Perioperative Division New Employee Orientation Aseptic Technique At














- Slides: 50
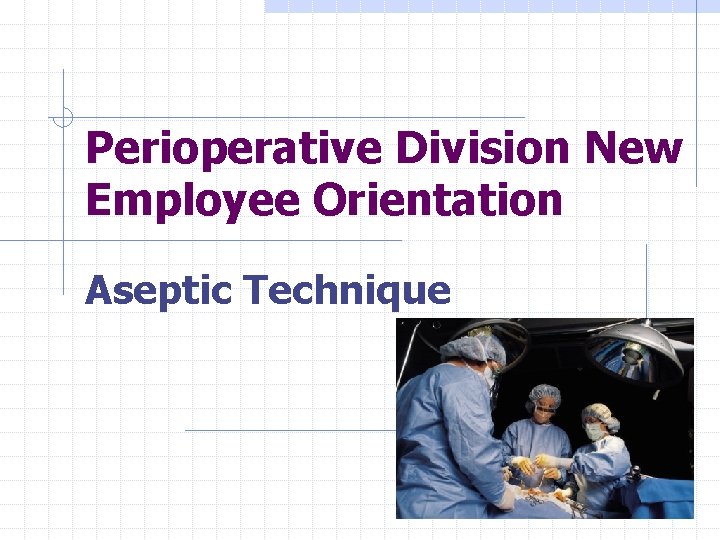
Perioperative Division New Employee Orientation Aseptic Technique

At the Movies… To fulfill the requirement for this module, view the videos: Aseptic technique: Stressing the Fundamentals Scrubbing, Gowning & Gloving
Reading Assignment UAB Hospital Standard: Perioperative Plan of Care UAB Hospital Interdisciplinary Standard: Creating and maintaining an aseptic environment UAB Hospital Interdisciplinary Standard: Surgical Site Skin Prep
The Sterile Conscience In the operating room maintenance of aseptic technique is critical to patient safety. Everyone who works in the OR should have a sterile conscience- this requires an individual who accidentally breaks sterile technique, to acknowledge and rectify the error, whether the break in sterile technique is observed by others or not
Objective 1 Identify the guiding principles of aseptic technique

Principles Guiding Surgical Aseptic Technique 1. Maintaining a sterile field requires that only sterile items may be used within this sterile field 2. All items opened to the sterile field are inspected before opening, if the sterility of any item is in question, the item must be considered unsterile 3. Any item added to the sterile field must be opened/dispensed in a way that maintains the sterility of the item 4. Any movement within or around a sterile field must be done in a way that does not contaminate the sterile field ( Rothrock, 2003)
Principles, continued… 5. Any permeation of a sterile barrier renders the item and/or area unsterile 6. Tables are considered to be sterile only at and above table level (Overhanging drape edges are not considered to be sterile) 7. Scrubbed persons will only touch sterile areas or items/Nonscrubbed persons only touch non-sterile items and surfaces 8. Sterile area of wrappers extends to 1 inch from the wrapper’s edge- the edges are considered unsterile (Rothrock, 2003)

Objective 2 Identify boundaries of the sterile field Q: What exactly is the sterile field? A: The sterile field consists of: the draped surgical patient, the sterile personnel (surgeon, assistants, scrub person) and all furniture and equipment which is covered with sterile drapes (ex: back table, mayo stand, operating microscopes, etc)
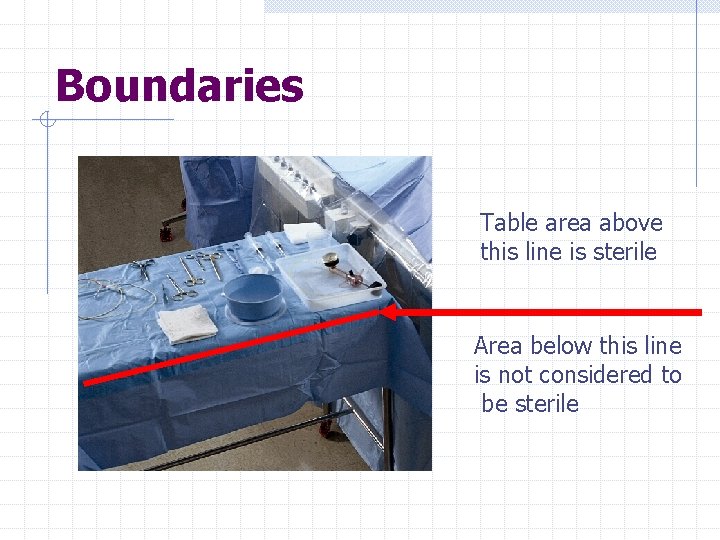
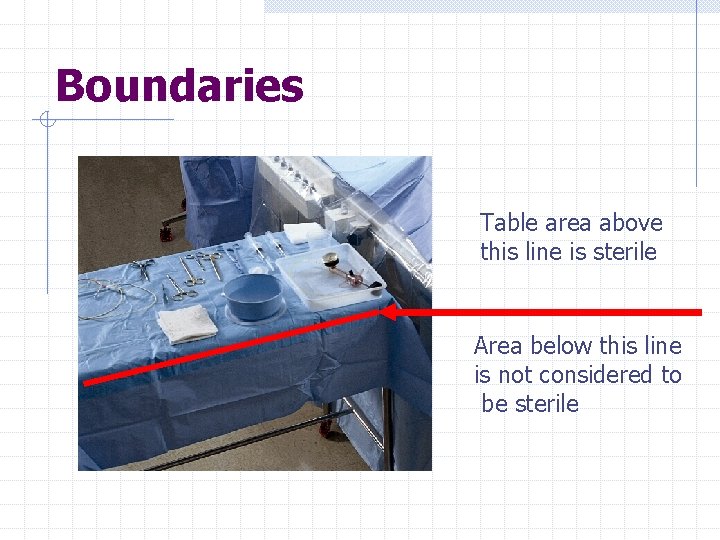
Boundaries Table area above this line is sterile Area below this line is not considered to be sterile
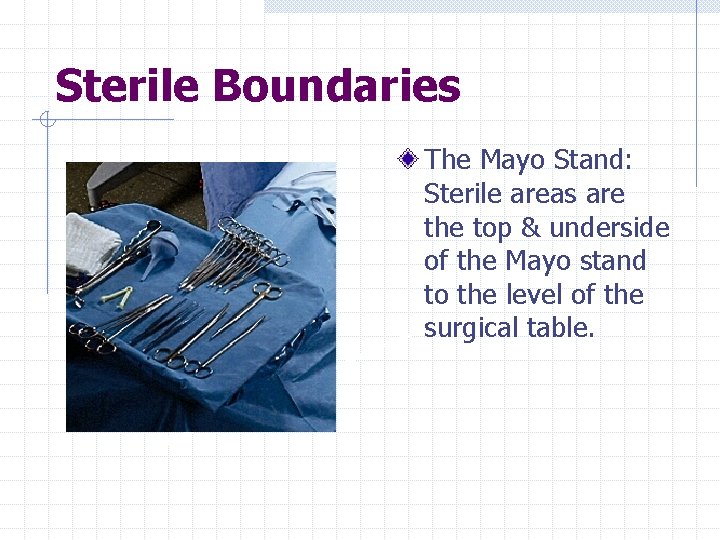
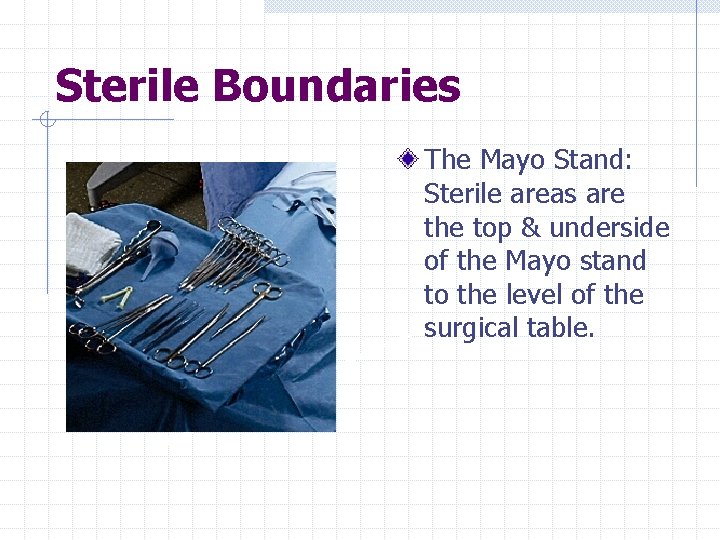
Sterile Boundaries The Mayo Stand: Sterile areas are the top & underside of the Mayo stand to the level of the surgical table.

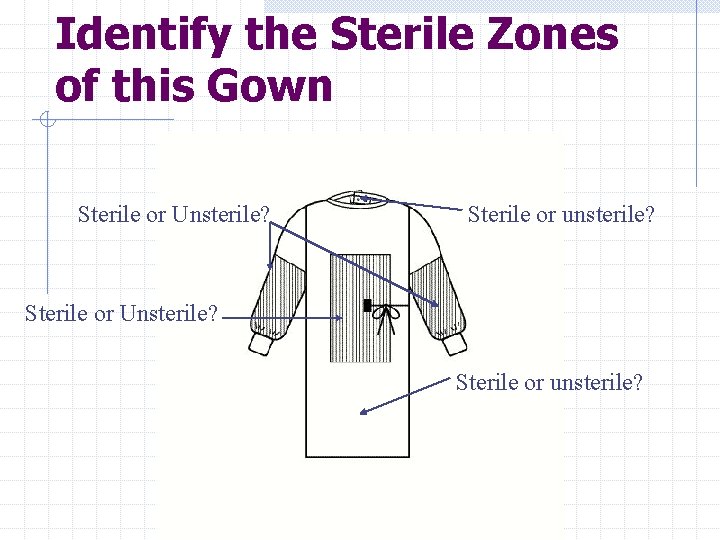
Objective 3 Describe areas of sterility of the sterile surgical gown
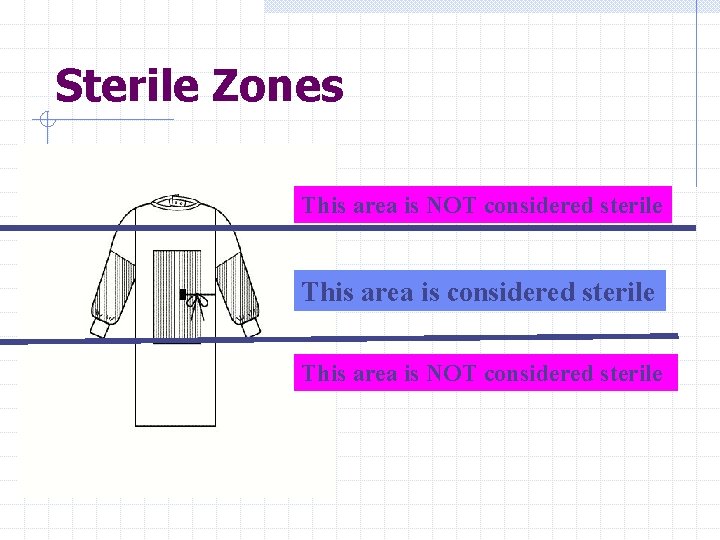
Sterile Areas of Surgical Gowns Front of gown, from chest level to table level The sleeve from 2 inches above the elbow to the stockinet cuff
Unsterile Areas of Gown Neckline Shoulders Under the arms The back (the back of a surgical gown cannot be considered sterile because it is not possible to observe the area constantly)
Gown Stockinet Cuff Are not considered sterile once pulled over the hands Cuff material absorbs perspiration from hands, so cannot be considered sterile Sterile gloves must cover the gown cuff
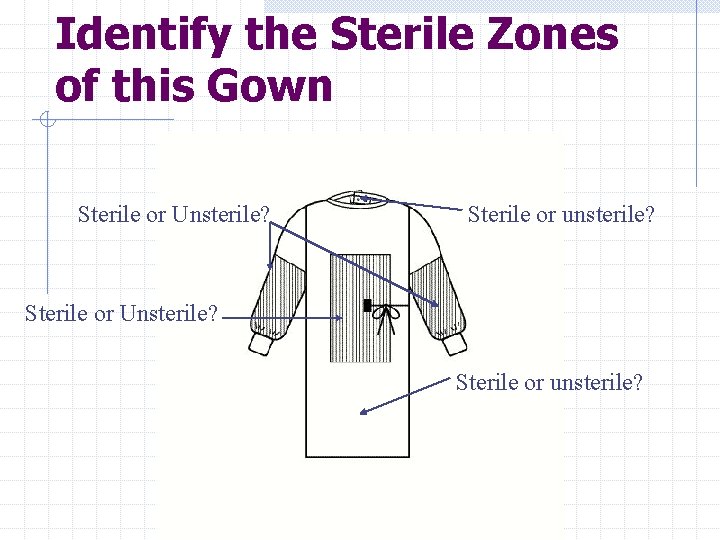
Identify the Sterile Zones of this Gown Sterile or Unsterile? Sterile or unsterile? Sterile or Unsterile? Sterile or unsterile?
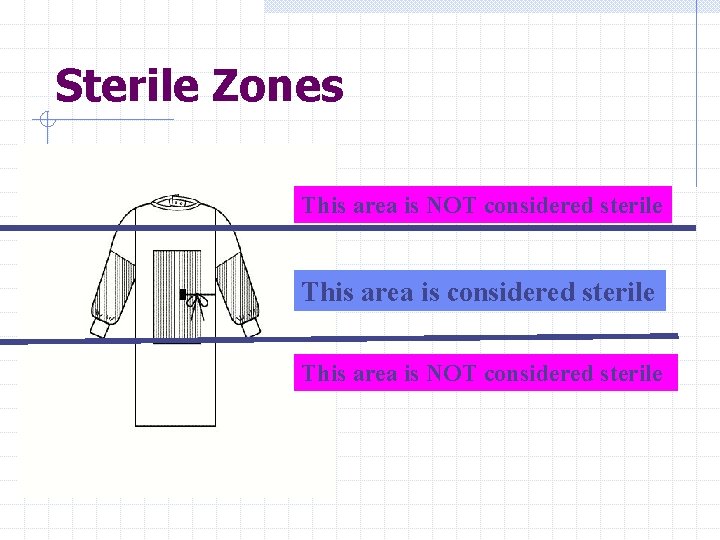
Sterile Zones This area is NOT considered sterile
Objective 4 Identify appropriate movement around sterile field Appropriate movement around the sterile field should not cause contamination of the field.
Scrubbed Persons Should stay close to the sterile field When passing a non-sterile area or persons, the scrubbed person faces the sterile field, and keeps their back toward the unsterile person or area If at all possible, allowing at least a 12 inch margin between the scrubbed person & unsterile areas minimizes risk of accidental contamination
Scrubbed Persons Sterile persons pass each other either front to front, or back to back A scrubbed person should not drop their arms below waist level; if this happens the hands should be considered contaminated, and the scrubbed person should change gloves
Movement within the Sterile Field An un-scrubbed person should not walk between 2 sterile fields—doing so carries a high risk of contaminating the sterile field
Scrubbed Persons Should only sit if the entire procedure is to be performed at sitting level. Changing levels during a case increases risk of contaminating the sterile field
Movement of Unsterile (Unscrubbed) Persons Unsterile persons should always face the sterile field when moving around in the OR- this reduces the risk of accidental contamination of the sterile area. An non-sterile person should observe a wide margin of safety when moving around the sterile field- at least 12 inches is recommended

OR Room Traffic into and out of the OR rooms should be kept to a minimum while the surgery is in progress – air currents, caused by the opening of doors and movement of personnel, carry bacteria and dust, increasing the risk of airborne contamination

Monitoring the Sterile Field AORN Recommended Practices (2003) states that the surgical field should be monitored continuously- this prevents inadvertent contamination from being undetected; allows for immediate corrective action if any contamination occurs
Objective 5 Identify furniture set-up for a typical OR suite: Back table Mayo stand Prep table Kick bucket Stools (standing & sitting) Other furniture as indicated by specific procedure
Objective 6 Demonstrate how to establish & maintain the sterile field To be completed with Preceptor in the OR

Opening Sterile Supplies Demonstrate opening and dispensing sterile supplies: w. Custom Packs w. Pouring solutions w. Wrapped items w. Delivering medications to the w. Peel-packed items sterile field w. Rigid instrument containers This activity to be completed with Preceptor in the OR
Handling Sterile Packages Sterile packages should only be placed on dry surfaces—Package is no longer sterile if placed on a wet surface If a wrapped package is dropped it is considered contaminated- even if the package is not torn, impact with floor may force unsterile air into the package
Inspection of Sterile Items When opening an item intended for sterile use, it is important to verify the sterility of that item. If the sterility of an item is in doubt, the item must be considered contaminated.

Inspection of Sterile Items Manufacturer sterilized items (implants, medication, catheters, etc) must be inspected for presence of an expiration date before opening onto the sterile field.
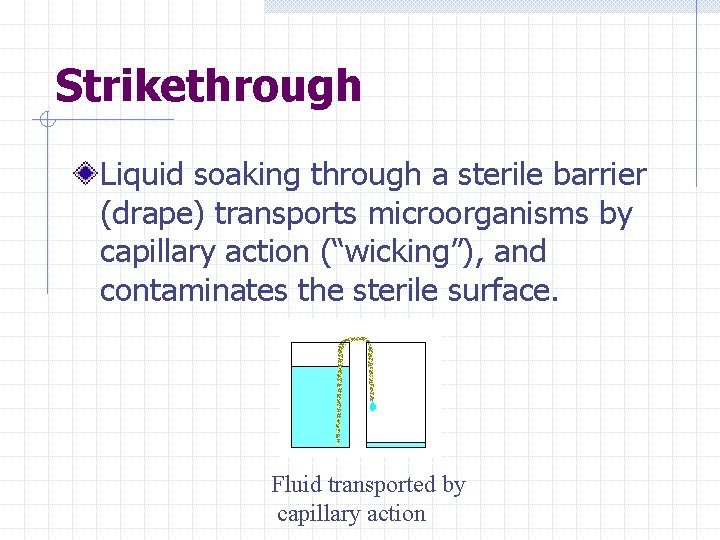
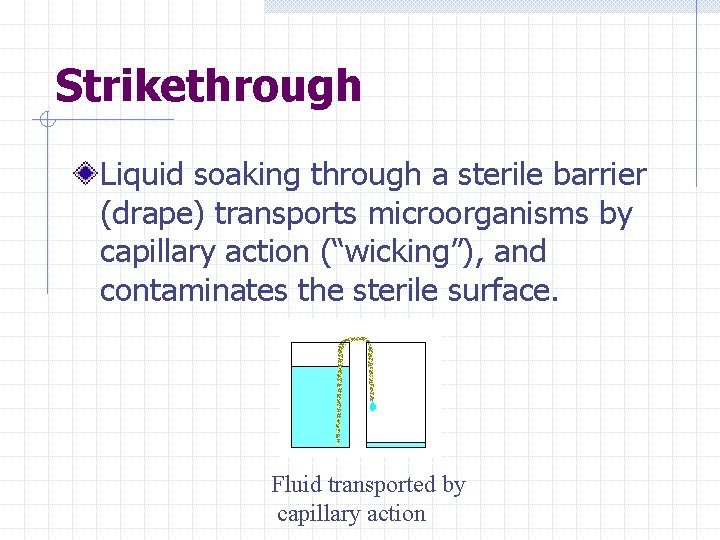
Strikethrough Liquid soaking through a sterile barrier (drape) transports microorganisms by capillary action (“wicking”), and contaminates the sterile surface. Fluid transported by capillary action

Strikethrough “Sterile” packages with water stains on the wrapper must be considered contaminated, even if the package does not feel damp

Inspection: Rigid Metal Sterilization Containers AKA Genesis Containers Filters should be intact If filters are dislodged or wet, the contents of the container are unsterile

Opening Sterile Items: Step 1 Determine package integrity before opening Inspect for wrapper tears, puncture holes, or stains indicating that the package has been wet Inspect for expiration date & external sterilization indicator
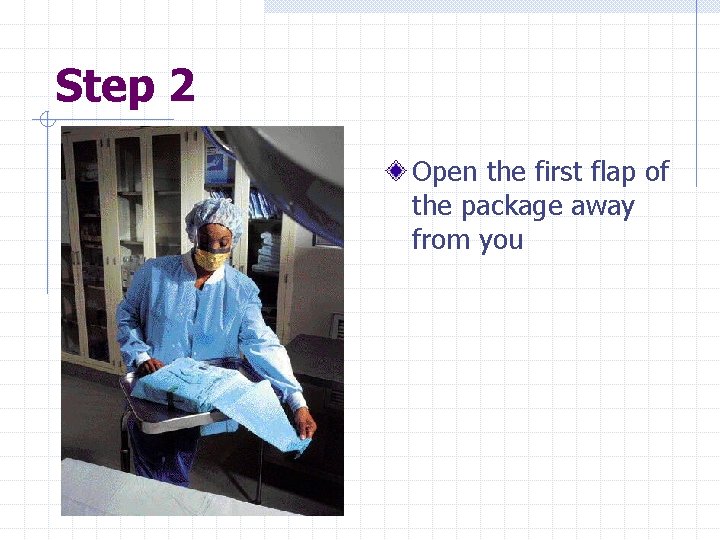
Step 2 Open the first flap of the package away from you
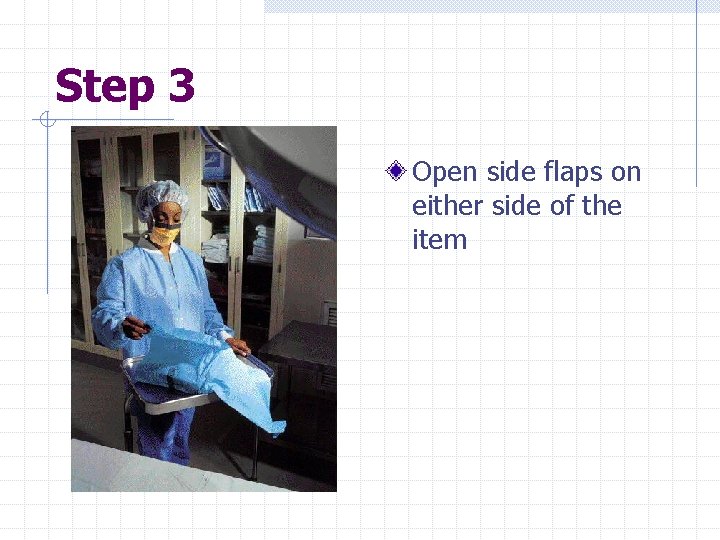
Step 3 Open side flaps on either side of the item
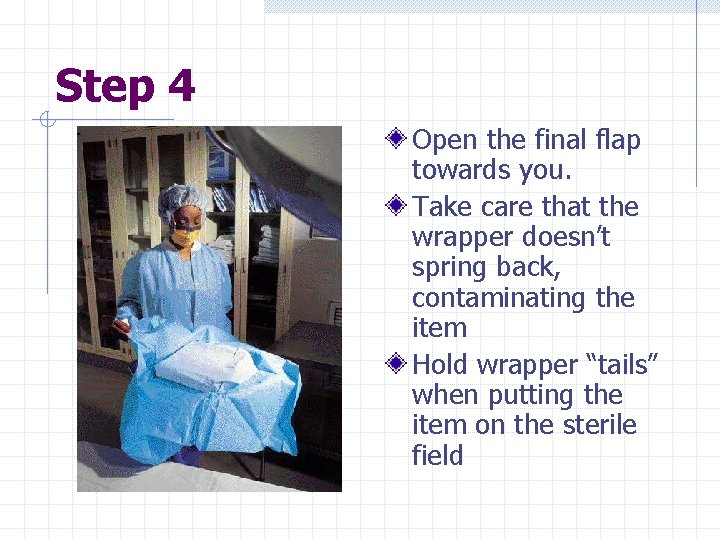
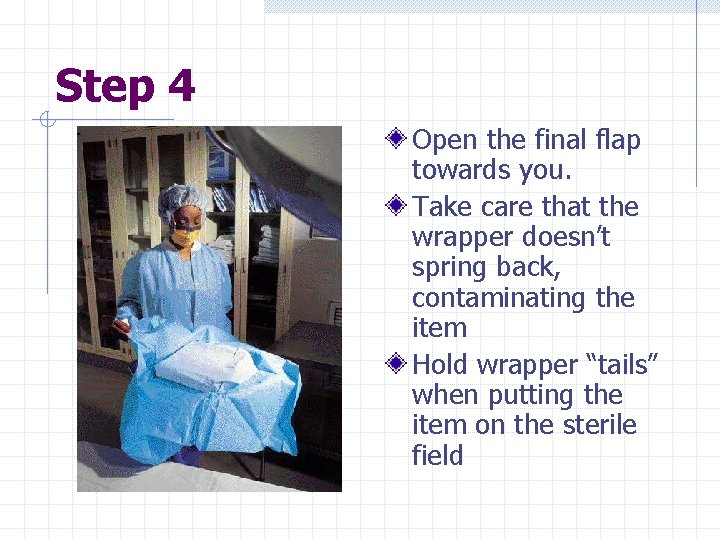
Step 4 Open the final flap towards you. Take care that the wrapper doesn’t spring back, contaminating the item Hold wrapper “tails” when putting the item on the sterile field
Dispensing Liquids to the Sterile Field When pouring liquids, do so in a way that avoids splashing Don’t allow fluids to drip down the side of the container The receptacle for the liquid should be either near the edge of the sterile field, or held by the scrub person, so that the unsterile person will not have to reach over the sterile field to pour the liquid

Dispensing Liquids to the Sterile Field AORN recommends: if the entire container of a liquid is not dispensed, the container and the remaining liquid should be discarded (Replacing the container lid might contaminate container and contents)
Surgical Draping Drapes used to establish the sterile field, including those used to cover the back table and Mayo stand should be made of impervious material to prevent contamination from fluid strike-through
Surgical Draping Drape starting from the intended incision site, outward to the periphery Use towels to form an initial barrier, then apply larger drapes Protect sterile gloved hands by cuffing drape material over the gloved hands
Surgical Draping Avoid fanning drapes-- this creates air currents which increase the risk of contamination Hold drapes above waist level when draping Surgical drapes should not be moved after they are positioned—moving the drape creates the risk of contamination

Securing Tubing, Cords Any tubing, cables and cords should be secured to the sterile drape with nonperforating clamps to avoid puncturing the sterile drapes
Objective 7 Identify/discuss problem solving for accidental contamination within the sterile field
Items Falling Below Level of Sterile Field If a drape or equipment falls below the level of the sterile field, it is considered contaminated—it cannot be pulled back up to sterile field level. (Example: if the suction tip falls below the level of the sterile field, it must be replaced, not pulled back up to the sterile field)
Items Falling below Level of Sterile Field Appropriate response: open another sterile item to replace the contaminated one Contaminated equipment/instruments may need to be flash sterilized if there is not a sterile replacement available

Sterile Gloves Should be inspected for holes after donning If a glove becomes contaminated during the surgical procedure it should be changed immediately
Gloves If the stockinet cuff is pulled over the hand, the hand should be considered contaminated If a glove is contaminated during the course of the surgical procedure, the preferred method of donning a new glove is to have another member of the sterile team put on the new glove If it is not possible for another member of the team to assist with gloving, the open gloving method should be used
References AORN (2002) Standards, Recommended Practices & Guidelines Roth (1994) Perioperative Nursing Core Curriculum Rothrock (2003) Alexander’s Care of the Patient in Surgery UAB Hospital Interdisciplinary Standard Creating and Maintaining an Aseptic Environment
Acknowledgements All images used with the permission of Kimberly Clark International
 Aseptic technique pharmacy
Aseptic technique pharmacy Aseptic garbing technique
Aseptic garbing technique Use of aseptic hood
Use of aseptic hood Aseptic technique clipart
Aseptic technique clipart Lafws
Lafws Tier 1 standard precautions
Tier 1 standard precautions Nih new employee orientation
Nih new employee orientation Fsu dean of students case management
Fsu dean of students case management New employee orientation
New employee orientation Employee attitudes and employee performance
Employee attitudes and employee performance Employee safety orientation quiz answers
Employee safety orientation quiz answers Employee socialization and orientation
Employee socialization and orientation Geocentric orientation
Geocentric orientation Perioperative care phases
Perioperative care phases Preoperative nursing definition
Preoperative nursing definition Perioperative case study nursing
Perioperative case study nursing Ccs perioperative guidelines
Ccs perioperative guidelines Preoperative nursing definition
Preoperative nursing definition Www.antt
Www.antt Pleocytosis pronunciation
Pleocytosis pronunciation Gowning introduction
Gowning introduction Asepsis
Asepsis Ekisha shoes
Ekisha shoes General aseptic fields
General aseptic fields Sterile products and aseptic techniques
Sterile products and aseptic techniques Aseptic packaging
Aseptic packaging Sterile products and aseptic techniques
Sterile products and aseptic techniques Short division vs long division
Short division vs long division Synthetic division
Synthetic division Long division terminology
Long division terminology Polynomial short division
Polynomial short division Employee motivation a powerful new model
Employee motivation a powerful new model Yale new haven hospital volunteer
Yale new haven hospital volunteer Skyward login new richmond
Skyward login new richmond Technique opératoire division
Technique opératoire division Northside hospital new hire orientation
Northside hospital new hire orientation Lions clubs international headquarters oak brook
Lions clubs international headquarters oak brook New distributor orientation program
New distributor orientation program New distributor orientation
New distributor orientation Famous toastmasters
Famous toastmasters New teacher orientation agenda
New teacher orientation agenda Gsu new student orientation
Gsu new student orientation Par panel bcps
Par panel bcps New nurses orientation
New nurses orientation Penn state factbook
Penn state factbook Rotary new member orientation
Rotary new member orientation Texas state new student orientation
Texas state new student orientation New teacher orientation presentation
New teacher orientation presentation Occ new student orientation
Occ new student orientation Fsu new faculty orientation
Fsu new faculty orientation Cpcc new student orientation
Cpcc new student orientation