Examination and Assessment of the Neonatal and of









- Slides: 55
Examination and Assessment of the Neonatal and of the Pediatric Patient Module D Walsh: Chapter 4
Objectives § Describe the factors that most influence neonatal outcome. § List criteria for determining whether an infant is large for gestational age, appropriate for gestational age, or small for gestational age. § List critical vital signs with normal values to be evaluated as part of the newborn's initial physical examination. § Describe criteria for determining whether an infant is displaying apneic spells. § Identify signs and symptoms of respiratory distress in the newborn. § Describe the technique for rapid identification of a pneumothorax in a newborn. § List the possible cardiovascular anomalies associated with different patterns of abnormal pulses. § List the elements of a normal abdominal examination and the significance of abnormal findings. § List the three types of scalp swelling observed in newborns and the characteristics and significance of each type. § List the most common structural abnormalities observed in the nose, lips, mouth, and oral cavity. § Describe the signs and symptoms of the most common types of birth injuries. § List the elements of a basic neurologic examination in the newborn. § Describe the signs and symptoms suggesting the presence of sepsis in the newborn. § List the laboratory tests most commonly done on the newborn and the range of normal values for each. § Identify and use historical and physical findings to develop a differential diagnosis of a child's respiratory condition. § Determine the severity of a child's respiratory condition. § Communicate important historical and physical findings concerning a child's respiratory condition to the health care team in a timely manner. § Assist in planning and executing evaluation and management of the pediatric patient.
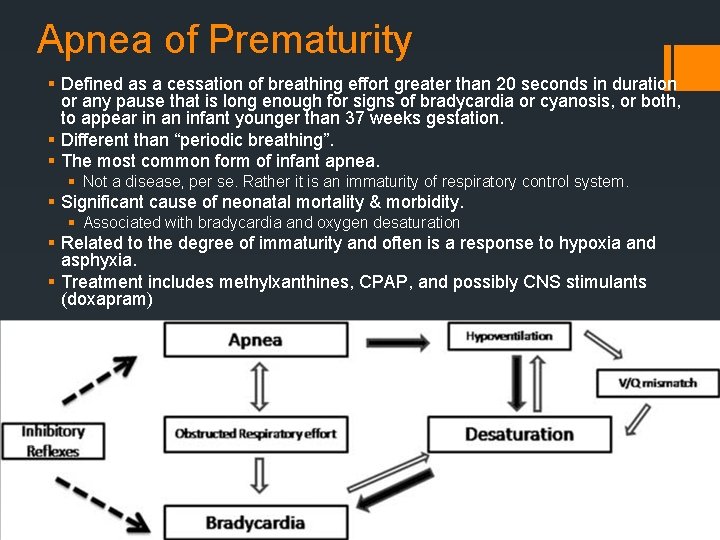
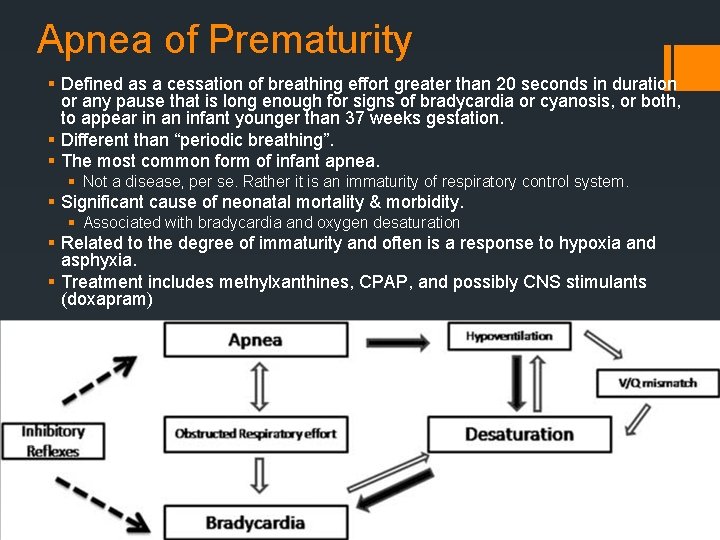
Apnea of Prematurity § Defined as a cessation of breathing effort greater than 20 seconds in duration or any pause that is long enough for signs of bradycardia or cyanosis, or both, to appear in an infant younger than 37 weeks gestation. § Different than “periodic breathing”. § The most common form of infant apnea. § Not a disease, per se. Rather it is an immaturity of respiratory control system. § Significant cause of neonatal mortality & morbidity. § Associated with bradycardia and oxygen desaturation § Related to the degree of immaturity and often is a response to hypoxia and asphyxia. § Treatment includes methylxanthines, CPAP, and possibly CNS stimulants (doxapram)
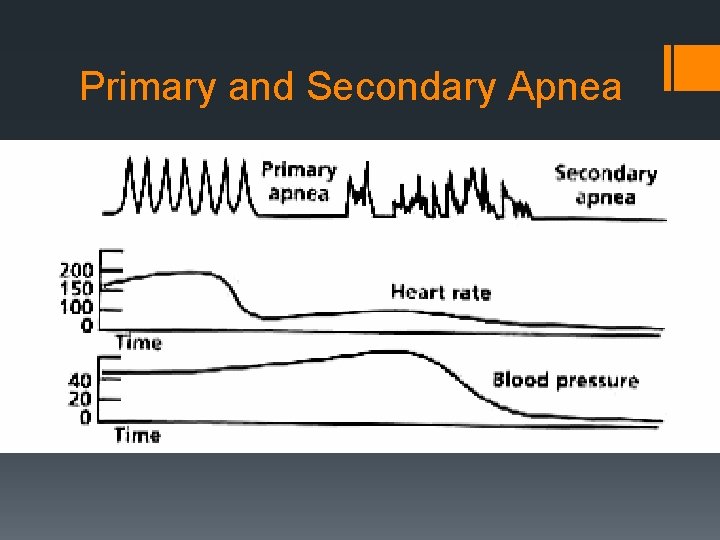
Apnea of Prematurity § Two Types: § Primary Apnea § Occurs as an initial response to hypoxia. § Reduction in heart rate and, to a lesser extent, blood pressure. § Responds well to stimulation. § Secondary Apnea § Occurs as a result of continued hypoxia. § Weak, gasping respirations. § Positive-pressure ventilation MUST be initiated. § Heart rate and blood pressure will fall and death will ensue if not treated quickly. § Apnea may occur in utero, and baby may be born in secondary apnea. ASSUME if apneic at birth.
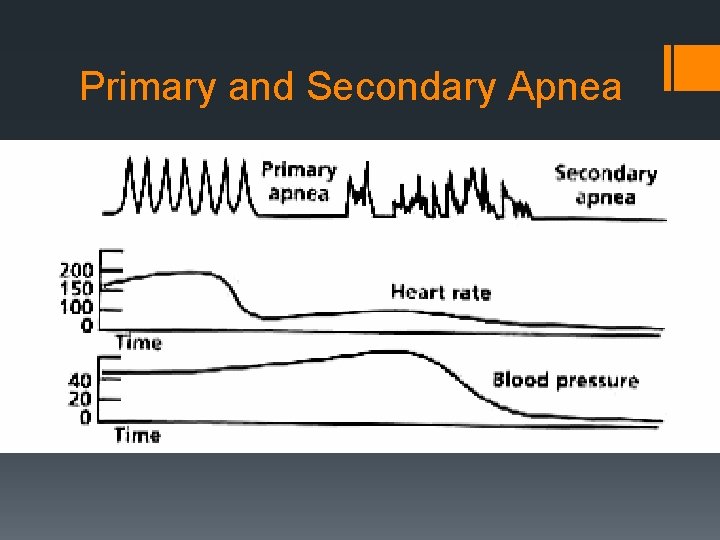
Primary and Secondary Apnea
Examination of the Neonatal Patient
Gestational Age Assessment
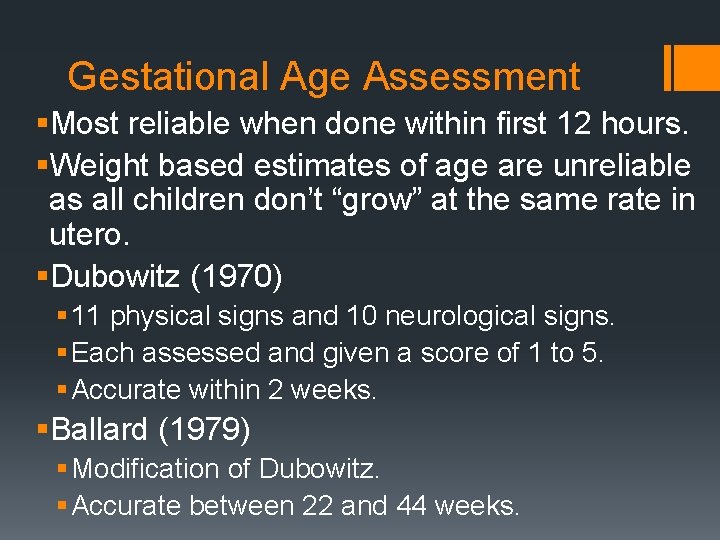
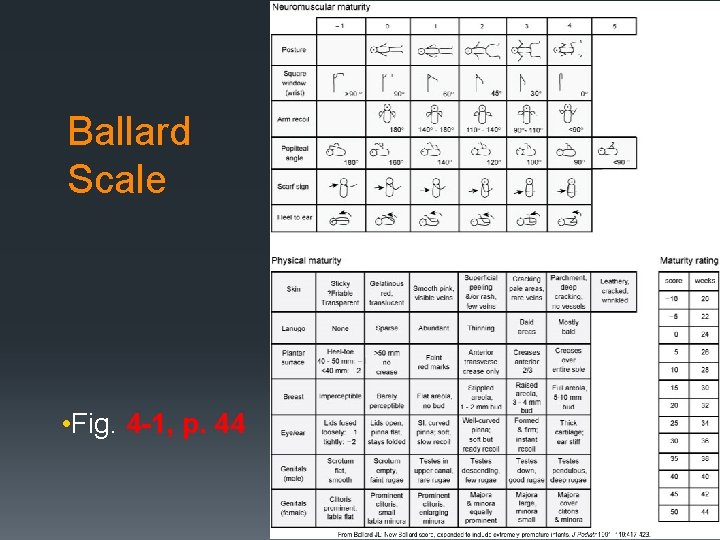
Gestational Age Assessment §Most reliable when done within first 12 hours. §Weight based estimates of age are unreliable as all children don’t “grow” at the same rate in utero. §Dubowitz (1970) § 11 physical signs and 10 neurological signs. § Each assessed and given a score of 1 to 5. § Accurate within 2 weeks. §Ballard (1979) § Modification of Dubowitz. § Accurate between 22 and 44 weeks.
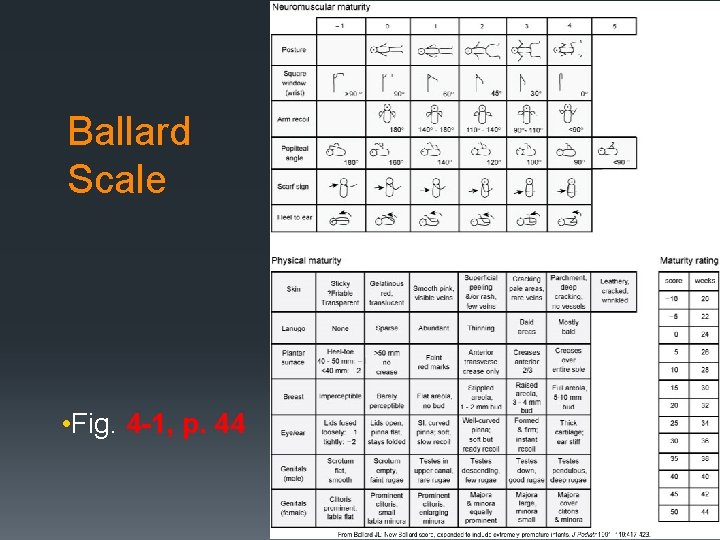
Ballard Scale • Fig. 4 -1, p. 44
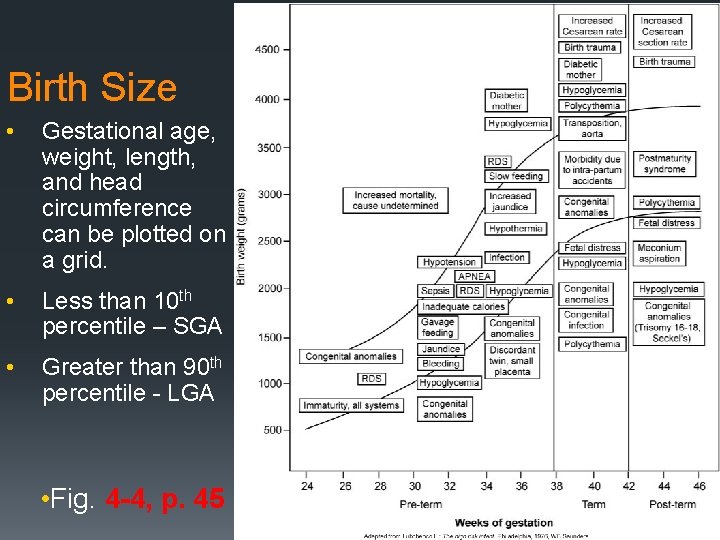
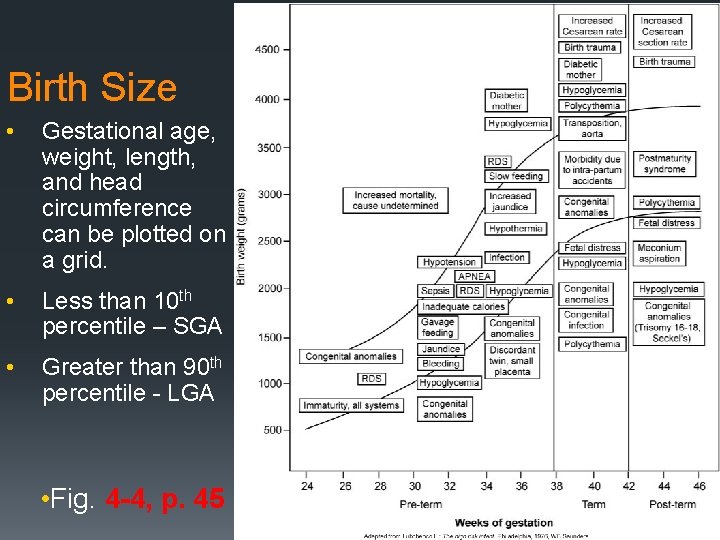
Birth Size • Gestational age, weight, length, and head circumference can be plotted on a grid. • Less than 10 th percentile – SGA • Greater than 90 th percentile - LGA • Fig. 4 -4, p. 45
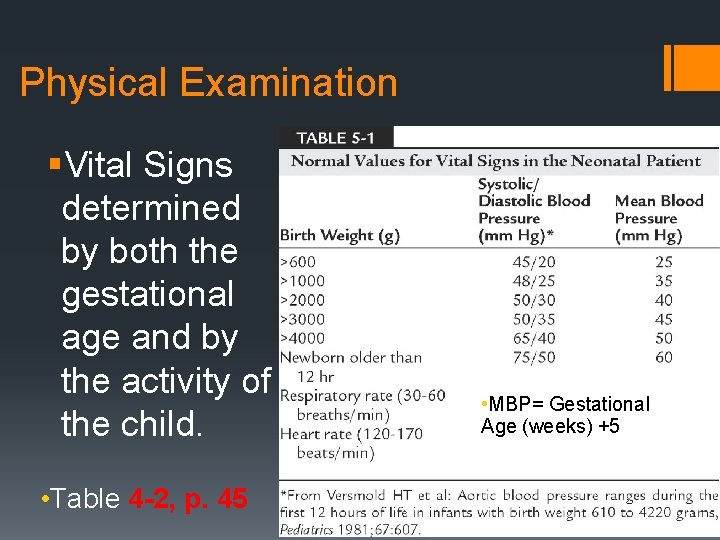
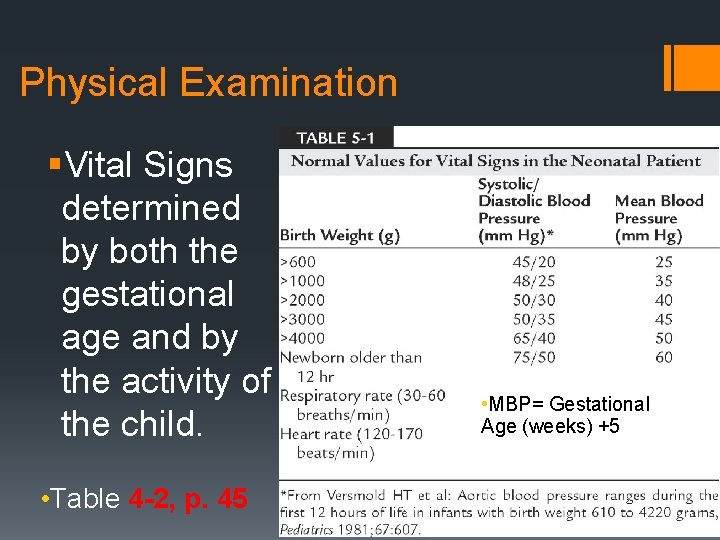
Physical Examination §Vital Signs determined by both the gestational age and by the activity of the child. • Table 4 -2, p. 45 • MBP= Gestational Age (weeks) +5
Common Dermal Findings §Vernix caseosa: § White cream cheese-like material that covers fetus. § Appears at 20 -24 weeks § Remains thick until 36 weeks § Disappears by 41 -42 weeks §Lanugo § Fine, downy hair that covers the fetal body § Appears at 26 weeks. § Thins and disappears by week 32.
Common Dermal Findings §Skin Maturity § 25 to 26 weeks – gelatinous and transparent (visible vessels)
Jaundice § Definition: Yellowish-orange skin color that accompanies increased levels of bilirubin in the blood. § aka hyperbilirubinemia. § Occurs due to the breakdown of old erythrocytes. § Eliminated by the intestinal tract or kidneys. § Bilirubin levels greater than 4 -6 mg/d. L will cause jaundice. § 25 to 50% of all term neonates have jaundice. § Quicker breakdown of erythrocytes in neonates. § Liver can’t handle the load.

Jaundice: Complications & Treatment §Kernicterus: Hyperbilirubinemia related encephalopathy. §Can lead to neurological deficits. §Treatment §Phototherapy lights (“bili lights”) §Exchange Transfusion
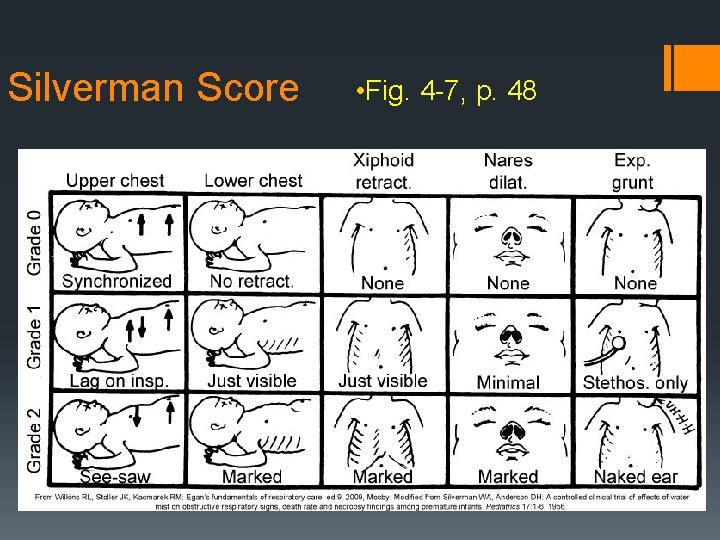
Physical Examination (cont. ) §Respiratory function §Rate (40 – 60/min) §Rhythm – periodic breathing §Silverman score §Respiratory Distress § Nasal flaring § Expiratory grunting § Retractions
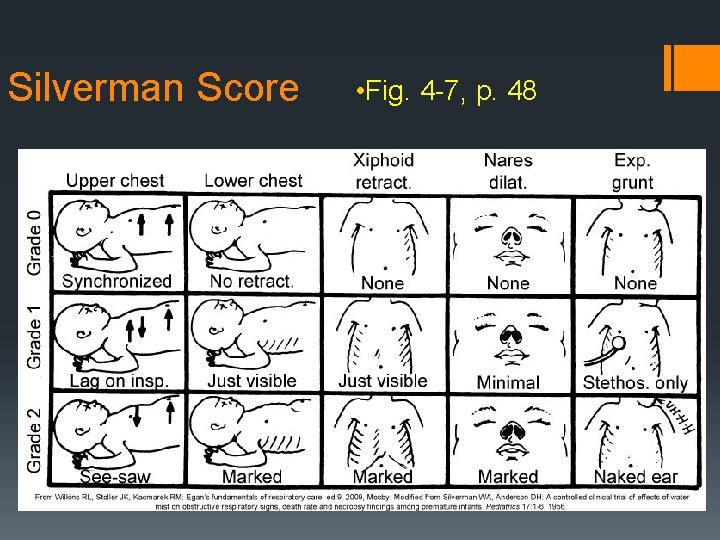
Silverman Score • Fig. 4 -7, p. 48
Physical Examination (cont. ) §Auscultation §Chest radiography
Physical Examination §Chest and cardiovascular system §Chest configuration §Pectus carinatum & pectus excavatum §Point of maximal cardiac impulse (PMI) §Transillumination (pneumothorax)


Physical Examination (cont. ) §Chest and cardiovascular system §Heart rate §Cardiac sounds §Pulses §Blood pressure §Pulse oximetry §Pre- and postductal
Physical Assessment §Abdomen §Contour §Obvious abdominal wall anomalies §Scaphoid §Auscultation and palpation §More than stomach §Cord §Anatomy §Gastroschisis vs. Omphalocele


Physical Examination §Head and neck §Shape of head §Fontanelles §Scalp edema §Face §Dysmorphic §Edema §Ears
Physical Examination (cont. ) §Head and neck § Nares § Mouth §Lips §Oral cavity § Tongue size (Pierre-Robin Syndrome – micrognathia) § Neck § Clavicles

Physical Examination (cont. ) §Musculoskeletal system, spine, and extremities §Dysmorphic §Number of digits §Abnormal positioning of joints §Spine §Dimple
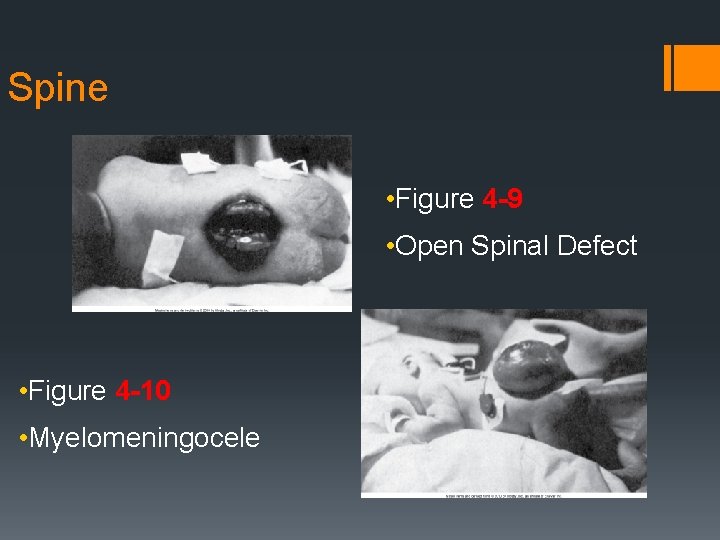
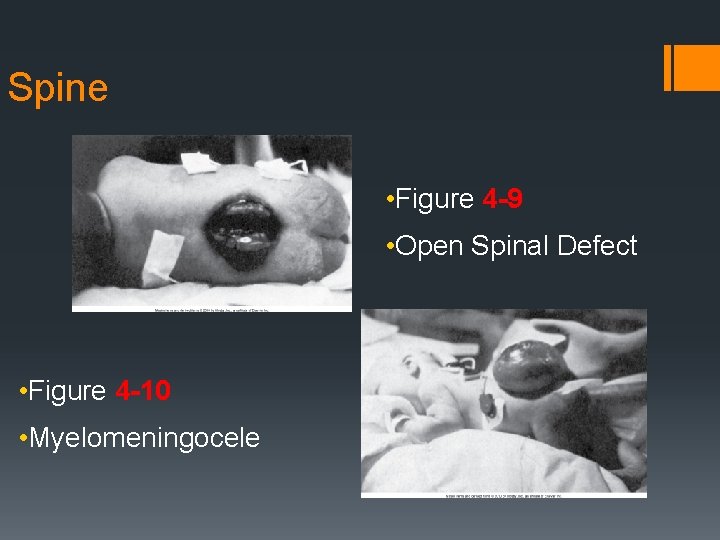
Spine • Figure 4 -9 • Open Spinal Defect • Figure 4 -10 • Myelomeningocele
Physical Examination §Cry §Strength §Sound
Neurologic Examination §Response to environment §Movement §Neonatal reflexes §Rooting §Grasp §Moro §Hearing

Moro Reflex
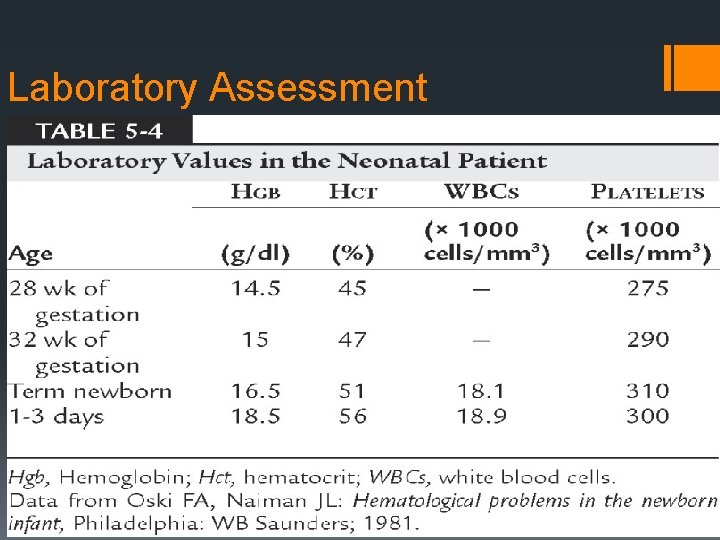
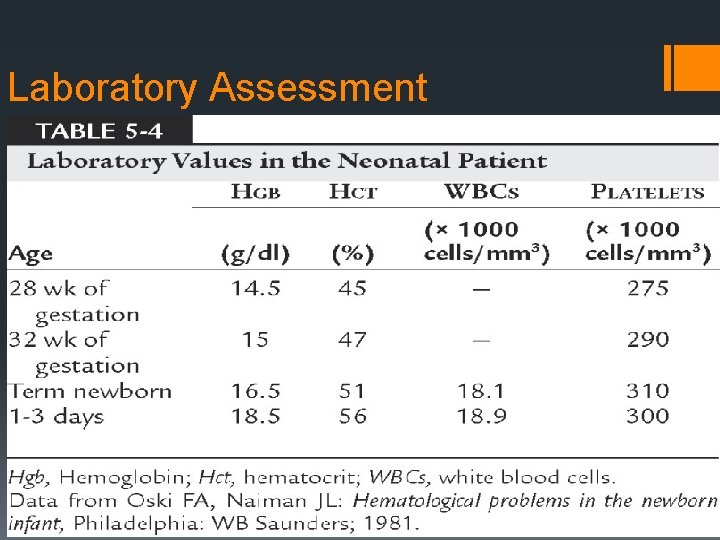
Laboratory Assessment
Laboratory Examination (cont. ) §Infection §Leukopenia (< 3, 500/mm 3) §Leukocytosis (> 25, 000/mm 3) §Platelets (<150, 000/mm 3) §Hemoglobin abnormalities §RBC (Rh) Isoimmunization §Hypoglycemia
Examination of the Pediatric Patient
Patient History §The history for a new patient can be divided into: §Chief complaint or primary concern §History of the present illness (HPI) §Past medical history (PMH) §Review of symptoms (ROS) §Family history (FH) §Social and environmental histories
Patient History (cont. ) §Chief complaint §Current signs and symptoms
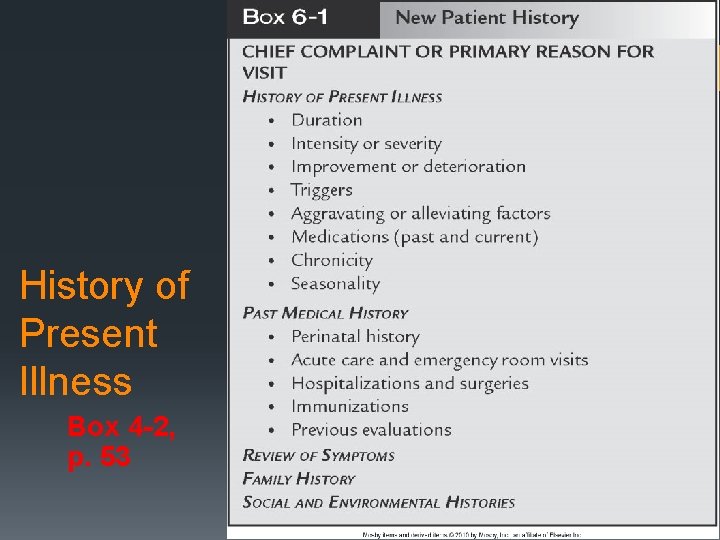
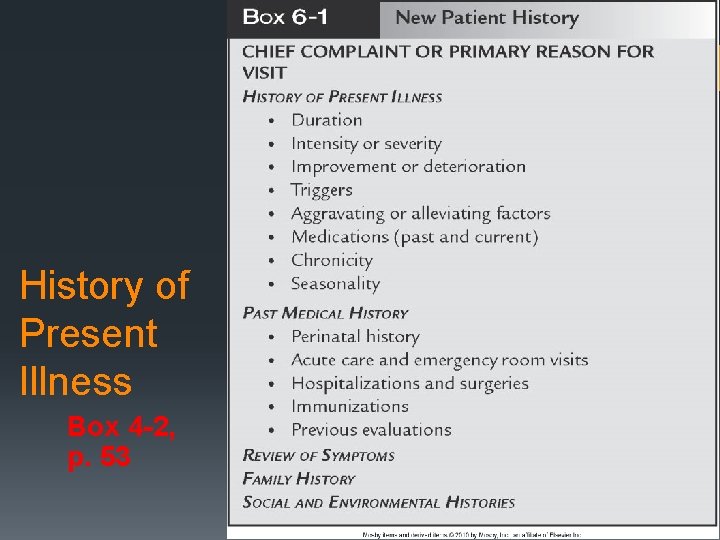
History of Present Illness Box 4 -2, p. 53
Past Medical History § Components of the PMH that may contribute to establishing a diagnosis: § History of prematurity § Birthweight § Need for and duration of oxygen therapy and/or assisted ventilation in the neonatal period § Previous emergency room visits or hospitalizations for respiratory disturbances (including ICU admissions and any need for assisted ventilation) § Previous surgeries § Immunization history
Family History §Important conditions §Biological parents §Siblings §Other close relatives
Social and Environmental History §Home life §Caregivers §School §Social participation §Exposures §Travel
Review of Symptoms §Symptoms not recognized with history. §Multiple body systems. §Pulmonary Examination §Non-pulmonary Examination §Laboratory Testing
Pulmonary Examination Inspection §Child in respiratory distress § Pulmonary: Tachypnea, breathlessness, head bobbing, grunting, nasal flaring, retractions. § Non-Pulmonary: Anxiety, fussiness, irritability and not able to recognize parents. §Crying child §Vital Signs § Respiratory rate assessment while sleeping §Chest abnormalities § Pectus carinatum and pectues excavatum §Abdominal paradox

Pulmonary Examination Palpation §Bronchial (rhonchal) and tactile fremitus §Position of trachea
Pulmonary Examination Percussion §More beneficial with older children than infants or neonates.
Pulmonary Examination Auscultation §Grunting §Stridor §Stertor §Wheezing §Monophonic vs Polyphonic
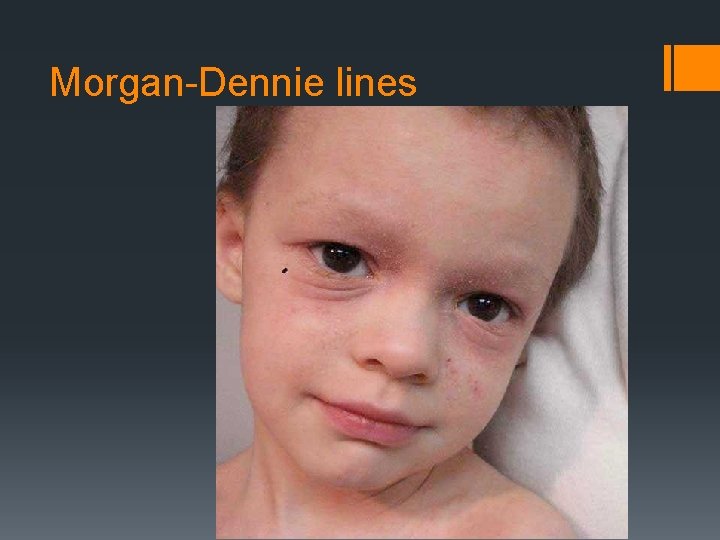
Non-Pulmonary Examination §General §Growth and developmental delay §Neurological abnormalities or cerebral palsy §Muscle weakness or atrophy §EENT §Signs of allergic disorders § Otitis media § Allergic shiners § Morgan-Denie Lines

Allergic Shiners
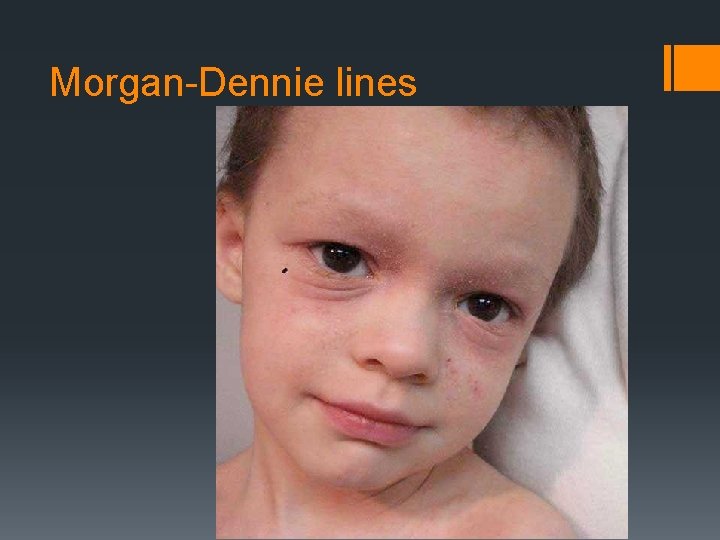
Morgan-Dennie lines
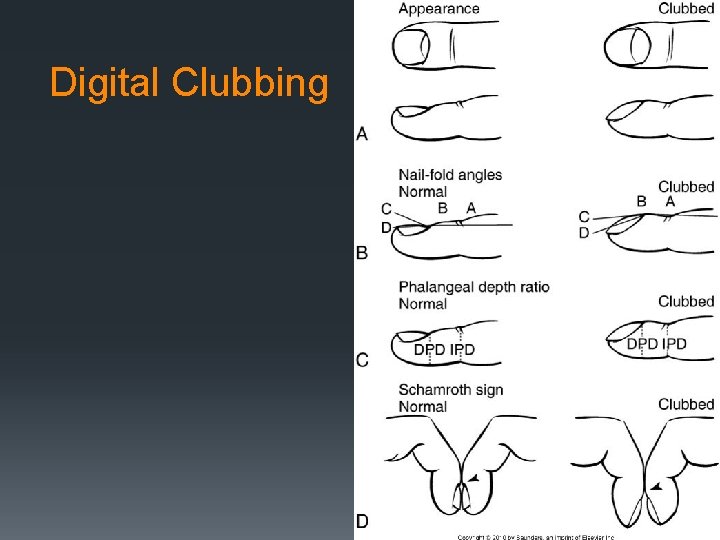
Non-Pulmonary Examination §Heart §Abnormal rhythms §Murmurs & gallops §Prominent 2 nd heart sound §Abdominal distention §Skin abnormalities §Extremities §Digital Clubbing
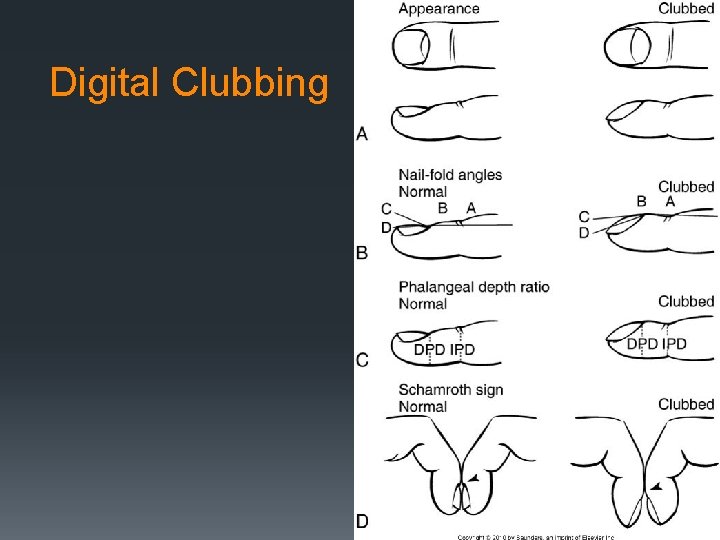
Digital Clubbing
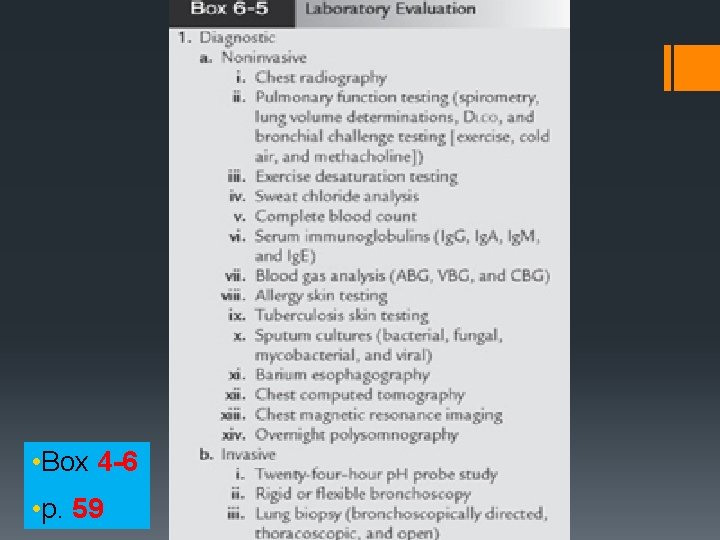
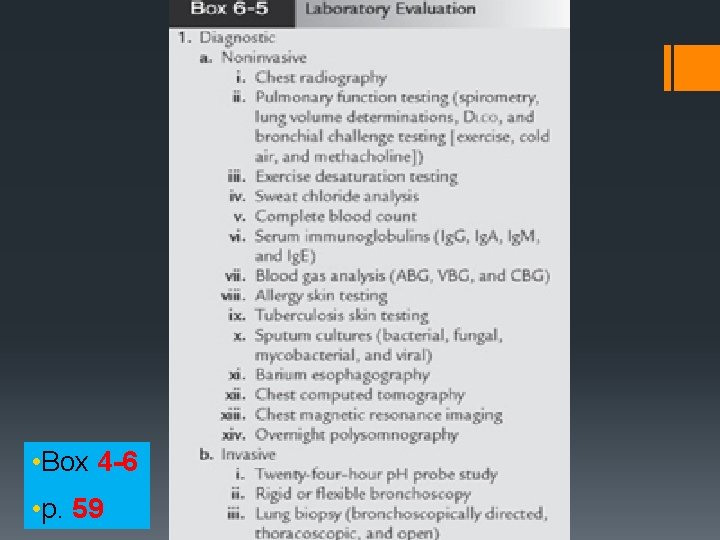
• Box 4 -6 • p. 59
 Neonatal jaundice physical examination
Neonatal jaundice physical examination Yorkshire neonatal network
Yorkshire neonatal network Vasculopatía lenticuloestriada definicion
Vasculopatía lenticuloestriada definicion Circulação fetal
Circulação fetal Triade neonatal
Triade neonatal Tamiz neonatal
Tamiz neonatal Ambiente termico neutro
Ambiente termico neutro Neonatal ölüm hızı
Neonatal ölüm hızı Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Riesgo de sepsis nanda
Riesgo de sepsis nanda Clasificacion de kramer ictericia
Clasificacion de kramer ictericia Underfive
Underfive Poliglobulia
Poliglobulia Formula para exanguinotransfusión
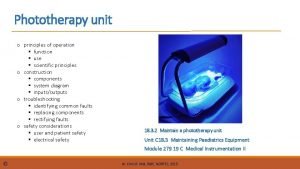
Formula para exanguinotransfusión Uses of phototherapy machine
Uses of phototherapy machine Parâmetros iniciais ventilação mecânica neonatal
Parâmetros iniciais ventilação mecânica neonatal Comfort b pain scale
Comfort b pain scale Halo cefalico
Halo cefalico Psychiatric nursing process
Psychiatric nursing process Suprasternal retraction
Suprasternal retraction Neonatarum
Neonatarum Neonatal sepsis
Neonatal sepsis Dope neonatal resuscitation
Dope neonatal resuscitation Management of neonatal jaundice pdf
Management of neonatal jaundice pdf Iap slides
Iap slides Apgar meaning
Apgar meaning Zonas de kramer ictericia neonatal
Zonas de kramer ictericia neonatal Niveles normales de bilirrubina en neonatos
Niveles normales de bilirrubina en neonatos Hipoglicemia neonatal
Hipoglicemia neonatal Escala kramer modificada
Escala kramer modificada Diagnostico de hiperbilirrubinemia neonatal
Diagnostico de hiperbilirrubinemia neonatal Zonas de kramer ictericia neonatal
Zonas de kramer ictericia neonatal Neonatal liver failure
Neonatal liver failure Valores de bilirrubina em rn
Valores de bilirrubina em rn Cuidados de enfermería en oxigenoterapia neonatal
Cuidados de enfermería en oxigenoterapia neonatal Circulação fetal
Circulação fetal Systolic ejection murmur left sternal border
Systolic ejection murmur left sternal border Hipernatremia neonatal
Hipernatremia neonatal Pacto pela redução da mortalidade materna e neonatal
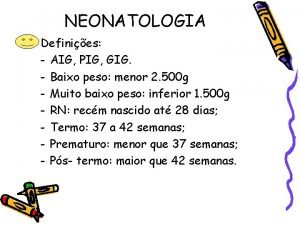
Pacto pela redução da mortalidade materna e neonatal Aig neonatologia
Aig neonatologia Neonatal alloimmün trombositopeni
Neonatal alloimmün trombositopeni Neonatal sepsis symptoms
Neonatal sepsis symptoms Neonatal sepsis nelson pediatrics
Neonatal sepsis nelson pediatrics Ictericia definicion
Ictericia definicion Neonatal progeria
Neonatal progeria Icterícia neonatal tratamento
Icterícia neonatal tratamento Hoja de balance hidrico en enfermeria
Hoja de balance hidrico en enfermeria Physiopathologie de l'ictère néonatal
Physiopathologie de l'ictère néonatal Neonatal cholestasis naspghan
Neonatal cholestasis naspghan Clasificacion de ictericia neonatal
Clasificacion de ictericia neonatal Jaundice level
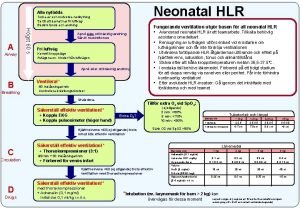
Jaundice level Neonatal hlr
Neonatal hlr Vasculopatia lenticulo estriada
Vasculopatia lenticulo estriada Reflejos en el período neonatal
Reflejos en el período neonatal Hepatomogaly
Hepatomogaly Tetanus
Tetanus