HESIATI Review Catherine Ramos Marin MSNEd WHCNP RN





- Slides: 125
HESI/ATI Review Catherine Ramos Marin, MSN/Ed, WHCNP, RN August 12, 2011
Physiological Changes in Pregnancy Ø Ø Ø Integumentary- as result of increased estrogen and progesterone- linea nigra, cholasma, and palmar erythema Neurological- Carpal Tunnel Syndrome, decreased attention span Heart- increased blood flow- 30 -50%, “physiological anemia 11 -12 Hgb
Physiological Changes in Pregnancy (Continued) n n n Supine Hypotension Syndrome- don’t have patient lie on her back (complaints of dizziness, diaphoresis and pallor) Respiratory Syndrome- increased oxygen requirements, Eyes, Ears, Nose and Throat- c/o blurry vision, increased mucus membranes, throat congestion
Physiological Changes in Pregnancy n n GI- gingivitis, ptyalism (increased saliva), heartburn Urinary System- Increased urgency, frequency and nocturia (1 st trimester), urine urgency and nocturia decreases (2 nd trimester), increased urgency and frequency (3 rd trimester) because fetus starts engaging in the pelvis
Physiological Changes in Pregnancy Ø Thyroid- increased size, HPL (humal placental lactogen- insulin antagonistincreases the number of circulating fatty acides to meet maternal metabolic needs and decreases maternal glucose utilization which increases glucose availability to the fetus- Macrosomia babies- decreased HPL and large babies ten to be Hypoglycemic
Physiological Changes in Pregnancy n Musculoskeletal System- diastasis recti, relaxin- produced by placenta and causes laxity of ligaments
Prenatal Labs n Blood Group with Rh factor, RPR, Hepatitis B, CBC, HIV, Sickle Cell screen for women at risk
Signs of Pregnancy n n n Presumptive changes- breast changes, n/v, amenorrhea, frequent urination, fatigue, uterine enlargement, quickening, linea nigra, melasma, striae gravidarum Probable- elevated HCG Definite- fetal heart tones
Gravida-parity • Gravida- number of times a woman has been pregnant • Para- number of times infants delivered after twenty weeks gestation born dead of alive • Remember, multiple births counts as one delivery • TPAL is a detailed description of Para
Danger Signs of Pregnancy Vaginal bleeding Ø Persistent vomiting Ø Chills and fever Ø Ruptured membranes Ø
Danger Signs of Pregnancy (Continued) n n n n Severe, persistent headache Visual disturbances Edema of face or hands Abdominal pain Epigastric pain Painful urination persistent vomiting Change in or absence of fetal movement (e. g. , no movement for 6 -8 hours)
Identifying the High-Risk Pregnancy Ø High-risk pregnancy Ø A concurrent disorder, pregnancyrelated complication, or external factor jeopardizes the health of the mother, fetus or both

Preterm Labor u. Terbutaline, Procardia, Nifedipine, Mg. So 4 u. For Terbutaline make sure you consider maternal pulse
Shoulder Dystocia n n n Dispositions leading to shoulder dystocia? Result- brachial plexus injury Mc. Roberts Maneuver
Positions other than cephalic (pages 604 -605, Pilletteri) n n n Transverse, Breech Usually at 34 weeks the presentation is established Leopold’s Maneuver n n n Grasp the uterine fundus between the thumb and middle finger of one hand Soft feeling (buttocks) Round, firm and easily moved (head)
Other presentations of fetus n If it is Breech n n n Complete, frank and footling Higher risk because of anoxia from prolapsed cord, traumatic injury to the aftercoming head Fracture of the spine or arm Dysfunctional labor Early rupture of membranes
Multiple Gestations n n Susceptible to complications such as PIH, hydramnios, placenta previa, preterm labor, and anemia Increased Incidence of Postpartum Bleeding
Placenta Ø 80% of low-lying placentas are resolved or go down in proper position by 28 weeks
Abruptio Placentae n n n n “Premature separation of the normally implanted placenta from the uterine wall Can occur from 20 weeks of pregnancy or in the 1 st or 2 nd stage of labor Factors: multiple gestations, hydramnios (excess fluid) cocaine use, decreased blood flow to the placenta Trauma to the abdomen Low serum folic acid level Vascular or renal disease Gestational hypertension
Abruptio Placentae n n Signs- abdominal pain, contractions, back pain Vaginal bleeding and uterine tenderness may be absent “Boardlike” abdomen, uterine irritability, tetanic contractions Result- hypotension, shock, fetal bradycardia and fetal death
Placenta Previa n n “Placenta implants in varying degrees in the lower uterine segment, below the presenting part of the baby” A total or complete previa covers the entire internal cervical os: Partia previa-covers part of the internal os Painless bleeding
Placenta Previa n n n Can be diagnosed as early as first 20 weeks of gestation. However, this usually resolves 90% of the time Need to be on pelvic rest (nothing in the vagina such as intercourse, tampon, douching) Avoid masturbation- don’t want uterine contractions
Maternal and Fetal Responses to Labor Ø Danger signs of labor - fetal Heart rate Ø Meconium staining Ø Hyperactivity Ø Ø Fetal acidosis
Maternal and Fetal Responses Ø Danger signs of labor - maternal Blood pressure Ø Abnormal pulse Ø Inadequate or prolonged contractions Ø Pathologic retraction ring Ø Abnormal lower abdominal contour Ø Apprehension Ø
Premature Rupture of Membranes n n n Loss of amniotic fluid before 37 weeks of pregnancy Usually associated with chorioamnionitis (infection in the fluid). Increased risk of cord prolapse
Complications of Premature Rupture of Membranes n Respiratory Distress Syndrome n Infants try to compensate by releasing surfactant (to aid in the maturation of the lungs)
NST AND CST n n n Non-stress test- evaluates HR in response to fetal movement Reactive= 2 -4 FHR accelerations in 10 minutes without side effects Contraction stress test-evaluates FHR in response to uterine contractions Negative-no late FHR decels produced by UCS Side effects of CST include overstiumulation of the uterus secondary to use of oxytocin
True vs. False Labor: Client Preparation n False Labor (Contractions) n n Benign and irregular contractions Felt first abdominally and remain confined to the abdomen and groin Often disappear with ambulation and sleep. Contractions do not increase in duration, frequency or intensity
False Labor (Cervix) n n No significant change in dilation or effacement Often remains in posterior position No significant bloody show Fetus- presenting part is not engage in pelvis
True Labor (Contractions) n n Contractions begin irregularly but become regular and predictable Felt first in lower back and sweep around to the abdomen in a wave Contractions continue no matter what the women’s level of activity Contractions increase in duration, frequency, and intensity
True Labor (Cervix) n n Progressive change in dilation and effacement Moves to anterior portion Bloody show Fetus is in the presenting part engages in pelvis
Labor Induction n Definition- the deliberate initiation of uterine contractions to stimulate labor before spontaneous onset to bring about the birth either by chemical or mechanical means
Methods include n n n Prostaglandins (Cervidil, prostin gel, Prepidil, Cytotec) applied cervically) Pitocin administration Amniotomy or stripping of membranes Nipple stimulation to trigger the release of endogenous oxytocin Sexual intercourse
Indications for induction of labor n n n n Postterm pregnancy (beyond 42 weeks) Premature or prolonged rupture of membranes Dystocia (prolonged, difficult labor) Maternal complications (Rh isoimmunization, Diabetes, Pulmonary disease, Pregnancy-induced hypertension) Fetal demise Chorioamnionitis Suspected fetal problems- Intrauterine Growth restriction and hydrops (fetal hemolytic disorder as result of Rh isoimmunization when maternal immune system attacks fetal red blood cells
Cervical Ripening and Assessment n n n Baseline data on fetal and maternal well -being (at least half an hour of monitoring) Fetal monitoring and uterine contraction monitoring is imperative Notify MD is hyperstimulation or fetal heart rate distress is noted
Oxytocin Induction n n Confirmation that the head is presented in a cephalic position and at 0 station (ideally) IUPC- Intrauterine Pressure Catheter monitors precisely frequency, duration, and intensity of contractions V/S done at least every 30 minutes and when dose is titrated FHTs and UCS monitored every 15 minutes I/Os
Oxytocin Induction (Continued) n n Bishop Score- rating that determines if the cervix is adequate for induction Titration of Oxytocin till UCs every 2 -3 minutes, lasting 60 -90 seconds, intensity 4090 mm HG (IUPC) Cervical dilation should be 1 cm/hr (ideally) Reassuring FHTs between 110 -160 beats/min
When to discontinue Oxytocin n n Frequency of UCs less than 2 minutes apart Contractions longer than 90 seconds Contractions intensity greater than 90 mm Hg on IUPC Uterine resting tone greater than 20 mm Hg between contractions (no rest between UCs)
Nonreassuring fetal heart rate n n n FHTs baseline less than 110 and greater than 160 beats/minute Loss of variability Late or prolonged decelerations
Intervention for oxytocin hyperstimulation n n n Turn off oxytocin Side-lying position, preferably left to increase uteroplacental perfusion Increase IVFs O 2 via mask 8 -10 L/min Tocolytics (Brethine subcutaneously or IV) Monitor FHTS and V/S Document responses to all above interventions
Need for Fetal Heart Rate Monitoring (Intermittent) n n n Home births and birthing centers Allows for greater maternal freedom of movement Non Stress Tests
Continuous Fetal Monitoring n n n Multiple gestations Placenta Previa Oxytocin infusion Fetal bradycardia Maternal Complications (Gestational Diabetes Intrauterine Growth Retardation
Continuous Fetal Monitoring n n n n Post dates Meconium-stained amniotic fluid Abruption placenta- suspected or actual Abnormal non-stress test Abnormal uterine contractions Fetal distress Provider preference and facility protocol
Fetal Heart Tones n n Between 110 -160 Early Decels- head comprehension Variable Decels- Cord compression Late Decels- Placental uterounsuffciency
Ruptured Membranes n n Nitrazine paper turns black or dark blue Vaginal fluid “ferns” under microscope Note color, amount of amniotic fluid If laboring mom ambulates, fetus MUST be at station zero or below (ENGAGED) or there is an increased risk chance of prolapsed cord
Rupture of Membranes n n Spontaneous rupture of membranes can initiate labor or can occur anytime during labor, most commonly during the transition phase Labor usually occur within 24 hours of rupture of membranes Prolonged rupture of membranes greater than 24 hour before delivery of fetus may lead to an infection Immediately following the rupture of membranes, assess fetal heart rate for abrupt decelerations indicative of fetal distress to rule out umbilical cord prolapse
Assessment of amniotic fluid n n n Color- pale to straw yellow Odor- should not be foul Clarity- watery and clear Volume between 500 to 1200 ml Nitrazine paper tests p. H of fluid wnd will turn deep blue determining alkalinity- if negative it remains yellow or it may be urine instead of amniotic fluid
Amniotomy n n “AROM”- Artificial Rupture of Membranes Nurse should record baseline of FHT prior and after procedure Assess color, amount, consistency and odor Document time of amniotomy and findings
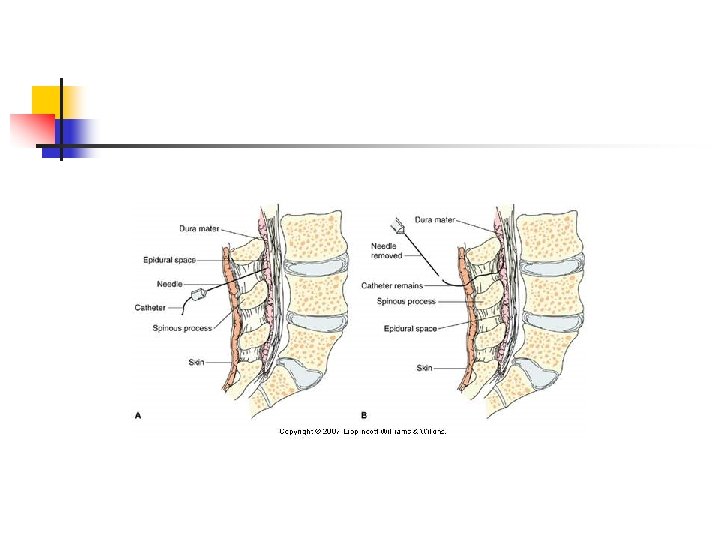
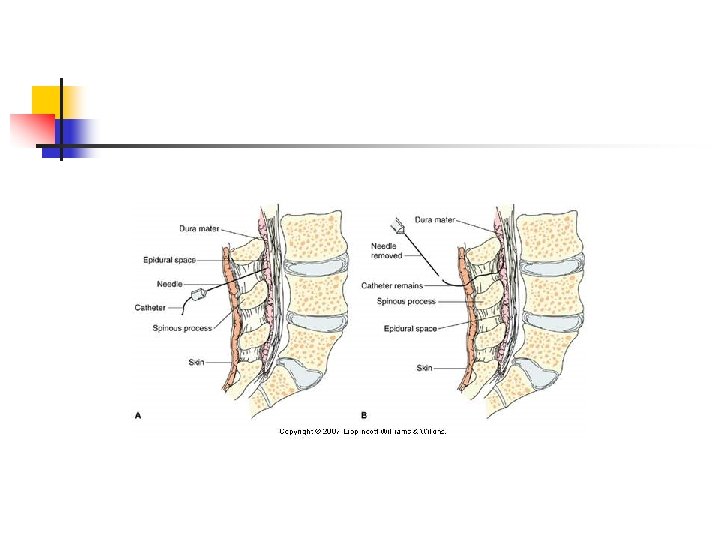
Regional Anesthesia Ø Injection of local anesthesia to block specific nerve pathways Ø Epidural anesthesia Nursing care Ø Administration Ø Ø Spinal anesthesia
Problems with the Passenger Prolapse of umbilical cord Ø Multiple gestation Ø
Prolapsed Cord n n It is safer for patient to remain in bed after rupture of membranes (especially in they rupture in Stage 1 of labor) Place patient in Tredelenberg or knee-chest position Also vaginally push the head back away from the cord. If during the V. E. you feel the cord you may not be able to let go and your hand may remain in place till C-section is performed.
Stages of labor n n Stage 1 - LAT Stage 2 - pushing at 10 cm to delivery of infant Stage 3 - Delivery of infant to Delivery of placenta Stage 4 - Delivery of Placenta to 2 -4 hours of recovery
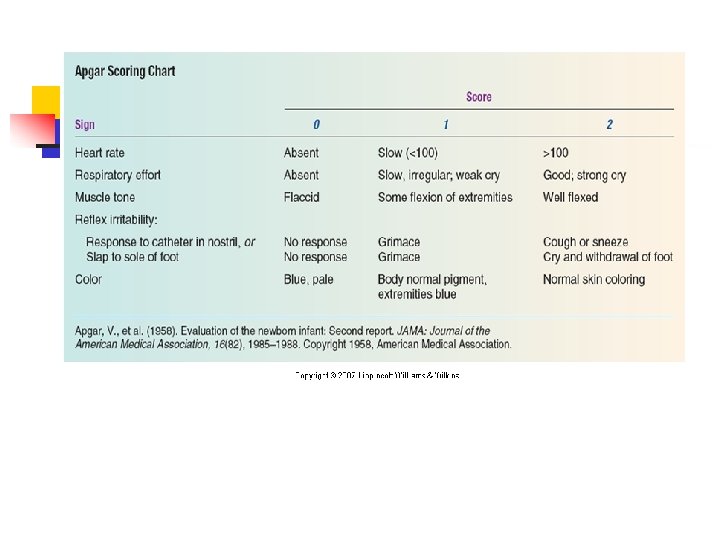
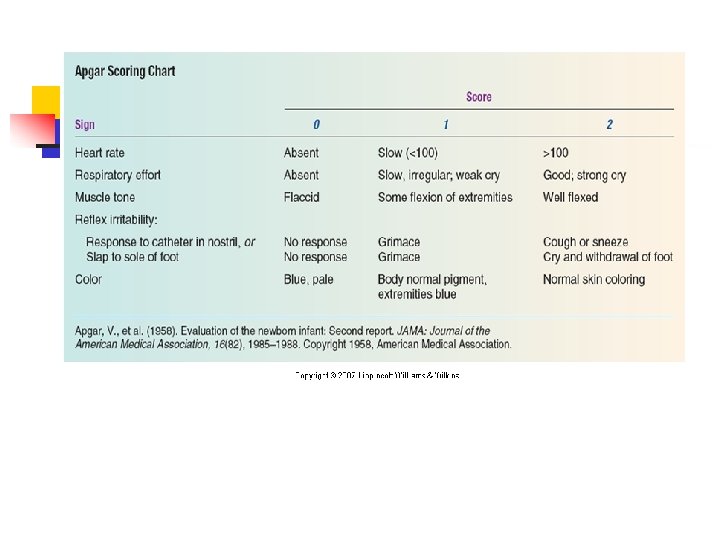
Assessment for Well. Being Ø Apgar scoring Heart rate Ø Respiratory effort Ø Muscle tone Ø Reflex irritability Ø Color Ø
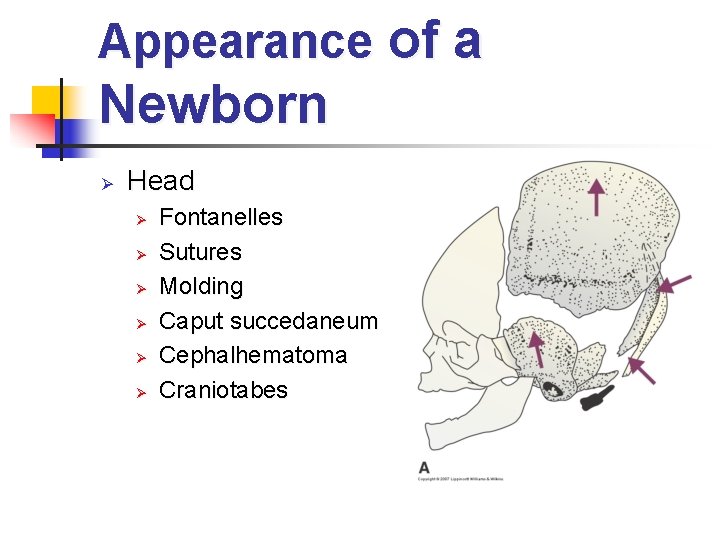
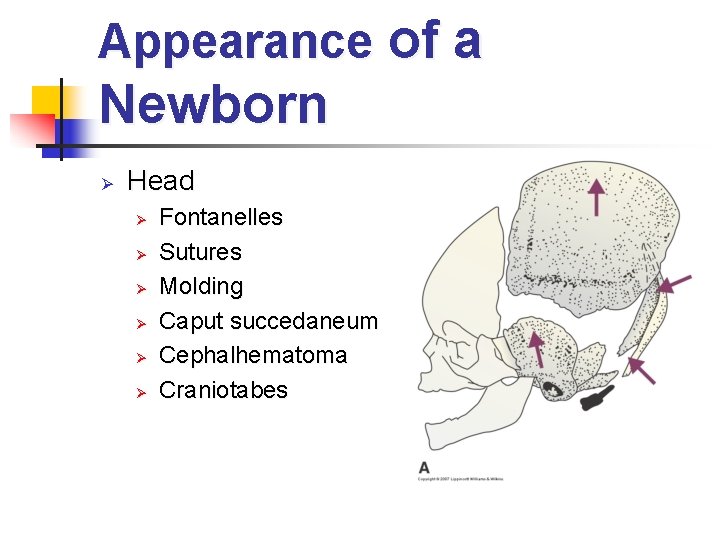
Appearance of a Newborn Ø Head Ø Ø Ø Fontanelles Sutures Molding Caput succedaneum Cephalhematoma Craniotabes
Appearance of a Newborn Ø Skin Vernix caseosa Ø Lanugo Ø Desquamation Ø Milia Ø Erythema toxicum Ø Forceps marks Ø
Appearance of a Newborn Eyes Ø Ears Ø Nose Ø Mouth Ø Neck Ø Chest Ø
Appearance of a Newborn Abdomen Ø Anogenital area Ø Ø Ø Male genitalia Female genitalia Back Ø Extremities Ø
FAS Newborn ØNote The Facial Features
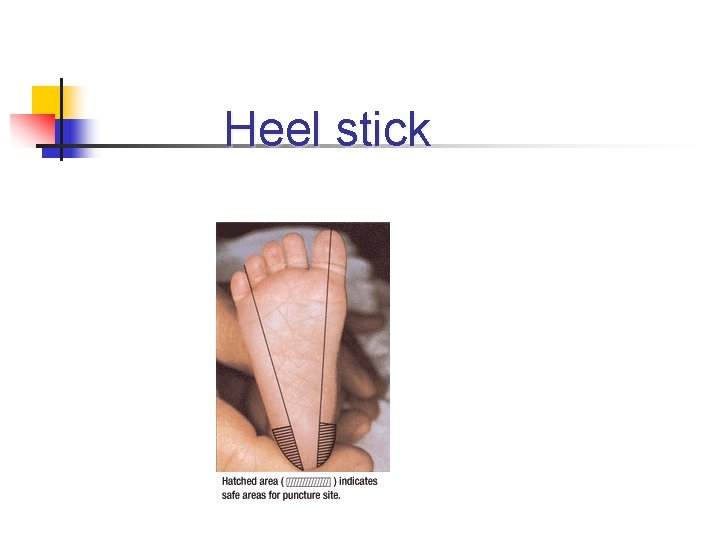
Assessment for Well. Being Keeping the newborn warm Ø Promoting adequate breathing pattern Ø Record of first cry Ø Inspection and care of umbilical cord Ø Eye care Ø Infection precautions Ø Heelstick- lateral portion of foot Ø
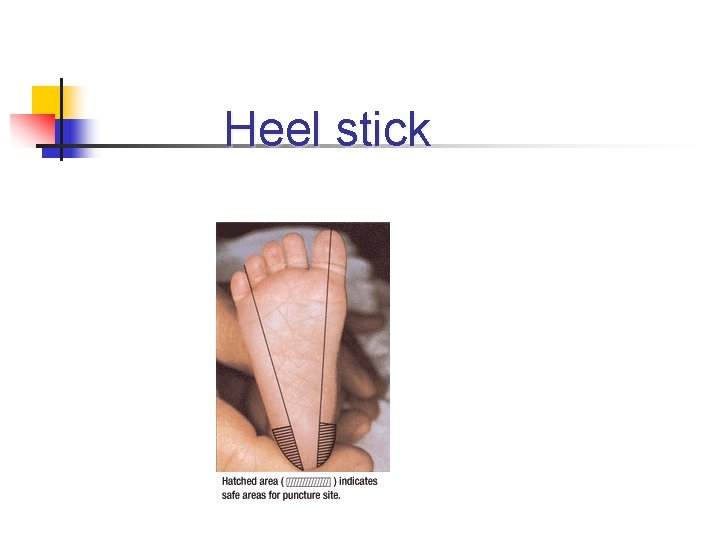
Heel stick
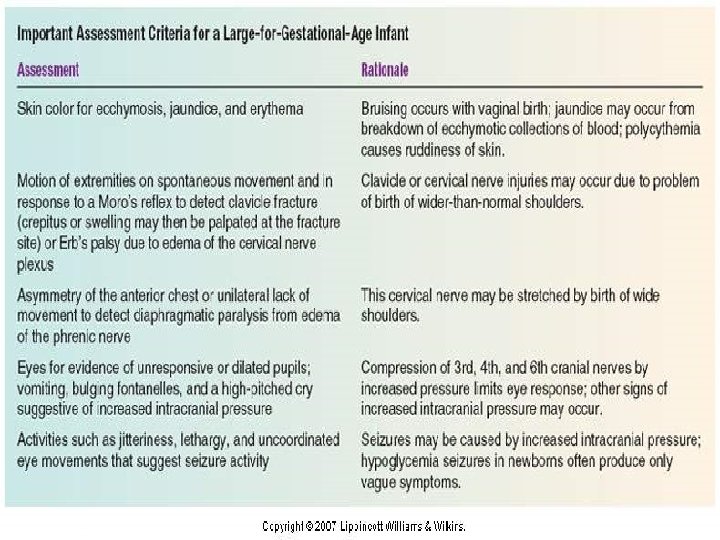
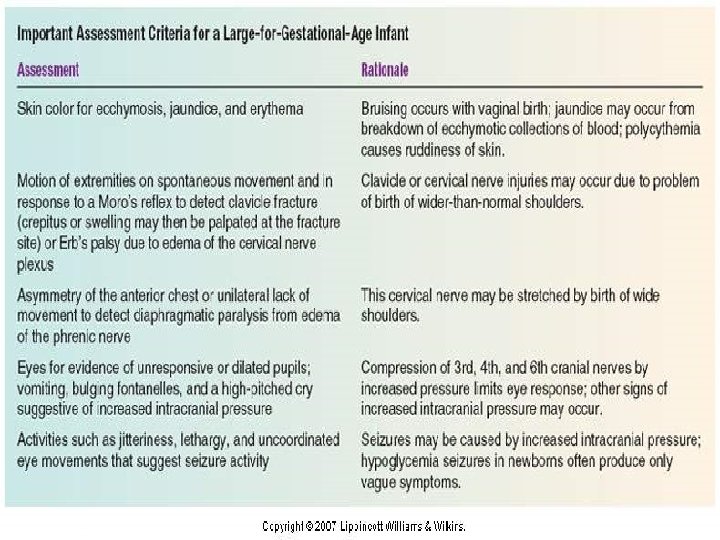
Altered Gestational Age or Birthweight Ø Large for gestational age Causes Ø Assessment Ø Appearance Ø Cardiovascular dysfunction Ø Hypoglycemia Ø
Altered Gestational Age or Birthweight Ø Small for gestational age Causes Ø Assessment Ø Prenatal Ø Appearance Ø Laboratory findings Ø


Hypoglycemia n n n Due to decreased glycogen storage in liver. Hypoglycemia usually happens to infants of Gestational Diabetes Mothers S/S includes jitteriness, tremors, lethargy, hypotonia, apnea weak or high -pitched cry, eye-rolling and seizures
Post Term Infant n n Definition- born after 42 weeks gestation Causes n Dysmaturity- uteroplacental insufficiency which may result in fetal hypoxia, fetal distress. This conditions can result in polycythemia (increase in the number of RBCs) and meconium aspiration and neonatal respiratory problems
Post Term Infant n In a fetus continues to grow- this can result in cephalopelvic disproportion and high insulin reserves and insufficient glucose reserves at birth. n n Birth Trauma- perinatal asphyxia, clavicle fracture, seizures, hypoglycemia and temperature instability- cold stress LGA or SGA
Post Term Infant n Persistent Pulmonary Hypertension (persistent fetal circulation) n n As a result from meconium aspiration Interference in the transition from fetal to neonatal circulation and the ductus arteriosus(connecting main artery and the aorta) and foramen ovale (shunt between the right and left atria)
Nursing Assessments 1. Signs and Symptoms n n n Wasted appearance (thin and loose skin) Peeling, cracked, dry skin Long thin body Meconium staining (fingernails) Long hair and nails Increased alert (similar to a 2 week old)
Signs and Symptoms of Postterm infant n n Difficulty establishing respirations (secondary to meconium aspiration) Signs and symptoms of cold stress Increased development of neurological skills Macrosomia
Nursing assessment of postterm infant n n n Observe for birth injury or trauma Respiratory status Reflexes Monitoring vital signs and temperature Monitoring intravenous fluids
Nursing Diagnoses n n n Ineffective airway clearance related to meconium aspiration Risk for aspiration related to the presence of meconium Ineffective thermoregulation related to decreased subcutaneous fat
Nursing interventions for the postterm infant n n n Assisting with surfactant lavages during delivery to prevent meconium aspiration Suctioning meconium from the neonate’s mouth and nares before the first breath Mechanical ventilation PRN
Nursing Interventions for the Postterm infant (continued) n n n Administering oxygen as prescribed Administering intravenous fluids Preparing or assisting with exchange transfusion if hematocrit is high
Nursing Interventions for the Postterm infant (continued) n Exchange Transfusion n First, aspirate stomach first in order to avoid potential aspiration. Then, the umbilical vein is catheterized as the site for transfusion. The procedure involves alternatively withdrawing 2 -10 ml of the infant’s blood and then replacing it with equal amounts of donor blood. Blood is exchanged slowly to prevent hypovolemia and hypervolemia. Takes 1 -3 hours.
Nursing Interventions for the Postterm infant (continued) n n n Provide thermoregulation in an incubator in order to avoid cold stress Provide early feedings to avoid hypoglycemia Identify and treating birth injuries
Newborn Assessment: Respiratory Distress n 5 symptoms of respiratory distress n n n Tachypnea Cyanosis Flaring nares Expiratory grunt Retractions
Neonates at risk for Respiratory Distress Syndrome Preterm infants n Infants of diabetic mothers n Infants born by cesarean birth n Decreased blood perfusion of the lungs (one cause is meconium aspiration) Remember, surfactant usually don’t form until 34 th week gestation n
Betamethasone ØInfants cannot receive surfactant after 34 weeks ØMeasure L/S ratio and PG hormone presence using amniocentesis
Sample Question n Which of the following signs pertaining to respirations indicate that a newborn is having no difficult adapting to extrauterine life? n n Expiratory grunting Respirations of 46/min Inspiratory nasal flaring Apnea for 10 second periods
Sample Question n Obligator nose breathing Respirations of 26/min Crackles and wheezing
Answer to Sample Question n Respirations of 46/min Apnea for 10 sec periods Obligatory nose breathing
Risk Factors contributing to RDS n n n Decreased gestational age Perinatal asphyxia Maternal diabetes Premature rupture of membranes Maternal use of barbiturates or narcotics close to birth Maternal hypotension
Risk Factors contributing to RDS (continued) n n n Cesarean birth without labor Hydrops fetalis (massive edema of the fetus caused by hyperbilirubinemia) Maternal bleeding during the third trimester
Assessment of infants with Respiratory Distress Syndrome n n Low Body Temperature Nasal Flaring Sternal and subcostal retractions Tachypnea (more than 60 respirations per minute) Cyanotic mucous membranes
Newborn Care: Positions for Sleep n n n Baby is to be positioned on the back Sudden Infant Death Syndromesudden, unexplained death of an infant younger than 1 year of age. Positioning on the back decreases the incidence of SIDS
Sleep Wake Cycle n n Supine position decreases risk for SIDS Sleep 16 our of 24 hours and 2 -3 hours at a time Don’t add cereal to diet till 4 -6 months of age Infants should never sleep in parents’ bed
Hyperbilirubinemia: Phototherapy Nursing Care n Hyperbilirubin- results from destruction of red blood cells either a normal physiologic process or abnormal destruction or RBCs
Physiologic Jaundice n n Benign condition Usually occurs after 24 hours of age
Pathologic Jaundice n n Before 24 hours or persistent after day 7 Bilirubin increases more than 0. 5 mg/dl/hr, peaks at greater than 13 mg/dl or associated with anemia and hepatosplenomegaly Rh incompatibility/isoimmunization, infection, RBC disorder Kernicterus (bilirubin encephalopathy) can result from untreated hypergbilirubinemia with bilirubin levels at or higher than 25 mg/dl.
Factors that affect development of hyperbilirubinemia n n n Increased RBC production or breakdown Rh or ABO incompatibility Decreased liver function Maternal enzymes in breast mil. Ineffective breastfeeding Certain medications (aspirin, tranquilizers, and sulfonamides).
Factors that affect development of hyperbilirubinemia(Continued) n n n Hypogycemia Hypothermia Anoxia
Lab Testing n n n Elevated serum bilirubin (direct and indirect) Blood group incapability between the mother and newborh Hemoglobin and hematocrit Direct Coomb’s test- reveals presence of antibody-coated (sensitized) Rh-positive RBCs in the newborn Electrolyte levels for dehydration from phototherapy (treatment of hyperbilirubinemia)
Nursing Assessments of Hyperbilirubinemia n n n Yellowish tint to skin, sclera and mucus membranes Press infant’s skin lightly and release and notice yellowish tint Note time of jaundice (integral in differentiating between physiologic and pathologic jaundice)
Circumcision Care n n n Circumcision- surgical removal of foreskin of penis Newborns with hypospadias and epispadias shouldn’t have circunmcisions Circumcision should not be done immediately because the Vitamin K the infant receives hasn’t kicked in and thermoregulation is not stabilized (cold stress can occur)
Circumcision Care n n Surgical methods include Yellen, Mogen, Gomco clamps and Plastibell Anesthesia is now mandatory for all circumcisions (ring block, dorsal penile nerve block and topical anesthetic) Circumcision site is covered with sterile petroleum With plastibell the foreskin drops off after 5 to 8 days
Circumcision Care n n n Postprocedure- bleeding assess every 15 minutes for the first hour then every hour for 24 hours. First voiding Check for bleeding Apply diapers loosely to prevent irritation Teach parents to keep area clean and check diaper every 4 hours
Circumcision Care n n n Notify provider if there is any redness, discharge, swelling, strong odor, tenderness, decrease in urination, or excessive crying from infant A film of yellowish mucus may form over the glans by day 2 and it is normal- don’t have to wash off Avoid premoistened towlettes to clean penis because they contain alcahol
Circumcision Care (Continued) n n n Circumcision will heal in a couple of weeks Monitor for hemorrhage, coldstress/hypoglycemia, complications (infection, urethral fistula, delayed healing and scarring, fibrous bands Provide discharge instructions to parents about signs and symptoms to observe for and how to report them to provider
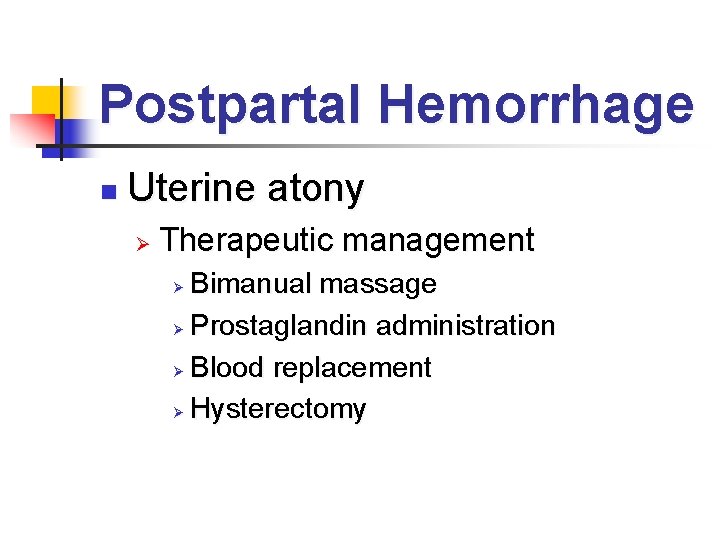
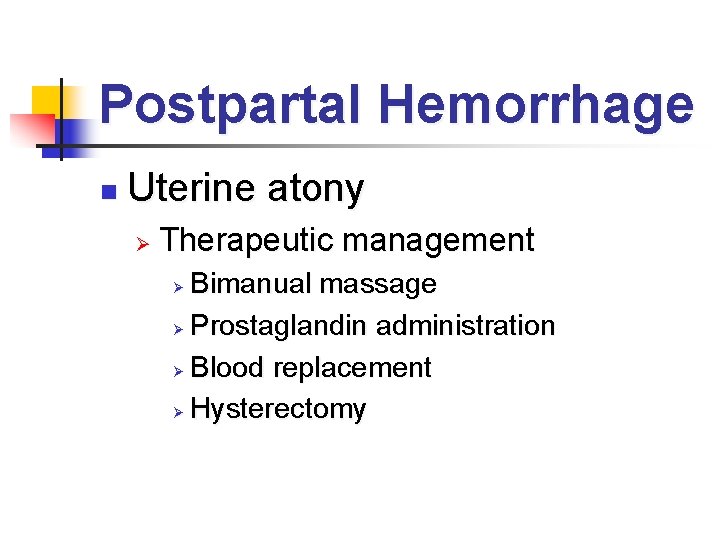
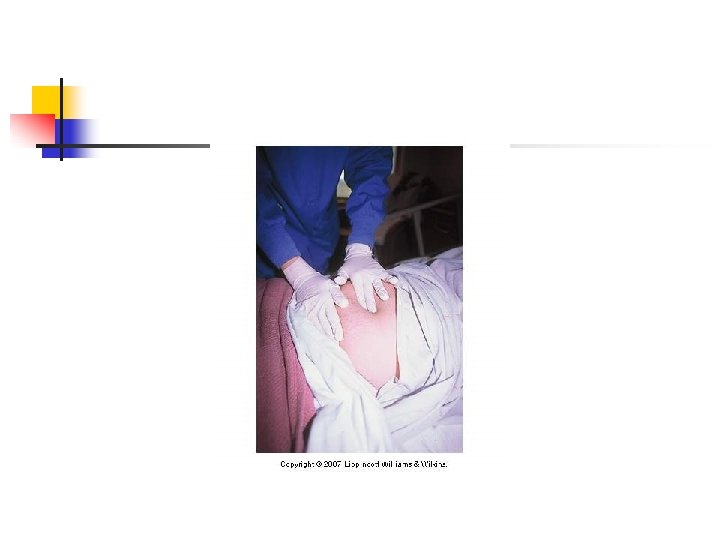
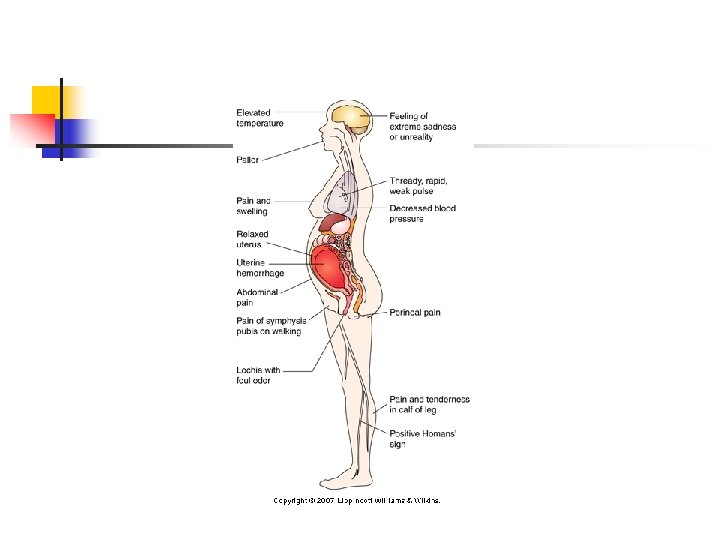
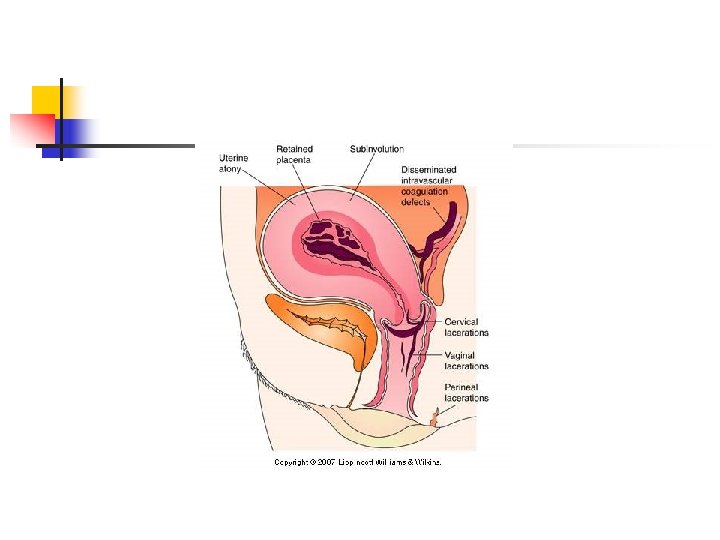
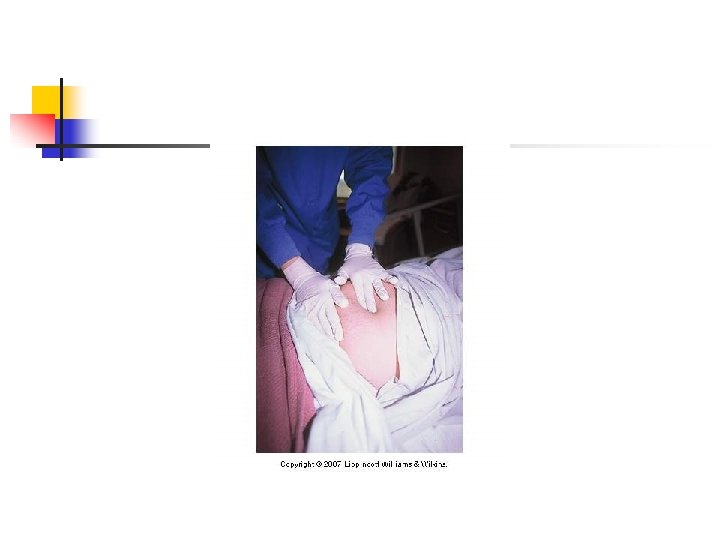
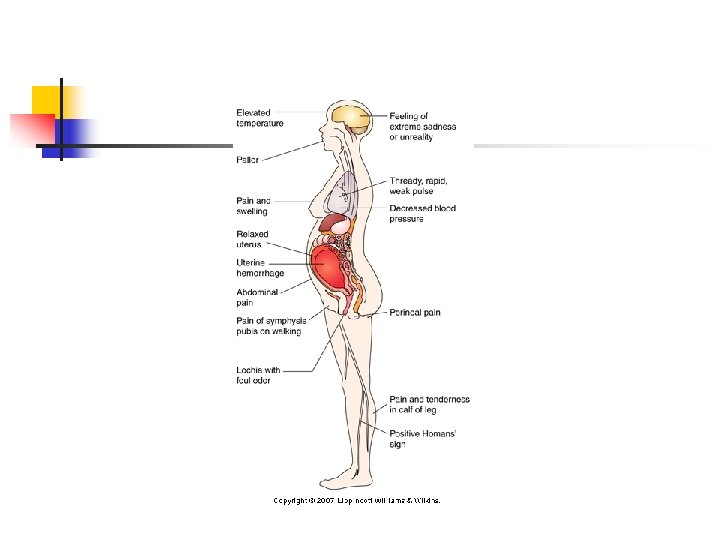
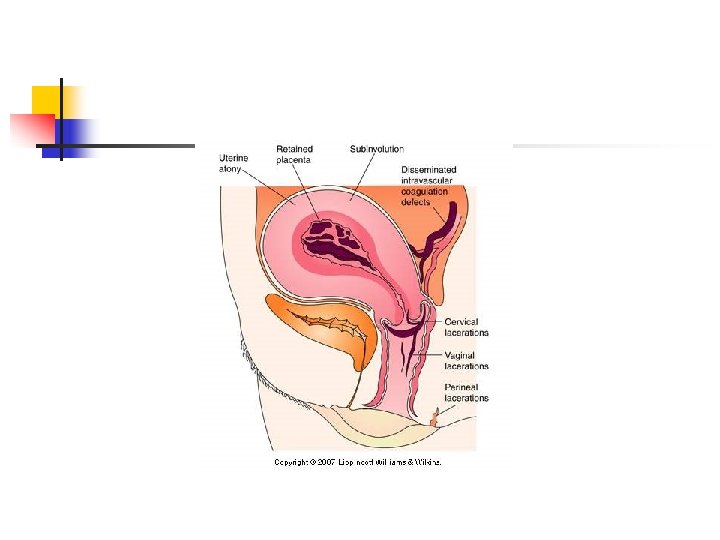
Postpartal Hemorrhage n Uterine atony Ø Therapeutic management Bimanual massage Ø Prostaglandin administration Ø Blood replacement Ø Hysterectomy Ø
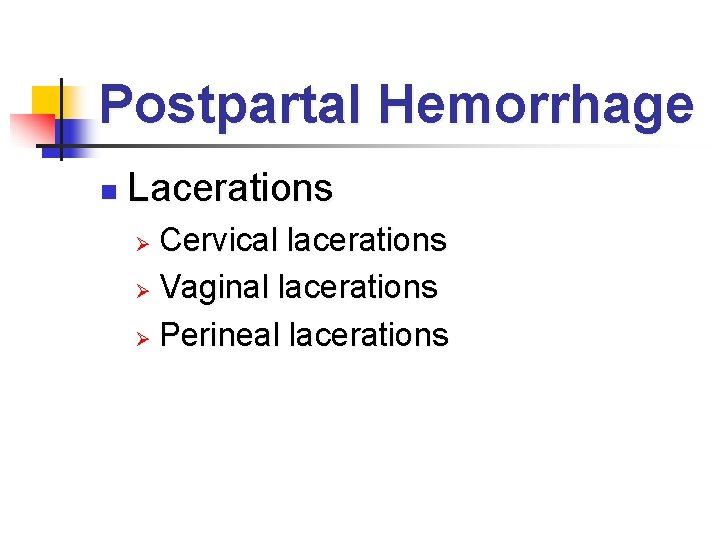
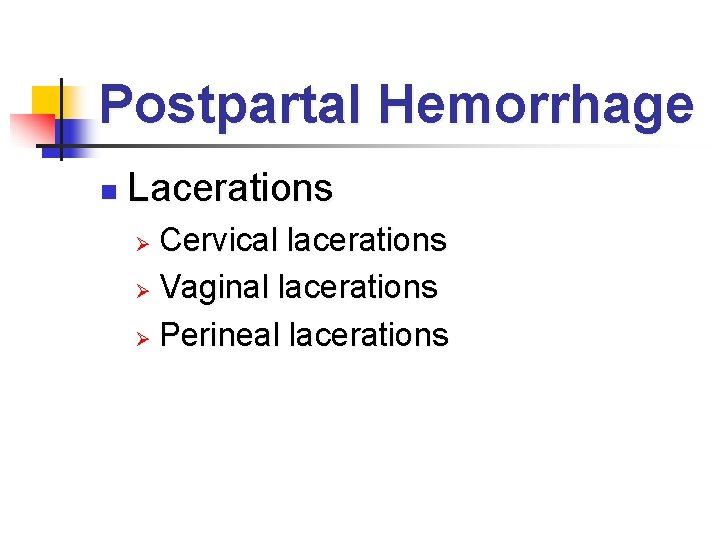
Postpartal Hemorrhage n Lacerations Cervical lacerations Ø Vaginal lacerations Ø Perineal lacerations Ø
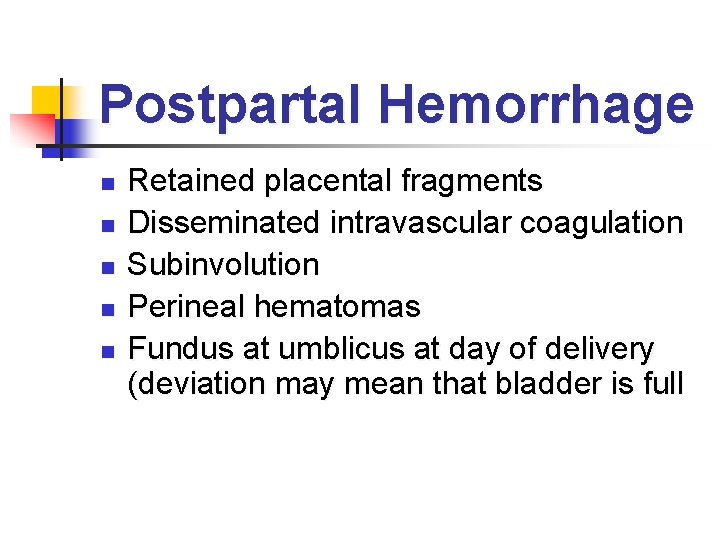
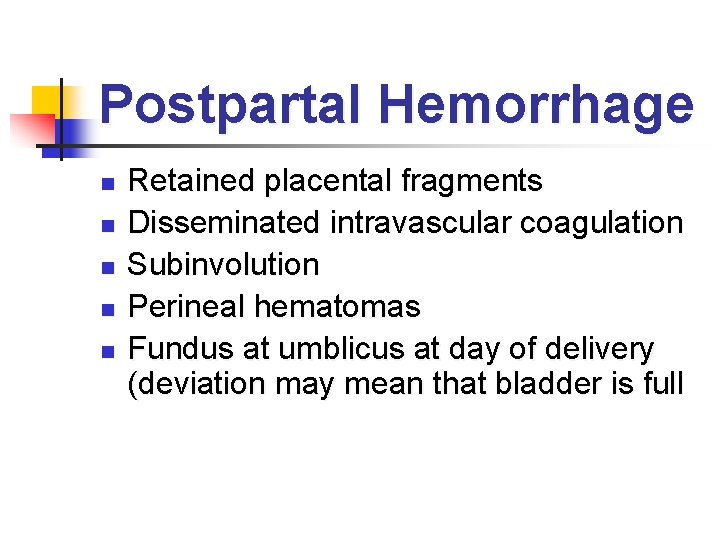
Postpartal Hemorrhage n n n Retained placental fragments Disseminated intravascular coagulation Subinvolution Perineal hematomas Fundus at umblicus at day of delivery (deviation may mean that bladder is full
Nursing Care: First 24 Hours Postpartum Assess peripheral circulation n Prevent/alleviate breast engorgement n Breast hygiene n Promote uterine involution n
Nursing Care: First 24 Hours Postpartum Perineal care n Perineal self-care n Rest n Adequate fluid intake n Prevent constipation n Prevent development of hemorrhoids n
Breastfeeding Problems n Mastitis (Signs and Symptoms) n n n Milk stasis from a blocked duct Nipple Trauma and cracked or fissured nipples Poor breastfeeding technique with improper latching of the infant onto the breast- sore and cracked nipples Decrease in Breastfeeding frequency due to supplementation with bottle feeding Poor Hygiene
Nursing Interventions for Mastitis n n n n Breast Hygiene (handwashing, frequent changes of breast pads, air-dry nipples) Client education Icepacks or warm packs for discomfort Continue breastfeeding every 2 -4 hours (especially on affected side) Encourage rest, analgesics and a fluid intake of at least 3000 ml per day Well-fitting bra Report redness and fever
Episiotomy Care n n Anesthetic spray, cortisone-based cream, sitz bath, witch hazel pads (decreases inflammation and relieve tension in the area) Perineal exercises (Kegel exercises)- start and stop voiding in midstream Ice packs for first 24 hours- reduceds perineal edema and hematoma formation After 24 hours dry heat (hot packs or moist heat with sitz bath & heating lamps)
Episiotomy Care (Continued) n n Nursing Diagnosis: Risk for infection related to lochia and episiotomy Good perineal care (handwashing, changing pads, washing front to back)
Psychological Changes n Development of parental love and positive family relationships Rooming-in Ø Sibling visitation Ø
Emotional and Psychological Complications Child born with illness or is physically challenged n Child who has died n Postpartal depression n Postpartal psychosis n

Postpartal Hemorrhage n Lacerations Cervical lacerations Ø Vaginal lacerations Ø Perineal lacerations Ø
Reproductive System Disorders Reproductive tract displacement n Separation of symphysis pubis n
Postpartal Hemorrhage Retained placental fragments n Disseminated intravascular coagulation n Subinvolution n Perineal hematomas n
Pulmonary Embolus n Obstruction of the pulmonary artery with a blood clot Usually a complication of thrombophlebitis Ø Therapeutic management Ø

Mastitis n Infection of the breast Prevention Ø Assessment Ø Therapeutic management Ø
 Alfredo ramos martinez
Alfredo ramos martinez Ramos da contabilidade
Ramos da contabilidade Tipos de acalculia
Tipos de acalculia Cuales son las venas para canalizar
Cuales son las venas para canalizar Ramos da contabilidade
Ramos da contabilidade Ramos pgs
Ramos pgs Lectio divina domingo de ramos
Lectio divina domingo de ramos Fernando ramos dentista
Fernando ramos dentista Margarita alonso ramos
Margarita alonso ramos Ramos subendocárdicos
Ramos subendocárdicos Ramos ages
Ramos ages Ramos da física
Ramos da física Historia do domingo de ramos
Historia do domingo de ramos Carlos higueras ramos
Carlos higueras ramos Ramo anterior
Ramo anterior Andrea ramos desnuda
Andrea ramos desnuda Ruiz ramos eliana
Ruiz ramos eliana Ramos
Ramos Thalia ramos
Thalia ramos Hoje é domingo de ramos?
Hoje é domingo de ramos? Rolando roberto brizuela ramos
Rolando roberto brizuela ramos Ramos de economia
Ramos de economia Toma de ramos utalca
Toma de ramos utalca Virginia pascual ramos
Virginia pascual ramos Objetivo del domingo de ramos
Objetivo del domingo de ramos Ramos
Ramos Murilo ramos rate my professor
Murilo ramos rate my professor Introduccion domingo de ramos
Introduccion domingo de ramos Nathalia ramos speaking spanish
Nathalia ramos speaking spanish Jorge ramos fun facts
Jorge ramos fun facts Preguntas domingo de ramos
Preguntas domingo de ramos Estruturalismo
Estruturalismo Ang himig ay mabilis na tinawatag na allegro.
Ang himig ay mabilis na tinawatag na allegro. Garcilaso de la vega esquema
Garcilaso de la vega esquema Morreu pedro ramos
Morreu pedro ramos Uml
Uml Hosanna al hijo de david domingo de ramos
Hosanna al hijo de david domingo de ramos Dr ernesto ramos martinez
Dr ernesto ramos martinez Sara del amo ramos
Sara del amo ramos Ubs vila ramos
Ubs vila ramos Imágenes de domingo de ramos
Imágenes de domingo de ramos Luiz felipe ramos
Luiz felipe ramos Crnea
Crnea Domingo de ramos ciclo c
Domingo de ramos ciclo c Luciana ramos lira
Luciana ramos lira Ramos da contabilidade
Ramos da contabilidade Dra denise hematologista
Dra denise hematologista Shane ramos
Shane ramos When mr ramos died 1/3
When mr ramos died 1/3 Secondary sex characteristics
Secondary sex characteristics Talambuhay ni socorro ramos
Talambuhay ni socorro ramos Pedro nogueira ramos
Pedro nogueira ramos Marin county probation department
Marin county probation department Marin gross
Marin gross Marin somborac
Marin somborac Marin svalina
Marin svalina Gregorio castillo marin
Gregorio castillo marin Marin farac
Marin farac Scoala gimnaziala marin preda pitesti
Scoala gimnaziala marin preda pitesti Marin herenda
Marin herenda Toata vara greierele a cantat cu fluierasul poezie
Toata vara greierele a cantat cu fluierasul poezie Ies diego marín aguilera
Ies diego marín aguilera Pablo molina marin
Pablo molina marin Marin tennis club
Marin tennis club Apa vie apa moarta marin sorescu
Apa vie apa moarta marin sorescu Esquema del genero narrativo
Esquema del genero narrativo Radovan marin
Radovan marin Mojca marin
Mojca marin Sonoma marin vector control
Sonoma marin vector control Prof. dr. astrid wallrabenstein
Prof. dr. astrid wallrabenstein Vistamar tuition
Vistamar tuition Dapaflifozina
Dapaflifozina Marin emergency radio authority
Marin emergency radio authority Kiara marin
Kiara marin San marin stem
San marin stem Jasenko marin
Jasenko marin Konstituert overlege
Konstituert overlege Ii gimnazija split
Ii gimnazija split Monolog marin sorescu
Monolog marin sorescu Serily
Serily Liceul de arta marin sorescu craiova
Liceul de arta marin sorescu craiova Marin kaluža
Marin kaluža Marin county ems
Marin county ems Marin litter
Marin litter Darinka gazibara
Darinka gazibara Marin držić biografija
Marin držić biografija Macarena garcia marin
Macarena garcia marin Marin
Marin Cercul de marin sorescu
Cercul de marin sorescu Sausalito marin city sanitary district
Sausalito marin city sanitary district Emmanuel marin
Emmanuel marin German eduardo marin cardenas
German eduardo marin cardenas Macarena garcia marin
Macarena garcia marin Gabrijela marin
Gabrijela marin Marin carbon project
Marin carbon project Photo de marin fils de nolwenn leroy
Photo de marin fils de nolwenn leroy Xerox copiers marin
Xerox copiers marin What is inclusion and exclusion criteria
What is inclusion and exclusion criteria Chapter review motion part a vocabulary review answer key
Chapter review motion part a vocabulary review answer key Narrative review vs systematic review
Narrative review vs systematic review Writ of certiorari ap gov example
Writ of certiorari ap gov example Nader amin-salehi
Nader amin-salehi Catherine jondreville
Catherine jondreville Gnosopraxique
Gnosopraxique Catherine weir
Catherine weir Elise gu
Elise gu Catherine armand
Catherine armand Catherine paradeise
Catherine paradeise Fondation john bost organigramme
Fondation john bost organigramme Catherine olivieri
Catherine olivieri St annes catholic high school for girls
St annes catholic high school for girls Catherine adloff
Catherine adloff Catherine wehlburg
Catherine wehlburg Catherine womack md
Catherine womack md Catherine gwynne
Catherine gwynne Catherine thieblemont
Catherine thieblemont Catherine bennett md
Catherine bennett md Catherine deneuve grey's anatomy
Catherine deneuve grey's anatomy Albert camus tujec
Albert camus tujec Catherine wishart
Catherine wishart Sophie cathérine bonaparte
Sophie cathérine bonaparte Catherine trenque
Catherine trenque Claire clairmont
Claire clairmont Catherine bosshart
Catherine bosshart Catherine robertson abc
Catherine robertson abc Catherine anquetil
Catherine anquetil