Heart Disease in Women Case Studies Tara Dall





- Slides: 88
Heart Disease in Women: Case Studies Tara Dall, MD Diplomate, American Board of Clinical Lipidology Medical Director, President Advanced Lipidology Delafield, WI www. advlip. com
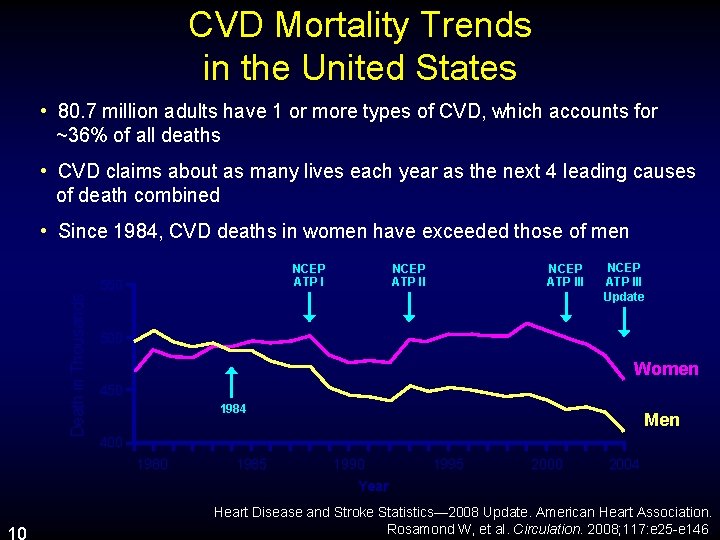
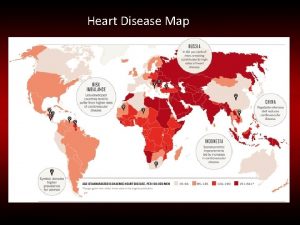
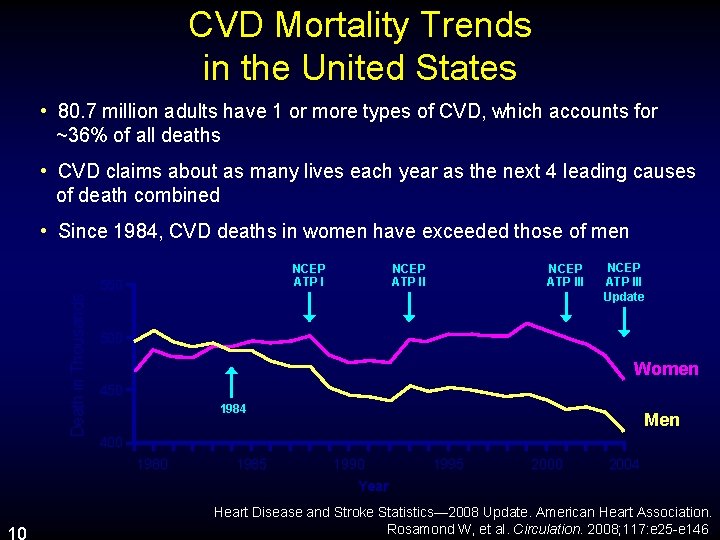
CVD Mortality Trends in the United States • 80. 7 million adults have 1 or more types of CVD, which accounts for ~36% of all deaths • CVD claims about as many lives each year as the next 4 leading causes of death combined • Since 1984, CVD deaths in women have exceeded those of men NCEP ATP I Death in Thousands 550 NCEP ATP III Update 500 Women 450 1984 Men 400 1985 1990 1995 2000 2004 Year 10 Heart Disease and Stroke Statistics— 2008 Update. American Heart Association. Rosamond W, et al. Circulation. 2008; 117: e 25 -e 146.
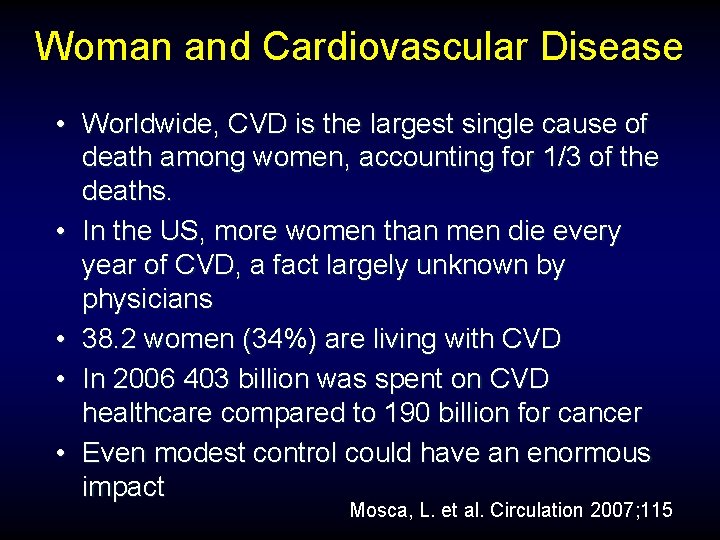
Woman and Cardiovascular Disease • Worldwide, CVD is the largest single cause of death among women, accounting for 1/3 of the deaths. • In the US, more women than men die every year of CVD, a fact largely unknown by physicians • 38. 2 women (34%) are living with CVD • In 2006 403 billion was spent on CVD healthcare compared to 190 billion for cancer • Even modest control could have an enormous impact Mosca, L. et al. Circulation 2007; 115
Risk Factors Cardiovascular Disease in Women • • Family History Age Smoking Diabetes • Hypertension • Obesity • Physical Inactivity • High Cholesterol – High Triglycerides – Low HDL
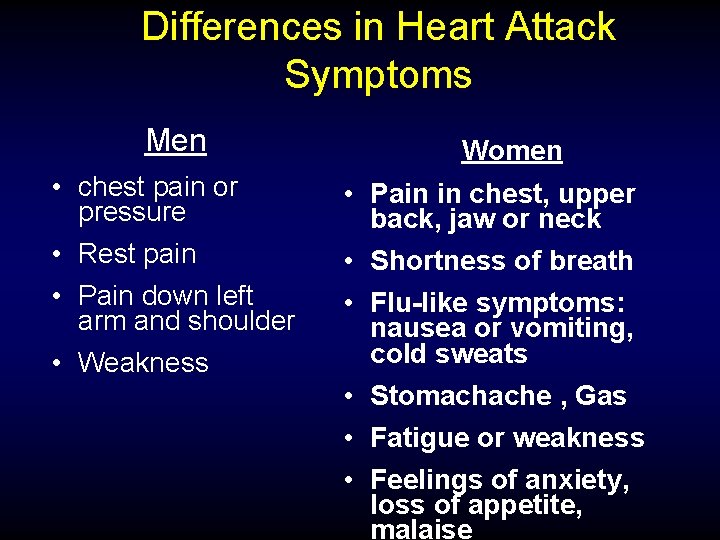
Differences in Heart Attack Symptoms Men • chest pain or pressure • Rest pain • Pain down left arm and shoulder • Weakness Women • Pain in chest, upper back, jaw or neck • Shortness of breath • Flu-like symptoms: nausea or vomiting, cold sweats • Stomachache , Gas • Fatigue or weakness • Feelings of anxiety, loss of appetite, malaise
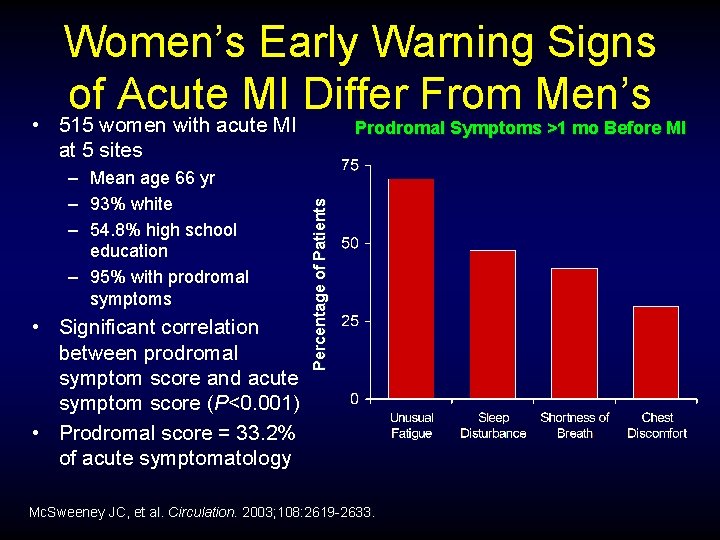
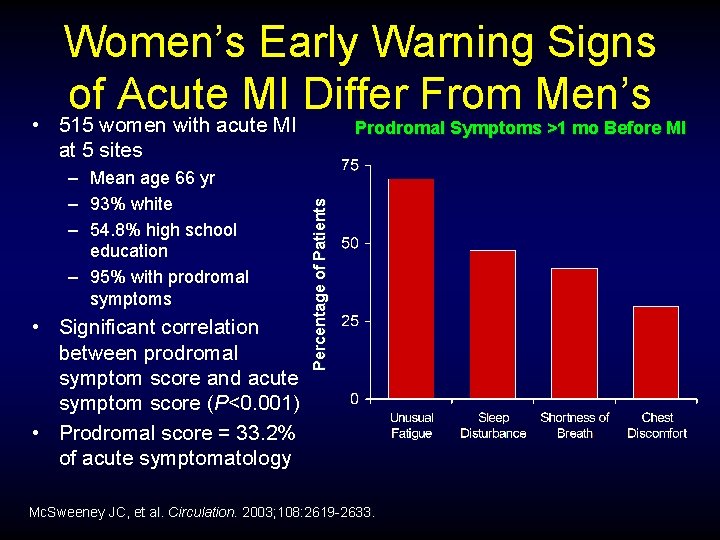
Women’s Early Warning Signs of Acute MI Differ From Men’s • 515 women with acute MI at 5 sites • Significant correlation between prodromal symptom score and acute symptom score (P<0. 001) • Prodromal score = 33. 2% of acute symptomatology Percentage of Patients – Mean age 66 yr – 93% white – 54. 8% high school education – 95% with prodromal symptoms Prodromal Symptoms >1 mo Before MI Mc. Sweeney JC, et al. Circulation. 2003; 108: 2619 -2633.
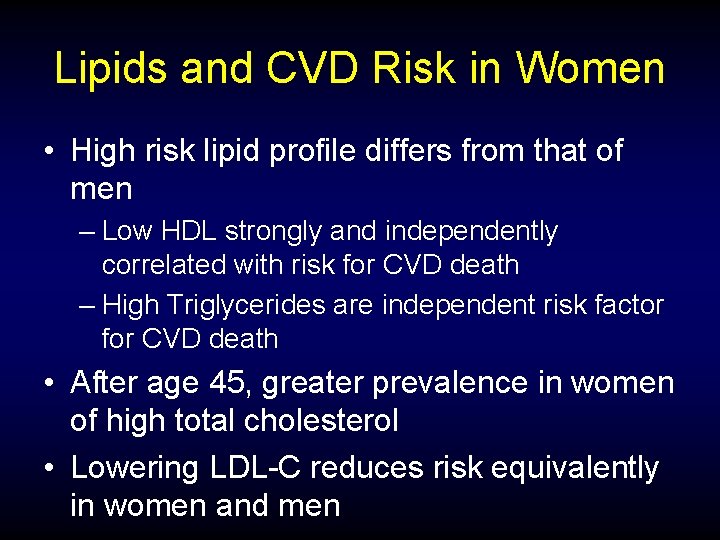
Lipids and CVD Risk in Women • High risk lipid profile differs from that of men – Low HDL strongly and independently correlated with risk for CVD death – High Triglycerides are independent risk factor for CVD death • After age 45, greater prevalence in women of high total cholesterol • Lowering LDL-C reduces risk equivalently in women and men

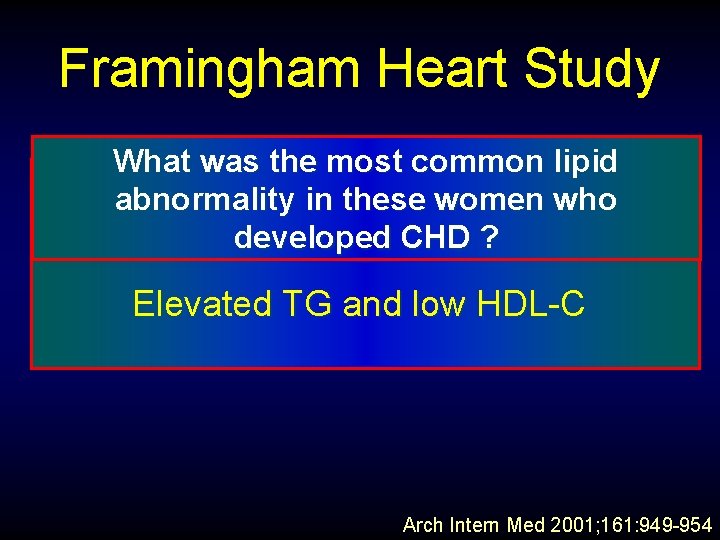
Framingham Heart Study • Among women subjects in Framingham who developed incident CHD during 12 year follow-up: • The MAJORITY (66%) of the women Did not have elevations of TC or LDL-C that would have qualified them for any primary prevention Lipid Trial Arch Intern Med 2001; 161: 949 -954
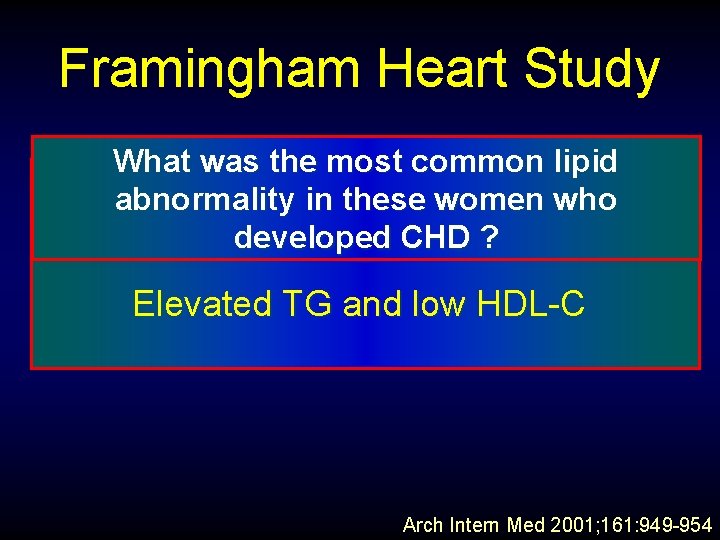
Framingham Heart Study What was the most common lipid Isolated hypertriglyceridemia abnormality in these women who (>200 mg. CHD /dl) ? developed Elevated TG and low HDL-C Arch Intern Med 2001; 161: 949 -954
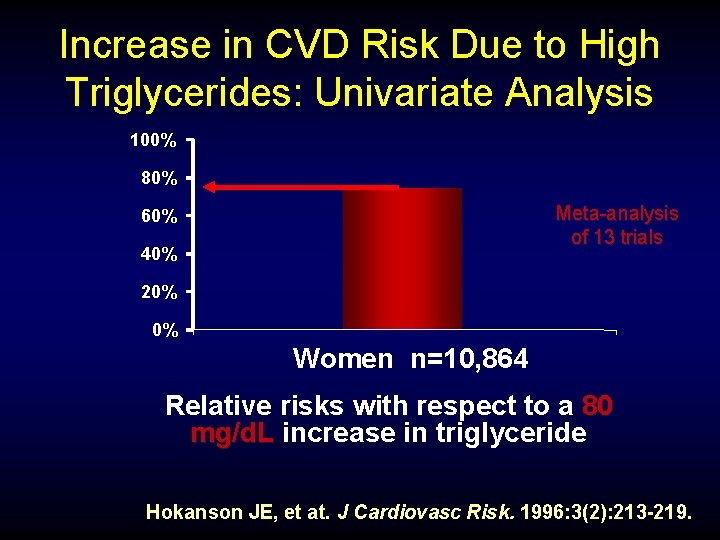
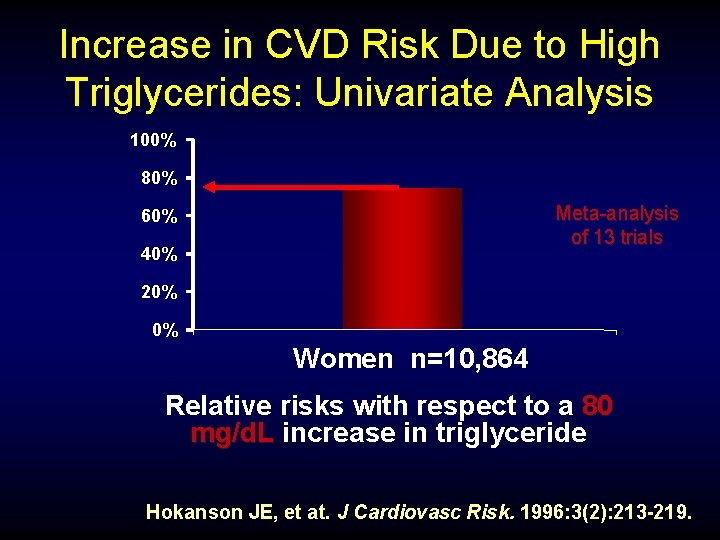
Increase in CVD Risk Due to High Triglycerides: Univariate Analysis 100% 80% Meta-analysis of 13 trials 60% 40% 20% 0% Women n=10, 864 Relative risks with respect to a 80 mg/d. L increase in triglyceride Hokanson JE, et at. J Cardiovasc Risk. 1996: 3(2): 213 -219.
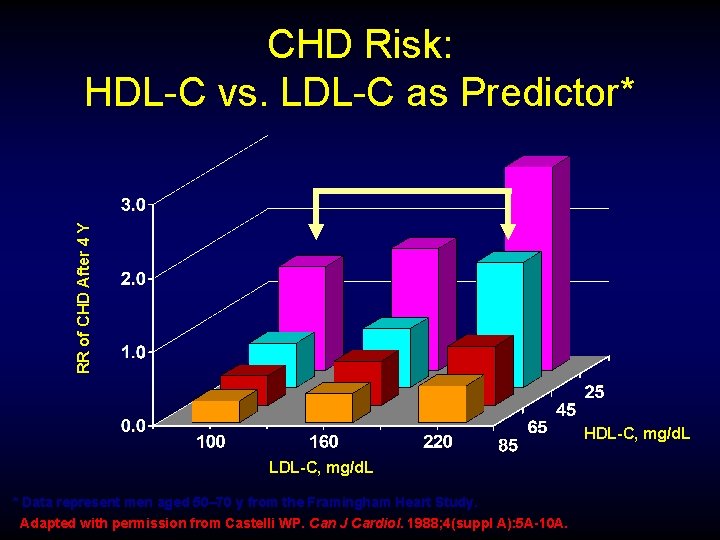
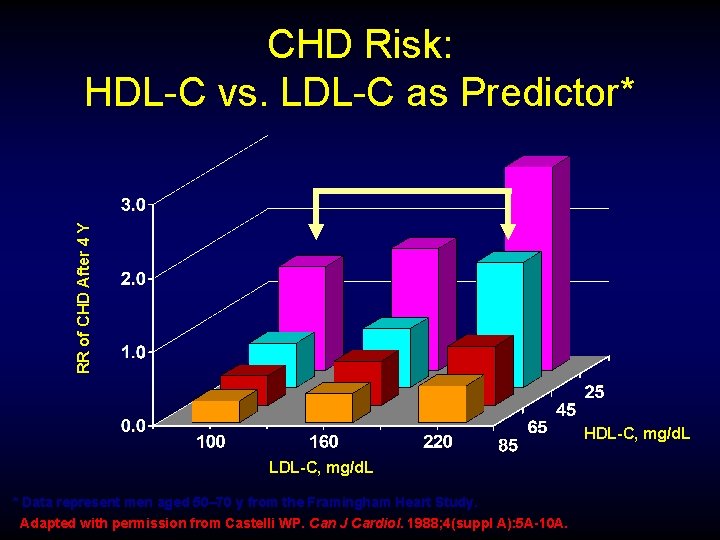
RR of CHD After 4 Y CHD Risk: HDL-C vs. LDL-C as Predictor* HDL-C, mg/d. L LDL-C, mg/d. L * Data represent men aged 50– 70 y from the Framingham Heart Study. Adapted with permission from Castelli WP. Can J Cardiol. 1988; 4(suppl A): 5 A-10 A.
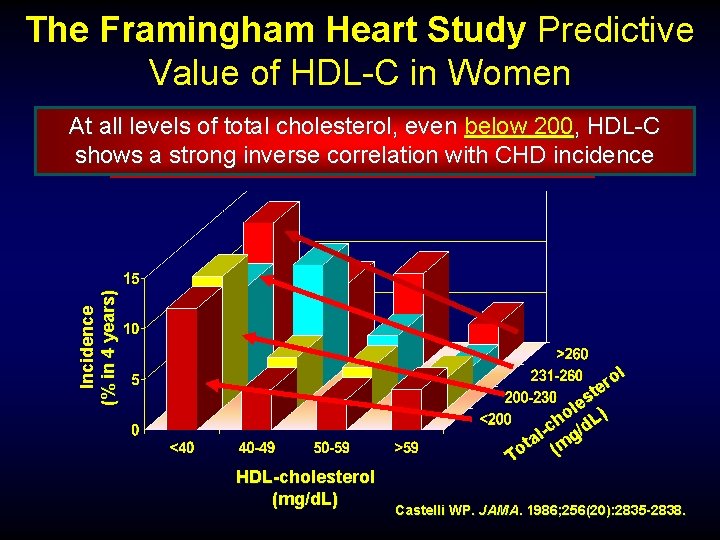
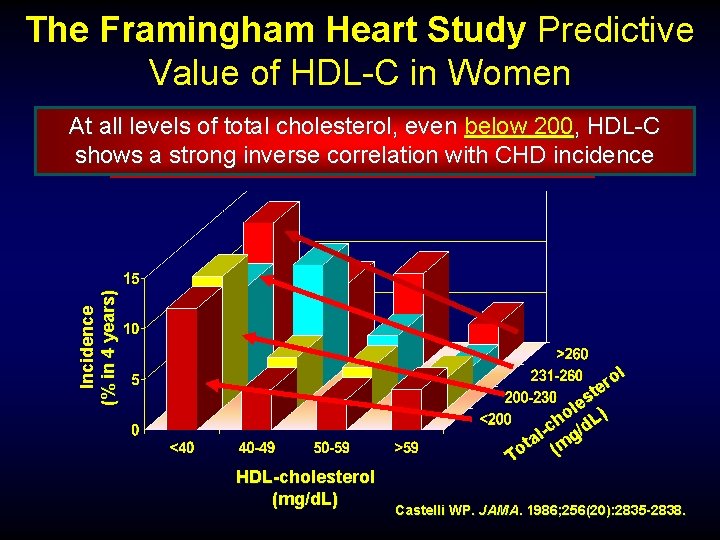
The Framingham Heart Study Predictive Value of HDL-C in Women Incidence (% in 4 years) At all levels total cholesterol, even below<45 200, HDL-C Twiceofas many women with HDL-C andinverse women without history shows a. Men strong correlation with CHD incidence mg/d. L suffered an MI over. CHD 4 years ol r te s le ) o L h -c g/d l ta (m o T HDL-cholesterol (mg/d. L) Castelli WP. JAMA. 1986; 256(20): 2835 -2838.
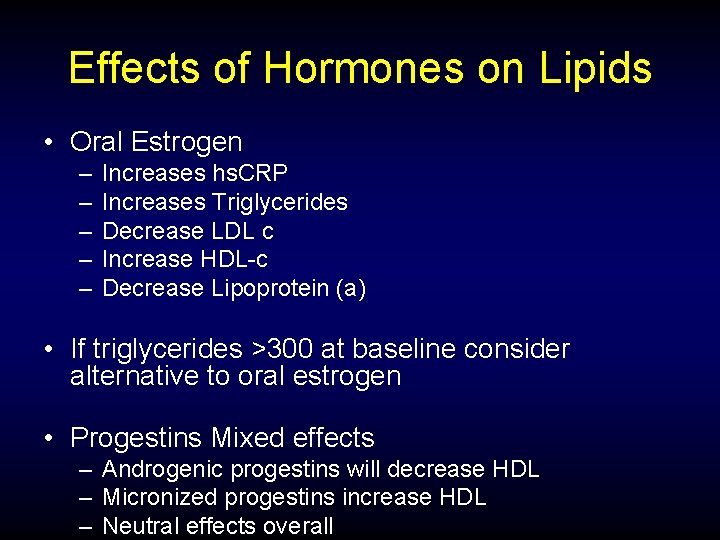
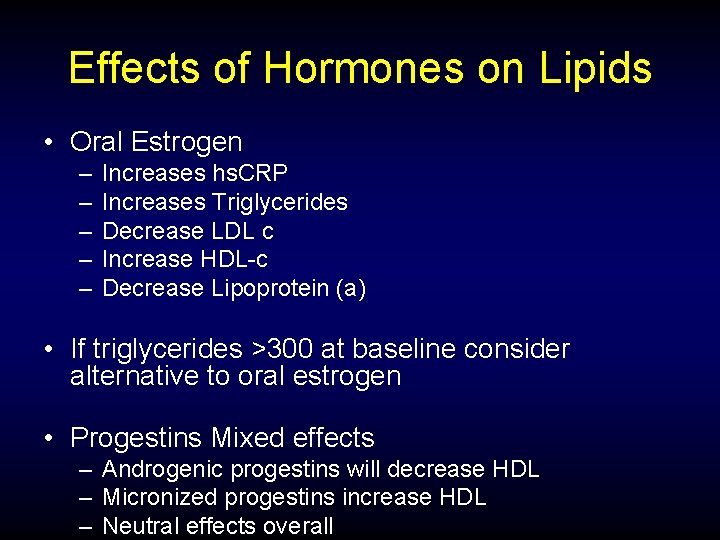
Effects of Hormones on Lipids • Oral Estrogen – – – Increases hs. CRP Increases Triglycerides Decrease LDL c Increase HDL-c Decrease Lipoprotein (a) • If triglycerides >300 at baseline consider alternative to oral estrogen • Progestins Mixed effects – Androgenic progestins will decrease HDL – Micronized progestins increase HDL – Neutral effects overall
Testosterone Primary effect on Lipids LOW HDL
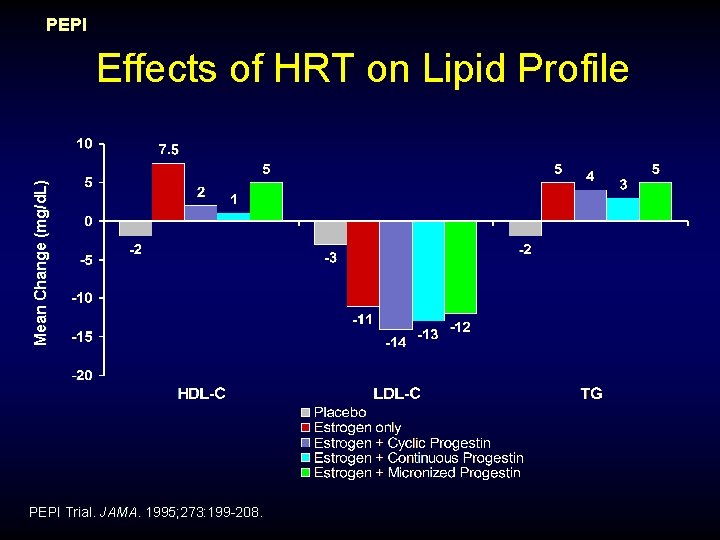
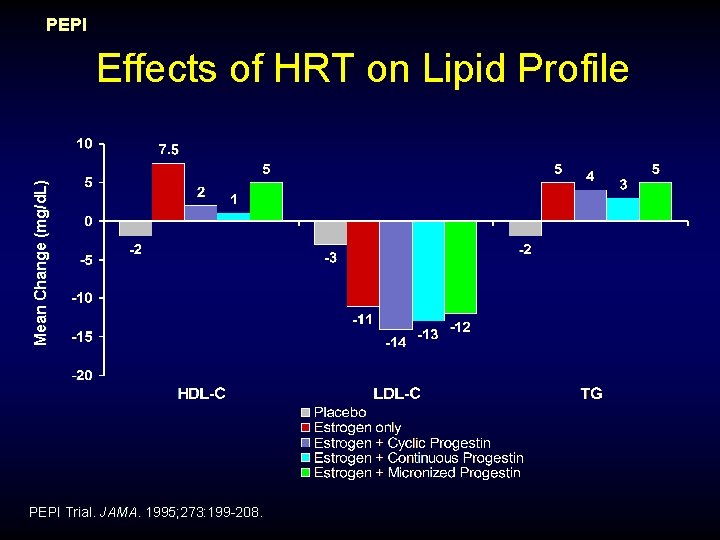
PEPI Mean Change (mg/d. L) Effects of HRT on Lipid Profile PEPI Trial. JAMA. 1995; 273: 199 -208.
Mosca, L. et al. Circulation 2007; 115
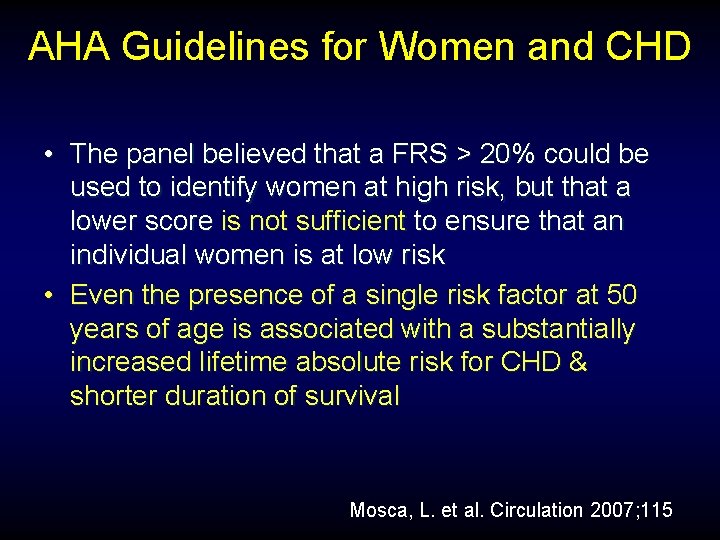
AHA Guidelines for Women and CHD • The panel believed that a FRS > 20% could be used to identify women at high risk, but that a lower score is not sufficient to ensure that an individual women is at low risk • Even the presence of a single risk factor at 50 years of age is associated with a substantially increased lifetime absolute risk for CHD & shorter duration of survival Mosca, L. et al. Circulation 2007; 115
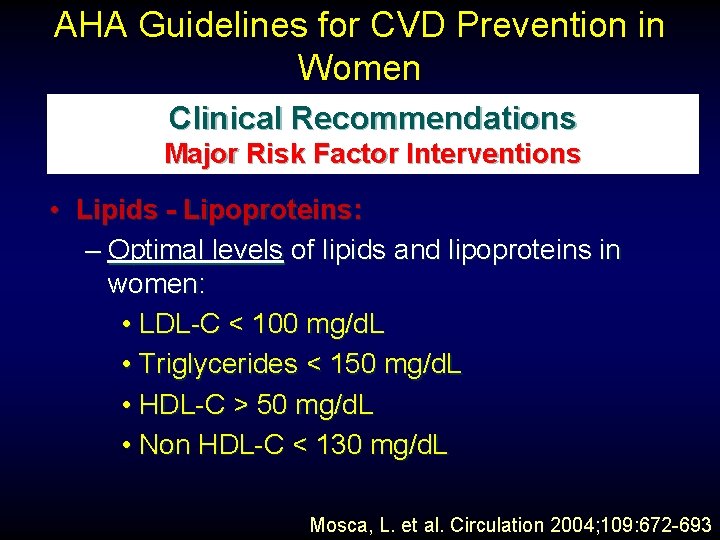
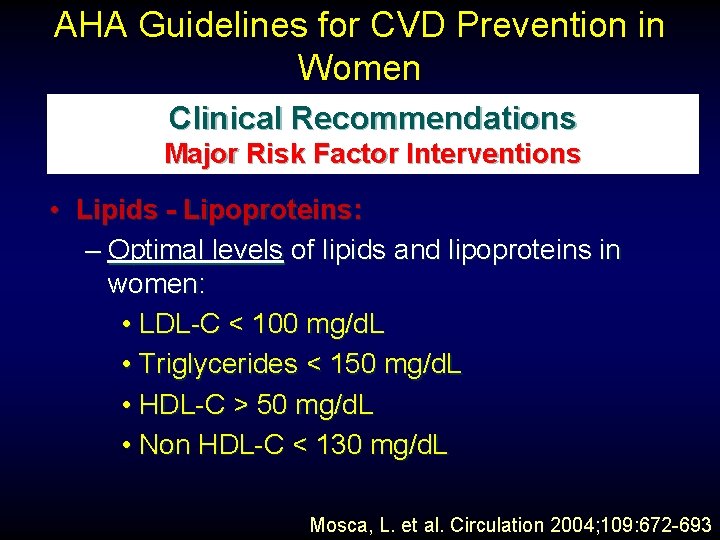
AHA Guidelines for CVD Prevention in Women Clinical Recommendations Major Risk Factor Interventions • Lipids - Lipoproteins: – Optimal levels of lipids and lipoproteins in women: • LDL-C < 100 mg/d. L • Triglycerides < 150 mg/d. L • HDL-C > 50 mg/d. L • Non HDL-C < 130 mg/d. L Mosca, L. et al. Circulation 2004; 109: 672 -693
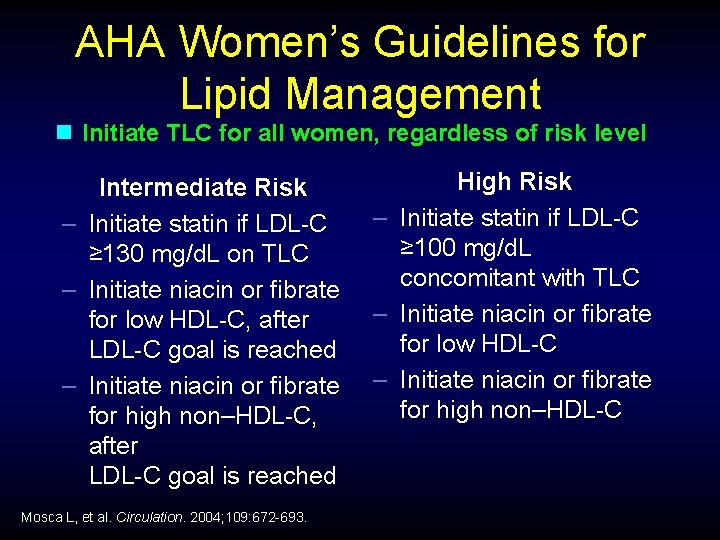
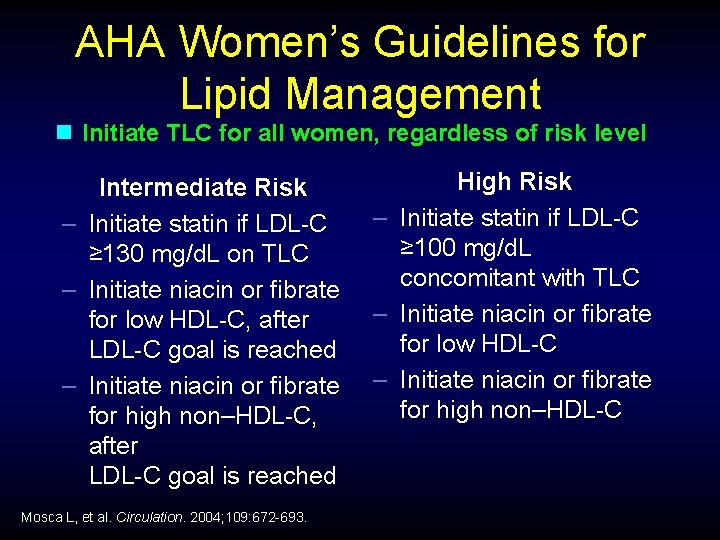
AHA Women’s Guidelines for Lipid Management n Initiate TLC for all women, regardless of risk level Intermediate Risk – Initiate statin if LDL-C ≥ 130 mg/d. L on TLC – Initiate niacin or fibrate for low HDL-C, after LDL-C goal is reached – Initiate niacin or fibrate for high non–HDL-C, after LDL-C goal is reached Mosca L, et al. Circulation. 2004; 109: 672 -693. High Risk – Initiate statin if LDL-C ≥ 100 mg/d. L concomitant with TLC – Initiate niacin or fibrate for low HDL-C – Initiate niacin or fibrate for high non–HDL-C
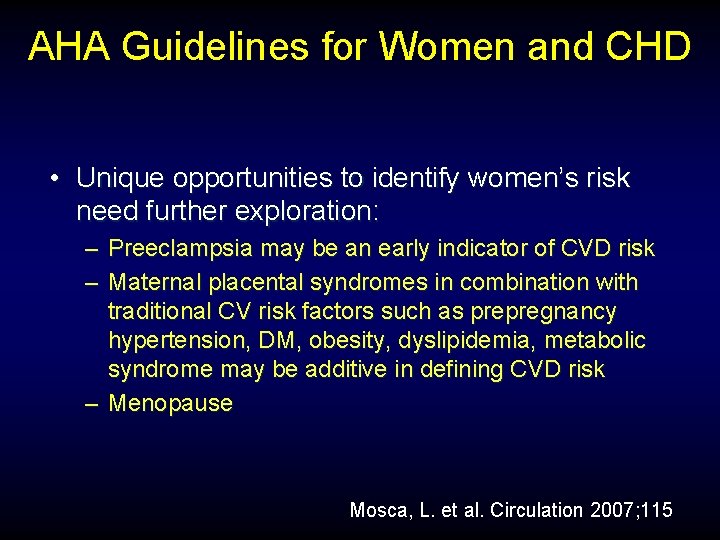
AHA Guidelines for Women and CHD • Unique opportunities to identify women’s risk need further exploration: – Preeclampsia may be an early indicator of CVD risk – Maternal placental syndromes in combination with traditional CV risk factors such as prepregnancy hypertension, DM, obesity, dyslipidemia, metabolic syndrome may be additive in defining CVD risk – Menopause Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Optimal Risk – Framingham global risk < 10% and a healthy lifestyle with NO risk factors Mosca, L. et al. Circulation 2007; 115
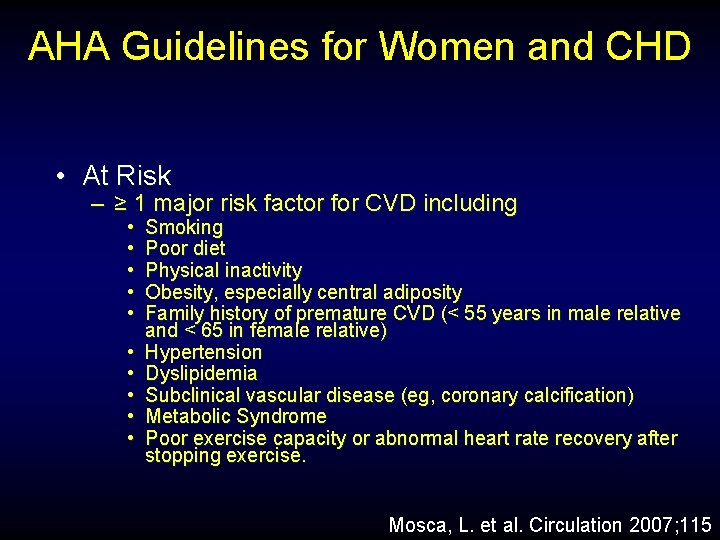
AHA Guidelines for Women and CHD • At Risk – ≥ 1 major risk factor for CVD including • • • Smoking Poor diet Physical inactivity Obesity, especially central adiposity Family history of premature CVD (< 55 years in male relative and < 65 in female relative) Hypertension Dyslipidemia Subclinical vascular disease (eg, coronary calcification) Metabolic Syndrome Poor exercise capacity or abnormal heart rate recovery after stopping exercise. Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • At High Risk – Established CHD – Cerebrovascular disease – Peripheral arterial disease – Abdominal aortic aneurysm – End-stage or chronic renal disease – Diabetes mellitus – 10 year Framingham global risk > 20% Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Cigarette Smoking (Class I, Level B) – Women should not smoke and should avoid environmental tobacco smoke – Provide counseling, nicotine replacement, and other pharmacotherapy as indicated with a behavioral program or formal smoking cessation program Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Weight Maintenance/reduction (Class I, Level B) – Women should maintain or lose weight through an appropriate balance of physical activity, caloric intake, and formal behavior programs when indicated to maintain/achieve a BMI between 18. 5 and 24. 9 kg/m 2 and a waist circumference ≤ 35 in Mosca, L. et al. Circulation 2004; 109: 672 -693
AHA Guidelines for Women and CHD • Physical Activity (Class I, Level B) – Women should accumulate a minimum of 30 minutes of moderate-intensity physical activity (brisk walking) on most and preferably all, days of the week Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Heart Healthy Diet (Class I, Level B) – Women should consume a diet rich in fruits and vegetables – Choose whole-grain, high fiber foods – Consume fish, especially oily fish at least twice a week – Limit intake of saturated fat to < 10% of energy, if possible to < 7% – Limit cholesterol to < 300 mg daily Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Heart Healthy Diet (Class I, Level B) – Limit alcohol intake to no more than 1 drink per day (12 oz bottle of beer, 5 oz glass of wine or a 1. 5 oz shot of 80 -proof spirit – Limit sodium intake to < 2. 3 grams/day (approximately 1 tsp salt) – Consumption of trans-fatty acids should be as low as possible (eg, < 1% of energy) Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Omega-3 Fatty Acids (Class IIb, Level B) – As an adjunct to diet, omega-3 FA in capsule form (approximately 850 -1000 mg of EPA and DHA) may be considered in women with CHD and higher doses (2 -4 grams) may be used for treatment of women with high Triglyceride levels. Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Depression (Class IIa, Level B) – Consider screening women with CHD for depression and refer/treat when indicated Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Blood Pressure: Lifestyle (Class I, Level B) – Encourage a BP of < 120/80 through lifestyle approaches such as weight control, increased physical activity, alcohol moderation, sodium restriction, and increased consumption of fresh fruits, vegetables, and low fat dairy products Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Blood Pressure: Pharmacotherapy (Class I, Level A) – Initial treatment of high-risk women should be with beta-blockers and/or ACE inhibitors/ARBs with addition of other drugs as needed to achieve goal BP Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Lipids: Lifestyle (Class I, Level B) – In high risk women when lipids are abnormal, saturated fat intake should be limited to < 7% of calories, cholesterol to < 200 mg/day Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Lipids: Pharmacotherapy for LDL Lowering, High Risk Women (Class I) – Utilize LDL-C lowering therapy simultaneously with lifestyle to achieve an LDL-C < 100 mg/dl (level A) – And similarly in women with other atherosclerotic CVD or diabetes or 10 -year absolute risk > 20% (level B) Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Lipids: Pharmacotherapy for LDL C Lowering, Very High Risk Women (Class IIa Level B) – Established CVD plus multiple major risk factors, severe and poorly controlled risk factors, or DM – A reduction to < 70 mg/d. L is reasonable – May require and LDL-combination drug regimen Mosca, L. et al. Circulation 2007; 115
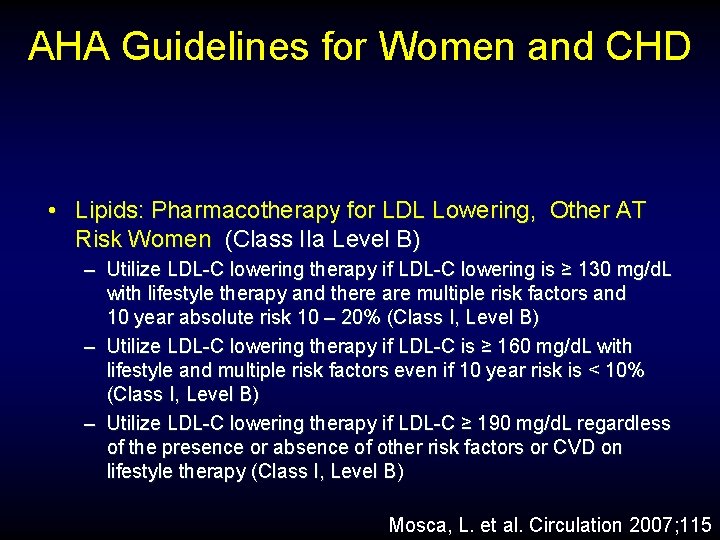
AHA Guidelines for Women and CHD • Lipids: Pharmacotherapy for LDL Lowering, Other AT Risk Women (Class IIa Level B) – Utilize LDL-C lowering therapy if LDL-C lowering is ≥ 130 mg/d. L with lifestyle therapy and there are multiple risk factors and 10 year absolute risk 10 – 20% (Class I, Level B) – Utilize LDL-C lowering therapy if LDL-C is ≥ 160 mg/d. L with lifestyle and multiple risk factors even if 10 year risk is < 10% (Class I, Level B) – Utilize LDL-C lowering therapy if LDL-C ≥ 190 mg/d. L regardless of the presence or absence of other risk factors or CVD on lifestyle therapy (Class I, Level B) Mosca, L. et al. Circulation 2007; 115
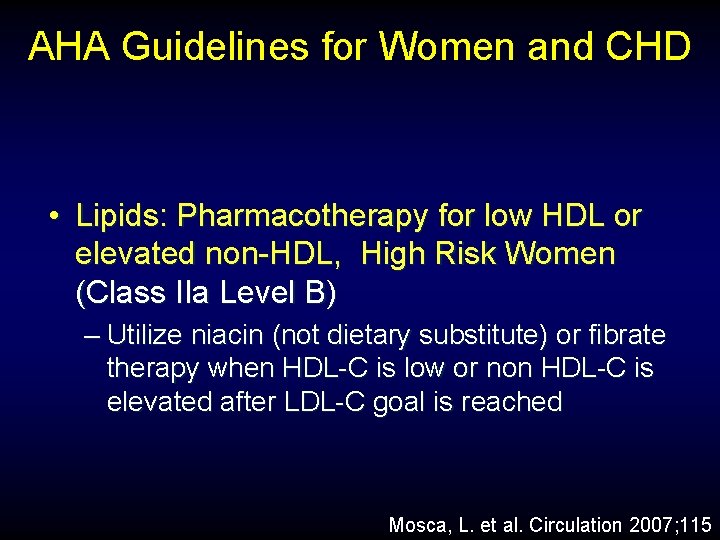
AHA Guidelines for Women and CHD • Lipids: Pharmacotherapy for low HDL or elevated non-HDL, High Risk Women (Class IIa Level B) – Utilize niacin (not dietary substitute) or fibrate therapy when HDL-C is low or non HDL-C is elevated after LDL-C goal is reached Mosca, L. et al. Circulation 2007; 115
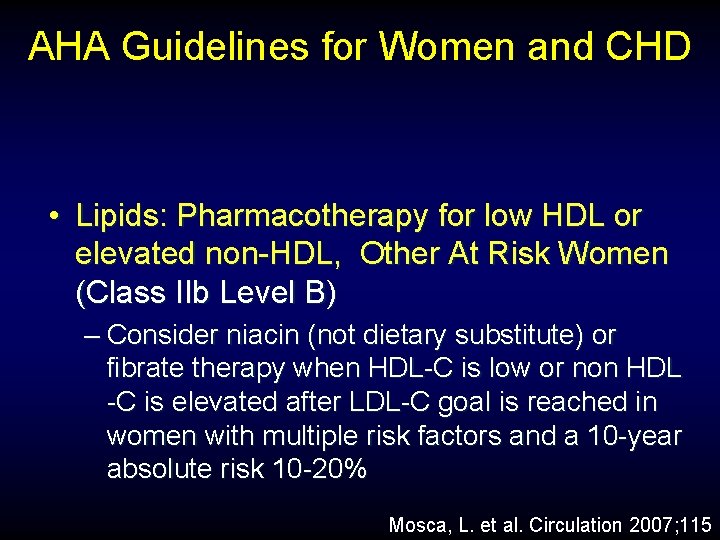
AHA Guidelines for Women and CHD • Lipids: Pharmacotherapy for low HDL or elevated non-HDL, Other At Risk Women (Class IIb Level B) – Consider niacin (not dietary substitute) or fibrate therapy when HDL-C is low or non HDL -C is elevated after LDL-C goal is reached in women with multiple risk factors and a 10 -year absolute risk 10 -20% Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Diabetes (Class I, Level C) – Lifestyle and pharmacotherapy should be used as indicated to achieve an Hgb. A 1 C (<7%) if this can be accomplished without significant hypoglycemia Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Aspirin – High Risk (Class I, Level A) – ASA therapy (75– 325 mg) should be used unless contraindicated – If a high-risk woman is intolerant of ASA, clopidogrel should be substituted Mosca, L. et al. Circulation 2004; 109: 672 -693
AHA Guidelines for Women and CHD • Aspirin – Other At Risk – In women ≥ 65, consider ASA (81 mg daily or 100 mg QOD) if BP is controlled and benefit for ischemic stroke and MI prevention is likely to outweigh risk of GI bleeding and hemorrhagic stroke (Class IIa, Level B) – In women < 65 when benefit for ischemic stroke prevention is likely to outweigh adverse effects of therapy (Class IIb, Level B) Mosca, L. et al. Circulation 2004; 109: 672 -693
AHA Guidelines for Women and CHD • Aldosterone Blockade (Class I, Level B) – Use aldosterone blockade after MI in women who do not have significant renal dysfunction or hyperkalemia who are already receiving therapeutic doses of an ACEI and beta-blocker, and have LVEF ≤ 40% with symptomatic heart failure Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Beta-blockers (Class I, Level A) – Should be used indefinitely in all high risk women who have had an MI, acute coronary symptoms or LV dysfunction unless contraindicated • ACE Inhibitors/ARBS (Class I, Level A) – ACEI should be used in high risk women unless contraindicated in women after MI and in those with heart failure or LVEF < 40% or with DM. Use ARBS if intolerant to ACEI Mosca, L. et al. Circulation 2007; 115
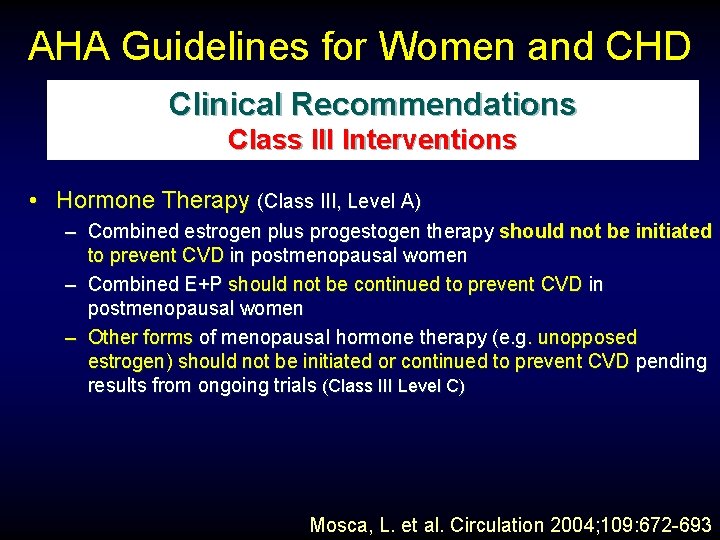
AHA Guidelines for Women and CHD • Not Useful/Effective and May Be Harmful) for CVD or MI prevention (Class III, Level A) – Menopausal Therapy: Hormonal therapy and SERMs should not be used form the primary or secondary prevention of CVD – Antioxidant supplements: (eg, vitamin E, C and beta carotene) should not be used for the primary or secondary prevention of CVD Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Not Useful/Effective and May Be Harmful) for CVD or MI prevention (Class III, Level B) – Routine use of aspirin in healthy women < 65 is not recommended to prevent MI Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD • Not Useful/Effective and May Be Harmful) for CVD or MI prevention (Class III, Level A) – Folic Acid with or without B 6 and B 12 supplementation should not be used for them primary or secondary prevention of CVD – Folic acid supplementation should be used in the childbearing years to prevent neural tube defects Mosca, L. et al. Circulation 2007; 115
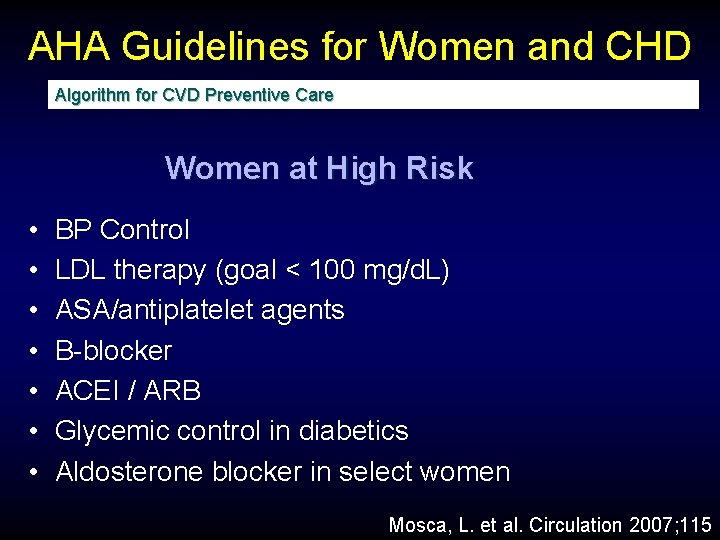
AHA Guidelines for Women and CHD Algorithm for CVD Preventive Care Women at High Risk • • BP Control LDL therapy (goal < 100 mg/d. L) ASA/antiplatelet agents Β-blocker ACEI / ARB Glycemic control in diabetics Aldosterone blocker in select women Mosca, L. et al. Circulation 2007; 115
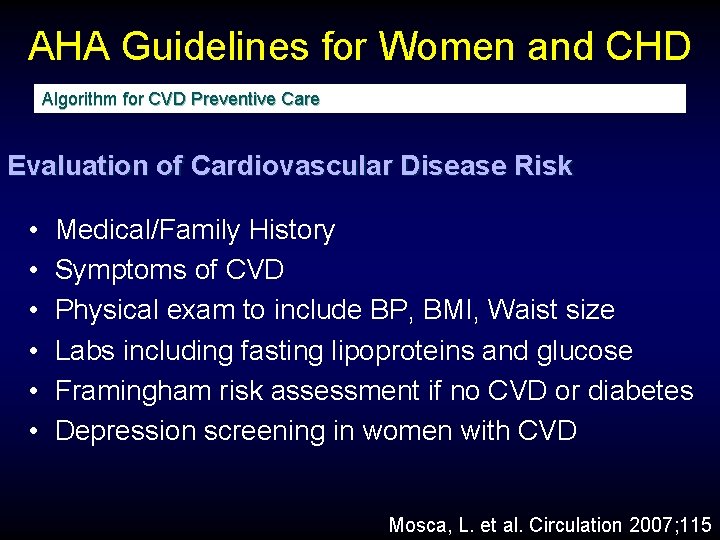
AHA Guidelines for Women and CHD Algorithm for CVD Preventive Care Evaluation of Cardiovascular Disease Risk • • • Medical/Family History Symptoms of CVD Physical exam to include BP, BMI, Waist size Labs including fasting lipoproteins and glucose Framingham risk assessment if no CVD or diabetes Depression screening in women with CVD Mosca, L. et al. Circulation 2007; 115
AHA Guidelines for Women and CHD Algorithm for CVD Preventive Care Implement Class I Lifestyle Recommendations • • Smoking cessation Heart-healthy eating program Regular physical activity Weight management Mosca, L. et al. Circulation 2007; 115

TLC Therapeutic Lifestyle Changes
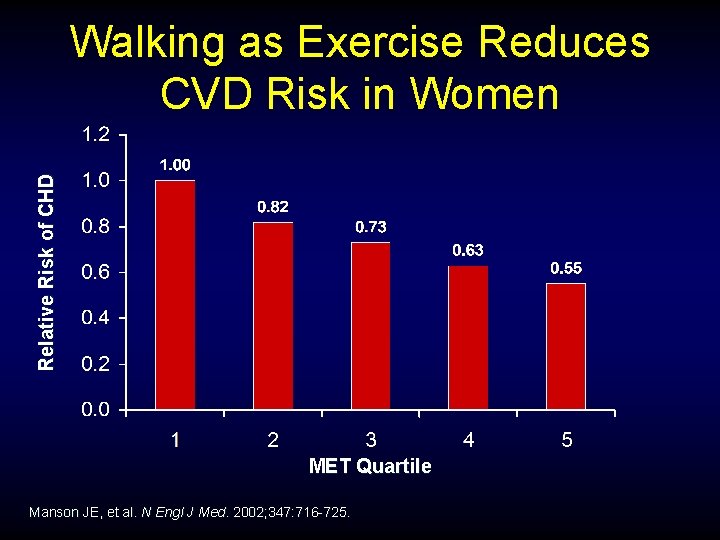
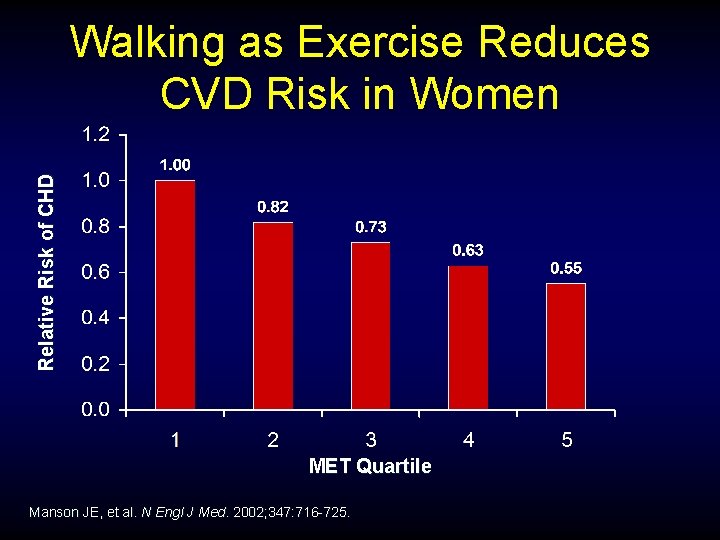
Relative Risk of CHD Walking as Exercise Reduces CVD Risk in Women MET Quartile Manson JE, et al. N Engl J Med. 2002; 347: 716 -725.
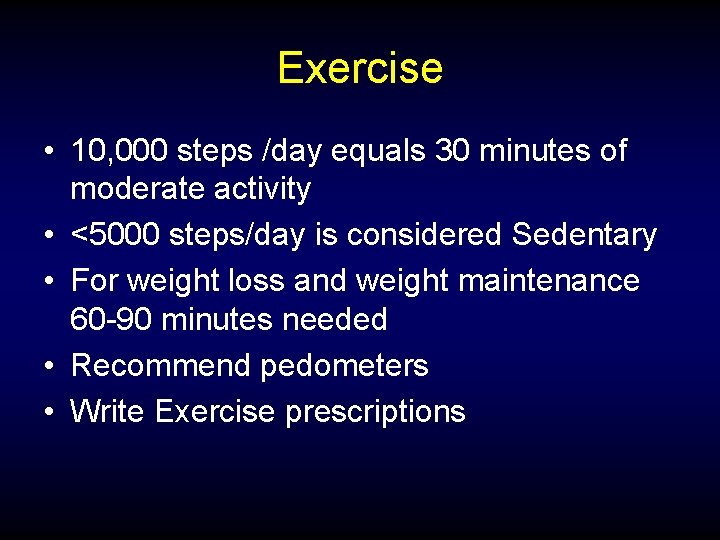
Exercise • 10, 000 steps /day equals 30 minutes of moderate activity • <5000 steps/day is considered Sedentary • For weight loss and weight maintenance 60 -90 minutes needed • Recommend pedometers • Write Exercise prescriptions
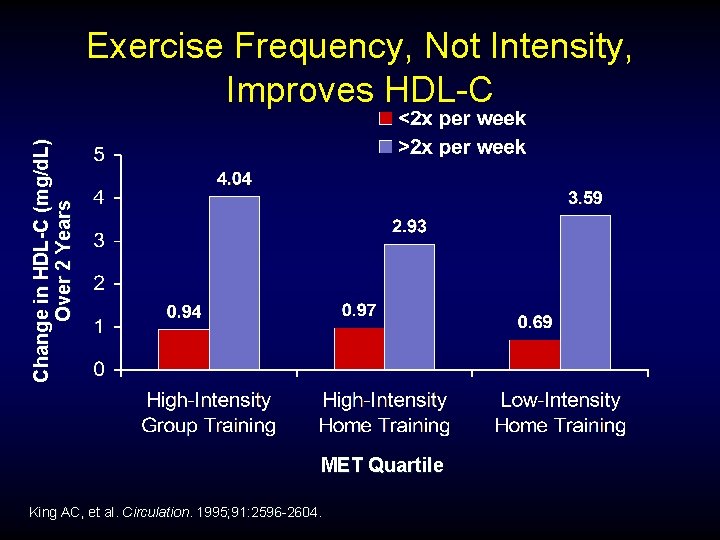
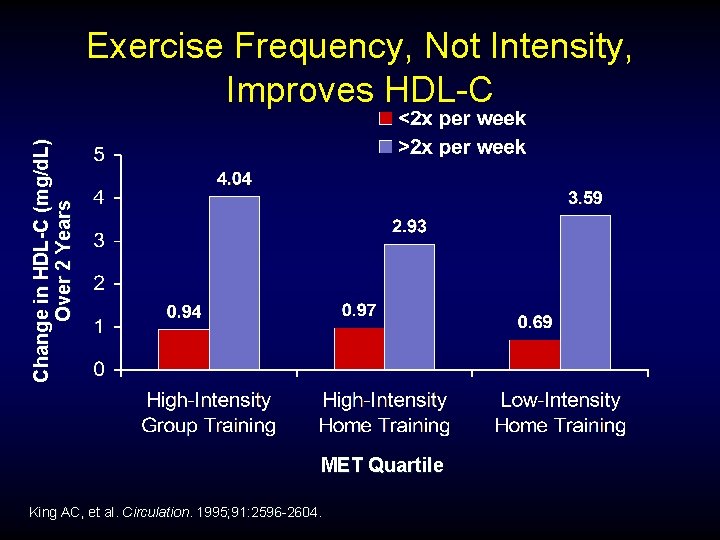
Change in HDL-C (mg/d. L) Over 2 Years Exercise Frequency, Not Intensity, Improves HDL-C MET Quartile King AC, et al. Circulation. 1995; 91: 2596 -2604.
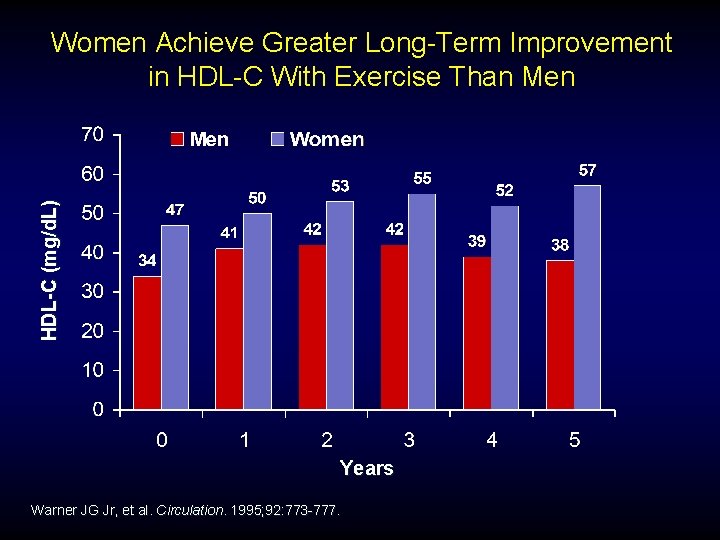
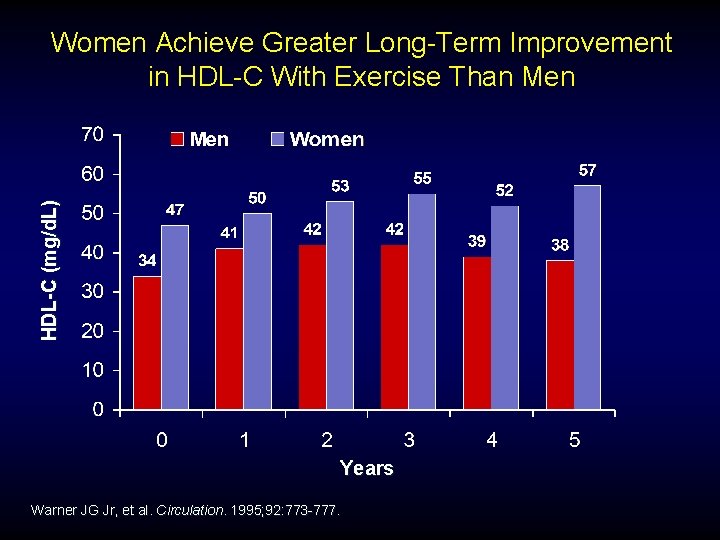
HDL-C (mg/d. L) Women Achieve Greater Long-Term Improvement in HDL-C With Exercise Than Men Years Warner JG Jr, et al. Circulation. 1995; 92: 773 -777.
Case #1 High HDL Protective? Not always?
C. H. 43 yr old WF • Lipid panel : – Total chol 251 – LDL 130 – HDL 88 – Trig 166 – Tchol/HDL 2. 9 – Non HDL 163
Pro. Inflammatory HDL-C New concept especially in setting of insulin resistance
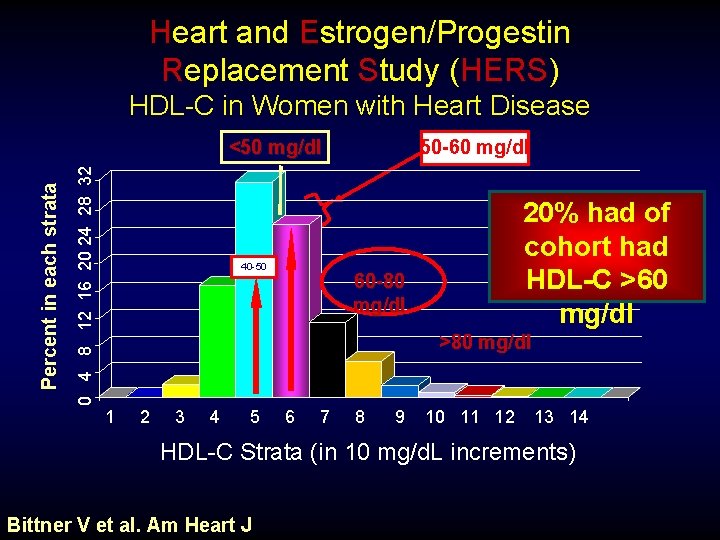
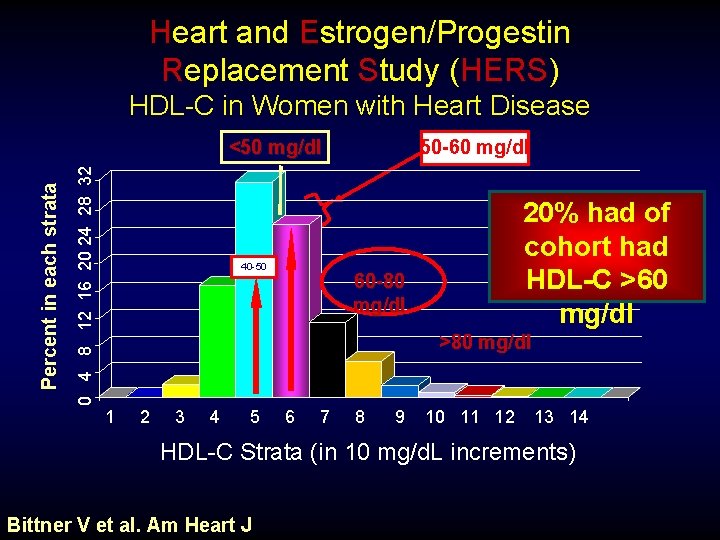
Heart and Estrogen/Progestin Replacement Study (HERS) HDL-C in Women with Heart Disease 50 -60 mg/dl 0 4 8 12 16 20 24 28 32 Percent in each strata <50 mg/dl 40 -50 20% had of cohort had HDL-C >60 mg/dl 60 -80 mg/dl >80 mg/dl 1 2 3 4 5 6 7 8 9 10 11 12 13 14 HDL-C Strata (in 10 mg/d. L increments) Bittner V et al. Am Heart J
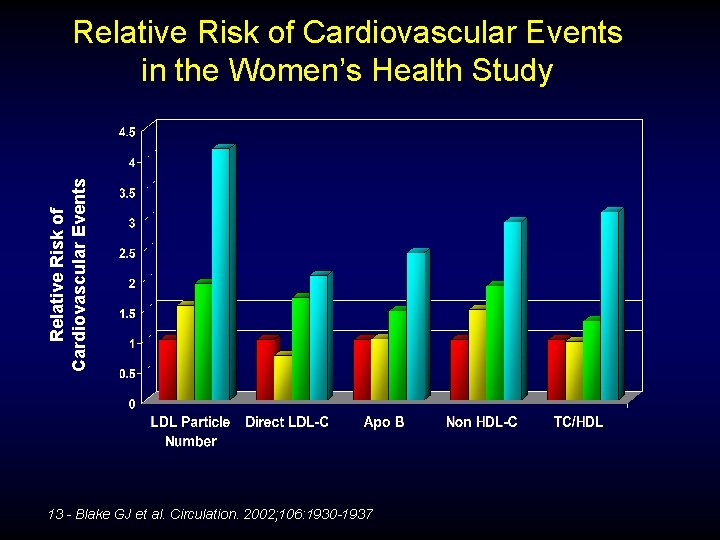
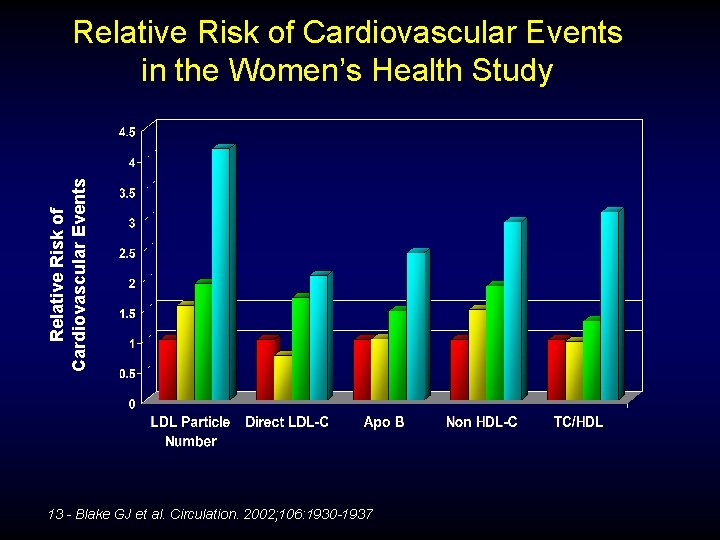
Relative Risk of Cardiovascular Events in the Women’s Health Study 13 - Blake GJ et al. Circulation. 2002; 106: 1930 -1937
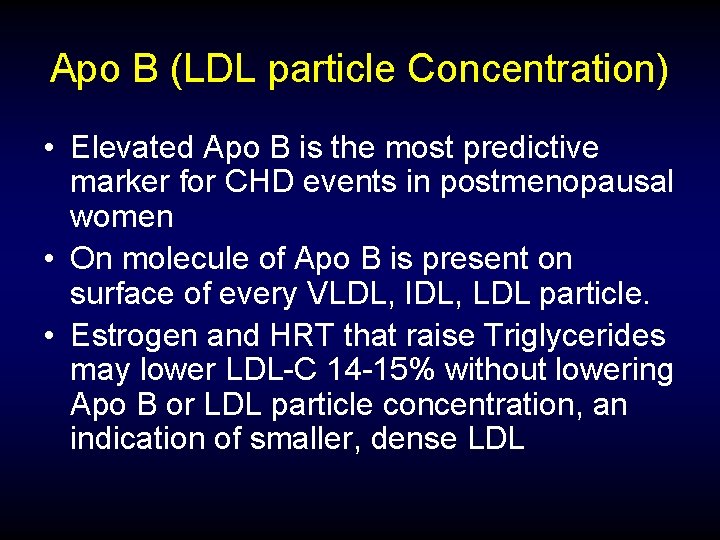
Apo B (LDL particle Concentration) • Elevated Apo B is the most predictive marker for CHD events in postmenopausal women • On molecule of Apo B is present on surface of every VLDL, IDL, LDL particle. • Estrogen and HRT that raise Triglycerides may lower LDL-C 14 -15% without lowering Apo B or LDL particle concentration, an indication of smaller, dense LDL
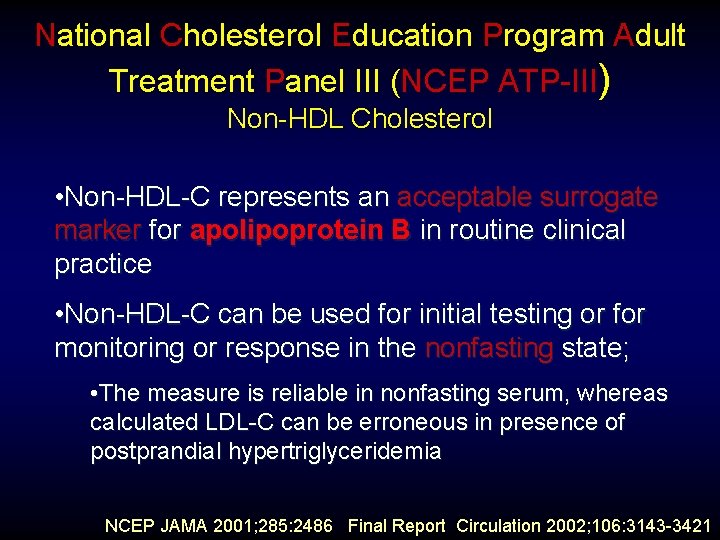
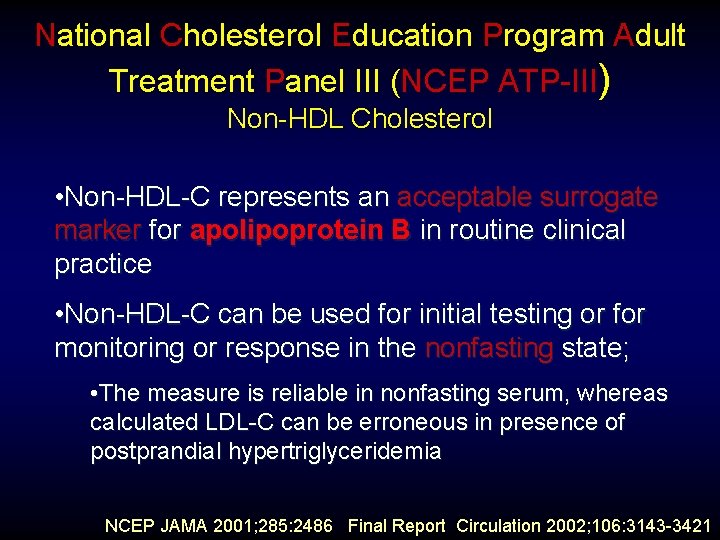
National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP-III) Non-HDL Cholesterol • Non-HDL-C represents an acceptable surrogate marker for apolipoprotein B in routine clinical practice • Non-HDL-C can be used for initial testing or for monitoring or response in the nonfasting state; • The measure is reliable in nonfasting serum, whereas calculated LDL-C can be erroneous in presence of postprandial hypertriglyceridemia NCEP JAMA 2001; 285: 2486 Final Report Circulation 2002; 106: 3143 -3421
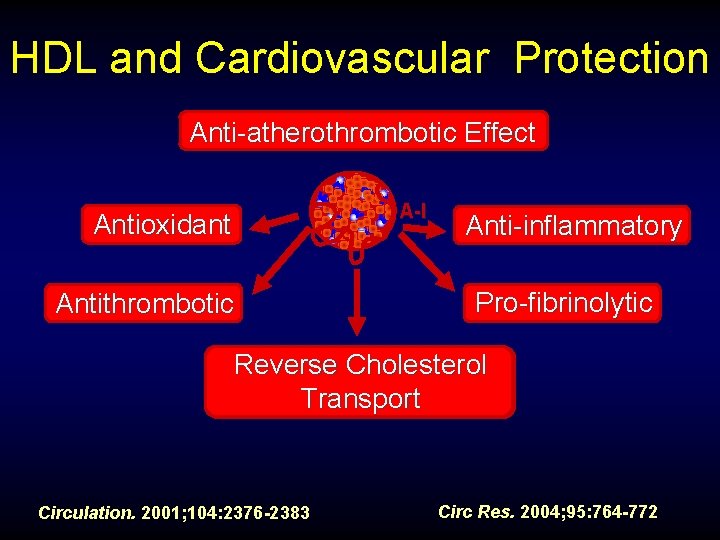
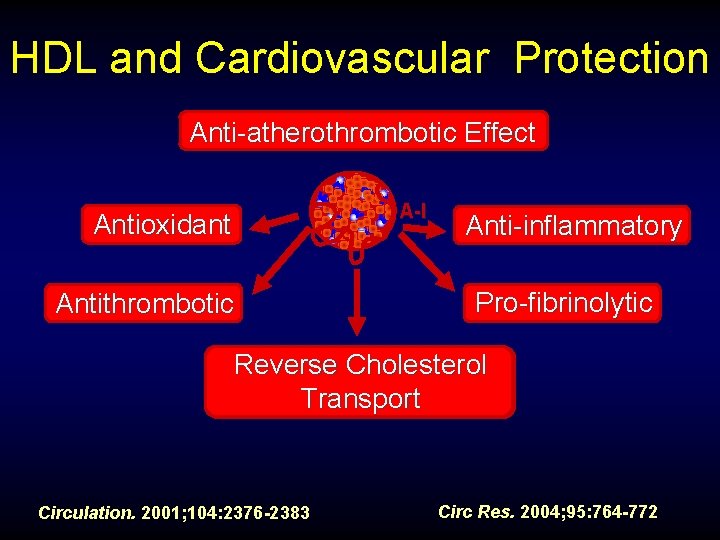
HDL and Cardiovascular Protection Anti-atherothrombotic Effect Antioxidant Antithrombotic A-I Anti-inflammatory Pro-fibrinolytic Reverse Cholesterol Enhanced Peripheral Transport Cholesterol Transport Circulation. 2001; 104: 2376 -2383 Circ Res. 2004; 95: 764 -772
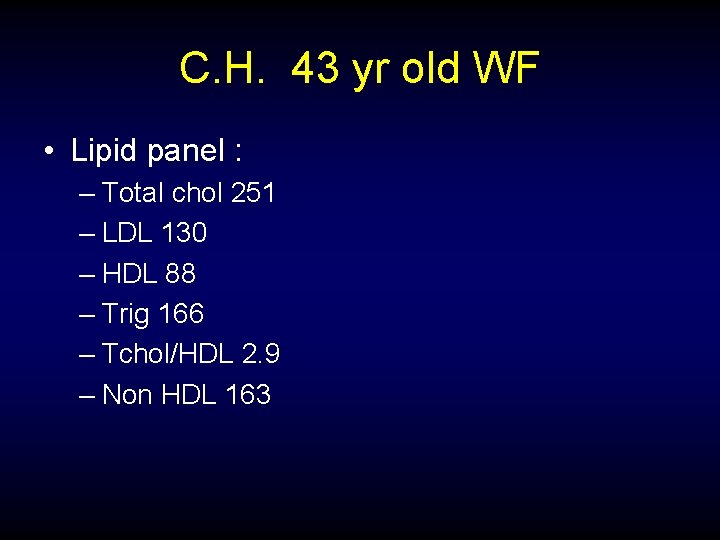
C. H. 43 yr old WF • Lipid panel : – Total chol 251 – LDL 130 – HDL 88 – Trig 166 – Tchol/HDL 2. 9 – Non HDL 163

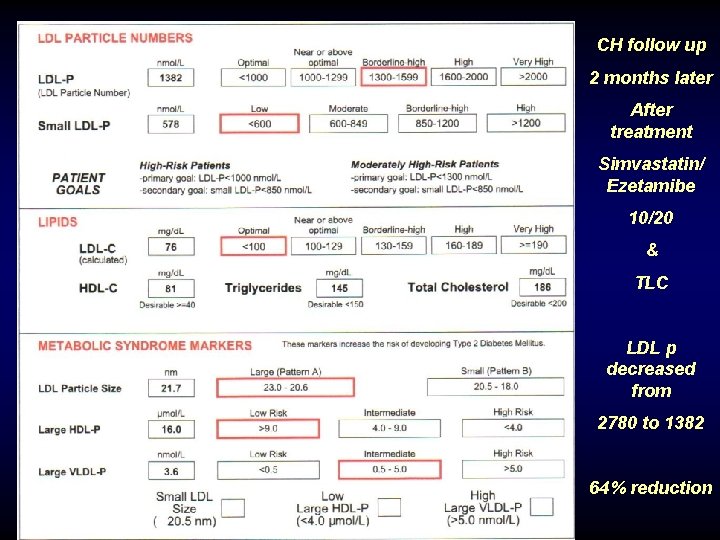
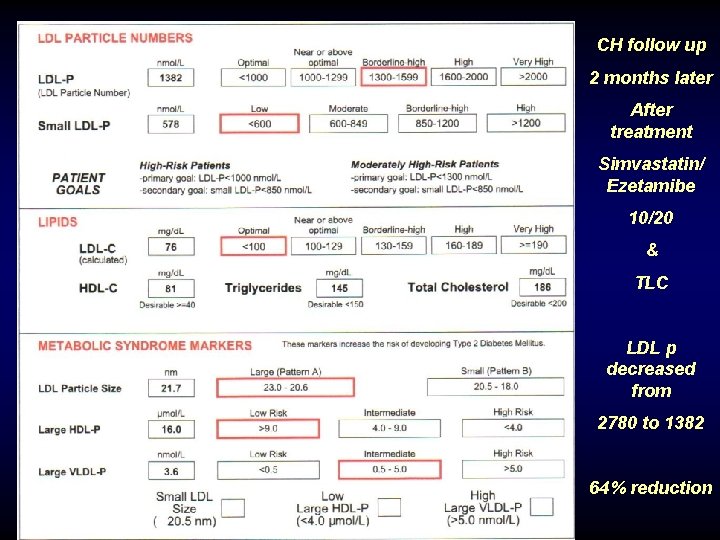
CH follow up 2 months later After treatment Simvastatin/ Ezetamibe 10/20 & TLC LDL p decreased from 2780 to 1382 64% reduction
Case #2 53 yr old WF High HDL, high hs. CRP on Premarin
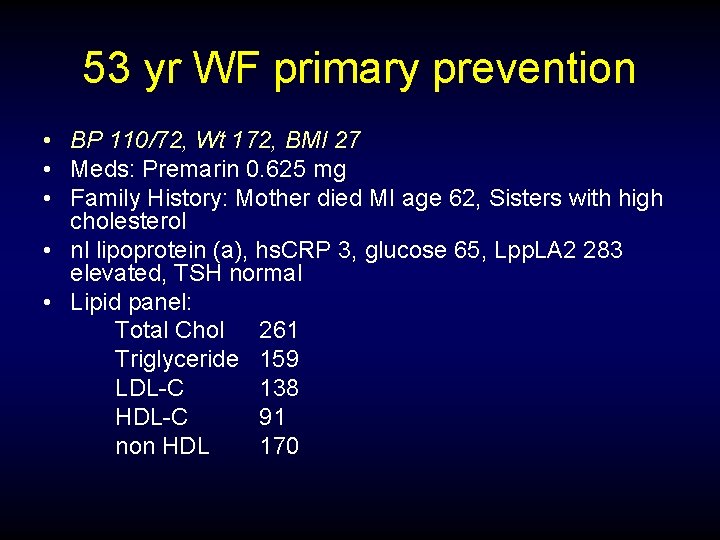
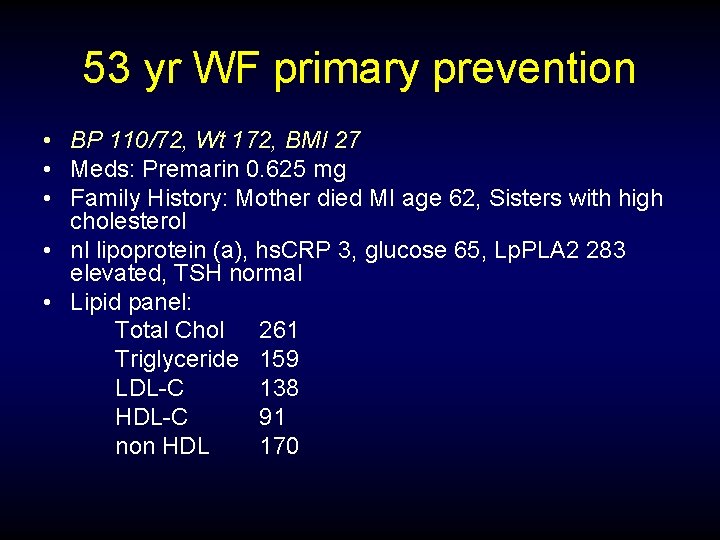
53 yr WF primary prevention • BP 110/72, Wt 172, BMI 27 • Meds: Premarin 0. 625 mg • Family History: Mother died MI age 62, Sisters with high cholesterol • nl lipoprotein (a), hs. CRP 3, glucose 65, Lpp. LA 2 283 elevated, TSH normal • Lipid panel: Total Chol 261 Triglyceride 159 LDL-C 138 HDL-C 91 non HDL 170
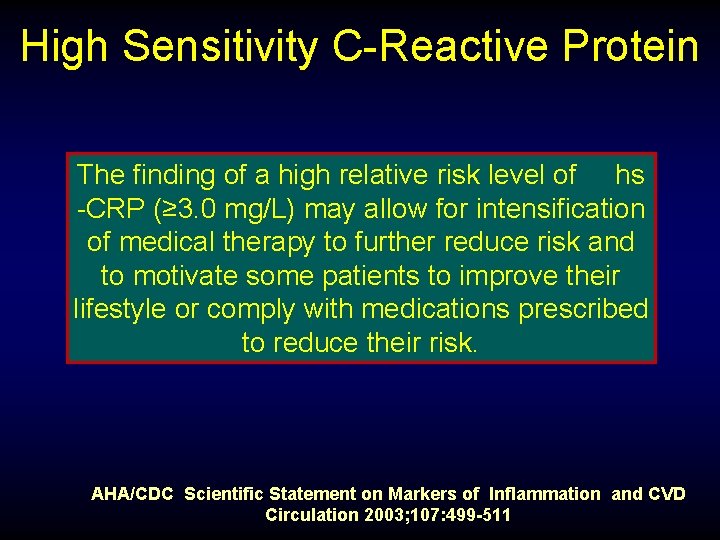
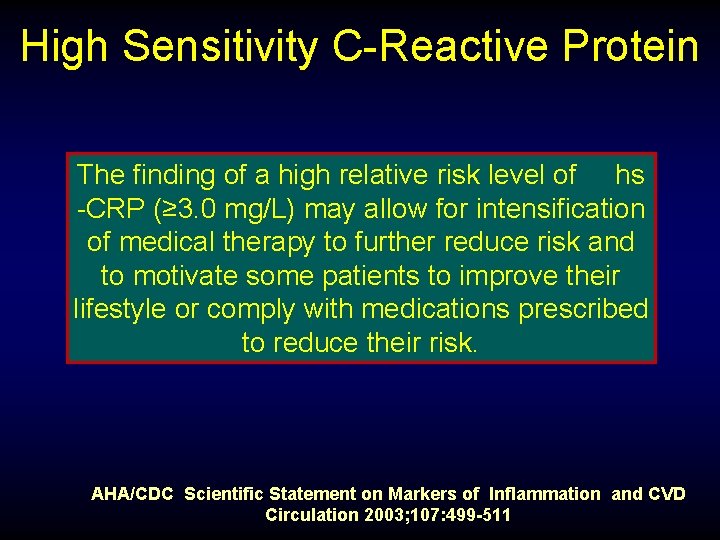
High Sensitivity C-Reactive Protein The finding of a high relative risk level of hs -CRP (≥ 3. 0 mg/L) may allow for intensification of medical therapy to further reduce risk and to motivate some patients to improve their lifestyle or comply with medications prescribed to reduce their risk. AHA/CDC Scientific Statement on Markers of Inflammation and CVD Circulation 2003; 107: 499 -511
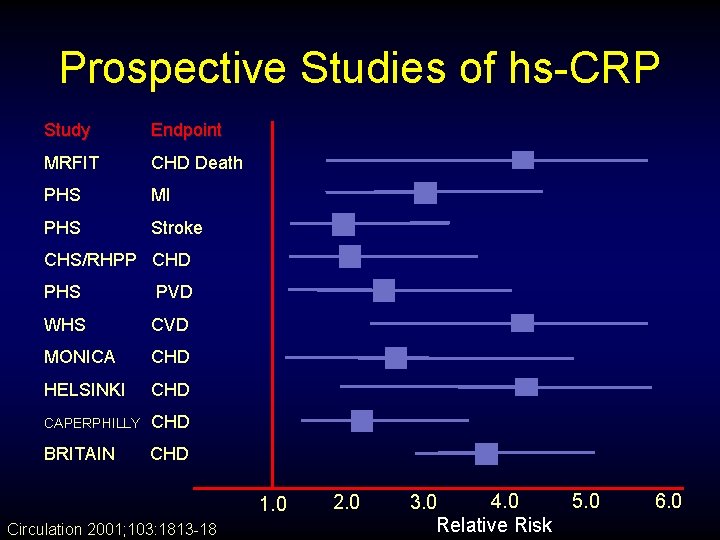
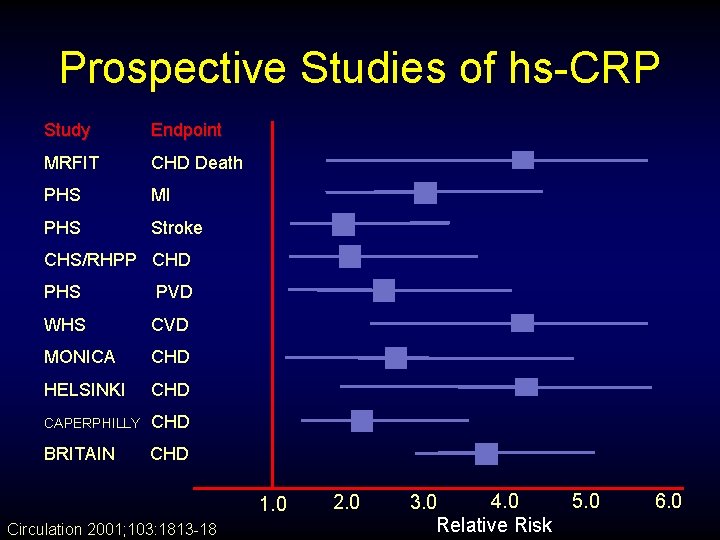
Prospective Studies of hs-CRP Study Endpoint MRFIT CHD Death PHS MI PHS Stroke CHS/RHPP CHD PHS PVD WHS CVD MONICA CHD HELSINKI CHD CAPERPHILLY CHD BRITAIN CHD 1. 0 Circulation 2001; 103: 1813 -18 2. 0 4. 0 5. 0 3. 0 Relative Risk 6. 0
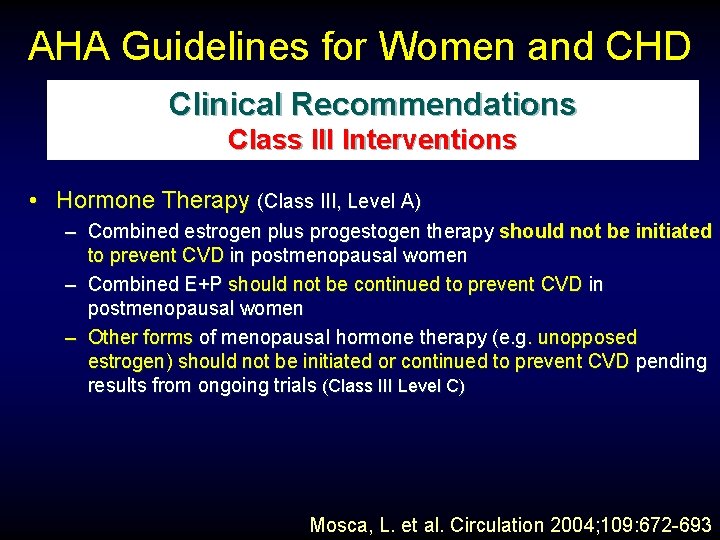
AHA Guidelines for Women and CHD Clinical Recommendations Class III Interventions • Hormone Therapy (Class III, Level A) – Combined estrogen plus progestogen therapy should not be initiated to prevent CVD in postmenopausal women – Combined E+P should not be continued to prevent CVD in postmenopausal women – Other forms of menopausal hormone therapy (e. g. unopposed estrogen) should not be initiated or continued to prevent CVD pending results from ongoing trials (Class III Level C) Mosca, L. et al. Circulation 2004; 109: 672 -693
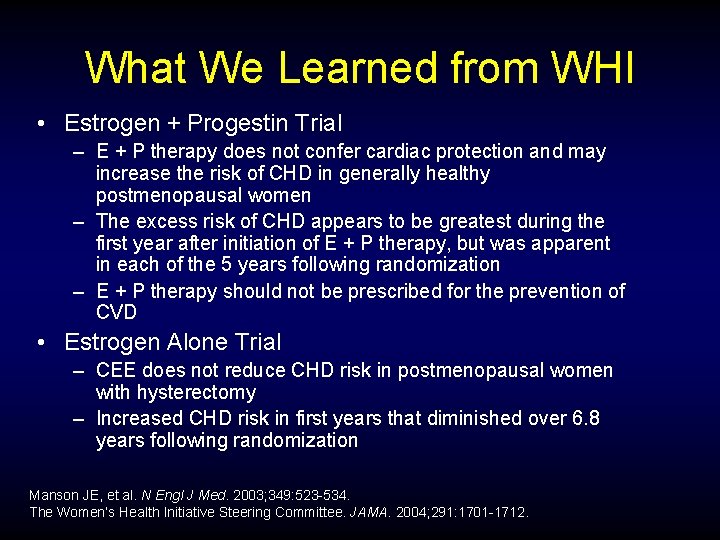
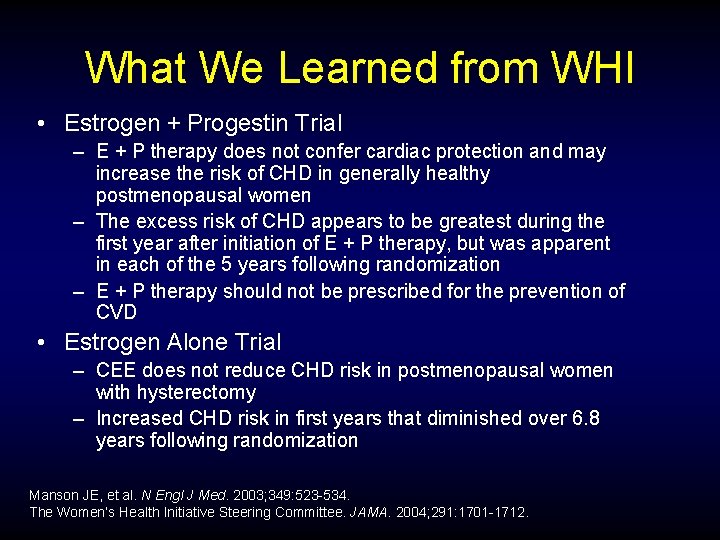
What We Learned from WHI • Estrogen + Progestin Trial – E + P therapy does not confer cardiac protection and may increase the risk of CHD in generally healthy postmenopausal women – The excess risk of CHD appears to be greatest during the first year after initiation of E + P therapy, but was apparent in each of the 5 years following randomization – E + P therapy should not be prescribed for the prevention of CVD • Estrogen Alone Trial – CEE does not reduce CHD risk in postmenopausal women with hysterectomy – Increased CHD risk in first years that diminished over 6. 8 years following randomization Manson JE, et al. N Engl J Med. 2003; 349: 523 -534. The Women’s Health Initiative Steering Committee. JAMA. 2004; 291: 1701 -1712.
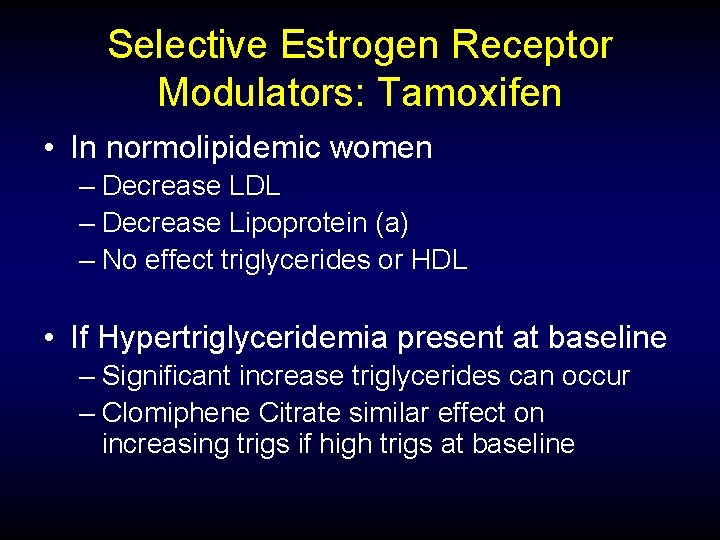
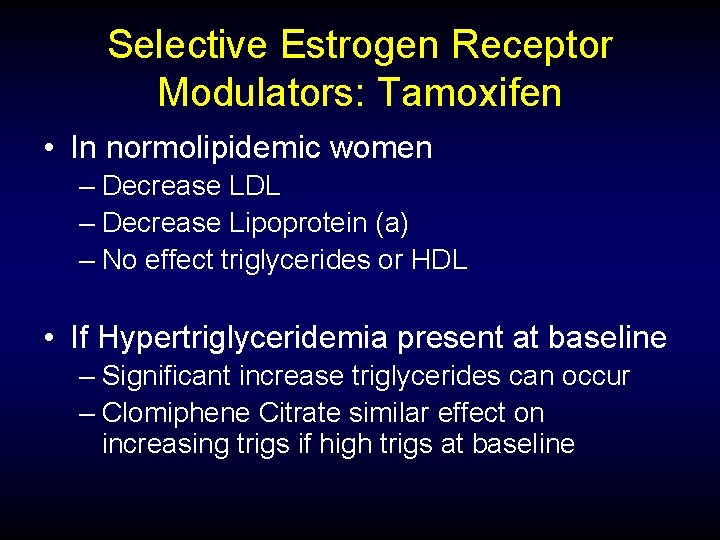
Selective Estrogen Receptor Modulators: Tamoxifen • In normolipidemic women – Decrease LDL – Decrease Lipoprotein (a) – No effect triglycerides or HDL • If Hypertriglyceridemia present at baseline – Significant increase triglycerides can occur – Clomiphene Citrate similar effect on increasing trigs if high trigs at baseline
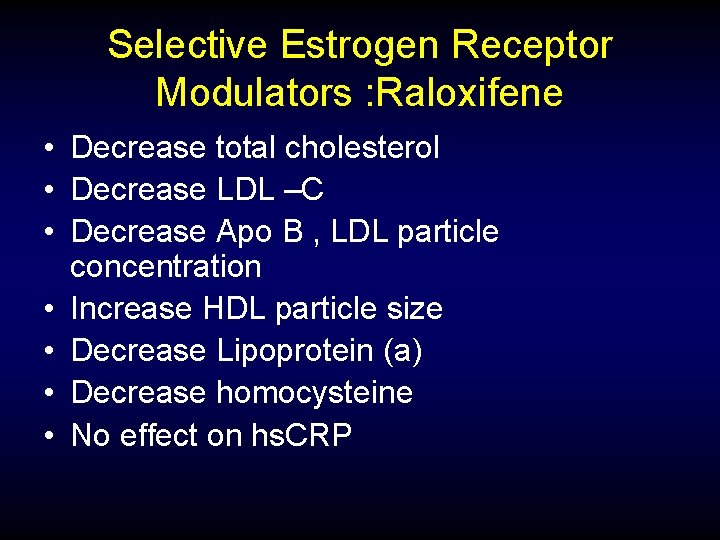
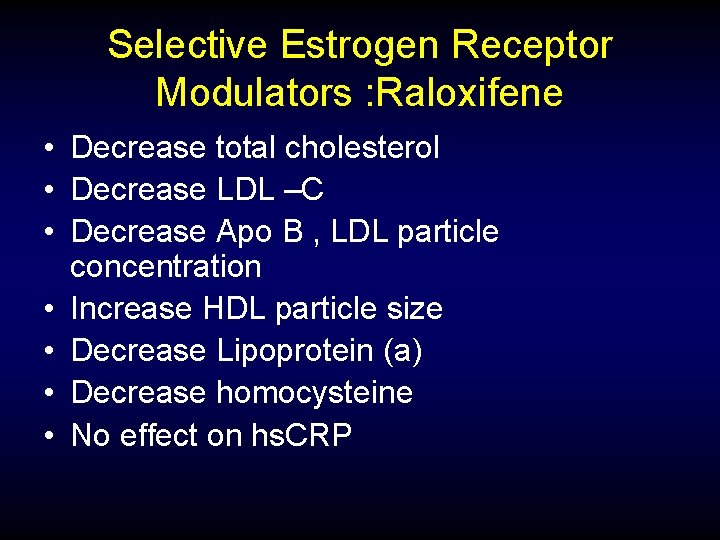
Selective Estrogen Receptor Modulators : Raloxifene • Decrease total cholesterol • Decrease LDL –C • Decrease Apo B , LDL particle concentration • Increase HDL particle size • Decrease Lipoprotein (a) • Decrease homocysteine • No effect on hs. CRP
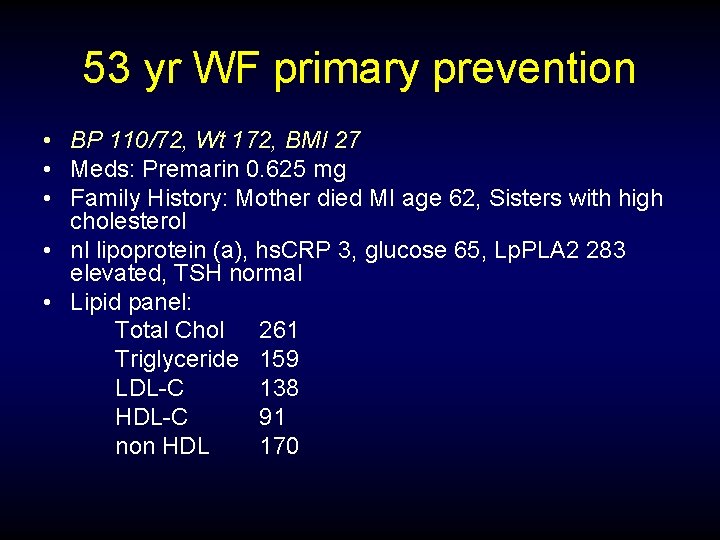
53 yr WF primary prevention • BP 110/72, Wt 172, BMI 27 • Meds: Premarin 0. 625 mg • Family History: Mother died MI age 62, Sisters with high cholesterol • nl lipoprotein (a), hs. CRP 3, glucose 65, Lp. PLA 2 283 elevated, TSH normal • Lipid panel: Total Chol 261 Triglyceride 159 LDL-C 138 HDL-C 91 non HDL 170

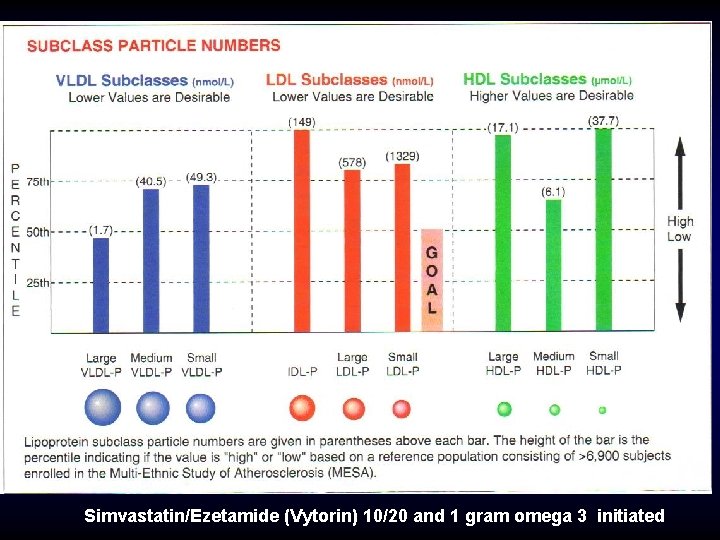
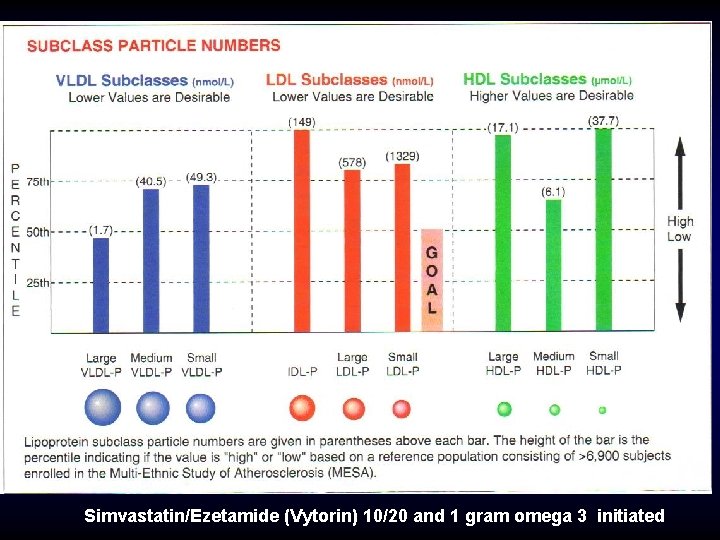
Simvastatin/Ezetamide (Vytorin) 10/20 and 1 gram omega 3 initiated
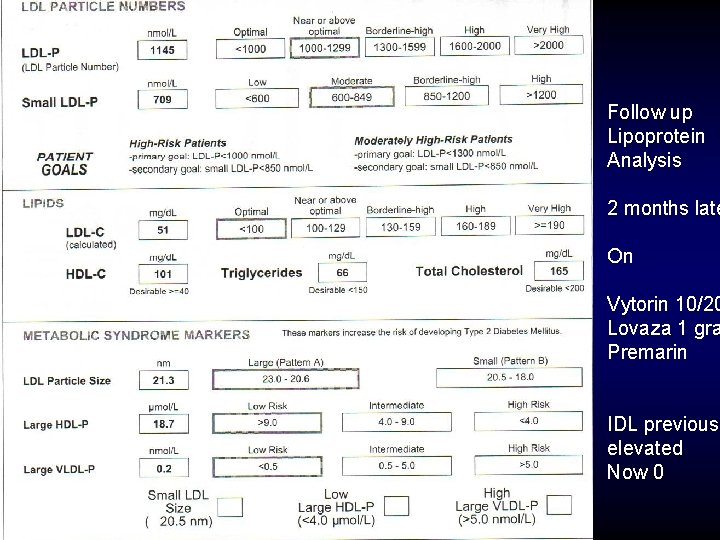
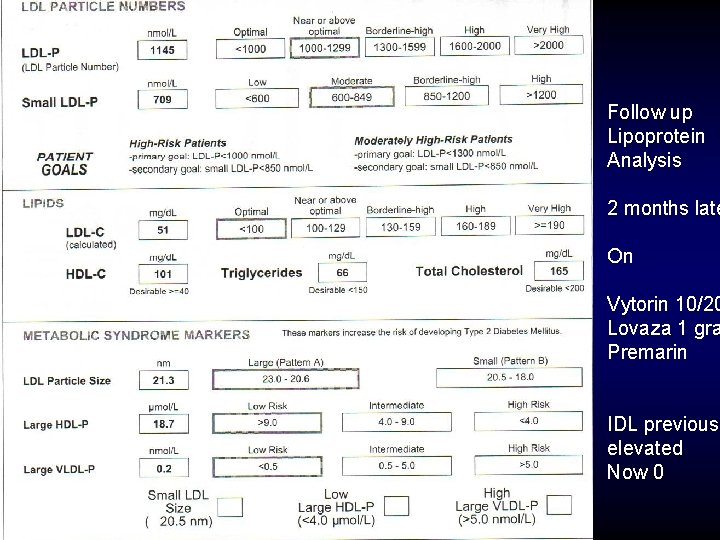
Follow up Lipoprotein Analysis 2 months late On Vytorin 10/20 Lovaza 1 gra Premarin IDL previousl elevated Now 0
Case #3 30 yr old WF Metabolic syndrome Severe hypertriglyceridemia
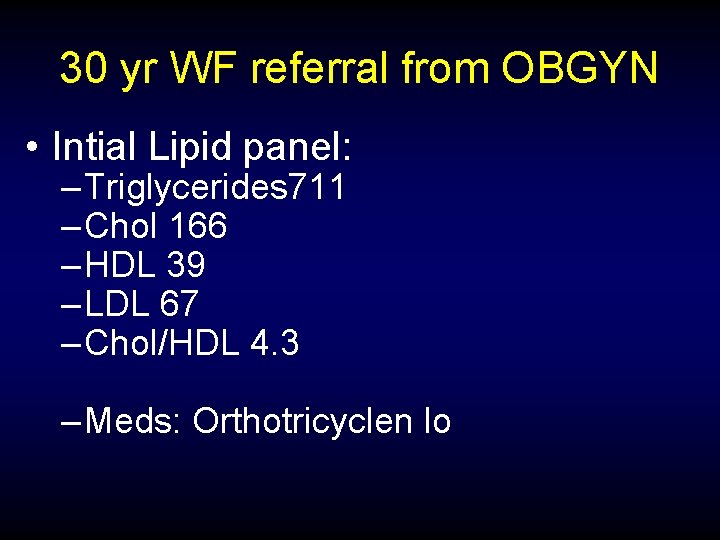
30 yr WF referral from OBGYN • Intial Lipid panel: – Triglycerides 711 – Chol 166 – HDL 39 – LDL 67 – Chol/HDL 4. 3 – Meds: Orthotricyclen lo
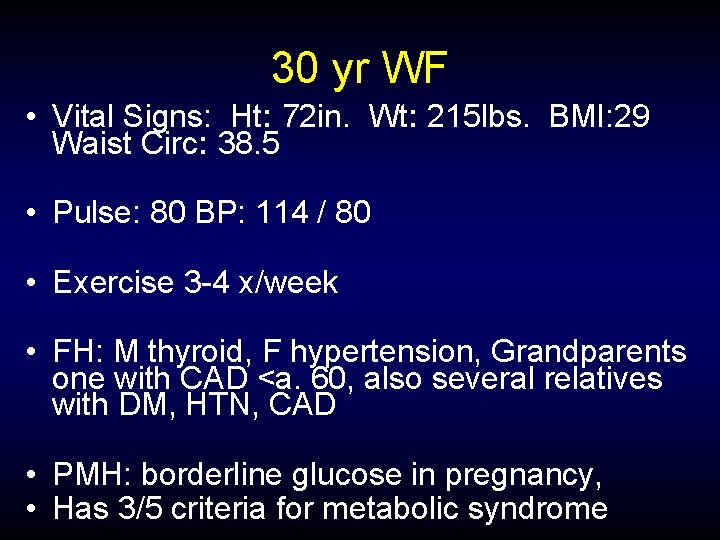
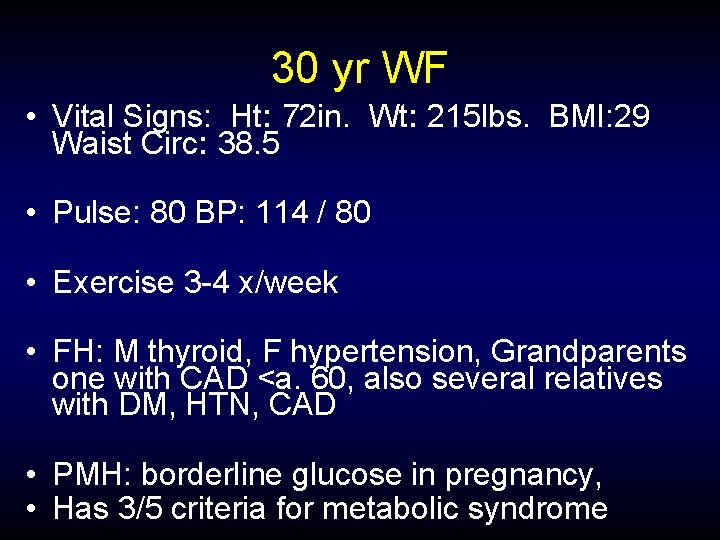
30 yr WF • Vital Signs: Ht: 72 in. Wt: 215 lbs. BMI: 29 Waist Circ: 38. 5 • Pulse: 80 BP: 114 / 80 • Exercise 3 -4 x/week • FH: M thyroid, F hypertension, Grandparents one with CAD <a. 60, also several relatives with DM, HTN, CAD • PMH: borderline glucose in pregnancy, • Has 3/5 criteria for metabolic syndrome
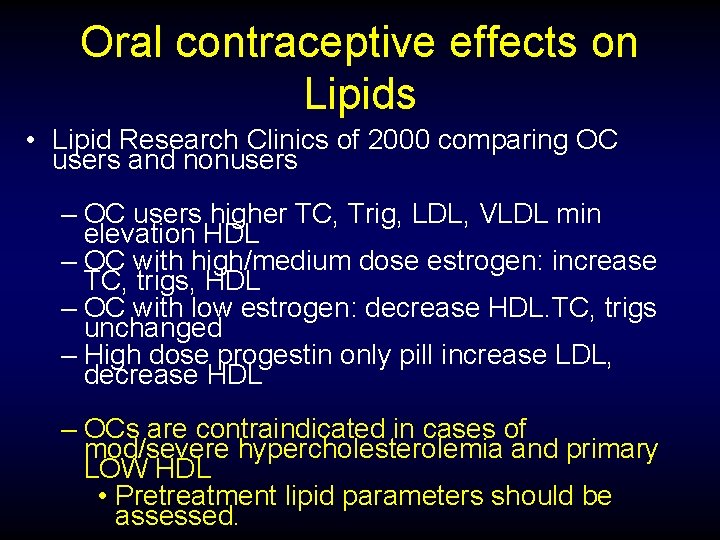
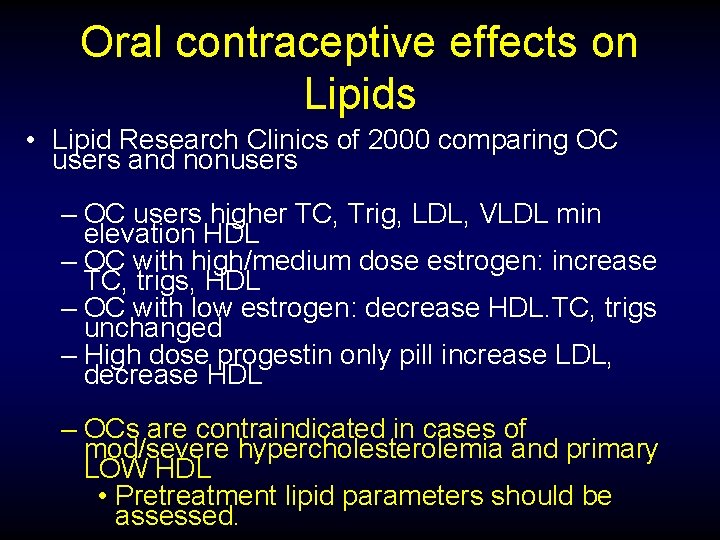
Oral contraceptive effects on Lipids • Lipid Research Clinics of 2000 comparing OC users and nonusers – OC users higher TC, Trig, LDL, VLDL min elevation HDL – OC with high/medium dose estrogen: increase TC, trigs, HDL – OC with low estrogen: decrease HDL. TC, trigs unchanged – High dose progestin only pill increase LDL, decrease HDL – OCs are contraindicated in cases of mod/severe hypercholesterolemia and primary LOW HDL • Pretreatment lipid parameters should be assessed.
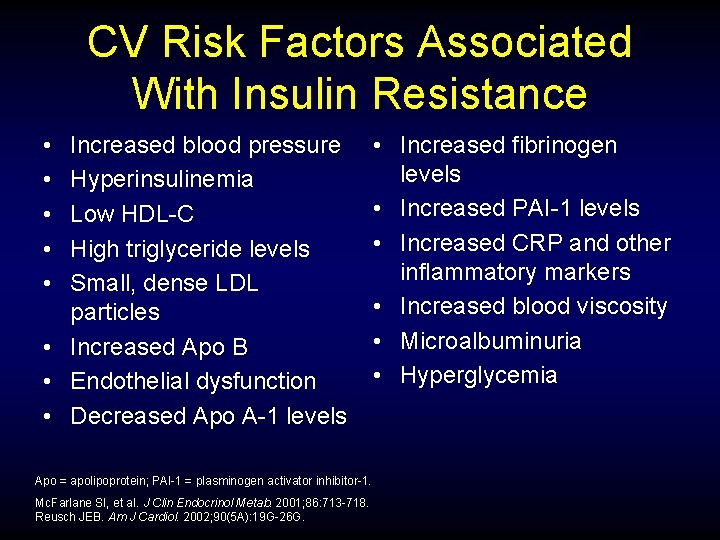
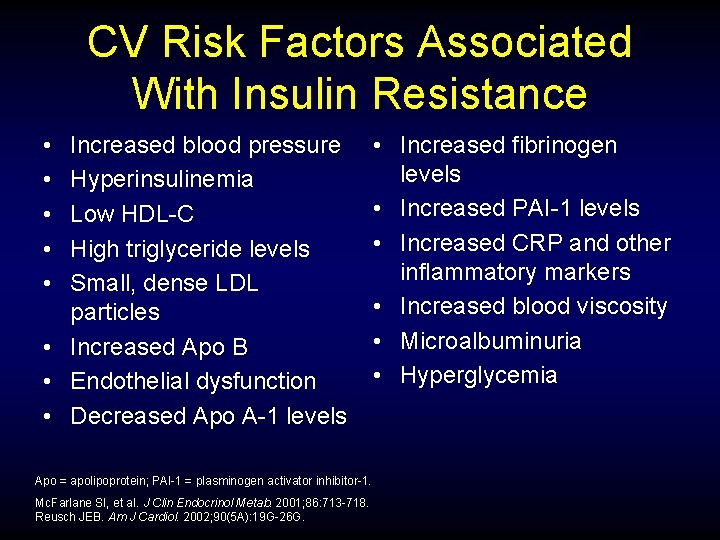
CV Risk Factors Associated With Insulin Resistance • • • Increased blood pressure Hyperinsulinemia Low HDL-C High triglyceride levels Small, dense LDL particles • Increased Apo B • Endothelial dysfunction • Decreased Apo A-1 levels Apo = apolipoprotein; PAI-1 = plasminogen activator inhibitor-1. Mc. Farlane SI, et al. J Clin Endocrinol Metab. 2001; 86: 713 -718. Reusch JEB. Am J Cardiol. 2002; 90(5 A): 19 G-26 G. • Increased fibrinogen levels • Increased PAI-1 levels • Increased CRP and other inflammatory markers • Increased blood viscosity • Microalbuminuria • Hyperglycemia
Therapeutic Lifestyle Changes in Metabolic Syndrome (NCEP ATP III) • The greatest benefit from successful therapeutic lifestyle changes (TLC) will occur in persons diagnosed with metabolic syndrome • TLC is an appropriate initial intervention for these patients National Cholesterol Education Program Adult Treatment Panel III. Circulation. 2002; 106: 3143 -3421.

Treatment Considerations 30 yr old with very high trigs and metabolic syndrome
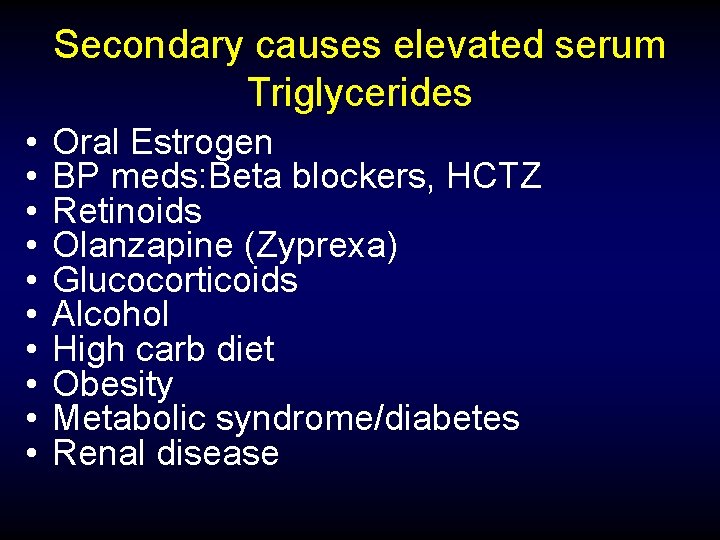
Secondary causes elevated serum Triglycerides • • • Oral Estrogen BP meds: Beta blockers, HCTZ Retinoids Olanzapine (Zyprexa) Glucocorticoids Alcohol High carb diet Obesity Metabolic syndrome/diabetes Renal disease
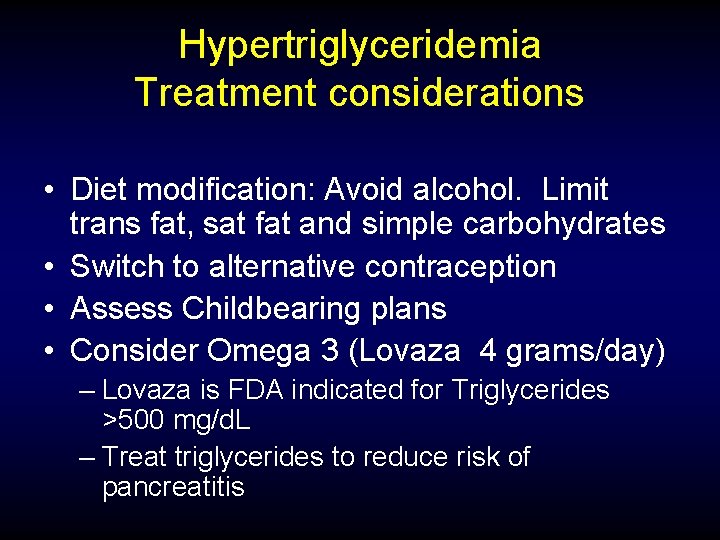
Hypertriglyceridemia Treatment considerations • Diet modification: Avoid alcohol. Limit trans fat, sat fat and simple carbohydrates • Switch to alternative contraception • Assess Childbearing plans • Consider Omega 3 (Lovaza 4 grams/day) – Lovaza is FDA indicated for Triglycerides >500 mg/d. L – Treat triglycerides to reduce risk of pancreatitis
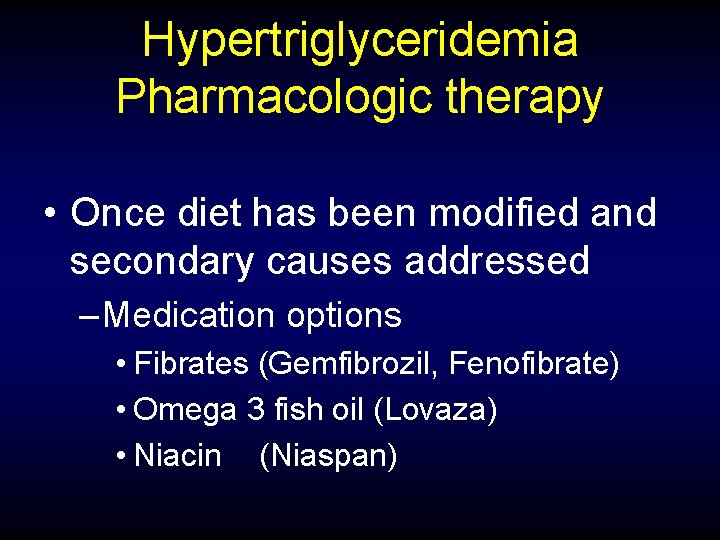
Hypertriglyceridemia Pharmacologic therapy • Once diet has been modified and secondary causes addressed – Medication options • Fibrates (Gemfibrozil, Fenofibrate) • Omega 3 fish oil (Lovaza) • Niacin (Niaspan)
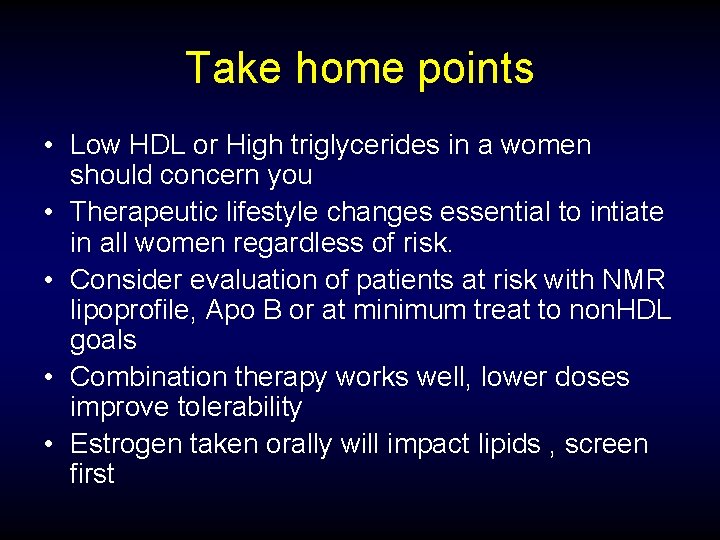
Take home points • Low HDL or High triglycerides in a women should concern you • Therapeutic lifestyle changes essential to intiate in all women regardless of risk. • Consider evaluation of patients at risk with NMR lipoprofile, Apo B or at minimum treat to non. HDL goals • Combination therapy works well, lower doses improve tolerability • Estrogen taken orally will impact lipids , screen first
 Tara dall
Tara dall Paradigm shift from women studies to gender studies
Paradigm shift from women studies to gender studies Best case worst case average case
Best case worst case average case Bharathi viswanathan
Bharathi viswanathan Karvonen formule
Karvonen formule Normal bpm for women
Normal bpm for women Heart disease symptoms
Heart disease symptoms Randi sokol
Randi sokol Cyanotic vs acyanotic
Cyanotic vs acyanotic Ronaldo heart disease
Ronaldo heart disease Murmur in asd
Murmur in asd Pediatric knee chest position
Pediatric knee chest position Feline
Feline Heart disease data
Heart disease data Samina waqar
Samina waqar Mitral regurgitation symptoms
Mitral regurgitation symptoms Site:slidetodoc.com
Site:slidetodoc.com Terrible t's cyanotic heart disease
Terrible t's cyanotic heart disease Lower lobe diversion
Lower lobe diversion Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Causes of valvular heart disease
Causes of valvular heart disease Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Causes of valvular heart disease
Causes of valvular heart disease Preload and afterload
Preload and afterload Causes of valvular heart disease
Causes of valvular heart disease Congenital heart disease pda
Congenital heart disease pda Fish mouth buttonhole stenosis
Fish mouth buttonhole stenosis Mitral facies
Mitral facies Coronary heart disease
Coronary heart disease Chronic coronary syndrome
Chronic coronary syndrome Strepsore
Strepsore Rheumatic heart disease causes
Rheumatic heart disease causes Superadded changes in coronary atherosclerosis
Superadded changes in coronary atherosclerosis Pac ecg
Pac ecg Nyha classification
Nyha classification Heart disease and stroke are the world's biggest killers
Heart disease and stroke are the world's biggest killers Chronic rheumatic heart disease
Chronic rheumatic heart disease Le conversioni di leopardi
Le conversioni di leopardi Prospetto ortogonale
Prospetto ortogonale Cameretta vista dall'alto disegno
Cameretta vista dall'alto disegno Domenico dall'olio
Domenico dall'olio Dall'infinitamente piccolo all'infinitamente grande
Dall'infinitamente piccolo all'infinitamente grande Caroline dall
Caroline dall La parola bullismo deriva dall'inglese
La parola bullismo deriva dall'inglese Dall'aurora al tramonto canto ingresso
Dall'aurora al tramonto canto ingresso Business planning. dall'idea al progetto imprenditoriale
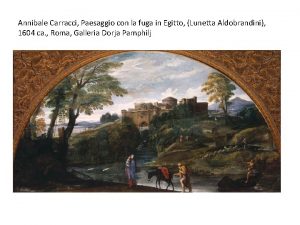
Business planning. dall'idea al progetto imprenditoriale Lunetta aldobrandini
Lunetta aldobrandini Nella cmr l'avaria è il danneggiamento della merce
Nella cmr l'avaria è il danneggiamento della merce La deriva dipende dall'angolo di campanatura delle ruote
La deriva dipende dall'angolo di campanatura delle ruote Il freno oleopneumatico agisce sull'albero di trasmissione
Il freno oleopneumatico agisce sull'albero di trasmissione Excursus normativo dall'integrazione all'inclusione
Excursus normativo dall'integrazione all'inclusione Dall'albero alla carta
Dall'albero alla carta Conversione dal bello al vero
Conversione dal bello al vero Pareggiate dell'imbianchino
Pareggiate dell'imbianchino Quale continente è tagliato a metà dall'equatore
Quale continente è tagliato a metà dall'equatore Ricordo quegli occhi pieni di vita
Ricordo quegli occhi pieni di vita Energia termica dall'oceano
Energia termica dall'oceano Esempi prove strutturate per classi parallele scuola media
Esempi prove strutturate per classi parallele scuola media Narrativa del 900
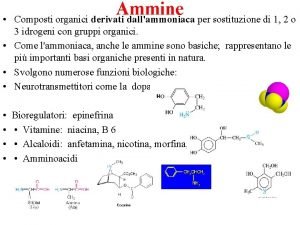
Narrativa del 900 Cicloesanammina
Cicloesanammina Celiac disease pes statement
Celiac disease pes statement Advantages of descriptive research
Advantages of descriptive research Times 100 case studies
Times 100 case studies Times 100 case studies
Times 100 case studies Holistic technology in professional ethics
Holistic technology in professional ethics Advantages and disadvantages of case control studies
Advantages and disadvantages of case control studies Advantages and disadvantages of case control studies
Advantages and disadvantages of case control studies Eu-gdpr-p
Eu-gdpr-p Gcse geography manchester case study
Gcse geography manchester case study Case studies on euthanasia
Case studies on euthanasia E procurement case studies
E procurement case studies Types of case studies
Types of case studies Definition of case study
Definition of case study Kellogg's crunchy nut bites market research
Kellogg's crunchy nut bites market research Nasa system failure case studies
Nasa system failure case studies Abo discrepancy
Abo discrepancy Chemistry-ethics case studies
Chemistry-ethics case studies Nspe board of ethical review
Nspe board of ethical review Goal2u
Goal2u Jmp case studies
Jmp case studies Case studies of rtos
Case studies of rtos Ferpa case studies
Ferpa case studies Social engineering case studies
Social engineering case studies Case studies
Case studies Financial management case study
Financial management case study Digital marketing case studies 2012
Digital marketing case studies 2012 Forensic entomology double puzzle answers
Forensic entomology double puzzle answers