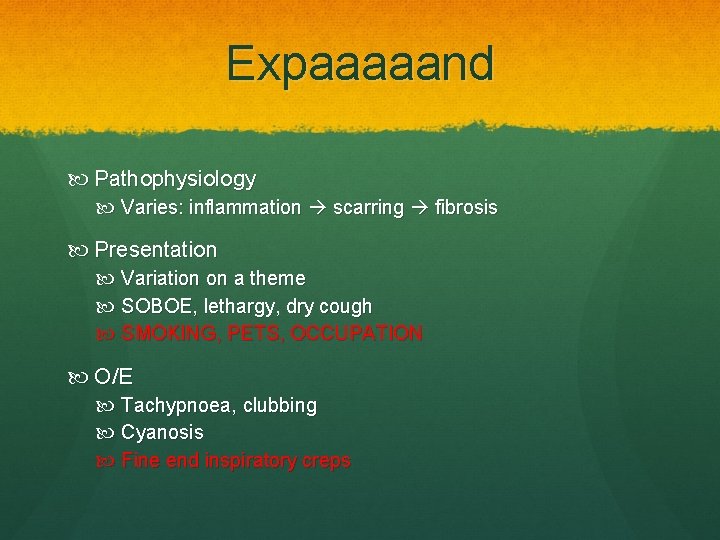
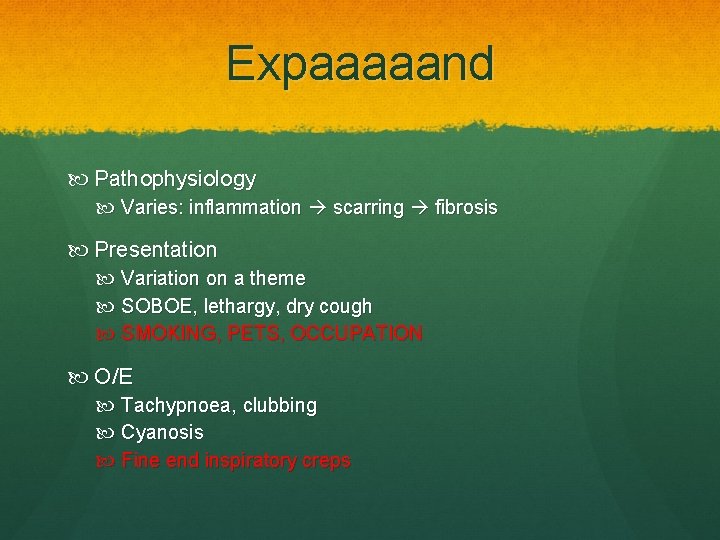
Expaaaaand Pathophysiology Varies: inflammation scarring fibrosis Presentation Variation on a theme SOBOE, lethargy, dry cough SMOKING, PETS, OCCUPATION O/E Tachypnoea, clubbing Cyanosis Fine end inspiratory creps

Investigation Investigations 1. Bedside Ø PEF (work v. home) Ø ABG sats Ø RR 2. Blood Ø FBC, U&Es, LFTs, CRP, ESR Ø ANA and Rf in IPF sometimes 3. Imaging Ø CXR Ø HRCT


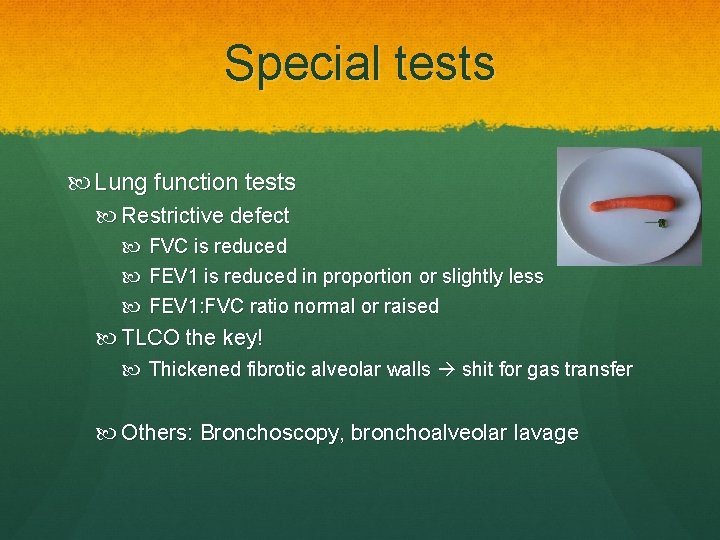
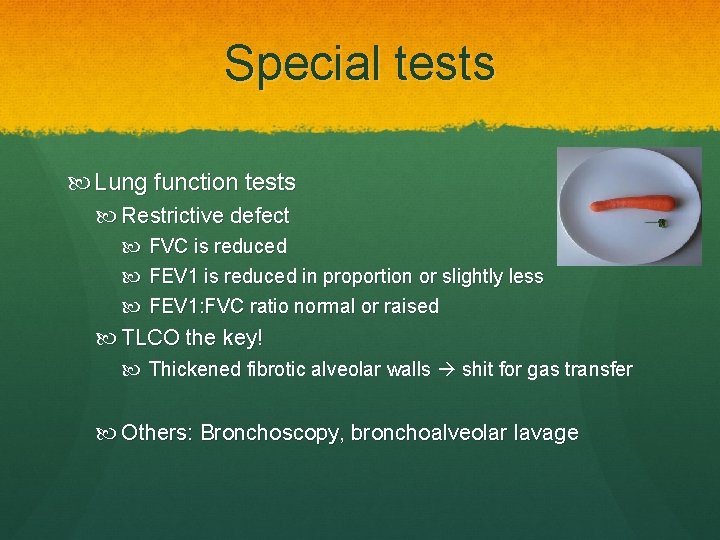
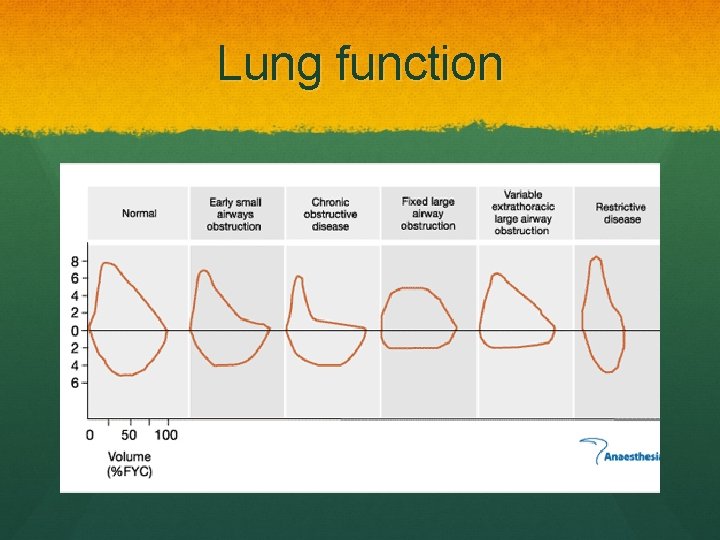
Special tests Lung function tests Restrictive defect FVC is reduced FEV 1 is reduced in proportion or slightly less FEV 1: FVC ratio normal or raised TLCO the key! Thickened fibrotic alveolar walls shit for gas transfer Others: Bronchoscopy, bronchoalveolar lavage
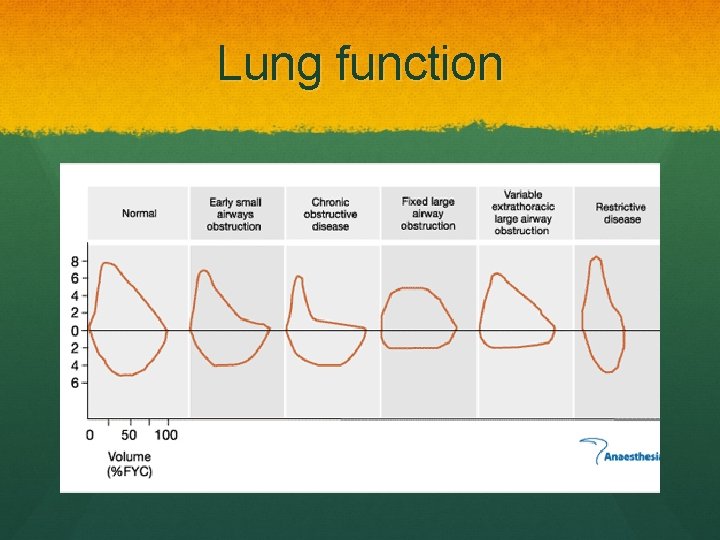
Lung function

Treatment Conservative Weight loss Increased exercise Smoking cessation Medical Oxygen Steroids Surgical Transplant
Extrinsic allergic alveolitis AKA- hypersensitivty penumonitis Type III hypersensitivity reaction Ø Prior sensitisation to inhaled antigen Examples 1. 2. 3. 4. Mould hay (farmer’s lung) Bird faeces (bird fancier’s lung) Cotton fibres (byssionosis) Sugar can fibres (bagassosis)

Famer’s lung

Bird fancier’s lung
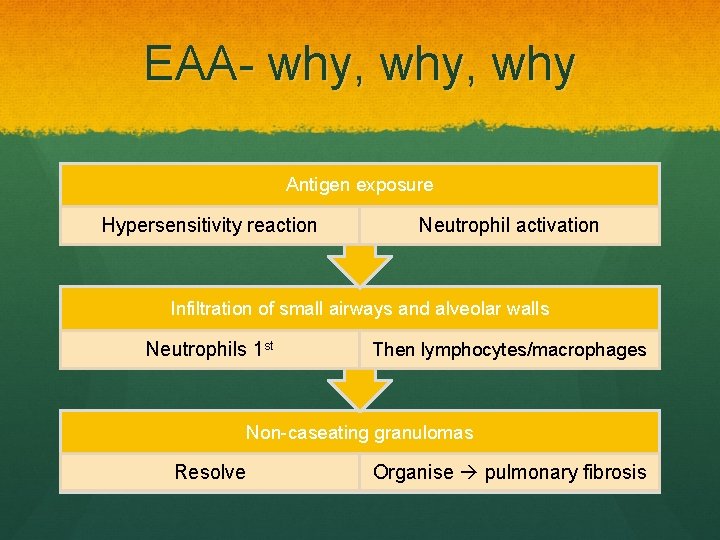
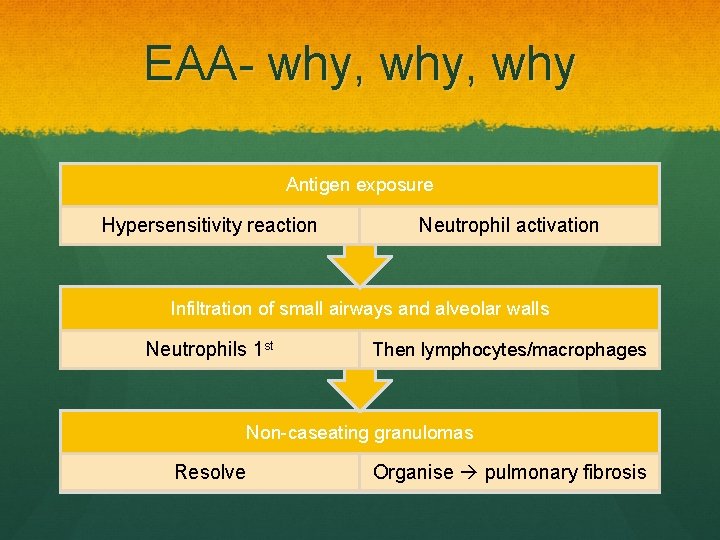
EAA- why, why Antigen exposure Hypersensitivity reaction Neutrophil activation Infiltration of small airways and alveolar walls Neutrophils 1 st Then lymphocytes/macrophages Non-caseating granulomas Resolve Organise pulmonary fibrosis
Clinical features Standard stuff Ø Ø Cough SOB Fever Malaise Acute onset hours after exposure Ø More insidious if long-term exposure to small amounts O/E: Coarse end inspiratory crackles- upper lung Ø http: //www. youtube. com/watch? v=HTNo_ovhcv 8
Investigations Bedside Bloods Neutrophil & leukocyte count Ig. G antibody titres

Investigations Imaging CXR Often normal in acute form Subacute- reticular nodular Shadowing Chronic- fibrosis with volume loss HRCT Special Lung function Bronchoalveolar lavage Hisolopathological diagnosis

Treatment Conservative Antigen avoidance!!!! Medical: ? Corticosteroids Yup, severe disease Speed initial recovery Prognosis Variable, depends on antigen avoidance
Idiopathic pulmonary fibrosis AKA- Cryptogenic Fibrosing Alveolitis, Usual Intersitial Pneumonitis Rare progressive chronic pulmonary fibrosis of unknown aetiology Peak @ 45 -65 yrs
IPF- patho Alveolar walls thickened because of fibrosis Predominantly lower lobes Number of chronic inflammatory cells in alveoli and interstitium Usual interstitial pneumonitis Other patterns: Desquamative interstitial pneumonitis Bronchiolitis obliterans
Clinical features Same old SOB Dry cough Fatigue Can get considerable weight loss More chronic/late stage Cyanosis Pulmonary hypertension/cor pulmonale Resp failure
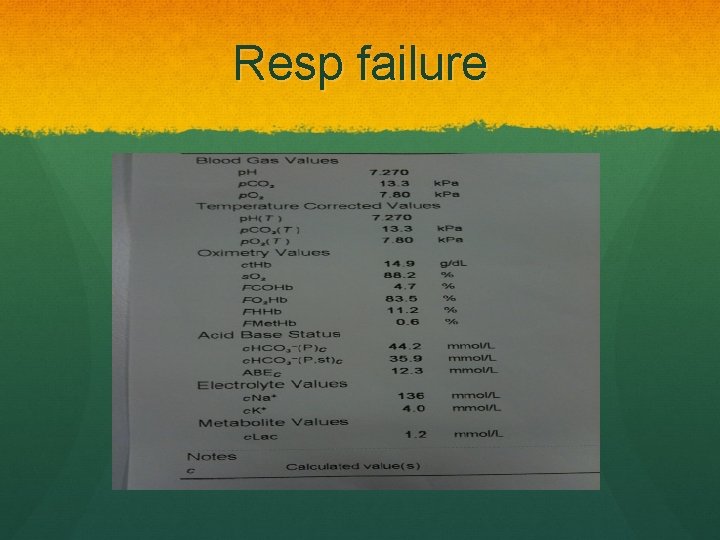
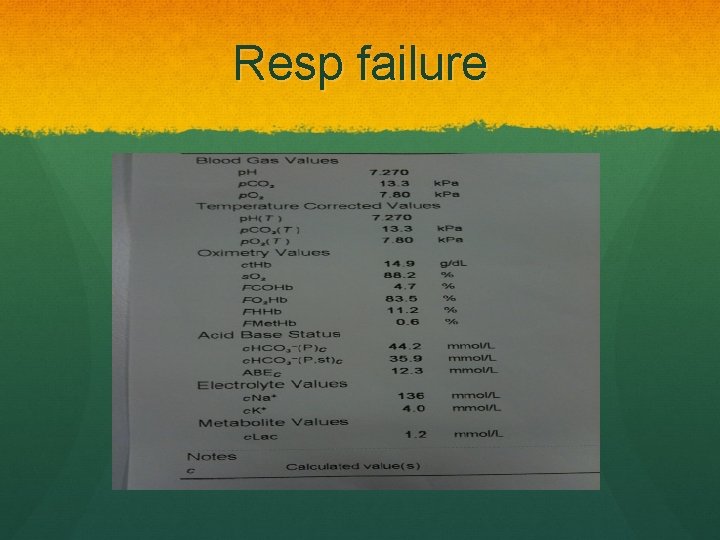
Resp failure
On examination O/E Clubbing 2/3!! Chest expansion reduced Fine-end inspiratory crackles N/B. Associations

Investigations Bedside ABG resp failure Bloods Autoantibodies ANA +ive in 1/3 Rf +ive in ½ Raised ESR
Investigations Imaging CXR HRCT Special Lung function BAL Neutrophils Transbronchial or open lung biopsy for histological diagnosis

Treatment Conservative Stop smoking Weight Exercise Medical 50% respond to immunosuppression with combo therapy recommended: Prednisolone 0. 5 mg/kg 1/12 Azathioprine 2 -3 mg/kg (can sub in cyclophosphamide for azathioprine) Oxygen Surgical Transplant
Prognosis 50% 5 year survival
More dust disease The pneumoconioses CABS Coal Worker’s pneumoconiosis Asbestosis Berylliosis Silicosis Group of disorders due to inhlation of mineral or biological dusts
Coal Worker’s pneumoconiosis Dose dependent Simple Coal dust deposition in the lung Asymptomatic Diagnosis made by several small round opacities on CXR Caplan’s Severe disease may progress to progressive massive fibrosis
Progressive massive fibrosis Large round fibrotic nodules >10 mm Upper lobes Scarring Dyspnoea, cough, sputum May be black if cavitating lesions

PMF
PMF treatment Progresses when exposure removed Unlike simple Prognosis is poor, no treatment Coal Workers Pneumoconiosis Scheme Pneumoconiosis Workers’ Compensation Act 1979 Lump sum compensation
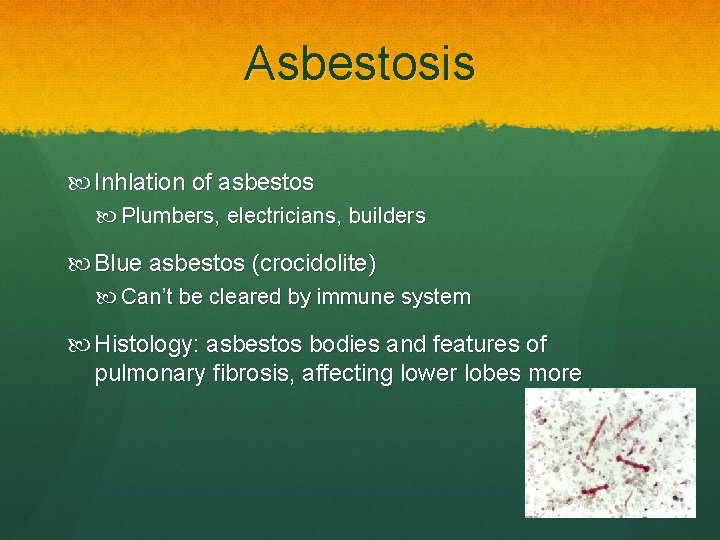
Asbestosis Inhlation of asbestos Plumbers, electricians, builders Blue asbestos (crocidolite) Can’t be cleared by immune system Histology: asbestos bodies and features of pulmonary fibrosis, affecting lower lobes more
Rx No treatment Considerable time lag: 20 -40 years following exposure Compensation Risk……….

Sarcoidosis A 25 -year old afro-Caribbean woman presents with SOB and bilateral leg lesions…… Multisystem granulomatous disorder of unknown aetiology Commonly effects the lungs Non-caseating granulomas Rare (19/100000 in UK) Peak 20 -40 yrs
Sarcoid path Non-caseating granulomas (Infiltrated by Th 1 lymphocytes and macrophages) (Fuse to multinucleated epithelioid cells) Resolution of granulomas 10 -20% persistent interstitial fibrosis
Clinical features 90% have pulmonary involvement SOB Chest pain Cough Non-specific features Lymphadeopathy Weight loss Fever Fatigue
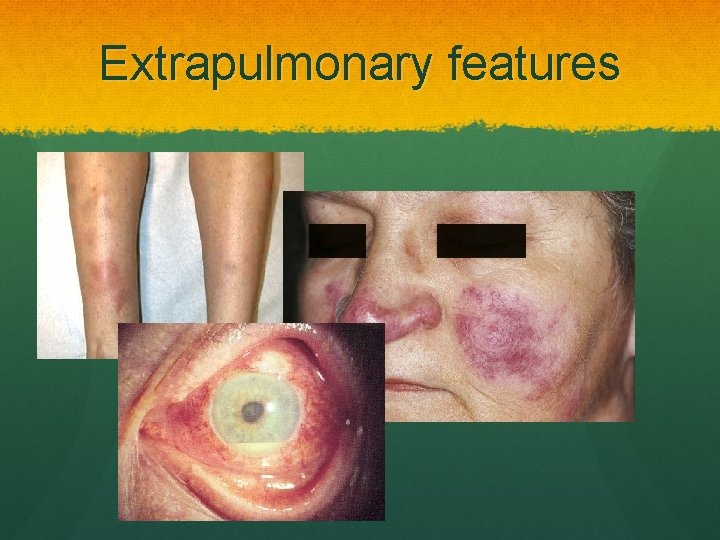
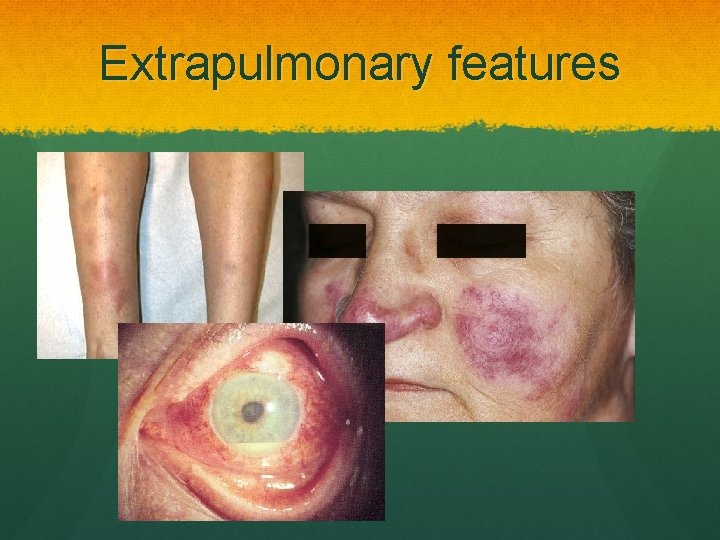
Extrapulmonary features
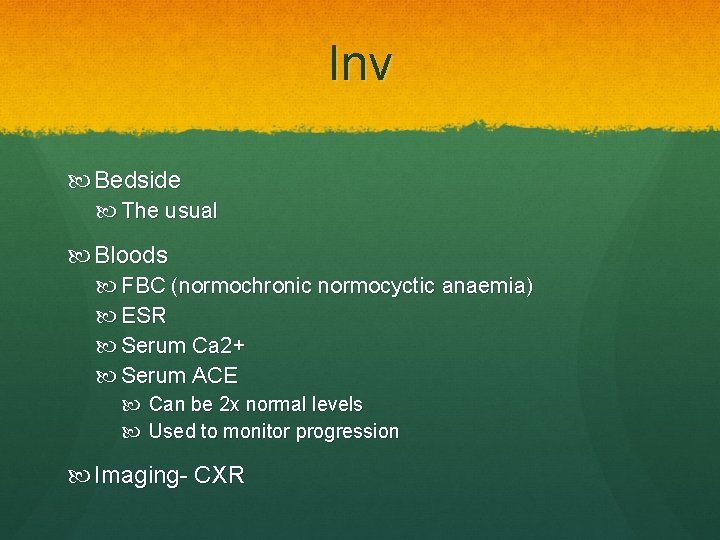
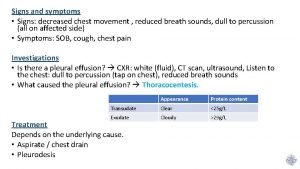
Inv Bedside The usual Bloods FBC (normochronic normocyctic anaemia) ESR Serum Ca 2+ Serum ACE Can be 2 x normal levels Used to monitor progression Imaging- CXR
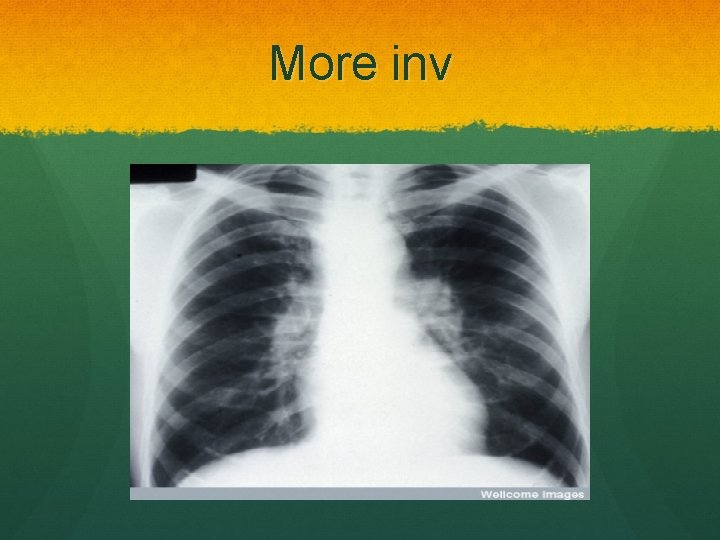
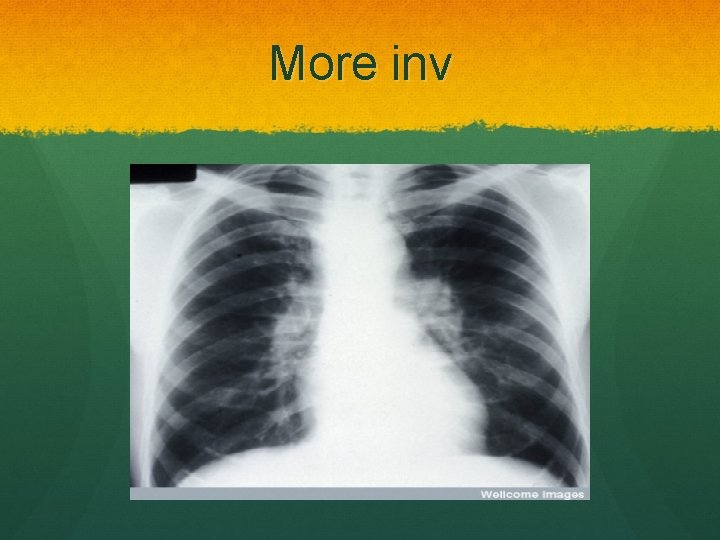
More inv
Expensive stuff HRCT Staging Identifying pulmonary fibrosis Biopsy GOLD standard for diagnosis
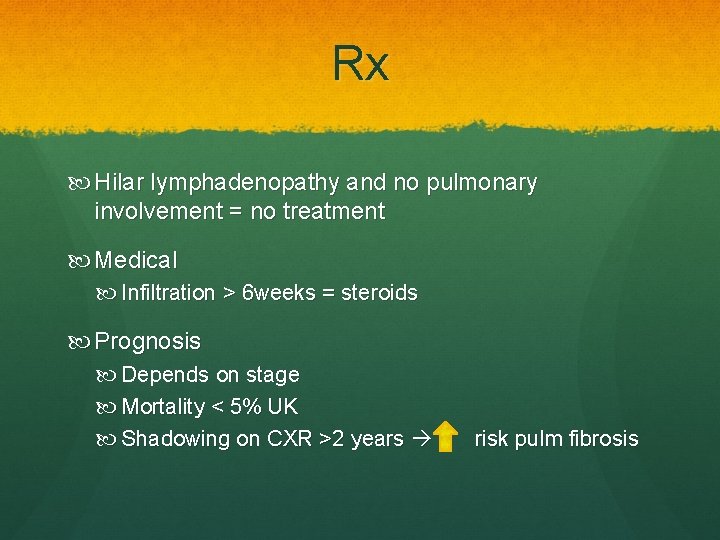
Rx Hilar lymphadenopathy and no pulmonary involvement = no treatment Medical Infiltration > 6 weeks = steroids Prognosis Depends on stage Mortality < 5% UK Shadowing on CXR >2 years risk pulm fibrosis
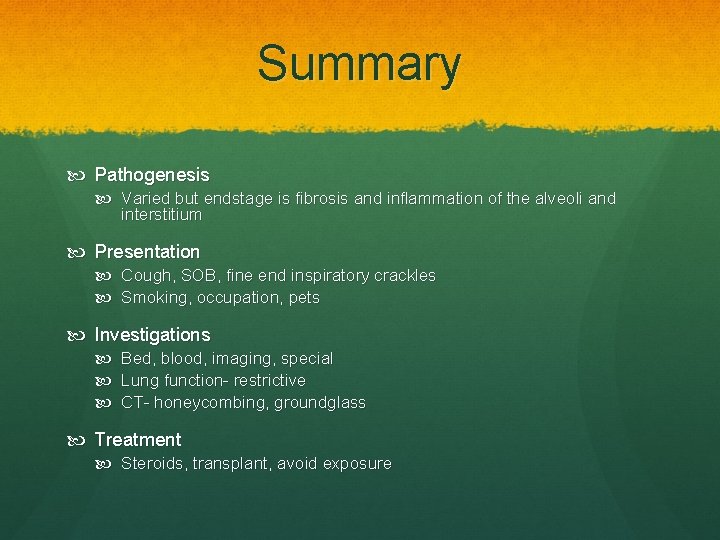
Summary Pathogenesis Varied but endstage is fibrosis and inflammation of the alveoli and interstitium Presentation Cough, SOB, fine end inspiratory crackles Smoking, occupation, pets Investigations Bed, blood, imaging, special Lung function- restrictive CT- honeycombing, groundglass Treatment Steroids, transplant, avoid exposure
Case study A 64 year old gentleman presents to his GP with increasing SOB over the last 6 months. His exercise tolerance has reduced to the point where walking to the corner shop makes him out of breath. He also complains of a dry cough. He has a past medical history of high blood pressure which is managed with Ramipril. He has never smoked and works as an office manager. On examination he is slightly short of breath with O 2 sats 93% on air and he has clubbing. Auscultation reveals bilateral basal fine end inspiratory crepitations and no wheeze.
? ? What are your main differential diagnoses for this gentleman? (make sure these include all important differentials that must be ruled out) How would you investigate this gentleman? What is your management plan? Will anything help? Can you tell me about the pathophysiology of ILD? Can you tell me some causative organisms for EAA?
Any questions
 Kerley b lines
Kerley b lines Caplan syndrome
Caplan syndrome Restrictive lung disease
Restrictive lung disease Dohányos tüdő
Dohányos tüdő Farmer's lung disease
Farmer's lung disease Obstructive vs restrictive
Obstructive vs restrictive Copd lungs images
Copd lungs images What is a restrictive lung disease
What is a restrictive lung disease Dpld lung disease
Dpld lung disease Obstructive and restrictive lung disease
Obstructive and restrictive lung disease Restrictive lung disease
Restrictive lung disease Paul lung biography
Paul lung biography Communicable disease and non communicable disease
Communicable disease and non communicable disease Hydrostatic vs osmotic pressure
Hydrostatic vs osmotic pressure Interstitial condensation definition
Interstitial condensation definition Epiphyseal line
Epiphyseal line Intracellular extracellular fluid
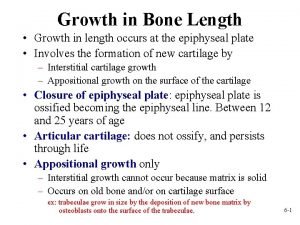
Intracellular extracellular fluid Interstitial and appositional growth of cartilage
Interstitial and appositional growth of cartilage Vacancy defect and interstitial defect
Vacancy defect and interstitial defect Interstitial alloy
Interstitial alloy Steel interstitial alloy
Steel interstitial alloy Interstitial pattern
Interstitial pattern Extracellular fluid and interstitial fluid
Extracellular fluid and interstitial fluid Interstitial velocity
Interstitial velocity Water balance regulation
Water balance regulation Solid
Solid Interstitial velocity
Interstitial velocity Colloid osmotic pressure vs hydrostatic pressure
Colloid osmotic pressure vs hydrostatic pressure Interstitial impurity atom
Interstitial impurity atom Interstitial and appositional growth of cartilage
Interstitial and appositional growth of cartilage Acute interstitial nephritis urine findings
Acute interstitial nephritis urine findings Chapter 26 fluid electrolyte and acid-base balance
Chapter 26 fluid electrolyte and acid-base balance Cardiovascular changes
Cardiovascular changes Hypoosmotic
Hypoosmotic Ecf icf and interstitial fluid
Ecf icf and interstitial fluid Peristalsis
Peristalsis Tightly attached ceiling
Tightly attached ceiling Thể thơ truyền thống
Thể thơ truyền thống Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau V. c c
V. c c Phép trừ bù
Phép trừ bù Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates