PHYSIOLOGY OF TESTIS HypothalamicPituitaryGonadal Axis Testis dual function
- Slides: 23
고환의 생리 (PHYSIOLOGY OF TESTIS)
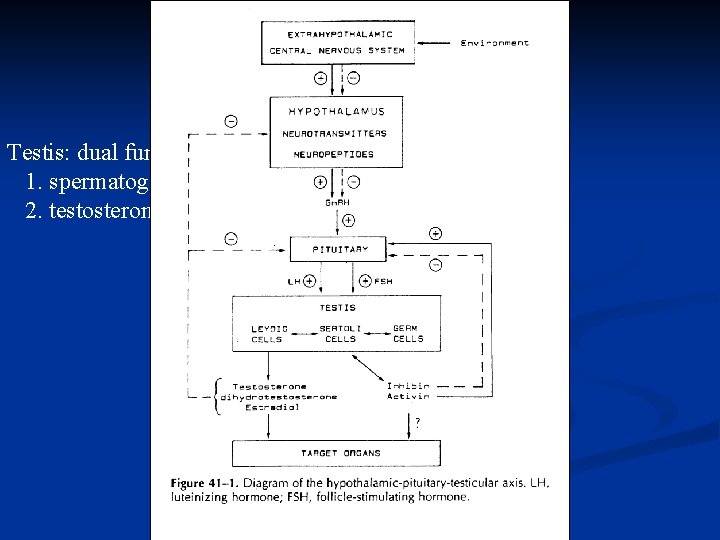
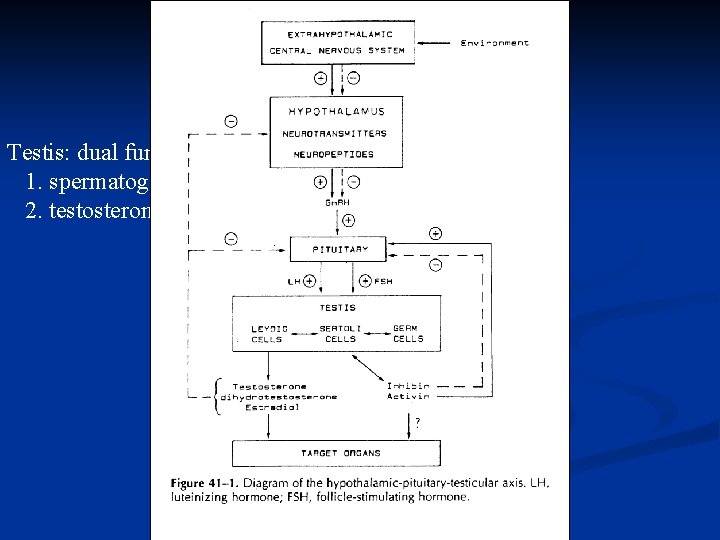
시상하부 뇌하수체 정소 축 Hypothalamic-Pituitary-Gonadal Axis Testis: dual function 1. spermatogenesis 2. testosterone formation
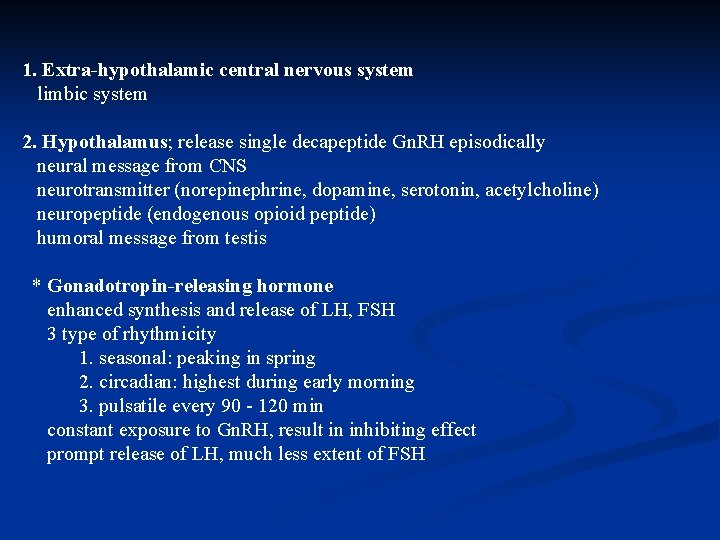
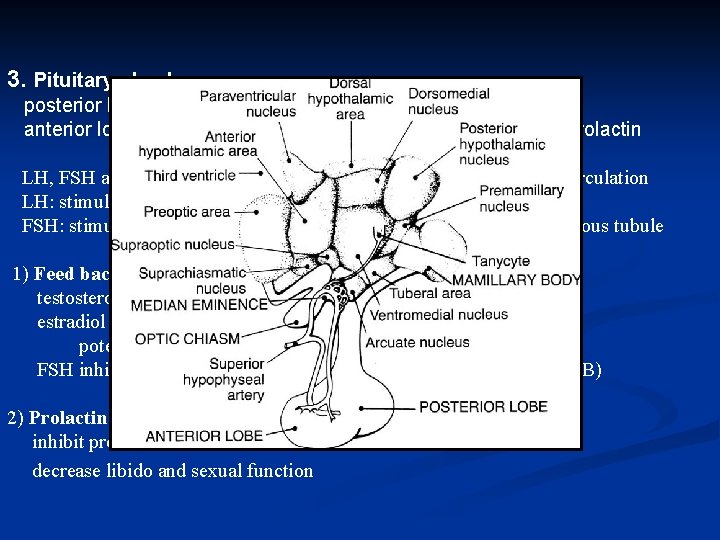
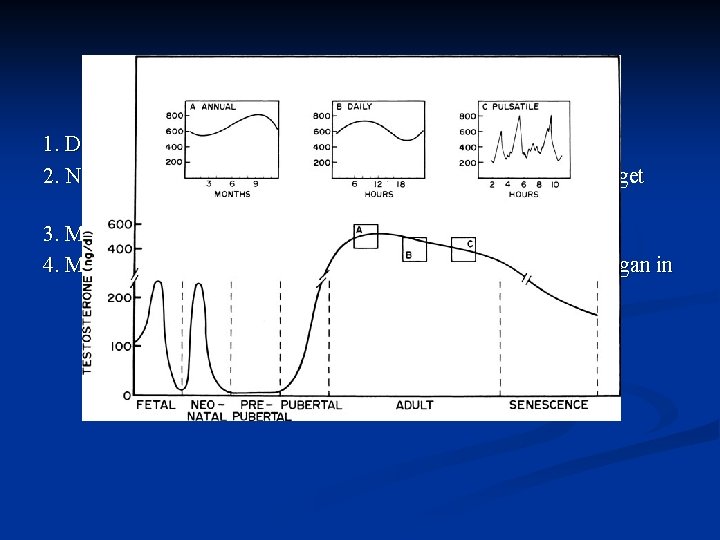
1. Extra-hypothalamic central nervous system limbic system 2. Hypothalamus; release single decapeptide Gn. RH episodically neural message from CNS neurotransmitter (norepinephrine, dopamine, serotonin, acetylcholine) neuropeptide (endogenous opioid peptide) humoral message from testis * Gonadotropin-releasing hormone enhanced synthesis and release of LH, FSH 3 type of rhythmicity 1. seasonal: peaking in spring 2. circadian: highest during early morning 3. pulsatile every 90 - 120 min constant exposure to Gn. RH, result in inhibiting effect prompt release of LH, much less extent of FSH
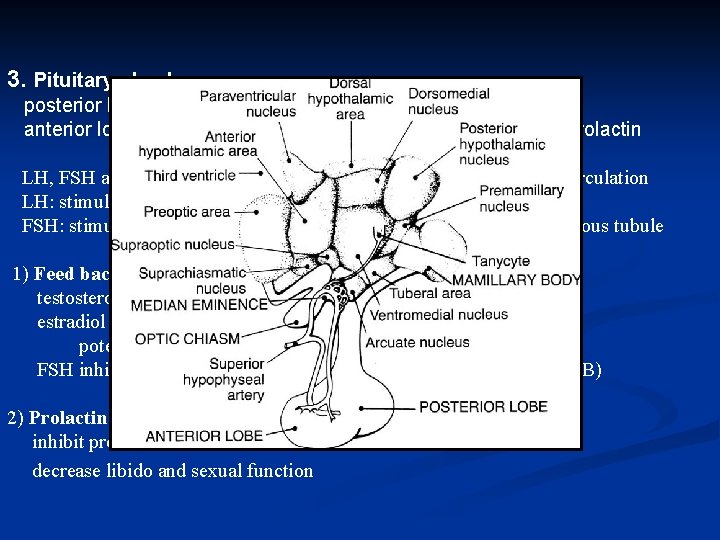
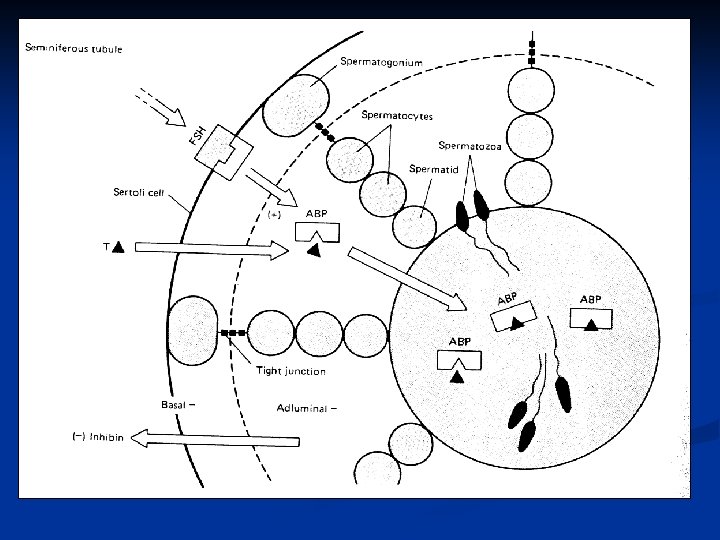
3. Pituitary gland posterior lobe (neurohypophysis): oxytocin, vasopressin anterior lobe (adenohypophysis): LH, FSH, ACTH, GH, TSH, prolactin LH, FSH are synthesized in pituitary gland, secretion into systemic circulation LH: stimulate testosterone production by Leydig cell in interstitium FSH: stimulation of Sertoli cell, support spermatogenesis in seminiferous tubule 1) Feed back control testosterone is primary inhibition of LH secretion estradiol (testis, peripheral conversion of androgen); potent inhibition of LH, FSH inhibited by inhibin (secreted primarily by Sertoli cell, inhibin B) 2) Prolactin inhibit production of Gn. RH decrease libido and sexual function
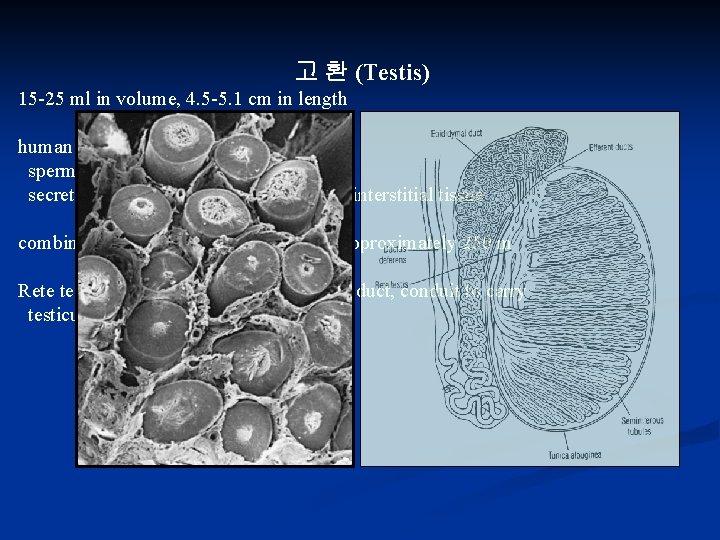
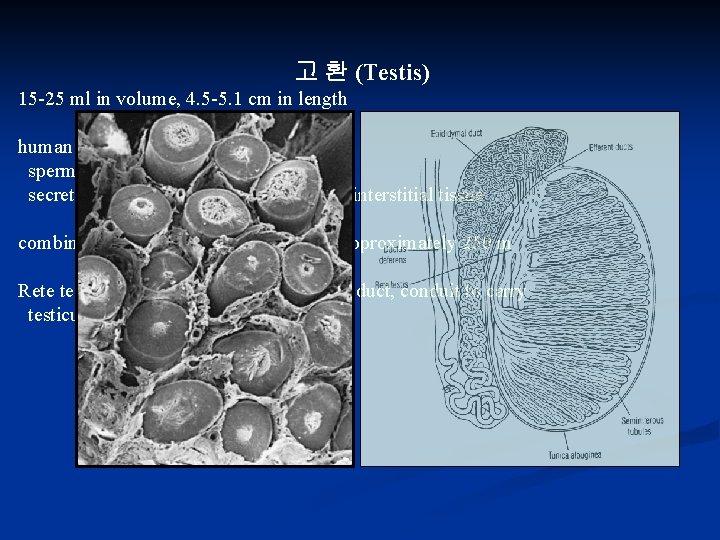
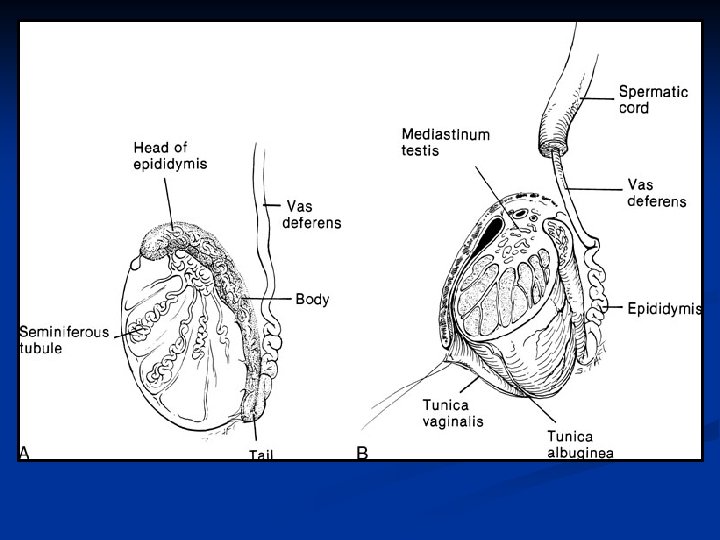
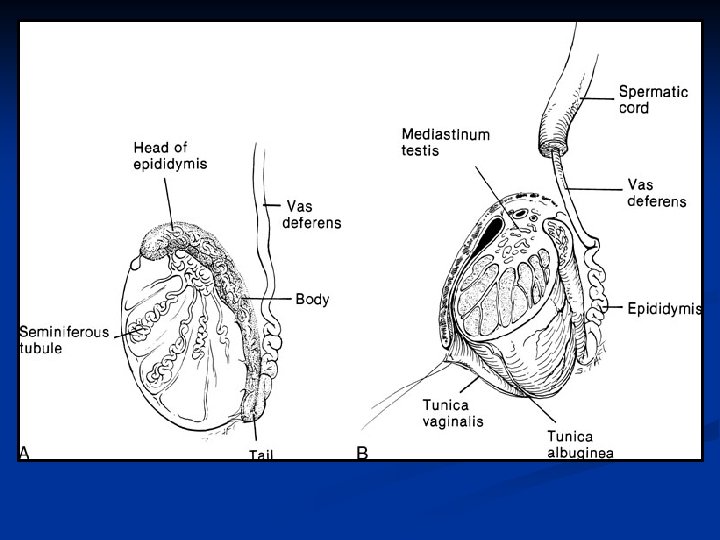
고 환 (Testis) 15 -25 ml in volume, 4. 5 -5. 1 cm in length human testis is an organ of dual function spermatogenesis in seminiferous tubule secretion of androgen by Leydig cell, in interstitial tissue combined length of 600 -1200 tubules is approximately 250 m Rete testis coalesce to form 6~12 efferent duct, conduit to carry testicular fluid and spermatozoa
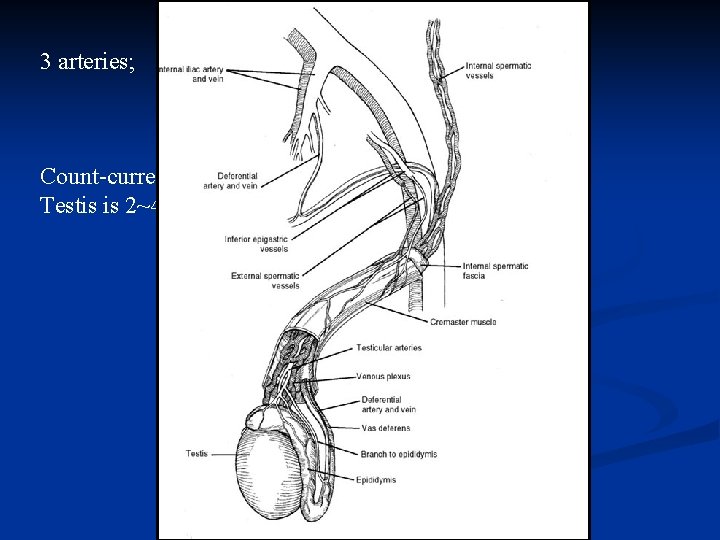
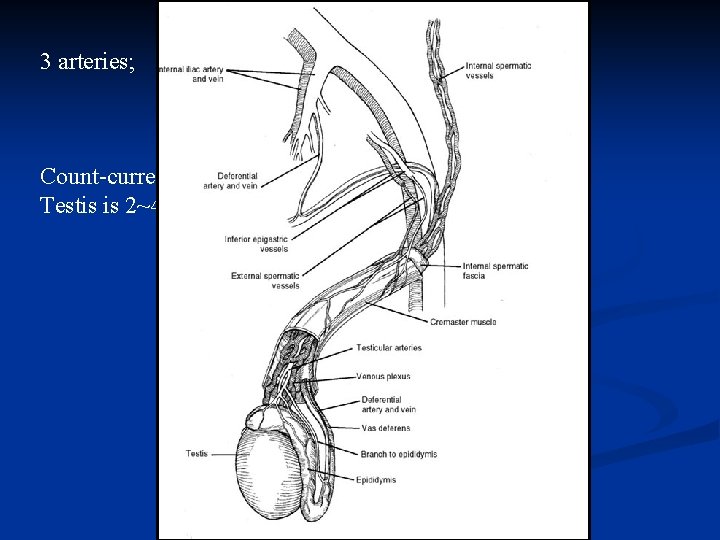
3 arteries; 1. internal spermatic artery 2. deferential artery 3. external spermatic or cremasteric artery Count-current exchange of heat in spermatic cord Testis is 2~4 o. C lower than rectal temperature
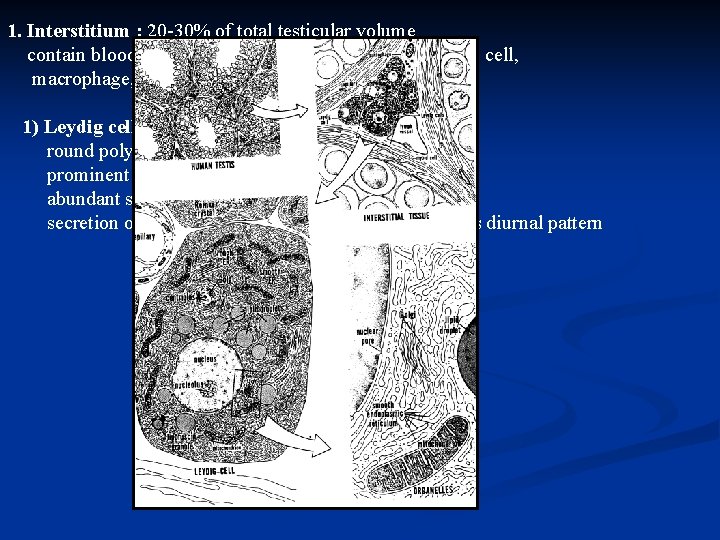
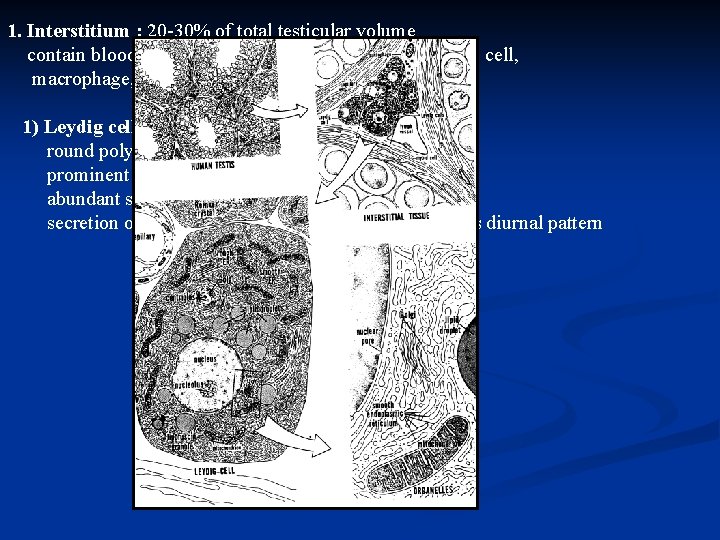
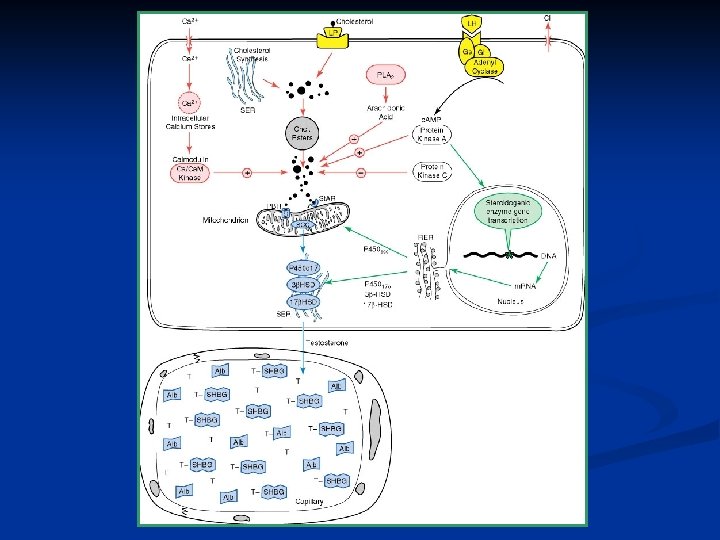
1. Interstitium : 20 -30% of total testicular volume contain blood vessel, lymphatics, fibroblastic supporting cell, macrophage, mast cell, Leydig cell. 1) Leydig cell round polygonal cytoplasm prominent mitochondria abundant s-ER secretion of testosterone response to LH pulse and has diurnal pattern
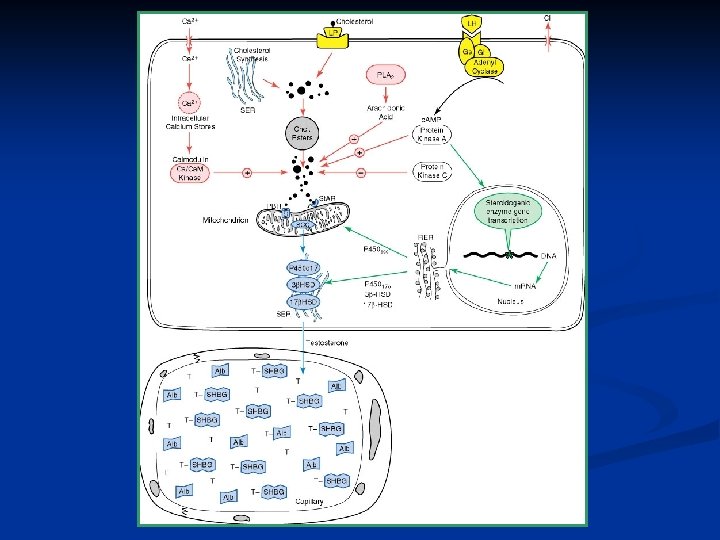
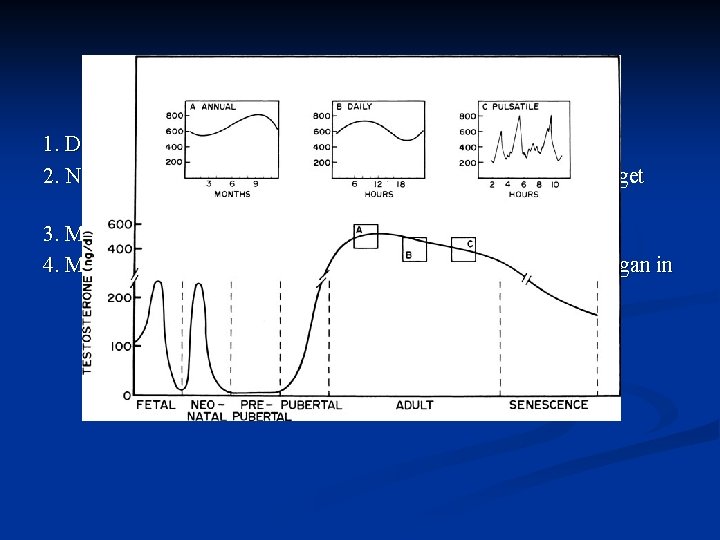
Major epochs in testosterone production 1. Differentiation and development of fetal reproductive tract 2. Neonatal organization or imprinting of androgen dependent target tissue 3. Masculainization of male at puberty 4. Maintenance of growth and function of androgen-dependent organ in adult
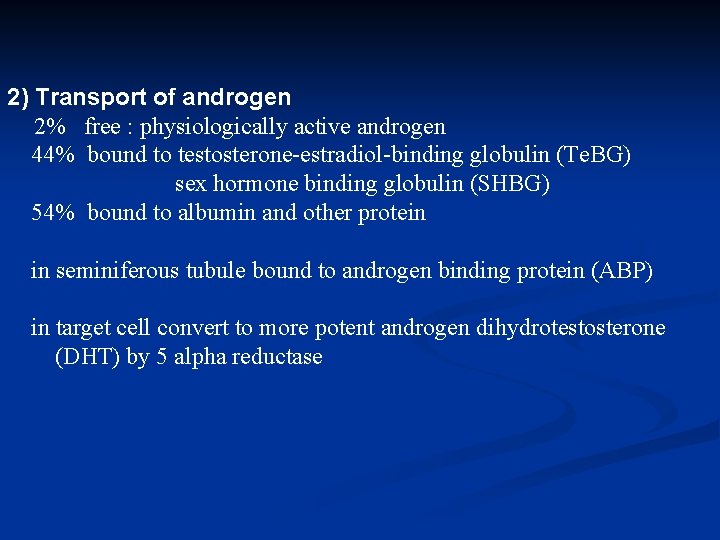
2) Transport of androgen 2% free : physiologically active androgen 44% bound to testosterone-estradiol-binding globulin (Te. BG) sex hormone binding globulin (SHBG) 54% bound to albumin and other protein in seminiferous tubule bound to androgen binding protein (ABP) in target cell convert to more potent androgen dihydrotestosterone (DHT) by 5 alpha reductase
3) Function of androgen target tissue a. regulation of gonadotropin secretion by hypothalamic-pituitary axis b. initiation and maintenance of spermatogenesis c. differentiation of internal and external male genital system during fetal development d. promotion of sexual maturation at puberty
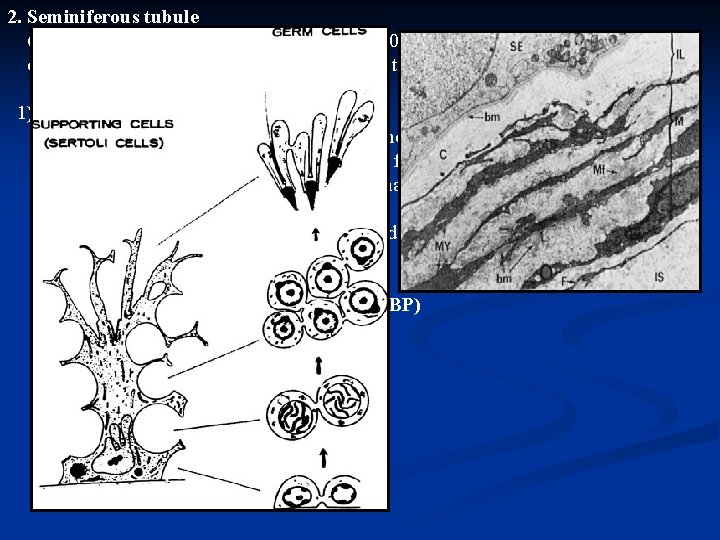
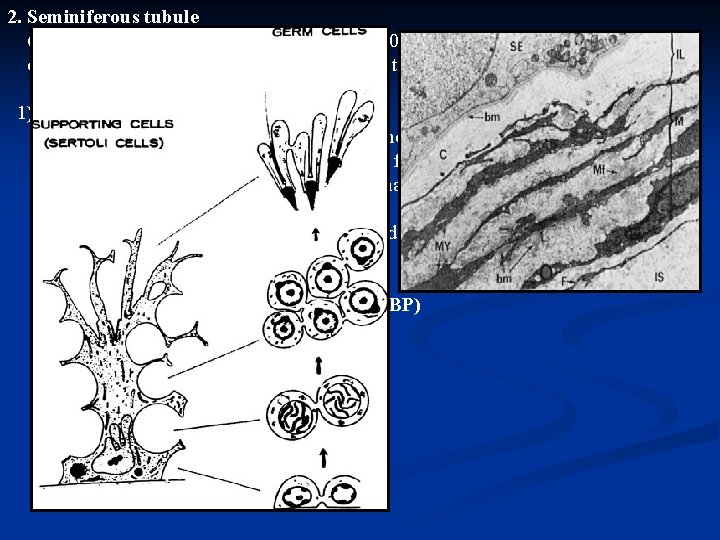
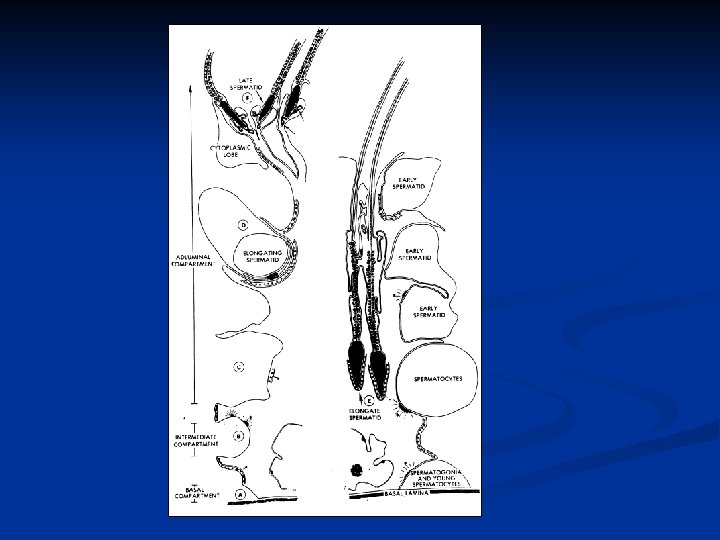
2. Seminiferous tubule 600 -1200 tubules in testis, approximately 250 m contain germ cell and Sertoli cell, 85 -90% of testicular volume 1) Sertoli cell linked by tight junction, divide into basal and adluminal compartment close approximation of myoid cell, serve to form blood-testis barrier create unique microenvironment in adluminal compartment facilitate spermatogenesis maintain in immunologically privileged location nourishment of developing germ cell phagocytosis damaged cell production of androgen binding protein (ABP) production of inhibin
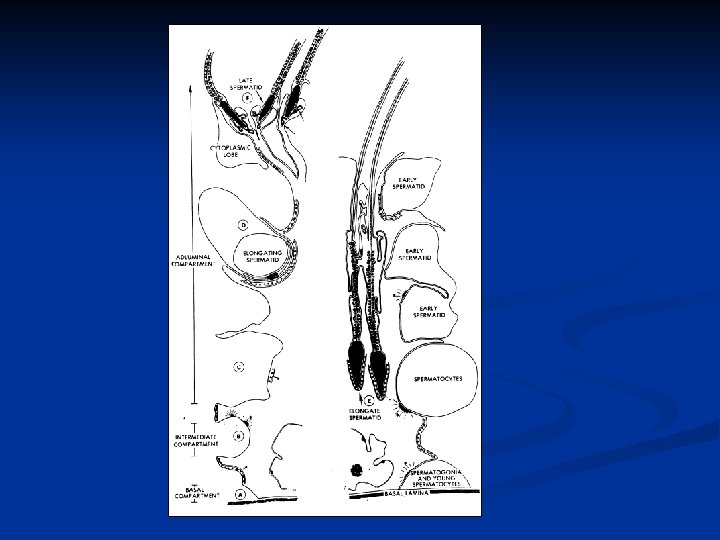
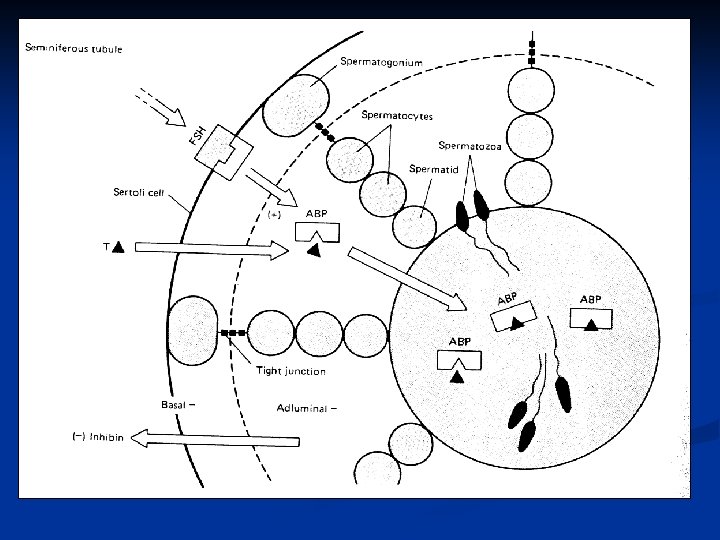
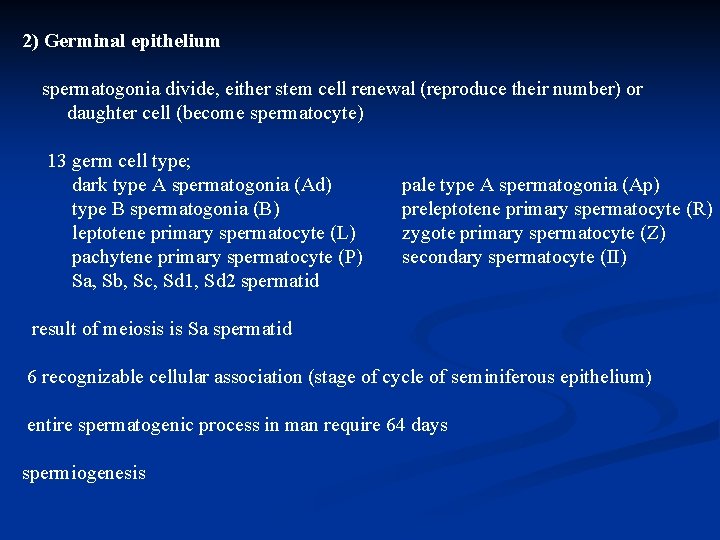
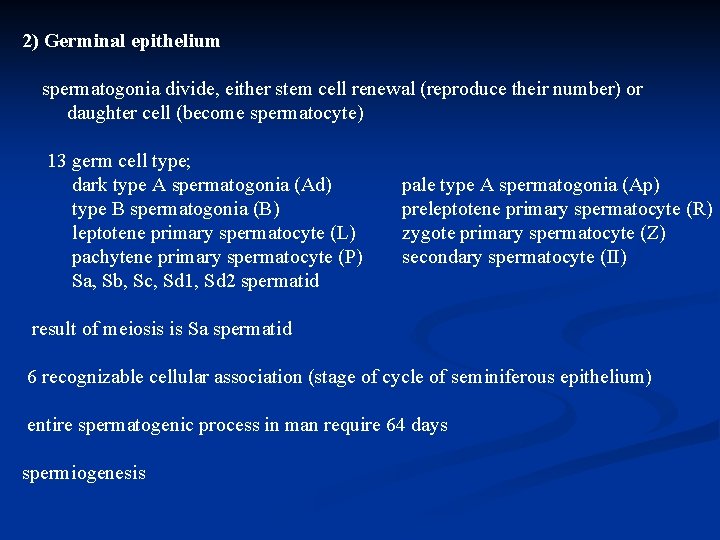
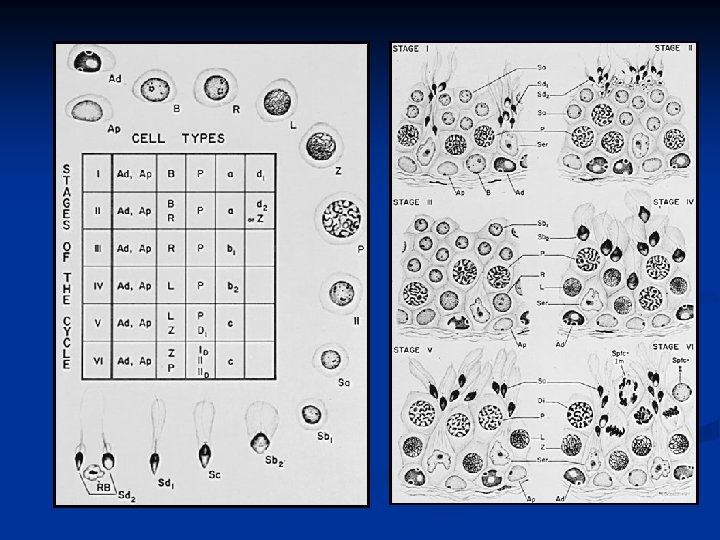
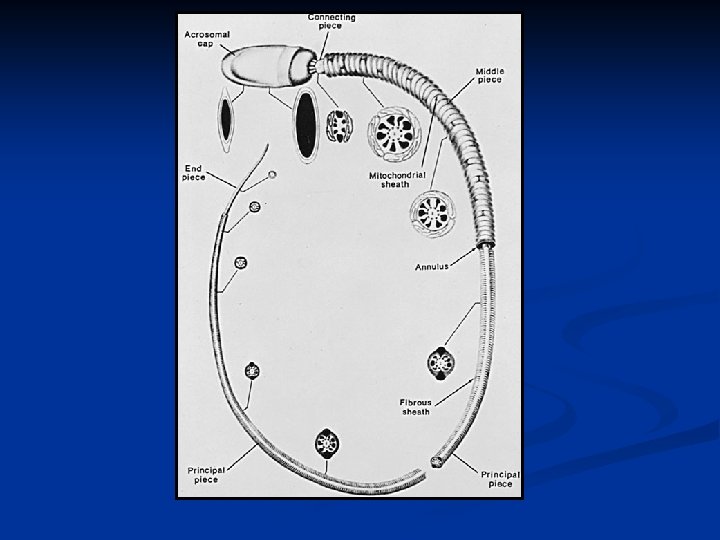
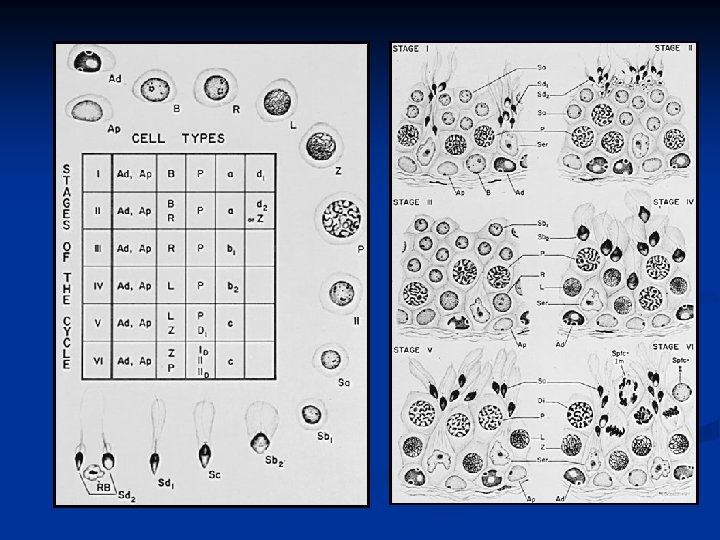
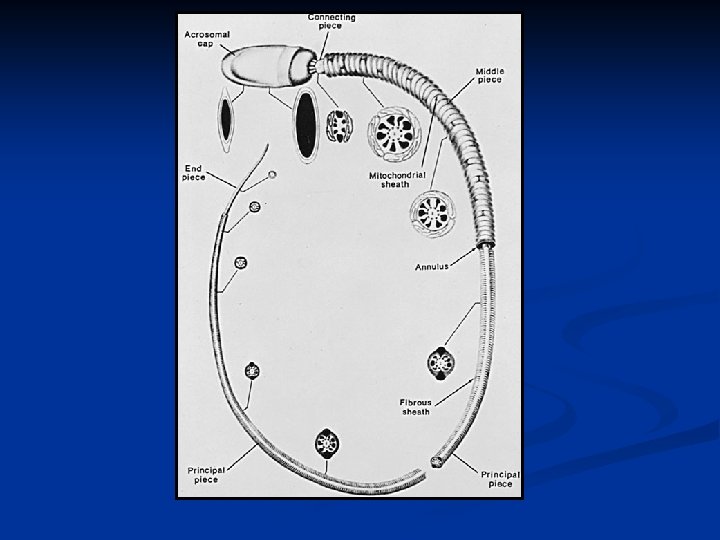
2) Germinal epithelium spermatogonia divide, either stem cell renewal (reproduce their number) or daughter cell (become spermatocyte) 13 germ cell type; dark type A spermatogonia (Ad) type B spermatogonia (B) leptotene primary spermatocyte (L) pachytene primary spermatocyte (P) Sa, Sb, Sc, Sd 1, Sd 2 spermatid pale type A spermatogonia (Ap) preleptotene primary spermatocyte (R) zygote primary spermatocyte (Z) secondary spermatocyte (II) result of meiosis is Sa spermatid 6 recognizable cellular association (stage of cycle of seminiferous epithelium) entire spermatogenic process in man require 64 days spermiogenesis
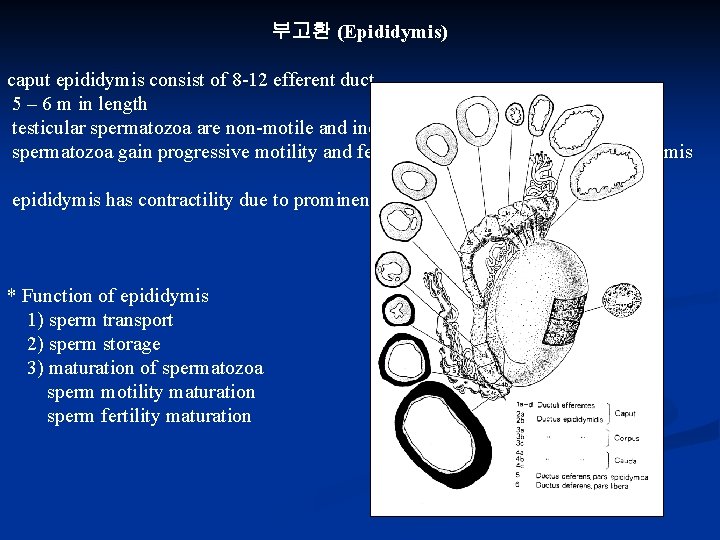
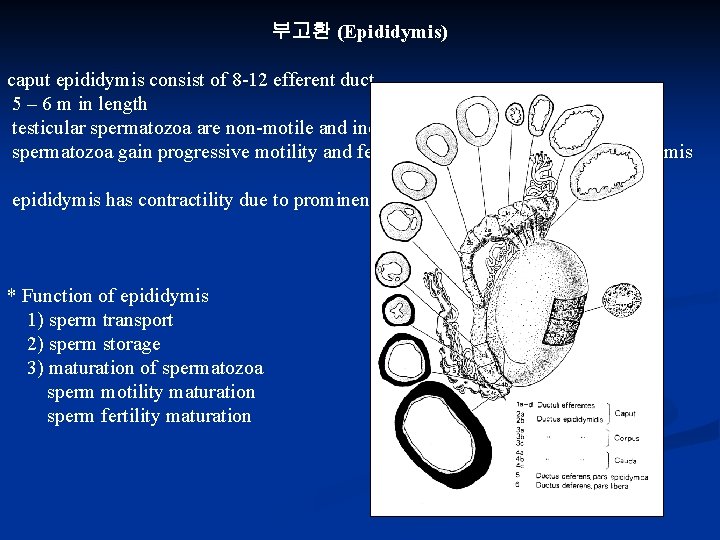
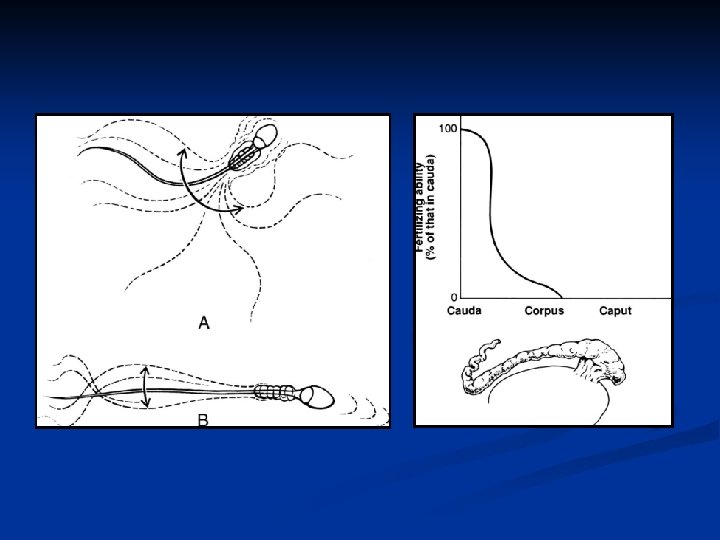
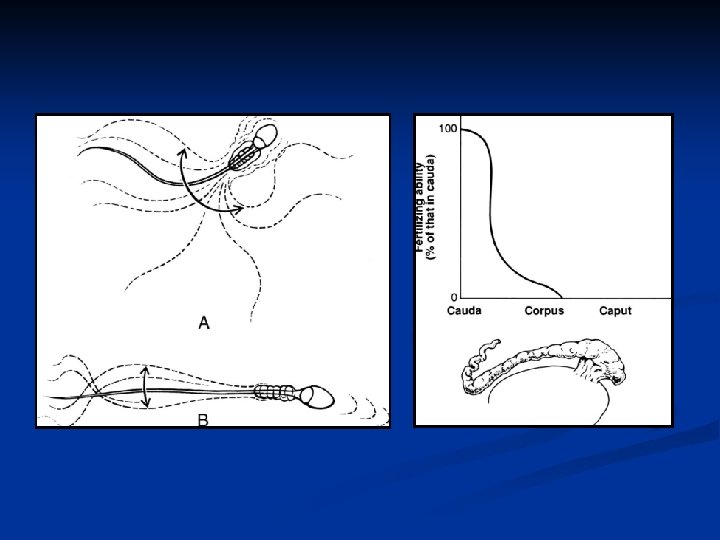
부고환 (Epididymis) caput epididymis consist of 8 -12 efferent duct 5 – 6 m in length testicular spermatozoa are non-motile and incapable of fertilizing ova spermatozoa gain progressive motility and fertilizing ability after passing epididymis has contractility due to prominent muscular development * Function of epididymis 1) sperm transport 2) sperm storage 3) maturation of spermatozoa sperm motility maturation sperm fertility maturation
정 낭 (SEMINAL VESICLE) major volume of seminal plasma from seminal vesicle (60%) provide nourishing substrate fructose prostaglandin, phosphorylcholine, coagulating substance seminal plasma has buffering effect on acidic vaginal environment
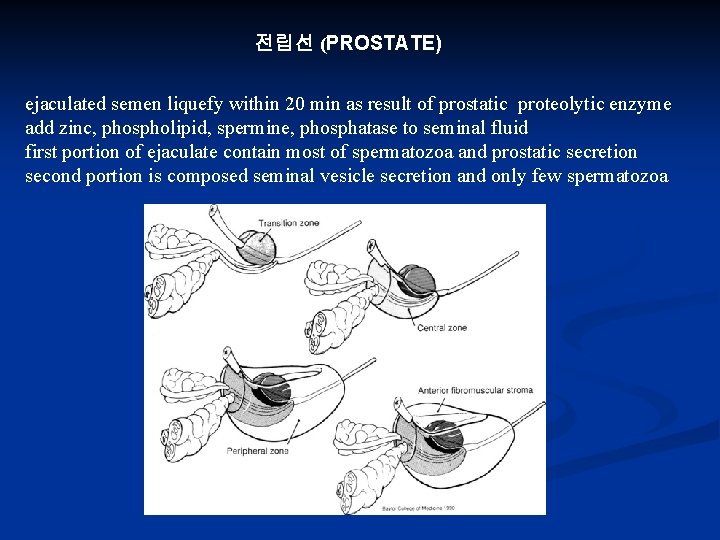
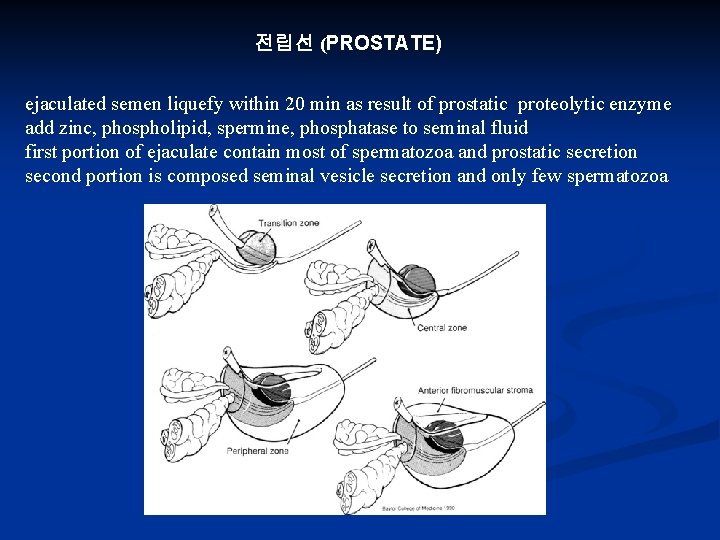
전립선 (PROSTATE) ejaculated semen liquefy within 20 min as result of prostatic proteolytic enzyme add zinc, phospholipid, spermine, phosphatase to seminal fluid first portion of ejaculate contain most of spermatozoa and prostatic secretion second portion is composed seminal vesicle secretion and only few spermatozoa