Reproductive Organs and Hormones Unit 2 What you

- Slides: 37
Reproductive Organs and Hormones Unit 2
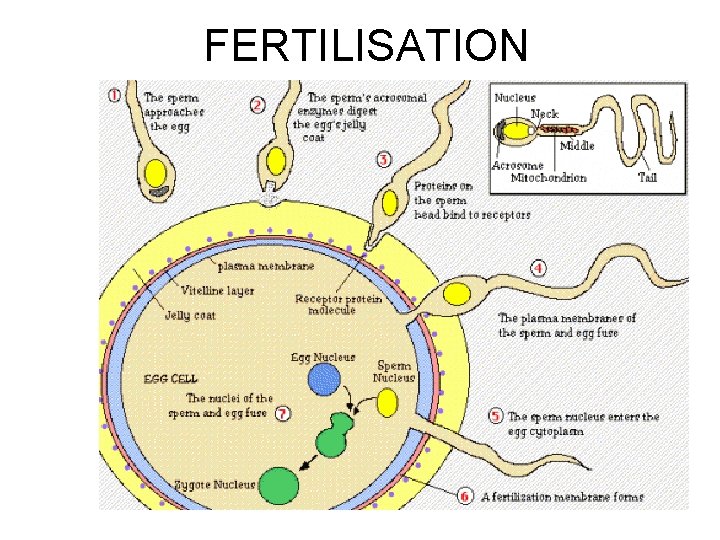
What you should know • The structure and function of reproductive organs and gametes and their role in fertilisation. • Gamete production in the testes. The roles of seminiferous tubules, interstitial cells, testosterone, prostate gland seminal vesicles. • Gamete production in the ovaries to include maturation of ova and the development of a follicle. Site of fertilisation in the oviduct and zygote formation.
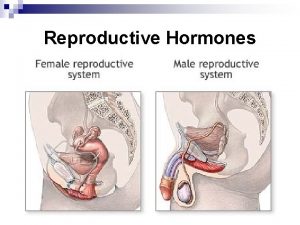
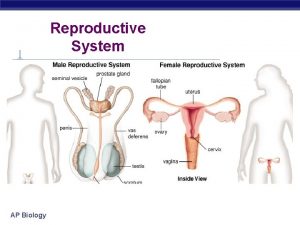
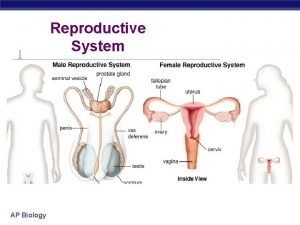
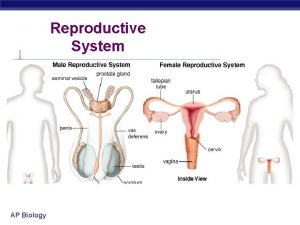
Reproductive Organs and Gametes • Prior Knowledge – Reproductive organs produce gametes – Male gamete- sperm – Female gamete- egg/ova – Male reproductive organ- testes – Female reproductive organ-ovary
Production of Gametes • A germ line is the sex cells (eggs and sperm) that are used by sexually reproducing organisms to pass on genes from generation to generation. • Gametes are produced by germline cells
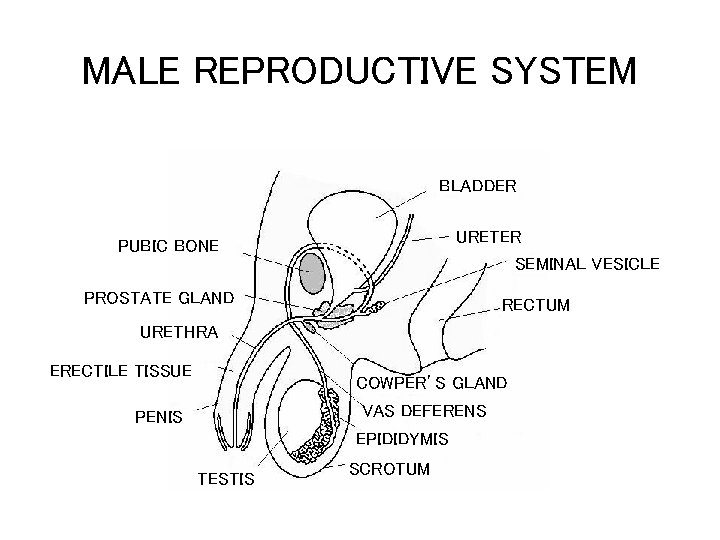
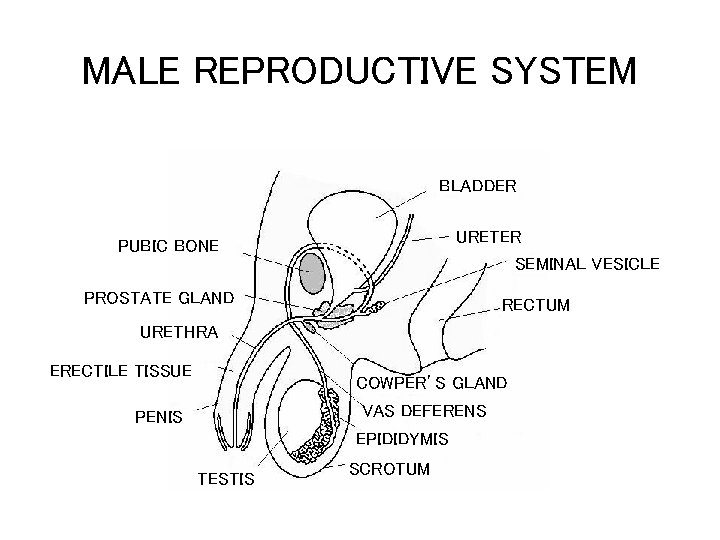
MALE REPRODUCTIVE SYSTEM BLADDER URETER SEMINAL VESICLE PUBIC BONE PROSTATE GLAND RECTUM URETHRA ERECTILE TISSUE COWPER’S GLAND VAS DEFERENS PENIS EPIDIDYMIS TESTIS SCROTUM
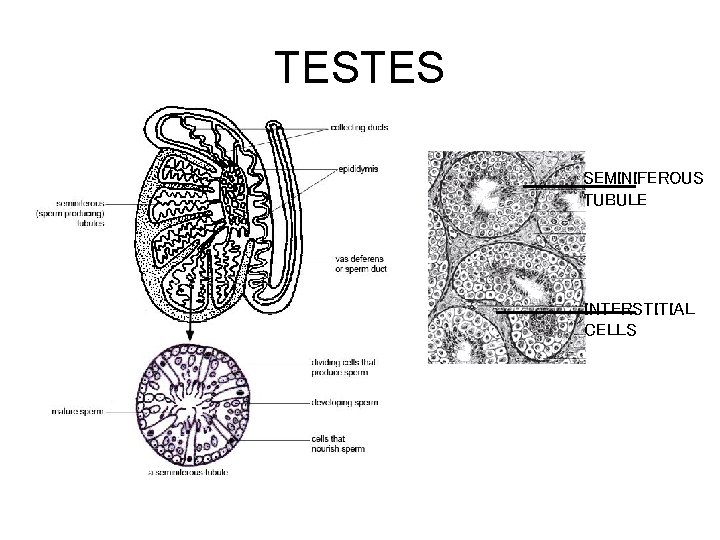
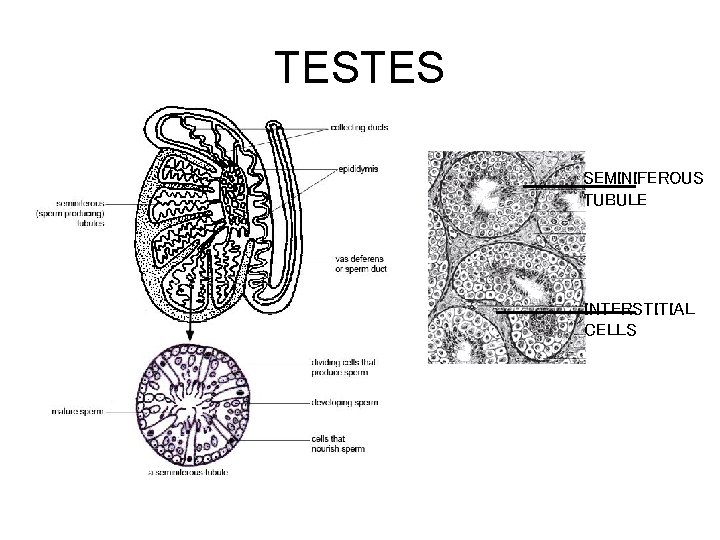
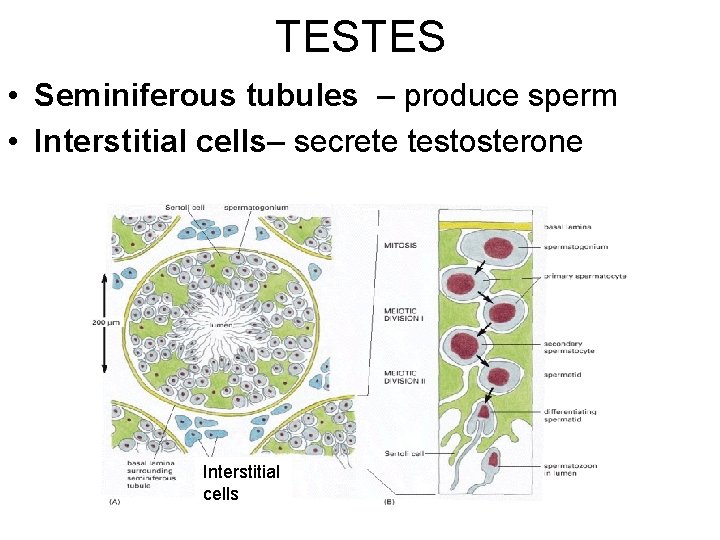
TESTES SEMINIFEROUS TUBULE INTERSTITIAL CELLS
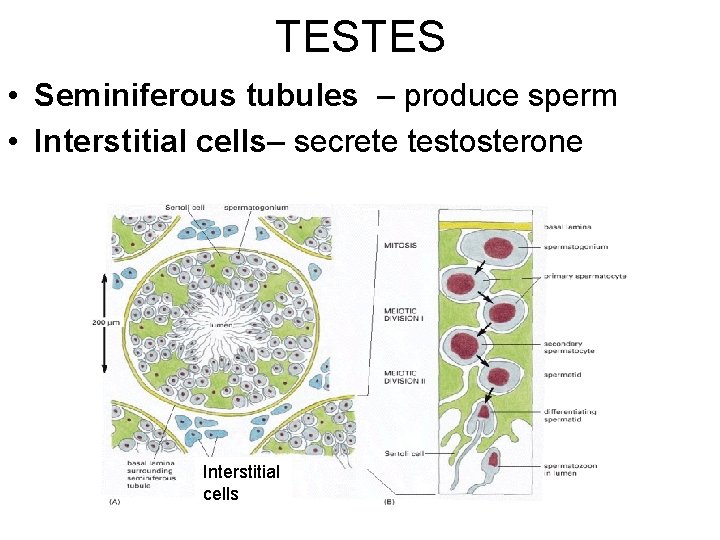
TESTES • Seminiferous tubules – produce sperm • Interstitial cells– secrete testosterone Interstitial cells
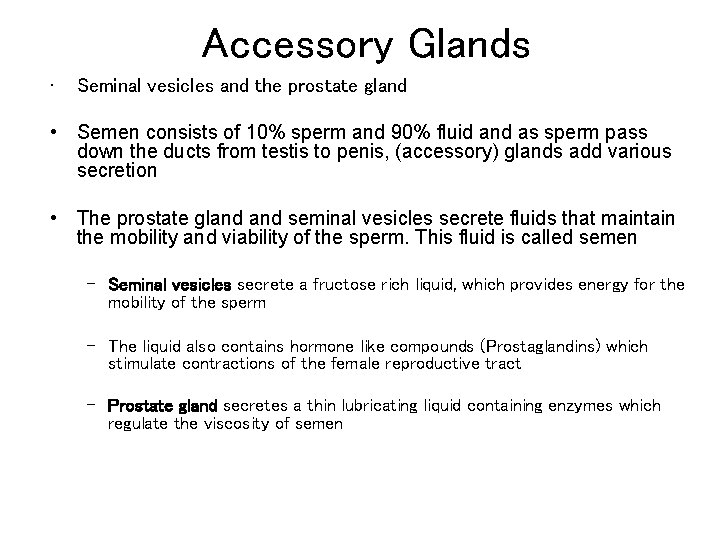
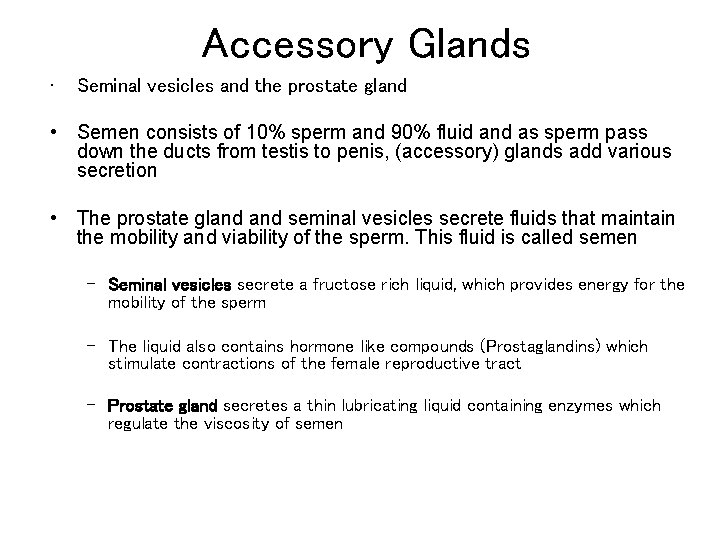
Accessory Glands • Seminal vesicles and the prostate gland • Semen consists of 10% sperm and 90% fluid and as sperm pass down the ducts from testis to penis, (accessory) glands add various secretion • The prostate gland seminal vesicles secrete fluids that maintain the mobility and viability of the sperm. This fluid is called semen – Seminal vesicles secrete a fructose rich liquid, which provides energy for the mobility of the sperm – The liquid also contains hormone like compounds (Prostaglandins) which stimulate contractions of the female reproductive tract – Prostate gland secretes a thin lubricating liquid containing enzymes which regulate the viscosity of semen
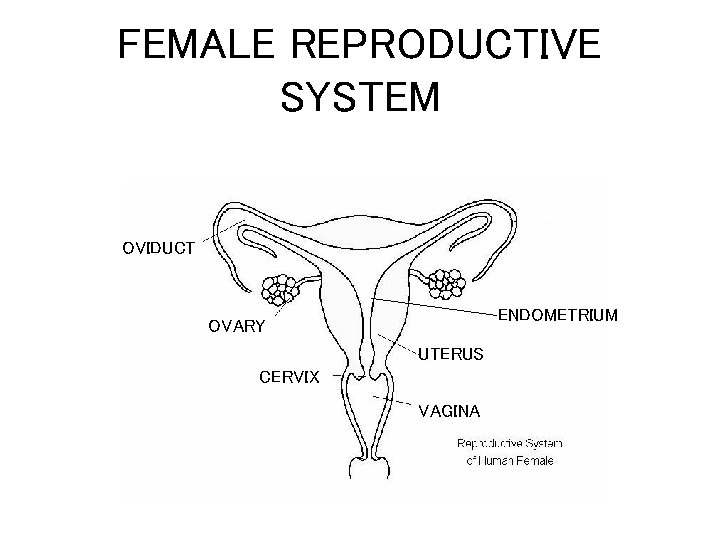
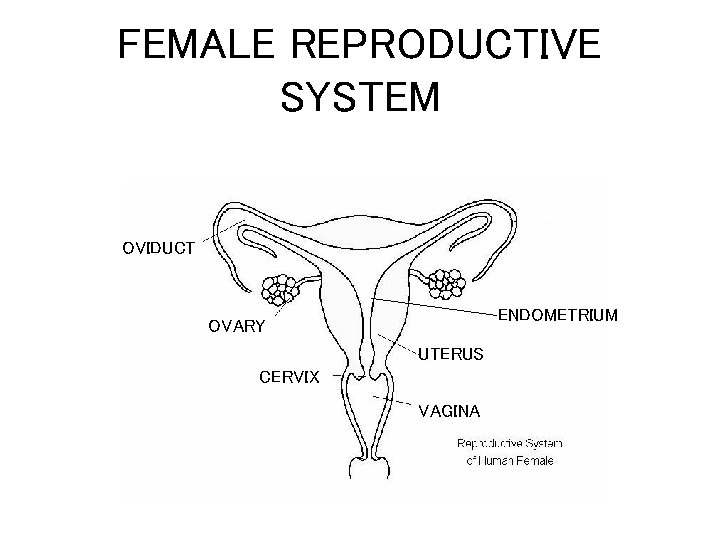
FEMALE REPRODUCTIVE SYSTEM OVIDUCT ENDOMETRIUM OVARY UTERUS CERVIX VAGINA
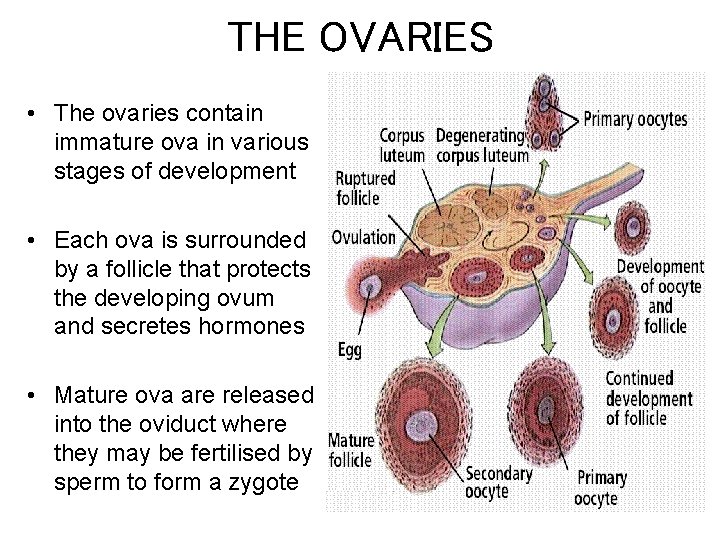
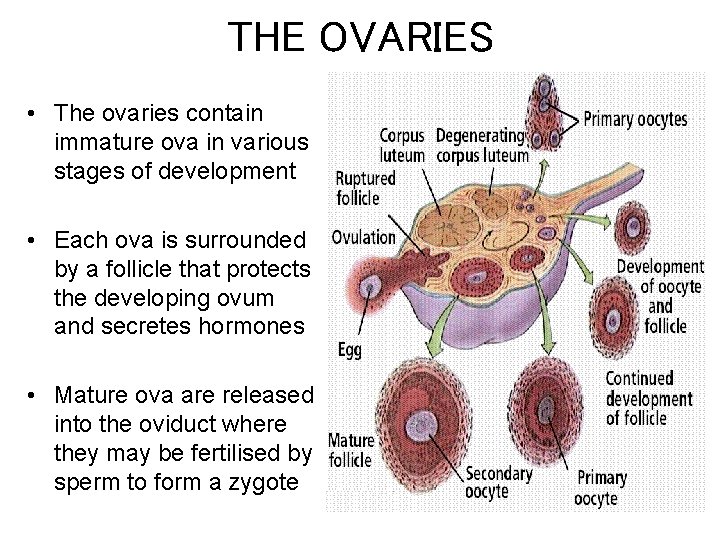
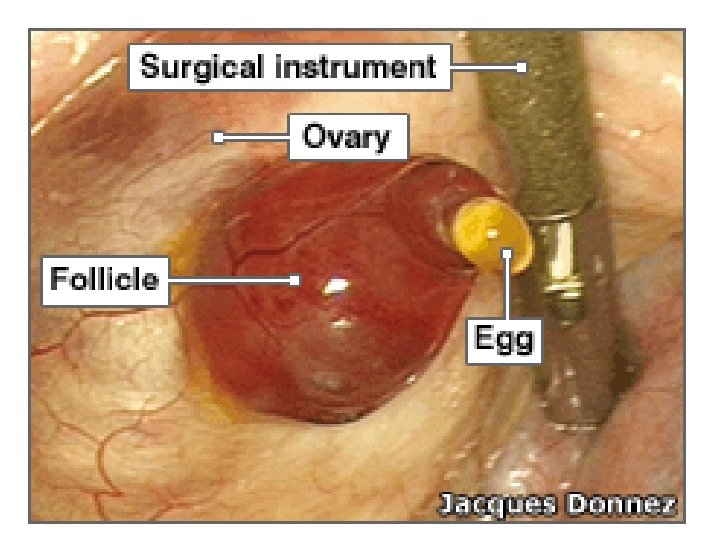
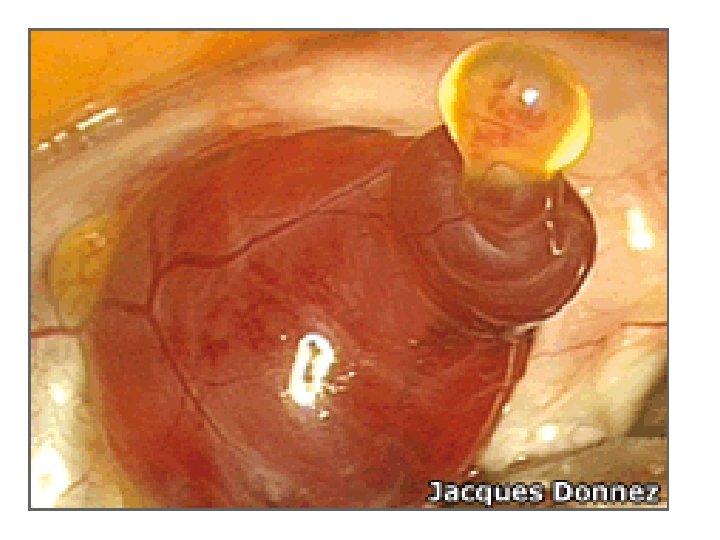
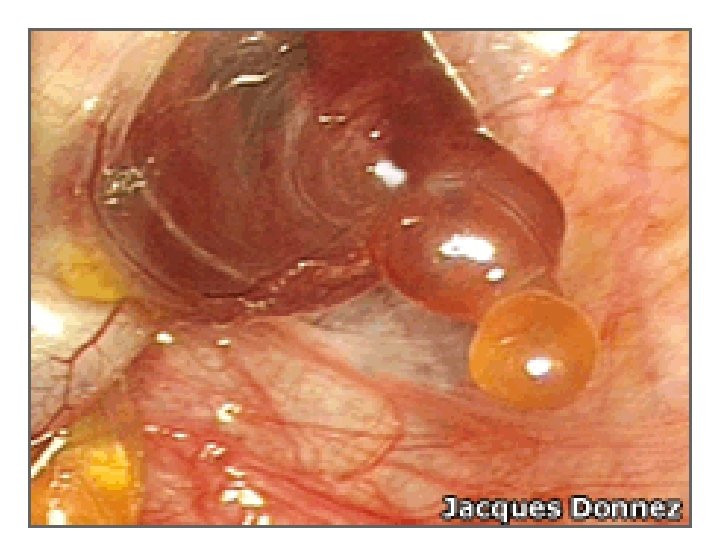
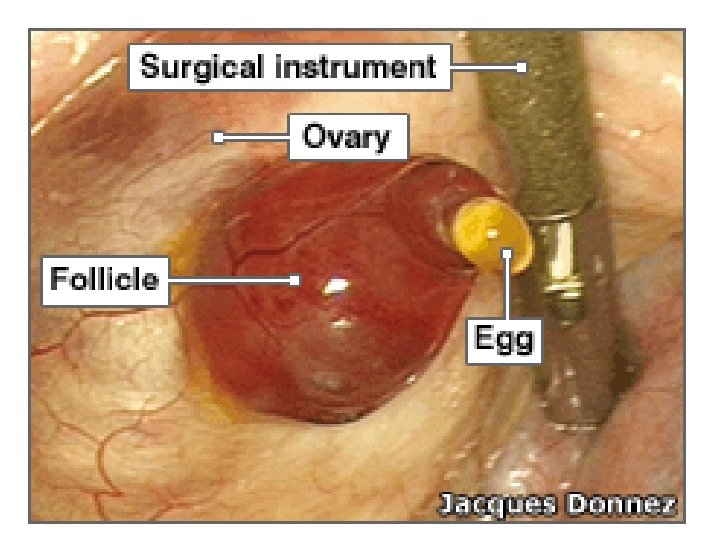
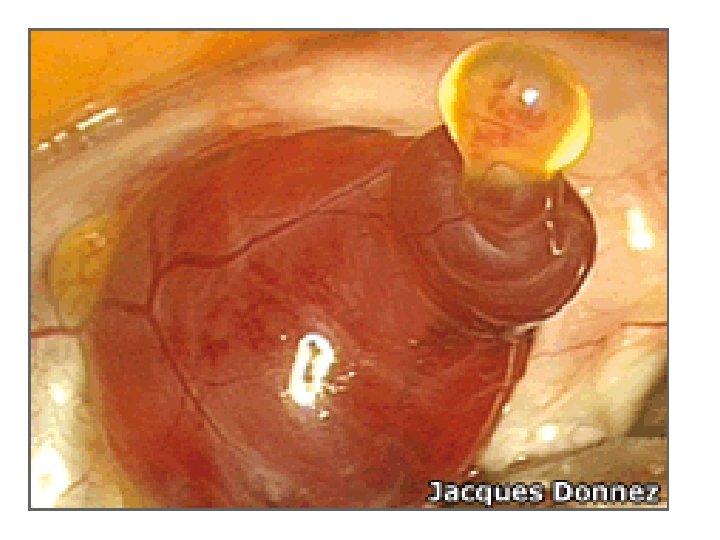
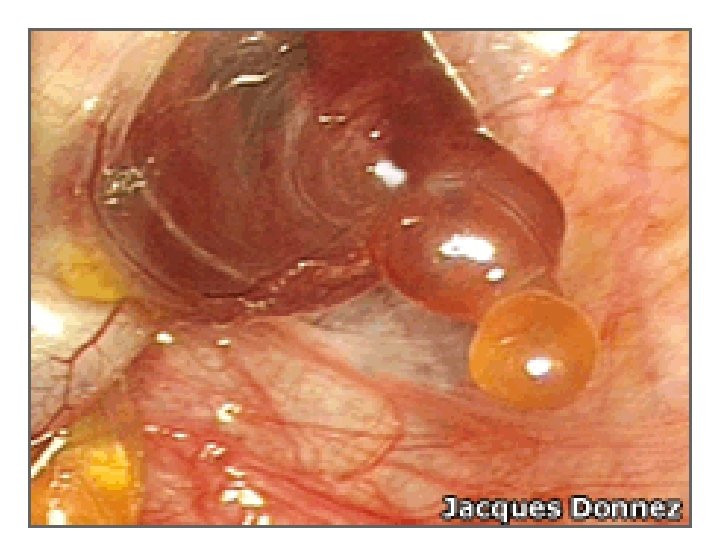
THE OVARIES • The ovaries contain immature ova in various stages of development • Each ova is surrounded by a follicle that protects the developing ovum and secretes hormones • Mature ova are released into the oviduct where they may be fertilised by sperm to form a zygote
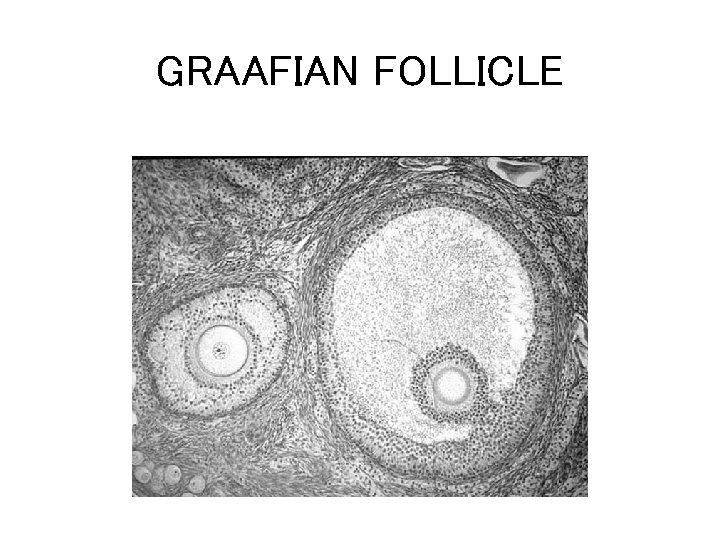
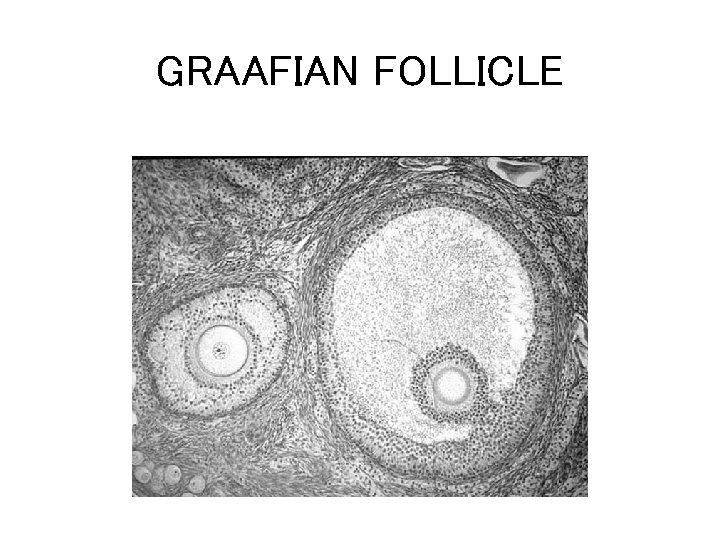
GRAAFIAN FOLLICLE
Human Ovulation

You should know • The structure and function of reproductive organs and gametes and their role in fertilisation. • Gamete production in the testes. The roles of seminiferous tubules, interstitial cells, testosterone, prostate gland seminal vesicles. • Gamete production in the ovaries to include maturation of ova and the development of a follicle. Site of fertilisation in the oviduct and zygote formation.
Hormonal Control
What You Should Know • Hormonal onset of puberty. Pituitary gland releases follicle stimulating hormone (FSH), luteinising hormone (LH) or interstitial cell stimulating hormone (ICSH) via the hypothalamus • Hormonal control of sperm production. FSH promotes sperm production and ICSH stimulates the production of testosterone. Testosterone also stimulates sperm production and activates the prostate gland seminal vesicles. Negative feedback control of testosterone by FSH and ICSH. • Hormonal control of the menstrual cycle. Development of a follicle and the endometrium in the uterus. Roles of FSH, LH, oestrogen and progesterone in the menstrual cycle. Development of a follicle, the corpus luteum and the endometrium. Follicular and luteal phases. Blastocyst implantation. Negative feedback control through pituitary gland, FSH and progesterone, leading to menstruation. •
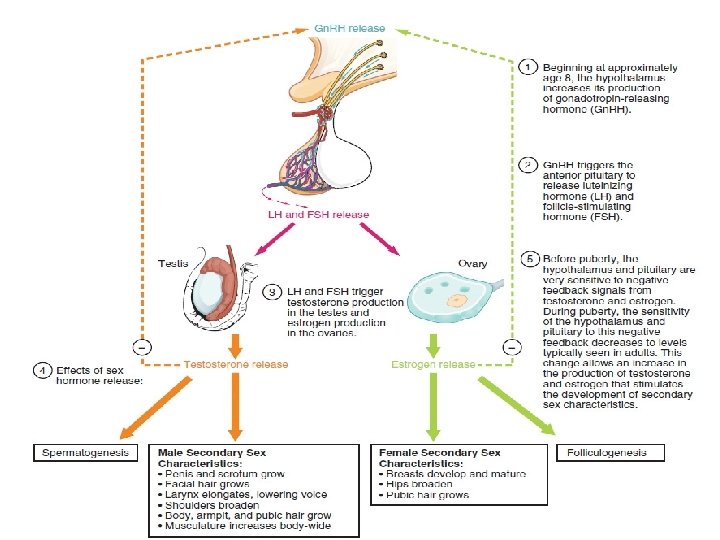
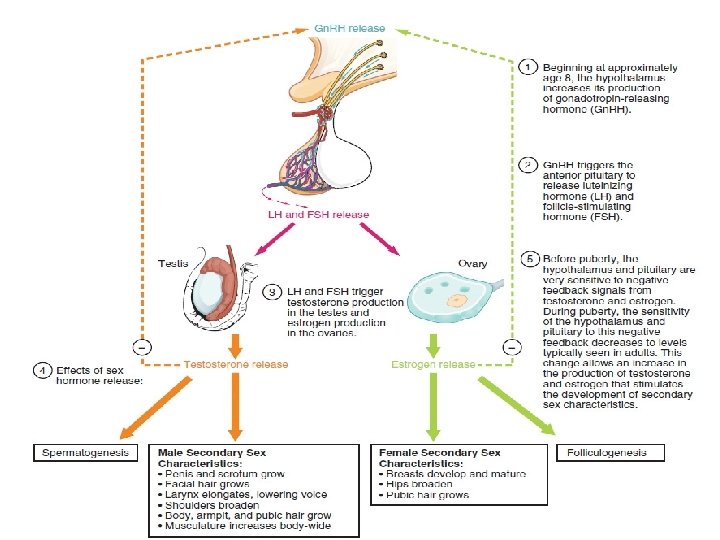
Hormones • Hormones are chemical messengers produced by cells that bind to receptors on the plasma membrane of other cells or enter other cells and alter the metabolic function of these cells. • In response to a signal from the brain, hormones are secreted directly into the blood by the glands that produce and store them. These glands make up what is known as the endocrine system • The testes and ovaries, or "gonads", are endocrine glands. – In males, testes produce sperm and secrete the male sex hormone testosterone; – in females, ovaries produce eggs and the female hormone oestrogen. – It is these hormones that determine secondary sex characteristics like muscle mass and facial hair. They also help to orchestrate sperm production, menstruation and pregnancy.
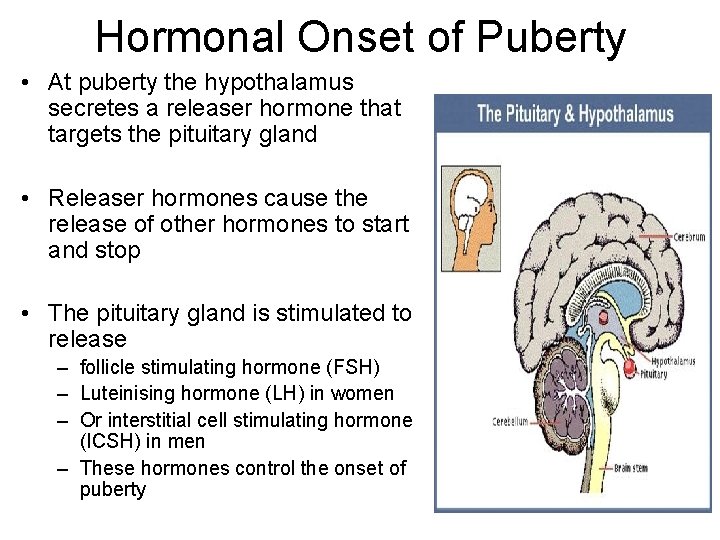
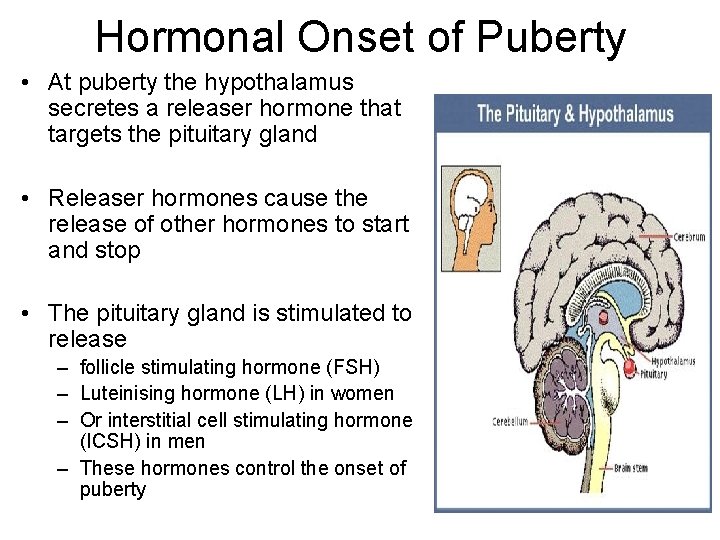
Hormonal Onset of Puberty • At puberty the hypothalamus secretes a releaser hormone that targets the pituitary gland • Releaser hormones cause the release of other hormones to start and stop • The pituitary gland is stimulated to release – follicle stimulating hormone (FSH) – Luteinising hormone (LH) in women – Or interstitial cell stimulating hormone (ICSH) in men – These hormones control the onset of puberty
Hormonal Control of Sperm Production
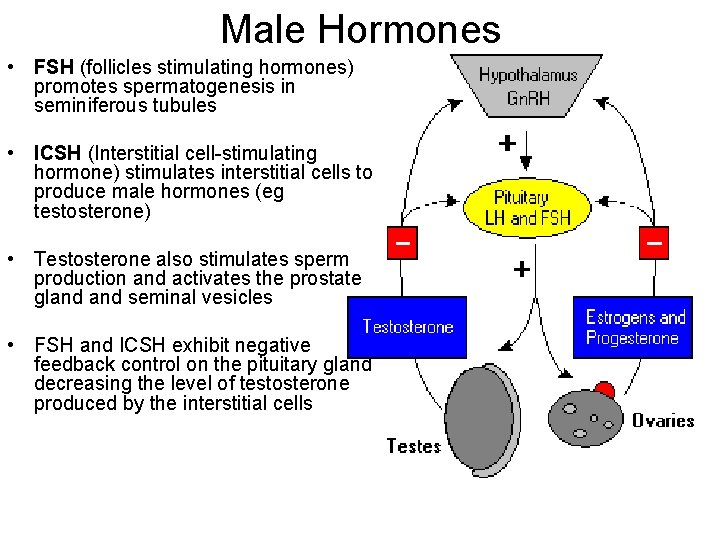
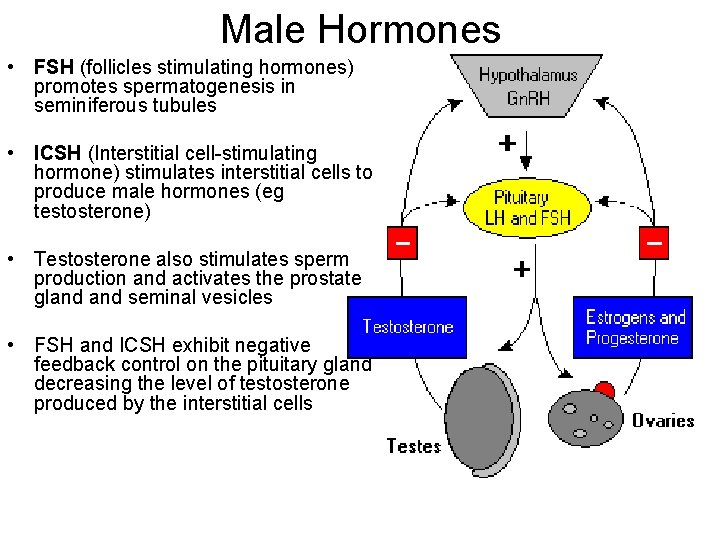
Male Hormones • FSH (follicles stimulating hormones) promotes spermatogenesis in seminiferous tubules • ICSH (Interstitial cell-stimulating hormone) stimulates interstitial cells to produce male hormones (eg testosterone) • Testosterone also stimulates sperm production and activates the prostate gland seminal vesicles • FSH and ICSH exhibit negative feedback control on the pituitary gland decreasing the level of testosterone produced by the interstitial cells
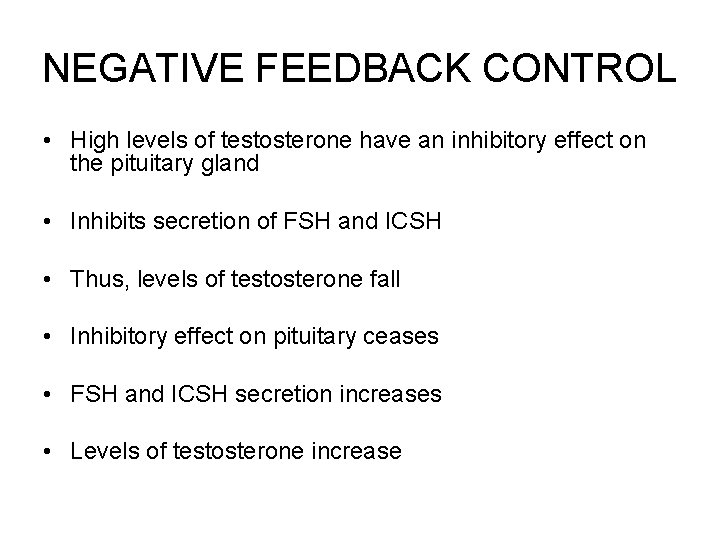
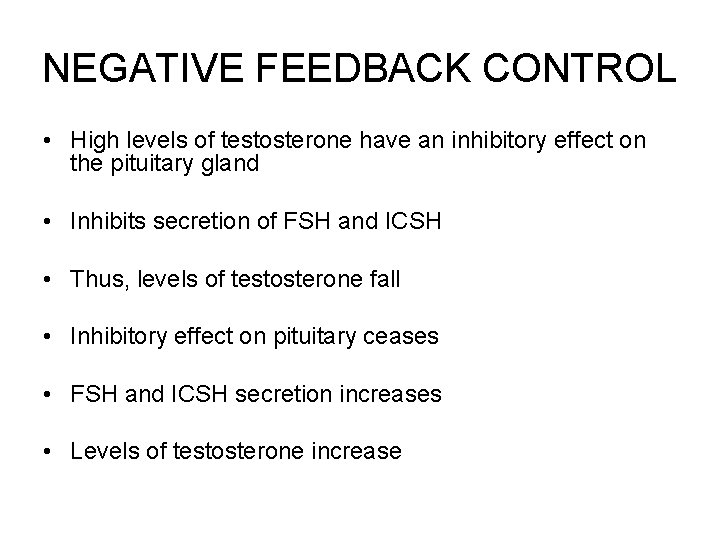
NEGATIVE FEEDBACK CONTROL • High levels of testosterone have an inhibitory effect on the pituitary gland • Inhibits secretion of FSH and ICSH • Thus, levels of testosterone fall • Inhibitory effect on pituitary ceases • FSH and ICSH secretion increases • Levels of testosterone increase
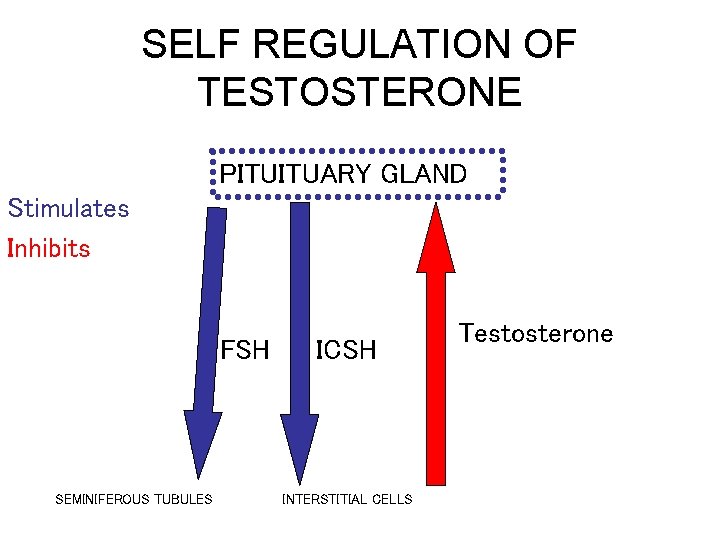
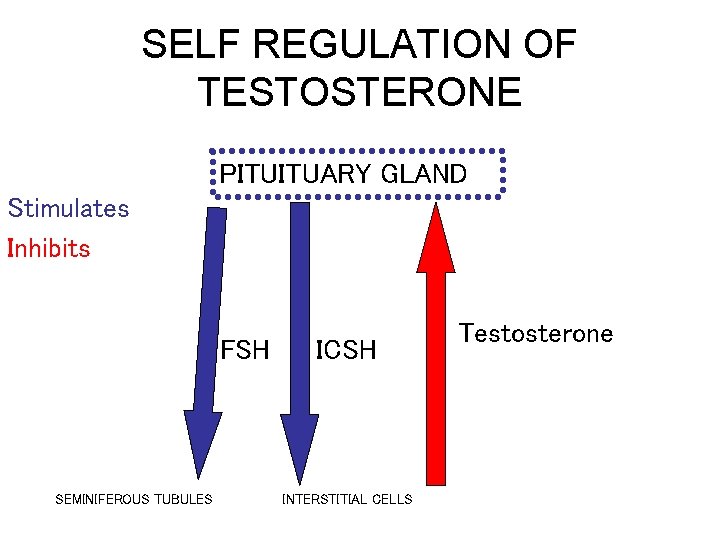
SELF REGULATION OF TESTOSTERONE PITUITUARY GLAND Stimulates Inhibits FSH SEMINIFEROUS TUBULES ICSH INTERSTITIAL CELLS Testosterone
Hormonal Control of the Menstrual Cycle
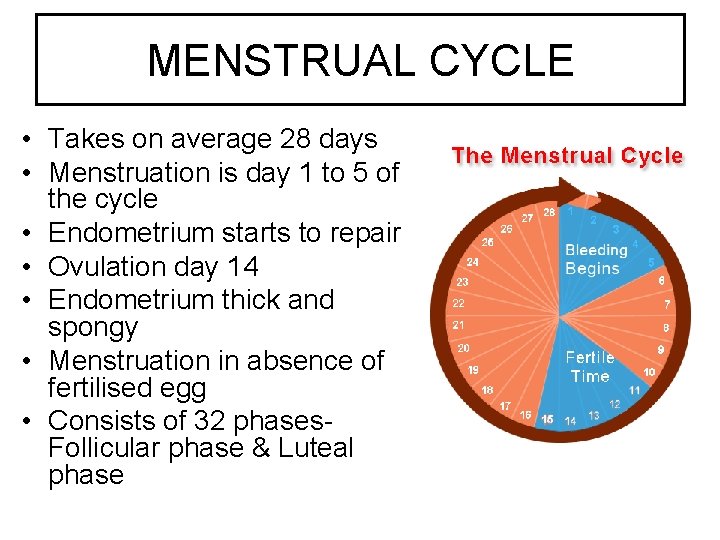
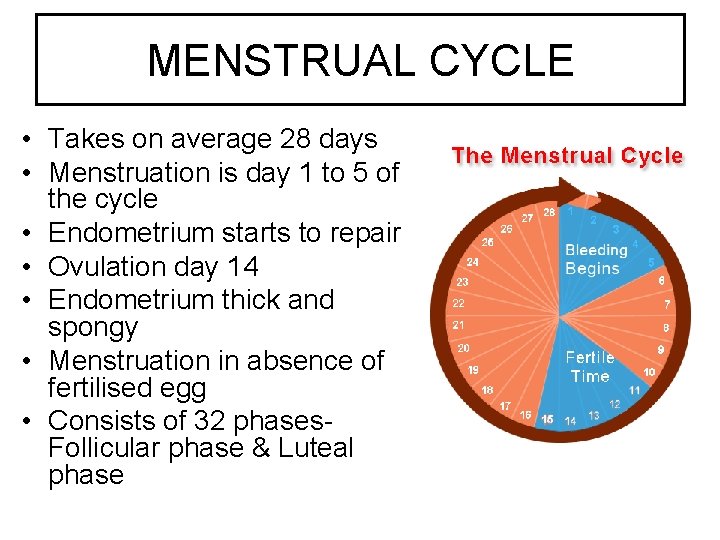
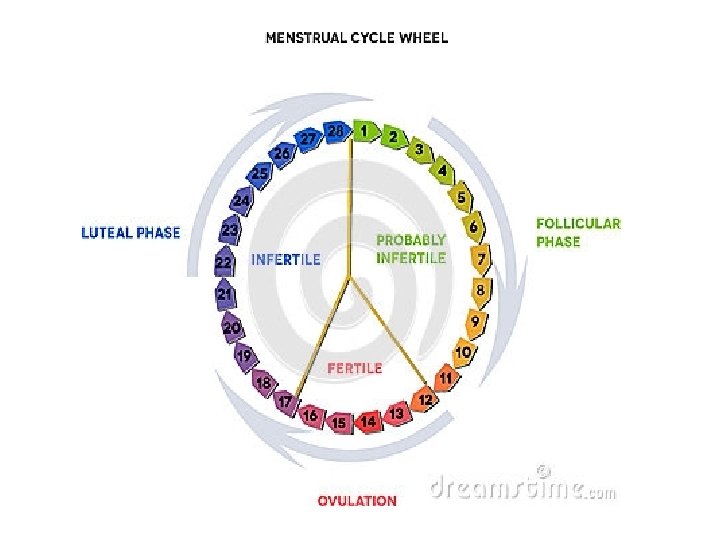
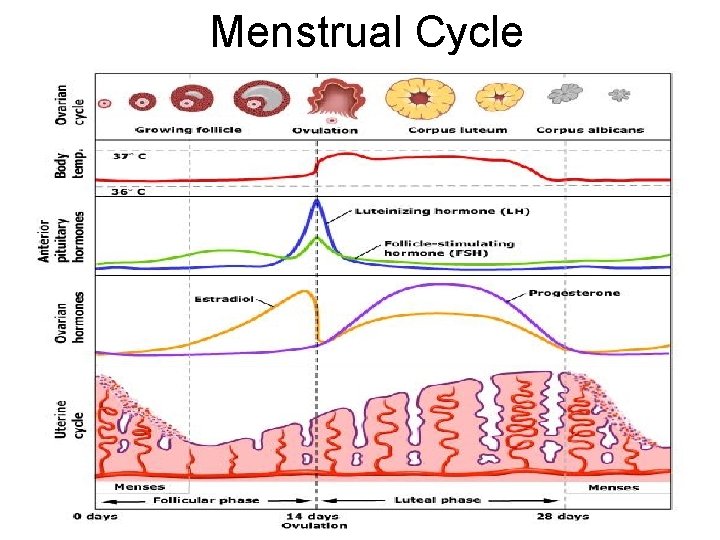
MENSTRUAL CYCLE • Takes on average 28 days • Menstruation is day 1 to 5 of the cycle • Endometrium starts to repair • Ovulation day 14 • Endometrium thick and spongy • Menstruation in absence of fertilised egg • Consists of 32 phases. Follicular phase & Luteal phase
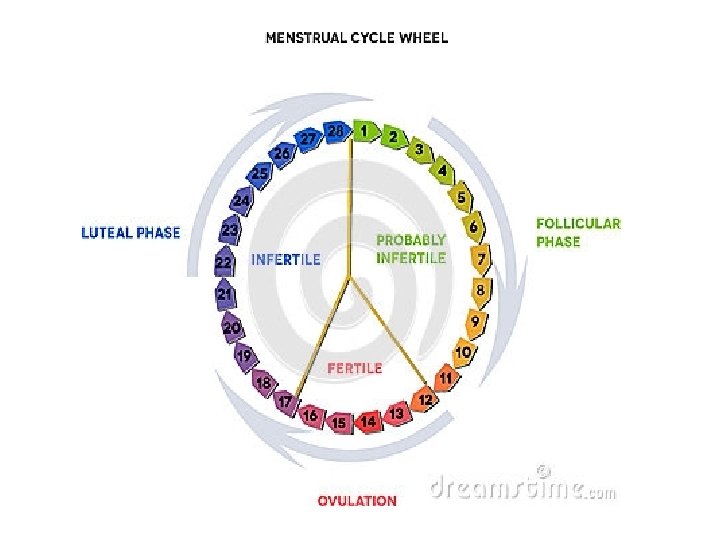
Follicular Phase • FSH – Causes development of follicles in ovary – Stimulates secretion of oestrogen by the follicle • oestrogen stimulates proliferation of the endometrium preparing it for implantation and affects the consistency of cervical mucus making it easier for sperm to penetrate
Luteal Phase • LH – Peak levels of oestrogen stimulate a surge in the secretion of LH which triggers ovulation – Causes Graafian follicle to rupture (ovulation) – Causes development of the corpus luteum from the follicle – Stimulates the corpus luteum to secrete progesterone
• Progesterone promotes further development and vascularisation of the endometrium preparing it to receive a blastocyst if fertilisation occurs • Ovum dies after 36 hours
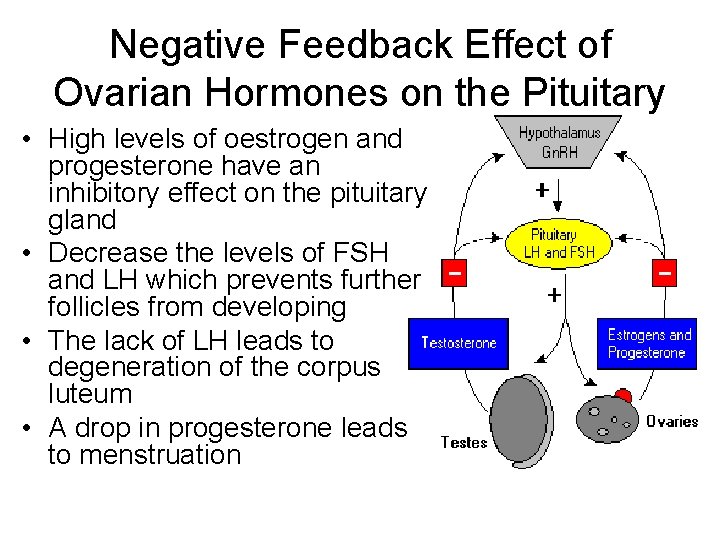
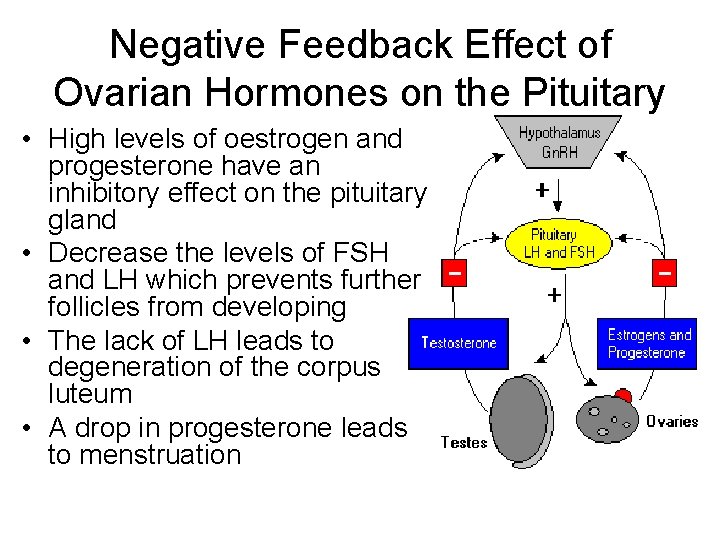
Negative Feedback Effect of Ovarian Hormones on the Pituitary • High levels of oestrogen and progesterone have an inhibitory effect on the pituitary gland • Decrease the levels of FSH and LH which prevents further follicles from developing • The lack of LH leads to degeneration of the corpus luteum • A drop in progesterone leads to menstruation
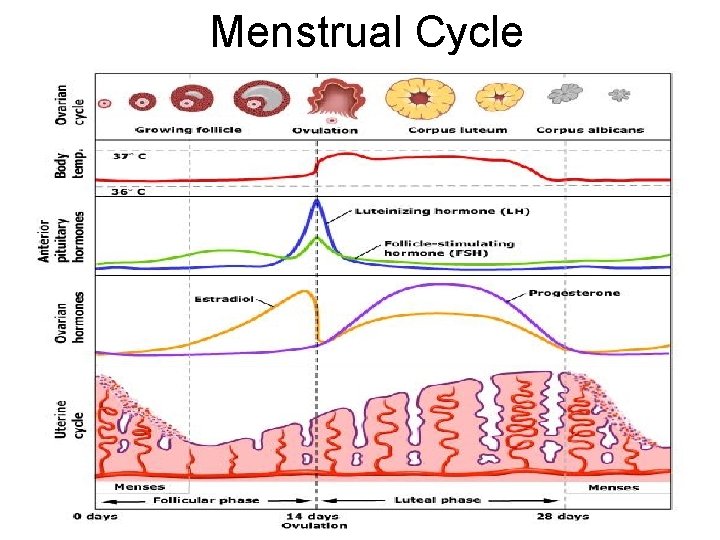
Menstrual Cycle
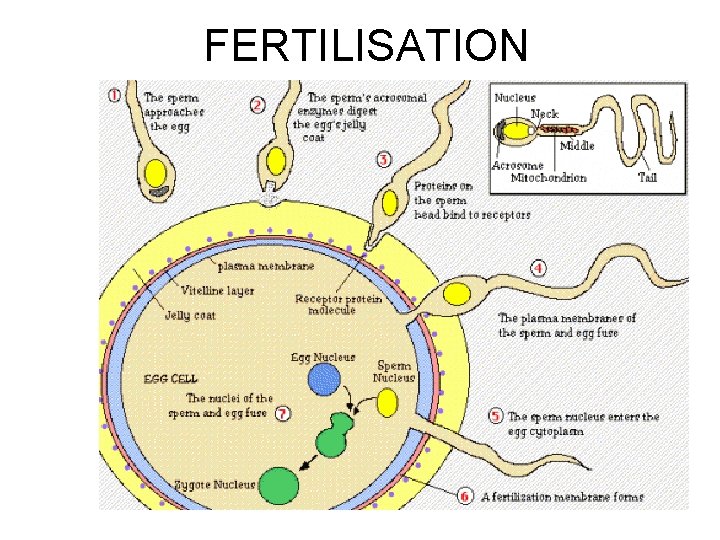
FERTILISATION
FERTILISATION
 Urethral opening female
Urethral opening female Sagittal female reproductive system
Sagittal female reproductive system Reproductive organs of the bull
Reproductive organs of the bull Genital development
Genital development Sheep reproductive system
Sheep reproductive system Oviduct funnel
Oviduct funnel Male reproductive organ
Male reproductive organ What is fgm
What is fgm Unit 6:14 reproductive system
Unit 6:14 reproductive system Lesson 3 the female reproductive system
Lesson 3 the female reproductive system Bioflix activity homeostasis hormones and homeostasis
Bioflix activity homeostasis hormones and homeostasis Oxication
Oxication Male and female hormones
Male and female hormones Male and female hormones
Male and female hormones Bioflix activity homeostasis high blood glucose
Bioflix activity homeostasis high blood glucose Respond to
Respond to Plant hormones and responses
Plant hormones and responses Madhukar mittal
Madhukar mittal Surfaces of thyroid gland
Surfaces of thyroid gland Phyllodes tumor mammogram
Phyllodes tumor mammogram Hormones
Hormones Unit 10, unit 10 review tests, unit 10 general test
Unit 10, unit 10 review tests, unit 10 general test Tell me what you eat and i shall tell you what you are
Tell me what you eat and i shall tell you what you are Primary and secondary retroperitoneal organs
Primary and secondary retroperitoneal organs Abdominal organs quadrants
Abdominal organs quadrants Biologymad kidney
Biologymad kidney Mouth function in digestive system
Mouth function in digestive system Body quadrants and organs
Body quadrants and organs Biomaterials artificial organs and tissue engineering
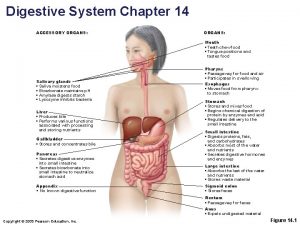
Biomaterials artificial organs and tissue engineering Accessory organs
Accessory organs Primary and secondary retroperitoneal organs
Primary and secondary retroperitoneal organs Lymphatic system organs and functions
Lymphatic system organs and functions 3 tissues of a plant
3 tissues of a plant Lymphatic system organs and functions
Lymphatic system organs and functions Plant tissue and organs
Plant tissue and organs Colonchyma
Colonchyma Frog artery
Frog artery Steroid hormone lipid
Steroid hormone lipid