PLEURAL EFFUSION hydrothorax The pleural space normally contains
- Slides: 19
PLEURAL EFFUSION (hydrothorax) The pleural space normally contains a very thin layer of fluid. A pleural effusion is present when there is an ↑ quantity of fluid in the pleural space. Etiology Normally, fluid enters the pleural space from: 1 - The capillaries in the visceral pleura and is removed via the lymphatics situated in the parietal pleura. ﺑﻮﺍﺑﺎﺕ ﺩﺧﻮﻝ ﻭﺧﺮﻭﺝ 2 - The interstitial spaces of the lung via the visceral pleura or 3 - The peritoneal cavity via small holes in the diaphragm. So, pleural effusion may develop when: 1 - There is ↑ pleural fluid formation (from the interstitial spaces of the lung, parietal pleura, or peritoneal cavity) or 2 - when there is ↓ fluid removal by the lymphatics.
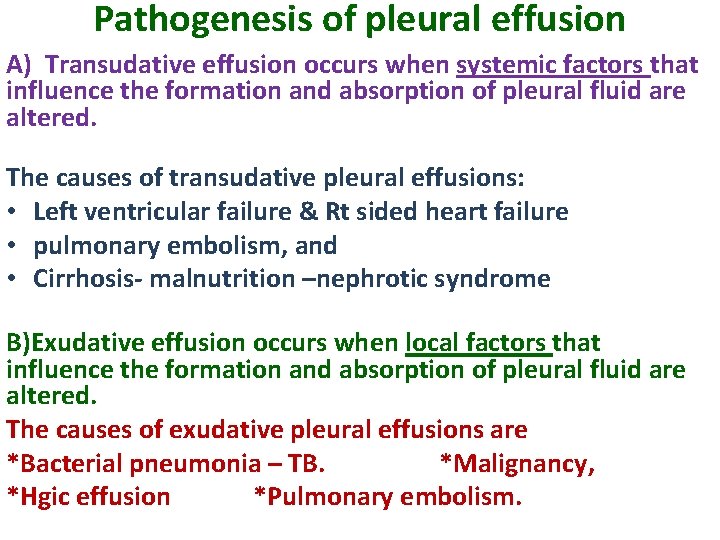
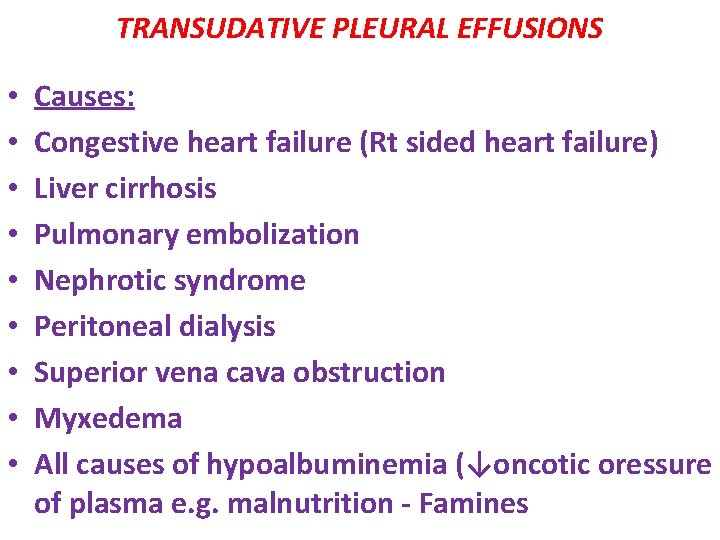
Pathogenesis of pleural effusion A) Transudative effusion occurs when systemic factors that influence the formation and absorption of pleural fluid are altered. The causes of transudative pleural effusions: • Left ventricular failure & Rt sided heart failure • pulmonary embolism, and • Cirrhosis- malnutrition –nephrotic syndrome B)Exudative effusion occurs when local factors that influence the formation and absorption of pleural fluid are altered. The causes of exudative pleural effusions are *Bacterial pneumonia – TB. *Malignancy, *Hgic effusion *Pulmonary embolism.
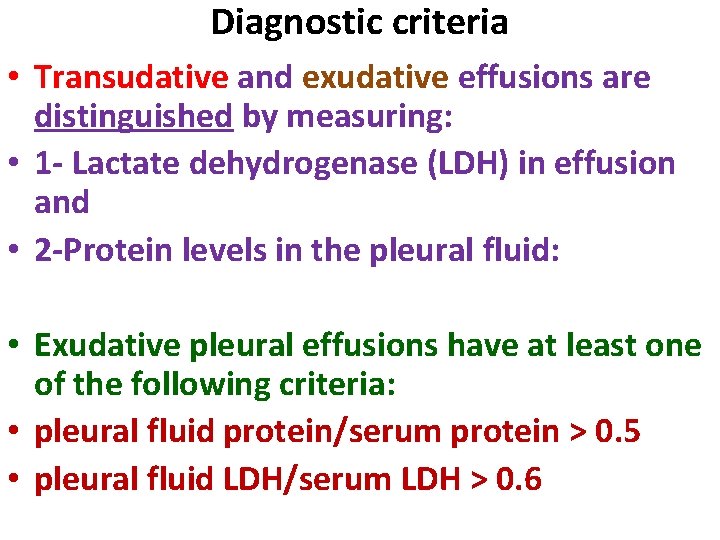
Diagnostic criteria • Transudative and exudative effusions are distinguished by measuring: • 1 - Lactate dehydrogenase (LDH) in effusion and • 2 -Protein levels in the pleural fluid: • Exudative pleural effusions have at least one of the following criteria: • pleural fluid protein/serum protein > 0. 5 • pleural fluid LDH/serum LDH > 0. 6
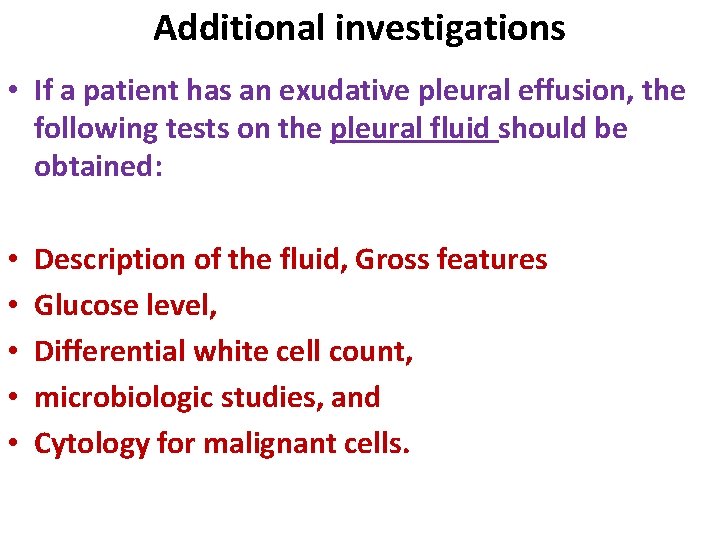
Additional investigations • If a patient has an exudative pleural effusion, the following tests on the pleural fluid should be obtained: • • • Description of the fluid, Gross features Glucose level, Differential white cell count, microbiologic studies, and Cytology for malignant cells.
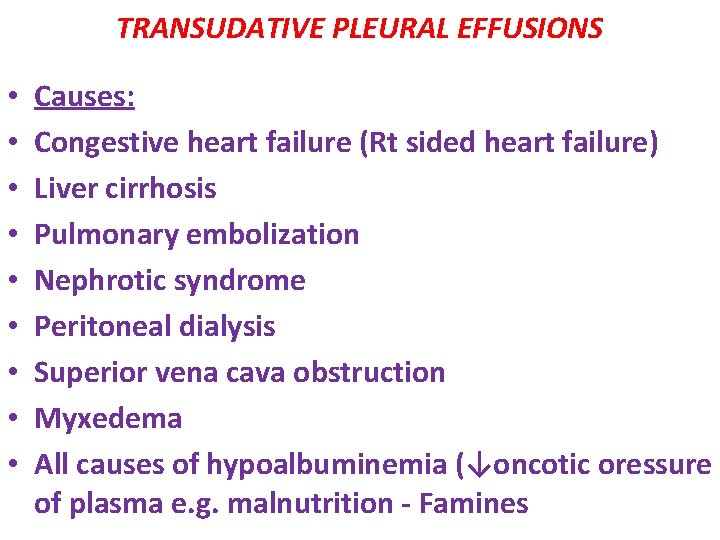
TRANSUDATIVE PLEURAL EFFUSIONS • • • Causes: Congestive heart failure (Rt sided heart failure) Liver cirrhosis Pulmonary embolization Nephrotic syndrome Peritoneal dialysis Superior vena cava obstruction Myxedema All causes of hypoalbuminemia (↓oncotic oressure of plasma e. g. malnutrition - Famines
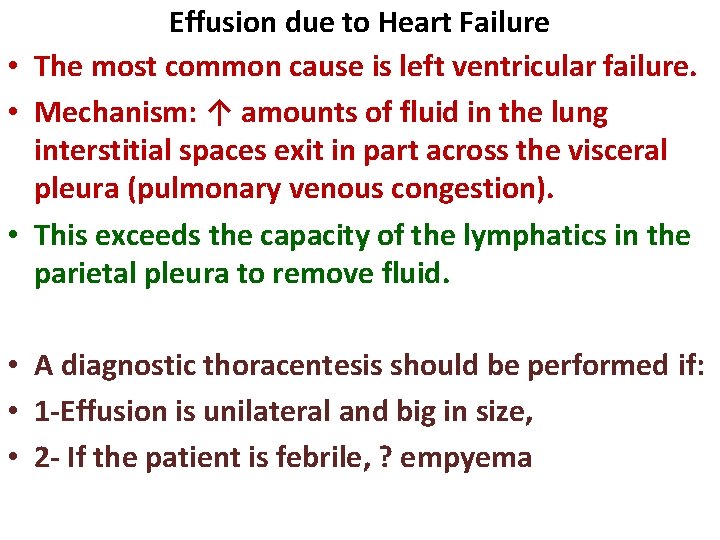
Effusion due to Heart Failure • The most common cause is left ventricular failure. • Mechanism: ↑ amounts of fluid in the lung interstitial spaces exit in part across the visceral pleura (pulmonary venous congestion). • This exceeds the capacity of the lymphatics in the parietal pleura to remove fluid. • A diagnostic thoracentesis should be performed if: • 1 -Effusion is unilateral and big in size, • 2 - If the patient is febrile, ? empyema
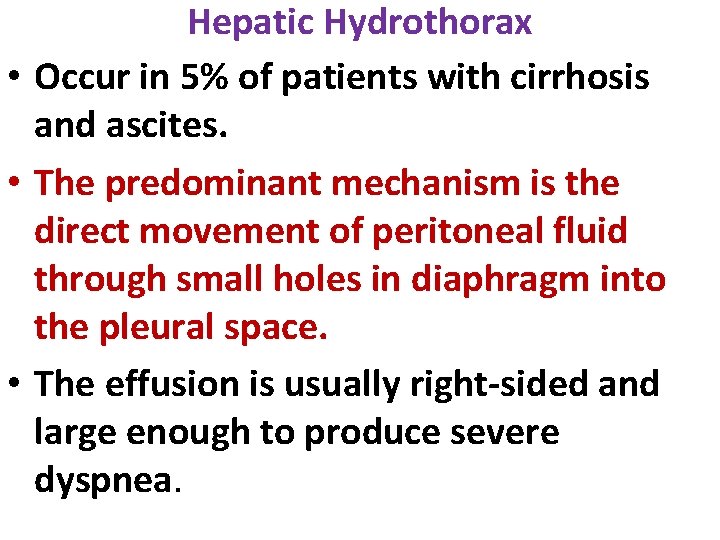
Hepatic Hydrothorax • Occur in 5% of patients with cirrhosis and ascites. • The predominant mechanism is the direct movement of peritoneal fluid through small holes in diaphragm into the pleural space. • The effusion is usually right-sided and large enough to produce severe dyspnea.
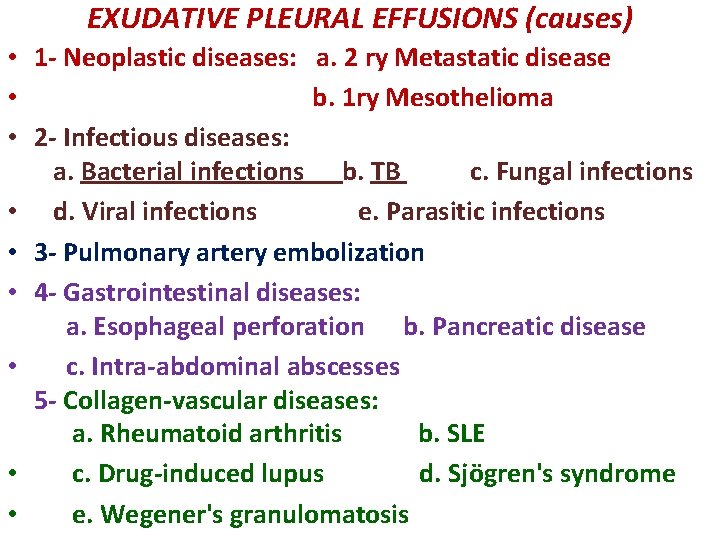
EXUDATIVE PLEURAL EFFUSIONS (causes) • 1 - Neoplastic diseases: a. 2 ry Metastatic disease • b. 1 ry Mesothelioma • 2 - Infectious diseases: a. Bacterial infections b. TB c. Fungal infections • d. Viral infections e. Parasitic infections • 3 - Pulmonary artery embolization • 4 - Gastrointestinal diseases: a. Esophageal perforation b. Pancreatic disease • c. Intra-abdominal abscesses 5 - Collagen-vascular diseases: a. Rheumatoid arthritis b. SLE • c. Drug-induced lupus d. Sjögren's syndrome • e. Wegener's granulomatosis
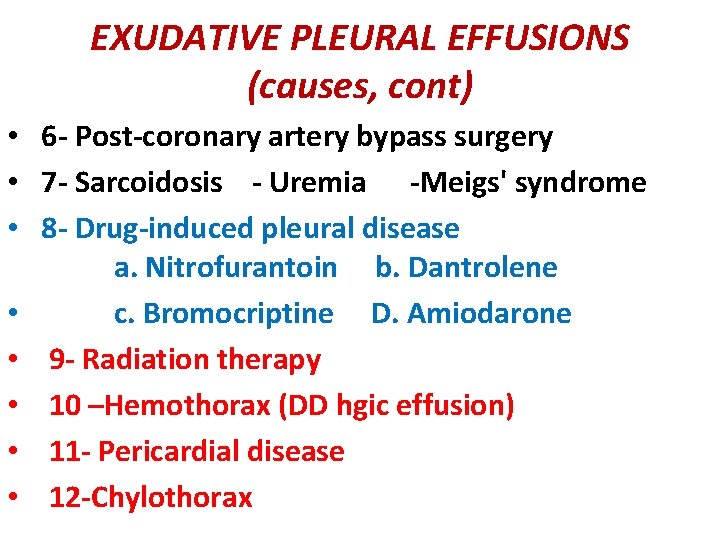
EXUDATIVE PLEURAL EFFUSIONS (causes, cont) • 6 - Post-coronary artery bypass surgery • 7 - Sarcoidosis - Uremia -Meigs' syndrome • 8 - Drug-induced pleural disease a. Nitrofurantoin b. Dantrolene • c. Bromocriptine D. Amiodarone • 9 - Radiation therapy • 10 –Hemothorax (DD hgic effusion) • 11 - Pericardial disease • 12 -Chylothorax
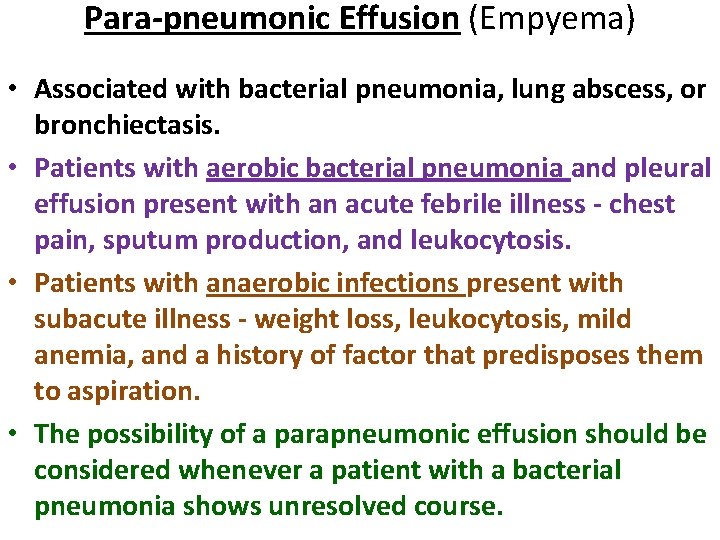
Para-pneumonic Effusion (Empyema) • Associated with bacterial pneumonia, lung abscess, or bronchiectasis. • Patients with aerobic bacterial pneumonia and pleural effusion present with an acute febrile illness - chest pain, sputum production, and leukocytosis. • Patients with anaerobic infections present with subacute illness - weight loss, leukocytosis, mild anemia, and a history of factor that predisposes them to aspiration. • The possibility of a parapneumonic effusion should be considered whenever a patient with a bacterial pneumonia shows unresolved course.
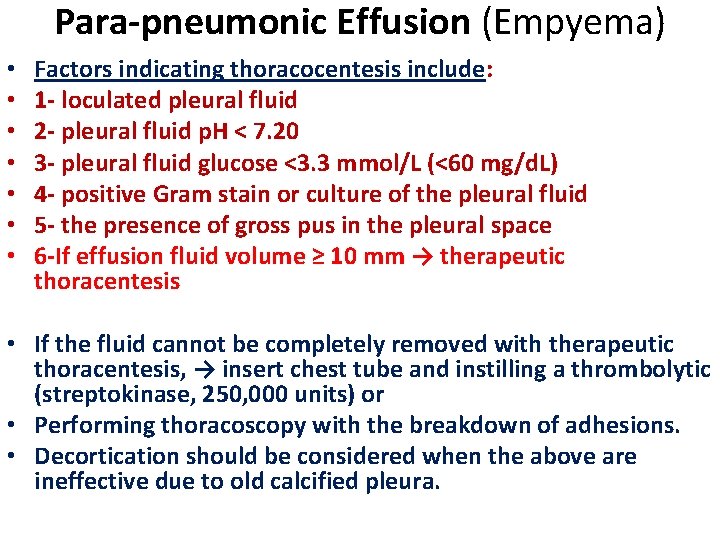
Para-pneumonic Effusion (Empyema) • • Factors indicating thoracocentesis include: 1 - loculated pleural fluid 2 - pleural fluid p. H < 7. 20 3 - pleural fluid glucose <3. 3 mmol/L (<60 mg/d. L) 4 - positive Gram stain or culture of the pleural fluid 5 - the presence of gross pus in the pleural space 6 -If effusion fluid volume ≥ 10 mm → therapeutic thoracentesis • If the fluid cannot be completely removed with therapeutic thoracentesis, → insert chest tube and instilling a thrombolytic (streptokinase, 250, 000 units) or • Performing thoracoscopy with the breakdown of adhesions. • Decortication should be considered when the above are ineffective due to old calcified pleura.
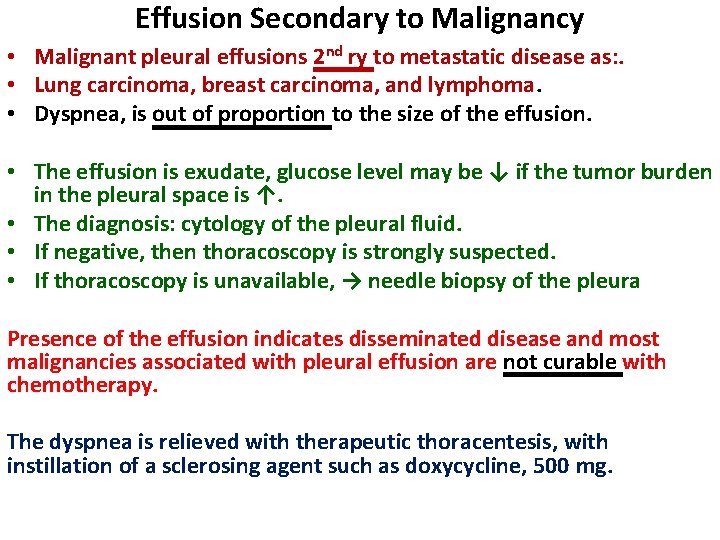
Effusion Secondary to Malignancy • Malignant pleural effusions 2 nd ry to metastatic disease as: . • Lung carcinoma, breast carcinoma, and lymphoma. • Dyspnea, is out of proportion to the size of the effusion. • The effusion is exudate, glucose level may be ↓ if the tumor burden in the pleural space is ↑. • The diagnosis: cytology of the pleural fluid. • If negative, then thoracoscopy is strongly suspected. • If thoracoscopy is unavailable, → needle biopsy of the pleura Presence of the effusion indicates disseminated disease and most malignancies associated with pleural effusion are not curable with chemotherapy. The dyspnea is relieved with therapeutic thoracentesis, with instillation of a sclerosing agent such as doxycycline, 500 mg.
Malignant Mesothelioma • Primary tumors that arise from the mesothelial cells that line the pleural space. • Most are related to asbestos exposure or smoking. • Chest pain and shortness of breath. • The chest X-ray: reveals a pleural effusion, generalized pleural thickening, and may be hemithorax. • Thoracoscopy or open pleural biopsy is usually necessary. • • Treatment: Radical surgery, chemotherapy, and radiation therapy.
Tuberculous pleural effusion • The most common cause of an exudative pleural effusion. • Due primarily to a hypersensitivity reaction to TB protein in the pleural space. • Symptoms: Fever, weight loss, dyspnea, and/or pleuritic chest pain. • Exudate with predominantly small lymphocytes • + High levels of TB markers in the pleural fluid (adenosine deaminase > 45 IU/L, interferon γ > 140 pg/m. L, or + ve (PCR) for tuberculous DNA). • Diagnosis can be established by culture of the pleural fluid, needle biopsy of the pleura, or thoracoscopy. • The recommended treatment of pleural and pulmonary tuberculosis is identical.
Hemothorax • Definition: • Bloody pleural fluid, with its hematocrit is > 50% that of the peripheral blood. • DD. hgic effusion: ˂ 50% hematocrit than peripheral blood • Most hemothoraces are the result of: • 1 -Trauma; • 2 -Rupture of a blood vessel or tumor in pleural space. • If the pleural hemorrhage exceeds 200 m. L/h, thoracotomy should be done which allows continuous quantification of bleeding → Cardiothoracic surgery. • If the bleeding from a laceration of the pleura, apposition of the two pleural surface is likely to stop the bleeding.
PNEUMOTHORAX • Presence of gas in the pleural space. • Types: 1 - Primary Spontaneous Pneumothorax: in the absence of underlying lung disease • Causes: Rupture of apical pleural blebs (small cystic spaces that lie immediately under the visceral pleura). • Occur almost exclusively in smokers, which suggests that these patients have subclinical lung disease. Usually recurrent. The initial treatment is simple aspiration. If the lung does not expand with aspiration, or if the patient has a recurrent pneumothorax, thoracoscopy with stapling of blebs is indicated.
2 -Secondary Spontaneous Pneumothorax occurs in its presence of chronic lung diseases such as : COPD. • Pneumothorax in patients with chronic lung disease is life-threatening ˃ in normal individuals because of the lack of pulmonary reserve in these patients. • Patients should be treated with tube thoracostomy insertion and the instillation of a sclerosing agent such as doxycycline.
3 - Traumatic Pneumothorax • Result from both penetrating and non-penetrating chest trauma (malignant infiltration). • Should be treated with tube thoracostomy unless they are very small. • If a hemo-pneumothorax is present, chest tube should be placed in the superior part of the hemithorax to evacuate the air, • and another should be placed in the inferior part of the hemithorax to remove the blood. • Iatrogenic pneumothorax is a common type of traumatic pneumothorax due to • 1 - transthoracic needle aspiration, • 2 -thoracentesis, and • 3 -Insertion of central IV catheters. PORT-A-CATH • .
4 - Tension Pneumothorax • The pressure in the pleural space is positive throughout the respiratory cycle. It is a medical emergency. • Occurs during mechanical ventilation or resuscitative efforts. • It is life-threatening because: • 1 -Ventilation is severely compromised and • 2 -The +ve pressure is transmitted to the mediastinum, which →↓ venous return to the heart and ↓ cardiac output. • The diagnosis: • A) Bulging hemi-thorax with no breath sounds and • B) Shift of the mediastinum to the contralateral side. • C)Marked hypoxemia. • A large-bore needle should be inserted into the pleural space through the 2 nd anterior intercostal space. • If big amount of gas escape the diagnosis is confirmed. The needle should be left in place until a thoracostomy tube can be inserted.