Cardiovascular Disease in Women Tara Dall MD FNLA




- Slides: 96
Cardiovascular Disease in Women Tara Dall, MD, FNLA Diplomate, American Board of Clinical Lipidology Medical Director, President Advanced Lipidology Delafield, WI www. advlip. com
Objectives • Discuss strategies to assess and stratify women into high risk, at risk, and ideal health categories for cardiovascular disease (CVD) • Review the American Heart Association (AHA) 2011 Guidelines approaches to CVD prevention for patients with hypertension, lipid abnormalities, and diabetes, with a focus on effectiveness in practice • Review the AHA 2011 Guidelines approach to pharmacological intervention for women at risk for cardiovascular events • Summarize commonly used therapies that should not be initiated for the prevention or treatment of CVD, because they lack benefit, or because risks outweigh benefits
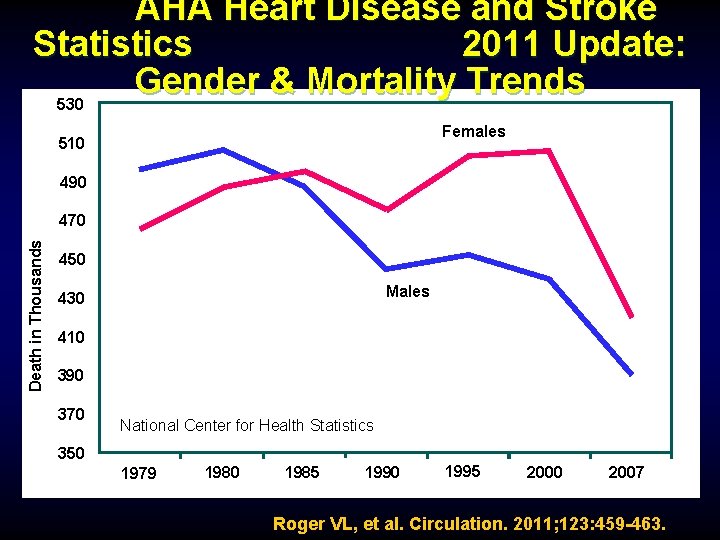
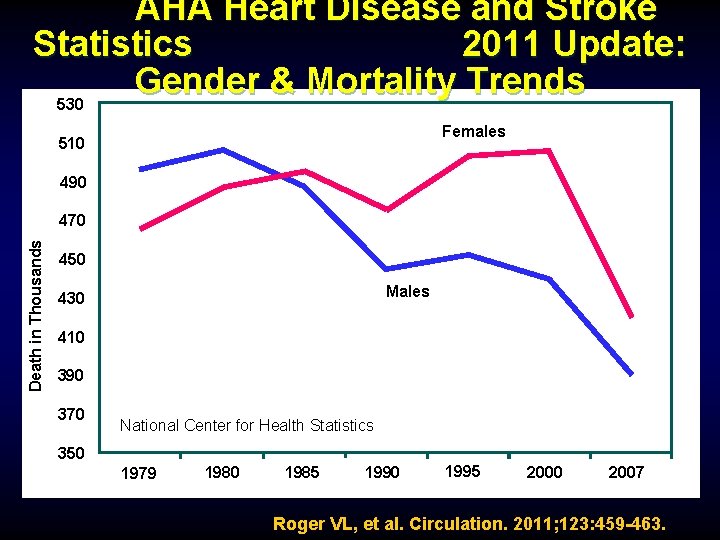
AHA Heart Disease and Stroke Statistics 2011 Update: Gender & Mortality Trends 530 Females 510 490 Death in Thousands 470 450 Males 430 410 390 370 National Center for Health Statistics 350 1979 1980 1985 1990 1995 2000 2007 Roger VL, et al. Circulation. 2011; 123: 459 -463.
AHA CVD Prevention Guidelines for Women CVD Challenges ► Evolving science suggests that the overwhelming majority of recommendations to prevent CVD are similar for women and men ► Notably aspirin is recommended for primary prevention of MI for men but not for women. ► Stroke accounts for a higher proportion of CVD events than CHD in females whereas the ratio is opposite for males (pregnancy, hormone therapy, atrial fibrillation & hypertension at age 65 or above) Mosca, L. et al. Circulation 2011; 123:
Differences in Heart Attack Symptoms Men • chest pain or pressure • Rest pain • Pain down left arm and shoulder • Weakness Women • Pain in chest, upper back, jaw or neck • Shortness of breath • Flu-like symptoms: nausea or vomiting, cold sweats • Stomachache , Gas • Fatigue or weakness • Feelings of anxiety, loss of appetite, malaise
Lipids and CVD Risk in Women • High risk lipid profile differs from that of men – Low HDL strongly and independently correlated with risk for CVD death – High Triglycerides are independent risk factor for CVD death • After age 45, greater prevalence in women of high total cholesterol • Lowering LDL-C reduces risk equivalently in women and men
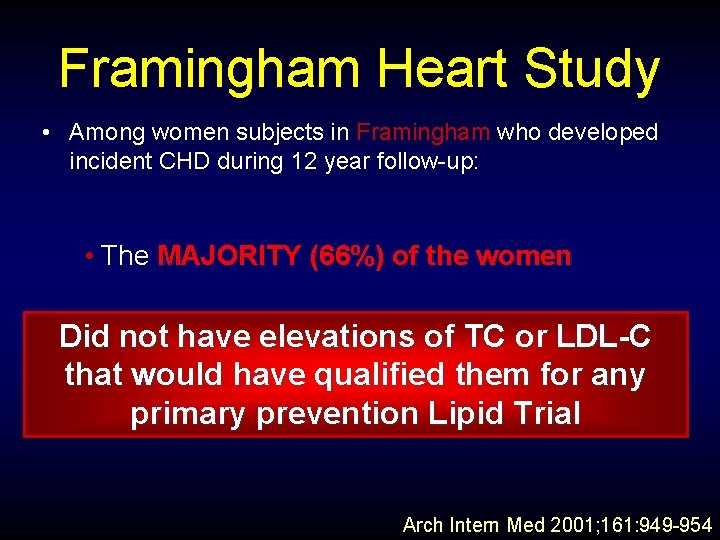
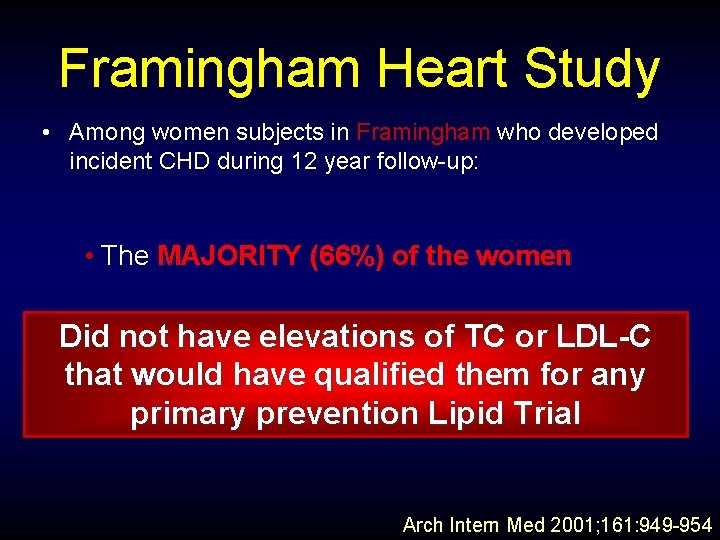
Framingham Heart Study • Among women subjects in Framingham who developed incident CHD during 12 year follow-up: • The MAJORITY (66%) of the women Did not have elevations of TC or LDL-C that would have qualified them for any primary prevention Lipid Trial Arch Intern Med 2001; 161: 949 -954
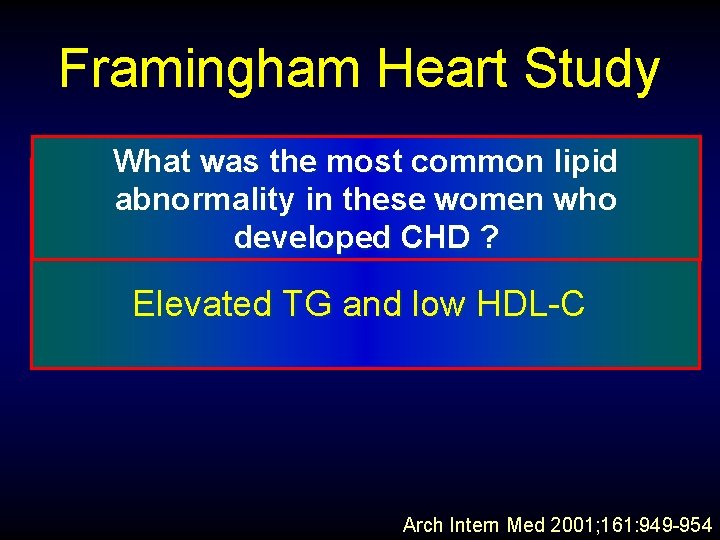
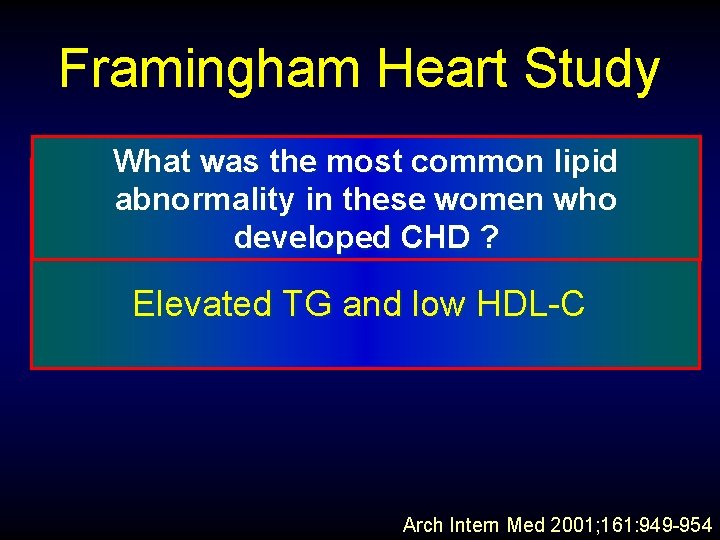
Framingham Heart Study What was the most common lipid Isolated hypertriglyceridemia abnormality in these women who (>200 mg. CHD /dl) ? developed Elevated TG and low HDL-C Arch Intern Med 2001; 161: 949 -954
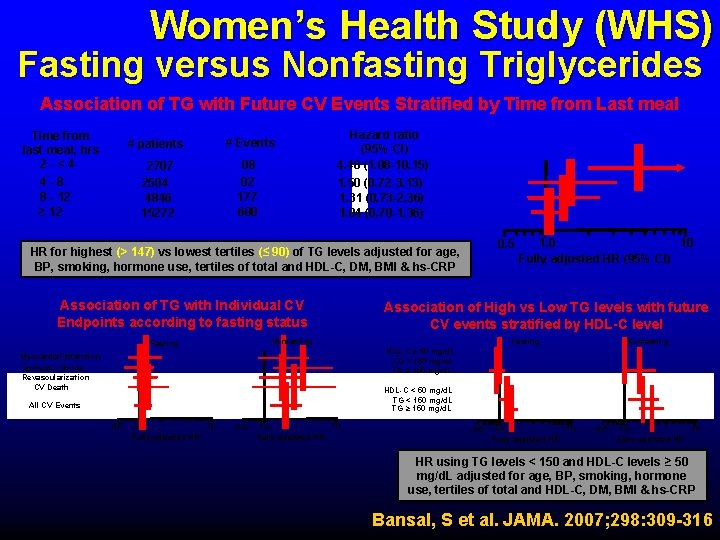
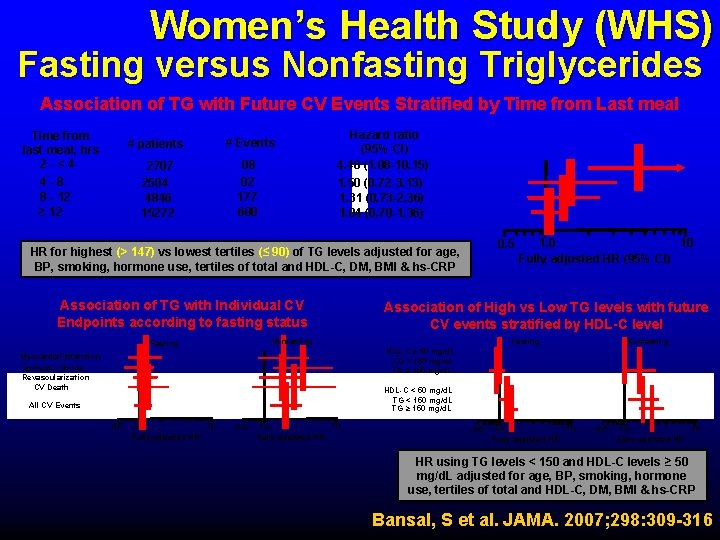
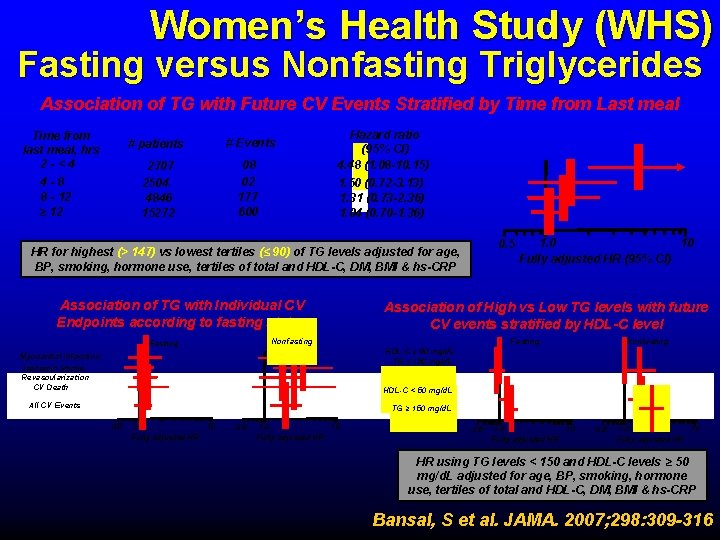
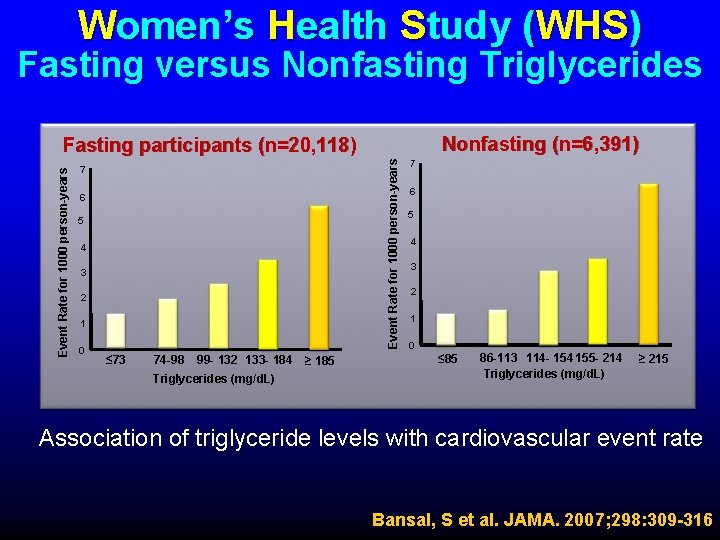
Women’s Health Study (WHS) Fasting versus Nonfasting Triglycerides Association of TG with Future CV Events Stratified by Time from Last meal Time from last meal, hrs 2 -<4 4 -8 8 - 12 ≥ 12 # patients # Events 2707 2504 4846 15272 08 02 177 600 Hazard ratio (95% CI) 4. 48 (1. 08 -10. 15) 1. 50 (0. 72 -3. 13) 1. 31 (0. 73 -2. 36) 1. 04 (0. 70 -1. 36) 0. 5 HR for highest (> 147) vs lowest tertiles (≤ 90) of TG levels adjusted for age, BP, smoking, hormone use, tertiles of total and HDL-C, DM, BMI & hs-CRP Association of TG with Individual CV Endpoints according to fasting status Association of High vs Low TG levels with future CV events stratified by HDL-C level Fasting Nonfasting Fasting 10 1. 0 Fully adjusted HR (95% CI) Nonfasting HDL-C ≥ 50 mg/d. L TG < 150 mg/d. L TG ≥ 150 mg/d. L Myocardial Infarction Ischemic Stroke Revascularization CV Death HDL-C < 50 mg/d. L TG < 150 mg/d. L TG ≥ 150 mg/d. L All CV Events 0. 5 1. 0 10 Fully adjusted HR HR using TG levels < 150 and HDL-C levels ≥ 50 mg/d. L adjusted for age, BP, smoking, hormone use, tertiles of total and HDL-C, DM, BMI & hs-CRP Bansal, S et al. JAMA. 2007; 298: 309 -316
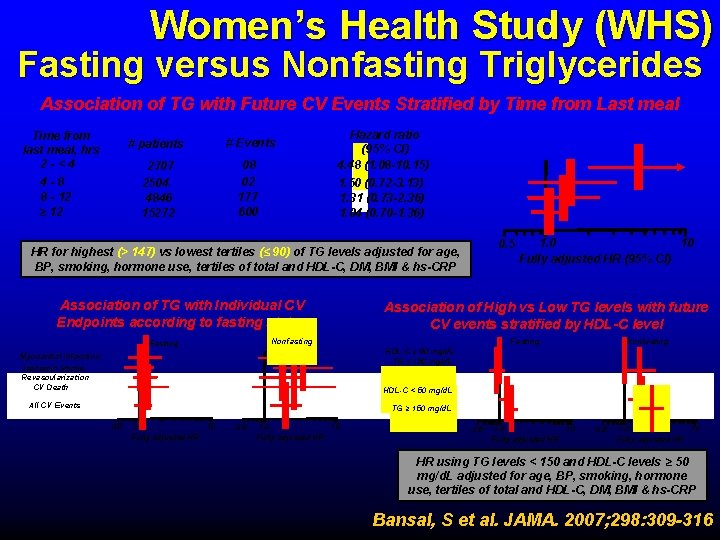
Women’s Health Study (WHS) Fasting versus Nonfasting Triglycerides Association of TG with Future CV Events Stratified by Time from Last meal Time from last meal, hrs 2 -<4 4 -8 8 - 12 ≥ 12 # patients # Events 2707 2504 4846 15272 08 02 177 600 Hazard ratio (95% CI) 4. 48 (1. 08 -10. 15) 1. 50 (0. 72 -3. 13) 1. 31 (0. 73 -2. 36) 1. 04 (0. 70 -1. 36) 0. 5 HR for highest (> 147) vs lowest tertiles (≤ 90) of TG levels adjusted for age, BP, smoking, hormone use, tertiles of total and HDL-C, DM, BMI & hs-CRP Association of TG with Individual CV Endpoints according to fasting status Association of High vs Low TG levels with future CV events stratified by HDL-C level Fasting Nonfasting Fasting 10 1. 0 Fully adjusted HR (95% CI) Nonfasting HDL-C ≥ 50 mg/d. L TG < 150 mg/d. L TG ≥ 150 mg/d. L Myocardial Infarction Ischemic Stroke Revascularization CV Death HDL-C < 50 mg/d. L TG < 150 mg/d. L TG ≥ 150 mg/d. L All CV Events 0. 5 1. 0 10 Fully adjusted HR HR using TG levels < 150 and HDL-C levels ≥ 50 mg/d. L adjusted for age, BP, smoking, hormone use, tertiles of total and HDL-C, DM, BMI & hs-CRP Bansal, S et al. JAMA. 2007; 298: 309 -316
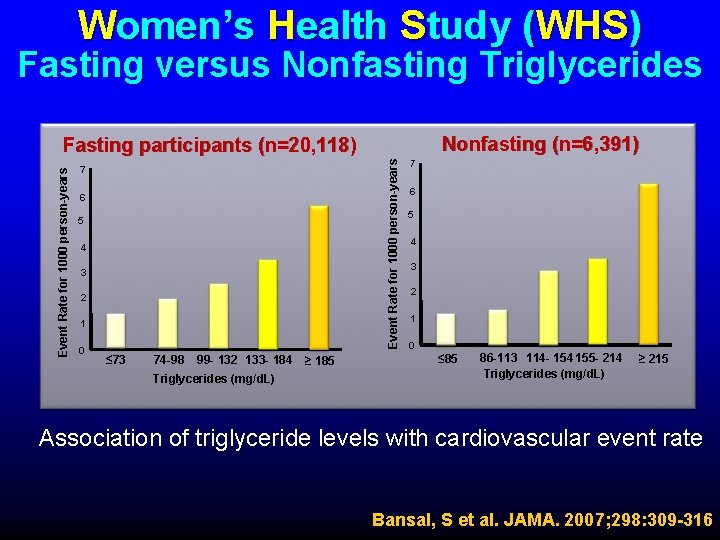
Women’s Health Study (WHS) Fasting versus Nonfasting Triglycerides Nonfasting (n=6, 391) Event Rate for 1000 person-years Fasting participants (n=20, 118) 7 6 5 4 3 2 1 0 ≤ 73 74 -98 99 - 132 133 - 184 Triglycerides (mg/d. L) ≥ 185 7 6 5 4 3 2 1 0 ≤ 85 86 -113 114 - 154 155 - 214 Triglycerides (mg/d. L) ≥ 215 Association of triglyceride levels with cardiovascular event rate Bansal, S et al. JAMA. 2007; 298: 309 -316
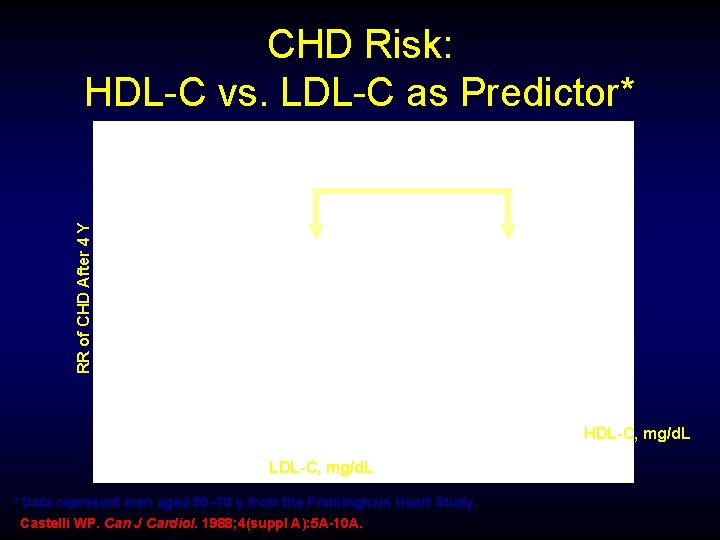
RR of CHD After 4 Y CHD Risk: HDL-C vs. LDL-C as Predictor* HDL-C, mg/d. L LDL-C, mg/d. L * Data represent men aged 50– 70 y from the Framingham Heart Study. Castelli WP. Can J Cardiol. 1988; 4(suppl A): 5 A-10 A.
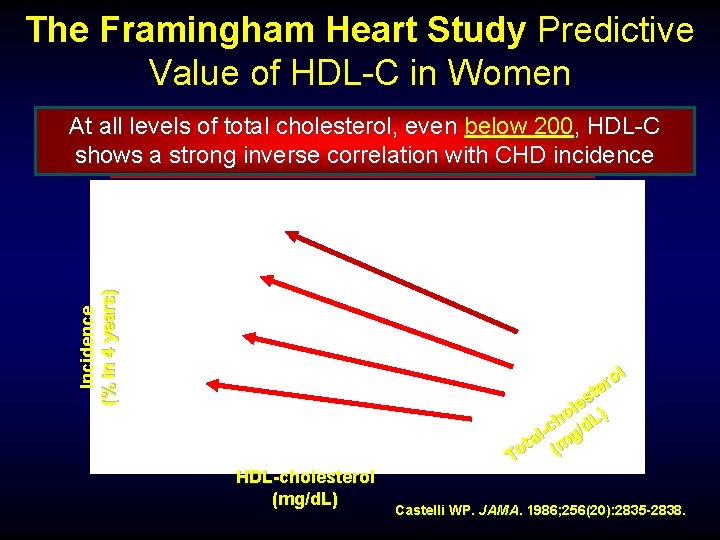
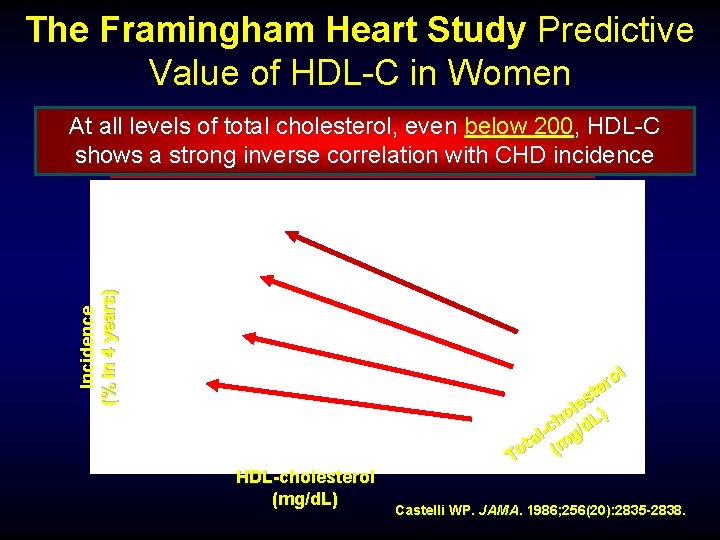
The Framingham Heart Study Predictive Value of HDL-C in Women Incidence (% in 4 years) At all levels total cholesterol, even below<45 200, HDL-C Twiceofas many women with HDL-C andinverse women without history shows a. Men strong correlation with CHD incidence mg/d. L suffered an MI over. CHD 4 years ol r te s le ) o L h -c g/d l ta (m o T HDL-cholesterol (mg/d. L) Castelli WP. JAMA. 1986; 256(20): 2835 -2838.
High HDL Protective? Not always?
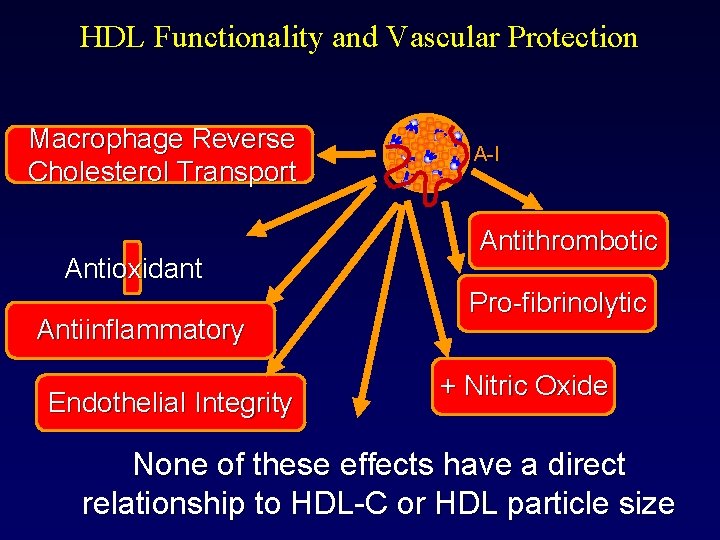
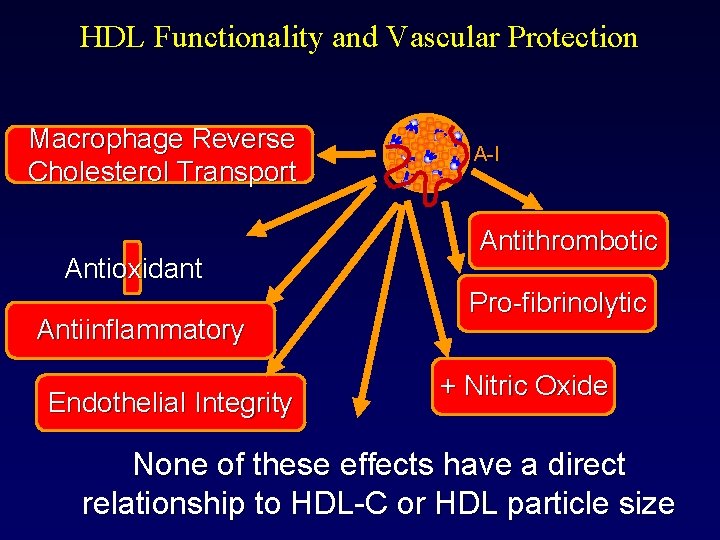
HDL Functionality and Vascular Protection Macrophage Reverse Cholesterol Transport Antioxidant Antiinflammatory Endothelial Integrity A-I Antithrombotic Pro-fibrinolytic + Nitric Oxide None of these effects have a direct relationship to HDL-C or HDL particle size
DYSFUNCTIONAL HDL-C New concept especially in setting of insulin resistance
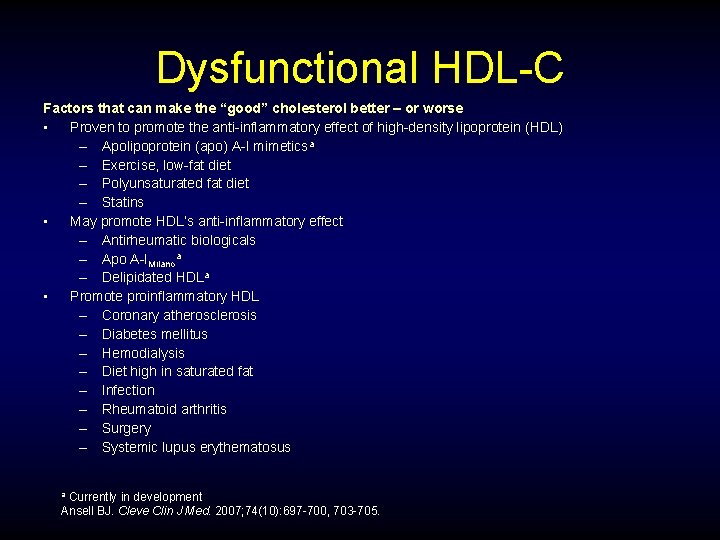
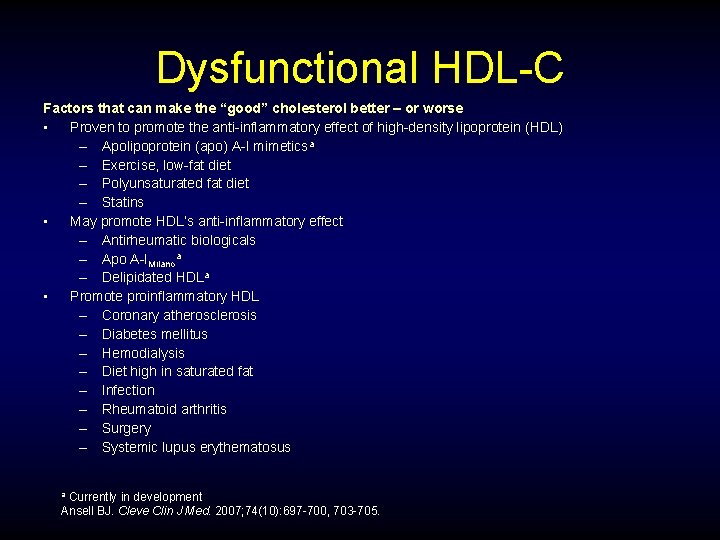
Dysfunctional HDL-C Factors that can make the “good” cholesterol better – or worse • Proven to promote the anti-inflammatory effect of high-density lipoprotein (HDL) – Apolipoprotein (apo) A-I mimeticsa – Exercise, low-fat diet – Polyunsaturated fat diet – Statins • May promote HDL’s anti-inflammatory effect – Antirheumatic biologicals – Apo A-IMilanoa – Delipidated HDLa • Promote proinflammatory HDL – Coronary atherosclerosis – Diabetes mellitus – Hemodialysis – Diet high in saturated fat – Infection – Rheumatoid arthritis – Surgery – Systemic lupus erythematosus Currently in development Ansell BJ. Cleve Clin J Med. 2007; 74(10): 697 -700, 703 -705. a
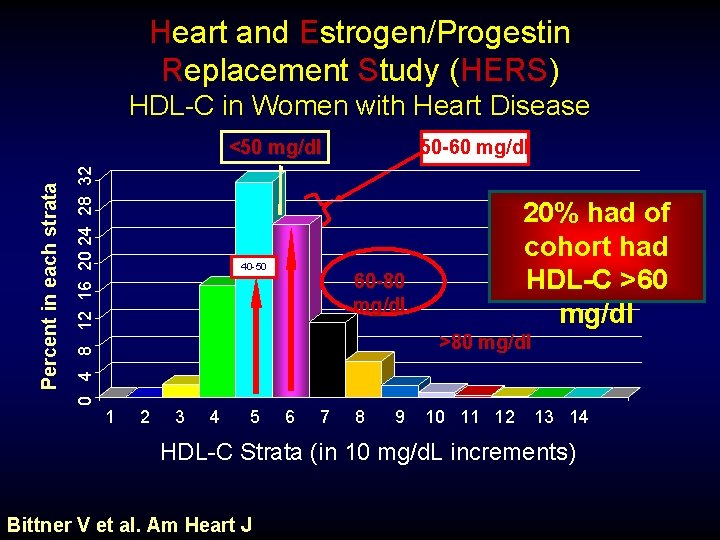
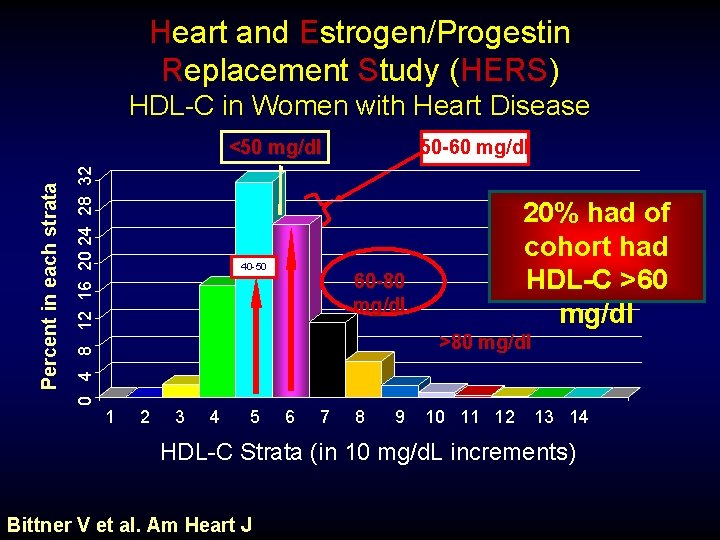
Heart and Estrogen/Progestin Replacement Study (HERS) HDL-C in Women with Heart Disease 50 -60 mg/dl 0 4 8 12 16 20 24 28 32 Percent in each strata <50 mg/dl 40 -50 20% had of cohort had HDL-C >60 mg/dl 60 -80 mg/dl >80 mg/dl 1 2 3 4 5 6 7 8 9 10 11 12 13 14 HDL-C Strata (in 10 mg/d. L increments) Bittner V et al. Am Heart J
Apo B (LDL particle Concentration) • Elevated Apo B is the most predictive marker for CHD events in postmenopausal women • On molecule of Apo B is present on surface of every VLDL, IDL, LDL particle. • Estrogen and HRT that raise Triglycerides may lower LDL-C 14 -15% without lowering Apo B or LDL particle concentration, an indication of smaller, dense LDL
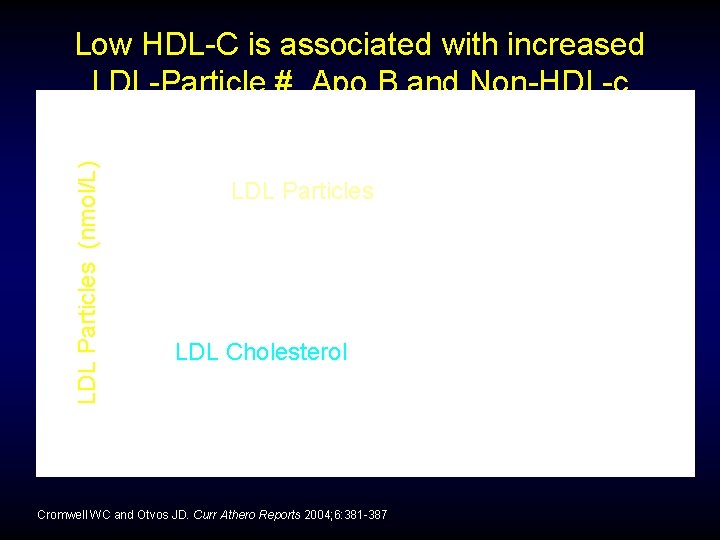
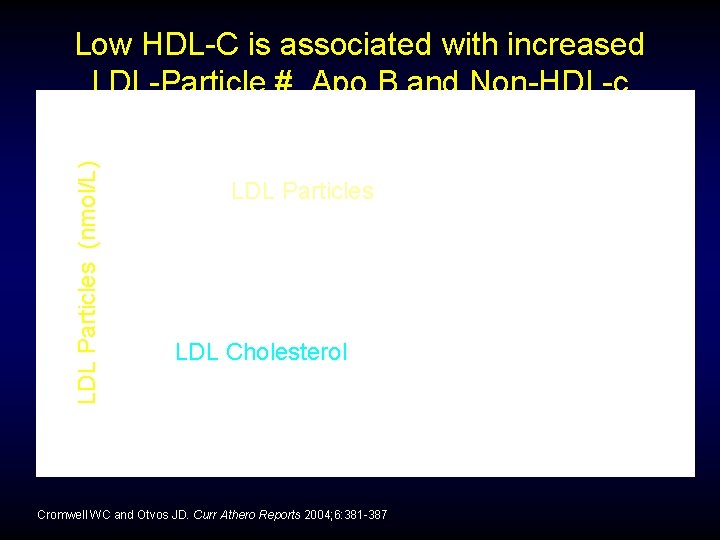
LDL Particles (nmol/L) Low HDL-C is associated with increased LDL-Particle #, Apo B and Non-HDL-c LDL Particles LDL Cholesterol HDL Cholesterol (mg/d. L) Cromwell WC and Otvos JD. Curr Athero Reports 2004; 6: 381 -387
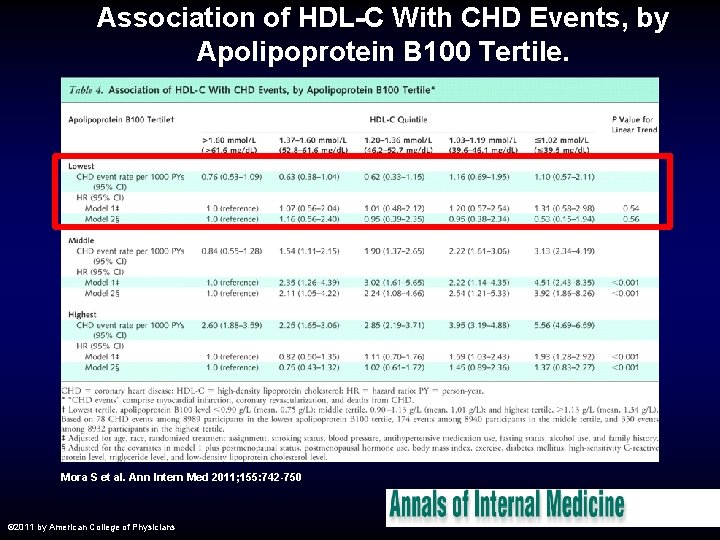
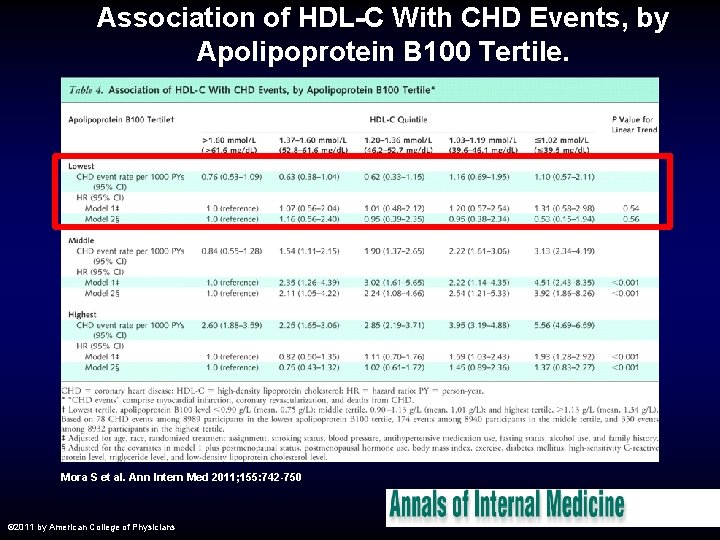
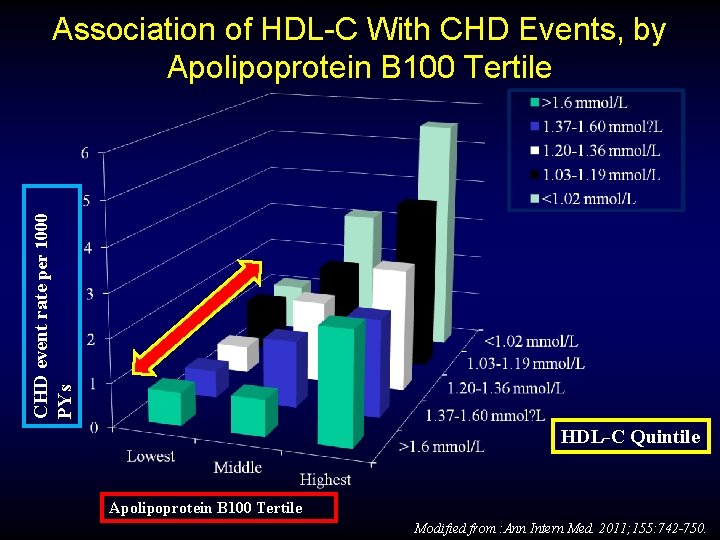
Association of HDL-C With CHD Events, by Apolipoprotein B 100 Tertile. Mora S et al. Ann Intern Med 2011; 155: 742 -750 © 2011 by American College of Physicians
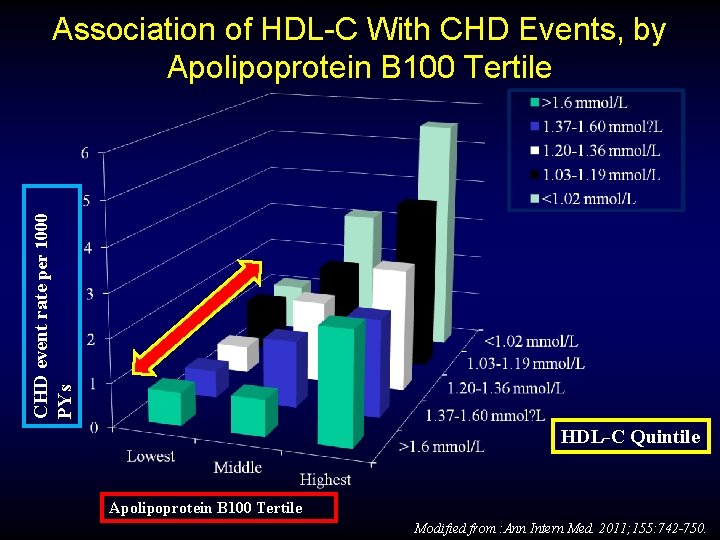
CHD event rate per 1000 PYs Association of HDL-C With CHD Events, by Apolipoprotein B 100 Tertile HDL-C Quintile Apolipoprotein B 100 Tertile Modified from : Ann Intern Med. 2011; 155: 742 -750.

hs. CRP
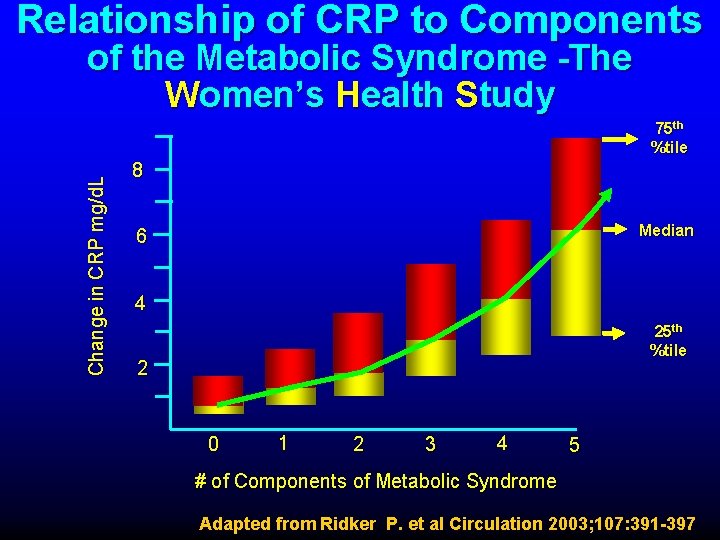
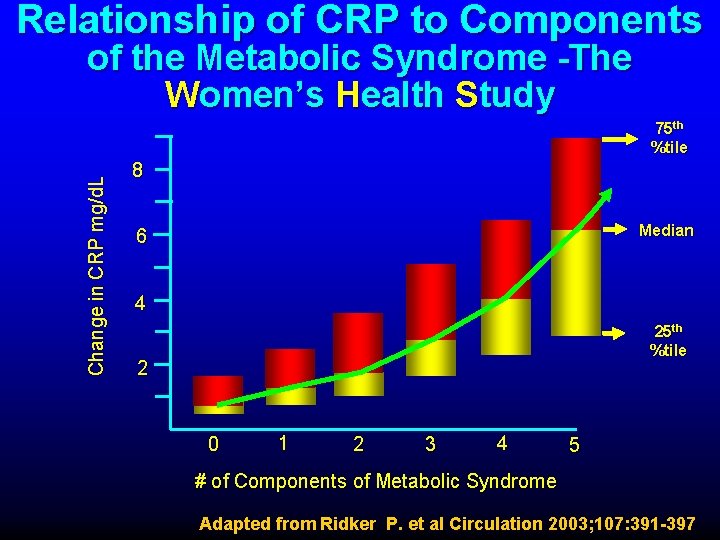
Relationship of CRP to Components of the Metabolic Syndrome -The Women’s Health Study Change in CRP mg/d. L 75 th %tile 8 Median 6 4 25 th %tile 2 0 1 2 3 4 5 # of Components of Metabolic Syndrome Adapted from Ridker P. et al Circulation 2003; 107: 391 -397
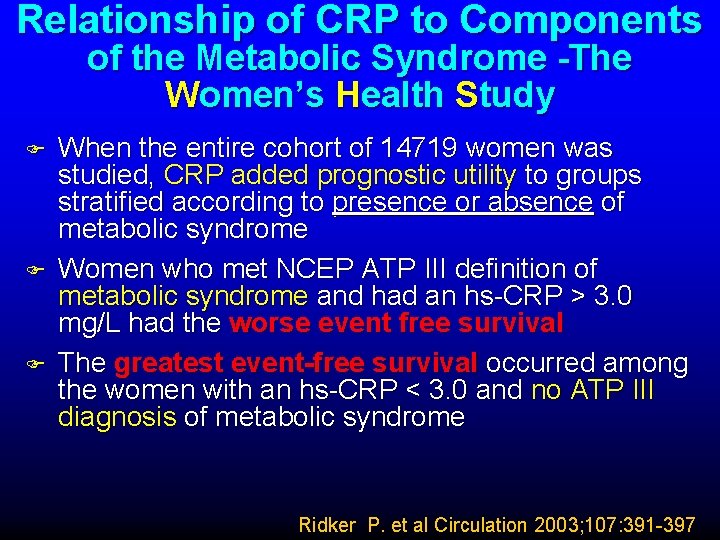
Relationship of CRP to Components of the Metabolic Syndrome -The Women’s Health Study F F F When the entire cohort of 14719 women was studied, CRP added prognostic utility to groups stratified according to presence or absence of metabolic syndrome Women who met NCEP ATP III definition of metabolic syndrome and had an hs-CRP > 3. 0 mg/L had the worse event free survival The greatest event-free survival occurred among the women with an hs-CRP < 3. 0 and no ATP III diagnosis of metabolic syndrome Ridker P. et al Circulation 2003; 107: 391 -397
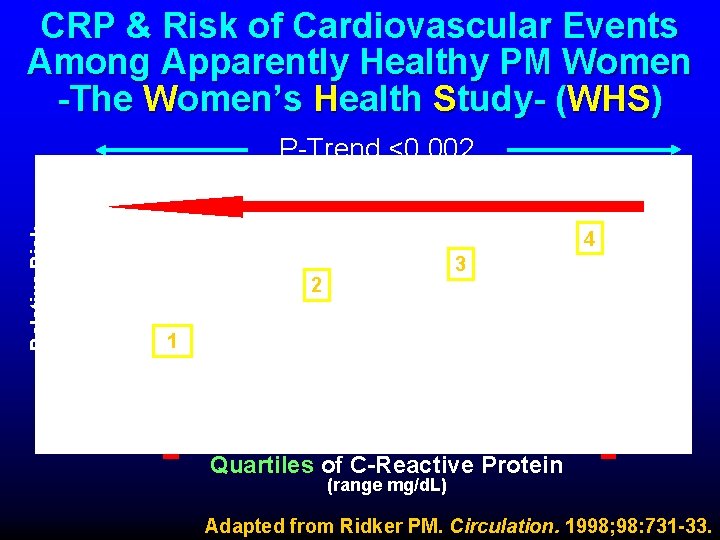
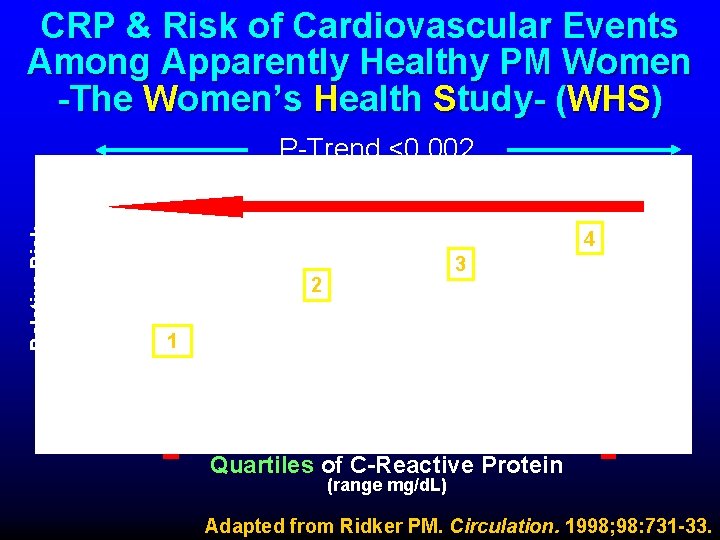
CRP & Risk of Cardiovascular Events Among Apparently Healthy PM Women -The Women’s Health Study- (WHS) Relative Risk P-Trend <0. 002 4 3 2 1 Quartiles of C-Reactive Protein (range mg/d. L) Adapted from Ridker PM. Circulation. 1998; 98: 731 -33.

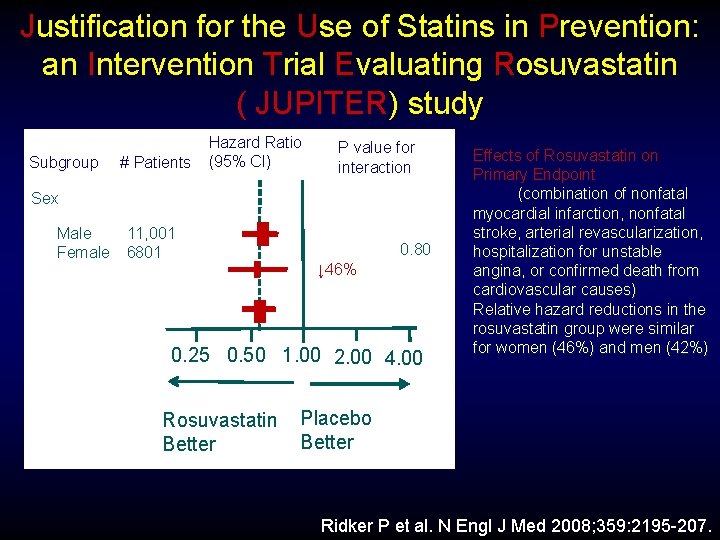
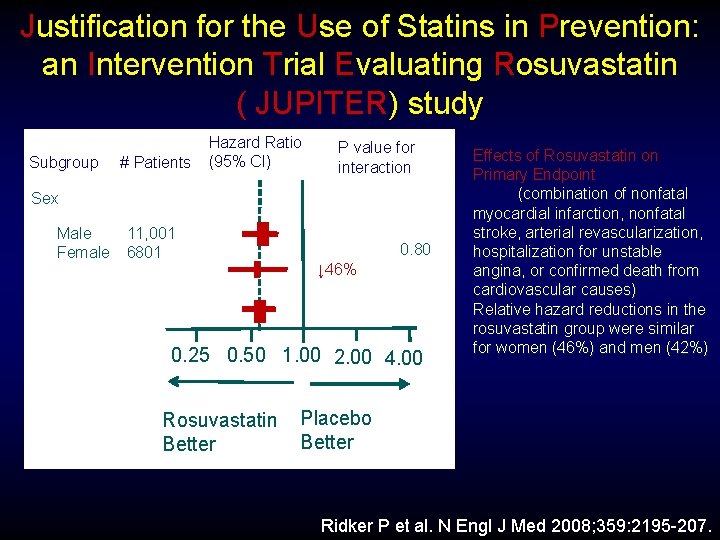
Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin ( JUPITER) study Subgroup # Patients Hazard Ratio (95% CI) P value for interaction Sex Male Female 11, 001 6801 0. 80 ↓ 46% 0. 25 0. 50 1. 00 2. 00 4. 00 Rosuvastatin Better Effects of Rosuvastatin on Primary Endpoint (combination of nonfatal myocardial infarction, nonfatal stroke, arterial revascularization, hospitalization for unstable angina, or confirmed death from cardiovascular causes) Relative hazard reductions in the rosuvastatin group were similar for women (46%) and men (42%) Placebo Better Ridker P et al. N Engl J Med 2008; 359: 2195 -207.
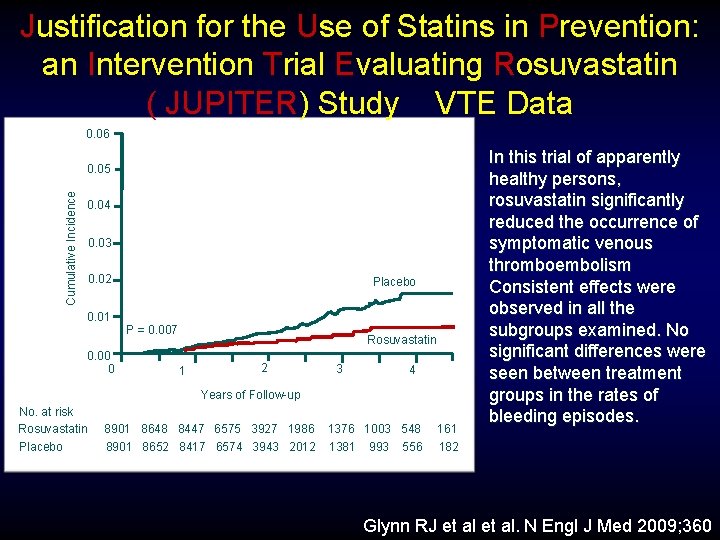
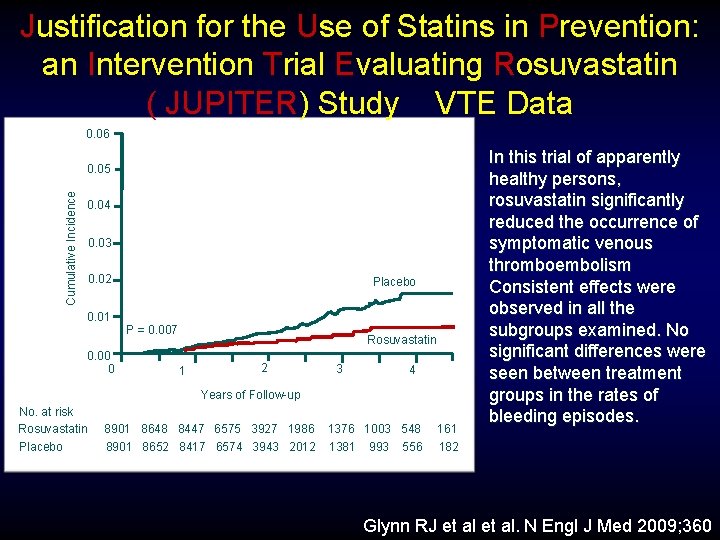
Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin ( JUPITER) Study VTE Data 0. 06 Cumulative Incidence 0. 05 0. 04 0. 03 0. 02 Placebo 0. 01 P = 0. 007 0. 00 0 Rosuvastatin 1 2 3 4 Years of Follow-up No. at risk Rosuvastatin Placebo 8901 8648 8447 6575 3927 1986 1376 1003 548 8901 8652 8417 6574 3943 2012 1381 993 556 161 182 In this trial of apparently healthy persons, rosuvastatin significantly reduced the occurrence of symptomatic venous thromboembolism Consistent effects were observed in all the subgroups examined. No significant differences were seen between treatment groups in the rates of bleeding episodes. Glynn RJ et al. N Engl J Med 2009; 360
Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin ( JUPITER) Study ►This trial provides a striking example of the error in estimation of risk that can occur if particle measurements are not done. ►The LDL-C of 108 mg/d. L was at the 25 th percentile of the population ►The Non-HDL-C of 134 mg/d. L was at the 30 th percentile ►The apo. B of 109 mg/d. L was at the 60 th percentile for men and 70 th percentile for women ►The discordance is substantial Sniderman A. Curr Athero Reports 2009; 11: 358 -363
Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin ( JUPITER) Study ►Based on LDL-C and non-HDL-C one would conclude LDL-P was low, but based on apo. B one would conclude it is not. ►The average was 66 years, thus the patients had been exposed to high levels of atherogenic particles for long periods of time ►Thus the event rate in the placebo group was not surprising and nor was the statin benefit Sniderman A. Curr Athero Reports 2009; 11: 358 -363
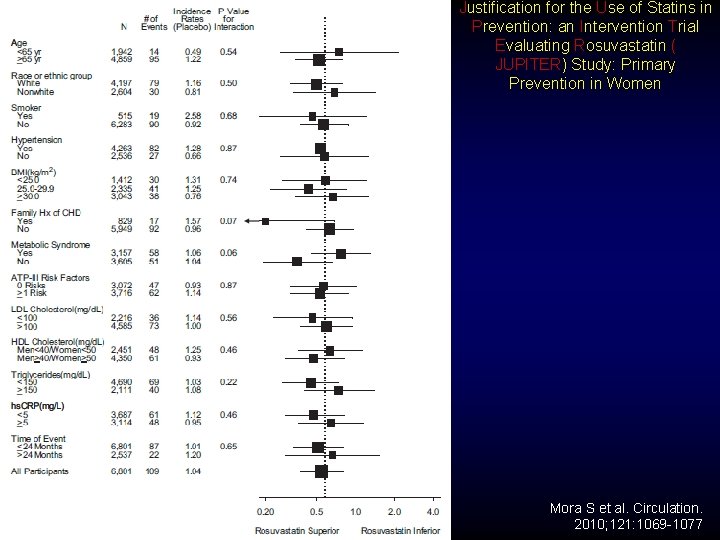
Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin ( JUPITER) Study: Primary Prevention in Women ►Absolute CVD rates (per 100 person-years) in JUPITER women (#6801) for rosuvastatin and placebo (0. 57 and 1. 04, respectively) were lower than for men (0. 88 and 1. 54, respectively), with similar relative risk reduction in women (hazard ratio, 0. 54; 95% confidence interval, 0. 37 to 0. 80; P=0. 002) and men (hazard ratio, 0. 58; 95% confidence interval, 0. 45 to 0. 73; P<0. 001). ►In women, there was significant reduction in revascularization/unstable angina and nonsignificant reductions in other components of the primary end point. ►Conclusion: JUPITER demonstrated that in primary prevention rosuvastatin reduced CVD events in women with a relative risk reduction similar to that in men Mora S et al. Circulation. 2010; 121: 1069 -1077
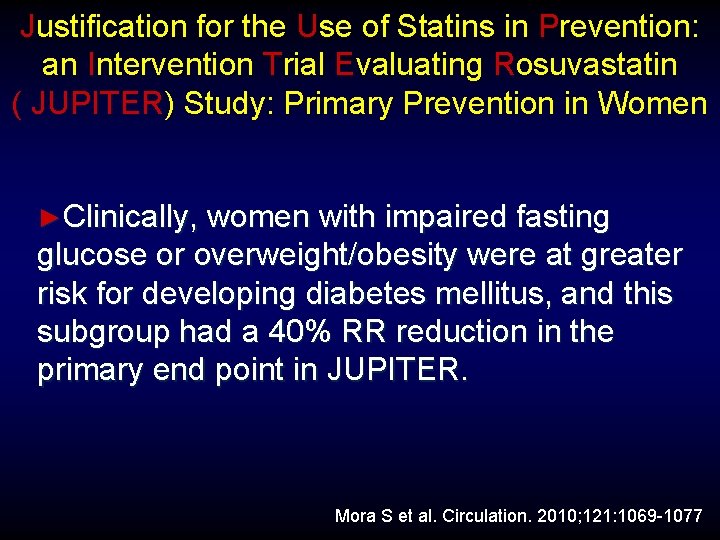
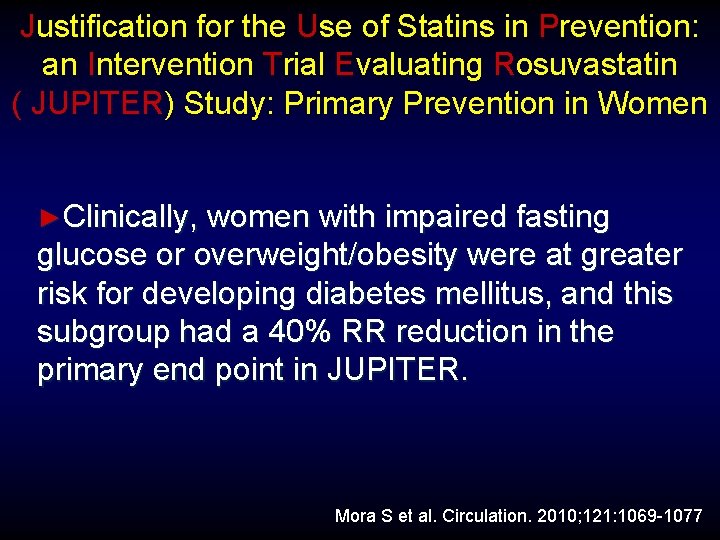
Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin ( JUPITER) Study: Primary Prevention in Women ►Clinically, women with impaired fasting glucose or overweight/obesity were at greater risk for developing diabetes mellitus, and this subgroup had a 40% RR reduction in the primary end point in JUPITER. Mora S et al. Circulation. 2010; 121: 1069 -1077
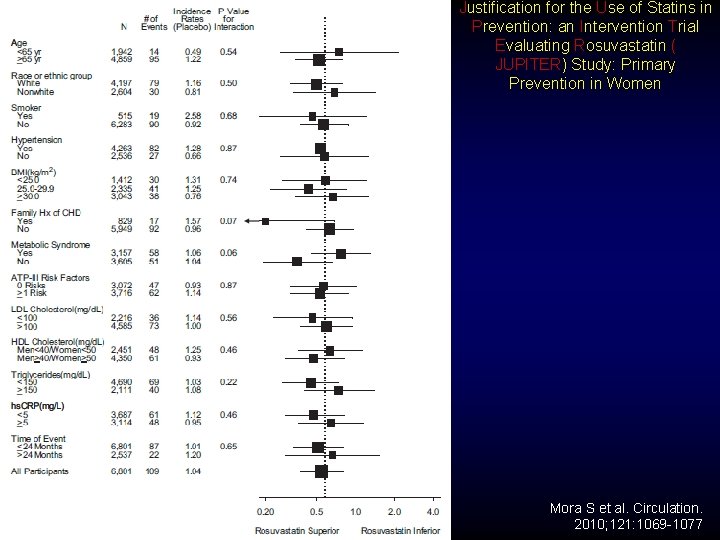
Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin ( JUPITER) Study: Primary Prevention in Women Mora S et al. Circulation. 2010; 121: 1069 -1077
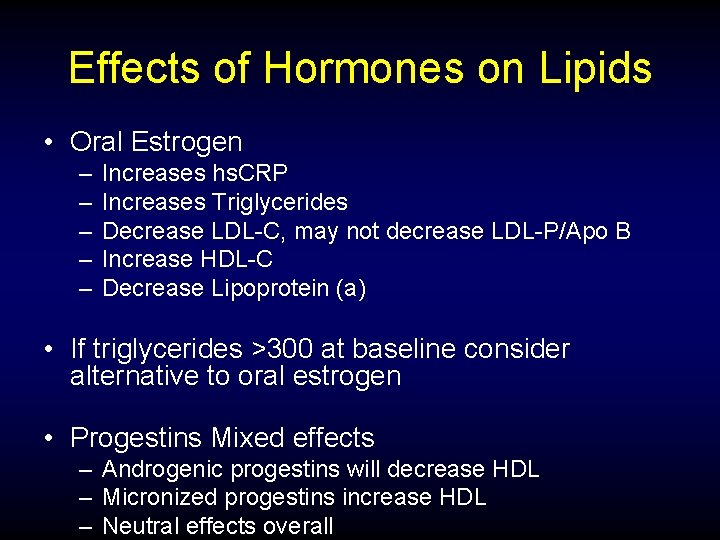
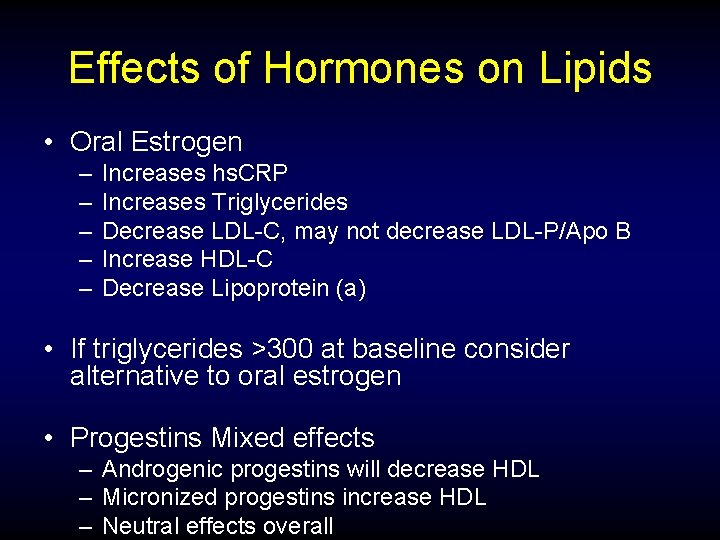
Effects of Hormones on Lipids • Oral Estrogen – – – Increases hs. CRP Increases Triglycerides Decrease LDL-C, may not decrease LDL-P/Apo B Increase HDL-C Decrease Lipoprotein (a) • If triglycerides >300 at baseline consider alternative to oral estrogen • Progestins Mixed effects – Androgenic progestins will decrease HDL – Micronized progestins increase HDL – Neutral effects overall
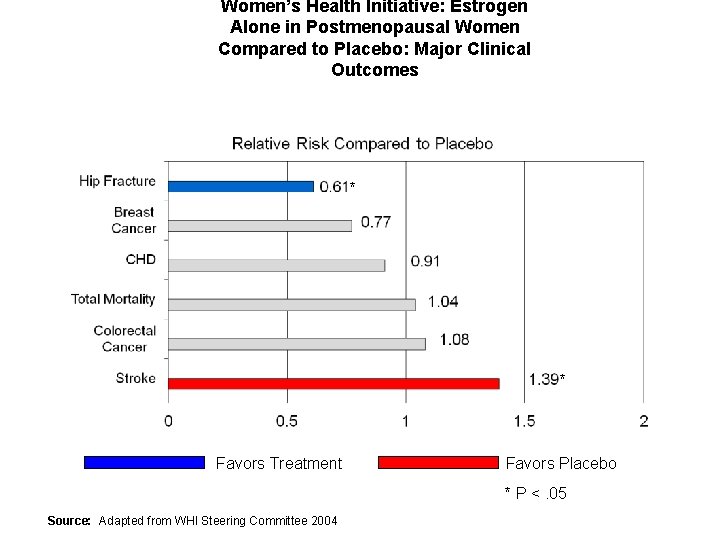
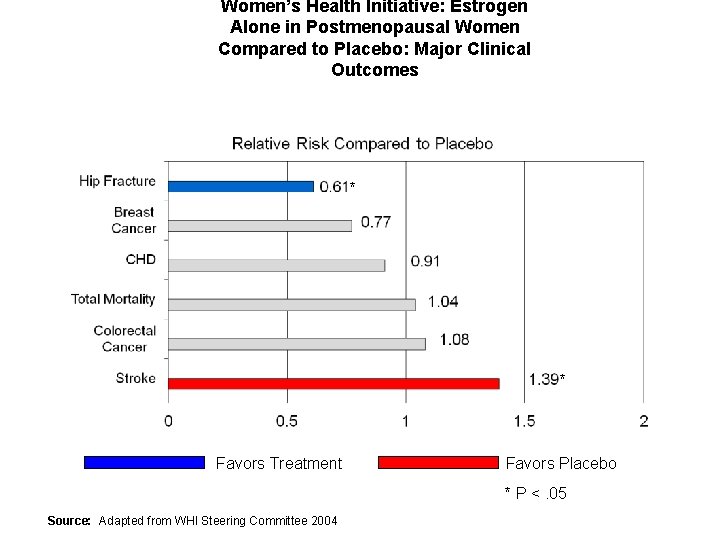
Women’s Health Initiative: Estrogen Alone in Postmenopausal Women Compared to Placebo: Major Clinical Outcomes * * Favors Treatment Favors Placebo * P <. 05 Source: Adapted from WHI Steering Committee 2004
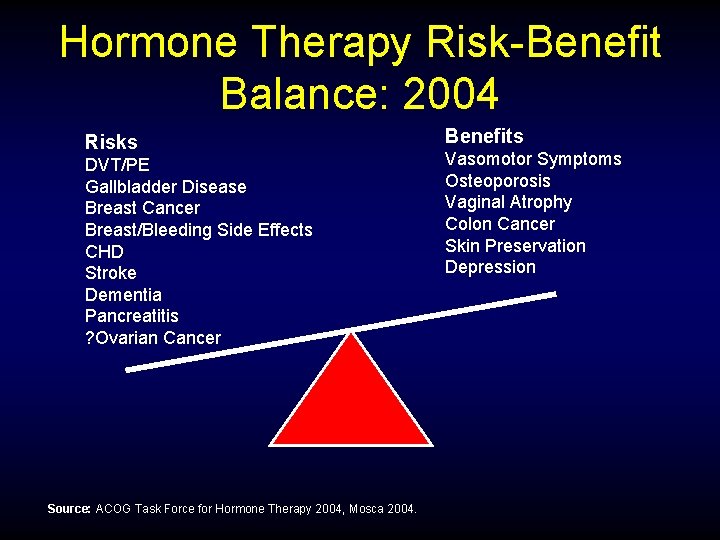
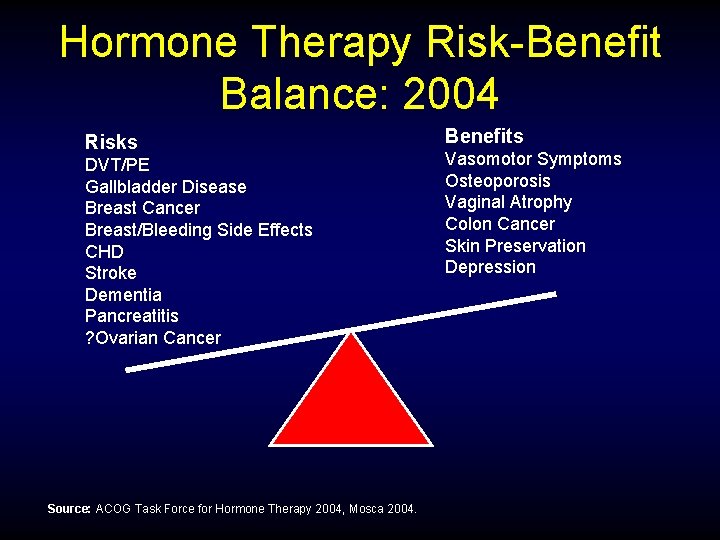
Hormone Therapy Risk-Benefit Balance: 2004 Risks DVT/PE Gallbladder Disease Breast Cancer Breast/Bleeding Side Effects CHD Stroke Dementia Pancreatitis ? Ovarian Cancer Source: ACOG Task Force for Hormone Therapy 2004, Mosca 2004. Benefits Vasomotor Symptoms Osteoporosis Vaginal Atrophy Colon Cancer Skin Preservation Depression
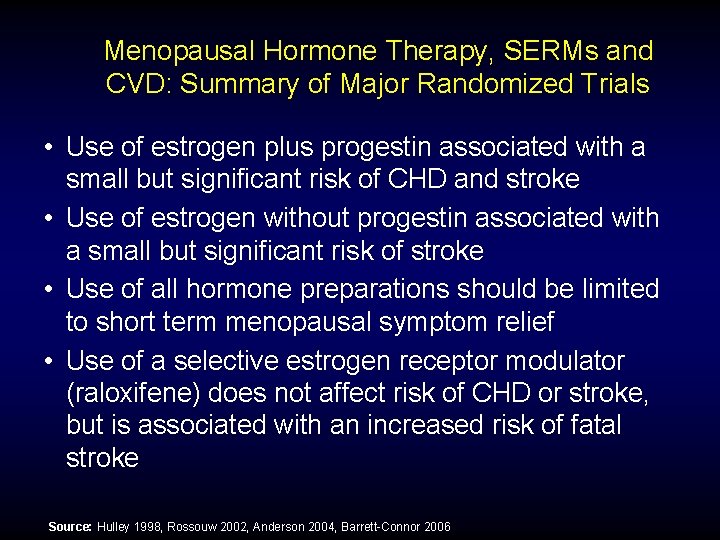
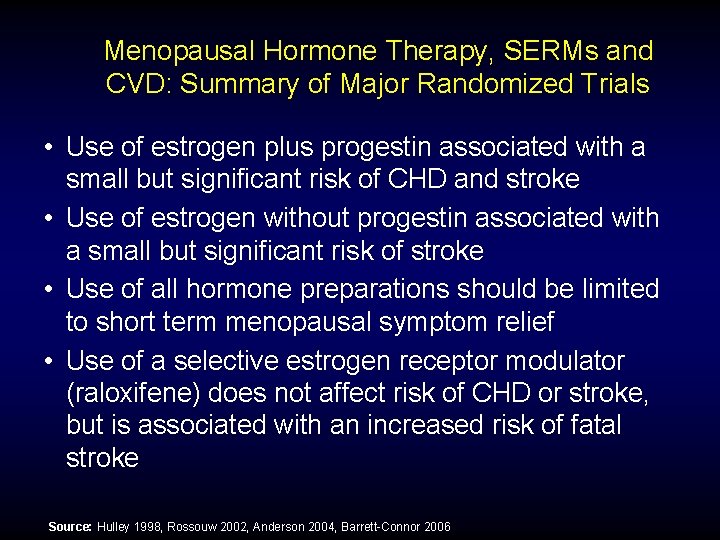
Menopausal Hormone Therapy, SERMs and CVD: Summary of Major Randomized Trials • Use of estrogen plus progestin associated with a small but significant risk of CHD and stroke • Use of estrogen without progestin associated with a small but significant risk of stroke • Use of all hormone preparations should be limited to short term menopausal symptom relief • Use of a selective estrogen receptor modulator (raloxifene) does not affect risk of CHD or stroke, but is associated with an increased risk of fatal stroke Source: Hulley 1998, Rossouw 2002, Anderson 2004, Barrett-Connor 2006
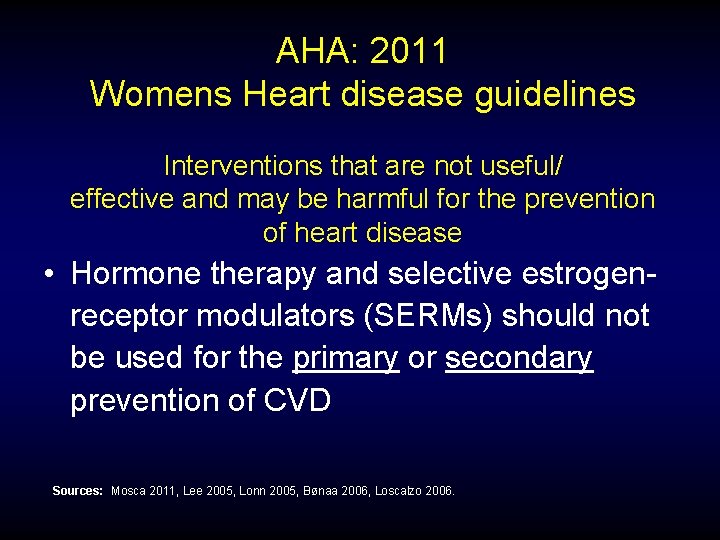
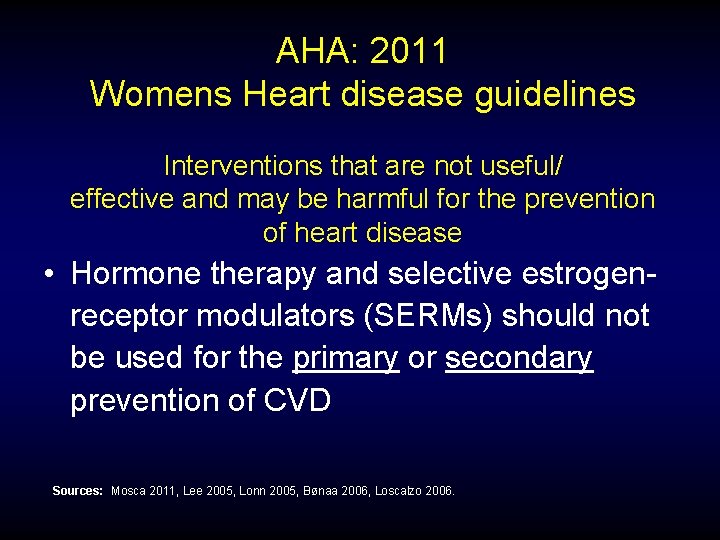
AHA: 2011 Womens Heart disease guidelines Interventions that are not useful/ effective and may be harmful for the prevention of heart disease • Hormone therapy and selective estrogenreceptor modulators (SERMs) should not be used for the primary or secondary prevention of CVD Sources: Mosca 2011, Lee 2005, Lonn 2005, Bønaa 2006, Loscalzo 2006.
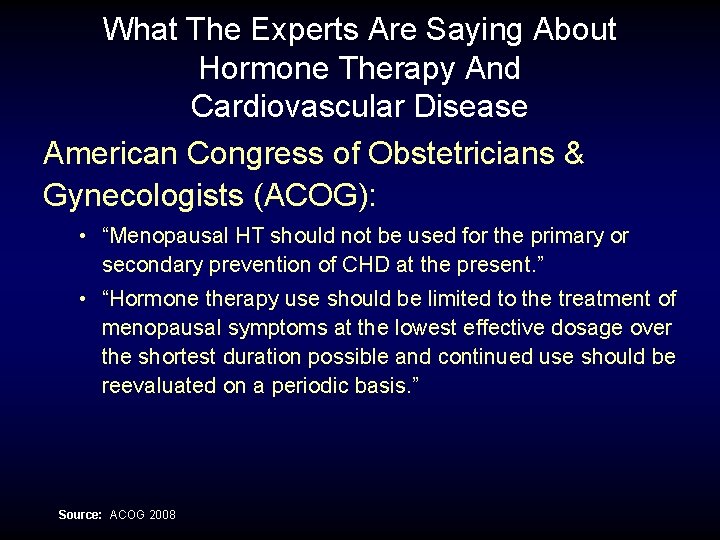
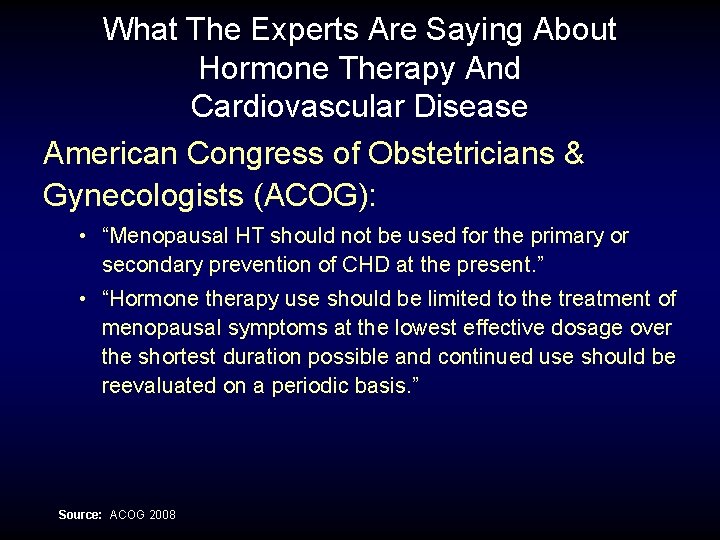
What The Experts Are Saying About Hormone Therapy And Cardiovascular Disease American Congress of Obstetricians & Gynecologists (ACOG): • “Menopausal HT should not be used for the primary or secondary prevention of CHD at the present. ” • “Hormone therapy use should be limited to the treatment of menopausal symptoms at the lowest effective dosage over the shortest duration possible and continued use should be reevaluated on a periodic basis. ” Source: ACOG 2008
15 Top Medical Organizations Agree on Hormone Therapy Use • New joint statement, prepared by The North American Menopause Society (NAMS), the American Society for Reproductive Medicine (ASRM), and The Endocrine Society, concludes that hormone therapy is still an acceptable treatment for menopausal symptoms. This statement has been endorsed by 12 other leading organizations in women’s health. • “We believe that too many symptomatic women are missing out on the proven benefits of hormone therapy because the results of the WHI, which studied the long-term use of hormones to prevent chronic disease, were misinterpreted for women with menopausal symptoms” said Dr. Margery Gass, Executive Director of NAMS. • The joint hormone therapy statement can be accessed on the NAMS website Menopause vol 19: 8, : 2012
North American Menopause Society 2012 Hormone Therapy Position Statement CVD Conclusions ►HT is currently not recommended for coronary protection in women of any age. ►Initiation of HT by women ages 50 to 59 years or by those within 10 years of menopause to treat typical menopausal symptoms does not seem to increase the risk of CHD events. ►There is emerging evidence that the initiation of ET in early postmenopause may reduce coronary artery disease and CHD risk. Menopause 2012; 19: 257 -271
North American Menopause Society 2012 Hormone Therapy Position Statement Duration of HT Use ►The recommendation for duration of therapy differs for EPT and ET. For EPT, duration is limited by the increased risk of breast cancer and breast cancer mortality associated with 3 to 5 years of use; for ET, a more favorable benefitrisk profile was observed during a mean of 7 years of use and 4 years of follow-up, a finding that allows more flexibility in duration of use. Menopause 2012; 19: 257 -271
North American Menopause Society 2012 Hormone Therapy Position Statement CONCLUSIONS Individualization is of key importance in the decision to use HT and should incorporate the woman’s health and quality of life priorities as well as her personal risk factors, such as risk of venous thrombosis, CHD, stroke, and breast cancer. Menopause 2012; 19: 257 -271
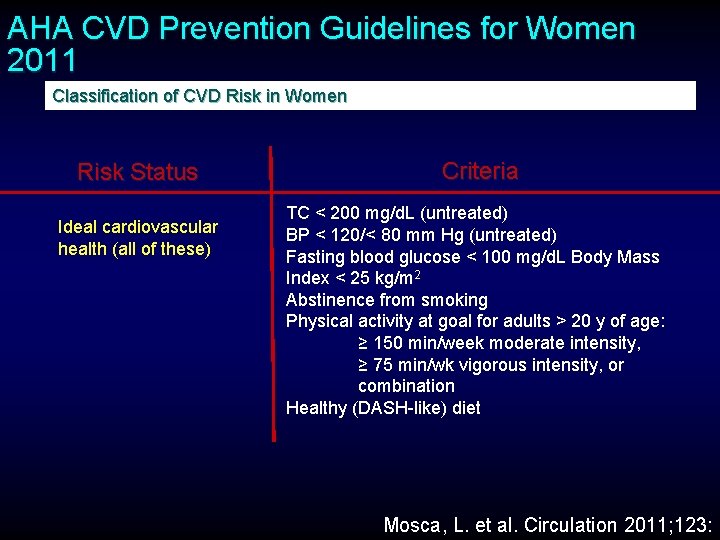
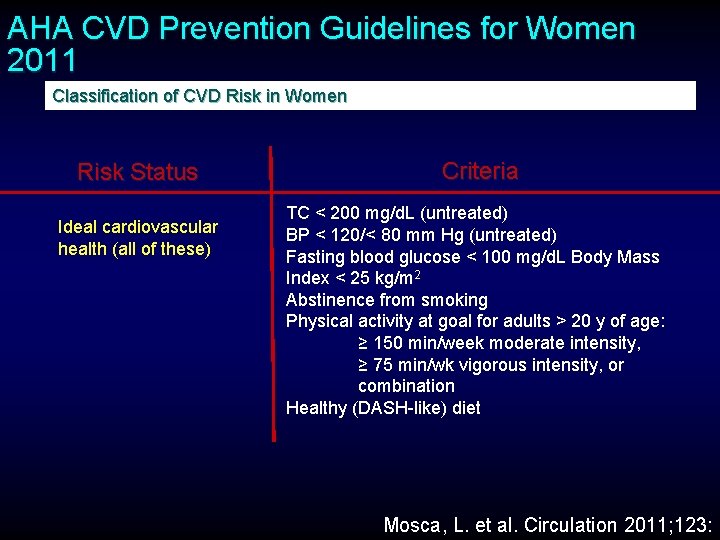
AHA CVD Prevention Guidelines for Women 2011 Classification of CVD Risk in Women Risk Status Ideal cardiovascular health (all of these) Criteria TC < 200 mg/d. L (untreated) BP < 120/< 80 mm Hg (untreated) Fasting blood glucose < 100 mg/d. L Body Mass Index < 25 kg/m 2 Abstinence from smoking Physical activity at goal for adults > 20 y of age: ≥ 150 min/week moderate intensity, ≥ 75 min/wk vigorous intensity, or combination Healthy (DASH-like) diet Mosca, L. et al. Circulation 2011; 123:
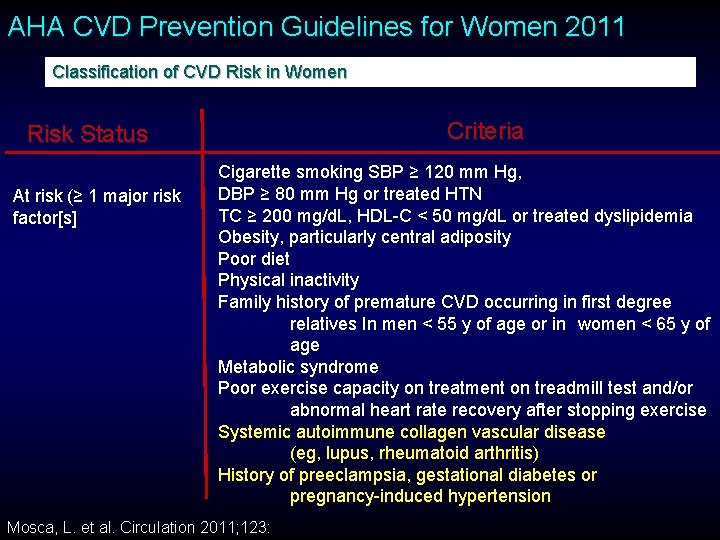
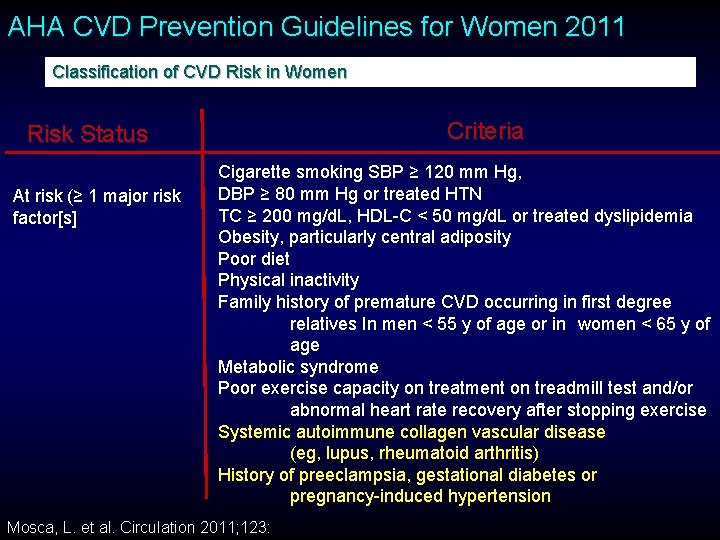
AHA CVD Prevention Guidelines for Women 2011 Classification of CVD Risk in Women Criteria Risk Status At risk (≥ 1 major risk factor[s] Cigarette smoking SBP ≥ 120 mm Hg, DBP ≥ 80 mm Hg or treated HTN TC ≥ 200 mg/d. L, HDL-C < 50 mg/d. L or treated dyslipidemia Obesity, particularly central adiposity Poor diet Physical inactivity Family history of premature CVD occurring in first degree relatives In men < 55 y of age or in women < 65 y of age Metabolic syndrome Poor exercise capacity on treatment on treadmill test and/or abnormal heart rate recovery after stopping exercise Systemic autoimmune collagen vascular disease (eg, lupus, rheumatoid arthritis) History of preeclampsia, gestational diabetes or pregnancy-induced hypertension Mosca, L. et al. Circulation 2011; 123:
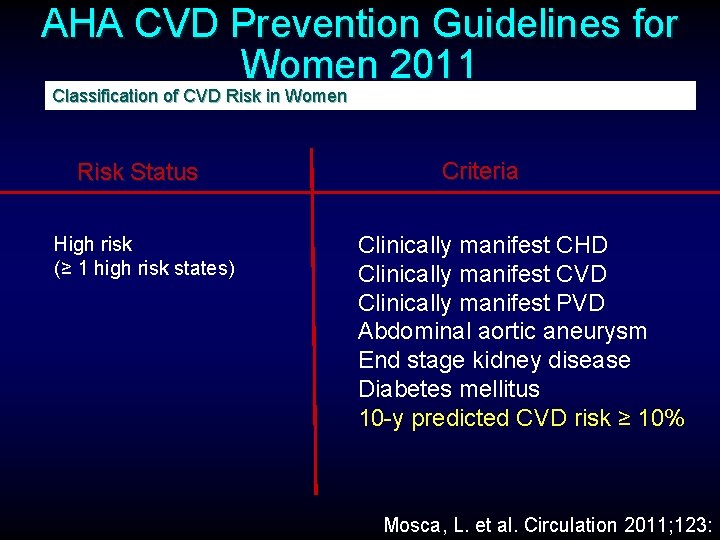
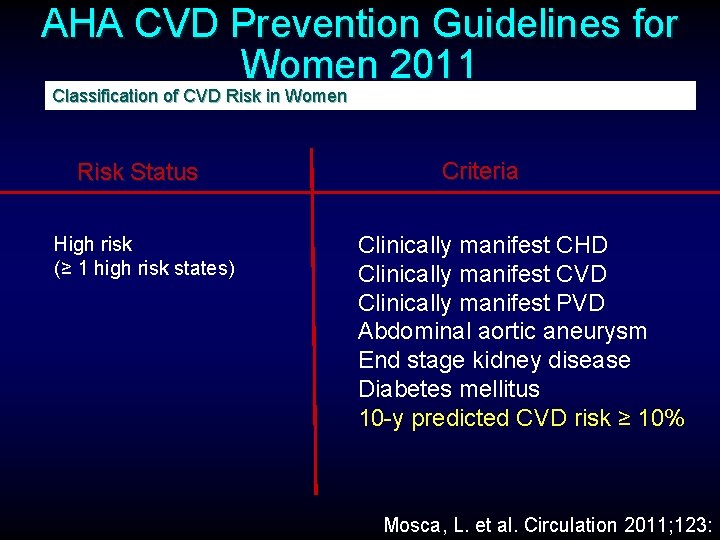
AHA CVD Prevention Guidelines for Women 2011 Classification of CVD Risk in Women Risk Status High risk (≥ 1 high risk states) Criteria Clinically manifest CHD Clinically manifest CVD Clinically manifest PVD Abdominal aortic aneurysm End stage kidney disease Diabetes mellitus 10 -y predicted CVD risk ≥ 10% Mosca, L. et al. Circulation 2011; 123:
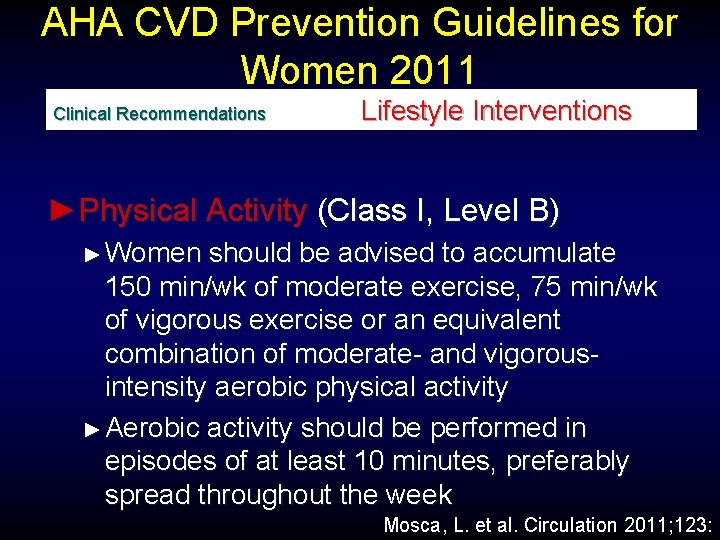
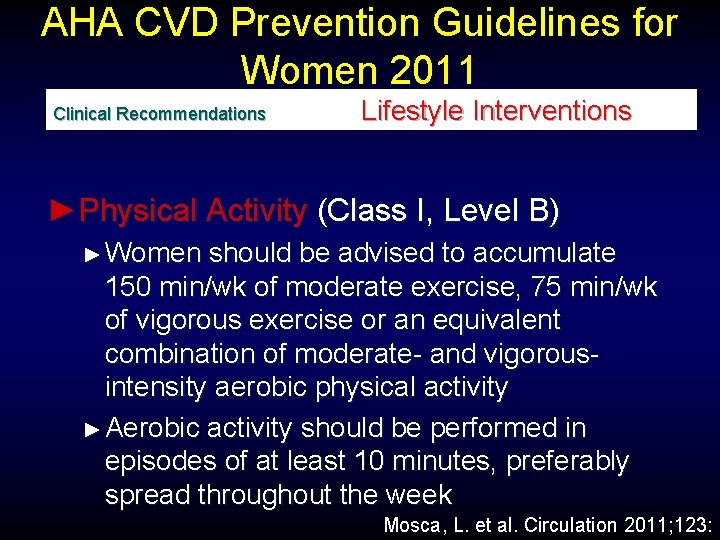
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Lifestyle Interventions ►Physical Activity (Class I, Level B) ► Women should be advised to accumulate 150 min/wk of moderate exercise, 75 min/wk of vigorous exercise or an equivalent combination of moderate- and vigorousintensity aerobic physical activity ► Aerobic activity should be performed in episodes of at least 10 minutes, preferably spread throughout the week Mosca, L. et al. Circulation 2011; 123:
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Lifestyle Interventions ►Physical Activity (Class I, Level B) ► ► ► Women should also be advised that additional cardiovascular benefits are provided by increasing moderate-intensity aerobic physical activity to 5 h (300 min/wk, 2 ½ h/wk of vigorousintensity physical activity, or an equivalent combination of both Women should be advised to engage in muscle-strengthening activities that involve all major muscle groups performed on ≥ 2 d/wk Women who need to loose weight or sustain weight loss should be advised to accumulate a minimum of 60 to 90 min of at least moderate-intensity physical activity (eg, brisk walking) on most, and preferably all, days of the week Mosca, L. et al. Circulation 2011; 123:
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Lifestyle Interventions ►Weight Maintenance (Class I; Level of Evidence B) ► Women should maintain or lose weight through an appropriate balance of physical activity, caloric intake, and formal behavioral programs when indicated to maintain or achieve an appropriate body weight (eg, BMI < 25 kg/m 2 in US women), waist size (eg, < 35 in), or other target metric of obesity Mosca, L. et al. Circulation 2011; 123:
AHA CVD Prevention Guidelines for Women Clinical Recommendations Lifestyle Interventions ►Omega-3 Fatty acids (Class IIb; Level of Evidence B) ► Consumption of omega-3 fatty acids in the form of fish or in capsule form (eg, EPA 1800 mg/d) may be considered in women with hypercholesterolemia and/or hypertriglyceridemia for primary and secondary prevention ► Note: Fish oil dietary supplements may have widely variable amounts of EPA and DHA (likely the only active ingredients) Mosca, L. et al. Circulation 2011; 123:
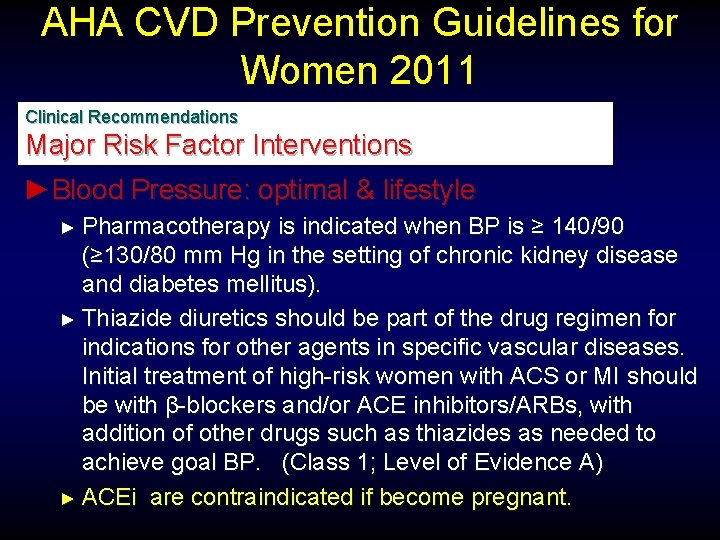
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Major Risk Factor Interventions ►Blood Pressure: optimal & lifestyle ► An optimal BP of <120/80 mm Hg should be encouraged through lifestyle approaches such as weight control, increased physical activity, alcohol moderation, sodium restriction, and increased consumption of fruits, vegetables and low-fat dairy products (Class 1; Level of Evidence B) Mosca, L. et al. Circulation 2011; 123:
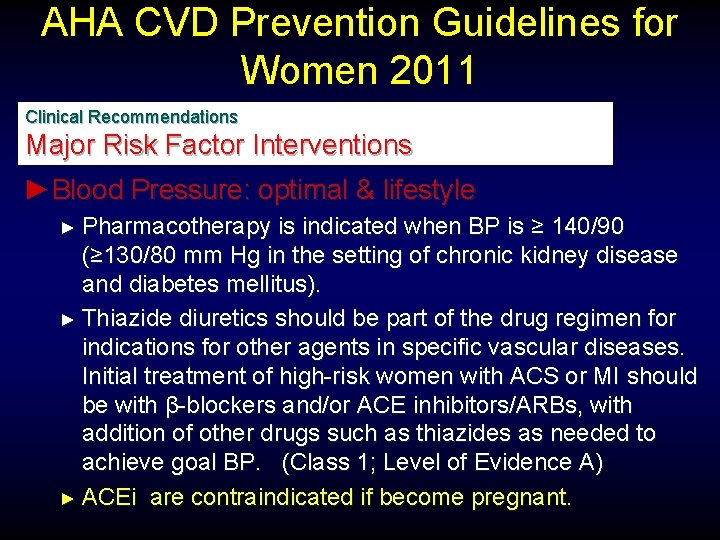
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Major Risk Factor Interventions ►Blood Pressure: optimal & lifestyle ► Pharmacotherapy is indicated when BP is ≥ 140/90 (≥ 130/80 mm Hg in the setting of chronic kidney disease and diabetes mellitus). ► Thiazide diuretics should be part of the drug regimen for indications for other agents in specific vascular diseases. Initial treatment of high-risk women with ACS or MI should be with β-blockers and/or ACE inhibitors/ARBs, with addition of other drugs such as thiazides as needed to achieve goal BP. (Class 1; Level of Evidence A) ► ACEi are contraindicated if become pregnant.
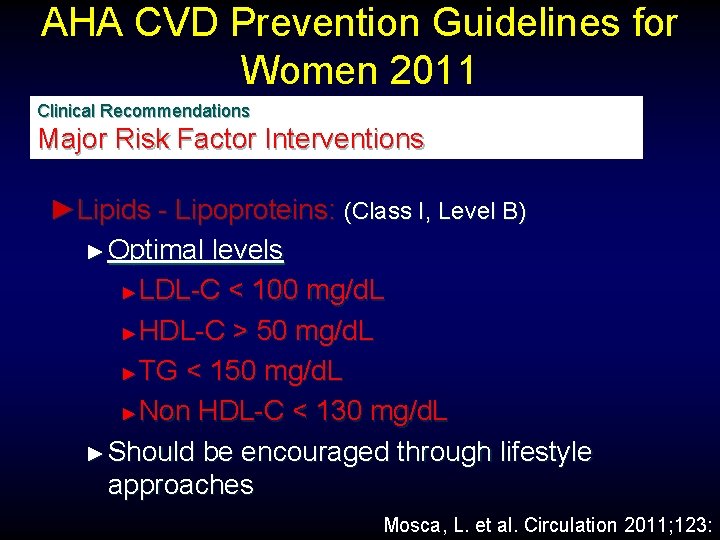
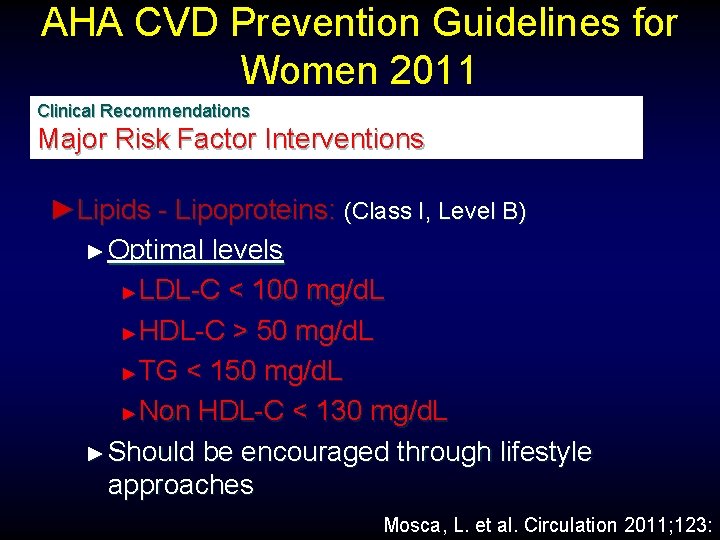
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Major Risk Factor Interventions ►Lipids - Lipoproteins: (Class I, Level B) ► Optimal levels ► LDL-C < 100 mg/d. L ► HDL-C > 50 mg/d. L ► TG < 150 mg/d. L ► Non HDL-C < 130 mg/d. L ► Should be encouraged through lifestyle approaches Mosca, L. et al. Circulation 2011; 123:
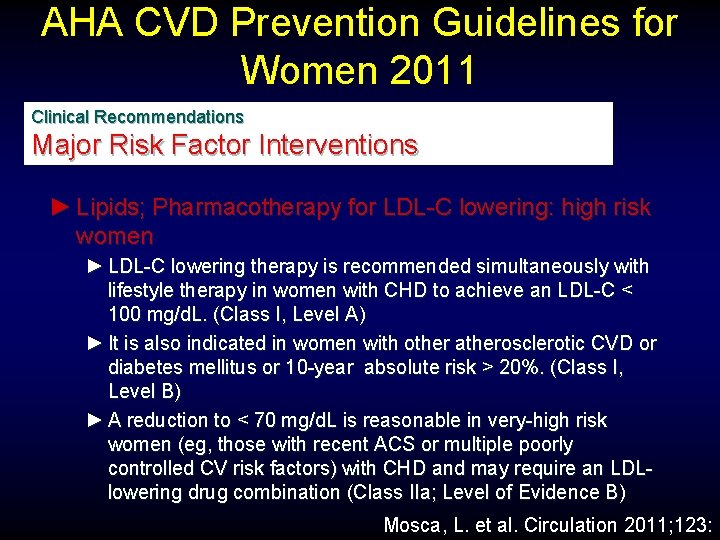
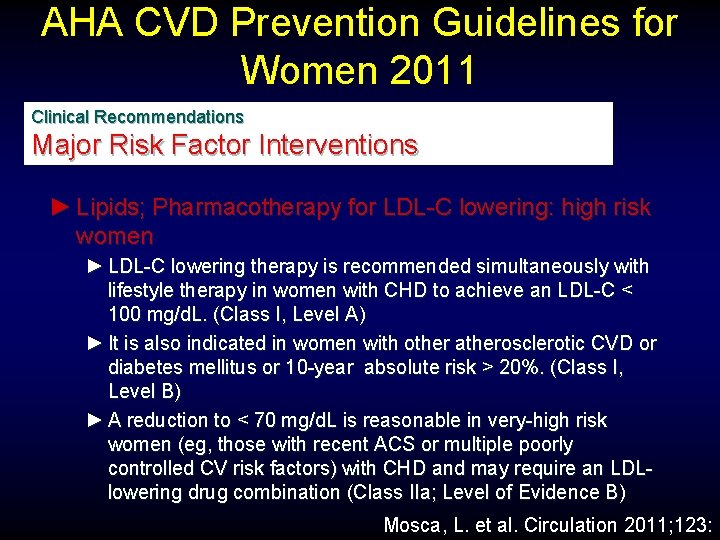
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Major Risk Factor Interventions ► Lipids; Pharmacotherapy for LDL-C lowering: high risk women ► LDL-C lowering therapy is recommended simultaneously with lifestyle therapy in women with CHD to achieve an LDL-C < 100 mg/d. L. (Class I, Level A) ► It is also indicated in women with other atherosclerotic CVD or diabetes mellitus or 10 -year absolute risk > 20%. (Class I, Level B) ► A reduction to < 70 mg/d. L is reasonable in very-high risk women (eg, those with recent ACS or multiple poorly controlled CV risk factors) with CHD and may require an LDLlowering drug combination (Class IIa; Level of Evidence B) Mosca, L. et al. Circulation 2011; 123:
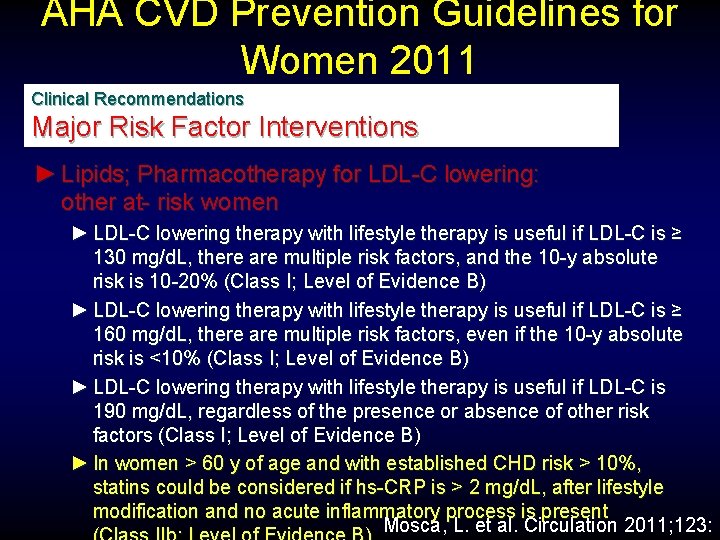
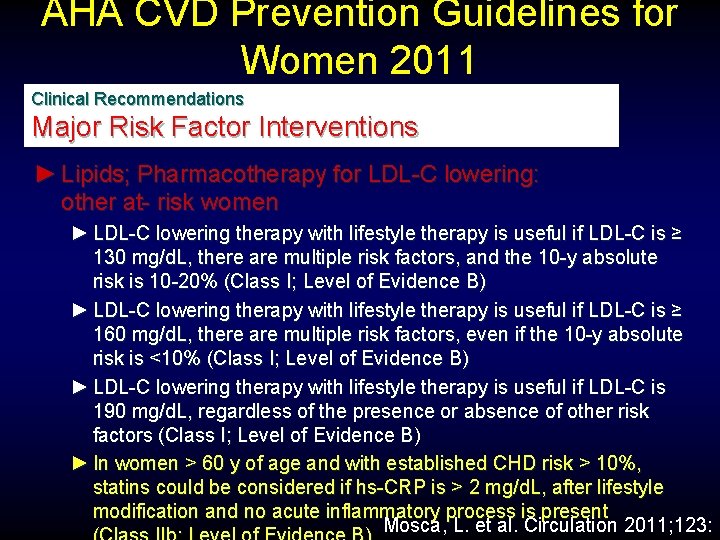
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Major Risk Factor Interventions ► Lipids; Pharmacotherapy for LDL-C lowering: other at- risk women ► LDL-C lowering therapy with lifestyle therapy is useful if LDL-C is ≥ 130 mg/d. L, there are multiple risk factors, and the 10 -y absolute risk is 10 -20% (Class I; Level of Evidence B) ► LDL-C lowering therapy with lifestyle therapy is useful if LDL-C is ≥ 160 mg/d. L, there are multiple risk factors, even if the 10 -y absolute risk is <10% (Class I; Level of Evidence B) ► LDL-C lowering therapy with lifestyle therapy is useful if LDL-C is 190 mg/d. L, regardless of the presence or absence of other risk factors (Class I; Level of Evidence B) ► In women > 60 y of age and with established CHD risk > 10%, statins could be considered if hs-CRP is > 2 mg/d. L, after lifestyle modification and no acute inflammatory process is present Mosca, L. et al. Circulation 2011; 123:
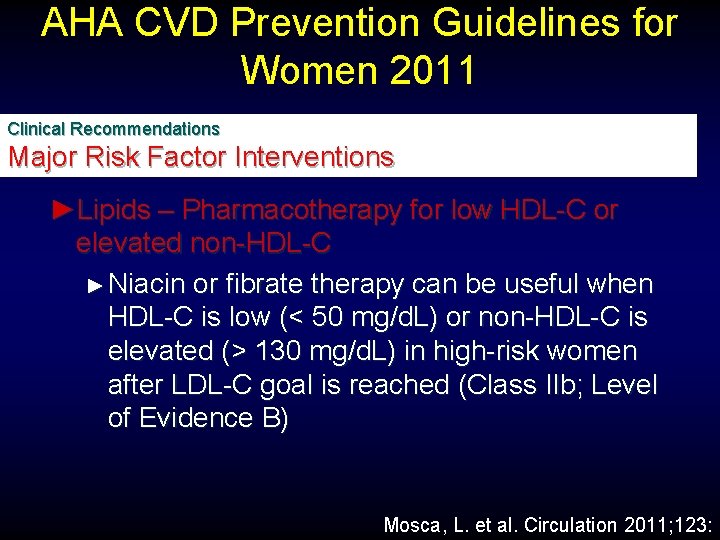
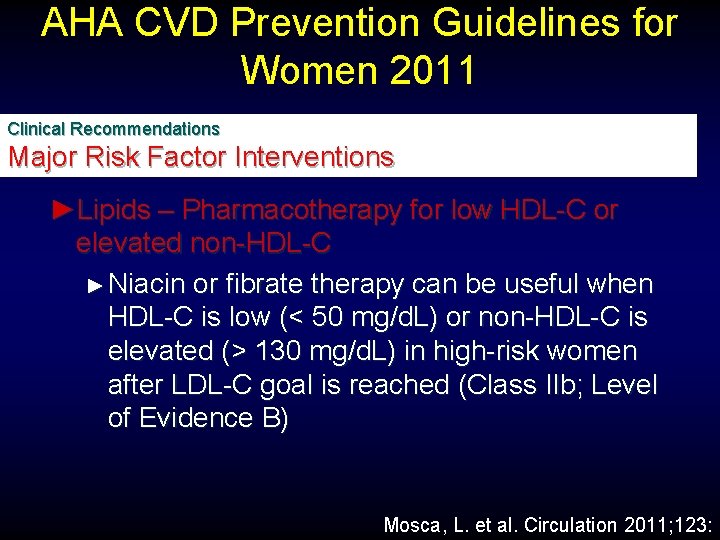
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Major Risk Factor Interventions ►Lipids – Pharmacotherapy for low HDL-C or elevated non-HDL-C ► Niacin or fibrate therapy can be useful when HDL-C is low (< 50 mg/d. L) or non-HDL-C is elevated (> 130 mg/d. L) in high-risk women after LDL-C goal is reached (Class IIb; Level of Evidence B) Mosca, L. et al. Circulation 2011; 123:
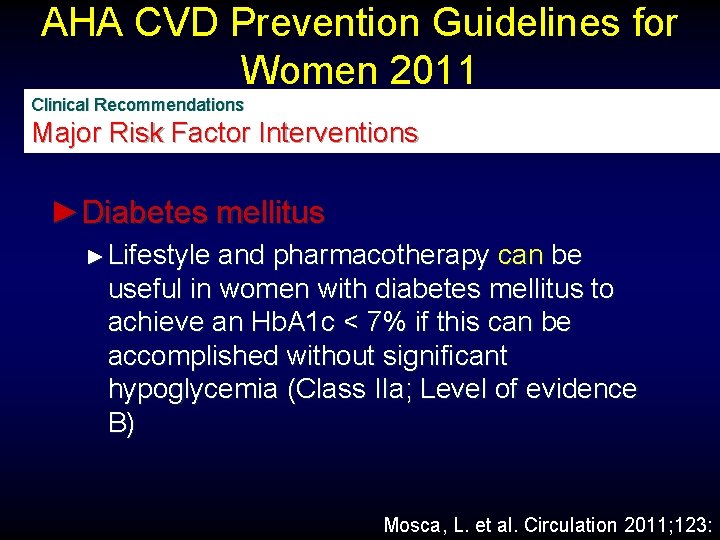
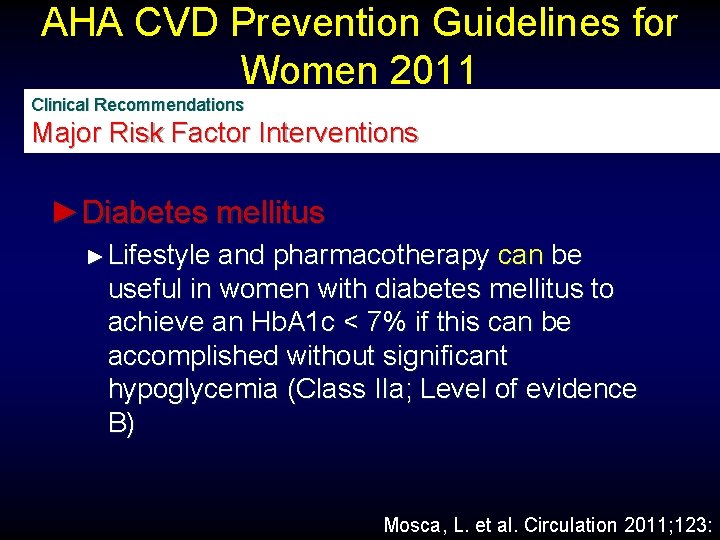
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Major Risk Factor Interventions ►Diabetes mellitus ► Lifestyle and pharmacotherapy can be useful in women with diabetes mellitus to achieve an Hb. A 1 c < 7% if this can be accomplished without significant hypoglycemia (Class IIa; Level of evidence B) Mosca, L. et al. Circulation 2011; 123:
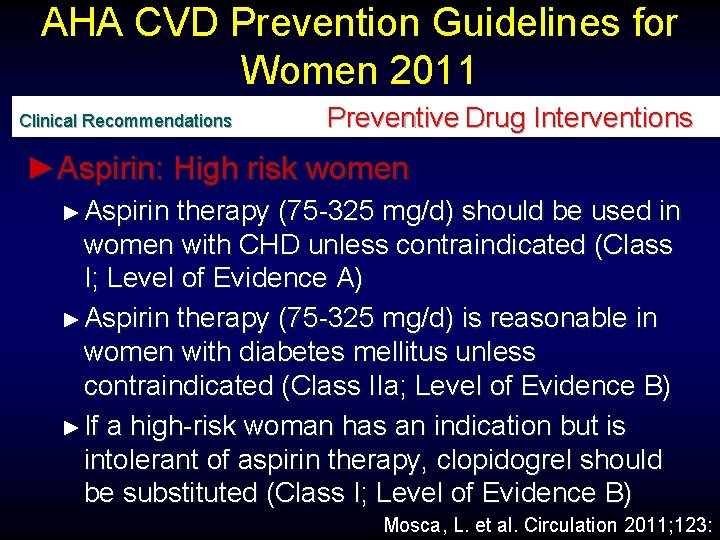
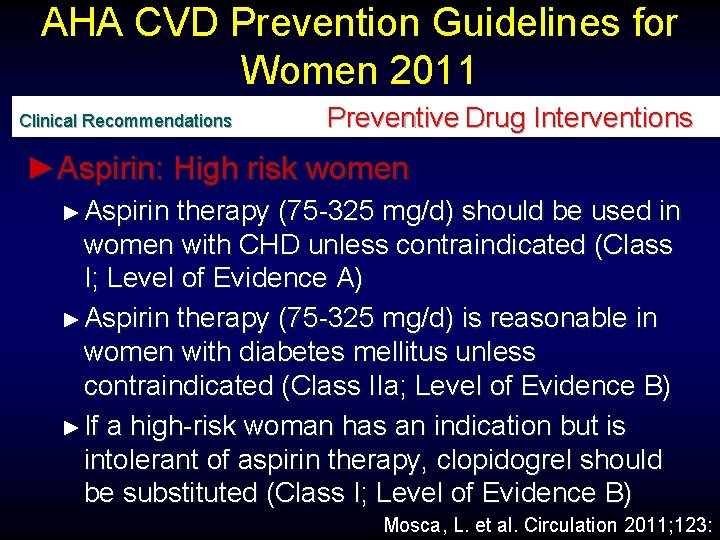
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Preventive Drug Interventions ►Aspirin: High risk women ► Aspirin therapy (75 -325 mg/d) should be used in women with CHD unless contraindicated (Class I; Level of Evidence A) ► Aspirin therapy (75 -325 mg/d) is reasonable in women with diabetes mellitus unless contraindicated (Class IIa; Level of Evidence B) ► If a high-risk woman has an indication but is intolerant of aspirin therapy, clopidogrel should be substituted (Class I; Level of Evidence B) Mosca, L. et al. Circulation 2011; 123:
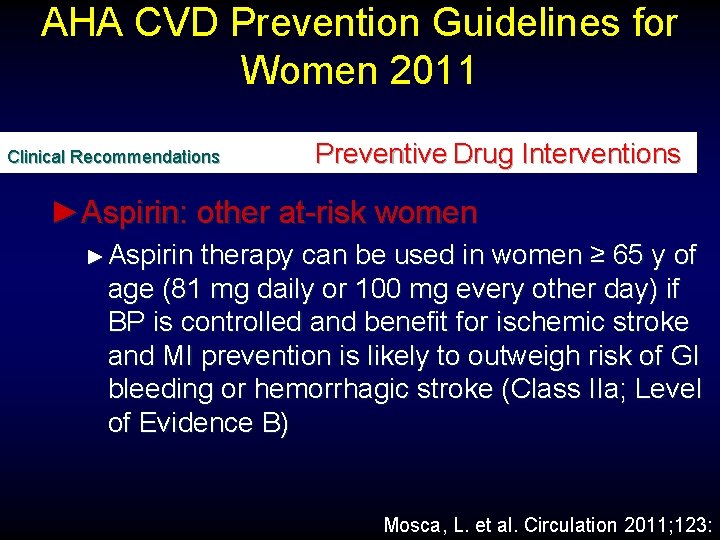
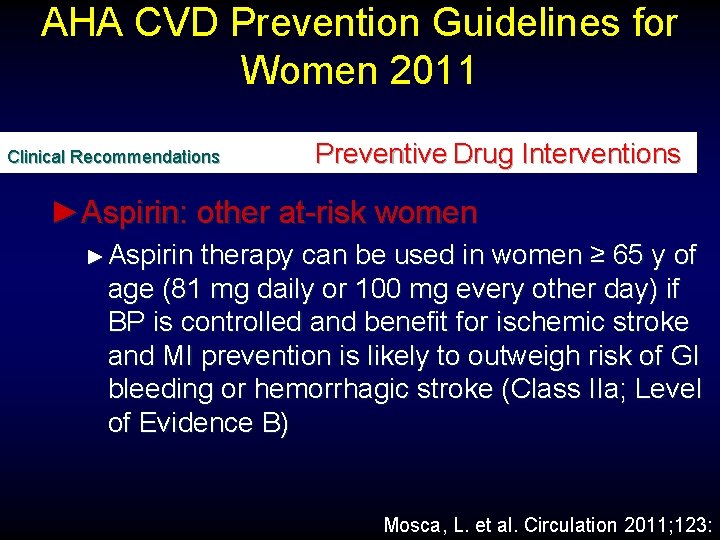
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Preventive Drug Interventions ►Aspirin: other at-risk women ► Aspirin therapy can be used in women ≥ 65 y of age (81 mg daily or 100 mg every other day) if BP is controlled and benefit for ischemic stroke and MI prevention is likely to outweigh risk of GI bleeding or hemorrhagic stroke (Class IIa; Level of Evidence B) Mosca, L. et al. Circulation 2011; 123:
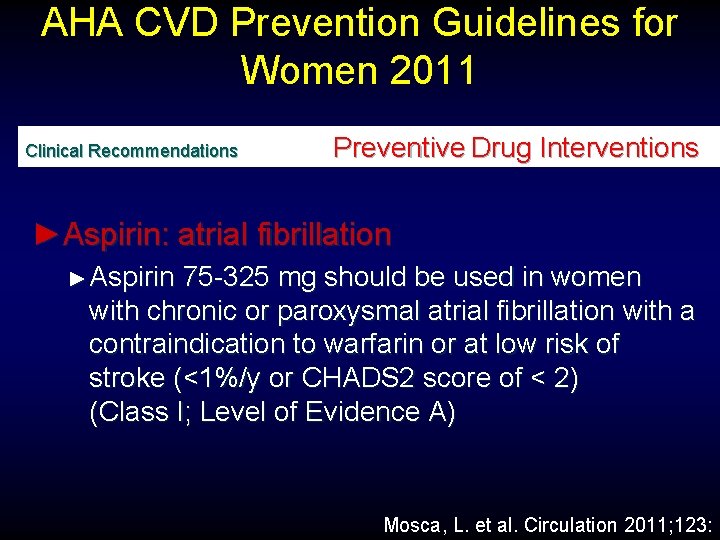
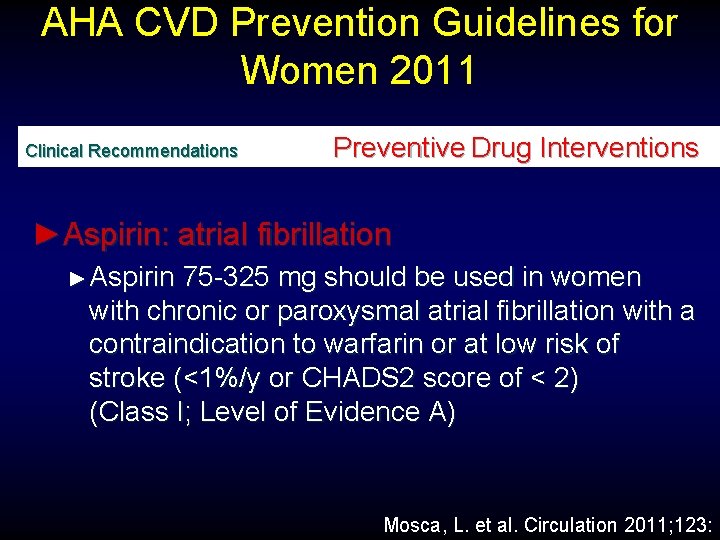
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Preventive Drug Interventions ►Aspirin: atrial fibrillation ► Aspirin 75 -325 mg should be used in women with chronic or paroxysmal atrial fibrillation with a contraindication to warfarin or at low risk of stroke (<1%/y or CHADS 2 score of < 2) (Class I; Level of Evidence A) Mosca, L. et al. Circulation 2011; 123:
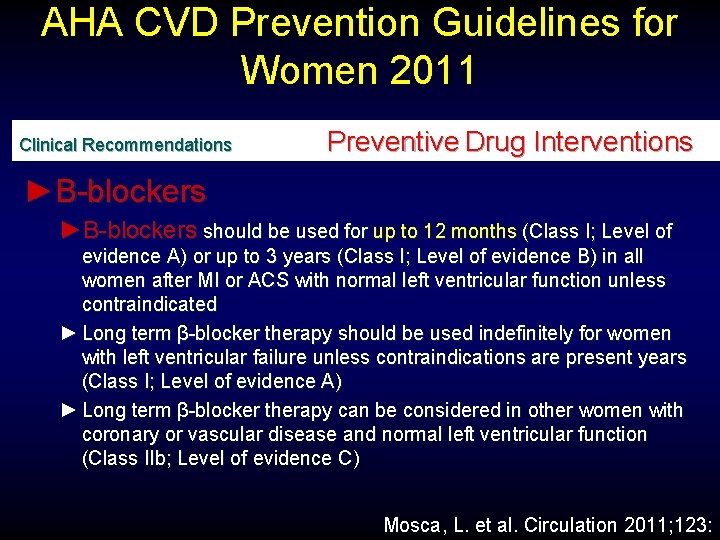
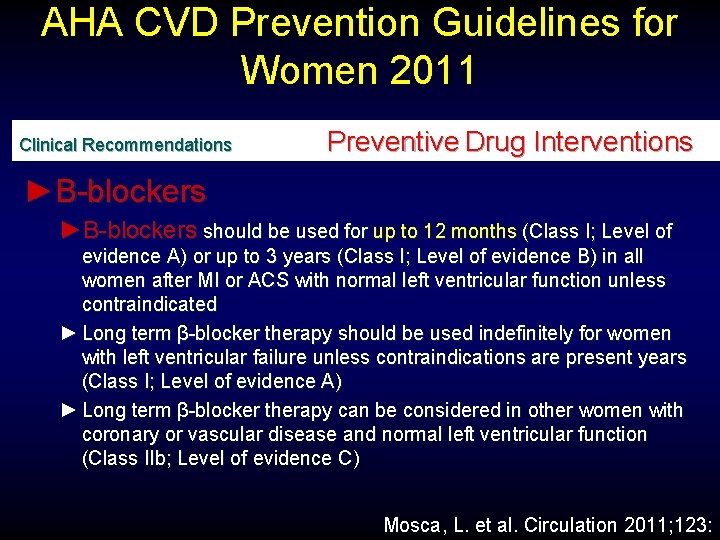
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Preventive Drug Interventions ►Β-blockers should be used for up to 12 months (Class I; Level of evidence A) or up to 3 years (Class I; Level of evidence B) in all women after MI or ACS with normal left ventricular function unless contraindicated ► Long term β-blocker therapy should be used indefinitely for women with left ventricular failure unless contraindications are present years (Class I; Level of evidence A) ► Long term β-blocker therapy can be considered in other women with coronary or vascular disease and normal left ventricular function (Class IIb; Level of evidence C) Mosca, L. et al. Circulation 2011; 123:
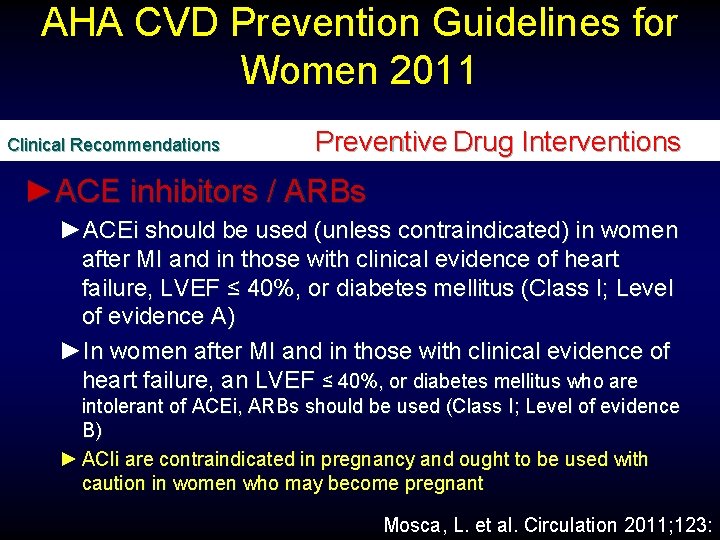
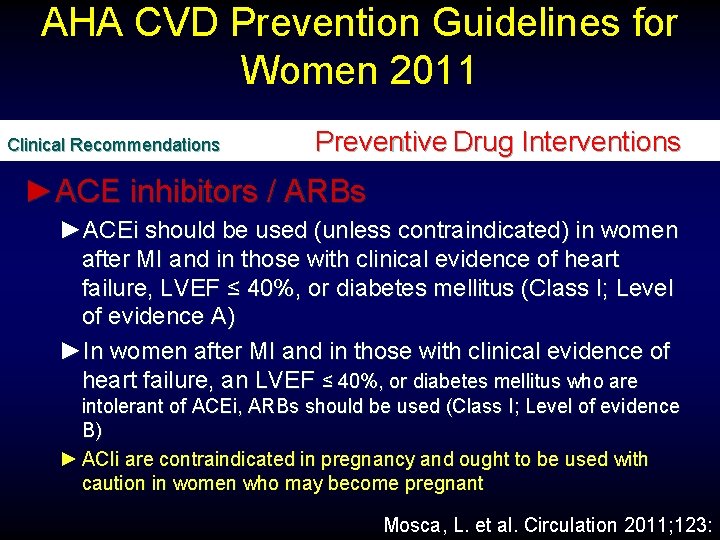
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Preventive Drug Interventions ►ACE inhibitors / ARBs ►ACEi should be used (unless contraindicated) in women after MI and in those with clinical evidence of heart failure, LVEF ≤ 40%, or diabetes mellitus (Class I; Level of evidence A) ►In women after MI and in those with clinical evidence of heart failure, an LVEF ≤ 40%, or diabetes mellitus who are intolerant of ACEi, ARBs should be used (Class I; Level of evidence B) ► ACIi are contraindicated in pregnancy and ought to be used with caution in women who may become pregnant Mosca, L. et al. Circulation 2011; 123:
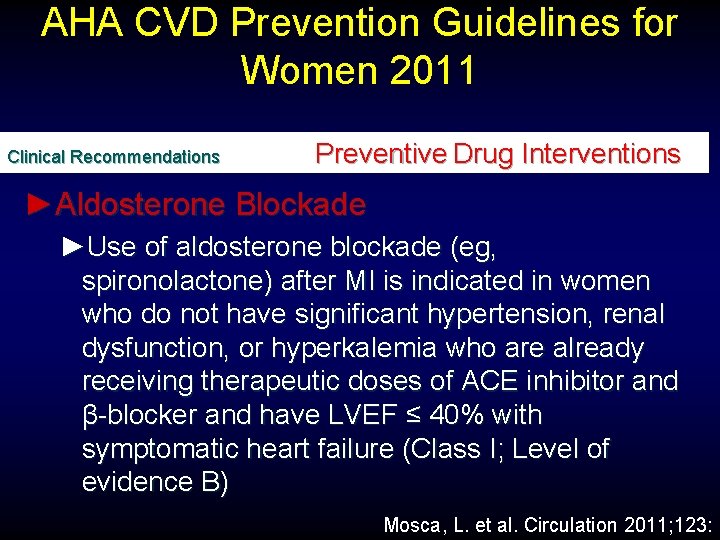
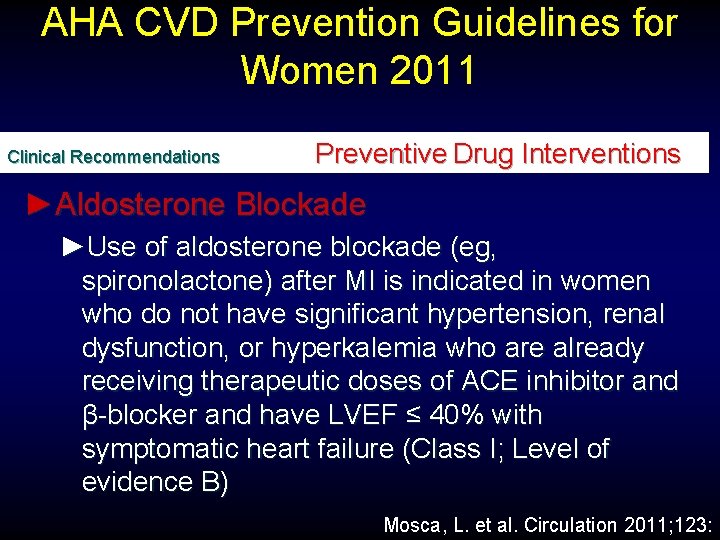
AHA CVD Prevention Guidelines for Women 2011 Clinical Recommendations Preventive Drug Interventions ►Aldosterone Blockade ►Use of aldosterone blockade (eg, spironolactone) after MI is indicated in women who do not have significant hypertension, renal dysfunction, or hyperkalemia who are already receiving therapeutic doses of ACE inhibitor and β-blocker and have LVEF ≤ 40% with symptomatic heart failure (Class I; Level of evidence B) Mosca, L. et al. Circulation 2011; 123:
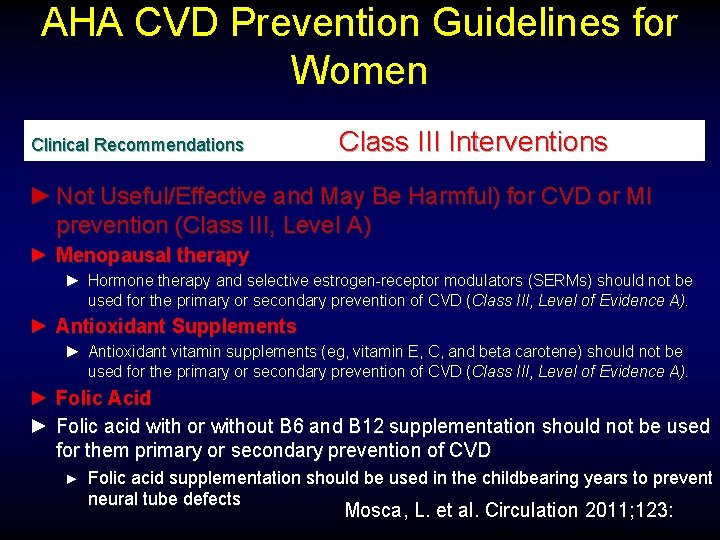
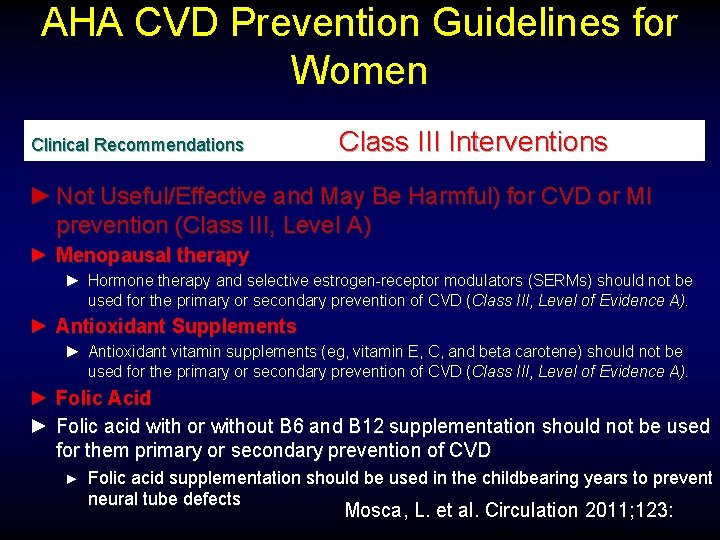
AHA CVD Prevention Guidelines for Women Clinical Recommendations Class III Interventions ► Not Useful/Effective and May Be Harmful) for CVD or MI prevention (Class III, Level A) ► Menopausal therapy ► Hormone therapy and selective estrogen-receptor modulators (SERMs) should not be used for the primary or secondary prevention of CVD (Class III, Level of Evidence A). ► Antioxidant Supplements ► Antioxidant vitamin supplements (eg, vitamin E, C, and beta carotene) should not be used for the primary or secondary prevention of CVD (Class III, Level of Evidence A). ► Folic Acid ► Folic acid with or without B 6 and B 12 supplementation should not be used for them primary or secondary prevention of CVD ► Folic acid supplementation should be used in the childbearing years to prevent neural tube defects Mosca, L. et al. Circulation 2011; 123:
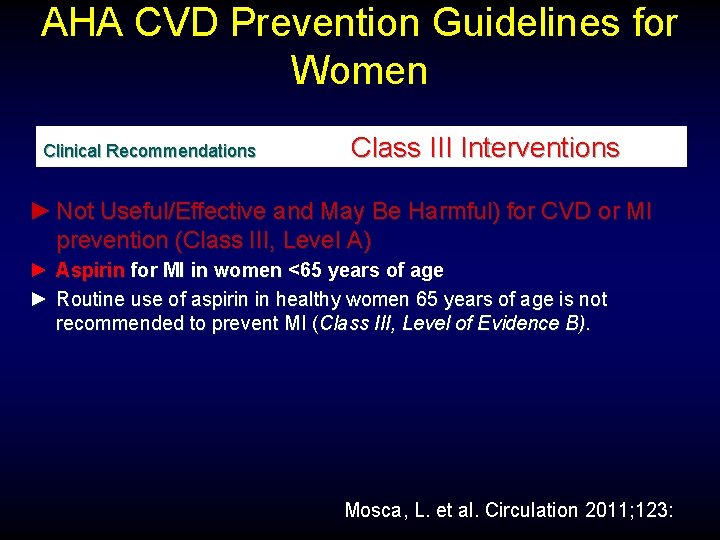
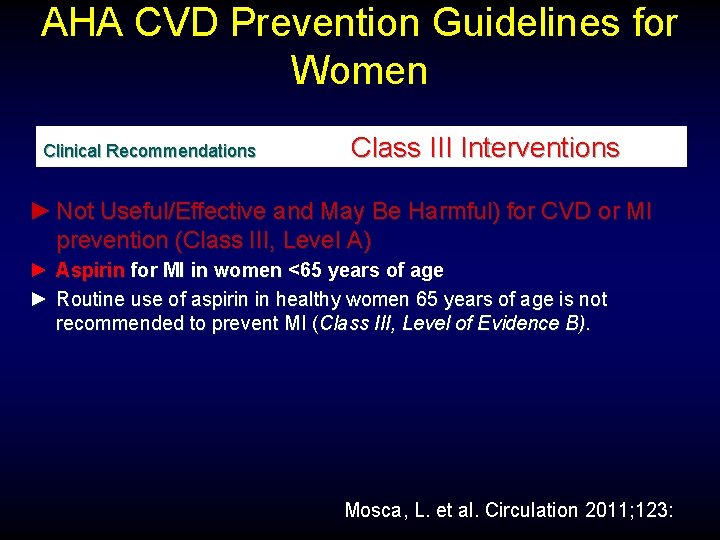
AHA CVD Prevention Guidelines for Women Clinical Recommendations Class III Interventions ► Not Useful/Effective and May Be Harmful) for CVD or MI prevention (Class III, Level A) ► Aspirin for MI in women <65 years of age ► Routine use of aspirin in healthy women 65 years of age is not recommended to prevent MI (Class III, Level of Evidence B). Mosca, L. et al. Circulation 2011; 123:
Case 30 yr old WF Metabolic syndrome Severe hypertriglyceridemia
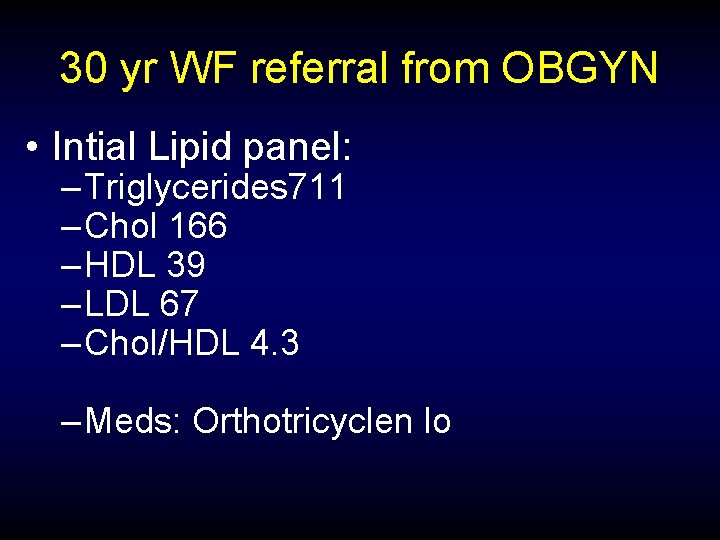
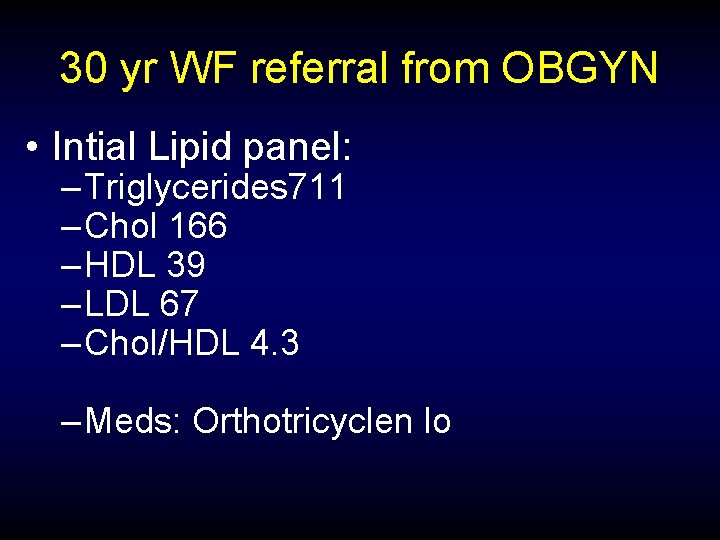
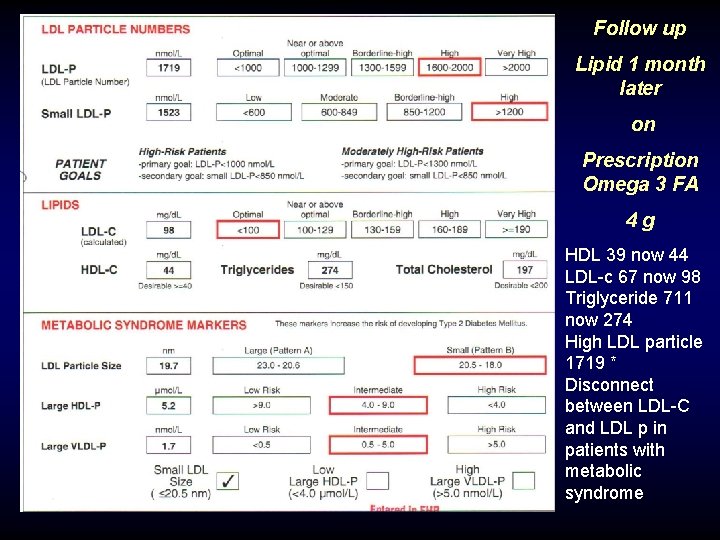
30 yr WF referral from OBGYN • Intial Lipid panel: – Triglycerides 711 – Chol 166 – HDL 39 – LDL 67 – Chol/HDL 4. 3 – Meds: Orthotricyclen lo
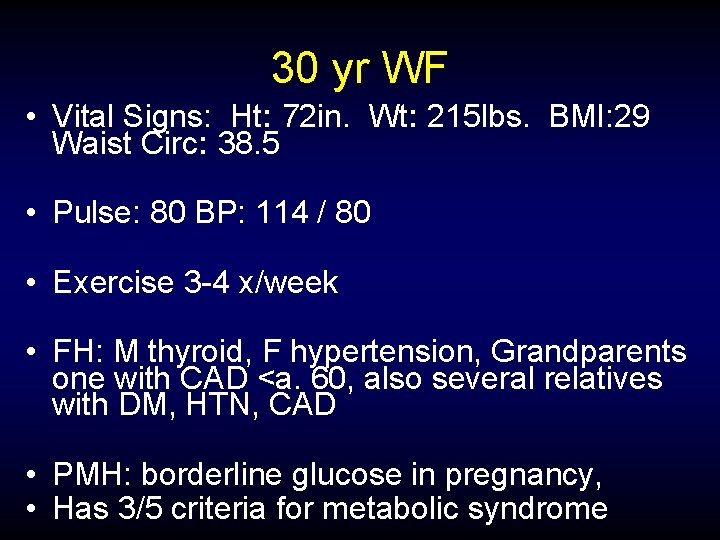
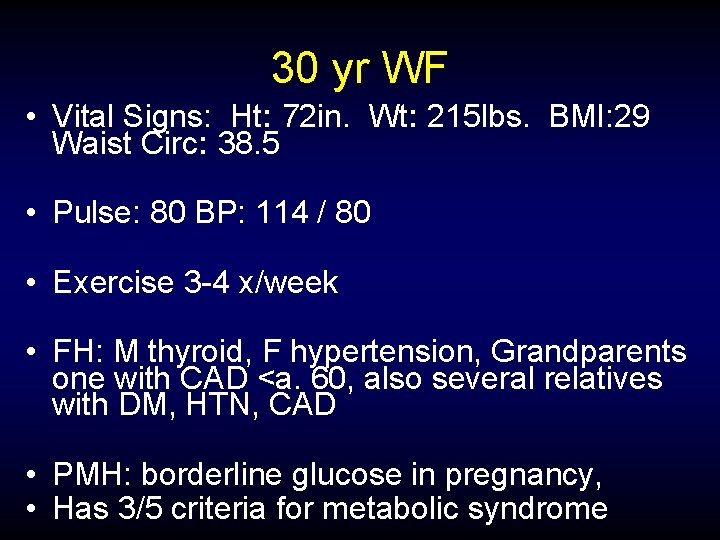
30 yr WF • Vital Signs: Ht: 72 in. Wt: 215 lbs. BMI: 29 Waist Circ: 38. 5 • Pulse: 80 BP: 114 / 80 • Exercise 3 -4 x/week • FH: M thyroid, F hypertension, Grandparents one with CAD <a. 60, also several relatives with DM, HTN, CAD • PMH: borderline glucose in pregnancy, • Has 3/5 criteria for metabolic syndrome

Treatment Considerations 30 yr old with very high trigs and metabolic syndrome
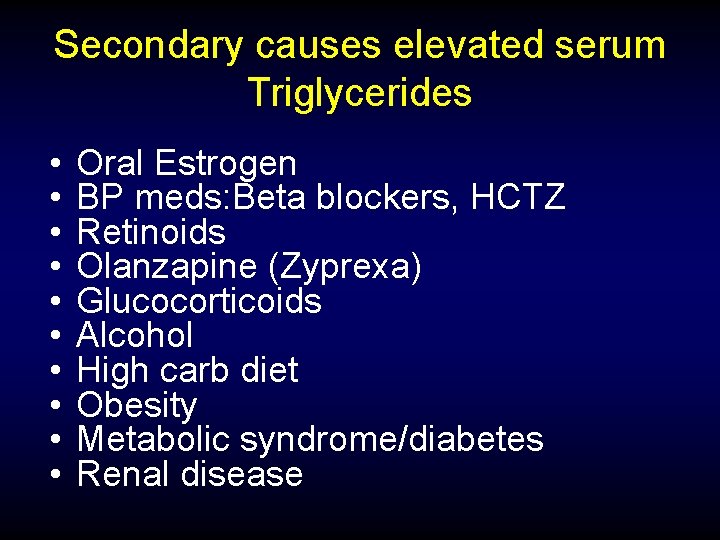
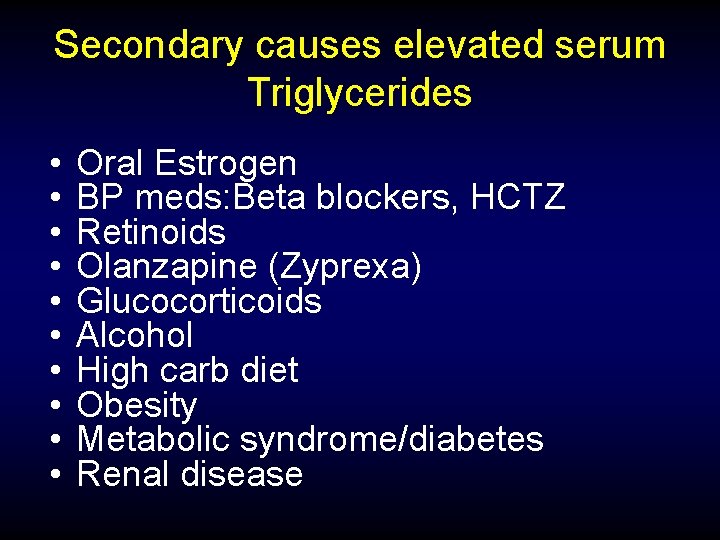
Secondary causes elevated serum Triglycerides • • • Oral Estrogen BP meds: Beta blockers, HCTZ Retinoids Olanzapine (Zyprexa) Glucocorticoids Alcohol High carb diet Obesity Metabolic syndrome/diabetes Renal disease
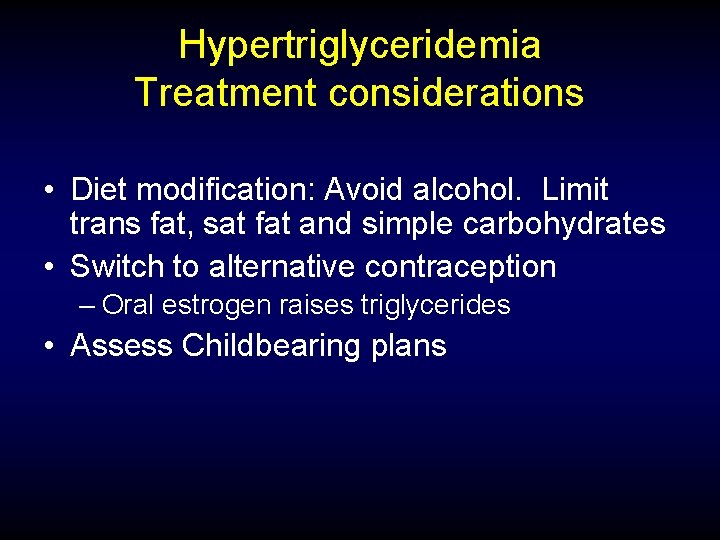
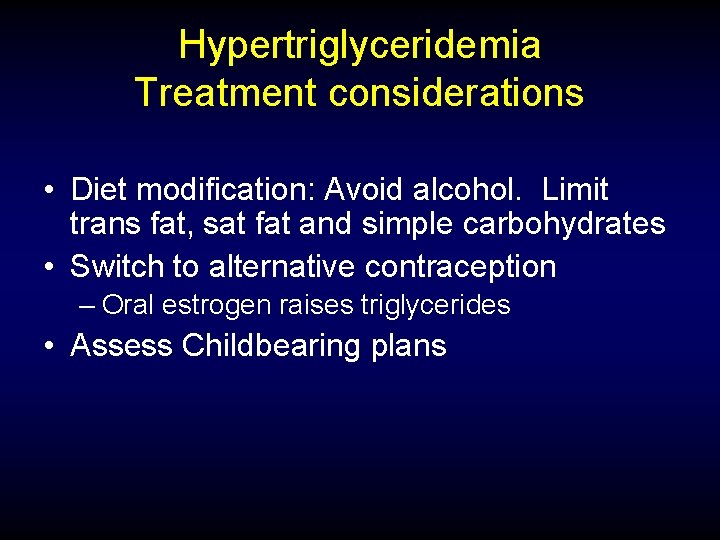
Hypertriglyceridemia Treatment considerations • Diet modification: Avoid alcohol. Limit trans fat, sat fat and simple carbohydrates • Switch to alternative contraception – Oral estrogen raises triglycerides • Assess Childbearing plans
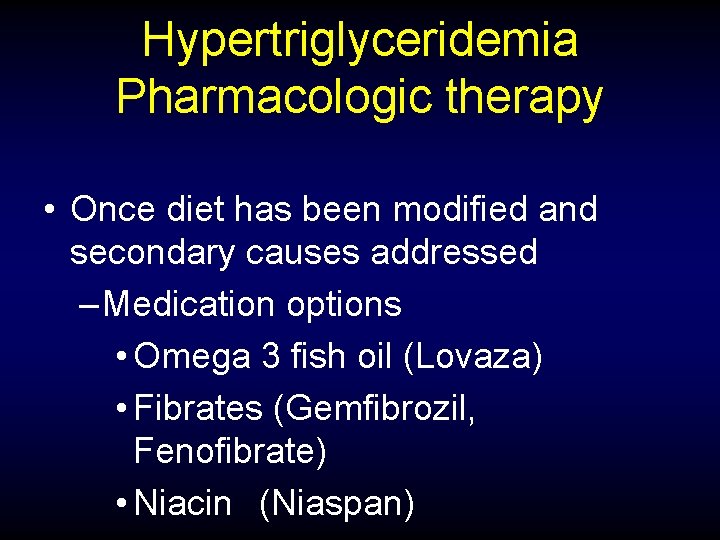
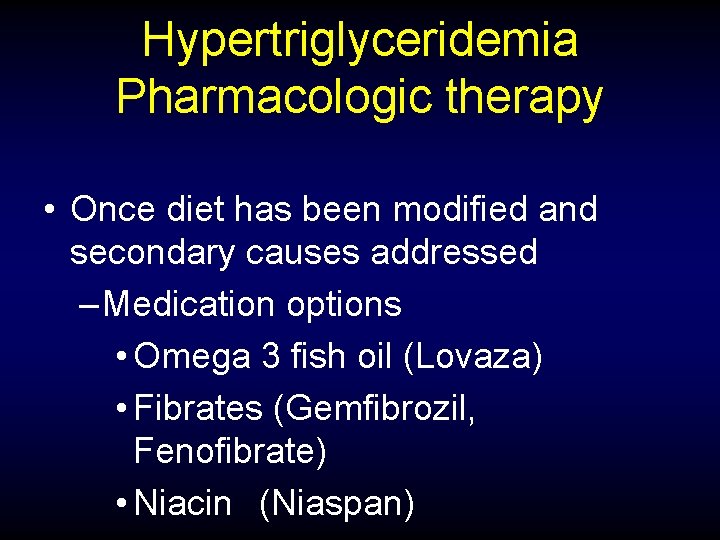
Hypertriglyceridemia Pharmacologic therapy • Once diet has been modified and secondary causes addressed – Medication options • Omega 3 fish oil (Lovaza) • Fibrates (Gemfibrozil, Fenofibrate) • Niacin (Niaspan)
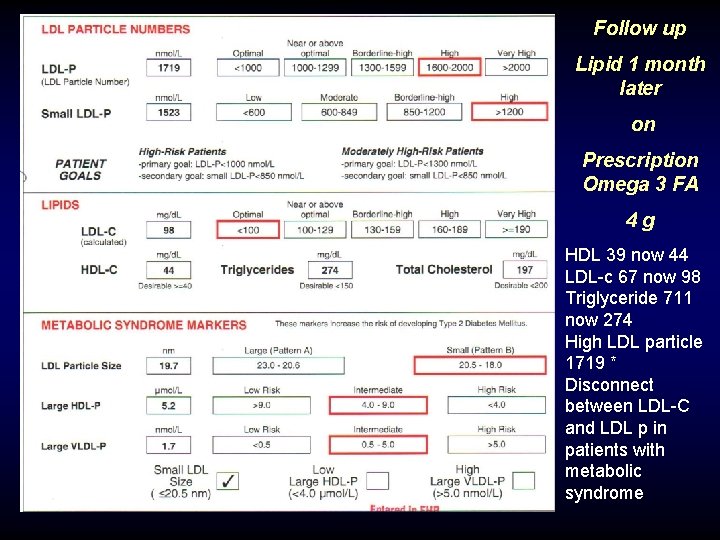
Follow up Lipid 1 month later on Prescription Omega 3 FA 4 g HDL 39 now 44 LDL-c 67 now 98 Triglyceride 711 now 274 High LDL particle 1719 * Disconnect between LDL-C and LDL p in patients with metabolic syndrome
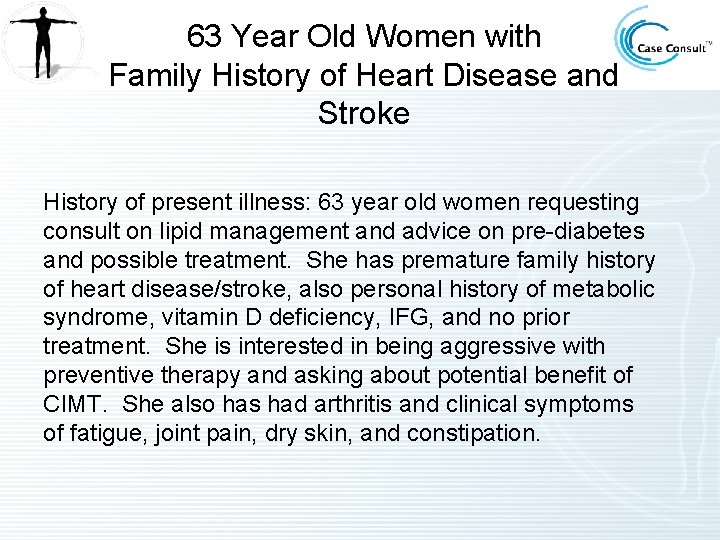
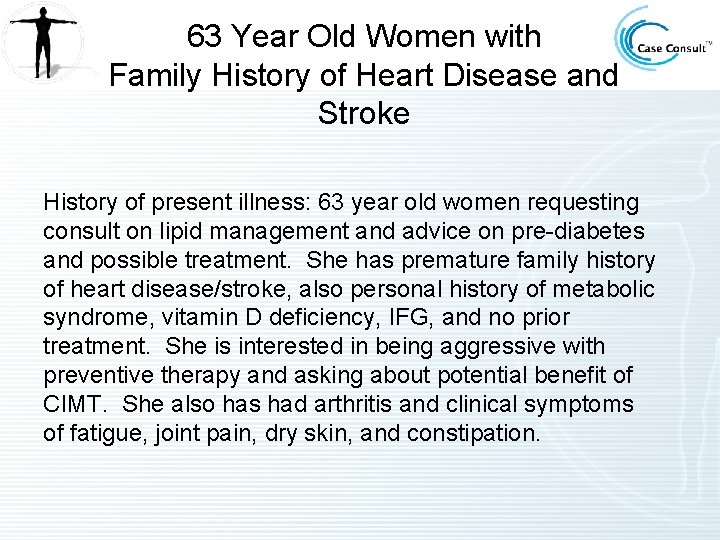
63 Year Old Women with Family History of Heart Disease and Stroke History of present illness: 63 year old women requesting consult on lipid management and advice on pre-diabetes and possible treatment. She has premature family history of heart disease/stroke, also personal history of metabolic syndrome, vitamin D deficiency, IFG, and no prior treatment. She is interested in being aggressive with preventive therapy and asking about potential benefit of CIMT. She also has had arthritis and clinical symptoms of fatigue, joint pain, dry skin, and constipation.
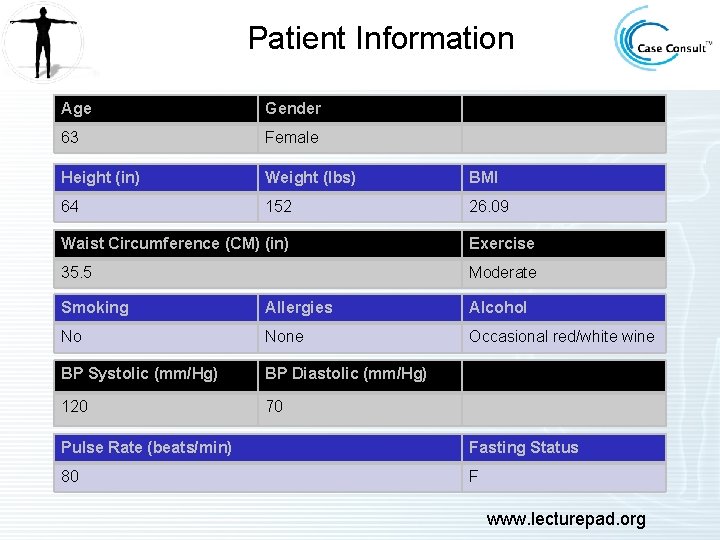
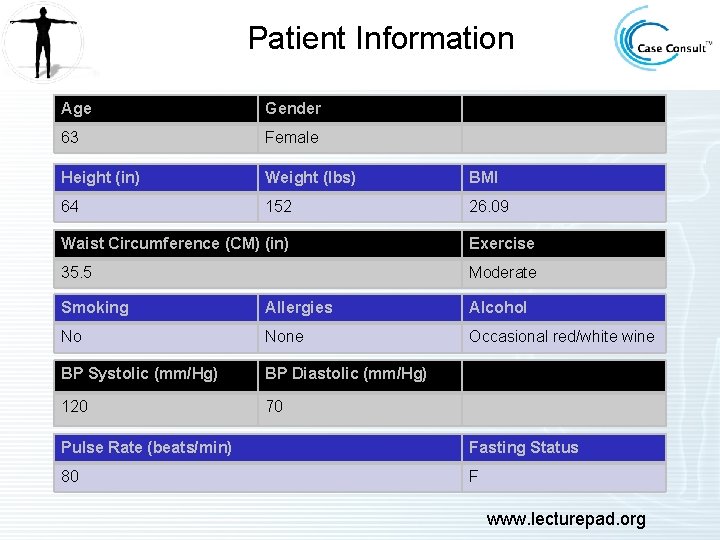
Patient Information Age Gender 63 Female Height (in) Weight (lbs) BMI 64 152 26. 09 Waist Circumference (CM) (in) Exercise 35. 5 Moderate Smoking Allergies Alcohol No None Occasional red/white wine BP Systolic (mm/Hg) BP Diastolic (mm/Hg) 120 70 Pulse Rate (beats/min) Fasting Status 80 F www. lecturepad. org
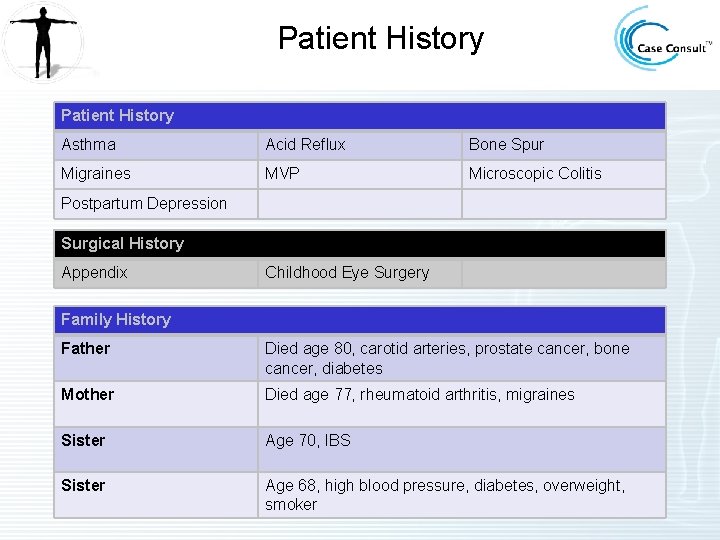
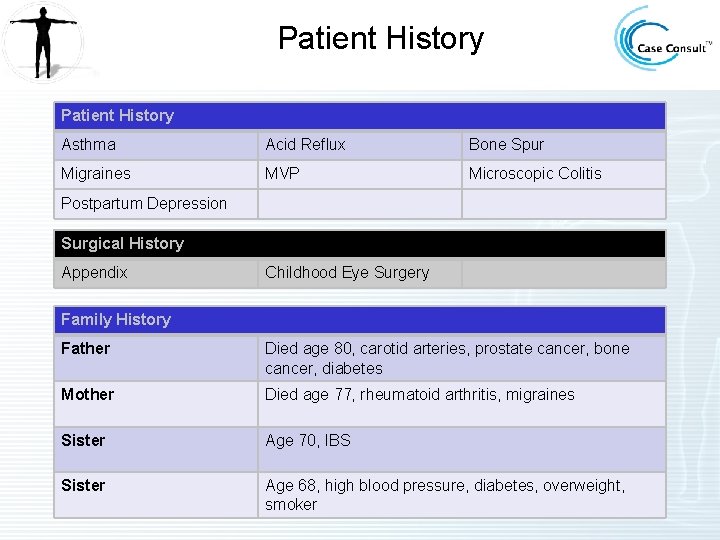
Patient History Asthma Acid Reflux Bone Spur Migraines MVP Microscopic Colitis Postpartum Depression Surgical History Appendix Childhood Eye Surgery Family History Father Died age 80, carotid arteries, prostate cancer, bone cancer, diabetes Mother Died age 77, rheumatoid arthritis, migraines Sister Age 70, IBS Sister Age 68, high blood pressure, diabetes, overweight, smoker
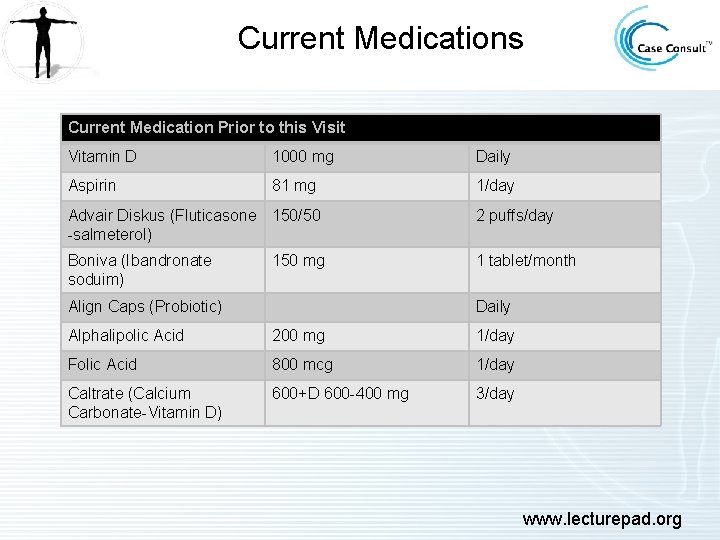
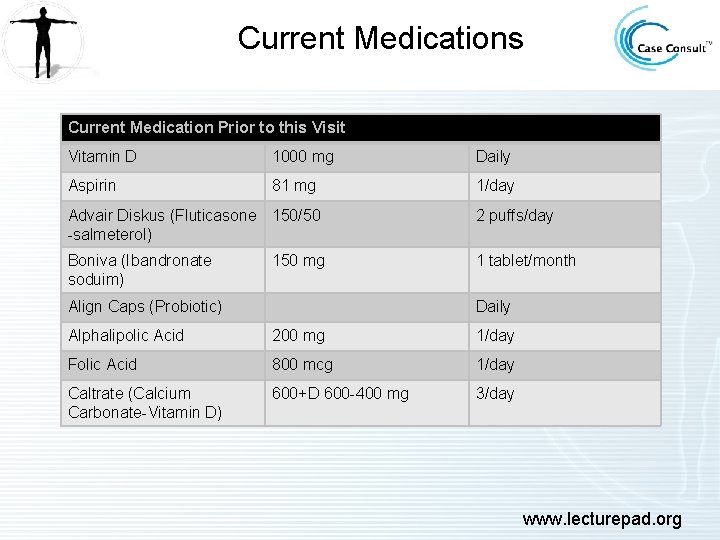
Current Medications Current Medication Prior to this Visit Vitamin D 1000 mg Daily Aspirin 81 mg 1/day Advair Diskus (Fluticasone 150/50 -salmeterol) 2 puffs/day Boniva (Ibandronate soduim) 1 tablet/month 150 mg Align Caps (Probiotic) Daily Alphalipolic Acid 200 mg 1/day Folic Acid 800 mcg 1/day Caltrate (Calcium Carbonate-Vitamin D) 600+D 600 -400 mg 3/day www. lecturepad. org
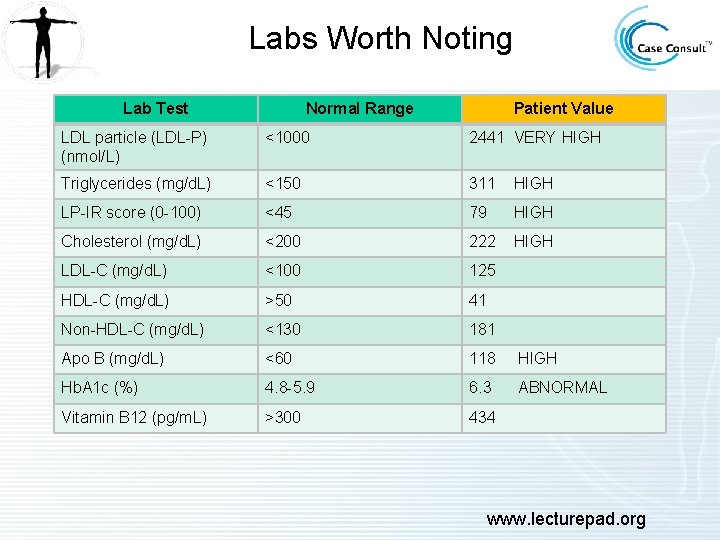
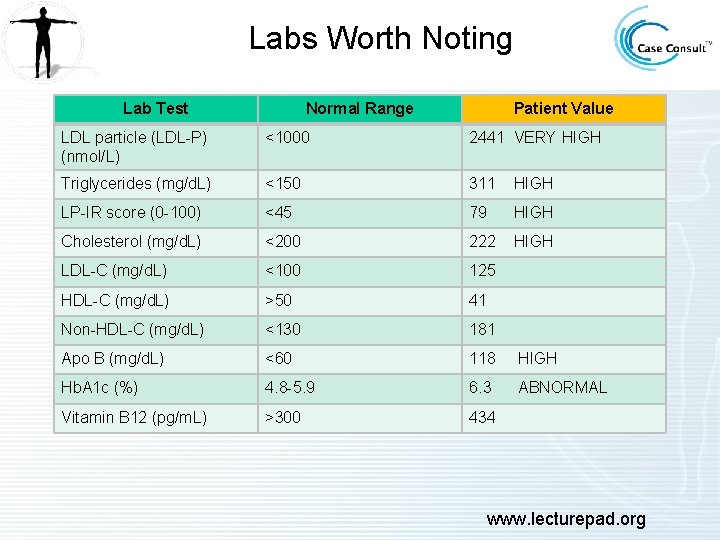
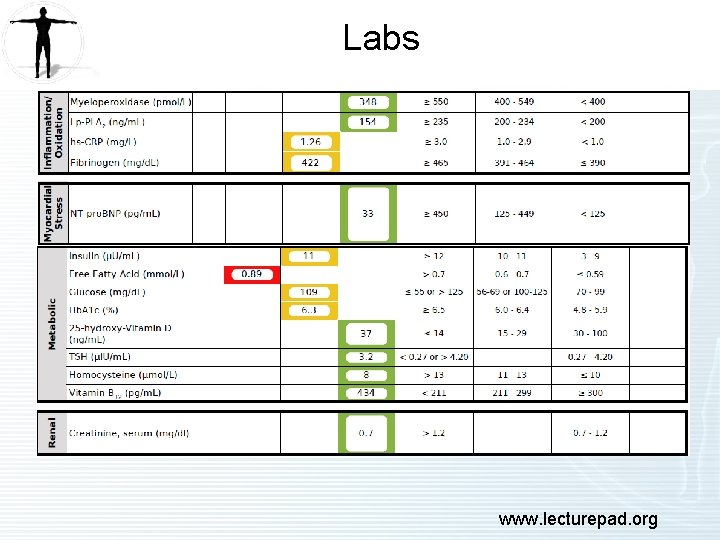
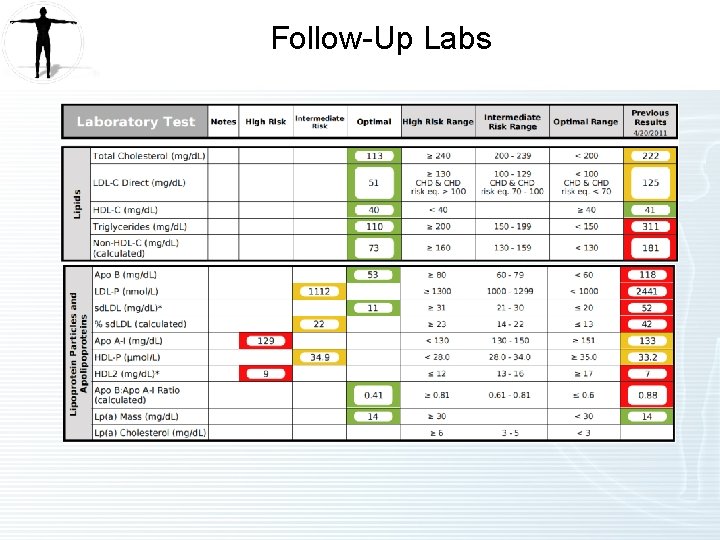
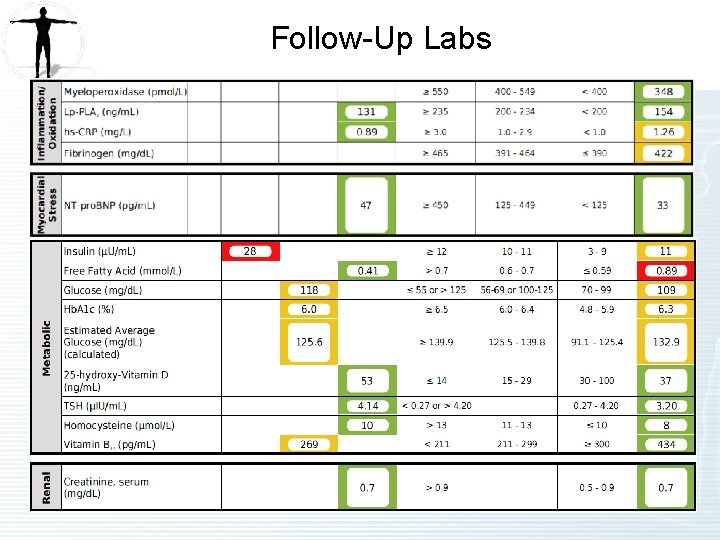
Labs Worth Noting Lab Test Normal Range Patient Value LDL particle (LDL-P) (nmol/L) <1000 2441 VERY HIGH Triglycerides (mg/d. L) <150 311 HIGH LP-IR score (0 -100) <45 79 HIGH Cholesterol (mg/d. L) <200 222 HIGH LDL-C (mg/d. L) <100 125 HDL-C (mg/d. L) >50 41 Non-HDL-C (mg/d. L) <130 181 Apo B (mg/d. L) <60 118 HIGH Hb. A 1 c (%) 4. 8 -5. 9 6. 3 ABNORMAL Vitamin B 12 (pg/m. L) >300 434 www. lecturepad. org
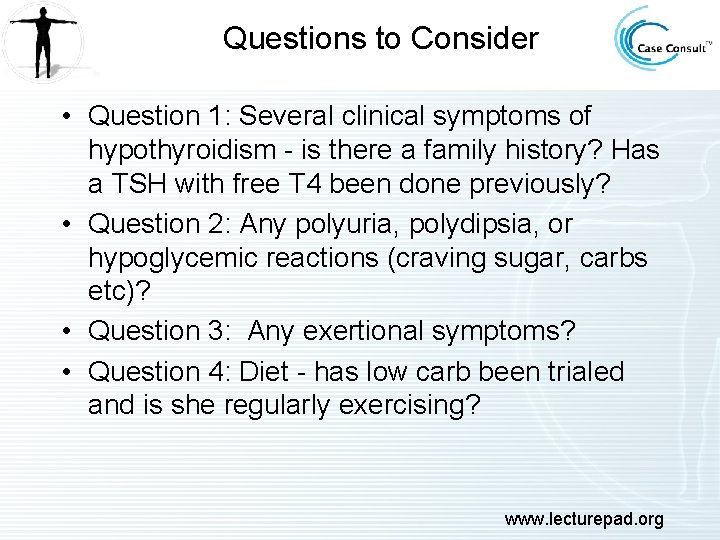
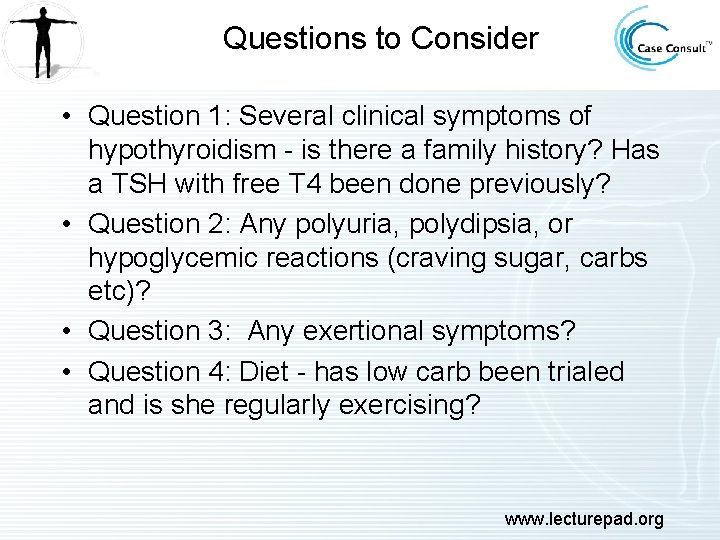
Questions to Consider • Question 1: Several clinical symptoms of hypothyroidism - is there a family history? Has a TSH with free T 4 been done previously? • Question 2: Any polyuria, polydipsia, or hypoglycemic reactions (craving sugar, carbs etc)? • Question 3: Any exertional symptoms? • Question 4: Diet - has low carb been trialed and is she regularly exercising? www. lecturepad. org
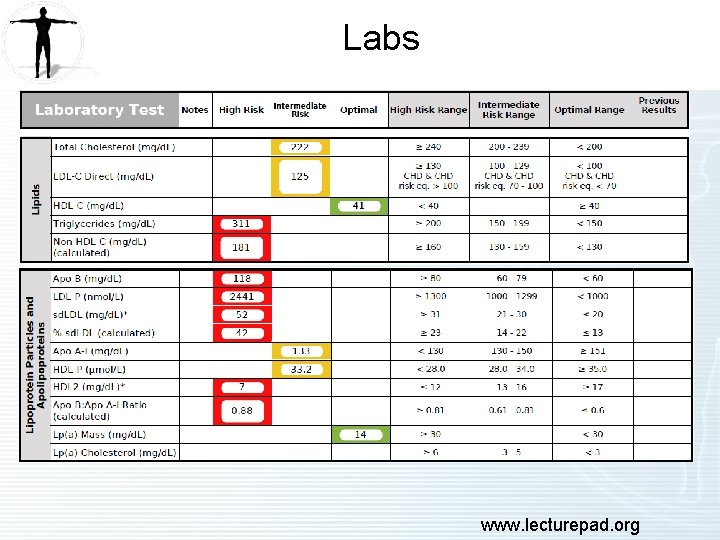
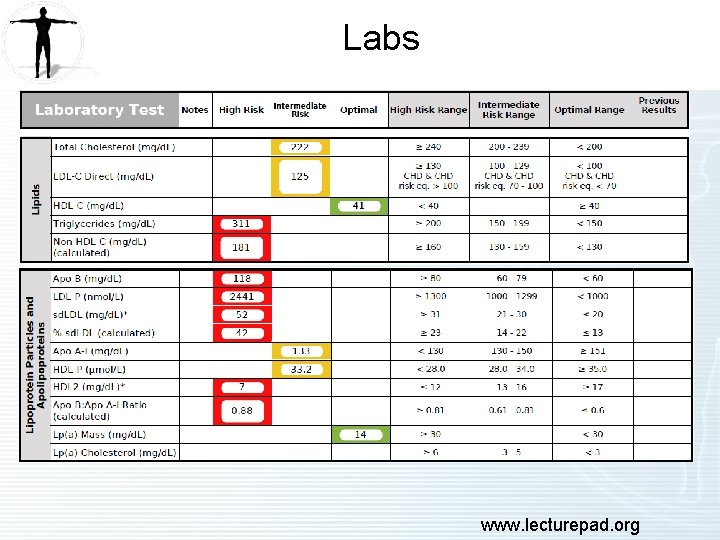
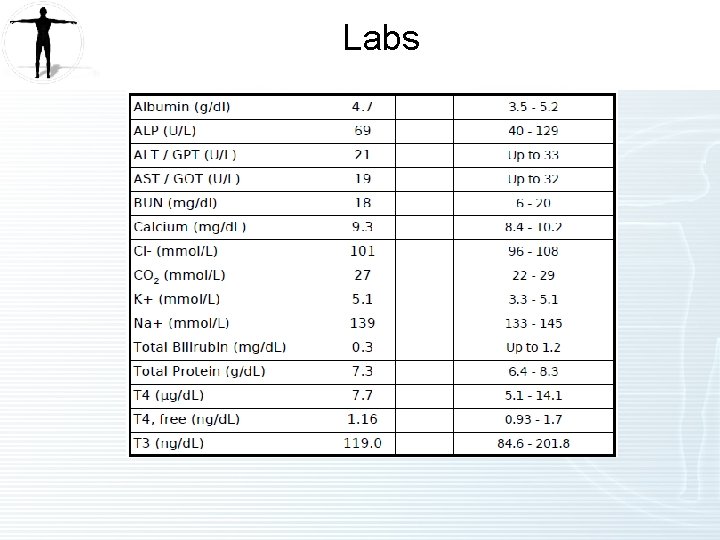
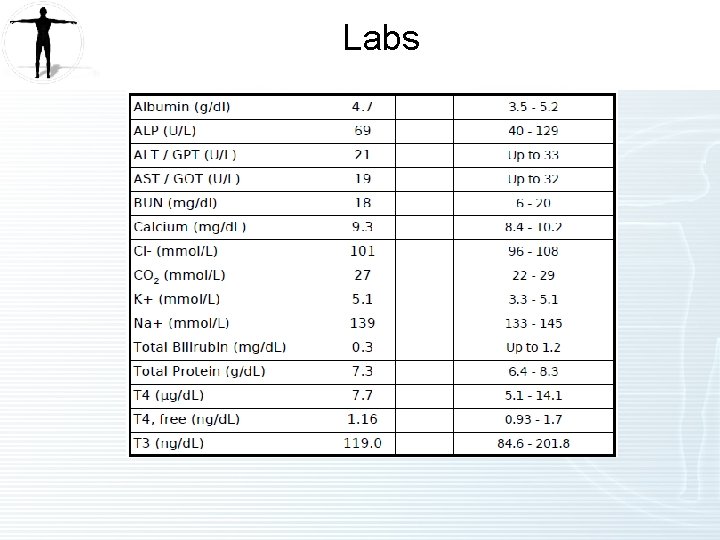
Labs www. lecturepad. org
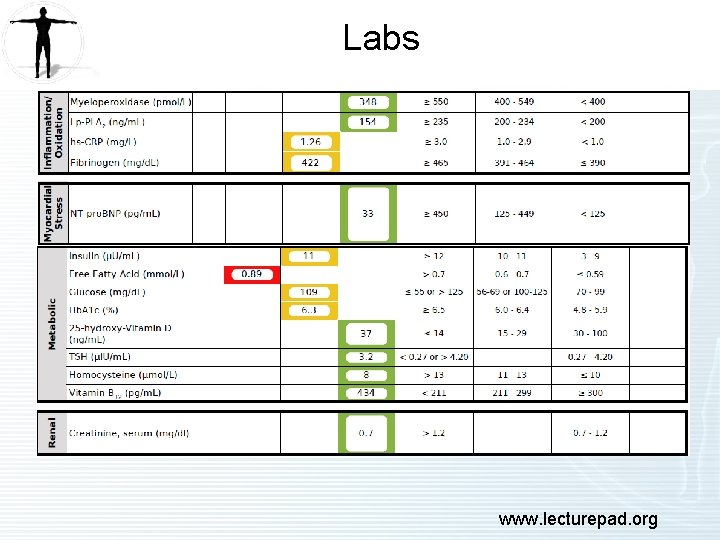
Labs www. lecturepad. org
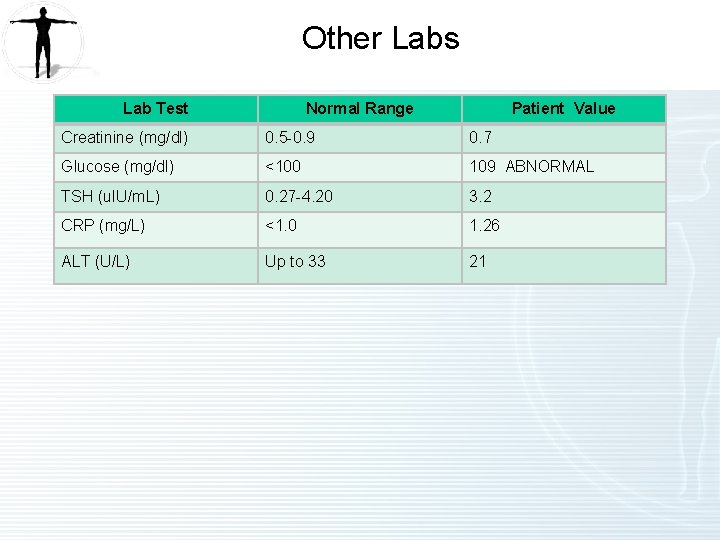
Labs
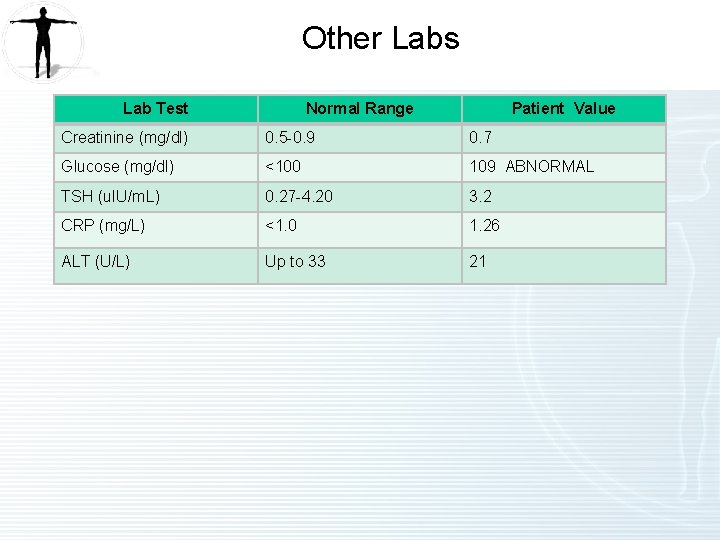
Other Labs Lab Test Normal Range Patient Value Creatinine (mg/dl) 0. 5 -0. 9 0. 7 Glucose (mg/dl) <100 109 ABNORMAL TSH (u. IU/m. L) 0. 27 -4. 20 3. 2 CRP (mg/L) <1. 0 1. 26 ALT (U/L) Up to 33 21
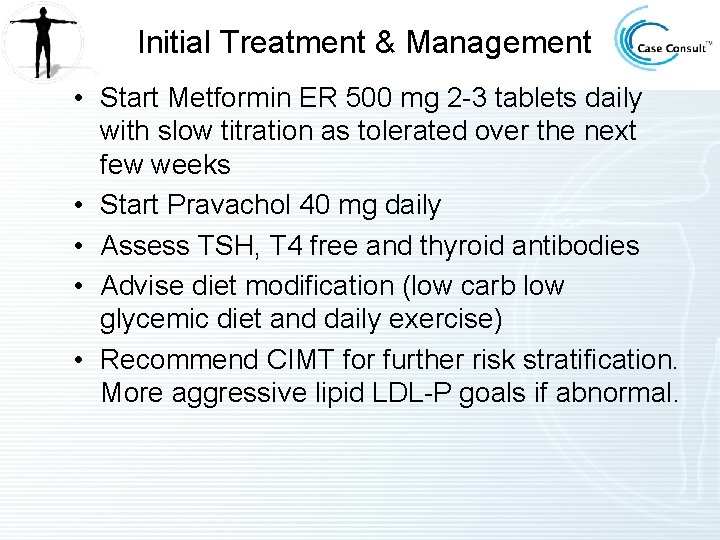
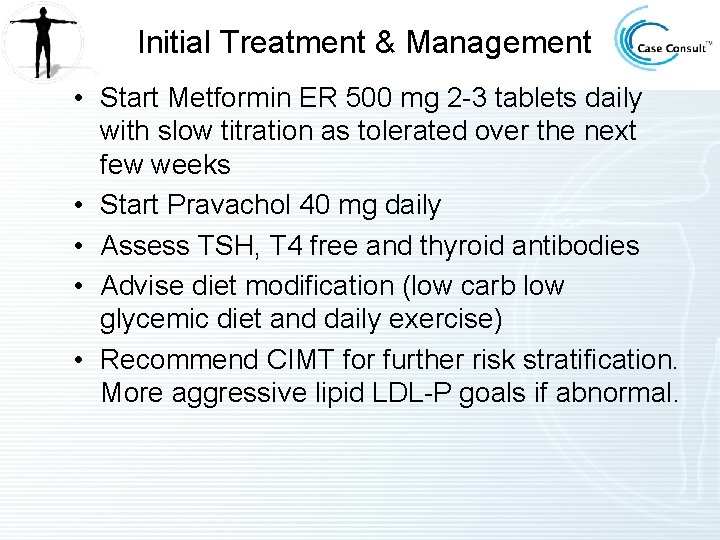
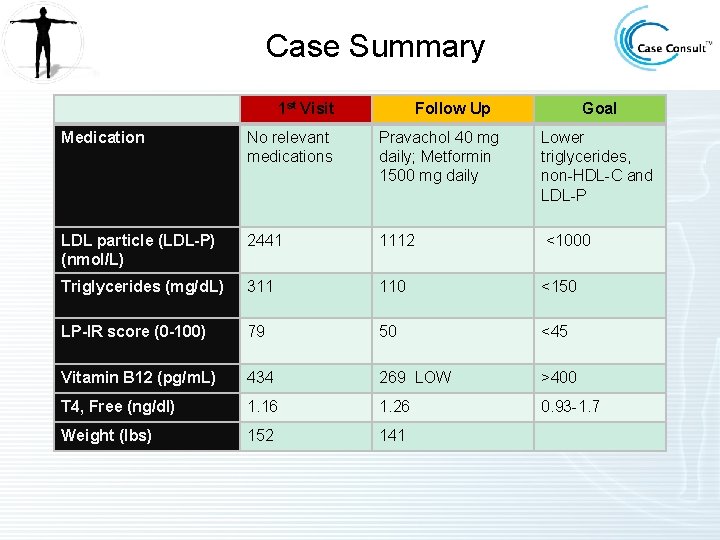
Initial Treatment & Management • Start Metformin ER 500 mg 2 -3 tablets daily with slow titration as tolerated over the next few weeks • Start Pravachol 40 mg daily • Assess TSH, T 4 free and thyroid antibodies • Advise diet modification (low carb low glycemic diet and daily exercise) • Recommend CIMT for further risk stratification. More aggressive lipid LDL-P goals if abnormal.
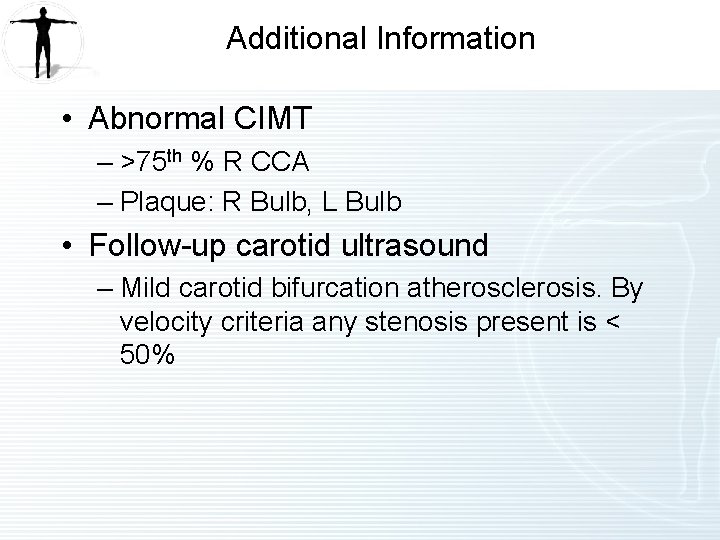
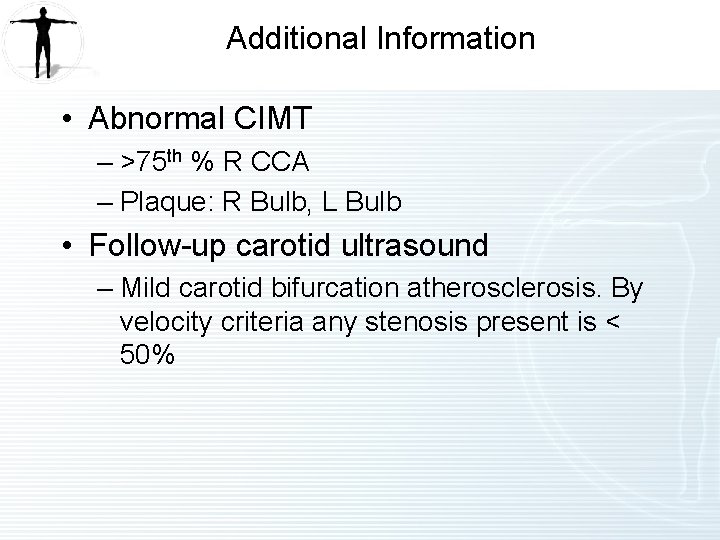
Additional Information • Abnormal CIMT – >75 th % R CCA – Plaque: R Bulb, L Bulb • Follow-up carotid ultrasound – Mild carotid bifurcation atherosclerosis. By velocity criteria any stenosis present is < 50%
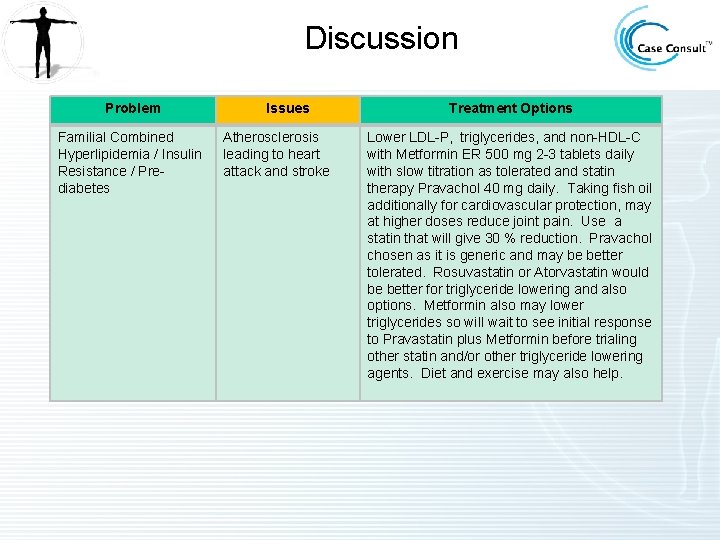
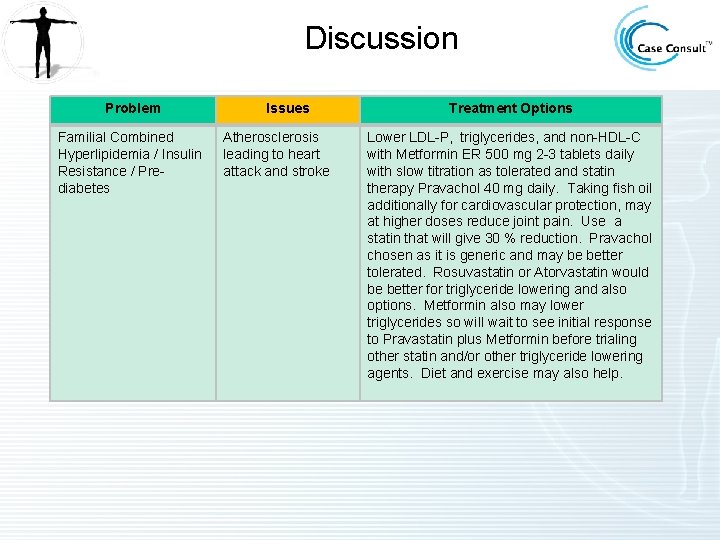
Discussion Problem Familial Combined Hyperlipidemia / Insulin Resistance / Prediabetes Issues Atherosclerosis leading to heart attack and stroke Treatment Options Lower LDL-P, triglycerides, and non-HDL-C with Metformin ER 500 mg 2 -3 tablets daily with slow titration as tolerated and statin therapy Pravachol 40 mg daily. Taking fish oil additionally for cardiovascular protection, may at higher doses reduce joint pain. Use a statin that will give 30 % reduction. Pravachol chosen as it is generic and may be better tolerated. Rosuvastatin or Atorvastatin would be better for triglyceride lowering and also options. Metformin also may lower triglycerides so will wait to see initial response to Pravastatin plus Metformin before trialing other statin and/or other triglyceride lowering agents. Diet and exercise may also help.
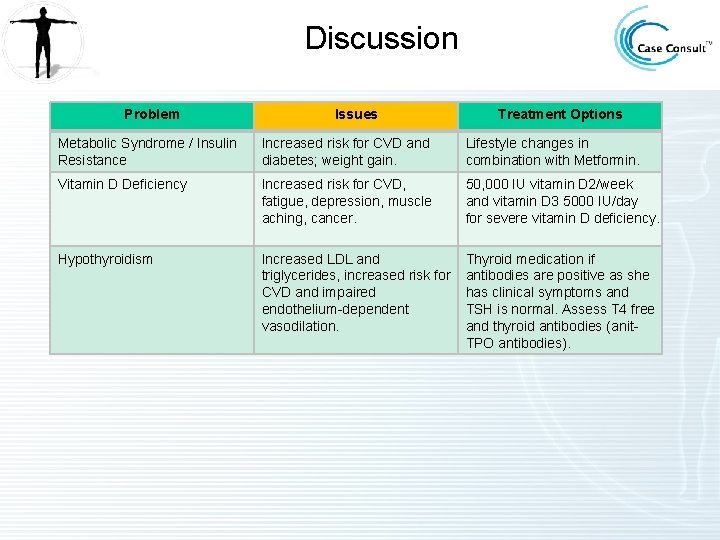
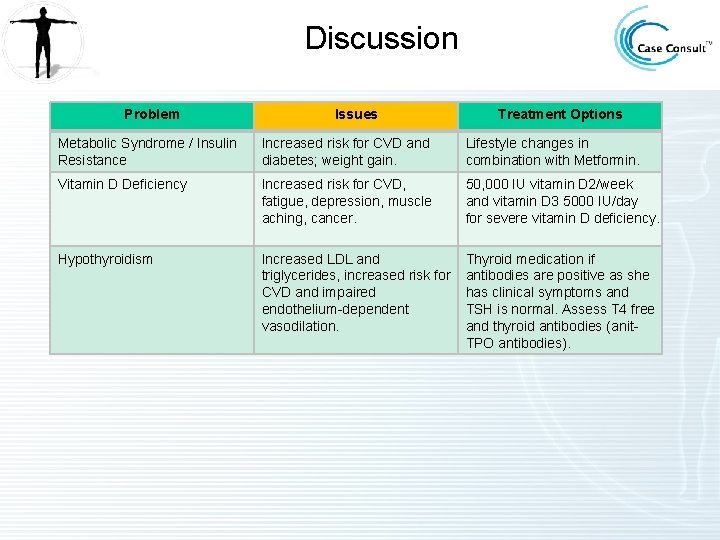
Discussion Problem Issues Treatment Options Metabolic Syndrome / Insulin Resistance Increased risk for CVD and diabetes; weight gain. Lifestyle changes in combination with Metformin. Vitamin D Deficiency Increased risk for CVD, fatigue, depression, muscle aching, cancer. 50, 000 IU vitamin D 2/week and vitamin D 3 5000 IU/day for severe vitamin D deficiency. Hypothyroidism Increased LDL and triglycerides, increased risk for CVD and impaired endothelium-dependent vasodilation. Thyroid medication if antibodies are positive as she has clinical symptoms and TSH is normal. Assess T 4 free and thyroid antibodies (anit. TPO antibodies).
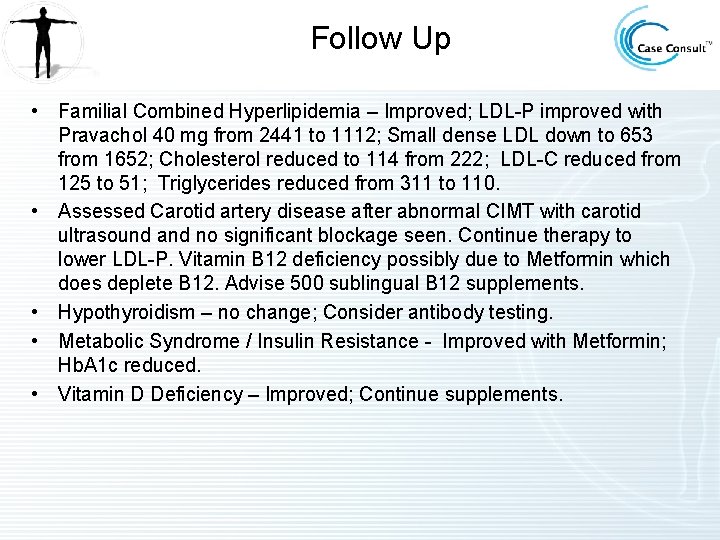
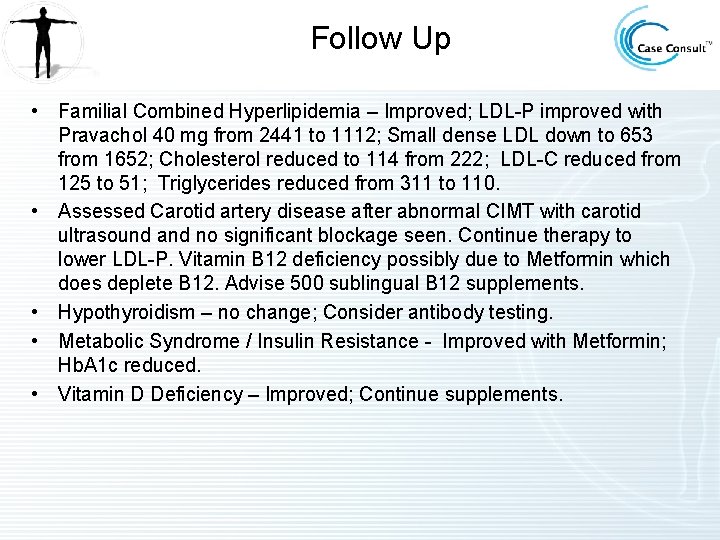
Follow Up • Familial Combined Hyperlipidemia – Improved; LDL-P improved with Pravachol 40 mg from 2441 to 1112; Small dense LDL down to 653 from 1652; Cholesterol reduced to 114 from 222; LDL-C reduced from 125 to 51; Triglycerides reduced from 311 to 110. • Assessed Carotid artery disease after abnormal CIMT with carotid ultrasound and no significant blockage seen. Continue therapy to lower LDL-P. Vitamin B 12 deficiency possibly due to Metformin which does deplete B 12. Advise 500 sublingual B 12 supplements. • Hypothyroidism – no change; Consider antibody testing. • Metabolic Syndrome / Insulin Resistance - Improved with Metformin; Hb. A 1 c reduced. • Vitamin D Deficiency – Improved; Continue supplements.
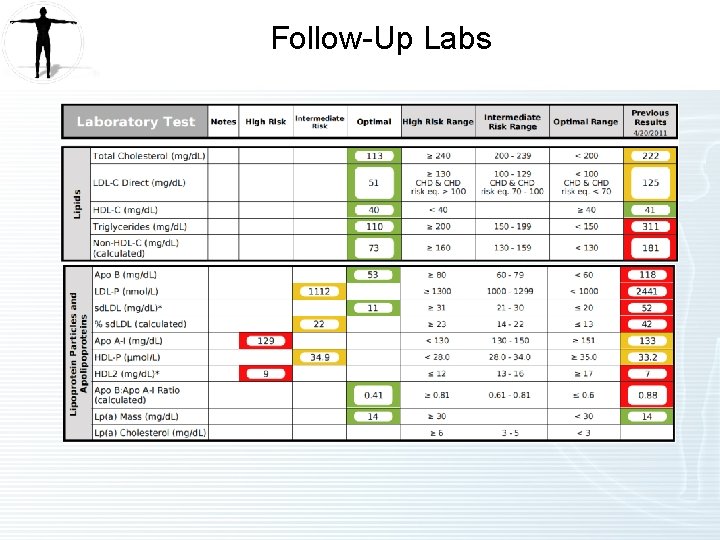
Follow-Up Labs
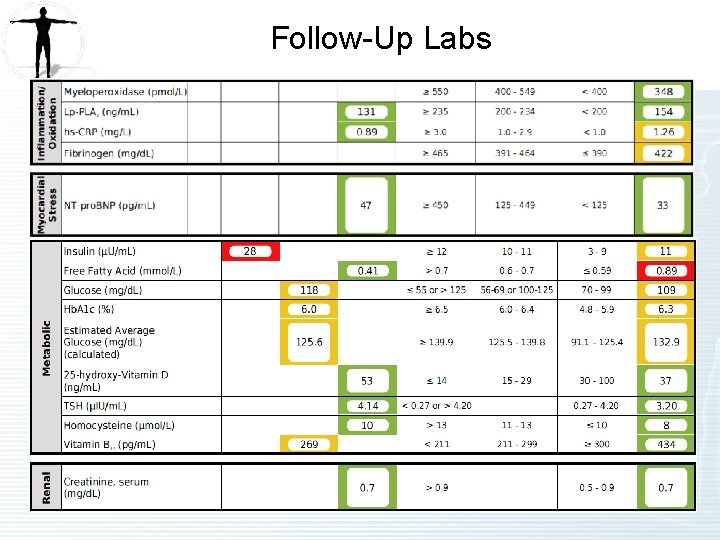
Follow-Up Labs

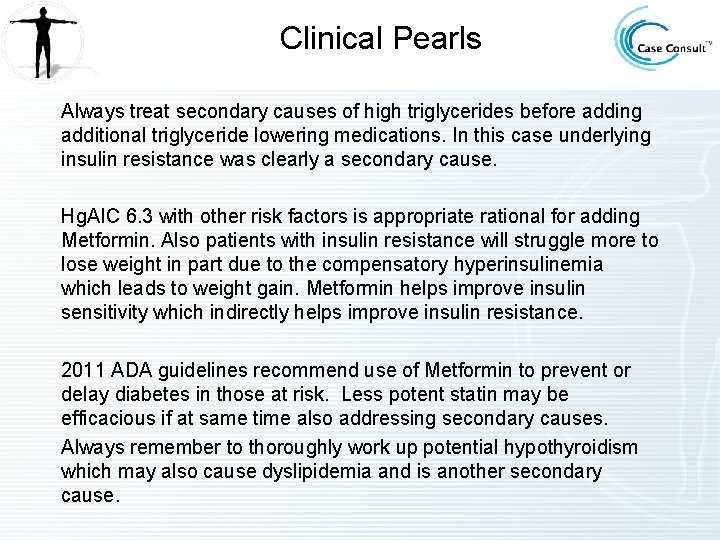
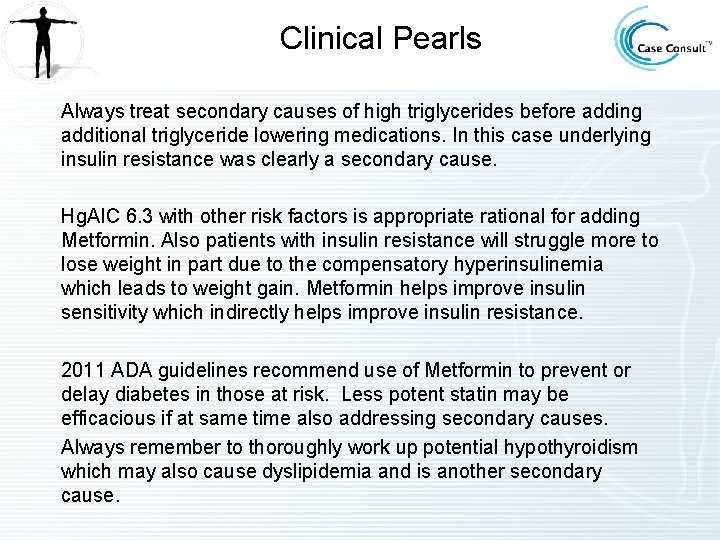
Clinical Pearls Always treat secondary causes of high triglycerides before adding additional triglyceride lowering medications. In this case underlying insulin resistance was clearly a secondary cause. Hg. AIC 6. 3 with other risk factors is appropriate rational for adding Metformin. Also patients with insulin resistance will struggle more to lose weight in part due to the compensatory hyperinsulinemia which leads to weight gain. Metformin helps improve insulin sensitivity which indirectly helps improve insulin resistance. 2011 ADA guidelines recommend use of Metformin to prevent or delay diabetes in those at risk. Less potent statin may be efficacious if at same time also addressing secondary causes. Always remember to thoroughly work up potential hypothyroidism which may also cause dyslipidemia and is another secondary cause.
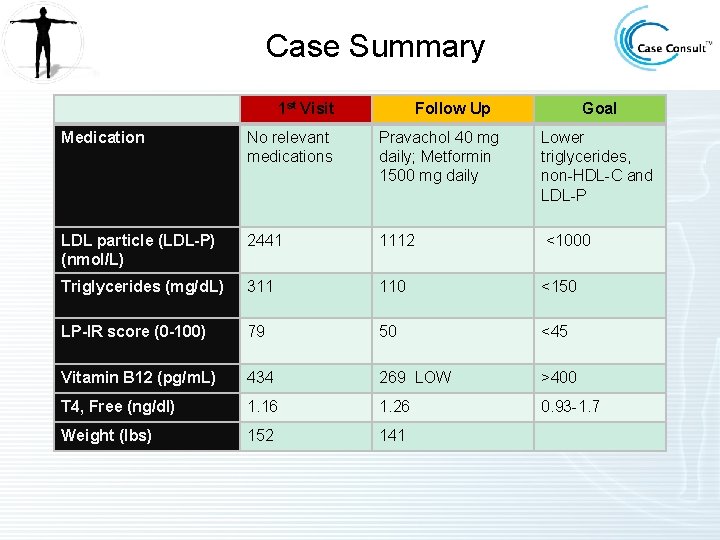
Case Summary 1 st Visit Follow Up Goal Medication No relevant medications Pravachol 40 mg daily; Metformin 1500 mg daily Lower triglycerides, non-HDL-C and LDL-P LDL particle (LDL-P) (nmol/L) 2441 1112 <1000 Triglycerides (mg/d. L) 311 110 <150 LP-IR score (0 -100) 79 50 <45 Vitamin B 12 (pg/m. L) 434 269 LOW >400 T 4, Free (ng/dl) 1. 16 1. 26 0. 93 -1. 7 Weight (lbs) 152 141
Take home points • Low HDL or High triglycerides in a women should concern you • Therapeutic lifestyle changes essential to intiate in all women regardless of risk. • Consider evaluation of patients at risk with NMR lipoprofile, Apo B, hs. CRP or at minimum treat to non. HDL goals • Estrogen taken orally will impact lipids , screen first
Questions? • taradall@lecturepad. org • Register free on nonprofit educational website www. lecturepad. org for more cases, live lectures and ongoing education from Dr. Tara Dall and other experts
 Tara dall md
Tara dall md Chapter 11 the cardiovascular system
Chapter 11 the cardiovascular system Cardiovascular disease risk factor
Cardiovascular disease risk factor Bharathi viswanathan
Bharathi viswanathan Infinitamente grande e infinitamente piccolo
Infinitamente grande e infinitamente piccolo Pareggiate dell'imbianchino
Pareggiate dell'imbianchino Cinzia parolini
Cinzia parolini Esempi prove strutturate per classi parallele scuola media
Esempi prove strutturate per classi parallele scuola media Cerchio parallelo al pv
Cerchio parallelo al pv Excursus storico dall'integrazione all'inclusione
Excursus storico dall'integrazione all'inclusione Caroline dall
Caroline dall Quale continente è tagliato a metà dall'equatore
Quale continente è tagliato a metà dall'equatore Paesaggio con fuga in egitto
Paesaggio con fuga in egitto Impianto autodiegetico
Impianto autodiegetico Letto visto dall'alto disegno
Letto visto dall'alto disegno Dal papiro alla carta
Dal papiro alla carta La parola bullismo deriva dall'inglese
La parola bullismo deriva dall'inglese La vita che avrai non sarà mai distante dall'amore che dai
La vita che avrai non sarà mai distante dall'amore che dai La forza centrifuga si modifica variando la velocità
La forza centrifuga si modifica variando la velocità Nella cmr la presa in carico è un atto complesso
Nella cmr la presa in carico è un atto complesso Composti organici derivati dall'ammoniaca
Composti organici derivati dall'ammoniaca Domenico dall'olio
Domenico dall'olio Dal bello al vero
Dal bello al vero Dall'aurora al tramonto canto ingresso
Dall'aurora al tramonto canto ingresso Energia termica dall'oceano
Energia termica dall'oceano Genitori giacomo leopardi
Genitori giacomo leopardi Nei freni la forza frenante è amplificata dall'abs
Nei freni la forza frenante è amplificata dall'abs Centro cardiovascular
Centro cardiovascular Lesson 11 cardiovascular system
Lesson 11 cardiovascular system Chapter 5 the cardiovascular system labeling exercises
Chapter 5 the cardiovascular system labeling exercises Clinica cardiovascular santa maria
Clinica cardiovascular santa maria What makes up the circulatory system
What makes up the circulatory system Atraumatic tip
Atraumatic tip Capillary bed labeled
Capillary bed labeled Chapter 17 cardiovascular emergencies
Chapter 17 cardiovascular emergencies Fsico
Fsico Introduction of heart
Introduction of heart Chapter 26 the child with a cardiovascular disorder
Chapter 26 the child with a cardiovascular disorder Figure 11-8 arteries
Figure 11-8 arteries Quiz sistema cardiovascular
Quiz sistema cardiovascular Its tubular dude
Its tubular dude Chapter 11 the cardiovascular system figure 11-2
Chapter 11 the cardiovascular system figure 11-2 Pequena circulacao
Pequena circulacao The ability to release maximum force very quickly
The ability to release maximum force very quickly Circulatory system tissue
Circulatory system tissue Chapter 46 the child with a cardiovascular alteration
Chapter 46 the child with a cardiovascular alteration Major arteries
Major arteries Rias hipertension arterial
Rias hipertension arterial Amit pursnani
Amit pursnani Riesgo cardiovascular por perimetro abdominal
Riesgo cardiovascular por perimetro abdominal Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 Chapter 13 cardiovascular system
Chapter 13 cardiovascular system What is cardiovascular endurance in health related fitness
What is cardiovascular endurance in health related fitness American board of cardiovascular medicine
American board of cardiovascular medicine Chapter 19 the cardiovascular system blood vessels
Chapter 19 the cardiovascular system blood vessels Chapter 11 the cardiovascular system figure 11-10 answers
Chapter 11 the cardiovascular system figure 11-10 answers The cardiovascular system includes the
The cardiovascular system includes the Isometric vs isotonic
Isometric vs isotonic When does stroke volume increase
When does stroke volume increase Pequena e grande circulação
Pequena e grande circulação Salud cardiovascular
Salud cardiovascular Generalidades del sistema cardiovascular
Generalidades del sistema cardiovascular Sistole
Sistole Chapter 26 the child with a cardiovascular disorder
Chapter 26 the child with a cardiovascular disorder Pithed rat
Pithed rat What is arteriolar tone
What is arteriolar tone Maniobra de pachon
Maniobra de pachon Rosita rodriguez
Rosita rodriguez Cardiovascular system
Cardiovascular system Advanced cardiovascular life support
Advanced cardiovascular life support Cmqcc cardiovascular toolkit
Cmqcc cardiovascular toolkit Chapter 11 the cardiovascular system
Chapter 11 the cardiovascular system Pequenos vasos sanguineos
Pequenos vasos sanguineos Exercício fisico
Exercício fisico Crash course heart
Crash course heart Wheezing
Wheezing Fitness chapter 7
Fitness chapter 7 Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Cardiovascular research institute basel
Cardiovascular research institute basel Bhf glasgow cardiovascular research centre
Bhf glasgow cardiovascular research centre Wolters kluwer
Wolters kluwer National cardiovascular partners
National cardiovascular partners Sistema cardiovascular sus partes
Sistema cardiovascular sus partes Paratiroidea
Paratiroidea Salud cardiovascular
Salud cardiovascular Tara maltby
Tara maltby Proyecto tara
Proyecto tara Etlw
Etlw Tara reid
Tara reid Tara thieme
Tara thieme Cod tara romania 642
Cod tara romania 642 Stefania koppel
Stefania koppel Tara codrului
Tara codrului Proyecto tara
Proyecto tara Tara bracco
Tara bracco Tara noble
Tara noble Tara sfanta in vremea mantuitorului proiect didactic
Tara sfanta in vremea mantuitorului proiect didactic