Epididymis ductus deferens spermatic cord seminal vesicles prostate
- Slides: 19
Epididymis, ductus deferens, spermatic cord, seminal vesicles, prostate Ágnes Nemeskéri 2020 Semmelweis University Department of Anatomy, Histology and Embryology Clinical Anatomy Research Laboratory nemeskeri. agnes@med. semmelweis-univ. hu
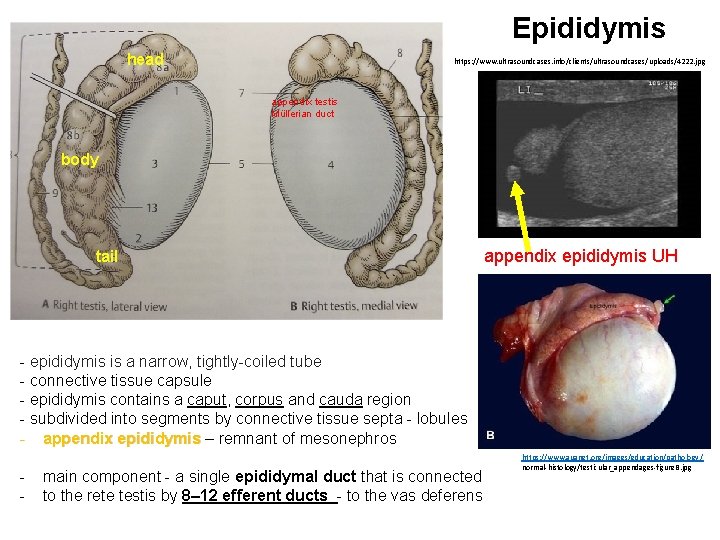
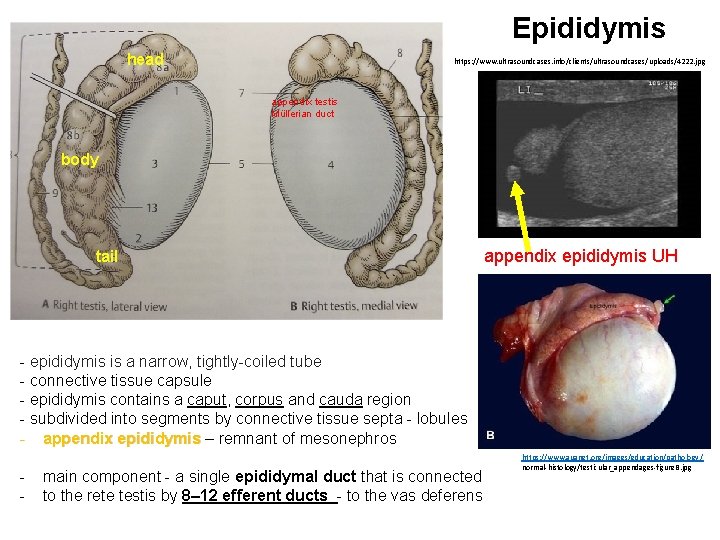
Epididymis head https: //www. ultrasoundcases. info/clients/ultrasoundcases/uploads/4222. jpg appendix testis Müllerian duct body tail appendix epididymis UH - epididymis is a narrow, tightly-coiled tube - connective tissue capsule - epididymis contains a caput, corpus and cauda region - subdivided into segments by connective tissue septa - lobules - appendix epididymis – remnant of mesonephros - main component - a single epididymal duct that is connected to the rete testis by 8– 12 efferent ducts - to the vas deferens https: //www. auanet. org/images/education/pathology / normal-histology/testicular_appendages-figure. B. jpg
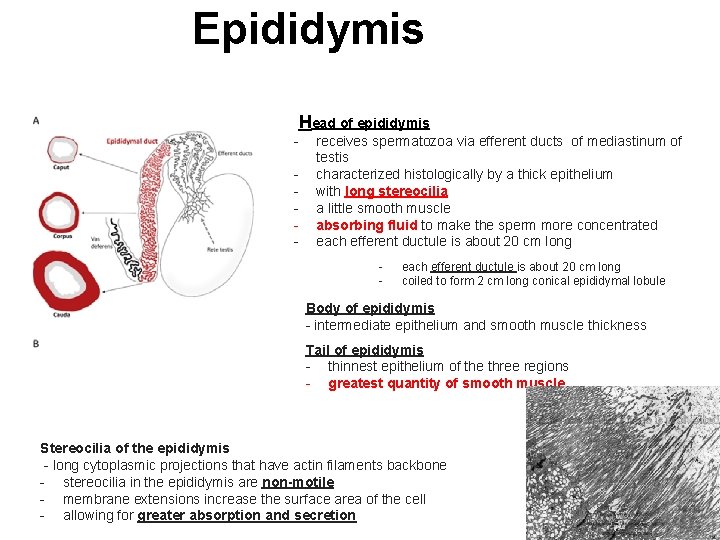
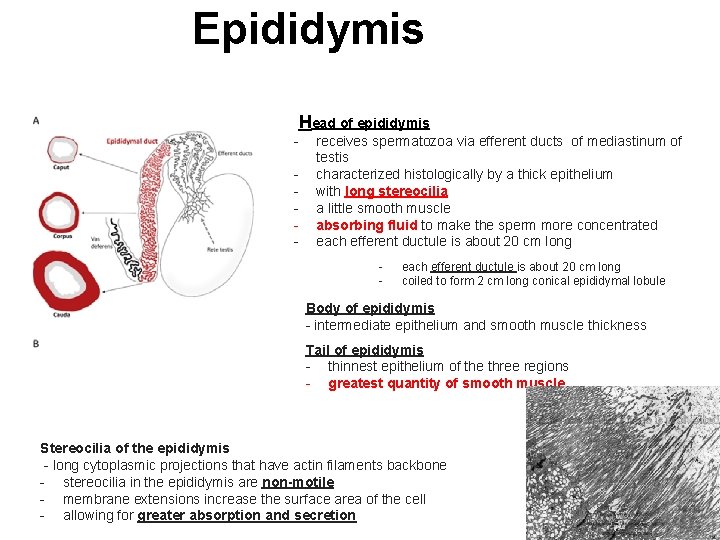
Epididymis Head of epididymis - receives spermatozoa via efferent ducts of mediastinum of testis characterized histologically by a thick epithelium with long stereocilia a little smooth muscle absorbing fluid to make the sperm more concentrated each efferent ductule is about 20 cm long - each efferent ductule is about 20 cm long coiled to form 2 cm long conical epididymal lobule Body of epididymis - intermediate epithelium and smooth muscle thickness Tail of epididymis - thinnest epithelium of the three regions - greatest quantity of smooth muscle Stereocilia of the epididymis - long cytoplasmic projections that have actin filaments backbone - stereocilia in the epididymis are non-motile - membrane extensions increase the surface area of the cell - allowing for greater absorption and secretion
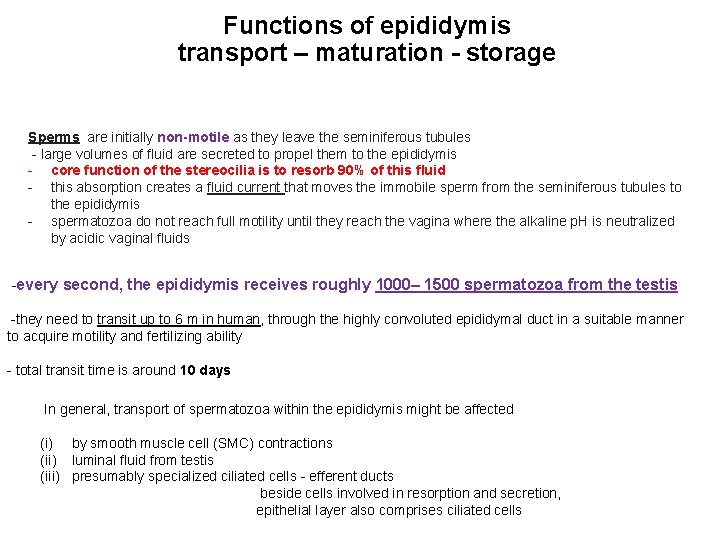
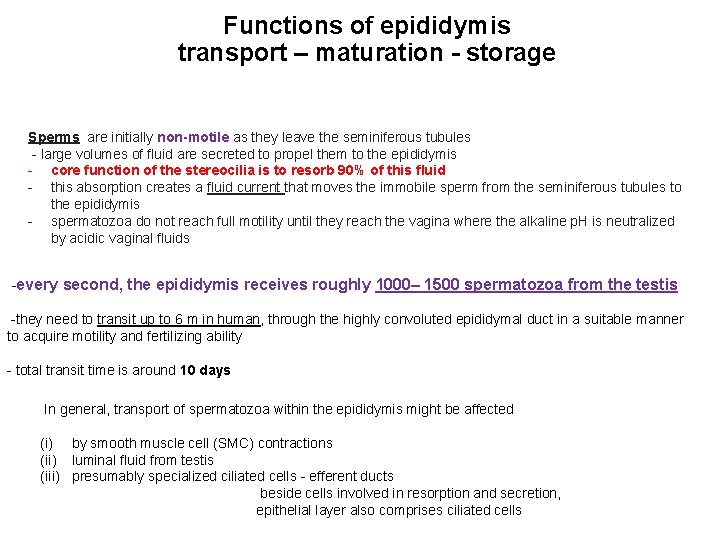
Functions of epididymis transport – maturation - storage Sperms are initially non-motile as they leave the seminiferous tubules - large volumes of fluid are secreted to propel them to the epididymis - core function of the stereocilia is to resorb 90% of this fluid - this absorption creates a fluid current that moves the immobile sperm from the seminiferous tubules to the epididymis - spermatozoa do not reach full motility until they reach the vagina where the alkaline p. H is neutralized by acidic vaginal fluids -every second, the epididymis receives roughly 1000– 1500 spermatozoa from the testis -they need to transit up to 6 m in human, through the highly convoluted epididymal duct in a suitable manner to acquire motility and fertilizing ability - total transit time is around 10 days In general, transport of spermatozoa within the epididymis might be affected (i) by smooth muscle cell (SMC) contractions (ii) luminal fluid from testis (iii) presumably specialized ciliated cells - efferent ducts beside cells involved in resorption and secretion, epithelial layer also comprises ciliated cells
Function of epididymis During their transit through the epididymis, spermatozoa mature and acquire motility and fertilizing capacity. The smooth muscle cells (SMCs) of the epididymal duct are thought to be responsible for the adequate transport of spermatozoa. Precise regulation of SMC function also represents a prerequisite for sperm maturation thereby contributing to male fertility.
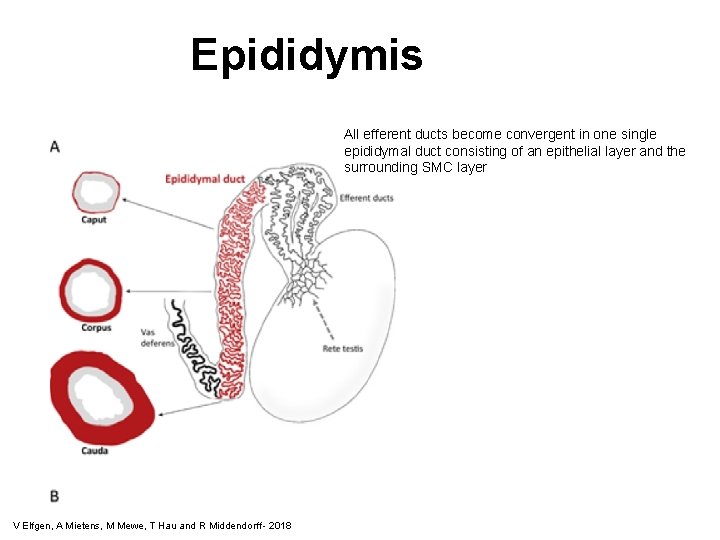
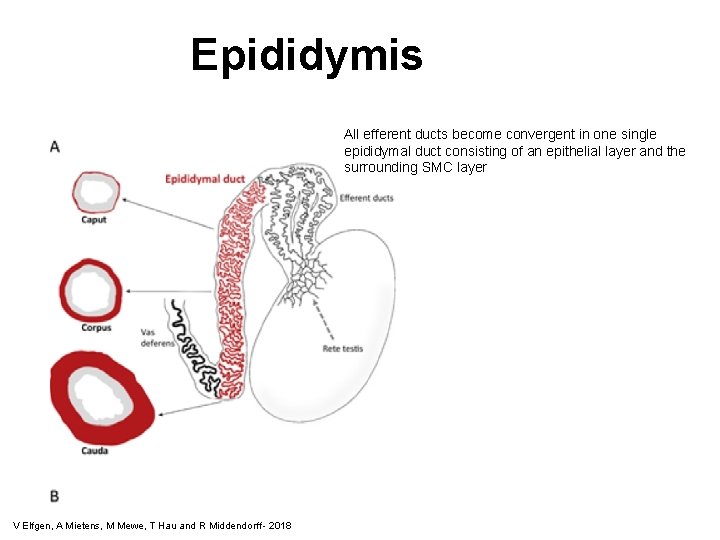
Epididymis All efferent ducts become convergent in one single epididymal duct consisting of an epithelial layer and the surrounding SMC layer V Elfgen, A Mietens, M Mewe, T Hau and R Middendorff - 2018
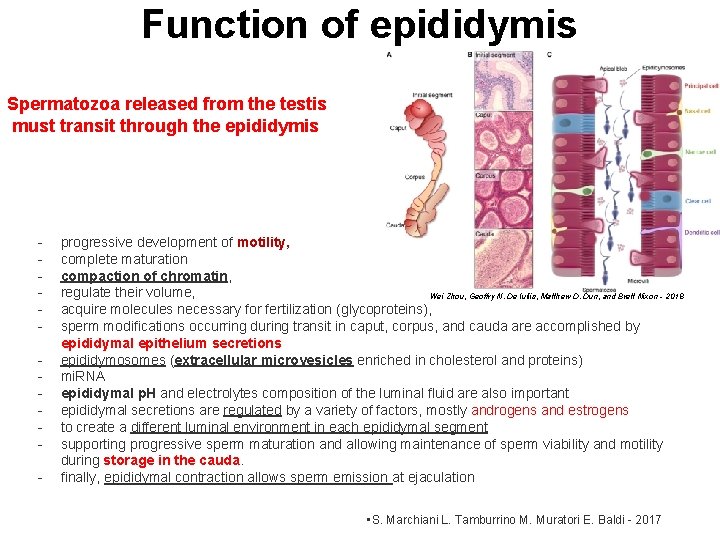
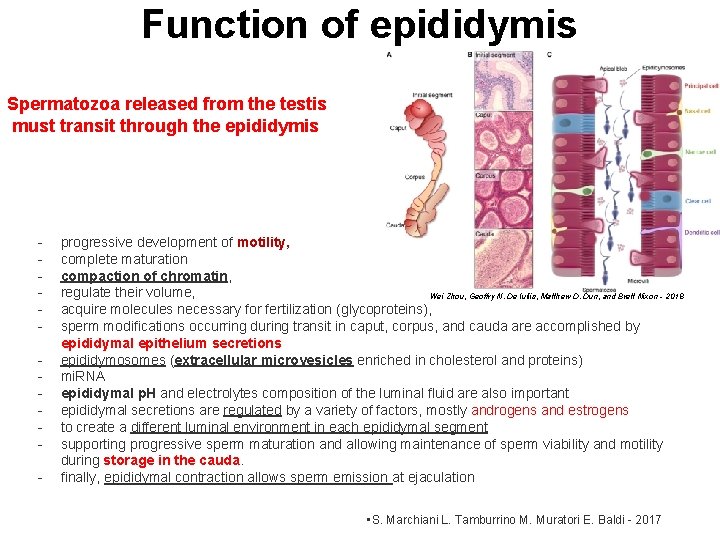
Function of epididymis Spermatozoa released from the testis must transit through the epididymis - progressive development of motility, complete maturation compaction of chromatin, regulate their volume, Wei Zhou, Geoffry N. De Iuliis, Matthew D. Dun, and Brett Nixon - 2018 acquire molecules necessary for fertilization (glycoproteins), sperm modifications occurring during transit in caput, corpus, and cauda are accomplished by epididymal epithelium secretions epididymosomes (extracellular microvesicles enriched in cholesterol and proteins) mi. RNA epididymal p. H and electrolytes composition of the luminal fluid are also important epididymal secretions are regulated by a variety of factors, mostly androgens and estrogens to create a different luminal environment in each epididymal segment supporting progressive sperm maturation and allowing maintenance of sperm viability and motility during storage in the cauda. finally, epididymal contraction allows sperm emission at ejaculation • S. Marchiani L. Tamburrino M. Muratori E. Baldi - 2017
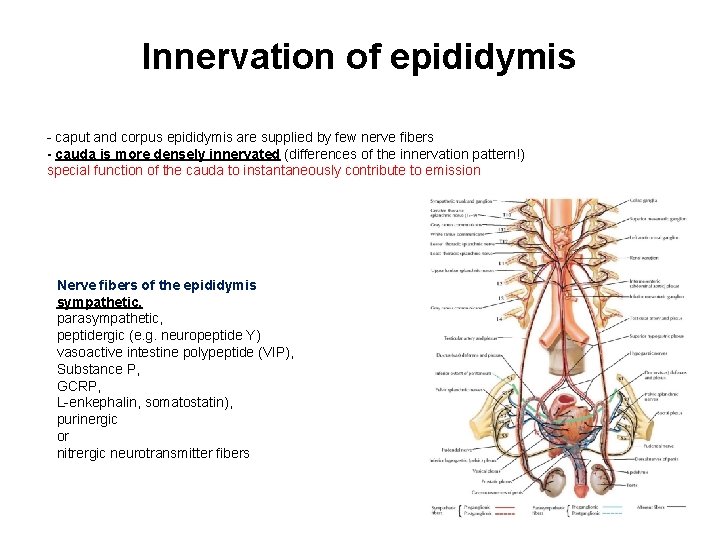
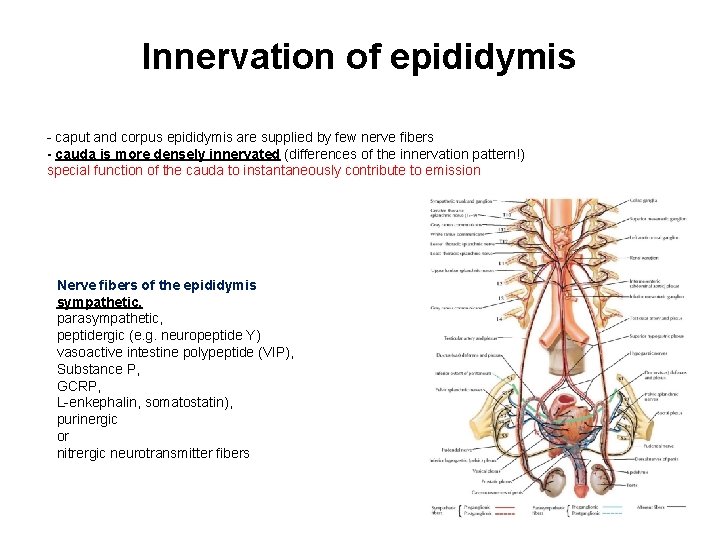
Innervation of epididymis - caput and corpus epididymis are supplied by few nerve fibers - cauda is more densely innervated (differences of the innervation pattern!) special function of the cauda to instantaneously contribute to emission Nerve fibers of the epididymis sympathetic, parasympathetic, peptidergic (e. g. neuropeptide Y) vasoactive intestine polypeptide (VIP), Substance P, GCRP, L-enkephalin, somatostatin), purinergic or nitrergic neurotransmitter fibers
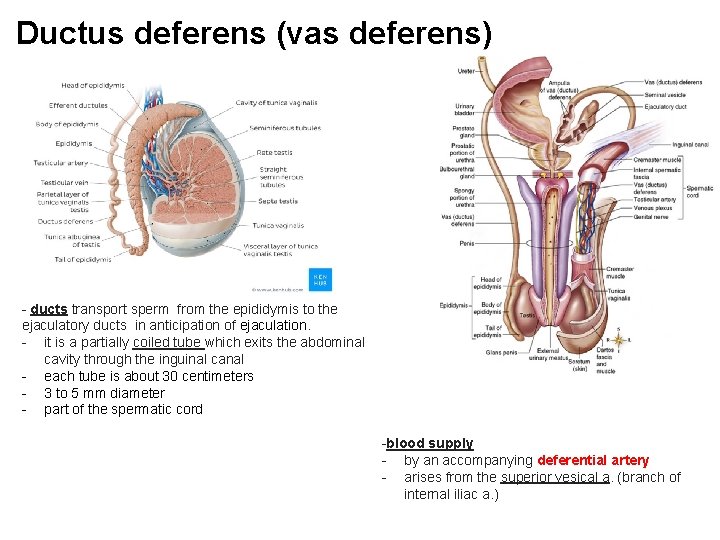
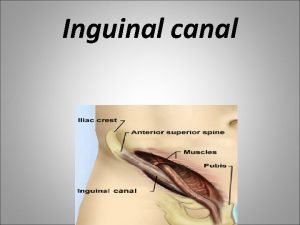
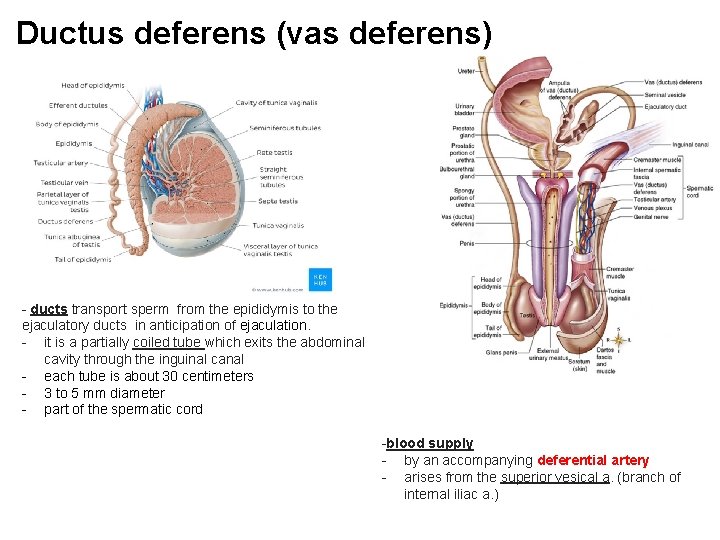
Ductus deferens (vas deferens) - ducts transport sperm from the epididymis to the ejaculatory ducts in anticipation of ejaculation. - it is a partially coiled tube which exits the abdominal cavity through the inguinal canal - each tube is about 30 centimeters - 3 to 5 mm diameter - part of the spermatic cord -blood supply - by an accompanying deferential artery - arises from the superior vesical a. (branch of internal iliac a. )
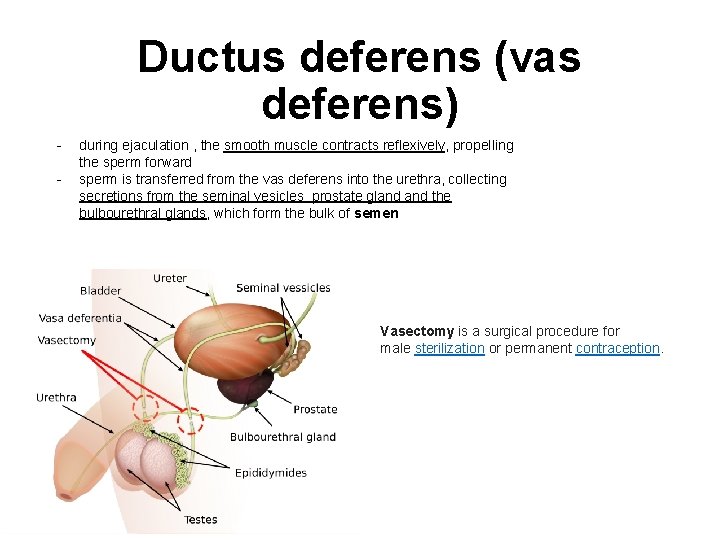
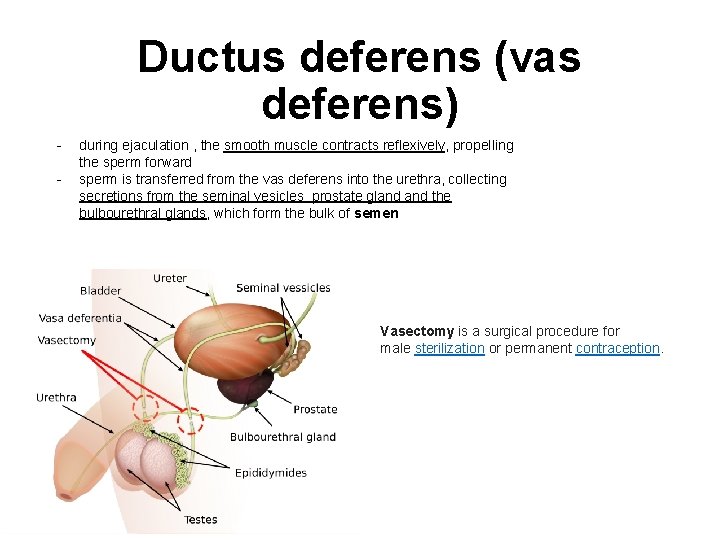
Ductus deferens (vas deferens) - during ejaculation , the smooth muscle contracts reflexively, propelling the sperm forward sperm is transferred from the vas deferens into the urethra, collecting secretions from the seminal vesicles prostate gland the bulbourethral glands, which form the bulk of semen Vasectomy is a surgical procedure for male sterilization or permanent contraception.
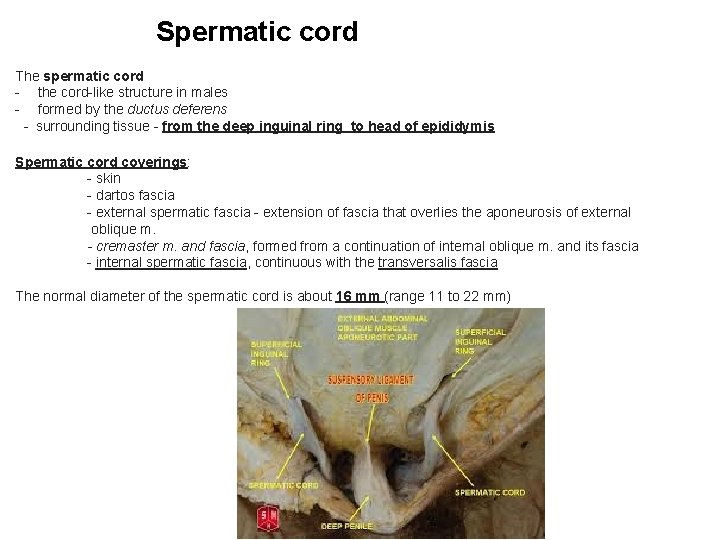
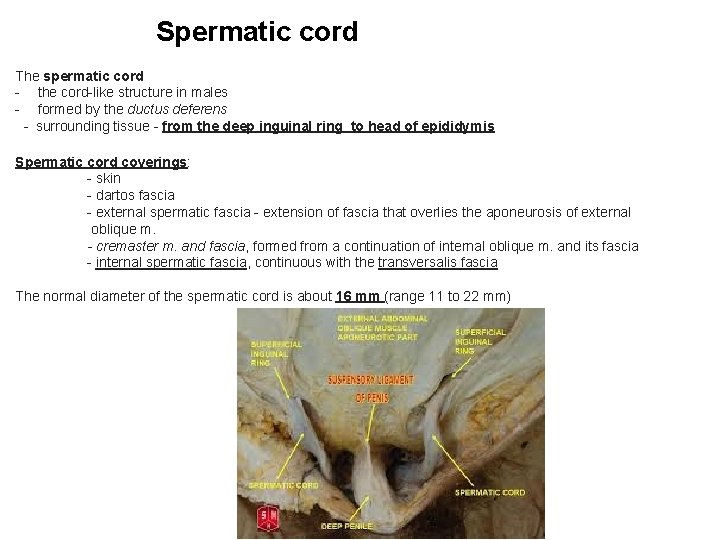
Spermatic cord The spermatic cord - the cord-like structure in males - formed by the ductus deferens - surrounding tissue - from the deep inguinal ring to head of epididymis Spermatic cord coverings: - skin - dartos fascia - external spermatic fascia - extension of fascia that overlies the aponeurosis of external oblique m. - cremaster m. and fascia, formed from a continuation of internal oblique m. and its fascia - internal spermatic fascia, continuous with the transversalis fascia The normal diameter of the spermatic cord is about 16 mm (range 11 to 22 mm)
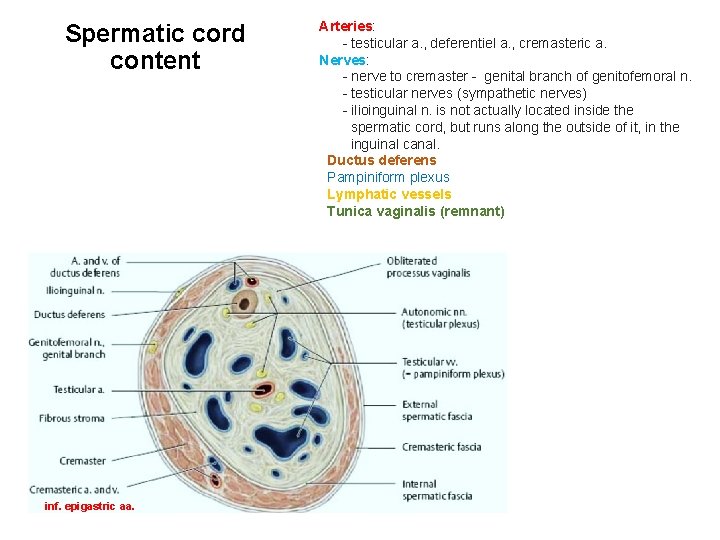
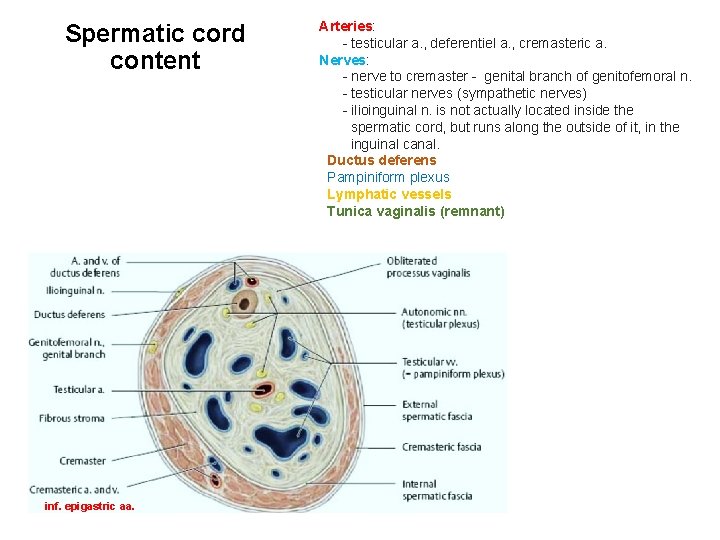
Spermatic cord content inf. epigastric aa. Arteries: - testicular a. , deferentiel a. , cremasteric a. Nerves: - nerve to cremaster - genital branch of genitofemoral n. - testicular nerves (sympathetic nerves) - ilioinguinal n. is not actually located inside the spermatic cord, but runs along the outside of it, in the inguinal canal. Ductus deferens Pampiniform plexus Lymphatic vessels Tunica vaginalis (remnant)
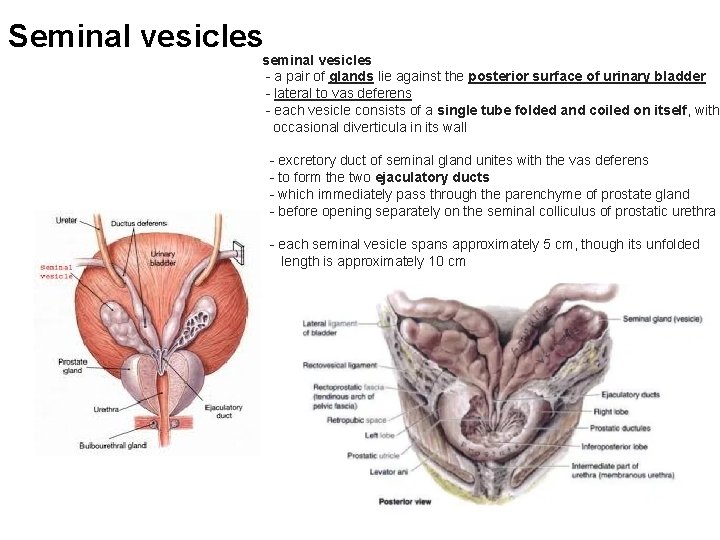
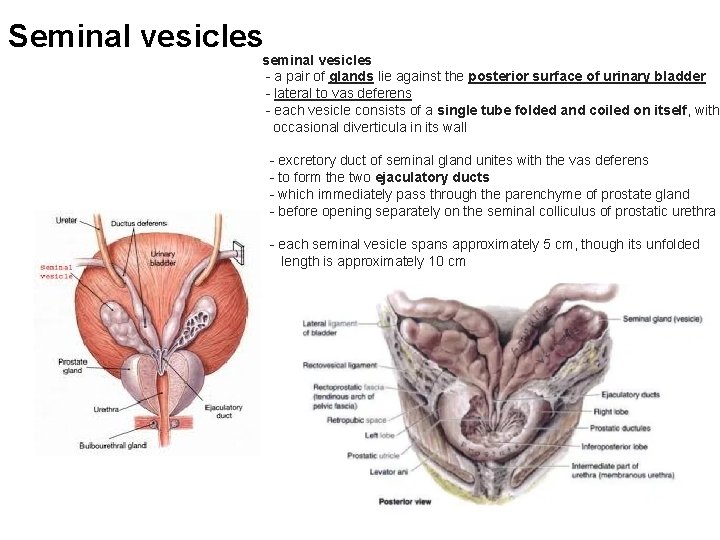
Seminal vesicles seminal vesicles - a pair of glands lie against the posterior surface of urinary bladder - lateral to vas deferens - each vesicle consists of a single tube folded and coiled on itself, with occasional diverticula in its wall - excretory duct of seminal gland unites with the vas deferens - to form the two ejaculatory ducts - which immediately pass through the parenchyme of prostate gland - before opening separately on the seminal colliculus of prostatic urethra - each seminal vesicle spans approximately 5 cm, though its unfolded length is approximately 10 cm
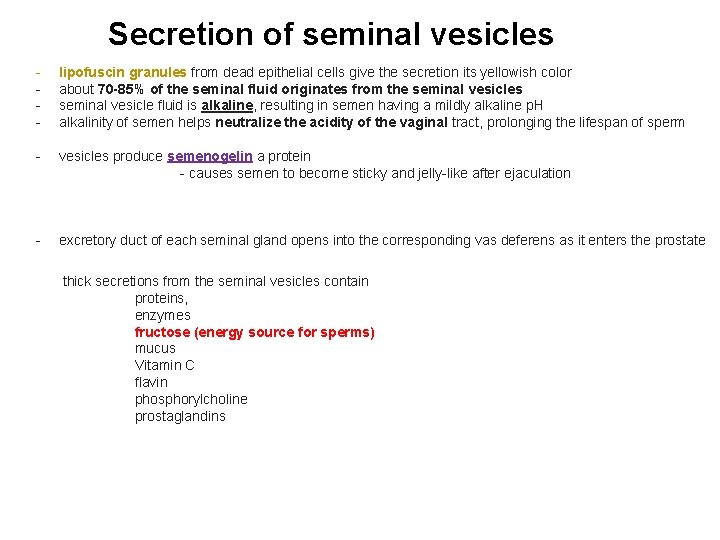
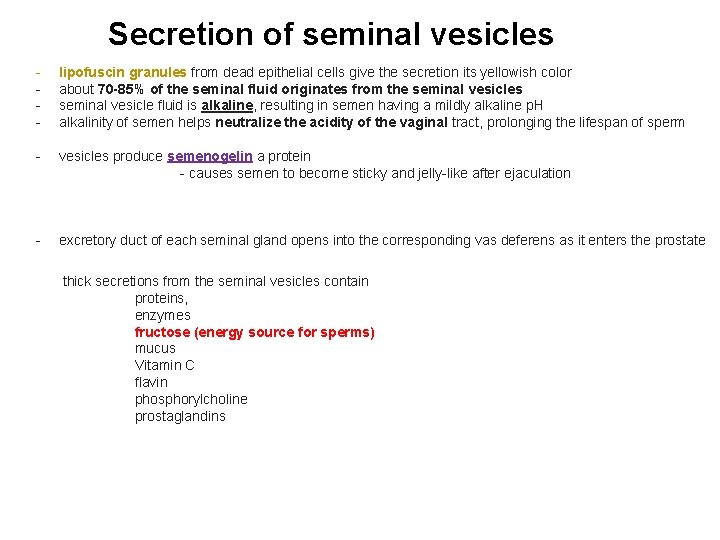
Secretion of seminal vesicles - lipofuscin granules from dead epithelial cells give the secretion its yellowish color about 70 -85% of the seminal fluid originates from the seminal vesicles seminal vesicle fluid is alkaline, resulting in semen having a mildly alkaline p. H alkalinity of semen helps neutralize the acidity of the vaginal tract, prolonging the lifespan of sperm - vesicles produce semenogelin a protein - causes semen to become sticky and jelly-like after ejaculation - excretory duct of each seminal gland opens into the corresponding vas deferens as it enters the prostate thick secretions from the seminal vesicles contain proteins, enzymes fructose (energy source for sperms) mucus Vitamin C flavin phosphorylcholine prostaglandins
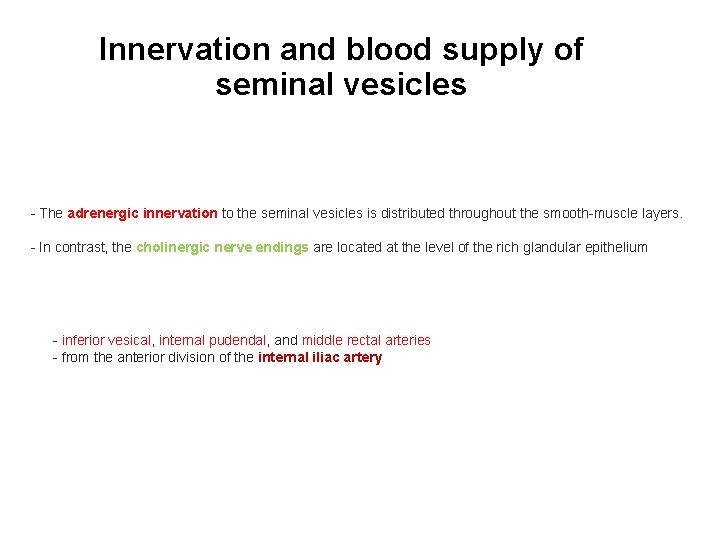
Innervation and blood supply of seminal vesicles - The adrenergic innervation to the seminal vesicles is distributed throughout the smooth-muscle layers. - In contrast, the cholinergic nerve endings are located at the level of the rich glandular epithelium - inferior vesical, internal pudendal, and middle rectal arteries - from the anterior division of the internal iliac artery
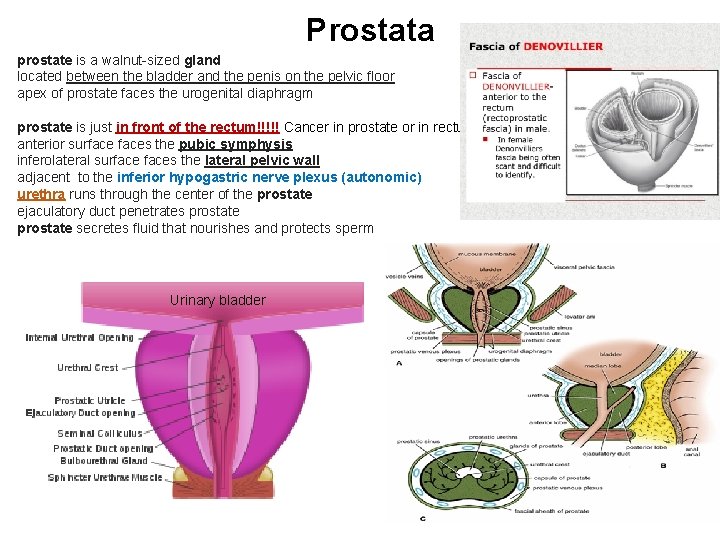
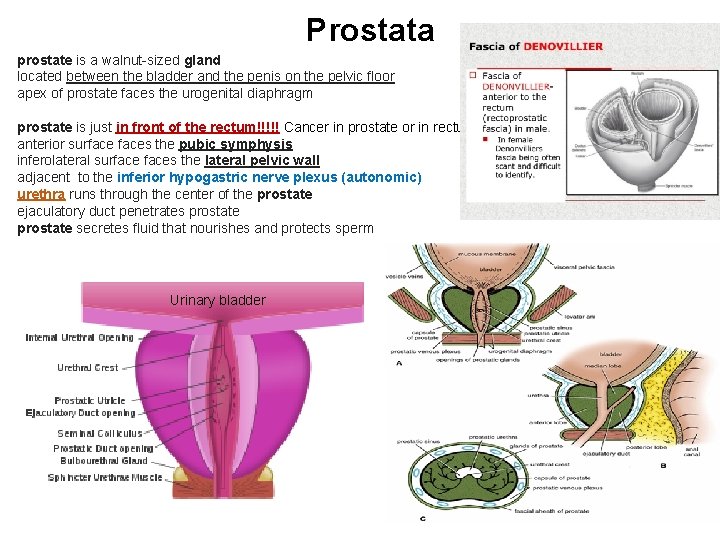
Prostata prostate is a walnut-sized gland located between the bladder and the penis on the pelvic floor apex of prostate faces the urogenital diaphragm prostate is just in front of the rectum!!!!! Cancer in prostate or in rectum!!!!! anterior surfaces the pubic symphysis inferolateral surfaces the lateral pelvic wall adjacent to the inferior hypogastric nerve plexus (autonomic) urethra runs through the center of the prostate ejaculatory duct penetrates prostate secretes fluid that nourishes and protects sperm Urinary bladder
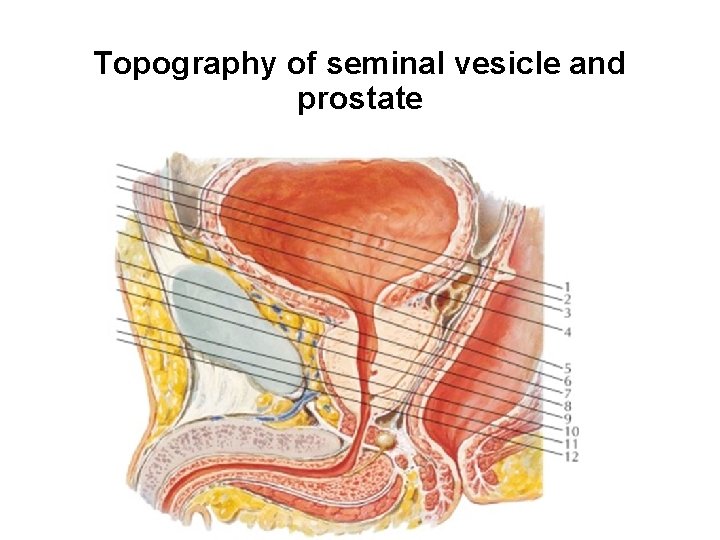
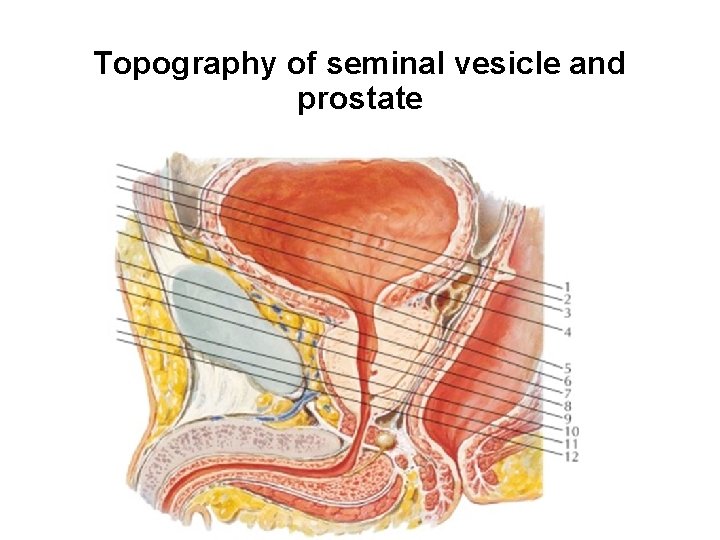
Topography of seminal vesicle and prostate
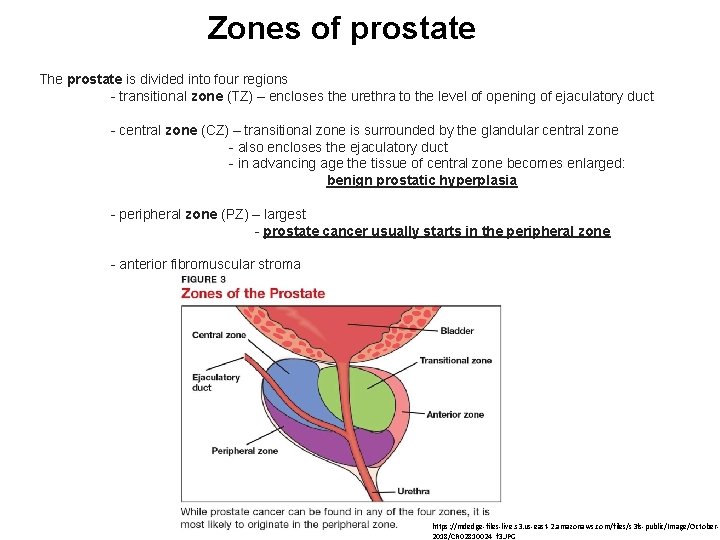
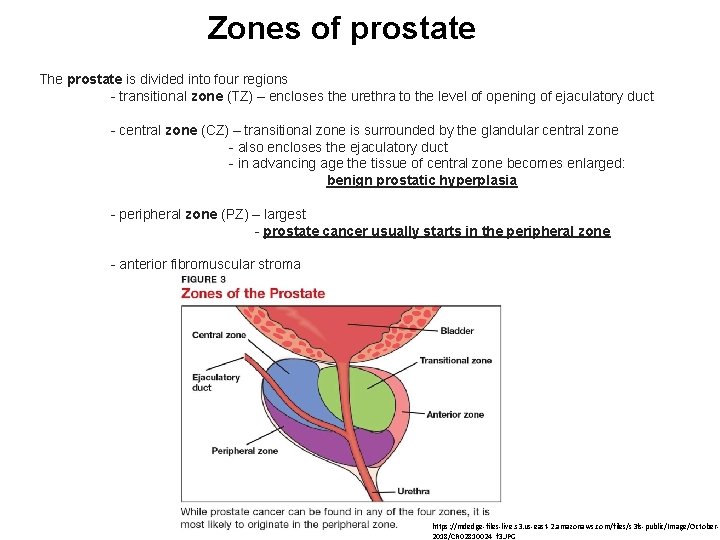
Zones of prostate The prostate is divided into four regions - transitional zone (TZ) – encloses the urethra to the level of opening of ejaculatory duct - central zone (CZ) – transitional zone is surrounded by the glandular central zone - also encloses the ejaculatory duct - in advancing age the tissue of central zone becomes enlarged: benign prostatic hyperplasia - peripheral zone (PZ) – largest - prostate cancer usually starts in the peripheral zone - anterior fibromuscular stroma https: //mdedge-files-live. s 3. us-east-2. amazonaws. com/files/s 3 fs-public/Image/October 2018/CR 02810024_f 3. JPG
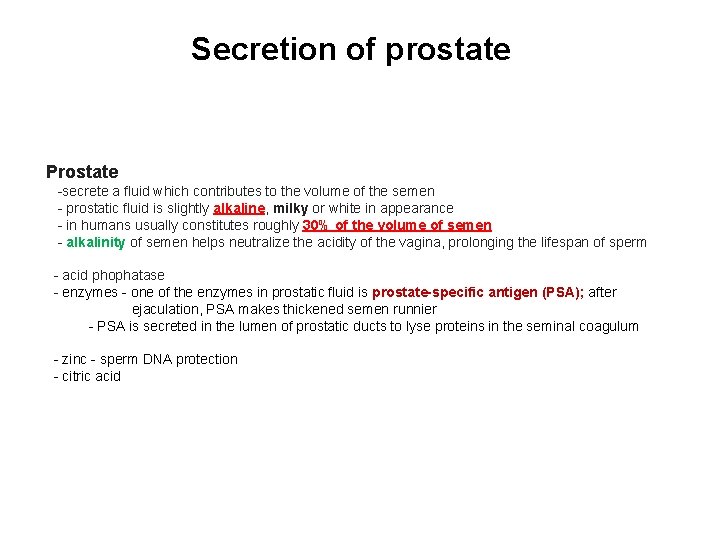
Secretion of prostate Prostate -secrete a fluid which contributes to the volume of the semen - prostatic fluid is slightly alkaline, milky or white in appearance - in humans usually constitutes roughly 30% of the volume of semen - alkalinity of semen helps neutralize the acidity of the vagina, prolonging the lifespan of sperm - acid phophatase - enzymes - one of the enzymes in prostatic fluid is prostate-specific antigen (PSA); after ejaculation, PSA makes thickened semen runnier - PSA is secreted in the lumen of prostatic ducts to lyse proteins in the seminal coagulum - zinc - sperm DNA protection - citric acid
 Spermatic cord function
Spermatic cord function Testes
Testes Prostate anatomy
Prostate anatomy Ligamentum pubocervicale
Ligamentum pubocervicale Ligamentum pubocervicale
Ligamentum pubocervicale Inguinal area
Inguinal area Pars inguinalis
Pars inguinalis Tubulus seminiferus rectus
Tubulus seminiferus rectus Lobes of prostate
Lobes of prostate Spigelian hernia
Spigelian hernia Funiculus spermaticus histology
Funiculus spermaticus histology Penis glans
Penis glans Function of the ductus deferens
Function of the ductus deferens Lig transversum cervicis
Lig transversum cervicis Ductus deferens
Ductus deferens Muscolo elevatore dell'ano
Muscolo elevatore dell'ano Perinuem
Perinuem Pembesaran pembuluh vena spermatic cord disebut
Pembesaran pembuluh vena spermatic cord disebut Covering of spermatic cord
Covering of spermatic cord Spermatic cord
Spermatic cord