1 st lecture ANTERIOR ABDOMINAL WALL AND INGUINAL
1 st lecture ANTERIOR ABDOMINAL WALL AND INGUINAL CANAL
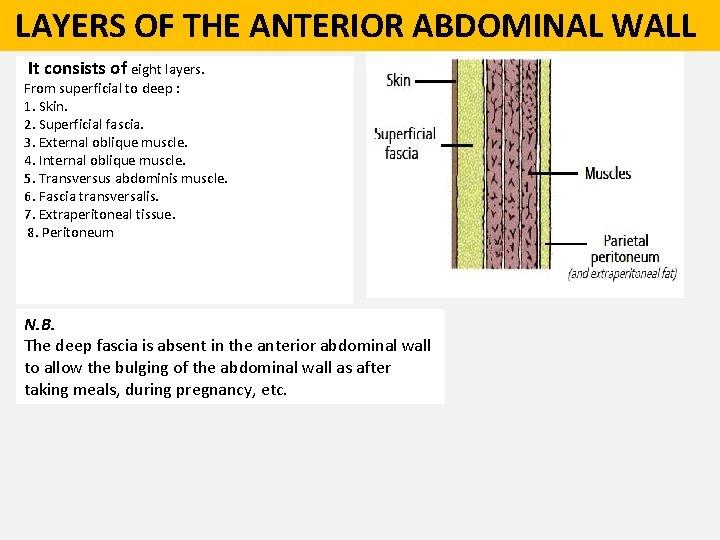
LAYERS OF THE ANTERIOR ABDOMINAL WALL It consists of eight layers. From superficial to deep : 1. Skin. 2. Superficial fascia. 3. External oblique muscle. 4. Internal oblique muscle. 5. Transversus abdominis muscle. 6. Fascia transversalis. 7. Extraperitoneal tissue. 8. Peritoneum N. B. The deep fascia is absent in the anterior abdominal wall to allow the bulging of the abdominal wall as after taking meals, during pregnancy, etc.
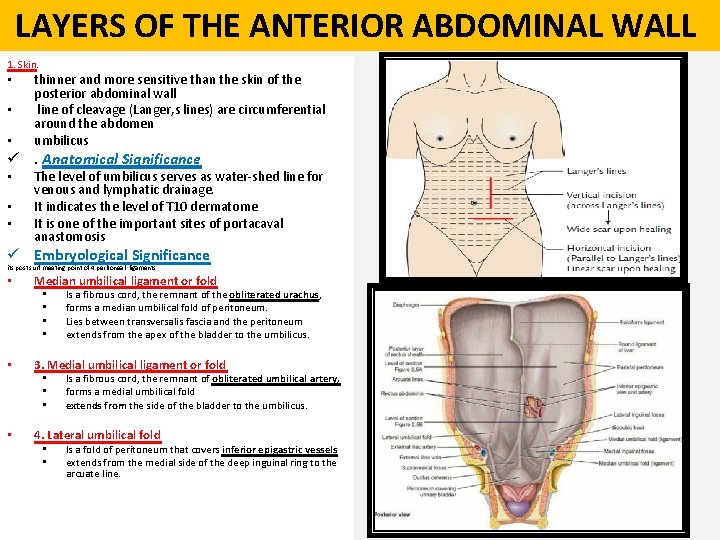
LAYERS OF THE ANTERIOR ABDOMINAL WALL 1. Skin. • • • thinner and more sensitive than the skin of the posterior abdominal wall line of cleavage (Langer, s lines) are circumferential around the abdomen umbilicus ü. Anatomical Significance • • • The level of umbilicus serves as water-shed line for venous and lymphatic drainage. It indicates the level of T 10 dermatome It is one of the important sites of portacaval anastomosis ü Embryological Significance its post surf meeting point of 4 peritoneal ligaments • Median umbilical ligament or fold • • • 3. Medial umbilical ligament or fold • • Is a fibrous cord, the remnant of the obliterated urachus, forms a median umbilical fold of peritoneum. Lies between transversalis fascia and the peritoneum extends from the apex of the bladder to the umbilicus. Is a fibrous cord, the remnant of obliterated umbilical artery, forms a medial umbilical fold extends from the side of the bladder to the umbilicus. 4. Lateral umbilical fold • • Is a fold of peritoneum that covers inferior epigastric vessels extends from the medial side of the deep inguinal ring to the arcuate line.
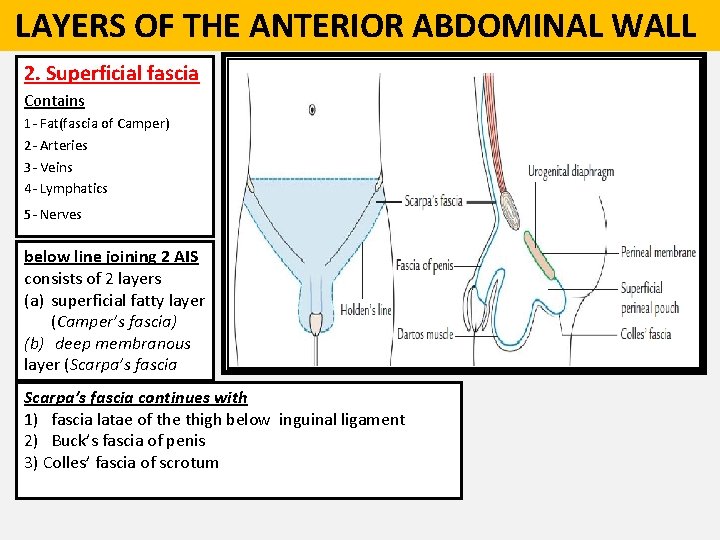
LAYERS OF THE ANTERIOR ABDOMINAL WALL 2. Superficial fascia Contains 1 - Fat(fascia of Camper) 2 - Arteries 3 - Veins 4 - Lymphatics 5 - Nerves below line joining 2 AIS consists of 2 layers (a) superficial fatty layer (Camper’s fascia) (b) deep membranous layer (Scarpa’s fascia continues with 1) fascia latae of the thigh below inguinal ligament 2) Buck’s fascia of penis 3) Colles’ fascia of scrotum
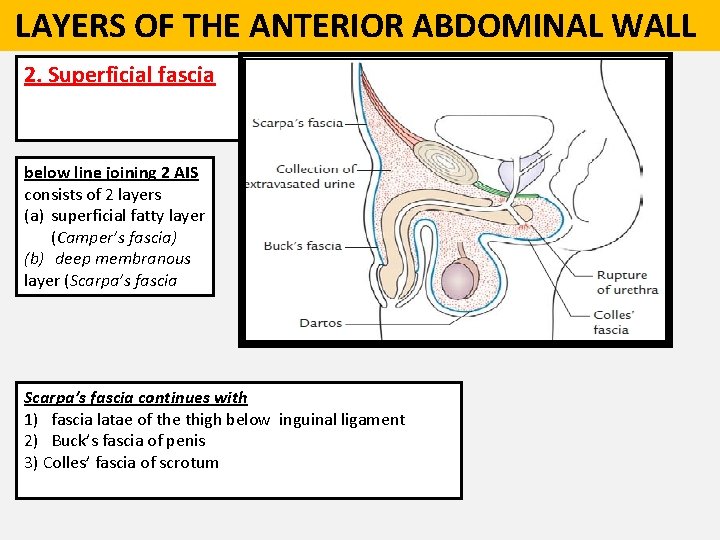
LAYERS OF THE ANTERIOR ABDOMINAL WALL 2. Superficial fascia below line joining 2 AIS consists of 2 layers (a) superficial fatty layer (Camper’s fascia) (b) deep membranous layer (Scarpa’s fascia continues with 1) fascia latae of the thigh below inguinal ligament 2) Buck’s fascia of penis 3) Colles’ fascia of scrotum
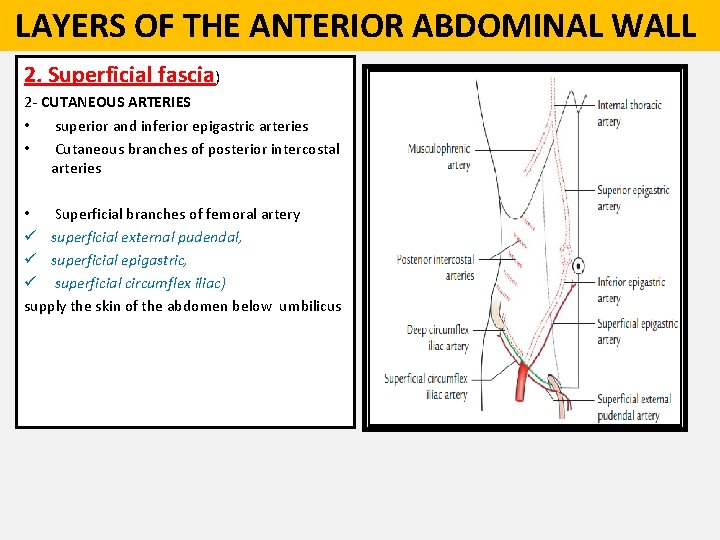
LAYERS OF THE ANTERIOR ABDOMINAL WALL 2. Superficial fascia) 2 - CUTANEOUS ARTERIES • superior and inferior epigastric arteries • Cutaneous branches of posterior intercostal arteries • Superficial branches of femoral artery ü superficial external pudendal, ü superficial epigastric, ü superficial circumflex iliac) supply the skin of the abdomen below umbilicus
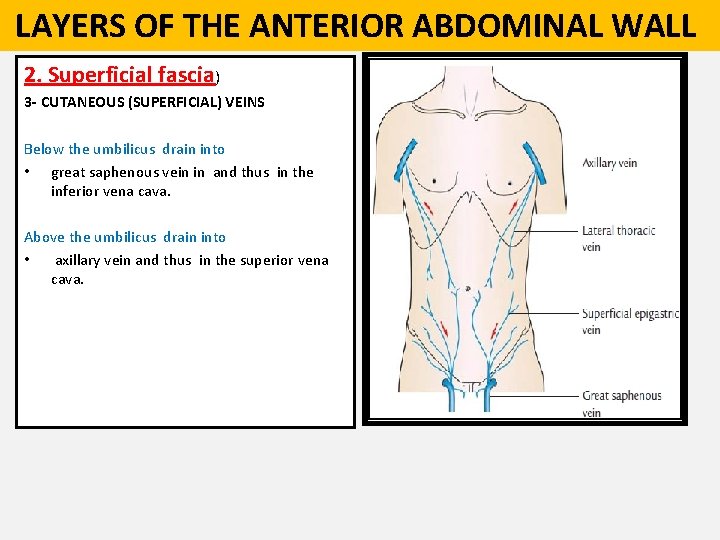
LAYERS OF THE ANTERIOR ABDOMINAL WALL 2. Superficial fascia) 3 - CUTANEOUS (SUPERFICIAL) VEINS Below the umbilicus drain into • great saphenous vein in and thus in the inferior vena cava. Above the umbilicus drain into • axillary vein and thus in the superior vena cava.
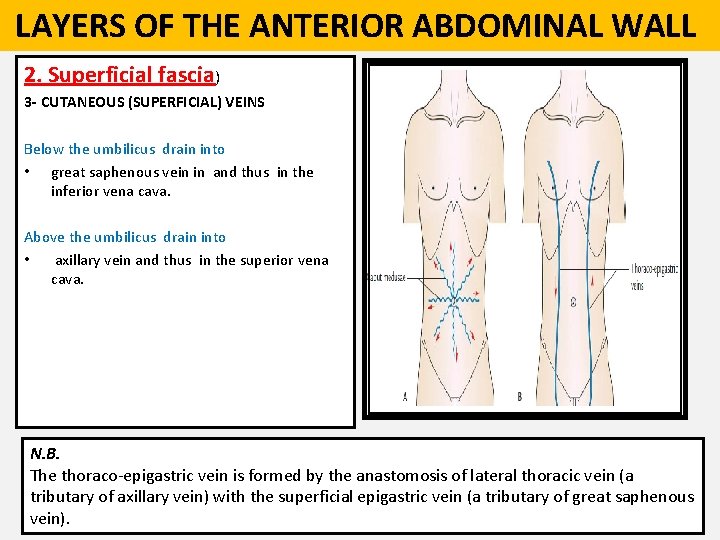
LAYERS OF THE ANTERIOR ABDOMINAL WALL 2. Superficial fascia) 3 - CUTANEOUS (SUPERFICIAL) VEINS Below the umbilicus drain into • great saphenous vein in and thus in the inferior vena cava. Above the umbilicus drain into • axillary vein and thus in the superior vena cava. N. B. The thoraco-epigastric vein is formed by the anastomosis of lateral thoracic vein (a tributary of axillary vein) with the superficial epigastric vein (a tributary of great saphenous vein).
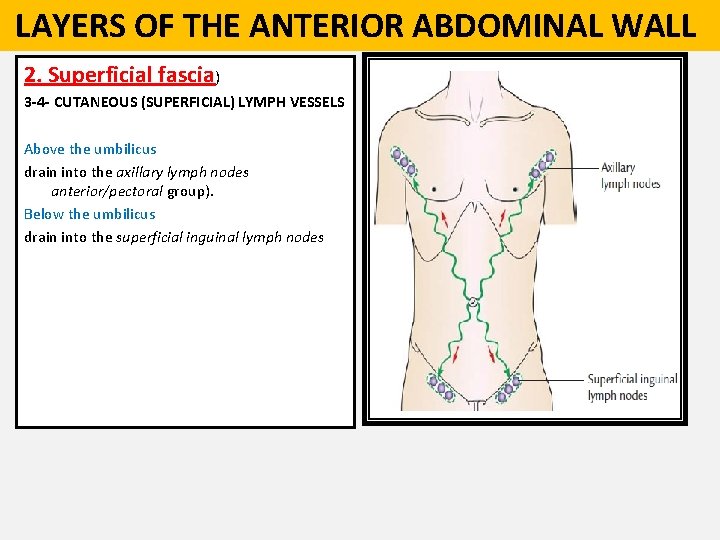
LAYERS OF THE ANTERIOR ABDOMINAL WALL 2. Superficial fascia) 3 -4 - CUTANEOUS (SUPERFICIAL) LYMPH VESSELS Above the umbilicus drain into the axillary lymph nodes anterior/pectoral group). Below the umbilicus drain into the superficial inguinal lymph nodes
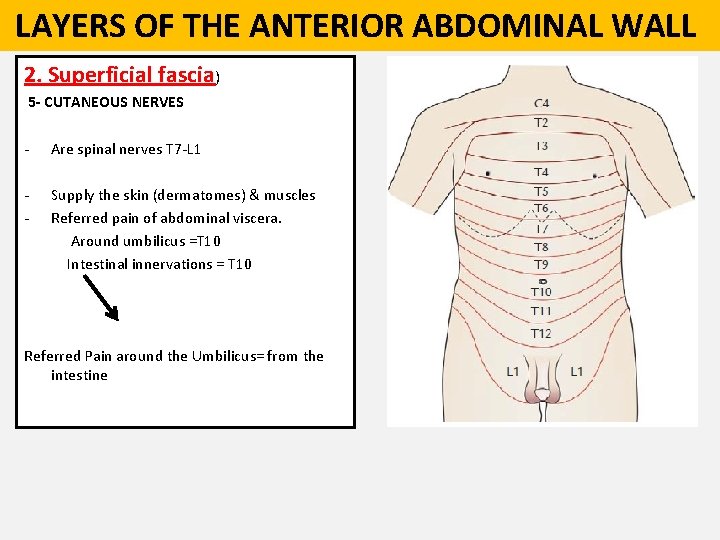
LAYERS OF THE ANTERIOR ABDOMINAL WALL 2. Superficial fascia) 5 - CUTANEOUS NERVES - Are spinal nerves T 7 -L 1 - Supply the skin (dermatomes) & muscles Referred pain of abdominal viscera. Around umbilicus =T 10 Intestinal innervations = T 10 Referred Pain around the Umbilicus= from the intestine
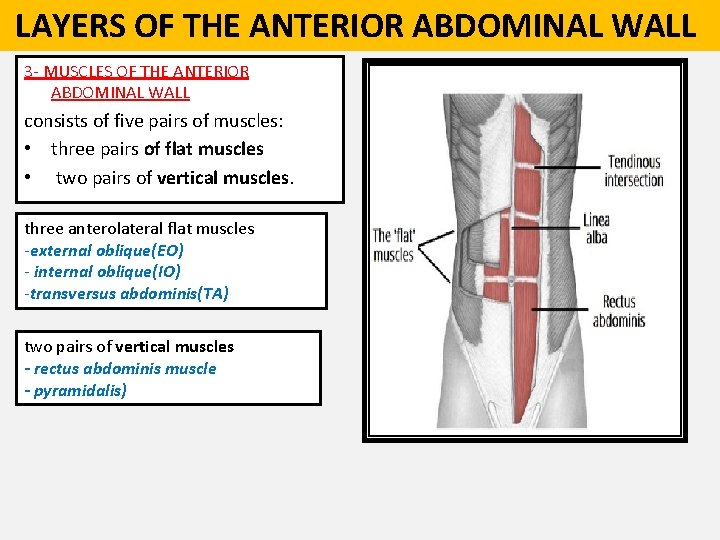
LAYERS OF THE ANTERIOR ABDOMINAL WALL 3 - MUSCLES OF THE ANTERIOR ABDOMINAL WALL consists of five pairs of muscles: • three pairs of flat muscles • two pairs of vertical muscles. three anterolateral flat muscles -external oblique(EO) - internal oblique(IO) -transversus abdominis(TA) two pairs of vertical muscles - rectus abdominis muscle - pyramidalis)
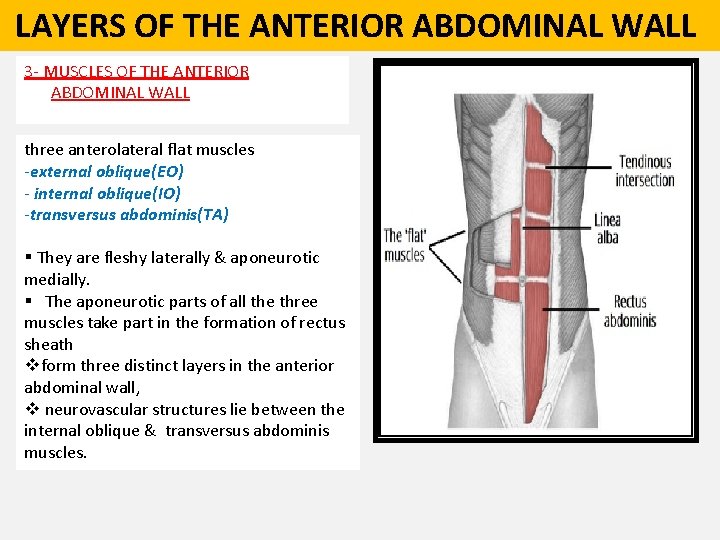
LAYERS OF THE ANTERIOR ABDOMINAL WALL 3 - MUSCLES OF THE ANTERIOR ABDOMINAL WALL three anterolateral flat muscles -external oblique(EO) - internal oblique(IO) -transversus abdominis(TA) § They are fleshy laterally & aponeurotic medially. § The aponeurotic parts of all the three muscles take part in the formation of rectus sheath vform three distinct layers in the anterior abdominal wall, v neurovascular structures lie between the internal oblique & transversus abdominis muscles.
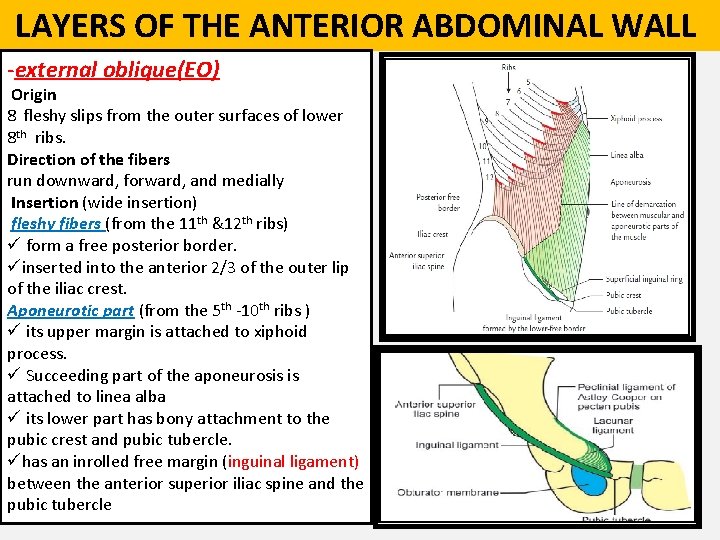
LAYERS OF THE ANTERIOR ABDOMINAL WALL -external oblique(EO) Origin 8 fleshy slips from the outer surfaces of lower 8 th ribs. Direction of the fibers run downward, forward, and medially Insertion (wide insertion) fleshy fibers (from the 11 th &12 th ribs) ü form a free posterior border. üinserted into the anterior 2/3 of the outer lip of the iliac crest. Aponeurotic part (from the 5 th -10 th ribs ) ü its upper margin is attached to xiphoid process. ü Succeeding part of the aponeurosis is attached to linea alba ü its lower part has bony attachment to the pubic crest and pubic tubercle. ühas an inrolled free margin (inguinal ligament) between the anterior superior iliac spine and the pubic tubercle
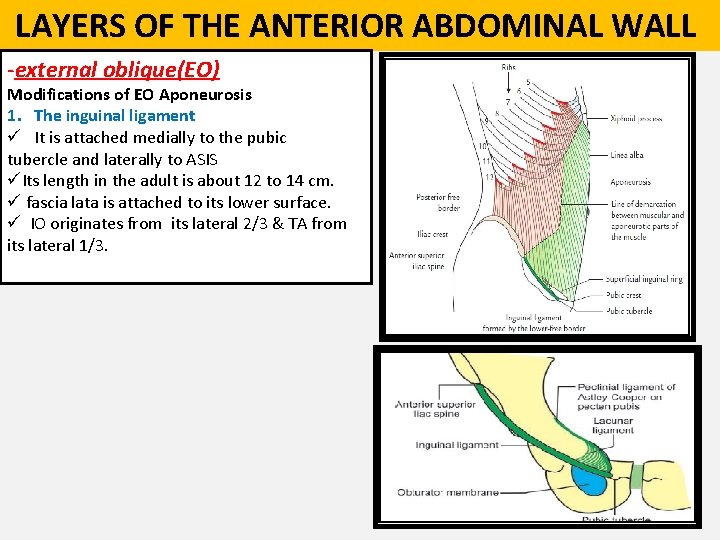
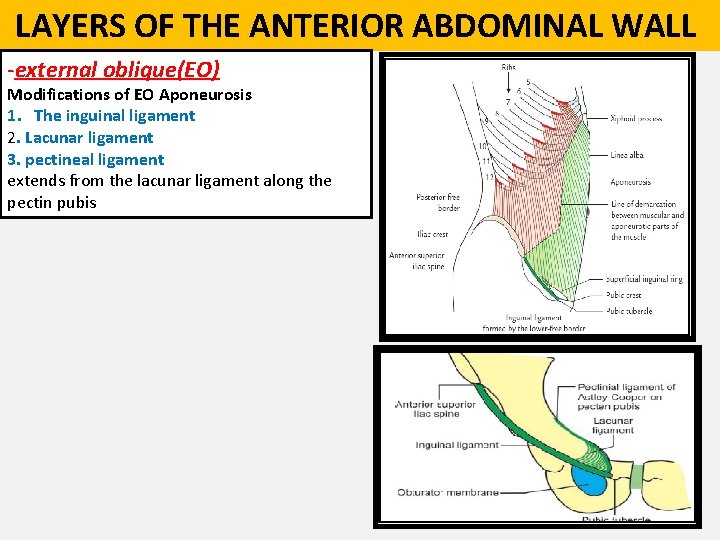
LAYERS OF THE ANTERIOR ABDOMINAL WALL -external oblique(EO) Modifications of EO Aponeurosis 1. The inguinal ligament ü It is attached medially to the pubic tubercle and laterally to ASIS üIts length in the adult is about 12 to 14 cm. ü fascia lata is attached to its lower surface. ü IO originates from its lateral 2/3 & TA from its lateral 1/3.
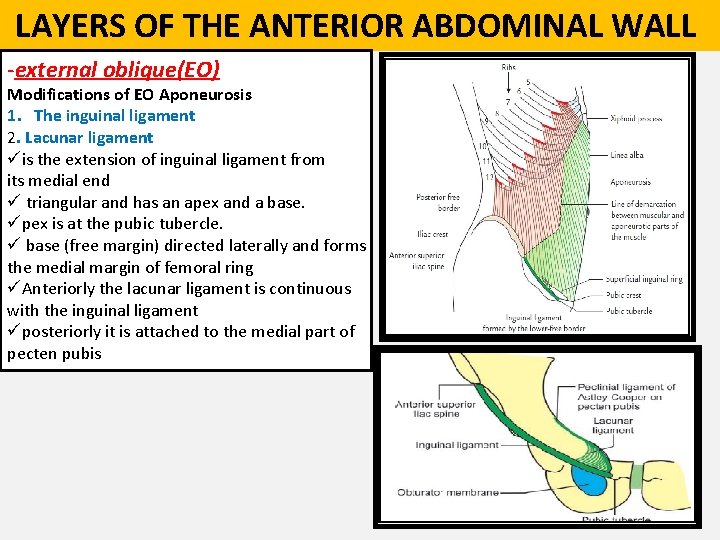
LAYERS OF THE ANTERIOR ABDOMINAL WALL -external oblique(EO) Modifications of EO Aponeurosis 1. The inguinal ligament 2. Lacunar ligament üis the extension of inguinal ligament from its medial end ü triangular and has an apex and a base. üpex is at the pubic tubercle. ü base (free margin) directed laterally and forms the medial margin of femoral ring üAnteriorly the lacunar ligament is continuous with the inguinal ligament üposteriorly it is attached to the medial part of pecten pubis
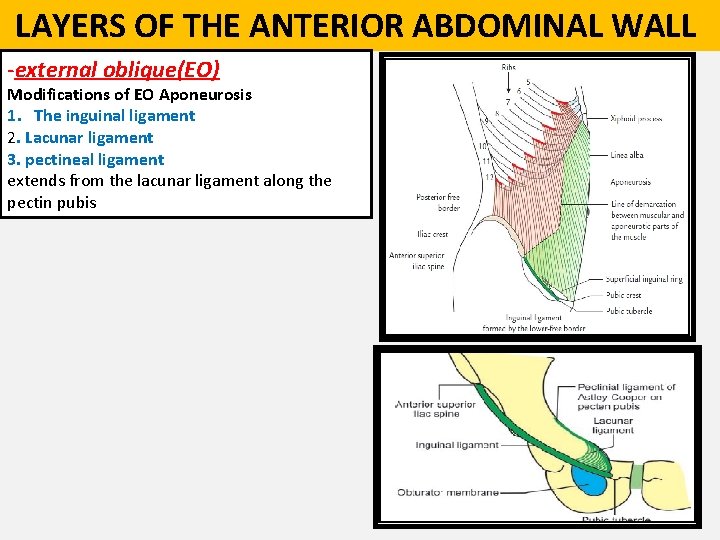
LAYERS OF THE ANTERIOR ABDOMINAL WALL -external oblique(EO) Modifications of EO Aponeurosis 1. The inguinal ligament 2. Lacunar ligament 3. pectineal ligament extends from the lacunar ligament along the pectin pubis
LAYERS OF THE ANTERIOR ABDOMINAL WALL -external oblique(EO) Modifications of EO Aponeurosis 1. The inguinal ligament 2. Lacunar ligament 3. pectineal ligament extends from the lacunar ligament along the pectin pubis
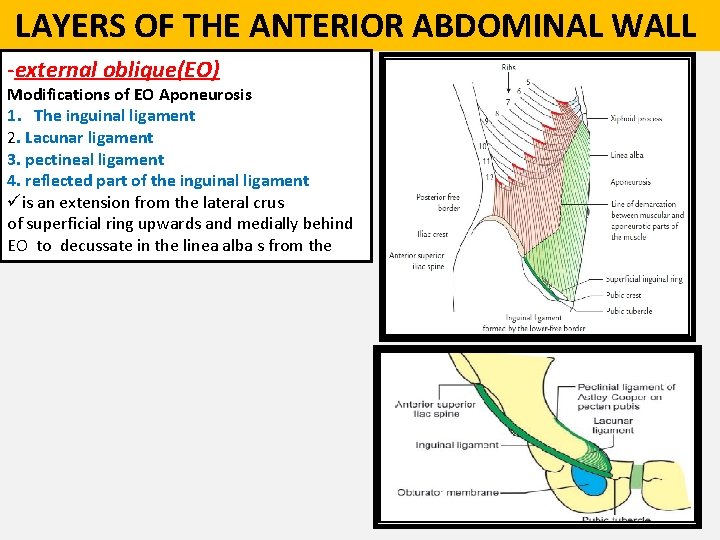
LAYERS OF THE ANTERIOR ABDOMINAL WALL -external oblique(EO) Modifications of EO Aponeurosis 1. The inguinal ligament 2. Lacunar ligament 3. pectineal ligament 4. reflected part of the inguinal ligament üis an extension from the lateral crus of superficial ring upwards and medially behind EO to decussate in the linea alba s from the
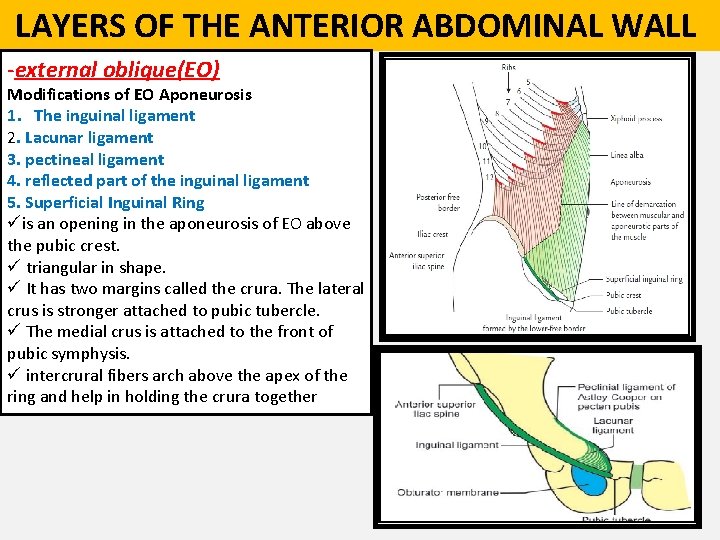
LAYERS OF THE ANTERIOR ABDOMINAL WALL -external oblique(EO) Modifications of EO Aponeurosis 1. The inguinal ligament 2. Lacunar ligament 3. pectineal ligament 4. reflected part of the inguinal ligament 5. Superficial Inguinal Ring üis an opening in the aponeurosis of EO above the pubic crest. ü triangular in shape. ü It has two margins called the crura. The lateral crus is stronger attached to pubic tubercle. ü The medial crus is attached to the front of pubic symphysis. ü intercrural fibers arch above the apex of the ring and help in holding the crura together
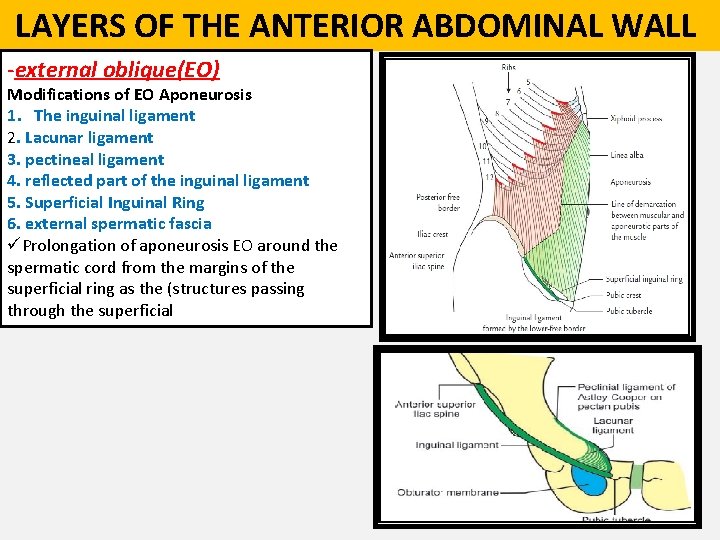
LAYERS OF THE ANTERIOR ABDOMINAL WALL -external oblique(EO) Modifications of EO Aponeurosis 1. The inguinal ligament 2. Lacunar ligament 3. pectineal ligament 4. reflected part of the inguinal ligament 5. Superficial Inguinal Ring 6. external spermatic fascia üProlongation of aponeurosis EO around the spermatic cord from the margins of the superficial ring as the (structures passing through the superficial
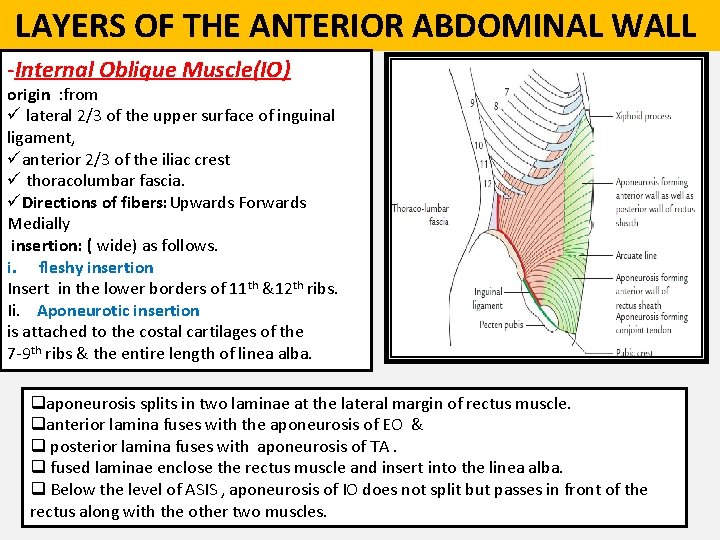
LAYERS OF THE ANTERIOR ABDOMINAL WALL -Internal Oblique Muscle(IO) origin : from ü lateral 2/3 of the upper surface of inguinal ligament, üanterior 2/3 of the iliac crest ü thoracolumbar fascia. üDirections of fibers: Upwards Forwards Medially insertion: ( wide) as follows. i. fleshy insertion Insert in the lower borders of 11 th &12 th ribs. Ii. Aponeurotic insertion is attached to the costal cartilages of the 7 -9 th ribs & the entire length of linea alba. qaponeurosis splits in two laminae at the lateral margin of rectus muscle. qanterior lamina fuses with the aponeurosis of EO & q posterior lamina fuses with aponeurosis of TA. q fused laminae enclose the rectus muscle and insert into the linea alba. q Below the level of ASIS , aponeurosis of IO does not split but passes in front of the rectus along with the other two muscles.
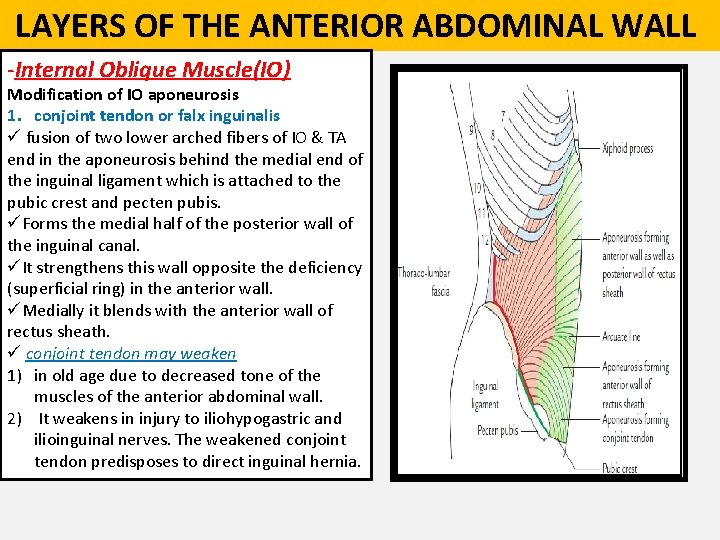
LAYERS OF THE ANTERIOR ABDOMINAL WALL -Internal Oblique Muscle(IO) Modification of IO aponeurosis 1. conjoint tendon or falx inguinalis ü fusion of two lower arched fibers of IO & TA end in the aponeurosis behind the medial end of the inguinal ligament which is attached to the pubic crest and pecten pubis. üForms the medial half of the posterior wall of the inguinal canal. üIt strengthens this wall opposite the deficiency (superficial ring) in the anterior wall. üMedially it blends with the anterior wall of rectus sheath. ü conjoint tendon may weaken 1) in old age due to decreased tone of the muscles of the anterior abdominal wall. 2) It weakens in injury to iliohypogastric and ilioinguinal nerves. The weakened conjoint tendon predisposes to direct inguinal hernia.
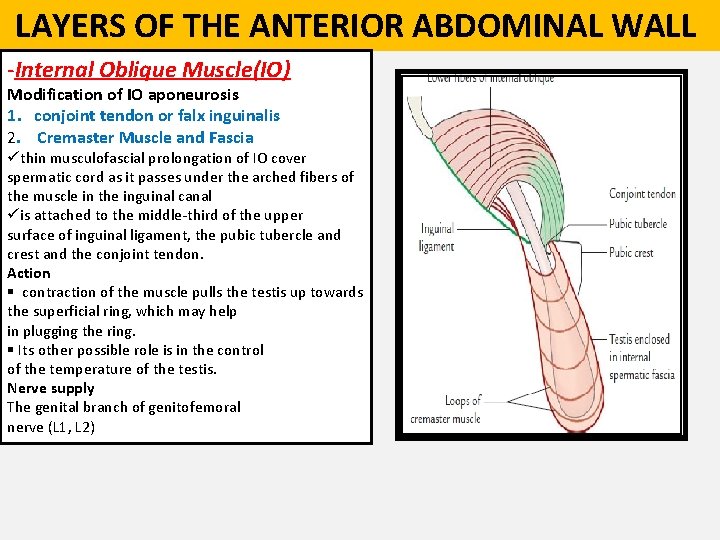
LAYERS OF THE ANTERIOR ABDOMINAL WALL -Internal Oblique Muscle(IO) Modification of IO aponeurosis 1. conjoint tendon or falx inguinalis 2. Cremaster Muscle and Fascia üthin musculofascial prolongation of IO cover spermatic cord as it passes under the arched fibers of the muscle in the inguinal canal üis attached to the middle-third of the upper surface of inguinal ligament, the pubic tubercle and crest and the conjoint tendon. Action § contraction of the muscle pulls the testis up towards the superficial ring, which may help in plugging the ring. § Its other possible role is in the control of the temperature of the testis. Nerve supply The genital branch of genitofemoral nerve (L 1, L 2)
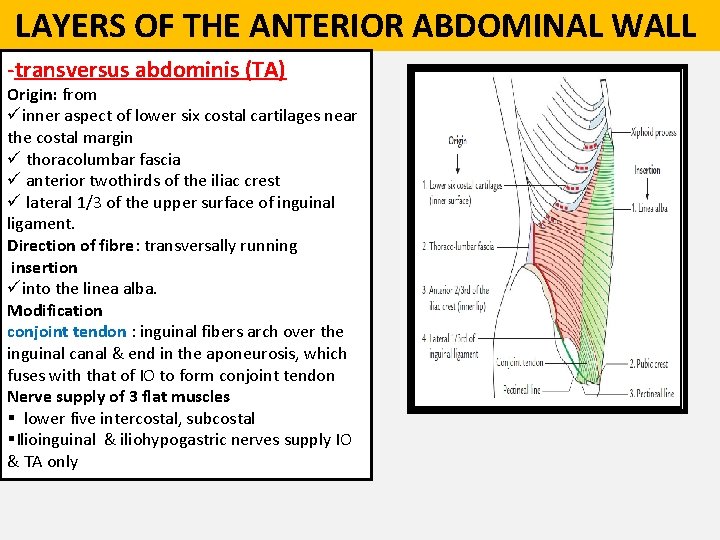
LAYERS OF THE ANTERIOR ABDOMINAL WALL -transversus abdominis (TA) Origin: from üinner aspect of lower six costal cartilages near the costal margin ü thoracolumbar fascia ü anterior twothirds of the iliac crest ü lateral 1/3 of the upper surface of inguinal ligament. Direction of fibre: transversally running insertion üinto the linea alba. Modification conjoint tendon : inguinal fibers arch over the inguinal canal & end in the aponeurosis, which fuses with that of IO to form conjoint tendon Nerve supply of 3 flat muscles § lower five intercostal, subcostal §Ilioinguinal & iliohypogastric nerves supply IO & TA only
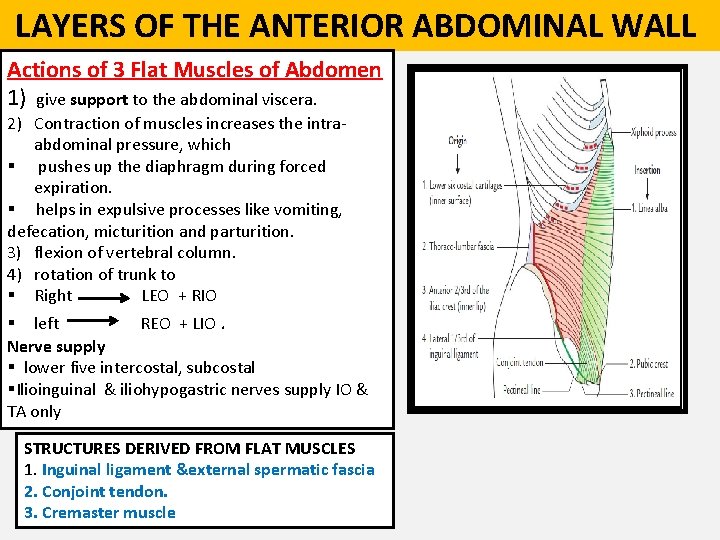
LAYERS OF THE ANTERIOR ABDOMINAL WALL Actions of 3 Flat Muscles of Abdomen 1) give support to the abdominal viscera. 2) Contraction of muscles increases the intraabdominal pressure, which § pushes up the diaphragm during forced expiration. § helps in expulsive processes like vomiting, defecation, micturition and parturition. 3) flexion of vertebral column. 4) rotation of trunk to § Right LEO + RIO § left REO + LIO. Nerve supply § lower five intercostal, subcostal §Ilioinguinal & iliohypogastric nerves supply IO & TA only STRUCTURES DERIVED FROM FLAT MUSCLES 1. Inguinal ligament &external spermatic fascia 2. Conjoint tendon. 3. Cremaster muscle
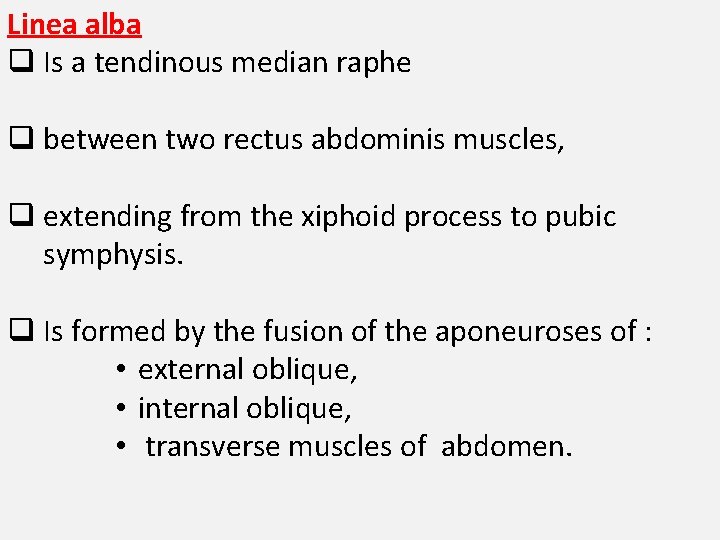
Linea alba q Is a tendinous median raphe q between two rectus abdominis muscles, q extending from the xiphoid process to pubic symphysis. q Is formed by the fusion of the aponeuroses of : • external oblique, • internal oblique, • transverse muscles of abdomen.

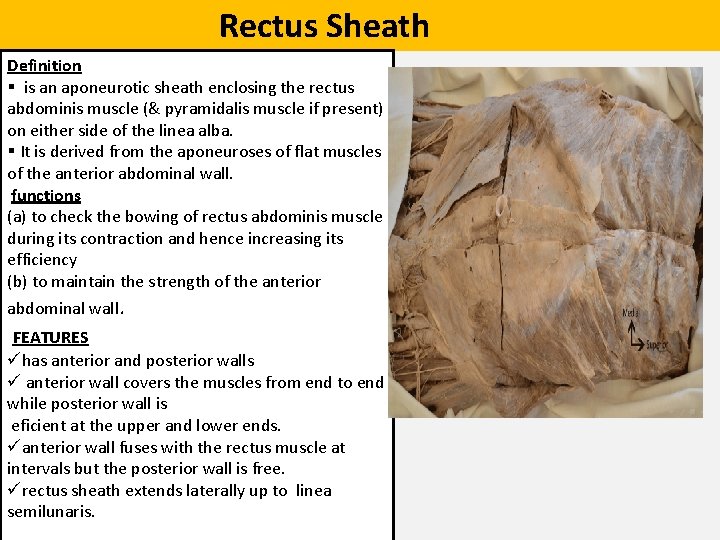
Rectus Sheath Definition § is an aponeurotic sheath enclosing the rectus abdominis muscle (& pyramidalis muscle if present) on either side of the linea alba. § It is derived from the aponeuroses of flat muscles of the anterior abdominal wall. functions (a) to check the bowing of rectus abdominis muscle during its contraction and hence increasing its efficiency (b) to maintain the strength of the anterior abdominal wall. FEATURES ühas anterior and posterior walls ü anterior wall covers the muscles from end to end while posterior wall is eficient at the upper and lower ends. üanterior wall fuses with the rectus muscle at intervals but the posterior wall is free. ürectus sheath extends laterally up to linea semilunaris.
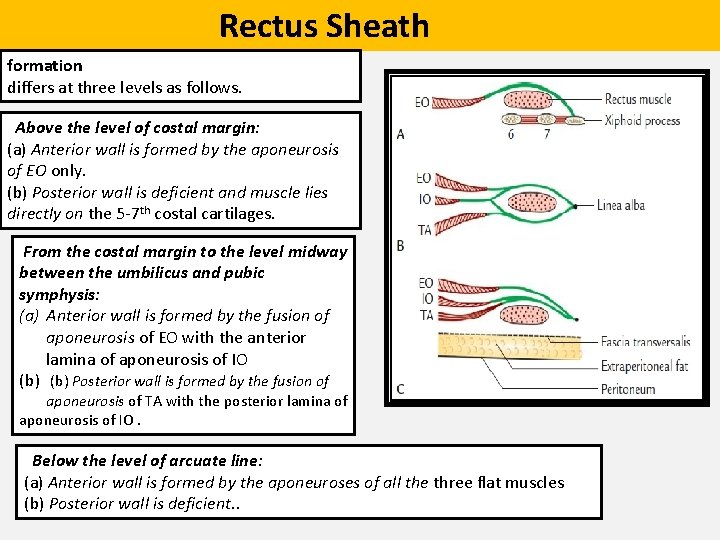
Rectus Sheath formation differs at three levels as follows. Above the level of costal margin: (a) Anterior wall is formed by the aponeurosis of EO only. (b) Posterior wall is deficient and muscle lies directly on the 5 -7 th costal cartilages. From the costal margin to the level midway between the umbilicus and pubic symphysis: (a) Anterior wall is formed by the fusion of aponeurosis of EO with the anterior lamina of aponeurosis of IO (b) Posterior wall is formed by the fusion of aponeurosis of TA with the posterior lamina of aponeurosis of IO. Below the level of arcuate line: (a) Anterior wall is formed by the aponeuroses of all the three flat muscles (b) Posterior wall is deficient. .
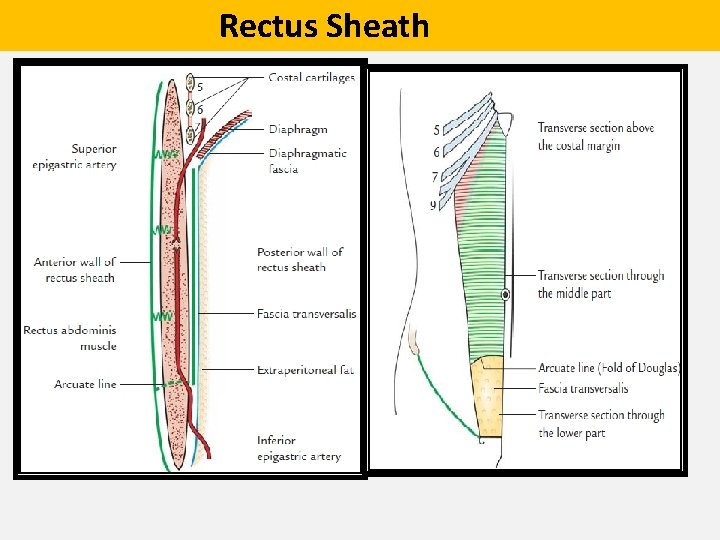
Rectus Sheath
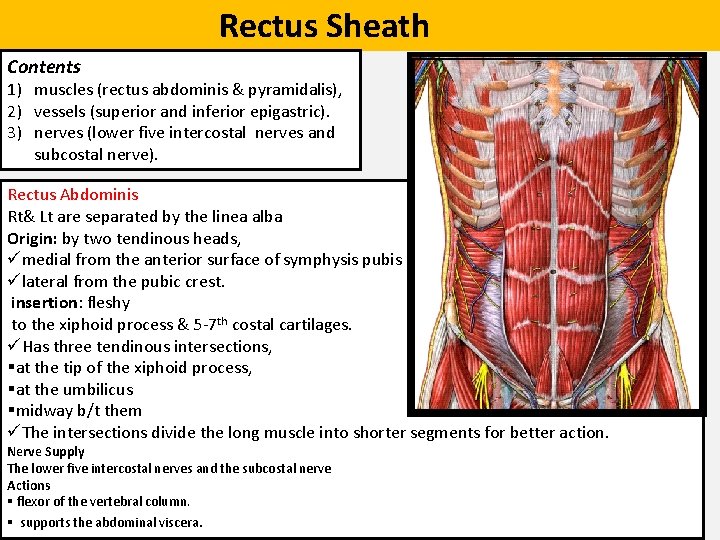
Rectus Sheath Contents 1) muscles (rectus abdominis & pyramidalis), 2) vessels (superior and inferior epigastric). 3) nerves (lower five intercostal nerves and subcostal nerve). Rectus Abdominis Rt& Lt are separated by the linea alba Origin: by two tendinous heads, ümedial from the anterior surface of symphysis pubis ülateral from the pubic crest. insertion: fleshy to the xiphoid process & 5 -7 th costal cartilages. üHas three tendinous intersections, §at the tip of the xiphoid process, §at the umbilicus §midway b/t them üThe intersections divide the long muscle into shorter segments for better action. Nerve Supply The lower five intercostal nerves and the subcostal nerve Actions § flexor of the vertebral column. § supports the abdominal viscera.
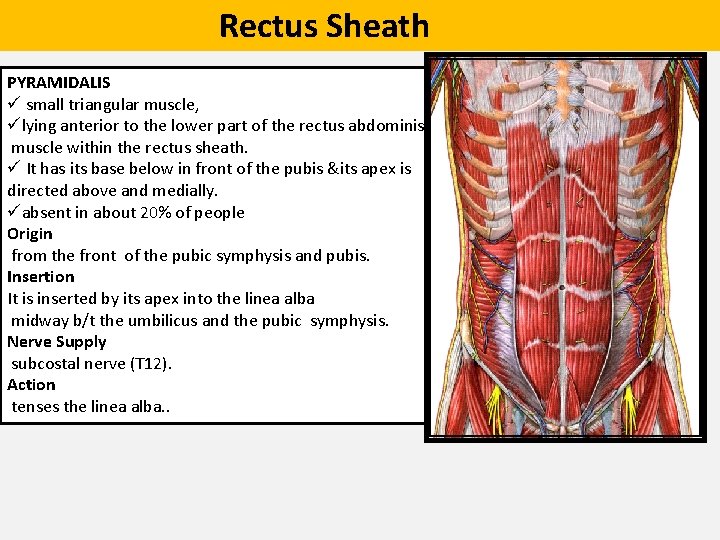
Rectus Sheath PYRAMIDALIS ü small triangular muscle, ülying anterior to the lower part of the rectus abdominis muscle within the rectus sheath. ü It has its base below in front of the pubis &its apex is directed above and medially. üabsent in about 20% of people Origin from the front of the pubic symphysis and pubis. Insertion It is inserted by its apex into the linea alba midway b/t the umbilicus and the pubic symphysis. Nerve Supply subcostal nerve (T 12). Action tenses the linea alba. .
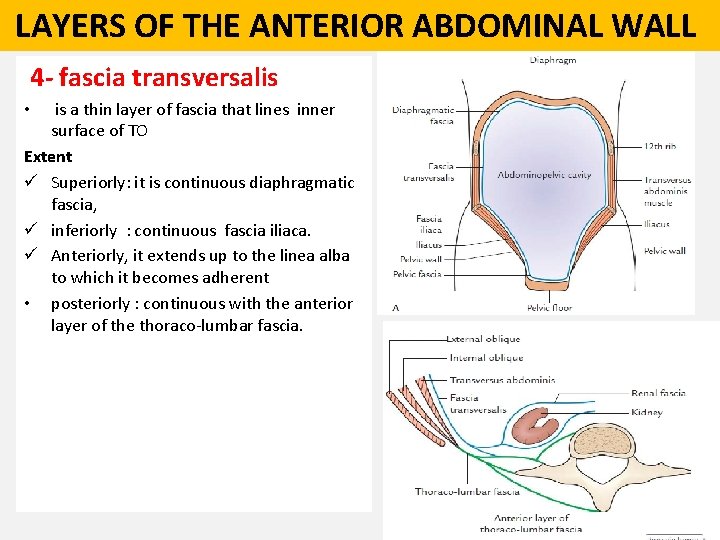
LAYERS OF THE ANTERIOR ABDOMINAL WALL 4 - fascia transversalis is a thin layer of fascia that lines inner surface of TO Extent ü Superiorly: it is continuous diaphragmatic fascia, ü inferiorly : continuous fascia iliaca. ü Anteriorly, it extends up to the linea alba to which it becomes adherent • posteriorly : continuous with the anterior layer of the thoraco-lumbar fascia. •
LAYERS OF THE ANTERIOR ABDOMINAL WALL 4 - fascia transversalis. Special features 1) deep inguinal ring: an oval opening about 1. 2 cm above the midinguinal point provides passage to the spermatic cord in male and round ligament of the uterus in female 2) internal spermatic fascia tubular prolongation around the spermatic cord as it passes through deep inguinal ring. 3. Anterior layer of femoral sheath Its prolongation into the thigh over the femoral vessels 4. iliopubic tract Ø thickened inferior margin of the fascia transversalis in the inguinal region. Ø appears as a fibrous band running parallel and posterior (deep) to the inguinal ligament. Ø demarcates the inferior edge of the deep ring. so it is a useful landmark during laparoscopic inguinal hernial repair.
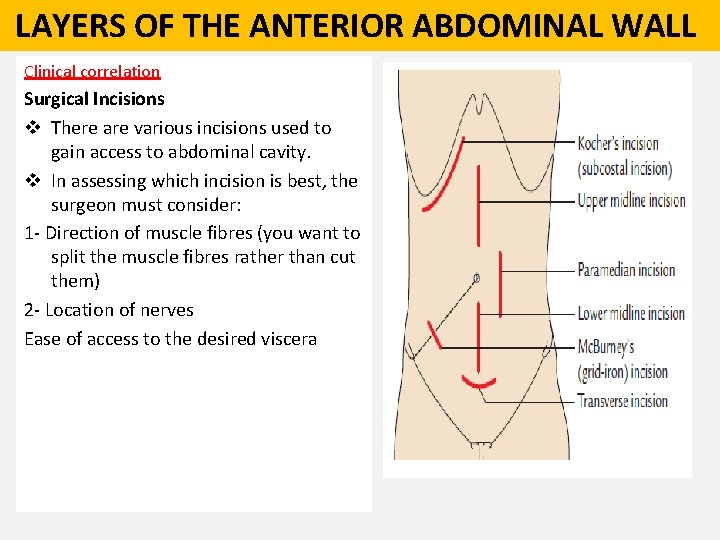
LAYERS OF THE ANTERIOR ABDOMINAL WALL Clinical correlation Surgical Incisions v There are various incisions used to gain access to abdominal cavity. v In assessing which incision is best, the surgeon must consider: 1 - Direction of muscle fibres (you want to split the muscle fibres rather than cut them) 2 - Location of nerves Ease of access to the desired viscera
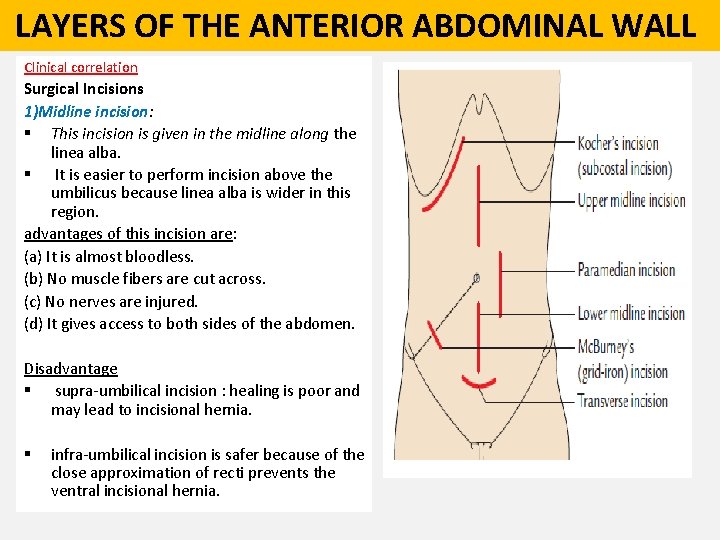
LAYERS OF THE ANTERIOR ABDOMINAL WALL Clinical correlation Surgical Incisions 1)Midline incision: § This incision is given in the midline along the linea alba. § It is easier to perform incision above the umbilicus because linea alba is wider in this region. advantages of this incision are: (a) It is almost bloodless. (b) No muscle fibers are cut across. (c) No nerves are injured. (d) It gives access to both sides of the abdomen. Disadvantage § supra-umbilical incision : healing is poor and may lead to incisional hernia. § infra-umbilical incision is safer because of the close approximation of recti prevents the ventral incisional hernia.
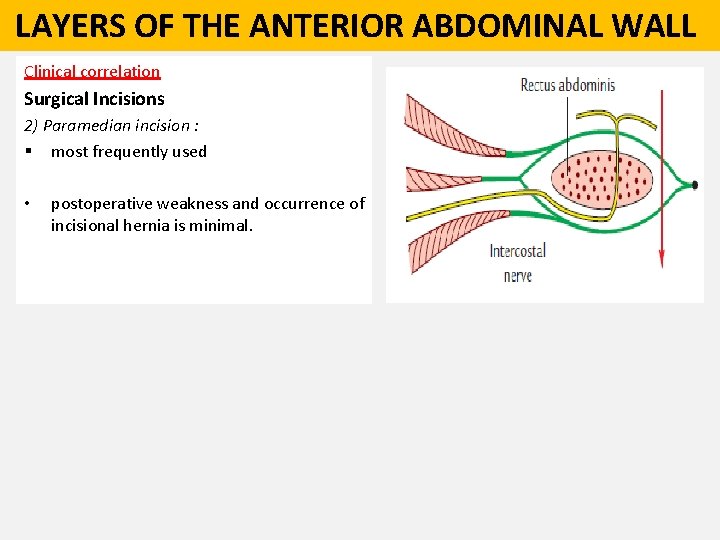
LAYERS OF THE ANTERIOR ABDOMINAL WALL Clinical correlation Surgical Incisions 2) Paramedian incision : § most frequently used • postoperative weakness and occurrence of incisional hernia is minimal.
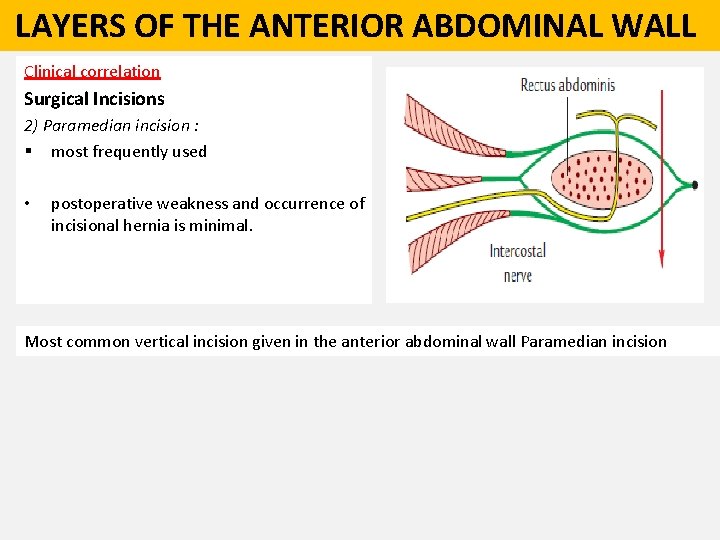
LAYERS OF THE ANTERIOR ABDOMINAL WALL Clinical correlation Surgical Incisions 2) Paramedian incision : § most frequently used • postoperative weakness and occurrence of incisional hernia is minimal. Most common vertical incision given in the anterior abdominal wall Paramedian incision

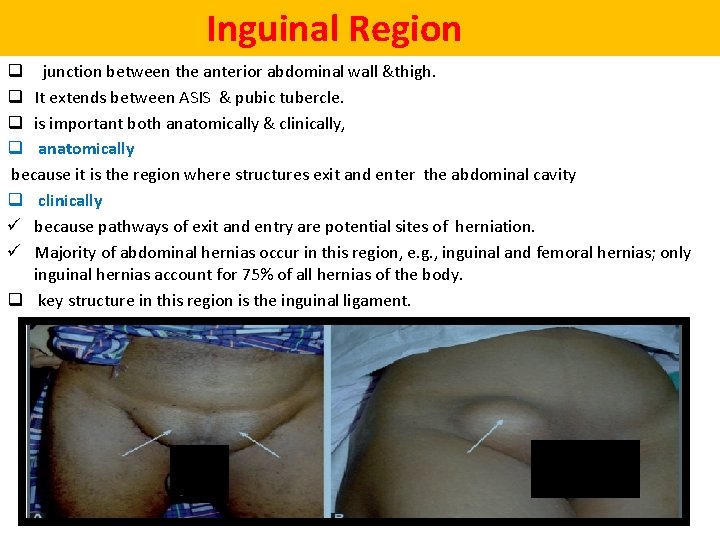
Inguinal Region q junction between the anterior abdominal wall &thigh. q It extends between ASIS & pubic tubercle. q is important both anatomically & clinically, q anatomically because it is the region where structures exit and enter the abdominal cavity q clinically ü because pathways of exit and entry are potential sites of herniation. ü Majority of abdominal hernias occur in this region, e. g. , inguinal and femoral hernias; only inguinal hernias account for 75% of all hernias of the body. q key structure in this region is the inguinal ligament.
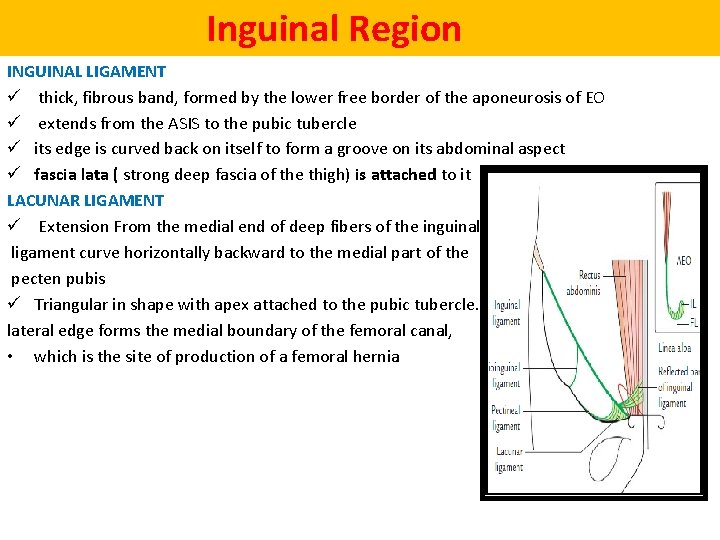
Inguinal Region INGUINAL LIGAMENT ü thick, fibrous band, formed by the lower free border of the aponeurosis of EO ü extends from the ASIS to the pubic tubercle ü its edge is curved back on itself to form a groove on its abdominal aspect ü fascia lata ( strong deep fascia of the thigh) is attached to it LACUNAR LIGAMENT ü Extension From the medial end of deep fibers of the inguinal ligament curve horizontally backward to the medial part of the pecten pubis ü Triangular in shape with apex attached to the pubic tubercle. Its sharp lateral edge forms the medial boundary of the femoral canal, • which is the site of production of a femoral hernia
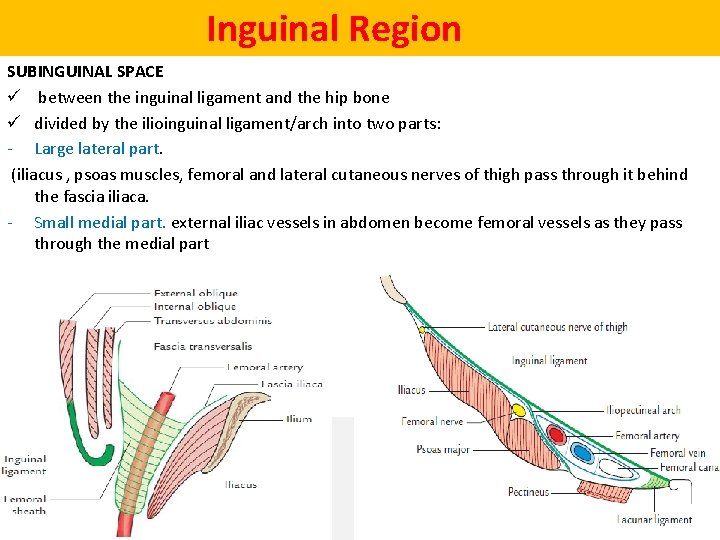
Inguinal Region SUBINGUINAL SPACE ü between the inguinal ligament and the hip bone ü divided by the ilioinguinal ligament/arch into two parts: - Large lateral part. (iliacus , psoas muscles, femoral and lateral cutaneous nerves of thigh pass through it behind the fascia iliaca. - Small medial part. external iliac vessels in abdomen become femoral vessels as they pass through the medial part
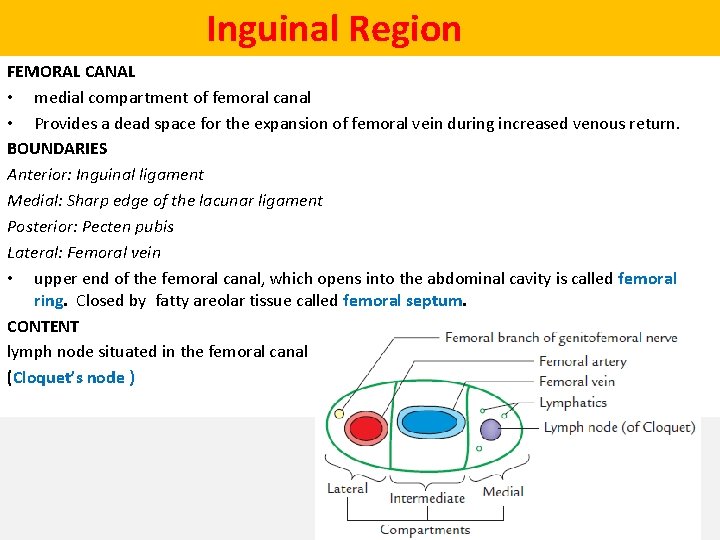
Inguinal Region FEMORAL CANAL • medial compartment of femoral canal • Provides a dead space for the expansion of femoral vein during increased venous return. BOUNDARIES Anterior: Inguinal ligament Medial: Sharp edge of the lacunar ligament Posterior: Pecten pubis Lateral: Femoral vein • upper end of the femoral canal, which opens into the abdominal cavity is called femoral ring. Closed by fatty areolar tissue called femoral septum. CONTENT lymph node situated in the femoral canal (Cloquet’s node )
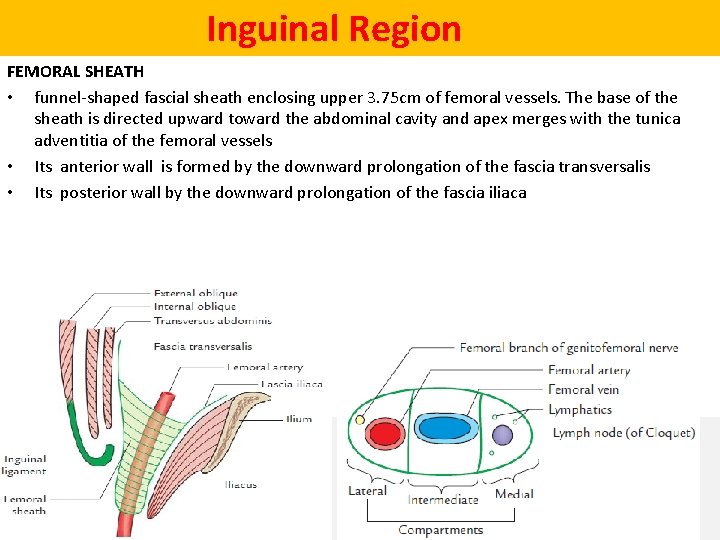
Inguinal Region FEMORAL SHEATH • funnel-shaped fascial sheath enclosing upper 3. 75 cm of femoral vessels. The base of the sheath is directed upward toward the abdominal cavity and apex merges with the tunica adventitia of the femoral vessels • Its anterior wall is formed by the downward prolongation of the fascia transversalis • Its posterior wall by the downward prolongation of the fascia iliaca
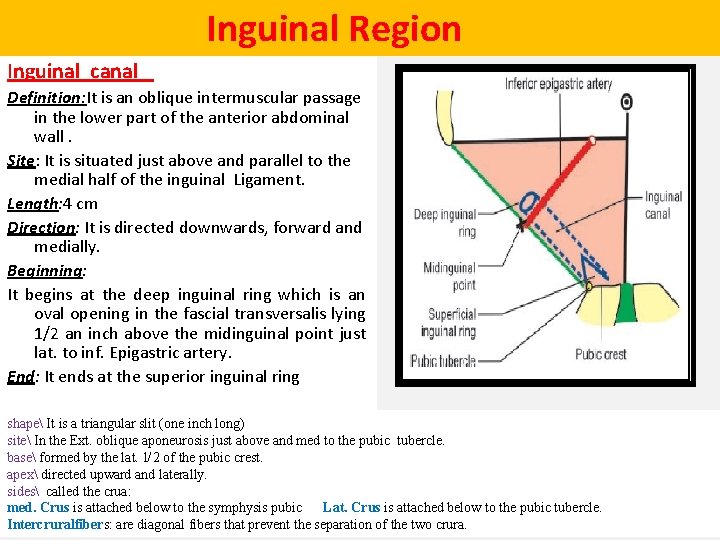
Inguinal Region Inguinal canal Definition: It is an oblique intermuscular passage in the lower part of the anterior abdominal wall. Site: It is situated just above and parallel to the medial half of the inguinal Ligament. Length: 4 cm Direction: It is directed downwards, forward and medially. Beginning: It begins at the deep inguinal ring which is an oval opening in the fascial transversalis lying 1/2 an inch above the midinguinal point just lat. to inf. Epigastric artery. End: It ends at the superior inguinal ring shape It is a triangular slit (one inch long) site In the Ext. oblique aponeurosis just above and med to the pubic tubercle. base formed by the lat. 1 2 of the pubic crest. apex directed upward and laterally. sides called the crua: med. Crus is attached below to the symphysis pubic Lat. Crus is attached below to the pubic tubercle. Intercruralfibers: are diagonal fibers that prevent the separation of the two crura.
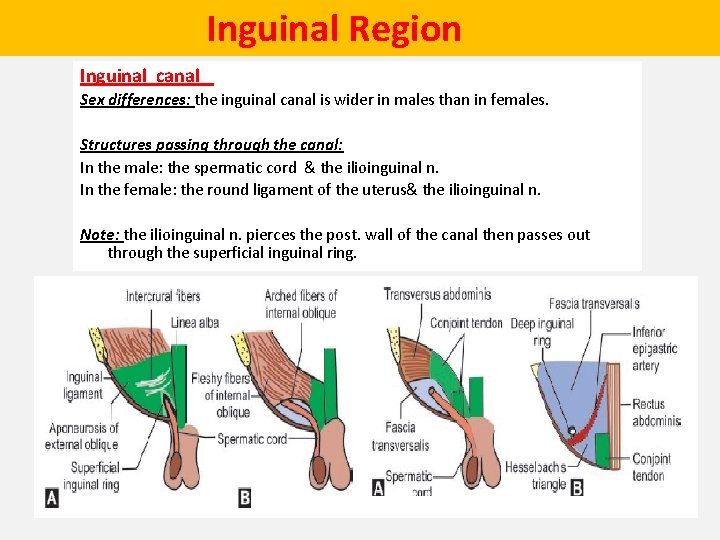
Inguinal Region Inguinal canal Sex differences: the inguinal canal is wider in males than in females. Structures passing through the canal: In the male: the spermatic cord & the ilioinguinal n. In the female: the round ligament of the uterus& the ilioinguinal n. Note: the ilioinguinal n. pierces the post. wall of the canal then passes out through the superficial inguinal ring.
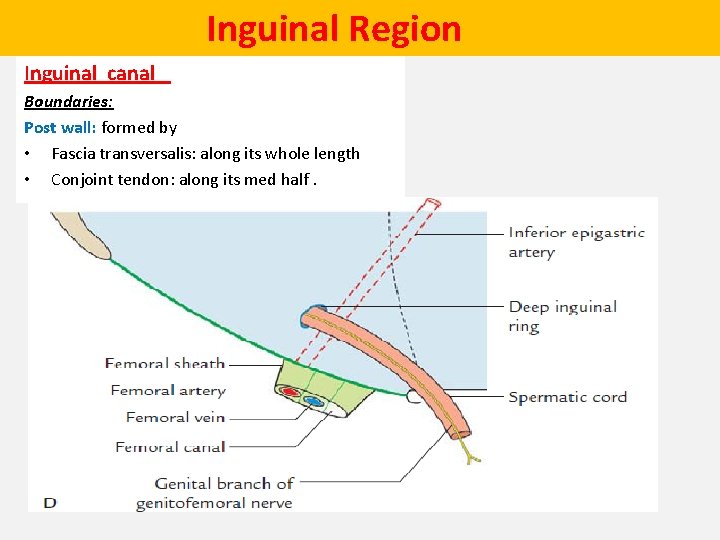
Inguinal Region Inguinal canal Boundaries: Post wall: formed by • Fascia transversalis: along its whole length • Conjoint tendon: along its med half.
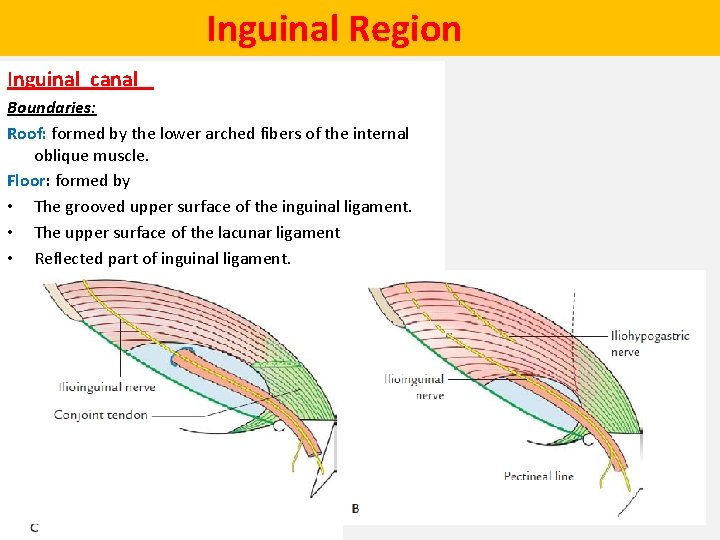
Inguinal Region Inguinal canal Boundaries: Roof: formed by the lower arched fibers of the internal oblique muscle. Floor: formed by • The grooved upper surface of the inguinal ligament. • The upper surface of the lacunar ligament • Reflected part of inguinal ligament.
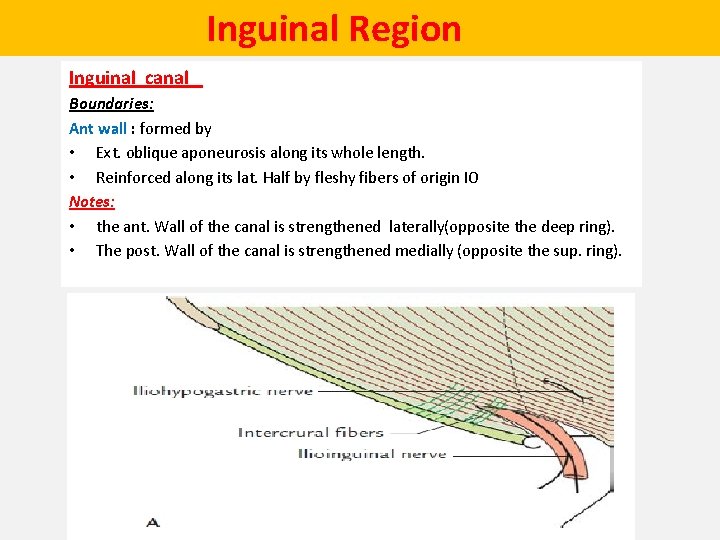
Inguinal Region Inguinal canal Boundaries: Ant wall : formed by • Ext. oblique aponeurosis along its whole length. • Reinforced along its lat. Half by fleshy fibers of origin IO Notes: • the ant. Wall of the canal is strengthened laterally(opposite the deep ring). • The post. Wall of the canal is strengthened medially (opposite the sup. ring).
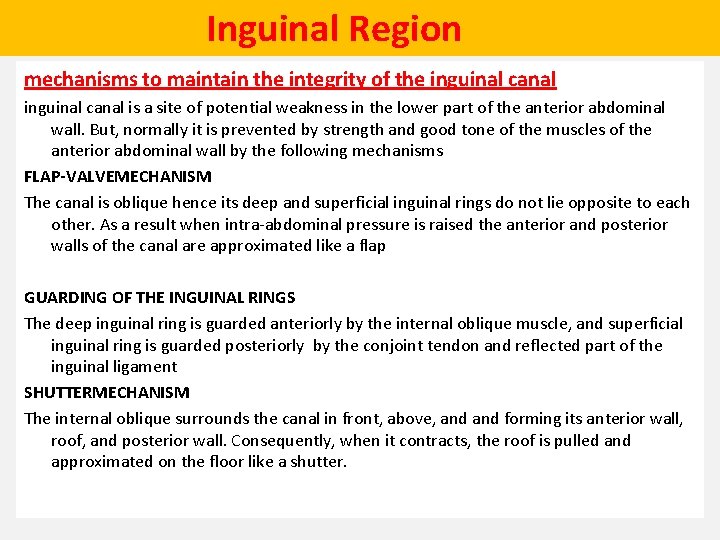
Inguinal Region mechanisms to maintain the integrity of the inguinal canal is a site of potential weakness in the lower part of the anterior abdominal wall. But, normally it is prevented by strength and good tone of the muscles of the anterior abdominal wall by the following mechanisms FLAP-VALVEMECHANISM The canal is oblique hence its deep and superficial inguinal rings do not lie opposite to each other. As a result when intra-abdominal pressure is raised the anterior and posterior walls of the canal are approximated like a flap GUARDING OF THE INGUINAL RINGS The deep inguinal ring is guarded anteriorly by the internal oblique muscle, and superficial inguinal ring is guarded posteriorly by the conjoint tendon and reflected part of the inguinal ligament SHUTTERMECHANISM The internal oblique surrounds the canal in front, above, and forming its anterior wall, roof, and posterior wall. Consequently, when it contracts, the roof is pulled and approximated on the floor like a shutter.
Inguinal Region mechanisms to maintain the integrity of the inguinal canal SLIT-VALVEMECHANISM The contraction of external oblique muscle approximates the two crura like a slit valve. The intercrural fibers also help in this act. BALL-VALVEMECHANISM Contraction of cremaster muscle pulls the testis up and the superficial inguinal ring is plugged by the spermatic cord.
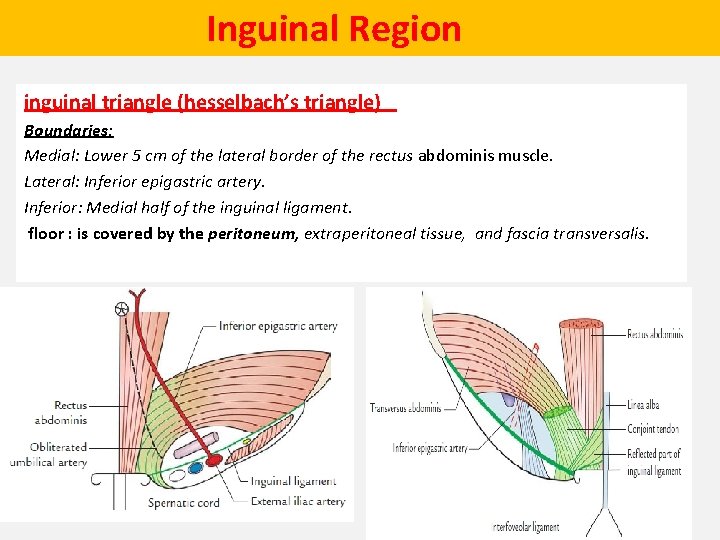
Inguinal Region inguinal triangle (hesselbach’s triangle) Boundaries: Medial: Lower 5 cm of the lateral border of the rectus abdominis muscle. Lateral: Inferior epigastric artery. Inferior: Medial half of the inguinal ligament. floor : is covered by the peritoneum, extraperitoneal tissue, and fascia transversalis.
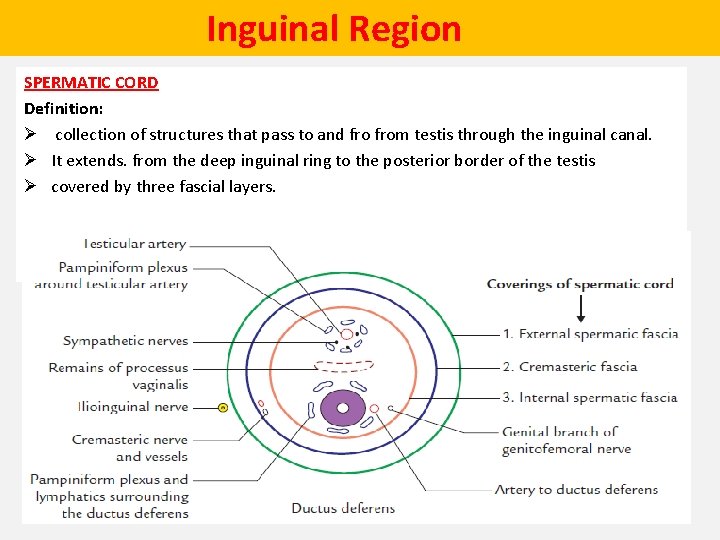
Inguinal Region SPERMATIC CORD Definition: Ø collection of structures that pass to and from testis through the inguinal canal. Ø It extends. from the deep inguinal ring to the posterior border of the testis Ø covered by three fascial layers.
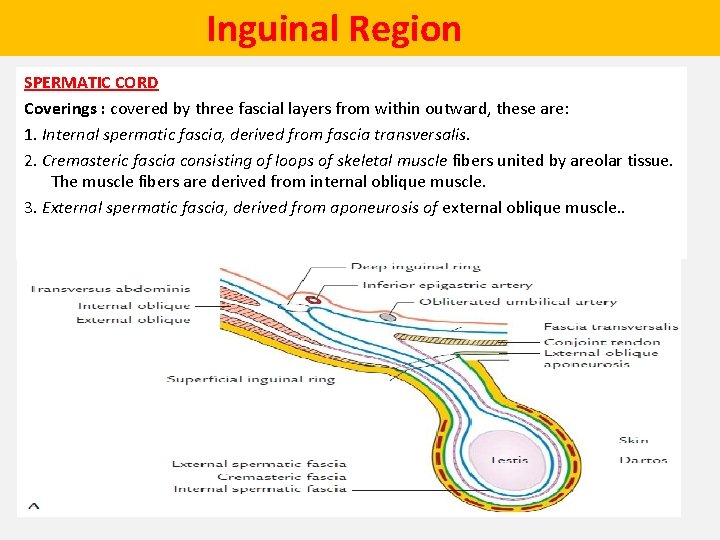
Inguinal Region SPERMATIC CORD Coverings : covered by three fascial layers from within outward, these are: 1. Internal spermatic fascia, derived from fascia transversalis. 2. Cremasteric fascia consisting of loops of skeletal muscle fibers united by areolar tissue. The muscle fibers are derived from internal oblique muscle. 3. External spermatic fascia, derived from aponeurosis of external oblique muscle. .
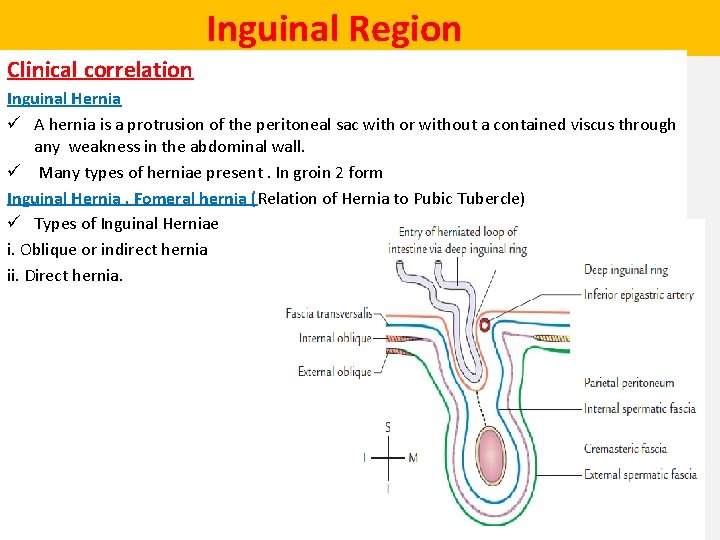
Inguinal Region Clinical correlation Inguinal Hernia ü A hernia is a protrusion of the peritoneal sac with or without a contained viscus through any weakness in the abdominal wall. ü Many types of herniae present. In groin 2 form Inguinal Hernia , Fomeral hernia (Relation of Hernia to Pubic Tubercle) ü Types of Inguinal Herniae i. Oblique or indirect hernia ii. Direct hernia.
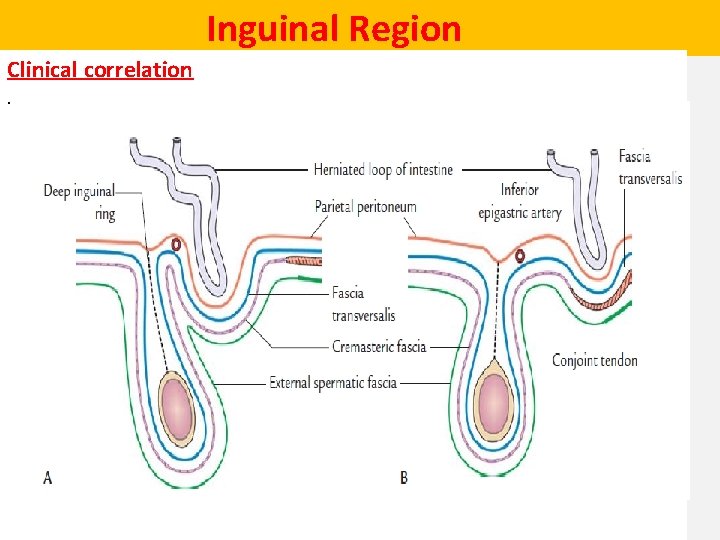
Inguinal Region Clinical correlation.

Inguinal Region Differentiation b/t direct &indirect herniae • • • Indirect or Oblique Inguinal Hernia It is more common in children and younger age boy congenital ( complete or partial patency of the processus vaginalis) hernia enters the inguinal canal via the deep inguinal ring and then passes through the entire inguinal canal to come out through the superficial inguinal ring. • It is inside the coverings of spermatic cord hence enters the scrotum. • neck of hernial sac is lateral to the inferior epigastric artery. • • Direct Inguinal Hernia imore common in old age. Acquired due weakness of abdominal muscles. There are various factors are responsible for weakening the anterior abdominal wall muscles, ü rise in intra-abdominal pressure, chronic constipation, chronic cough, lifting heavy weights, etc. ). • hernia enters the inguinal canal through the Hesselbach’s triangle. • The hernia comes out via the superficial inguinal ring. It lies outside the spermatic cord. • • The neck of hernial sac is medial to the inferior epigastric artery.
- Slides: 57