Review on Mycotic Aneurysm Joint Hospital Surgical Grand

- Slides: 30
Review on Mycotic Aneurysm Joint Hospital Surgical Grand Round Li Hoi Man Princess Margaret Hospital 26/4/2014
Content History Definition Pathogenesis Disease characteristics Diagnosis Treatment
History of Mycotic Aneurysm 1844: Rokitansky 1 described abscess in the walls of arteries 1851: Koch 2 reported the sudden death of a 22/M from a ruptured SMA aneurysm while treating I. E. 1885: Sir William Osler 3 proposed a causal relationship between infection of the aortic wall and subsequent aneurysm formation
Definition Initially signified an infected aneurysm found in association with bacterial endocarditis Nowadays denote an infected aneurysm of any type Mycotic aneurysm: both true and false aneurysms that are associated with infection of the arterial wall
Pathogenesis 1. Oslerian mycotic aneurysms Embolization of infected cardiac vegetations 2. Haematogenous seeding Bacteremia microbial seeding of arteries arteritis aneurysm formation 3. Infected aneurysms Bacteremia lodge within the intramural thrombus and arteriosclerotic intima 4. Others Mechanical arterial injury with contamination Contiguous spread

Epidemiology Era of bacterial endocarditis: 2 nd -4 th decades Now: elderly 6 th-8 th decades Male predominance (> 2/3) Higher prevalence in drug addicts and patients with AIDS
Clinical presentation S/S from infection / bacteremia: S/S secondary to local arterial involvement / aneurysm formation: Localized tenderness, bruits, neurologic defects, pulsatile masses Thrombosis / thromboembolization Rupture pseudoaneurysm hypotensive shock, life-threatening haemorrhage
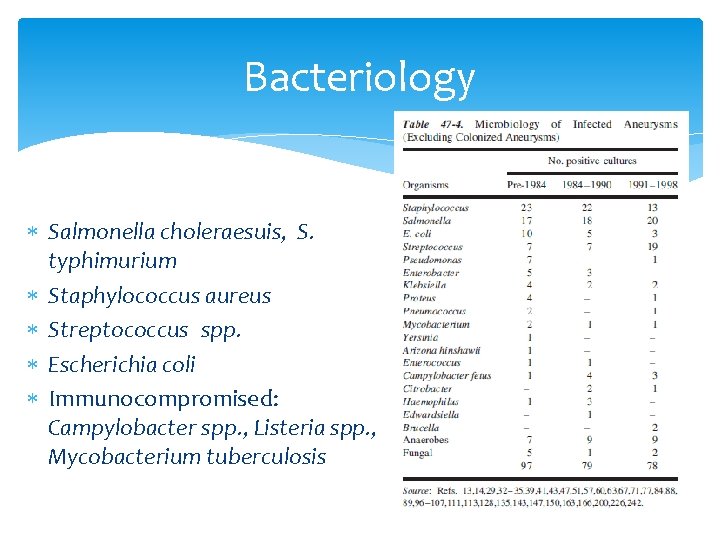
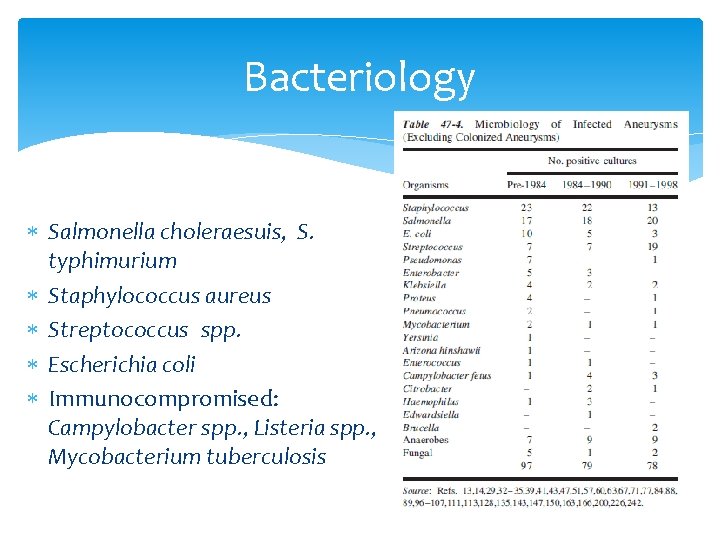
Bacteriology Salmonella choleraesuis, S. typhimurium Staphylococcus aureus Streptococcus spp. Escherichia coli Immunocompromised: Campylobacter spp. , Listeria spp. , Mycobacterium tuberculosis
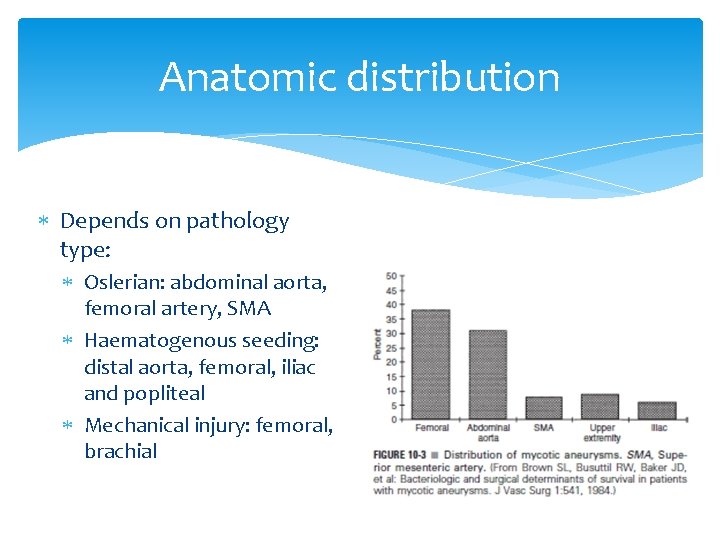
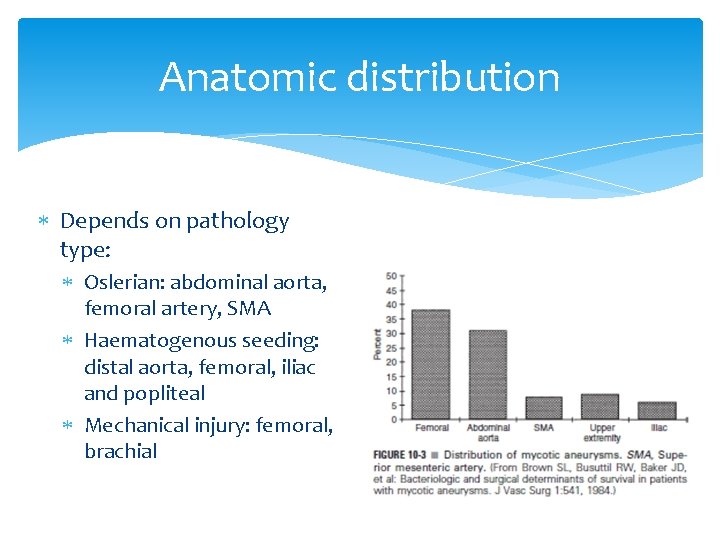
Anatomic distribution Depends on pathology type: Oslerian: abdominal aorta, femoral artery, SMA Haematogenous seeding: distal aorta, femoral, iliac and popliteal Mechanical injury: femoral, brachial
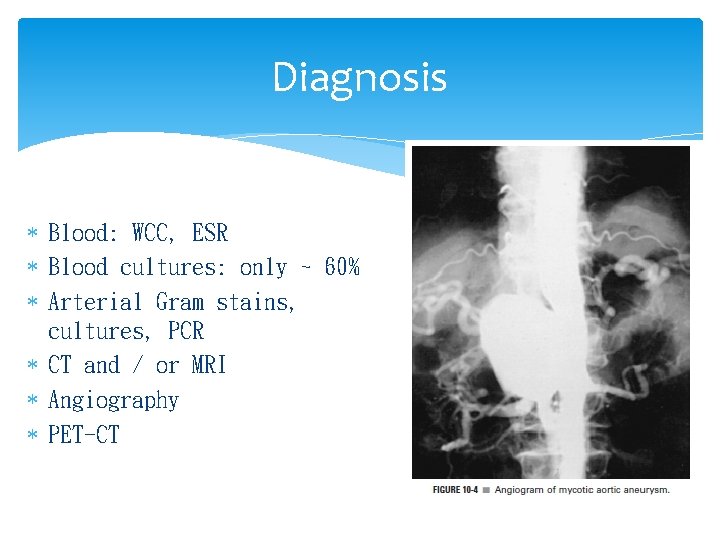
Diagnosis Blood: WCC, ESR Blood cultures: only ~ 60% Arterial Gram stains, cultures, PCR CT and / or MRI Angiography PET-CT
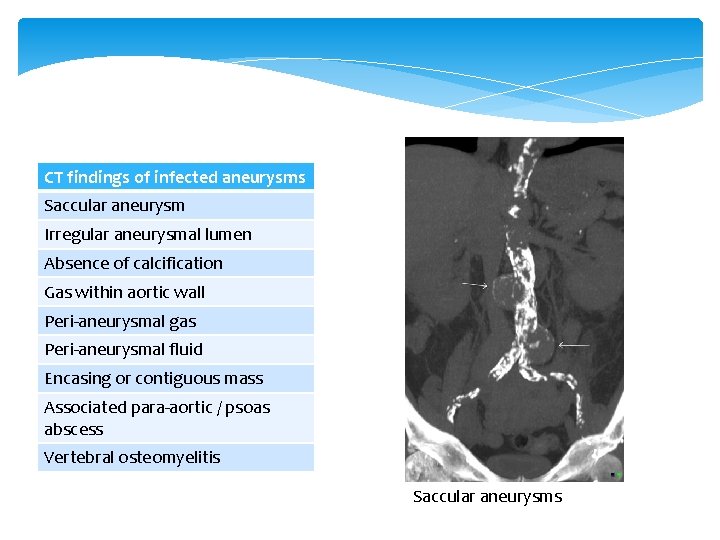
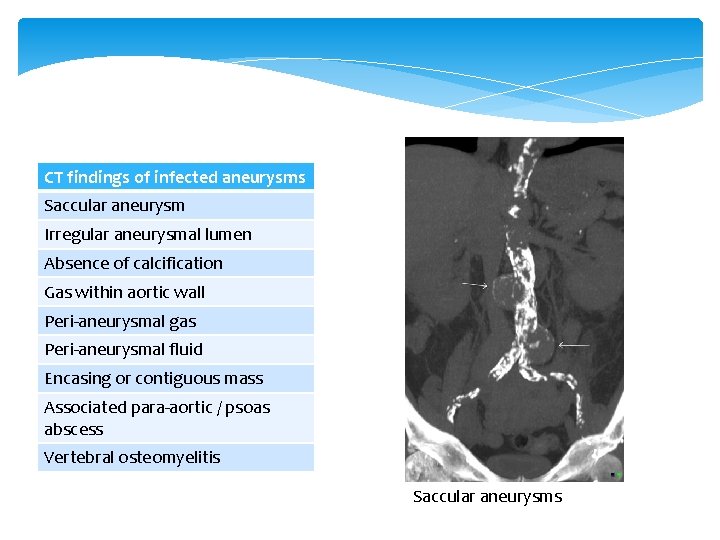
CT findings of infected aneurysms Saccular aneurysm Irregular aneurysmal lumen Absence of calcification Gas within aortic wall Peri-aneurysmal gas Peri-aneurysmal fluid Encasing or contiguous mass Associated para-aortic / psoas abscess Vertebral osteomyelitis Saccular aneurysms
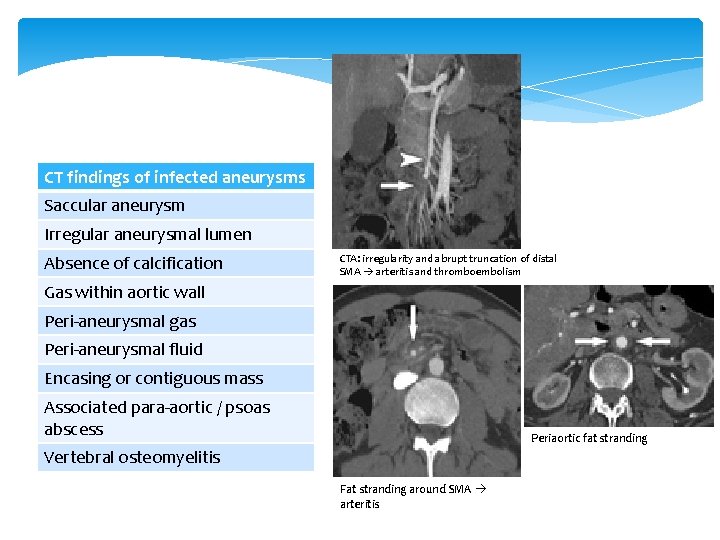
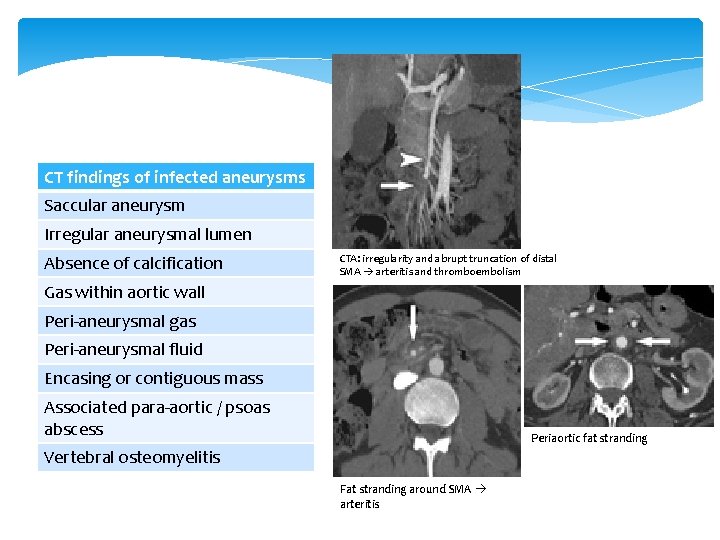
CT findings of infected aneurysms Saccular aneurysm Irregular aneurysmal lumen Absence of calcification CTA: irregularity and abrupt truncation of distal SMA arteritis and thromboembolism Gas within aortic wall Peri-aneurysmal gas Peri-aneurysmal fluid Encasing or contiguous mass Associated para-aortic / psoas abscess Periaortic fat stranding Vertebral osteomyelitis Fat stranding around SMA arteritis
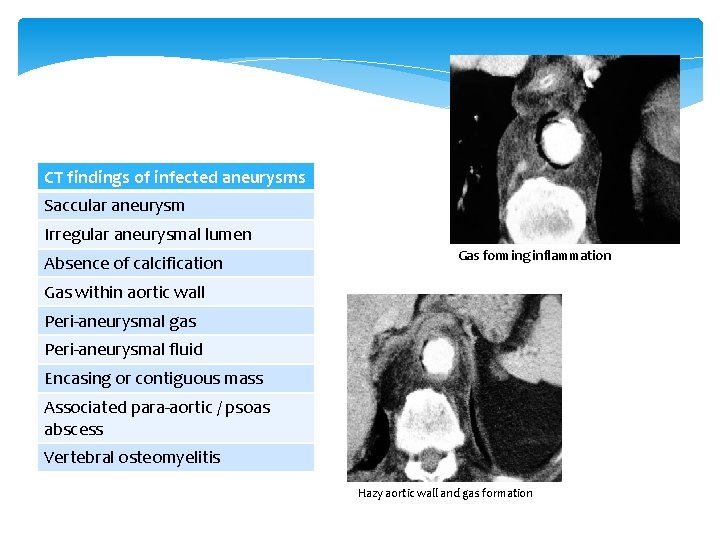
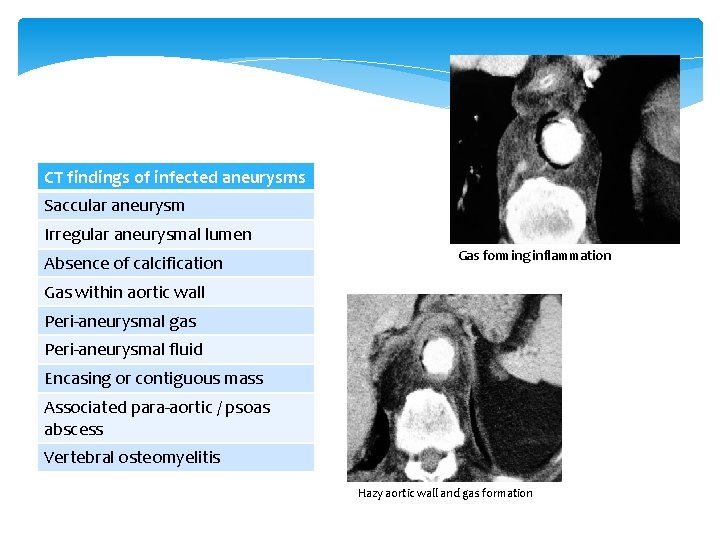
CT findings of infected aneurysms Saccular aneurysm Irregular aneurysmal lumen Absence of calcification Gas forming inflammation Gas within aortic wall Peri-aneurysmal gas Peri-aneurysmal fluid Encasing or contiguous mass Associated para-aortic / psoas abscess Vertebral osteomyelitis Hazy aortic wall and gas formation
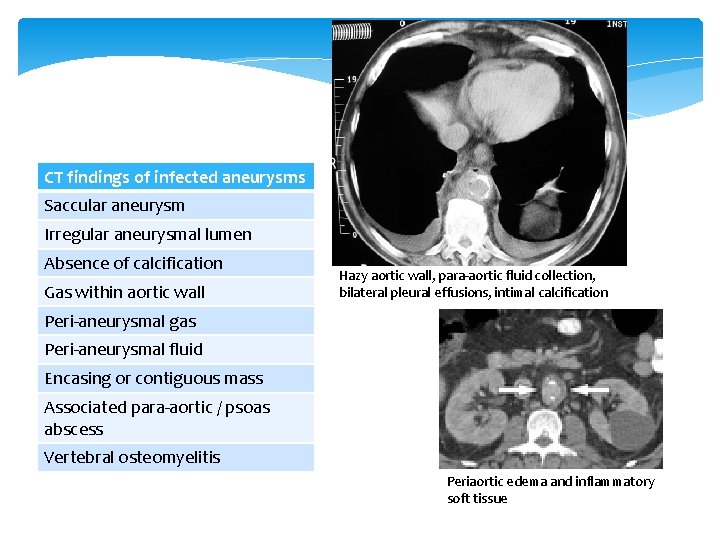
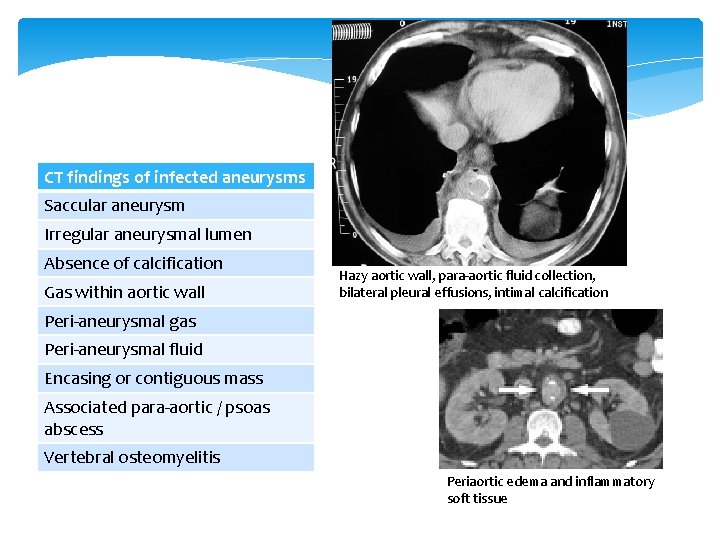
CT findings of infected aneurysms Saccular aneurysm Irregular aneurysmal lumen Absence of calcification Gas within aortic wall Hazy aortic wall, para-aortic fluid collection, bilateral pleural effusions, intimal calcification Peri-aneurysmal gas Peri-aneurysmal fluid Encasing or contiguous mass Associated para-aortic / psoas abscess Vertebral osteomyelitis Periaortic edema and inflammatory soft tissue
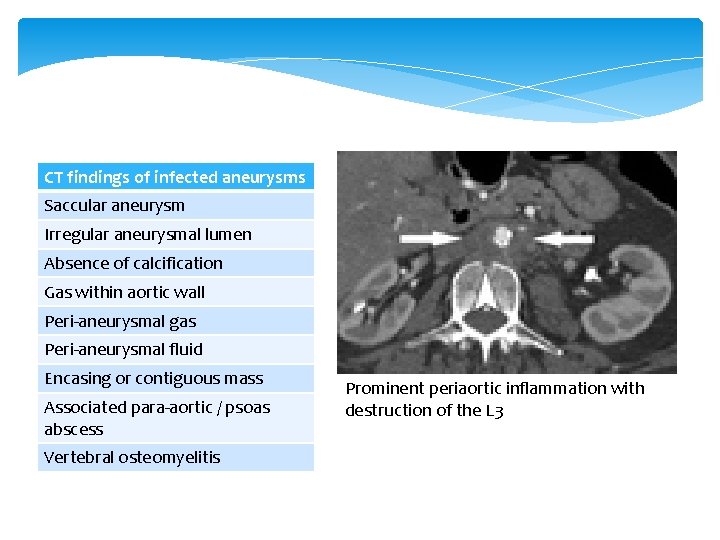
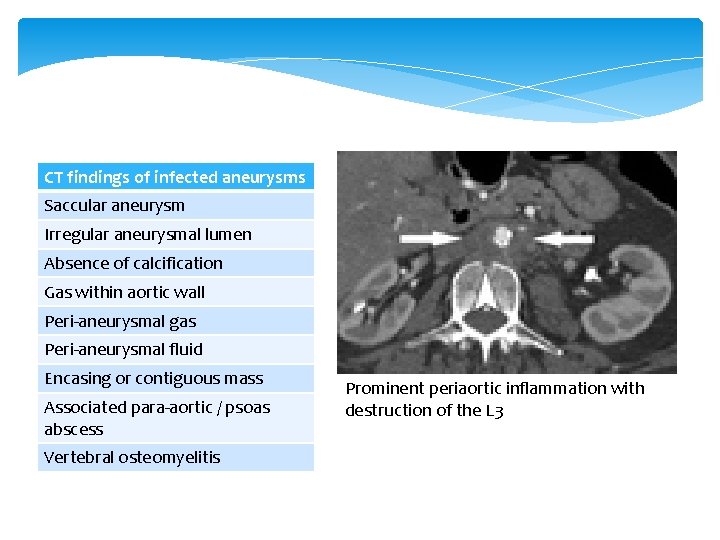
CT findings of infected aneurysms Saccular aneurysm Irregular aneurysmal lumen Absence of calcification Gas within aortic wall Peri-aneurysmal gas Peri-aneurysmal fluid Encasing or contiguous mass Associated para-aortic / psoas abscess Vertebral osteomyelitis Prominent periaortic inflammation with destruction of the L 3
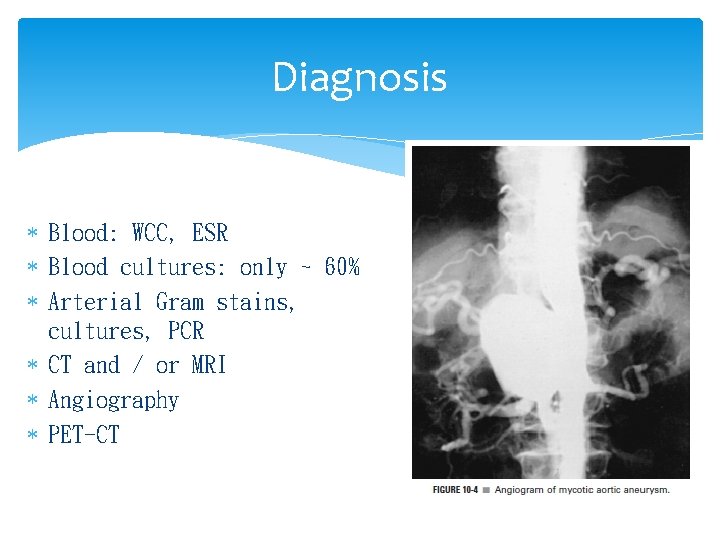
Diagnosis Blood: WCC, ESR Blood cultures: only ~ 60% Arterial Gram stains, cultures, PCR CT and / or MRI Angiography PET-CT
Diagnosis Blood: WCC, ESR Blood cultures: only ~ 60% Arterial Gram stains, cultures, PCR CT and / or MRI Angiography PET-CT
Principles of Management Control of sepsis Arterial reconstruction
Control of sepsis Antibiotic therapy Broad-spectrum, high dose, according to c/st Extend for at least 6 weeks post-op Lifelong if prosthetic reconstructions involved Surgical debridement Aggressive wide debridement Drains
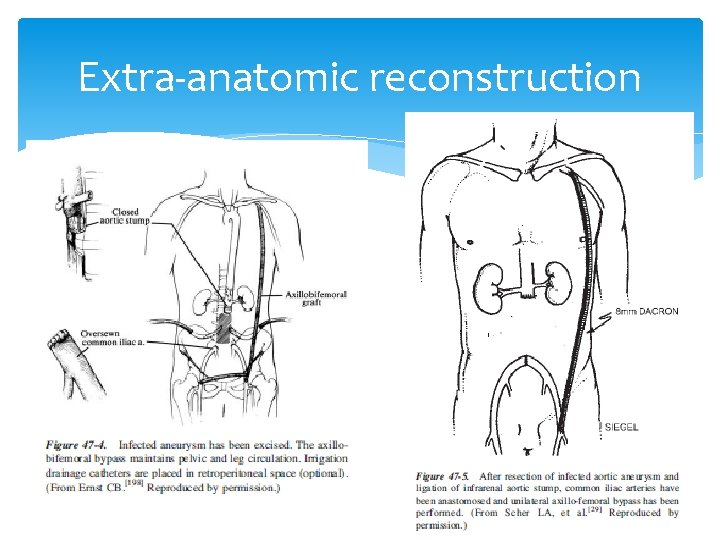
Arterial reconstruction Open approach - extra-anatomic reconstruction In-situ reconstruction - EVAR
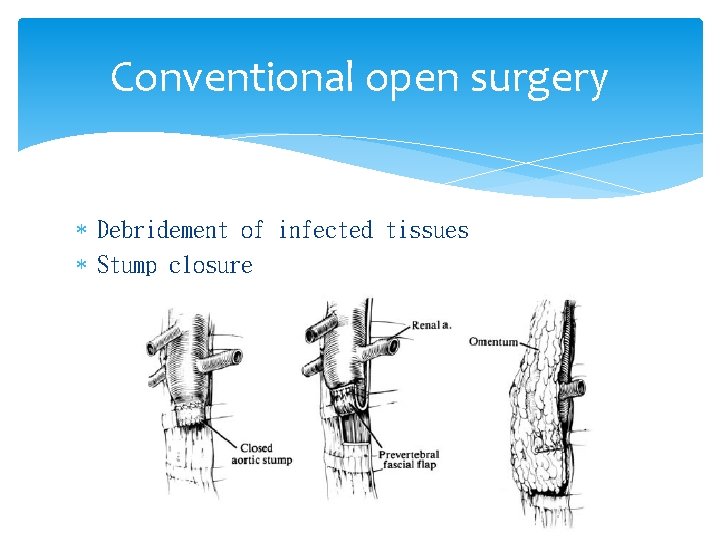
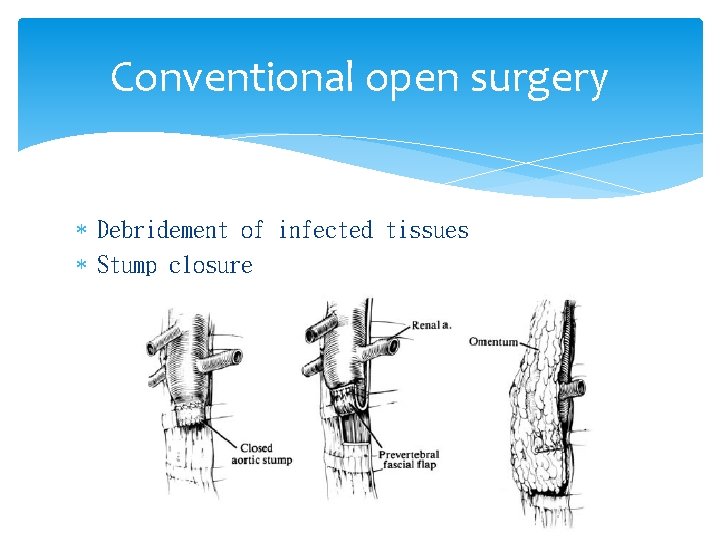
Conventional open surgery Debridement of infected tissues Stump closure
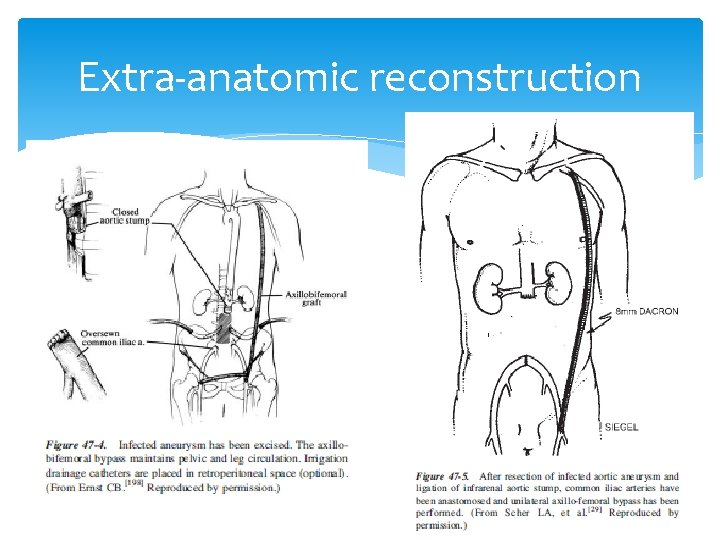
Extra-anatomic reconstruction
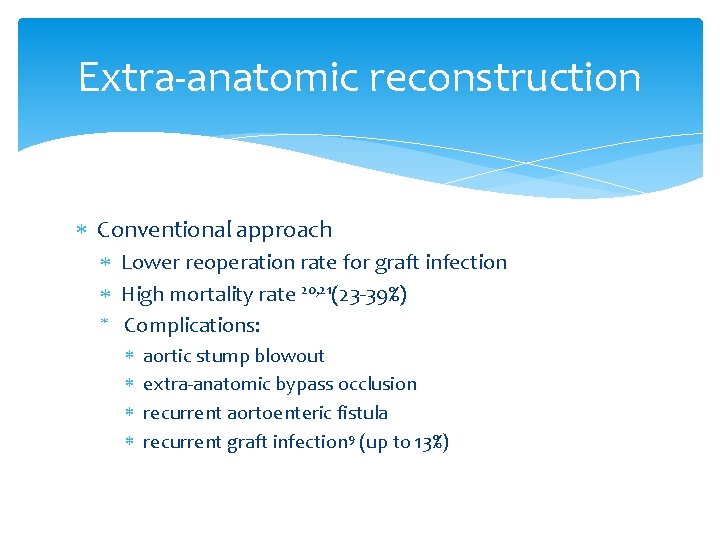
Extra-anatomic reconstruction Conventional approach Lower reoperation rate for graft infection High mortality rate 20, 21(23 -39%) Complications: aortic stump blowout extra-anatomic bypass occlusion recurrent aortoenteric fistula recurrent graft infection 9 (up to 13%)
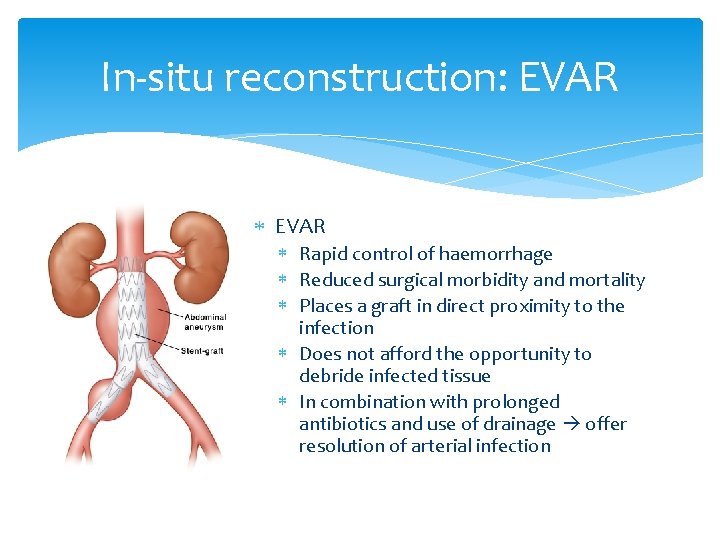
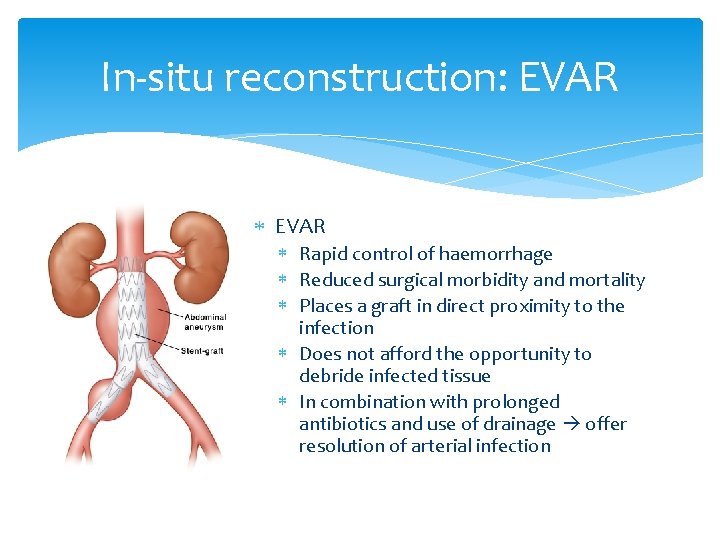
In-situ reconstruction: EVAR Rapid control of haemorrhage Reduced surgical morbidity and mortality Places a graft in direct proximity to the infection Does not afford the opportunity to debride infected tissue In combination with prolonged antibiotics and use of drainage offer resolution of arterial infection
Comparison between open vs EVAR Kan 12 reviewed on efficacy of EVAR in infected AAA, 41 cases, EVAR (n=20) vs conventional surgery (n=21) - Early (30 days) post-op mortality similar - Late (2 year) mortality greater in conventional surgery (10% vs 25%) - Aneurysm-related event-free survival similar
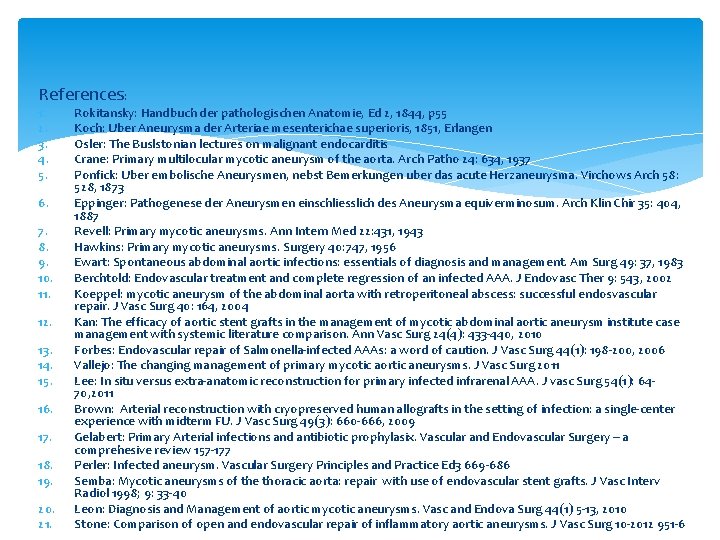
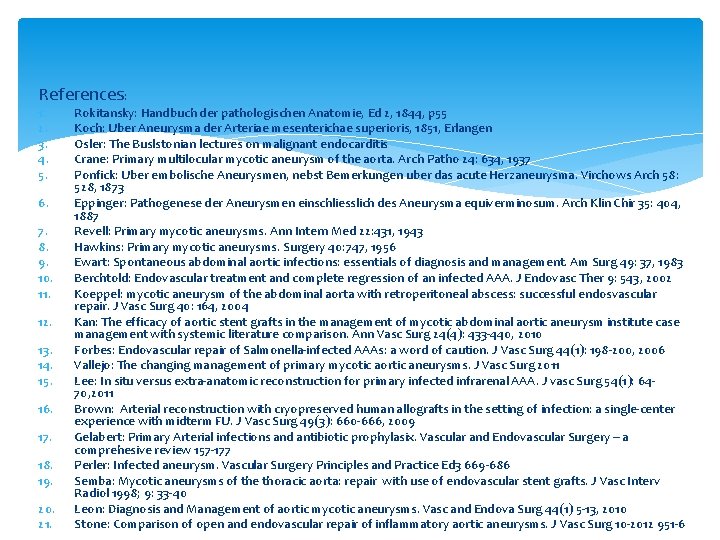
References: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. Rokitansky: Handbuch der pathologischen Anatomie, Ed 2, 1844, p 55 Koch: Uber Aneurysma der Arteriae mesenterichae superioris, 1851, Erlangen Osler: The Buslstonian lectures on malignant endocarditis Crane: Primary multilocular mycotic aneurysm of the aorta. Arch Patho 24: 634, 1937 Ponfick: Uber embolische Aneurysmen, nebst Bemerkungen uber das acute Herzaneurysma. Virchows Arch 58: 528, 1873 Eppinger: Pathogenese der Aneurysmen einschliesslich des Aneurysma equiverminosum. Arch Klin Chir 35: 404, 1887 Revell: Primary mycotic aneurysms. Ann Intern Med 22: 431, 1943 Hawkins: Primary mycotic aneurysms. Surgery 40: 747, 1956 Ewart: Spontaneous abdominal aortic infections: essentials of diagnosis and management. Am Surg 49: 37, 1983 Berchtold: Endovascular treatment and complete regression of an infected AAA. J Endovasc Ther 9: 543, 2002 Koeppel: mycotic aneurysm of the abdominal aorta with retroperitoneal abscess: successful endosvascular repair. J Vasc Surg 40: 164, 2004 Kan: The efficacy of aortic stent grafts in the management of mycotic abdominal aortic aneurysm institute case management with systemic literature comparison. Ann Vasc Surg 24(4): 433 -440, 2010 Forbes: Endovascular repair of Salmonella-infected AAAs: a word of caution. J Vasc Surg 44(1): 198 -200, 2006 Vallejo: The changing management of primary mycotic aortic aneurysms. J Vasc Surg 2011 Lee: In situ versus extra-anatomic reconstruction for primary infected infrarenal AAA. J vasc Surg 54(1): 6470, 2011 Brown: Arterial reconstruction with cryopreserved human allografts in the setting of infection: a single-center experience with midterm FU. J Vasc Surg 49(3): 660 -666, 2009 Gelabert: Primary Arterial infections and antibiotic prophylasix. Vascular and Endovascular Surgery – a comprehesive review 157 -177 Perler: Infected aneurysm. Vascular Surgery Principles and Practice Ed 3 669 -686 Semba: Mycotic aneurysms of the thoracic aorta: repair with use of endovascular stent grafts. J Vasc Interv Radiol 1998; 9: 33 -40 Leon: Diagnosis and Management of aortic mycotic aneurysms. Vasc and Endova Surg 44(1) 5 -13, 2010 Stone: Comparison of open and endovascular repair of inflammatory aortic aneurysms. J Vasc Surg 10 -2012 951 -6
~ The End ~
Our cases M/65, GPH, walks unaided LLQ pain with radiation to back and subjective fever for 1/52 Temp 37. 7 abd: 5 cm expansile mass, tender CT: 5. 2 cm infra-renal AAA with impending rupture and para-aortic fat stranding Put on augmentin and flagyl Blood c/st, TB, widal test, Treponema: all –ve EVAR done FU CT showed no endoleak and aortic sac wall thickening showed interval improvement Lifelong levofloxacin 750 mg daily
Our cases M/65 GPH Abd pain x 1/12 CT: 2. 9 cm infrarenal AAA with eccentric mural thrombus EVAR + fem-fem bypass on 5/2010 Blood C/st: salmonella sensitive to ciprofloxacin Subsequent CT: resolution of the inflammatory changes Antibiotic coverage discontinued 1 year later FU CT 2. 5 years later: ? Relapse of infection with increased perigraft soft tissue swelling Treated with a 8 -week course of rocephin 2 gm daily then changed to azithromycin 500 mg daily po afterwards
 Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Mycotic infection rabbit
Mycotic infection rabbit Wellspan inet
Wellspan inet Lafayette surgical imaging
Lafayette surgical imaging Berry aneurysm vs charcot bouchard
Berry aneurysm vs charcot bouchard Berry aneurysm
Berry aneurysm Avm vs aneurysm
Avm vs aneurysm Paraclinoid ica
Paraclinoid ica Brain aneurysm causes
Brain aneurysm causes Aneurysm
Aneurysm Un koodave porakkanum
Un koodave porakkanum Thoracic aortic aneurysm
Thoracic aortic aneurysm Ventricular wall aneurysm
Ventricular wall aneurysm Stent graft
Stent graft Thorasic aortic aneurysm
Thorasic aortic aneurysm Definition of hospital pharmacist
Definition of hospital pharmacist Lamb grading chart
Lamb grading chart Ligamentum nuchae
Ligamentum nuchae Temporary wood joints
Temporary wood joints Memorandum joint venture
Memorandum joint venture Lamb grading chart
Lamb grading chart Depression movement
Depression movement Corner joint symbol
Corner joint symbol Chapter review motion part a vocabulary review answer key
Chapter review motion part a vocabulary review answer key Uncontrollable spending ap gov
Uncontrollable spending ap gov