COACH A Novel Approach for Improving Access to




- Slides: 47
COACH A Novel Approach for Improving Access to Care for Frail Seniors in PEI
Dr. Tim Stultz MD COE, Kirsten Mallard NP Provincial Geriatric Program Making the Connection Oct. 16, 2015
The Problems of Aging
What is the COACH Team? Caring for Older Adults in Community and at Home • Integrated, interdisciplinary expert team with the frail senior patient/client at the centre • Created through stronger collaboration of existing resources in three partner programs (Home Care, Geriatric Program, Primary Care) • Does not replace referral to Geriatric Program • Separate stream for small group of most complex patients/clients to pilot the team approach
Evidence from Other Jurisdictions • Project work began with consideration of best practice models of care and approaches in other provinces • Development of COACH Team benefited from learning from 2 teams • Integrated Client Care Program (Toronto, ON) – partnership between Primary Care and Home Care • Care for Seniors Program (North Perth, ON) – Nurse Practitioner led partnership between Primary Care, Home Care and Geriatric Program
Objectives of the COACH Team • Improve access to care for frail seniors • Increase awareness and expertise re: complex geriatric syndromes • Improve quality of care for frail seniors and their family/caregivers
• Who is on the COACH Team? Core members: • Geriatric Program Nurse Practitioner
Role of the Geriatric Program NP in COACH The “glue” between the programs and services • Comprehensive Geriatric Assessment • 1. 5 to 2 hours to complete • Medical and social history, current meds, physical exam and functional, cognitive and mood assessments • Expertise on complex geriatric syndromes • Strong focus on communication, integration and collaboration • Credentials: • Clinical training with Geriatricians • Collaborative member of Geriatric Program team
• Who is on the COACH Team? Core members: • Geriatric Program Nurse Practitioner • Family physician
Role of Primary Care Physician and NP in COACH • Maintain lead on medical care for patients • Provide feedback/input on proposed team model and processes • Provide feedback on patients identified to participate in pilot • Work collaboratively with the team and share information on patients • Provide feedback/input to the evaluation of the pilot
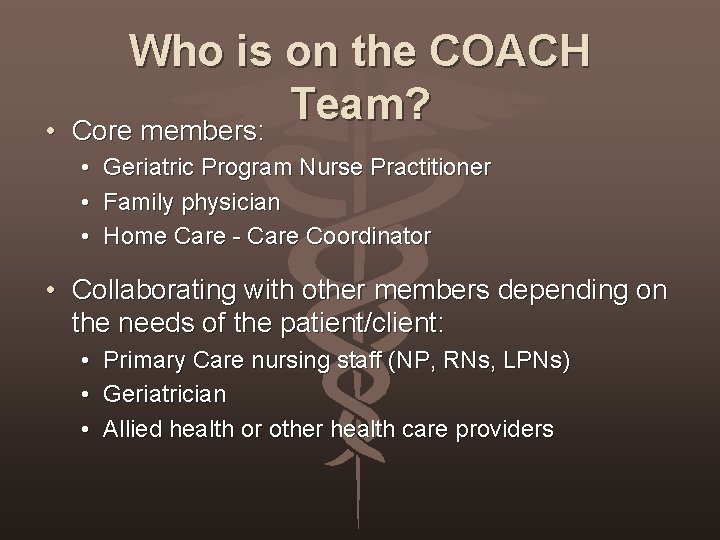
• Who is on the COACH Team? Core members: • • • Geriatric Program Nurse Practitioner Family physician Home Care - Care Coordinator • Collaborating with other members depending on the needs of the patient/client: • • • Primary Care nursing staff (NP, RNs, LPNs) Geriatrician Allied health or other health care providers
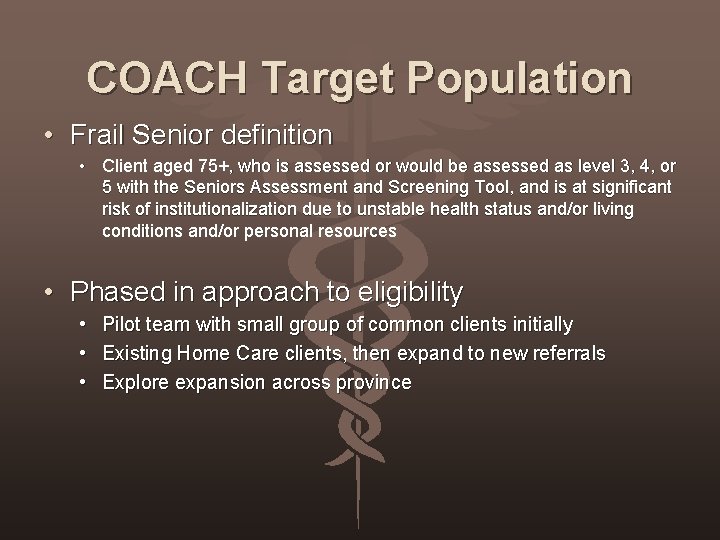
COACH Target Population • Frail Senior definition • Client aged 75+, who is assessed or would be assessed as level 3, 4, or 5 with the Seniors Assessment and Screening Tool, and is at significant risk of institutionalization due to unstable health status and/or living conditions and/or personal resources • Phased in approach to eligibility • • • Pilot team with small group of common clients initially Existing Home Care clients, then expand to new referrals Explore expansion across province
Pilot Participants • Existing Home Care frail senior clients who are also a patient of Montague Health Centre (approximately 60 total common clients) • For pilot, focusing on 15 to 20 individuals with highest complexity, based on: • Inpatient admissions • Visits to ER • Office visits to primary care • Previous referral to Geriatric Program • Feedback/input from physicians
Functions of COACH Team • Comprehensive geriatric assessment • Home visits • Connect with patient in hospital and timely post-discharge follow up • Facilitating collaborative care planning and Advance Care Plan • Sharing of information for smoother transitions of care • Priority access to enhanced Home Care resources, Geriatric Program Nurse Practitioner and Geriatrician (collaboration or consult, as required) • Teaching/support to client, family/caregivers and health care providers on complex geriatric syndromes
Other pilot objectives - COACH Team • Develop Frail Senior Care Pathway • Validate team model and processes • Develop efficient documentation and communication processes • Define eligibility criteria and plan for growth/expansion of COACH post-pilot
Pilot Timelines • Pilot from January to October 2015 • Preliminary evaluation – April 2015 • Also ongoing evaluation throughout pilot, using quality improvement approach • Full evaluation at end of pilot

MY ROLE
First Steps… • Once identified through Home Care & after consultation with Family Physicians… • Phone call to patient and/or caregiver to seek consent and arrange for initial home visit. • CGA’s completed on every COACH patient over the first few months.
First Steps… Prior to visiting home: Review Paper chart from clinic looking at PMHX, medications, resources in home if any. Review ISM (Home Care Chart), Drug information system (DIS), Cerner for blood work, recent hospital documents related to admissions, ER visits, specialty consultations. Communicate with team members involved.
Comprehensive Geriatric Assessment (CGA) • • • Listen!!! HPI… Review of medical and social history Chronic diseases Current medications Physical examination Functional assessment (ADL’s & IADL’s) Cognitive assessment Mood assessment/Sleep/Appetite Home Supports/Resources Discussion around Advanced Care Planning
Focus… Complex Geriatric Syndromes such as delirium, depression, varying stages of dementia (BPSD), falls, de-conditioning, mobility, incontinence, functional decline, medications. Guidelines (HTN, Diabetes) Recommendations often around symptom management, sleep disturbance, medications, community resources, Home Care Services, Catastrophic drug plan, etc.
All This Info…. . Focus is to really look at the information collected and stick to the objectives of COACH which is to… • Improve access to care for frail seniors • Increase awareness and expertise re: complex geriatric syndromes • Improve quality of care for frail seniors and their family/caregivers

Integrated Team
As Part of This Project… • Consulted collaborating Geriatrician as needed. • Really made an effort to connect with the Family Physician to collaborate & discuss recommendations. • Jointly with Home Care Coordinator created the plan of care. • Patient/Care Giver involved in decision making process and care plan. • Ongoing Support to Patient & Family
COACH • The NP works with other sectors across the continuum to coordinate care and support patients as they transition between sectors, including home, emergency, acute care, community care, LTC, Respite, Restorative. (Dr. Prasad et al. , 2013) • Use SBAR to communicate.
COACH CASE – Mrs. J
Mrs. J o 79 year old lady, lives with spouse, who is currently on dialysis. Assessed by Geriatrics in the past and diagnosed with Mixed Dementia in 2012. Noted Functional decline since then & today has findings of low mood & mild agitation. Also congested cough present. o Collateral information from son who is the primary caregiver. No other family on Island.
Functional Status o She sponge bathes herself twice a week (? ) and feels she does not need anymore assistance. o Tried home support and inconsistent with service. Declined Day Program. o Incontinent of urine at times. o Unsteady on feet, has had 2 falls 6 -12 months and now uses a walker. Increased difficulty transferring from sitting to standing. o All IADL’s by caregiver. Prompting with ADL’s
PMHX o o o o Epilepsy (1945) ? Hypothyroidism – resolved HTN Chronic Vertigo Osteoporosis Mild COPD Appendectomy, Tubal Ligation, Rt. & Lt. Cataract removed, thoracic kyphosis, ? Parkinsons 2011
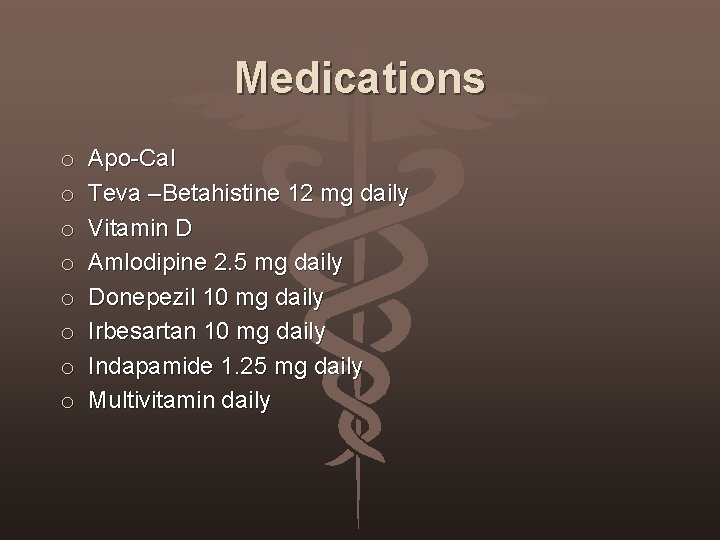
Medications o o o o Apo-Cal Teva –Betahistine 12 mg daily Vitamin D Amlodipine 2. 5 mg daily Donepezil 10 mg daily Irbesartan 10 mg daily Indapamide 1. 25 mg daily Multivitamin daily
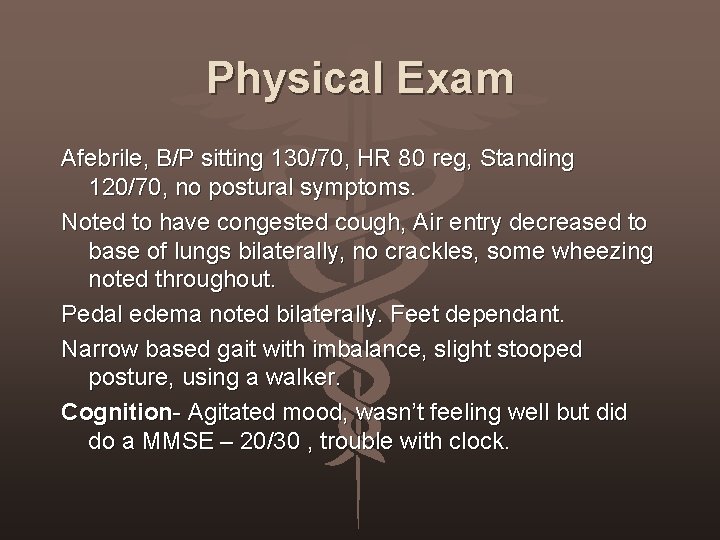
Physical Exam Afebrile, B/P sitting 130/70, HR 80 reg, Standing 120/70, no postural symptoms. Noted to have congested cough, Air entry decreased to base of lungs bilaterally, no crackles, some wheezing noted throughout. Pedal edema noted bilaterally. Feet dependant. Narrow based gait with imbalance, slight stooped posture, using a walker. Cognition- Agitated mood, wasn’t feeling well but did do a MMSE – 20/30 , trouble with clock.
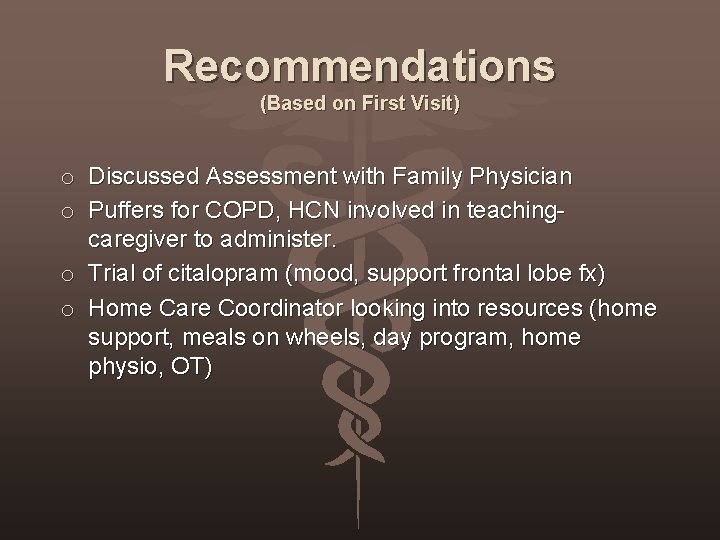
Recommendations (Based on First Visit) o Discussed Assessment with Family Physician o Puffers for COPD, HCN involved in teachingcaregiver to administer. o Trial of citalopram (mood, support frontal lobe fx) o Home Care Coordinator looking into resources (home support, meals on wheels, day program, home physio, OT)
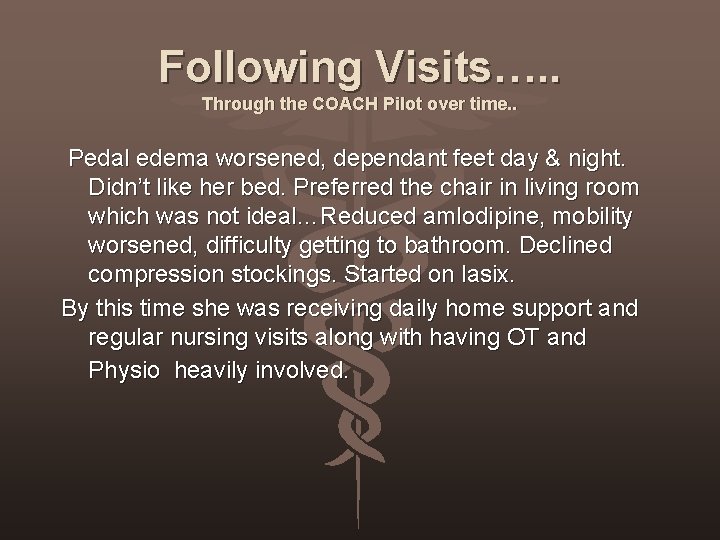
Following Visits…. . Through the COACH Pilot over time. . Pedal edema worsened, dependant feet day & night. Didn’t like her bed. Preferred the chair in living room which was not ideal…Reduced amlodipine, mobility worsened, difficulty getting to bathroom. Declined compression stockings. Started on lasix. By this time she was receiving daily home support and regular nursing visits along with having OT and Physio heavily involved.
Home Care Coordinator very involved working with Caregiver in an attempt to control her edema. Fell in the bathroom, injured her leg which impacted her mobility. Family physician away. Visit to Emerg for xray and rule out fracture. But… Able to send an SBAR to Emergency doc with update to communicate issues. Was admitted. Able to make some medication adjustments with some improvement and then discussed taking a Restorative Approach
Different covering physician. Agreed to plan, family consented. Contacted another physician to see if he would accept the transfer to Colville…she was then transferred for Respite specifically for a restorative approach. Team from LTC, Home Care, Family met at the facility, reviewed function and goals of care. Able to get her measured for compression hose. Noted BIG improvement to her lower legs/feet. Reduced lasix. Mobility improved substantially. During her respite able to have equipment put in at home and caregiver was rejuvinated. Discharged home in two weeks.
Other Examples…. • • • Medication changes/adjustments in consultation with GP’s. . educating families, staff on side effects and routine follow up. Did it improve/decrease symptoms? Regular contact with Care Coordinator – knowing who to call. Mrs. C with very vascular presentation of dementia, challenging symptoms. Team involved to organize increased service to avoid hospitalization following an arm fracture. Mr. C patient in his early 90’s living with his sister who has dementia…he was adamant about staying home, difficult to get him to see his GP, team collaborated heavily. Mr. H caregiver indicated that before COACH he was admitted monthly to hospital. She is feeling supported and this has not happened since the pilot began. Team has identified that patients have little awareness around Catastrophic drug plan so was able to introduce this (coverage for diabetic meds, antipsychotics, dementia meds, etc. )
Ongoing Support • Regularly followed by care coordination and home care services. • Updates provided to Family Doctors. • Rounds every Weds morning with Team to discuss Coach patients and Care Plans. Access to Geriatrician. • Family supported. • Connect with Acute Care for inpatient assessment & discharge follow up. Involved in Care Planning.
Other Benefits • Staff education around complex Geriatric Syndromes and use of medications. Importance of CGA. • Family education regarding Dementia & common Geriatric conditions. • Continuity of Care. • Email Alert of Acute Care Admission • Team Support - Collaboration!
Identified Challenges • • Admin/office/charts Communication/Documentation Lack of shared electronic chart COACH NP or Family Physician role with patient health issues. • Availability • Identified that if we are going to support these frail older adults at home, more Home Care resources are needed (respite, access to evening & night cares)
As Part of This Project… • Consulted collaborating Geriatrician as needed. • Really made an effort to connect with the Family Physician to collaborate & discuss recommendations. • Jointly with Home Care Coordinator created the plan of care. • Patient/Care Giver involved in decision making process and care plan. • Ongoing Support to Patient & Family
Evaluation
Evaluation • Overwhelmingly positive • Reductions in drugs- improved physical and mental wellbeing • Home visit repeatedly cited as key feature of the program • Skills of NP were exceptional
Evaluation • Only recommendations: • • More NP’s More respite

Donepezil$40/month Rollator Walker$300 Having COACH come to your HOME - PRICE LESS!!

Currently Geriatricians NP Geriatrics Restorative care west COACH Queens COACH Prince Vision Integrated Seamless Acute care Restorative care COACH Restorative Home care east Palliative care Restorative care PCH Restorative care PE Home COACH Kings
Questions?