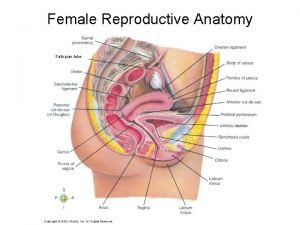
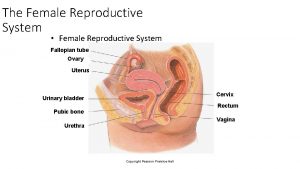
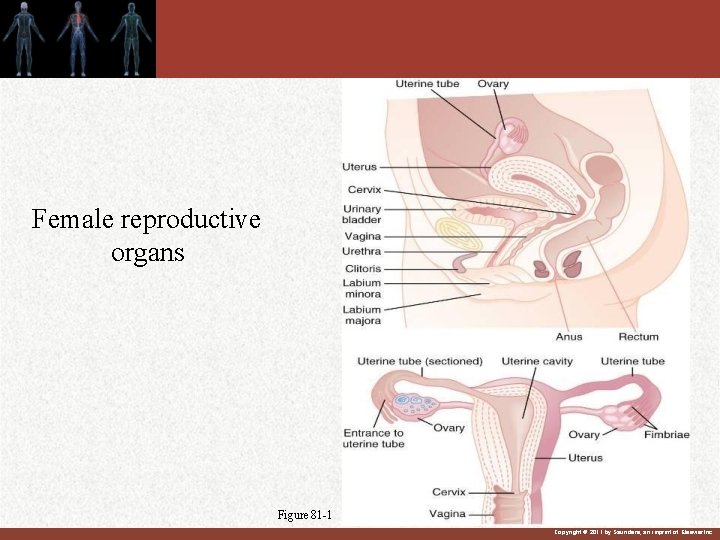
FEMALE REPRODUCTUVE SYSTEM Female reproductive organs Figure 81



















- Slides: 79
FEMALE REPRODUCTUVE SYSTEM
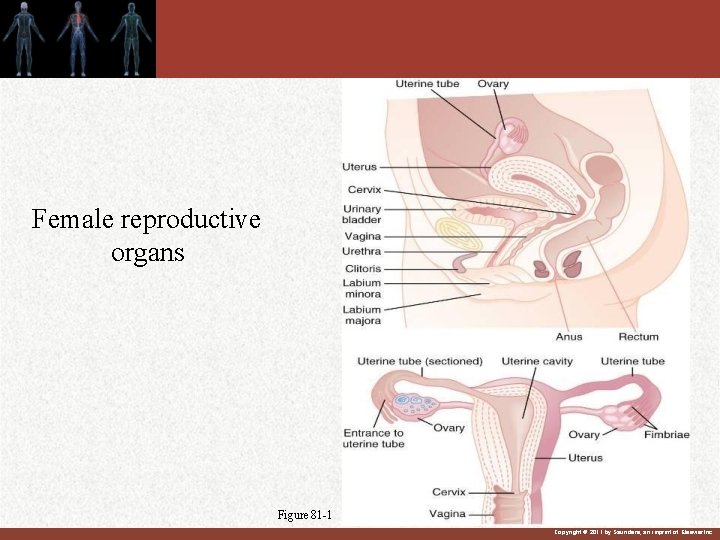
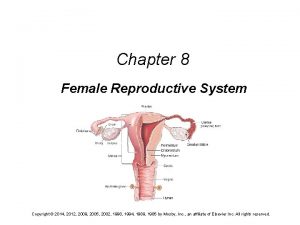
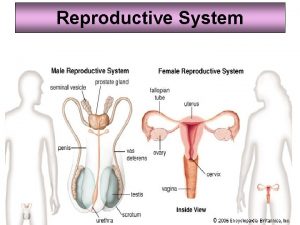
Female reproductive organs Figure 81 -1 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
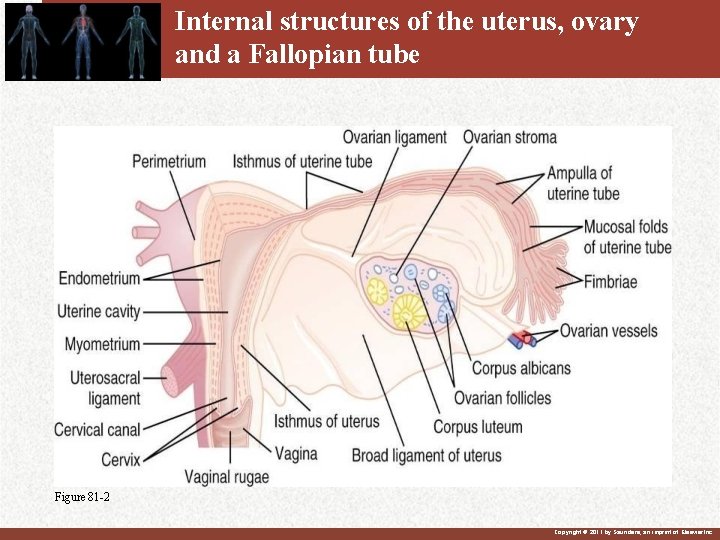
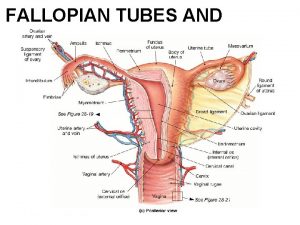
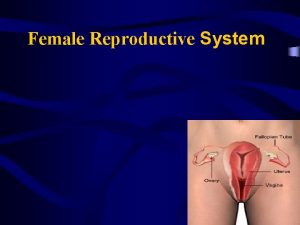
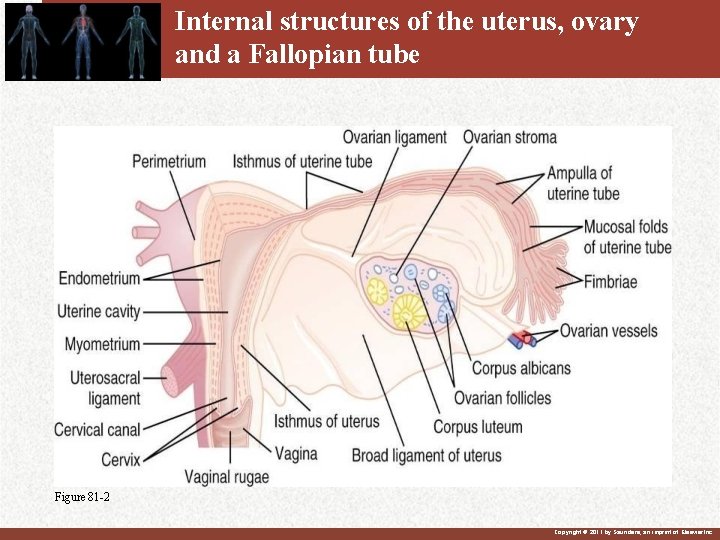
Internal structures of the uterus, ovary and a Fallopian tube Figure 81 -2 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Primordial germ cells become oogonia or primordial ova. Fundamental reproductive unit = single ovarian follicle, composed of one germ cell (oocyte), surrounded by endocrine cells. Oogenesis : A developing egg (Oocyte) becomes Mature egg (Ovum) through series of steps. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
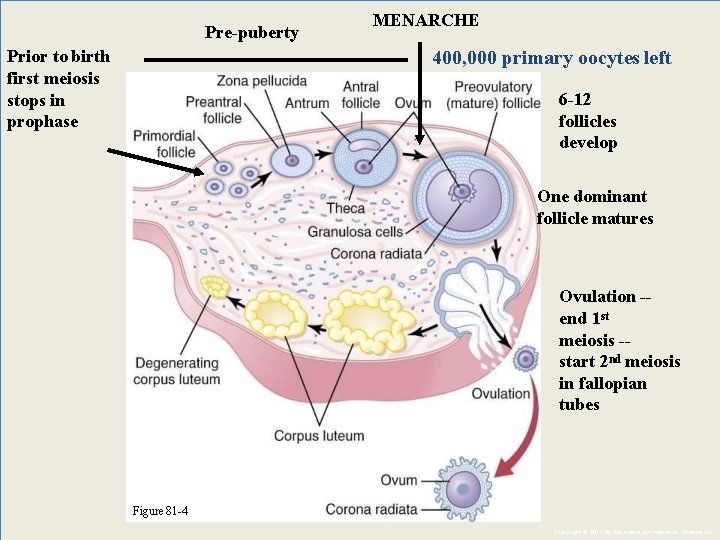
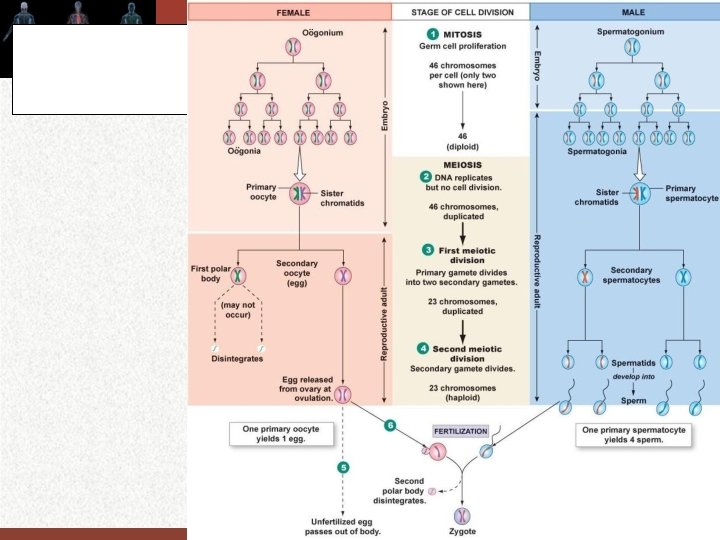
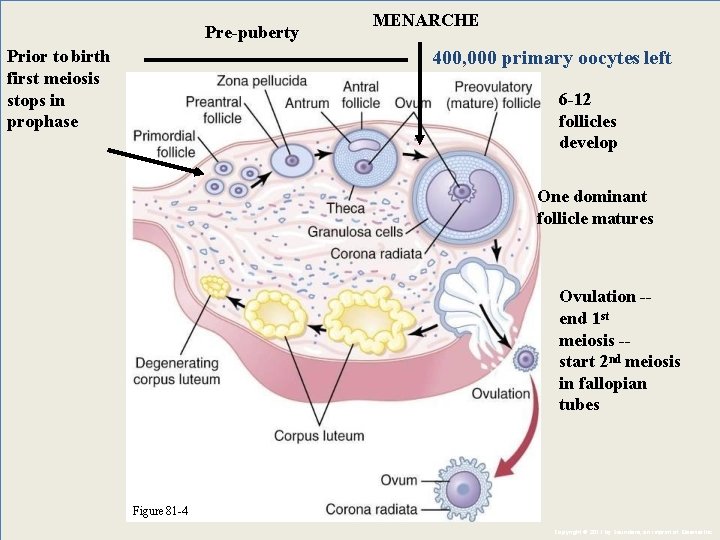
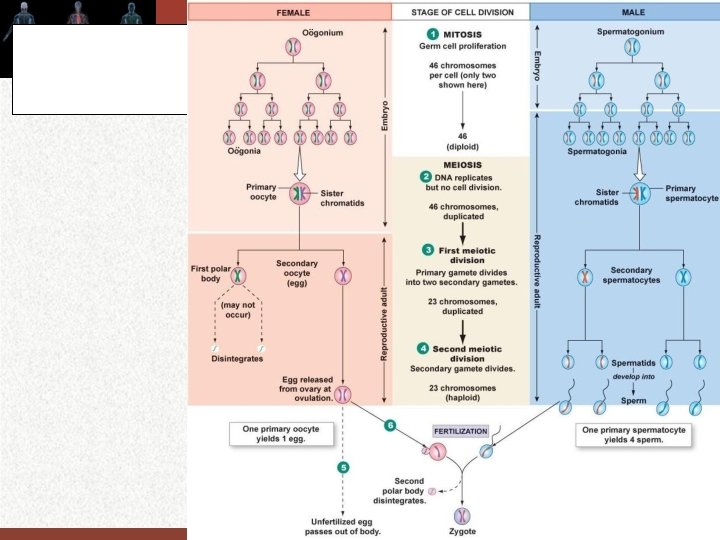
Oogenesis: Oogonia produced by mitotic division (max # = 7 mil), Then during the last part (5 th month) of fetal life , prophase of 1 st meiosis starts but do not complete – becomes primary oocyte (they contain diploid number of chromosomes 46 but do not separate). The primary oocytes stay in this meiotic arrest for years until prepare for ovulation. Number of primary oocytes decreases throughout childhood from 1 -2 mil to 400, 000 just before puberty. Before birth each oocyte surrounded by single layer of granulosa cells -- called primordial follicle -- complete about 6 mos after birth Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
OOGENESIS The undefferentiated primordial germ cells in the fetal ovaries , the Oogonia divided mitotically to give rise to 6 -7 million Oogonia by th the 5 month of gestation when the mitotic proliferation ceases
OOGENESIS During the last part of fetal life, the oogonia begin the early steps of the first meiotic division but do not complete it and now called primary oocytes contain 46 chromosomes and remain in this state of meiotic arrest until prepare for ovulation

Before birth each primary oocyte is surrounded by single layer of connective tissue derived granulosa cells now called primary follicle. Oocytes that are not incorporate into follicles self destructed by apoptosis (cell suicide) At birth only about 2 million primary follicles remain each contain single primary oocyte capable to produce a single ovum. No new oocytes or follicles appear after birth

Even before puberty primary follicles start to develop and it is either : A- Will reach maturity and ovulate OR B- Will degenerate by atresia Most of the follicles undergo atresia and until puberty only 300, 000 remain and only 400 will mature and relieve ova

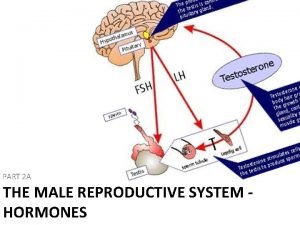
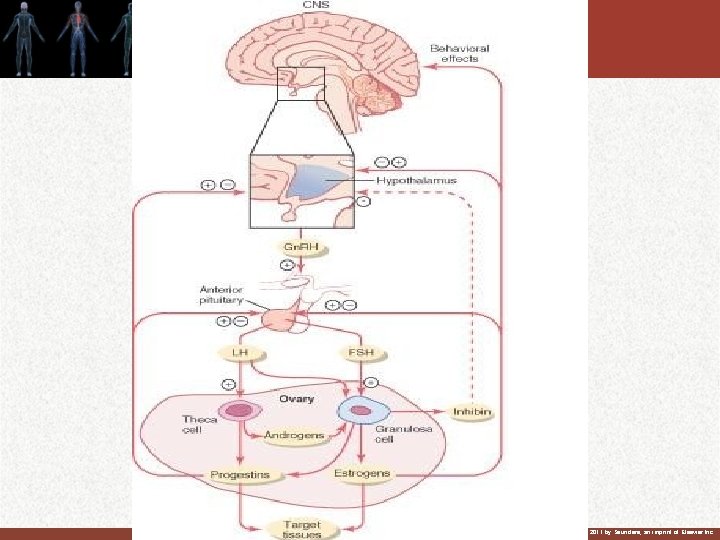
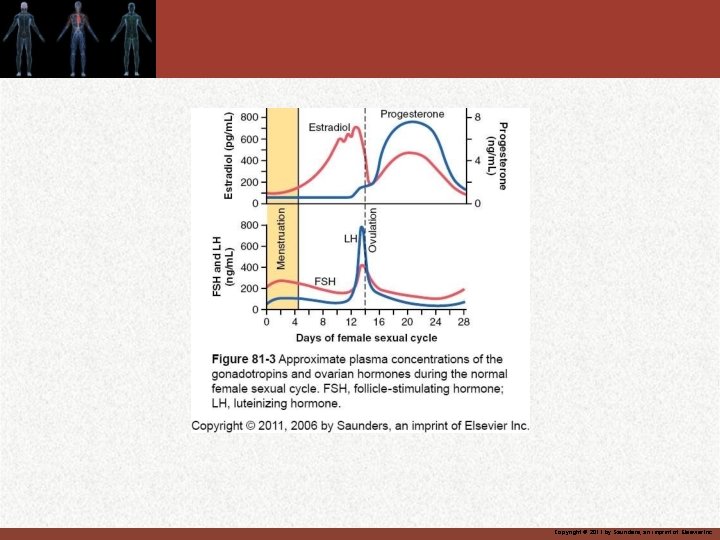
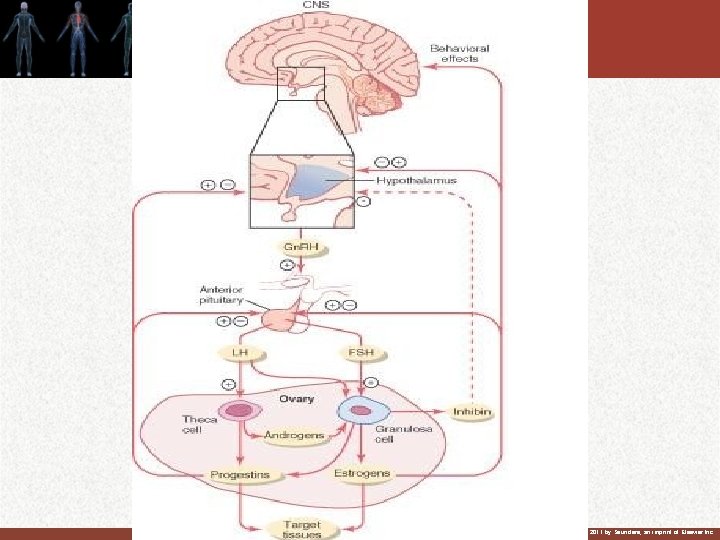
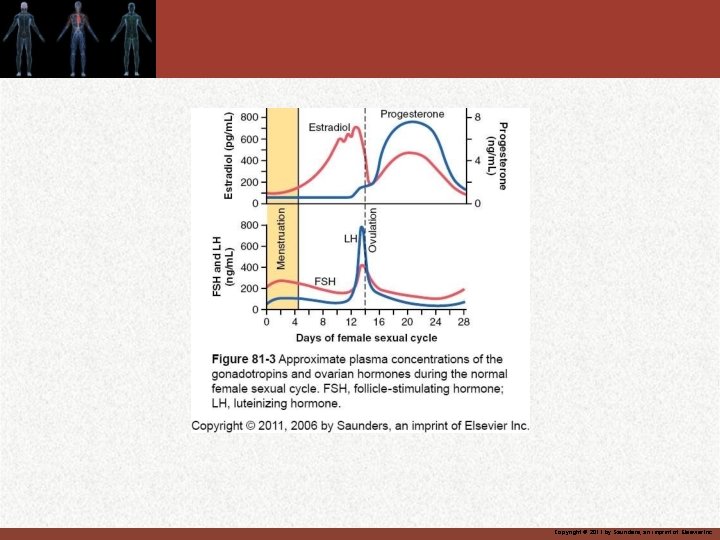
Female hormonal system 1. Hypothalamic releasing hormone, gonadotropin releasing hormone Gn. RH 2. Anterior pituitary sex hormones , FST and LH 3. Ovarian hormones , estrogen and progesterone secreted in response to pituitary hormones 4. These hormones secreted at different rate during different parts of the female monthly sexual cycle.
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.




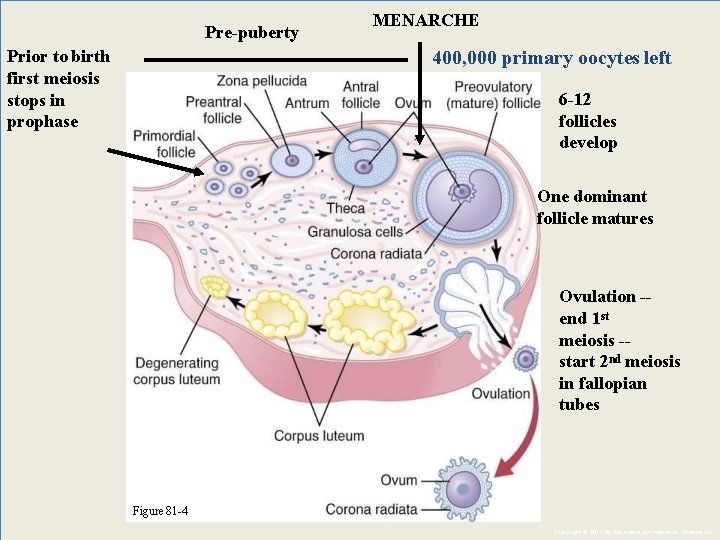
Pre-puberty Prior to birth first meiosis stops in prophase MENARCHE 400, 000 primary oocytes left 6 -12 follicles develop One dominant follicle matures Ovulation -end 1 st meiosis -start 2 nd meiosis in fallopian tubes Figure 81 -4 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
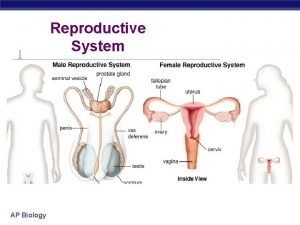
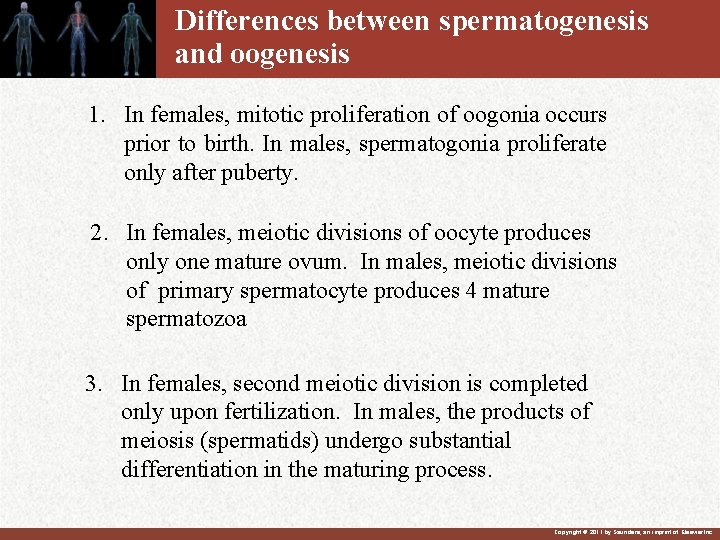
Differences between spermatogenesis and oogenesis 1. In females, mitotic proliferation of oogonia occurs prior to birth. In males, spermatogonia proliferate only after puberty. 2. In females, meiotic divisions of oocyte produces only one mature ovum. In males, meiotic divisions of primary spermatocyte produces 4 mature spermatozoa 3. In females, second meiotic division is completed only upon fertilization. In males, the products of meiosis (spermatids) undergo substantial differentiation in the maturing process. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
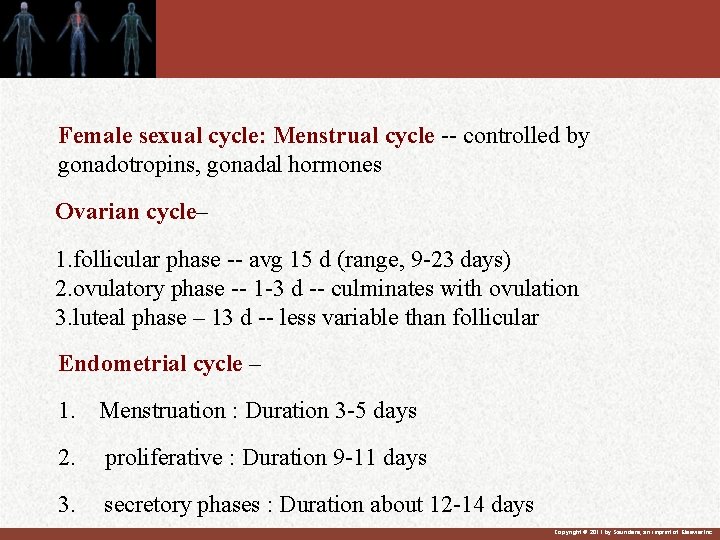
The Basics Gametogenesis
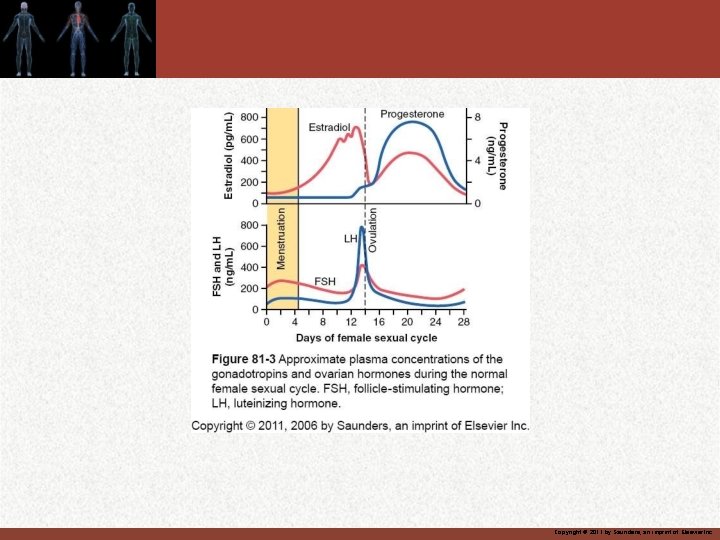
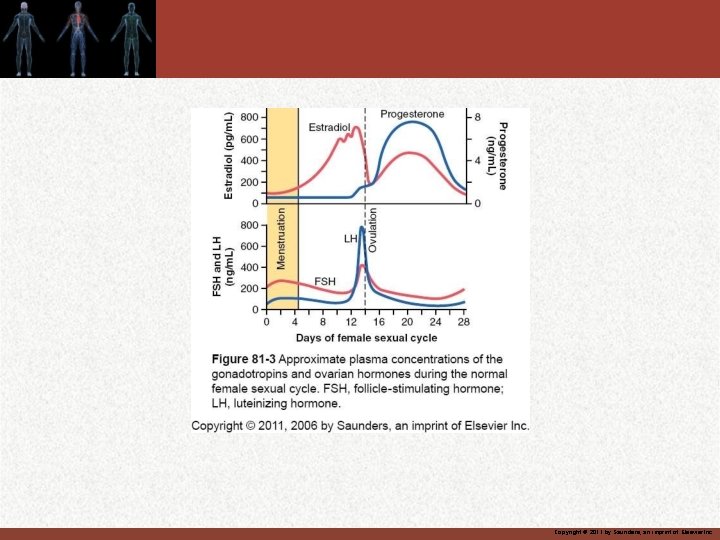
Female sexual cycle: Menstrual cycle -- controlled by gonadotropins, gonadal hormones Ovarian cycle– 1. follicular phase -- avg 15 d (range, 9 -23 days) 2. ovulatory phase -- 1 -3 d -- culminates with ovulation 3. luteal phase – 13 d -- less variable than follicular Endometrial cycle – 1. Menstruation : Duration 3 -5 days 2. proliferative : Duration 9 -11 days 3. secretory phases : Duration about 12 -14 days Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
OVARIAN CYCLE In female child each ovum is surrounded by single granulosa cells sheath called primordial follicle. Granulosa cells provide nourishment to the ovum and secrete oocyte maturation inhibition factor that keep the ovum in suspended in its primordial state. After puberty LH and FSH increase and cause growth of the follicle to becomes primary follicle.
Some spindle cells derived from ovary interstitium Collect in several layers outside granulosa giving rise to mass of cells outside granulosa cells called theca cells. 1 - Theca interna secrete estrogen and progesterone 2 -Theca externa form capsule of the developing follicle
After expulsion of the ovum from the follicle the remaining granulosa and theca interna cells change into lutein cells and growth to form corpus luteum. Now 1 -Granulosa cells form progesterone and estrogen 2 -Theca cells form androgen androstenedion and testosterone which are change by aromatase enzyme in the granulosa cells to estrogen


Introduction: • Ovarian cycle is a series of monthly repetitive physiological and developmental changes in the ovaries, which prepare the ovaries for ovulation and subsequent development of a C. L whose hormones will assist in regulating the uterine cycle and, if the implantation of a developing embryo occurs, assist in regulating the pregnancy. • It is regulated by FSH and LH from the anterior pit. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
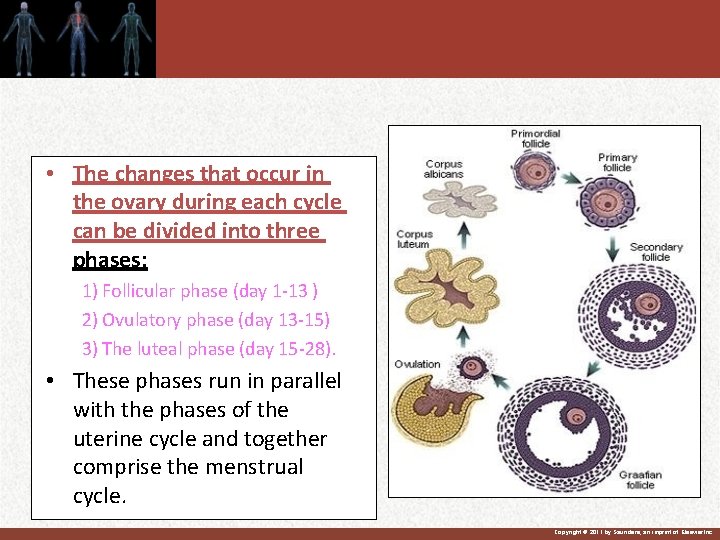
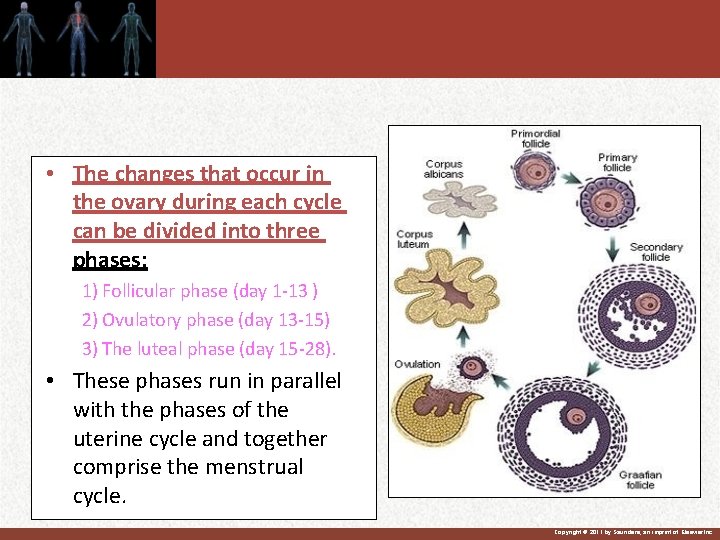
• The changes that occur in the ovary during each cycle can be divided into three phases: 1) Follicular phase (day 1 -13 ) 2) Ovulatory phase (day 13 -15) 3) The luteal phase (day 15 -28). • These phases run in parallel with the phases of the uterine cycle and together comprise the menstrual cycle. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
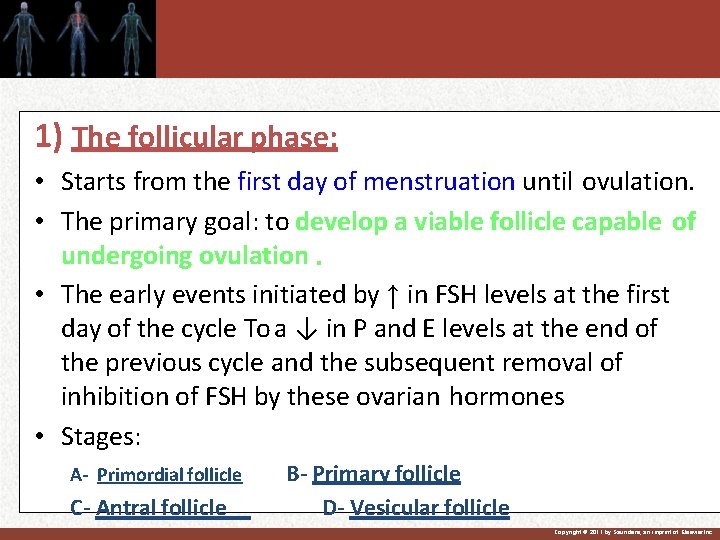
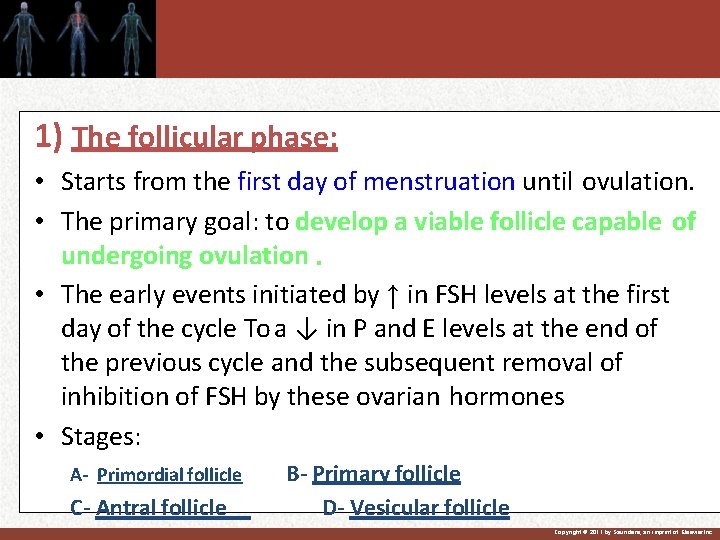
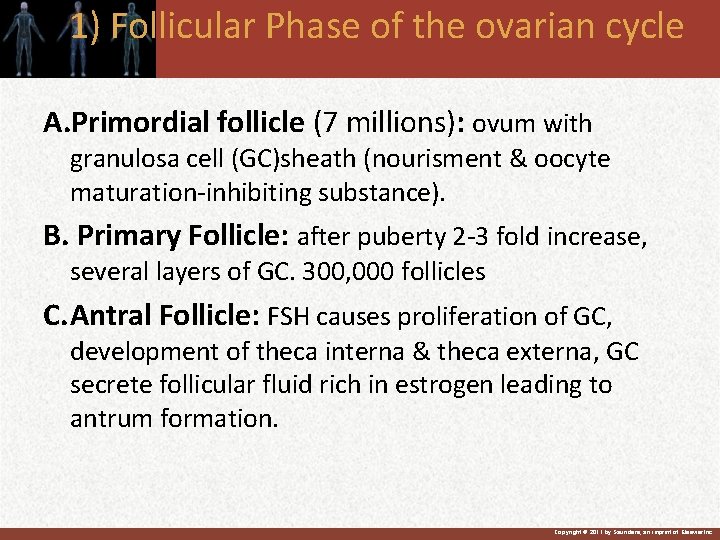
1) The follicular phase: • Starts from the first day of menstruation until ovulation. • The primary goal: to develop a viable follicle capable of undergoing ovulation. • The early events initiated by ↑ in FSH levels at the first day of the cycle To a ↓ in P and E levels at the end of the previous cycle and the subsequent removal of inhibition of FSH by these ovarian hormones • Stages: A- Primordial follicle C- Antral follicle B- Primary follicle D- Vesicular follicle Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
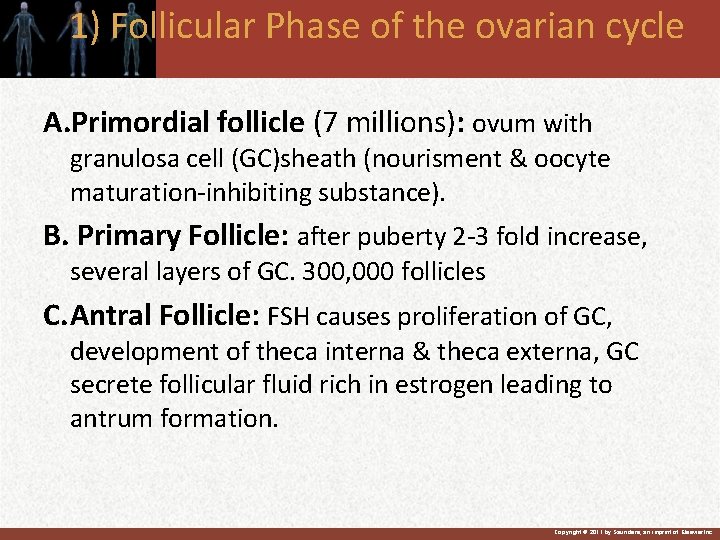
1) Follicular Phase of the ovarian cycle A. Primordial follicle (7 millions): ovum with granulosa cell (GC)sheath (nourisment & oocyte maturation-inhibiting substance). B. Primary Follicle: after puberty 2 -3 fold increase, several layers of GC. 300, 000 follicles C. Antral Follicle: FSH causes proliferation of GC, development of theca interna & theca externa, GC secrete follicular fluid rich in estrogen leading to antrum formation. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
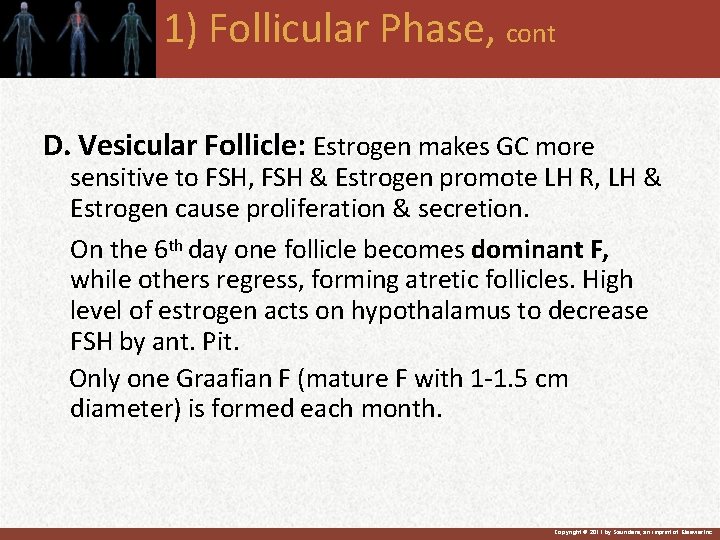
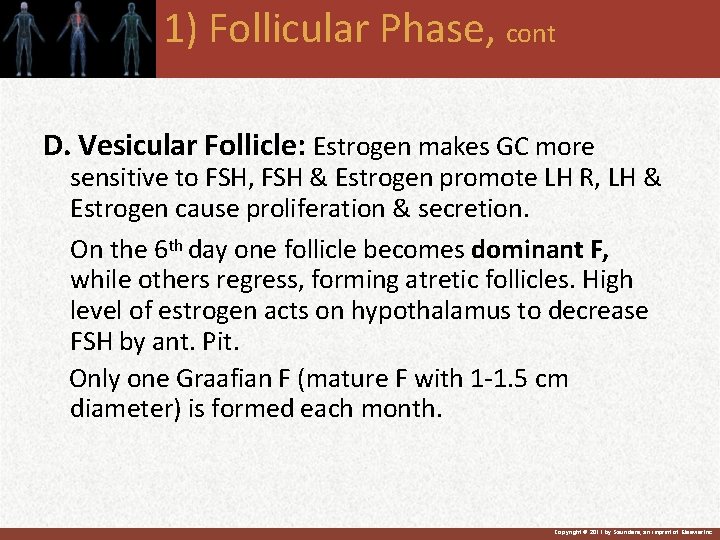
1) Follicular Phase, cont D. Vesicular Follicle: Estrogen makes GC more sensitive to FSH, FSH & Estrogen promote LH R, LH & Estrogen cause proliferation & secretion. On the 6 th day one follicle becomes dominant F, while others regress, forming atretic follicles. High level of estrogen acts on hypothalamus to decrease FSH by ant. Pit. Only one Graafian F (mature F with 1 -1. 5 cm diameter) is formed each month. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
A) Approximately 400 oocytes are ovulated over the course of a lifetime. B) At ovulation: • The follicle ruptures→ releasing the secondary oocyte and corona radiata into the peritoneal cavity to be taken up by the oviduct. • The zona granulosa and thecal cells remain in the ovary. • Discharge of the ovum occur (with part of the cumulus) of the mature Graafian follicle from the surface of ovary at the middle of the cycle (14+2 days before the subsequent menstruation). Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
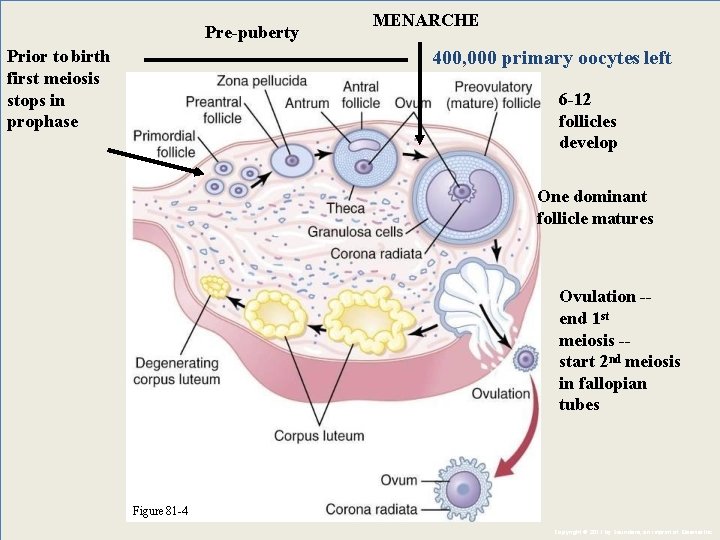
Pre-puberty Prior to birth first meiosis stops in prophase MENARCHE 400, 000 primary oocytes left 6 -12 follicles develop One dominant follicle matures Ovulation -end 1 st meiosis -start 2 nd meiosis in fallopian tubes Figure 81 -4 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.

Corpus luteum (CL): Occur after ovulation, ↓ Morphological changes occur in the remaining part of the follicle within the next 2 -3 days converting it to CL. Formed from: – The zona granulosa →granulosa lutein – Theca cells → theca lutein cells & some capilaries & c. t. } Cells become cuboidal with central nucleus Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Corpus leutum 1 - Granulosa cells secrete mainly progesterone and estrogen 2 - Theca cells form androgen, androstenedione and testosterone and these converted by enzyme aromatase in the granulosa cells into estrogen 3 -Local hormone in the follicular fluid called luteinizationinhibiting factor hold luteinization until after ovulation
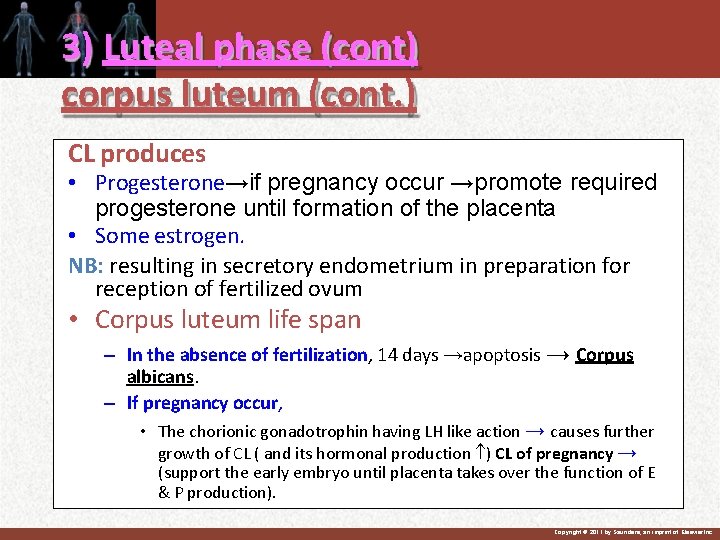
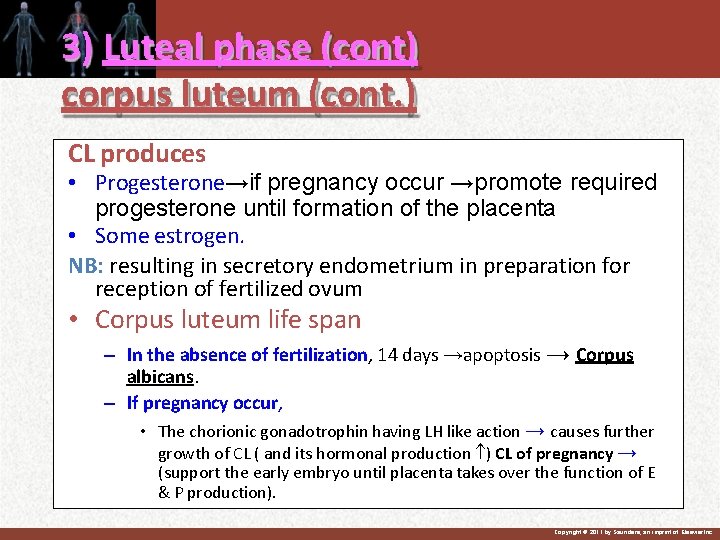
3) Luteal phase (cont) corpus luteum (cont. ) CL produces • Progesterone→if pregnancy occur →promote required progesterone until formation of the placenta • Some estrogen. NB: resulting in secretory endometrium in preparation for reception of fertilized ovum • Corpus luteum life span – In the absence of fertilization, 14 days →apoptosis → Corpus albicans. – If pregnancy occur, • The chorionic gonadotrophin having LH like action → causes further growth of CL ( and its hormonal production ) CL of pregnancy → (support the early embryo until placenta takes over the function of E & P production). Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
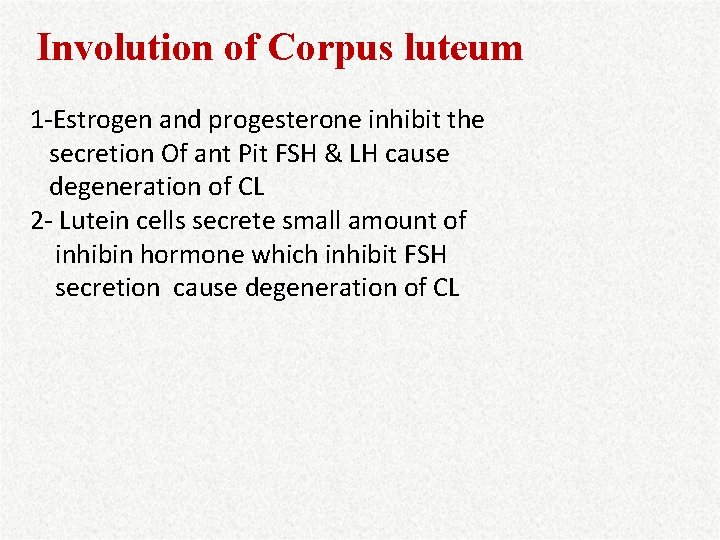
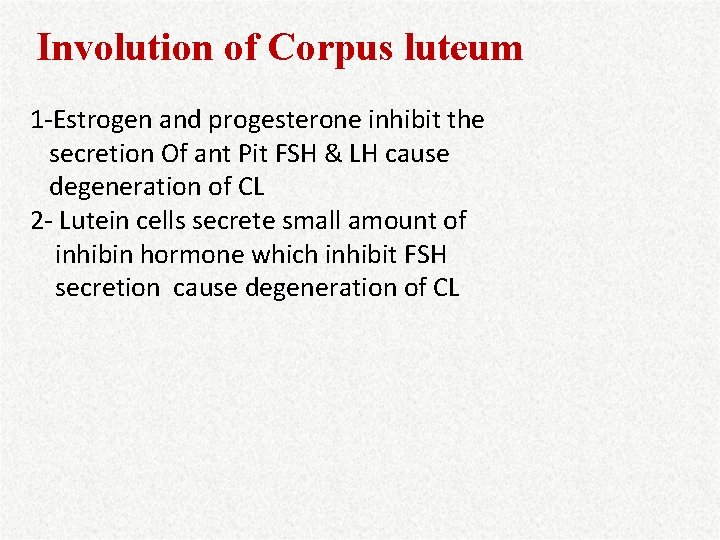
Involution of Corpus luteum 1 -Estrogen and progesterone inhibit the secretion Of ant Pit FSH & LH cause degeneration of CL 2 - Lutein cells secrete small amount of inhibin hormone which inhibit FSH secretion cause degeneration of CL


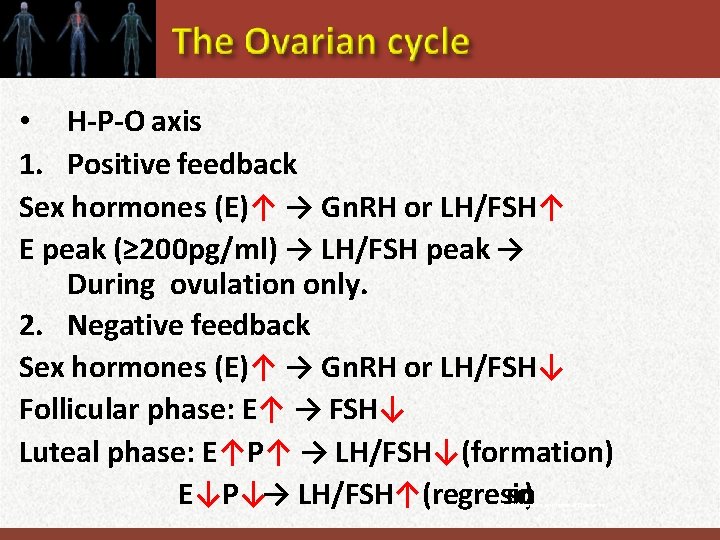
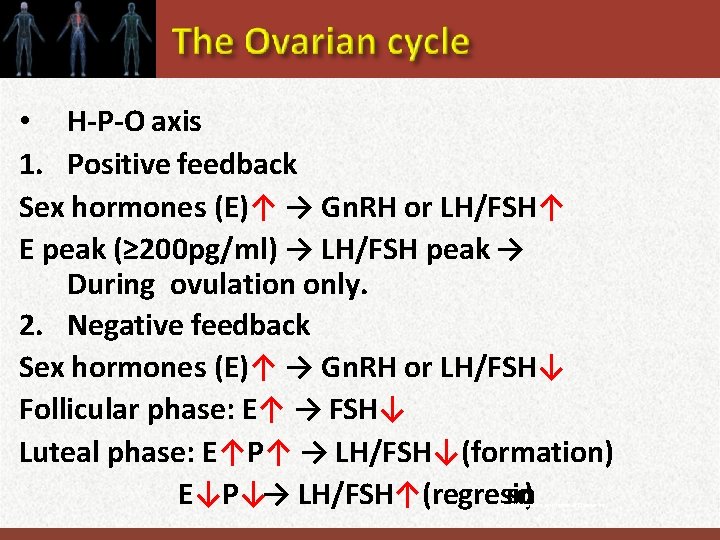
• H-P-O axis 1. Positive feedback Sex hormones (E)↑ → Gn. RH or LH/FSH↑ E peak (≥ 200 pg/ml) → LH/FSH peak → During ovulation only. 2. Negative feedback Sex hormones (E)↑ → Gn. RH or LH/FSH↓ Follicular phase: E↑ → FSH↓ Luteal phase: E↑P↑ → LH/FSH↓(formation) E↓P↓→ LH/FSH↑(regression) C pyrig o© 1 htby 1 Sa unders, an imprint of Elsevier Inc.
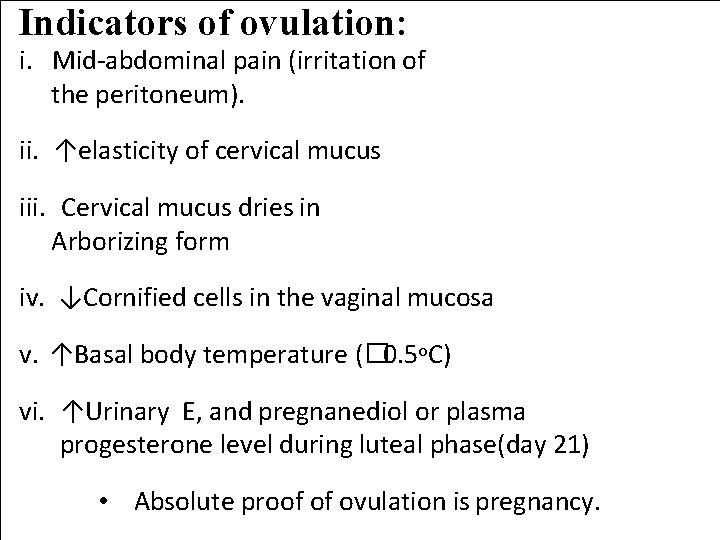
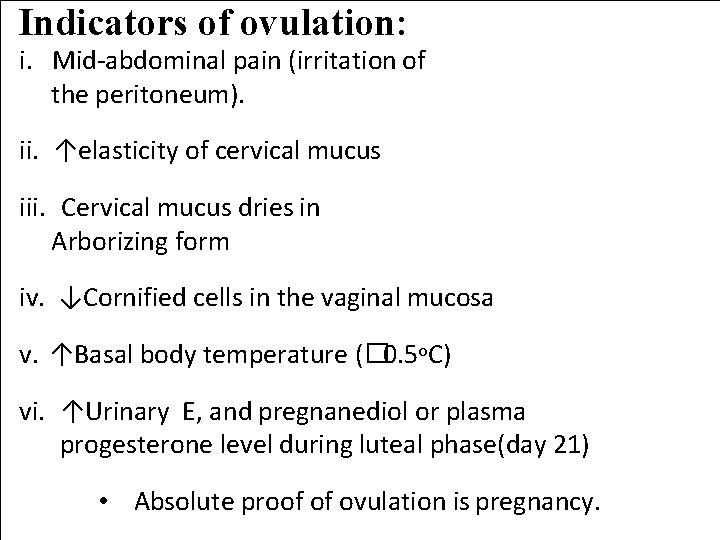
Indicators of ovulation: i. Mid-abdominal pain (irritation of the peritoneum). ii. ↑elasticity of cervical mucus iii. Cervical mucus dries in Arborizing form iv. ↓Cornified cells in the vaginal mucosa v. ↑Basal body temperature (� 0. 5 o. C) vi. ↑Urinary E, and pregnanediol or plasma progesterone level during luteal phase(day 21) • Absolute proof of ovulation is pregnancy.

C. Luteal phase a. Interval between ovulation and menstrual flow (15 th - 28 th day). b. Duration is κ: 14± 2 d (t½ = corpus luteum). c. Day of ovulation = Length of the menstrual cycle - 14 d d. Predominant Hormone: Progesterone nc.
Corpus luteum • Provides necessary hormones for implantation of blastocyst and maintenance of zygote until placenta can take over 80% granulosa cells, 20% thecal cells If not fertilization, will regress in about 14 d Avascular scar = corpus albicans Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
SUMMAR OF OVARIAN CYCLE 1. Every 28 d Gn. H cause growth of 8 -12 new follicles 2. Only one of them grow and become mature and Ovulates 3. During growth of follicles estrogen mainly secretd 4. After ovulation secretory cell of ovulated follicle develop into Corpus Luteum and secrete large amount of progesterone and estrogen 5. After 2 weeks CL degenrates and estrogen and progesterone decrease menstruation begins. 6. A new ovarian cycle then follow
MONTHLY ENDOMETRIAL CYCLE AND MENSTRUATION 1. Proliferation phase (Estrogen phase) 2. Secretory phase (Progesterone phase) 3. Menstruation.

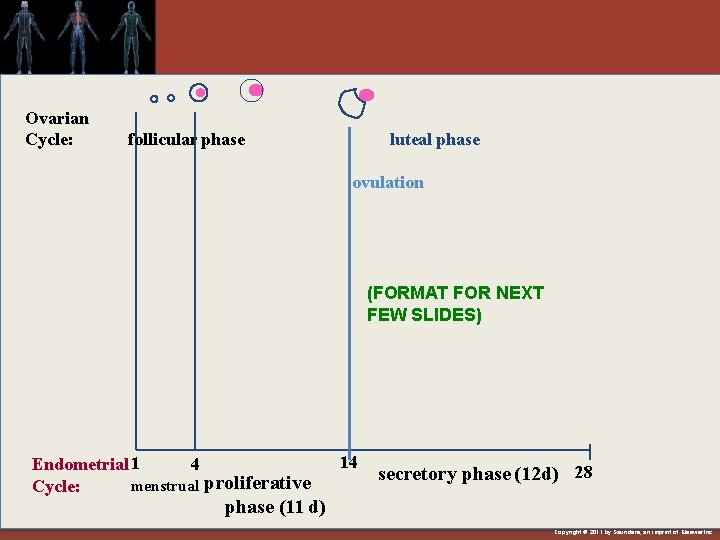
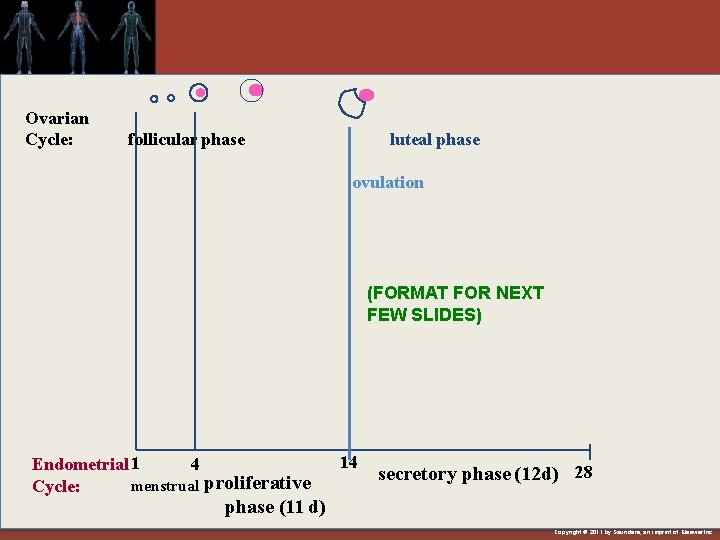
Ovarian Cycle: follicular phase luteal phase ovulation (FORMAT FOR NEXT FEW SLIDES) Endometrial 1 4 menstrual proliferative Cycle: 14 secretory phase (12 d) 28 phase (11 d) Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
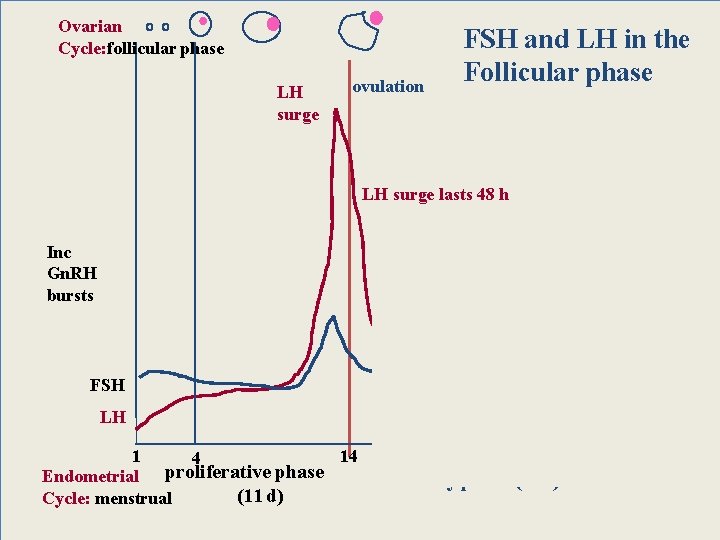
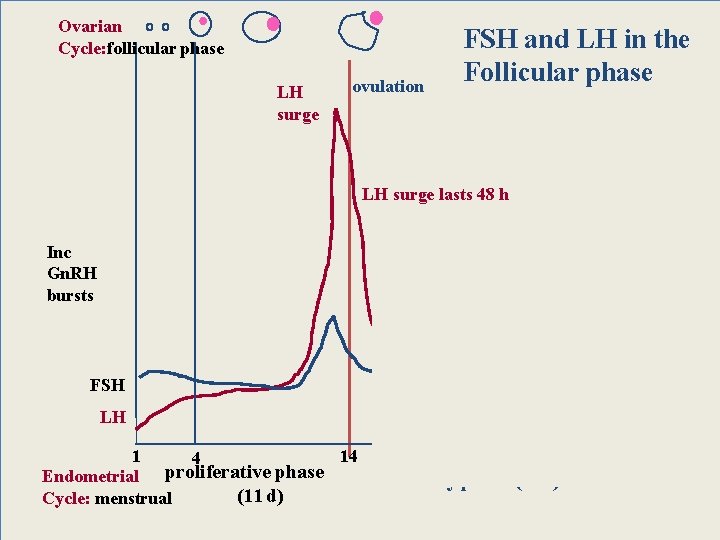
Ovarian Cycle: follicular phase LH surge ovulation FSH and LH in the Follicular phase LH surge lasts 48 h Inc Gn. RH bursts FSH LH 1 14 4 Endometrial proliferative phase (11 d) Cycle: menstrual secretory phase (12 d) 28
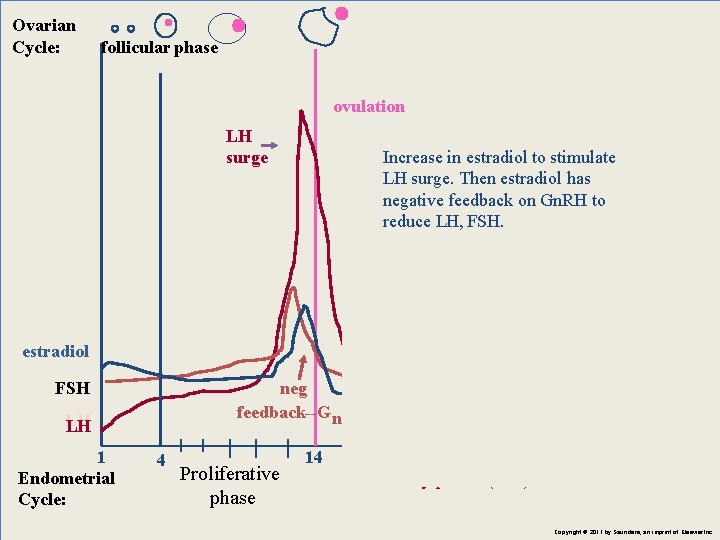
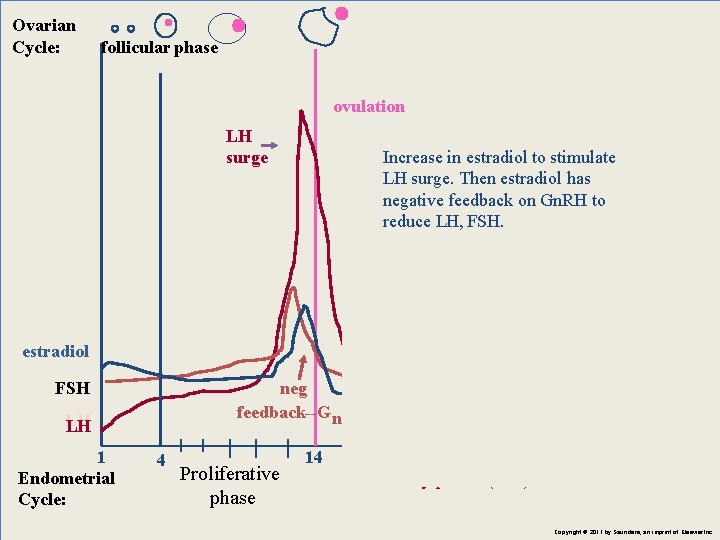
Ovarian Cycle: follicular phase ovulation LH surge Increase in estradiol to stimulate LH surge. Then estradiol has negative feedback on Gn. RH to reduce LH, FSH. estradiol neg feedback--G n. RH FSH L LH H 1 Endometrial Cycle: 4 Proliferative phase 14 Secretory phase (12 d) 28 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
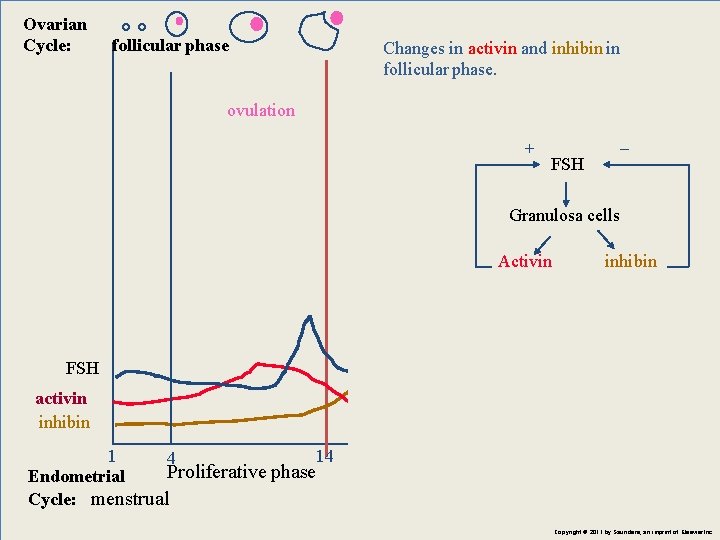
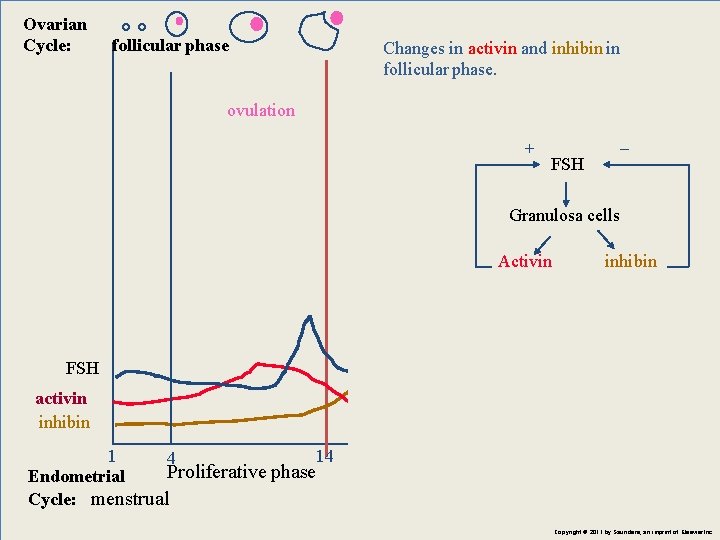
Ovarian Cycle: follicular phase Changes in activin and inhibin in follicular phase. ovulation + _ FSH Granulosa cells Activin inhibin activin FSH activin inhibin 1 14 4 Proliferative phase Endometrial Cycle: menstrual inhibin Secretory phase (12 d)28 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
The uterine cycle and normal menstruation: Because of the monthly cyclic production of estrogens and progesterone, the endometrial lining of the uterus passes into three phases. They are; 1. Proliferative phase 2. Secretory (or luteal phase) 3. menstrual phase. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.

1 -Proliferative phase • About 9 -11 days in duration. • Estrogen secreted by the developing follicle causes proliferation of the epithelial cells left after endometrial desquamation. • Endothelial re-epithelialization occurs within 4 -7 days after the beginning of menstruation (when bleeding ceases). • The next 7 -10 days the endometrial thickness reach to about 3 -5 mm (formation of new endometrial glands and blood vessels). Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
2. The secretory phase (progesterone phase, luteal phase) • Duration about 14 days. • Occurs after ovulation. • Estrogens cause slight cellular proliferation, & progesterone causes marked swelling and further increase in blood supply to the endometrium. • During the secretory phase, the endometrium provides appropriate conditions for implantation of a fertilized ovum. • Within 3 -4 days ovum enter the uterine cavity from fallopian tube and another 4 -5 days for implantation. During this intervals uterine secretions (uterine milk) provide nutrition for the early dividing ovum. • Once the ovum implants, trophoblastic cells of the blastocyst begin to digest the endometrium. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
3. Normal menstruation • If no Fertilization cause involution of corpus luteum. • Duration 3 -5 days (1 -8 days range). Blood loss up to 80 ml (average 30 -40 ml). Bleeding can increase by medications and diseases affect the clotting mechanism. • 24 hours before menstruation blood vessels become vasospastic, presumably because of vasoconstrictor types of prostaglandins. • The vasospasm + ↓ nutrients + ↓ hormonal stimulation endometrial necrosis Hemorrhage + Sloughing of outer layers of the endometrium • Prostaglandins and desquamated tissues initiate uterine contractions that expel the uterine contents. • The menstrual fluid is non-clotting because of released fibrinolysin. Clots presence may indicate uterine pathology. • Menstrual flow is rich in leukocytes. This explain the resistance of uterus to infection during menstruation. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
ABNORMAL BLEEDING 1. Menorrhagia (hypermenorrhea): is heavy or prolonged menstrual flow during regular period. 2. Hypomenorrhea : Slight menstrual flow, obstruction as hymen or cervical obstruction
3. Metrorrhagia (Intermenstrual bleeding): Bleeding at any time betwewn menstrual period. 4. Polymenorrhea : Frequent period 5. Oligomenorrhea : More than 45 days, decrease bleeding in amount , anovulation can be endocrine cause
2011 by Saunders, an imprint of Elsevier Inc.
H-P-O axis 1. Positive feedback Sex hormones (E)↑ → Gn. RH or LH/FSH↑ E peak (≥ 200 pg/ml) → LH/FSH peak → During ovulation only. 2. Negative feedback Sex hormones (E)↑ → Gn. RH or LH/FSH↓ Follicular phase: E↑ → FSH↓ Luteal phase: E↑P↑ → LH/FSH↓(formation) E↓P↓→ LH/FSH↑( regression),

Ovarian Cycle: Corpus albicans + Luteal phase ovulation + _ FSH Granulosa cells Activin inhibin activin FSH inhibin 14 4 1 Proliferative phase Endometrial (11 d) menstrual Cycle: Secretory phase (12 d) 28 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.

Ovarian Cycle: + Corpus albicans Luteal phase Levels of estradiol in luteal phase ovulation + _ FSH Granulosa cells Activin inhibin estradiol FSH 1 Endometrial Cycle: 4 14 proliferative phase secretory phase inhibin 28 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
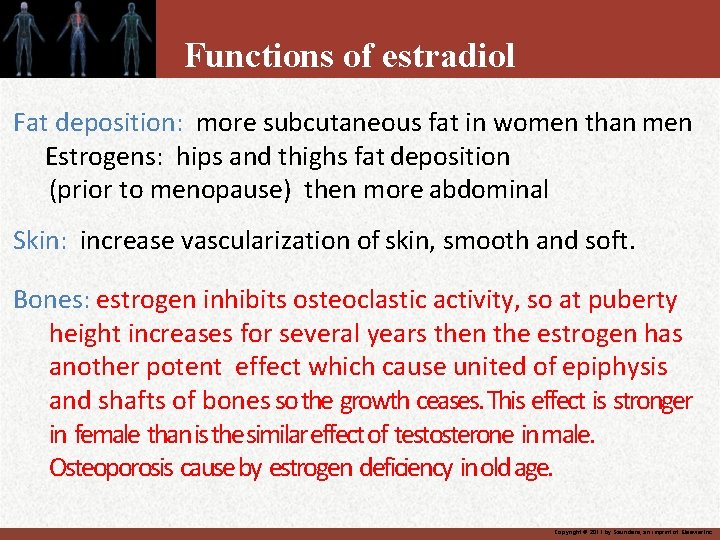
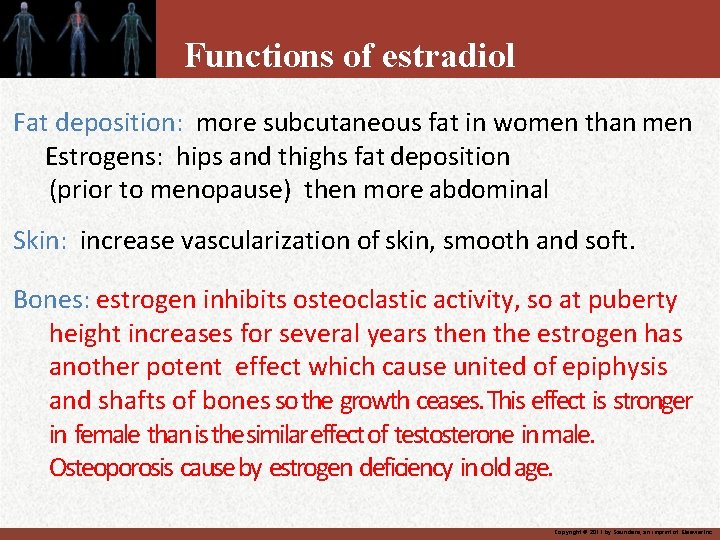
Functions of estradiol Fat deposition: more subcutaneous fat in women than men Estrogens: hips and thighs fat deposition (prior to menopause) then more abdominal Skin: increase vascularization of skin, smooth and soft. Bones: estrogen inhibits osteoclastic activity, so at puberty height increases for several years then the estrogen has another potent effect which cause united of epiphysis and shafts of bones so the growth ceases. This effect is stronger in female than is the similar effect of testosterone in male. Osteoporosis cause by estrogen deficiency in old age. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.

Copyright © 2011 by Saunders, an imprint of Elsevier Inc.

Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
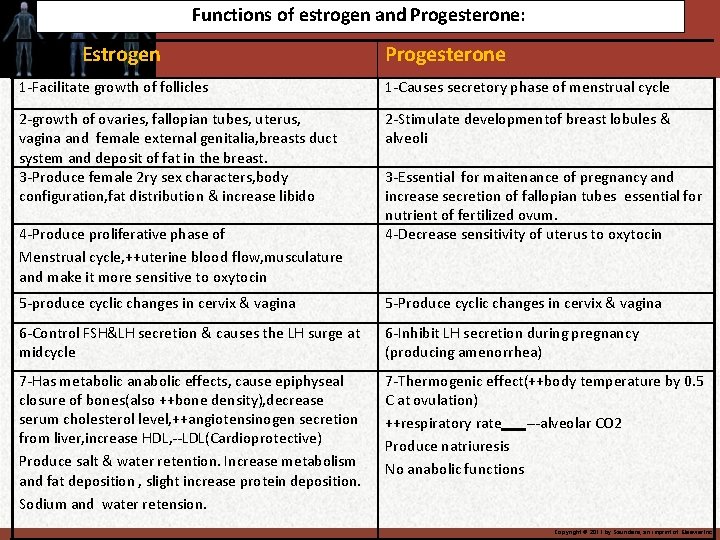
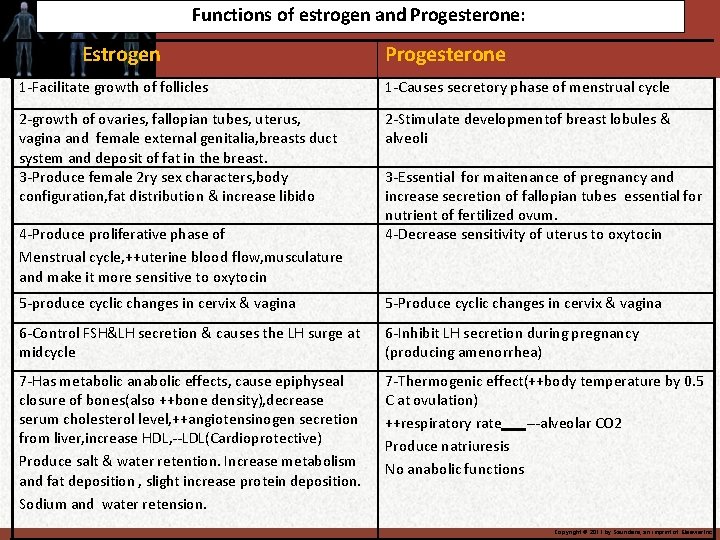
Functions of estrogen and Progesterone: Estrogen Progesterone 1 -Facilitate growth of follicles 1 -Causes secretory phase of menstrual cycle 2 -growth of ovaries, fallopian tubes, uterus, vagina and female external genitalia, breasts duct system and deposit of fat in the breast. 3 -Produce female 2 ry sex characters, body configuration, fat distribution & increase libido 2 -Stimulate developmentof breast lobules & alveoli 4 -Produce proliferative phase of Menstrual cycle, ++uterine blood flow, musculature and make it more sensitive to oxytocin 3 -Essential for maitenance of pregnancy and increase secretion of fallopian tubes essential for nutrient of fertilized ovum. 4 -Decrease sensitivity of uterus to oxytocin 5 -produce cyclic changes in cervix & vagina 5 -Produce cyclic changes in cervix & vagina 6 -Control FSH&LH secretion & causes the LH surge at midcycle 6 -Inhibit LH secretion during pregnancy (producing amenorrhea) 7 -Has metabolic anabolic effects, cause epiphyseal closure of bones(also ++bone density), decrease serum cholesterol level, ++angiotensinogen secretion from liver, increase HDL, --LDL(Cardioprotective) Produce salt & water retention. Increase metabolism and fat deposition , slight increase protein deposition. Sodium and water retension. 7 -Thermogenic effect(++body temperature by 0. 5 C at ovulation) ++respiratory rate ---alveolar CO 2 Produce natriuresis No anabolic functions Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Female sexual act 1 -Stimulation of female sexual act : Thinking lead to sexual desire and this desire change during the cycle reaching the peak near ovulation because of high estrogen. Physical stimulation as in male (perineal region). Same nerve signals. 2 -Female erection and lubrication (clitoris): as the penis control by parasympathetic nerves, same mechanism as in male 3 -Female orgasm (female climax): Analog to emission and ejaculation in male.
Female sexual response -- process is similar in males and females: 1) Excitement phase: caused by psychological or physical stimulation; engorgement and erection of clitoris, vaginal congestion -- due to NO, secreted by parasympathetic nerves 2) Plateau phase: intensification of these responses, increased HR, BP, respiratory rate, muscle tension 3) Orgasmic phase: culmination of sexual excitement, intense physical pleasure 4)Resolution phase: returns genitalia and body systems to pre-arousal state Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Male and female sexual response Differences: Women don’t require refractory time before beginning excitation again No ejaculation in the female Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Female sexual dysfunction May be as high as 45% in women aged 16 -50 yrs mechanisms: psychological illness unknown Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
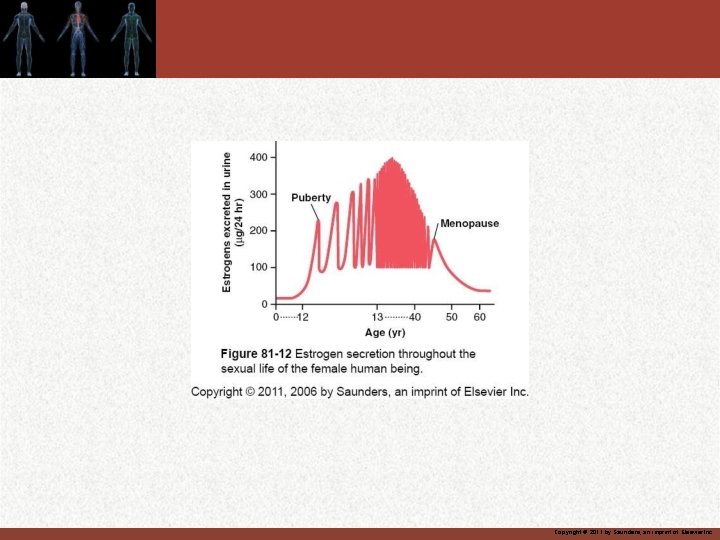
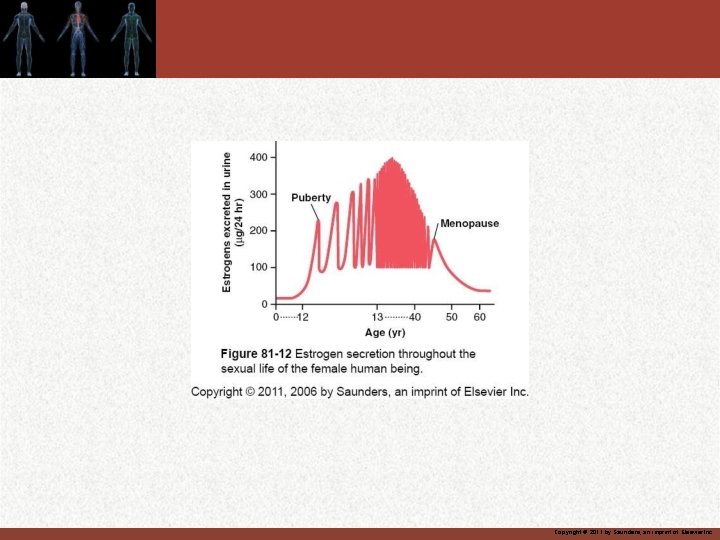
Menopause Defn: obsolescence of ovaries, no estradiol production, ova only occasional secondary follicle, few primary follicles Occurs at 51. 4 yr of age (average) Due to reduction in estrogen, low levels of inhibin, no negative feedback of LH and FSH; therefore, high levels LH and FSH Can occur naturally, due to surgery or as a result of chemotherapy Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Women’s Health Initiative • Increased risk of CHD, stroke, pulm embolis (3 x), breast cancer • “HRT regimen should not be initiated or continued for primary prevention of CHD” JAMA 2002 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Physiological changes in the body during menopause 1 -Hot flushes 2 -Irritability 3 -Anxiety 4 - Fatigue 5 - Psychic dyspnea 6 -Decrease strength of the bones 7 -Vaginal dryness 8 -Gradual atrophy of genital organs Small dose of estrogen reverse these symptoms
Polycystic ovary syndrome Affects 10% of reproductive age women Characteristics: hyperandrogenemia oligomenorrhea obesity hirsutism infertility enlarged cystic ovaries Rx: metformin, anti-androgens? Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Abnormal secretion of the ovaries: 1 -Hypogonadism reduce secretion A- Before puberty cause infantile sexual organs, no secondary sexual character and tall female B- After puberty cause infantile sexual organs include the uterus, small vagina, breast atrophy C-Irregularity of menses and amenorrhea. 2 -hypersecretion rare (granulosa cell tumor) and mainly cause irregular bleeding.
Female fertility: 1 -Fertile period of each cycle (4 -5 days), before ovulation 2 -Rhythm method for contraceptive (75%). 3 - Hormonal suppression of fertility (the pills) : use of estrogen or progesterone in the first half of the cycle prevent ovulation by prevent preovulatory surge of LH secretion by pituitary gland (90%). 4 - Female sterility : A-Failure of ovulation mainly reduce gonadotropin hormone B-Endometriosis , salpingitis,
 Male reproductuve system
Male reproductuve system Mucous membrane reproductive system
Mucous membrane reproductive system Female reproductive organs sagittal section
Female reproductive organs sagittal section Ovarian duct
Ovarian duct Figure 28-2 the female reproductive system
Figure 28-2 the female reproductive system Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Reproductive organs of the bull
Reproductive organs of the bull Genital development
Genital development Female cow reproductive system
Female cow reproductive system Sperm duct
Sperm duct Function of reproductive organs
Function of reproductive organs Function of uterine cavity
Function of uterine cavity Frog testis labeled
Frog testis labeled Female reproductive system with baby
Female reproductive system with baby Female reproductive system external
Female reproductive system external Female reproductive system pregnancy
Female reproductive system pregnancy Male fallopian tube
Male fallopian tube Unit 5 lesson 3 the female reproductive system
Unit 5 lesson 3 the female reproductive system Anatomy of ovary slideshare
Anatomy of ovary slideshare Uterus function
Uterus function Uterus is the part of which system in pila
Uterus is the part of which system in pila Pig reproductive anatomy
Pig reproductive anatomy Chapter 16 the reproductive system
Chapter 16 the reproductive system Female cow reproductive system
Female cow reproductive system Differences between male and female reproductive organ
Differences between male and female reproductive organ Plot
Plot Fsh and lh in female reproductive system
Fsh and lh in female reproductive system Corpus luteum in female reproductive system
Corpus luteum in female reproductive system Lesson 3 the female reproductive system
Lesson 3 the female reproductive system Female reproductive system colour
Female reproductive system colour External genitalia of female
External genitalia of female Chapter 8 female reproductive system
Chapter 8 female reproductive system 90/2
90/2 Conclusion of female reproductive system
Conclusion of female reproductive system Prostatic urethra male
Prostatic urethra male Female reproductive system pathology
Female reproductive system pathology Female reproductive system label
Female reproductive system label Bovine female reproductive system
Bovine female reproductive system Female reproductive system pathology
Female reproductive system pathology Female reproductive system pathology
Female reproductive system pathology Female reproductive system
Female reproductive system Hysterosalpingoophorectomy
Hysterosalpingoophorectomy Uterine seal
Uterine seal Bovine female reproductive system
Bovine female reproductive system Oviduct
Oviduct Female reproductive system pathology
Female reproductive system pathology Female anatomy
Female anatomy Vagina diagram labeled
Vagina diagram labeled Female reproductive
Female reproductive Fertilization
Fertilization Female reproductive system external
Female reproductive system external Anterior view of the female reproductive system
Anterior view of the female reproductive system Female reproductive system
Female reproductive system Female external reproductive system
Female external reproductive system Similarities between male and female reproductive system
Similarities between male and female reproductive system Animal female reproductive system diagram
Animal female reproductive system diagram Chapter 16 lesson 3 the female reproductive system
Chapter 16 lesson 3 the female reproductive system Pea size glands flanking the vagina
Pea size glands flanking the vagina Sperm fructose
Sperm fructose Female reproductive system se-6
Female reproductive system se-6 Where does meiosis occur in plants
Where does meiosis occur in plants Hyogonadism
Hyogonadism Cartilaginous fish reproduction
Cartilaginous fish reproduction Distinguish between ova, ovaries, and ovulation
Distinguish between ova, ovaries, and ovulation Main part of seed
Main part of seed Chapter 16 the reproductive system figure 16-2
Chapter 16 the reproductive system figure 16-2 Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Parturition
Parturition Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Figure 16-2 is a longitudinal section of a testis
Figure 16-2 is a longitudinal section of a testis Left lower quadrant organs
Left lower quadrant organs Primary sex organs of the female *
Primary sex organs of the female * Female organs
Female organs Female organs
Female organs Female organs
Female organs Function of fallopian tube
Function of fallopian tube Inguinal
Inguinal Compylotropous ovules are found in
Compylotropous ovules are found in Female dog reproductive anatomy
Female dog reproductive anatomy Fallopian tube
Fallopian tube