Joint Hospital Surgical Grand Round 18 Apr 2009

- Slides: 31
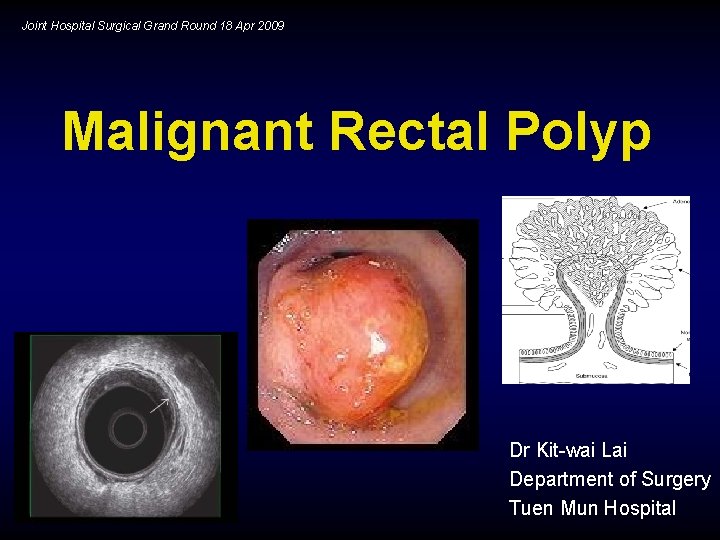
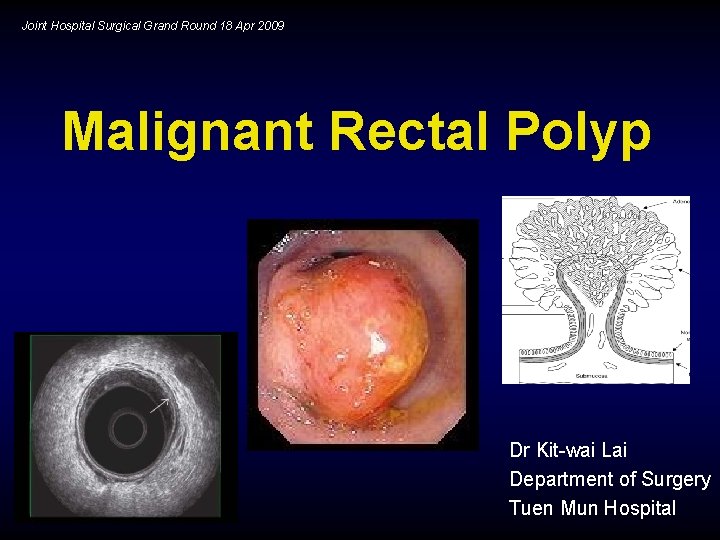
Joint Hospital Surgical Grand Round 18 Apr 2009 Malignant Rectal Polyp Dr Kit-wai Lai Department of Surgery Tuen Mun Hospital
Malignant Rectal Polyp • Polyps with cancer cells penetrating the muscularis mucosa • Invasion limited to submucosa • i. e. T 1 lesion
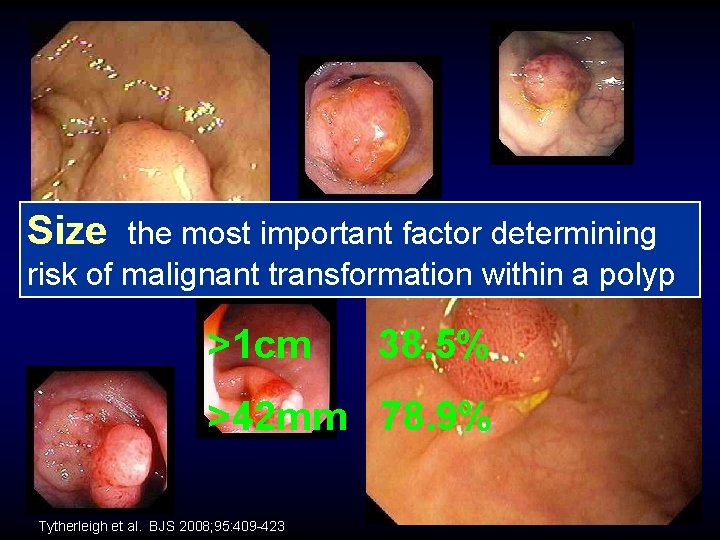
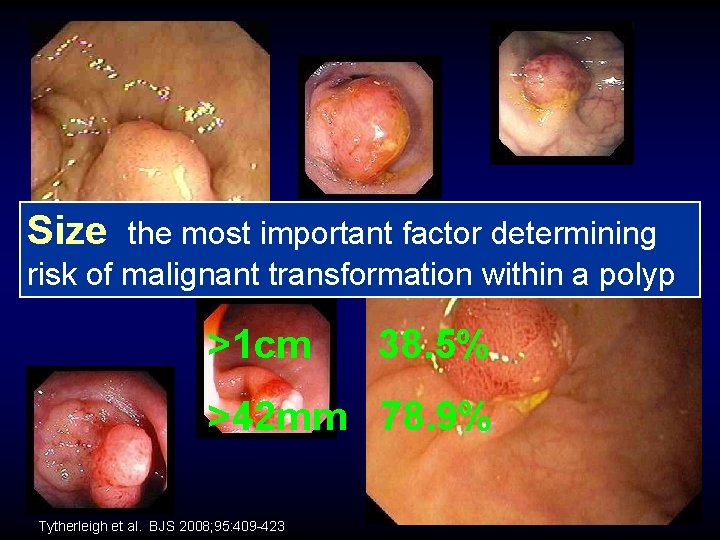
Size Malignant? the most important factor determining risk of malignant transformation within a polyp >1 cm 38. 5% >42 mm 78. 9% Tytherleigh et al. BJS 2008; 95: 409 -423
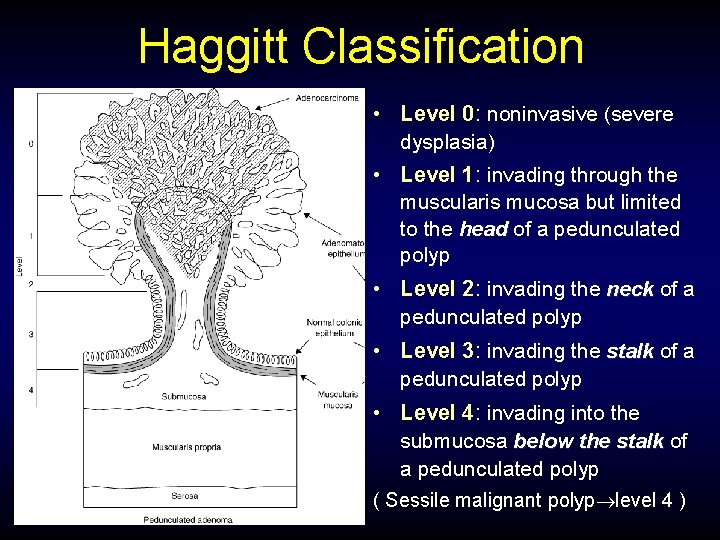
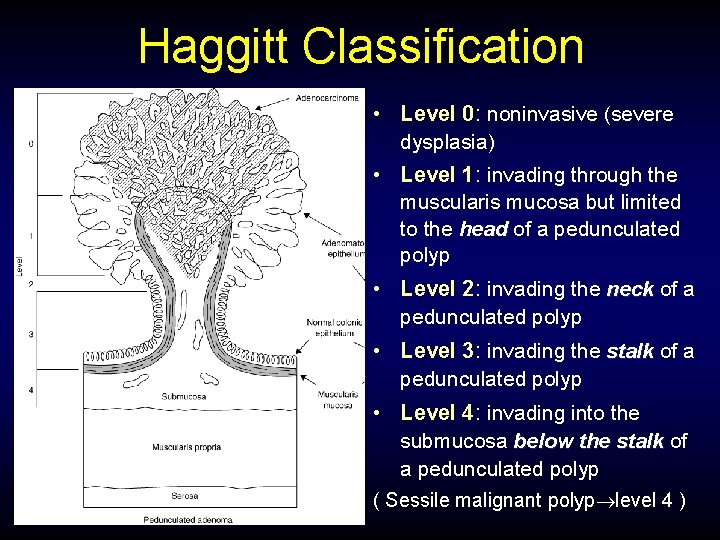
Haggitt Classification • Level 0: noninvasive (severe dysplasia) • Level 1: invading through the muscularis mucosa but limited to the head of a pedunculated polyp • Level 2: invading the neck of a pedunculated polyp • Level 3: invading the stalk of a pedunculated polyp • Level 4: invading into the submucosa below the stalk of a pedunculated polyp ( Sessile malignant polyp level 4 )
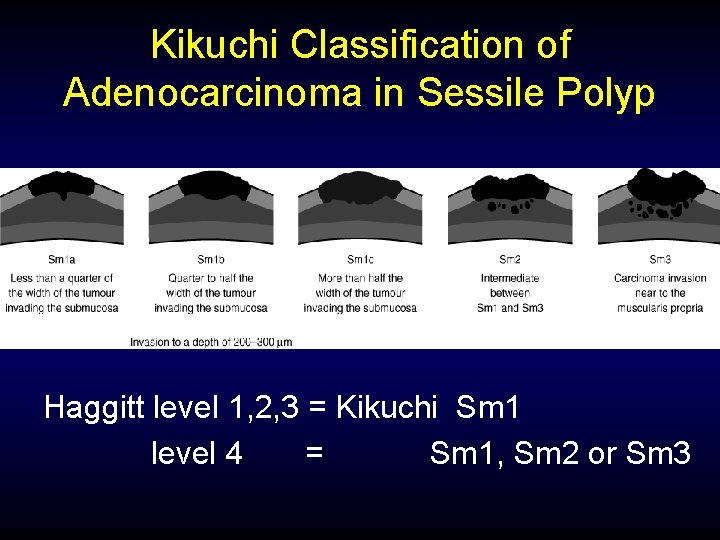
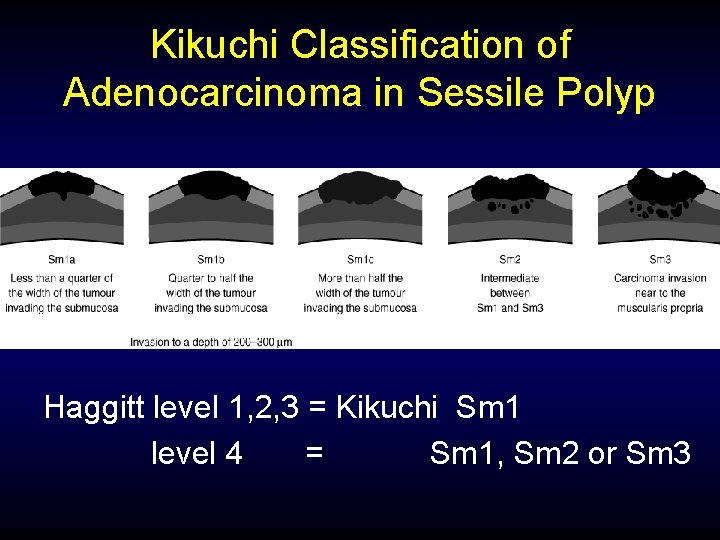
Kikuchi Classification of Adenocarcinoma in Sessile Polyp Haggitt level 1, 2, 3 = Kikuchi Sm 1 level 4 = Sm 1, Sm 2 or Sm 3
Staging is critical to management Histological Assessment Most important factor to predict risk of lymphatic spread Local Therapy Opportunity of cure with less detriment Tytherleigh et al. BJS 2008; 95: 409 -423
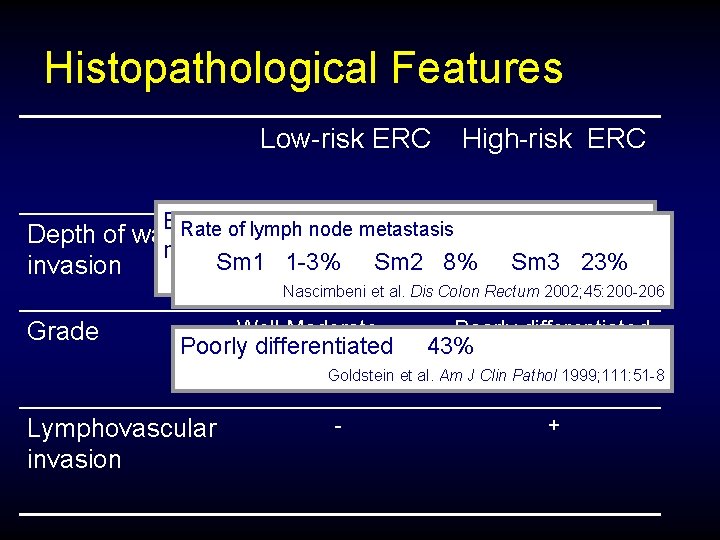
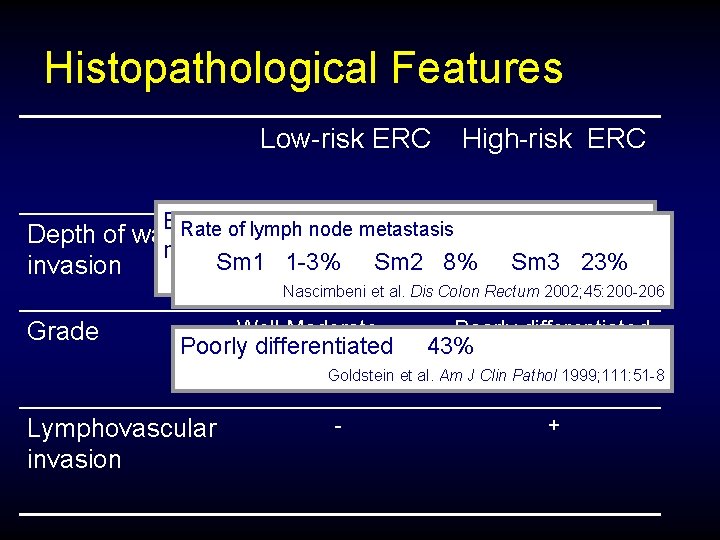
Histopathological Features Low-risk ERC High-risk ERC Best estimate of the probability of regional LN lymph node 1 -3 metastasis. Kikuchi Sm 3 & Depth of wall Rate of. Haggitt metastasis (possibly Sm 2) Sm 1 1 -3% Sm 3 23% Kikuchi Sm 1 &Sm 2 8% invasion Bretagnol et al. Dis Colon Rectum 2007; 50: 523 -533 (possibly Sm 2) Nascimbeni et al. Dis Colon Rectum 2002; 45: 200 -206 Grade Well Moderate Poorlydifferentiated Poorly differentiated 43% Undifferentiated Goldstein et al. Am J Clin Pathol 1999; 111: 51 -8 Lymphovascular invasion - +
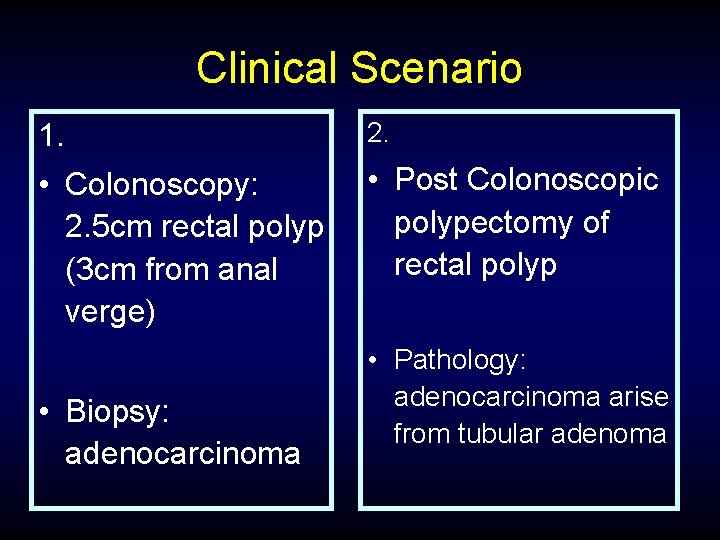
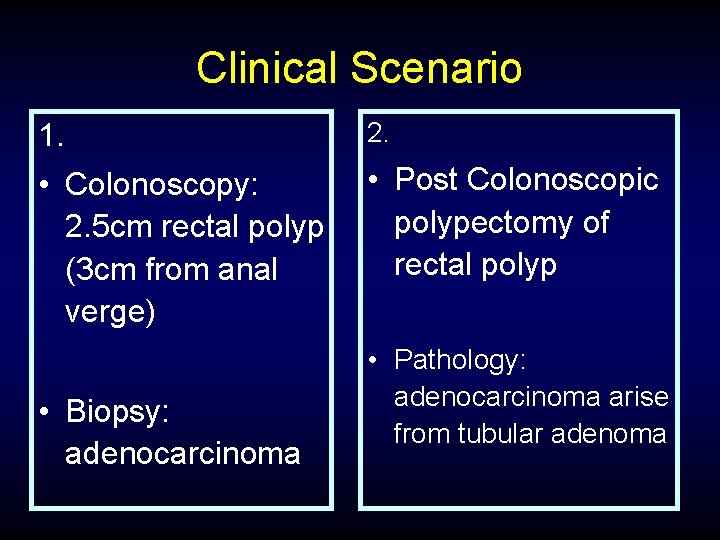
Clinical Scenario 1. 2. • Colonoscopy: 2. 5 cm rectal polyp (3 cm from anal verge) • Post Colonoscopic polypectomy of rectal polyp • Biopsy: adenocarcinoma • Pathology: adenocarcinoma arise from tubular adenoma
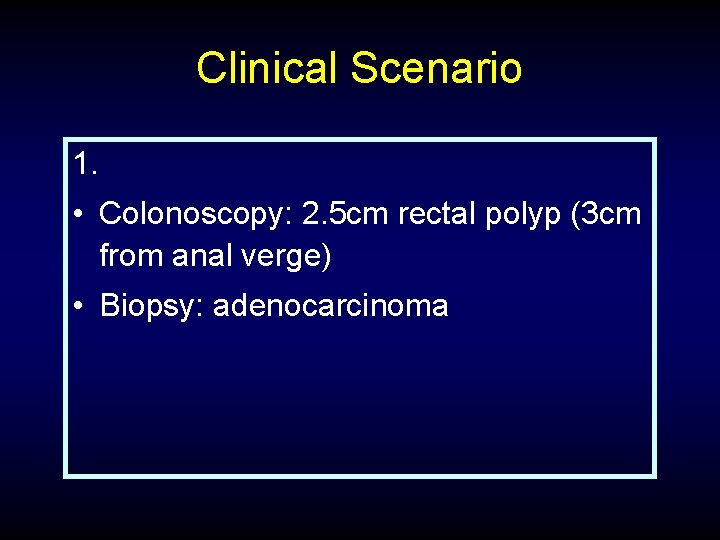
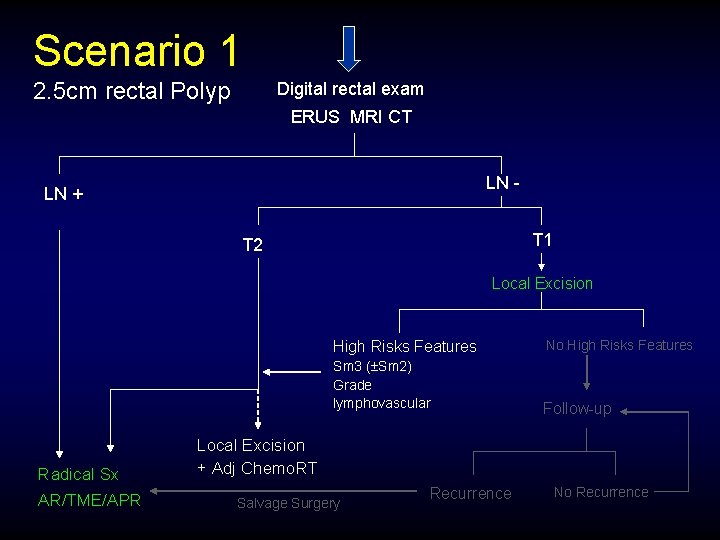
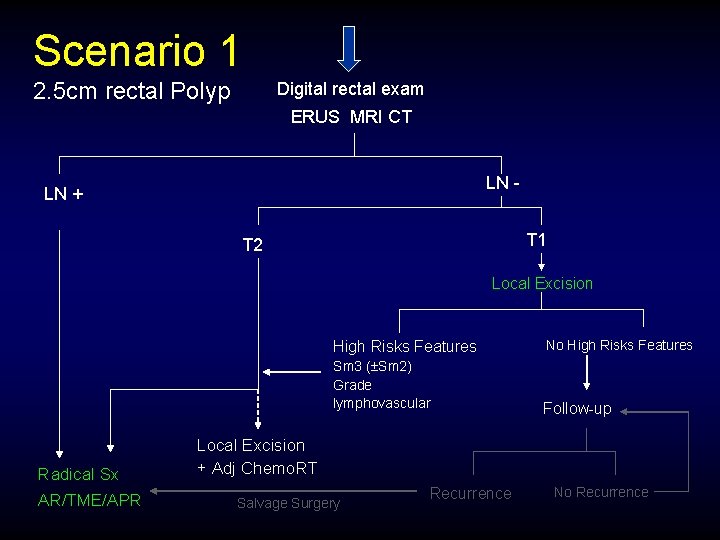
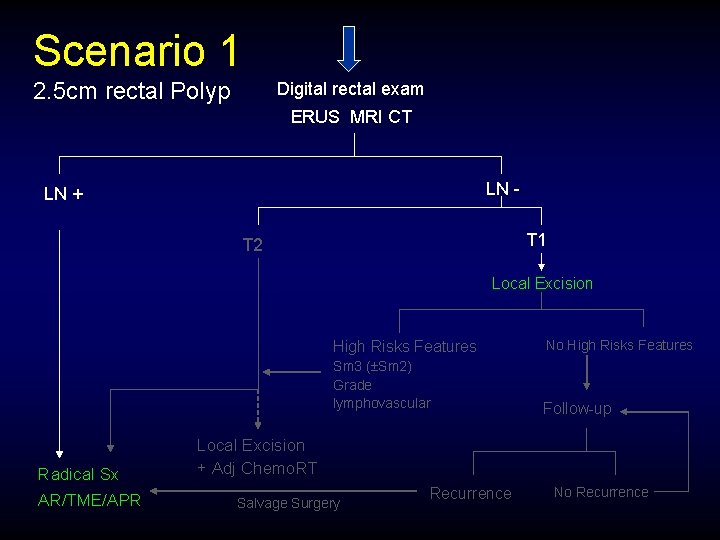
Clinical Scenario 1. • Colonoscopy: 2. 5 cm rectal polyp (3 cm from anal verge) • Biopsy: adenocarcinoma
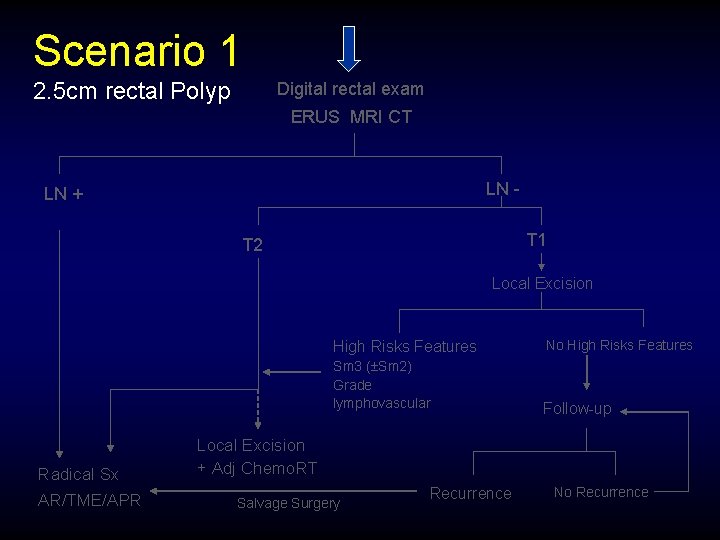
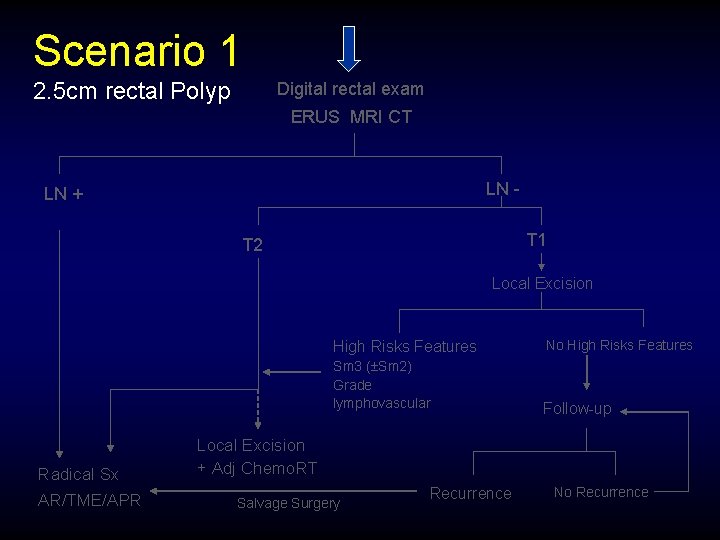
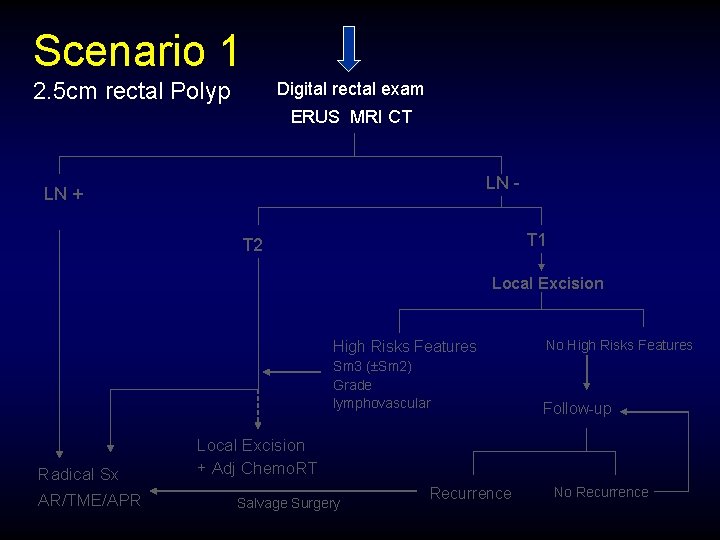
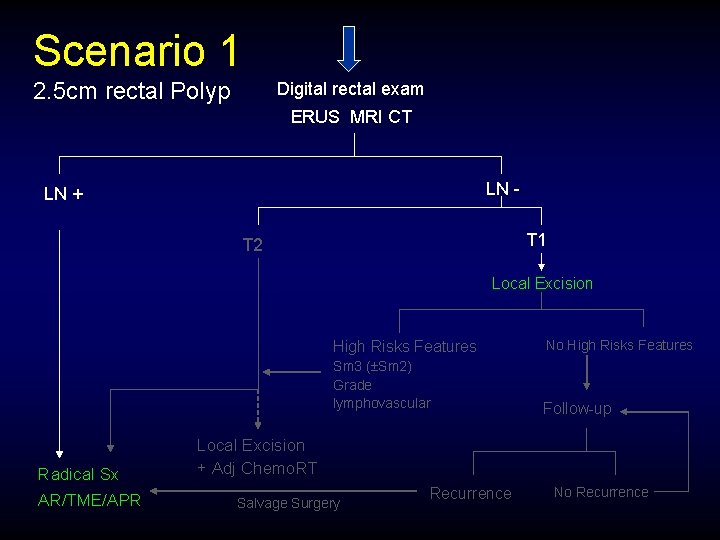
Scenario 1 2. 5 cm rectal Polyp Digital rectal exam ERUS MRI CT LN - LN + T 1 T 2 Local Excision Radical Sx AR/TME/APR High Risks Features No High Risks Features Sm 3 ( Sm 2) Grade lymphovascular Follow-up Local Excision + Adj Chemo. RT Salvage Surgery Recurrence No Recurrence
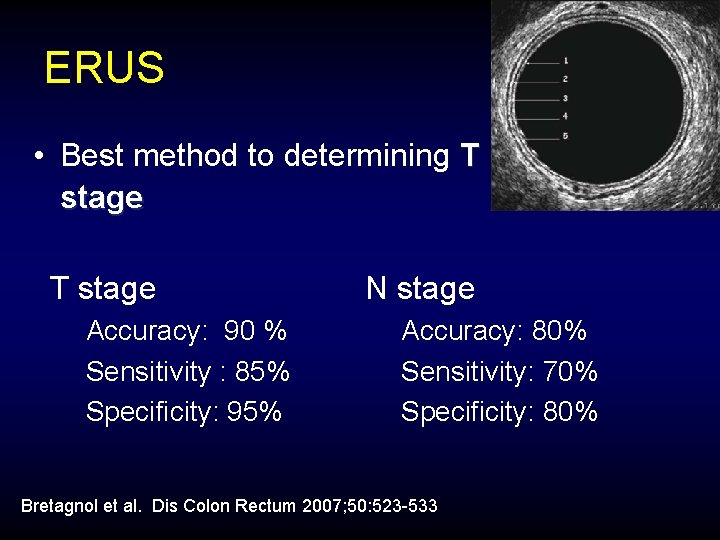
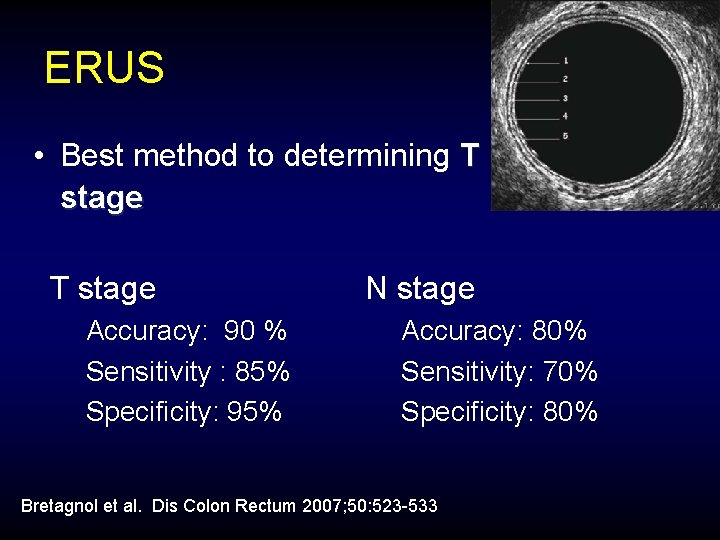
ERUS • Best method to determining T stage Accuracy: 90 % Sensitivity : 85% Specificity: 95% N stage Accuracy: 80% Sensitivity: 70% Specificity: 80% Bretagnol et al. Dis Colon Rectum 2007; 50: 523 -533
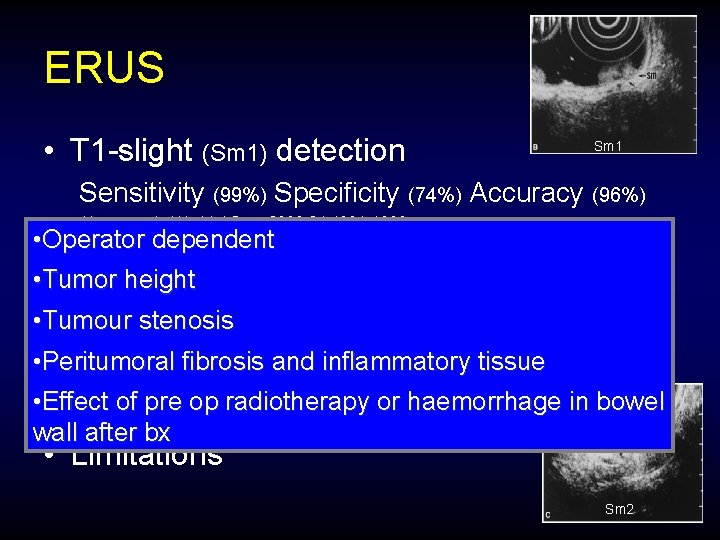
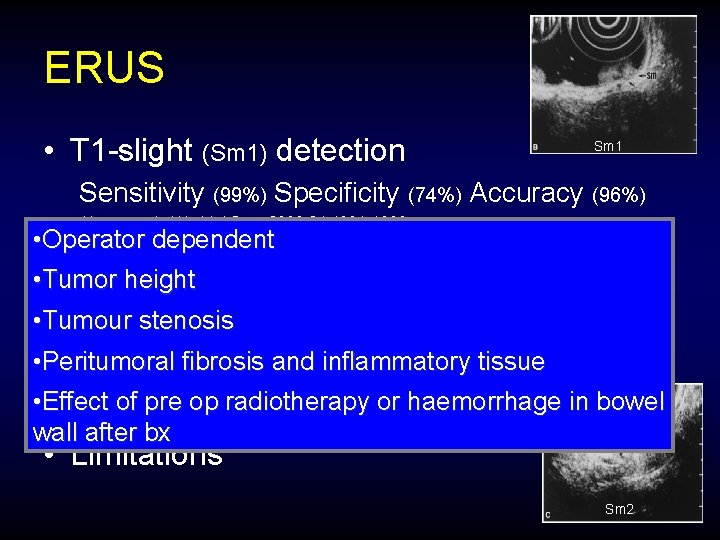
ERUS • T 1 -slight (Sm 1) detection Sm 1 Sensitivity (99%) Specificity (74%) Accuracy (96%) Akasu et al. World J Surg 2000; 24: 1061 -1068 • Operator dependent • May assess residual • Tumor height tumour following polypectomy • Tumour stenosis • Follow up after local excision or radical • Peritumoral fibrosis and inflammatory tissue surgery • Effect of pre op radiotherapy or haemorrhage in bowel Hernandez De Anda et al. Dis Colon Rectum 2004; 47: 818– 824 wall after bx • Limitations Sm 2
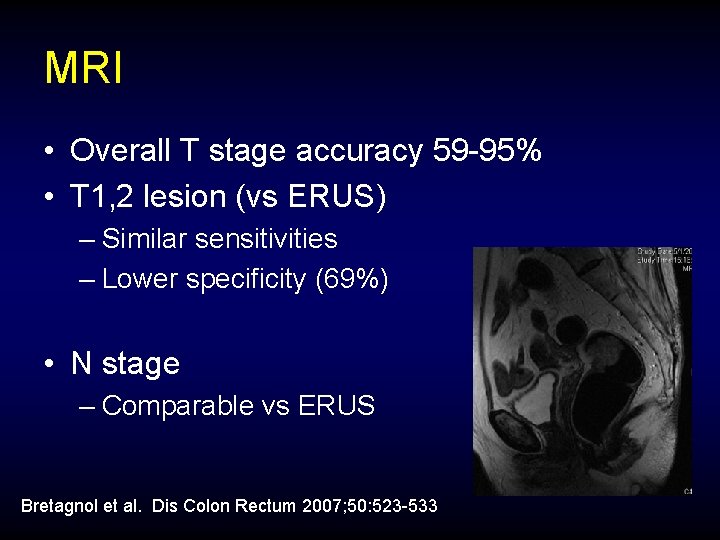
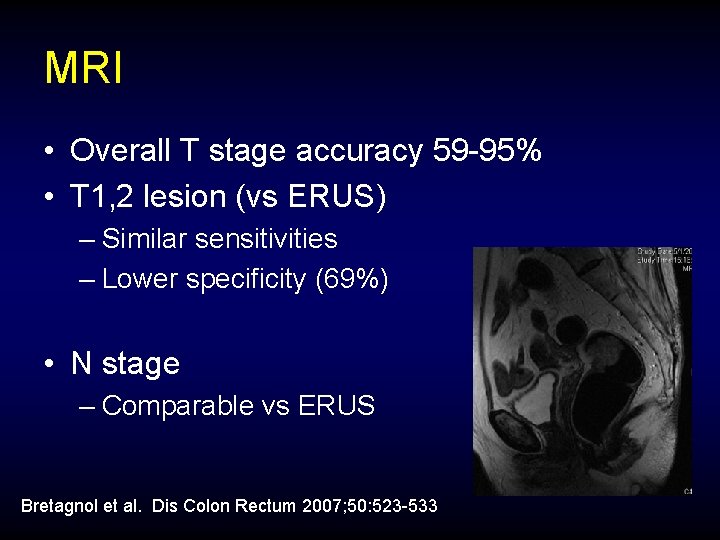
MRI • Overall T stage accuracy 59 -95% • T 1, 2 lesion (vs ERUS) – Similar sensitivities – Lower specificity (69%) • N stage – Comparable vs ERUS Bretagnol et al. Dis Colon Rectum 2007; 50: 523 -533
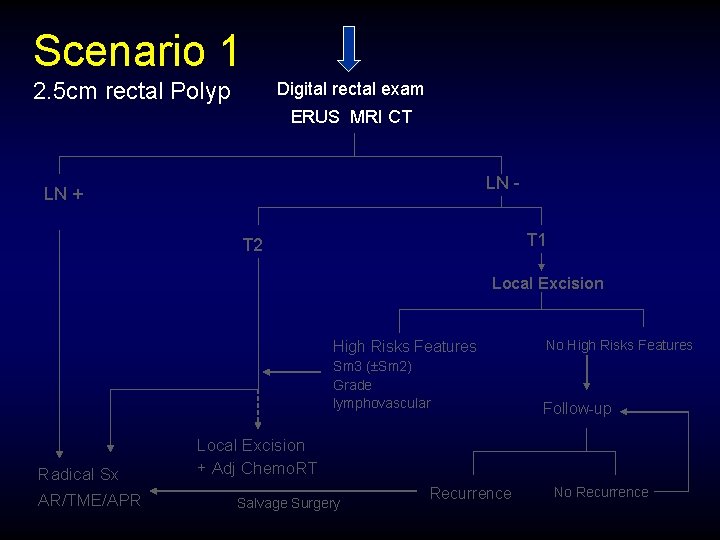
Scenario 1 2. 5 cm rectal Polyp Digital rectal exam ERUS MRI CT LN - LN + T 1 T 2 Local Excision Radical Sx AR/TME/APR High Risks Features No High Risks Features Sm 3 ( Sm 2) Grade lymphovascular Follow-up Local Excision + Adj Chemo. RT Salvage Surgery Recurrence No Recurrence
Local Excision • Potential advantage – Sphincter preservation – Minimal mortality and morbidity – Low urinary/sexual dysfunction risk
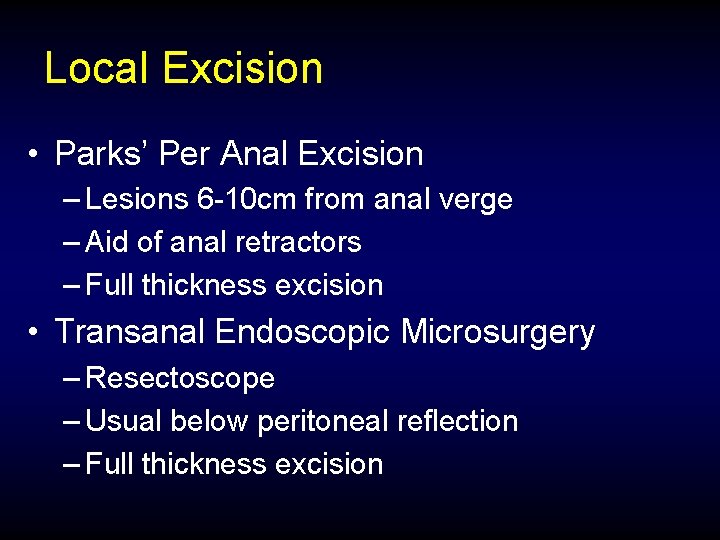
Local Excision • Parks’ Per Anal Excision – Lesions 6 -10 cm from anal verge – Aid of anal retractors – Full thickness excision • Transanal Endoscopic Microsurgery – Resectoscope – Usual below peritoneal reflection – Full thickness excision
Local Excision LR Bretagnol et al. Dis Colon Rectum 2007; 50: 523 -533
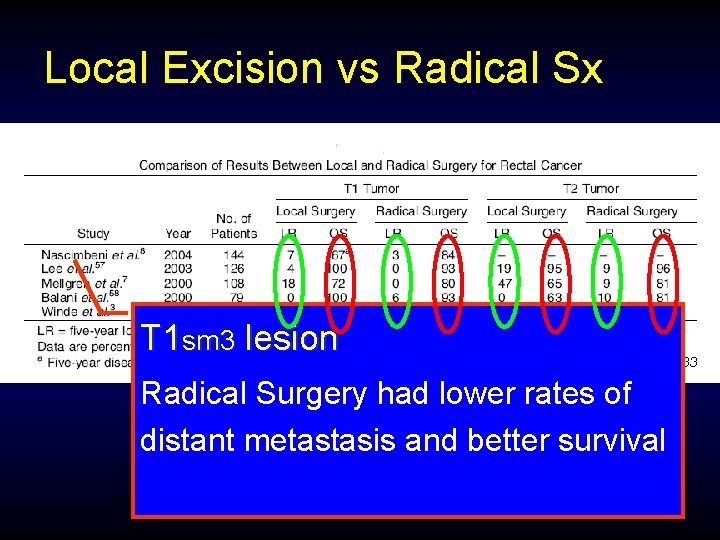
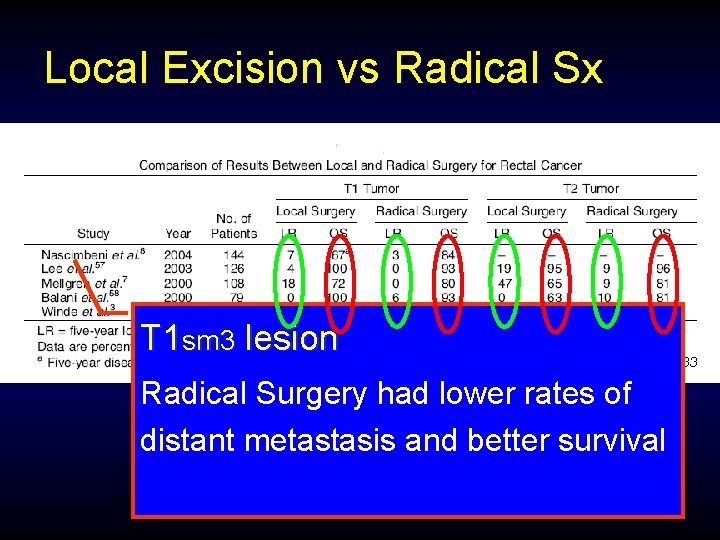
Local Excision vs Radical Sx T 1 sm 3 lesion Bretagnol et al. Dis Colon Rectum 2007; 50: 523 -533 Radical Surgery had lower rates of distant metastasis and better survival
Scenario 1 2. 5 cm rectal Polyp Digital rectal exam ERUS MRI CT LN - LN + T 1 T 2 Local Excision Radical Sx AR/TME/APR High Risks Features No High Risks Features Sm 3 ( Sm 2) Grade lymphovascular Follow-up Local Excision + Adj Chemo. RT Salvage Surgery Recurrence No Recurrence
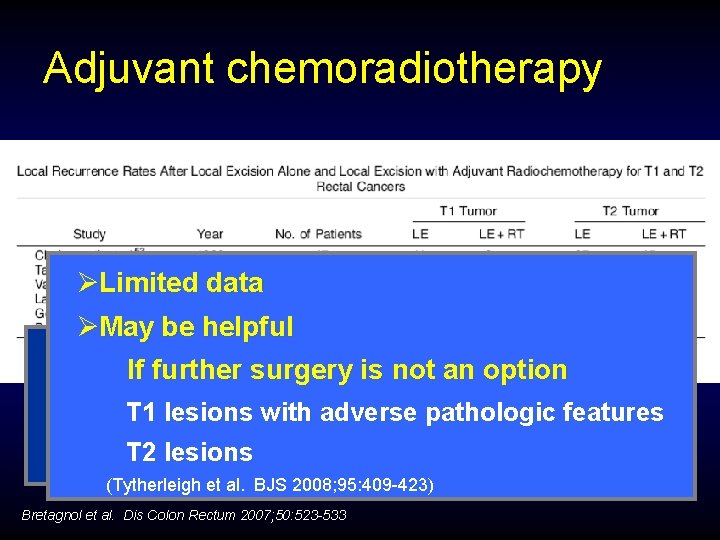
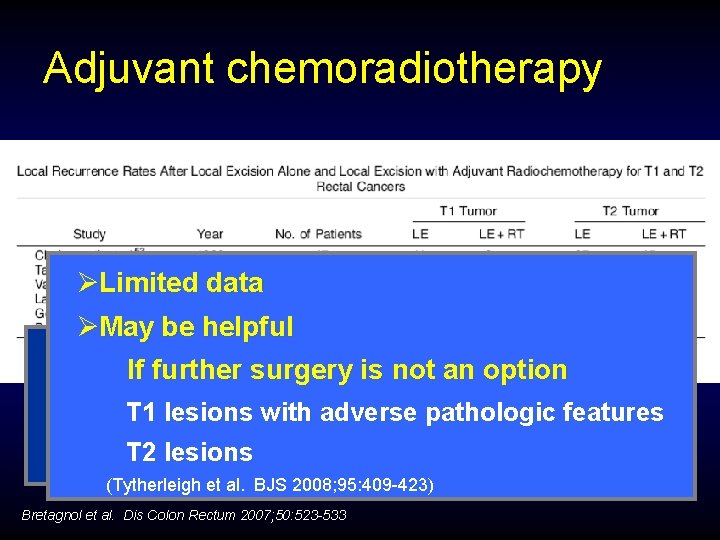
Adjuvant chemoradiotherapy ØLimited data ØMay be helpful Difficult to interpret If further surgery is not an option Most retrospective studies T 1 lesions with adverse pathologic features Lack of controlled data T 2 regime lesions Adjuvant not always based on a defined protocol (Tytherleigh et al. BJS 2008; 95: 409 -423) Bretagnol et al. Dis Colon Rectum 2007; 50: 523 -533
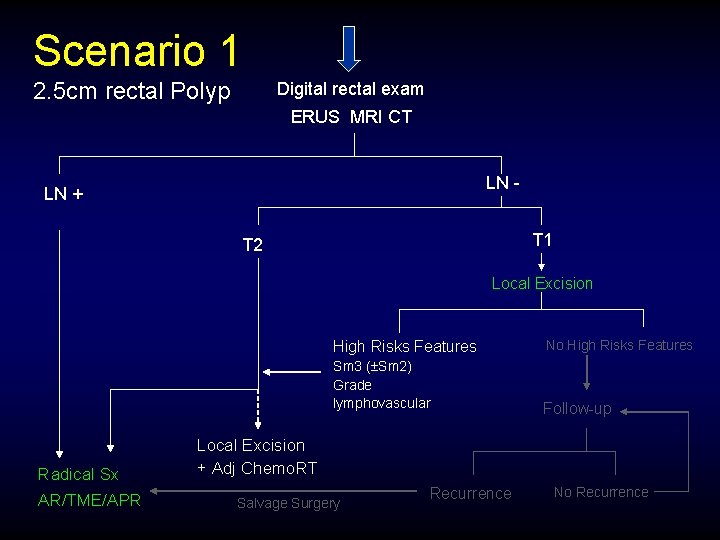
Scenario 1 2. 5 cm rectal Polyp Digital rectal exam ERUS MRI CT LN - LN + T 1 T 2 Local Excision Radical Sx AR/TME/APR High Risks Features No High Risks Features Sm 3 ( Sm 2) Grade lymphovascular Follow-up Local Excision + Adj Chemo. RT Salvage Surgery Recurrence No Recurrence
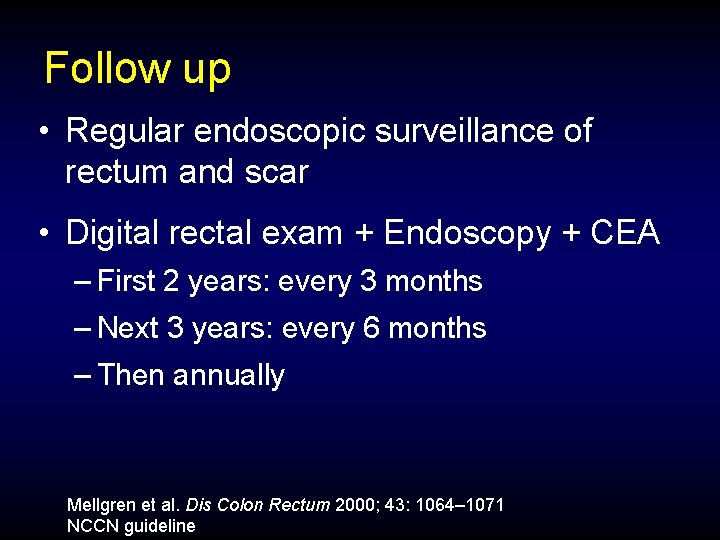
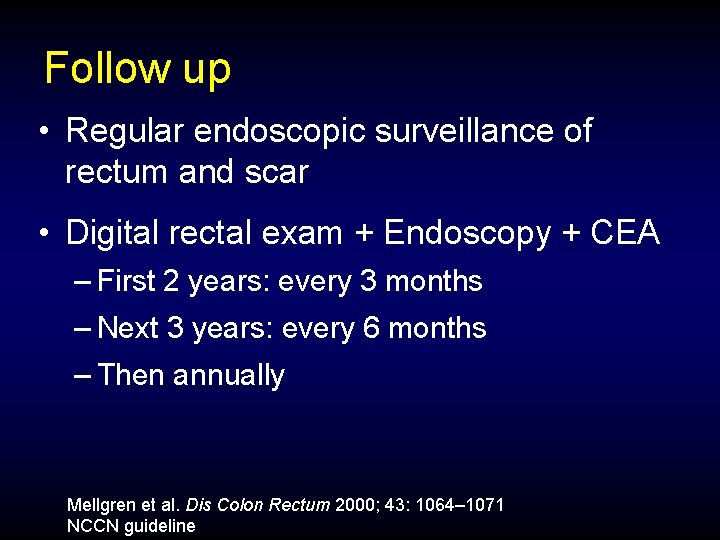
Follow up • Regular endoscopic surveillance of rectum and scar • Digital rectal exam + Endoscopy + CEA – First 2 years: every 3 months – Next 3 years: every 6 months – Then annually Mellgren et al. Dis Colon Rectum 2000; 43: 1064– 1071 NCCN guideline
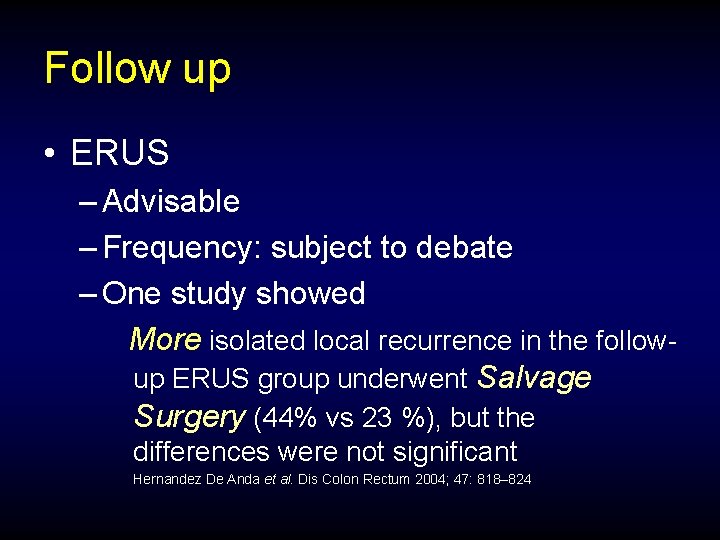
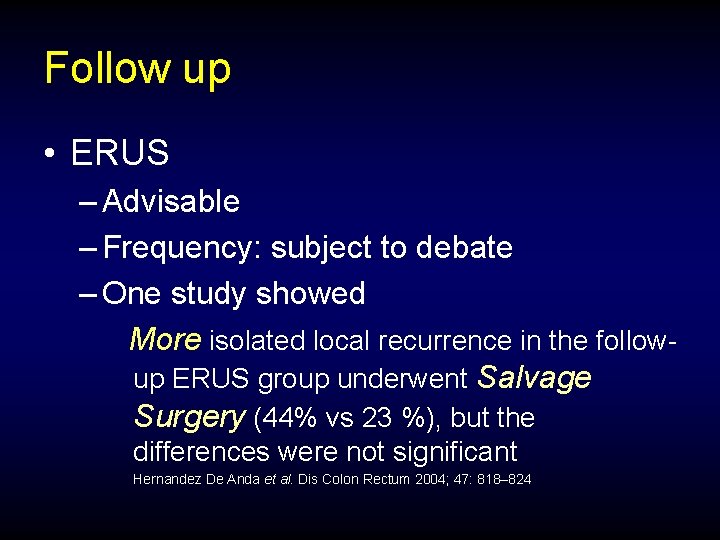
Follow up • ERUS – Advisable – Frequency: subject to debate – One study showed More isolated local recurrence in the followup ERUS group underwent Salvage Surgery (44% vs 23 %), but the differences were not significant Hernandez De Anda et al. Dis Colon Rectum 2004; 47: 818– 824
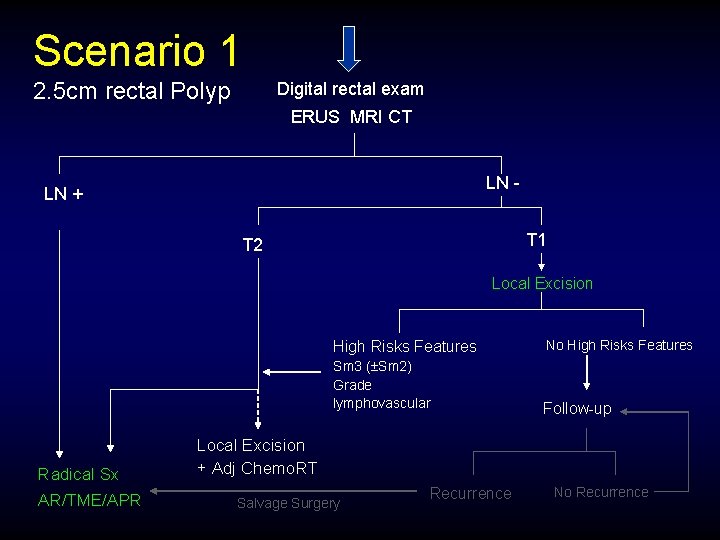
Scenario 1 2. 5 cm rectal Polyp Digital rectal exam ERUS MRI CT LN - LN + T 1 T 2 Local Excision Radical Sx AR/TME/APR High Risks Features No High Risks Features Sm 3 ( Sm 2) Grade lymphovascular Follow-up Local Excision + Adj Chemo. RT Salvage Surgery Recurrence No Recurrence
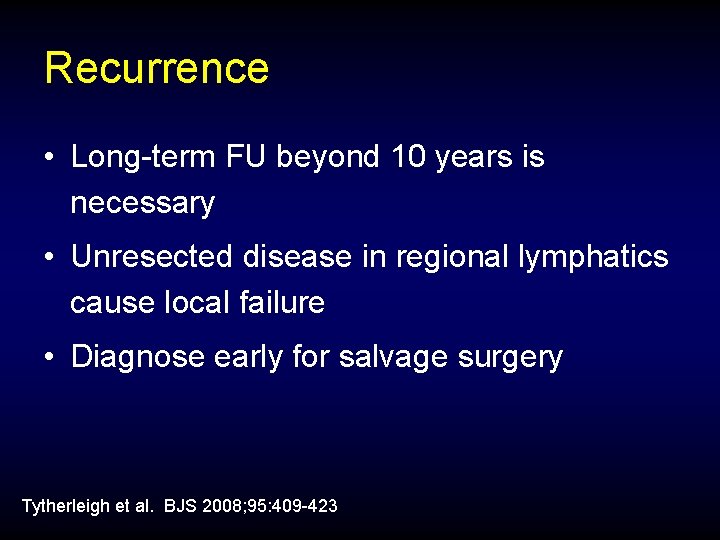
Recurrence • Long-term FU beyond 10 years is necessary • Unresected disease in regional lymphatics cause local failure • Diagnose early for salvage surgery Tytherleigh et al. BJS 2008; 95: 409 -423
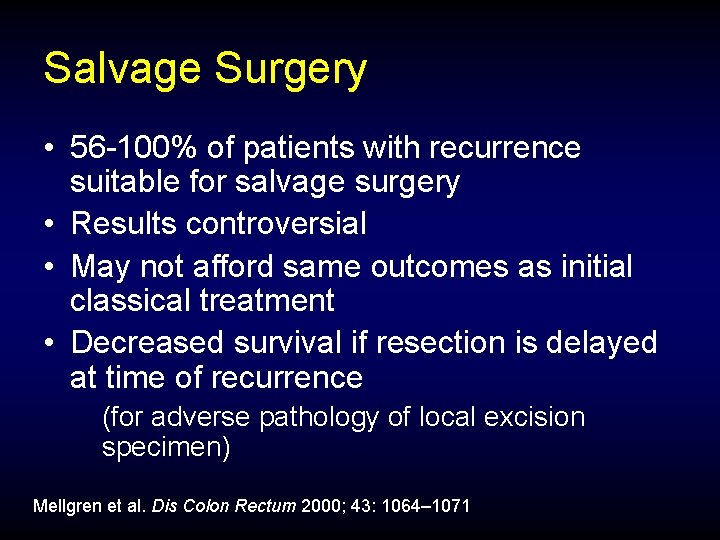
Salvage Surgery • 56 -100% of patients with recurrence suitable for salvage surgery • Results controversial • May not afford same outcomes as initial classical treatment • Decreased survival if resection is delayed at time of recurrence (for adverse pathology of local excision specimen) Mellgren et al. Dis Colon Rectum 2000; 43: 1064– 1071
Clinical Scenario 2. • Colonoscopic polypectomy of rectal polyp • Pathology: adenocarcinoma arise from tubular adenoma
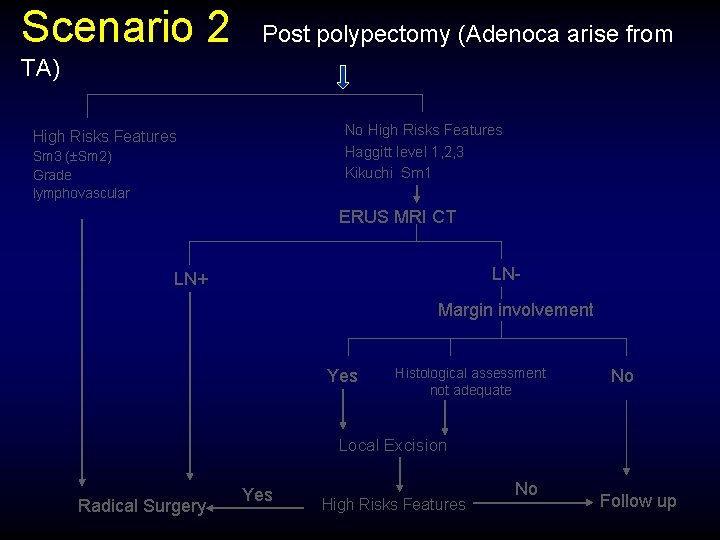
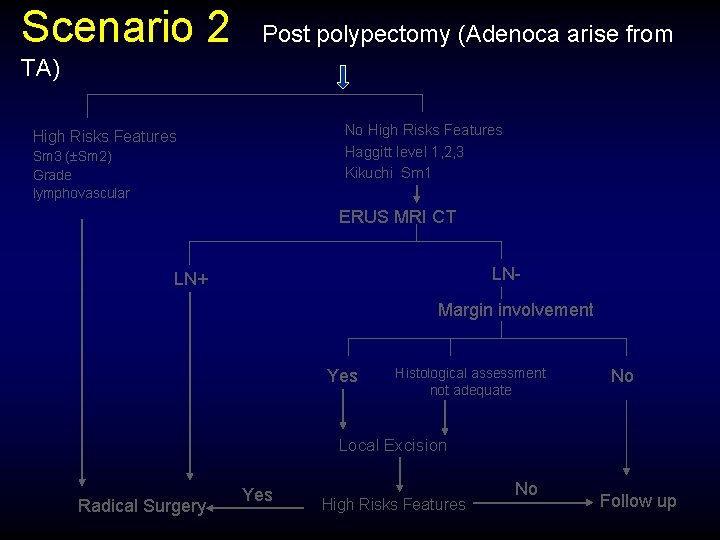
Scenario 2 Post polypectomy (Adenoca arise from TA) No High Risks Features Haggitt level 1, 2, 3 Kikuchi Sm 1 High Risks Features Sm 3 ( Sm 2) Grade lymphovascular ERUS MRI CT LN- LN+ Margin involvement Yes Histological assessment not adequate No Local Excision Radical Surgery Yes High Risks Features No Follow up
Summary Staging and Adequate Histological Assessment is crucial in management of malignant rectal polyp
Summary • Local excision Recommended for low risk T 1 sm 1 lesion Adjuvant therapy considered in high risk T 1, T 2 if surgery not an option • Radical Surgery Recommended for high risk T 1 , T 2 lesion • Recurrence Diagnose early for salvage surgery

Thank You
 Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Tmh
Tmh Esophgeal varices
Esophgeal varices Broad based protrusion
Broad based protrusion Inet wellspan
Inet wellspan December round the world
December round the world Pqr gmp requirements
Pqr gmp requirements What does apr stand for
What does apr stand for Cours cap apr
Cours cap apr Apr air purifying respirator
Apr air purifying respirator Apr vs ear
Apr vs ear Jan fab mar
Jan fab mar Apr vs ear
Apr vs ear àpr
àpr Ncaa apr database
Ncaa apr database Nominal versus real returns
Nominal versus real returns Sistem za centralizovano prijavljivanje korisnika apr
Sistem za centralizovano prijavljivanje korisnika apr Ground round hospital
Ground round hospital Hospital pharmacy space requirements
Hospital pharmacy space requirements Joint venture account
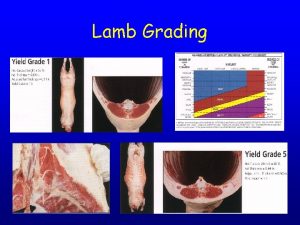
Joint venture account Lamb quality grades
Lamb quality grades Break joint vs spool joint
Break joint vs spool joint Membrane tectoria
Membrane tectoria Condyloid ellipsoidal joint
Condyloid ellipsoidal joint Permanent fastening methods
Permanent fastening methods Stapler history
Stapler history There are dangling modifiers in this descriptor
There are dangling modifiers in this descriptor Surgical planning laboratory
Surgical planning laboratory