Compliance Compliance is the extent to which the
- Slides: 18
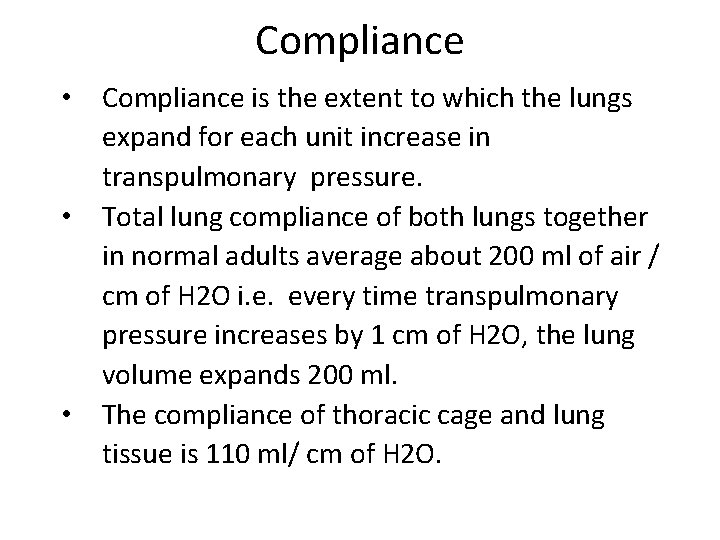
Compliance • Compliance is the extent to which the lungs expand for each unit increase in transpulmonary pressure. • Total lung compliance of both lungs together in normal adults average about 200 ml of air / cm of H 2 O i. e. every time transpulmonary pressure increases by 1 cm of H 2 O, the lung volume expands 200 ml. • The compliance of thoracic cage and lung tissue is 110 ml/ cm of H 2 O.
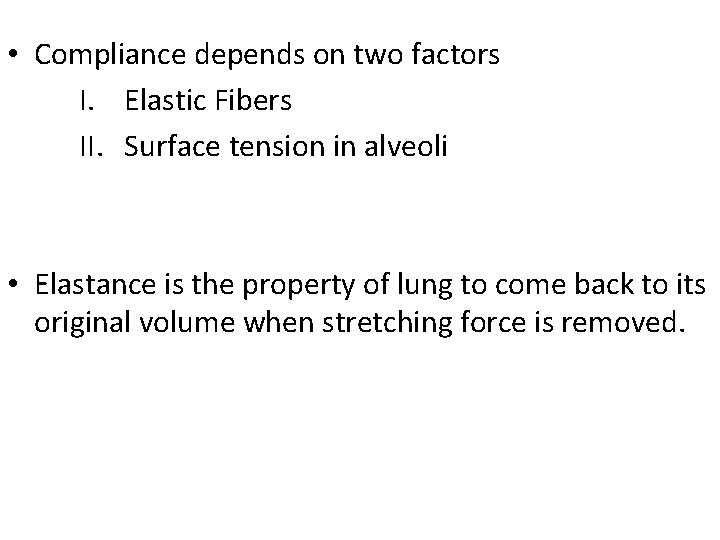
• Compliance depends on two factors I. Elastic Fibers II. Surface tension in alveoli • Elastance is the property of lung to come back to its original volume when stretching force is removed.
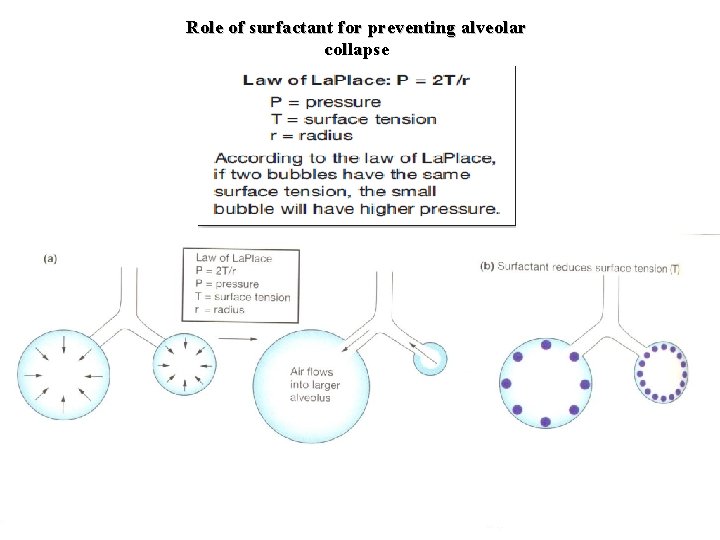
Surface Tension in Alveoli • The law of La. Place states that the pressure within a fluid-lined alveolus depends on two factors: the surface tension of the fluid and the radius of the alveolus. This relationship is expressed by the equation P = 2. T/ r
Surfactant • It is a mixture containing lipoprotein such as dipalmitoylphosphatidylcholine, apoproteins and calcium ions • Secreted by type II alveolar cells. • Secretion starts at 25 th week of gestation, peak at 32 nd week. • Hyaline membrane disease
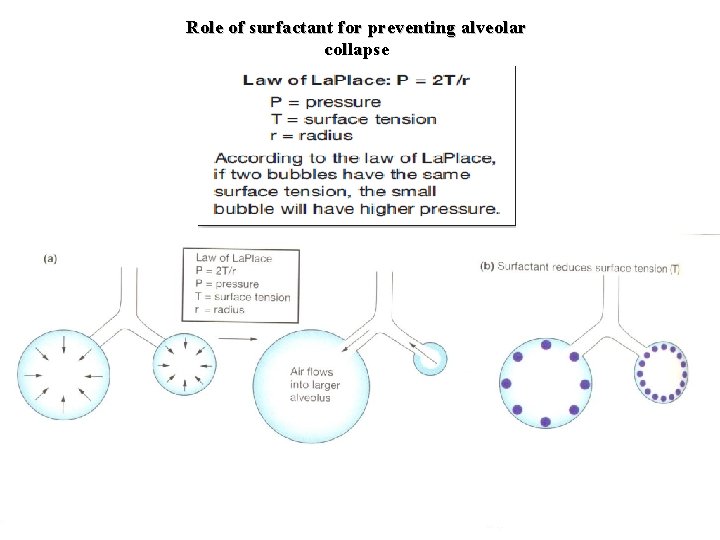
Role of surfactant for preventing alveolar collapse
Airway resistance • Poiseuille’s Law R is directly proportional to Lη/r
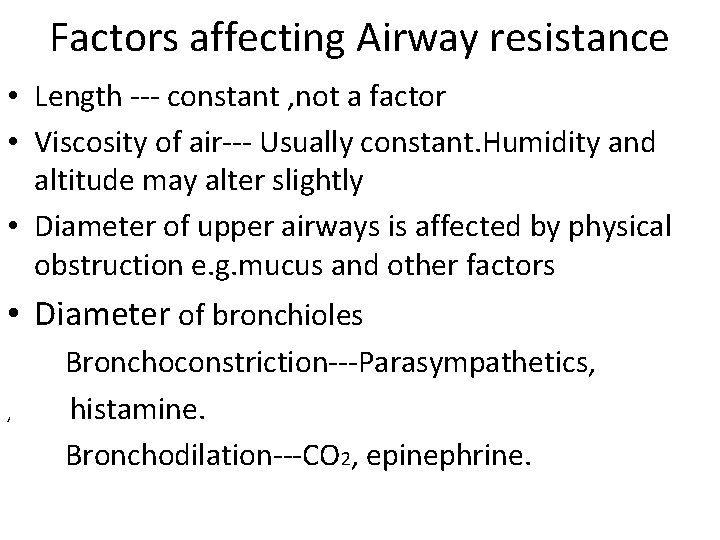
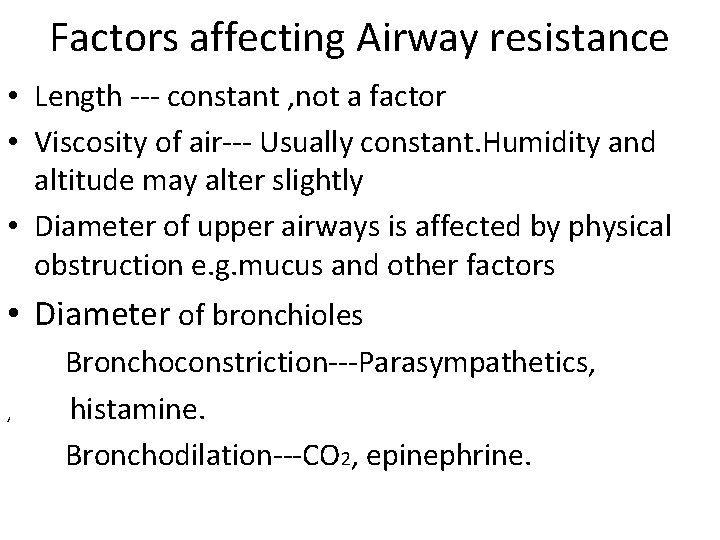
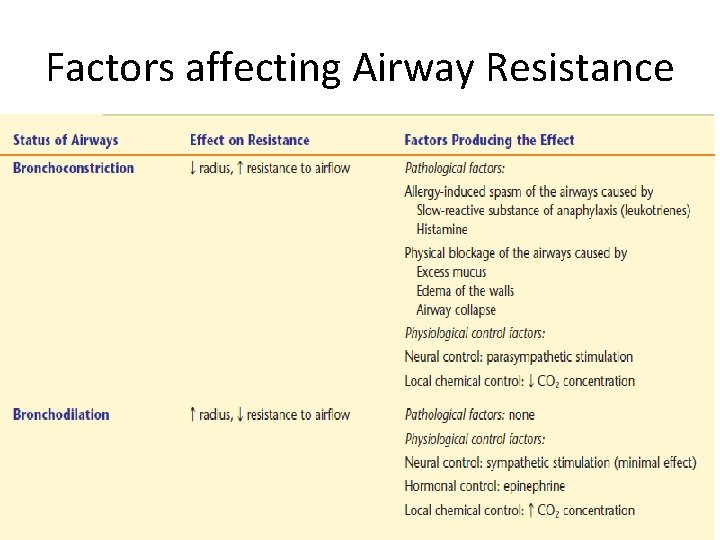
Factors affecting Airway resistance • Length --- constant , not a factor • Viscosity of air--- Usually constant. Humidity and altitude may alter slightly • Diameter of upper airways is affected by physical obstruction e. g. mucus and other factors • Diameter of bronchioles , Bronchoconstriction---Parasympathetics, histamine. Bronchodilation---CO 2, epinephrine.
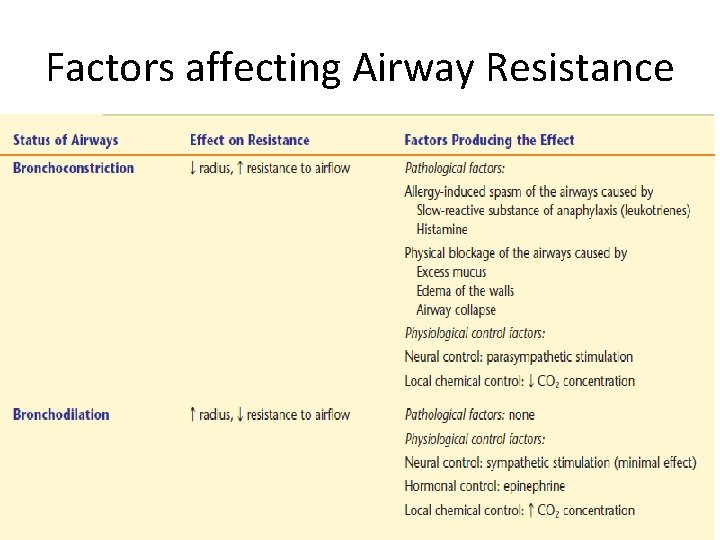
Factors affecting Airway Resistance
Obstructive Airway Diseases • Chronic Bronchitis • Asthma • Emphysema
Fibrotic lung diseases • Often results from the chronic inhalation of fine particulate matter that escapes the mucus lining of the airways and reaches the exchange epithelium of the alveoli , eventually resulting in formation of inelastic scar tissue. • The proliferation of inelastic scar tissue in the lung is called fibrotic lung disease or fibrosis. • Inorganic particles that can trigger fibrosis are asbestos, coal dust, silicon, and even dust and pollutants of urban areas.
Pulmonary Ventilation Pulmonary ventilation is defined as inflow & outflow of air between the atmosphere & the lung alveoli Inflow Inspiration Outflow Expiration
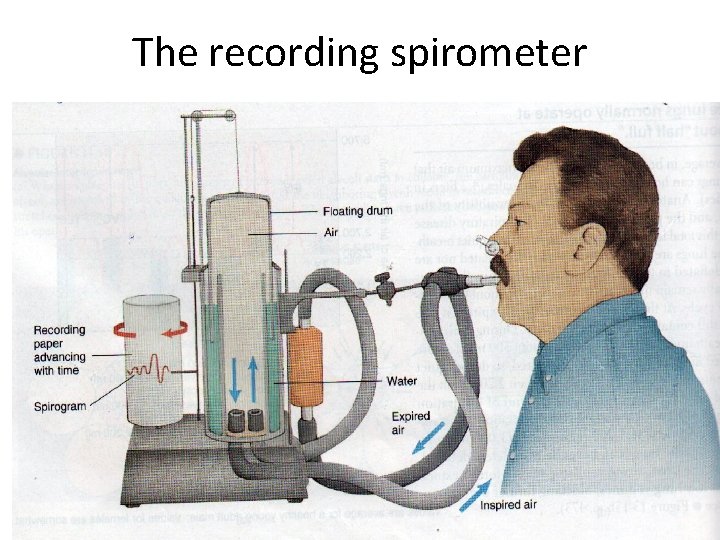
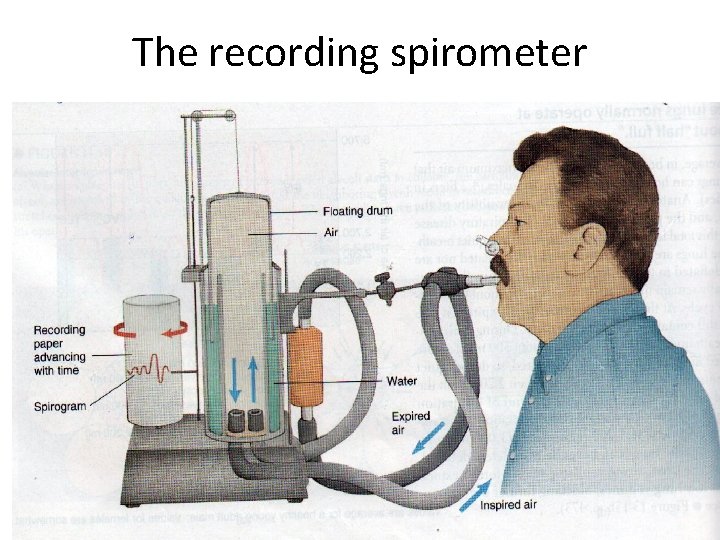
The recording spirometer
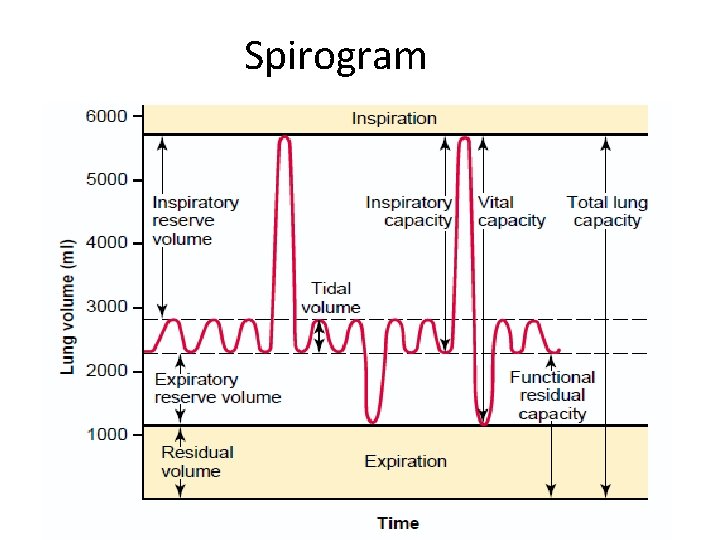
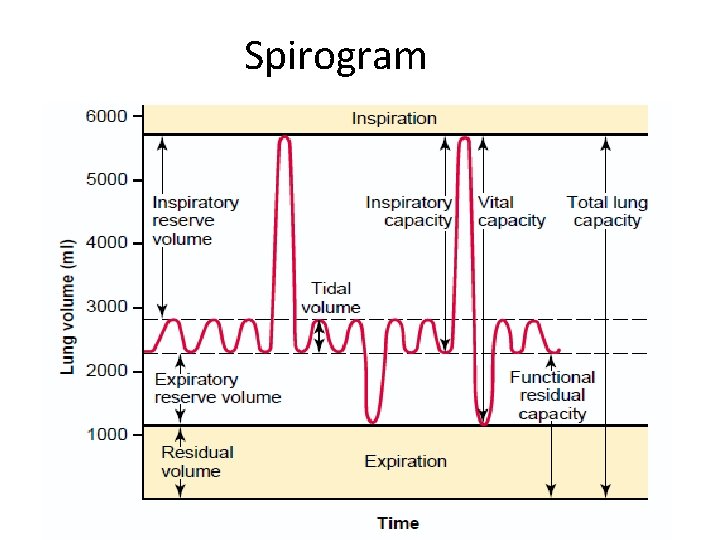
Spirogram
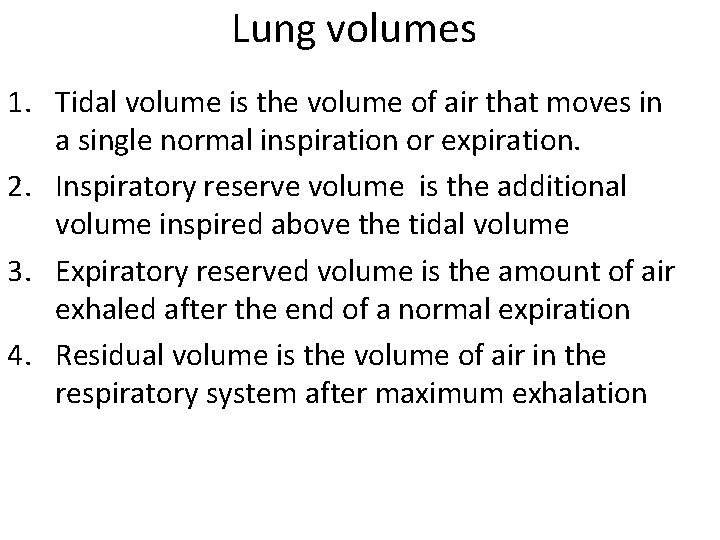
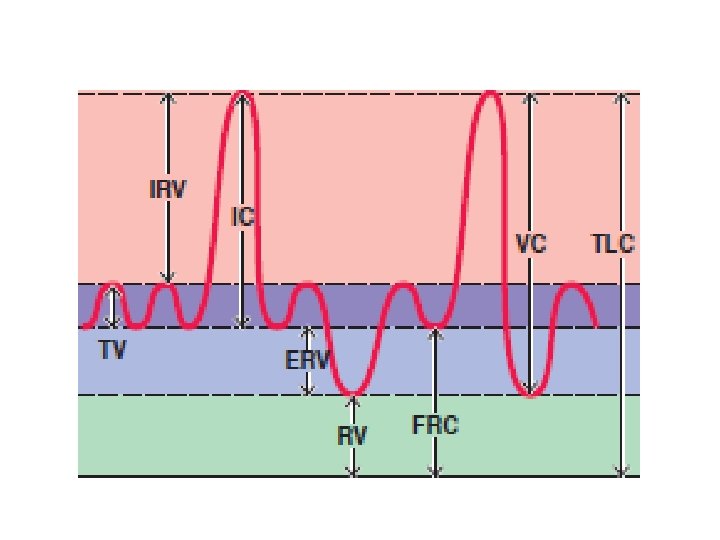
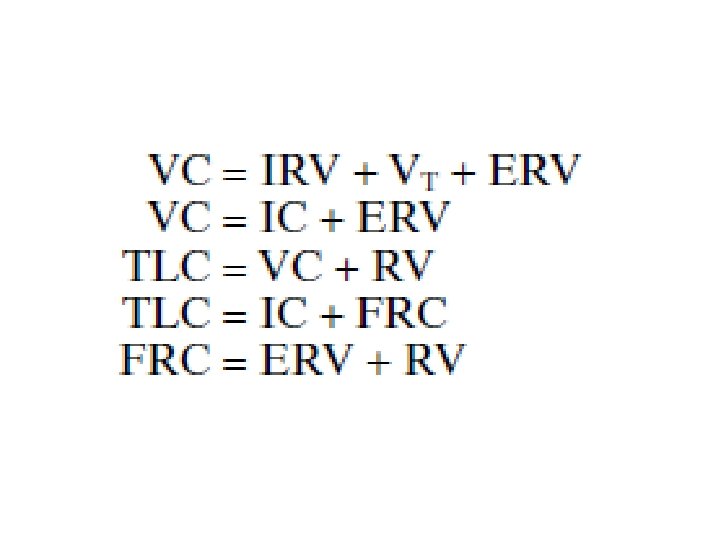
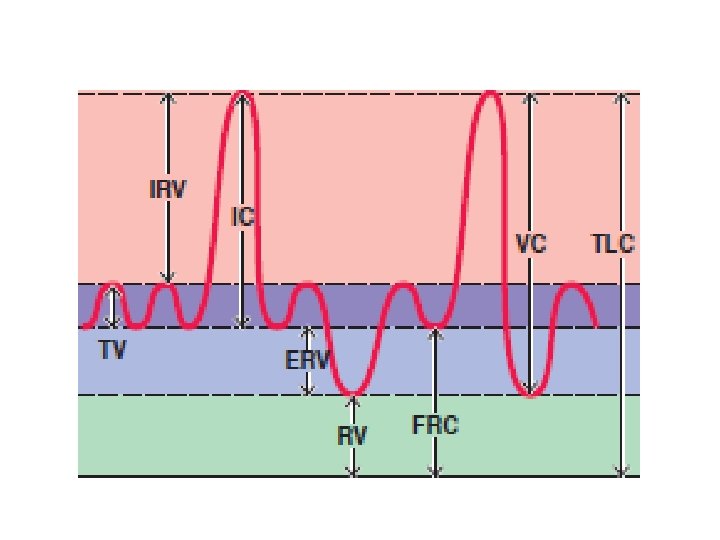
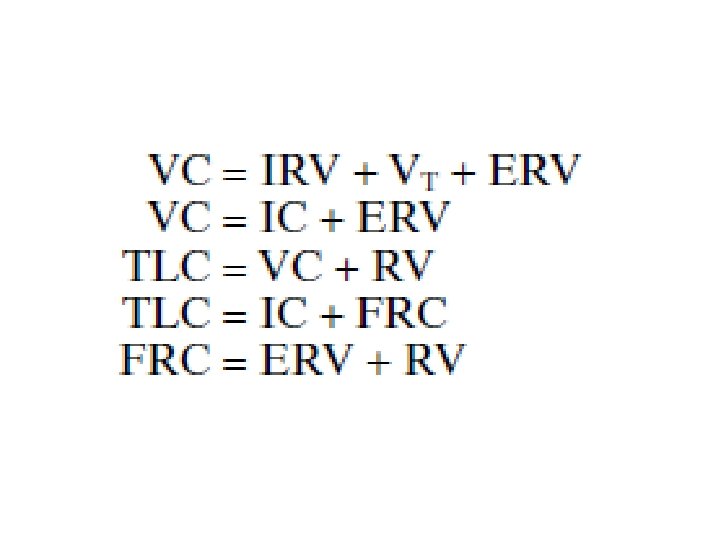
Lung volumes 1. Tidal volume is the volume of air that moves in a single normal inspiration or expiration. 2. Inspiratory reserve volume is the additional volume inspired above the tidal volume 3. Expiratory reserved volume is the amount of air exhaled after the end of a normal expiration 4. Residual volume is the volume of air in the respiratory system after maximum exhalation
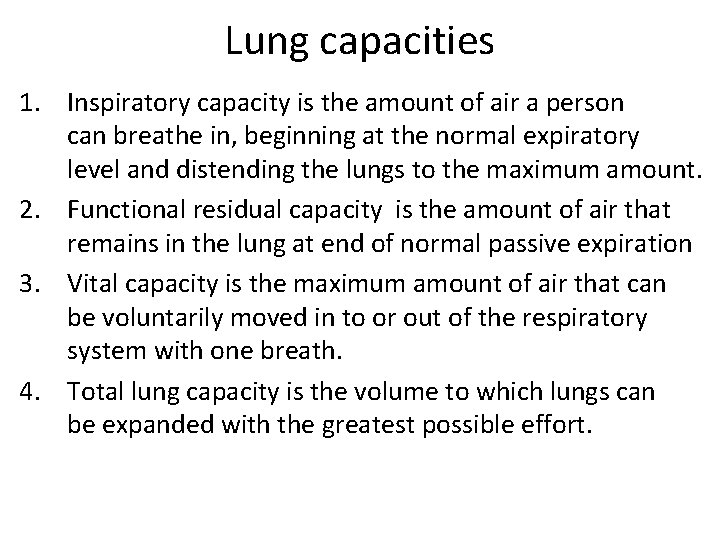
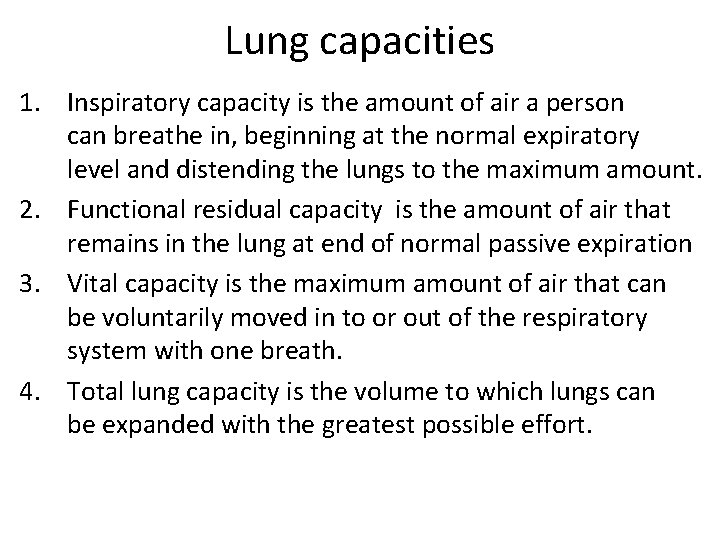
Lung capacities 1. Inspiratory capacity is the amount of air a person can breathe in, beginning at the normal expiratory level and distending the lungs to the maximum amount. 2. Functional residual capacity is the amount of air that remains in the lung at end of normal passive expiration 3. Vital capacity is the maximum amount of air that can be voluntarily moved in to or out of the respiratory system with one breath. 4. Total lung capacity is the volume to which lungs can be expanded with the greatest possible effort.
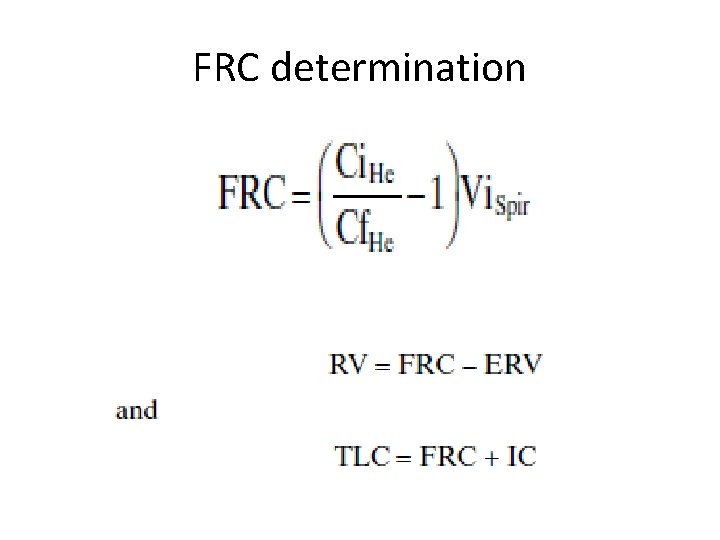
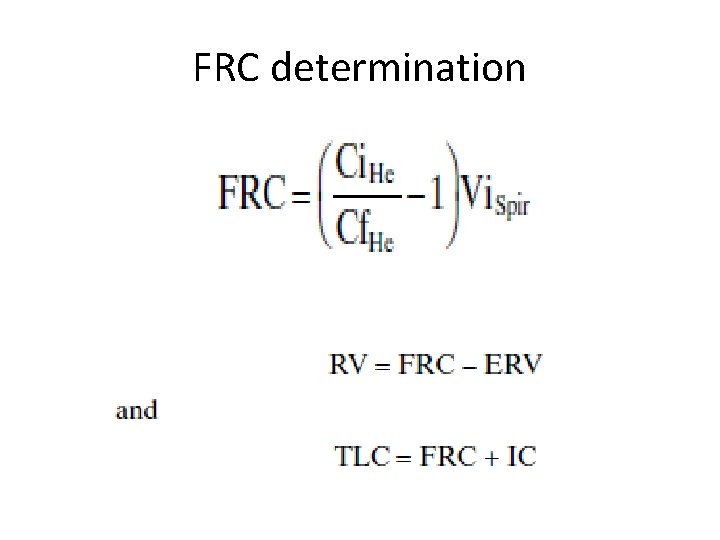
FRC determination
 Which bird can rotate its neck backwards to a large extent
Which bird can rotate its neck backwards to a large extent To what extent has canada affirmed collective rights
To what extent has canada affirmed collective rights Uk at its greatest extent
Uk at its greatest extent Extent of researcher interference
Extent of researcher interference Importance of nature of delinquency
Importance of nature of delinquency Face validity examples
Face validity examples To what extent should we embrace globalization
To what extent should we embrace globalization To what extent should internationalism be pursued
To what extent should internationalism be pursued To what extent has canada affirmed collective rights
To what extent has canada affirmed collective rights To what extent should nation be the foundation of identity?
To what extent should nation be the foundation of identity? Apush essay prompts
Apush essay prompts To what extent should we embrace nationalism
To what extent should we embrace nationalism Is resistance to liberalism justified
Is resistance to liberalism justified To what extent has beowulf remained an epic hero?
To what extent has beowulf remained an epic hero? Extent of researcher interference
Extent of researcher interference How do neurotransmitters influence behavior
How do neurotransmitters influence behavior To what extent adverbs
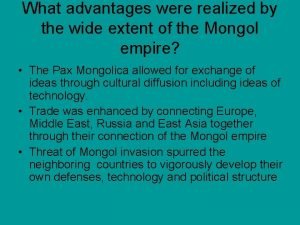
To what extent adverbs Wide extent
Wide extent