Joint Hospital Surgical Grand Round 17 January 2009
- Slides: 36
Joint Hospital Surgical Grand Round 17 January 2009 Peptic Ulcer Rebleeding An Evidence-Based Management Dr Shirley Yuk-Wah Liu Department of Surgery Prince of Wales Hospital The Chinese University of Hong Kong
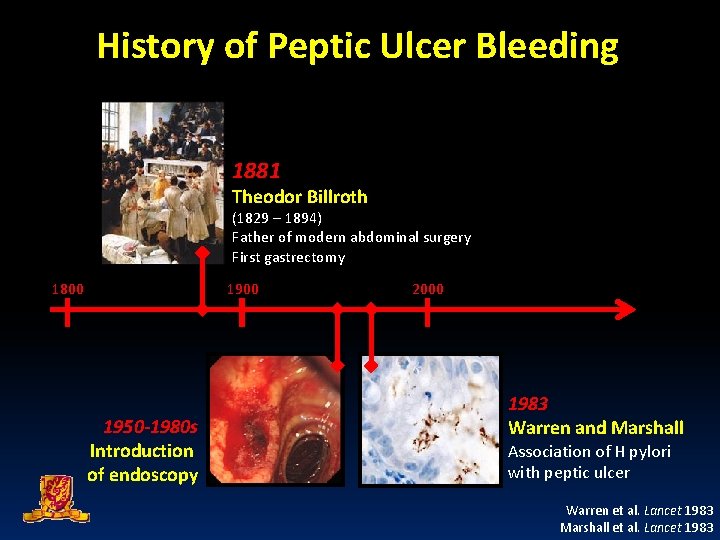
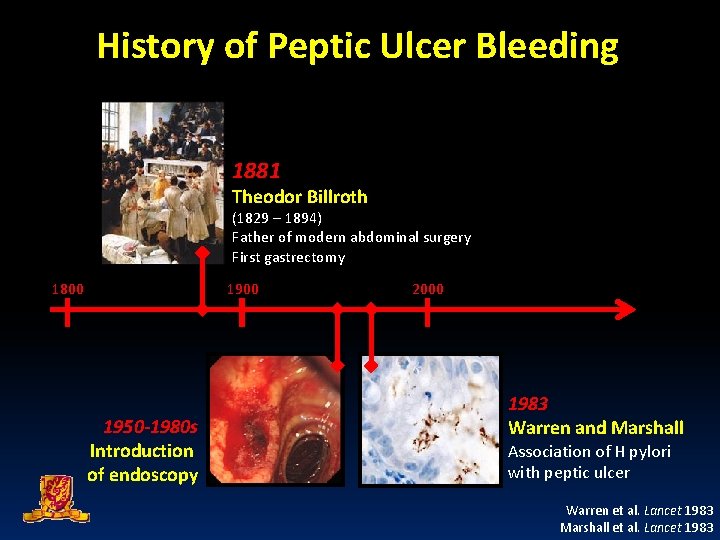
History of Peptic Ulcer Bleeding 1881 Theodor Billroth (1829 – 1894) Father of modern abdominal surgery First gastrectomy 1800 1950 -1980 s Introduction of endoscopy 2000 1983 Warren and Marshall Association of H pylori with peptic ulcer Warren et al. Lancet 1983 Marshall et al. Lancet 1983
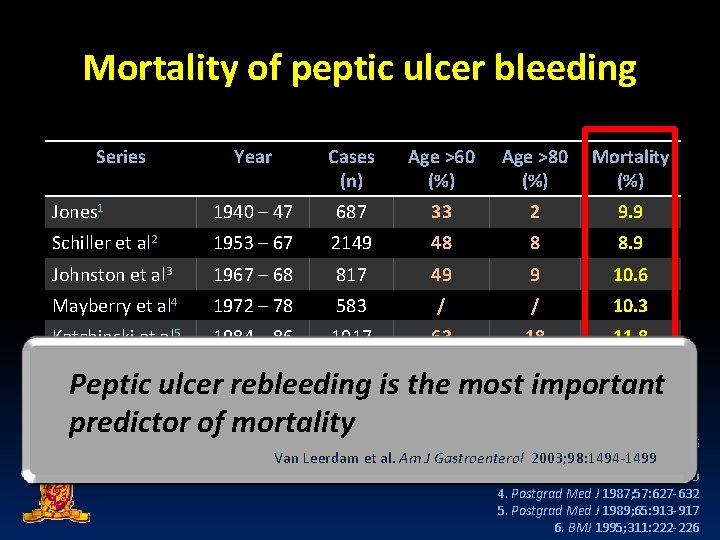
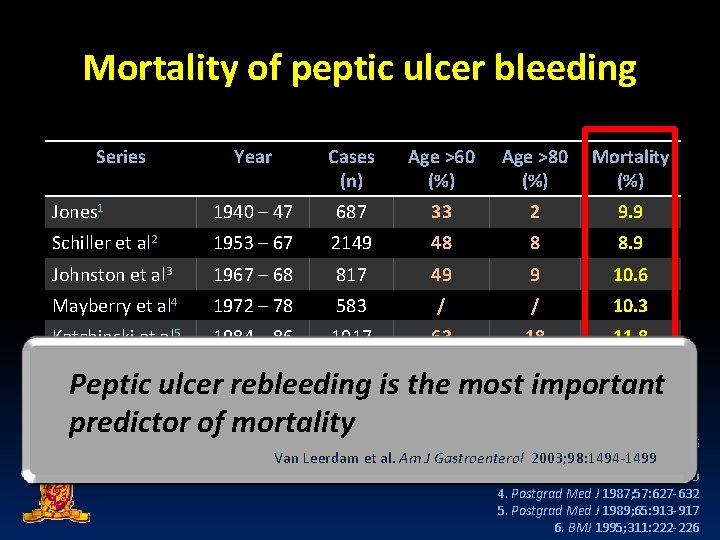
Mortality of peptic ulcer bleeding Series Year Cases (n) Age >60 (%) Age >80 (%) Mortality (%) Jones 1 1940 – 47 687 33 2 9. 9 Schiller et al 2 1953 – 67 2149 48 8 8. 9 Johnston et al 3 1967 – 68 817 49 9 10. 6 Mayberry et al 4 1972 – 78 583 / / 10. 3 Katchinski et al 5 1984 – 86 1017 63 18 11. 8 1993 4185 68 27 11. 0 Rockall et al 6 Peptic ulcer rebleeding is the most important predictor of mortality 1. BMJ 1947; 2: 441 -446 Van Leerdam et al. Am J Gastroenterol 2003; 98: 1494 -1499 2. BMJ 1970; 2: 7 -14 3. BMJ 1973; 3: 655 -660 4. Postgrad Med J 1987; 57: 627 -632 5. Postgrad Med J 1989; 65: 913 -917 6. BMJ 1995; 311: 222 -226
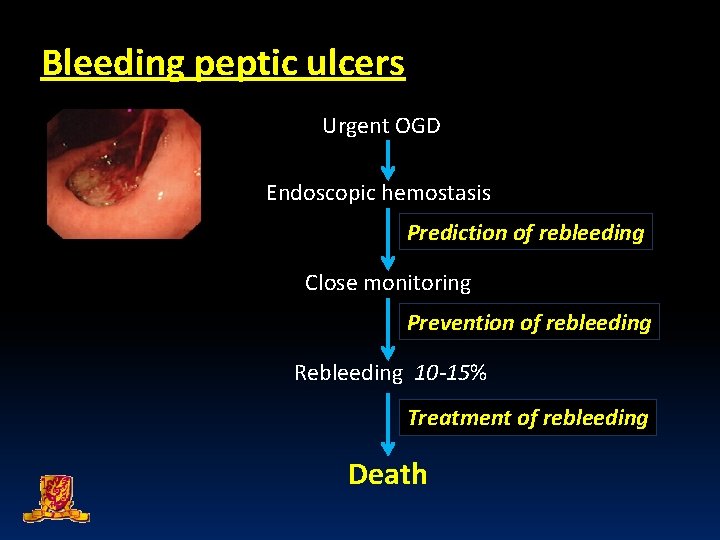
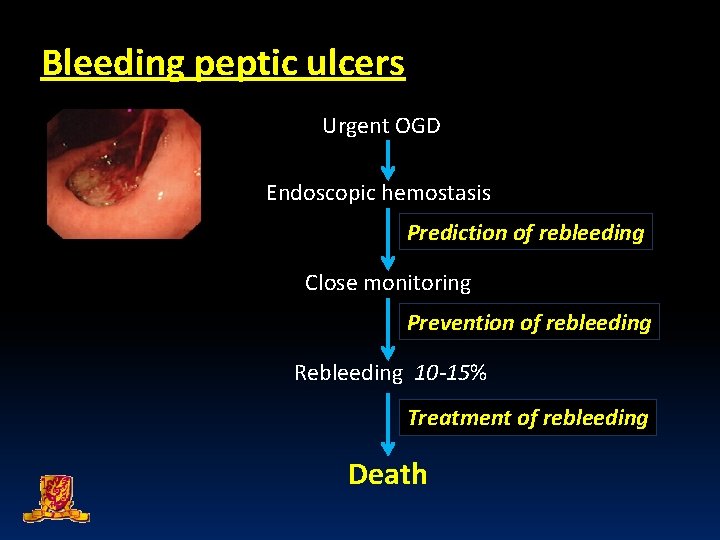
Bleeding peptic ulcers Urgent OGD Endoscopic hemostasis Prediction of rebleeding Close monitoring Prevention of rebleeding Rebleeding 10 -15% Treatment of rebleeding Death
Joint Hospital Surgical Grand Round 17 Jan 2009 Peptic Ulcer Rebleeding: An Evidence-based Management P REDICTION OF ULCER REBLEEDING
Q Who are at risk of rebleeding? 10 studies published Evaluation on factors predicting rebleeding after endoscopic hemostasis
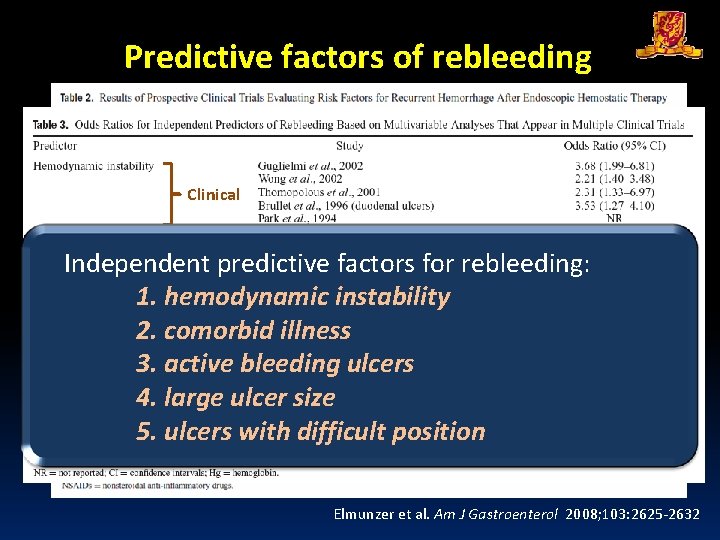
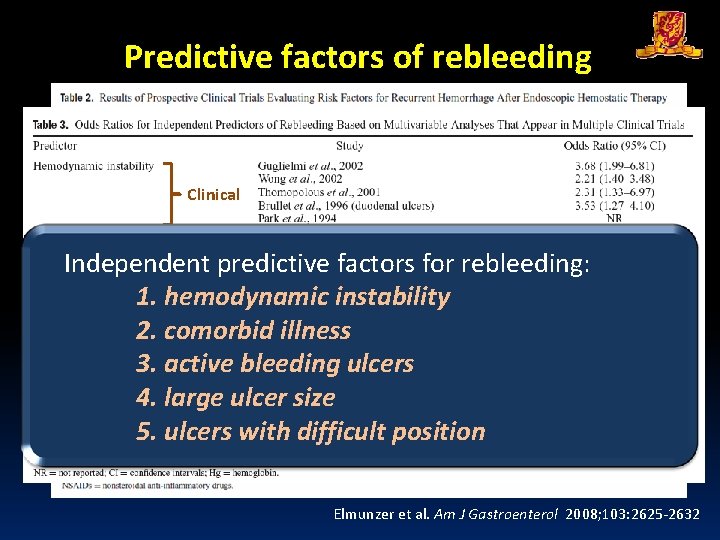
Predictive factors of rebleeding Meta-analysis Clinical Independent predictive factors for rebleeding: 1. hemodynamic instability 2. comorbid Endoscopic illness 3. active bleeding ulcers 4. large ulcer size 5. ulcers with difficult position Elmunzer et al. Am J Gastroenterol 2008; 103: 2625 -2632
Joint Hospital Surgical Grand Round 17 Jan 2009 Peptic Ulcer Rebleeding: An Evidence-based Management P REVENTION OF ULCER REBLEEDING
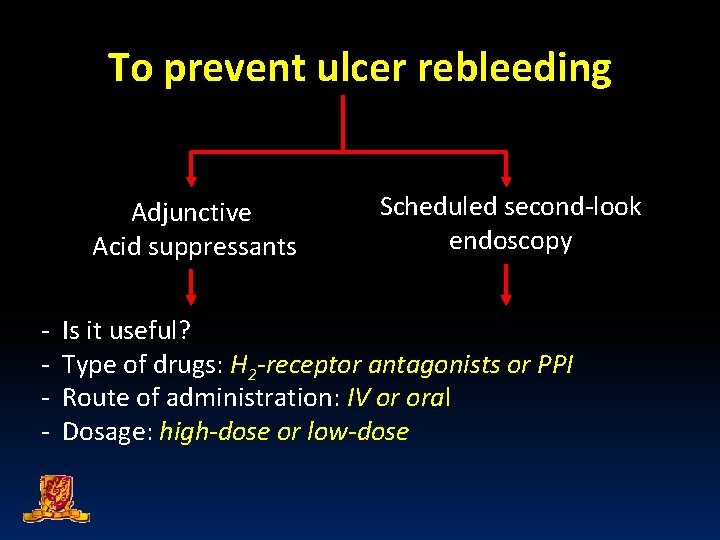
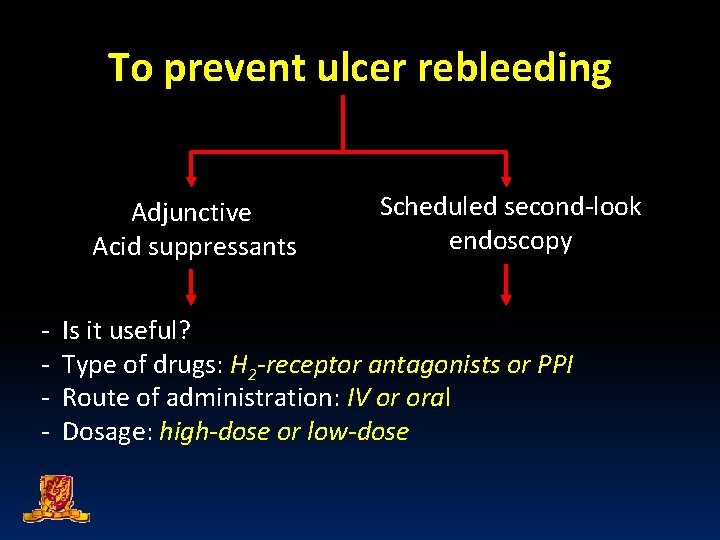
To prevent ulcer rebleeding Adjunctive Acid suppressants - Scheduled second-look endoscopy Is it useful? Type of drugs: H 2 -receptor antagonists or PPI Route of administration: IV or oral Dosage: high-dose or low-dose
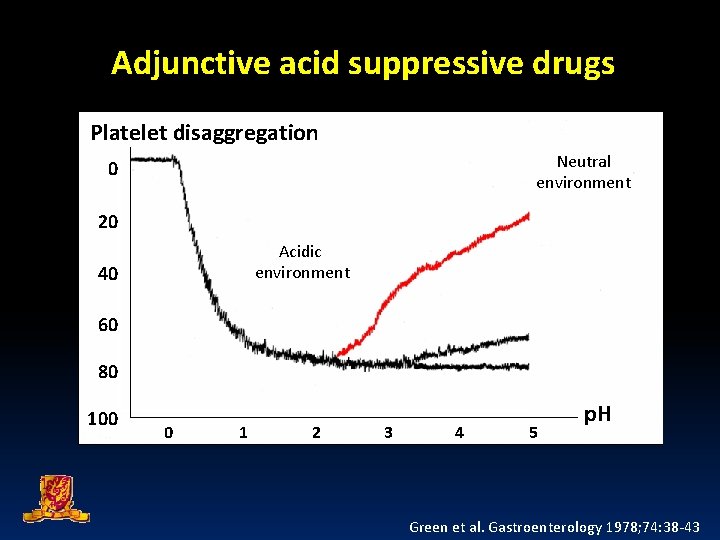
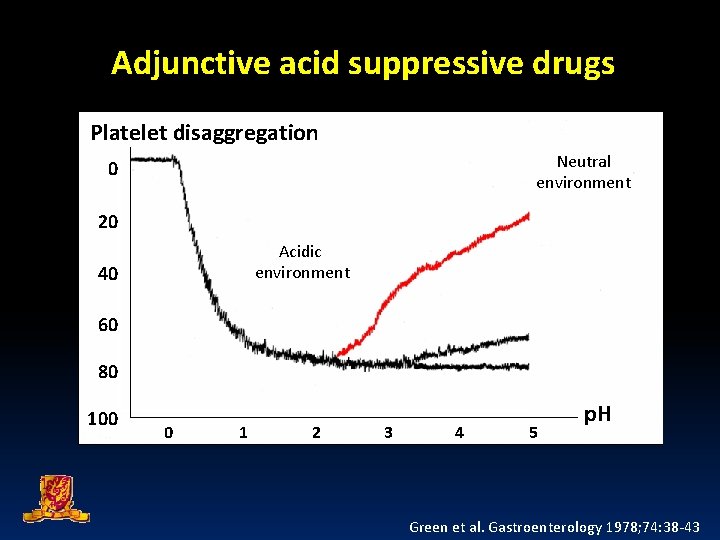
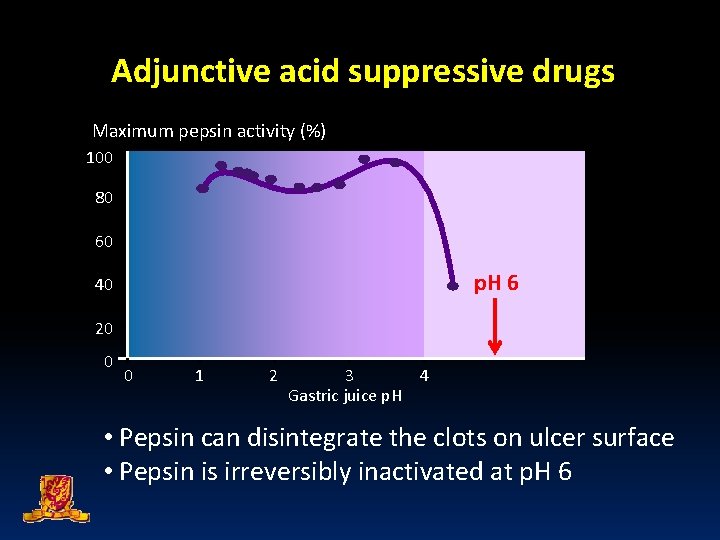
Adjunctive acid suppressive drugs Platelet disaggregation Neutral environment 0 20 Acidic environment 40 60 80 100 0 1 2 3 4 5 p. H Green et al. Gastroenterology 1978; 74: 38 -43
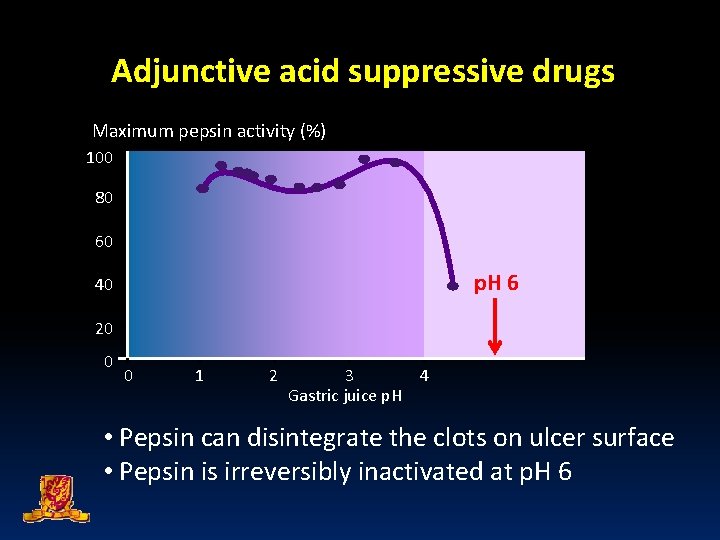
Adjunctive acid suppressive drugs Maximum pepsin activity (%) 100 80 60 p. H 6 40 20 0 0 1 2 3 4 Gastric juice p. H • Pepsin can disintegrate the clots on ulcer surface • Pepsin is irreversibly inactivated at p. H 6
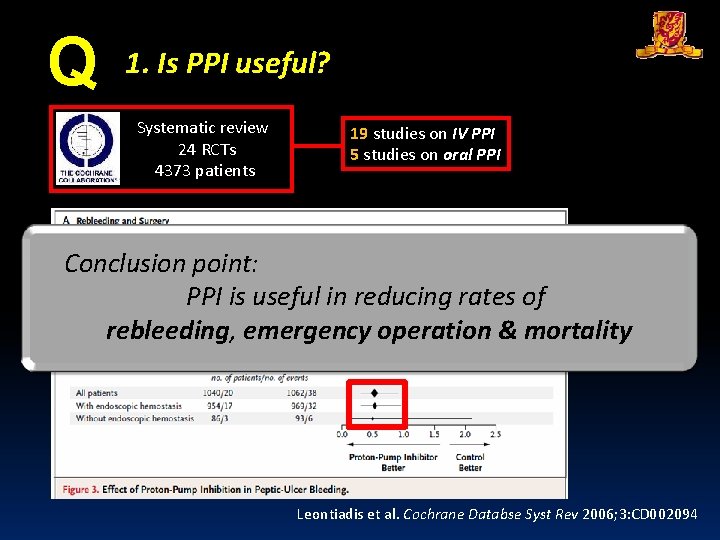
Q 1. Is acid suppressive drugs useful? 24 RCT published Comparison of PPI to placebo in preventing rebleeding
First RCT on PPI vs placebo Daneshmend et al. Br Med J 1992; 304: 143 -147
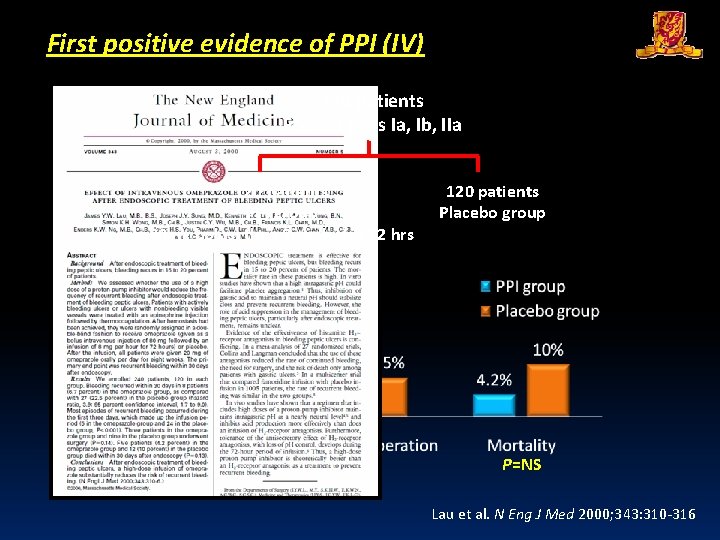
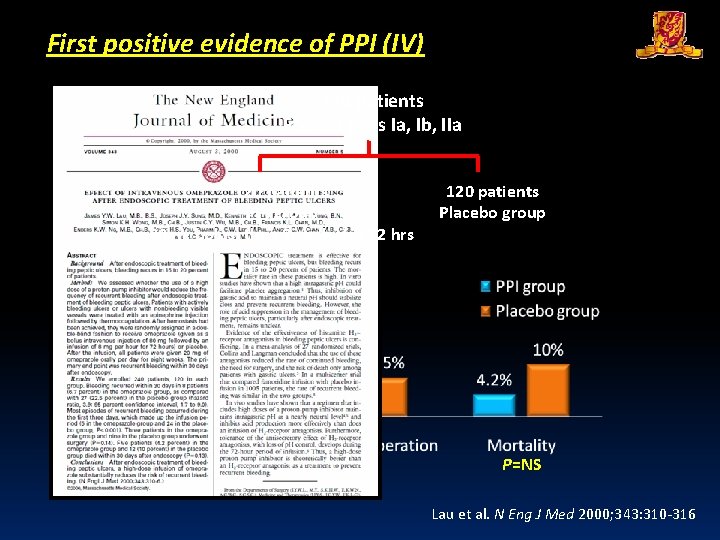
First positive evidence of PPI (IV) 240 patients Forrest class Ia, Ib, IIa 120 patients PPI group 80 mg bolus, then 8 mg/hr for 72 hrs P<0. 001 P=NS 120 patients Placebo group P=NS Lau et al. N Eng J Med 2000; 343: 310 -316
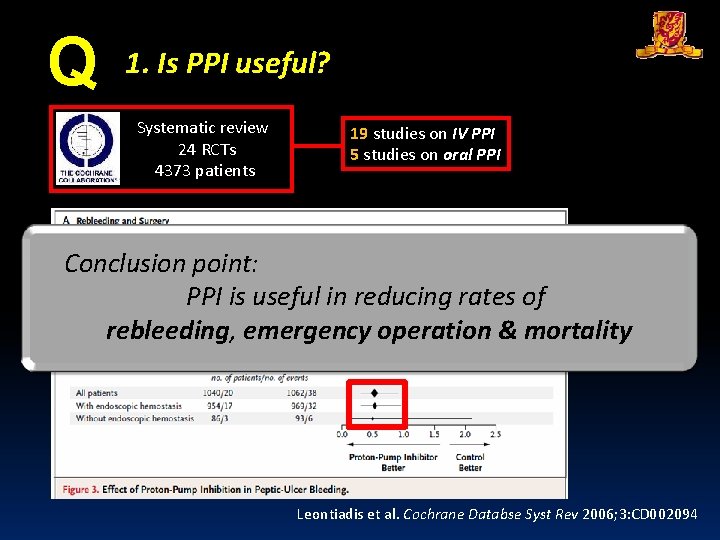
Q 1. Is PPI useful? Systematic review 24 RCTs 4373 patients 19 studies on IV PPI 5 studies on oral PPI Conclusion point: PPI is useful in reducing rates of rebleeding, emergency operation & mortality Leontiadis et al. Cochrane Databse Syst Rev 2006; 3: CD 002094
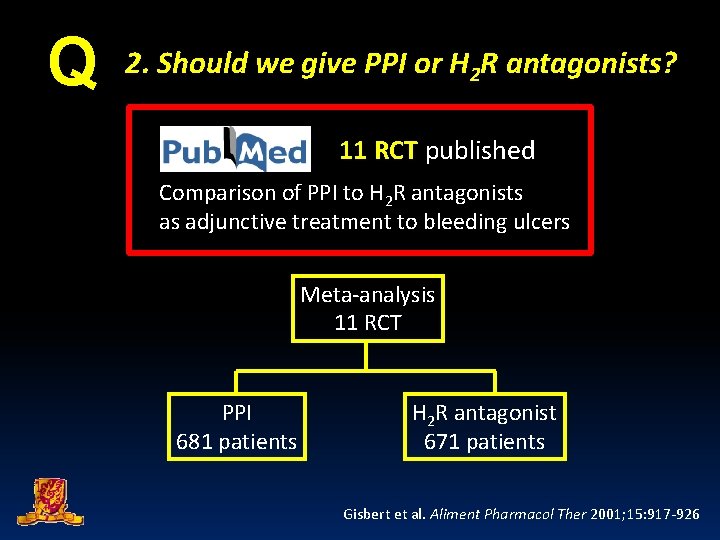
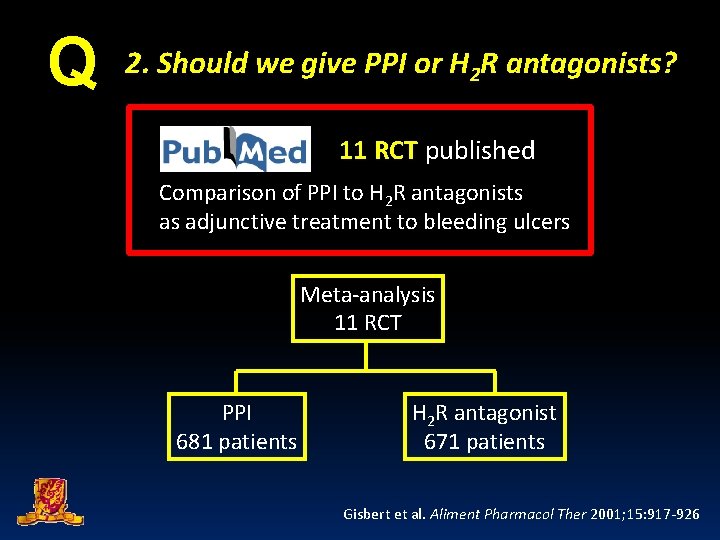
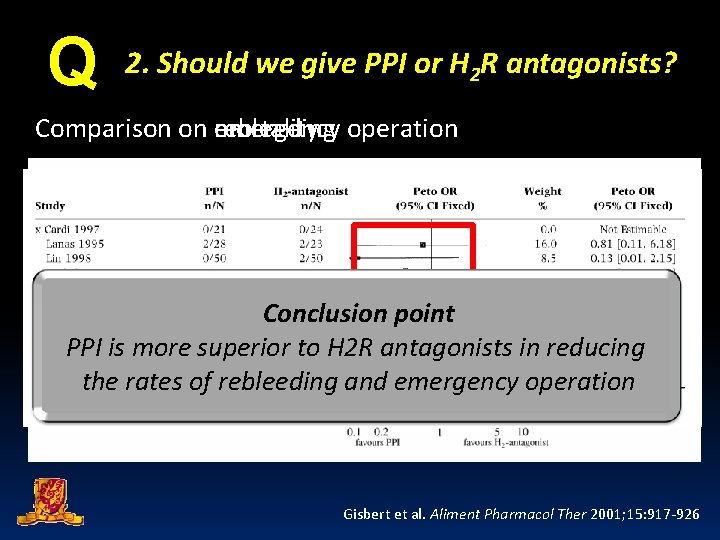
Q 2. Should we give PPI or H 2 R antagonists? 11 RCT published Comparison of PPI to H 2 R antagonists as adjunctive treatment to bleeding ulcers Meta-analysis 11 RCT PPI 681 patients H 2 R antagonist 671 patients Gisbert et al. Aliment Pharmacol Ther 2001; 15: 917 -926
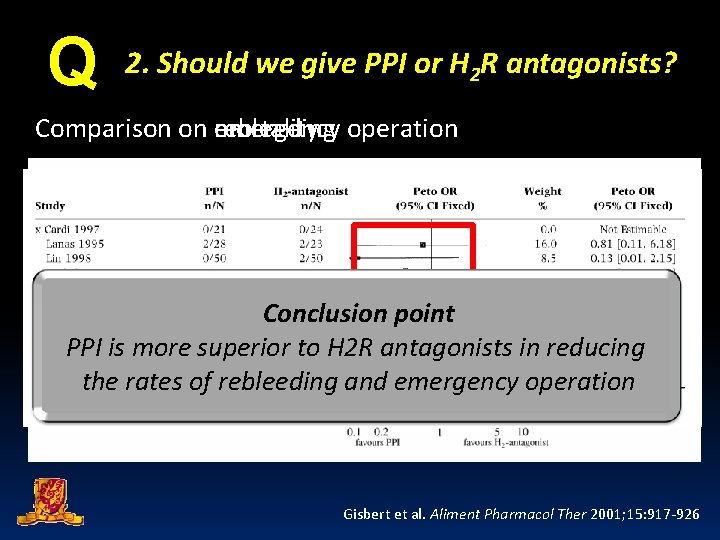
Q 2. Should we give PPI or H 2 R antagonists? mortality operation Comparison on emergency rebleeding Conclusion point PPI is more superior to H 2 R antagonists in reducing the rates of rebleeding and emergency operation Gisbert et al. Aliment Pharmacol Ther 2001; 15: 917 -926
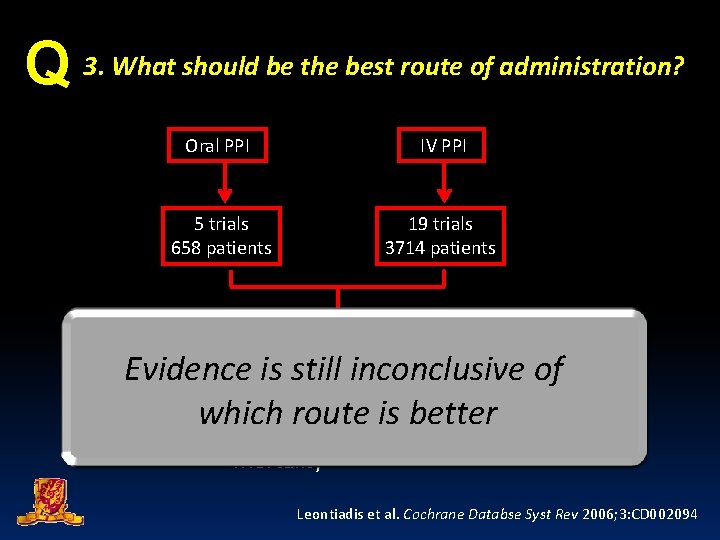
Q 3. What should be the best route of administration? 0 RCT published No RCT performed on direct comparison of oral versus IV PPI
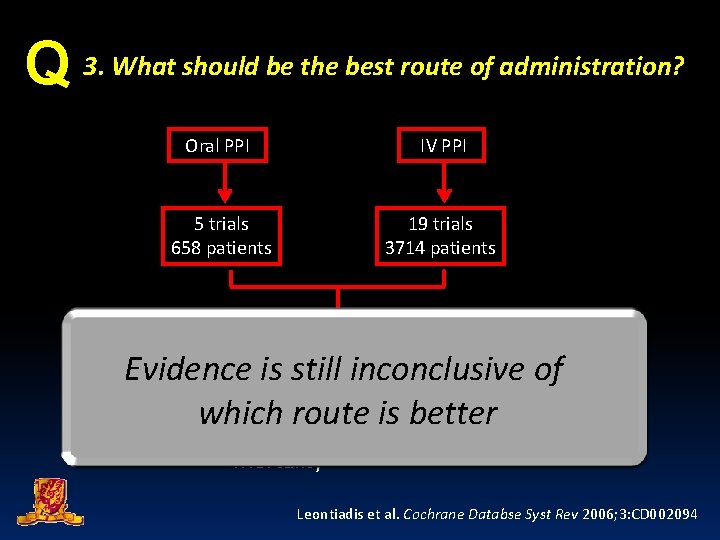
Q 3. What should be the best route of administration? Oral PPI IV PPI 5 trials 658 patients 19 trials 3714 patients Meta-regression analysis: Evidence is still on inconclusive No difference - Rebleeding which route is better - Emergency operation - Mortality of Leontiadis et al. Cochrane Databse Syst Rev 2006; 3: CD 002094
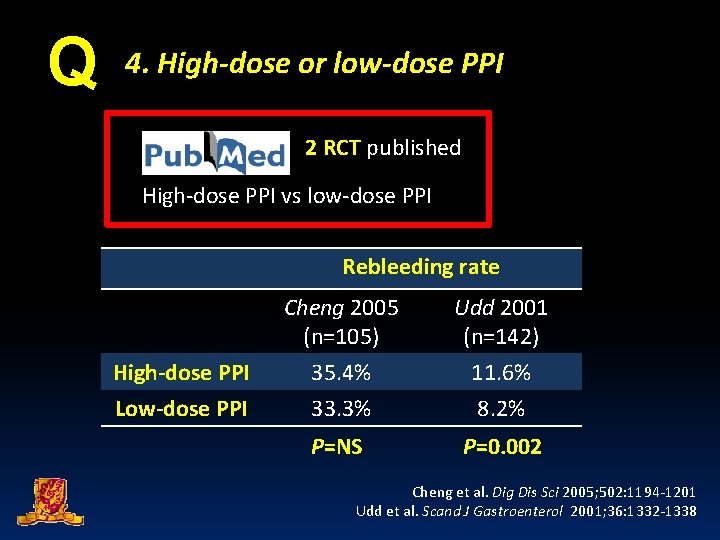
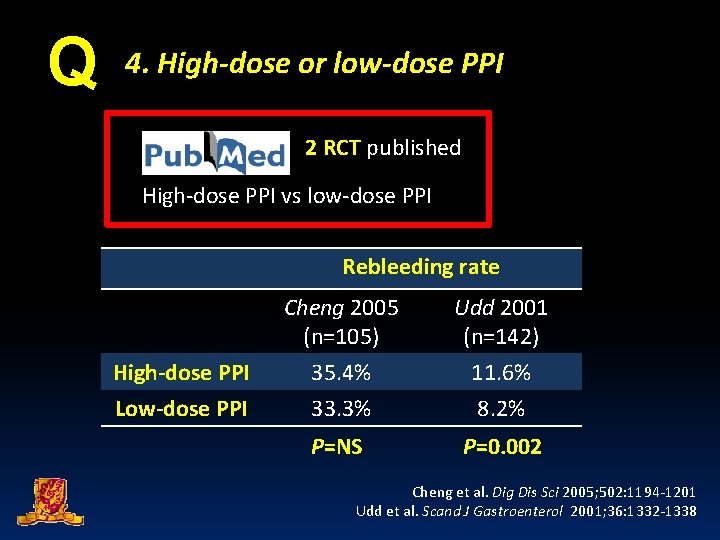
Q 4. High-dose or low-dose PPI 2 RCT published High-dose PPI vs low-dose PPI Rebleeding rate High-dose PPI Low-dose PPI Cheng 2005 (n=105) Udd 2001 (n=142) 35. 4% 33. 3% 11. 6% 8. 2% P=NS P=0. 002 Cheng et al. Dig Dis Sci 2005; 502: 1194 -1201 Udd et al. Scand J Gastroenterol 2001; 36: 1332 -1338
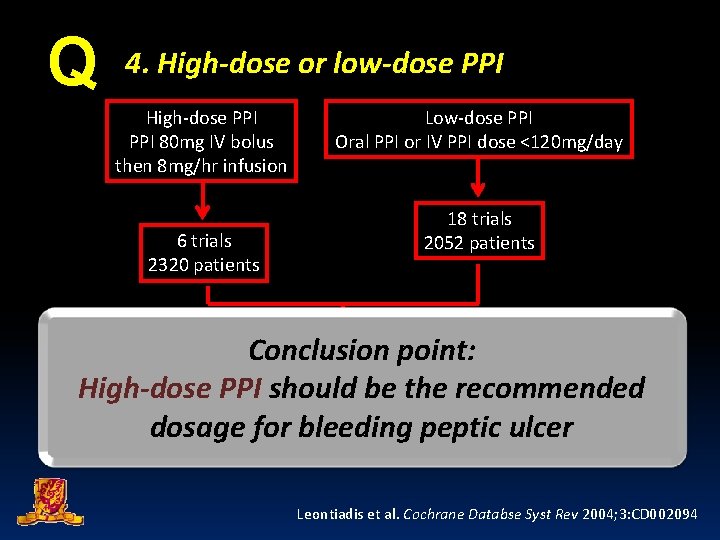
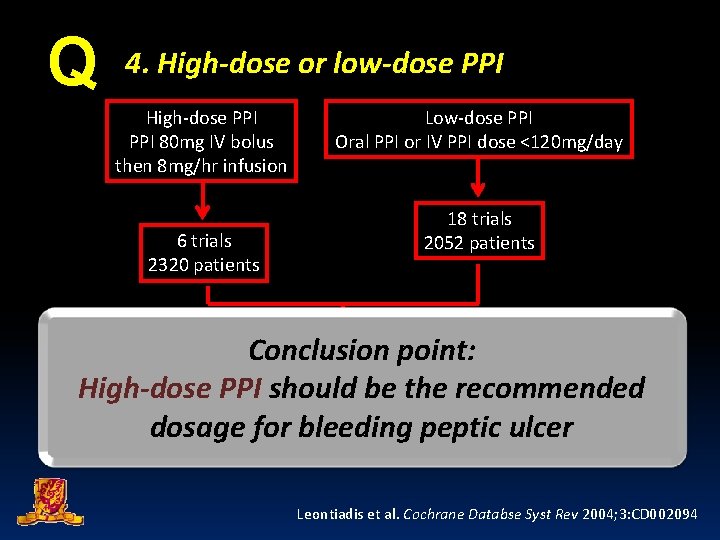
Q 4. High-dose or low-dose PPI High-dose PPI 80 mg IV bolus then 8 mg/hr infusion 6 trials 2320 patients Low-dose PPI Oral PPI or IV PPI dose <120 mg/day 18 trials 2052 patients Conclusion point: Emergency surgery Rebleeding High-dose PPI bereduced the recommended 36/1149 (3. 1%) 59/1171 (5. 0%) Both should significantly Only high-dose PPIbleeding significantly reduce the need dosage for peptic ulcer OR=0. 61, 95% C. I. 0. 40 -0. 93, P=0. 02 Leontiadis et al. Cochrane Databse Syst Rev 2004; 3: CD 002094
To prevent ulcer rebleeding Adjunctive Acid suppressants Scheduled second-look endoscopy Is it useful ?
Scheduled second-look endoscopy Rationale – To treat before clinical rebleeding occurs – To perform second-look OGD within 16 – 24 hours after primary endoscopic hemostasis Villanueva et al. Gastrointest Endosc 1994; 40: 34 -39 Saeed et al. Endoscopy 1996; 28: 288 -294 Rutgeerts et al. Lancet 1997; 350: 692 -696 Messmann et al. Endoscopy 1998; 30: 583 -589 Chiu et al. Gut 2003; 52: 1403 -1407
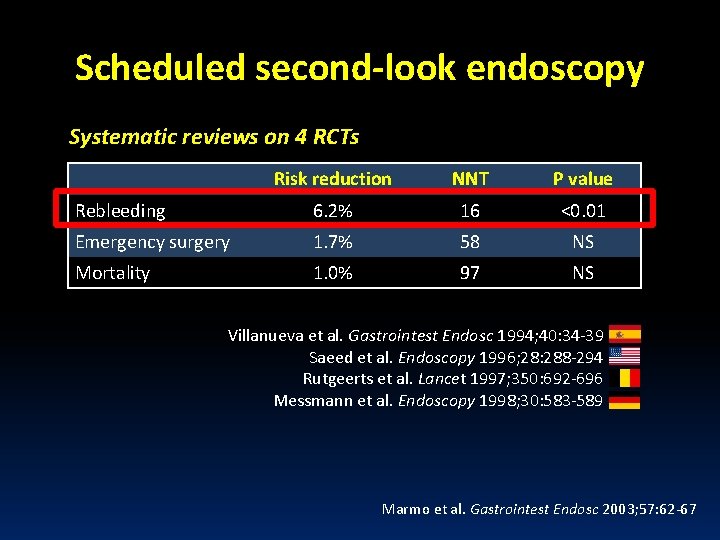
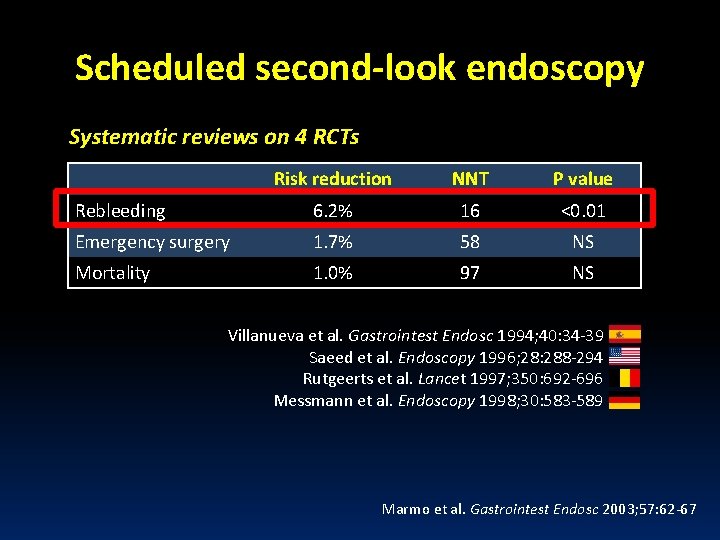
Scheduled second-look endoscopy Systematic reviews on 4 RCTs Risk reduction NNT P value Rebleeding 6. 2% 16 <0. 01 Emergency surgery 1. 7% 58 NS Mortality 1. 0% 97 NS Villanueva et al. Gastrointest Endosc 1994; 40: 34 -39 Saeed et al. Endoscopy 1996; 28: 288 -294 Rutgeerts et al. Lancet 1997; 350: 692 -696 Messmann et al. Endoscopy 1998; 30: 583 -589 Marmo et al. Gastrointest Endosc 2003; 57: 62 -67
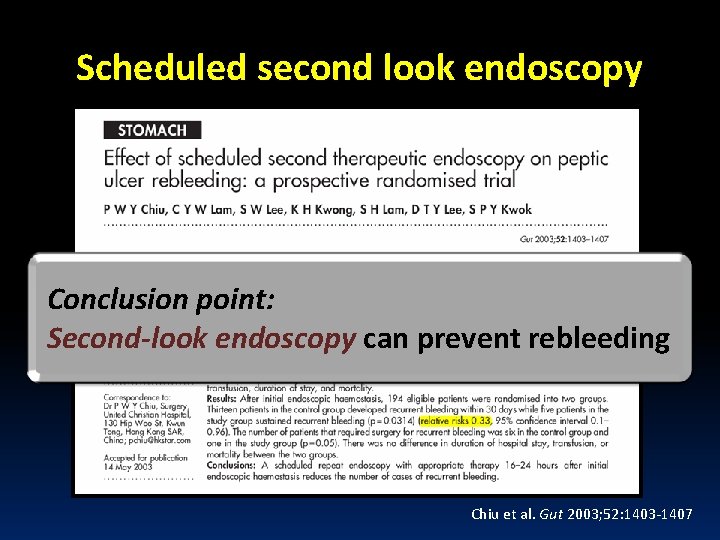
Scheduled second look endoscopy Forrest class Ia to IIb bleeding ulcers Conclusion point: Second-look endoscopy can prevent rebleeding P=0. 03 P=0. 05 P=NS Chiu et al. Gut 2003; 52: 1403 -1407
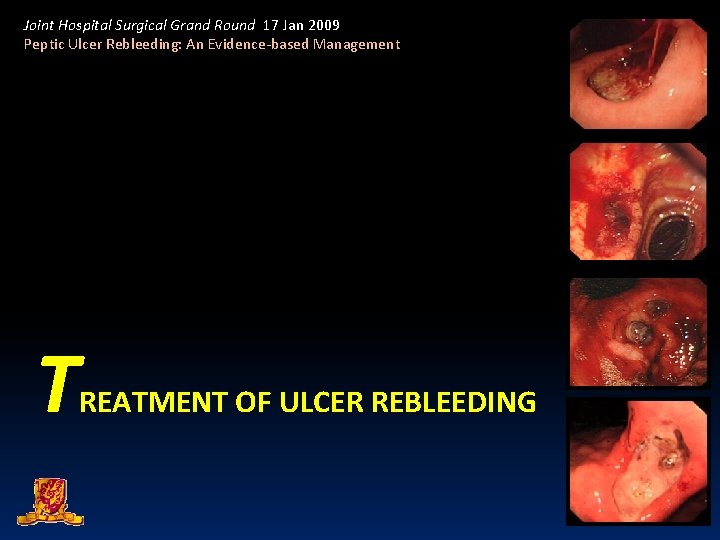
Joint Hospital Surgical Grand Round 17 Jan 2009 Peptic Ulcer Rebleeding: An Evidence-based Management T REATMENT OF ULCER REBLEEDING
Q How to treat rebleeding? A. Endoscopic re-treatment B. Immediate surgery C. Angiographic embolization What is the best treatment option? What type of emergency operations to perform?
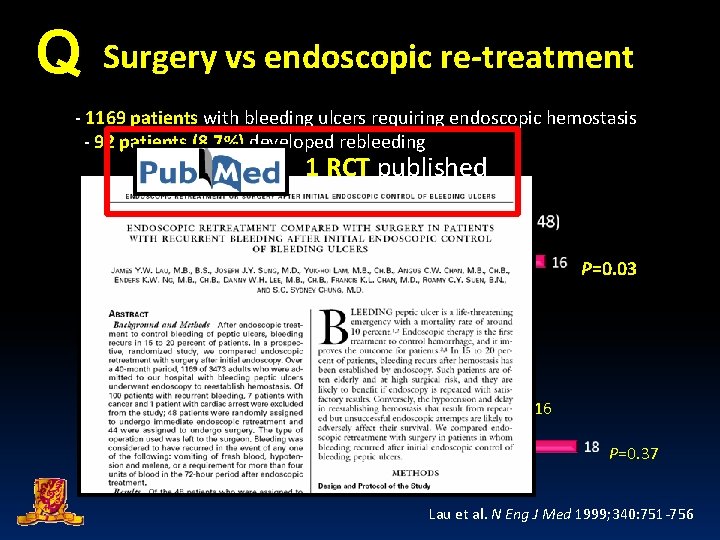
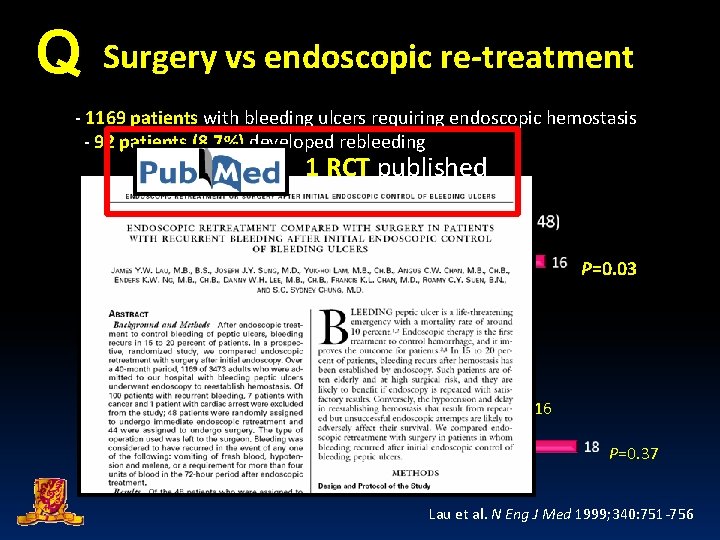
Q Surgery vs endoscopic re-treatment - 1169 patients with bleeding ulcers requiring endoscopic hemostasis - 92 patients (8. 7%) developed rebleeding 1 RCT published P=0. 03 P=0. 27 P=0. 59 P=0. 16 P=0. 37 Lau et al. N Eng J Med 1999; 340: 751 -756
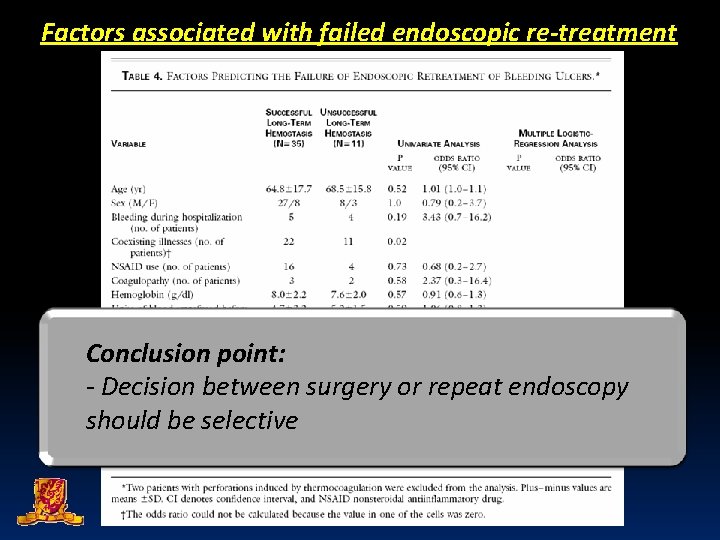
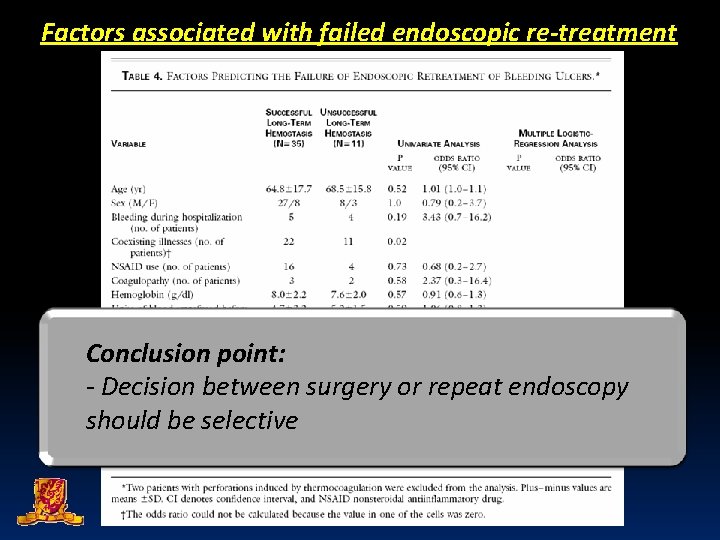
Factors associated with failed endoscopic re-treatment Conclusion point: - Decision between surgery or repeat endoscopy should be selective
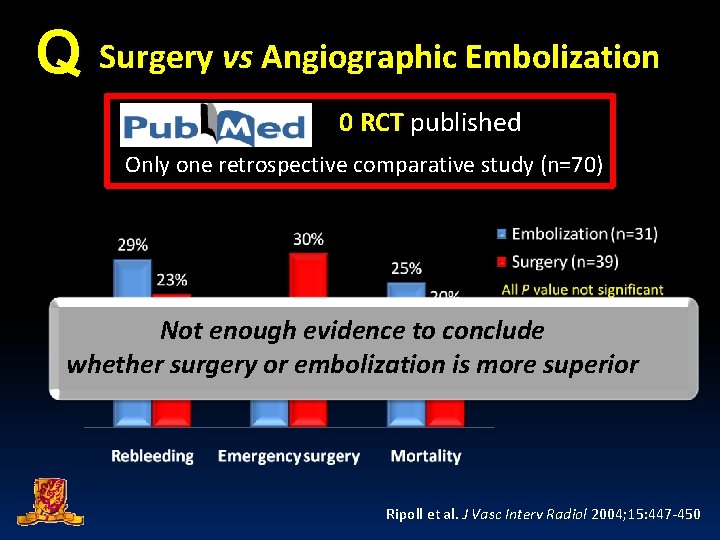
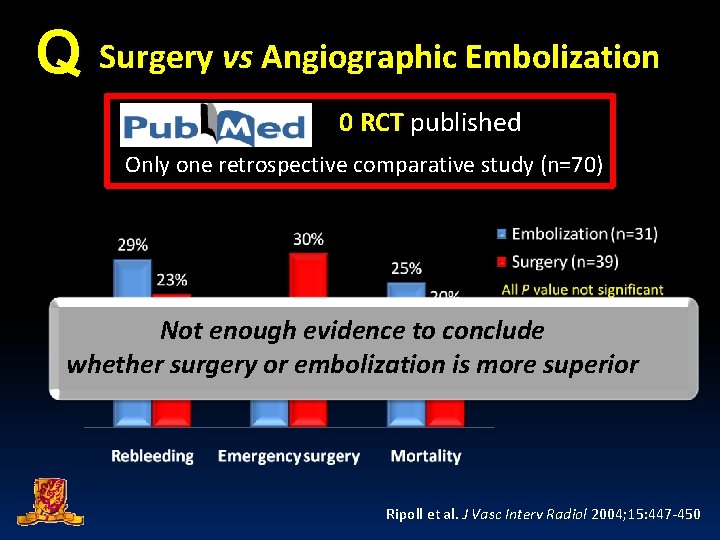
Q Surgery vs Angiographic Embolization 0 RCT published Only one retrospective comparative study (n=70) Not enough evidence to conclude whether surgery or embolization is more superior Ripoll et al. J Vasc Interv Radiol 2004; 15: 447 -450
Q Angiographic embolization vs endoscopic re-treatment 0 RCT published No RCT evidence to compare angiographic embolization to repeat endoscopy
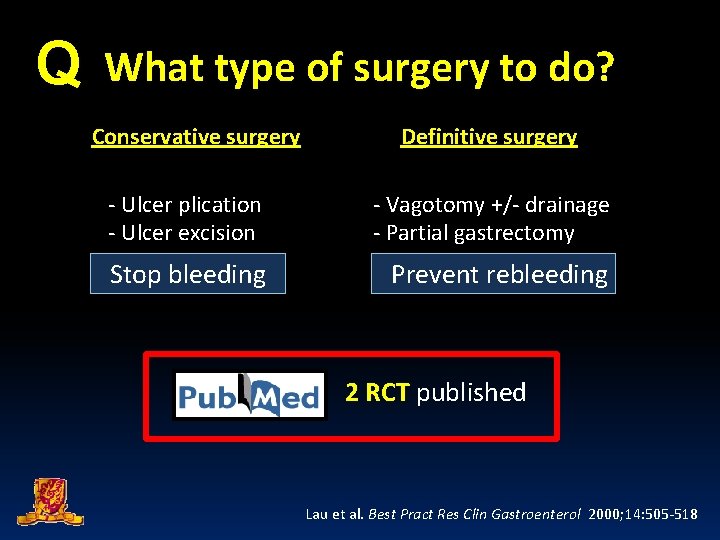
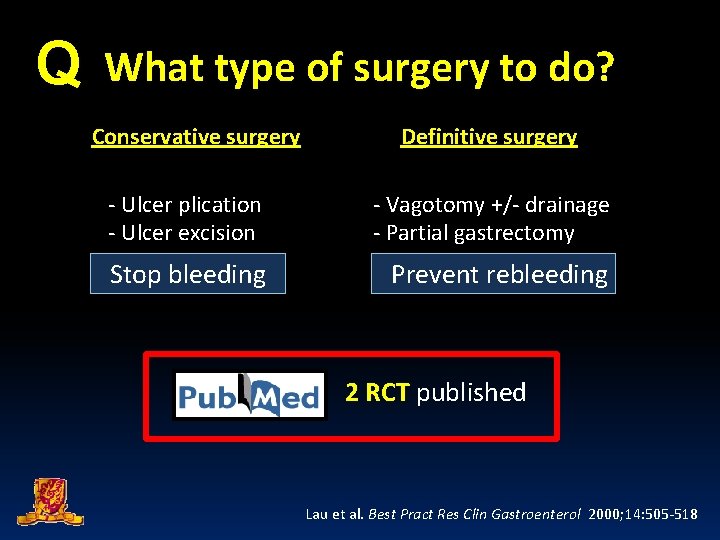
Q What type of surgery to do? Conservative surgery Definitive surgery - Ulcer plication - Ulcer excision - Vagotomy +/- drainage - Partial gastrectomy Stop bleeding Prevent rebleeding 2 RCT published Lau et al. Best Pract Res Clin Gastroenterol 2000; 14: 505 -518
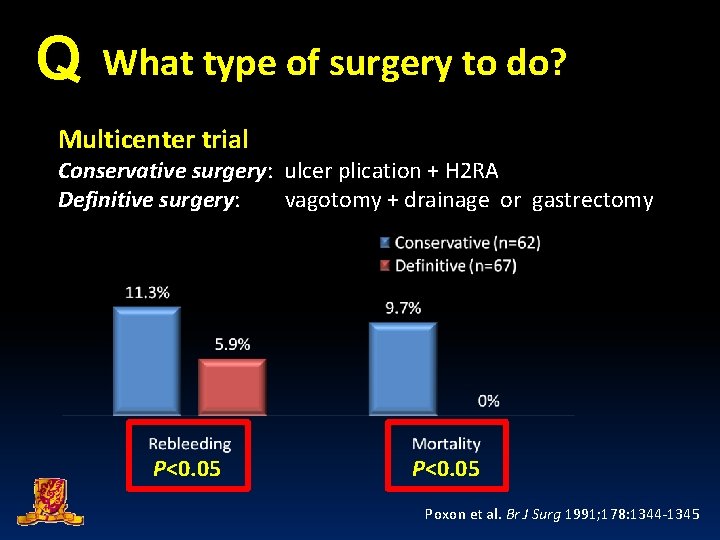
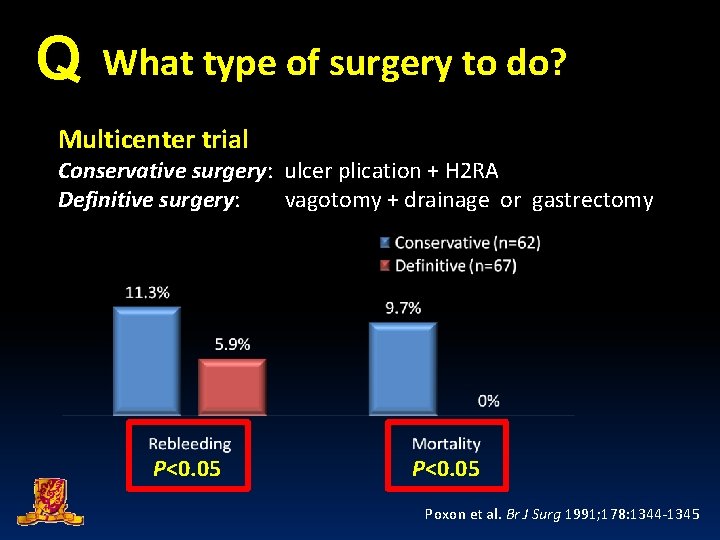
Q What type of surgery to do? Multicenter trial Conservative surgery: ulcer plication + H 2 RA Definitive surgery: vagotomy + drainage or gastrectomy P<0. 05 Poxon et al. Br J Surg 1991; 178: 1344 -1345
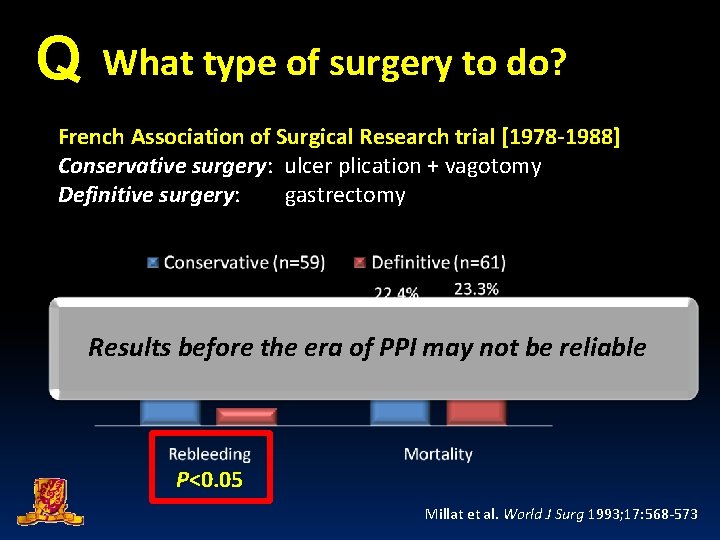
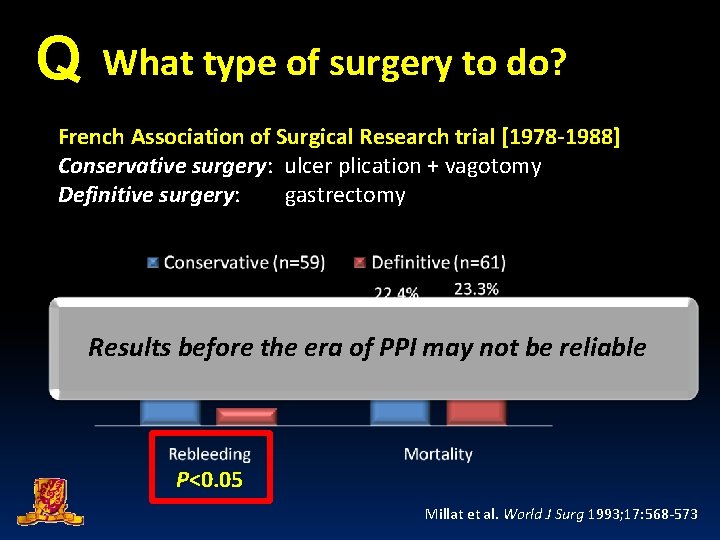
Q What type of surgery to do? French Association of Surgical Research trial [1978 -1988] Conservative surgery: ulcer plication + vagotomy Definitive surgery: gastrectomy Results before the era of PPI may not be reliable P<0. 05 Millat et al. World J Surg 1993; 17: 568 -573
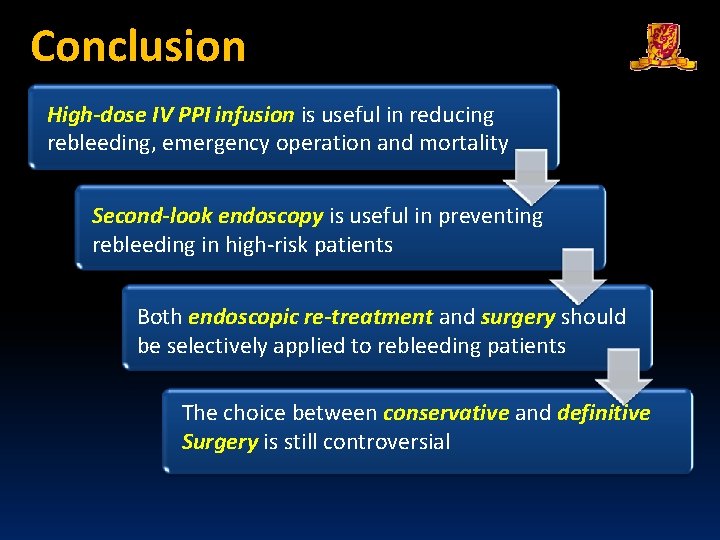
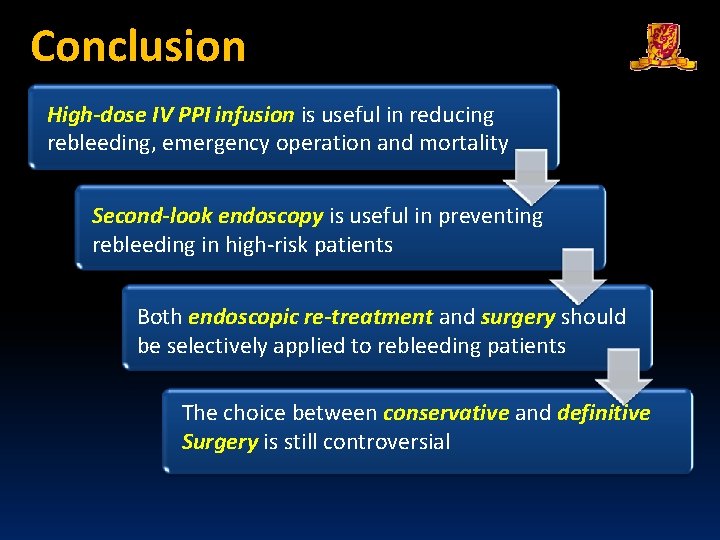
Conclusion High-dose IV PPI infusion is useful in reducing rebleeding, emergency operation and mortality Second-look endoscopy is useful in preventing rebleeding in high-risk patients Both endoscopic re-treatment and surgery should be selectively applied to rebleeding patients The choice between conservative and definitive Surgery is still controversial
Department of Surgery The Chinese University of Hong Kong
 Joint hospital surgical grand round
Joint hospital surgical grand round Tmh
Tmh Esophgeal varices
Esophgeal varices Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round January 2016 chemistry regents answers
January 2016 chemistry regents answers 9 months before january 26 2009
9 months before january 26 2009 Imaging at lafayette surgical specialty hospital
Imaging at lafayette surgical specialty hospital Inet wellspan
Inet wellspan December round the world
December round the world Ground round hospital
Ground round hospital Hospital pharmacy organization
Hospital pharmacy organization External occipital protuberance
External occipital protuberance A grade lamb
A grade lamb Hinge joint
Hinge joint Permanent joints
Permanent joints Memorandum joint venture account
Memorandum joint venture account Break joint vs spool joint
Break joint vs spool joint Diagnostic suffixes
Diagnostic suffixes Basic surgical techniques semmelweis
Basic surgical techniques semmelweis Avagard surgical scrub instructions
Avagard surgical scrub instructions Conclusion of medical surgical nursing
Conclusion of medical surgical nursing Which suffix means to break or surgical fracture?
Which suffix means to break or surgical fracture? Surgical metabolism
Surgical metabolism Tatum surgical
Tatum surgical Vitamin abcde surgical sieve
Vitamin abcde surgical sieve Qrc surgical
Qrc surgical Prevention of vte in nonorthopedic surgical patients
Prevention of vte in nonorthopedic surgical patients Congenital flat foot
Congenital flat foot Lyphadenitis
Lyphadenitis Managing surgical smoke
Managing surgical smoke Surgical audit examples
Surgical audit examples What part of the surgical gown is considered sterile
What part of the surgical gown is considered sterile Surgical bandage types
Surgical bandage types Voluntary surgical contraception
Voluntary surgical contraception