Pneumonia Attila Somfay Dept Pulmonology University of Szeged






- Slides: 49

Pneumonia Attila Somfay Dept. Pulmonology, University of Szeged, Deszk, Hungary
Pneumonia • Very common (1 -10/1000), significant mortality • Severity assessment, aided by score, is a key management step • Caused by a variety of different pathogens • Antibiotic treatment initially nearly always empirical, local guidelines and microbial resistance rates may support it
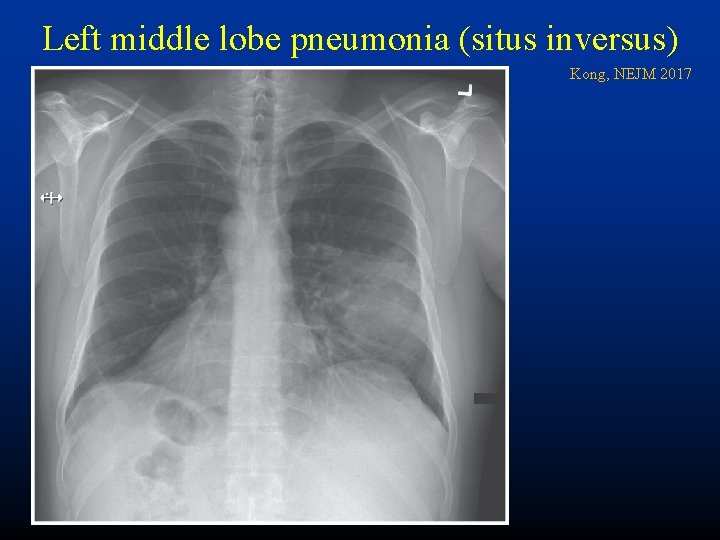
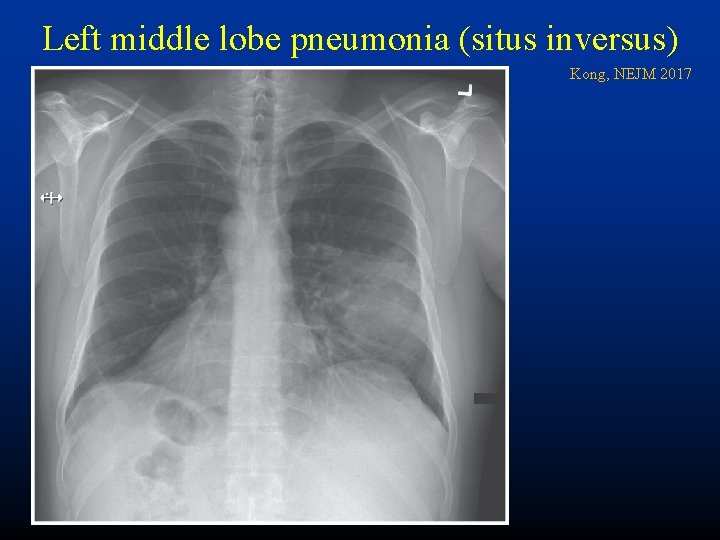
Left middle lobe pneumonia (situs inversus) Kong, NEJM 2017
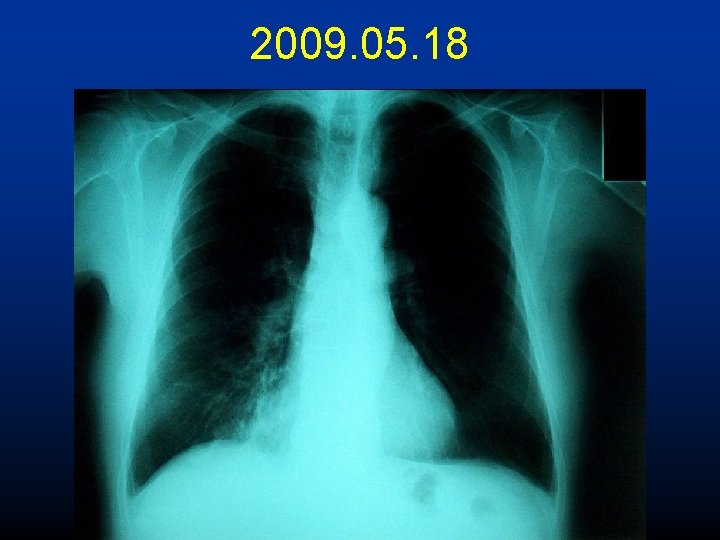
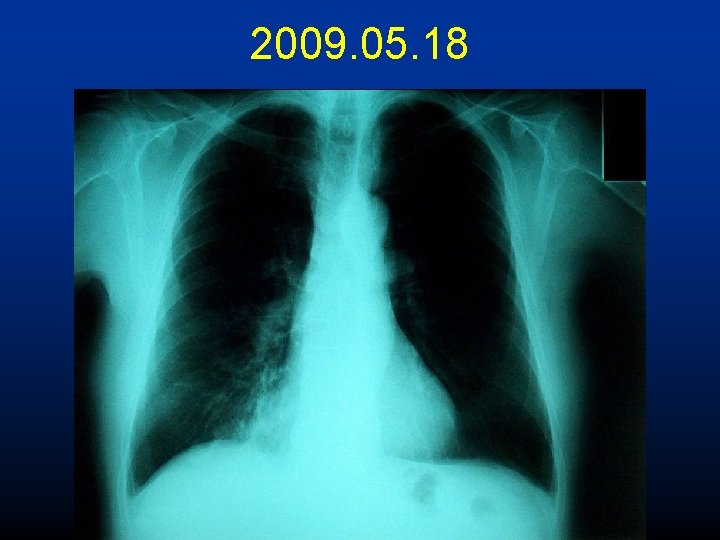
2009. 05. 18
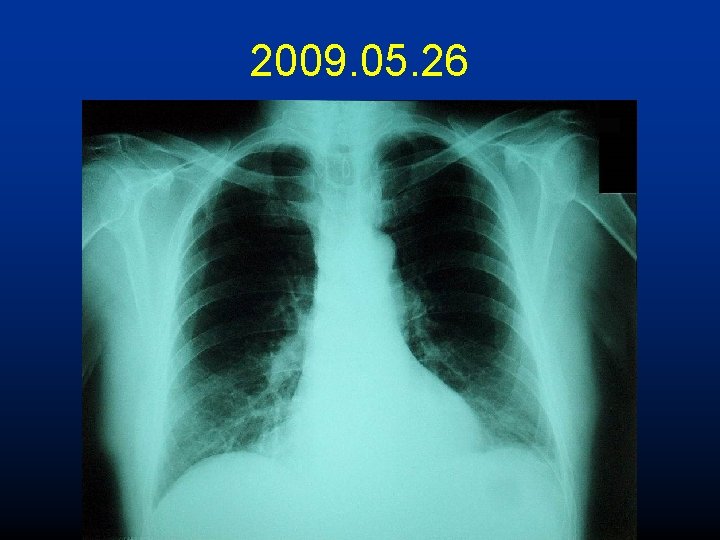
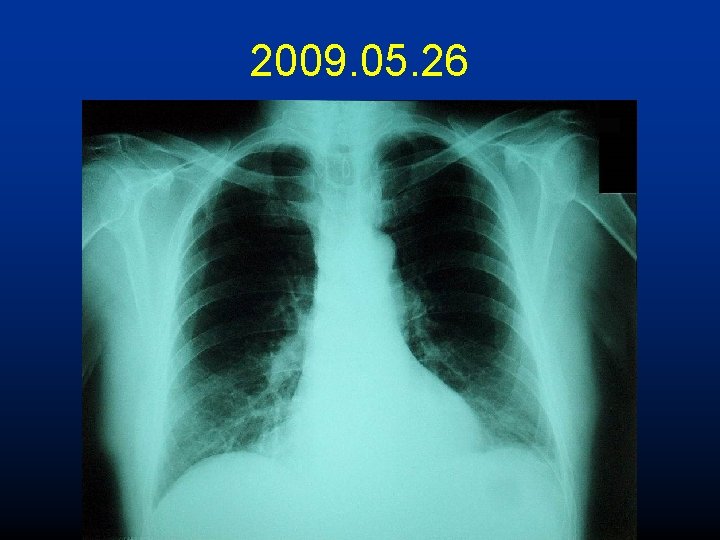
2009. 05. 26
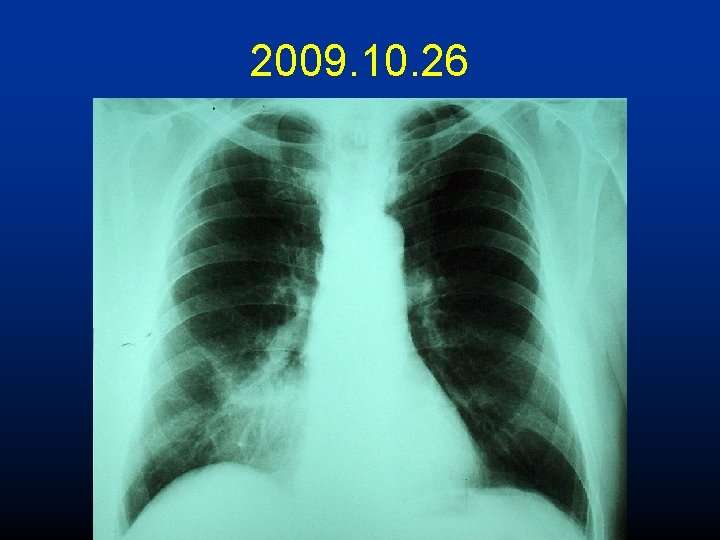
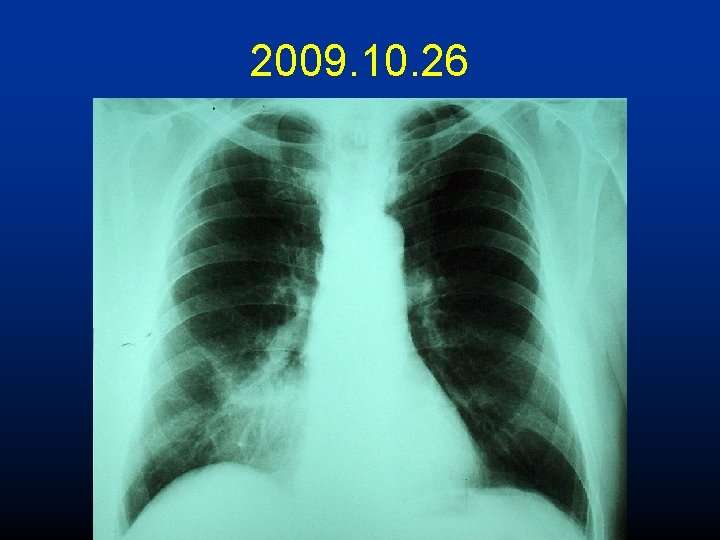
2009. 10. 26
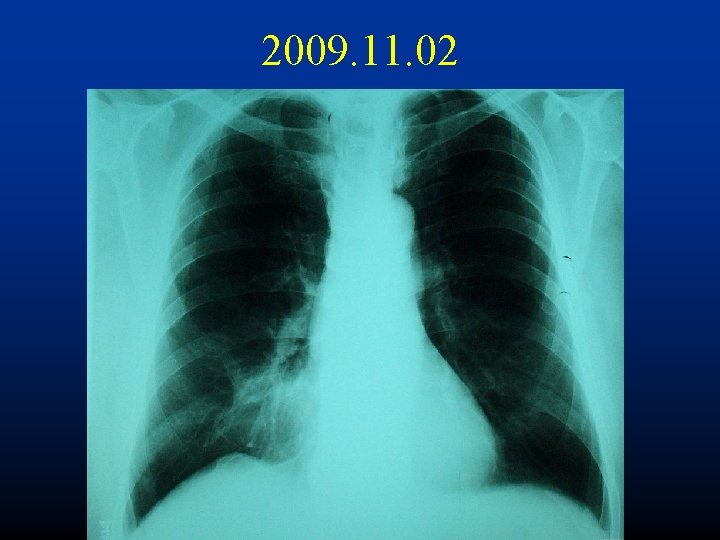
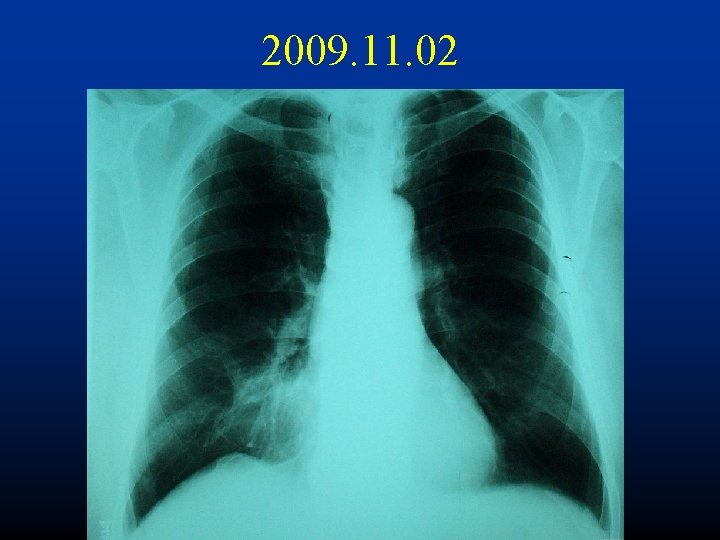
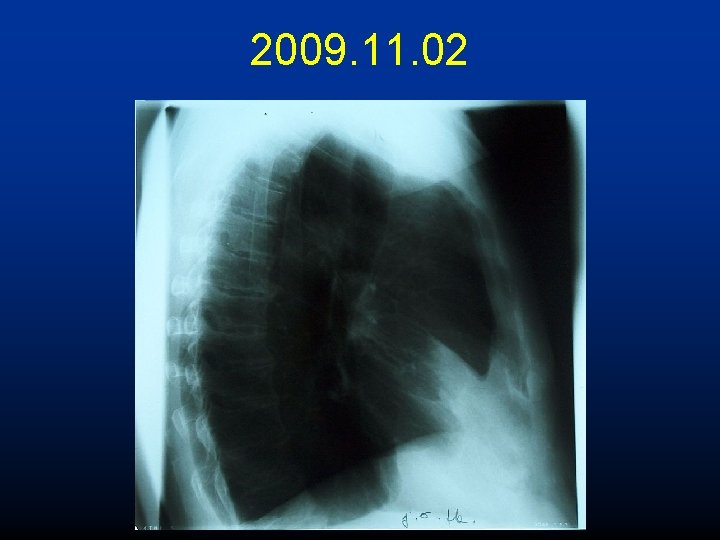
2009. 11. 02
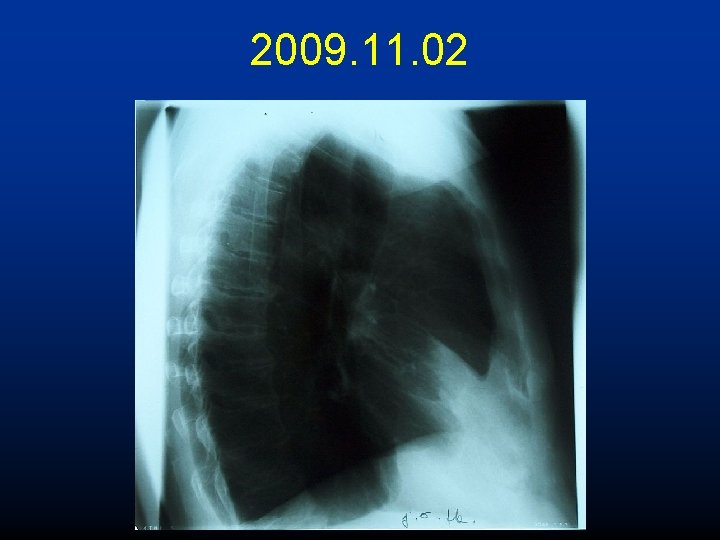
2009. 11. 02
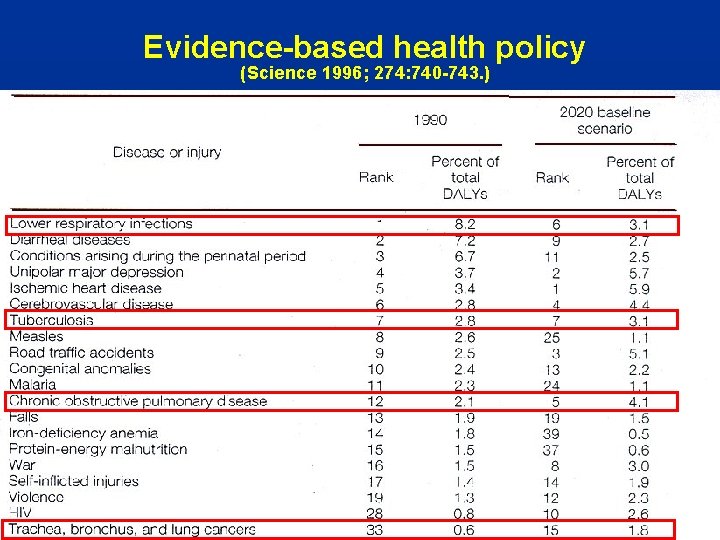
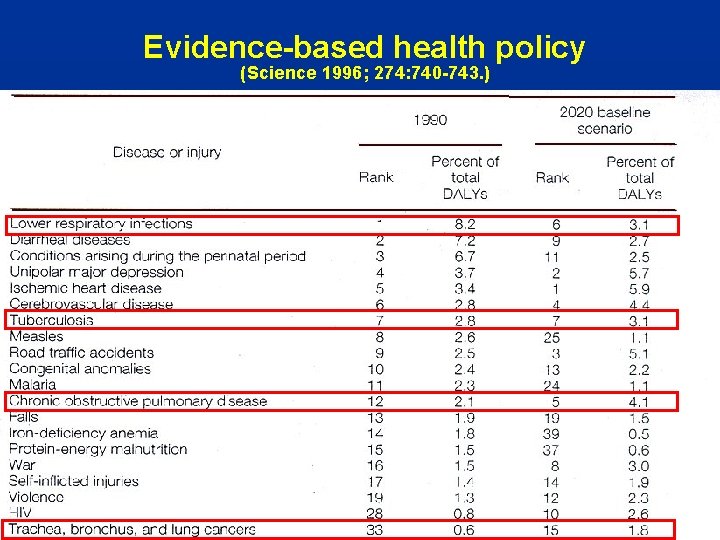
Evidence-based health policy (Science 1996; 274: 740 -743. )
Definition Acute, infectious inflammation of the lower respiratory tract parenchyma (distal to bronchiolus terminalis).
Pathogens • Bacteria /aerobic, anaerobic, atypical/ • Virus /influenza , parainfluenza, adenovirus, herpesvirus, cytomegalovirus, RSV/ • Fungi /Aspergillus, Candida/ • Parasites /Pneumocystis jiroveci, Toxoplasma gondii, Ascaris lumbricoides/
Clinical classification • Community-acquired, CAP • Nosocomial, hospital-acquired, HAP, VAP • • • Aspiration and anaerobic Pneumonia in the immuncompromised host AIDS-related Reccurent Pneumonias peculiar to specific geographical areas
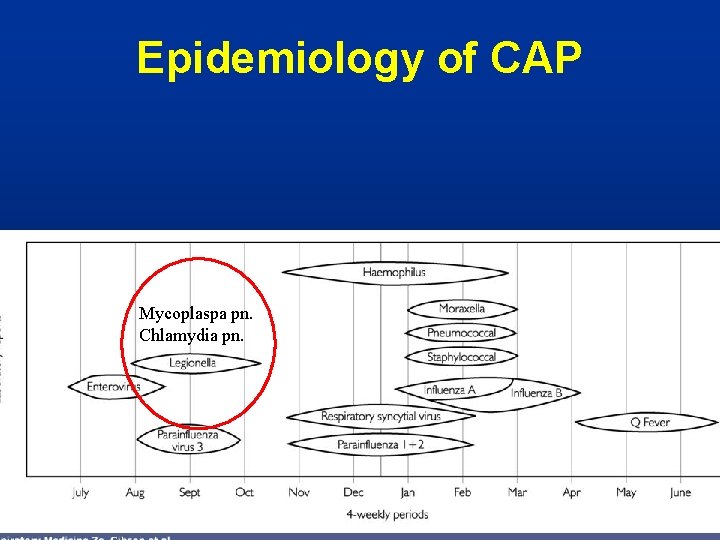
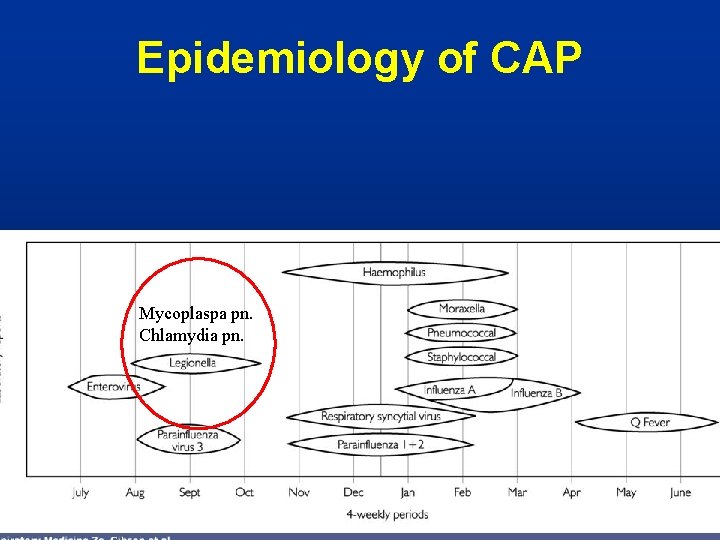
Epidemiology of CAP Mycoplaspa pn. Chlamydia pn.
Pathogenesis • • Inhalation of infected droplets Aspiration /residents from nasopharynx/ Spread through bloodstream Direkt spread (concomittant)
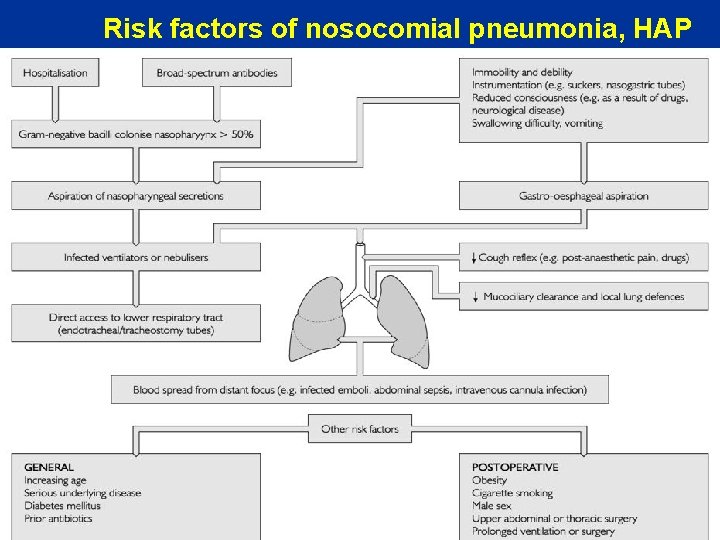
Risk factors • • • Prolonged supine position Antibiotics, antacids Patient contact Decreased defense mechanisms Infected health care materials
Etiology • • 1. Streptococcus pneumoniae 40 -60% 2. Mycoplasma pneumoniae 10 -20% 3. Haemophilus influenzae 6 -10% 4. Influenza A 5 -8%
Clinical features I. • General symptoms – malaise, anorexia – sweating, rigors – myalgia, arthralgia – headache – fast (bacteremia) vs. slow (Mycoplasma) progression – marked confusion (Legionella, psittacosis) – acute abdominal or urinary problem (lower lobe, age!)
Clinical features II. • Respiratory symptoms - cough, dsypnea, pleural pain - purulent sputum, hemoptysis • Physical signs - high fever and rigor (Pneumococus) - little or no fever (elderly, seriously ill) - herpes labialis (Pneumococcus) - dullness, inspiratory crackles, bronchial breathing - upper abd. tenderness (lower lobe) - rash (antibiotic, mycoplasma, psittacosis)
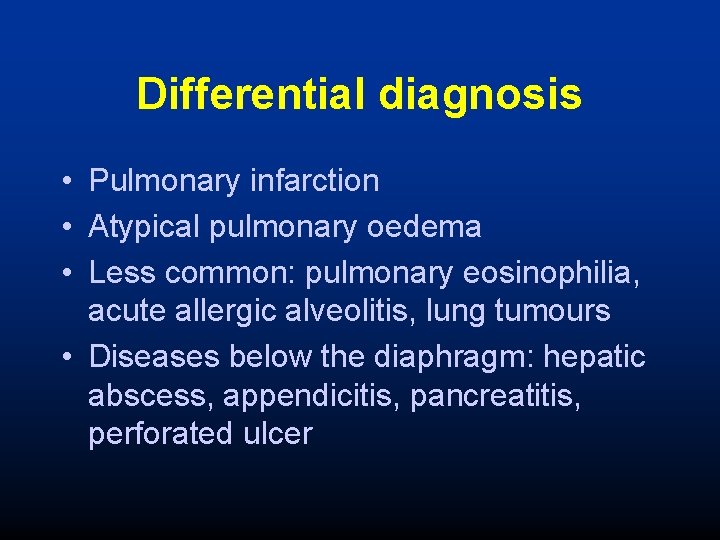
Differential diagnosis • Pulmonary infarction • Atypical pulmonary oedema • Less common: pulmonary eosinophilia, acute allergic alveolitis, lung tumours • Diseases below the diaphragm: hepatic abscess, appendicitis, pancreatitis, perforated ulcer
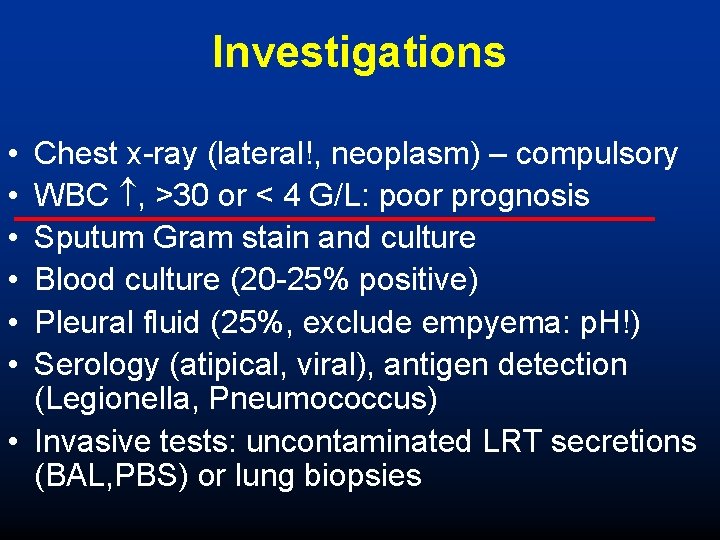
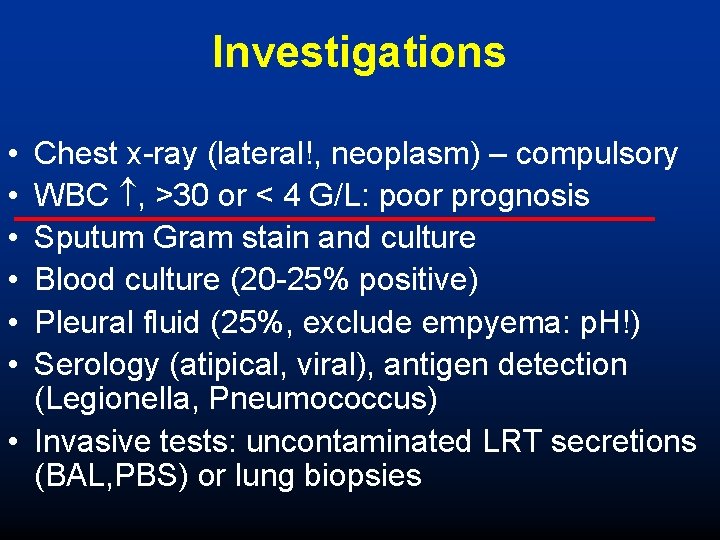
Investigations • • • Chest x-ray (lateral!, neoplasm) – compulsory WBC , >30 or < 4 G/L: poor prognosis Sputum Gram stain and culture Blood culture (20 -25% positive) Pleural fluid (25%, exclude empyema: p. H!) Serology (atipical, viral), antigen detection (Legionella, Pneumococcus) • Invasive tests: uncontaminated LRT secretions (BAL, PBS) or lung biopsies
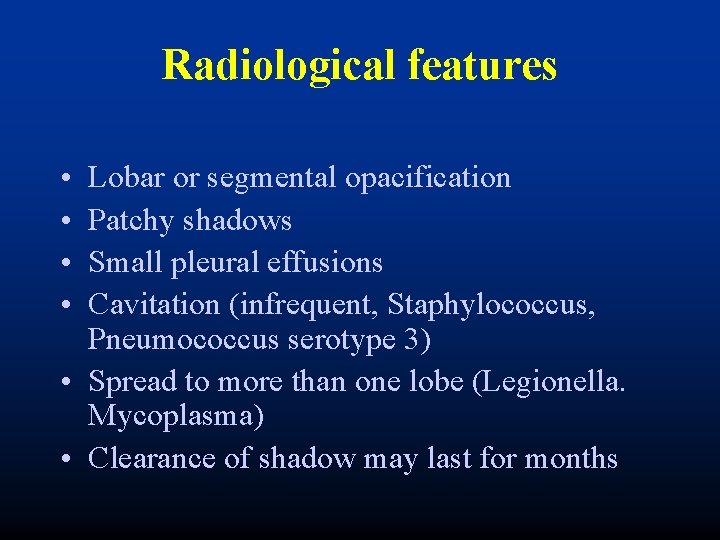
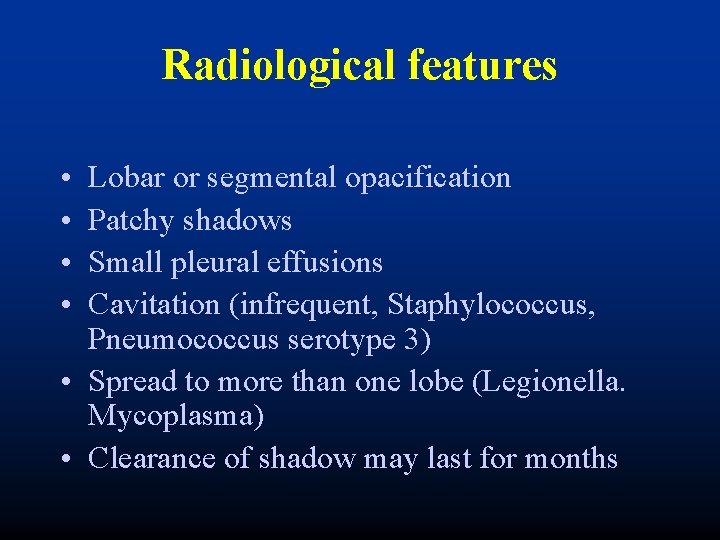
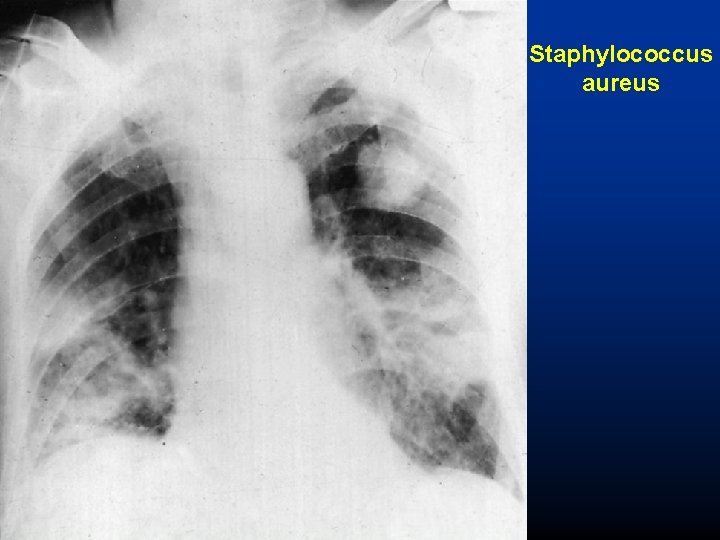
Radiological features • • Lobar or segmental opacification Patchy shadows Small pleural effusions Cavitation (infrequent, Staphylococcus, Pneumococcus serotype 3) • Spread to more than one lobe (Legionella. Mycoplasma) • Clearance of shadow may last for months
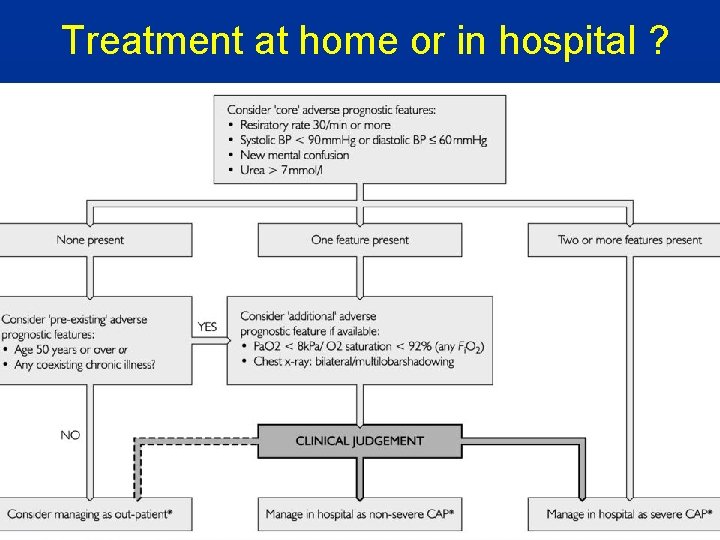
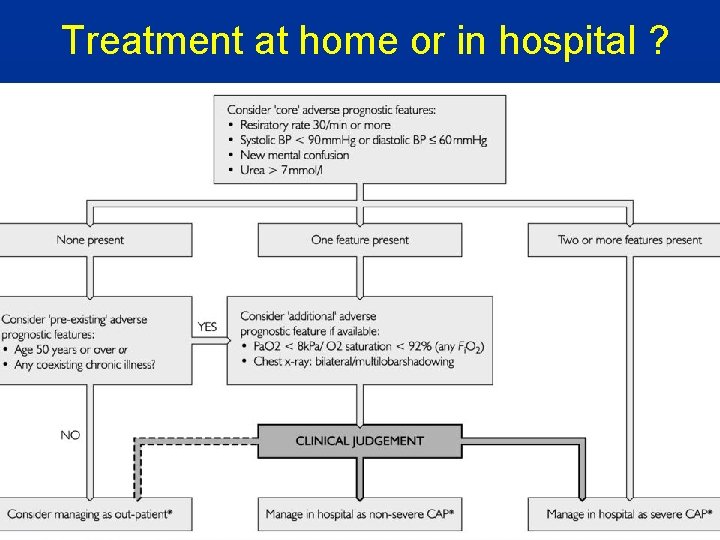
Treatment at home or in hospital ?
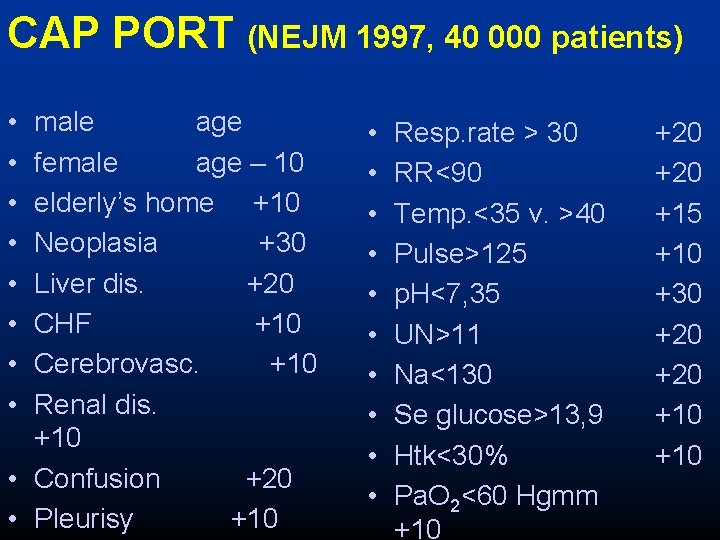
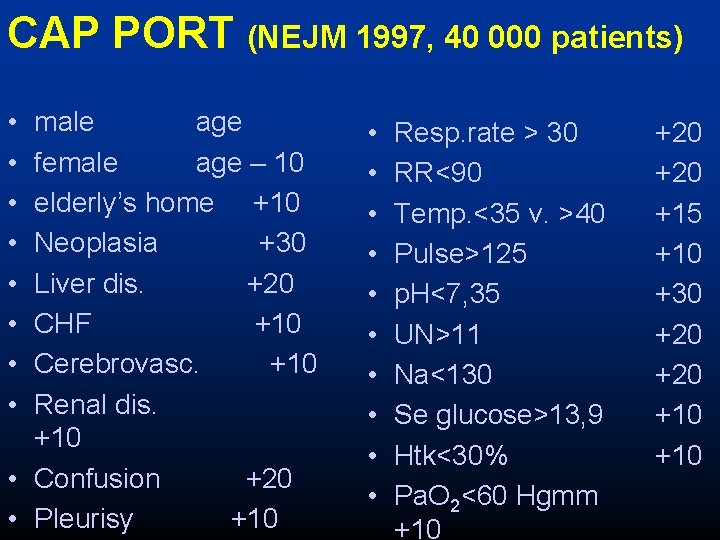
CAP PORT (NEJM 1997, 40 000 patients) • • male age female age – 10 elderly’s home +10 Neoplasia +30 Liver dis. +20 CHF +10 Cerebrovasc. +10 Renal dis. +10 • Confusion +20 • Pleurisy +10 • • • Resp. rate > 30 RR<90 Temp. <35 v. >40 Pulse>125 p. H<7, 35 UN>11 Na<130 Se glucose>13, 9 Htk<30% Pa. O 2<60 Hgmm +10 +20 +15 +10 +30 +20 +10
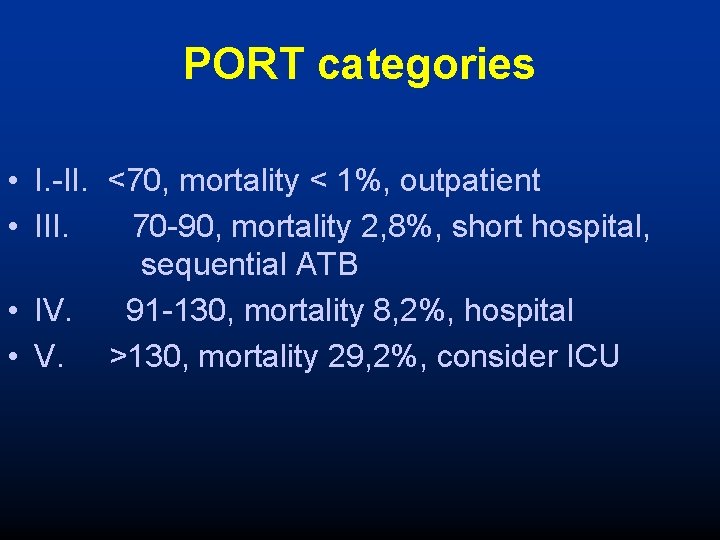
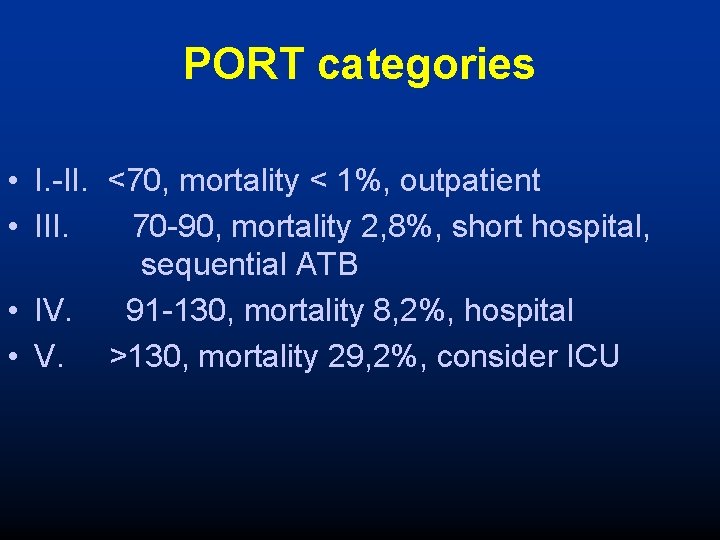
PORT categories • I. -II. <70, mortality < 1%, outpatient • III. 70 -90, mortality 2, 8%, short hospital, sequential ATB • IV. 91 -130, mortality 8, 2%, hospital • V. >130, mortality 29, 2%, consider ICU
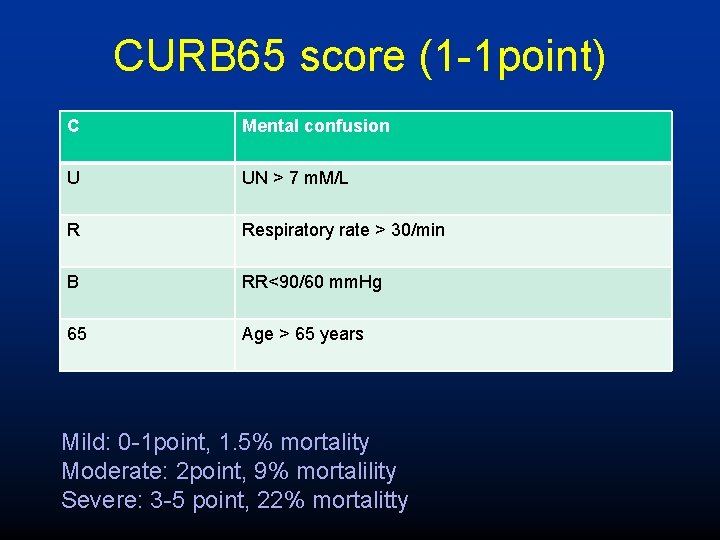
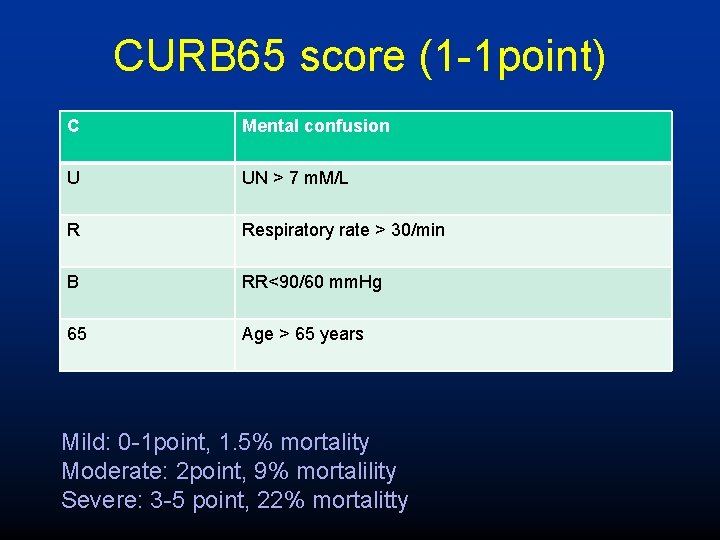
CURB 65 score (1 -1 point) C Mental confusion U UN > 7 m. M/L R Respiratory rate > 30/min B RR<90/60 mm. Hg 65 Age > 65 years Mild: 0 -1 point, 1. 5% mortality Moderate: 2 point, 9% mortalility Severe: 3 -5 point, 22% mortalitty
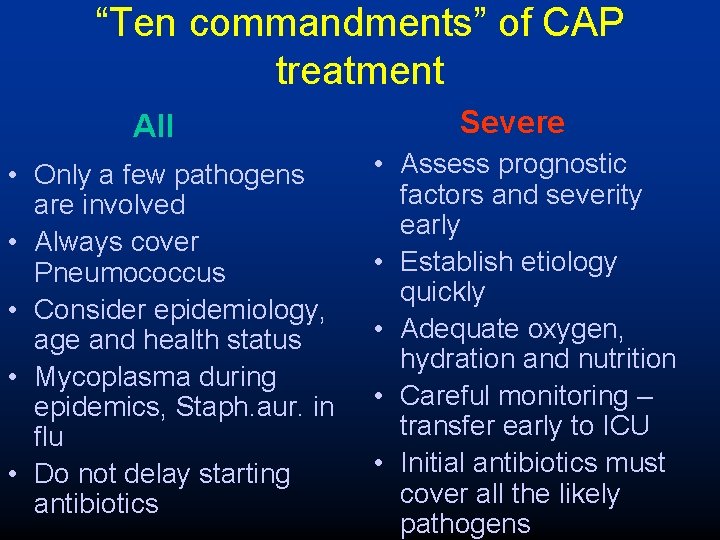
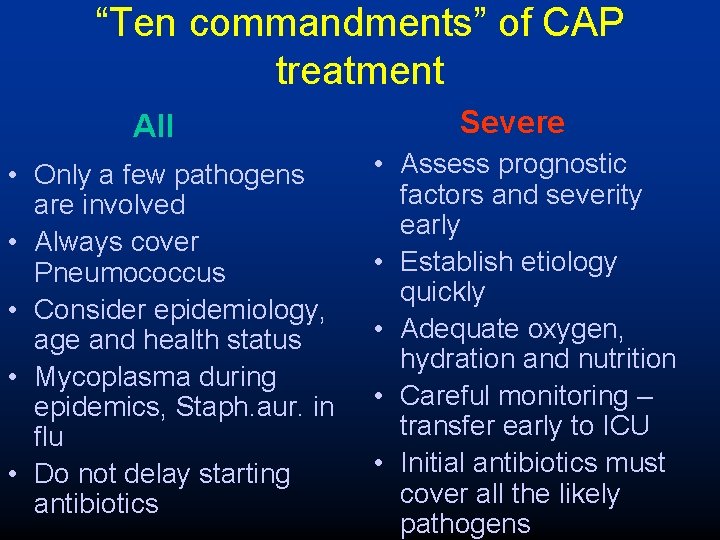
“Ten commandments” of CAP treatment All • Only a few pathogens are involved • Always cover Pneumococcus • Consider epidemiology, age and health status • Mycoplasma during epidemics, Staph. aur. in flu • Do not delay starting antibiotics Severe • Assess prognostic factors and severity early • Establish etiology quickly • Adequate oxygen, hydration and nutrition • Careful monitoring – transfer early to ICU • Initial antibiotics must cover all the likely pathogens
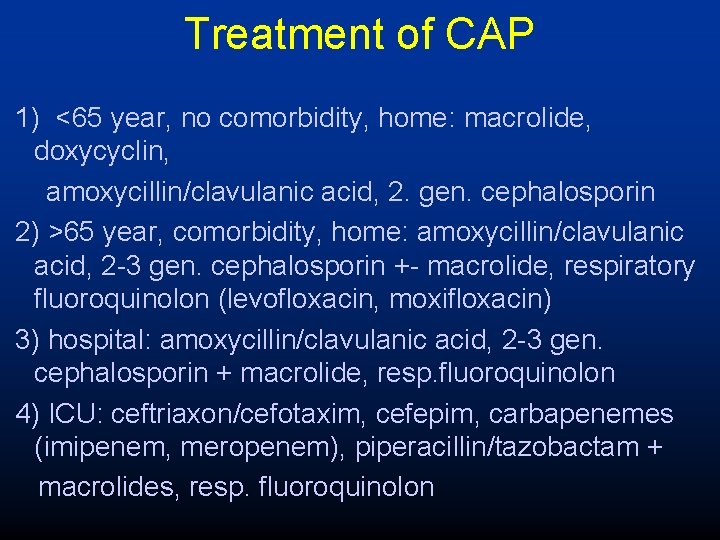
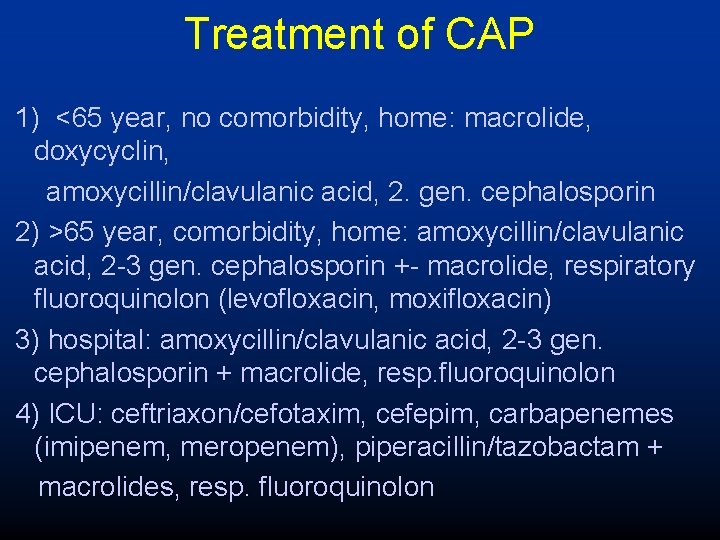
Treatment of CAP 1) <65 year, no comorbidity, home: macrolide, doxycyclin, amoxycillin/clavulanic acid, 2. gen. cephalosporin 2) >65 year, comorbidity, home: amoxycillin/clavulanic acid, 2 -3 gen. cephalosporin +- macrolide, respiratory fluoroquinolon (levofloxacin, moxifloxacin) 3) hospital: amoxycillin/clavulanic acid, 2 -3 gen. cephalosporin + macrolide, resp. fluoroquinolon 4) ICU: ceftriaxon/cefotaxim, cefepim, carbapenemes (imipenem, meropenem), piperacillin/tazobactam + macrolides, resp. fluoroquinolon
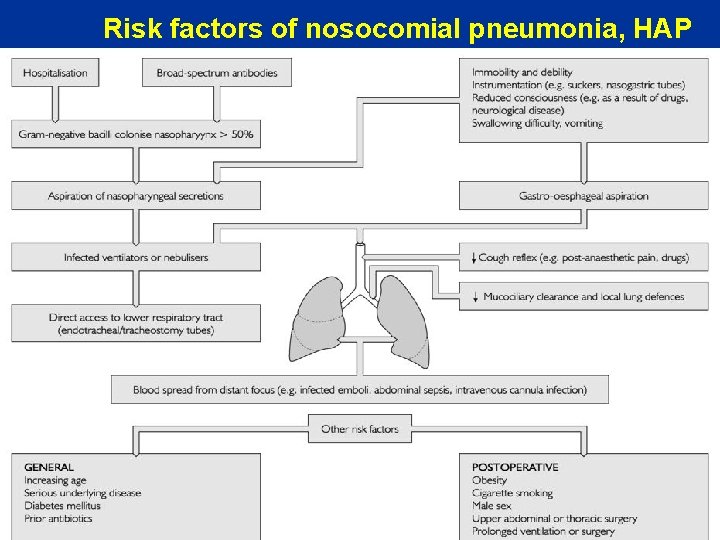
Risk factors of nosocomial pneumonia, HAP
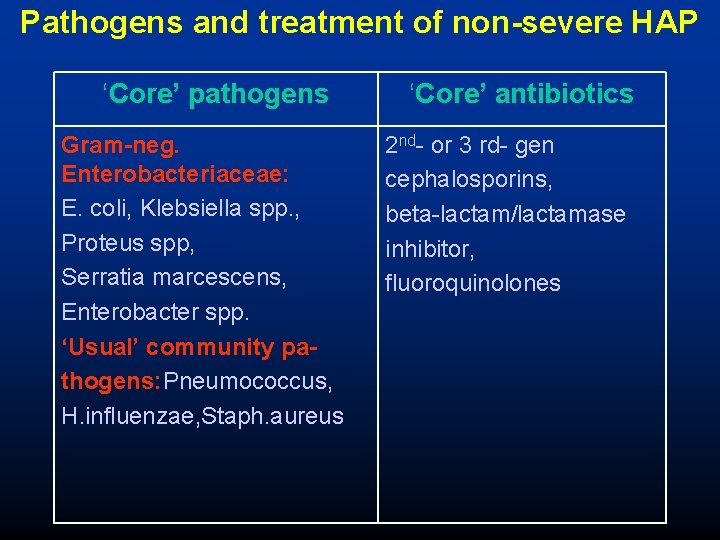
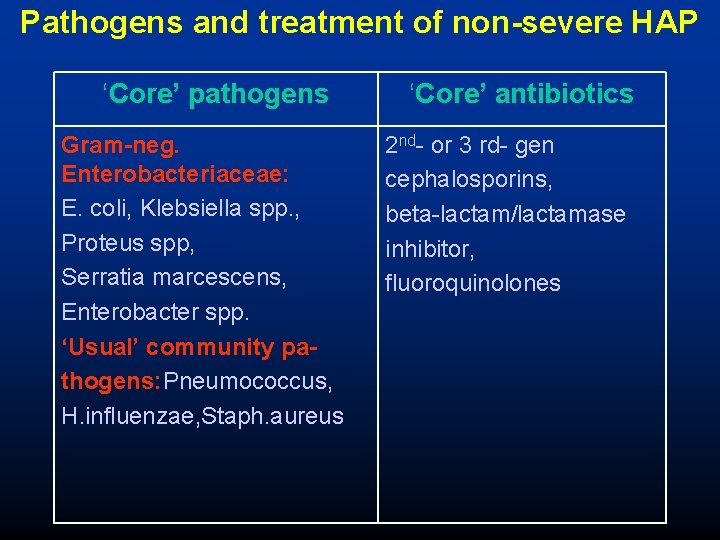
Pathogens and treatment of non-severe HAP ‘Core’ pathogens Gram-neg. Enterobacteriaceae: E. coli, Klebsiella spp. , Proteus spp, Serratia marcescens, Enterobacter spp. ‘Usual’ community pathogens: Pneumococcus, H. influenzae, Staph. aureus ‘Core’ antibiotics 2 nd- or 3 rd- gen cephalosporins, beta-lactam/lactamase inhibitor, fluoroquinolones
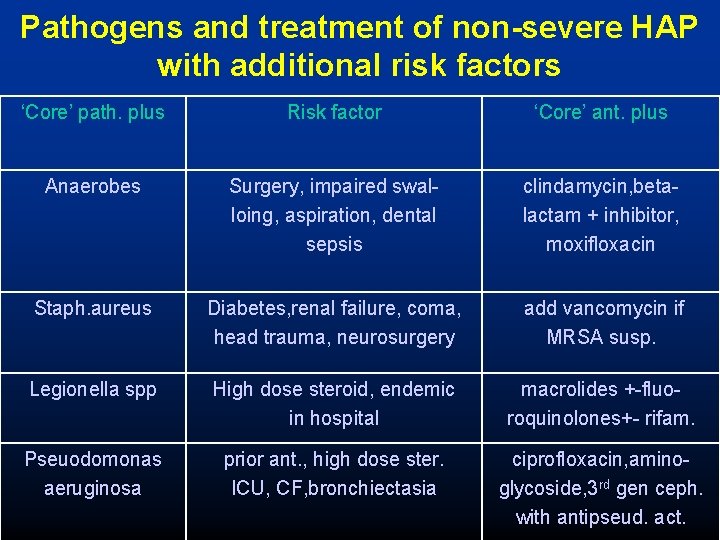
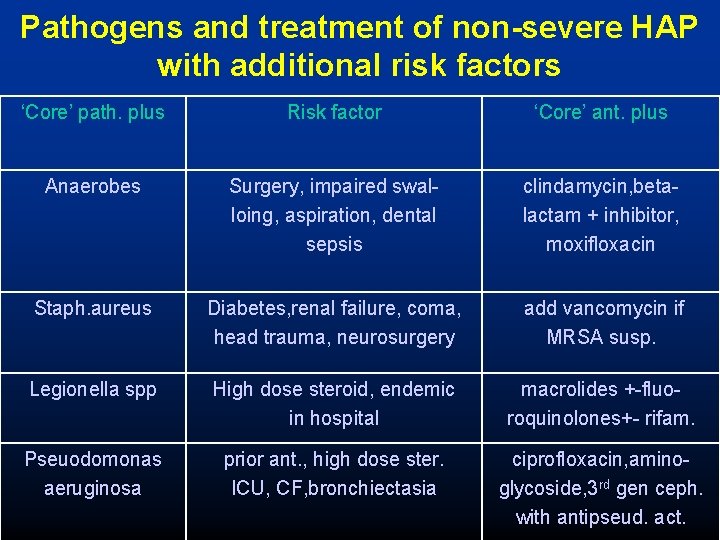
Pathogens and treatment of non-severe HAP with additional risk factors ‘Core’ path. plus Risk factor ‘Core’ ant. plus Anaerobes Surgery, impaired swalloing, aspiration, dental sepsis clindamycin, betalactam + inhibitor, moxifloxacin Staph. aureus Diabetes, renal failure, coma, head trauma, neurosurgery add vancomycin if MRSA susp. Legionella spp High dose steroid, endemic in hospital macrolides +-fluoroquinolones+- rifam. Pseuodomonas aeruginosa prior ant. , high dose ster. ICU, CF, bronchiectasia ciprofloxacin, aminoglycoside, 3 rd gen ceph. with antipseud. act.
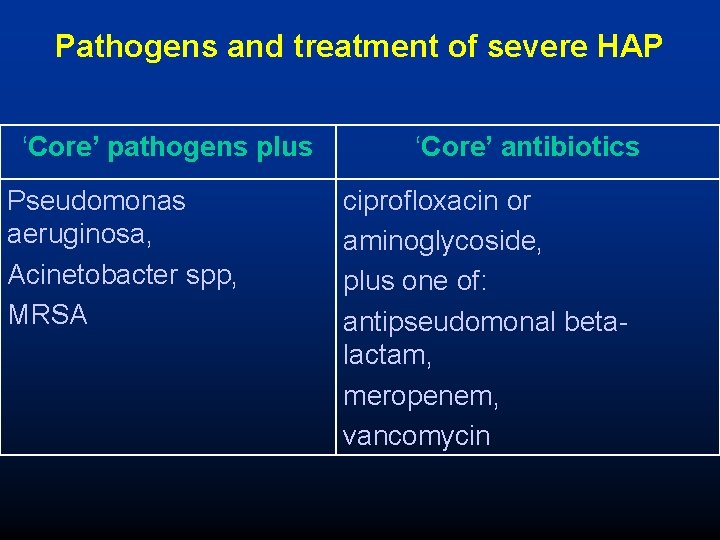
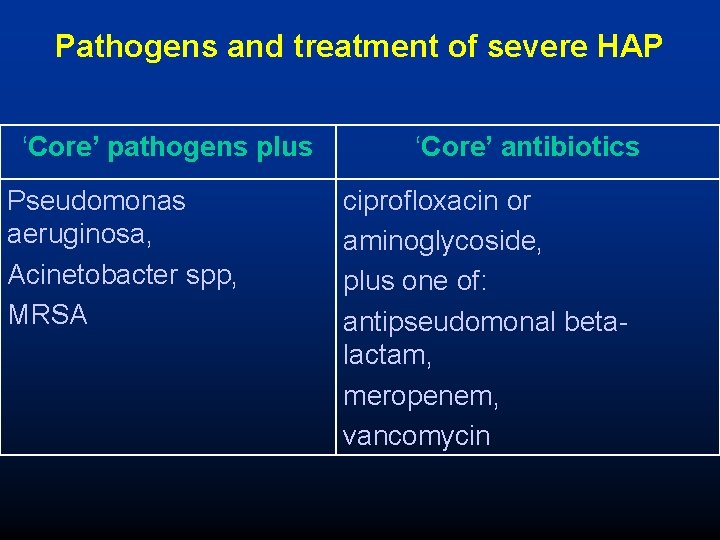
Pathogens and treatment of severe HAP ‘Core’ pathogens plus Pseudomonas aeruginosa, Acinetobacter spp, MRSA ‘Core’ antibiotics ciprofloxacin or aminoglycoside, plus one of: antipseudomonal betalactam, meropenem, vancomycin
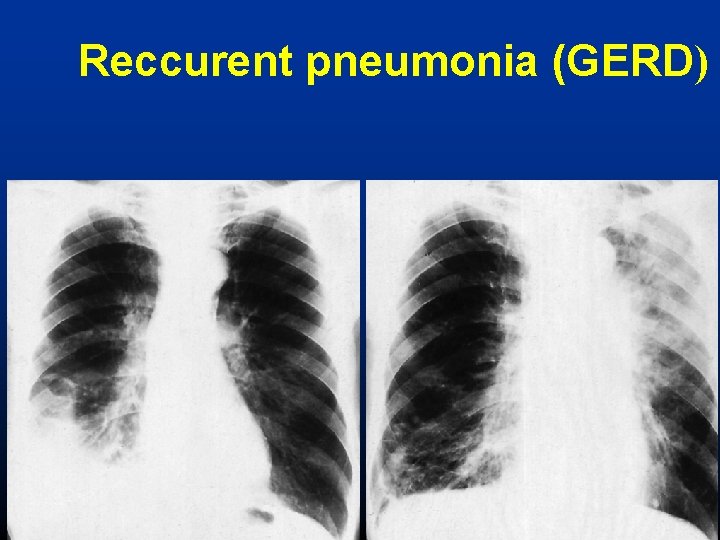
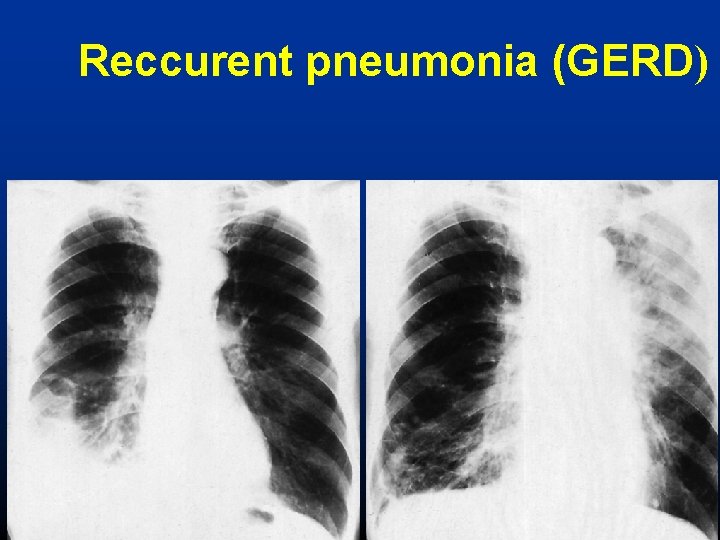
Reccurent pneumonia (GERD)
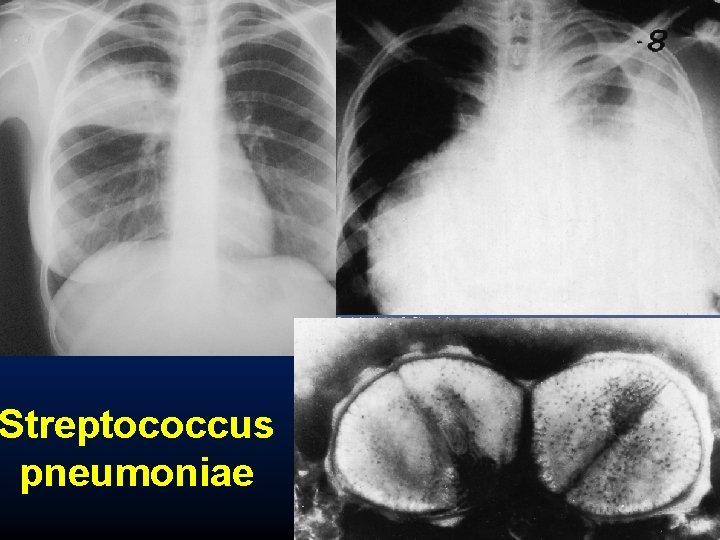
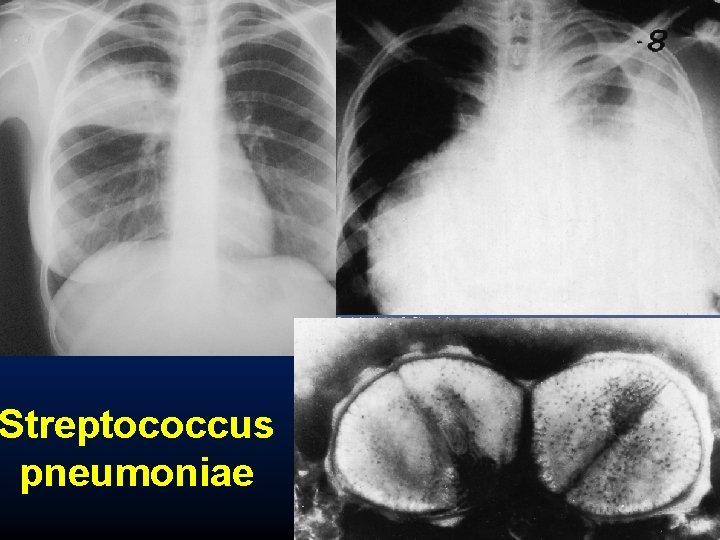
Streptococcus pneumoniae
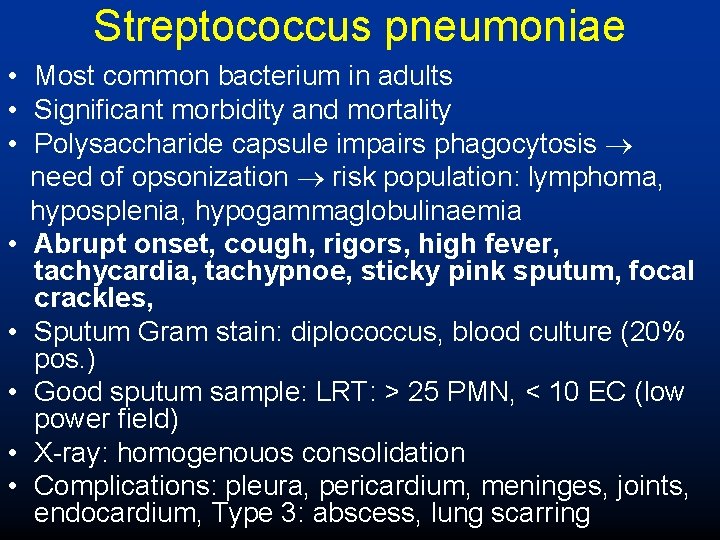
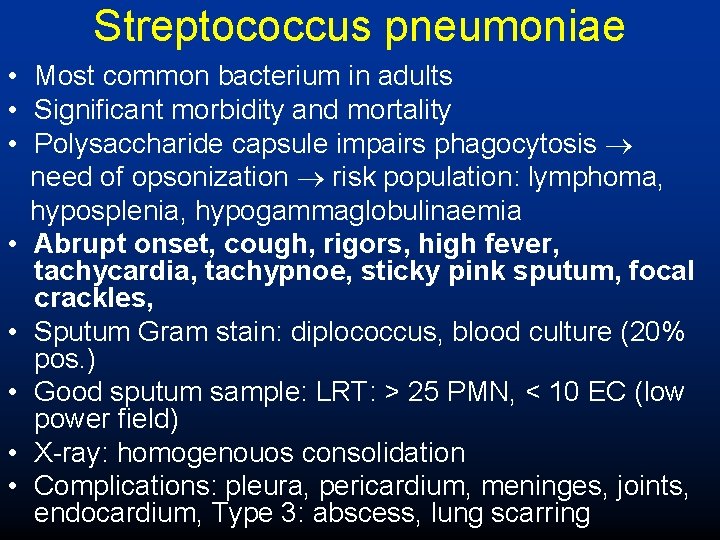
Streptococcus pneumoniae • Most common bacterium in adults • Significant morbidity and mortality • Polysaccharide capsule impairs phagocytosis need of opsonization risk population: lymphoma, hyposplenia, hypogammaglobulinaemia • Abrupt onset, cough, rigors, high fever, tachycardia, tachypnoe, sticky pink sputum, focal crackles, • Sputum Gram stain: diplococcus, blood culture (20% pos. ) • Good sputum sample: LRT: > 25 PMN, < 10 EC (low power field) • X-ray: homogenouos consolidation • Complications: pleura, pericardium, meninges, joints, endocardium, Type 3: abscess, lung scarring
Streptococcus pneumoniae II. • Treatment: – Penicillin, ampicillin, amoxycillin – Cephalosporins 2 -3 gen. – Macrolides – Carbapenems (imipenem, meropenem) • Prevention – 23 or 8 -valent vaccines, 90% adult types – Chronic lung, heart, liver, renal disease, HIV – Diabetes, after spelenctomy, sickle-cell disease
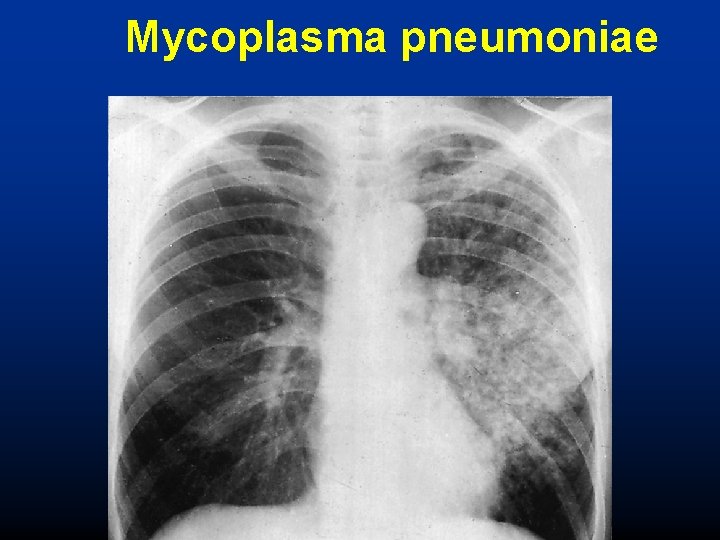
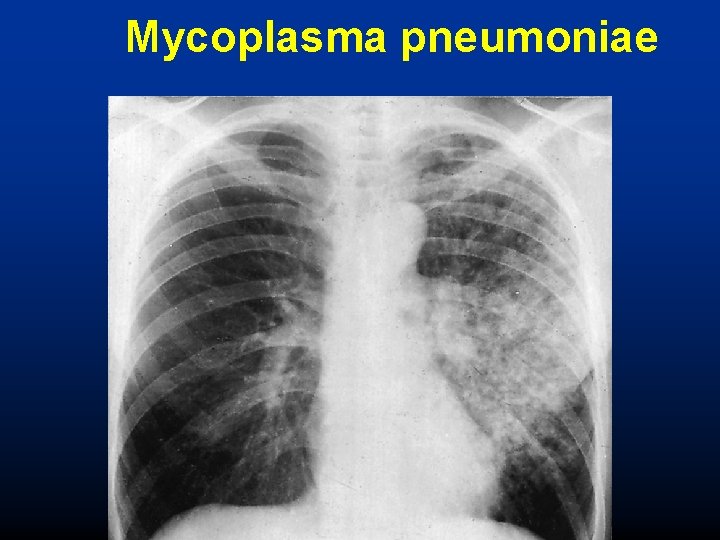
Mycoplasma pneumoniae
Mycoplasma pneumoniae (Atypical pneumonia) • • • Atypical pathogen, moderate morbidity, low mortality Close communities (schools, barracks, dormitories) Intracellular pathogen (Chlamydia, Legionella) Patchy, inhomogenous consolidation on X-ray Extrapulmonary manifestations: lymphadenopathy, cardiac, neurological, skin lesions, gatrointestinal, haematological, musculoskeletal • Treatment: macrolides, tetracyclin, fluoroquinolones
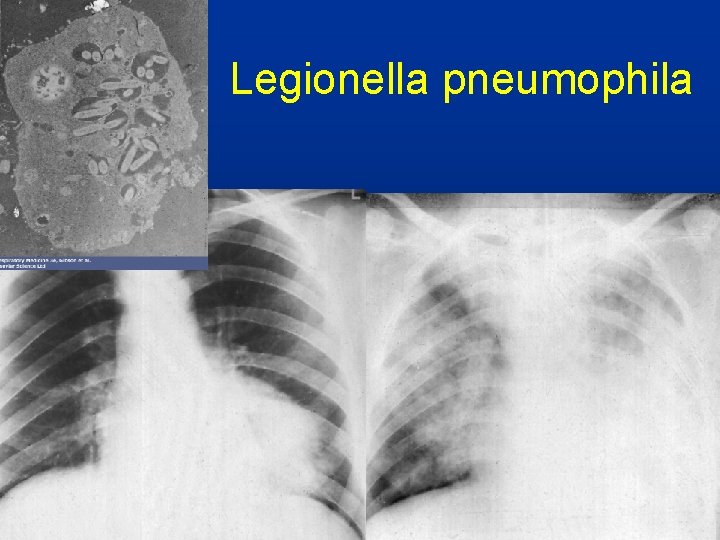
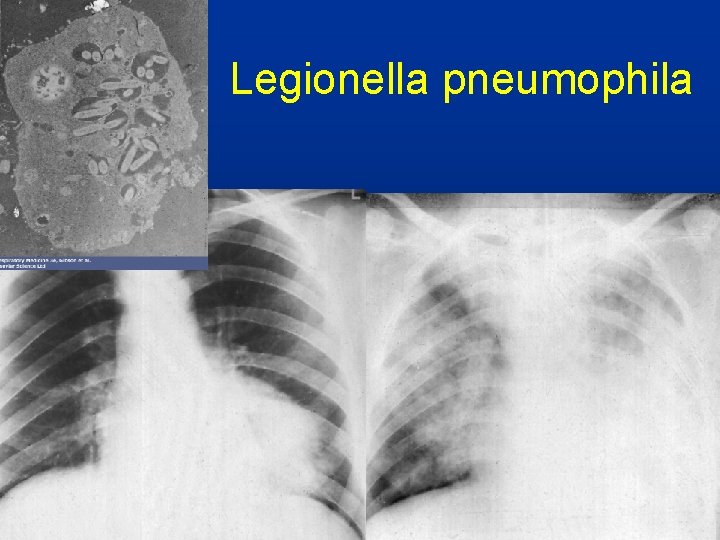
Legionella pneumophila
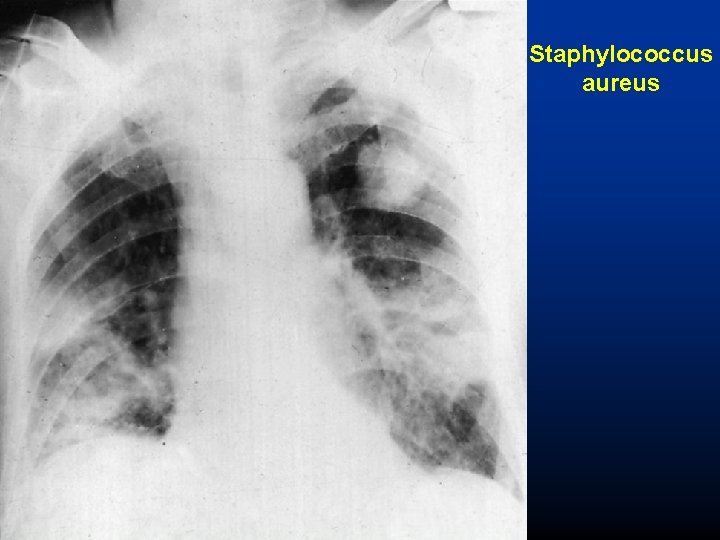
Staphylococcus aureus
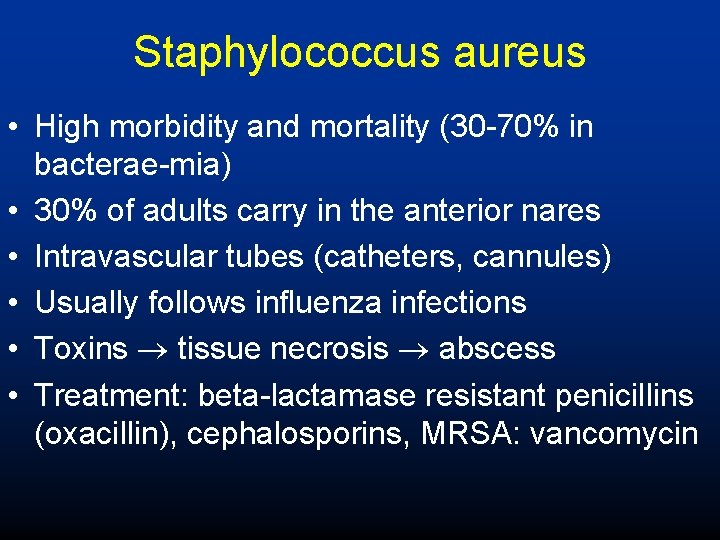
Staphylococcus aureus • High morbidity and mortality (30 -70% in bacterae-mia) • 30% of adults carry in the anterior nares • Intravascular tubes (catheters, cannules) • Usually follows influenza infections • Toxins tissue necrosis abscess • Treatment: beta-lactamase resistant penicillins (oxacillin), cephalosporins, MRSA: vancomycin
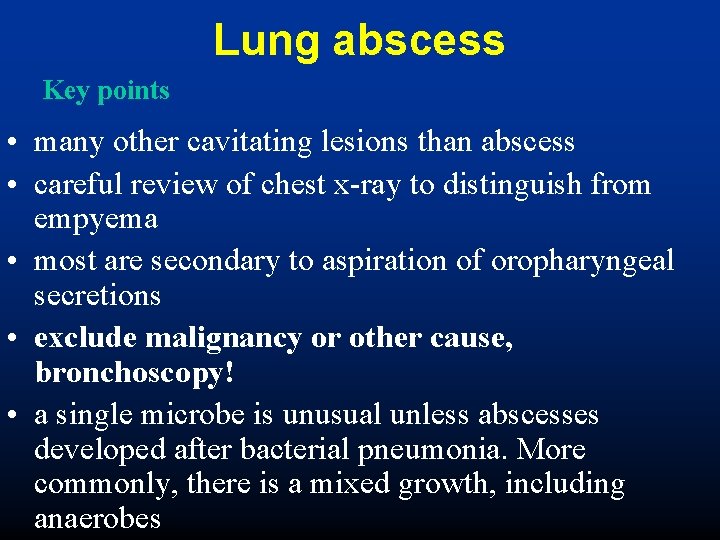
Lung abscess Key points • many other cavitating lesions than abscess • careful review of chest x-ray to distinguish from empyema • most are secondary to aspiration of oropharyngeal secretions • exclude malignancy or other cause, bronchoscopy! • a single microbe is unusual unless abscesses developed after bacterial pneumonia. More commonly, there is a mixed growth, including anaerobes





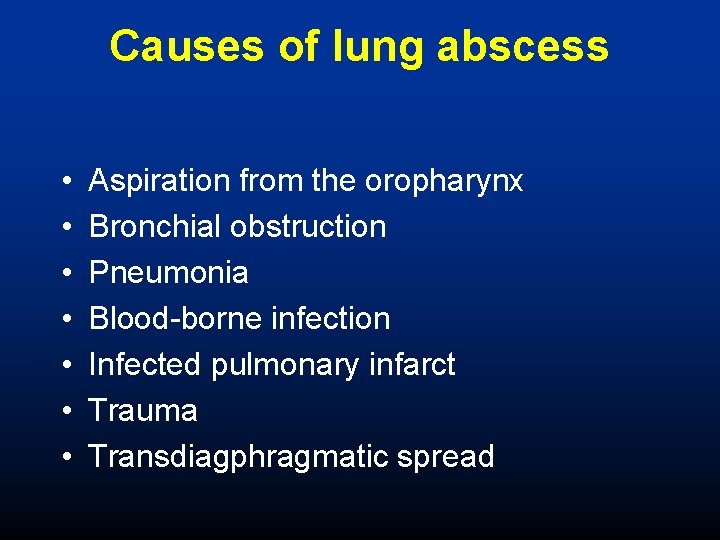
Causes of lung abscess • • Aspiration from the oropharynx Bronchial obstruction Pneumonia Blood-borne infection Infected pulmonary infarct Trauma Transdiagphragmatic spread
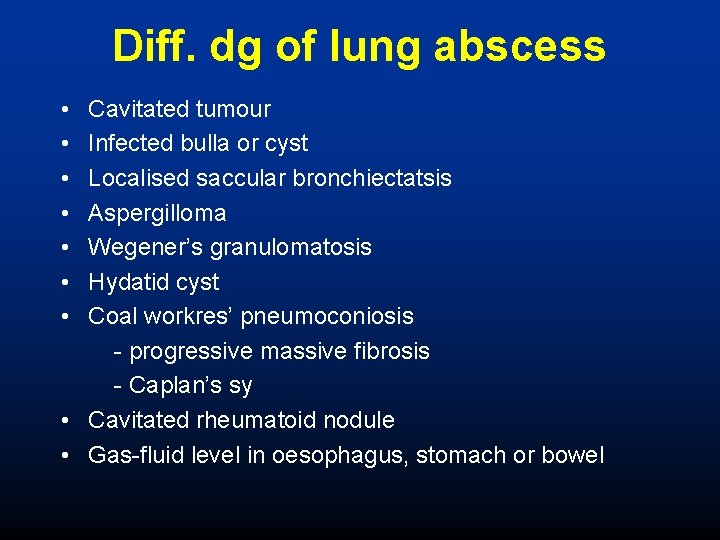
Diff. dg of lung abscess • • Cavitated tumour Infected bulla or cyst Localised saccular bronchiectatsis Aspergilloma Wegener’s granulomatosis Hydatid cyst Coal workres’ pneumoconiosis - progressive massive fibrosis - Caplan’s sy • Cavitated rheumatoid nodule • Gas-fluid level in oesophagus, stomach or bowel
Treatment of lung abscess • Based on bacteriologic findings • Penicillin (amoxicillin/clavulanic acid) • Clindamycin + aminoglycosid (mixed flora) • moxifloxacin
 Cor pulmonale chronicum
Cor pulmonale chronicum Somfay attila
Somfay attila Somfay attila
Somfay attila Dr somfay attila
Dr somfay attila Uhs pulmonology
Uhs pulmonology Anterior axillary line
Anterior axillary line Fcps pulmonology
Fcps pulmonology Pne/o medical term
Pne/o medical term Dr mester lajos szeged
Dr mester lajos szeged Polyuria okai
Polyuria okai Központi adatnyilvántartás lekérdezés
Központi adatnyilvántartás lekérdezés Gábor dénes szeged szakok
Gábor dénes szeged szakok Neurológiai klinika szeged
Neurológiai klinika szeged Szeged
Szeged Tankerület szeged
Tankerület szeged Határrendészeti kirendeltség szeged
Határrendészeti kirendeltség szeged Foramen rotundum ct
Foramen rotundum ct Pt dept logistik
Pt dept logistik La revenue dept
La revenue dept Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Poster affiliation
Poster affiliation Finance dept structure
Finance dept structure Dept ind onegov
Dept ind onegov Rowan county medicaid transportation
Rowan county medicaid transportation La city fire interview
La city fire interview Department of finance and administration
Department of finance and administration Rewley house continuing education library
Rewley house continuing education library Nys department of homeland security
Nys department of homeland security Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Vaginal dept
Vaginal dept Gome dept
Gome dept Worcester plumbing inspector
Worcester plumbing inspector Albany county dss
Albany county dss Dept of education
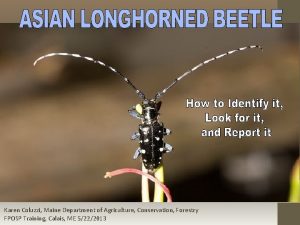
Dept of education Maine dept of agriculture
Maine dept of agriculture Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) Dept nmr spectroscopy
Dept nmr spectroscopy Nebraska dept of agriculture
Nebraska dept of agriculture Dept a
Dept a Gome dept
Gome dept Gome dept
Gome dept Dept. name of organization
Dept. name of organization Bromocicloesano
Bromocicloesano Affiliate disclodures
Affiliate disclodures Dept of education
Dept of education Ohio dept of dd
Ohio dept of dd Fl dept of agriculture
Fl dept of agriculture Iit
Iit Central islip fire department
Central islip fire department Gome dept
Gome dept