COPD Attila Somfay Dept Pulmonology University of Szeged








- Slides: 55

COPD Attila Somfay Dept. Pulmonology, University of Szeged, Deszk, Hungary
Chronic obstructive bronchitis and emphysema chronic obstructive airway disease (COAD, COLD) ( chronic obstructive pulmonary disease ) COPD
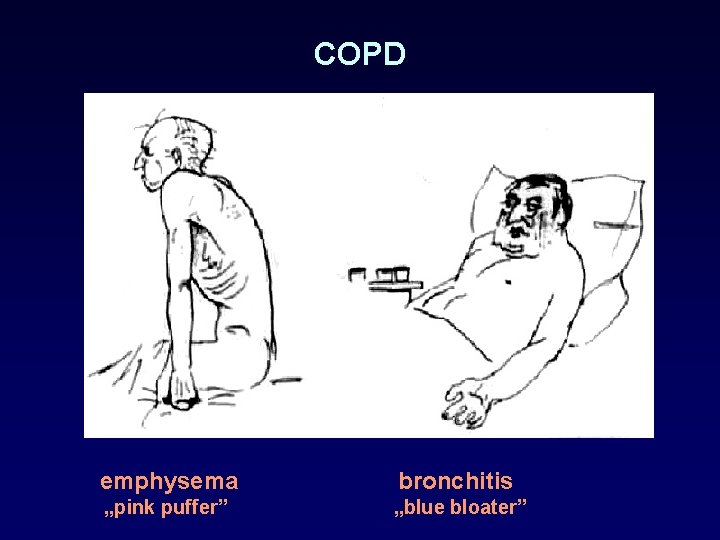
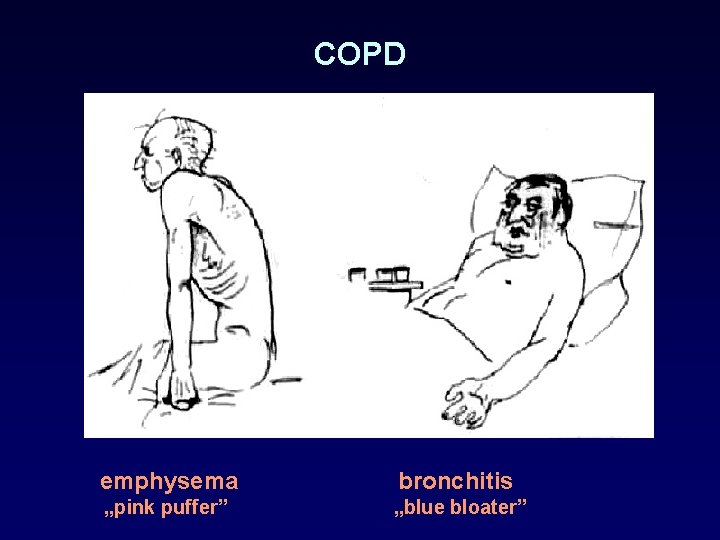
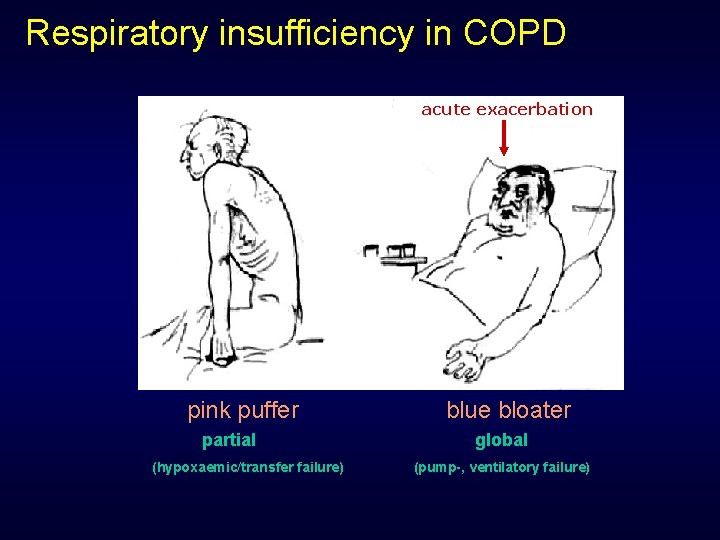
COPD emphysema bronchitis „pink puffer” „blue bloater”
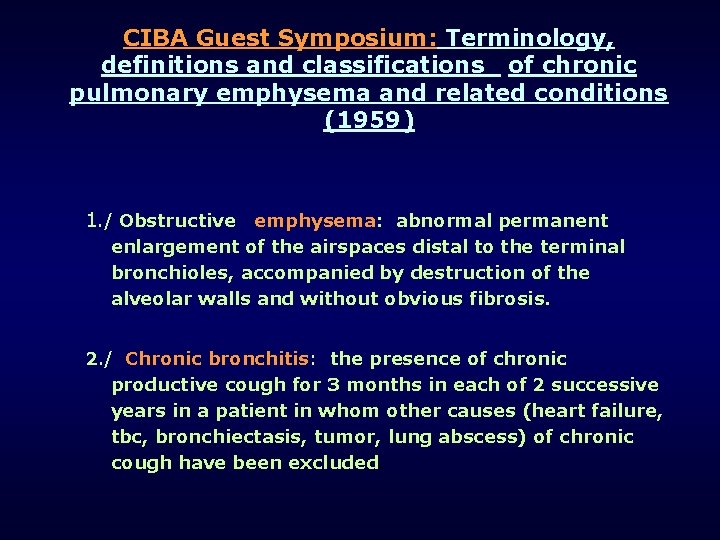
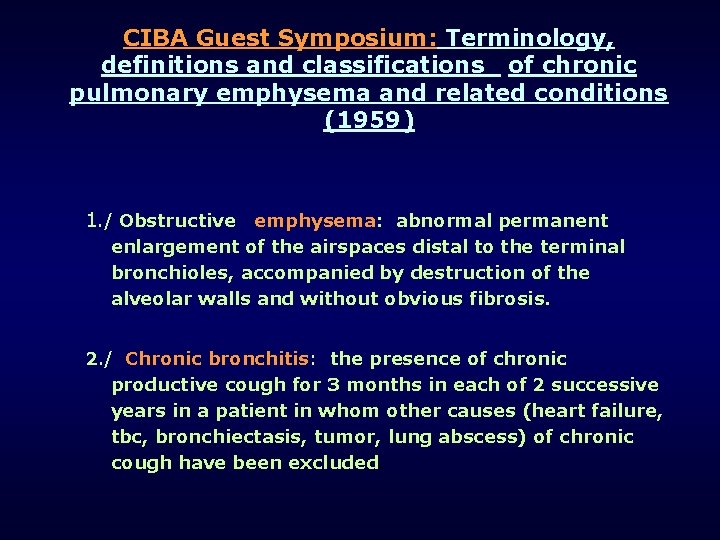
CIBA Guest Symposium: Terminology, definitions and classifications of chronic pulmonary emphysema and related conditions (1959) 1. / Obstructive emphysema: abnormal permanent enlargement of the airspaces distal to the terminal bronchioles, accompanied by destruction of the alveolar walls and without obvious fibrosis. 2. / Chronic bronchitis: the presence of chronic productive cough for 3 months in each of 2 successive years in a patient in whom other causes (heart failure, tbc, bronchiectasis, tumor, lung abscess) of chronic cough have been excluded.
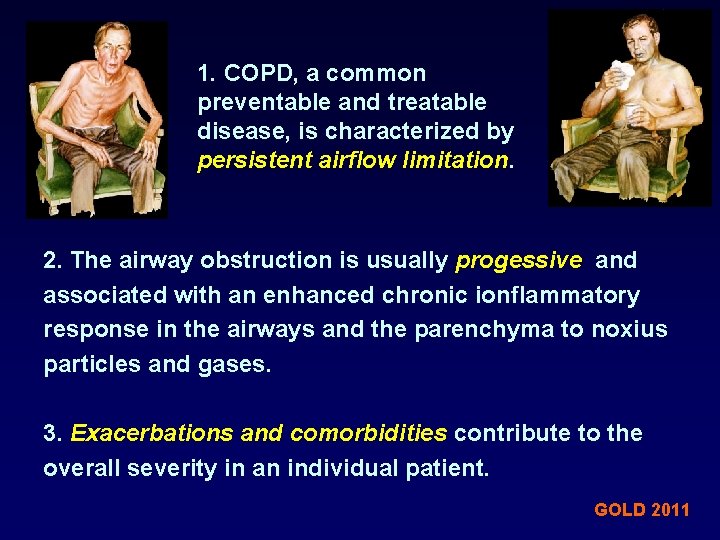
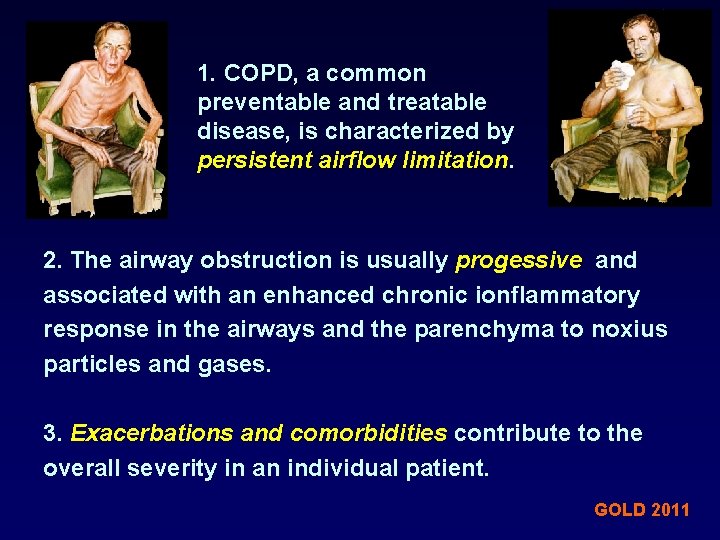
1. COPD, a common preventable and treatable disease, is characterized by persistent airflow limitation. 2. The airway obstruction is usually progessive and associated with an enhanced chronic ionflammatory response in the airways and the parenchyma to noxius particles and gases. 3. Exacerbations and comorbidities contribute to the overall severity in an individual patient. GOLD 2011



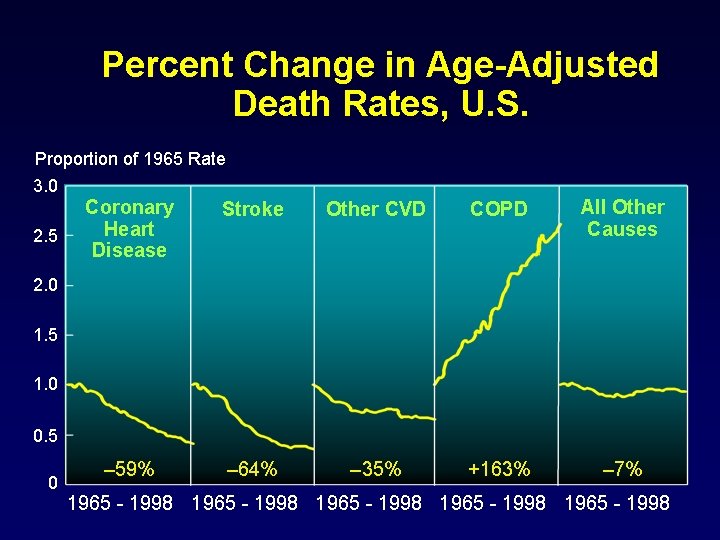
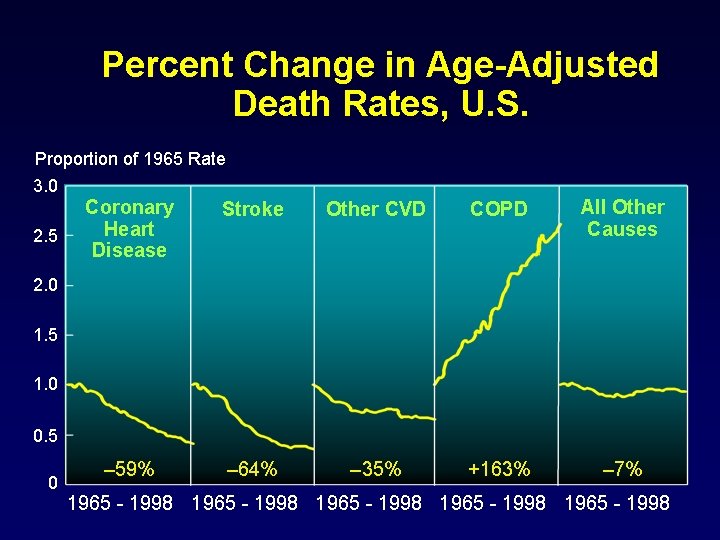
Percent Change in Age-Adjusted Death Rates, U. S. Proportion of 1965 Rate 3. 0 2. 5 Coronary Heart Disease Stroke Other CVD COPD All Other Causes – 59% – 64% – 35% +163% – 7% 2. 0 1. 5 1. 0 0. 5 0 1965 - 1998 1965 - 1998
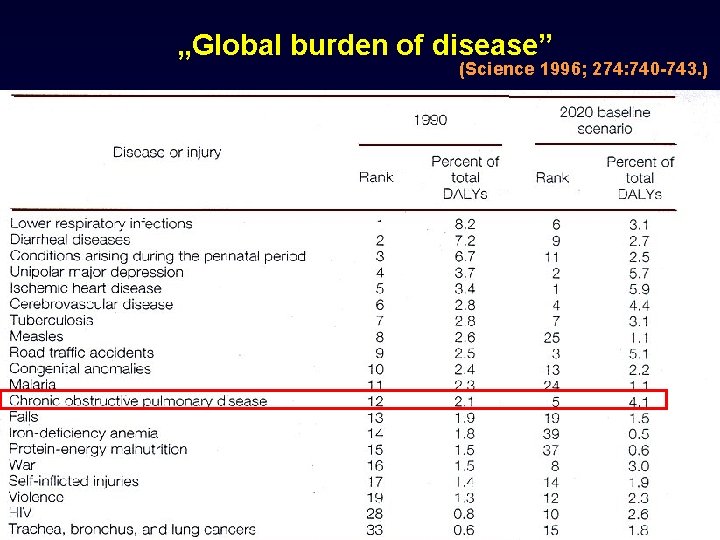
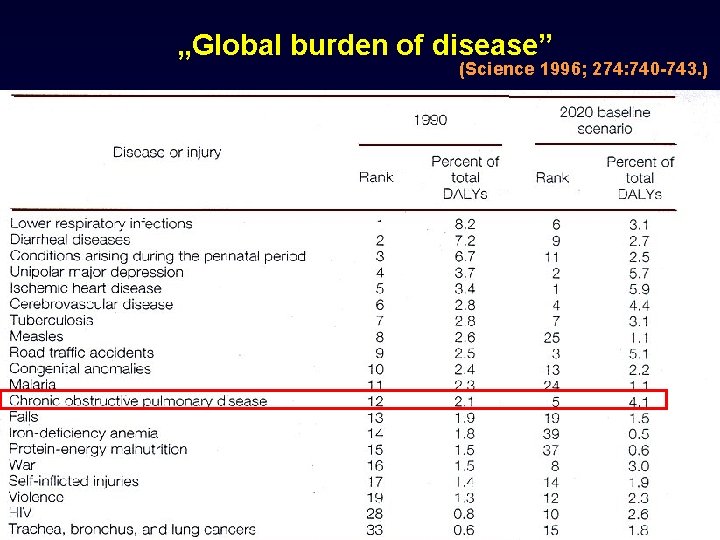
„Global burden of disease” (Science 1996; 274: 740 -743. )
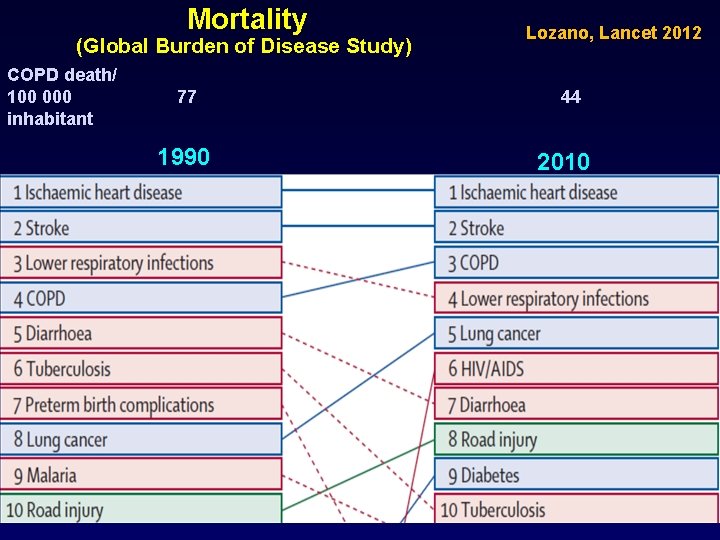
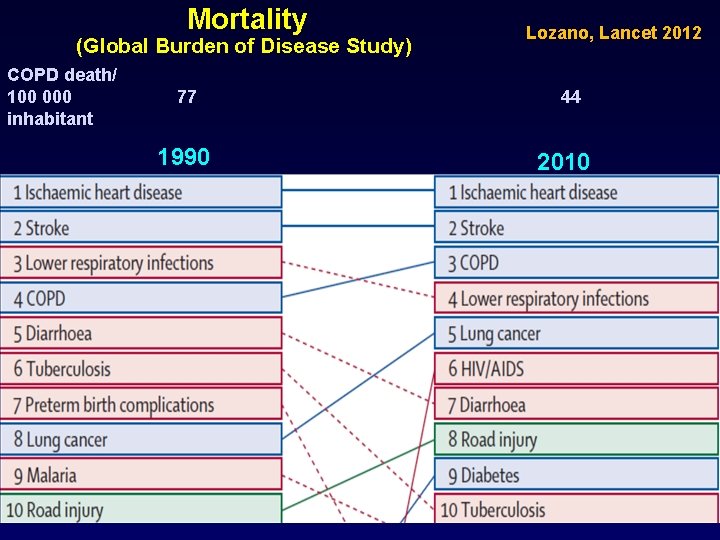
Mortality (Global Burden of Disease Study) COPD death/ 100 000 inhabitant 77 1990 Lozano, Lancet 2012 44 2010
Epidemiology 4 -7% of adult population, 9 -10 % for those over 40 Prevalence expected to rise 3 x in 10 years. By 2020, it becomes the 3 rd most frequent cause of death
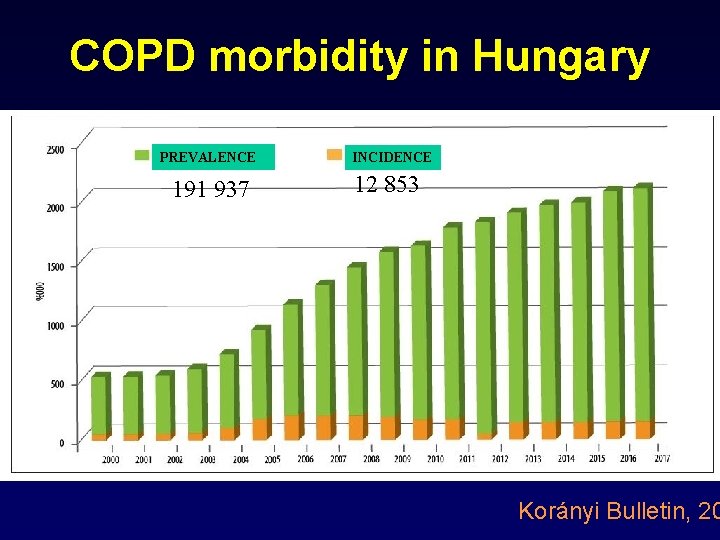
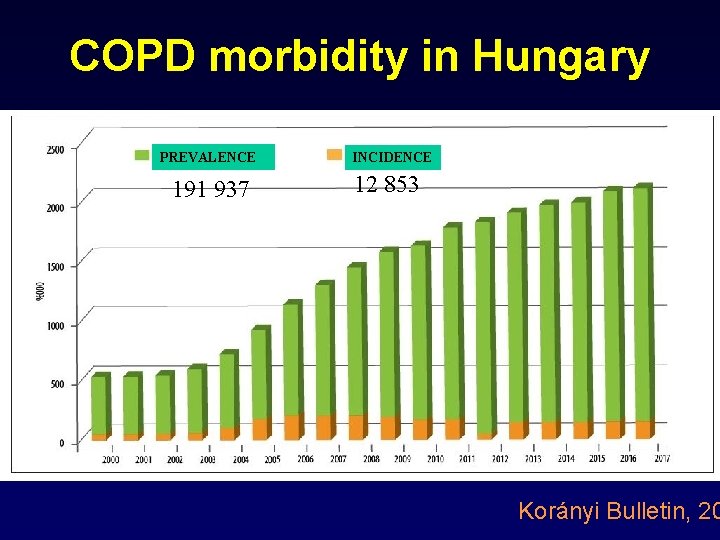
COPD morbidity in Hungary PREVALENCE 191 937 INCIDENCE 12 853 Korányi Bulletin, 20
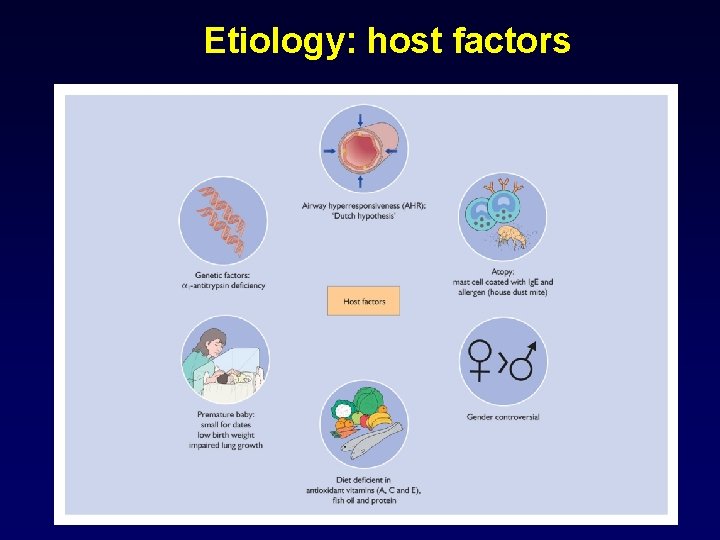
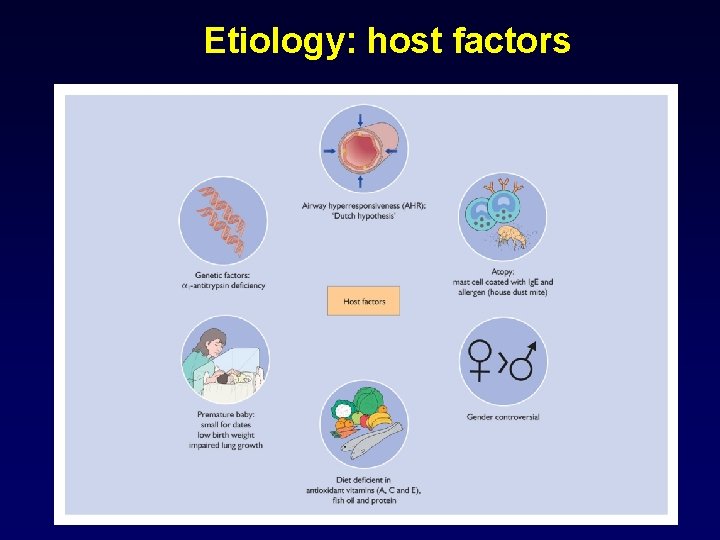
Etiology: host factors

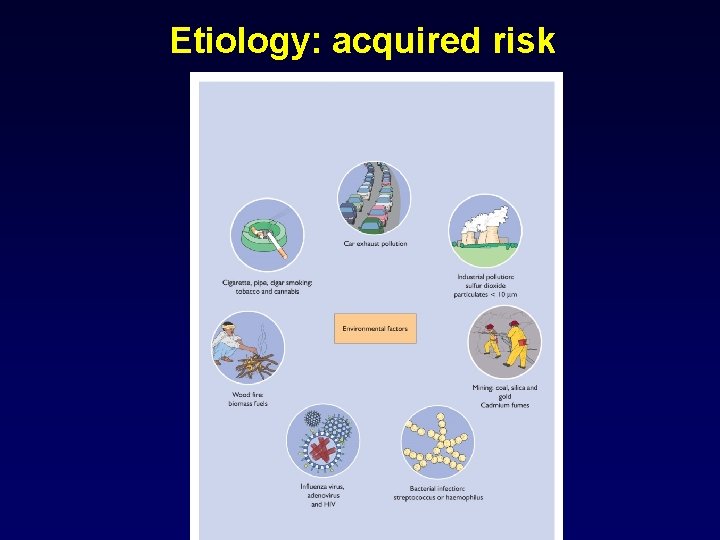
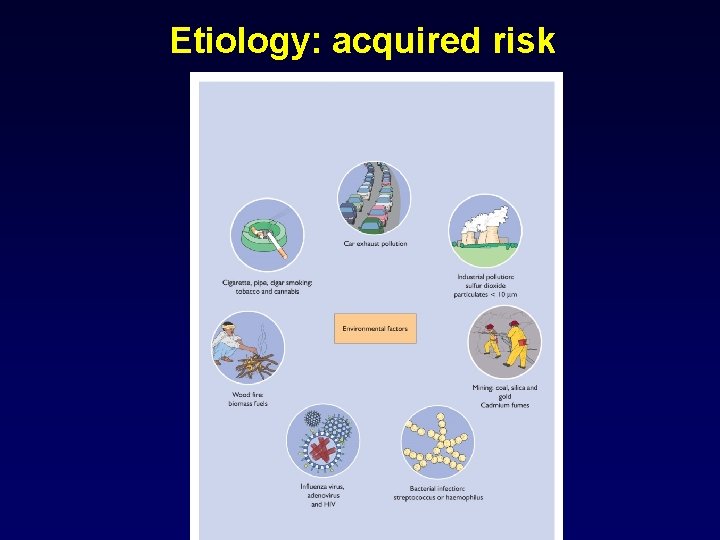
Etiology: acquired risk
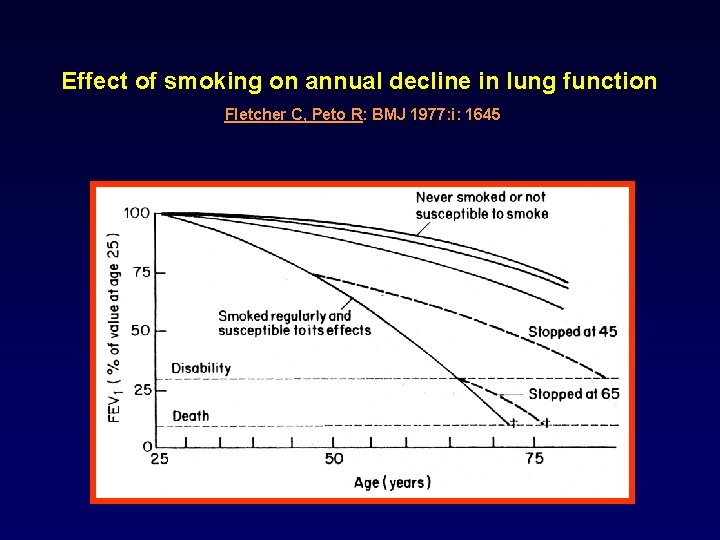
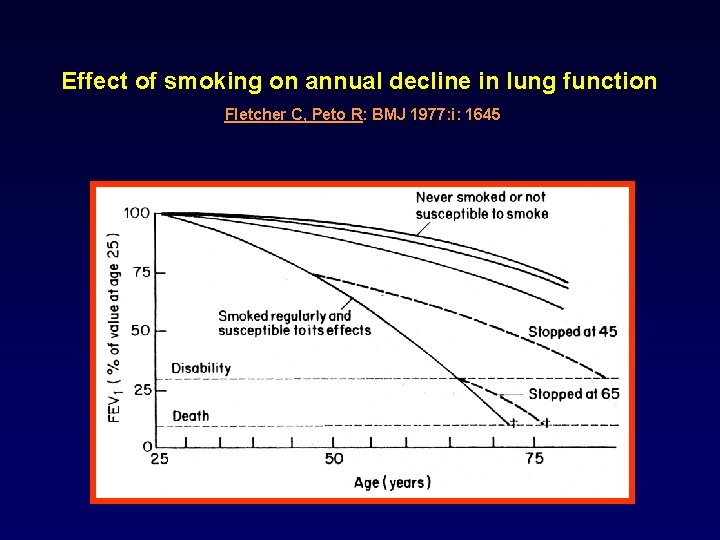
Effect of smoking on annual decline in lung function Fletcher C, Peto R: BMJ 1977: i: 1645

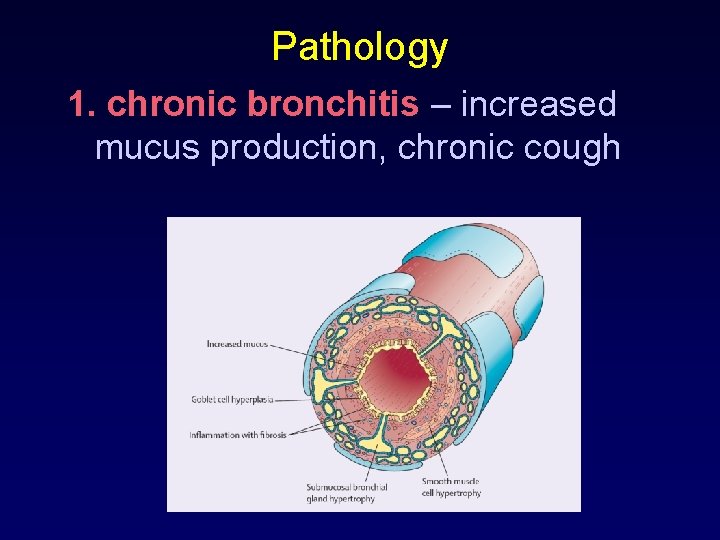
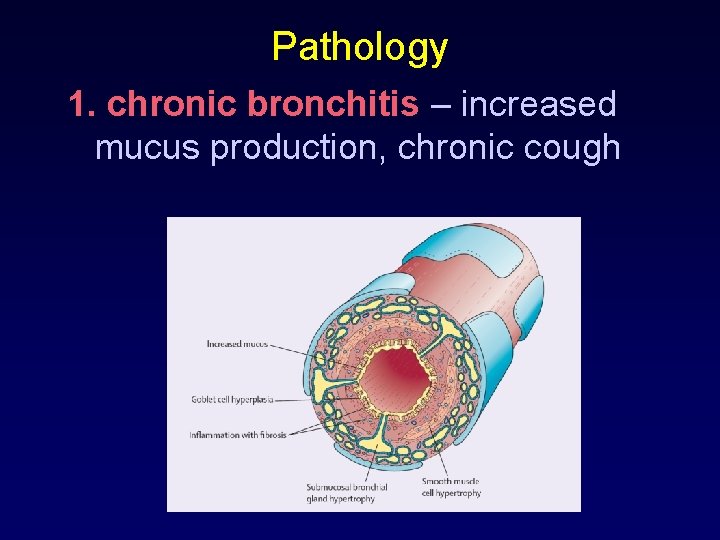
Pathology 1. chronic bronchitis – increased mucus production, chronic cough
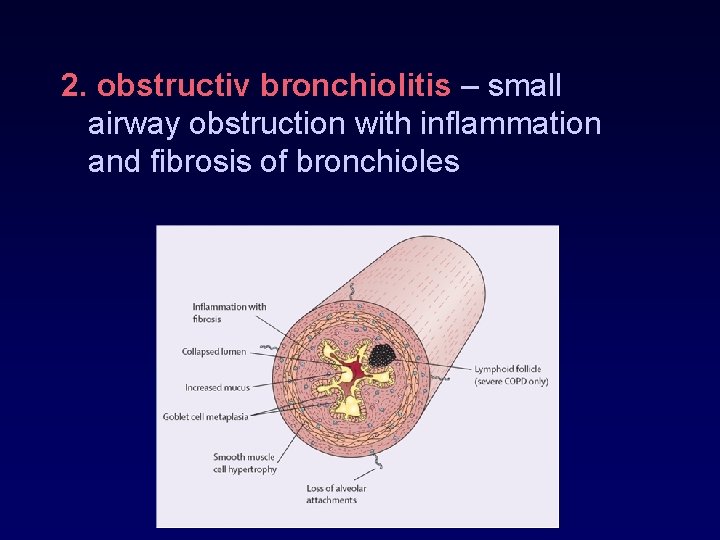
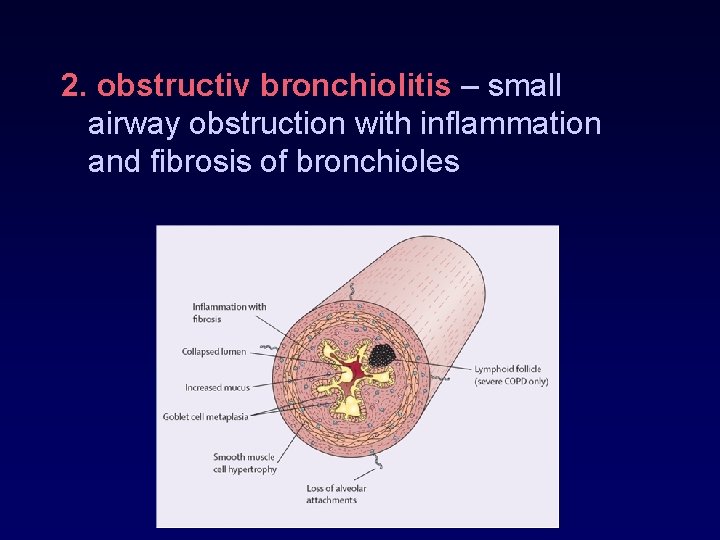
2. obstructiv bronchiolitis – small airway obstruction with inflammation and fibrosis of bronchioles
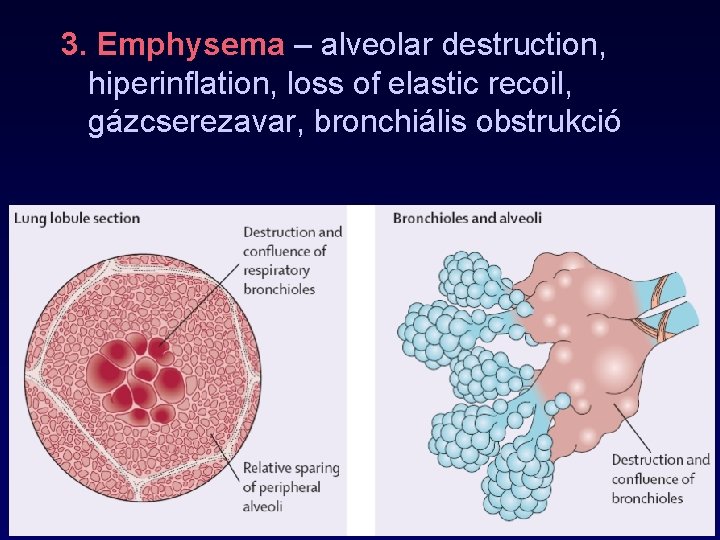
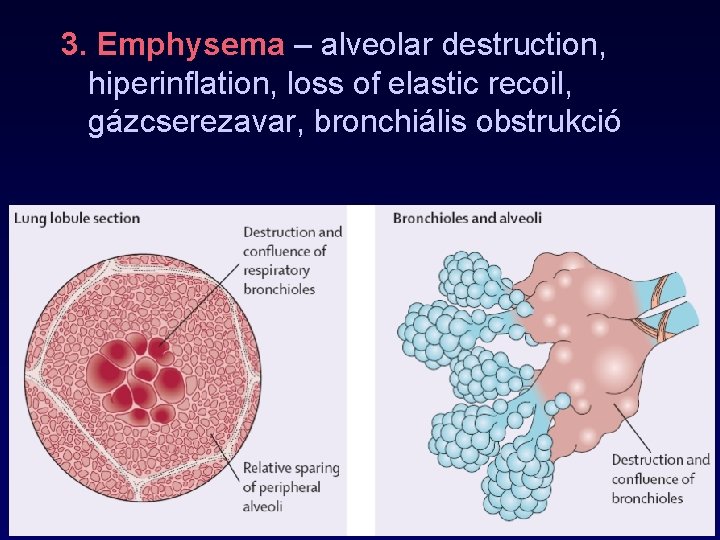
3. Emphysema – alveolar destruction, hiperinflation, loss of elastic recoil, gázcserezavar, bronchiális obstrukció
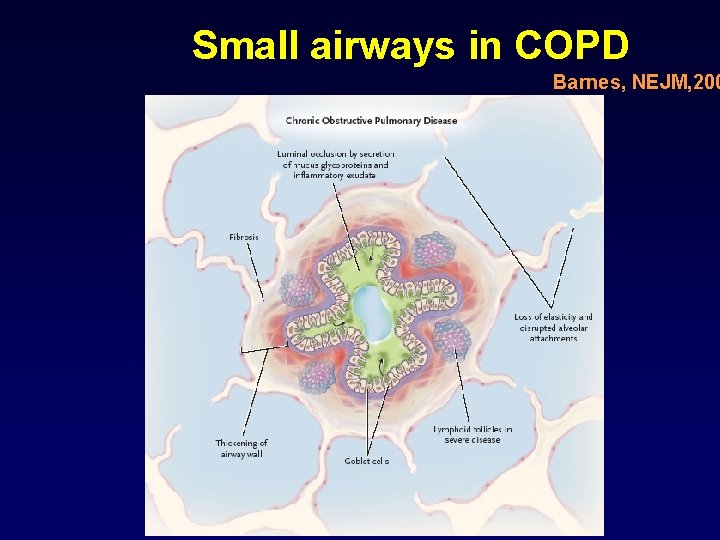
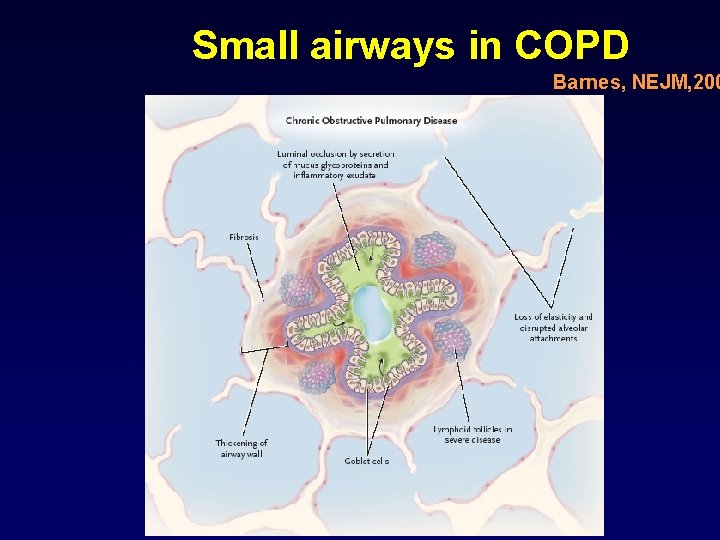
Small airways in COPD Barnes, NEJM, 200
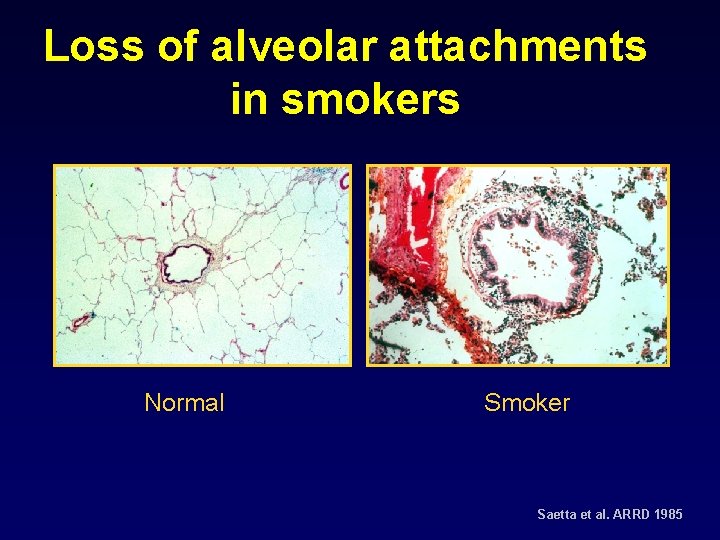
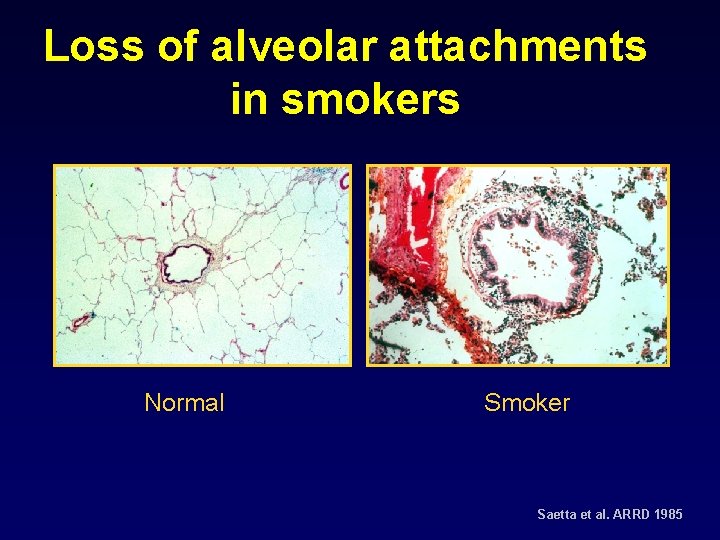
Loss of alveolar attachments in smokers Normal Smoker Saetta et al. ARRD 1985
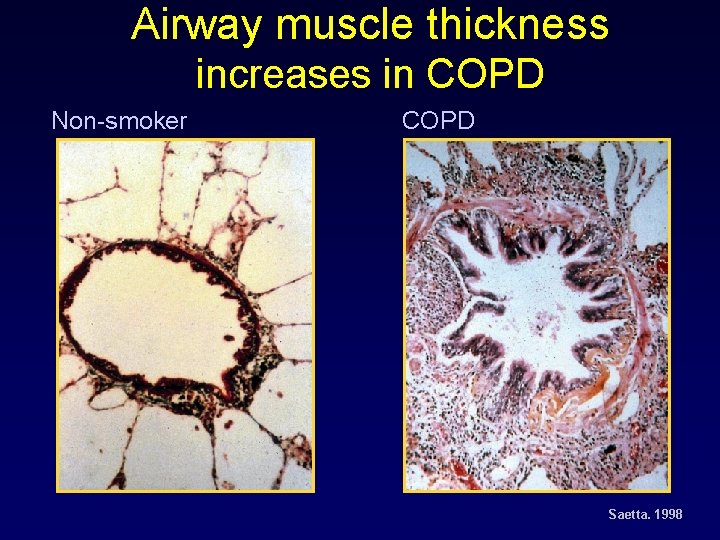
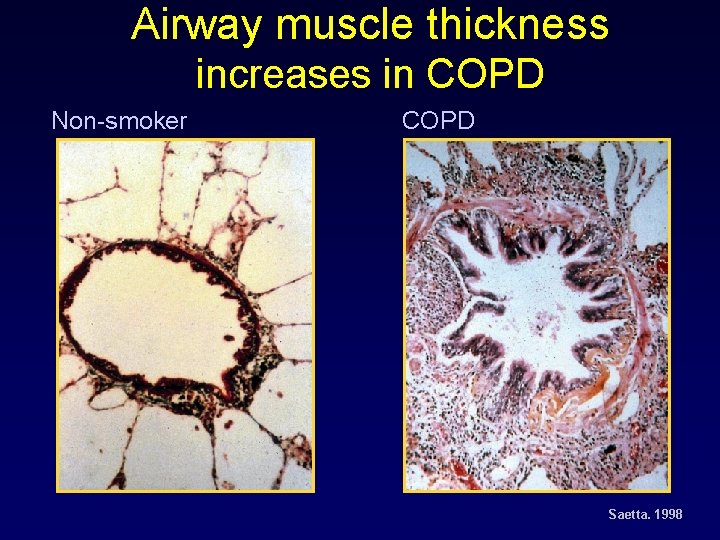
Airway muscle thickness increases in COPD Non-smoker COPD Saetta. 1998
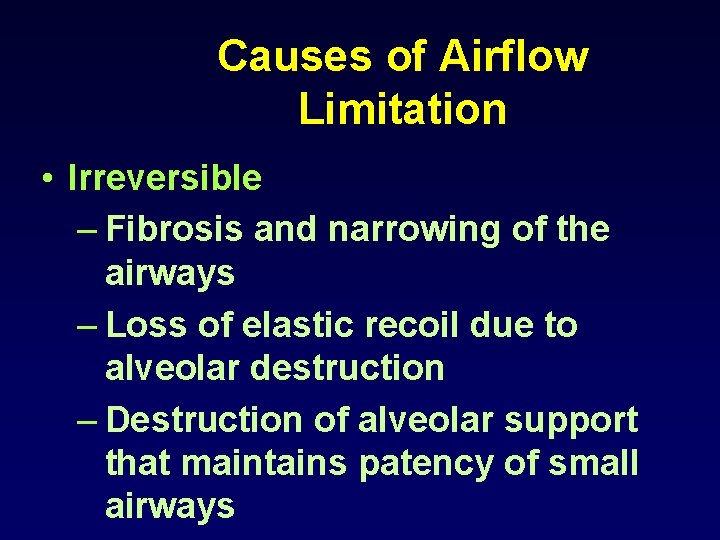
Causes of Airflow Limitation • Irreversible – Fibrosis and narrowing of the airways – Loss of elastic recoil due to alveolar destruction – Destruction of alveolar support that maintains patency of small airways
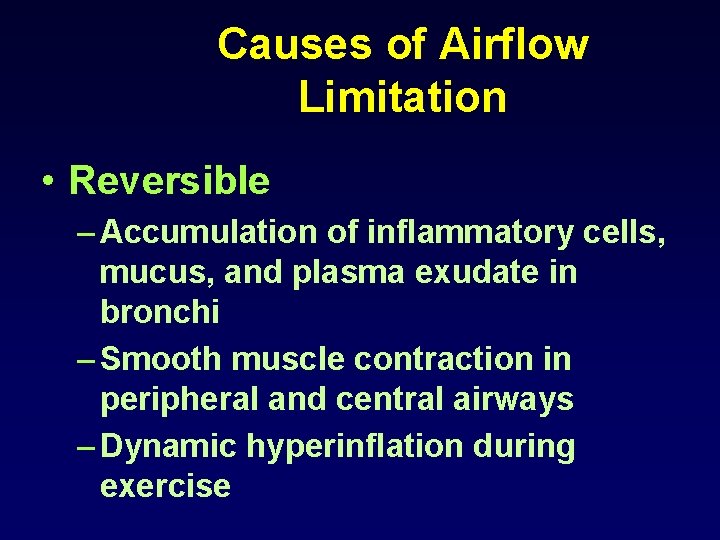
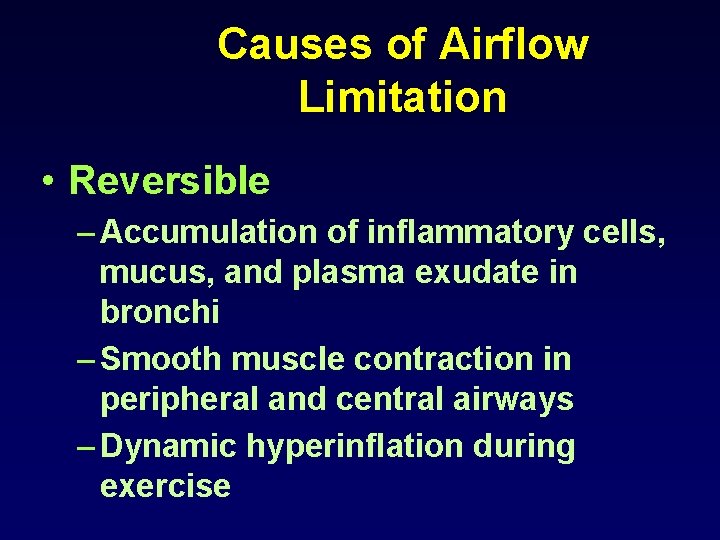
Causes of Airflow Limitation • Reversible – Accumulation of inflammatory cells, mucus, and plasma exudate in bronchi – Smooth muscle contraction in peripheral and central airways – Dynamic hyperinflation during exercise
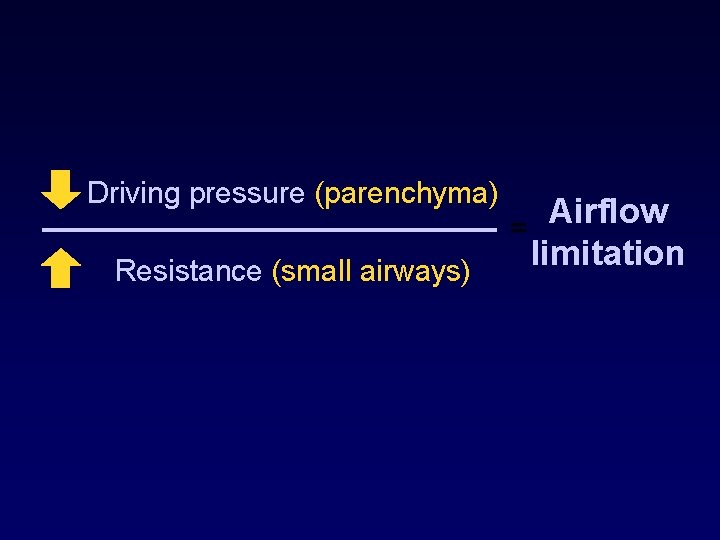
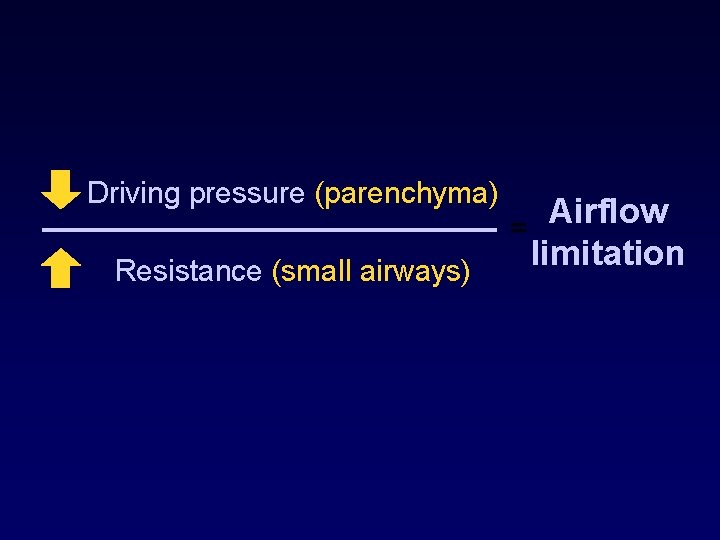
Driving pressure (parenchyma) Resistance (small airways) Airflow = limitation
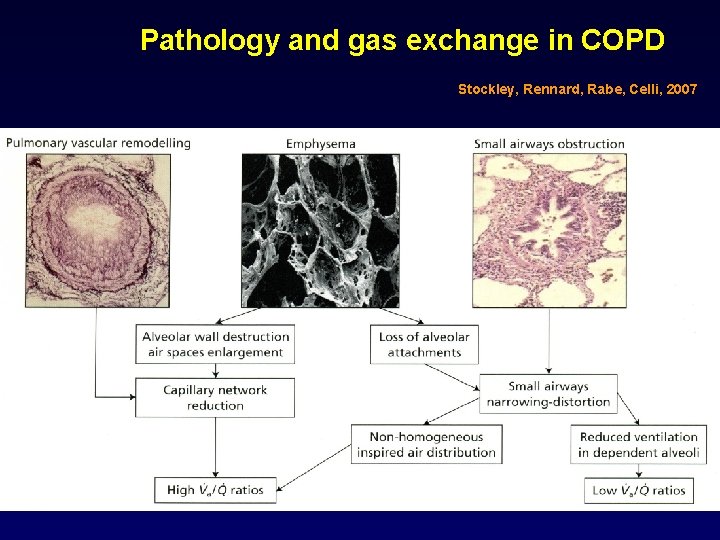
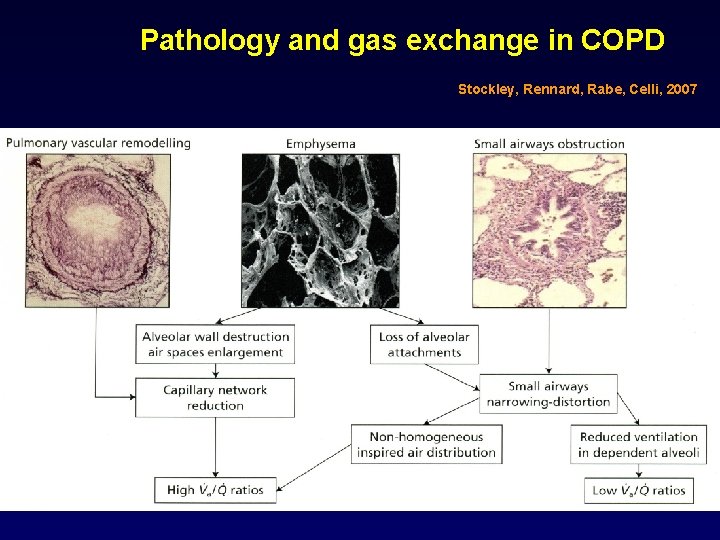
Pathology and gas exchange in COPD Stockley, Rennard, Rabe, Celli, 2007
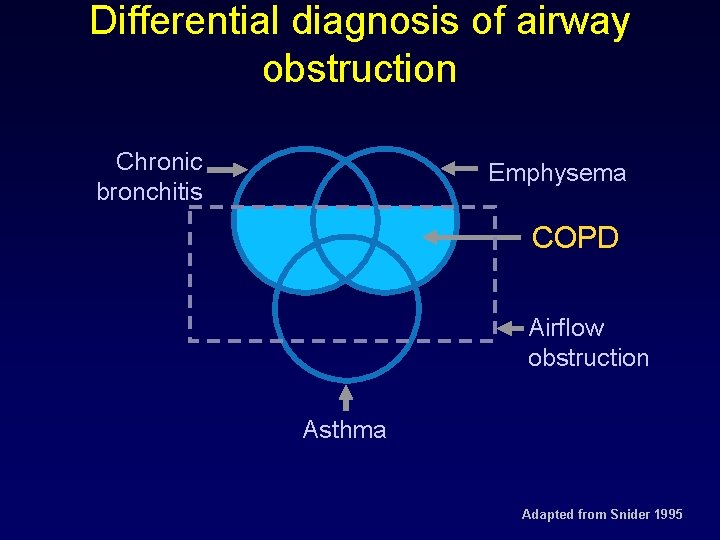
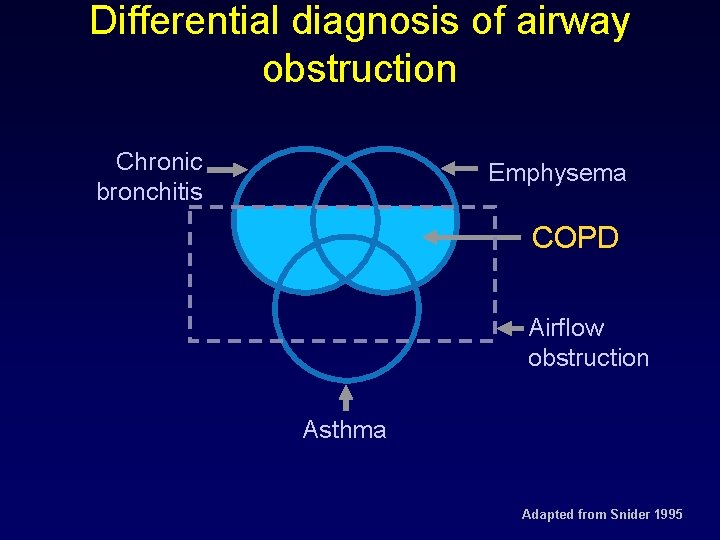
Differential diagnosis of airway obstruction Chronic bronchitis Emphysema COPD Airflow obstruction Asthma Adapted from Snider 1995
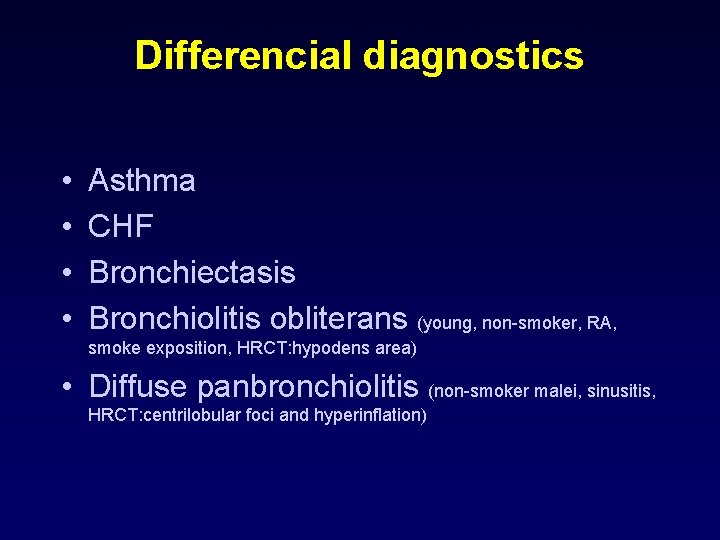
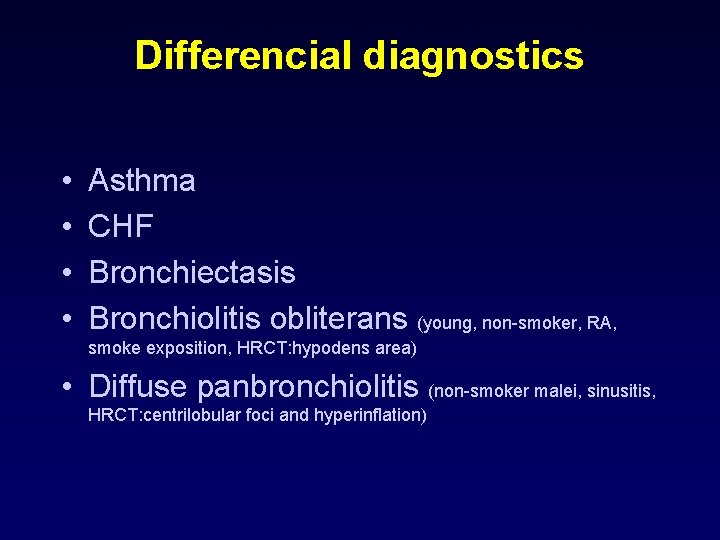
Differencial diagnostics • • Asthma CHF Bronchiectasis Bronchiolitis obliterans (young, non-smoker, RA, smoke exposition, HRCT: hypodens area) • Diffuse panbronchiolitis (non-smoker malei, sinusitis, HRCT: centrilobular foci and hyperinflation)
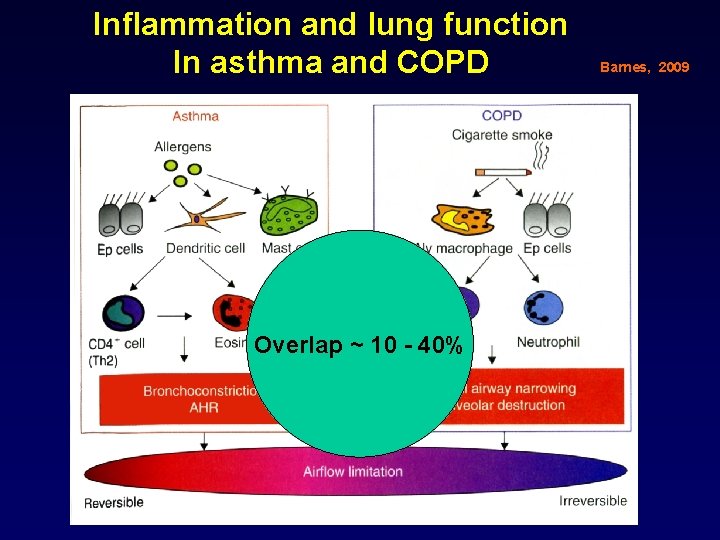
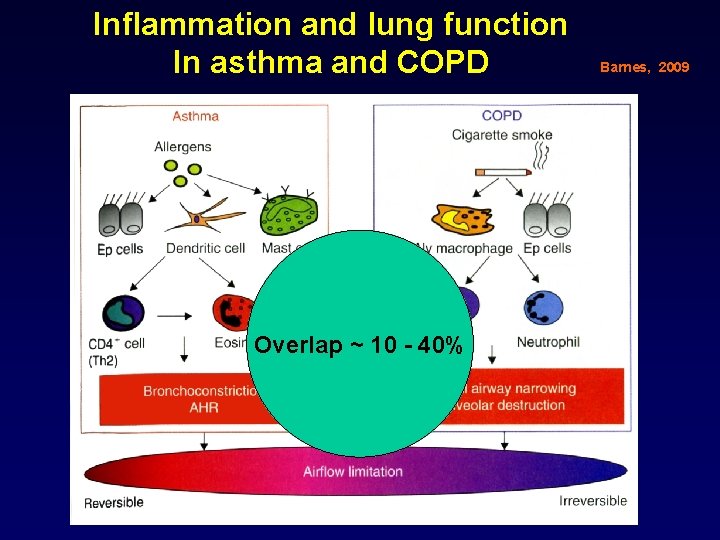
Inflammation and lung function In asthma and COPD Overlap ~ 10 - 40% Barnes, 2009
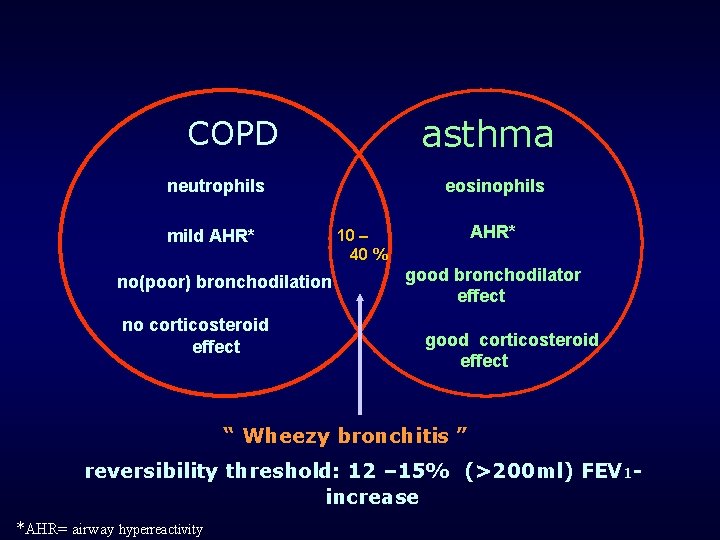
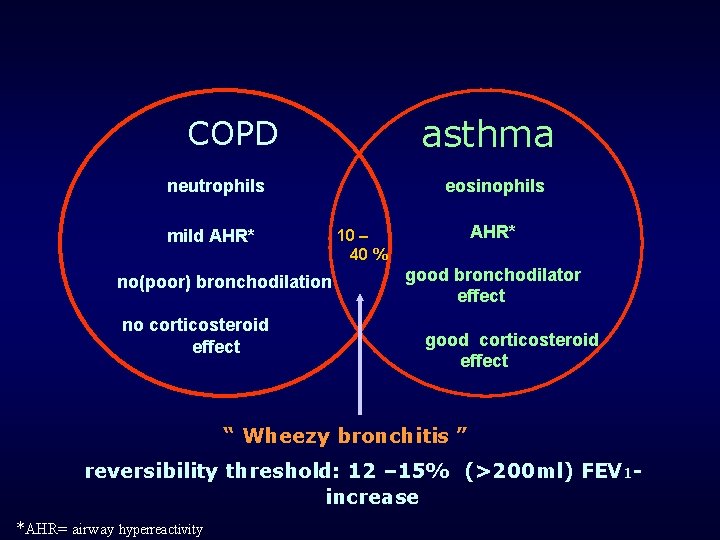
asthma COPD neutrophils mild AHR* no(poor) bronchodilation no corticosteroid effect eosinophils AHR* 10 – 40 % good bronchodilator effect good corticosteroid effect “ Wheezy bronchitis ” reversibility threshold: 12 – 15% (>200 ml) FEV 1 increase *AHR= airway hyperreactivity
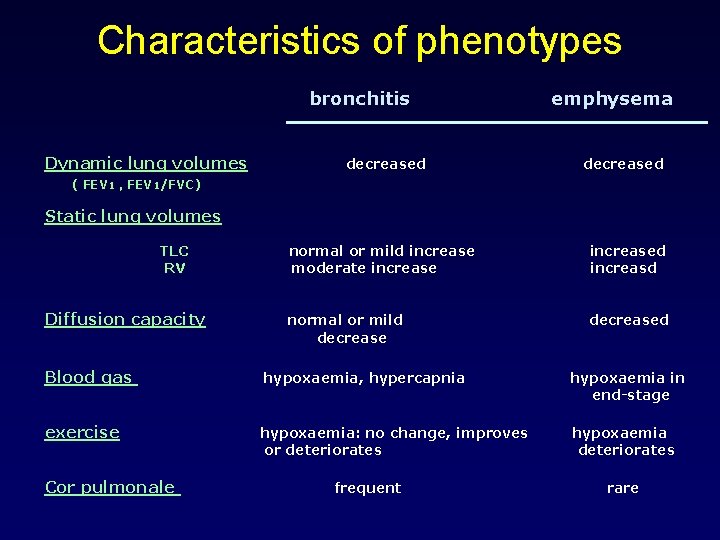
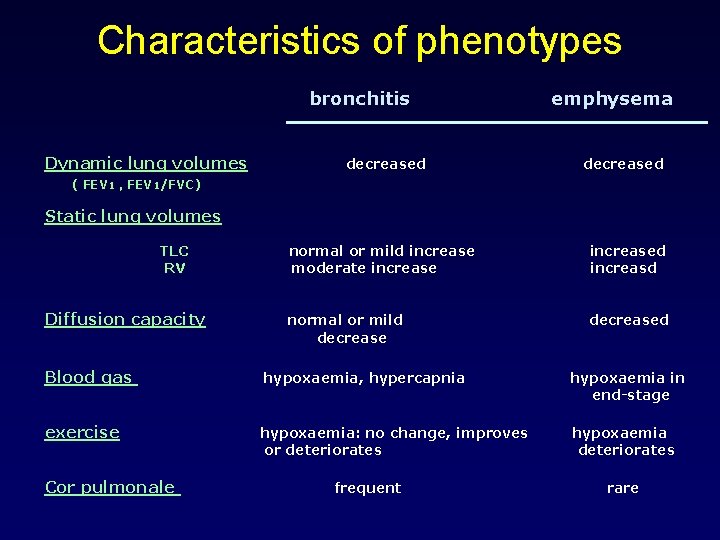
Characteristics of phenotypes bronchitis Dynamic lung volumes decreased emphysema decreased ( FEV 1 , FEV 1/FVC) Static lung volumes TLC RV Diffusion capacity normal or mild increase moderate increased increasd normal or mild decreased Blood gas hypoxaemia, hypercapnia hypoxaemia in end-stage exercise hypoxaemia: no change, improves or deteriorates hypoxaemia deteriorates Cor pulmonale frequent rare
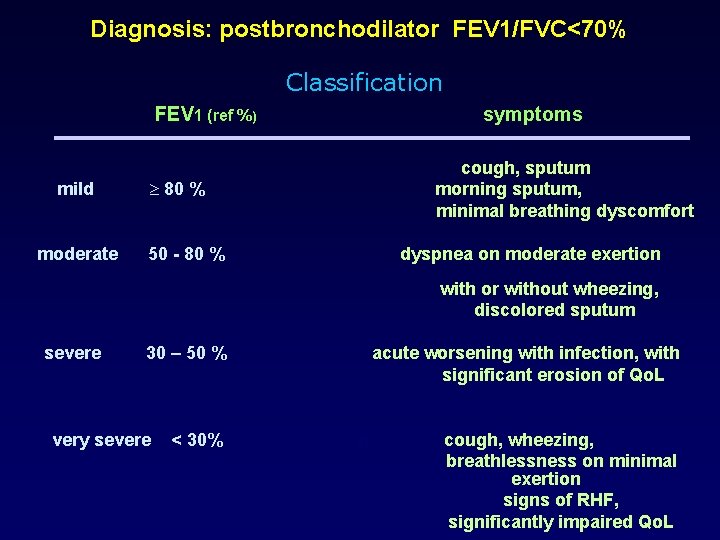
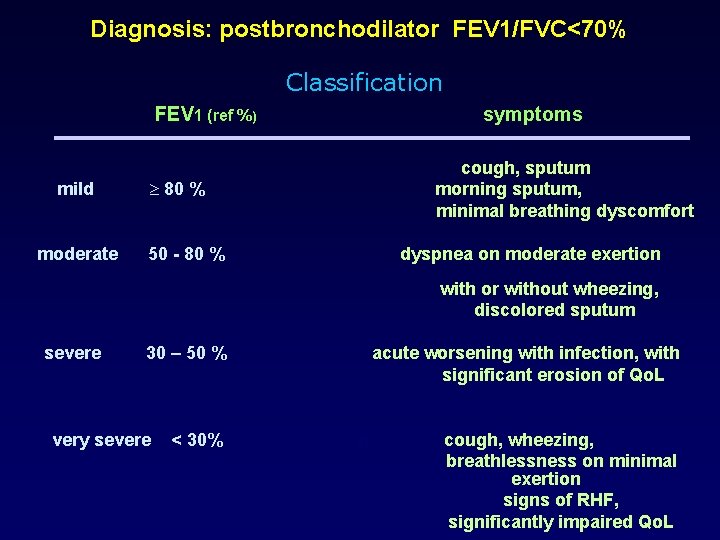
Diagnosis: postbronchodilator FEV 1/FVC<70% Classification FEV 1 (ref %) mild moderate symptoms cough, sputum morning sputum, minimal breathing dyscomfort 80 % 50 - 80 % dyspnea on moderate exertion with or without wheezing, discolored sputum severe 30 – 50 % very severe < 30% acute worsening with infection, with significant erosion of Qo. L n cough, wheezing, breathlessness on minimal exertion signs of RHF, significantly impaired Qo. L
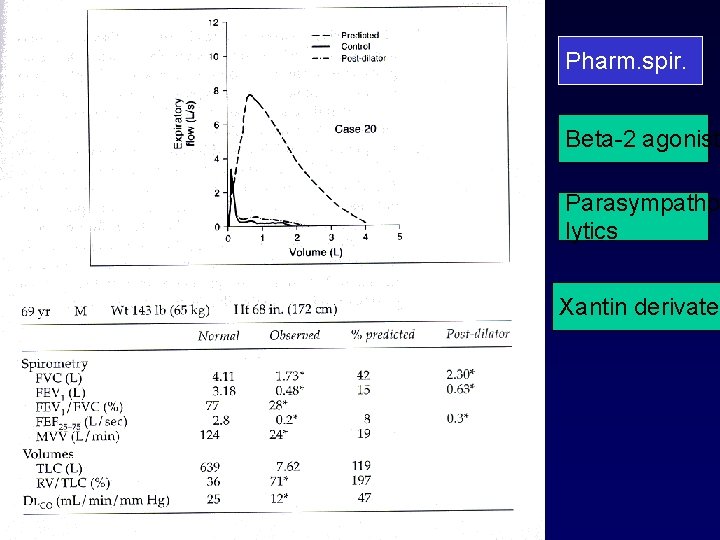
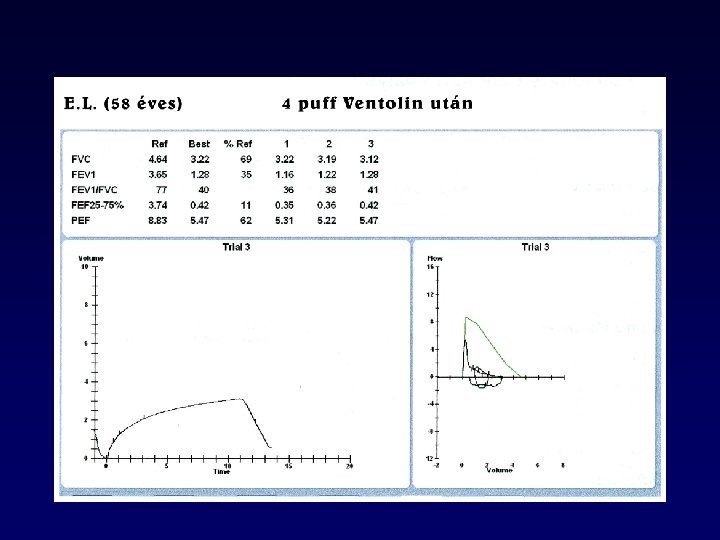
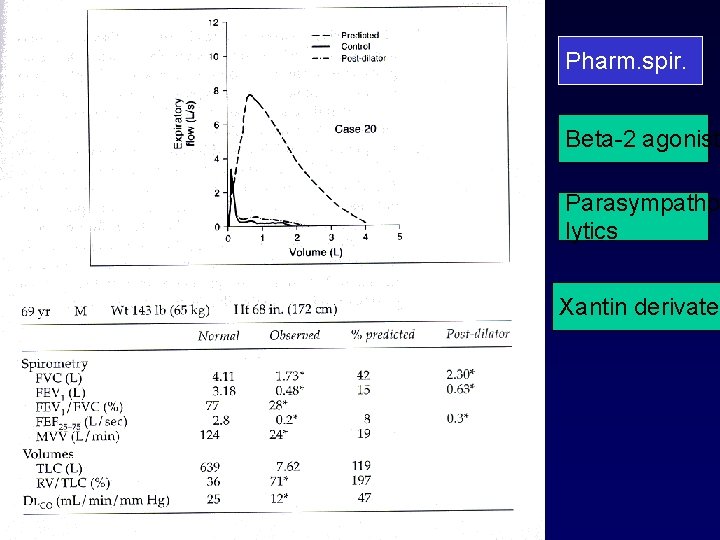
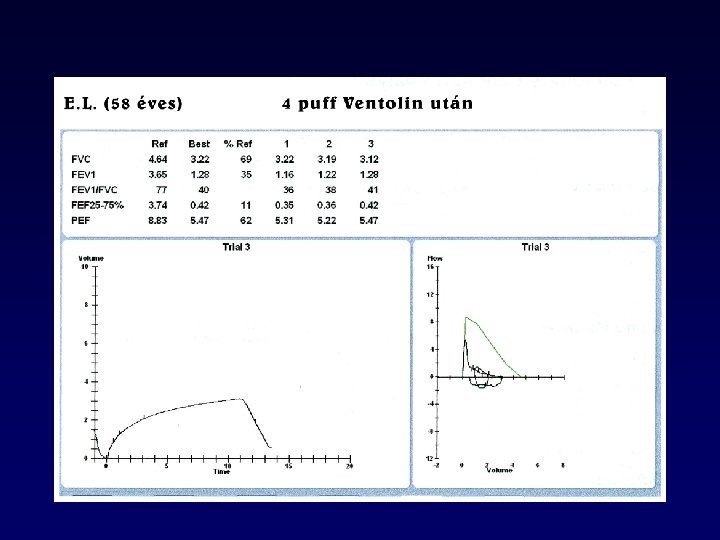
Pharm. spir. Beta-2 agonist Parasympatholytics Xantin derivate
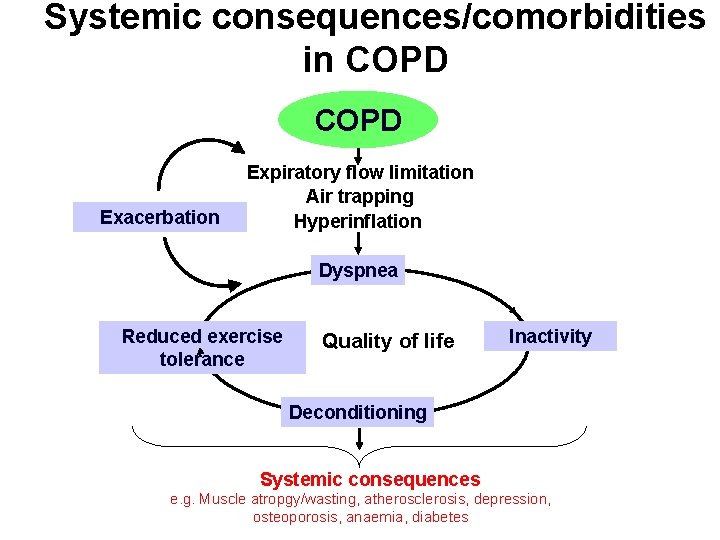
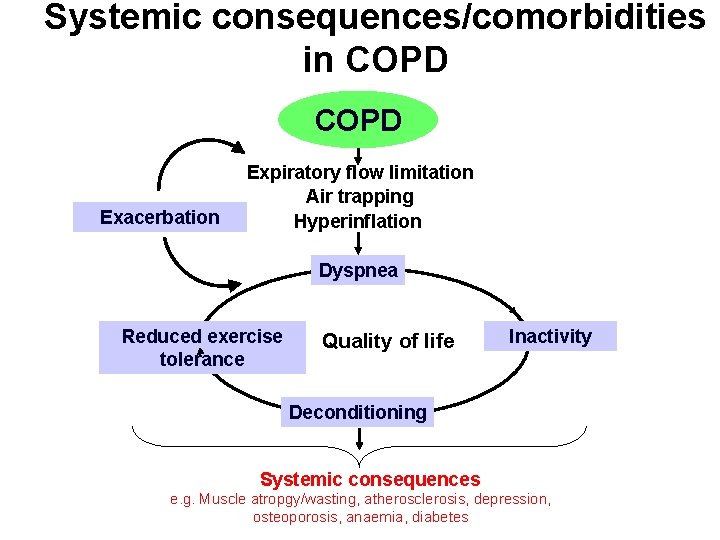
Systemic consequences/comorbidities in COPD Exacerbation Expiratory flow limitation Air trapping Hyperinflation Dyspnea Reduced exercise tolerance Quality of life Inactivity Deconditioning Systemic consequences e. g. Muscle atropgy/wasting, atherosclerosis, depression, osteoporosis, anaemia, diabetes
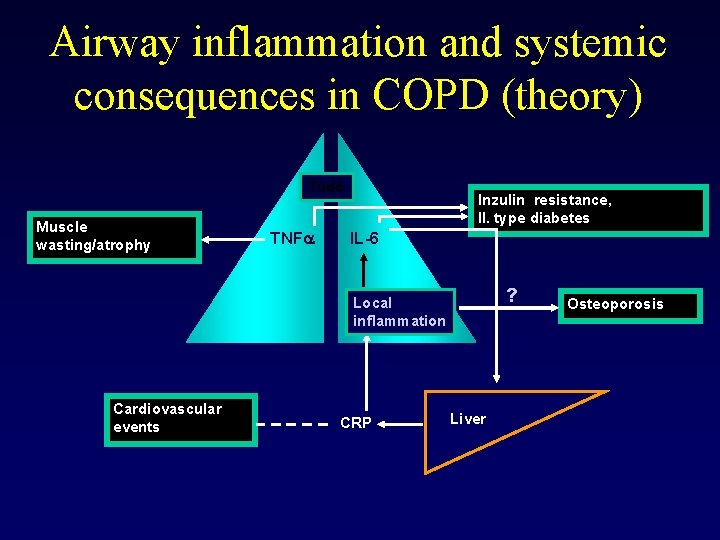
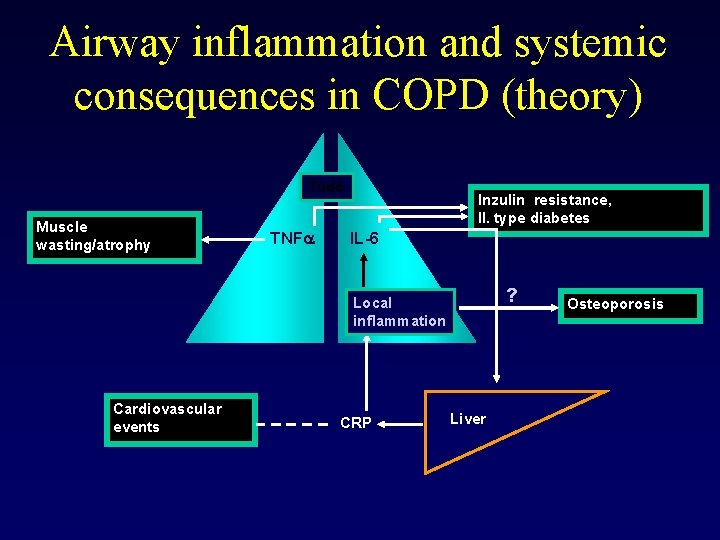
Airway inflammation and systemic consequences in COPD (theory) Tüdő Muscle wasting/atrophy TNFa Inzulin resistance, II. type diabetes IL-6 ? Local inflammation Cardiovascular events CRP Liver Osteoporosis

GOLD Workshop Report Four components of COPD Management 1. Asses and monitor disease 2. Reduce risk factors 3. Manage stabil COPD l Education l Pharmacologic. Gyógyszeres l Non-pharmacologic 4. Manage exacerbations

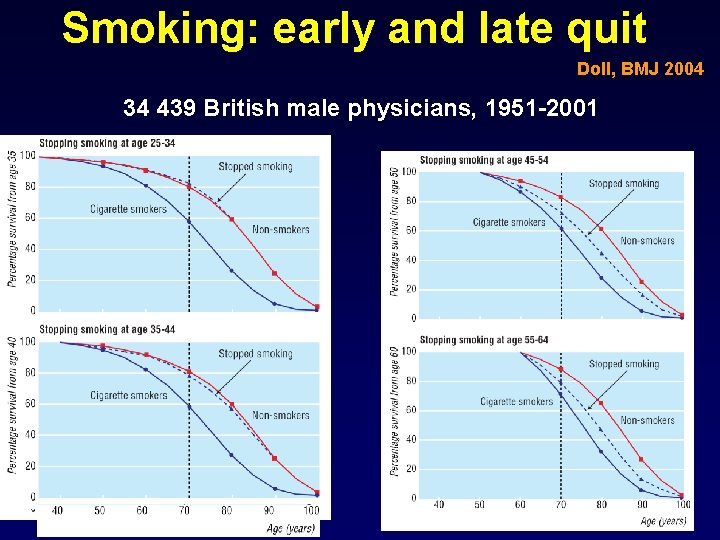
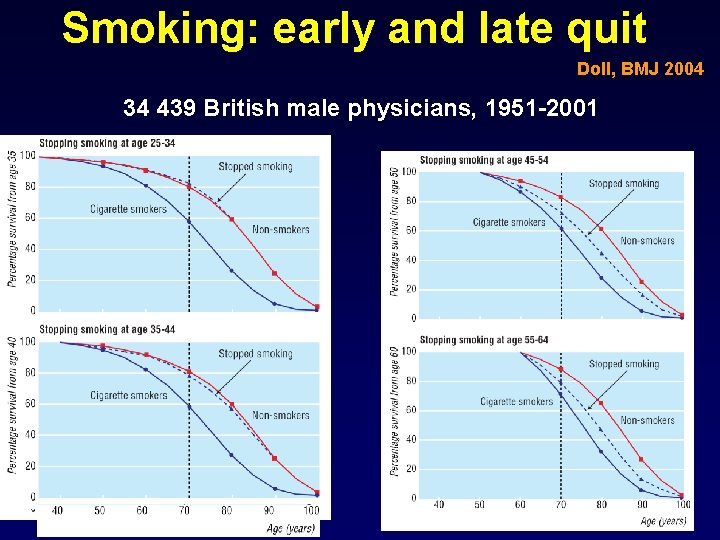
Smoking: early and late quit Doll, BMJ 2004 34 439 British male physicians, 1951 -2001
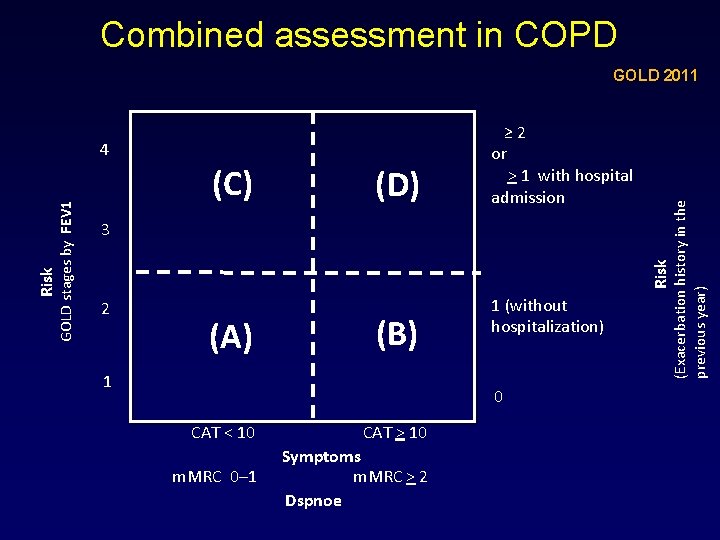
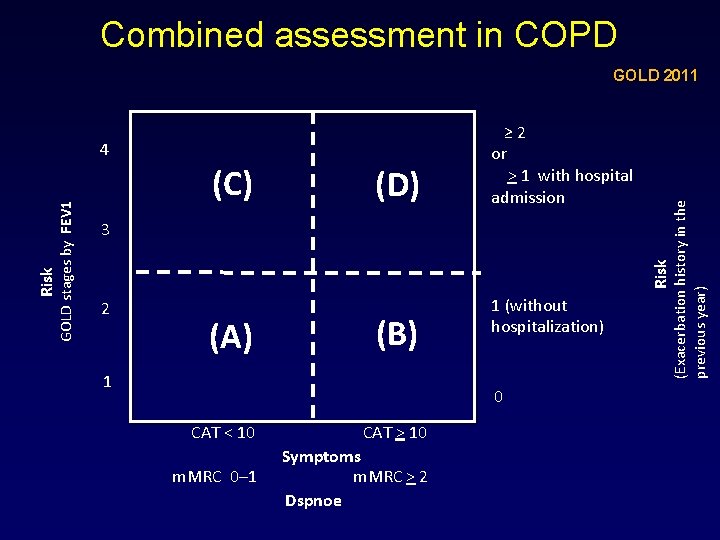
Combined assessment in COPD (C) (D) Risk 3 Risk GOLD stages by FEV 1 4 ≥ 2 or > 1 with hospital admission (Exacerbation history in the previous year) GOLD 2011 2 (A) (B) 1 1 (without hospitalization) 0 CAT < 10 CAT > 10 m. MRC 0– 1 Symptoms m. MRC > 2 Dspnoe
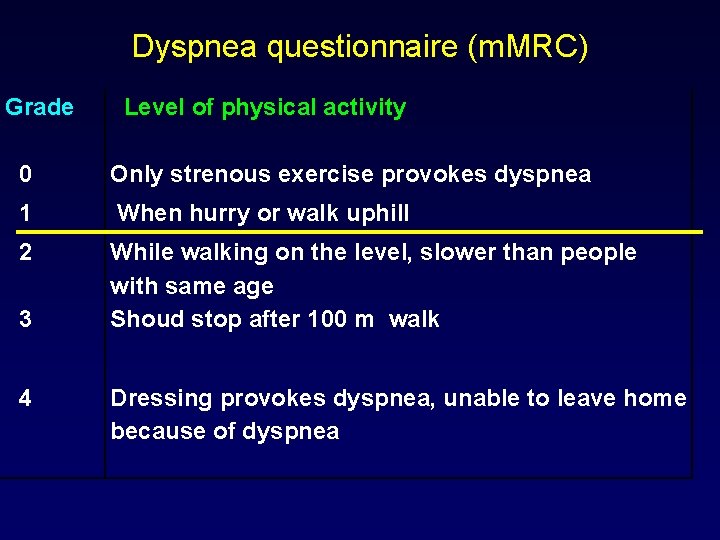
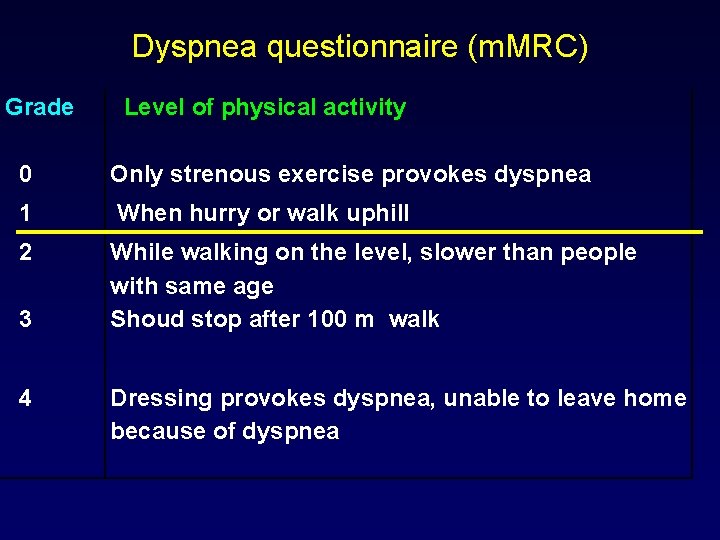
Dyspnea questionnaire (m. MRC) Grade Level of physical activity 0 Only strenous exercise provokes dyspnea 1 When hurry or walk uphill 2 While walking on the level, slower than people with same age Shoud stop after 100 m walk 3 4 Dressing provokes dyspnea, unable to leave home because of dyspnea
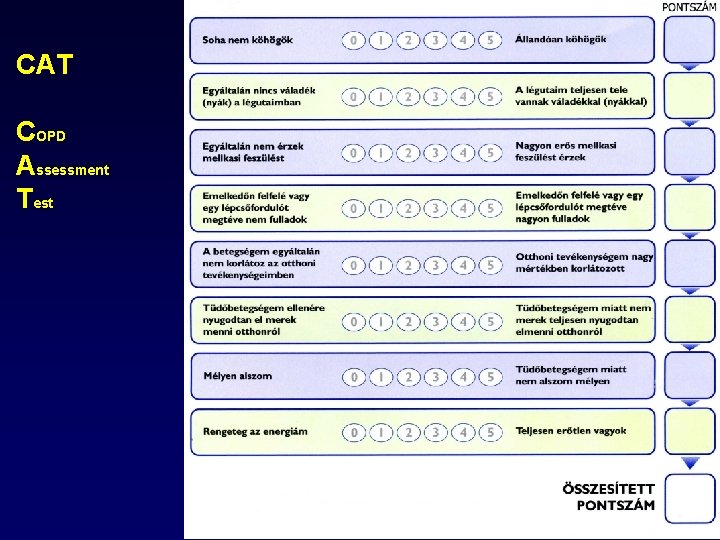
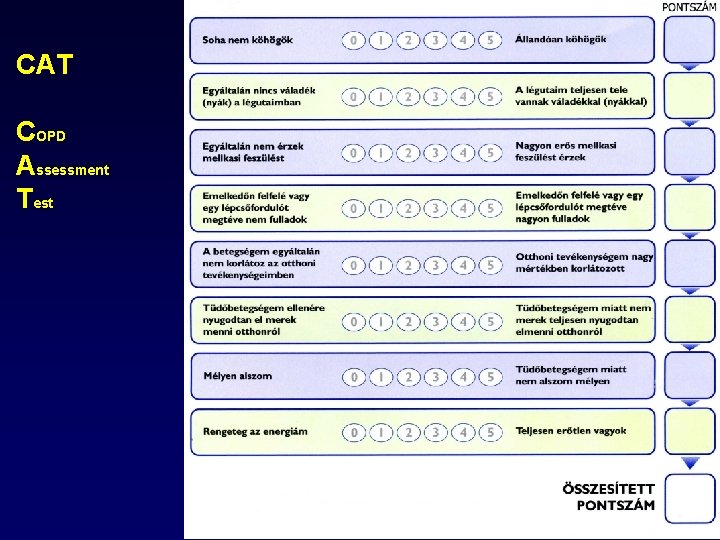
CAT COPD Assessment Test
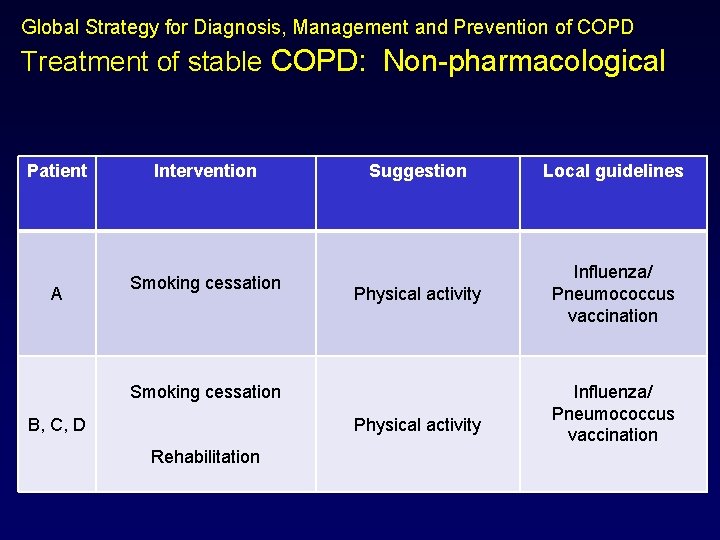
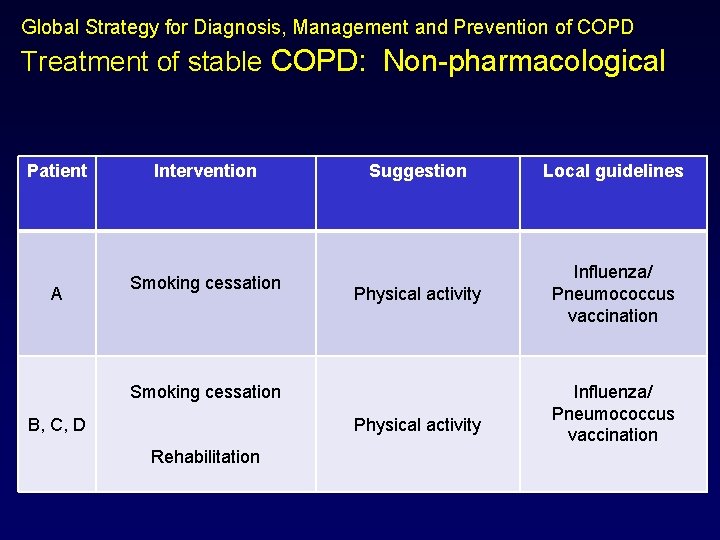
Global Strategy for Diagnosis, Management and Prevention of COPD Treatment of stable COPD: Non-pharmacological Patient A Intervention Smoking cessation Suggestion Local guidelines Physical activity Influenza/ Pneumococcus vaccination Smoking cessation B, C, D Physical activity Rehabilitation Influenza/ Pneumococcus vaccination
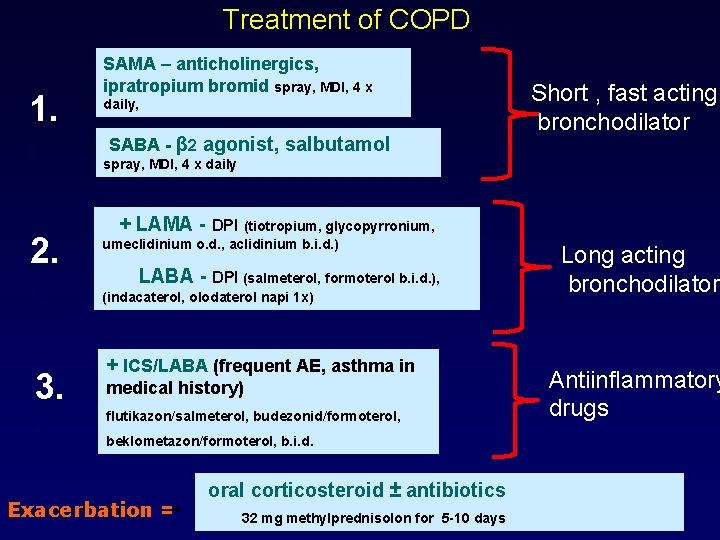
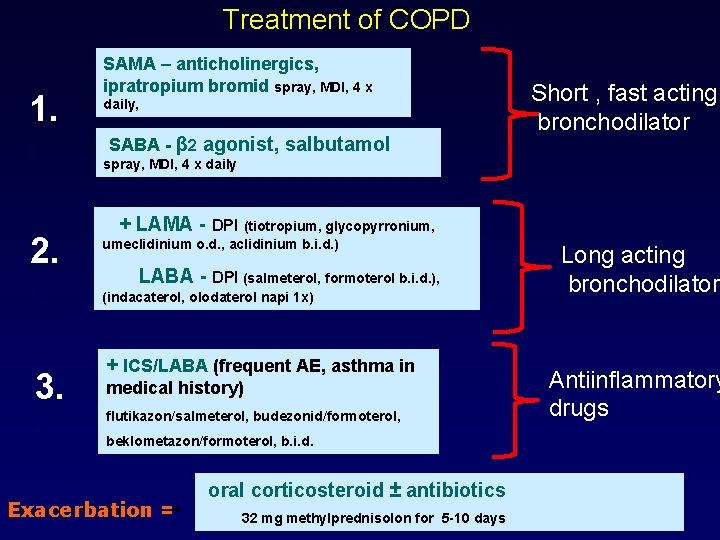
Treatment of COPD 1. . SAMA – anticholinergics, ipratropium bromid spray, MDI, 4 x daily, SABA - β 2 agonist, salbutamol Short , fast acting bronchodilator spray, MDI, 4 x daily 2. . 3. . + LAMA - DPI (tiotropium, glycopyrronium, umeclidinium o. d. , aclidinium b. i. d. ) LABA - DPI (salmeterol, formoterol b. i. d. ), (indacaterol, olodaterol napi 1 x) + ICS/LABA (frequent AE, asthma in medical history) flutikazon/salmeterol, budezonid/formoterol, beklometazon/formoterol, b. i. d. Exacerbation = oral corticosteroid ± antibiotics 32 mg methylprednisolon for 5 -10 days Long acting bronchodilator Antiinflammatory drugs
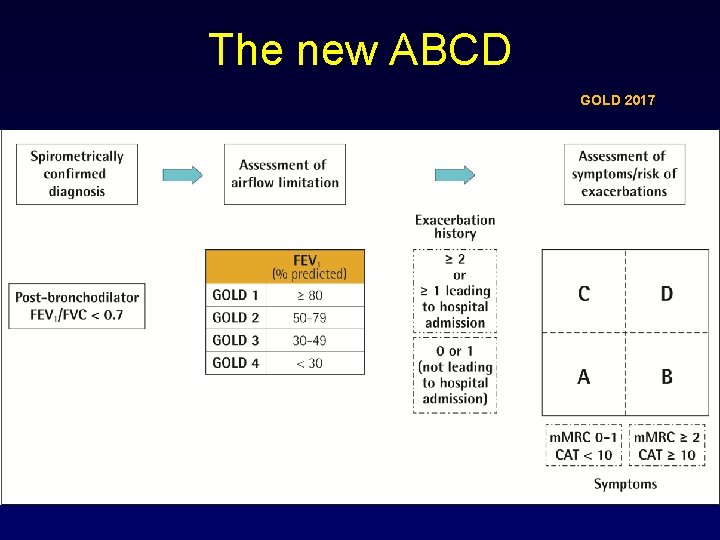
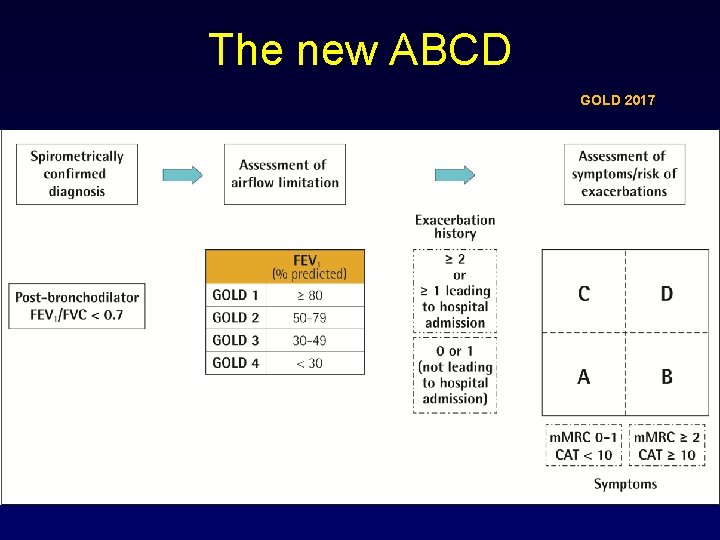
The new ABCD GOLD 2017
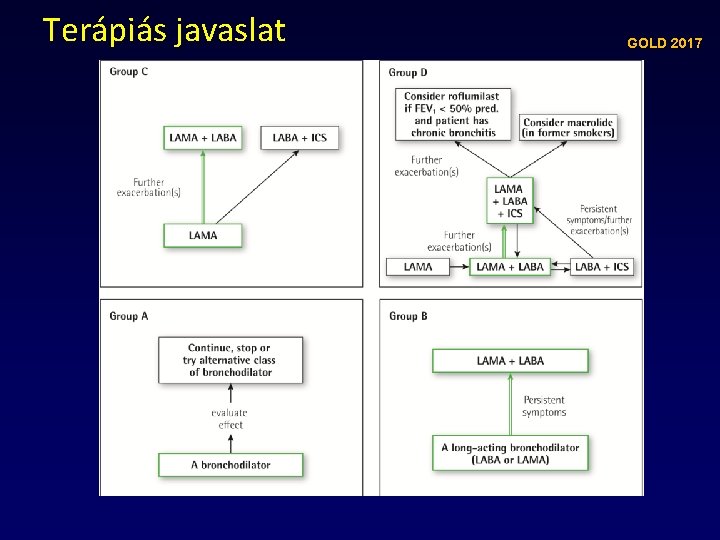
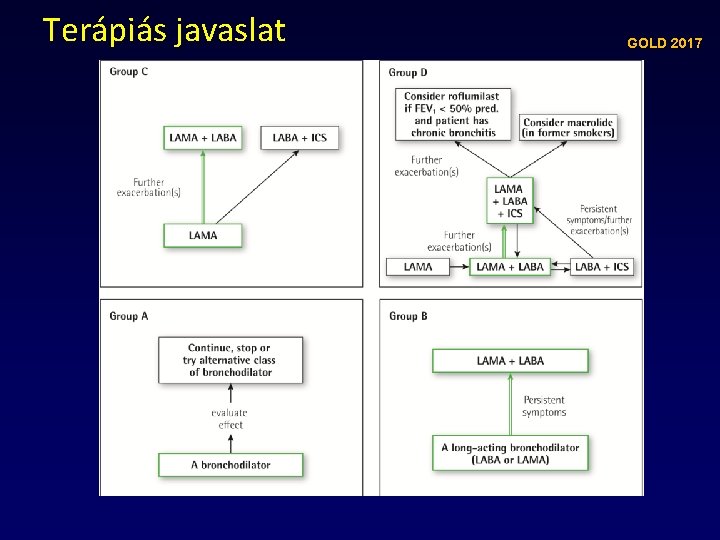
Terápiás javaslat GOLD 2017
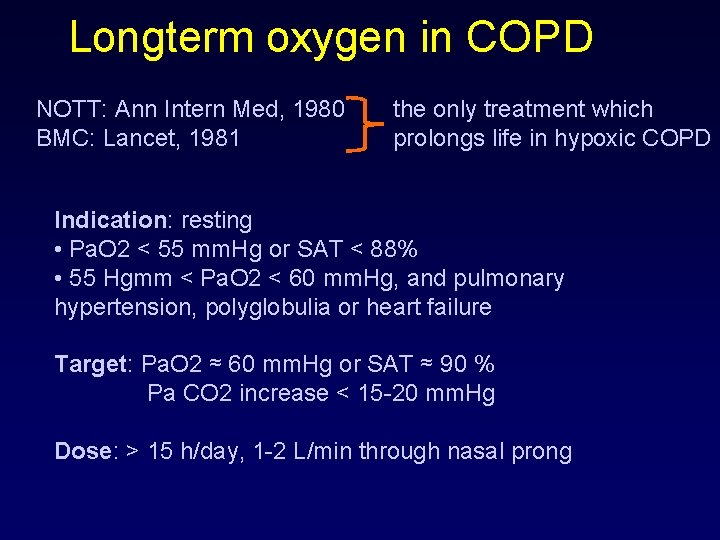
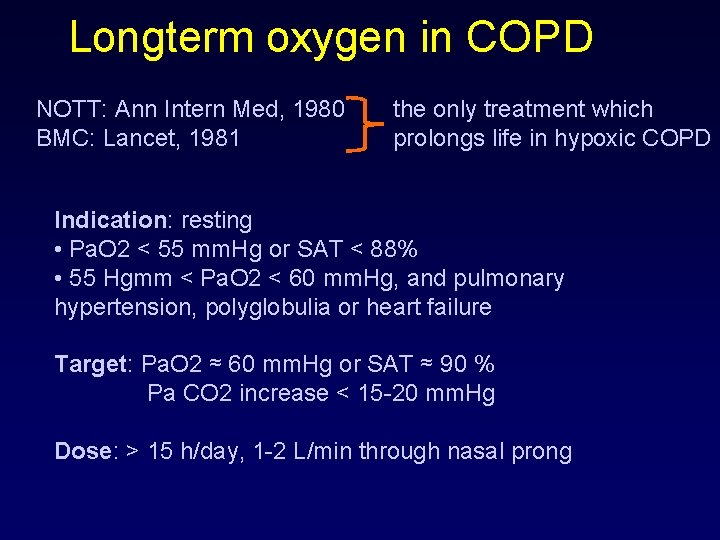
Longterm oxygen in COPD NOTT: Ann Intern Med, 1980 BMC: Lancet, 1981 the only treatment which prolongs life in hypoxic COPD Indication: resting • Pa. O 2 < 55 mm. Hg or SAT < 88% • 55 Hgmm < Pa. O 2 < 60 mm. Hg, and pulmonary hypertension, polyglobulia or heart failure Target: Pa. O 2 ≈ 60 mm. Hg or SAT ≈ 90 % Pa CO 2 increase < 15 -20 mm. Hg Dose: > 15 h/day, 1 -2 L/min through nasal prong
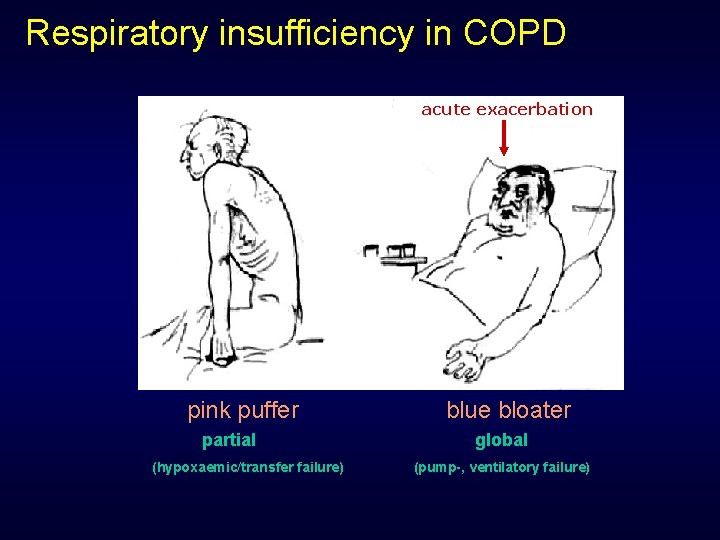
Respiratory insufficiency in COPD acute exacerbation pink puffer partial (hypoxaemic/transfer failure) blue bloater global (pump-, ventilatory failure)
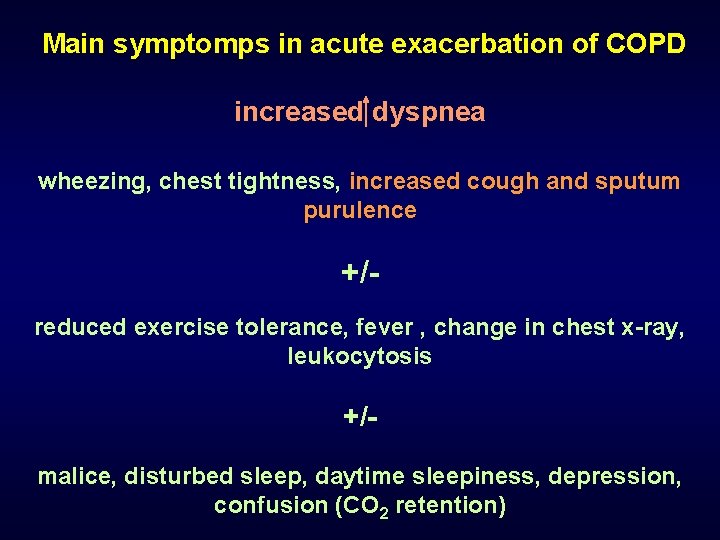
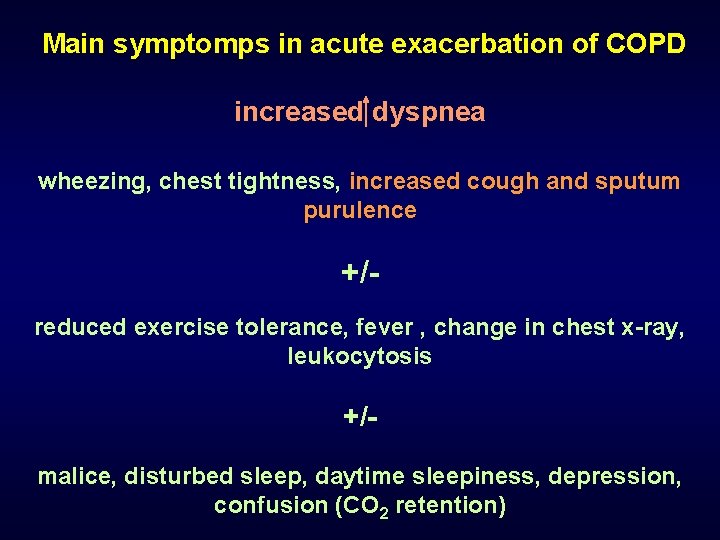
Main symptomps in acute exacerbation of COPD increased dyspnea wheezing, chest tightness, increased cough and sputum purulence +/reduced exercise tolerance, fever , change in chest x-ray, leukocytosis +/malice, disturbed sleep, daytime sleepiness, depression, confusion (CO 2 retention)
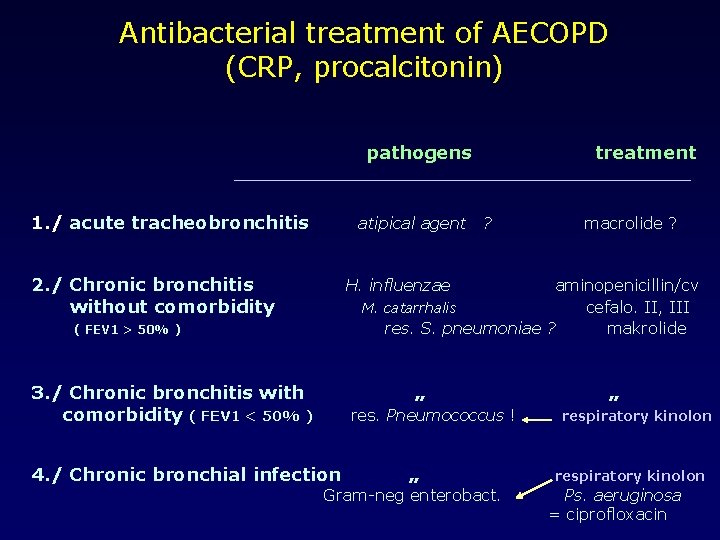
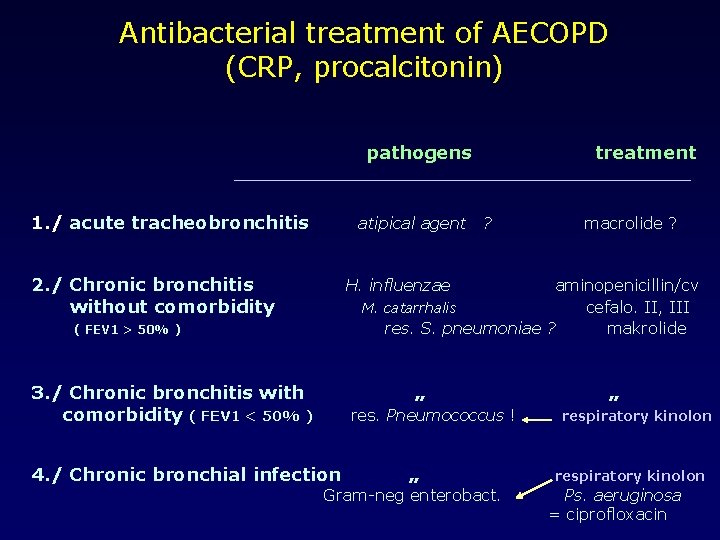
Antibacterial treatment of AECOPD (CRP, procalcitonin) pathogens 1. / acute tracheobronchitis atipical agent 2. / Chronic bronchitis without comorbidity treatment ? macrolide ? H. influenzae aminopenicillin/cv M. catarrhalis cefalo. II, III res. S. pneumoniae ? makrolide ( FEV 1 > 50% ) 3. / Chronic bronchitis with comorbidity ( FEV 1 < 50% ) „ res. Pneumococcus ! 4. / Chronic bronchial infection „ Gram-neg enterobact. „ respiratory kinolon Ps. aeruginosa = ciprofloxacin
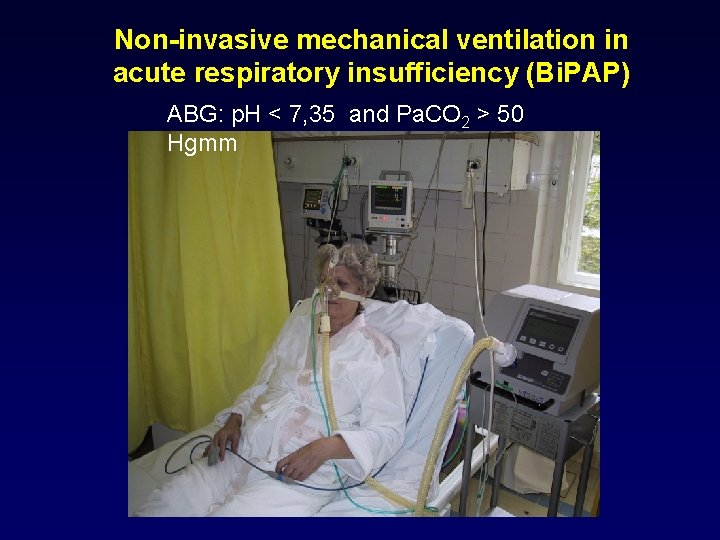
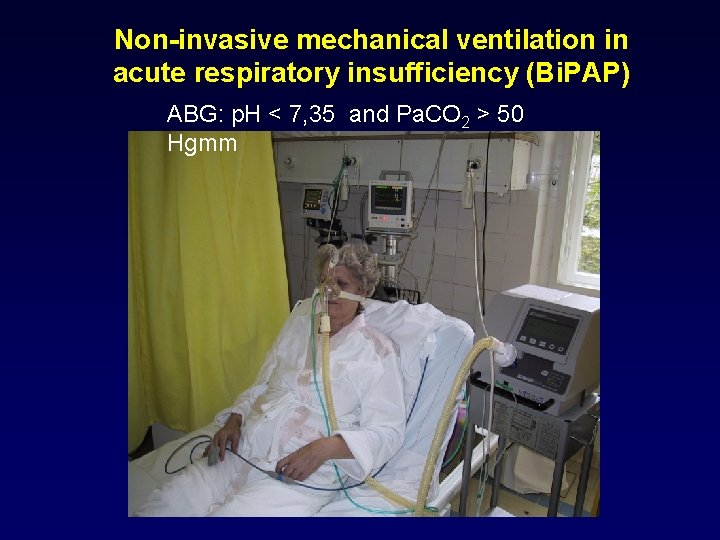
Non-invasive mechanical ventilation in acute respiratory insufficiency (Bi. PAP) ABG: p. H < 7, 35 and Pa. CO 2 > 50 Hgmm
 Somfay attila
Somfay attila Somfay attila
Somfay attila Somfay attila
Somfay attila Dr somfay attila
Dr somfay attila Uhs pulmonology
Uhs pulmonology Mcps anatomy
Mcps anatomy Fcps pulmonology
Fcps pulmonology Phren/o medical terminology
Phren/o medical terminology Takcs
Takcs Központi adatnyilvántartás lekérdezés
Központi adatnyilvántartás lekérdezés Gábor dénes szeged szakok
Gábor dénes szeged szakok Neurológiai klinika szeged
Neurológiai klinika szeged Szeged
Szeged Tankerület szeged
Tankerület szeged Szeged hrk
Szeged hrk Ablako
Ablako Dr mester lajos szeged
Dr mester lajos szeged Copd abcd assessment
Copd abcd assessment Conditietraining amsterdam oost
Conditietraining amsterdam oost Interstitialis rajzolat a tüdőben
Interstitialis rajzolat a tüdőben Copd obstruktionsgrad
Copd obstruktionsgrad Intercostaalspieren
Intercostaalspieren Copd national action plan
Copd national action plan Tam chứng anthonisen
Tam chứng anthonisen Emphysème
Emphysème Fever in copd
Fever in copd Ibratropium
Ibratropium Barrel chested man
Barrel chested man Asthma vs copd spirometry
Asthma vs copd spirometry Niv modes and settings
Niv modes and settings Centrilobular emphysema
Centrilobular emphysema Bitemporal wasting in copd
Bitemporal wasting in copd Copd treatment gold
Copd treatment gold Ipass the baton example
Ipass the baton example Cv rizikó
Cv rizikó Exacerbatie copd
Exacerbatie copd Lets be copd
Lets be copd Copd exacerbation nursing management
Copd exacerbation nursing management Cat score copd
Cat score copd Copd types
Copd types Thick dark yellow mucus
Thick dark yellow mucus Pulmonary disease definition
Pulmonary disease definition Non pharmacological treatment for copd
Non pharmacological treatment for copd Asthma vs copd spirometry
Asthma vs copd spirometry Zorgleefplan 4 domeinen
Zorgleefplan 4 domeinen Terminale copd
Terminale copd Concept map neuman systems model
Concept map neuman systems model Copd v/q mismatch
Copd v/q mismatch Cat score copd
Cat score copd Emphysema lungs
Emphysema lungs Fever in copd
Fever in copd Micah ennis
Micah ennis Pt dept logistik
Pt dept logistik La city fire interview
La city fire interview Hjdkdkd
Hjdkdkd Liz welch mississippi
Liz welch mississippi