Good morning Testis Epididymis and Spermatic cord Dr



- Slides: 47

Good morning
Testis, Epididymis and Spermatic cord Dr. Qudsia Sultana
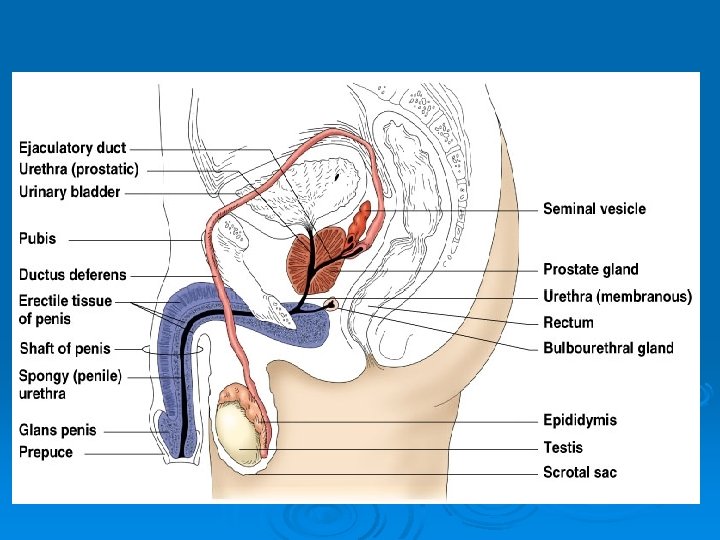
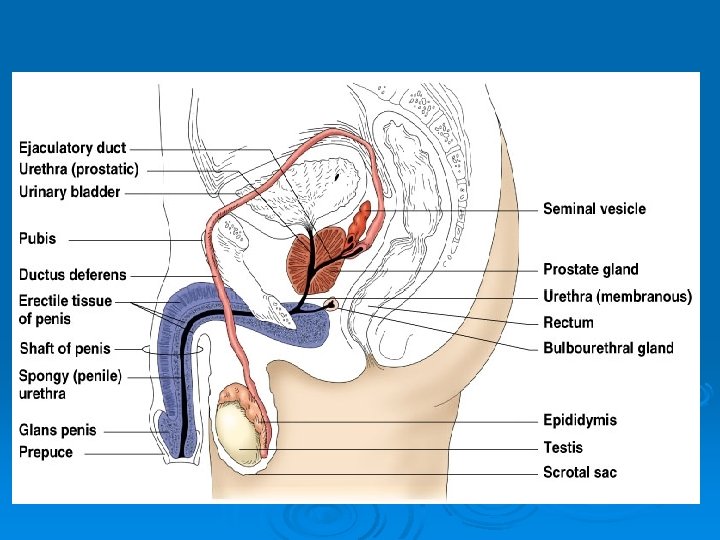
Male Reproductive System Ø Testis Ø Epididymis Ø Ductus deferens Ø Seminal vesicles Ø Ejaculatory ducts Ø Penis Accessory structures : Prostate and Bulbo-urethral glands
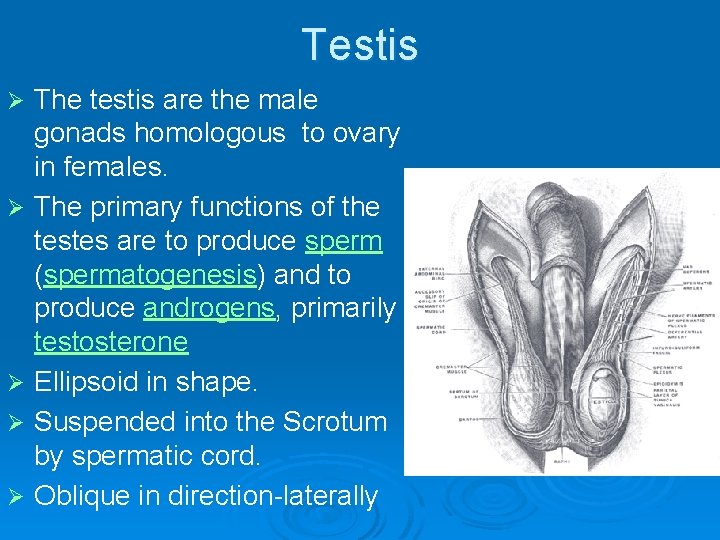
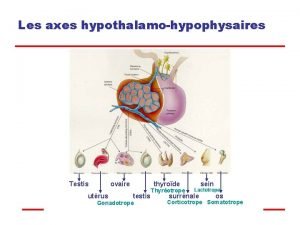
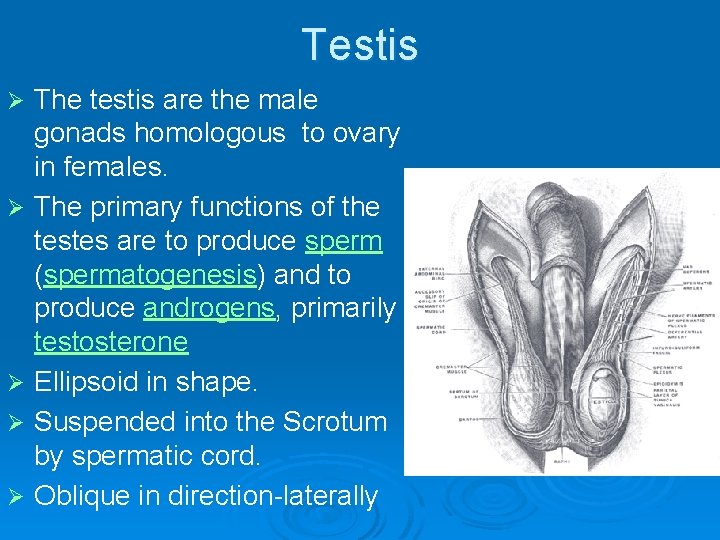
Testis Ø Ø Ø The testis are the male gonads homologous to ovary in females. The primary functions of the testes are to produce sperm (spermatogenesis) and to produce androgens, primarily testosterone Ellipsoid in shape. Suspended into the Scrotum by spermatic cord. Oblique in direction-laterally
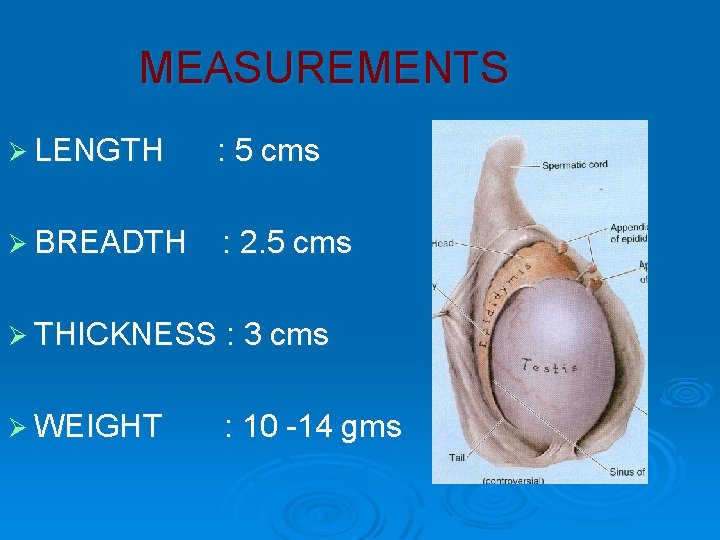
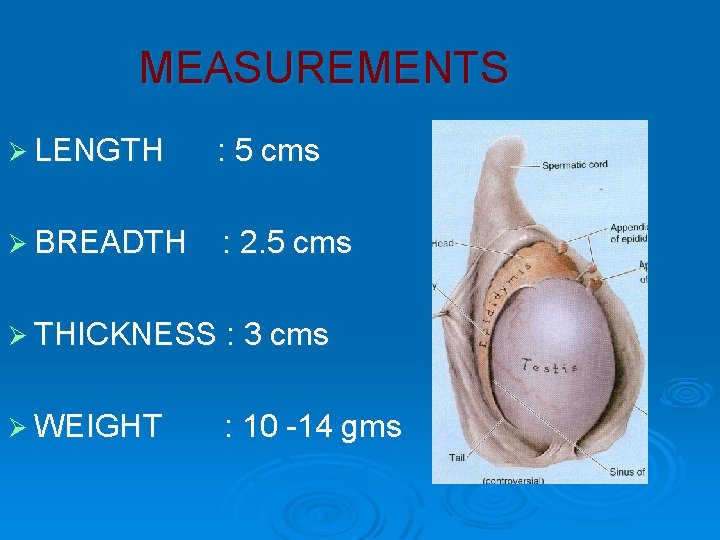
MEASUREMENTS Ø LENGTH : 5 cms Ø BREADTH : 2. 5 cms Ø THICKNESS : 3 cms Ø WEIGHT : 10 -14 gms
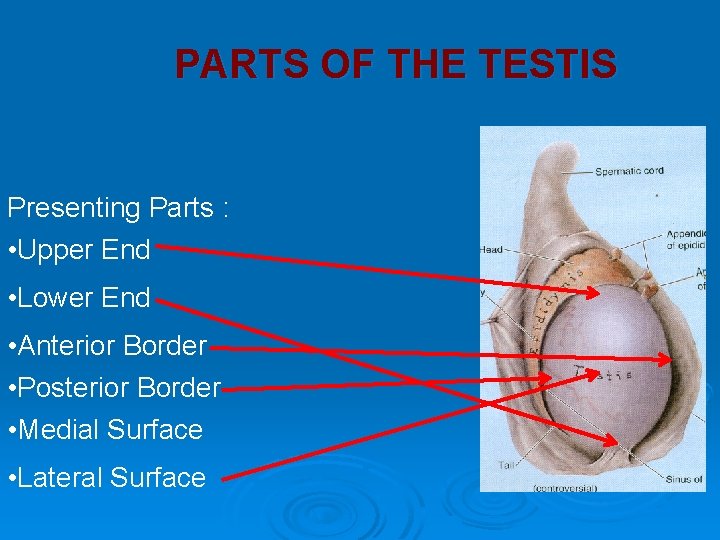
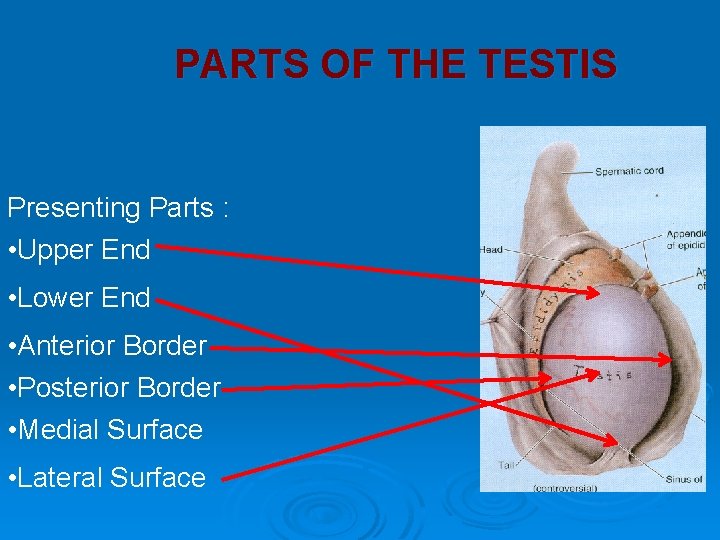
PARTS OF THE TESTIS Presenting Parts : • Upper End • Lower End • Anterior Border • Posterior Border • Medial Surface • Lateral Surface
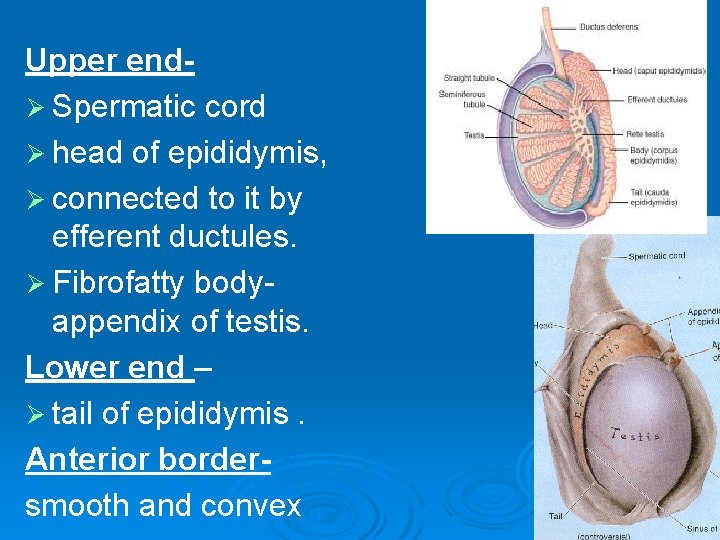
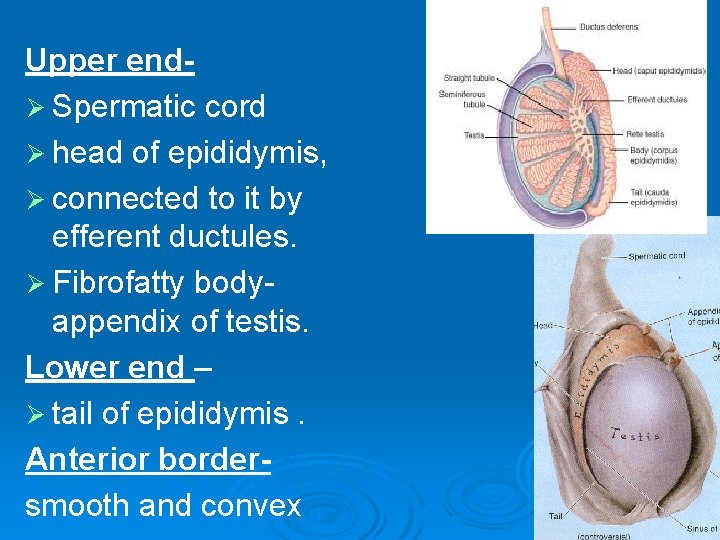
Upper endØ Spermatic cord Ø head of epididymis, Ø connected to it by efferent ductules. Ø Fibrofatty bodyappendix of testis. Lower end – Ø tail of epididymis. Anterior bordersmooth and convex
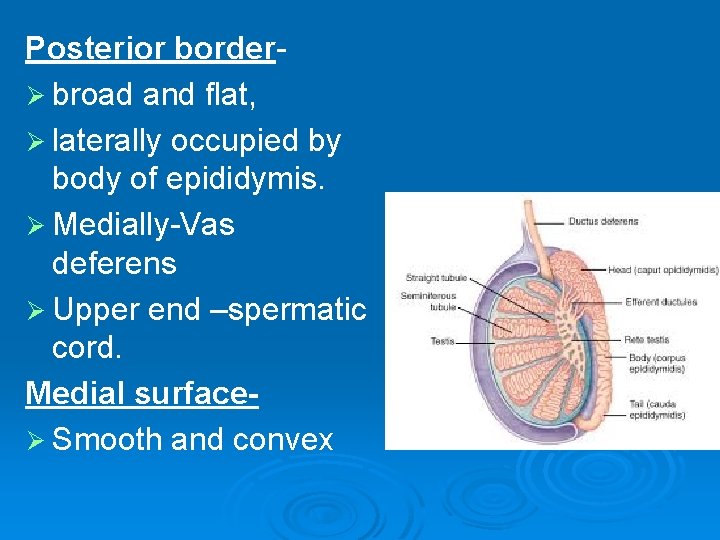
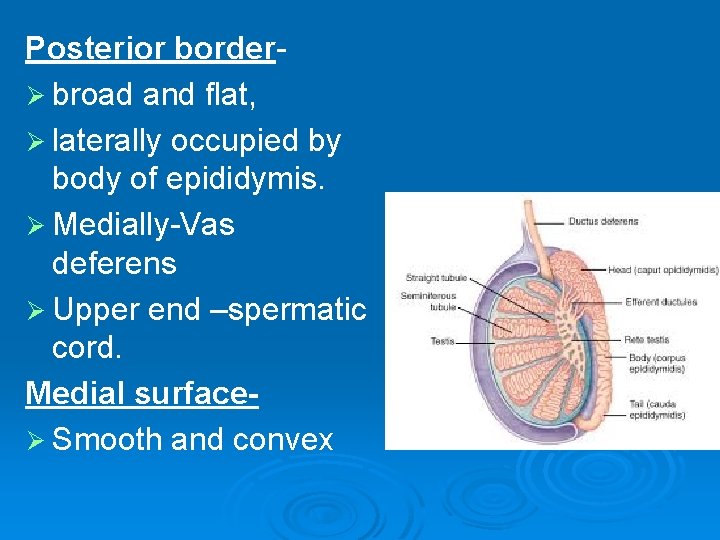
Posterior borderØ broad and flat, Ø laterally occupied by body of epididymis. Ø Medially-Vas deferens Ø Upper end –spermatic cord. Medial surfaceØ Smooth and convex
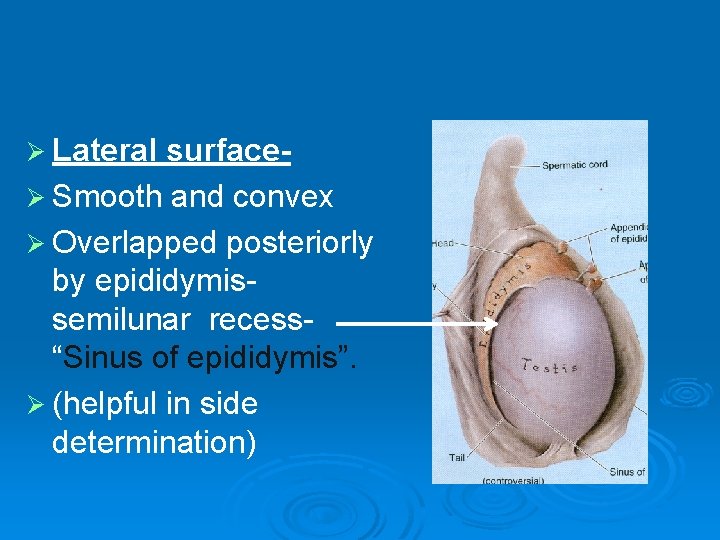
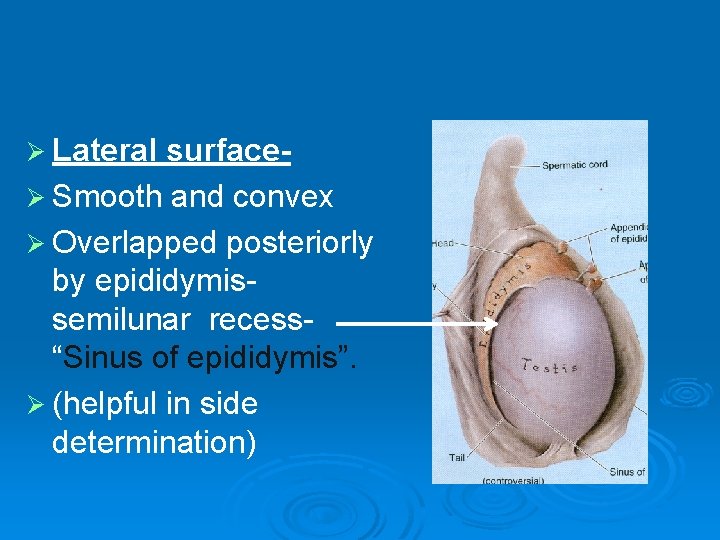
Ø Lateral surfaceØ Smooth and convex Ø Overlapped posteriorly by epididymissemilunar recess“Sinus of epididymis”. Ø (helpful in side determination)
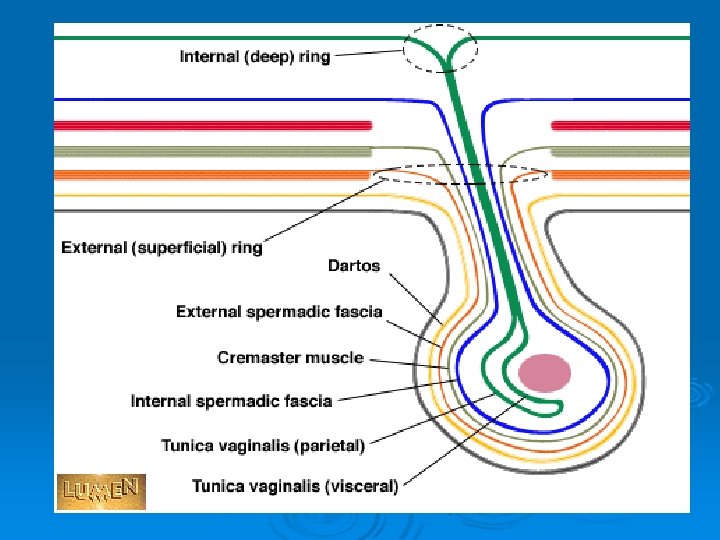
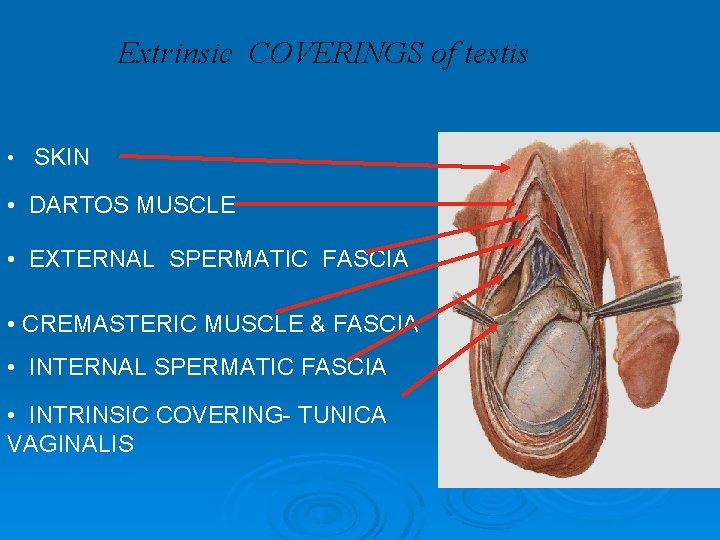
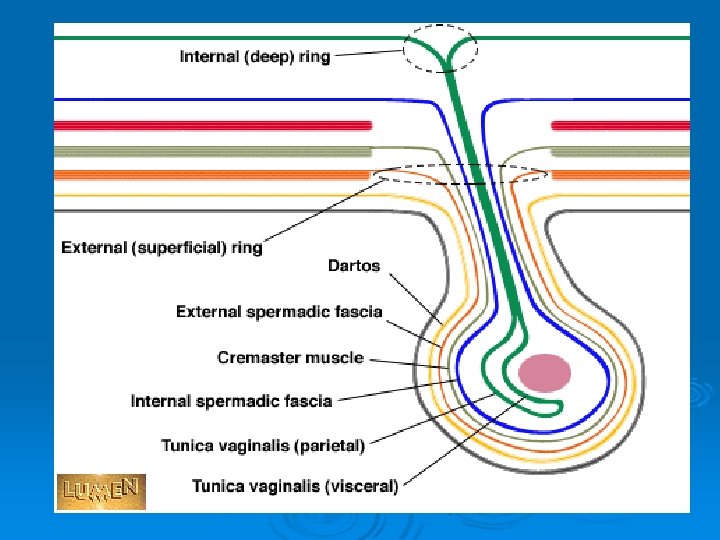
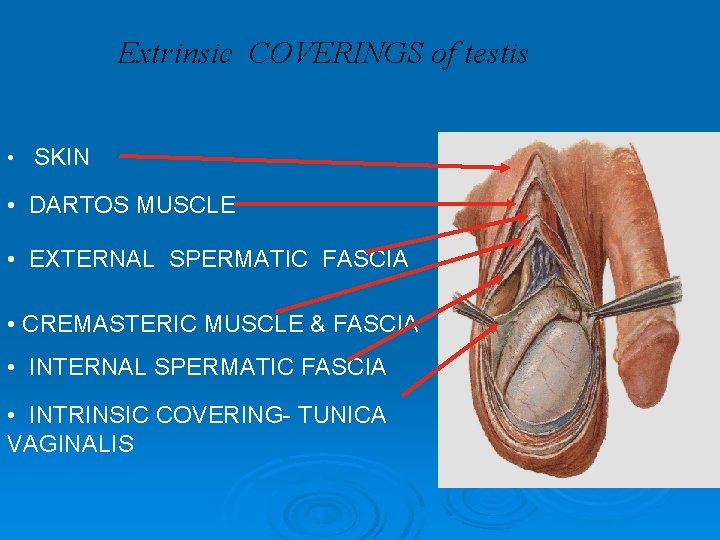
Extrinsic COVERINGS of testis • SKIN • DARTOS MUSCLE • EXTERNAL SPERMATIC FASCIA • CREMASTERIC MUSCLE & FASCIA • INTERNAL SPERMATIC FASCIA • INTRINSIC COVERING- TUNICA VAGINALIS
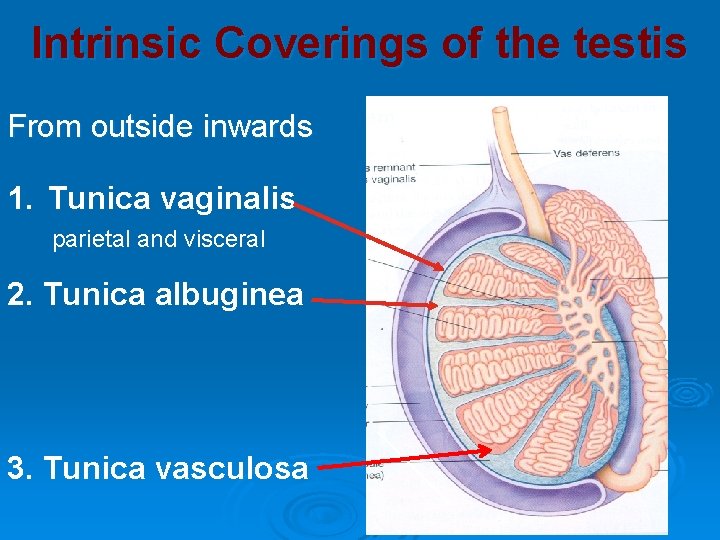
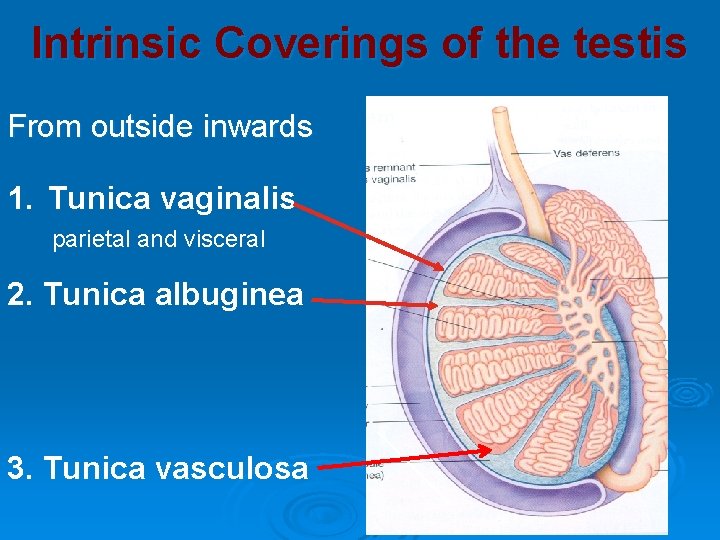
Intrinsic Coverings of the testis From outside inwards 1. Tunica vaginalis parietal and visceral 2. Tunica albuginea 3. Tunica vasculosa
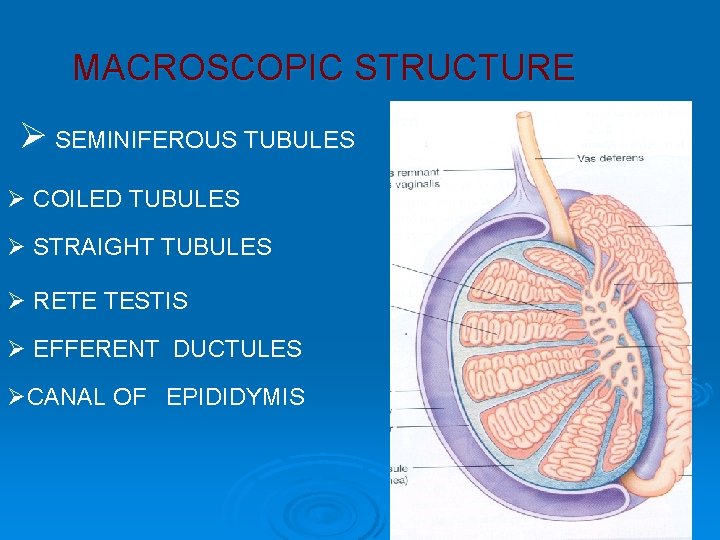
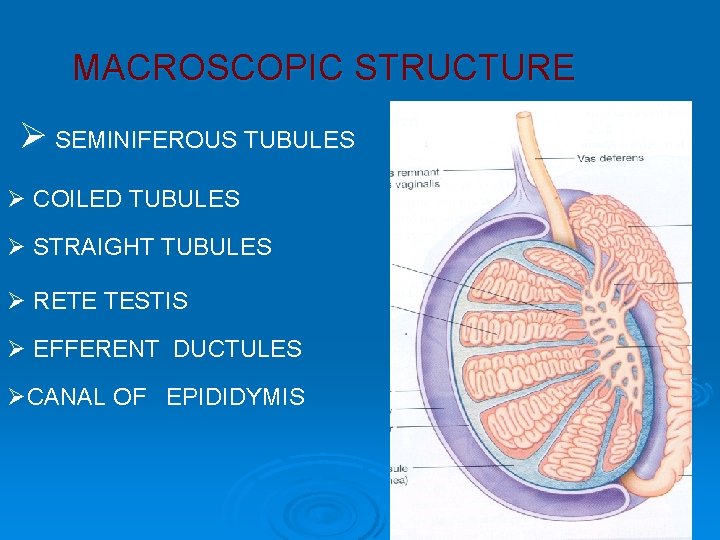
MACROSCOPIC STRUCTURE Ø SEMINIFEROUS TUBULES Ø COILED TUBULES Ø STRAIGHT TUBULES Ø RETE TESTIS Ø EFFERENT DUCTULES ØCANAL OF EPIDIDYMIS
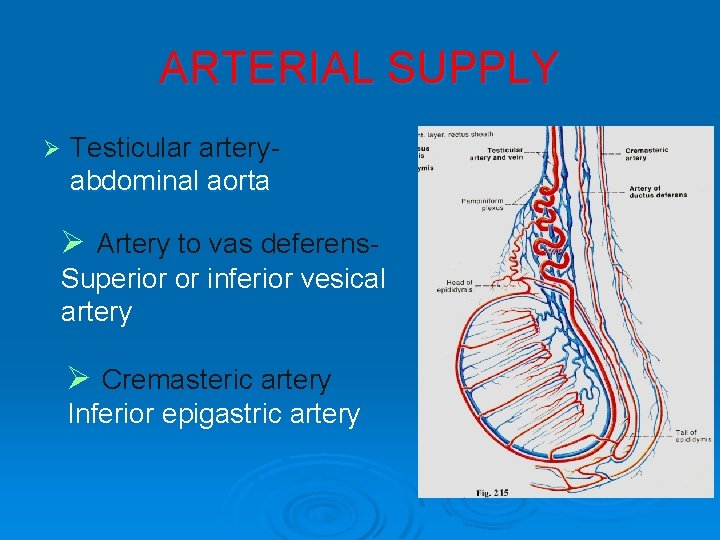
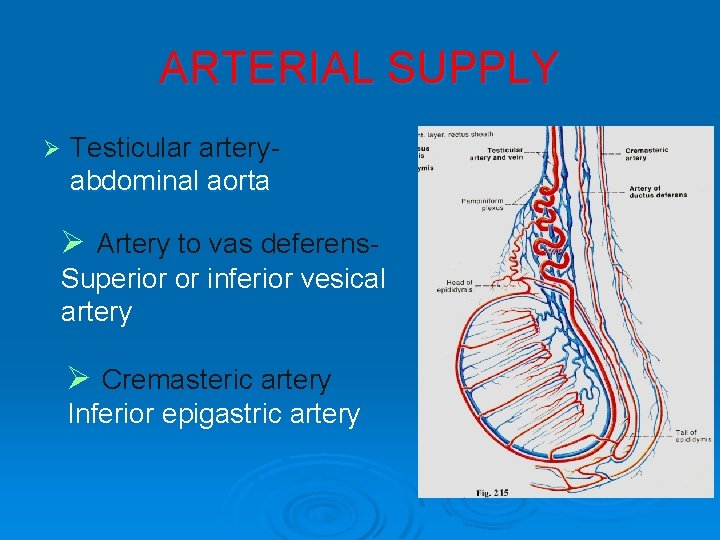
ARTERIAL SUPPLY Ø Testicular arteryabdominal aorta Ø Artery to vas deferens. Superior or inferior vesical artery Ø Cremasteric artery Inferior epigastric artery
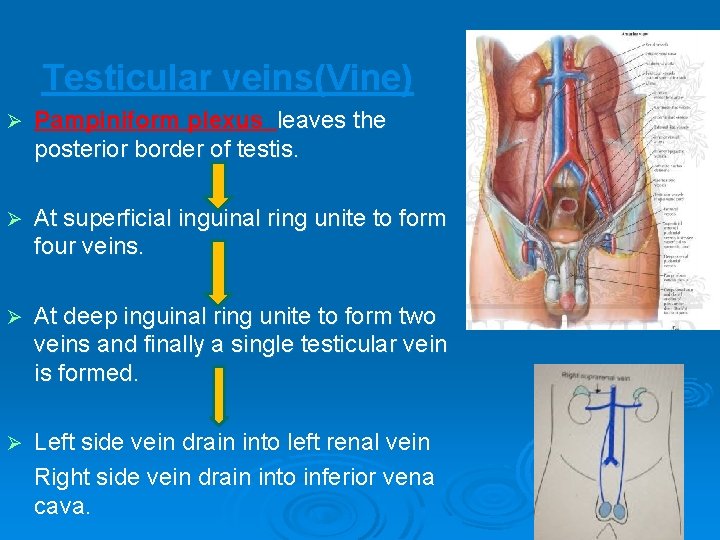
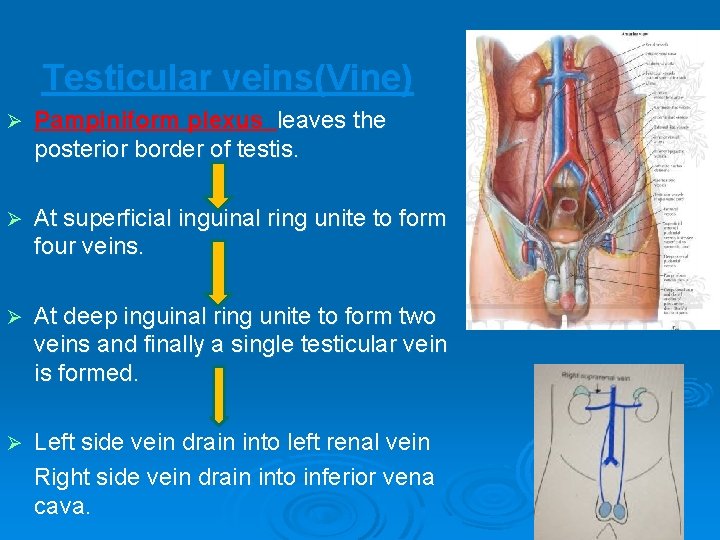
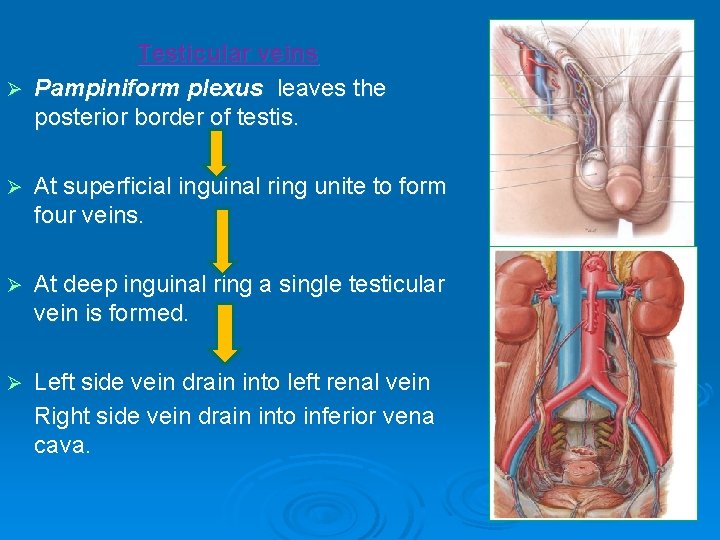
Testicular veins(Vine) Ø Pampiniform plexus leaves the posterior border of testis. Ø At superficial inguinal ring unite to form four veins. Ø At deep inguinal ring unite to form two veins and finally a single testicular vein is formed. Ø Left side vein drain into left renal vein Right side vein drain into inferior vena cava.
Ø Counter current heat exchange Ø The heat conveyed by the arteries of testis-absorbedveins of pampiniform plexus. Ø Scrotal temp of testis-3 to 40 c less than abdomen.
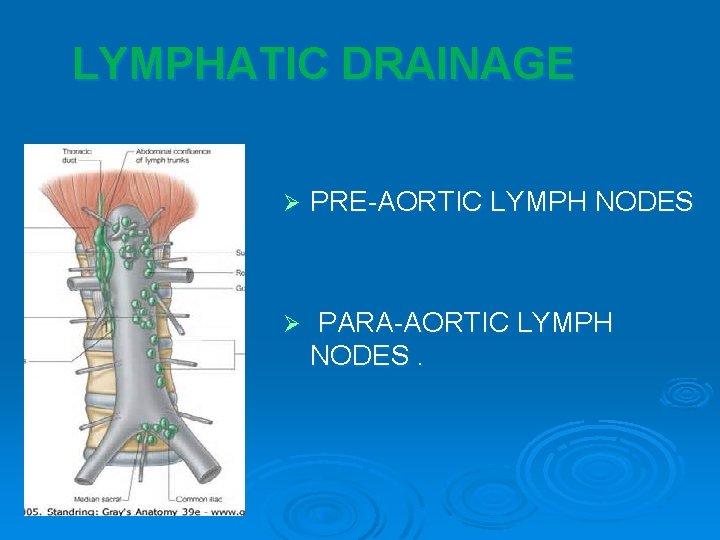
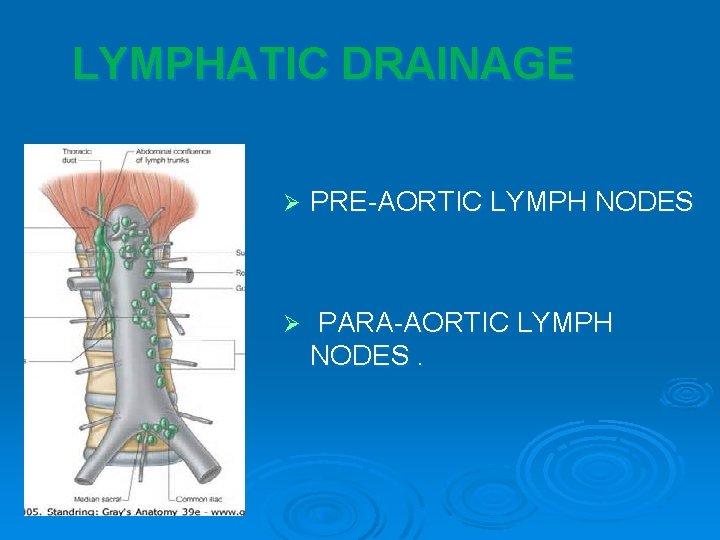
LYMPHATIC DRAINAGE Ø PRE-AORTIC LYMPH NODES Ø PARA-AORTIC LYMPH NODES.
NERVE SUPPLY - Sympathetic – Renal and aortic plexuses. - Pre ganglionic fibres -T 10 and T 11 segments of spinal cord. - Referred pain from testis to umbilicus can be due to segmental innervation.
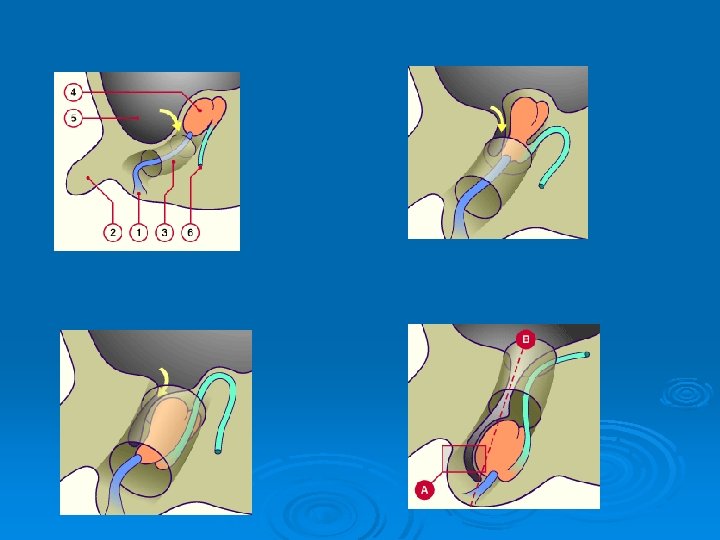
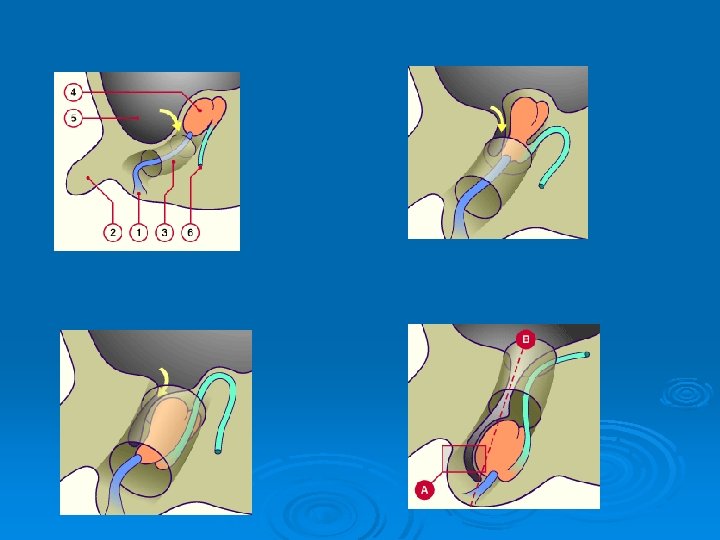
DESCENT OF TESTIS v. TESTIS develops retro peritoneal in dorsal abdominal wall at the level of T 10 - T 12. STARTS descending from second month of intra uterine life. v
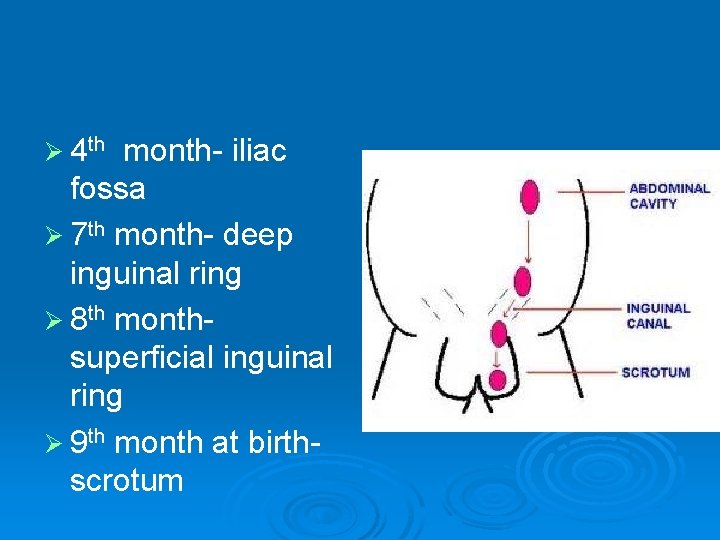
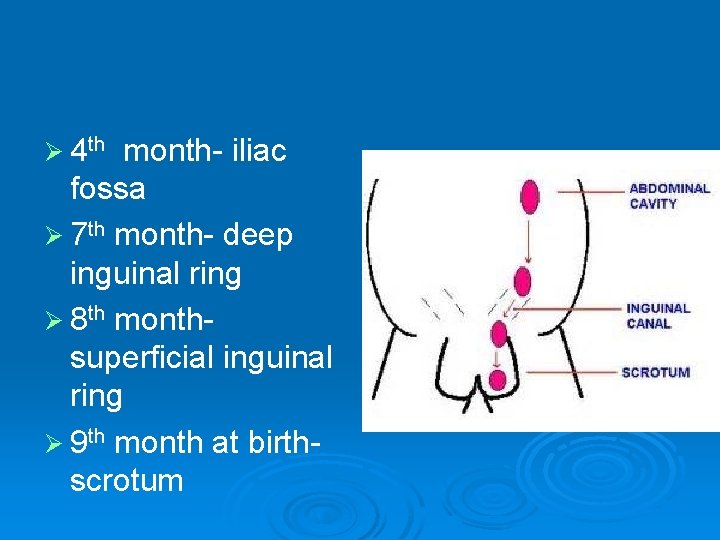
Ø 4 th month- iliac fossa Ø 7 th month- deep inguinal ring Ø 8 th monthsuperficial inguinal ring Ø 9 th month at birthscrotum
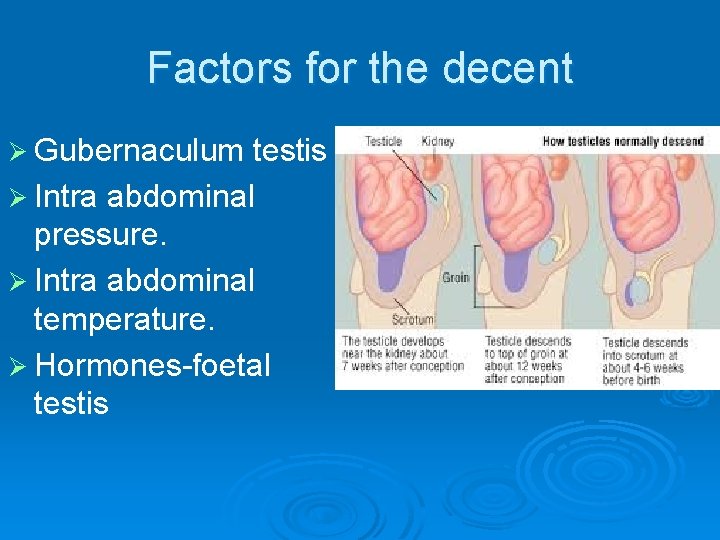
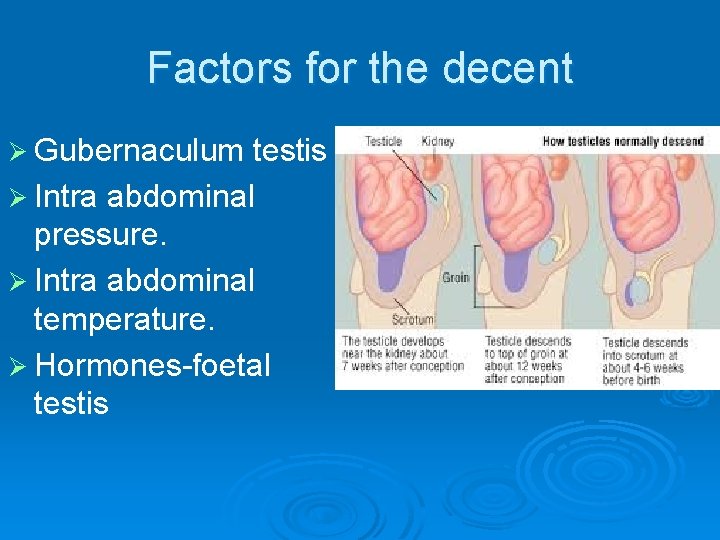
Factors for the decent Ø Gubernaculum testis Ø Intra abdominal pressure. Ø Intra abdominal temperature. Ø Hormones-foetal testis
APPLIED ANATOMY Ø MONORCHISM- unilateral absence of testis Ø ANORCHISM –bilateral absence of testis

UNDESCENDED TESTIS (cryptorchidism) CAUSES: -MUSCULAR HYPOTONIA -GUBERNACULUM DYSFUNCTION -HORMONES COMPLICATIONS: - TRAUMA E - EPIDIDYMO-ORCHITIS S - STERILITY T - TORSION I - INDIRECT HERNIA S - SEMINOMA OF TESTIS
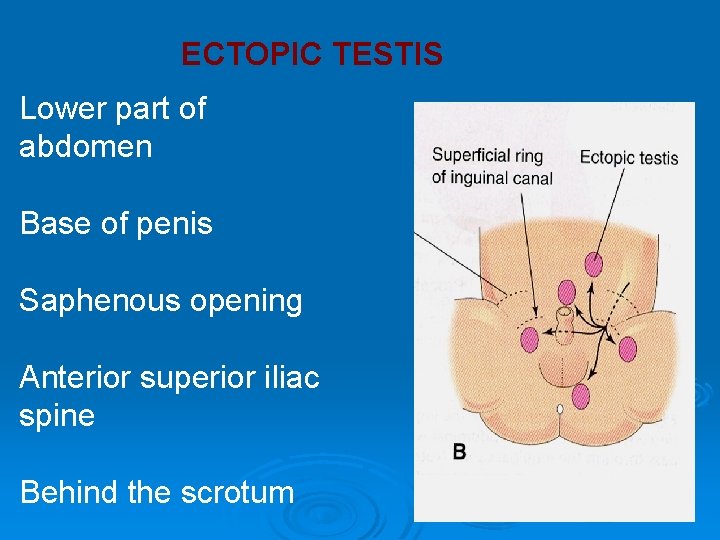
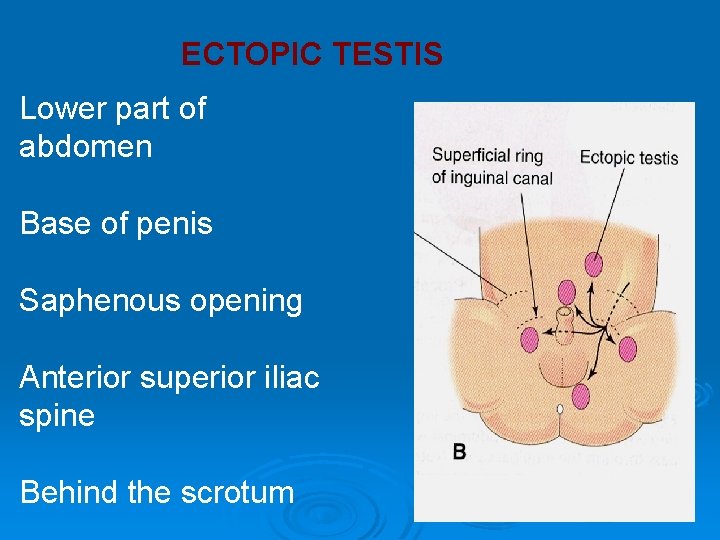
ECTOPIC TESTIS Lower part of abdomen Base of penis Saphenous opening Anterior superior iliac spine Behind the scrotum
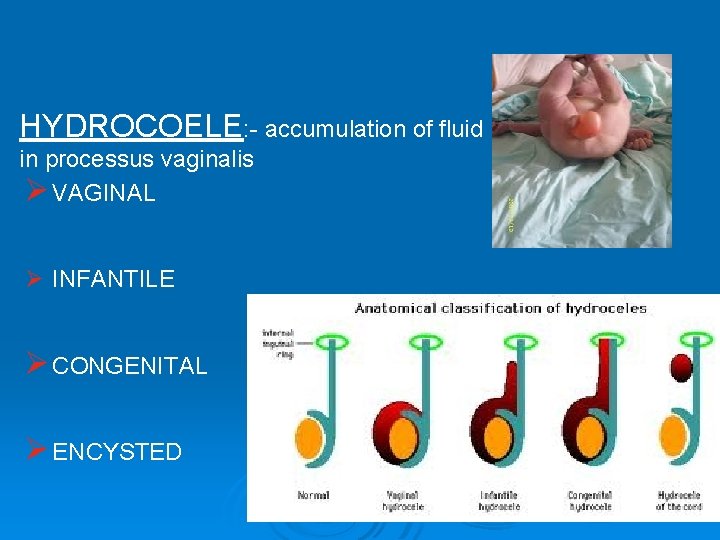
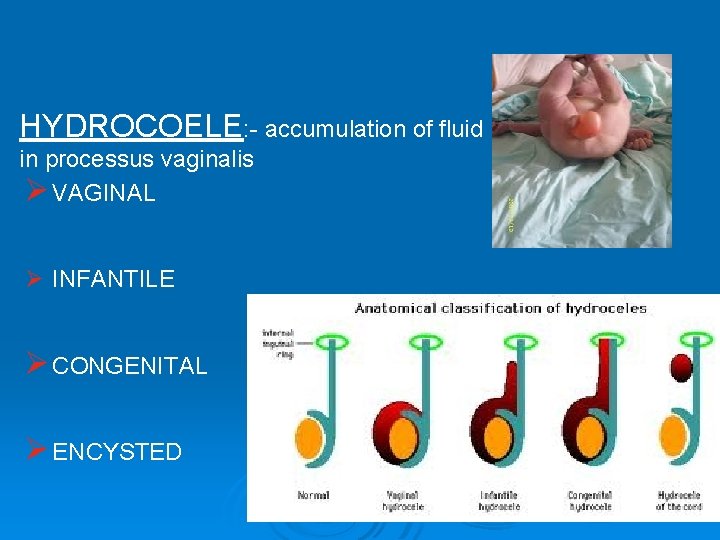
HYDROCOELE: - accumulation of fluid in processus vaginalis Ø VAGINAL Ø INFANTILE Ø CONGENITAL Ø ENCYSTED
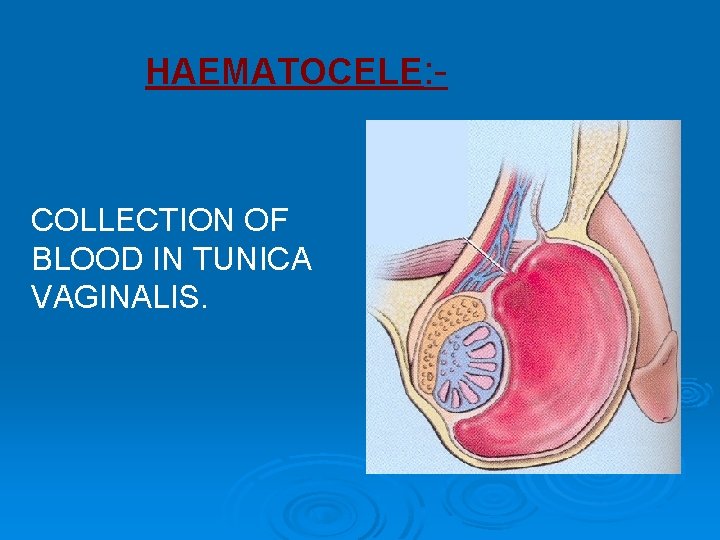
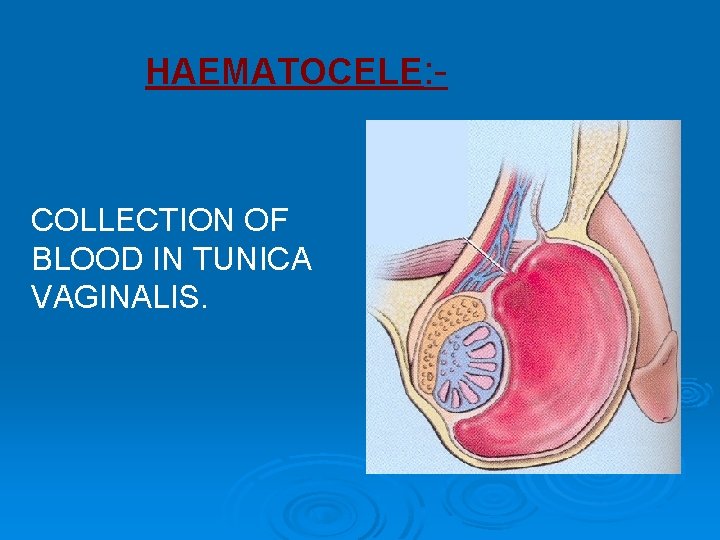
HAEMATOCELE: - COLLECTION OF BLOOD IN TUNICA VAGINALIS.
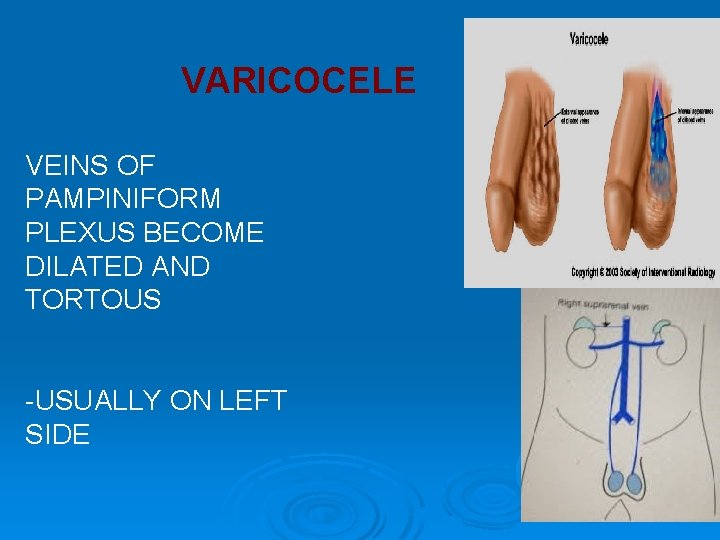
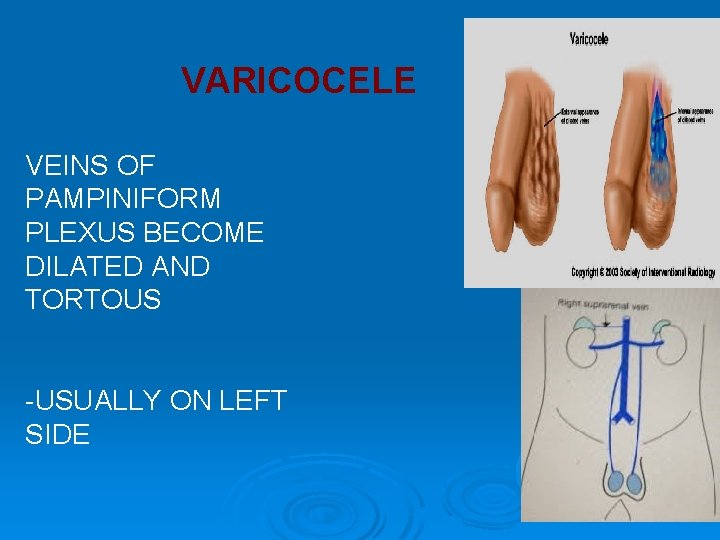
VARICOCELE VEINS OF PAMPINIFORM PLEXUS BECOME DILATED AND TORTOUS -USUALLY ON LEFT SIDE
LYMPH VARIX -LYMPHATIC VESSELS OF THE CORD BECOMES DILATED AND TORTOUS -CAUSED BY OBSTRUCTION DUE TO FILARIASIS
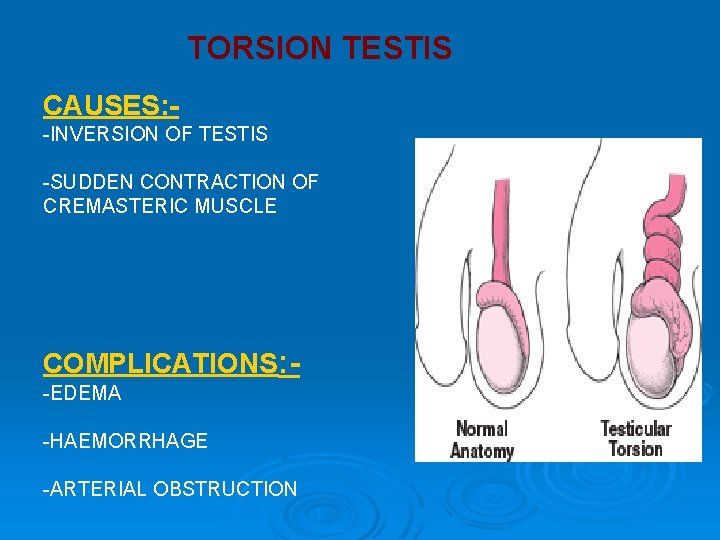
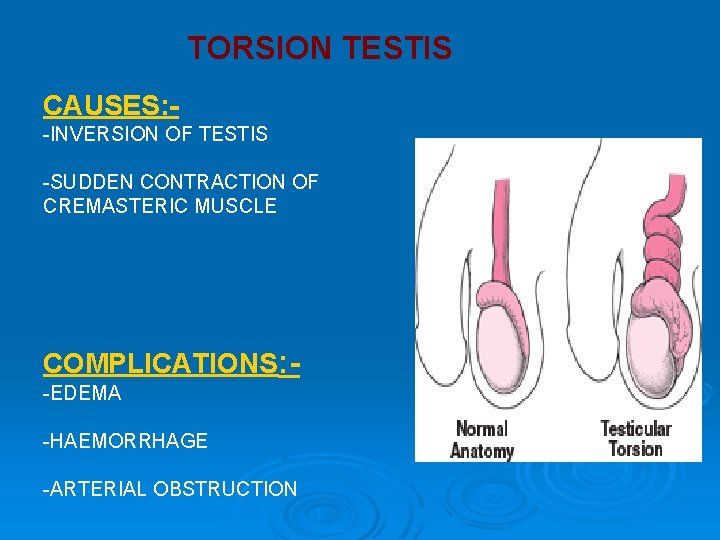
TORSION TESTIS CAUSES: -INVERSION OF TESTIS -SUDDEN CONTRACTION OF CREMASTERIC MUSCLE COMPLICATIONS: -EDEMA -HAEMORRHAGE -ARTERIAL OBSTRUCTION
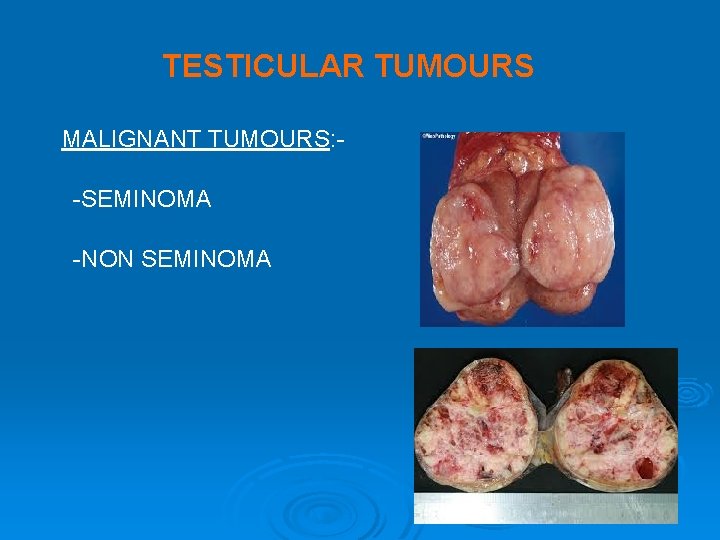
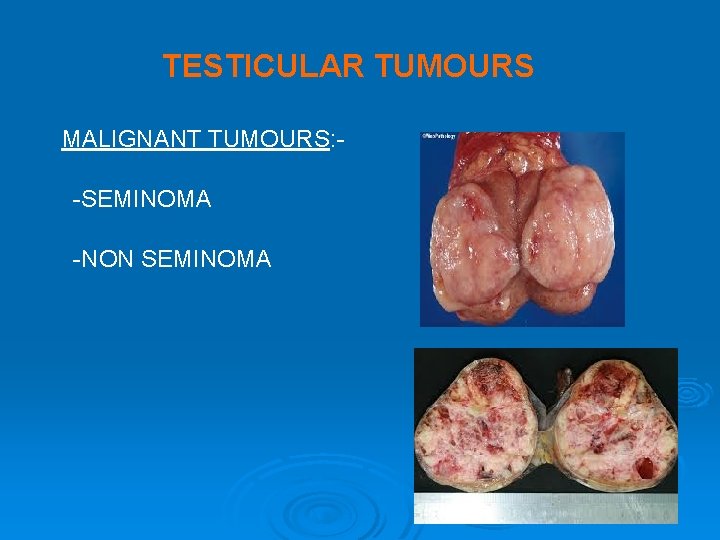
TESTICULAR TUMOURS MALIGNANT TUMOURS: -SEMINOMA -NON SEMINOMA
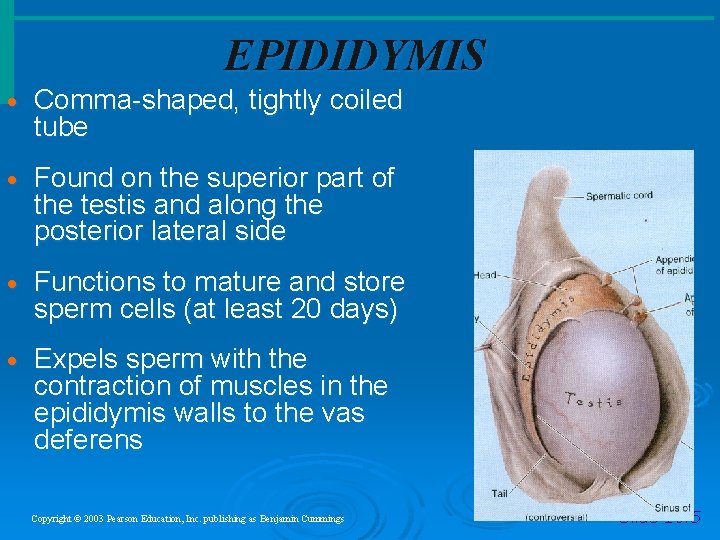
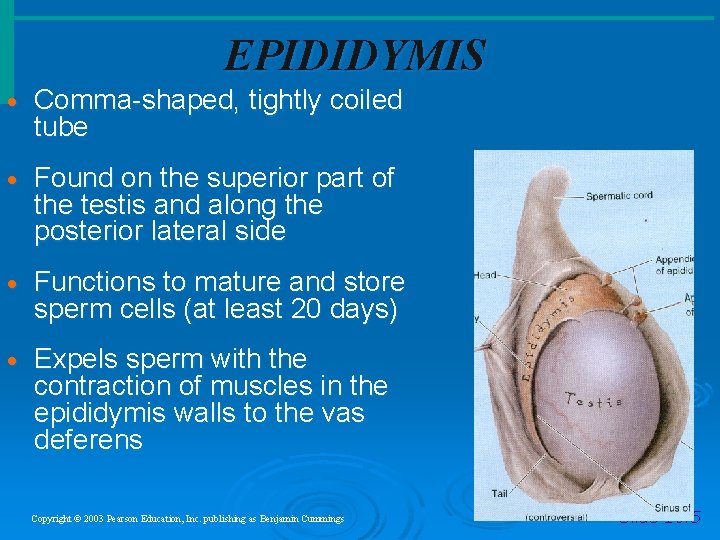
EPIDIDYMIS · Comma-shaped, tightly coiled tube · Found on the superior part of the testis and along the posterior lateral side · Functions to mature and store sperm cells (at least 20 days) · Expels sperm with the contraction of muscles in the epididymis walls to the vas deferens Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide 16. 5
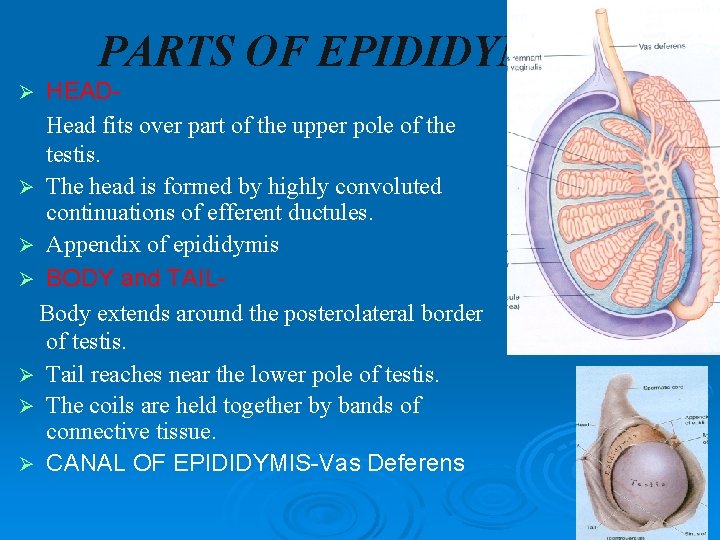
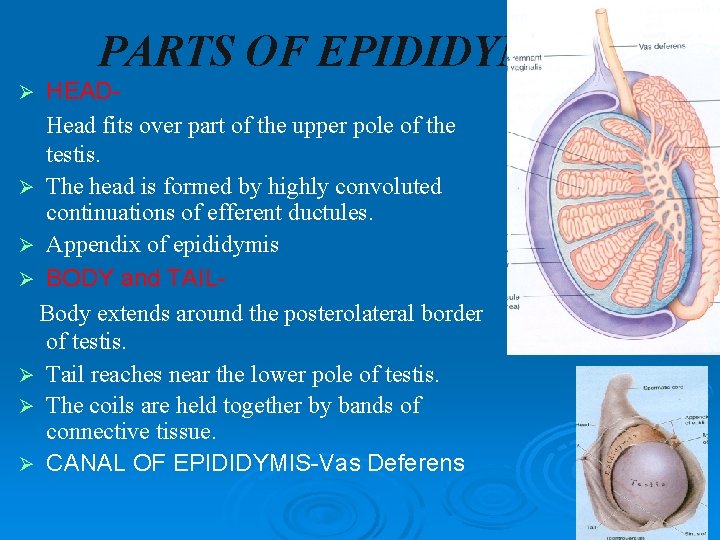
PARTS OF EPIDIDYMIS HEADHead fits over part of the upper pole of the testis. Ø The head is formed by highly convoluted continuations of efferent ductules. Ø Appendix of epididymis Ø BODY and TAILBody extends around the posterolateral border of testis. Ø Tail reaches near the lower pole of testis. Ø The coils are held together by bands of connective tissue. Ø CANAL OF EPIDIDYMIS-Vas Deferens Ø
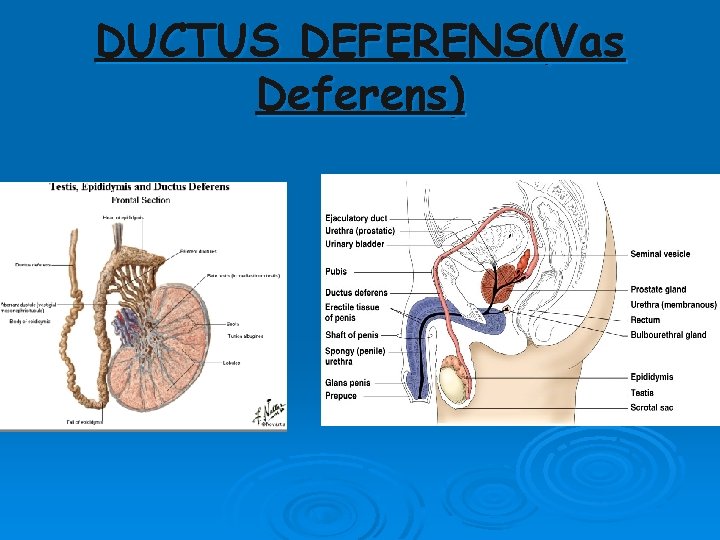
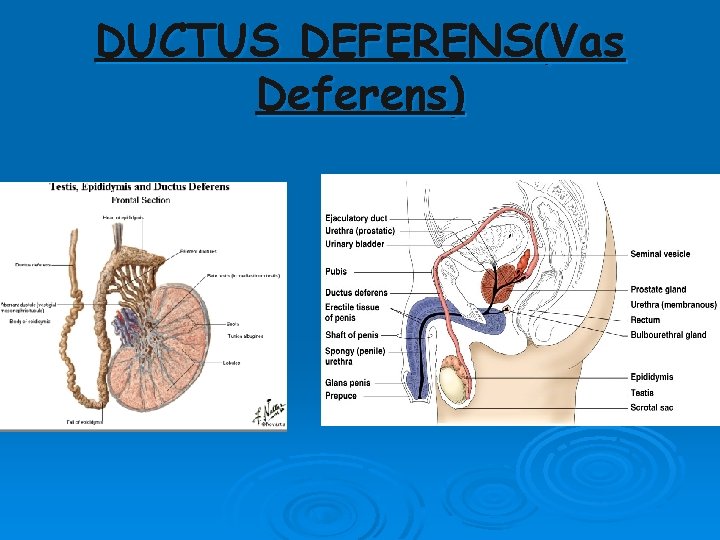
DUCTUS DEFERENS(Vas Deferens)
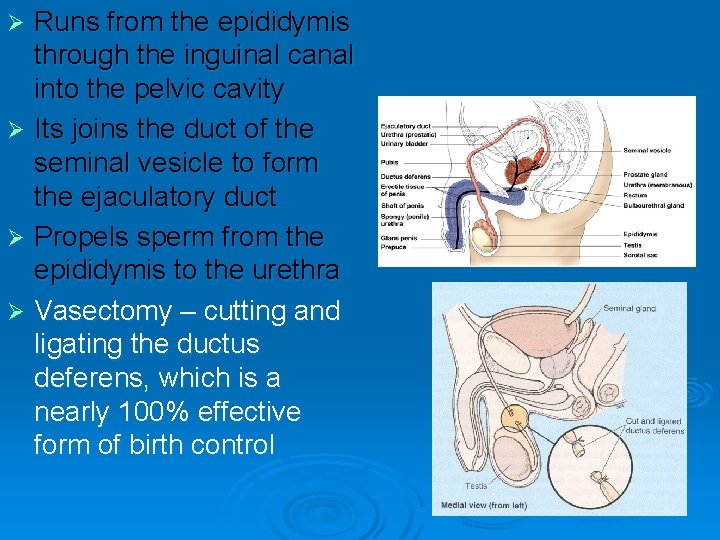
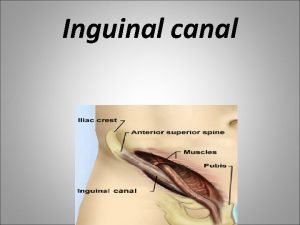
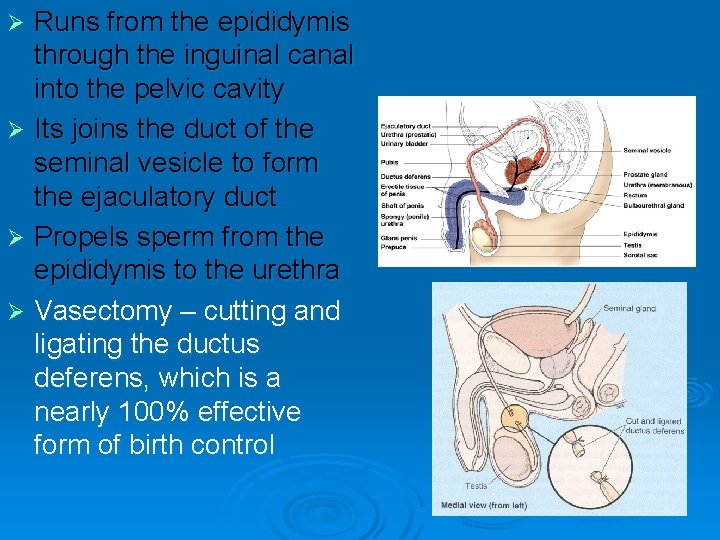
Runs from the epididymis through the inguinal canal into the pelvic cavity Ø Its joins the duct of the seminal vesicle to form the ejaculatory duct Ø Propels sperm from the epididymis to the urethra Ø Vasectomy – cutting and ligating the ductus deferens, which is a nearly 100% effective form of birth control Ø
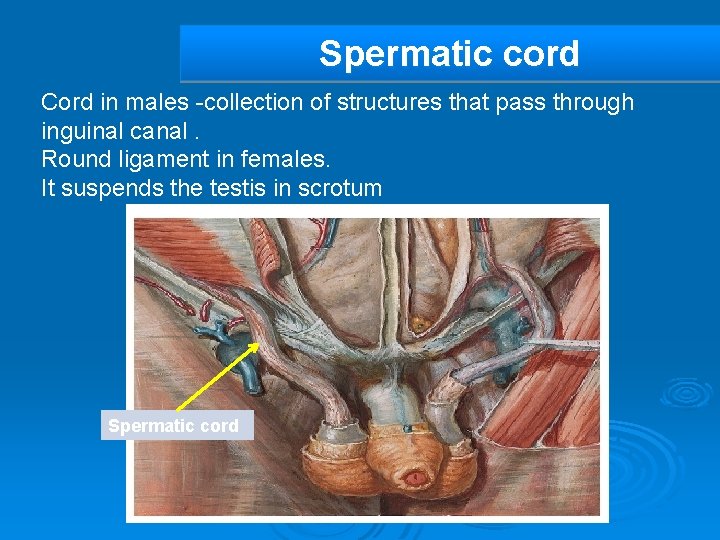
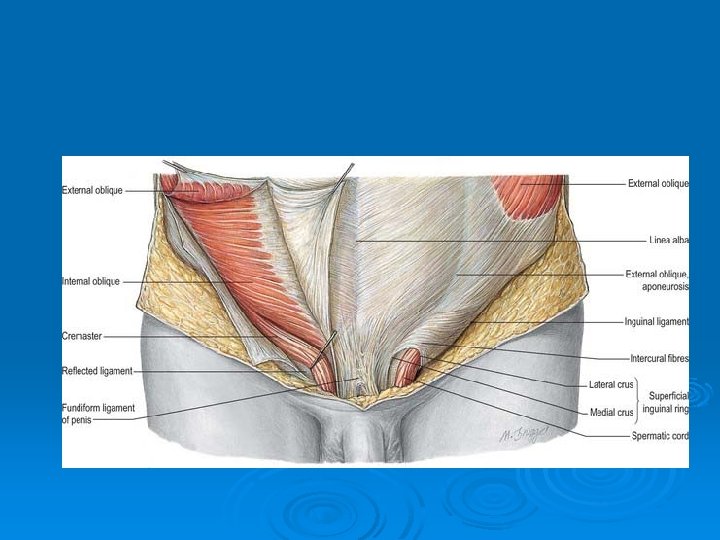
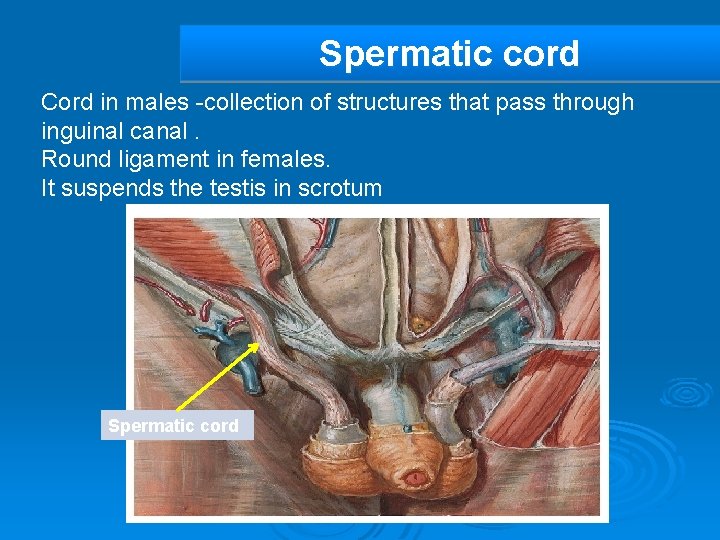
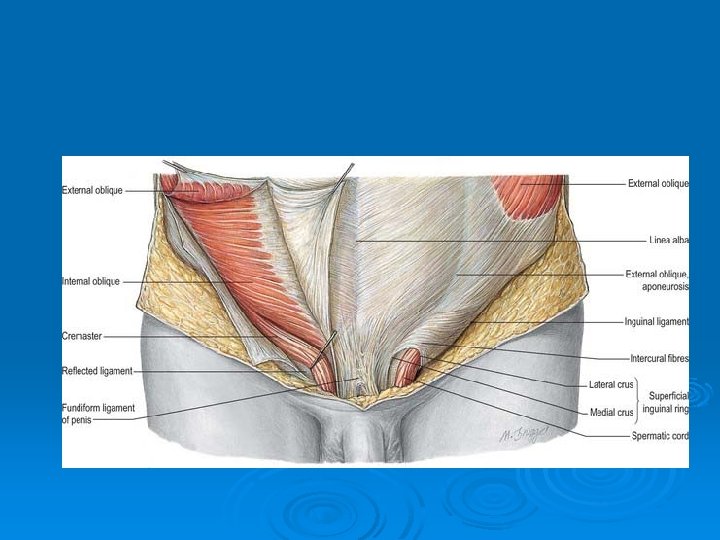
Spermatic cord Cord in males -collection of structures that pass through inguinal canal. Round ligament in females. It suspends the testis in scrotum Spermatic cord
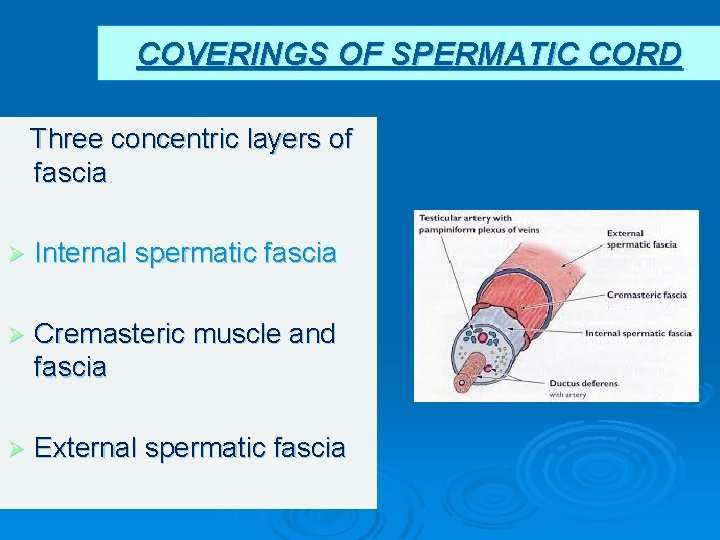
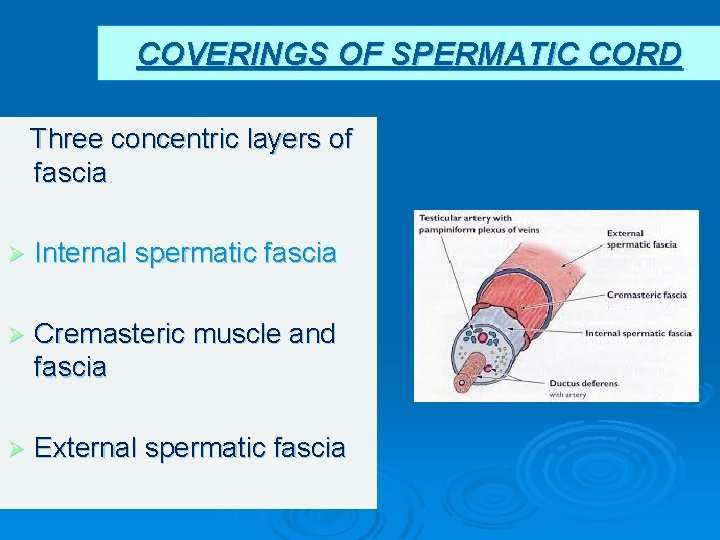
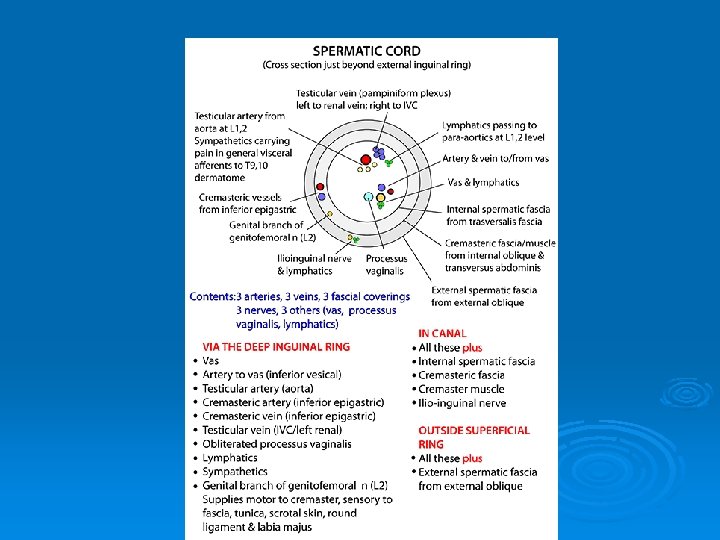
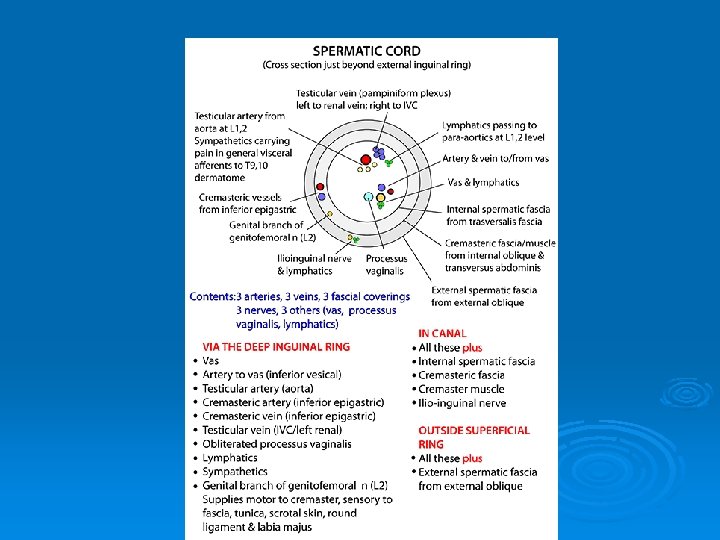
COVERINGS OF SPERMATIC CORD Three concentric layers of fascia. Ø Internal spermatic fascia Ø Cremasteric muscle and fascia Ø External spermatic fascia
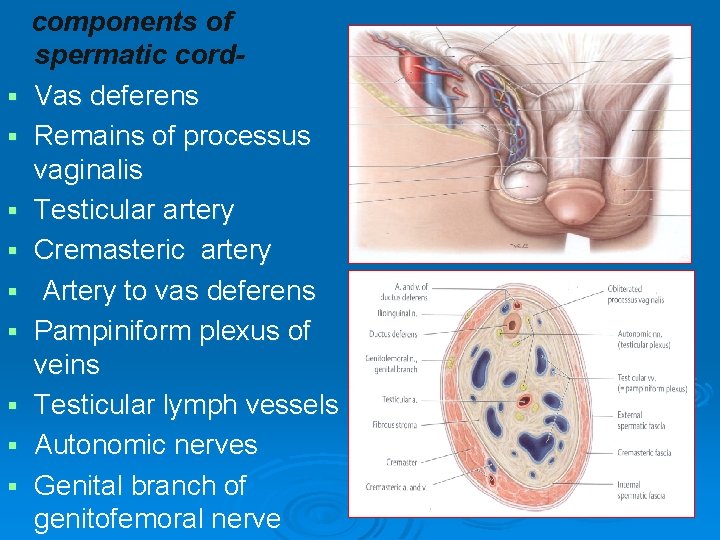
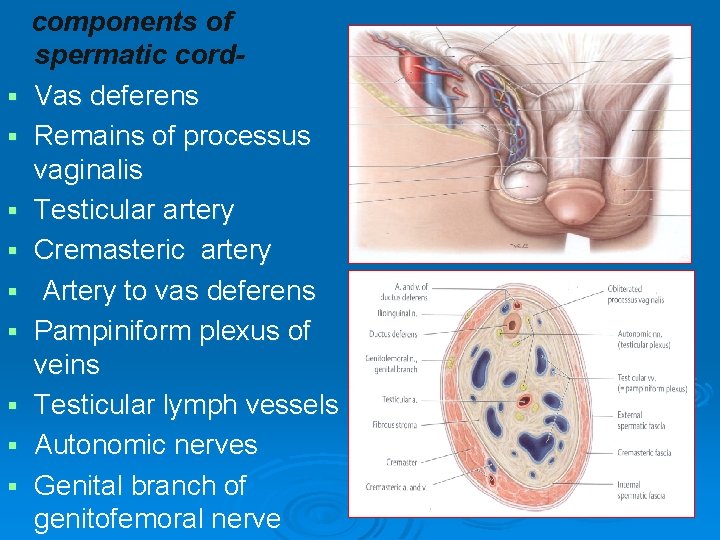
§ § § § § components of spermatic cord. Vas deferens Remains of processus vaginalis Testicular artery Cremasteric artery Artery to vas deferens Pampiniform plexus of veins Testicular lymph vessels Autonomic nerves Genital branch of genitofemoral nerve
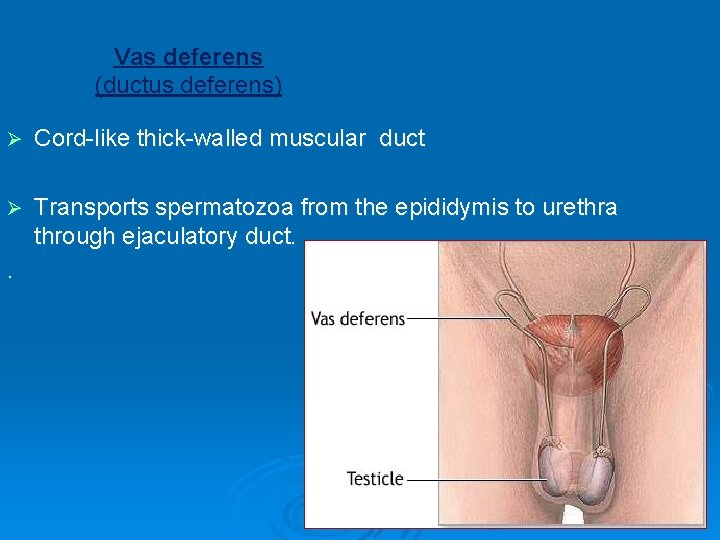
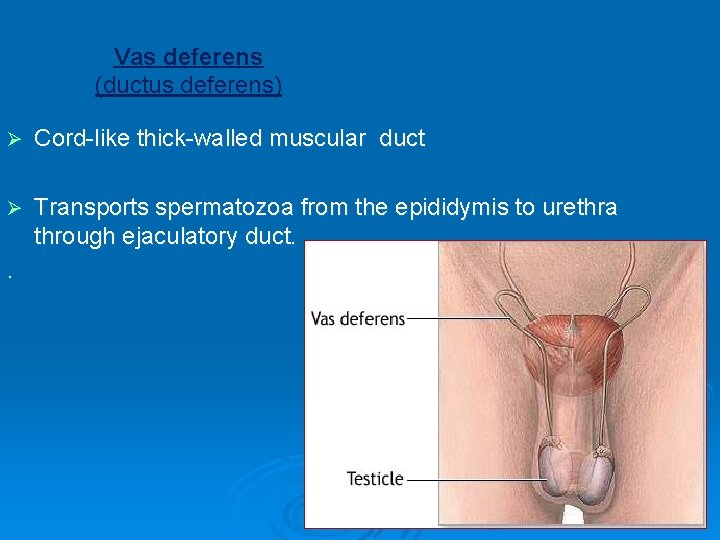
Vas deferens (ductus deferens) Ø Cord-like thick-walled muscular duct Ø Transports spermatozoa from the epididymis to urethra through ejaculatory duct. .
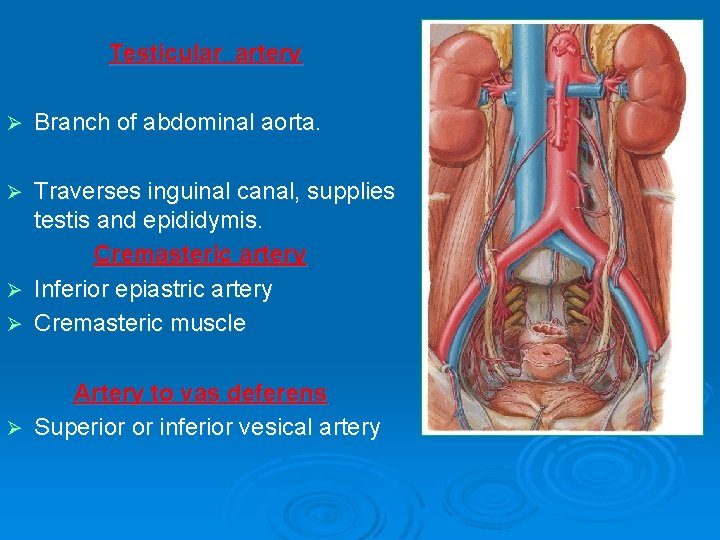
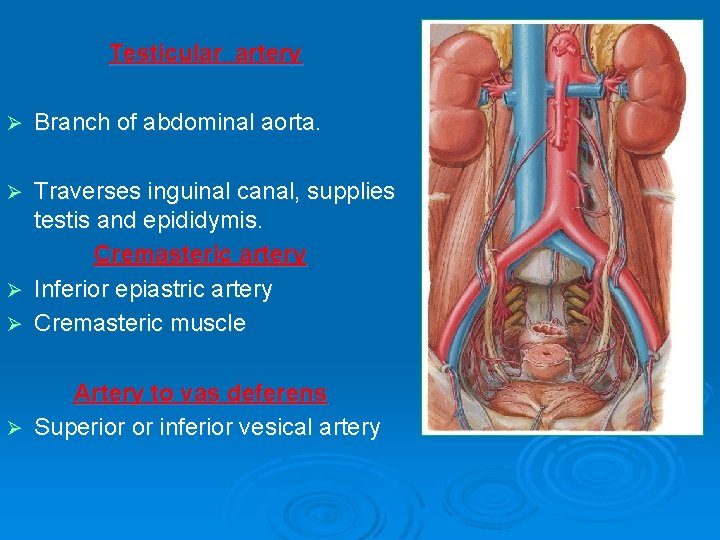
Testicular artery Ø Branch of abdominal aorta. Traverses inguinal canal, supplies testis and epididymis. Cremasteric artery Ø Inferior epiastric artery Ø Cremasteric muscle Ø Artery to vas deferens Ø Superior or inferior vesical artery
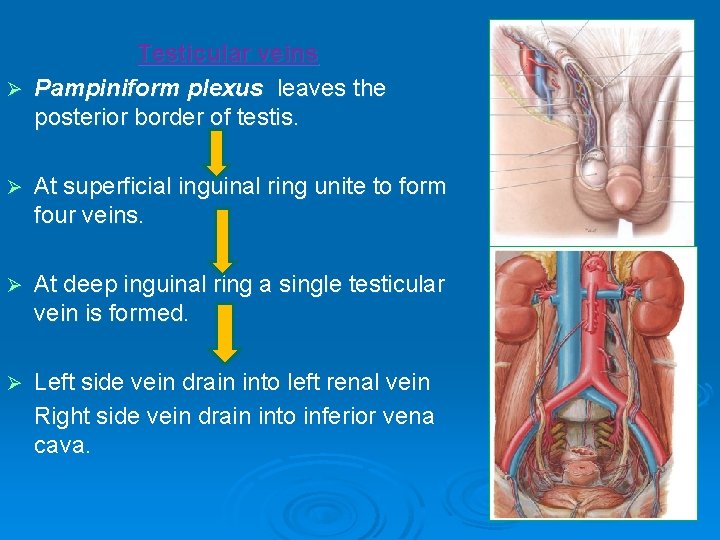
Testicular veins Ø Pampiniform plexus leaves the posterior border of testis. Ø At superficial inguinal ring unite to form four veins. Ø At deep inguinal ring a single testicular vein is formed. Ø Left side vein drain into left renal vein Right side vein drain into inferior vena cava.
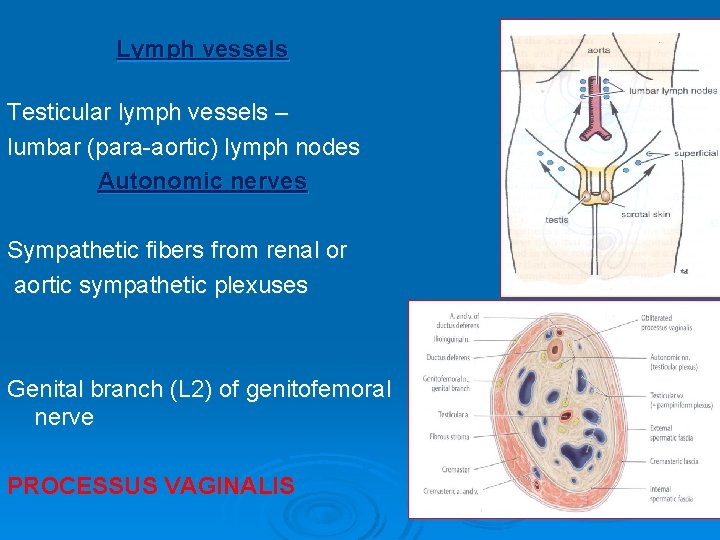
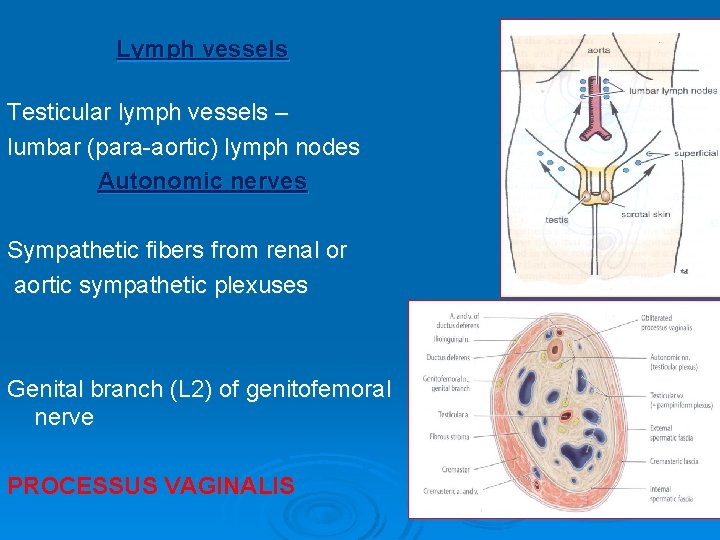
Lymph vessels Testicular lymph vessels – lumbar (para-aortic) lymph nodes Autonomic nerves Sympathetic fibers from renal or aortic sympathetic plexuses Genital branch (L 2) of genitofemoral nerve PROCESSUS VAGINALIS
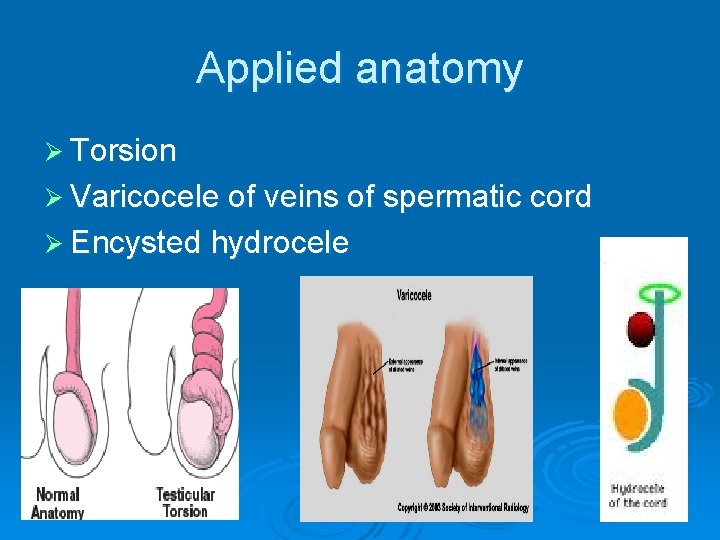
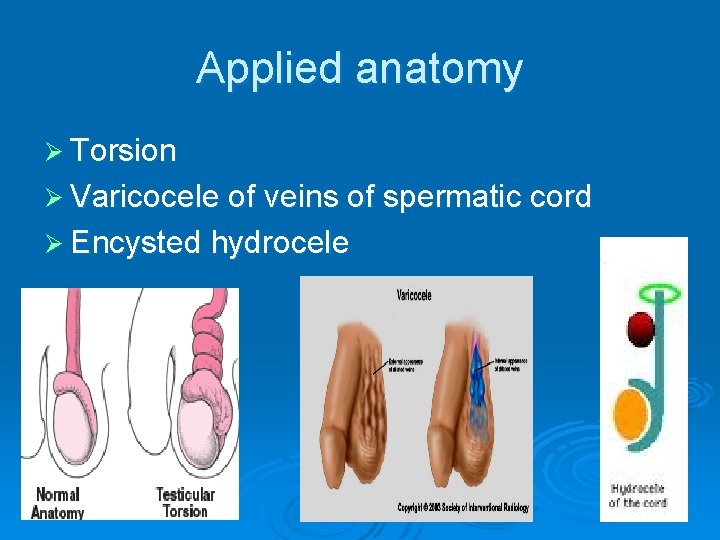
Applied anatomy Ø Torsion Ø Varicocele of veins of spermatic cord Ø Encysted hydrocele

 Good afternoon buenas tardes
Good afternoon buenas tardes Ejaculatory duct
Ejaculatory duct Mnemonic for contents of spermatic cord
Mnemonic for contents of spermatic cord External ring hernia
External ring hernia Hesselbach's triangle borders
Hesselbach's triangle borders Spermatic cord coverings
Spermatic cord coverings Dartos muscle
Dartos muscle Inversion of testis
Inversion of testis Deep fascia of abdominal wall
Deep fascia of abdominal wall Dr hassan urology
Dr hassan urology Superficial inguinal ring
Superficial inguinal ring Urinary bladder
Urinary bladder Terminologi medis sistem reproduksi
Terminologi medis sistem reproduksi Spermatic cord contents rule of 3's
Spermatic cord contents rule of 3's Indirect v direct hernia
Indirect v direct hernia Mesovarium
Mesovarium Secrotal
Secrotal Good morning class
Good morning class Good afternoon teachers
Good afternoon teachers Good morning and welcome back
Good morning and welcome back Good morning good morning to you i am glad to see you
Good morning good morning to you i am glad to see you Hello, good afternoon
Hello, good afternoon Hello good afternoon teacher
Hello good afternoon teacher Good morning hello
Good morning hello Function of testicle
Function of testicle Cat vagina
Cat vagina Muscolo elevatore dell'ano
Muscolo elevatore dell'ano Quizlet
Quizlet The epididymis is a long coiled tube that sits atop the
The epididymis is a long coiled tube that sits atop the Funiculus spermaticus
Funiculus spermaticus Ligamentum pubocervicale
Ligamentum pubocervicale Good morning ladies and gentleman
Good morning ladies and gentleman Good charlotte the young and the hopeless
Good charlotte the young and the hopeless Good morning good lookin
Good morning good lookin Good morning, students
Good morning, students Good evening ladies and gentlemen. we are now
Good evening ladies and gentlemen. we are now Good thought good words good deeds
Good thought good words good deeds You are good you are good when theres nothing good in me
You are good you are good when theres nothing good in me What are gonads
What are gonads Gental organ
Gental organ Morning i see you in the sunrise every morning
Morning i see you in the sunrise every morning Brother john lyrics
Brother john lyrics Good morning and welcome back
Good morning and welcome back Good morning and assalamualaikum
Good morning and assalamualaikum Good morning lady and gentlemen
Good morning lady and gentlemen Good morning to one and all
Good morning to one and all Good morning and welcome back
Good morning and welcome back Good morning, boys and girls
Good morning, boys and girls