Unit 5 Cardiovascular Disease Cardiovascular Disease Overview 1


- Slides: 40
Unit # 5 Cardiovascular Disease
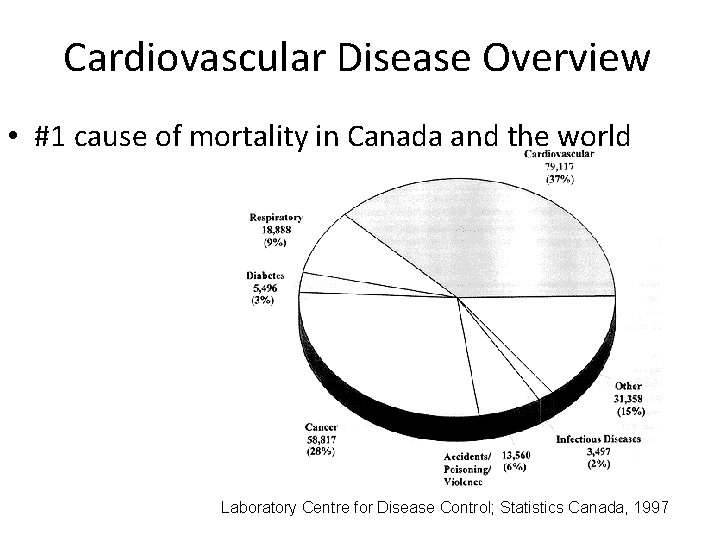
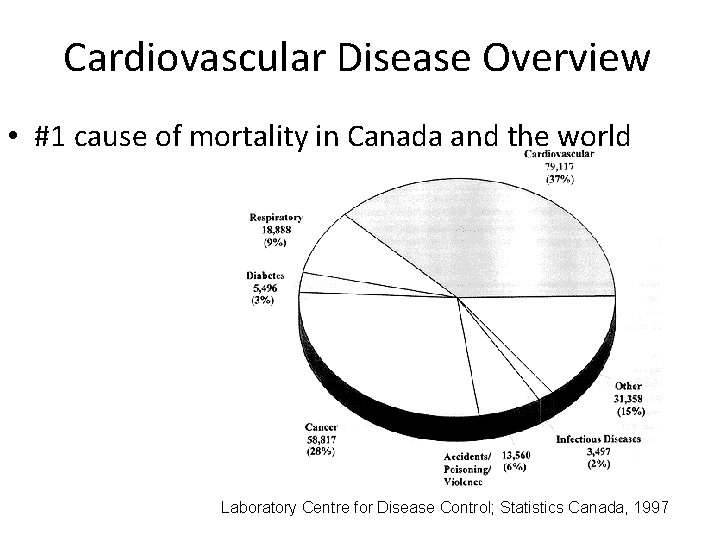
Cardiovascular Disease Overview • #1 cause of mortality in Canada and the world Laboratory Centre for Disease Control; Statistics Canada, 1997
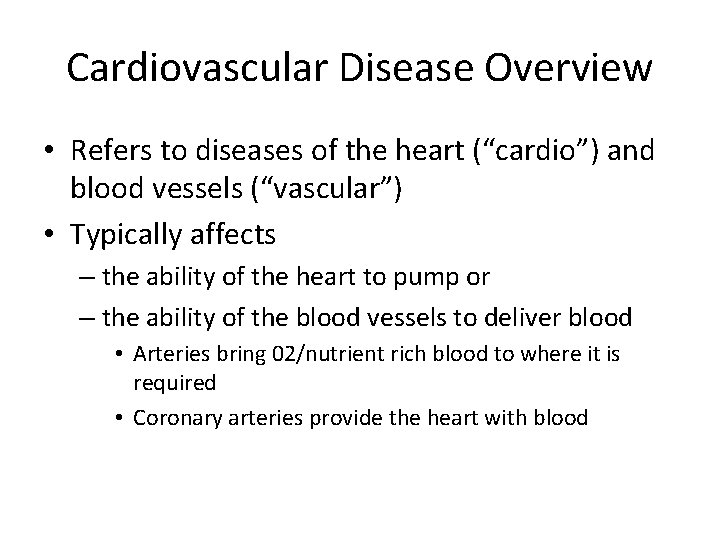
Cardiovascular Disease Overview • Refers to diseases of the heart (“cardio”) and blood vessels (“vascular”) • Typically affects – the ability of the heart to pump or – the ability of the blood vessels to deliver blood • Arteries bring 02/nutrient rich blood to where it is required • Coronary arteries provide the heart with blood
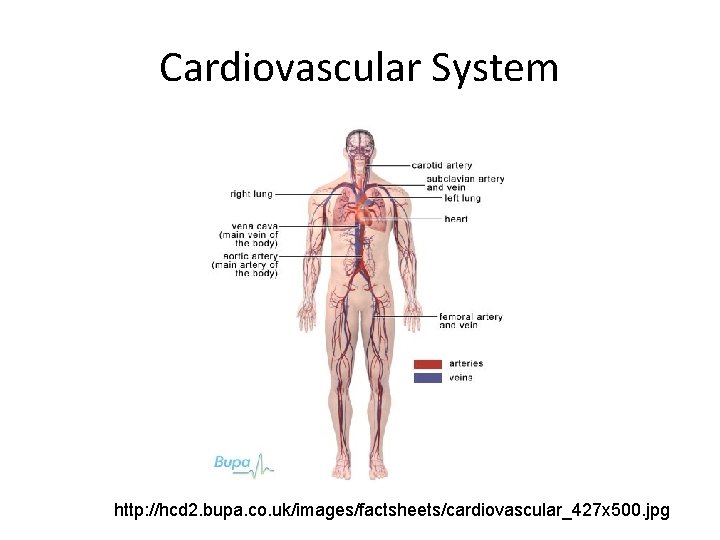
Cardiovascular System http: //hcd 2. bupa. co. uk/images/factsheets/cardiovascular_427 x 500. jpg
Major forms of Cardiovascular Disease (CVD) • Atherosclerosis: progressive narrowing of the arteries typically caused by fatty deposits • Coronary Artery Disease (CAD)/ coronary heart disease (CHD): atherosclerosis of the coronary artery • Heart Failure • Hypertension (high blood pressure) • Cerebrovascular disease
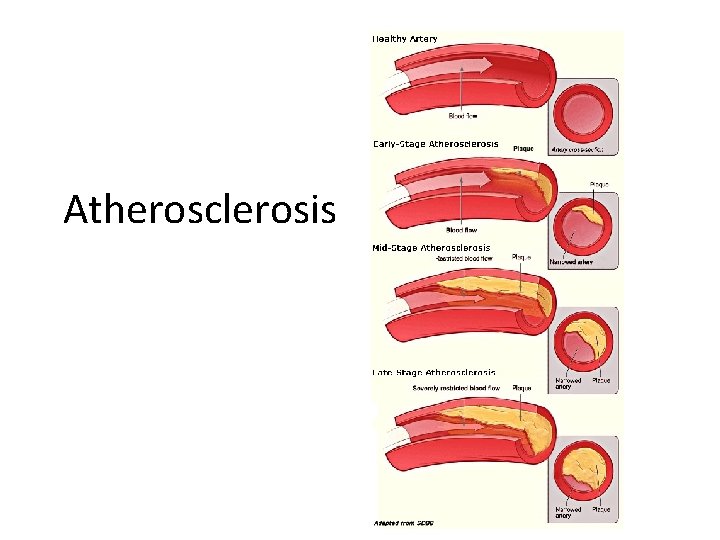
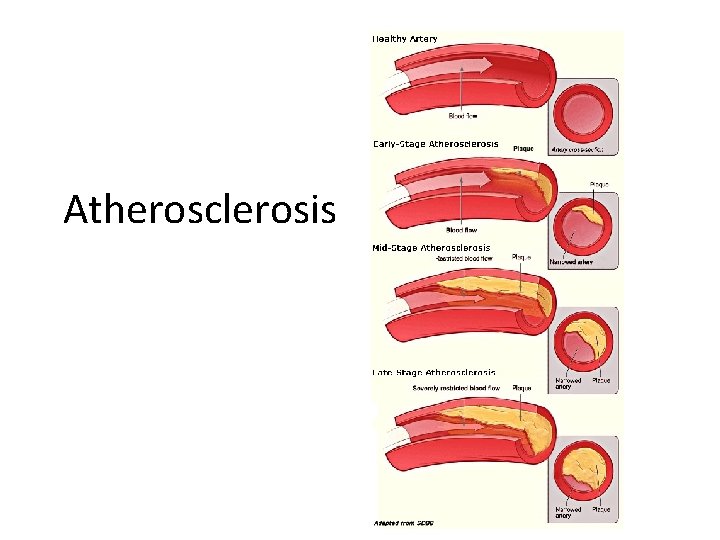
Atherosclerosis
Development of Atherosclerosis 1. Begins with a lesion (injury) to the inner wall of the artery. This is typically caused by ______ or _________ 2. Dietary _________is converted into cholesterol, which can be carried in the blood by a type of lipoprotein called low-density lipoprotein (LDL; aka ‘bad cholesterol’)
Development of Atherosclerosis • 3. This LDL become oxidized by free radicals in the blood stream. This oxidized LDL (ox-LDL) causes further damage to the artery wall, while calcium, cellular waste and platelets get deposited into the area
Development of Atherosclerosis • 4. Macrophages infiltrate the area to try to repair the damage by absorbing the ox-LDL • 5. These macrophages then become enlarged foam cells, which cannot process the ox-LDL
Development of Atherosclerosis • 6. The foam cells then rupture, depositing more ox-LDL into the artery wall, narrowing it
Development of Atherosclerosis • 7. More macrophages are then recruited to help with the damage, leading to more deposition of ox-LDL. This area narrowed by cholesterol is called a _____
• 8. Smooth muscle cells on the artery wall then form a hard cover the inflamed area, narrowing the artery
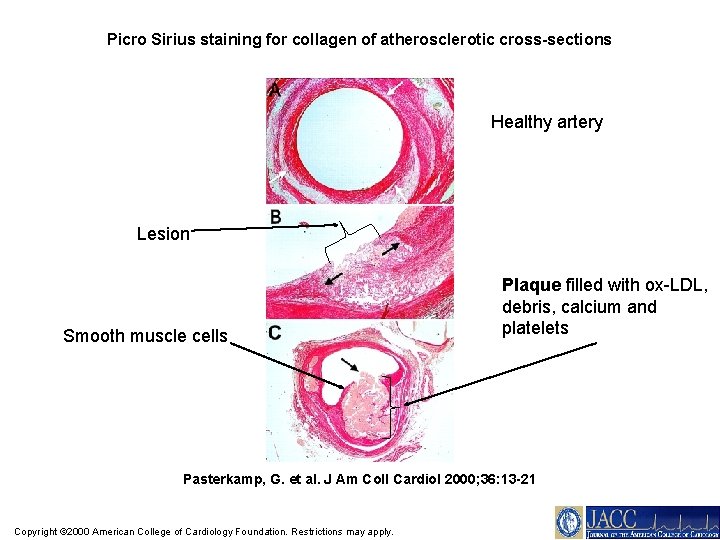
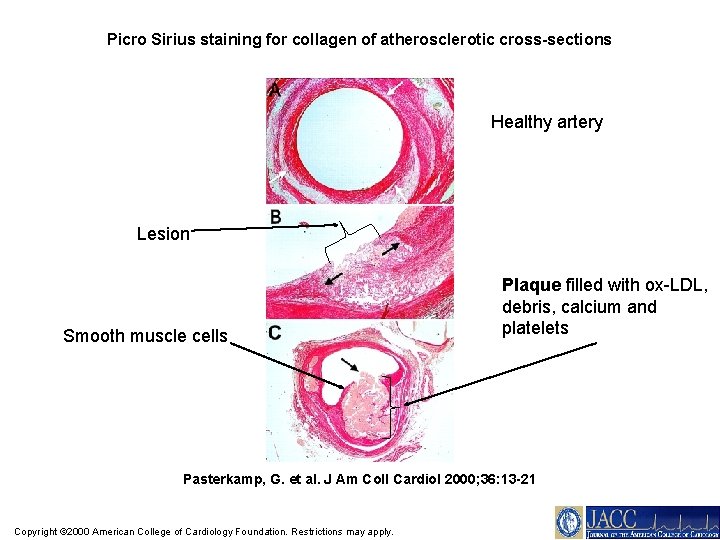
Picro Sirius staining for collagen of atherosclerotic cross-sections Healthy artery Lesion Smooth muscle cells Plaque filled with ox-LDL, debris, calcium and platelets Pasterkamp, G. et al. J Am Coll Cardiol 2000; 36: 13 -21 Copyright © 2000 American College of Cardiology Foundation. Restrictions may apply.
Major Consequences of Atherosclerosis 1. Atherosclerosis can reduce the elasticity of the arteries, making them less able to respond to demand putting more strain on the heart
Major Consequences of Atherosclerosis • 2. Atherosclerosis can cause an aneurism, a dilation of the artery, which can eventually rupture, leaking blood into the surroundings (haemorrhage)
Major Consequences of Atherosclerosis 3. Atherosclerosis reduces blood flow and can completely block blood flow if a thrombus (blood clot) gets lodged there
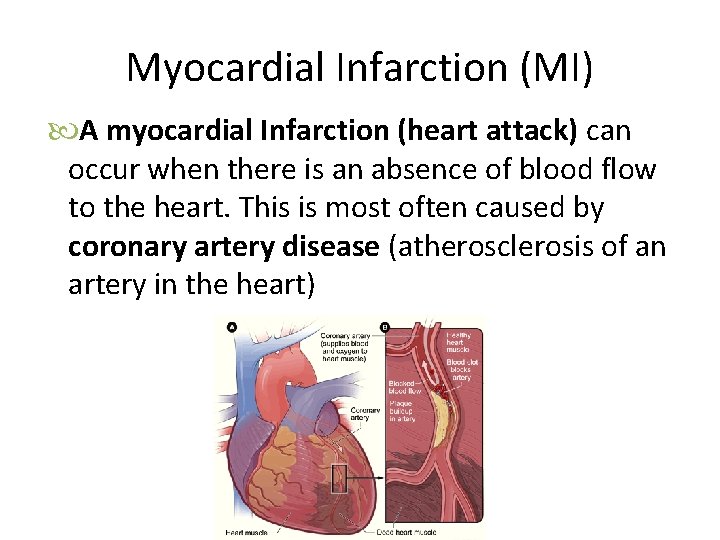
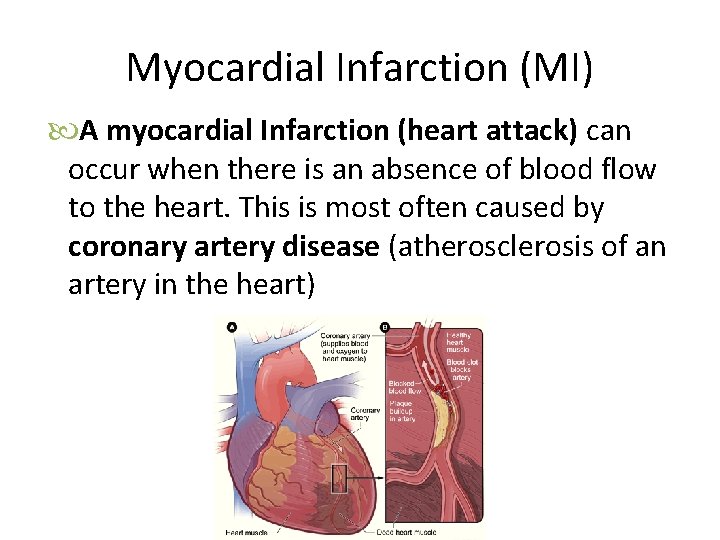
Myocardial Infarction (MI) A myocardial Infarction (heart attack) can occur when there is an absence of blood flow to the heart. This is most often caused by coronary artery disease (atherosclerosis of an artery in the heart)
Warning signs of an MI • Pain – Sudden; constant pain in the chest, neck, jaw, shoulder, arms or pack – Pain feels like burning, squeezing, heaviness, tightness, pressure • Shortness of breath • Nausea – Indigestion, vomiting • Sweating • Fear – Anxiety, denial
Responding to the signs of an MI • CALL 911! • All activity should be stopped, lie/sit comfortably • If chest pain is experienced, swallow a 325 mg tablet of Aspirin (acetylsalicylic acid; thins blood) • If you take nitro-glycerine, take normal dosage • Patient should rest comfortably and wait for emergency response • CPR can be performed by a trained person
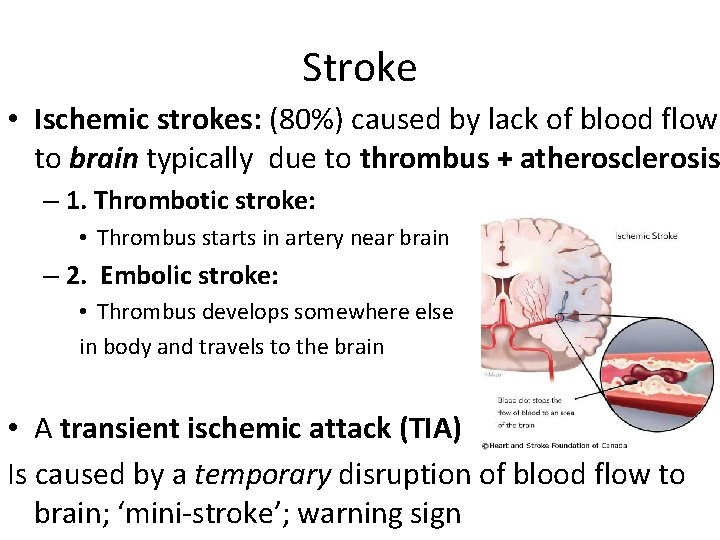
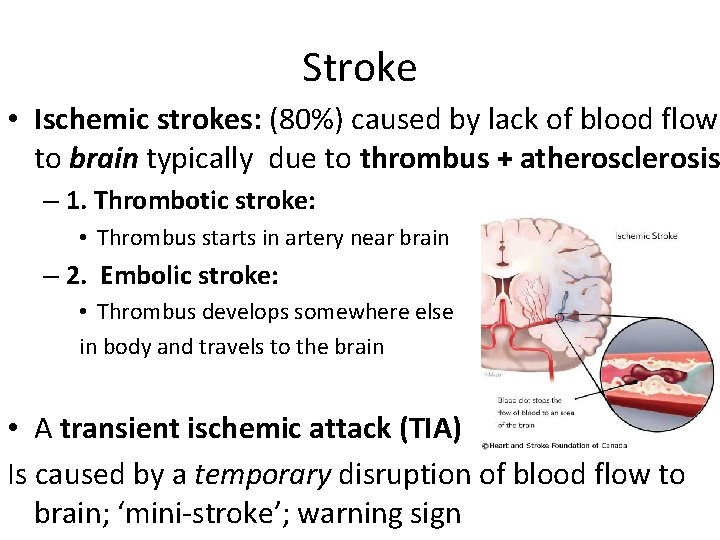
Stroke • Ischemic strokes: (80%) caused by lack of blood flow to brain typically due to thrombus + atherosclerosis – 1. Thrombotic stroke: • Thrombus starts in artery near brain – 2. Embolic stroke: • Thrombus develops somewhere else in body and travels to the brain • A transient ischemic attack (TIA) Is caused by a temporary disruption of blood flow to brain; ‘mini-stroke’; warning sign
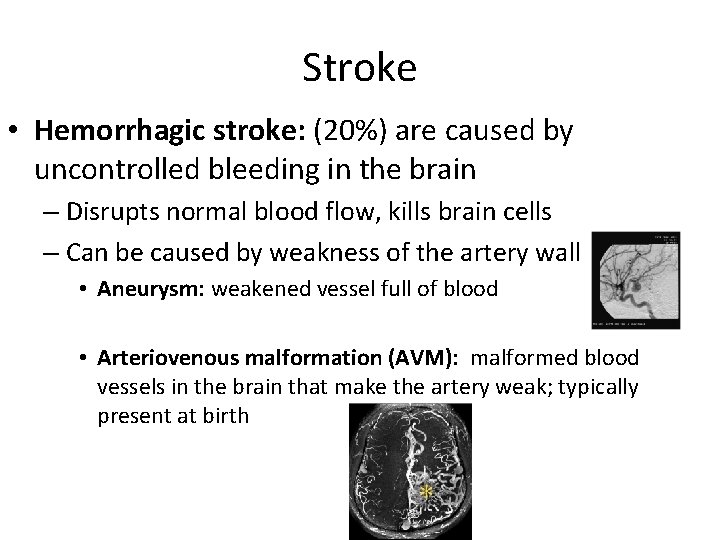
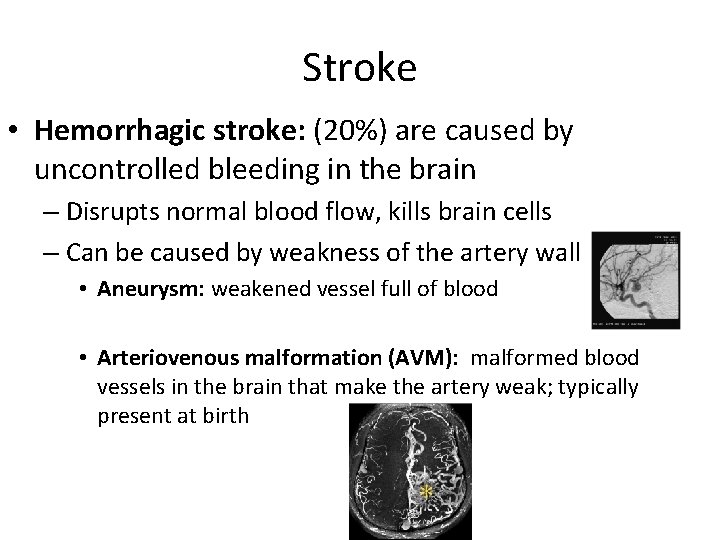
Stroke • Hemorrhagic stroke: (20%) are caused by uncontrolled bleeding in the brain – Disrupts normal blood flow, kills brain cells – Can be caused by weakness of the artery wall • Aneurysm: weakened vessel full of blood • Arteriovenous malformation (AVM): malformed blood vessels in the brain that make the artery weak; typically present at birth
5 Stroke Warning Signs • Weakness- sudden loss of strength, numb face, arms of legs • Trouble speaking- both understanding and speaking • Vision problems • Headache • Dizziness
Stroke Response • CALL 911! • Patient should rest comfortably • TIME is the most important factor in stroke recovery. For most cases of stroke, a patient has a narrow window of time (60 minutes) to get to the hospital to minimize its lasting effects

CVD RISK FACTORS
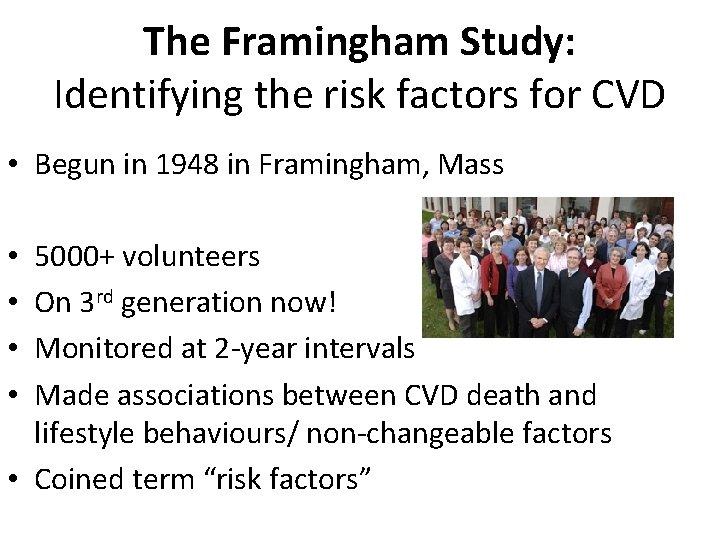
The Framingham Study: Identifying the risk factors for CVD • Begun in 1948 in Framingham, Mass 5000+ volunteers On 3 rd generation now! Monitored at 2 -year intervals Made associations between CVD death and lifestyle behaviours/ non-changeable factors • Coined term “risk factors” • •
CVD Risk Factors • Major Changeable – Hypertension, high blood cholesterol, tobacco smoke, physical inactivity, obesity, diabetes • Minor Changeable – Stress, low omega-3 FA, high alcohol consumption • Non-Changeable – Age, male gender, heredity, ethnicity
Major Changeable CVD Risk Factors • Hypertension = high arterial blood pressure – Can cause damage to blood vessels, put extra strain on the heart – Cause of hypertension can be unknown. However, high body fat, high salt intake, lack of exercise are known risk factors
Major Changeable CVD Risk Factors • High serum (blood) cholesterol – Typically caused by eating too much saturated fat – Can deposit in artery walls • LDL/VLDL = “bad” cholesterol – Recall: ox-LDL deposits in artery walls, forms plaque • HDL = “good” cholesterol – Lowers ox-LDL deposition in artery walls!
Major Changeable CVD Risk Factors • Tobacco smoke • Nicotine can cause lesions in the artery wall • Carbon monoxide in cigarette smoke is doubly damaging – causes lesions in the artery wall – decreases the ability of the blood to transport oxygen
Major Changeable CVD Risk Factors Physical Inactivity: exercise can lower blood pressure, increase HDL and lower LDL and VLDL, reduce stress, maintain body weight and control type II Diabetes. • Obesity/overweight, especially abdominal obesity – Can lead to hypertension, low HDL, type II diabetes Diabetes Mellitus: impaired ability of the blood to store glucose (sugar)

Other risk factors for CVD Stress: increases blood pressure, increases blood clotting, can increase cholesterol levels Low Omega-3 fatty acid intake: found in cold water fish fat, inverse correlation with CVD Alcohol: low daily intake (1 -2 glasses per day) of alcohol has been associated with lower risk of CVD! However, high intake can damage the heart muscle and increase CVD risk.
Major non-changeable risk factors for CVD Age : the older you are, the higher the risk Gender: males are at higher risk than females. Biological difference or cultural difference? Heredity Ethnicity: Higher risk in African Canadians, Latinos, Aboriginals and South Asians
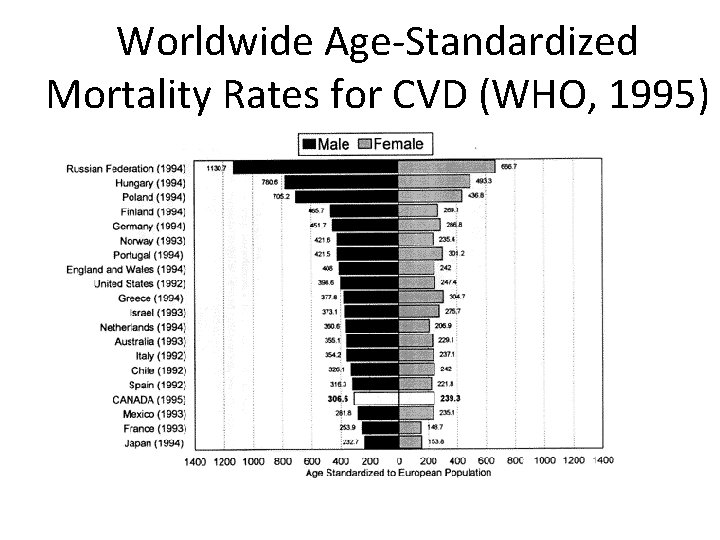
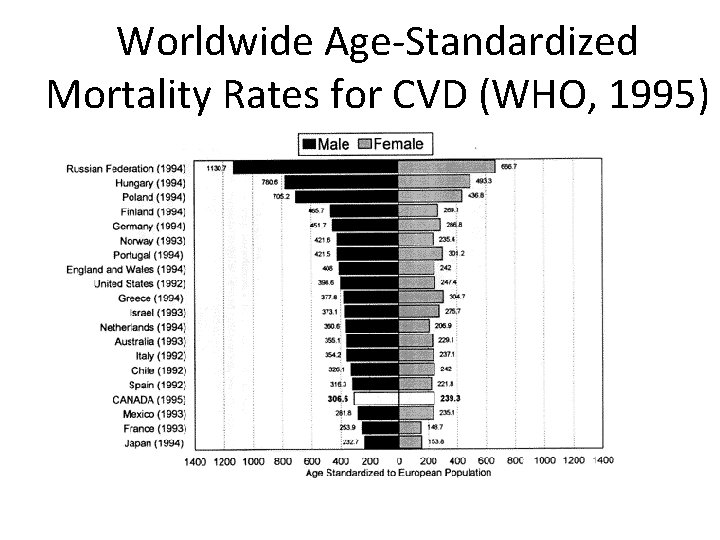
Worldwide Age-Standardized Mortality Rates for CVD (WHO, 1995)
Prevention of CVD: Primary vs. Secondary Prevention • Primary prevention looks to reduce risk factors to prevent a disease before it starts – Ex’s: • Secondary prevention focuses on treatment and early detection to prevent morbidity and mortality after a disease has started – Ex’s:
Treatment of CVD • The decline in the cases of CVD-related deaths in North America is mainly due to medical advances such as – Heart transplants – Artificial hearts: now used as a bridge during surgery, possible permanent devices in the future – Implanted pacemakers http: //cardiophile. org/wp-content/uploads/2008/11/scout-scan-of-pacemaker. jpg
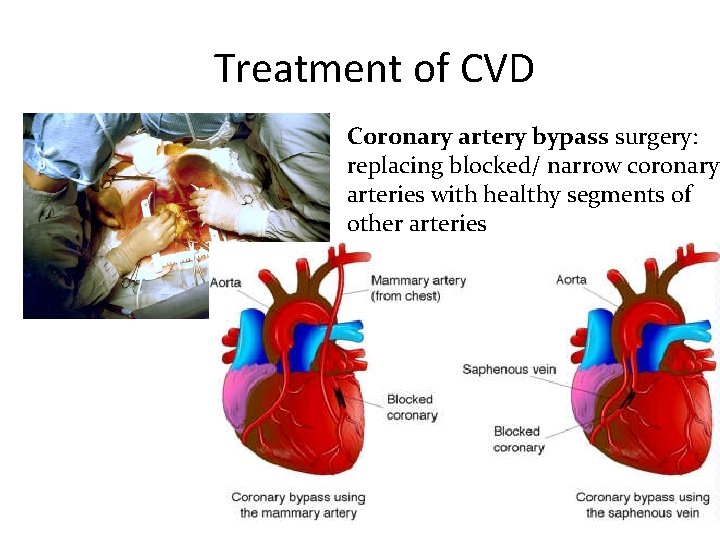
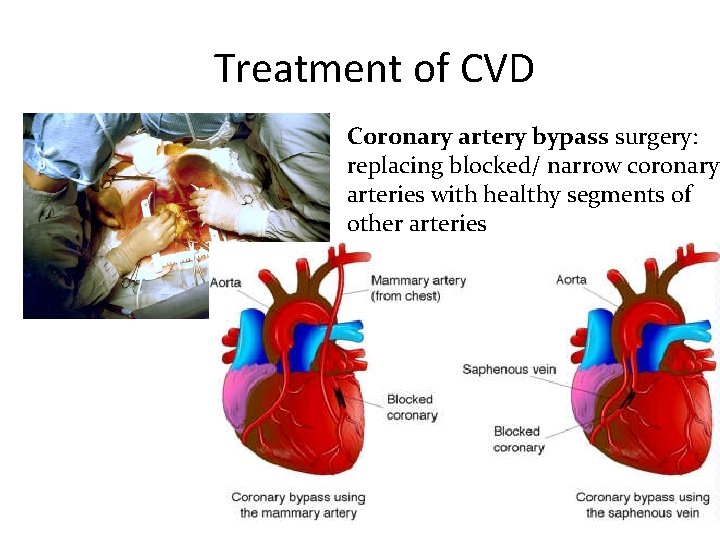
Treatment of CVD Coronary artery bypass surgery: replacing blocked/ narrow coronary arteries with healthy segments of other arteries
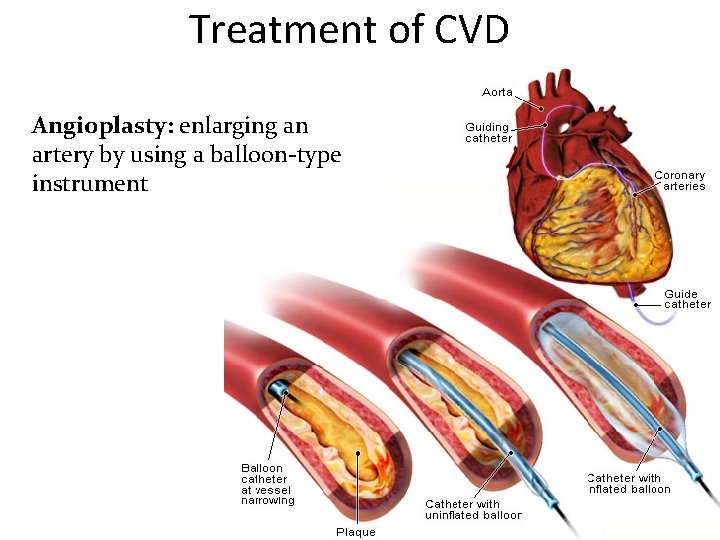
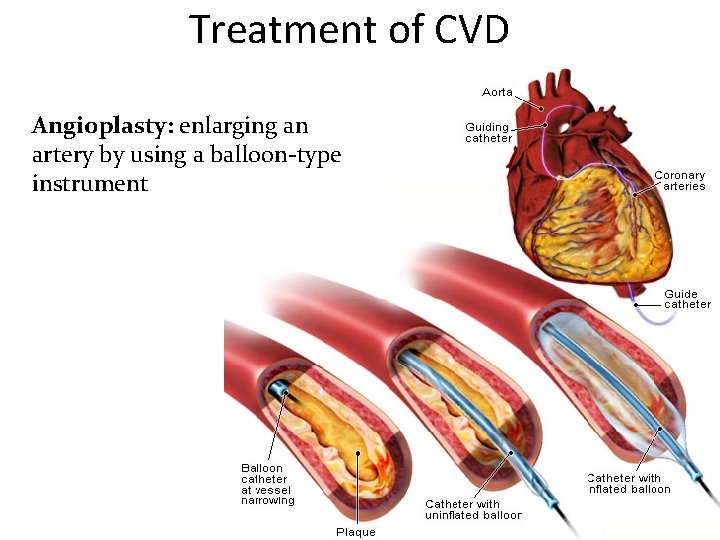
Treatment of CVD Angioplasty: enlarging an artery by using a balloon-type instrument
Treatment of CVD Drugs: target lowering blood pressure, reducing blood cholesterol, opening blood vessels, stabilizing heart rhythm Improvements in ambulance service and emergency room care Cardiac rehabilitation programs
Treatment of CVD • Public education and motivation campaigns • Screening • Aspirin: decreases tendency of blood to clot. Side effects can be serious! Take only if prescribed by doctor • Cardiopulmonary resuscitation (CPR) training of many individuals
 Anatomy blood vessels
Anatomy blood vessels Cardiovascular disease risk factor
Cardiovascular disease risk factor Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Bharathi viswanathan
Bharathi viswanathan What is informal email
What is informal email Unit 6 review questions
Unit 6 review questions Capillary bed labeled
Capillary bed labeled Riesgo cardiovascular por perimetro abdominal
Riesgo cardiovascular por perimetro abdominal Semiologia aparato cardiovascular
Semiologia aparato cardiovascular What makes up the cardiovascular system
What makes up the cardiovascular system Rias cardiovascular
Rias cardiovascular Rat cvs simulation
Rat cvs simulation National cardiovascular partners
National cardiovascular partners Totally tubular dude
Totally tubular dude Cardiovascular drift
Cardiovascular drift Crash course cardiovascular system
Crash course cardiovascular system Chapter 5 the cardiovascular system
Chapter 5 the cardiovascular system Chapter 46 the child with a cardiovascular alteration
Chapter 46 the child with a cardiovascular alteration Chapter 26 the child with a cardiovascular disorder
Chapter 26 the child with a cardiovascular disorder Chapter 25 assessment of cardiovascular function
Chapter 25 assessment of cardiovascular function Figure 11-9 is a diagram of the hepatic portal circulation
Figure 11-9 is a diagram of the hepatic portal circulation Figure 11-12 is a diagram of a capillary bed
Figure 11-12 is a diagram of a capillary bed Chapter 11 the cardiovascular system
Chapter 11 the cardiovascular system Lesson 11 cardiovascular system
Lesson 11 cardiovascular system American board of cardiovascular medicine
American board of cardiovascular medicine Battiti ectopici ventricolari forum
Battiti ectopici ventricolari forum Centro cardiovascular
Centro cardiovascular Tissue in cardiovascular system
Tissue in cardiovascular system Generalidades del sistema cardiovascular
Generalidades del sistema cardiovascular Cardiovascular research institute basel
Cardiovascular research institute basel Introduction to cardiovascular system
Introduction to cardiovascular system 5 components of health related fitness
5 components of health related fitness Stent placement
Stent placement Salud cardiovascular
Salud cardiovascular Grade 7 physical fitness
Grade 7 physical fitness Salud cardiovascular
Salud cardiovascular Estratificacion de riesgo cardiovascular acsm
Estratificacion de riesgo cardiovascular acsm Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Chapter 7 cardiovascular fitness
Chapter 7 cardiovascular fitness Chapter 16 cardiovascular emergencies
Chapter 16 cardiovascular emergencies Chapter 13 cardiovascular system
Chapter 13 cardiovascular system