Aortic Infection Osler used the term mycotic aneurysm






















- Slides: 69

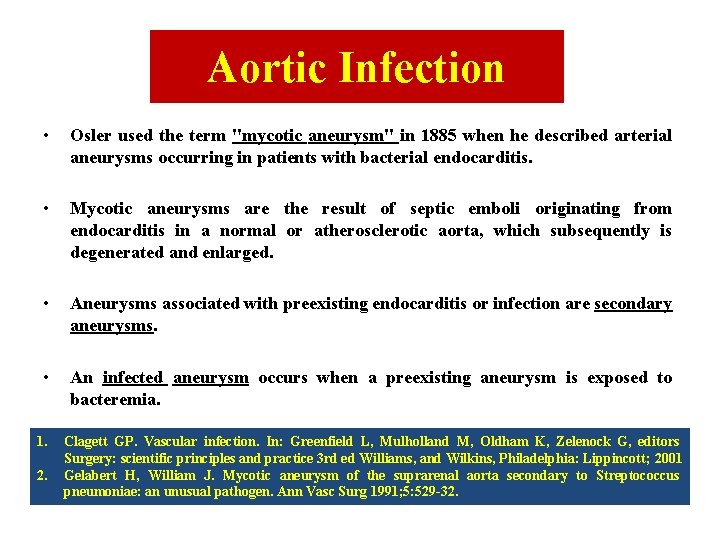
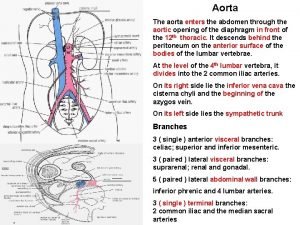
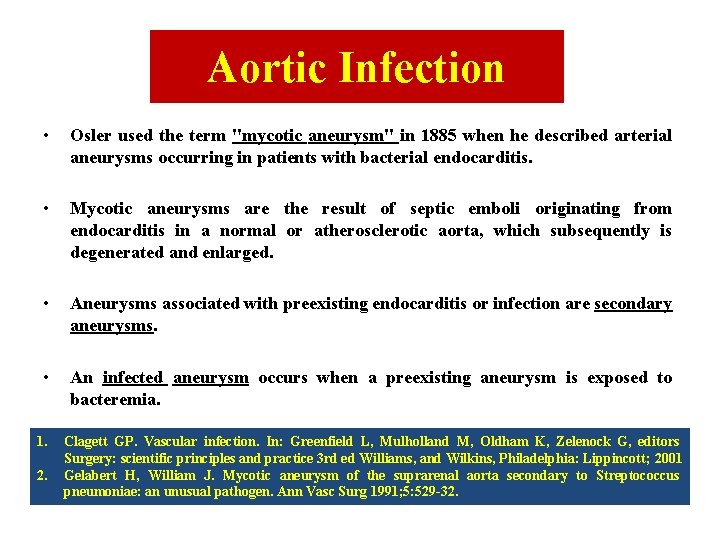
Aortic Infection • Osler used the term "mycotic aneurysm" in 1885 when he described arterial aneurysms occurring in patients with bacterial endocarditis. • Mycotic aneurysms are the result of septic emboli originating from endocarditis in a normal or atherosclerotic aorta, which subsequently is degenerated and enlarged. • Aneurysms associated with preexisting endocarditis or infection are secondary aneurysms. • An infected aneurysm occurs when a preexisting aneurysm is exposed to bacteremia. 1. Clagett GP. Vascular infection. In: Greenfield L, Mulholland M, Oldham K, Zelenock G, editors Surgery: scientific principles and practice 3 rd ed Williams, and Wilkins, Philadelphia: Lippincott; 2001 Gelabert H, William J. Mycotic aneurysm of the suprarenal aorta secondary to Streptococcus pneumoniae: an unusual pathogen. Ann Vasc Surg 1991; 5: 529 -32.



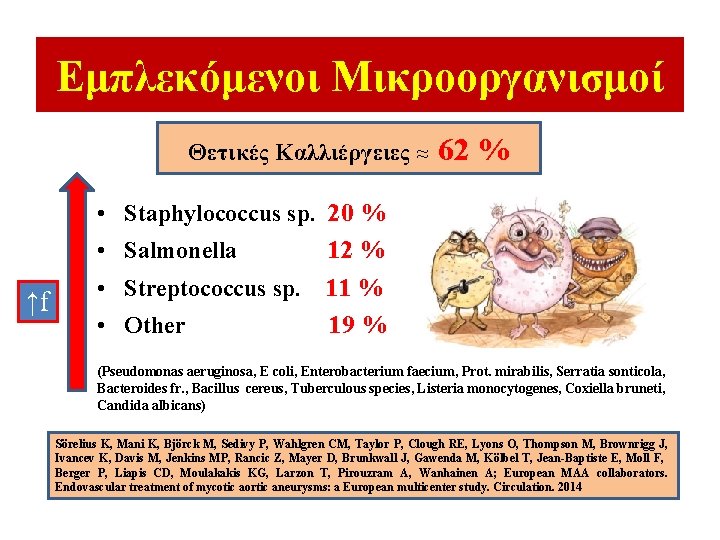
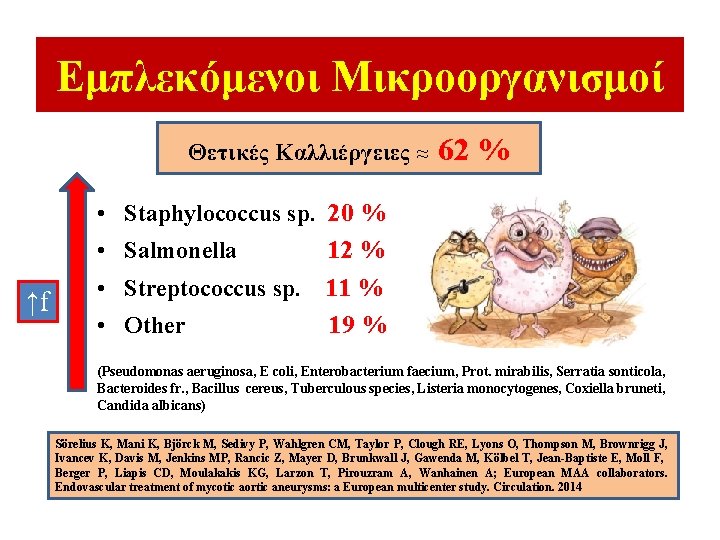
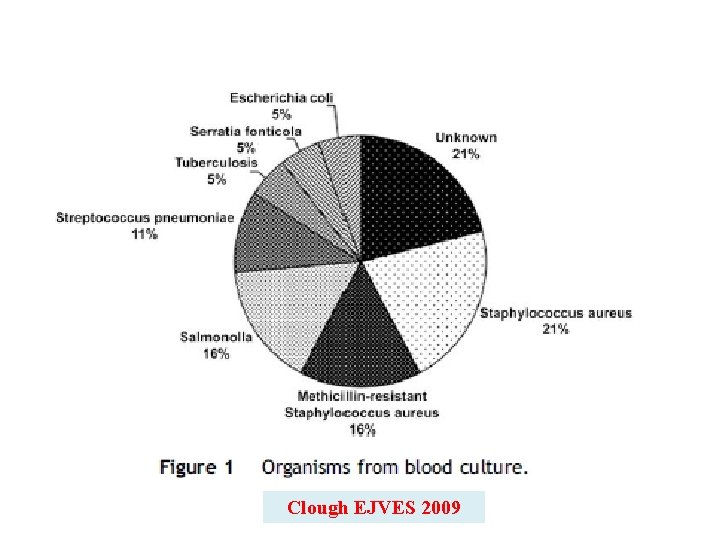
Εμπλεκόμενοι Μικροοργανισμοί Θετικές Καλλιέργειες ≈ 62 % • Staphylococcus sp. 20 % • Salmonella 12 % ↑f • Streptococcus sp. 11 % • Other 19 % (Pseudomonas aeruginosa, E coli, Enterobacterium faecium, Prot. mirabilis, Serratia sonticola, Bacteroides fr. , Bacillus cereus, Tuberculous species, Listeria monocytogenes, Coxiella bruneti, Candida albicans) Sörelius K, Mani K, Björck M, Sedivy P, Wahlgren CM, Taylor P, Clough RE, Lyons O, Thompson M, Brownrigg J, Ivancev K, Davis M, Jenkins MP, Rancic Z, Mayer D, Brunkwall J, Gawenda M, Kölbel T, Jean-Baptiste E, Moll F, Berger P, Liapis CD, Moulakakis KG, Larzon T, Pirouzram A, Wanhainen A; European MAA collaborators. Endovascular treatment of mycotic aortic aneurysms: a European multicenter study. Circulation. 2014
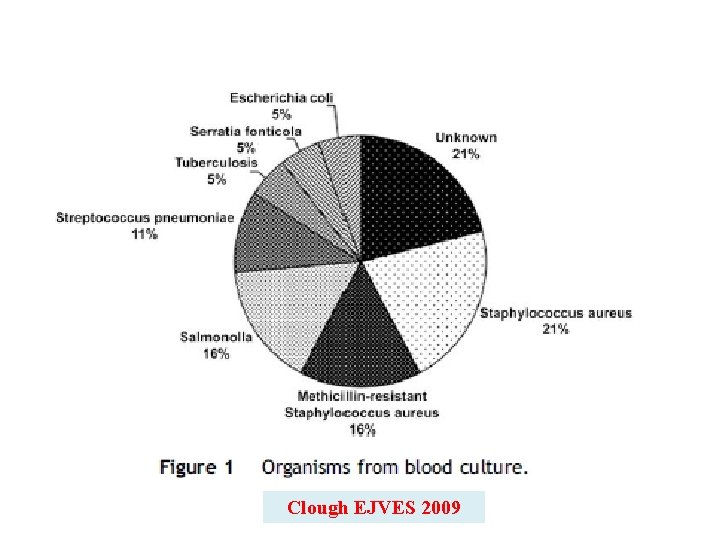
Clough EJVES 2009
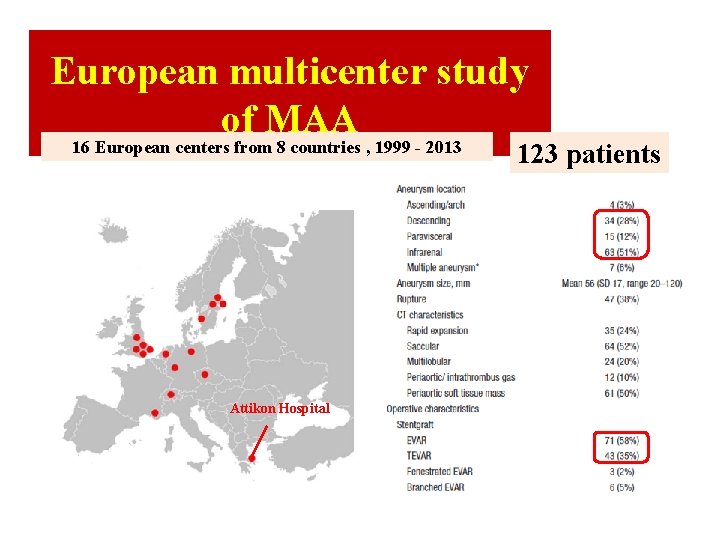
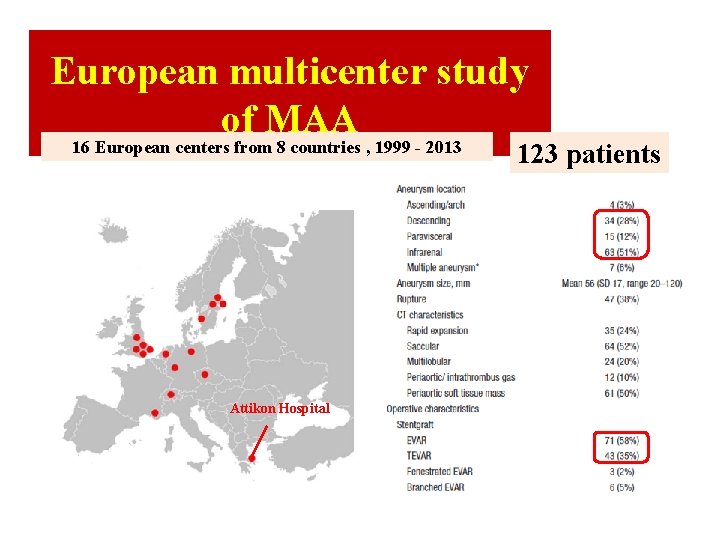
European multicenter study of MAA 16 European centers from 8 countries , 1999 - 2013 Attikon Hospital 123 patients
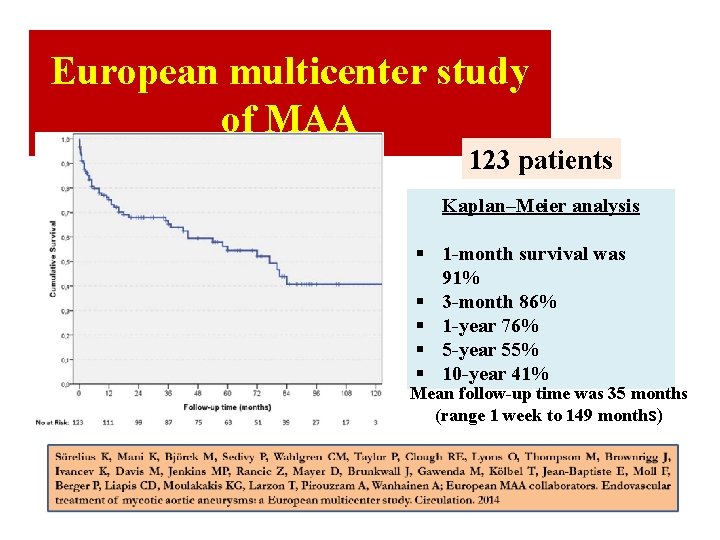
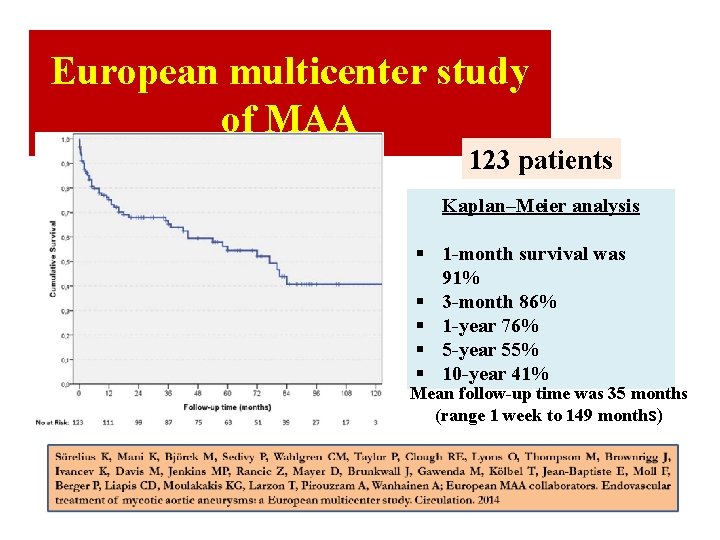
European multicenter study of MAA 123 patients Kaplan–Meier analysis § 1 -month survival was 91% § 3 -month 86% § 1 -year 76% § 5 -year 55% § 10 -year 41% Mean follow-up time was 35 months (range 1 week to 149 months)
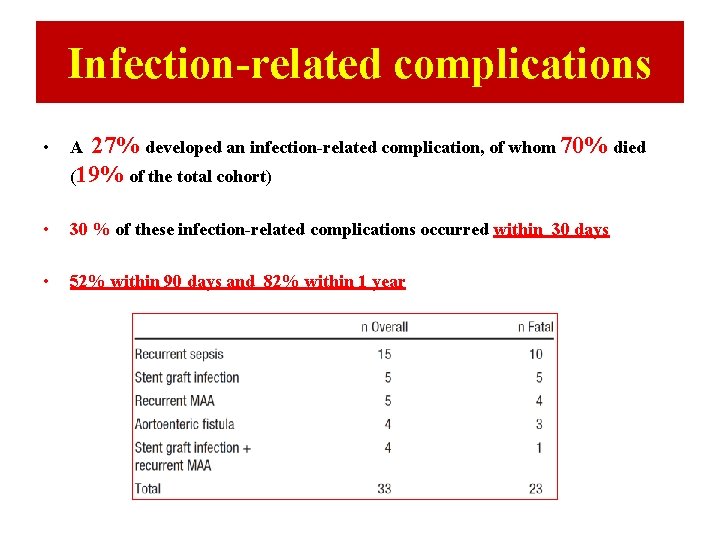
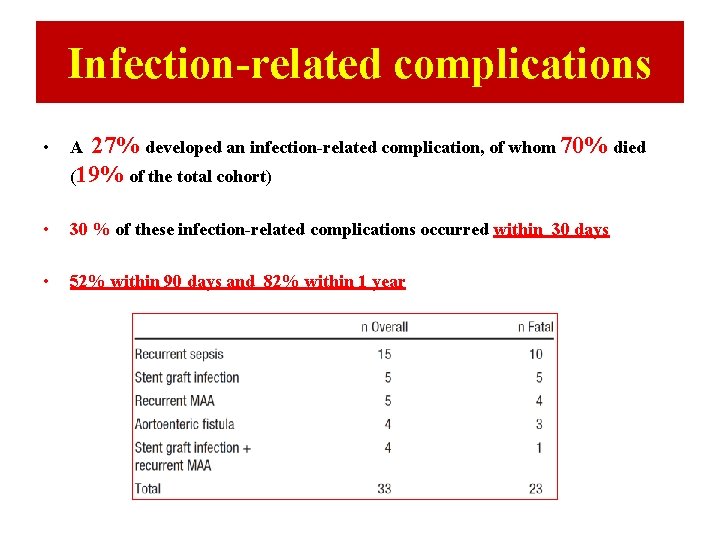
Infection-related complications • A 27% developed an infection-related complication, of whom 70% died (19% of the total cohort) • 30 % of these infection-related complications occurred within 30 days • 52% within 90 days and 82% within 1 year
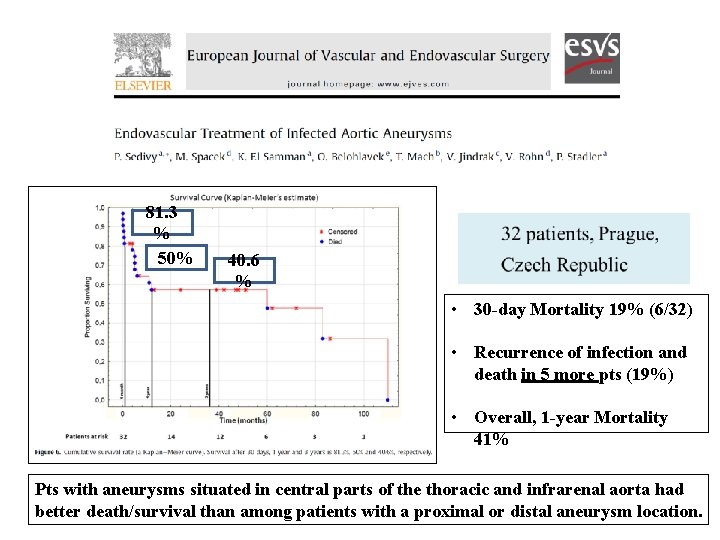
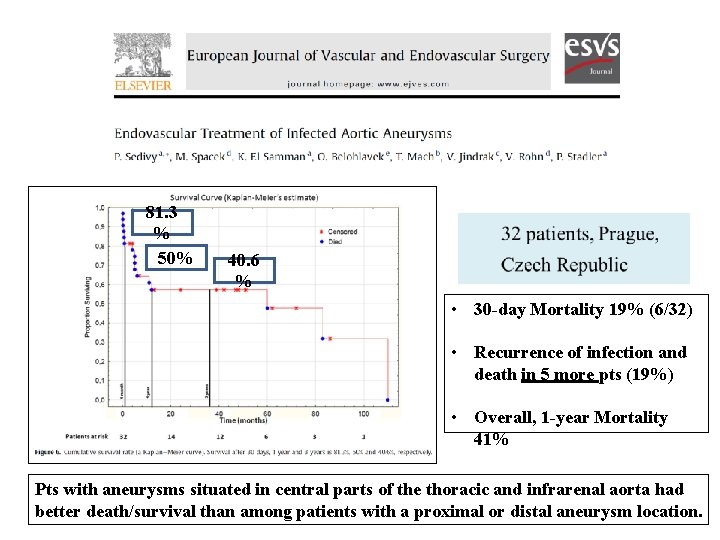
81. 3 % 50% 40. 6 % • 30 -day Mortality 19% (6/32) • Recurrence of infection and death in 5 more pts (19%) • Overall, 1 -year Mortality 41% Pts with aneurysms situated in central parts of the thoracic and infrarenal aorta had better death/survival than among patients with a proximal or distal aneurysm location.
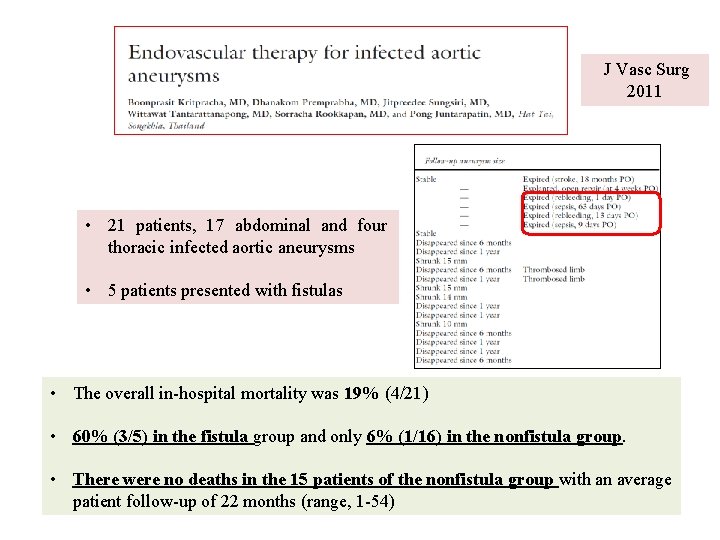
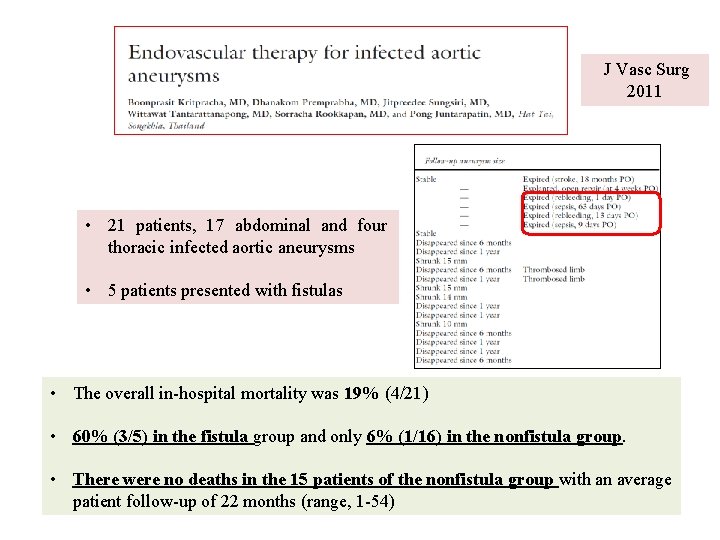
J Vasc Surg 2011 • 21 patients, 17 abdominal and four thoracic infected aortic aneurysms • 5 patients presented with fistulas • The overall in-hospital mortality was 19% (4/21) • 60% (3/5) in the fistula group and only 6% (1/16) in the nonfistula group. • There were no deaths in the 15 patients of the nonfistula group with an average patient follow-up of 22 months (range, 1 -54)
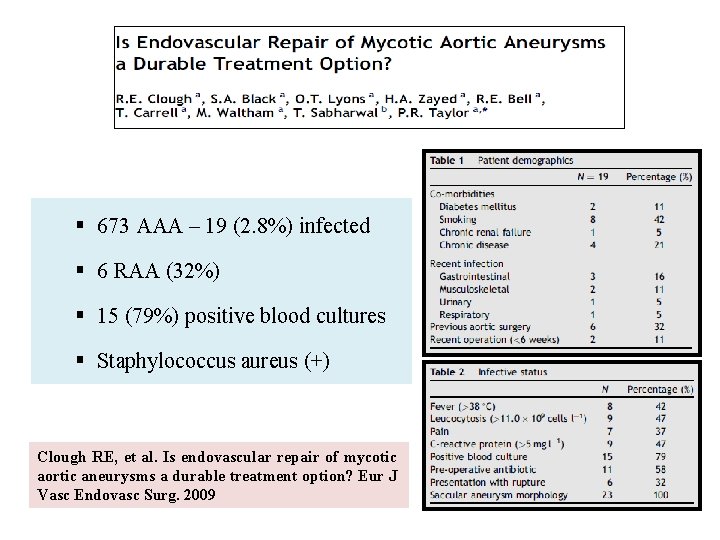
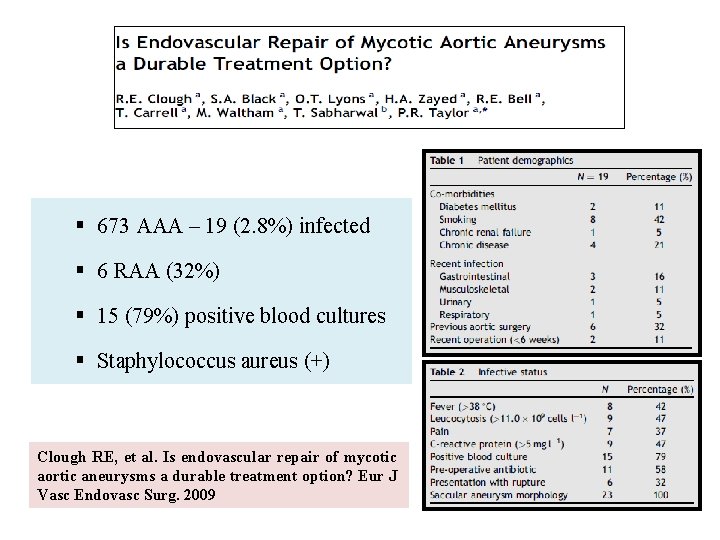
§ 673 AAA – 19 (2. 8%) infected § 6 RAA (32%) § 15 (79%) positive blood cultures § Staphylococcus aureus (+) Clough RE, et al. Is endovascular repair of mycotic aortic aneurysms a durable treatment option? Eur J Vasc Endovasc Surg. 2009
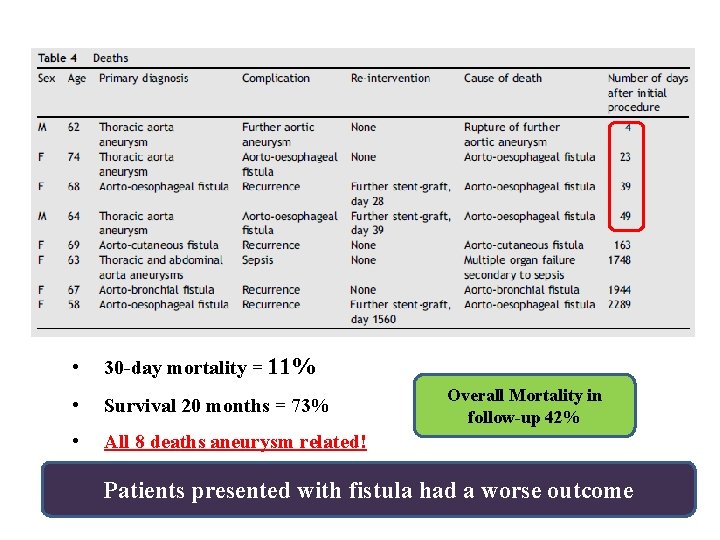
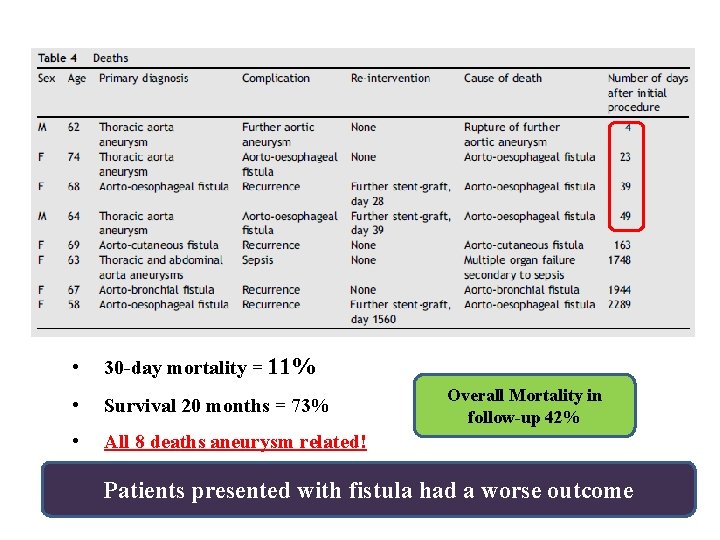
• 30 -day mortality = 11% • Survival 20 months = 73% Overall Mortality in follow-up 42% • All 8 deaths aneurysm related! Patients presented with fistula had a worse outcome
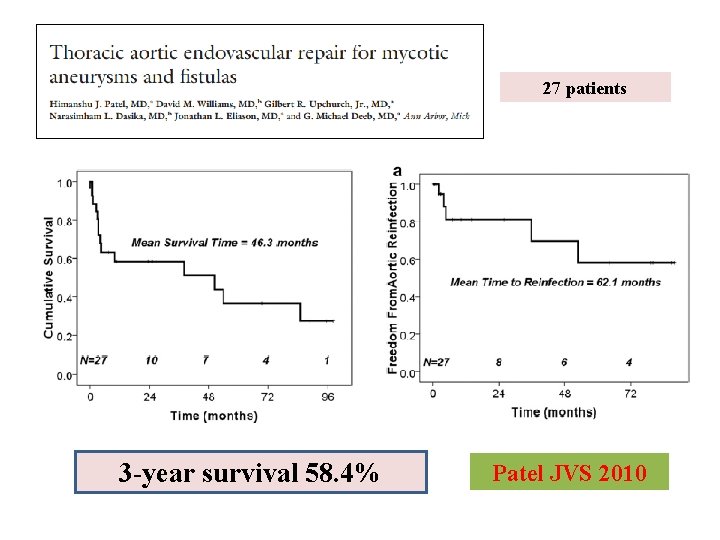
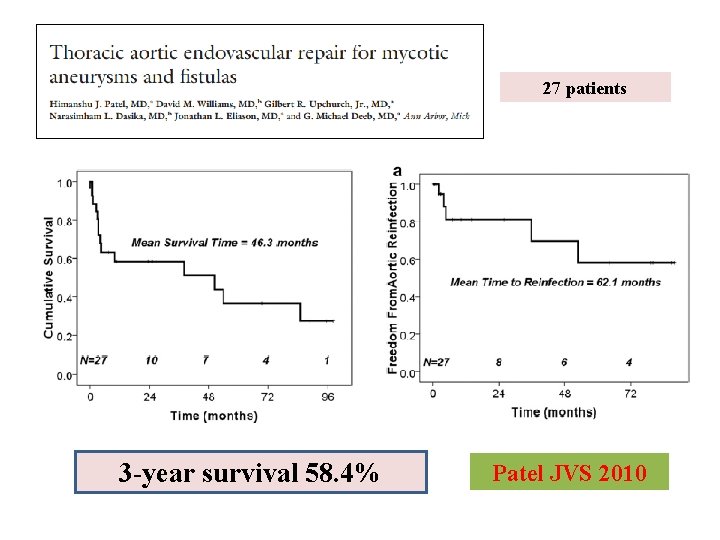
27 patients 3 -year survival 58. 4% Patel JVS 2010
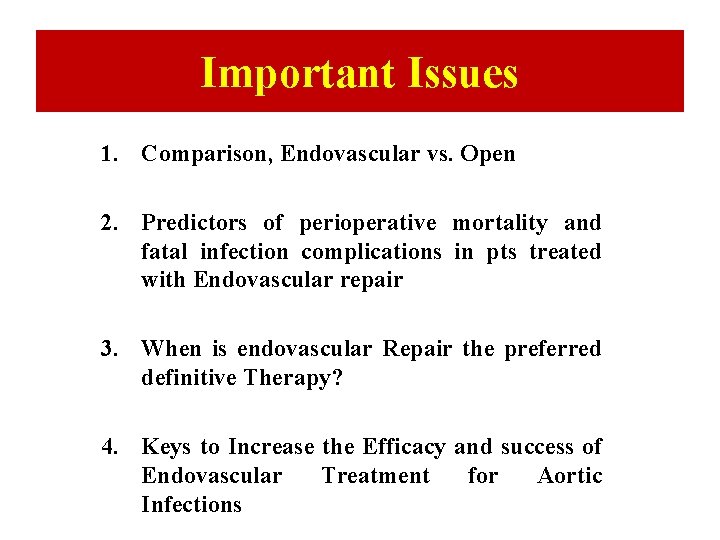
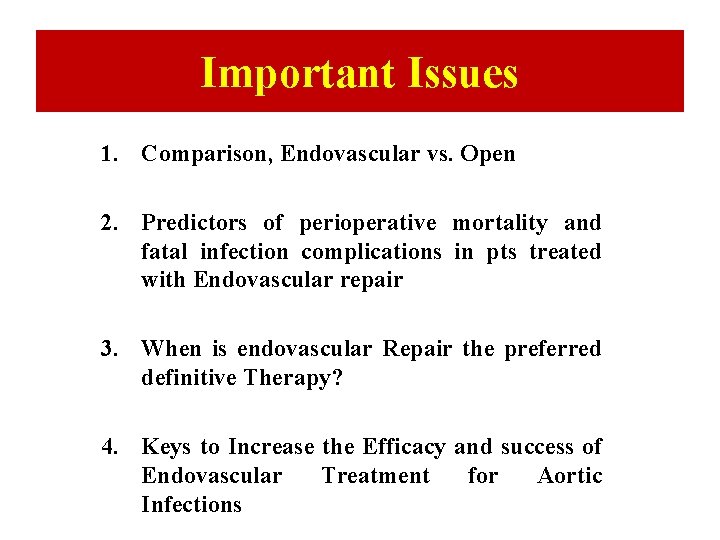
Important Issues 1. Comparison, Endovascular vs. Open 2. Predictors of perioperative mortality and fatal infection complications in pts treated with Endovascular repair 3. When is endovascular Repair the preferred definitive Therapy? 4. Keys to Increase the Efficacy and success of Endovascular Treatment for Aortic Infections
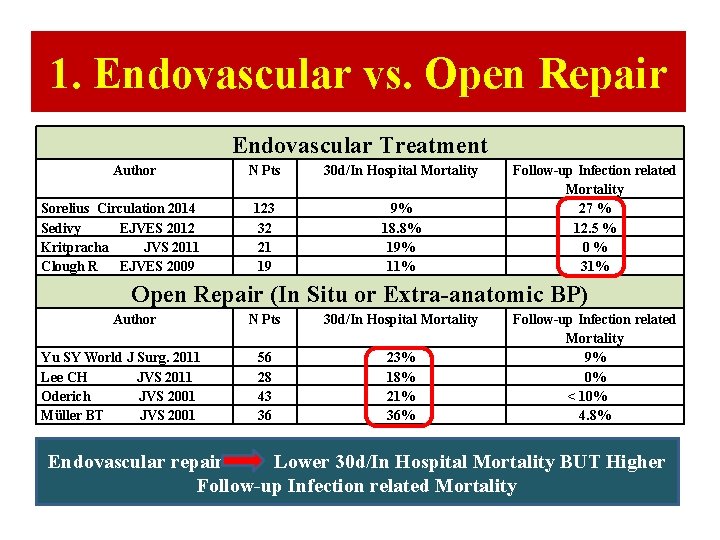
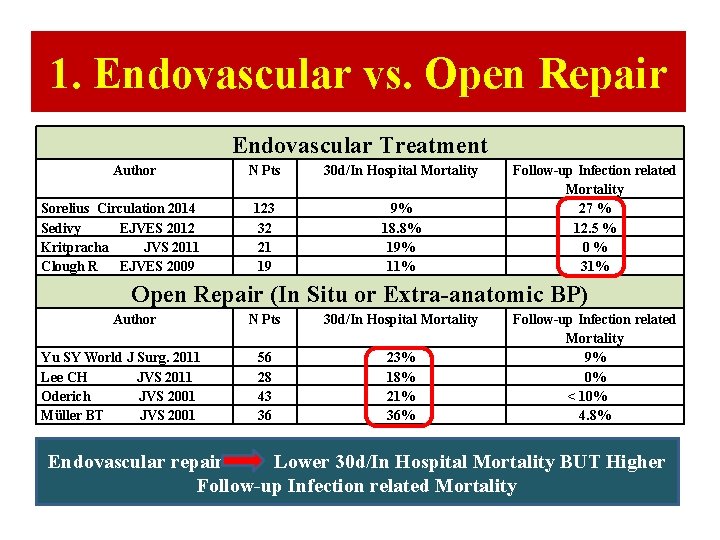
1. Endovascular vs. Open Repair Endovascular Treatment Author Sorelius Circulation 2014 Sedivy EJVES 2012 Kritpracha JVS 2011 Clough R EJVES 2009 N Pts 30 d/In Hospital Mortality 123 32 21 19 9% 18. 8% 19% 11% Follow-up Infection related Mortality 27 % 12. 5 % 0 % 31% Open Repair (In Situ or Extra-anatomic BP) Author Yu SY World J Surg. 2011 Lee CH JVS 2011 Oderich JVS 2001 Müller BT JVS 2001 N Pts 30 d/In Hospital Mortality 56 28 43 36 23% 18% 21% 36% Follow-up Infection related Mortality 9% 0% < 10% 4. 8% Endovascular repair Lower 30 d/In Hospital Mortality BUT Higher Follow-up Infection related Mortality
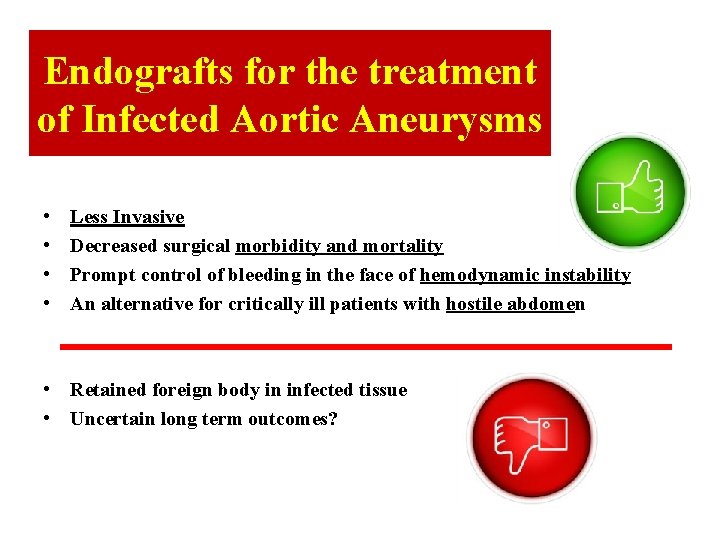
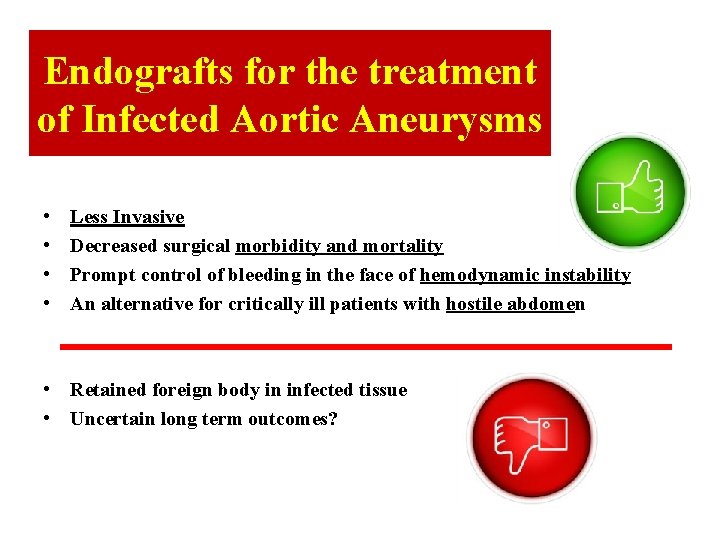
Endografts for the treatment of Infected Aortic Aneurysms • • Less Invasive Decreased surgical morbidity and mortality Prompt control of bleeding in the face of hemodynamic instability An alternative for critically ill patients with hostile abdomen • Retained foreign body in infected tissue • Uncertain long term outcomes?
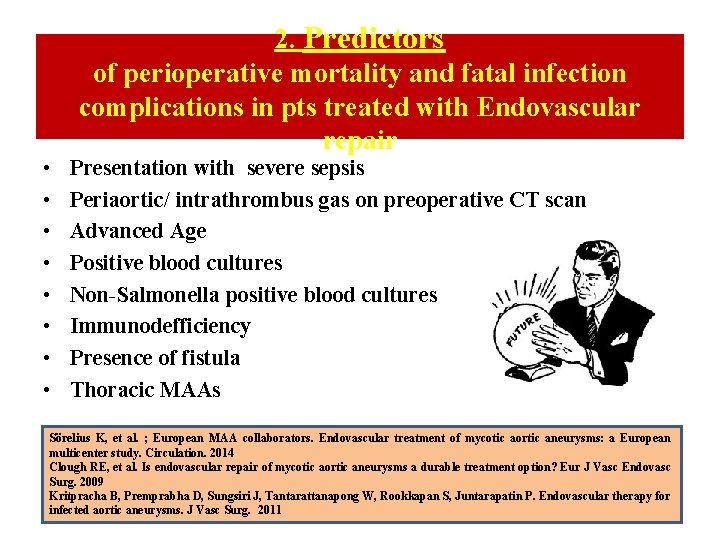
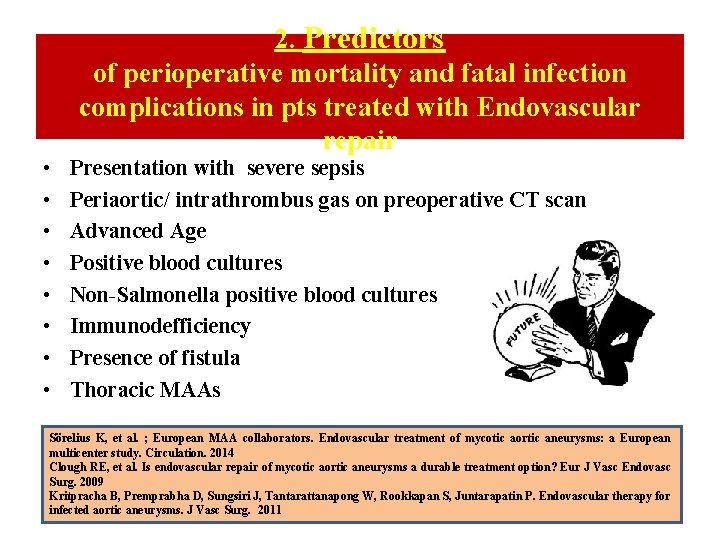
• • 2. Predictors of perioperative mortality and fatal infection complications in pts treated with Endovascular repair Presentation with severe sepsis Periaortic/ intrathrombus gas on preoperative CT scan Advanced Age Positive blood cultures Non-Salmonella positive blood cultures Immunodefficiency Presence of fistula Thoracic MAAs Sörelius K, et al. ; European MAA collaborators. Endovascular treatment of mycotic aortic aneurysms: a European multicenter study. Circulation. 2014 Clough RE, et al. Is endovascular repair of mycotic aortic aneurysms a durable treatment option? Eur J Vasc Endovasc Surg. 2009 Kritpracha B, Premprabha D, Sungsiri J, Tantarattanapong W, Rookkapan S, Juntarapatin P. Endovascular therapy for infected aortic aneurysms. J Vasc Surg. 2011
3. When is endovascular Repair the preferred definitive Therapy? • Good response to preoperative antibiotic therapy • Absence of severe sepsis on presentation • Absence of Periaortic gas on preoperative CT scan, limited purulence or less virulent infection • Absence of fistula on presentation
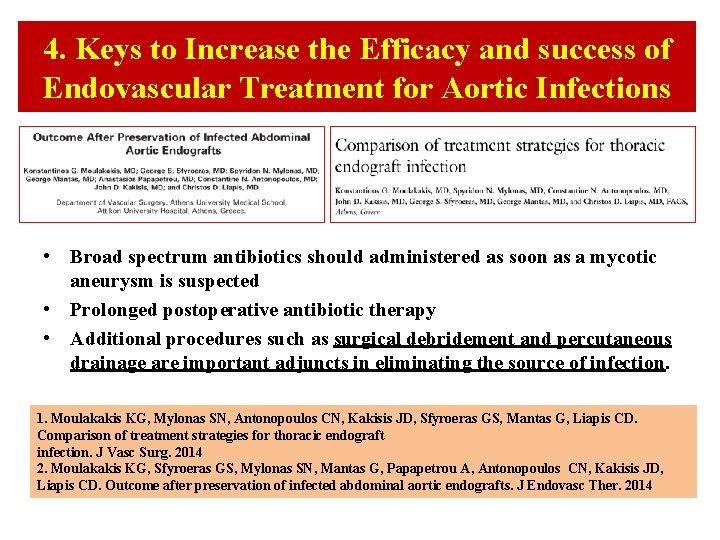
4. Keys to Increase the Efficacy and success of Endovascular Treatment for Aortic Infections • Broad spectrum antibiotics should administered as soon as a mycotic aneurysm is suspected • Prolonged postoperative antibiotic therapy • Additional procedures such as surgical debridement and percutaneous drainage are important adjuncts in eliminating the source of infection. 1. Moulakakis KG, Mylonas SN, Antonopoulos CN, Kakisis JD, Sfyroeras GS, Mantas G, Liapis CD. Comparison of treatment strategies for thoracic endograft infection. J Vasc Surg. 2014 2. Moulakakis KG, Sfyroeras GS, Mylonas SN, Mantas G, Papapetrou A, Antonopoulos CN, Kakisis JD, Liapis CD. Outcome after preservation of infected abdominal aortic endografts. J Endovasc Ther. 2014
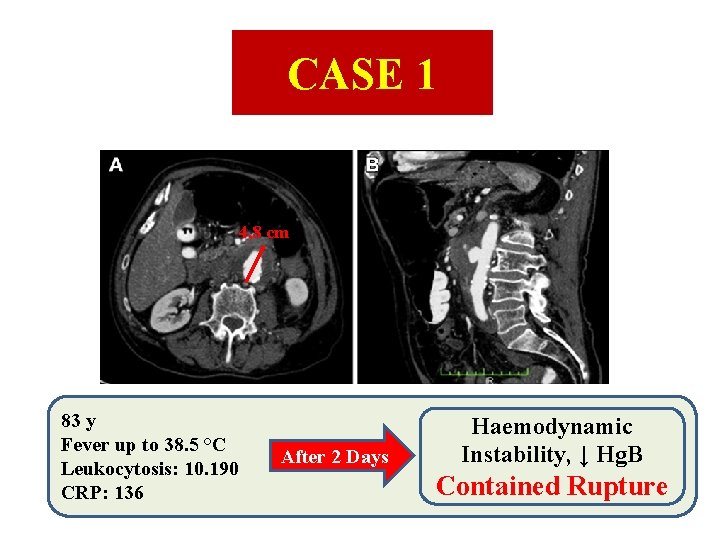
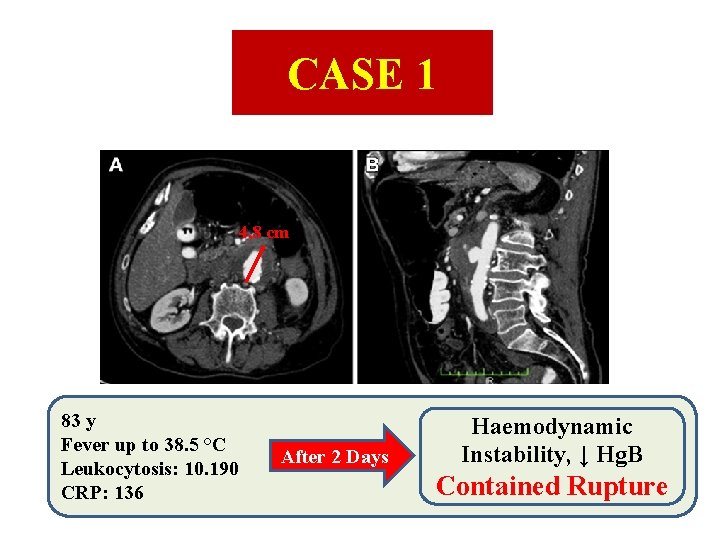
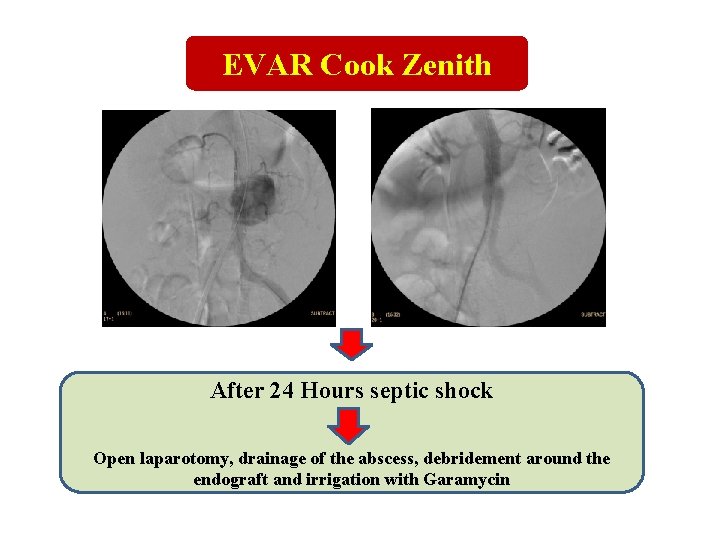
CASE 1 4, 8 cm 83 y Fever up to 38. 5 °C Leukocytosis: 10. 190 CRP: 136 After 2 Days Haemodynamic Instability, ↓ Hg. B Contained Rupture
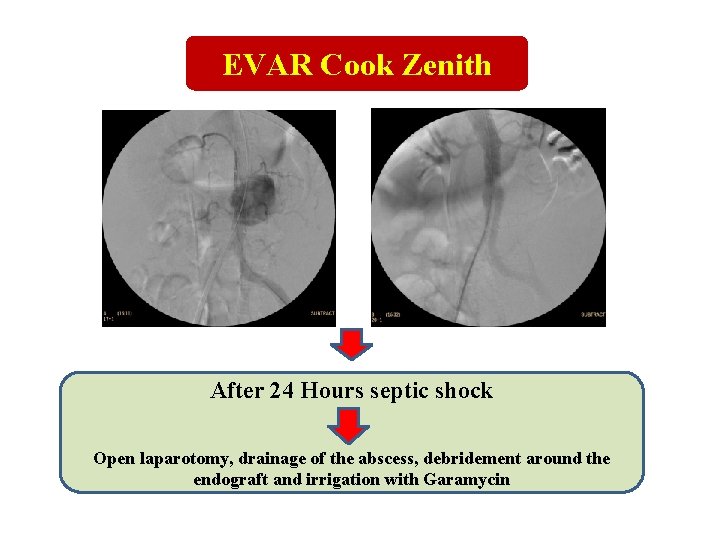
EVAR Cook Zenith After 24 Hours septic shock Open laparotomy, drainage of the abscess, debridement around the endograft and irrigation with Garamycin
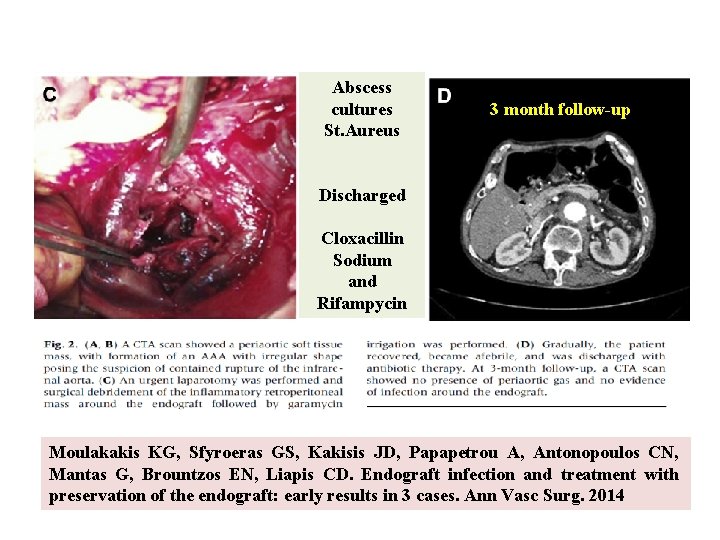
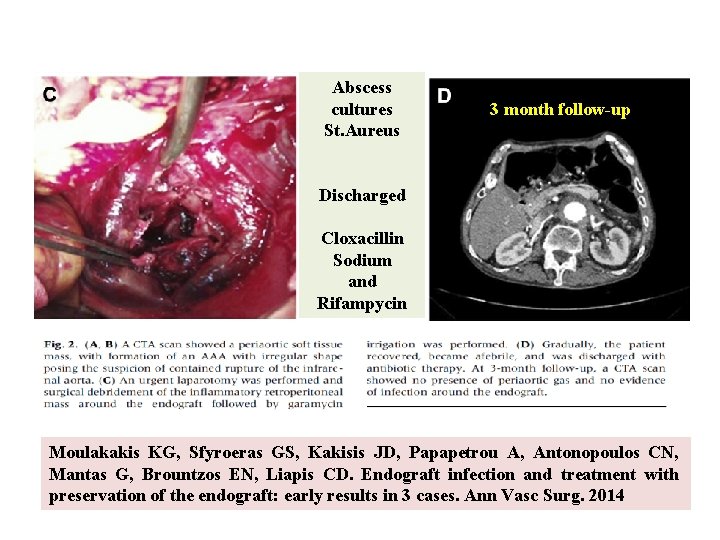
Abscess cultures St. Aureus 3 month follow-up Discharged Cloxacillin Sodium and Rifampycin Moulakakis KG, Sfyroeras GS, Kakisis JD, Papapetrou A, Antonopoulos CN, Mantas G, Brountzos EN, Liapis CD. Endograft infection and treatment with preservation of the endograft: early results in 3 cases. Ann Vasc Surg. 2014
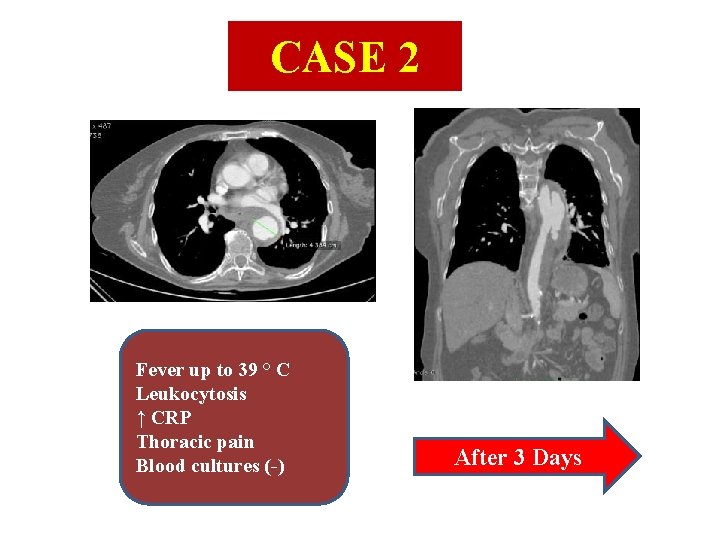
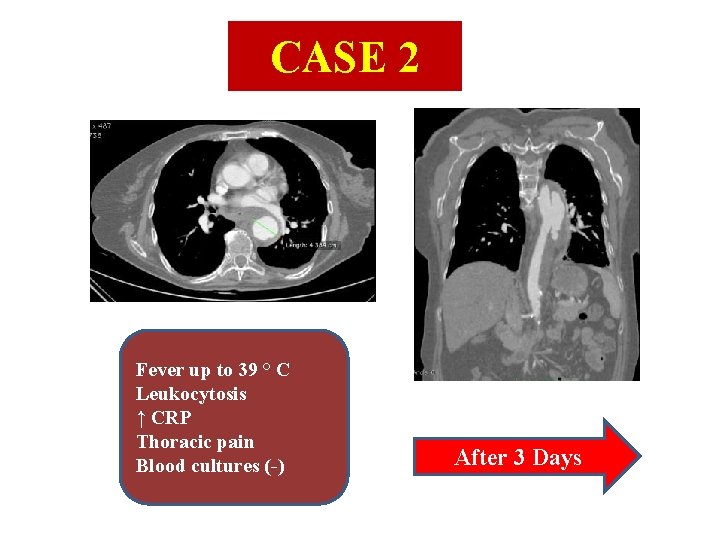
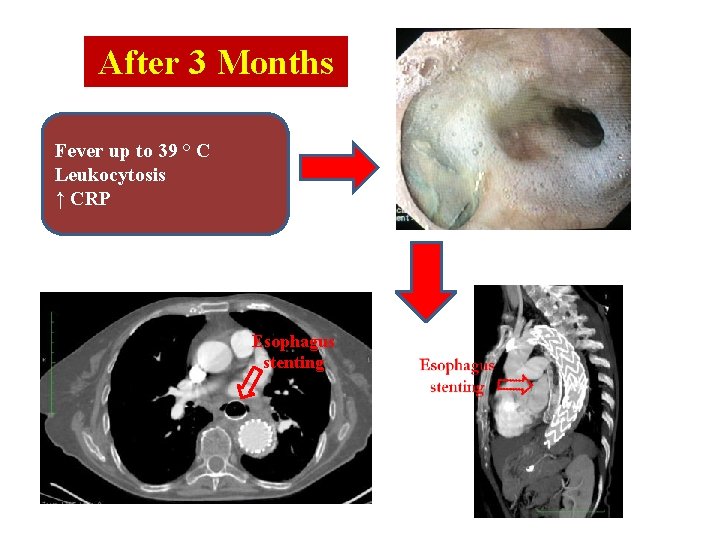
CASE 2 Fever up to 39 ° C Leukocytosis ↑ CRP Thoracic pain Blood cultures (-) After 3 Days
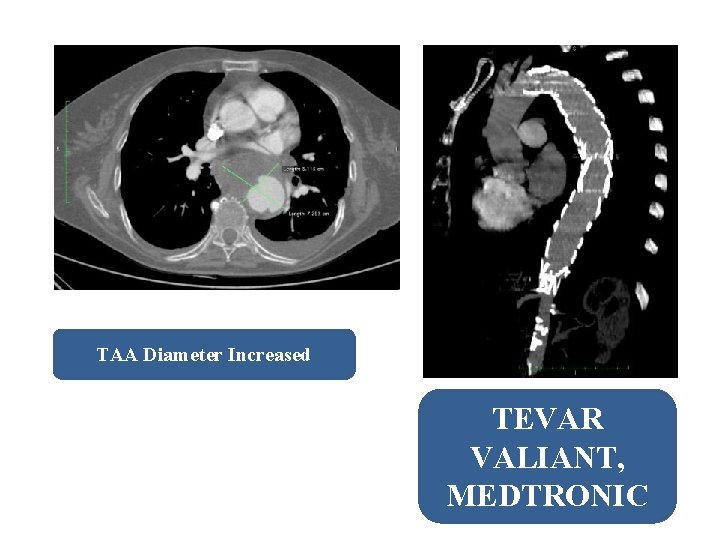
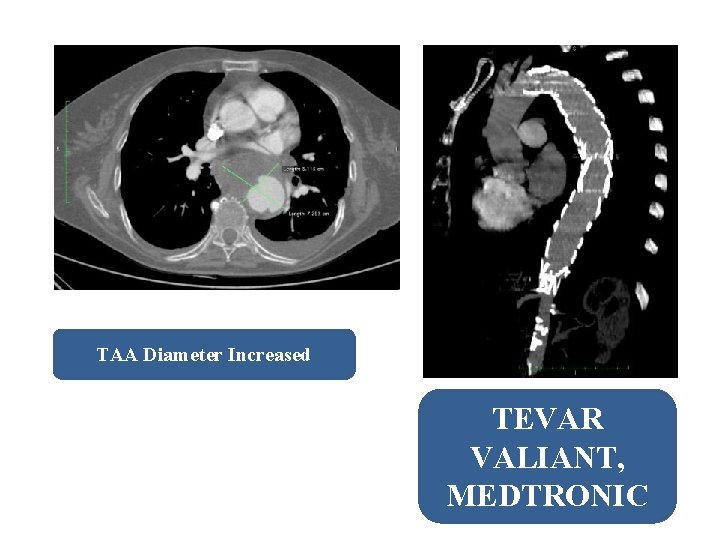
TAA Diameter Increased TEVAR VALIANT, MEDTRONIC
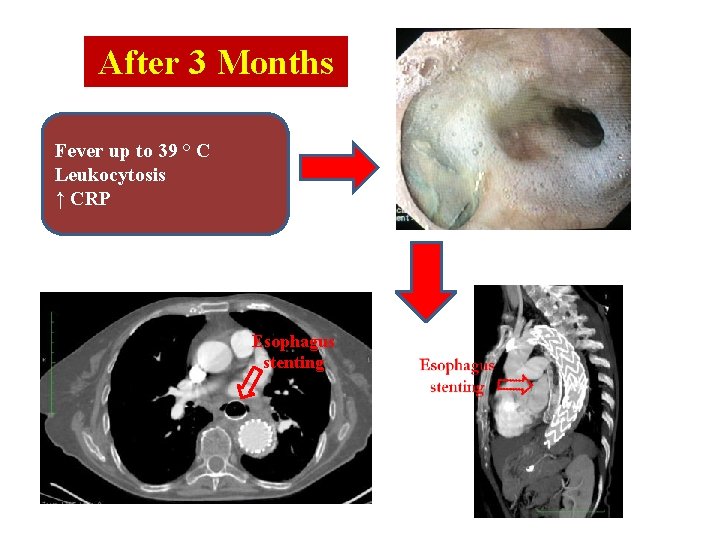
After 3 Months Fever up to 39 ° C Leukocytosis ↑ CRP Esophagus stenting

Esophagectomy and Gastric pull Discharged Cloxacillin Sodium and Rifampycin
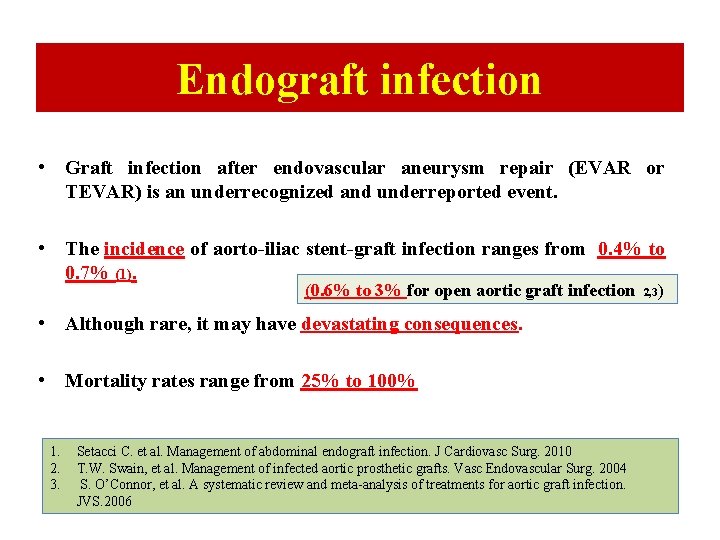
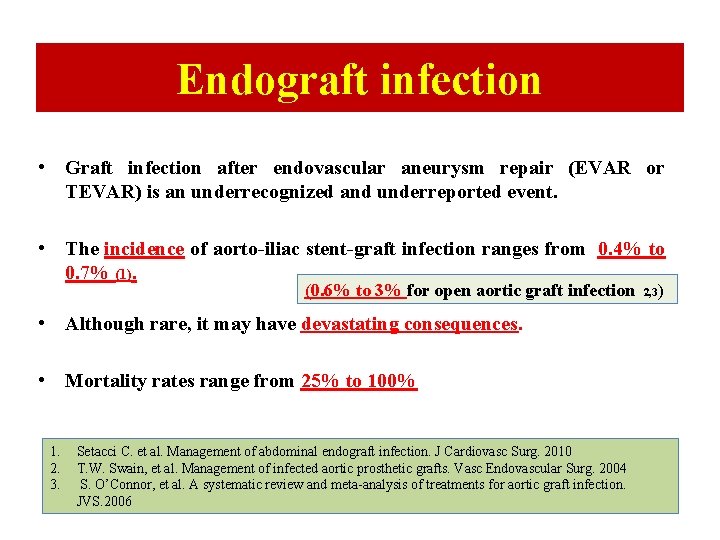
Endograft infection • Graft infection after endovascular aneurysm repair (EVAR or TEVAR) is an underrecognized and underreported event. • The incidence of aorto-iliac stent-graft infection ranges from 0. 4% to 0. 7% (1). (0. 6% to 3% for open aortic graft infection 2, 3) • Although rare, it may have devastating consequences. • Mortality rates range from 25% to 100% 1. 2. 3. Setacci C. et al. Management of abdominal endograft infection. J Cardiovasc Surg. 2010 T. W. Swain, et al. Management of infected aortic prosthetic grafts. Vasc Endovascular Surg. 2004 S. O’Connor, et al. A systematic review and meta-analysis of treatments for aortic graft infection. JVS. 2006
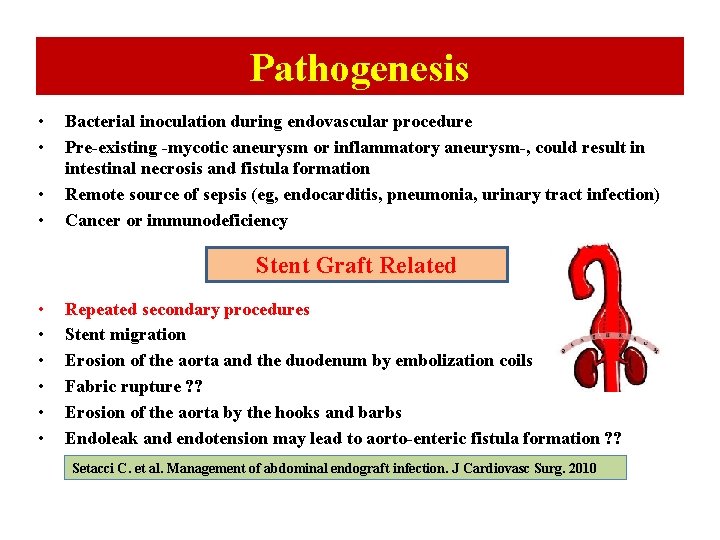
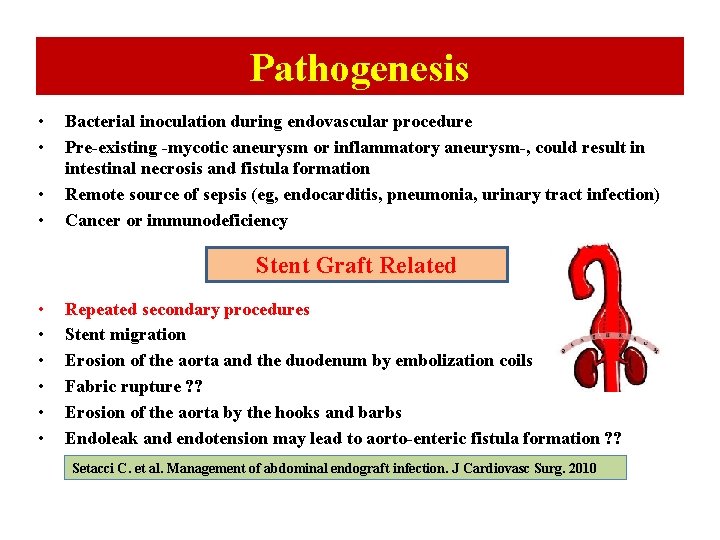
Pathogenesis • • Bacterial inoculation during endovascular procedure Pre-existing -mycotic aneurysm or inflammatory aneurysm-, could result in intestinal necrosis and fistula formation Remote source of sepsis (eg, endocarditis, pneumonia, urinary tract infection) Cancer or immunodeficiency Stent Graft Related • • • Repeated secondary procedures Stent migration Erosion of the aorta and the duodenum by embolization coils Fabric rupture ? ? Erosion of the aorta by the hooks and barbs Endoleak and endotension may lead to aorto-enteric fistula formation ? ? Setacci C. et al. Management of abdominal endograft infection. J Cardiovasc Surg. 2010
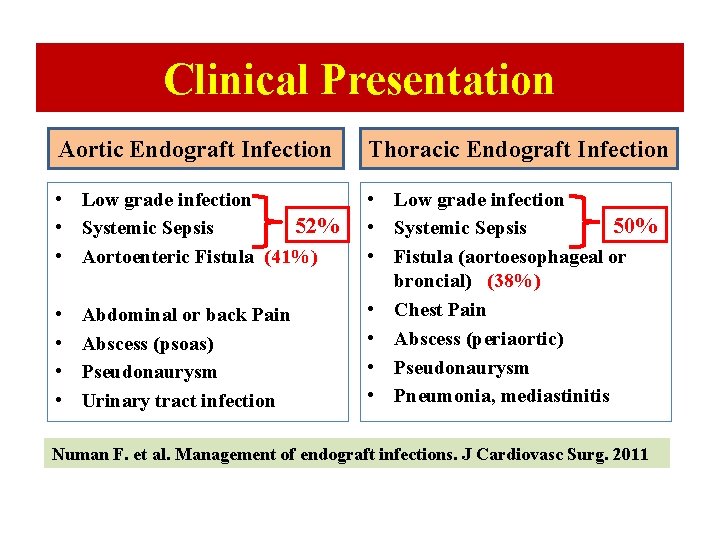
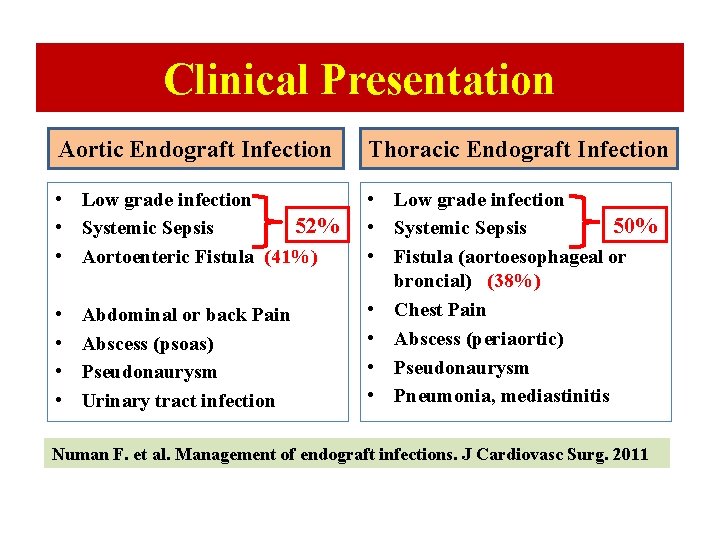
Clinical Presentation Aortic Endograft Infection Thoracic Endograft Infection • Low grade infection 52% • Systemic Sepsis • Aortoenteric Fistula (41%)% • Low grade infection 50% • Systemic Sepsis • Fistula (aortoesophageal or % broncial) (38%) • Chest Pain • Abscess (periaortic) • Pseudonaurysm • Pneumonia, mediastinitis • • Abdominal or back Pain Abscess (psoas) Pseudonaurysm Urinary tract infection Numan F. et al. Management of endograft infections. J Cardiovasc Surg. 2011
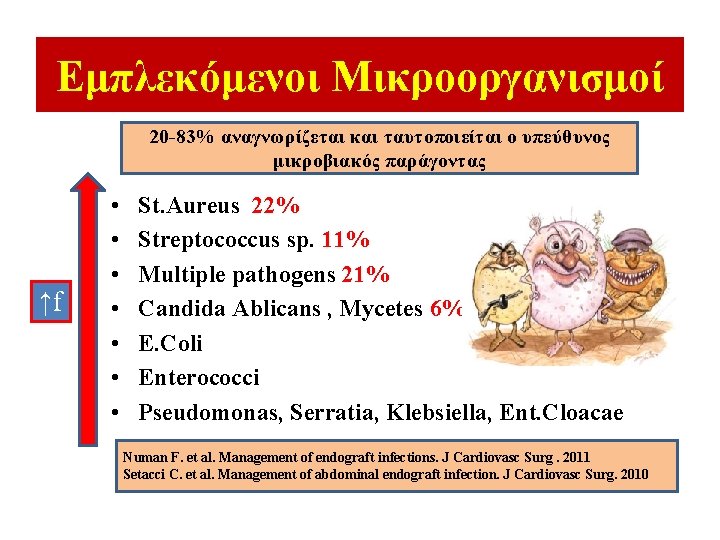
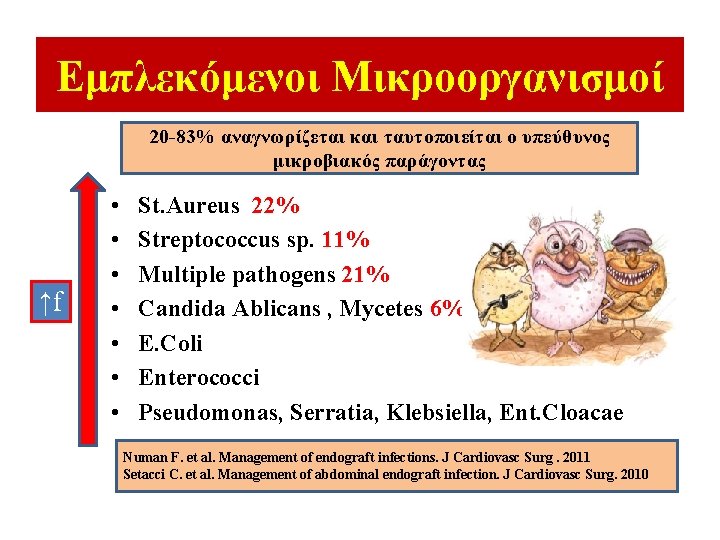
Εμπλεκόμενοι Μικροοργανισμοί 20 -83% αναγνωρίζεται και ταυτοποιείται ο υπεύθυνος μικροβιακός παράγοντας ↑f • • St. Aureus 22% Streptococcus sp. 11% Multiple pathogens 21% Candida Ablicans , Mycetes 6% E. Coli Enterococci Pseudomonas, Serratia, Klebsiella, Ent. Cloacae Numan F. et al. Management of endograft infections. J Cardiovasc Surg. 2011 Setacci C. et al. Management of abdominal endograft infection. J Cardiovasc Surg. 2010

Management of Infected Endograft Depends on : 1. 2. 3. 4. Patient’s clinical status Co-morbidities Presence of preoperative sepsis Microorganisms involved


Management of Infected Endograft Graft Excision is the GOLD STANDARD • Graft Excision & Extra-anatomic bypass • Neo-aortoiliac System Procedure • In Situ Aortic Graft Replacement (Homograft, Silver Graft) High mortality and morbidity rates, especially when undertaken in unstable, septic patients with severe comorbidities Variable results on patency and reinfection rates Fiorani P, et al. Endovascular graft infection: preliminary results of an international enquiry. JEVT 2003






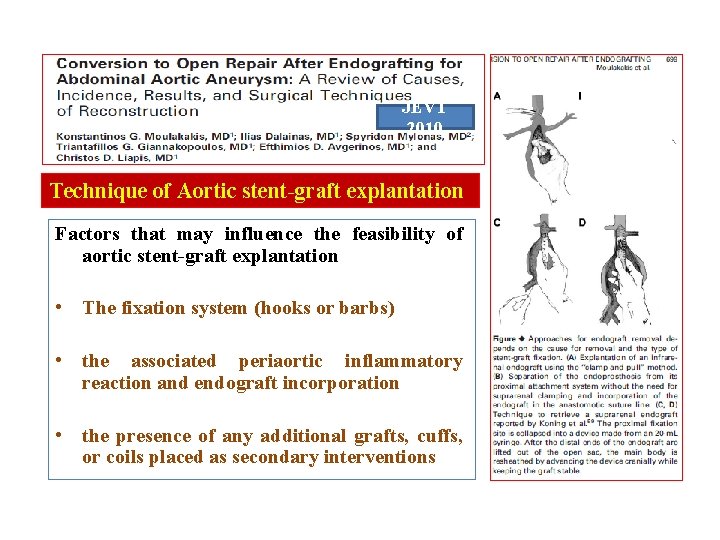
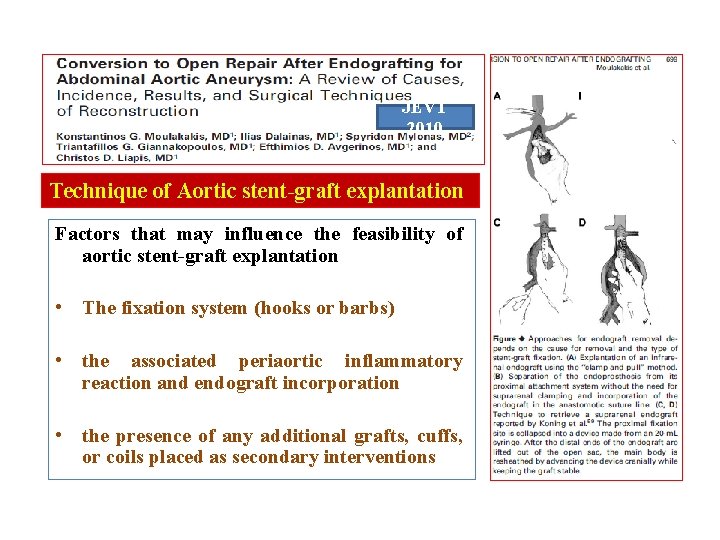
JEVT 2010 Technique of Aortic stent-graft explantation Factors that may influence the feasibility of aortic stent-graft explantation • The fixation system (hooks or barbs) • the associated periaortic inflammatory reaction and endograft incorporation • the presence of any additional grafts, cuffs, or coils placed as secondary interventions

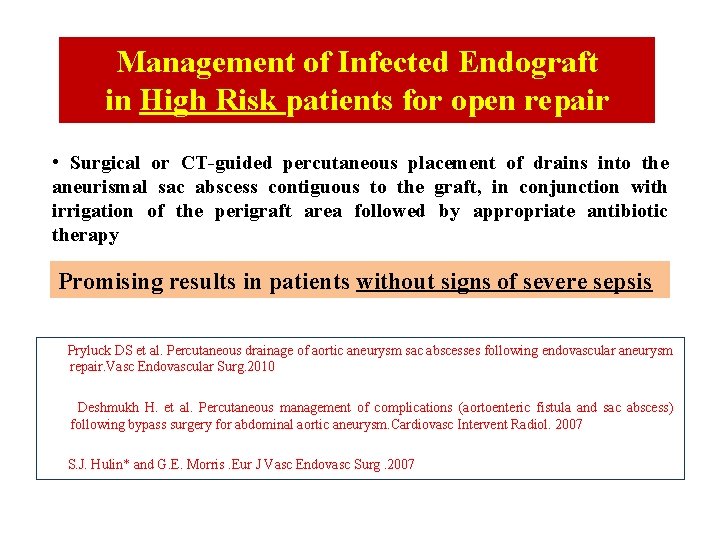
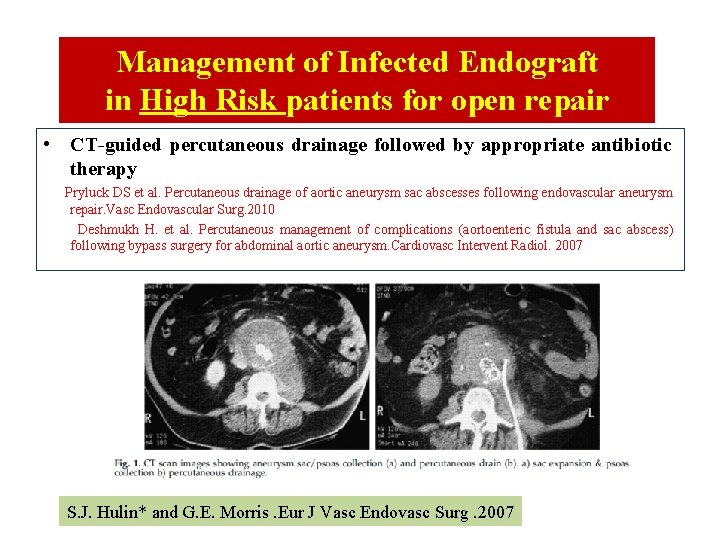
Management of Infected Endograft in High Risk patients for open repair • Surgical or CT-guided percutaneous placement of drains into the aneurismal sac abscess contiguous to the graft, in conjunction with irrigation of the perigraft area followed by appropriate antibiotic therapy Promising results in patients without signs of severe sepsis Pryluck DS et al. Percutaneous drainage of aortic aneurysm sac abscesses following endovascular aneurysm repair. Vasc Endovascular Surg. 2010 Deshmukh H. et al. Percutaneous management of complications (aortoenteric fistula and sac abscess) following bypass surgery for abdominal aortic aneurysm. Cardiovasc Intervent Radiol. 2007 S. J. Hulin* and G. E. Morris. Eur J Vasc Endovasc Surg. 2007
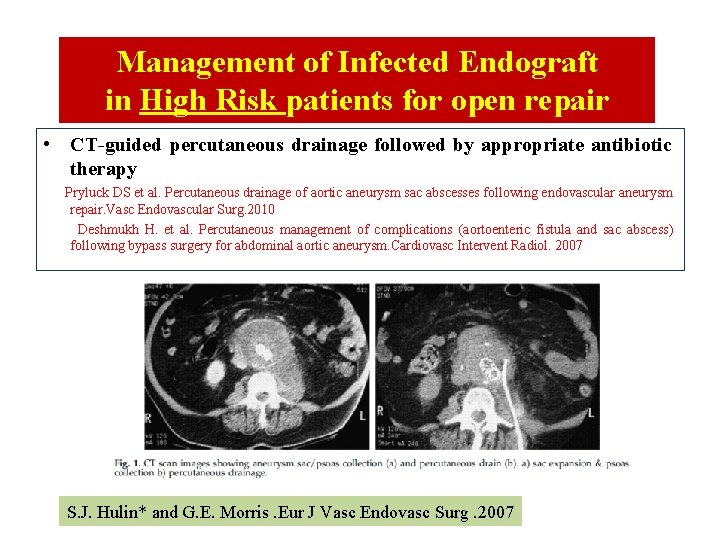
Management of Infected Endograft in High Risk patients for open repair • CT-guided percutaneous drainage followed by appropriate antibiotic therapy Pryluck DS et al. Percutaneous drainage of aortic aneurysm sac abscesses following endovascular aneurysm repair. Vasc Endovascular Surg. 2010 Deshmukh H. et al. Percutaneous management of complications (aortoenteric fistula and sac abscess) following bypass surgery for abdominal aortic aneurysm. Cardiovasc Intervent Radiol. 2007 S. J. Hulin* and G. E. Morris. Eur J Vasc Endovasc Surg. 2007
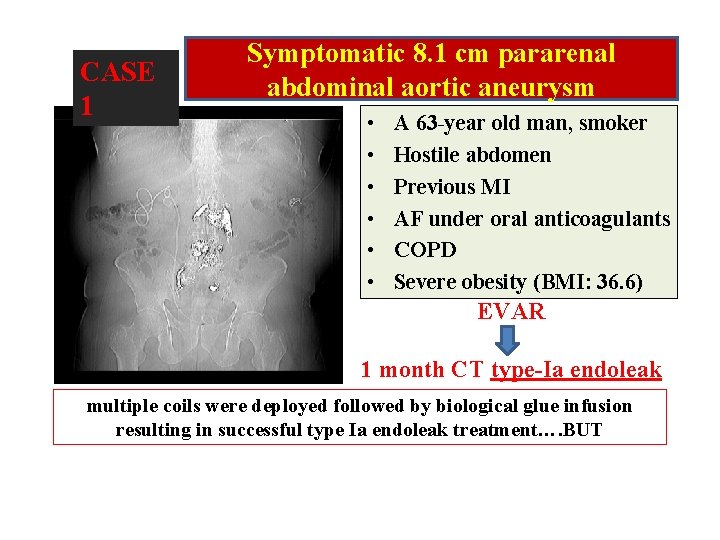
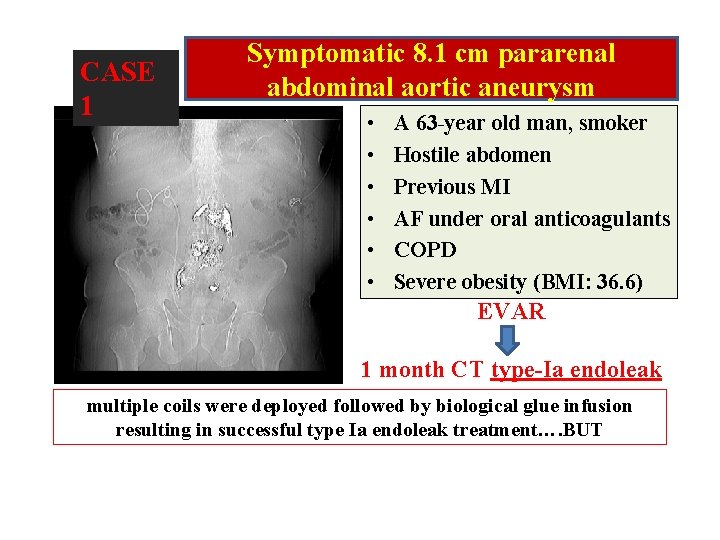
CASE 1 Symptomatic 8. 1 cm pararenal abdominal aortic aneurysm • • • A 63 -year old man, smoker Hostile abdomen Previous MI AF under oral anticoagulants COPD Severe obesity (BMI: 36. 6) EVAR 1 month CT type-Ia endoleak multiple coils were deployed followed by biological glue infusion resulting in successful type Ia endoleak treatment…. BUT
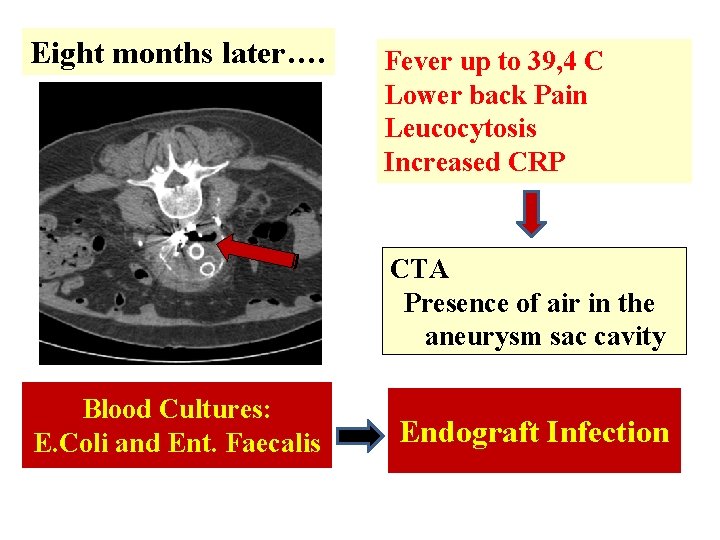
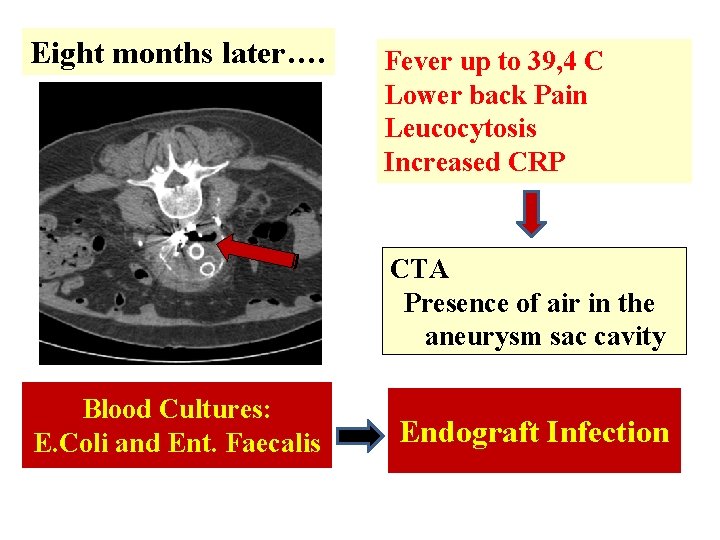
Eight months later…. Fever up to 39, 4 C Lower back Pain Leucocytosis Increased CRP CTA Presence of air in the aneurysm sac cavity Blood Cultures: E. Coli and Ent. Faecalis Endograft Infection
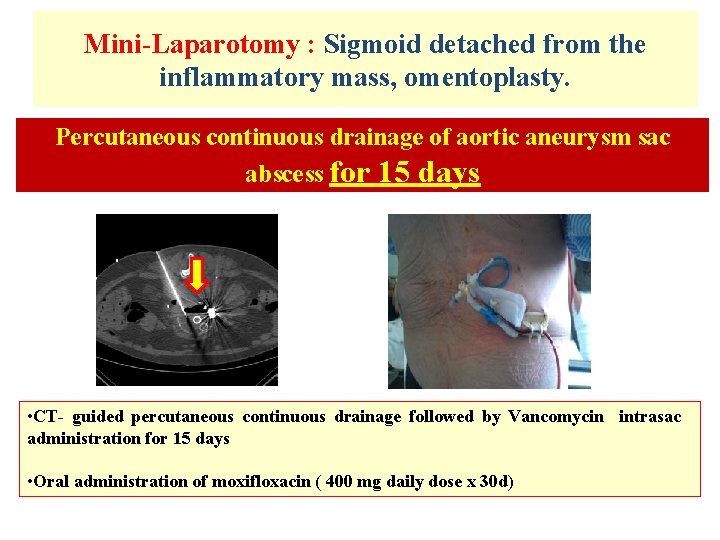
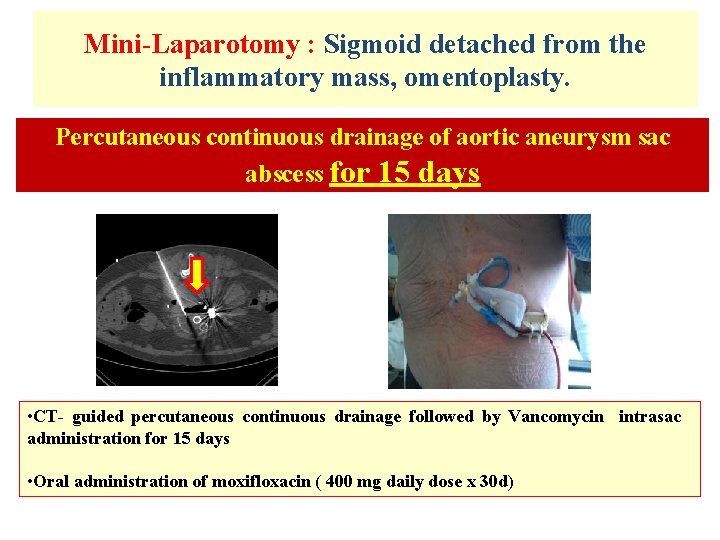
Mini-Laparotomy : Sigmoid detached from the inflammatory mass, omentoplasty. Percutaneous continuous drainage of aortic aneurysm sac abscess for 15 days • CT- guided percutaneous continuous drainage followed by Vancomycin intrasac administration for 15 days • Oral administration of moxifloxacin ( 400 mg daily dose x 30 d)
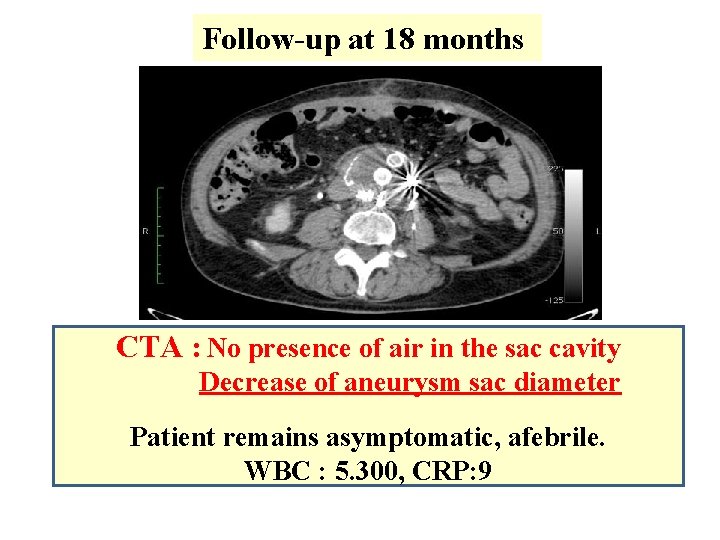
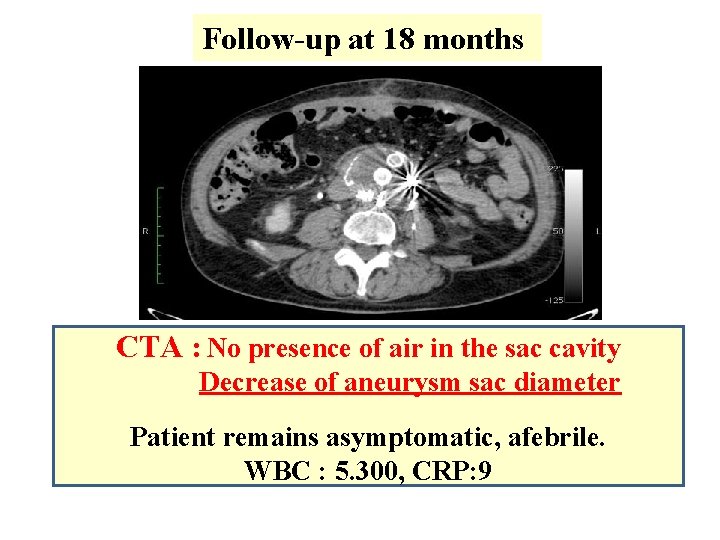
Follow-up at 18 months CTA : No presence of air in the sac cavity Decrease of aneurysm sac diameter Patient remains asymptomatic, afebrile. WBC : 5. 300, CRP: 9
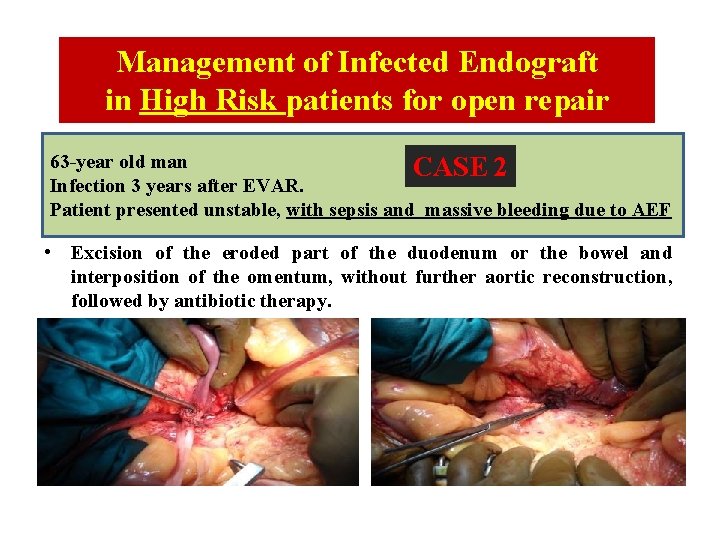
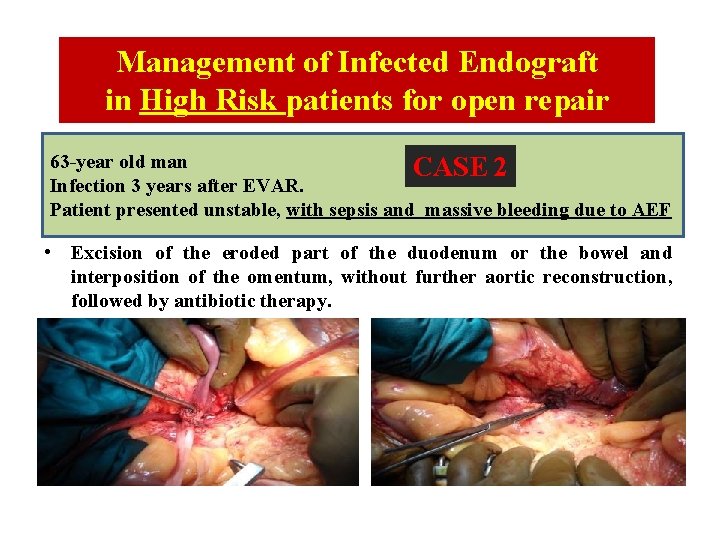
Management of Infected Endograft in High Risk patients for open repair 63 -year old man CASE 2 Infection 3 years after EVAR. Patient presented unstable, with sepsis and massive bleeding due to AEF • Excision of the eroded part of the duodenum or the bowel and interposition of the omentum, without further aortic reconstruction, followed by antibiotic therapy.
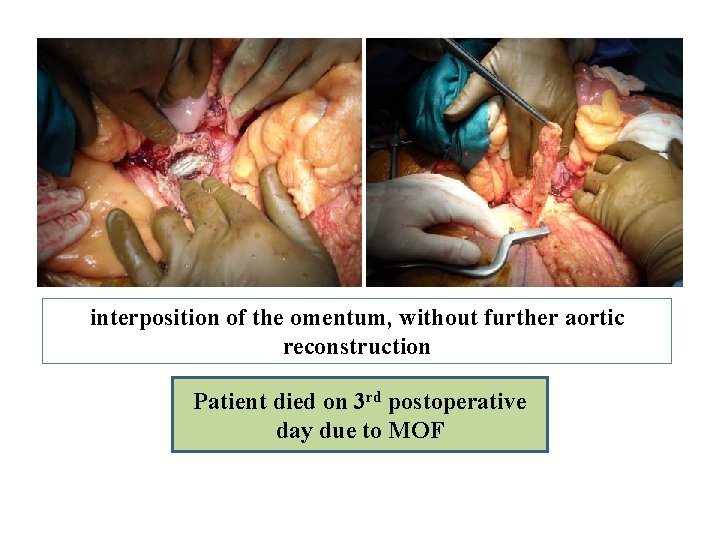
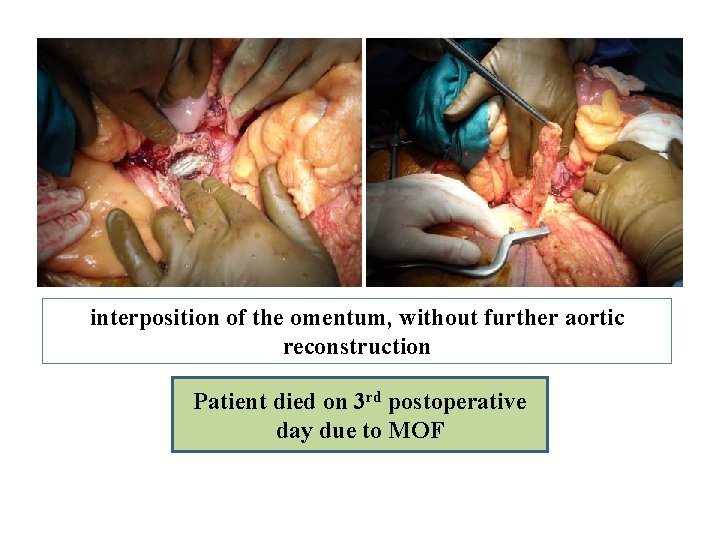
interposition of the omentum, without further aortic reconstruction Patient died on 3 rd postoperative day due to MOF
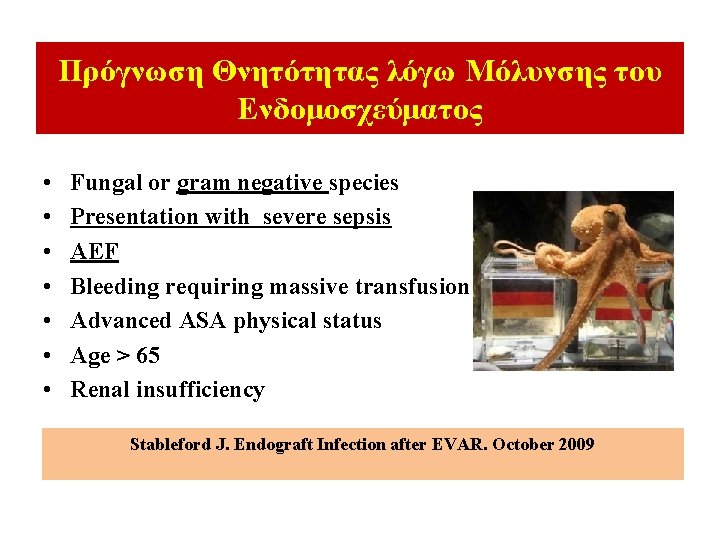
Πρόγνωση Θνητότητας λόγω Μόλυνσης του Ενδομοσχεύματος • • Fungal or gram negative species Presentation with severe sepsis AEF Bleeding requiring massive transfusion Advanced ASA physical status Age > 65 Renal insufficiency Stableford J. Endograft Infection after EVAR. October 2009
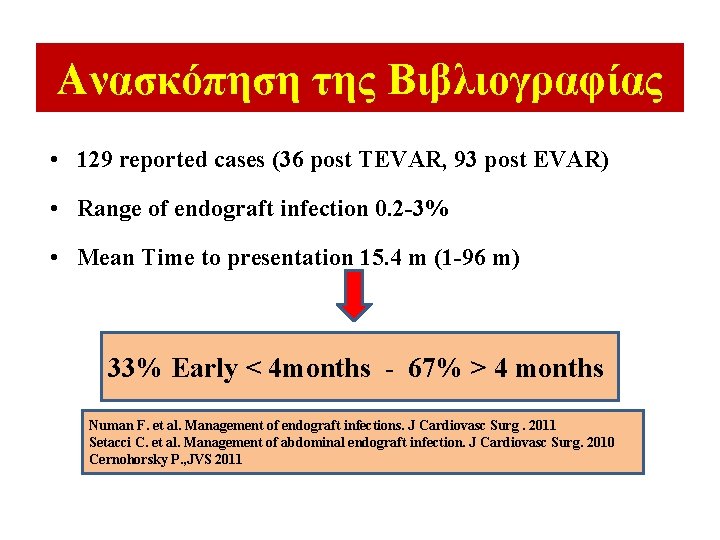
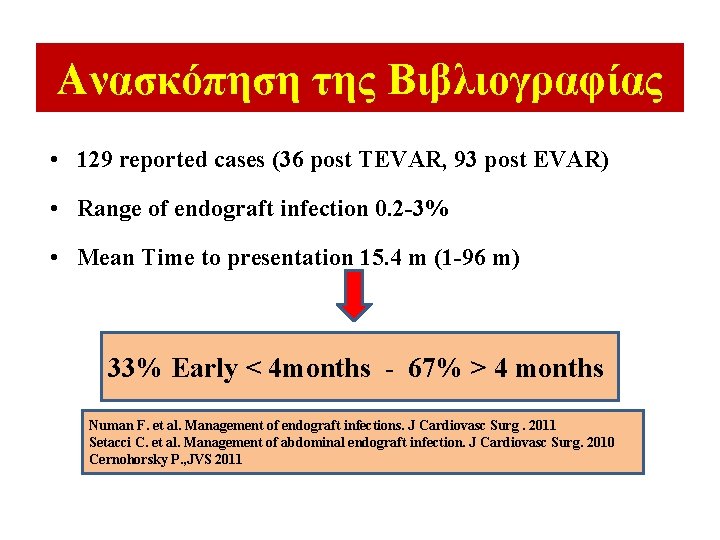
Ανασκόπηση της Βιβλιογραφίας • 129 reported cases (36 post TEVAR, 93 post EVAR) • Range of endograft infection 0. 2 -3% • Mean Time to presentation 15. 4 m (1 -96 m) 33% Early < 4 months - 67% > 4 months Numan F. et al. Management of endograft infections. J Cardiovasc Surg. 2011 Setacci C. et al. Management of abdominal endograft infection. J Cardiovasc Surg. 2010 Cernohorsky P. , JVS 2011

Ανασκόπηση της Βιβλιογραφίας (Σειρές ≥ 3 pts) Author Pts Type of Endograft Procedure Schlensak C. , JVS 2001 5 Stentor 2, Vanguard 3 EVAR Eggebrecht H. , JEVT 2004 3 N. D. TEVAR Sharif MA, JVS 2007 6 Zenith 4, Talent 2 EVAR Brown KE. , JVS 2008 6 TAG 5, Cuff 1 EVAR Girdauskas E, J. Thor. Card. Surg. 2008 4 N. D. TEVAR Sarantzis N. , JEVT 2008 5 Ebdofit 3, Anaconda 1, Powerlink 1 EVAR Heyer KS, JVIR 2009 10 TAG 4, Excluder 3, Zenith 2, Ancure 1 5 EVAR 5 TEVAR Kelso RL, JVS 2009 4 Excluder 2, Aneu. Rx 1, Ancure 1 EVAR Chiesa R. , J. Card. Surg. 2010 7 Zenith 3, Endofit 1, TAG 1, Relay 1, N. D. 1 TEVAR Cernohorsky P. , JVS 2011 12 Zenith 3, Talent 9 2 TEVAR/ 10 EVAR
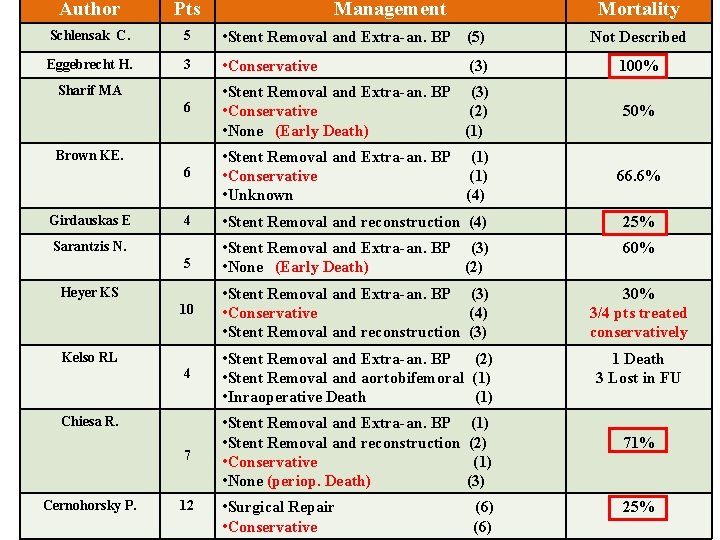
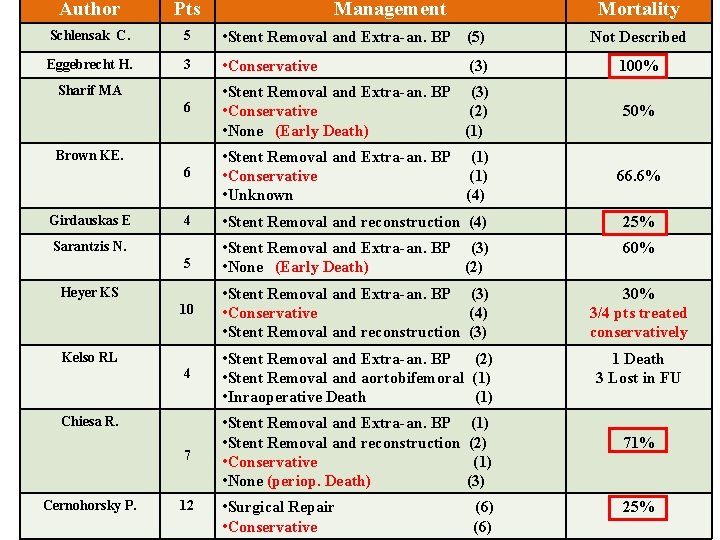
Author Pts Schlensak C. 5 • Stent Removal and Extra-an. BP (5) Not Described Eggebrecht H. 3 • Conservative (3) 100% 6 • Stent Removal and Extra-an. BP (3) • Conservative (2) • None (Early Death) (1) 50% 6 • Stent Removal and Extra-an. BP (1) • Conservative (1) • Unknown (4) 66. 6% 4 • Stent Removal and reconstruction (4) 25% 5 • Stent Removal and Extra-an. BP (3) • None (Early Death) (2) 60% 10 • Stent Removal and Extra-an. BP (3) • Conservative (4) • Stent Removal and reconstruction (3) 30% 3/4 pts treated conservatively 4 • Stent Removal and Extra-an. BP (2) • Stent Removal and aortobifemoral (1) • Inraoperative Death (1) 1 Death 3 Lost in FU 7 • Stent Removal and Extra-an. BP (1) • Stent Removal and reconstruction (2) • Conservative (1) • None (periop. Death) (3) Sharif MA Brown KE. Girdauskas E Sarantzis N. Heyer KS Kelso RL Chiesa R. Cernohorsky P. 12 Management • Surgical Repair (6) • Conservative (6) Mortality 71% 25%
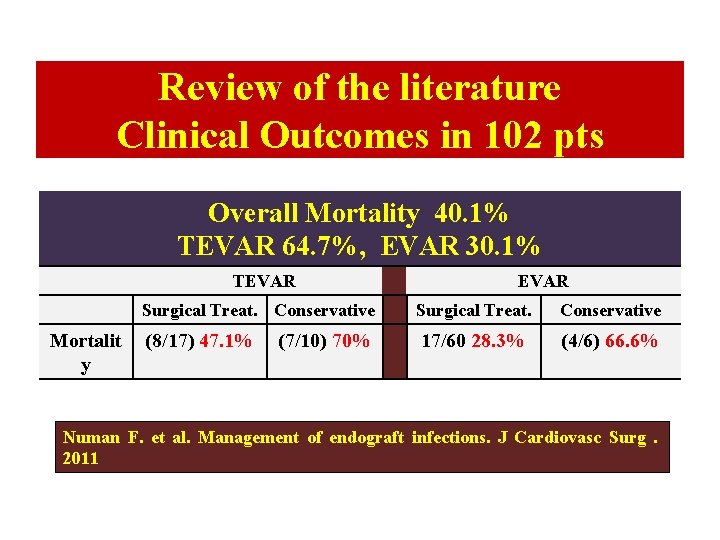
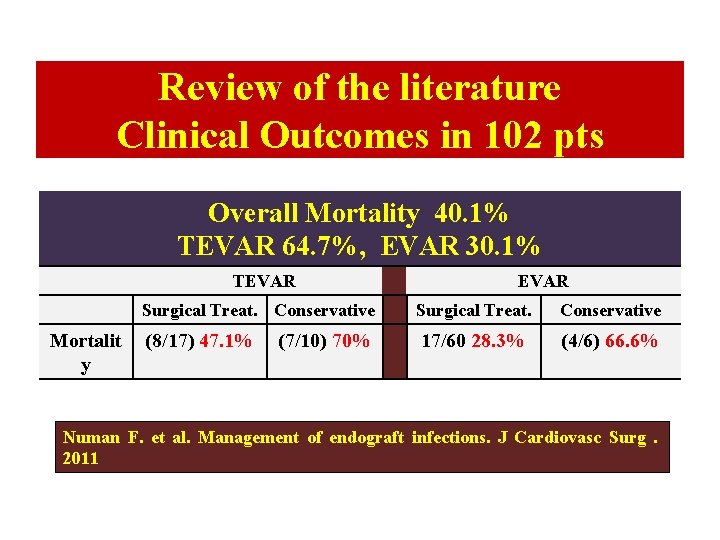
Review of the literature Clinical Outcomes in 102 pts Overall Mortality 40. 1% TEVAR 64. 7%, EVAR 30. 1% TEVAR Mortalit y EVAR Surgical Treat. Conservative Surgical Treat. Conservative (8/17) 47. 1% 17/60 28. 3% (4/6) 66. 6% (7/10) 70% Numan F. et al. Management of endograft infections. J Cardiovasc Surg . 2011
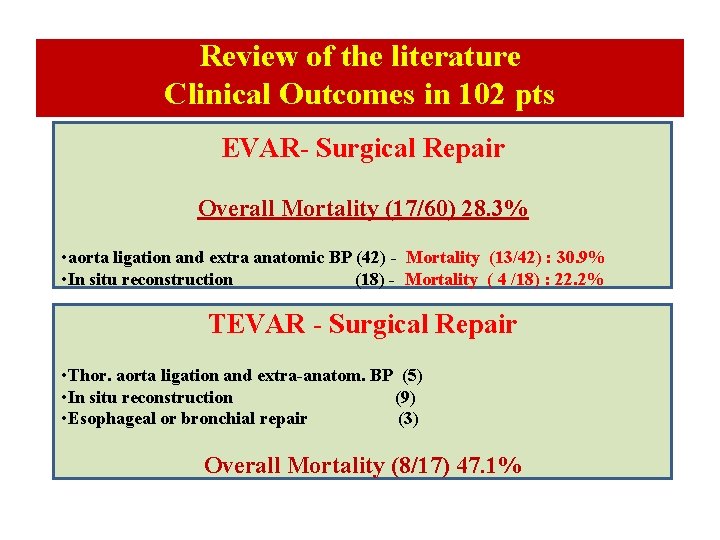
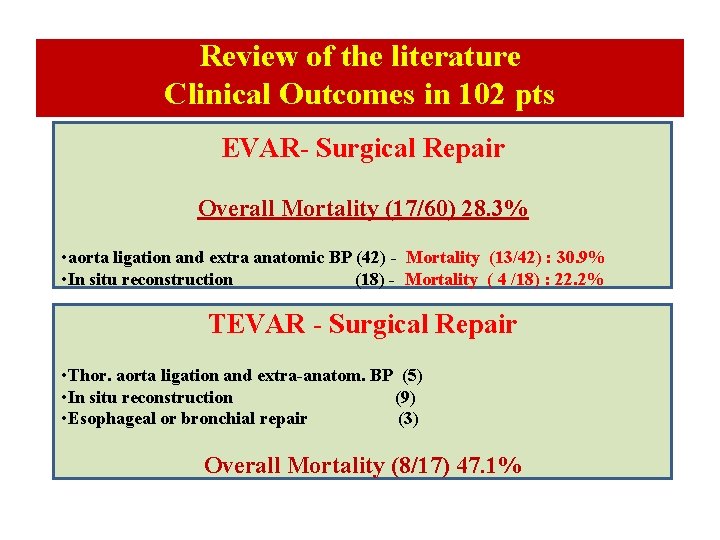
Review of the literature Clinical Outcomes in 102 pts EVAR- Surgical Repair Overall Mortality (17/60) 28. 3% • aorta ligation and extra anatomic BP (42) - Mortality (13/42) : 30. 9% • In situ reconstruction (18) - Mortality ( 4 /18) : 22. 2% TEVAR - Surgical Repair • Thor. aorta ligation and extra-anatom. BP (5) • In situ reconstruction (9) • Esophageal or bronchial repair (3) Overall Mortality (8/17) 47. 1%

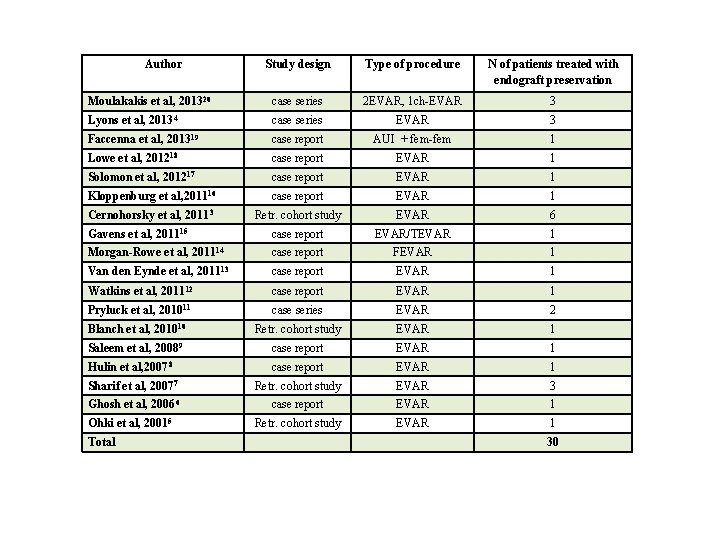
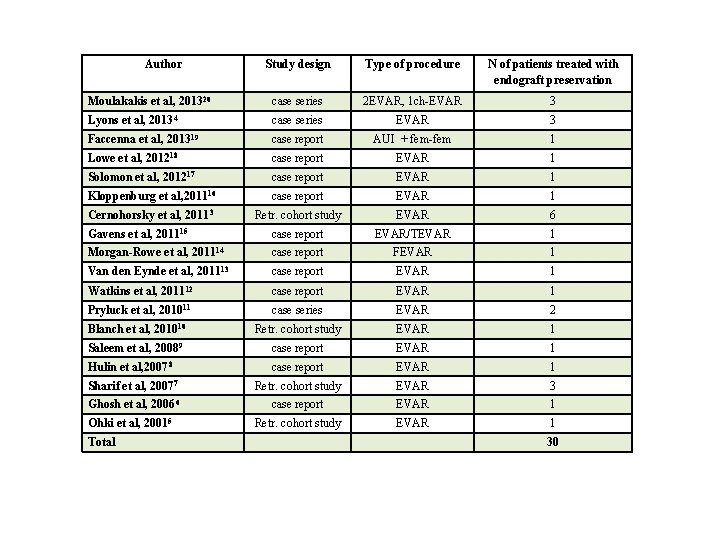
Author Study design Type of procedure N of patients treated with endograft preservation Moulakakis et al, 201320 case series 2 EVAR, 1 ch-EVAR 3 Lyons et al, 20134 case series EVAR 3 Faccenna et al, 201319 case report AUI + fem-fem 1 Lowe et al, 201218 case report EVAR 1 Solomon et al, 201217 case report EVAR 1 Kloppenburg et al, 201116 case report EVAR 1 Cernohorsky et al, 20113 Retr. cohort study EVAR 6 Gavens et al, 201115 case report EVAR/TEVAR 1 Morgan-Rowe et al, 201114 case report FEVAR 1 Van den Eynde et al, 201113 case report EVAR 1 Watkins et al, 201112 case report EVAR 1 Pryluck et al, 201011 case series EVAR 2 Blanch et al, 201010 Retr. cohort study EVAR 1 Saleem et al, 20089 case report EVAR 1 Hulin et al, 20078 case report EVAR 1 Sharif et al, 20077 Retr. cohort study EVAR 3 Ghosh et al, 20066 case report EVAR 1 Retr. cohort study EVAR 1 30 Ohki et al, 20015 Total
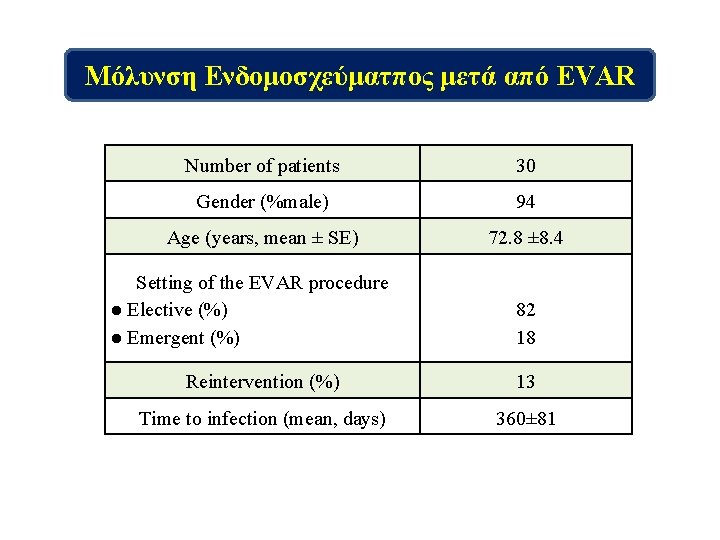
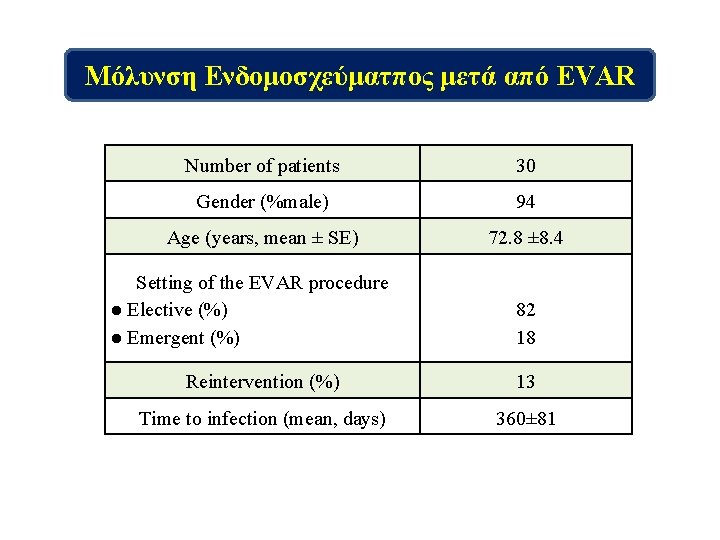
Μόλυνση Ενδομοσχεύματπος μετά από EVAR Number of patients 30 Gender (%male) 94 Age (years, mean ± SE) 72. 8 ± 8. 4 Setting of the EVAR procedure ● Elective (%) ● Emergent (%) 82 18 Reintervention (%) 13 Time to infection (mean, days) 360± 81



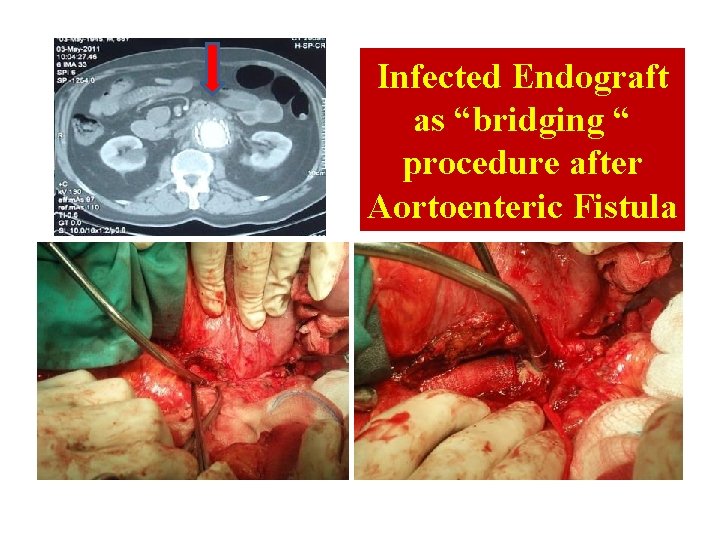
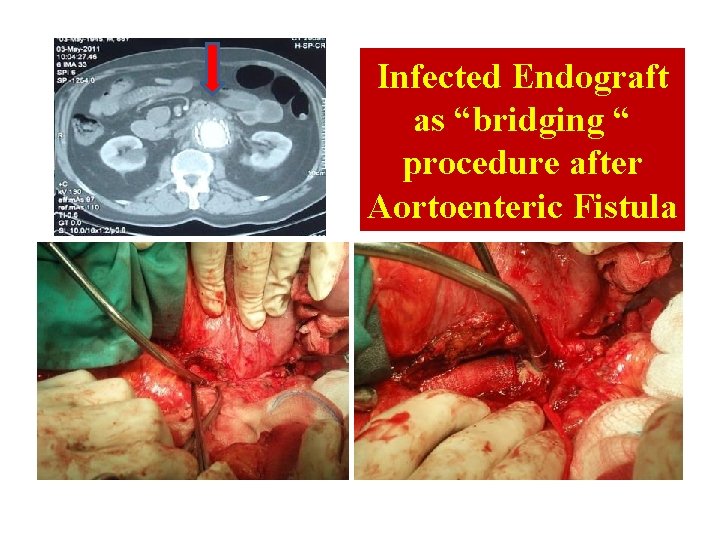
Infected Endograft as “bridging “ procedure after Aortoenteric Fistula

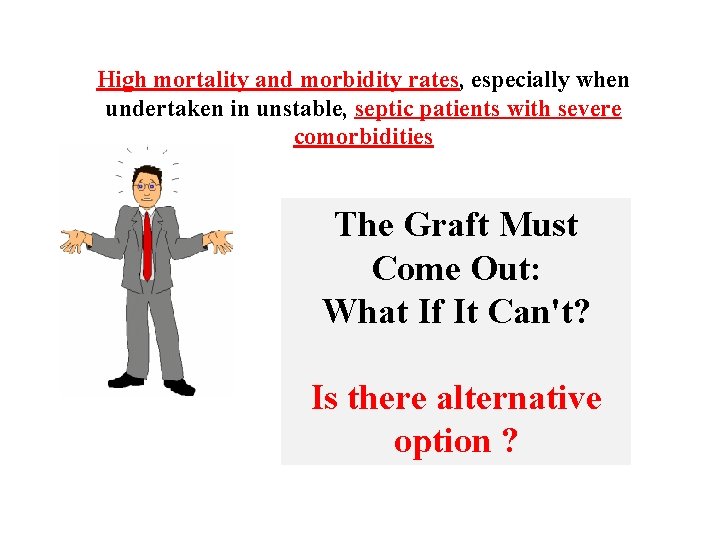
High mortality and morbidity rates, especially when undertaken in unstable, septic patients with severe comorbidities The Graft Must Come Out: What If It Can't? Is there alternative option ?
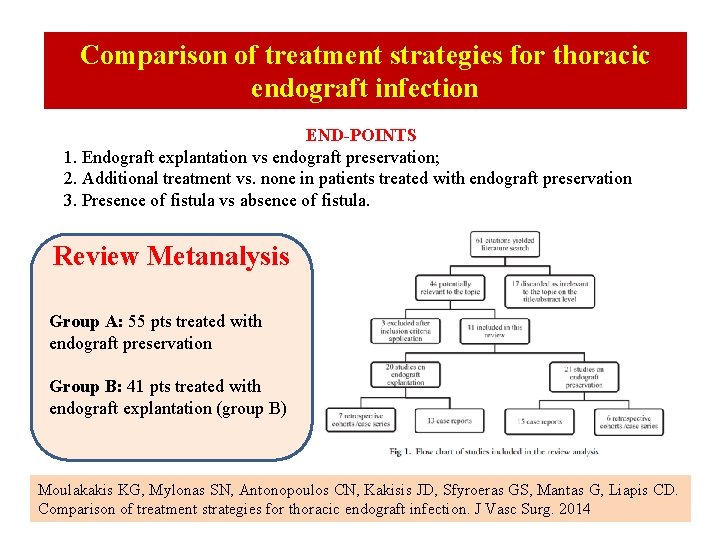
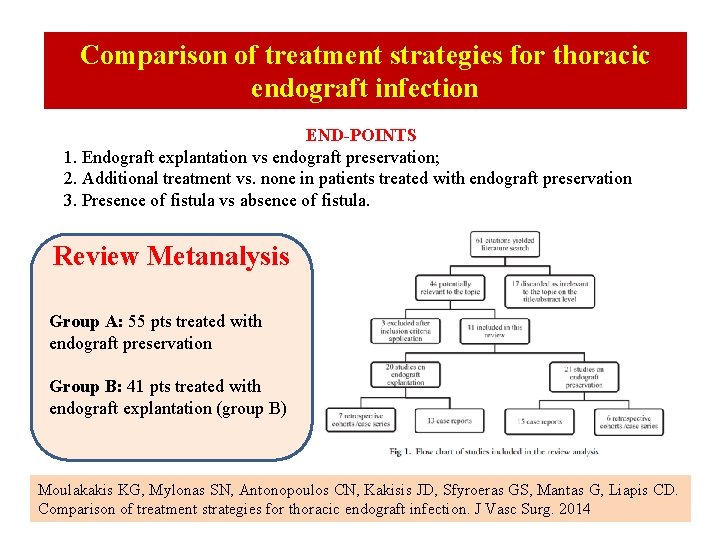
Comparison of treatment strategies for thoracic endograft infection END-POINTS 1. Endograft explantation vs endograft preservation; 2. Additional treatment vs. none in patients treated with endograft preservation 3. Presence of fistula vs absence of fistula. Review Metanalysis Group A: 55 pts treated with endograft preservation Group B: 41 pts treated with endograft explantation (group B) Moulakakis KG, Mylonas SN, Antonopoulos CN, Kakisis JD, Sfyroeras GS, Mantas G, Liapis CD. Comparison of treatment strategies for thoracic endograft infection. J Vasc Surg. 2014

 Mycotic infection rabbit
Mycotic infection rabbit Thalasemia
Thalasemia Pathophysiology of aortic aneurysm ppt
Pathophysiology of aortic aneurysm ppt Thorasic aortic aneurysm
Thorasic aortic aneurysm Interventionsstudier
Interventionsstudier Flexion del codo
Flexion del codo Father of modern medicine
Father of modern medicine Hiperaldosteronismo primario clinica
Hiperaldosteronismo primario clinica Zveren injury
Zveren injury Osler node
Osler node Osler's nodes
Osler's nodes Berry aneurysm vs charcot bouchard
Berry aneurysm vs charcot bouchard Berry aneurysm
Berry aneurysm Avm vs aneurysm
Avm vs aneurysm Paraclinoid ica
Paraclinoid ica Wide neck aneurysm
Wide neck aneurysm Aneurysm
Aneurysm Aneurysm
Aneurysm Ventricular wall aneurysm
Ventricular wall aneurysm Korotkoff sound
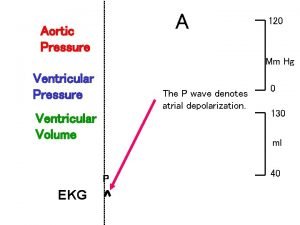
Korotkoff sound Aortic area 1 and 2
Aortic area 1 and 2 Aortic valve anatomy
Aortic valve anatomy Axial vs appendicular skeleton
Axial vs appendicular skeleton Pleura location
Pleura location Dvi aortic valve
Dvi aortic valve Pulmonary ligament
Pulmonary ligament Major arteries of the ascending aorta and aortic arch
Major arteries of the ascending aorta and aortic arch Tibial pulse
Tibial pulse Dvi aortic valve
Dvi aortic valve Branches off aortic arch
Branches off aortic arch Valve resistance formula
Valve resistance formula Spermatic cord components
Spermatic cord components Dvi in echo
Dvi in echo Continuity equation echo
Continuity equation echo Mitral regurgitation murmur
Mitral regurgitation murmur Aortic valve dimensionless index
Aortic valve dimensionless index Aortic body
Aortic body Patent ductus arteriosus pathophysiology
Patent ductus arteriosus pathophysiology Lordotic chest x ray
Lordotic chest x ray Dr m chadi alraies
Dr m chadi alraies Aortic pressure curve
Aortic pressure curve Recurrent laryngeal nerve
Recurrent laryngeal nerve Aortic valve leaflets
Aortic valve leaflets Dobutamine dose
Dobutamine dose Aortic semi lunar valve
Aortic semi lunar valve Peripheral signs of aortic regurgitation
Peripheral signs of aortic regurgitation Right and left aortic sinus
Right and left aortic sinus Crux cordis
Crux cordis Aortic disection
Aortic disection Aortic stanosis
Aortic stanosis Semilunar
Semilunar Aortic bifurcation surface anatomy
Aortic bifurcation surface anatomy Aortic arch branches
Aortic arch branches Type b aortic dissection
Type b aortic dissection Endocardium sheep heart
Endocardium sheep heart Sternocostal surface of heart
Sternocostal surface of heart Left lumbar
Left lumbar Www.youtube.comwatch
Www.youtube.comwatch Heart parts
Heart parts Annulus of vieussens
Annulus of vieussens Firas mussa md
Firas mussa md Long medium and short term planning in primary schools
Long medium and short term planning in primary schools Term-to-term rule
Term-to-term rule Long term memory vs short term memory
Long term memory vs short term memory Term-to-term rule
Term-to-term rule Short term hr planning
Short term hr planning Position-to-term
Position-to-term Difference between long term and short term liabilities
Difference between long term and short term liabilities Long-term liabilities examples
Long-term liabilities examples Minterm maxterm
Minterm maxterm