Neonatal seizures Clinical types Classification of neonatal seizures
- Slides: 21
Neonatal seizures
Clinical types (Classification) of neonatal seizures: 1. Focal clonic seizures: Consist of rhythmic twitching of muscle groups, particularly those of the extremities and face. They are often associated with localized structural lesions, infections and subarachnoid hemorrhage.
2. Multifocal clonic seizures: Are similar to focal clonic seizures but differing in that many muscle groups are involved, frequently simultaneously. 3. Tonic seizures: Are characterized by rigid posturing of the extremities and trunk, and sometimes associated with fixed deviation of the eyes.
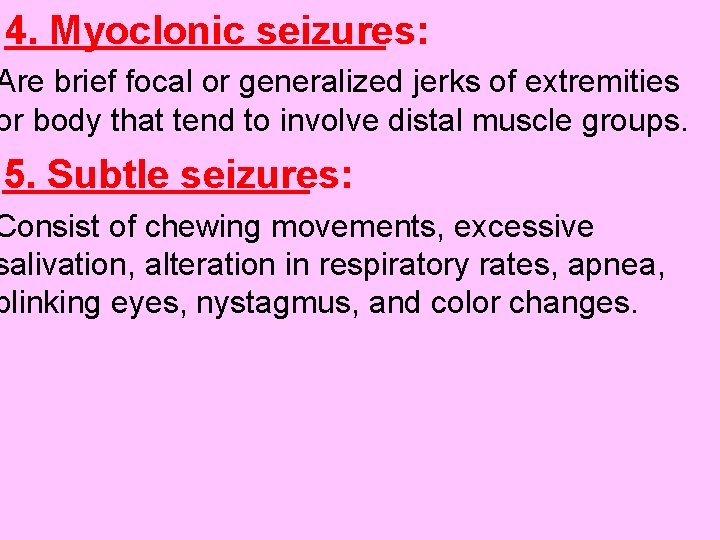
4. Myoclonic seizures: Are brief focal or generalized jerks of extremities or body that tend to involve distal muscle groups. 5. Subtle seizures: Consist of chewing movements, excessive salivation, alteration in respiratory rates, apnea, blinking eyes, nystagmus, and color changes.
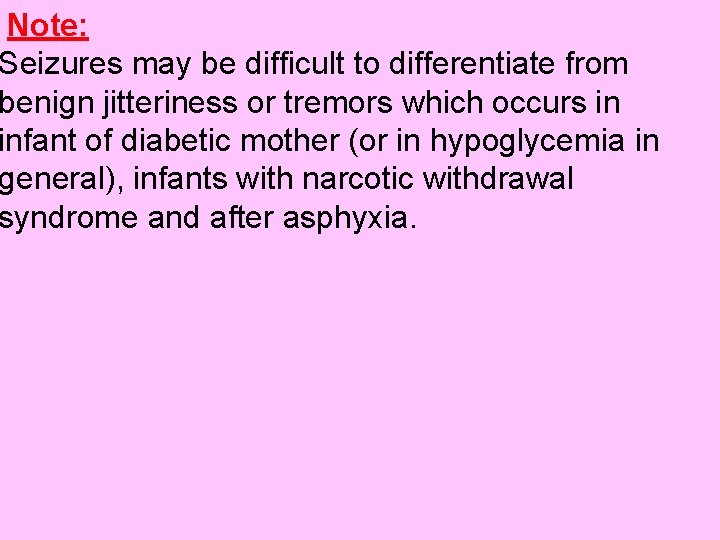
Note: Seizures may be difficult to differentiate from benign jitteriness or tremors which occurs in infant of diabetic mother (or in hypoglycemia in general), infants with narcotic withdrawal syndrome and after asphyxia.
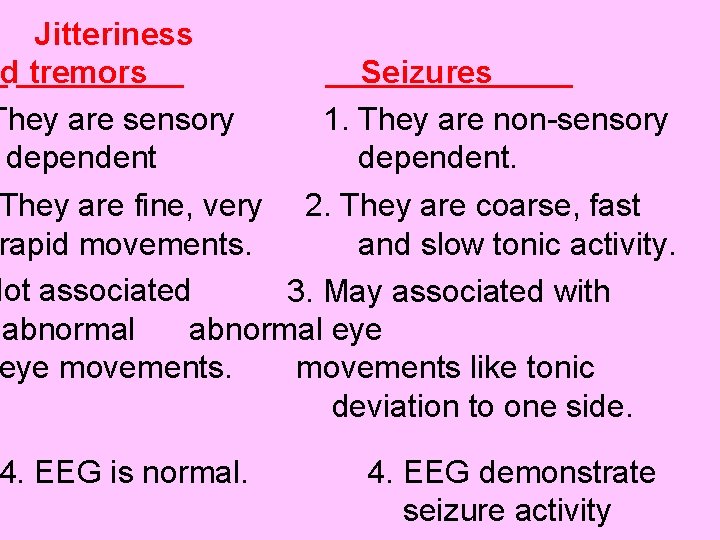
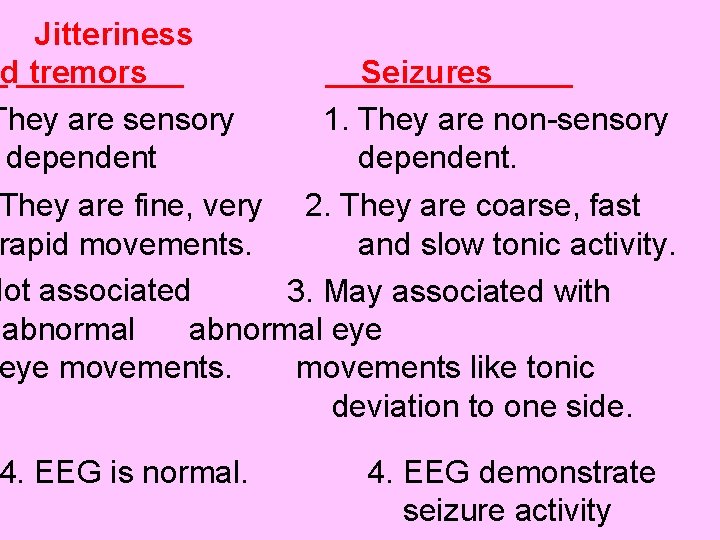
Jitteriness nd tremors They are sensory dependent Seizures 1. They are non-sensory dependent. They are fine, very 2. They are coarse, fast rapid movements. and slow tonic activity. Not associated 3. May associated with abnormal eye movements like tonic deviation to one side. 4. EEG is normal. 4. EEG demonstrate seizure activity
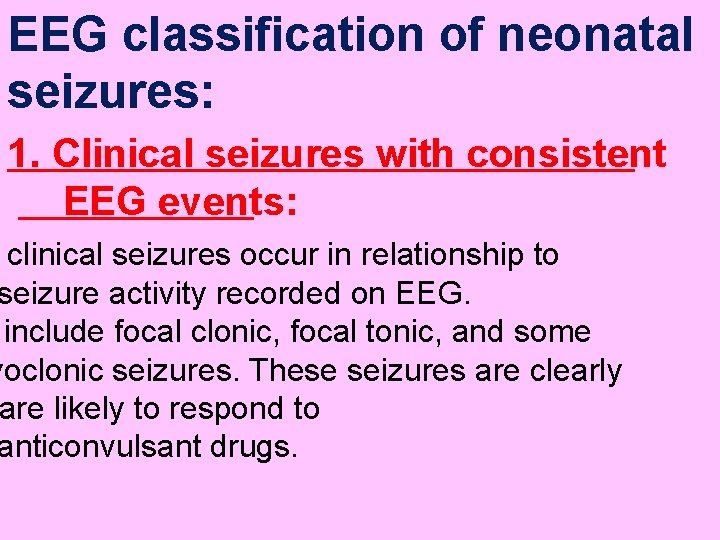
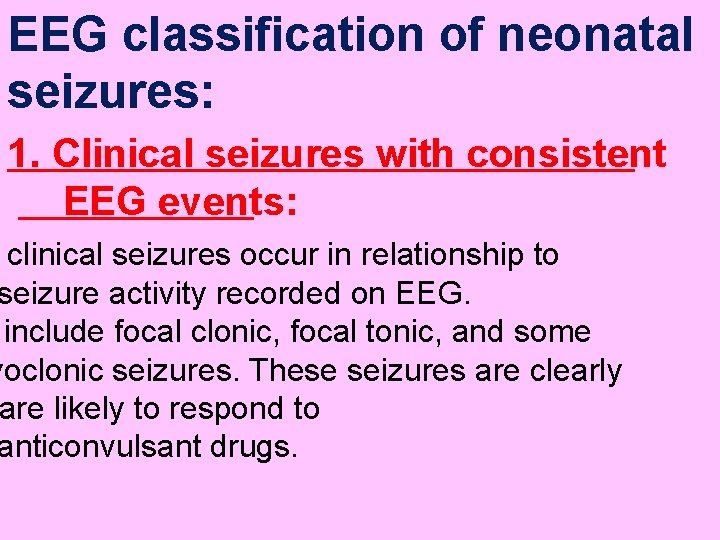
EEG classification of neonatal seizures: 1. Clinical seizures with consistent EEG events: clinical seizures occur in relationship to seizure activity recorded on EEG. include focal clonic, focal tonic, and some yoclonic seizures. These seizures are clearly are likely to respond to anticonvulsant drugs.
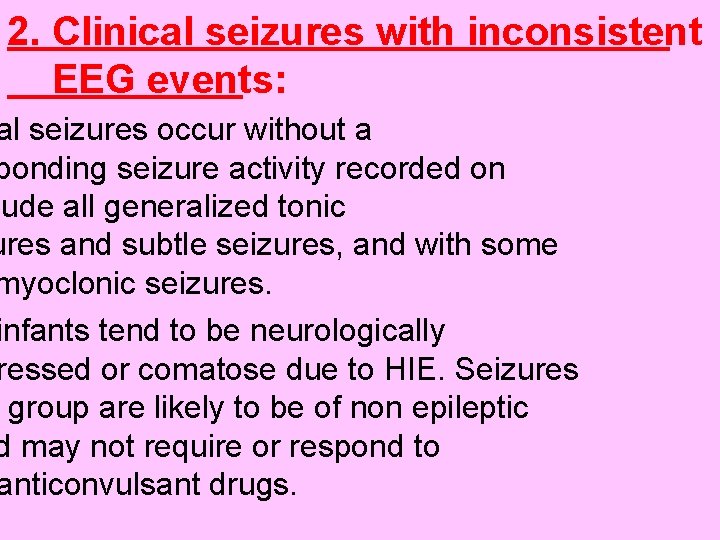
2. Clinical seizures with inconsistent EEG events: al seizures occur without a ponding seizure activity recorded on lude all generalized tonic ures and subtle seizures, and with some myoclonic seizures. infants tend to be neurologically ressed or comatose due to HIE. Seizures group are likely to be of non epileptic d may not require or respond to anticonvulsant drugs.
3. Electric seizures without clinical seizures: aracterized by mark abnormal EEG ut clinical seizures. Its may develop in s who are not on onvulsant drugs or electric seizure may n patient with focal tonic or clonic thout clinical seizures after introduction of anticonvulsant drugs.
Etiology of neonatal seizures: ypoxic – ischemic encephalopathy (HIE) tasphyxial seizure : it’s a common e of seizures in full term infants, usually s 12 -24 hr after onset of birth asphyxia en are refractory to usual doses of anticonvulsant drugs. tasphyxial seizures also may be due to c abnormalities associated with onatal asphyxia, such as hypoglycemia and ypocalcaemia.
aventricular hemorrhage (IVH): it’s a n cause of seizures in premature and often occurs between 1 and 3 e. Seizures due to IVH are sociated with bulging fontanel, hemorrhagic spinal fluid (CSF), anemia, lethargy and coma. Hypoglycemia: Seizures occurs when blood cose levels decline to the lowest postnatal 1 -2 hr of age or 24 -48 hr after poor onal intake) and its well responding to lucose administration.
ocalcaemia and hypomagnesemia: veloped in high risk infants and respond well to calcium and/or magnesium therapy. 5. Infections: like meningitis, encephalitis or TORCH infections. onatremia (S. sodium<135 m. Eq/l) or Hypernatremia (S. sodium >150 m. Eq/l. al brain abnormalities: e. g. lissencephaly and schizencephaly.
nborn error of metabolism: e. g. urea cycle cts, maple syrup urine disease (MSUD), and non ketotic hyperglycemia. izure is associated with lethargy, acidosis, and family history of infants death. jection of local anesthetic into fetal scalp g labor cause seizure in delivery room sociated with transient bradycardia and fixed ed pupils and sometime with respiratory depression required ventilation.
Pyridoxine dependency: its rare autosomal order characterized by eralized clonic seizures shortly after birth ns of fetal distress in utero. These zures are resistant to usual anticonvulsant drugs. Treatment: I. V. pyridoxine 100 -200 mg (bolus ch abruptly stop seizures and rmalize EEG, then lifelong supplementation of oral pyridoxine 10 mg/day. ntreated patients have persistent seizures and sever mental retardation.
gn familial neonatal seizures: an osomal dominant condition started on 2 nd day of life with seizures frequency of ay. Patients are normal between seizures which stop in 1 -6 mo of age. Drug withdrawal seizures: Its may occur in room or may delayed for several eks due to prolonged excretion of the drug he neonate. These drugs are barbiturates, azepines, heroin and methadone h are taken by the mother. Infants have rritability and lethargy with myoclonus or clonic seizures
Investigations of neonatal seizures: od sample for glucose, sodium, calcium, magnesium, and bilirubin levels. 2. Blood, urine, or CSF cultures if infection is suspected.
mbar puncture for measurements of CSF , protein, and glucose and for culture. Its ated in all neonates with seizure, unless olic cause is obvious such as hypoglycemia or hypocalcaemia. CSF findings may indicate meningitis (bacterial viral), encephalitis or intracranial hemorrhage CSF) and its should be done after the signs of raised intracranial pressure.
tic Resonance Imaging (MRI), or d Tomography(CT) or cerebral asonography for diagnosis of suspicion of H or structural brain abnormalities or in case of unexplained seizures. 5. EEG. 6. Tests for inborn error of metabolism.
Treatment of neonatal seizure: pecific treatment for underlying causes gitis, hypoglycemia, a, hypomagnesemia, atremia, and vitamin B 6 (pyridoxine) deficiency or dependency.
2. Anticonvulsant therapy: Phenobarbital: 20 -30 mg/kg I. V. (loading dose) owed by maintenance dose of 5 mg/kg/24 hr in 2 divided doses. ntoin: 10 -20 mg/kg I. V. (loading dose) owed by maintenance dose of 5 mg/kg/24 hr 2 divided doses. m: 0. 1 -0. 3 mg/kg followed by rbital or phyntoin maintenance herapy.
Prognosis of neonatal seizures: Its depend mainly on the primary cause and severity of the seizures. In case of hypoglycemic infants of diabetic mothers or hypocalcaemia associated with excessive phosphate feeding, the prognosis is excellent. Neonates with intractable seizures due to sever HIE or structural brain abnormalities usually does not respond to anticonvulsant drugs with high risk of status epilepticus and early death.
 Febrile convulsion
Febrile convulsion Non epileptic seizures
Non epileptic seizures Pediatric seizures
Pediatric seizures Lorna myers pnes
Lorna myers pnes Tremors and seizures
Tremors and seizures Basic mechanisms underlying seizures and epilepsy
Basic mechanisms underlying seizures and epilepsy Psychomotor seizures
Psychomotor seizures Psychomotor seizures
Psychomotor seizures Hemorrhagic irregular tissue fragments
Hemorrhagic irregular tissue fragments Nursing management of encephalitis
Nursing management of encephalitis Seizures
Seizures Tonic-clonic seizures
Tonic-clonic seizures Myoclonic vs tonic clonic seizure
Myoclonic vs tonic clonic seizure What to do if someone has a seizure
What to do if someone has a seizure Simple partial seizures vs complex
Simple partial seizures vs complex Simple partial seizures vs complex
Simple partial seizures vs complex Types of clinical refraction
Types of clinical refraction Certificate iv in clinical classification nsw
Certificate iv in clinical classification nsw Refraction definition
Refraction definition Yorkshire and humber neonatal network
Yorkshire and humber neonatal network Lenticulo estriado
Lenticulo estriado Circulação neonatal
Circulação neonatal