1 AHAACC Guidelines for Secondary Prevention for Patients




- Slides: 75

1
AHA/ACC Guidelines for Secondary Prevention for Patients with Coronary and Other Atherosclerotic Vascular Disease: 2006 Update Gregg C. Fonarow, MD and Sidney Smith Jr, MD on behalf of the Secondary Prevention Writing Group 2
Introduction This slide set was adapted from the AHA/ACC Secondary Prevention for Patients with Coronary and Other Atherosclerotic Vascular Disease: 2006 Update The full-text guidelines are available on the Web sites of the AHA (www. americanheart. org) and the ACC (www. acc. org) Circulation 2006; 113: 2363 -2372 and J Am Coll Cardiol 2006; 47: 2130 -2139 3
Introduction • Since the 2001 update of the AHA/ACC consensus statement on secondary prevention, important evidence from clinical trials has emerged that further supports and broadens the merits of aggressive risk reduction therapies • This growing body of evidence confirms that aggressive comprehensive risk factor management improves survival, reduces recurrent events and the need for interventional procedures, and improves the quality of life • The secondary prevention patient population includes those with established coronary and other atherosclerotic vascular disease, including peripheral arterial disease, atherosclerotic aortic disease and carotid artery disease. 4
AHA Secondary Prevention for Patients with Coronary Artery and Other Atherosclerotic Vascular Disease Writing Committee Members Sidney C. Smith, Jr, MD; Jerilyn Allen, RN, Sc. D; Steven N. Blair, PED; Robert O. Bonow, MD; Lawrence M. Brass, MD; Gregg C. Fonarow, MD; Scott M. Grundy, MD, Ph. D; Loren Hiratzka, MD ; Daniel Jones, MD; Harlan M. Krumholz, MD; Lori Mosca, MD, Ph. D, MPH; Richard C. Pasternak, MD*; Thomas Pearson, MD, MPH, Ph. D; Marc A. Pfeffer, MD, Ph. D; Kathryn A. Taubert, Ph. D Circulation 2006; 113: 2363 -2372 and J Am Coll Cardiol 2006; 47: 2130 -2139 *Dr. Pasternak withdrew from the Writing Group on June 22 nd, 2004, when he accepted an offer of employment as Vice President, Clinical Research, Cardiovascular and Atherosclerosis at Merck Research Laboratories. 5
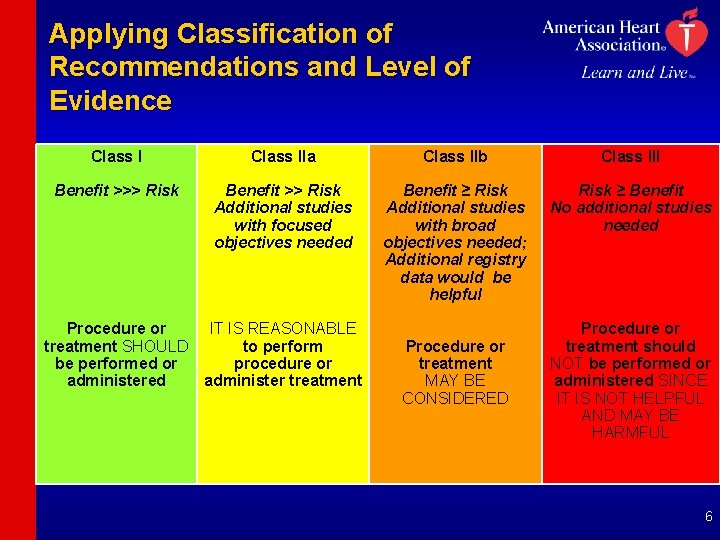
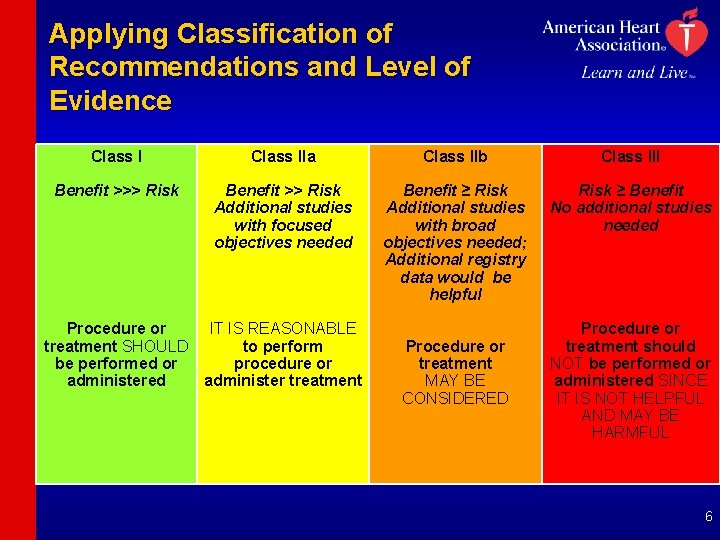
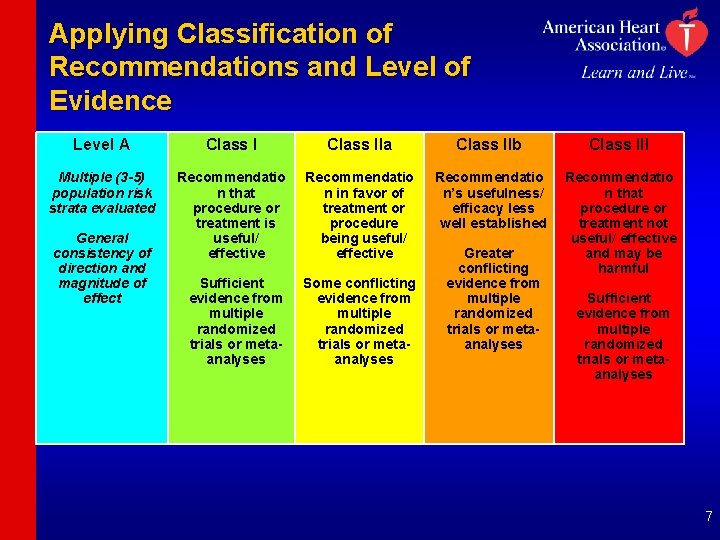
Applying Classification of Recommendations and Level of Evidence Class IIa Class IIb Class III Benefit >>> Risk Benefit >> Risk Additional studies with focused objectives needed Benefit ≥ Risk Additional studies with broad objectives needed; Additional registry data would be helpful Risk ≥ Benefit No additional studies needed Procedure or IT IS REASONABLE treatment SHOULD to perform be performed or procedure or administered administer treatment Procedure or treatment MAY BE CONSIDERED Procedure or treatment should NOT be performed or administered SINCE IT IS NOT HELPFUL AND MAY BE HARMFUL 6
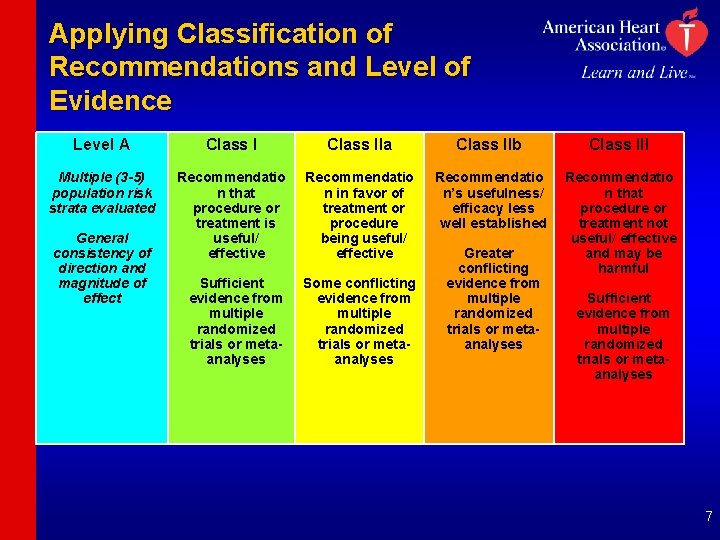
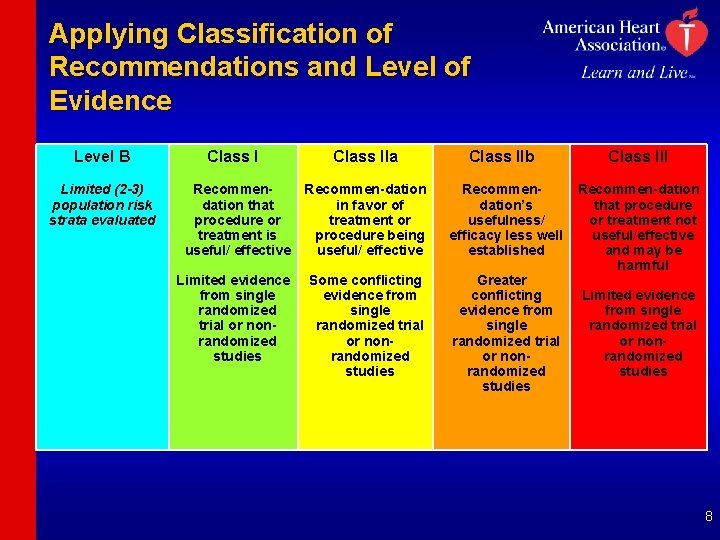
Applying Classification of Recommendations and Level of Evidence Level A Class IIa Class IIb Class III Multiple (3 -5) population risk strata evaluated Recommendatio n that procedure or treatment is useful/ effective Recommendatio n in favor of treatment or procedure being useful/ effective Recommendatio n’s usefulness/ efficacy less well established Sufficient evidence from multiple randomized trials or metaanalyses Some conflicting evidence from multiple randomized trials or metaanalyses Recommendatio n that procedure or treatment not useful/ effective and may be harmful General consistency of direction and magnitude of effect Greater conflicting evidence from multiple randomized trials or metaanalyses Sufficient evidence from multiple randomized trials or metaanalyses 7
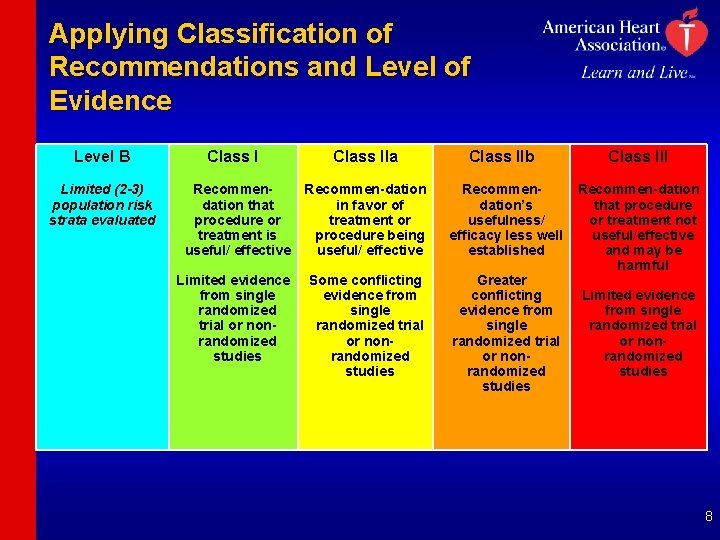
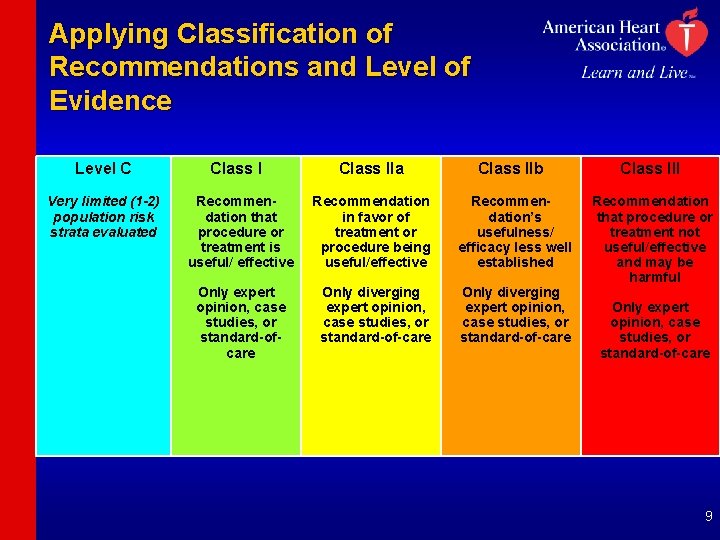
Applying Classification of Recommendations and Level of Evidence Level B Limited (2 -3) population risk strata evaluated Class IIa Class IIb Recommendation that procedure or treatment is useful/ effective Recommen-dation in favor of treatment or procedure being useful/ effective Recommendation’s usefulness/ efficacy less well established Limited evidence from single randomized trial or nonrandomized studies Some conflicting evidence from single randomized trial or nonrandomized studies Greater conflicting evidence from single randomized trial or nonrandomized studies Class III Recommen-dation that procedure or treatment not useful/effective and may be harmful Limited evidence from single randomized trial or nonrandomized studies 8
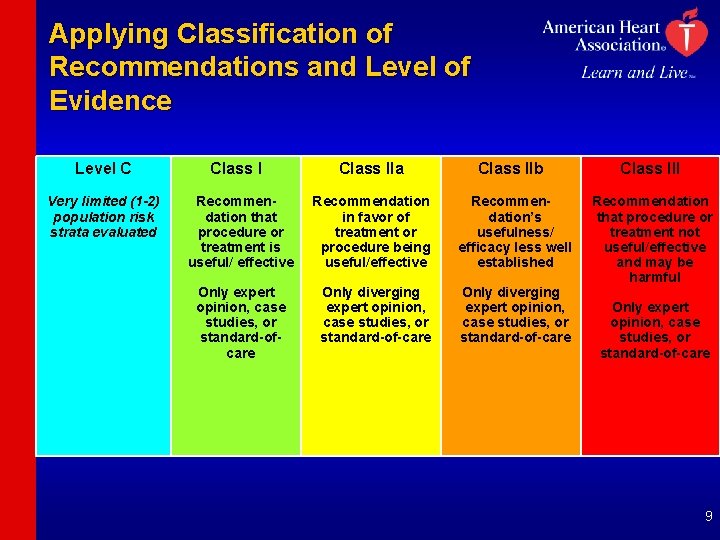
Applying Classification of Recommendations and Level of Evidence Level C Very limited (1 -2) population risk strata evaluated Class I Recommendation that procedure or treatment is useful/ effective Only expert opinion, case studies, or standard-ofcare Class IIa Class IIb Recommendation in favor of treatment or procedure being useful/effective Recommendation’s usefulness/ efficacy less well established Only diverging expert opinion, case studies, or standard-of-care Class III Recommendation that procedure or treatment not useful/effective and may be harmful Only expert opinion, case studies, or standard-of-care 9
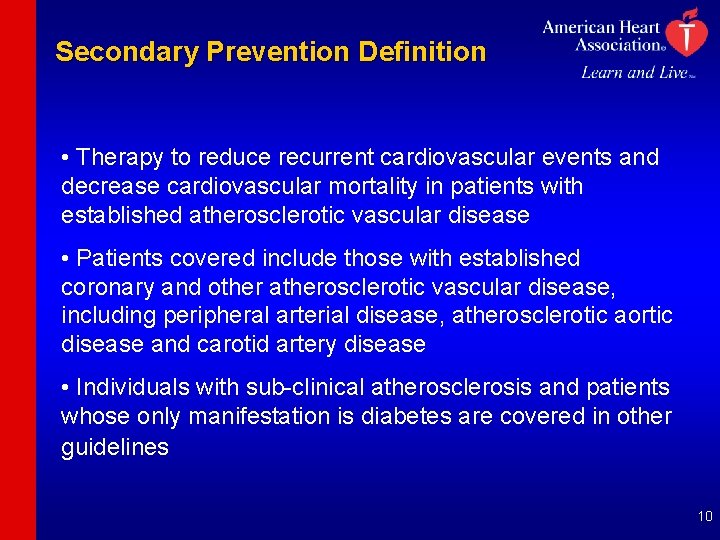
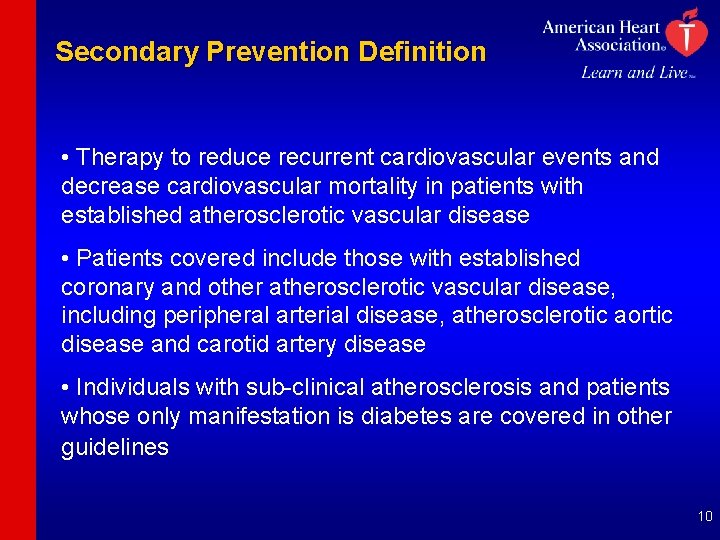
Secondary Prevention Definition • Therapy to reduce recurrent cardiovascular events and decrease cardiovascular mortality in patients with established atherosclerotic vascular disease • Patients covered include those with established coronary and other atherosclerotic vascular disease, including peripheral arterial disease, atherosclerotic aortic disease and carotid artery disease • Individuals with sub-clinical atherosclerosis and patients whose only manifestation is diabetes are covered in other guidelines 10
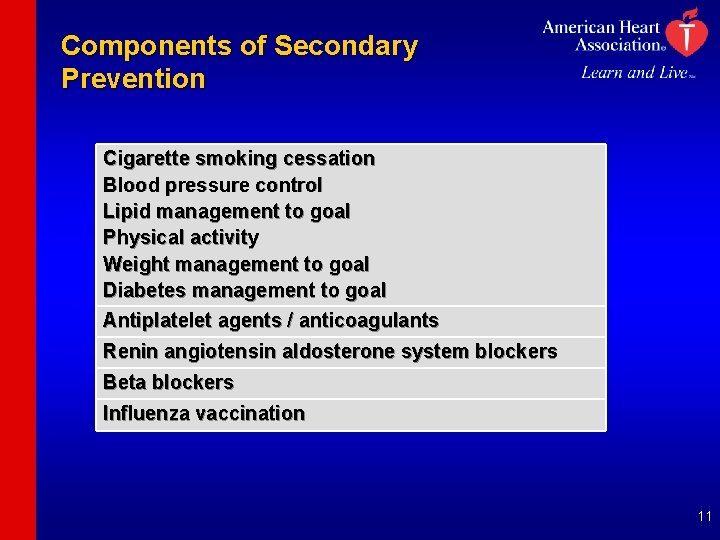
Components of Secondary Prevention Cigarette smoking cessation Blood pressure control Lipid management to goal Physical activity Weight management to goal Diabetes management to goal Antiplatelet agents / anticoagulants Renin angiotensin aldosterone system blockers Beta blockers Influenza vaccination 11
Evidence Based Therapies The writing group emphasizes the importance of giving consideration to the use of cardiovascular medications that have been proven to be of benefit in randomized clinical trials. This approach strengthens the evidence-based foundation for therapeutic application of these guidelines. The committee acknowledges that in many trials there is under-representation of ethnic minorities, women, and the elderly. 12
Cigarette Smoking Recommendations Goal: Complete Cessation and No Exposure to Environmental Tobacco Smoke • Ask about tobacco use status at every visit. • Advise every tobacco user to quit. • Assess the tobacco user’s willingness to quit. • Assist by counseling and developing a plan for quitting. • Arrange follow-up, referral to special programs, or pharmacotherapy (including nicotine replacement and bupropion. • Urge avoidance of exposure to environmental tobacco smoke at work and home. 13
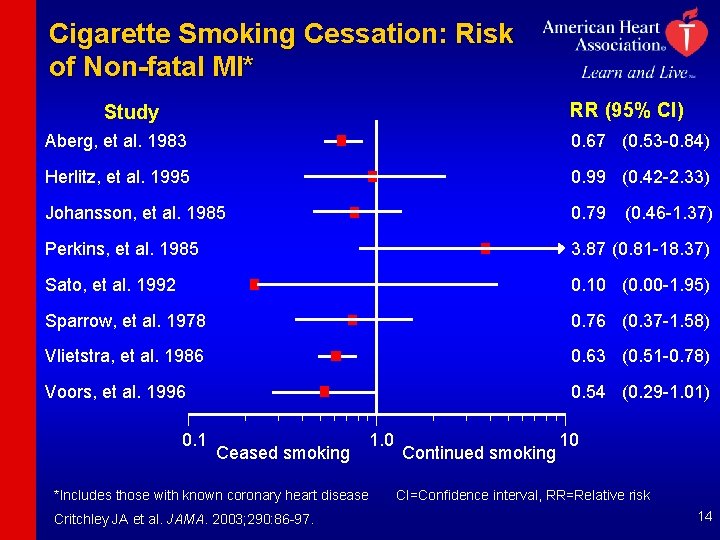
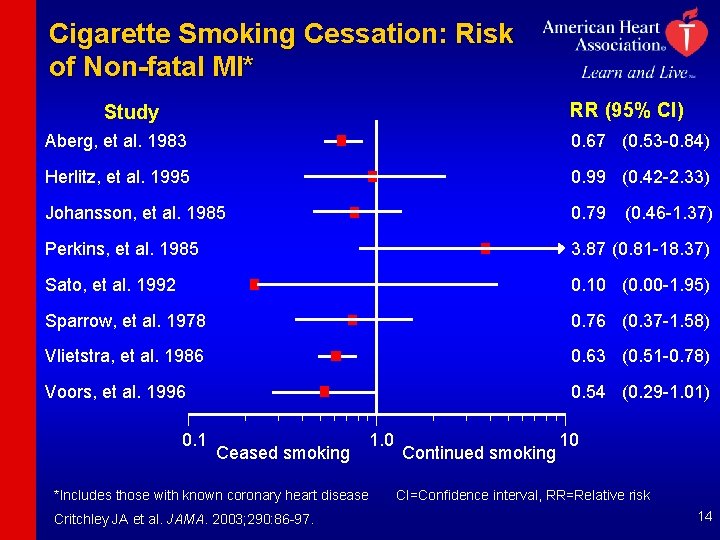
Cigarette Smoking Cessation: Risk of Non-fatal MI* RR (95% Cl) Study Aberg, et al. 1983 0. 67 (0. 53 -0. 84) Herlitz, et al. 1995 0. 99 (0. 42 -2. 33) Johansson, et al. 1985 0. 79 Perkins, et al. 1985 3. 87 (0. 81 -18. 37) Sato, et al. 1992 0. 10 (0. 00 -1. 95) Sparrow, et al. 1978 0. 76 (0. 37 -1. 58) Vlietstra, et al. 1986 0. 63 (0. 51 -0. 78) Voors, et al. 1996 0. 54 (0. 29 -1. 01) 0. 1 Ceased smoking 1. 0 *Includes those with known coronary heart disease Critchley JA et al. JAMA. 2003; 290: 86 -97. Continued smoking (0. 46 -1. 37) 10 CI=Confidence interval, RR=Relative risk 14
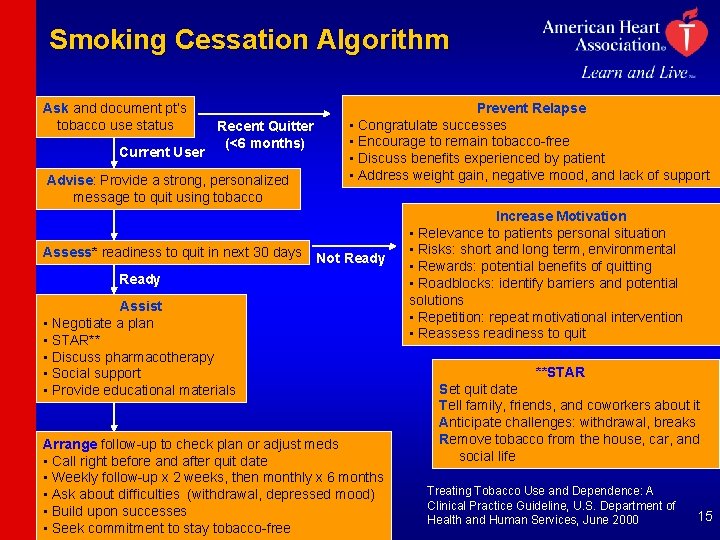
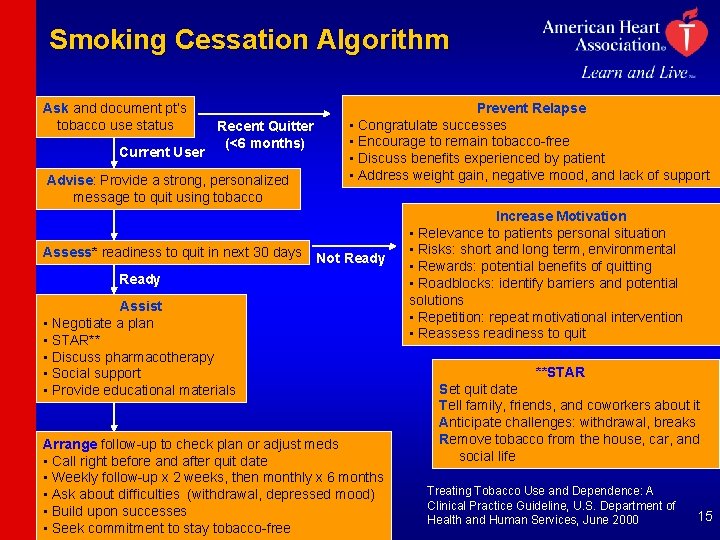
Smoking Cessation Algorithm Ask and document pt’s tobacco use status Current User Recent Quitter (<6 months) Advise: Provide a strong, personalized message to quit using tobacco Assess* readiness to quit in next 30 days Prevent Relapse • Congratulate successes • Encourage to remain tobacco-free • Discuss benefits experienced by patient • Address weight gain, negative mood, and lack of support Not Ready Assist • Negotiate a plan • STAR** • Discuss pharmacotherapy • Social support • Provide educational materials Arrange follow-up to check plan or adjust meds • Call right before and after quit date • Weekly follow-up x 2 weeks, then monthly x 6 months • Ask about difficulties (withdrawal, depressed mood) • Build upon successes • Seek commitment to stay tobacco-free Increase Motivation • Relevance to patients personal situation • Risks: short and long term, environmental • Rewards: potential benefits of quitting • Roadblocks: identify barriers and potential solutions • Repetition: repeat motivational intervention • Reassess readiness to quit **STAR Set quit date Tell family, friends, and coworkers about it Anticipate challenges: withdrawal, breaks Remove tobacco from the house, car, and social life Treating Tobacco Use and Dependence: A Clinical Practice Guideline, U. S. Department of Health and Human Services, June 2000 15
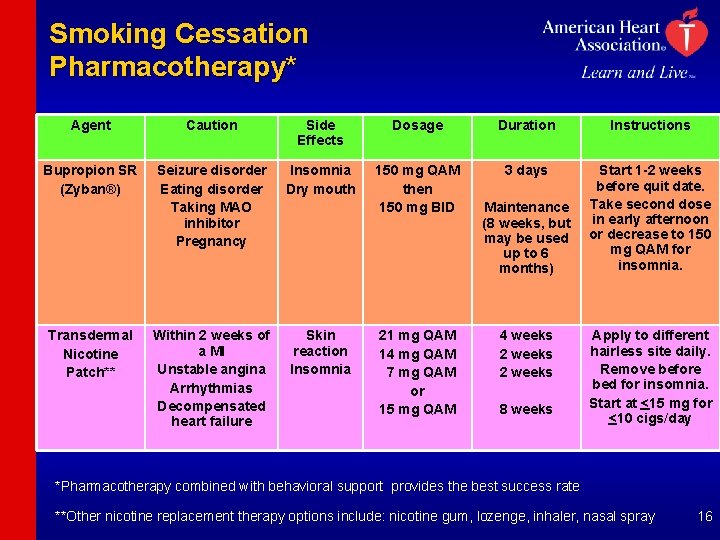
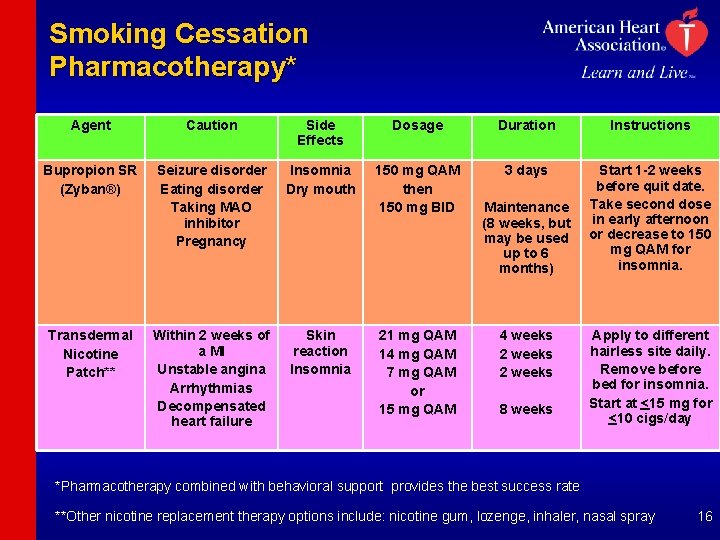
Smoking Cessation Pharmacotherapy* Agent Caution Side Effects Dosage Duration Instructions Bupropion SR (Zyban®) Seizure disorder Eating disorder Taking MAO inhibitor Pregnancy Insomnia Dry mouth 150 mg QAM then 150 mg BID 3 days Start 1 -2 weeks before quit date. Take second dose in early afternoon or decrease to 150 mg QAM for insomnia. Within 2 weeks of a MI Unstable angina Arrhythmias Decompensated heart failure Skin reaction Insomnia Transdermal Nicotine Patch** 21 mg QAM 14 mg QAM 7 mg QAM or 15 mg QAM Maintenance (8 weeks, but may be used up to 6 months) 4 weeks 2 weeks 8 weeks Apply to different hairless site daily. Remove before bed for insomnia. Start at <15 mg for <10 cigs/day *Pharmacotherapy combined with behavioral support provides the best success rate **Other nicotine replacement therapy options include: nicotine gum, lozenge, inhaler, nasal spray 16
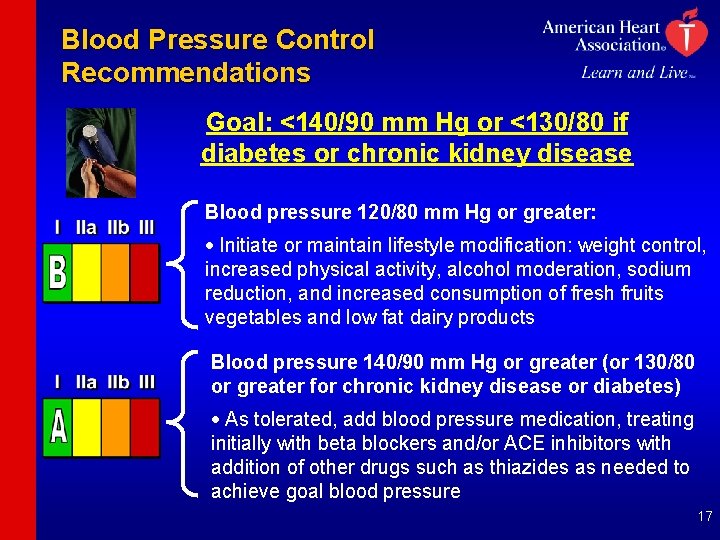
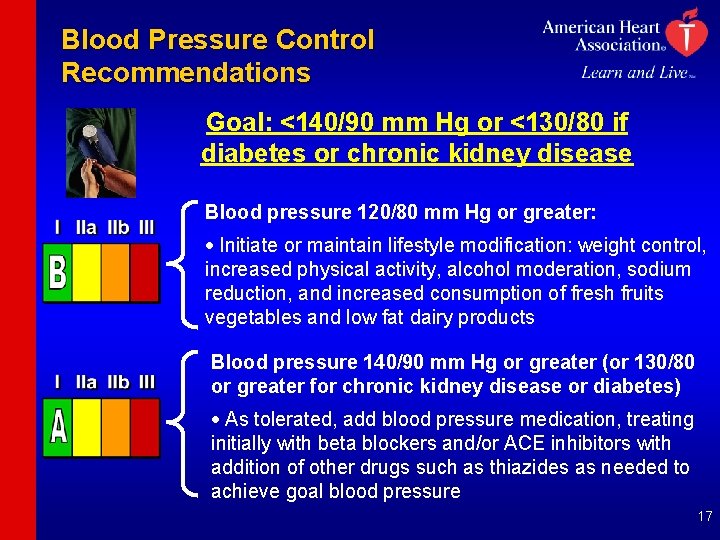
Blood Pressure Control Recommendations Goal: <140/90 mm Hg or <130/80 if diabetes or chronic kidney disease Blood pressure 120/80 mm Hg or greater: · Initiate or maintain lifestyle modification: weight control, increased physical activity, alcohol moderation, sodium reduction, and increased consumption of fresh fruits vegetables and low fat dairy products Blood pressure 140/90 mm Hg or greater (or 130/80 or greater for chronic kidney disease or diabetes) · As tolerated, add blood pressure medication, treating initially with beta blockers and/or ACE inhibitors with addition of other drugs such as thiazides as needed to achieve goal blood pressure 17
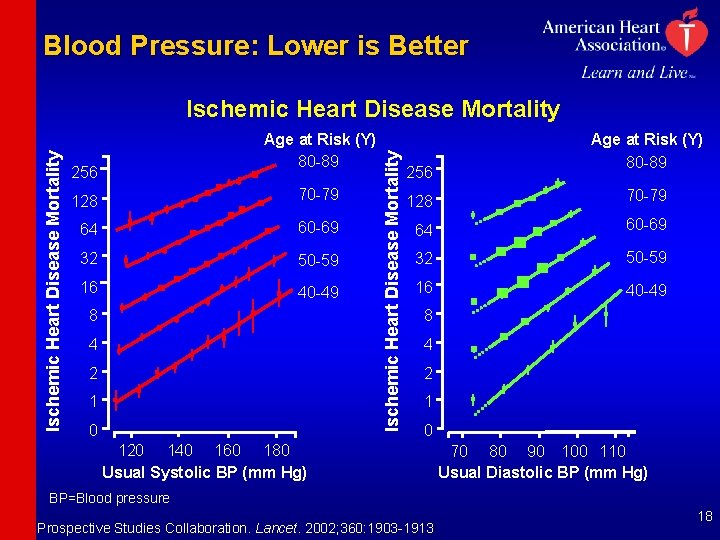
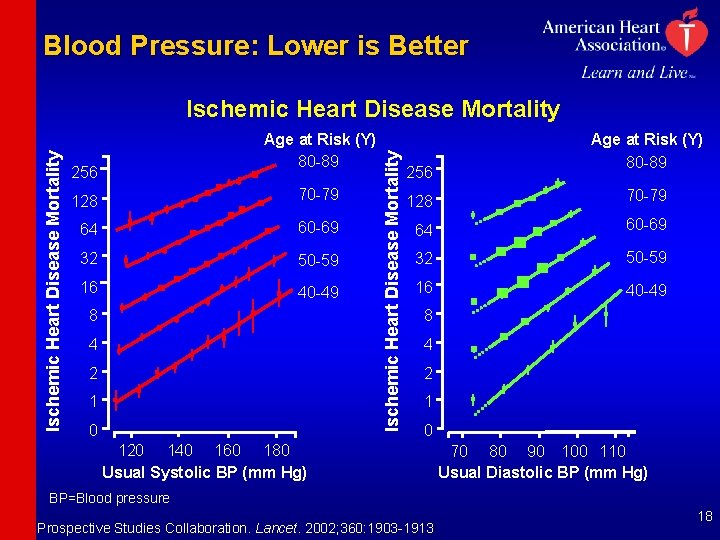
Blood Pressure: Lower is Better Age at Risk (Y) 80 -89 256 128 70 -79 64 60 -69 32 50 -59 16 40 -49 8 4 2 1 0 Ischemic Heart Disease Mortality 256 Age at Risk (Y) 80 -89 128 70 -79 64 60 -69 32 50 -59 16 40 -49 8 4 2 1 0 120 140 160 180 Usual Systolic BP (mm Hg) 70 80 90 100 110 Usual Diastolic BP (mm Hg) BP=Blood pressure Prospective Studies Collaboration. Lancet. 2002; 360: 1903 -1913 18
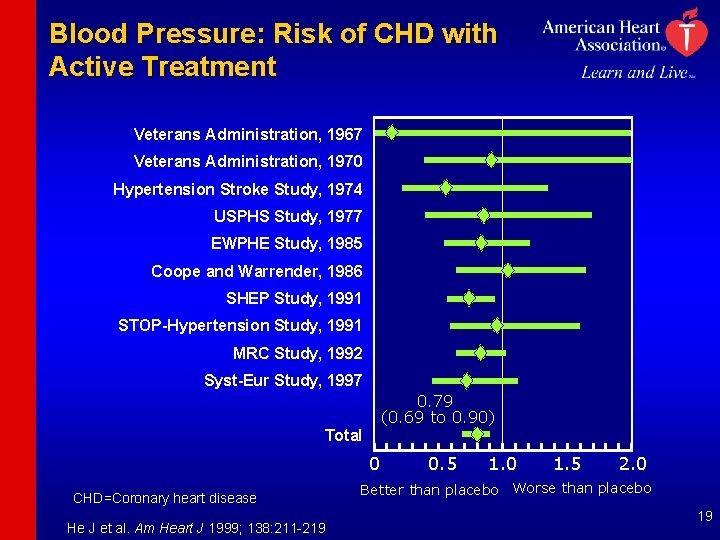
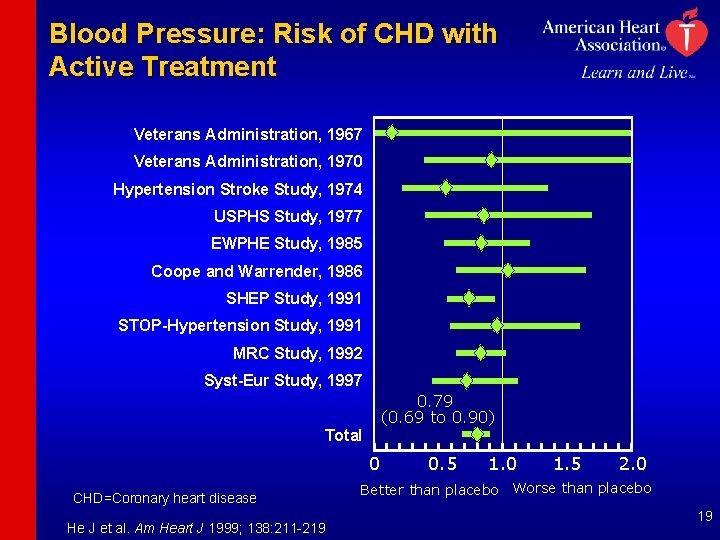
Blood Pressure: Risk of CHD with Active Treatment Veterans Administration, 1967 Veterans Administration, 1970 Hypertension Stroke Study, 1974 USPHS Study, 1977 EWPHE Study, 1985 Coope and Warrender, 1986 SHEP Study, 1991 STOP-Hypertension Study, 1991 MRC Study, 1992 Syst-Eur Study, 1997 0. 79 (0. 69 to 0. 90) Total 0 CHD=Coronary heart disease He J et al. Am Heart J 1999; 138: 211 -219 0. 5 1. 0 1. 5 2. 0 Better than placebo Worse than placebo 19
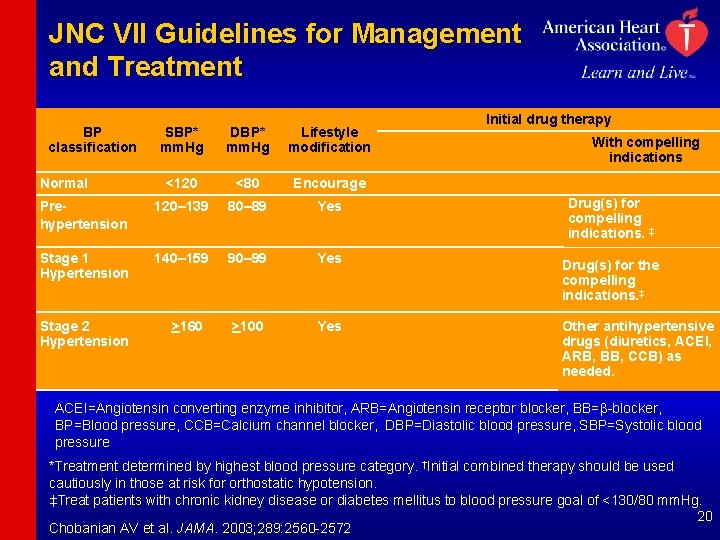
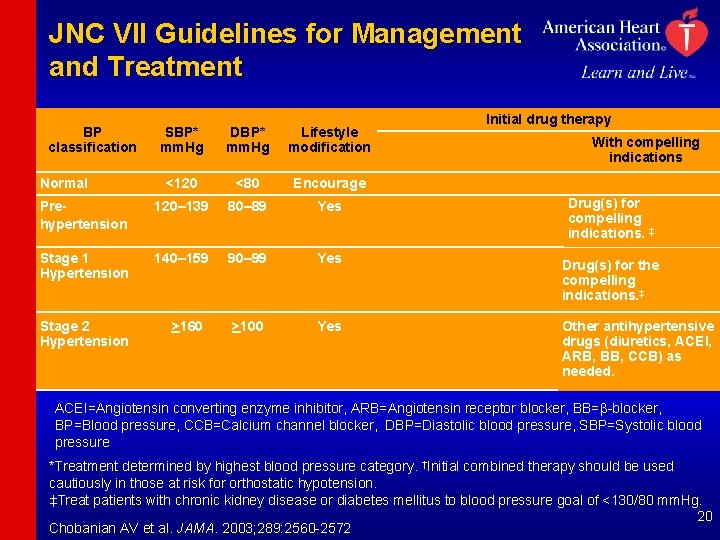
JNC VII Guidelines for Management and Treatment BP classification SBP* mm. Hg DBP* mm. Hg Lifestyle modification <120 <80 Encourage Prehypertension 120– 139 80– 89 Yes Stage 1 Hypertension 140– 159 90– 99 Yes >100 Yes Normal Stage 2 Hypertension >160 Initial drug therapy With compelling indications Drug(s) for compelling indications. ‡ Drug(s) for the compelling indications. ‡ Other antihypertensive drugs (diuretics, ACEI, ARB, BB, CCB) as needed. ACEI=Angiotensin converting enzyme inhibitor, ARB=Angiotensin receptor blocker, BB=b-blocker, BP=Blood pressure, CCB=Calcium channel blocker, DBP=Diastolic blood pressure, SBP=Systolic blood pressure *Treatment determined by highest blood pressure category. †Initial combined therapy should be used cautiously in those at risk for orthostatic hypotension. ‡Treat patients with chronic kidney disease or diabetes mellitus to blood pressure goal of <130/80 mm. Hg. 20 Chobanian AV et al. JAMA. 2003; 289: 2560 -2572
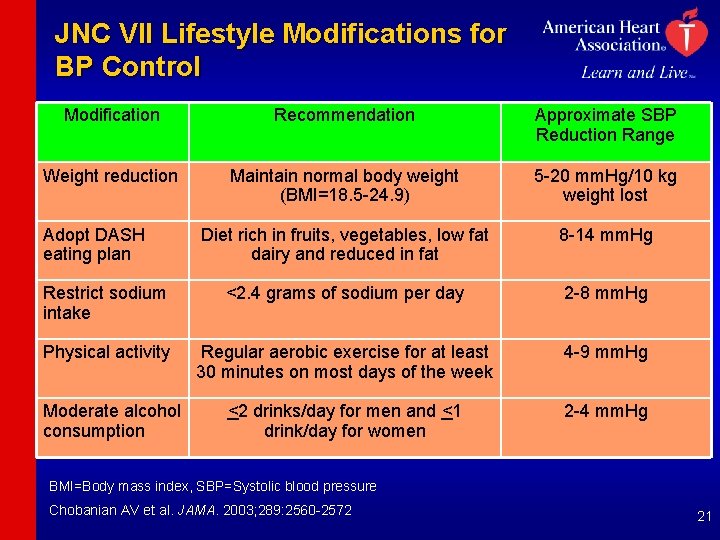
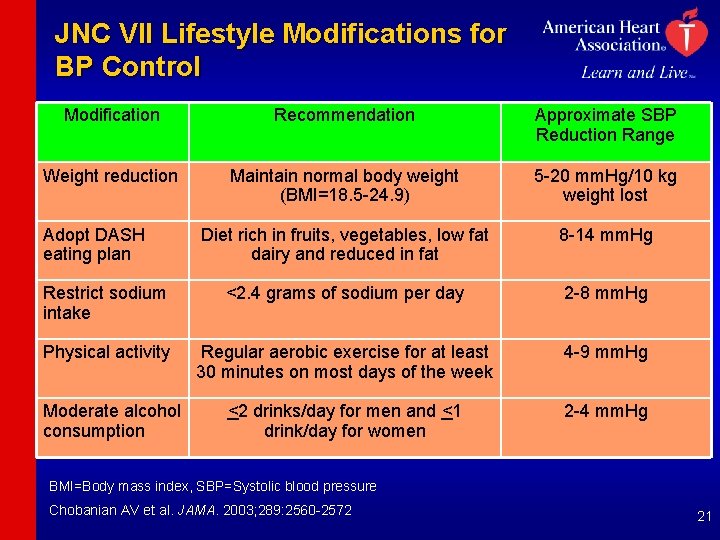
JNC VII Lifestyle Modifications for BP Control Modification Recommendation Approximate SBP Reduction Range Weight reduction Maintain normal body weight (BMI=18. 5 -24. 9) 5 -20 mm. Hg/10 kg weight lost Diet rich in fruits, vegetables, low fat dairy and reduced in fat 8 -14 mm. Hg Restrict sodium intake <2. 4 grams of sodium per day 2 -8 mm. Hg Physical activity Regular aerobic exercise for at least 30 minutes on most days of the week 4 -9 mm. Hg <2 drinks/day for men and <1 drink/day for women 2 -4 mm. Hg Adopt DASH eating plan Moderate alcohol consumption BMI=Body mass index, SBP=Systolic blood pressure Chobanian AV et al. JAMA. 2003; 289: 2560 -2572 21
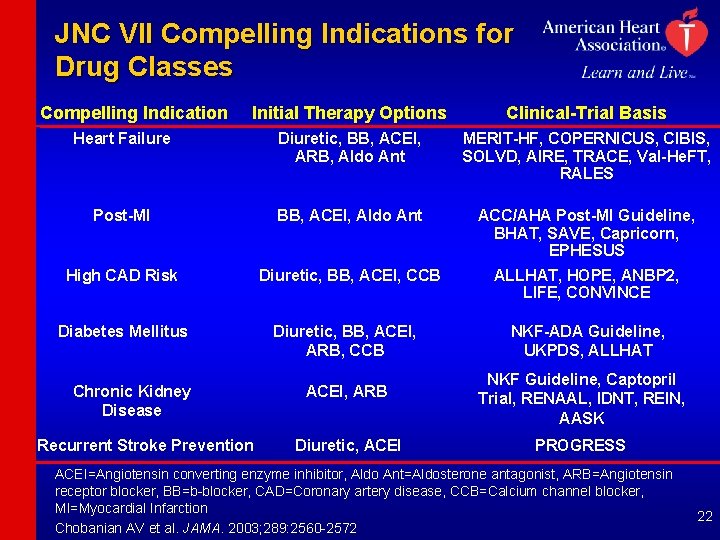
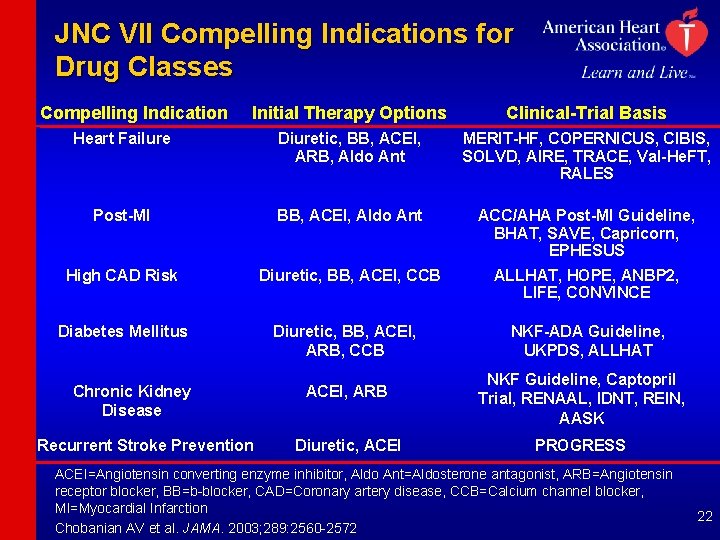
JNC VII Compelling Indications for Drug Classes Compelling Indication Initial Therapy Options Clinical-Trial Basis Heart Failure Diuretic, BB, ACEI, ARB, Aldo Ant MERIT-HF, COPERNICUS, CIBIS, SOLVD, AIRE, TRACE, Val-He. FT, RALES Post-MI BB, ACEI, Aldo Ant ACC/AHA Post-MI Guideline, BHAT, SAVE, Capricorn, EPHESUS High CAD Risk Diuretic, BB, ACEI, CCB ALLHAT, HOPE, ANBP 2, LIFE, CONVINCE Diabetes Mellitus Chronic Kidney Disease Recurrent Stroke Prevention Diuretic, BB, ACEI, ARB, CCB NKF-ADA Guideline, UKPDS, ALLHAT ACEI, ARB NKF Guideline, Captopril Trial, RENAAL, IDNT, REIN, AASK Diuretic, ACEI PROGRESS ACEI=Angiotensin converting enzyme inhibitor, Aldo Ant=Aldosterone antagonist, ARB=Angiotensin receptor blocker, BB=b-blocker, CAD=Coronary artery disease, CCB=Calcium channel blocker, MI=Myocardial Infarction Chobanian AV et al. JAMA. 2003; 289: 2560 -2572 22
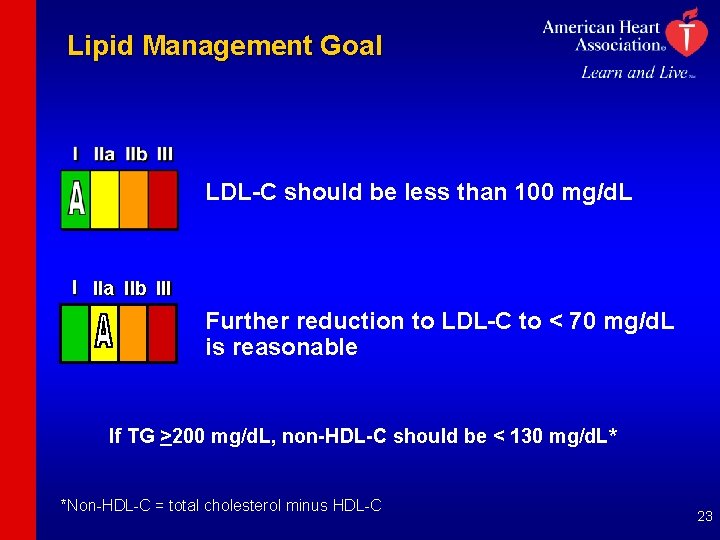
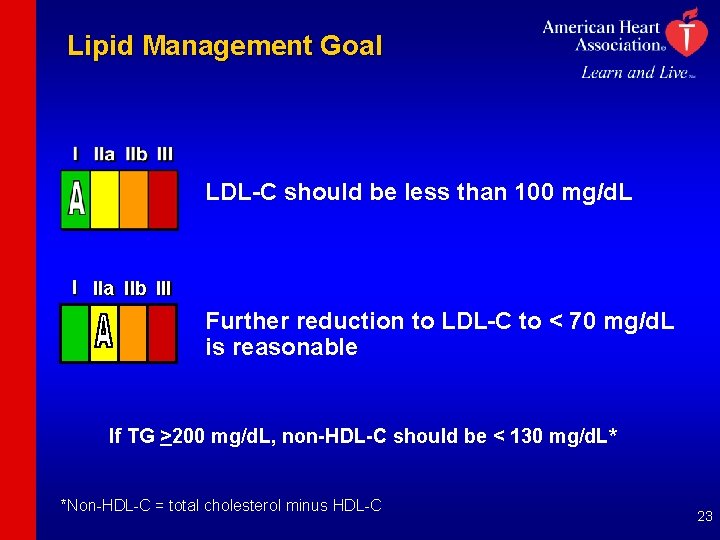
Lipid Management Goal LDL-C should be less than 100 mg/d. L I IIa IIb III Further reduction to LDL-C to < 70 mg/d. L is reasonable If TG >200 mg/d. L, non-HDL-C should be < 130 mg/d. L* *Non-HDL-C = total cholesterol minus HDL-C 23
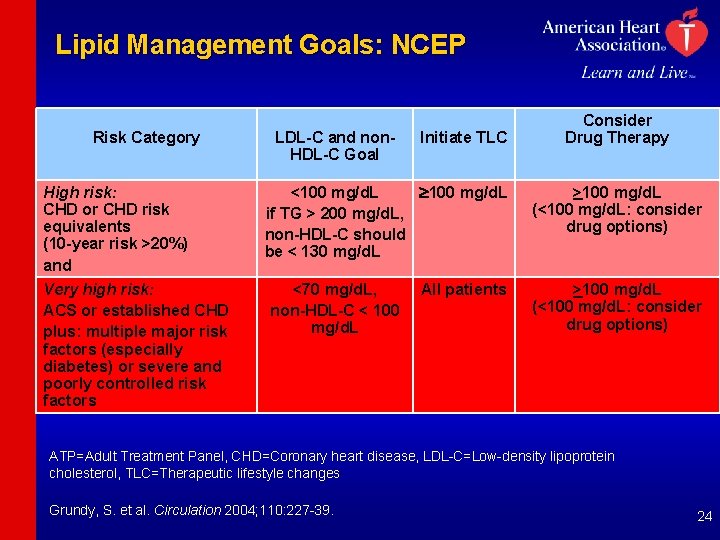
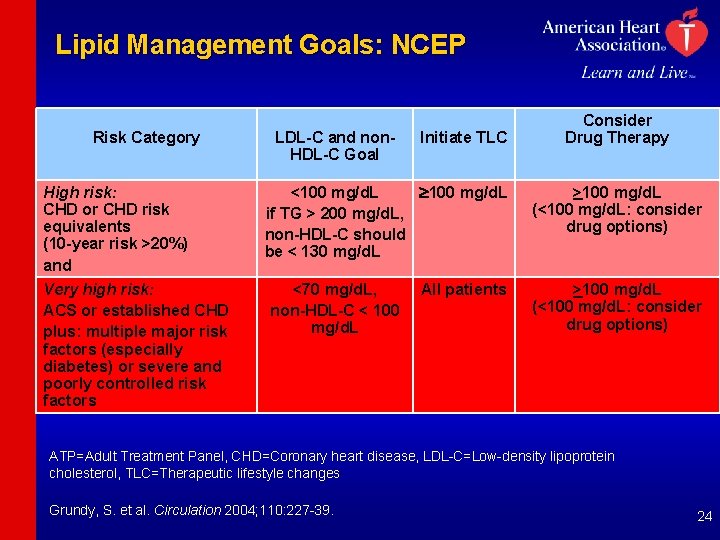
Lipid Management Goals: NCEP Risk Category High risk: CHD or CHD risk equivalents (10 -year risk >20%) and Very high risk: ACS or established CHD plus: multiple major risk factors (especially diabetes) or severe and poorly controlled risk factors LDL-C and non. HDL-C Goal Initiate TLC <100 mg/d. L if TG > 200 mg/d. L, non-HDL-C should be < 130 mg/d. L <70 mg/d. L, non-HDL-C < 100 mg/d. L All patients Consider Drug Therapy >100 mg/d. L (<100 mg/d. L: consider drug options) ATP=Adult Treatment Panel, CHD=Coronary heart disease, LDL-C=Low-density lipoprotein cholesterol, TLC=Therapeutic lifestyle changes Grundy, S. et al. Circulation 2004; 110: 227 -39. 24
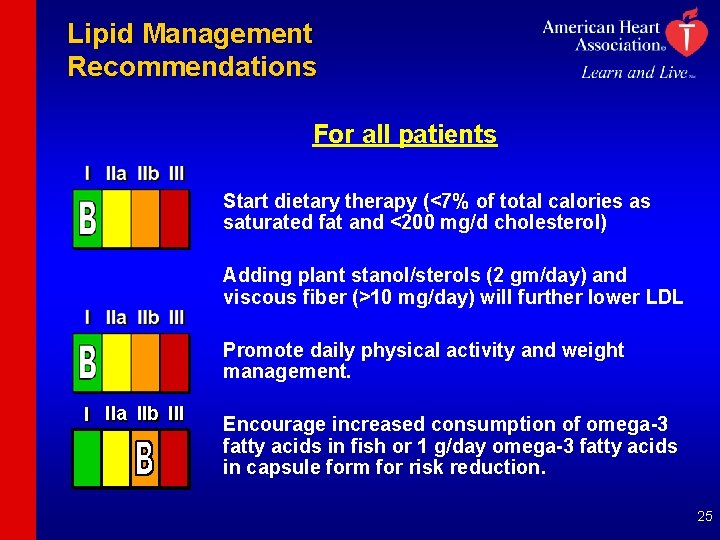
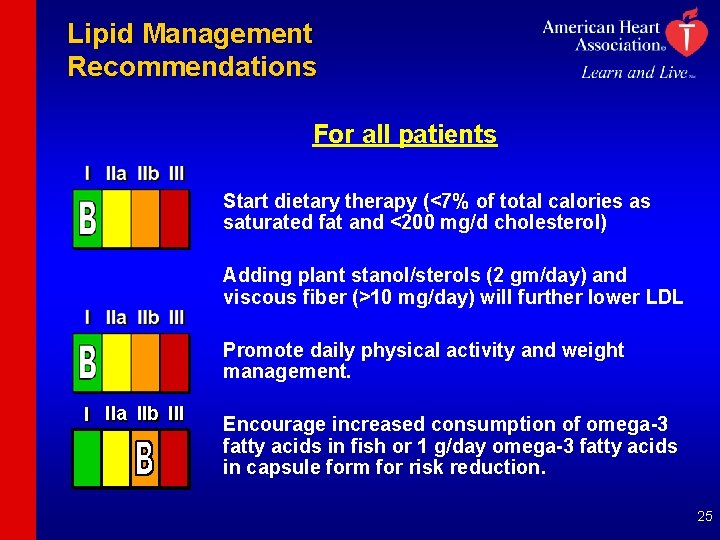
Lipid Management Recommendations For all patients Start dietary therapy (<7% of total calories as saturated fat and <200 mg/d cholesterol) Adding plant stanol/sterols (2 gm/day) and viscous fiber (>10 mg/day) will further lower LDL Promote daily physical activity and weight management. I IIa IIb III Encourage increased consumption of omega-3 fatty acids in fish or 1 g/day omega-3 fatty acids in capsule form for risk reduction. 25
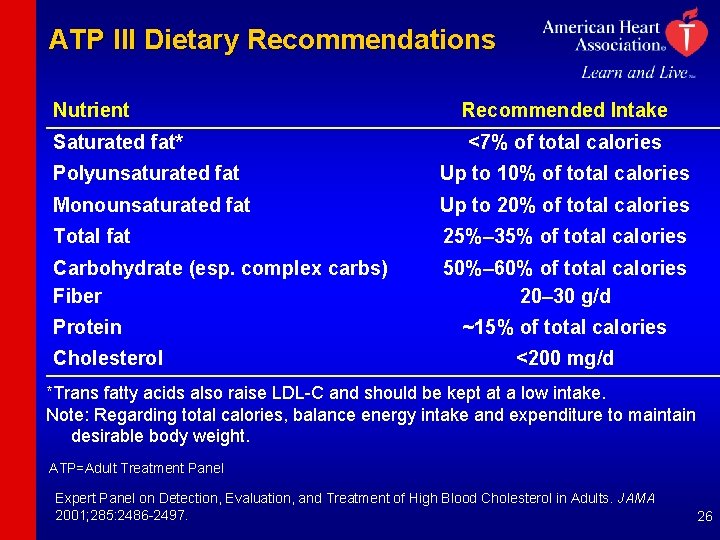
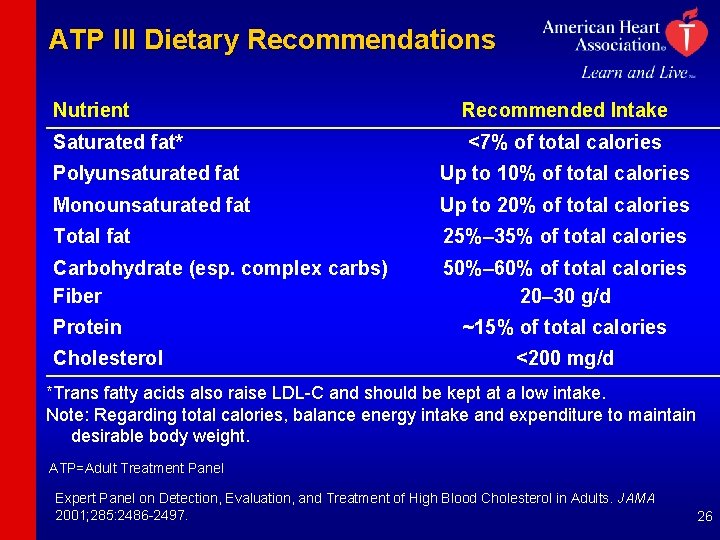
ATP III Dietary Recommendations Nutrient Saturated fat* Recommended Intake <7% of total calories Polyunsaturated fat Up to 10% of total calories Monounsaturated fat Up to 20% of total calories Total fat 25%– 35% of total calories Carbohydrate (esp. complex carbs) Fiber 50%– 60% of total calories 20– 30 g/d Protein Cholesterol ~15% of total calories <200 mg/d *Trans fatty acids also raise LDL-C and should be kept at a low intake. Note: Regarding total calories, balance energy intake and expenditure to maintain desirable body weight. ATP=Adult Treatment Panel Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA 2001; 285: 2486 -2497. 26
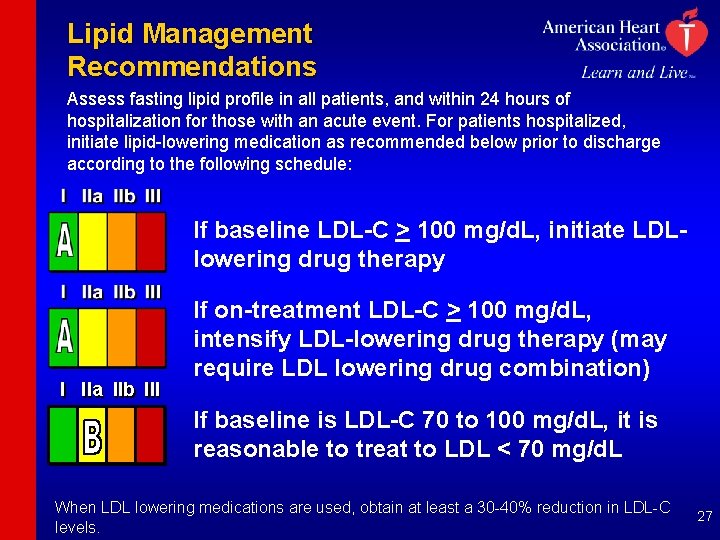
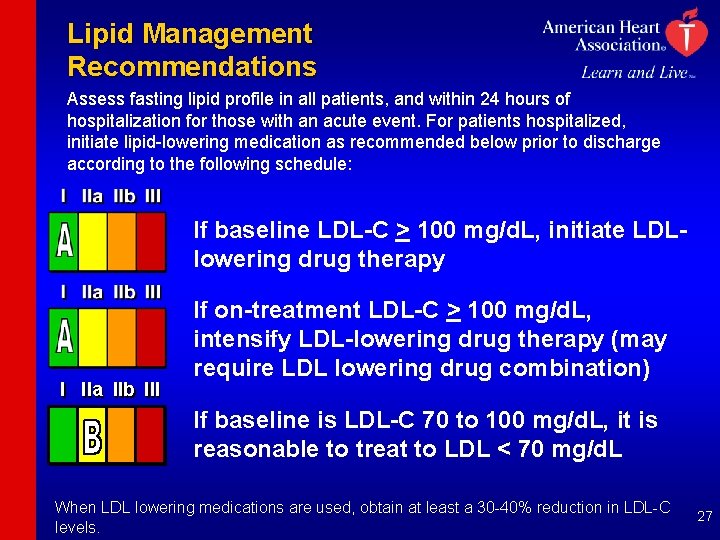
Lipid Management Recommendations Assess fasting lipid profile in all patients, and within 24 hours of hospitalization for those with an acute event. For patients hospitalized, initiate lipid-lowering medication as recommended below prior to discharge according to the following schedule: If baseline LDL-C > 100 mg/d. L, initiate LDLlowering drug therapy I IIa IIb III If on-treatment LDL-C > 100 mg/d. L, intensify LDL-lowering drug therapy (may require LDL lowering drug combination) If baseline is LDL-C 70 to 100 mg/d. L, it is reasonable to treat to LDL < 70 mg/d. L When LDL lowering medications are used, obtain at least a 30 -40% reduction in LDL-C levels. 27
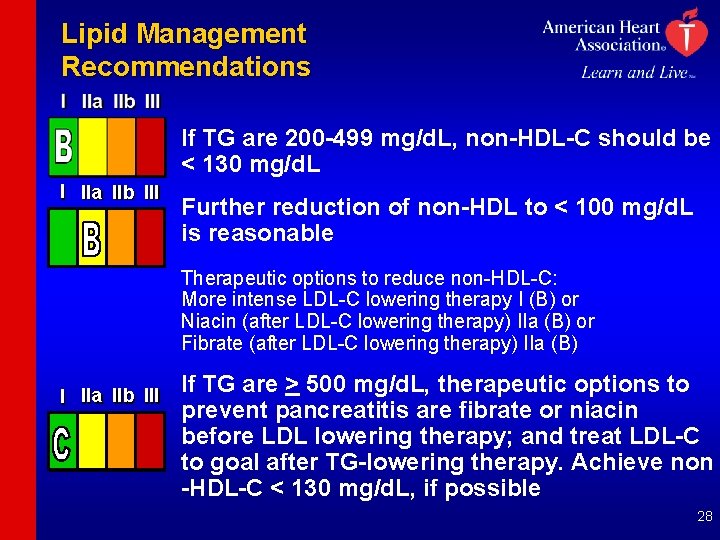
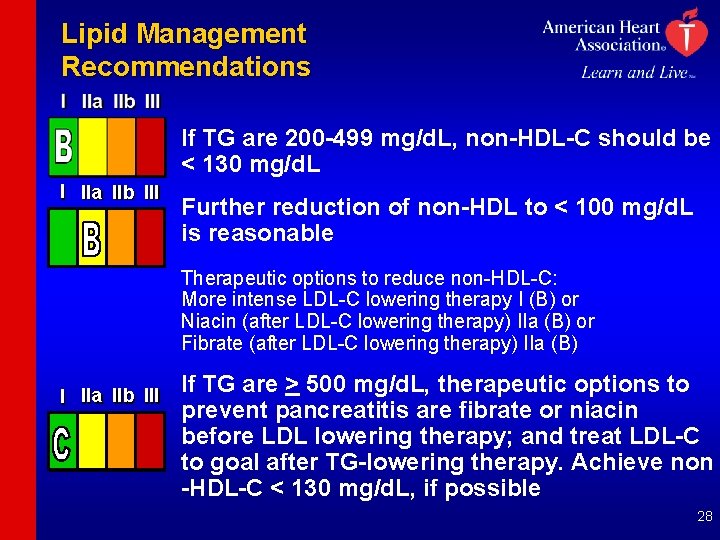
Lipid Management Recommendations If TG are 200 -499 mg/d. L, non-HDL-C should be < 130 mg/d. L I IIa IIb III Further reduction of non-HDL to < 100 mg/d. L is reasonable Therapeutic options to reduce non-HDL-C: More intense LDL-C lowering therapy I (B) or Niacin (after LDL-C lowering therapy) IIa (B) or Fibrate (after LDL-C lowering therapy) IIa (B) I IIa IIb III If TG are > 500 mg/d. L, therapeutic options to prevent pancreatitis are fibrate or niacin before LDL lowering therapy; and treat LDL-C to goal after TG-lowering therapy. Achieve non -HDL-C < 130 mg/d. L, if possible 28
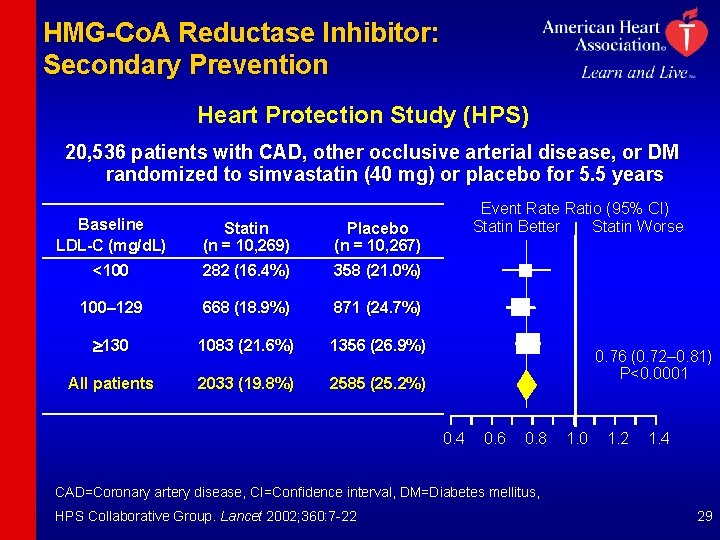
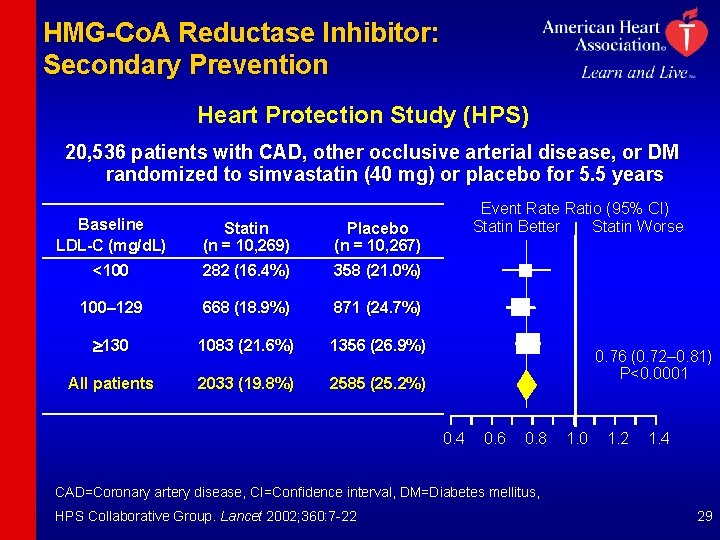
HMG-Co. A Reductase Inhibitor: Secondary Prevention Heart Protection Study (HPS) 20, 536 patients with CAD, other occlusive arterial disease, or DM randomized to simvastatin (40 mg) or placebo for 5. 5 years Baseline LDL-C (mg/d. L) <100 Statin (n = 10, 269) 282 (16. 4%) Placebo (n = 10, 267) 358 (21. 0%) 100– 129 668 (18. 9%) 871 (24. 7%) 130 1083 (21. 6%) 1356 (26. 9%) All patients 2033 (19. 8%) 2585 (25. 2%) Event Rate Ratio (95% CI) Statin Better Statin Worse 0. 76 (0. 72– 0. 81) P<0. 0001 0. 4 0. 6 0. 8 1. 0 1. 2 1. 4 CAD=Coronary artery disease, CI=Confidence interval, DM=Diabetes mellitus, HPS Collaborative Group. Lancet 2002; 360: 7 -22 29
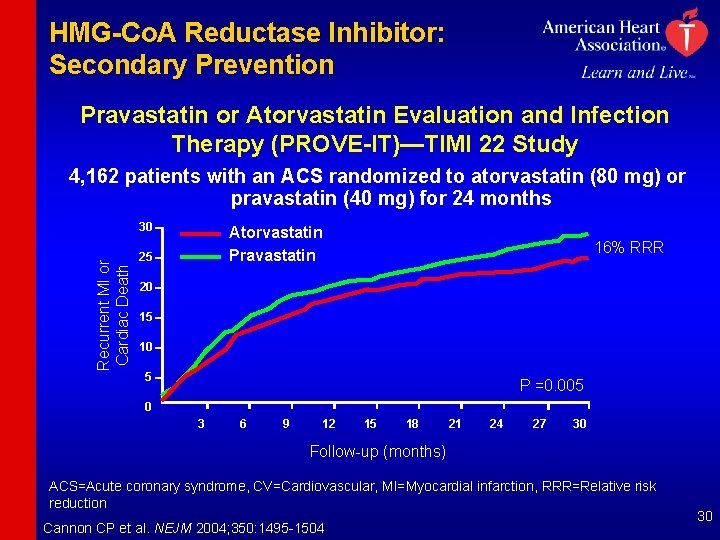
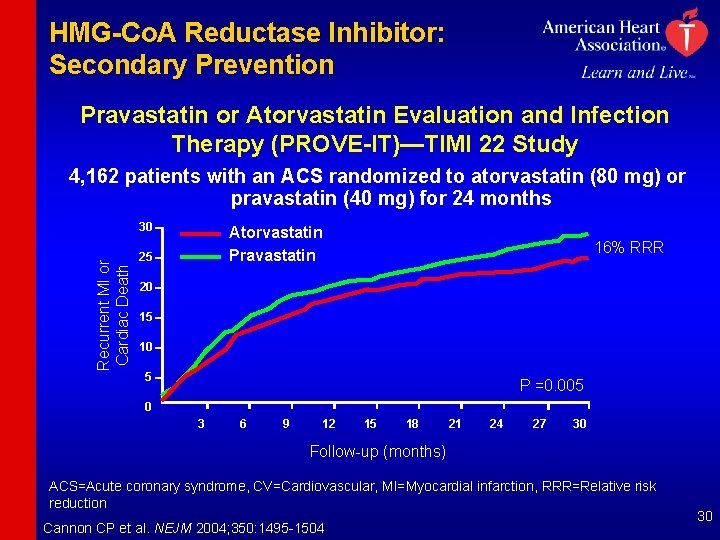
HMG-Co. A Reductase Inhibitor: Secondary Prevention Pravastatin or Atorvastatin Evaluation and Infection Therapy (PROVE-IT)—TIMI 22 Study 4, 162 patients with an ACS randomized to atorvastatin (80 mg) or pravastatin (40 mg) for 24 months Recurrent MI or Cardiac Death 30 Atorvastatin Pravastatin 25 16% RRR 20 15 10 5 P =0. 005 0 3 6 9 12 15 18 21 24 27 30 Follow-up (months) ACS=Acute coronary syndrome, CV=Cardiovascular, MI=Myocardial infarction, RRR=Relative risk reduction Cannon CP et al. NEJM 2004; 350: 1495 -1504 30
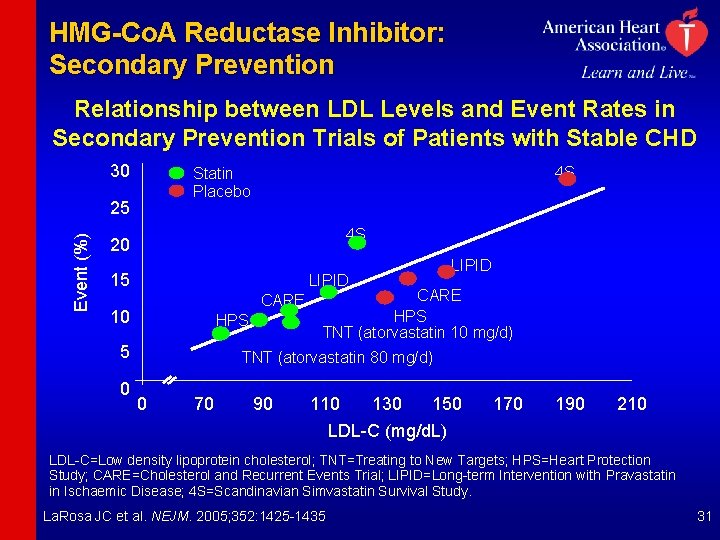
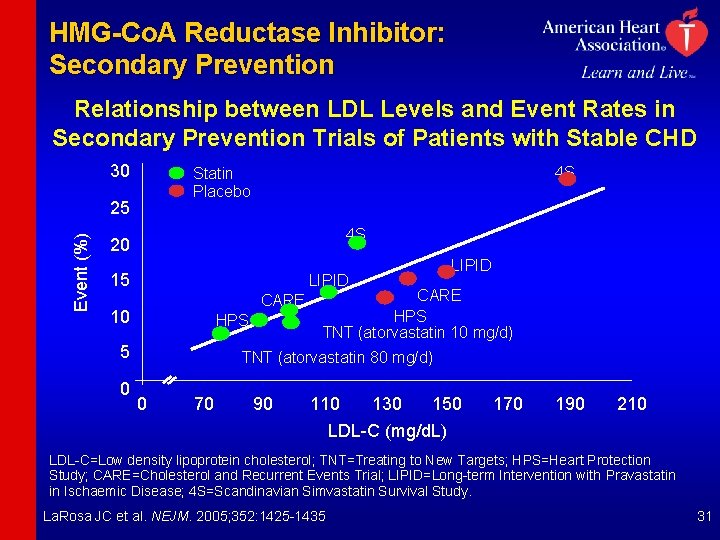
HMG-Co. A Reductase Inhibitor: Secondary Prevention Relationship between LDL Levels and Event Rates in Secondary Prevention Trials of Patients with Stable CHD 30 25 Event (%) 4 S Statin Placebo 4 S 20 15 LIPID CARE 10 HPS 5 0 LIPID CARE HPS TNT (atorvastatin 10 mg/d) TNT (atorvastatin 80 mg/d) 0 70 90 110 130 150 LDL-C (mg/d. L) 170 190 210 LDL-C=Low density lipoprotein cholesterol; TNT=Treating to New Targets; HPS=Heart Protection Study; CARE=Cholesterol and Recurrent Events Trial; LIPID=Long-term Intervention with Pravastatin in Ischaemic Disease; 4 S=Scandinavian Simvastatin Survival Study. La. Rosa JC et al. NEJM. 2005; 352: 1425 -1435 31
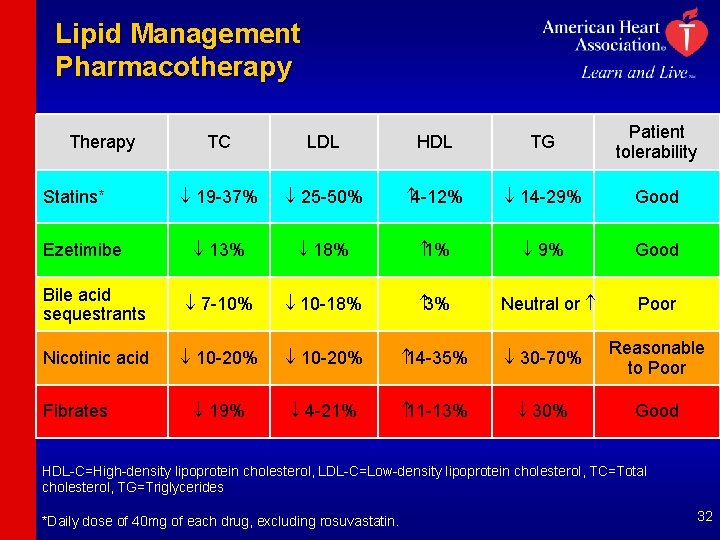
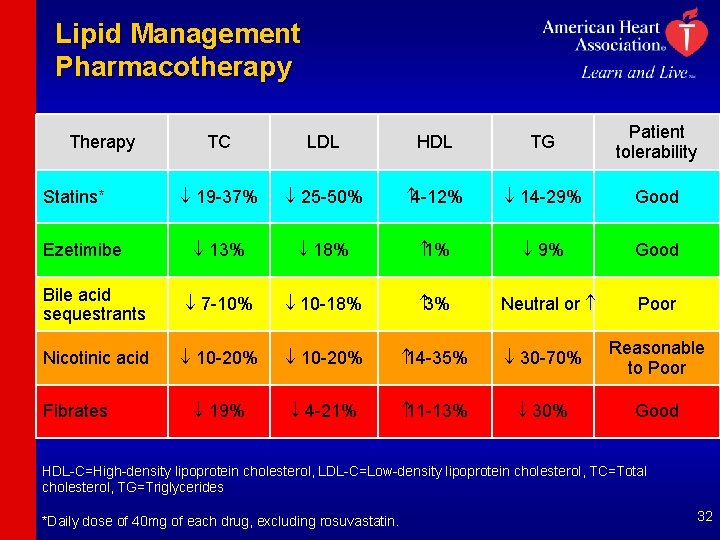
Lipid Management Pharmacotherapy TC LDL HDL TG Patient tolerability ¯ 19 -37% ¯ 25 -50% 4 -12% ¯ 14 -29% Good ¯ 13% ¯ 18% 1% ¯ 9% Good Bile acid sequestrants ¯ 7 -10% ¯ 10 -18% 3% Nicotinic acid ¯ 10 -20% 14 -35% ¯ 30 -70% Reasonable to Poor ¯ 19% ¯ 4 -21% 11 -13% ¯ 30% Good Therapy Statins* Ezetimibe Fibrates Neutral or Poor HDL-C=High-density lipoprotein cholesterol, LDL-C=Low-density lipoprotein cholesterol, TC=Total cholesterol, TG=Triglycerides *Daily dose of 40 mg of each drug, excluding rosuvastatin. 32
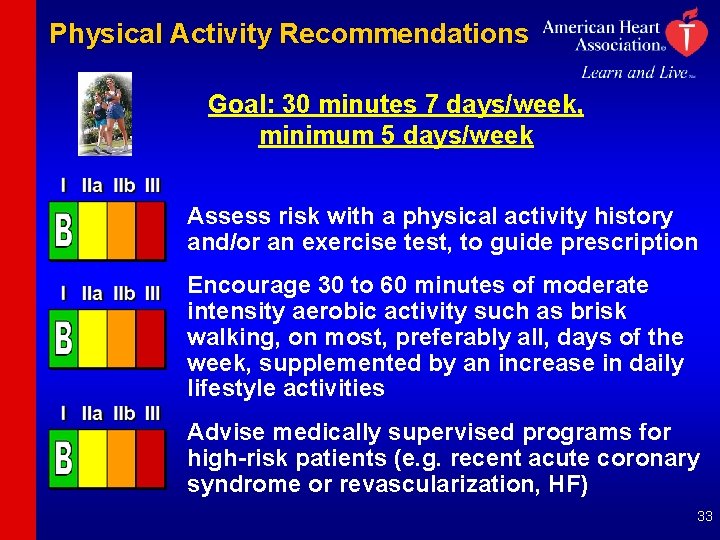
Physical Activity Recommendations Goal: 30 minutes 7 days/week, minimum 5 days/week Assess risk with a physical activity history and/or an exercise test, to guide prescription Encourage 30 to 60 minutes of moderate intensity aerobic activity such as brisk walking, on most, preferably all, days of the week, supplemented by an increase in daily lifestyle activities Advise medically supervised programs for high-risk patients (e. g. recent acute coronary syndrome or revascularization, HF) 33
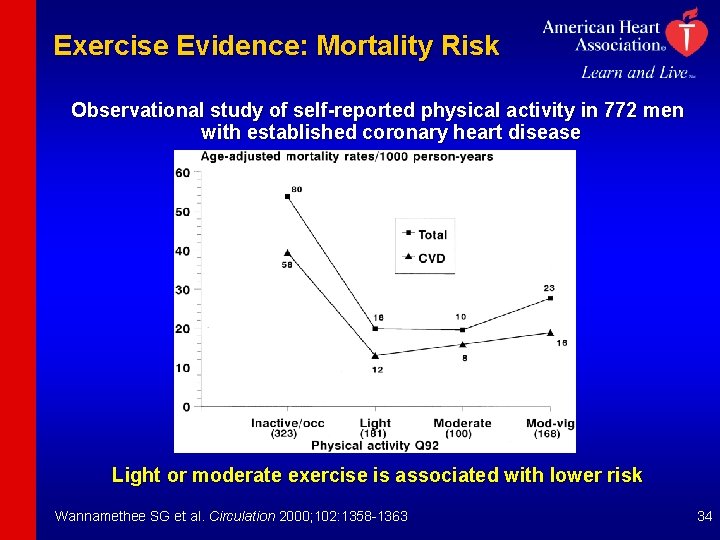
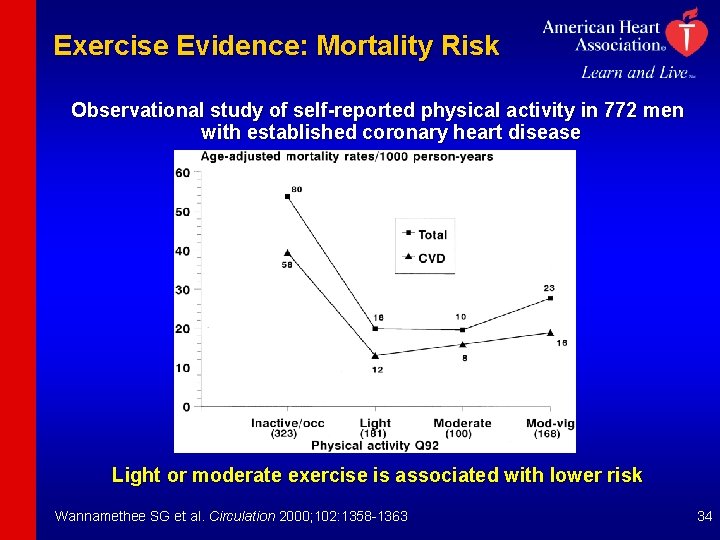
Exercise Evidence: Mortality Risk Observational study of self-reported physical activity in 772 men with established coronary heart disease Light or moderate exercise is associated with lower risk Wannamethee SG et al. Circulation 2000; 102: 1358 -1363 34
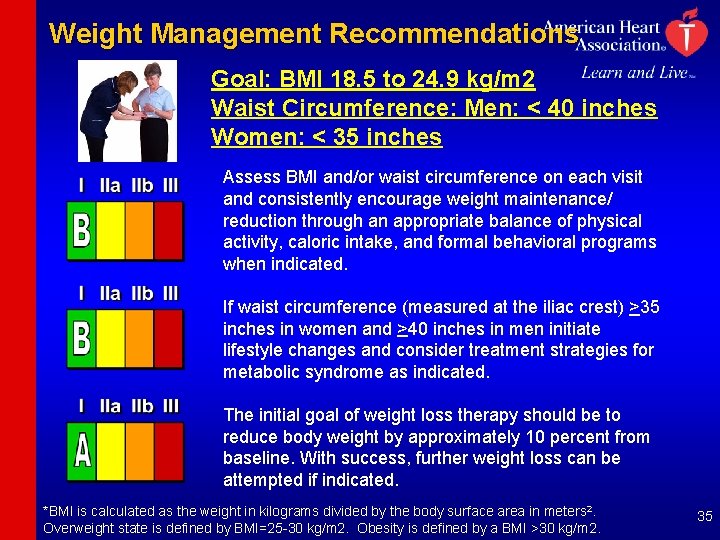
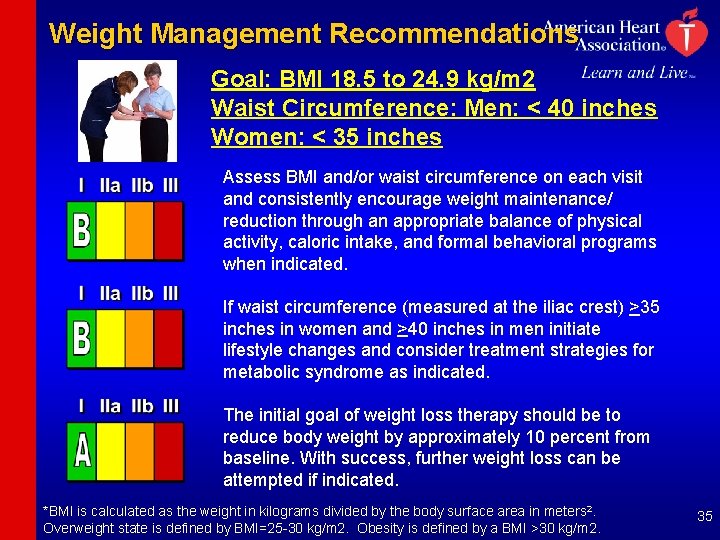
Weight Management Recommendations Goal: BMI 18. 5 to 24. 9 kg/m 2 Waist Circumference: Men: < 40 inches Women: < 35 inches Assess BMI and/or waist circumference on each visit and consistently encourage weight maintenance/ reduction through an appropriate balance of physical activity, caloric intake, and formal behavioral programs when indicated. If waist circumference (measured at the iliac crest) >35 inches in women and >40 inches in men initiate lifestyle changes and consider treatment strategies for metabolic syndrome as indicated. The initial goal of weight loss therapy should be to reduce body weight by approximately 10 percent from baseline. With success, further weight loss can be attempted if indicated. *BMI is calculated as the weight in kilograms divided by the body surface area in meters 2. Overweight state is defined by BMI=25 -30 kg/m 2. Obesity is defined by a BMI >30 kg/m 2. 35
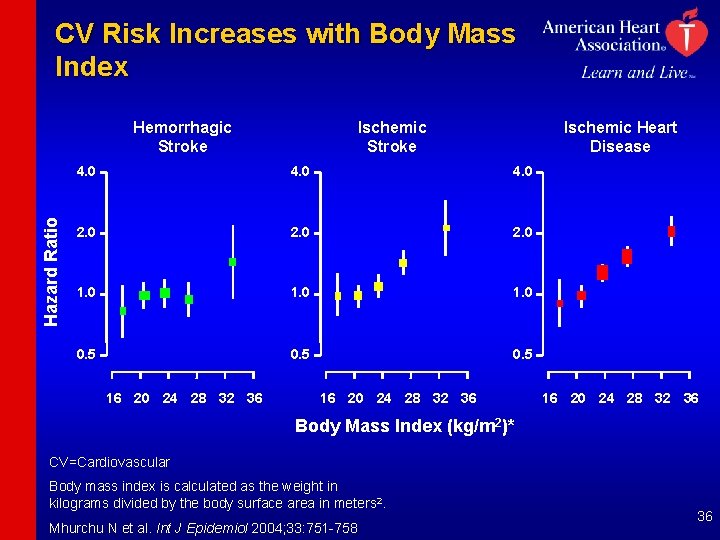
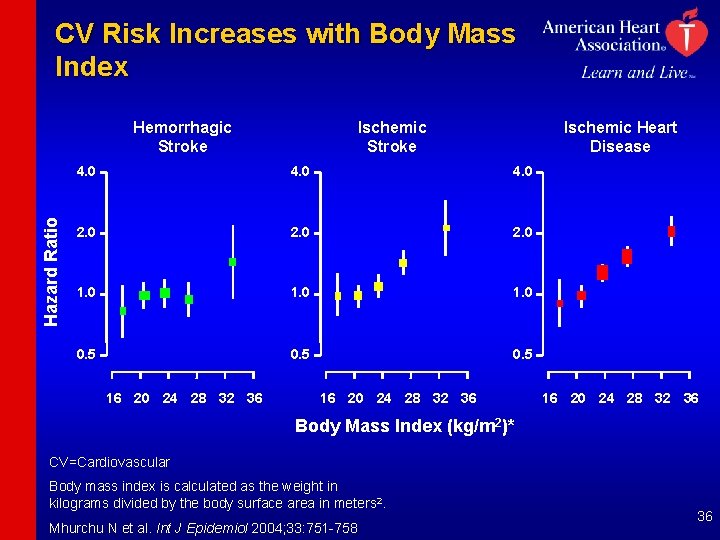
CV Risk Increases with Body Mass Index Hazard Ratio Hemorrhagic Stroke Ischemic Heart Disease 4. 0 2. 0 1. 0 0. 5 16 20 24 28 32 36 Body Mass Index (kg/m 2)* CV=Cardiovascular Body mass index is calculated as the weight in kilograms divided by the body surface area in meters 2. Mhurchu N et al. Int J Epidemiol 2004; 33: 751 -758 36
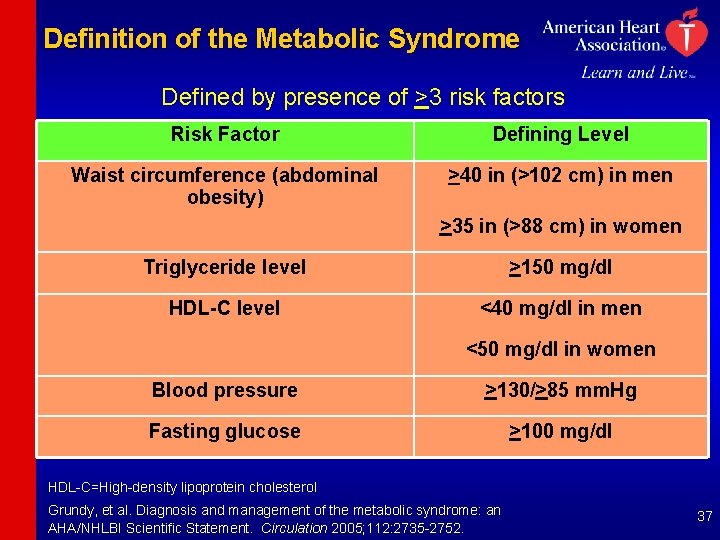
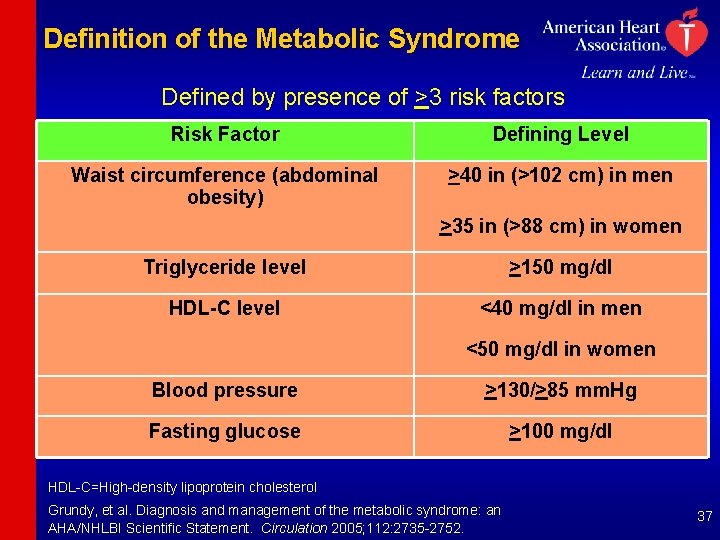
Definition of the Metabolic Syndrome Defined by presence of >3 risk factors Risk Factor Defining Level Waist circumference (abdominal obesity) >40 in (>102 cm) in men >35 in (>88 cm) in women Triglyceride level >150 mg/dl HDL-C level <40 mg/dl in men <50 mg/dl in women Blood pressure >130/>85 mm. Hg Fasting glucose >100 mg/dl HDL-C=High-density lipoprotein cholesterol Grundy, et al. Diagnosis and management of the metabolic syndrome: an AHA/NHLBI Scientific Statement. Circulation 2005; 112: 2735 -2752. 37
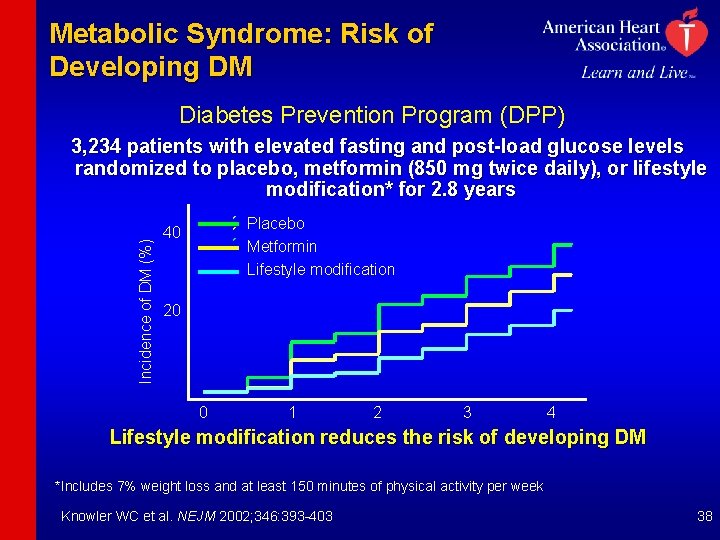
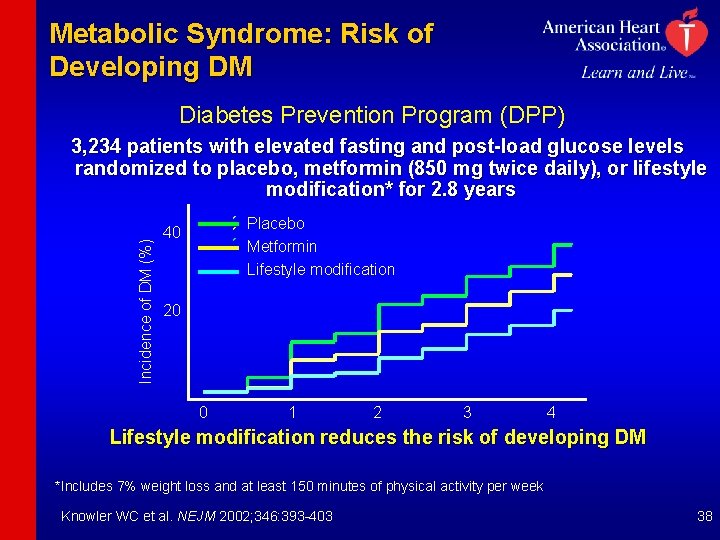
Metabolic Syndrome: Risk of Developing DM Diabetes Prevention Program (DPP) Incidence of DM (%) 3, 234 patients with elevated fasting and post-load glucose levels randomized to placebo, metformin (850 mg twice daily), or lifestyle modification* for 2. 8 years Placebo Metformin Lifestyle modification 40 20 0 1 2 3 4 Lifestyle modification reduces the risk of developing DM *Includes 7% weight loss and at least 150 minutes of physical activity per week Knowler WC et al. NEJM 2002; 346: 393 -403 38
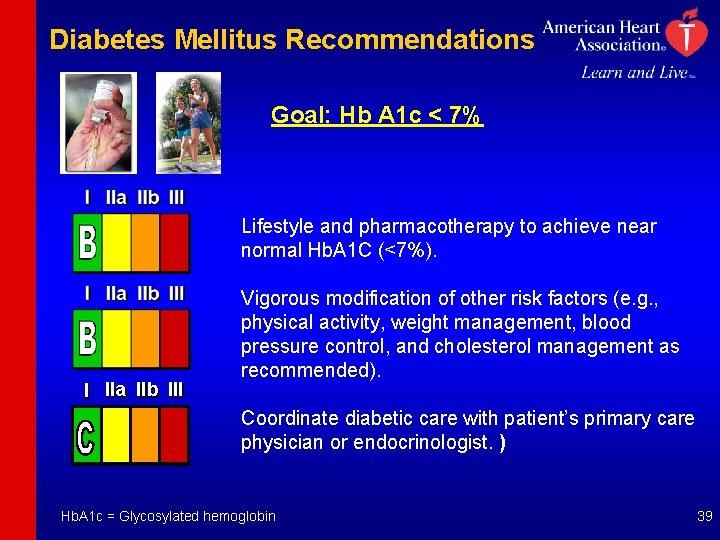
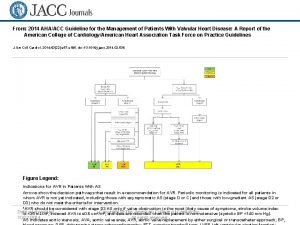
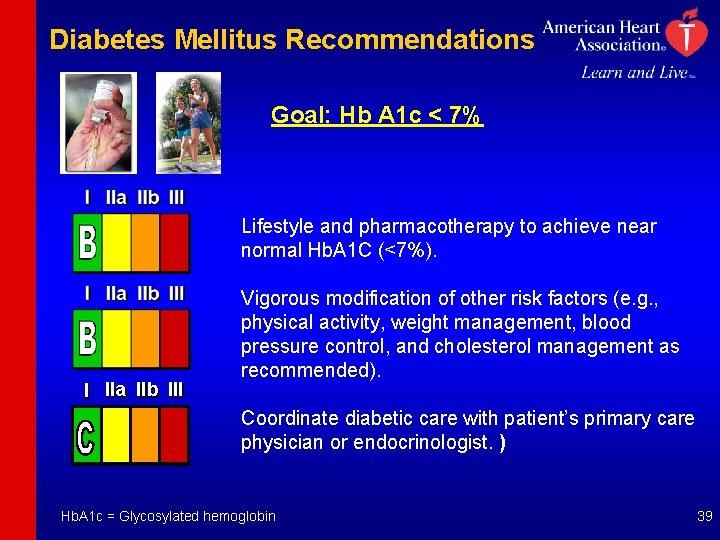
Diabetes Mellitus Recommendations Goal: Hb A 1 c < 7% Lifestyle and pharmacotherapy to achieve near normal Hb. A 1 C (<7%). I IIa IIb III Vigorous modification of other risk factors (e. g. , physical activity, weight management, blood pressure control, and cholesterol management as recommended). Coordinate diabetic care with patient’s primary care physician or endocrinologist. ) Hb. A 1 c = Glycosylated hemoglobin 39

Antiplatelet Agents / Anticoagulation Recommendations 40
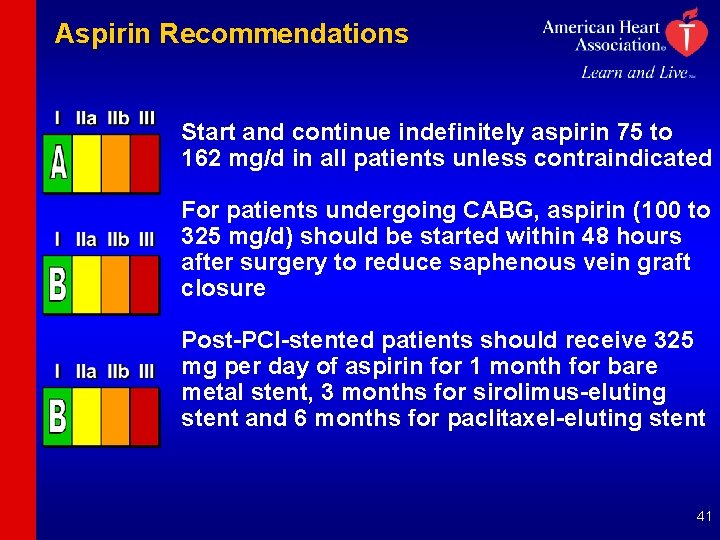
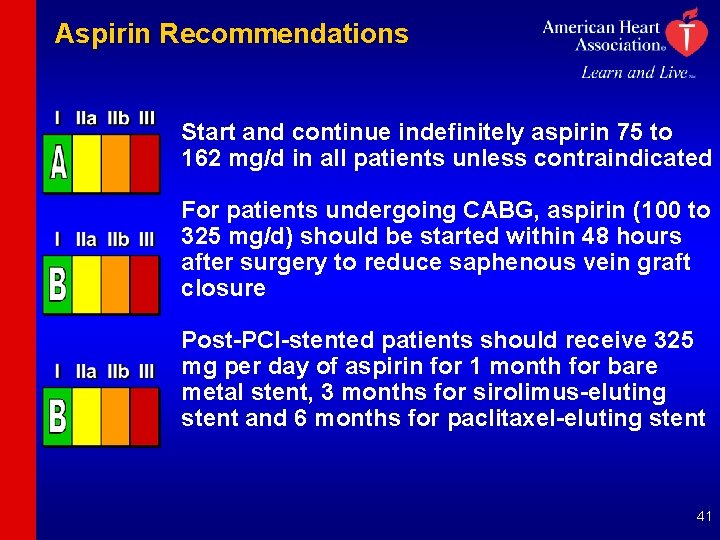
Aspirin Recommendations Start and continue indefinitely aspirin 75 to 162 mg/d in all patients unless contraindicated For patients undergoing CABG, aspirin (100 to 325 mg/d) should be started within 48 hours after surgery to reduce saphenous vein graft closure Post-PCI-stented patients should receive 325 mg per day of aspirin for 1 month for bare metal stent, 3 months for sirolimus-eluting stent and 6 months for paclitaxel-eluting stent 41
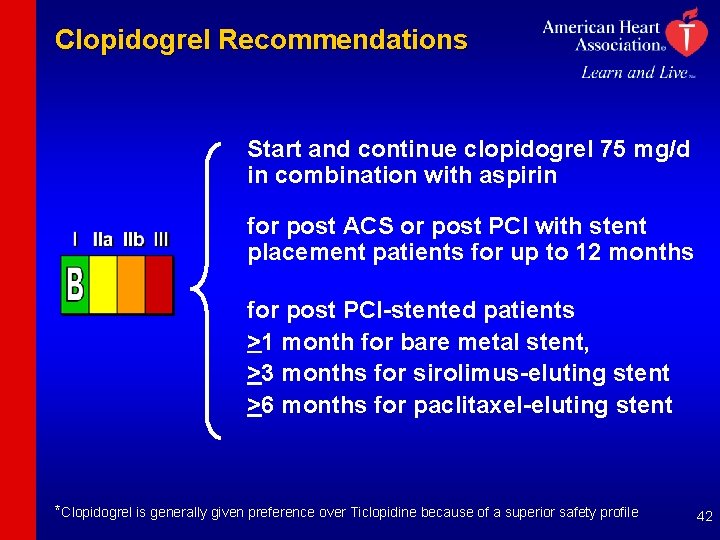
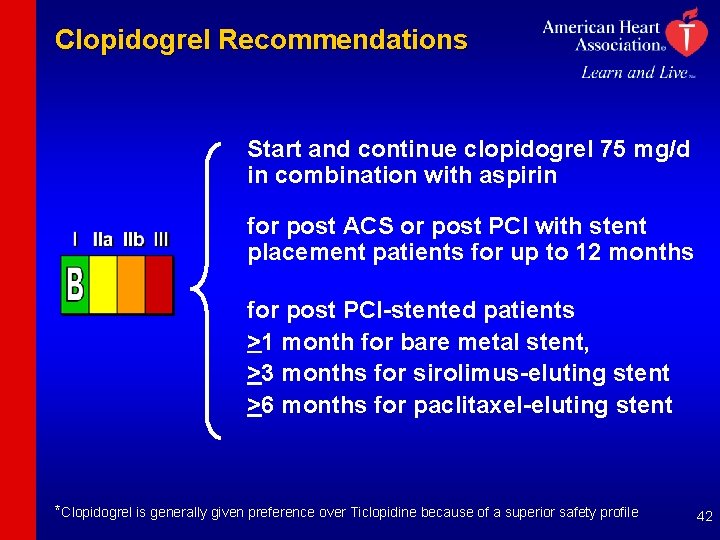
Clopidogrel Recommendations Start and continue clopidogrel 75 mg/d in combination with aspirin for post ACS or post PCI with stent placement patients for up to 12 months for post PCI-stented patients >1 month for bare metal stent, >3 months for sirolimus-eluting stent >6 months for paclitaxel-eluting stent *Clopidogrel is generally given preference over Ticlopidine because of a superior safety profile 42
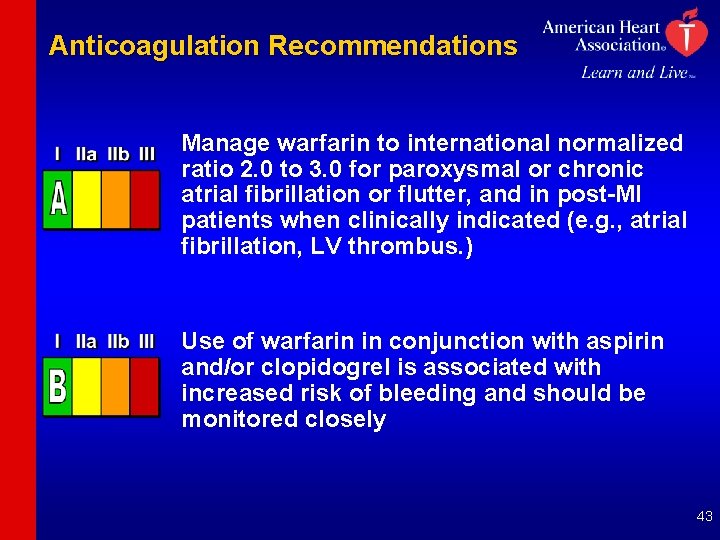
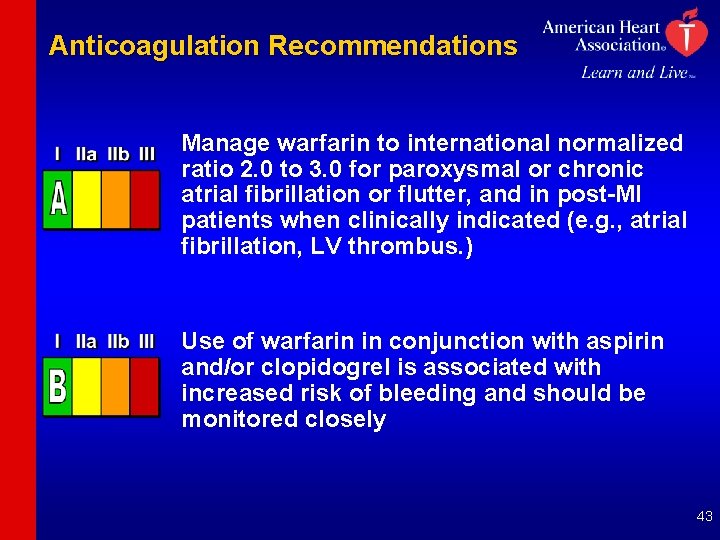
Anticoagulation Recommendations Manage warfarin to international normalized ratio 2. 0 to 3. 0 for paroxysmal or chronic atrial fibrillation or flutter, and in post-MI patients when clinically indicated (e. g. , atrial fibrillation, LV thrombus. ) Use of warfarin in conjunction with aspirin and/or clopidogrel is associated with increased risk of bleeding and should be monitored closely 43
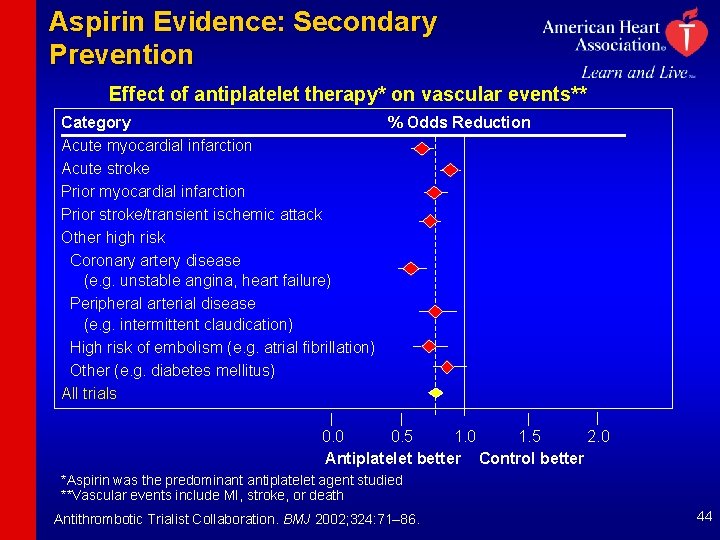
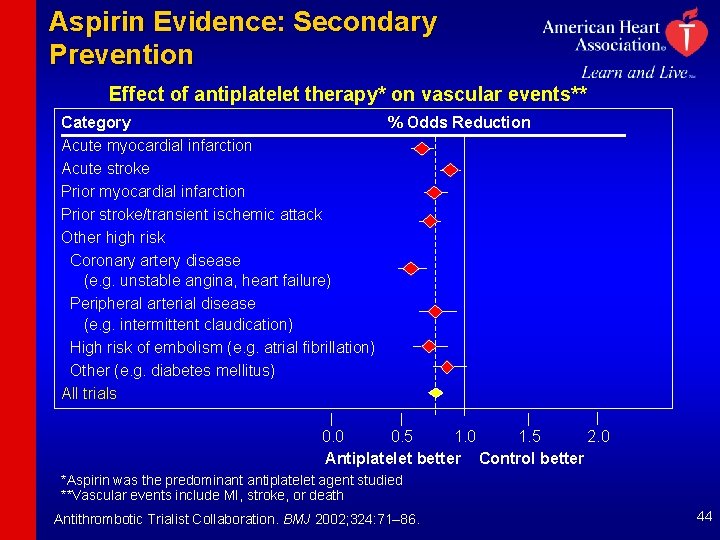
Aspirin Evidence: Secondary Prevention Effect of antiplatelet therapy* on vascular events** Category % Odds Reduction Acute myocardial infarction Acute stroke Prior myocardial infarction Prior stroke/transient ischemic attack Other high risk Coronary artery disease (e. g. unstable angina, heart failure) Peripheral arterial disease (e. g. intermittent claudication) High risk of embolism (e. g. atrial fibrillation) Other (e. g. diabetes mellitus) All trials 0. 0 0. 5 1. 0 1. 5 2. 0 Antiplatelet better Control better *Aspirin was the predominant antiplatelet agent studied **Vascular events include MI, stroke, or death Antithrombotic Trialist Collaboration. BMJ 2002; 324: 71– 86. 44
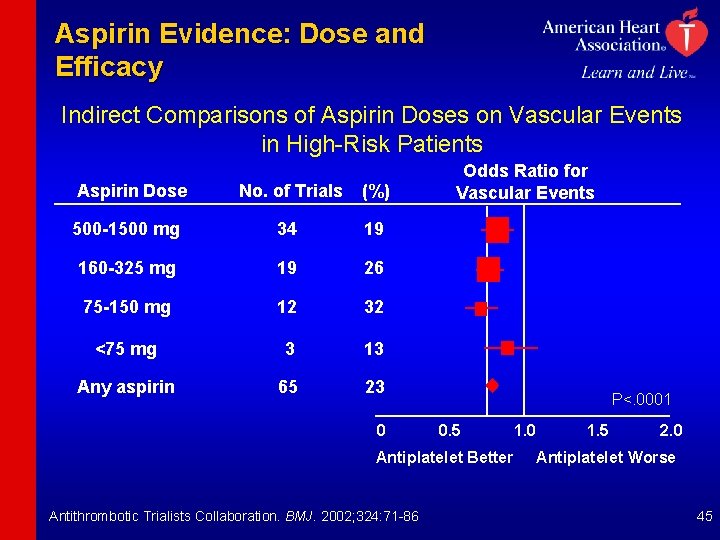
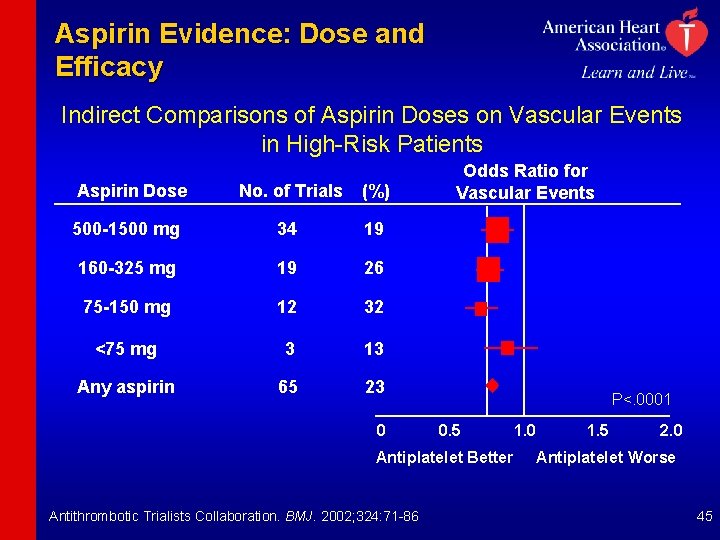
Aspirin Evidence: Dose and Efficacy Indirect Comparisons of Aspirin Doses on Vascular Events in High-Risk Patients Aspirin Dose No. of Trials (%) 500 -1500 mg 34 19 160 -325 mg 19 26 75 -150 mg 12 32 <75 mg 3 13 Any aspirin 65 23 0 Odds Ratio for Vascular Events P<. 0001 0. 5 Antiplatelet Better Antithrombotic Trialists Collaboration. BMJ. 2002; 324: 71 -86 1. 0 1. 5 2. 0 Antiplatelet Worse 45
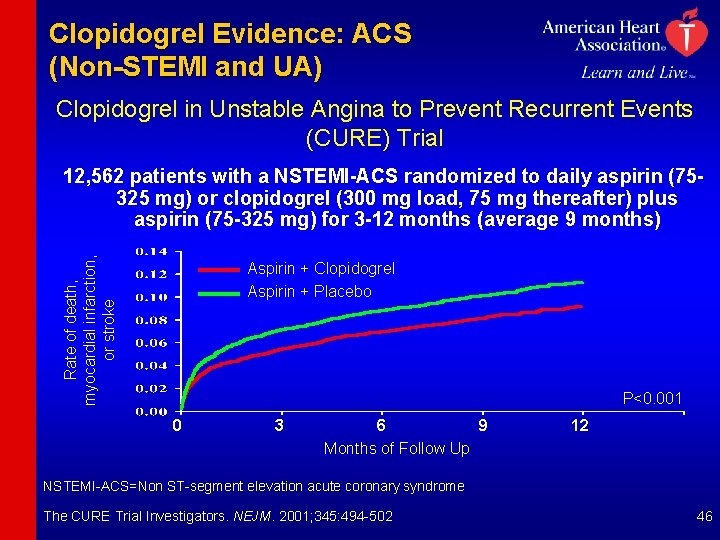
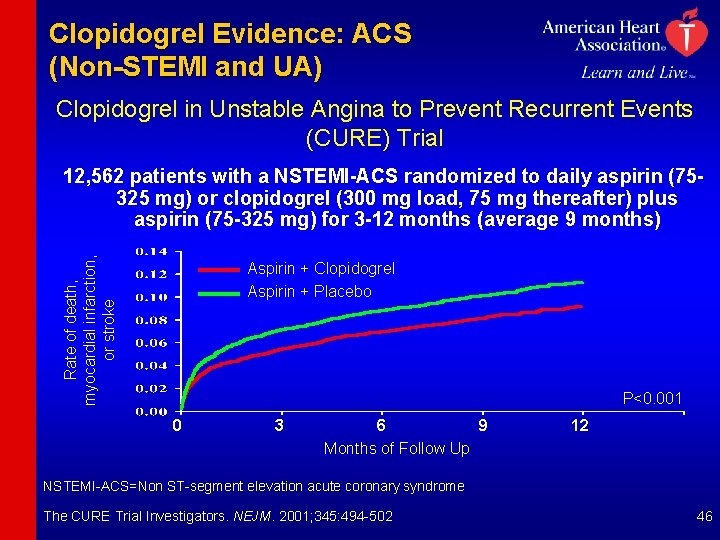
Clopidogrel Evidence: ACS (Non-STEMI and UA) Clopidogrel in Unstable Angina to Prevent Recurrent Events (CURE) Trial Rate of death, myocardial infarction, or stroke 12, 562 patients with a NSTEMI-ACS randomized to daily aspirin (75325 mg) or clopidogrel (300 mg load, 75 mg thereafter) plus aspirin (75 -325 mg) for 3 -12 months (average 9 months) Aspirin + Clopidogrel Aspirin + Placebo P<0. 001 0 3 6 9 12 Months of Follow Up NSTEMI-ACS=Non ST-segment elevation acute coronary syndrome The CURE Trial Investigators. NEJM. 2001; 345: 494 -502 46
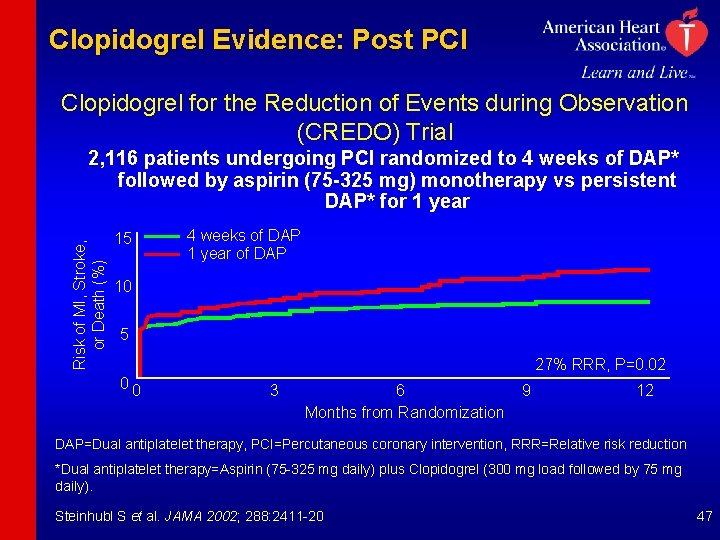
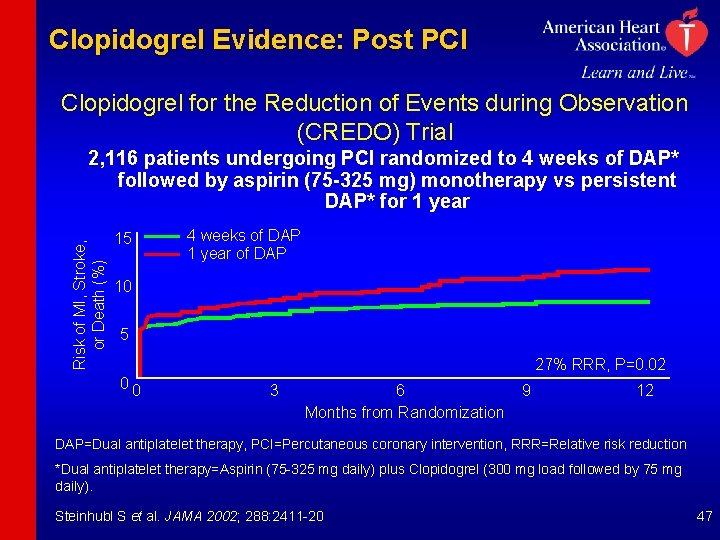
Clopidogrel Evidence: Post PCI Clopidogrel for the Reduction of Events during Observation (CREDO) Trial Risk of MI, Stroke, or Death (%) 2, 116 patients undergoing PCI randomized to 4 weeks of DAP* followed by aspirin (75 -325 mg) monotherapy vs persistent DAP* for 1 year 15 4 weeks of DAP 1 year of DAP 10 5 27% RRR, P=0. 02 00 3 6 Months from Randomization 9 12 DAP=Dual antiplatelet therapy, PCI=Percutaneous coronary intervention, RRR=Relative risk reduction *Dual antiplatelet therapy=Aspirin (75 -325 mg daily) plus Clopidogrel (300 mg load followed by 75 mg daily). Steinhubl S et al. JAMA 2002; 288: 2411 -20 47
Renin-Angiotensin-Aldosterone System Blockers Recommendations 48
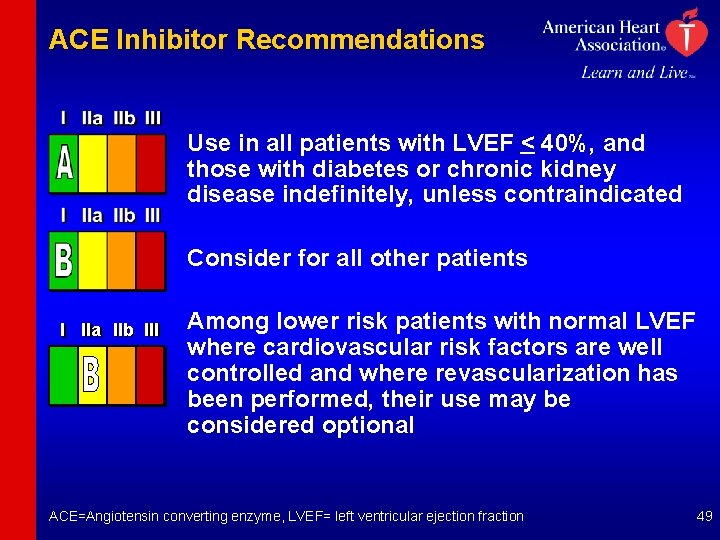
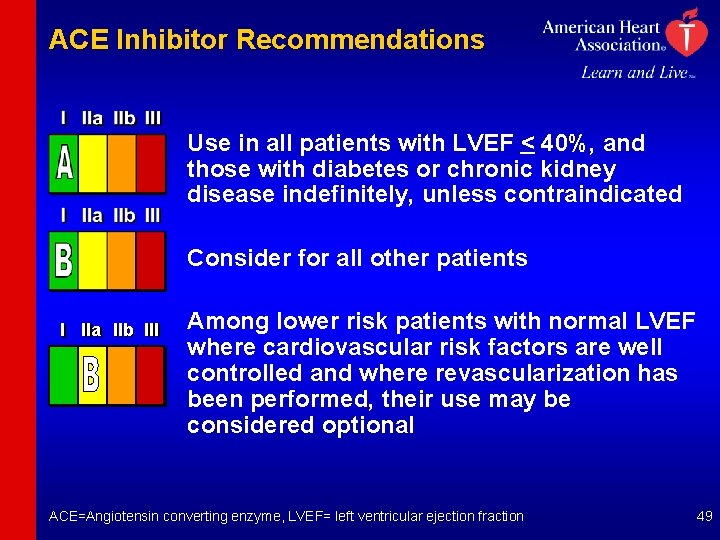
ACE Inhibitor Recommendations Use in all patients with LVEF < 40%, and those with diabetes or chronic kidney disease indefinitely, unless contraindicated Consider for all other patients I IIa IIb III Among lower risk patients with normal LVEF where cardiovascular risk factors are well controlled and where revascularization has been performed, their use may be considered optional ACE=Angiotensin converting enzyme, LVEF= left ventricular ejection fraction 49
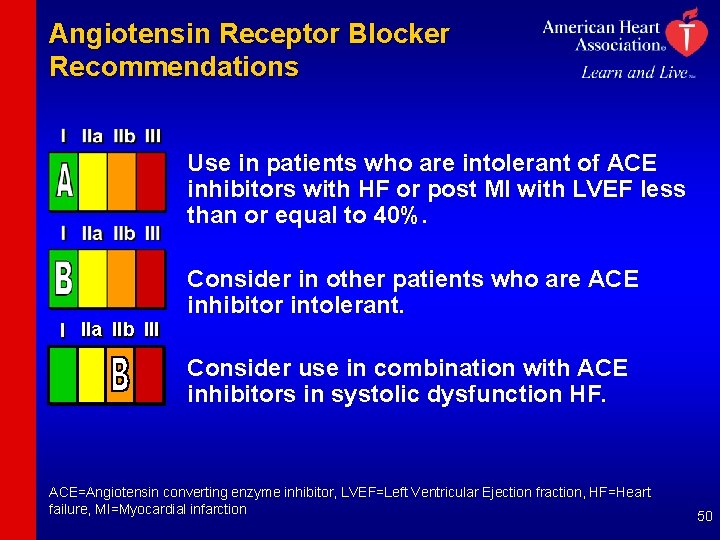
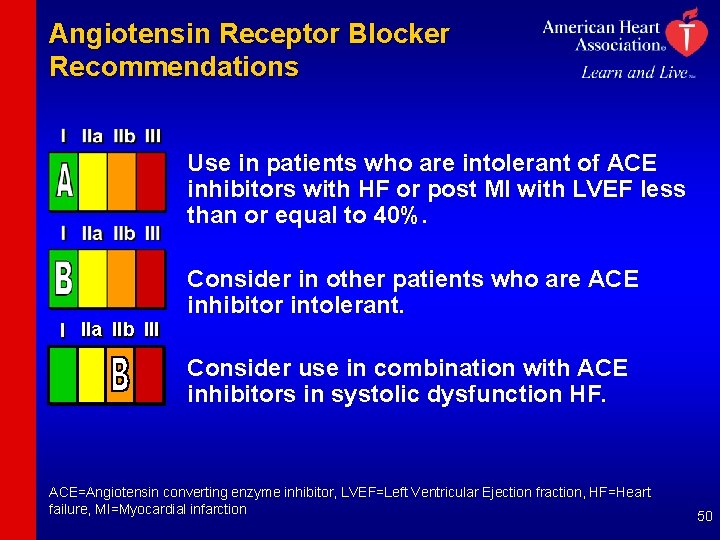
Angiotensin Receptor Blocker Recommendations Use in patients who are intolerant of ACE inhibitors with HF or post MI with LVEF less than or equal to 40%. Consider in other patients who are ACE inhibitor intolerant. I IIa IIb III Consider use in combination with ACE inhibitors in systolic dysfunction HF. ACE=Angiotensin converting enzyme inhibitor, LVEF=Left Ventricular Ejection fraction, HF=Heart failure, MI=Myocardial infarction 50
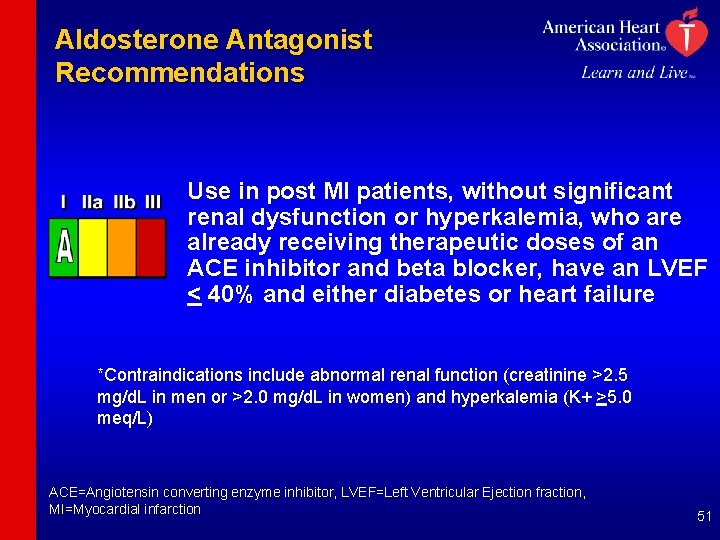
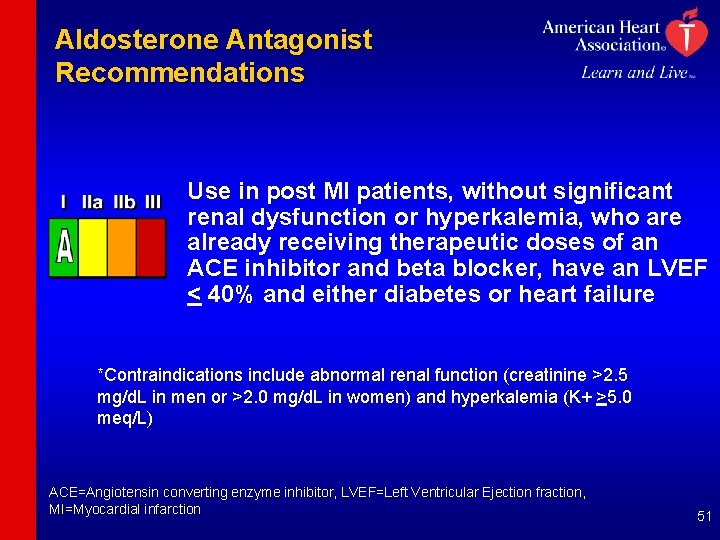
Aldosterone Antagonist Recommendations Use in post MI patients, without significant renal dysfunction or hyperkalemia, who are already receiving therapeutic doses of an ACE inhibitor and beta blocker, have an LVEF < 40% and either diabetes or heart failure *Contraindications include abnormal renal function (creatinine >2. 5 mg/d. L in men or >2. 0 mg/d. L in women) and hyperkalemia (K+ >5. 0 meq/L) ACE=Angiotensin converting enzyme inhibitor, LVEF=Left Ventricular Ejection fraction, MI=Myocardial infarction 51
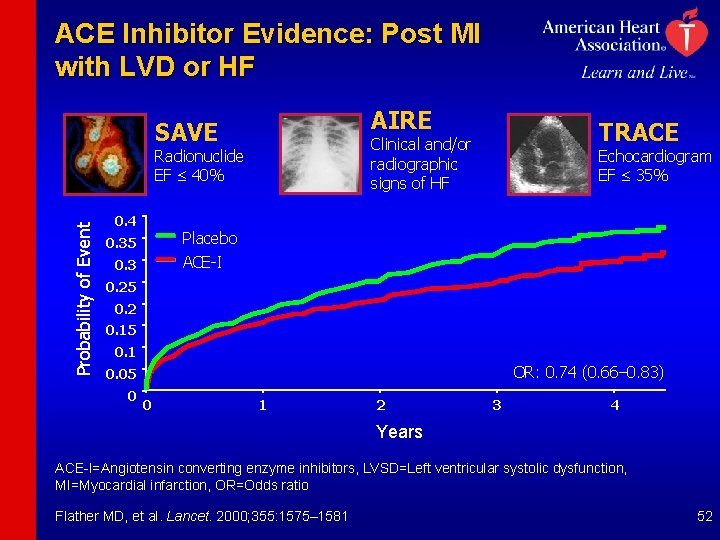
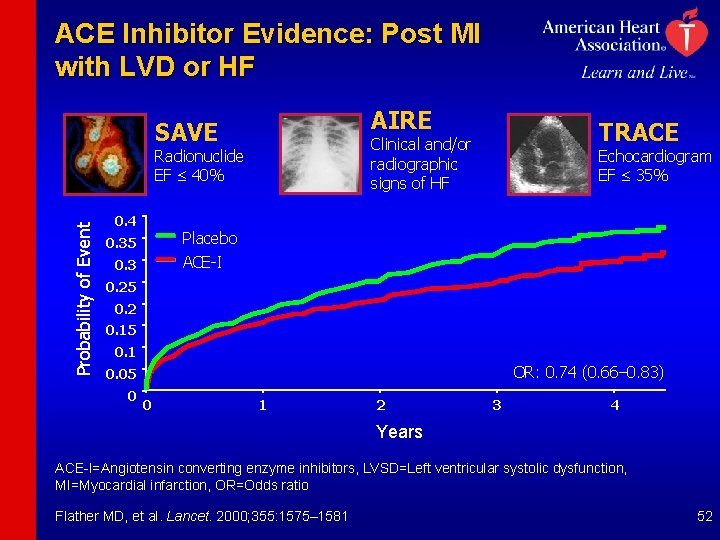
ACE Inhibitor Evidence: Post MI with LVD or HF AIRE SAVE Probability of Event Radionuclide EF £ 40% 0. 4 TRACE Clinical and/or radiographic signs of HF Echocardiogram EF £ 35% Placebo ACE-I 0. 35 0. 3 0. 25 0. 2 0. 15 0. 1 OR: 0. 74 (0. 66– 0. 83) 0. 05 0 0 1 2 3 4 Years ACE-I=Angiotensin converting enzyme inhibitors, LVSD=Left ventricular systolic dysfunction, MI=Myocardial infarction, OR=Odds ratio Flather MD, et al. Lancet. 2000; 355: 1575– 1581 52
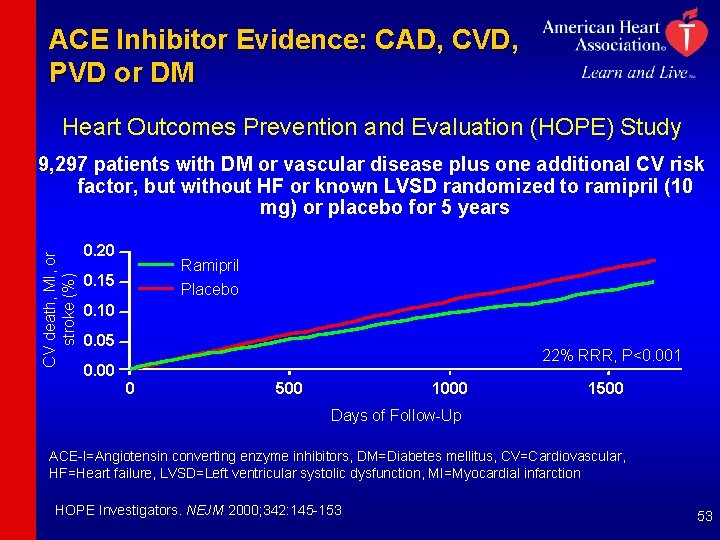
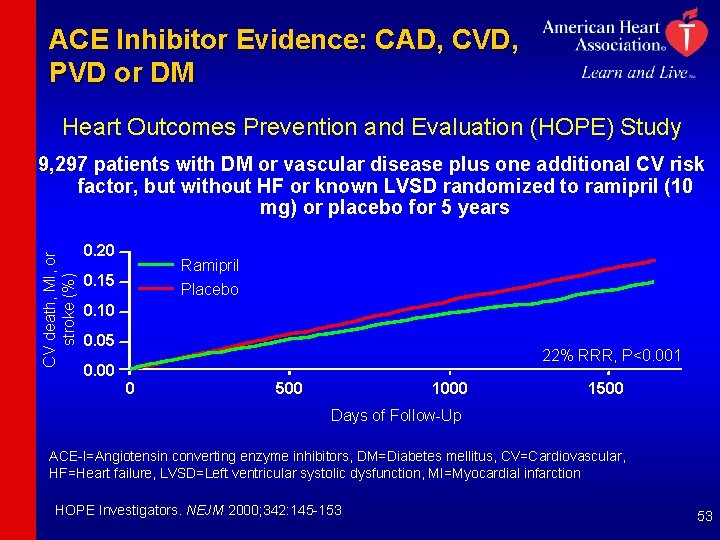
ACE Inhibitor Evidence: CAD, CVD, PVD or DM Heart Outcomes Prevention and Evaluation (HOPE) Study CV death, MI, or stroke (%) 9, 297 patients with DM or vascular disease plus one additional CV risk 9, factor, but without HF or known LVSD randomized to ramipril (10 mg) or placebo for 5 years 0. 20 Ramipril Placebo 0. 15 0. 10 0. 05 22% RRR, P<0. 001 0. 00 0 500 1000 1500 Days of Follow-Up ACE-I=Angiotensin converting enzyme inhibitors, DM=Diabetes mellitus, CV=Cardiovascular, HF=Heart failure, LVSD=Left ventricular systolic dysfunction, MI=Myocardial infarction HOPE Investigators. NEJM 2000; 342: 145 -153 53
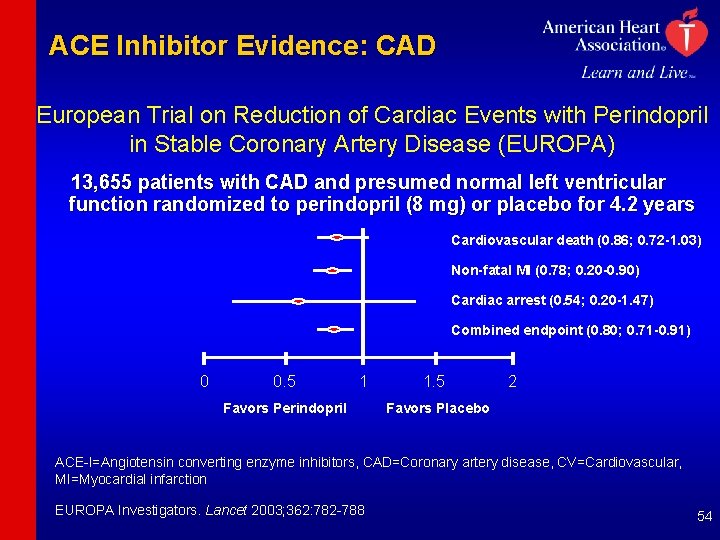
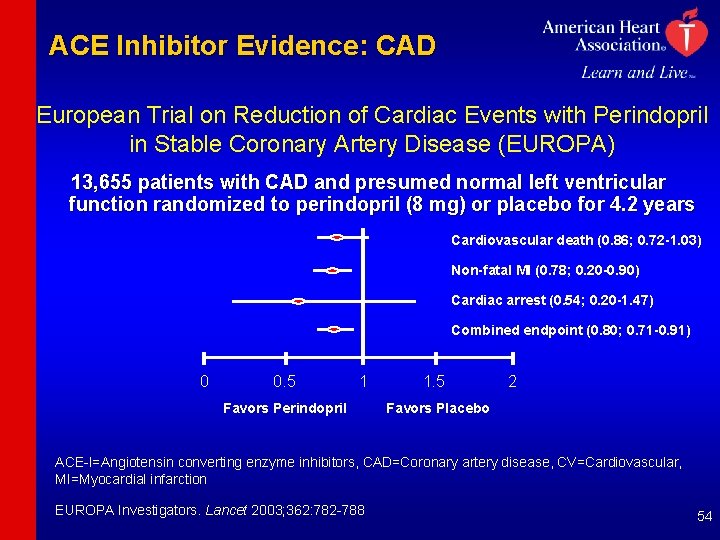
ACE Inhibitor Evidence: CAD European Trial on Reduction of Cardiac Events with Perindopril in Stable Coronary Artery Disease (EUROPA) 13, 655 patients with CAD and presumed normal left ventricular function randomized to perindopril (8 mg) or placebo for 4. 2 years Cardiovascular death (0. 86; 0. 72 -1. 03) Non-fatal MI (0. 78; 0. 20 -0. 90) Cardiac arrest (0. 54; 0. 20 -1. 47) Combined endpoint (0. 80; 0. 71 -0. 91) 0 0. 5 1 Favors Perindopril 1. 5 2 Favors Placebo ACE-I=Angiotensin converting enzyme inhibitors, CAD=Coronary artery disease, CV=Cardiovascular, MI=Myocardial infarction EUROPA Investigators. Lancet 2003; 362: 782 -788 54
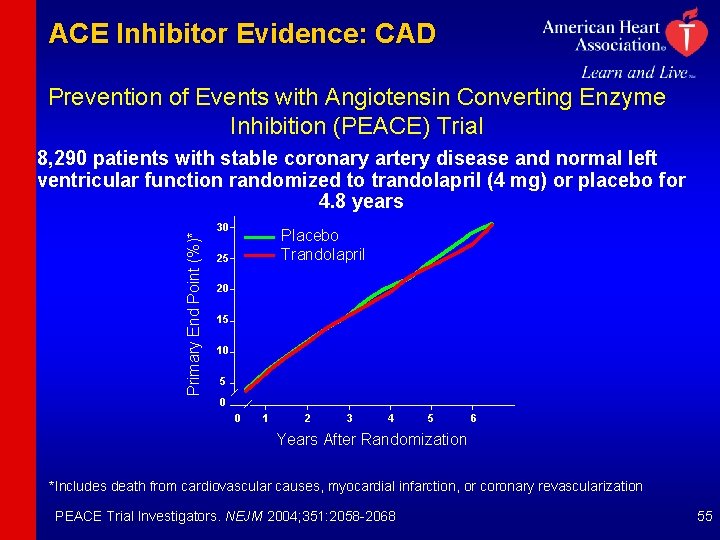
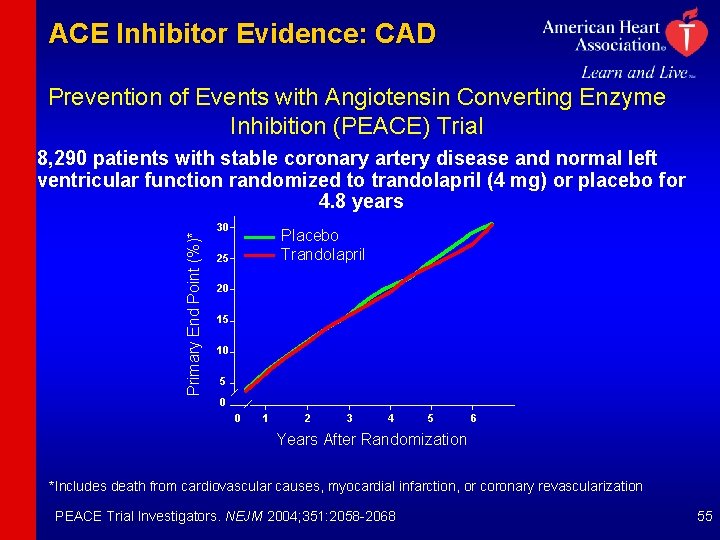
ACE Inhibitor Evidence: CAD Prevention of Events with Angiotensin Converting Enzyme Inhibition (PEACE) Trial Primary End Point (%)* 8, 290 patients with stable coronary artery disease and normal left ventricular function randomized to trandolapril (4 mg) or placebo for 4. 8 years 30 Placebo Trandolapril 25 20 15 10 5 0 0 1 2 3 4 5 6 Years After Randomization *Includes death from cardiovascular causes, myocardial infarction, or coronary revascularization PEACE Trial Investigators. NEJM 2004; 351: 2058 -2068 55
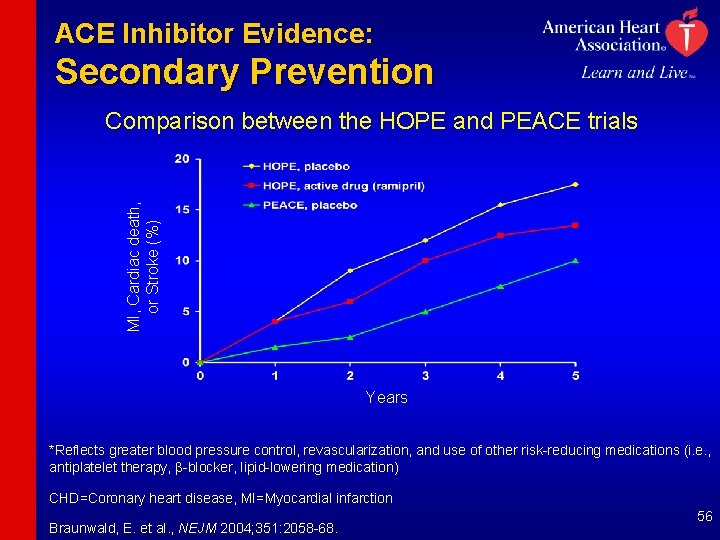
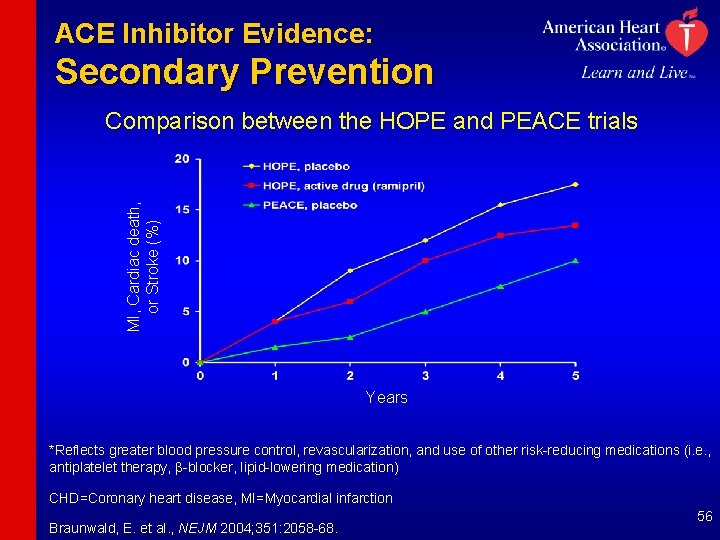
ACE Inhibitor Evidence: Secondary Prevention MI, Cardiac death, or Stroke (%) Comparison between the HOPE and PEACE trials Years *Reflects greater blood pressure control, revascularization, and use of other risk-reducing medications (i. e. , antiplatelet therapy, b-blocker, lipid-lowering medication) CHD=Coronary heart disease, MI=Myocardial infarction Braunwald, E. et al. , NEJM 2004; 351: 2058 -68. 56
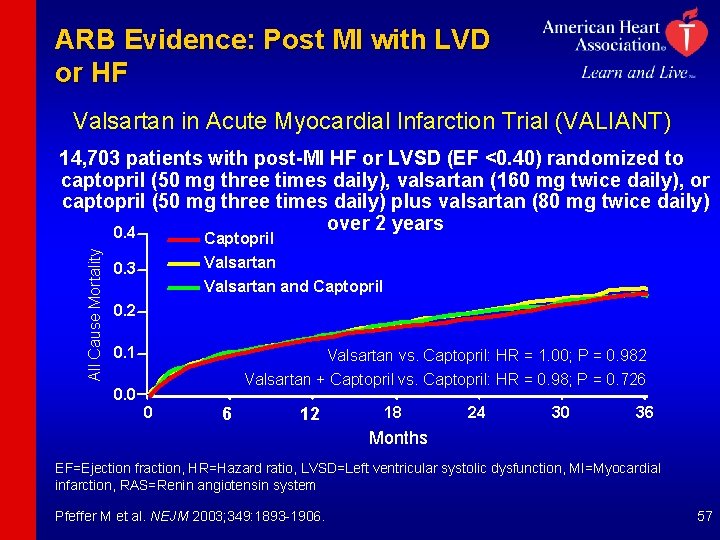
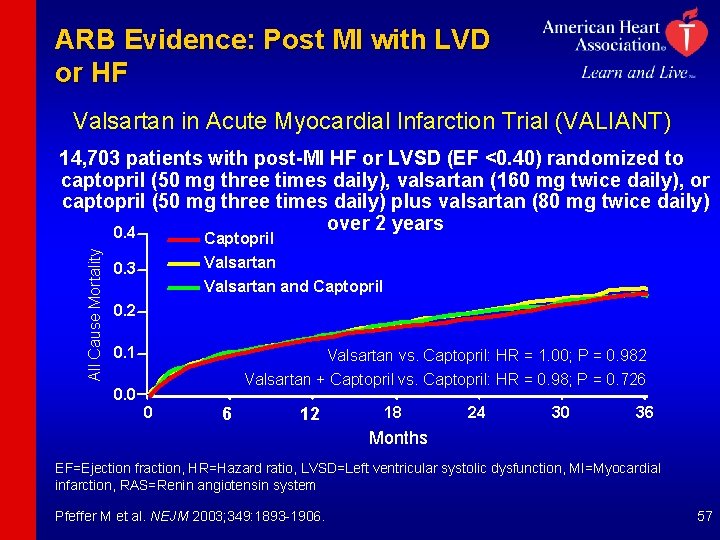
ARB Evidence: Post MI with LVD or HF Valsartan in Acute Myocardial Infarction Trial (VALIANT) All Cause Mortality 14, 703 patients with post-MI HF or LVSD (EF <0. 40) randomized to captopril (50 mg three times daily), valsartan (160 mg twice daily), or captopril (50 mg three times daily) plus valsartan (80 mg twice daily) over 2 years 0. 4 Captopril Valsartan 0. 3 Valsartan and Captopril 0. 2 0. 1 Valsartan vs. Captopril: HR = 1. 00; P = 0. 982 Valsartan + Captopril vs. Captopril: HR = 0. 98; P = 0. 726 0. 0 0 6 12 18 24 30 36 Months EF=Ejection fraction, HR=Hazard ratio, LVSD=Left ventricular systolic dysfunction, MI=Myocardial infarction, RAS=Renin angiotensin system Pfeffer M et al. NEJM 2003; 349: 1893 -1906. 57
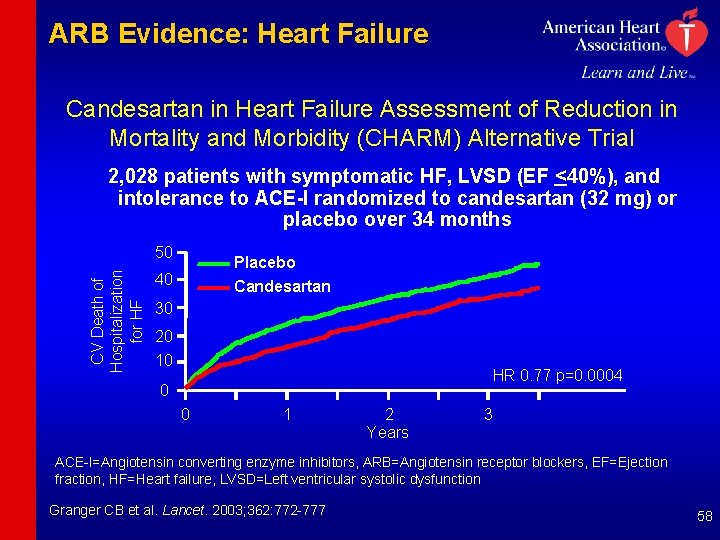
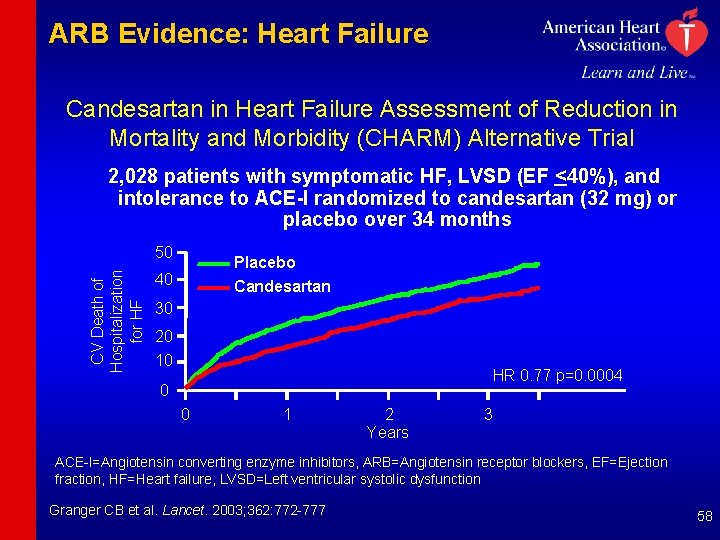
ARB Evidence: Heart Failure Candesartan in Heart Failure Assessment of Reduction in Mortality and Morbidity (CHARM) Alternative Trial 2, 028 patients with symptomatic HF, LVSD (EF <40%), and intolerance to ACE-I randomized to candesartan (32 mg) or placebo over 34 months CV Death of Hospitalization for HF 50 Placebo Candesartan 40 30 20 10 HR 0. 77 p=0. 0004 0 0 1 2 Years 3 ACE-I=Angiotensin converting enzyme inhibitors, ARB=Angiotensin receptor blockers, EF=Ejection fraction, HF=Heart failure, LVSD=Left ventricular systolic dysfunction Granger CB et al. Lancet. 2003; 362: 772 -777 58
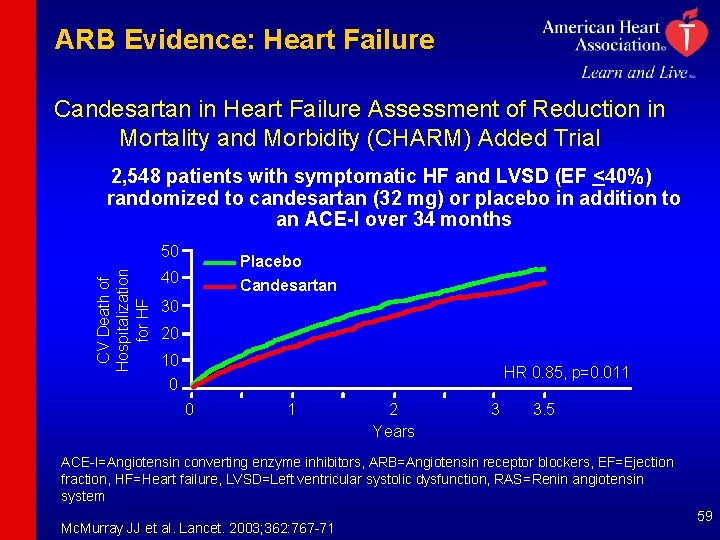
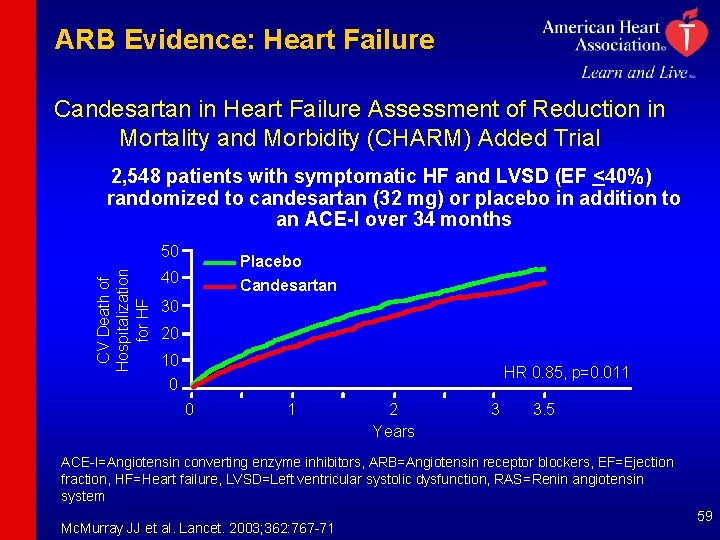
ARB Evidence: Heart Failure Candesartan in Heart Failure Assessment of Reduction in Mortality and Morbidity (CHARM) Added Trial 2, 548 patients with symptomatic HF and LVSD (EF <40%) randomized to candesartan (32 mg) or placebo in addition to an ACE-I over 34 months CV Death of Hospitalization for HF 50 Placebo 40 Candesartan 30 20 10 HR 0. 85, p=0. 011 0 0 1 2 Years 3 3. 5 ACE-I=Angiotensin converting enzyme inhibitors, ARB=Angiotensin receptor blockers, EF=Ejection fraction, HF=Heart failure, LVSD=Left ventricular systolic dysfunction, RAS=Renin angiotensin system Mc. Murray JJ et al. Lancet. 2003; 362: 767 -71 59
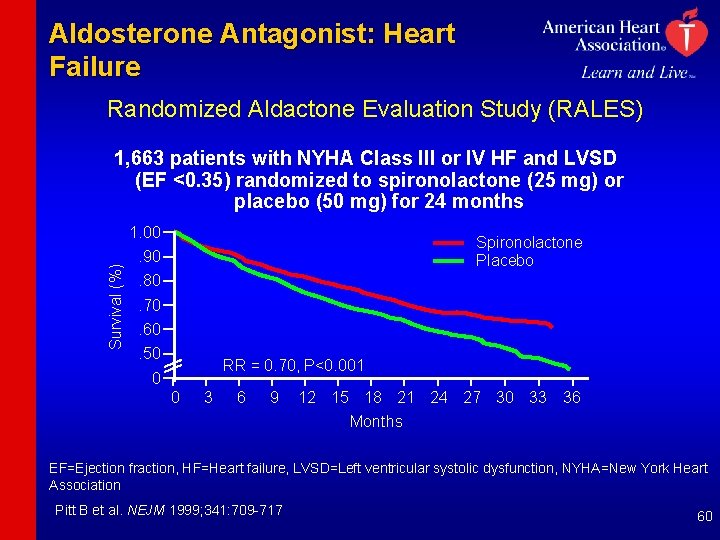
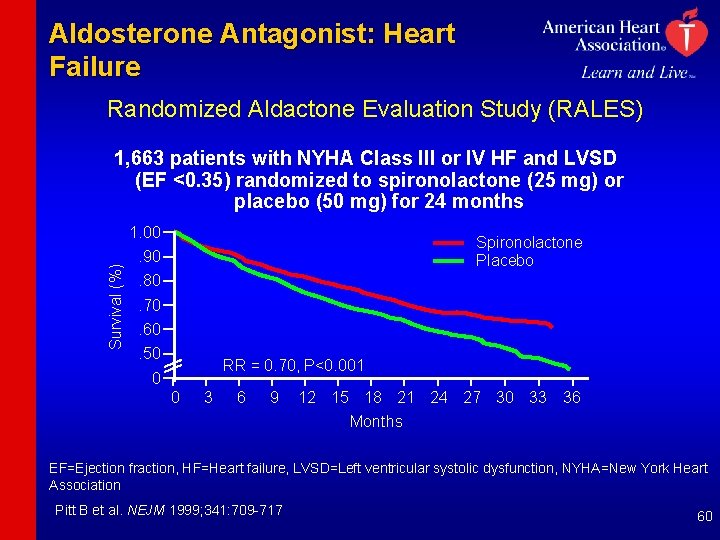
Aldosterone Antagonist: Heart Failure Randomized Aldactone Evaluation Study (RALES) 1, 663 patients with NYHA Class III or IV HF and LVSD (EF <0. 35) randomized to spironolactone (25 mg) or placebo (50 mg) for 24 months Survival (%) 1. 00 Spironolactone Placebo . 90. 80. 70. 60. 50 RR = 0. 70, P<0. 001 0 0 3 6 9 12 15 18 21 24 27 30 33 36 Months EF=Ejection fraction, HF=Heart failure, LVSD=Left ventricular systolic dysfunction, NYHA=New York Heart Association Pitt B et al. NEJM 1999; 341: 709 -717 60
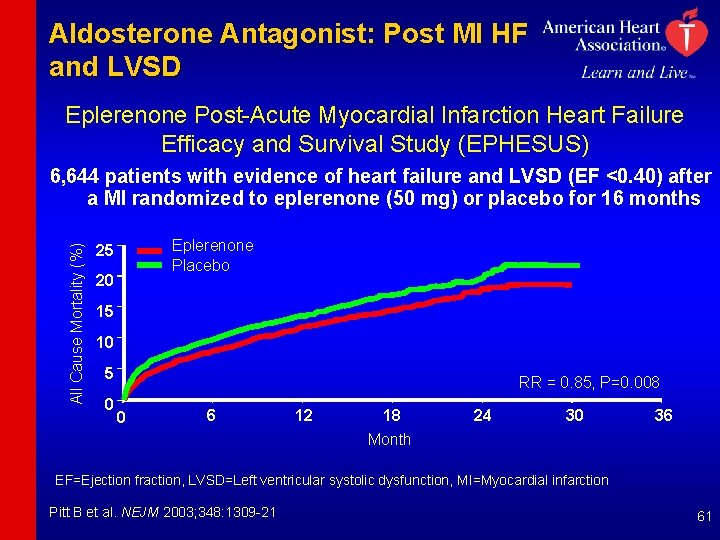
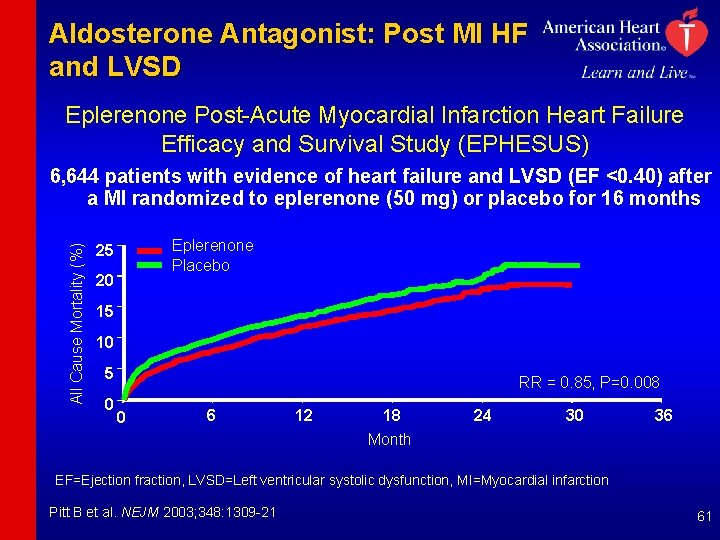
Aldosterone Antagonist: Post MI HF and LVSD Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS) All Cause Mortality (%) 6, 644 patients with evidence of heart failure and LVSD (EF <0. 40) after a MI randomized to eplerenone (50 mg) or placebo for 16 months Eplerenone Placebo 25 20 15 10 5 0 RR = 0. 85, P=0. 008 0 6 12 18 24 30 36 Month EF=Ejection fraction, LVSD=Left ventricular systolic dysfunction, MI=Myocardial infarction Pitt B et al. NEJM 2003; 348: 1309 -21 61

b-blocker Recommendations 62
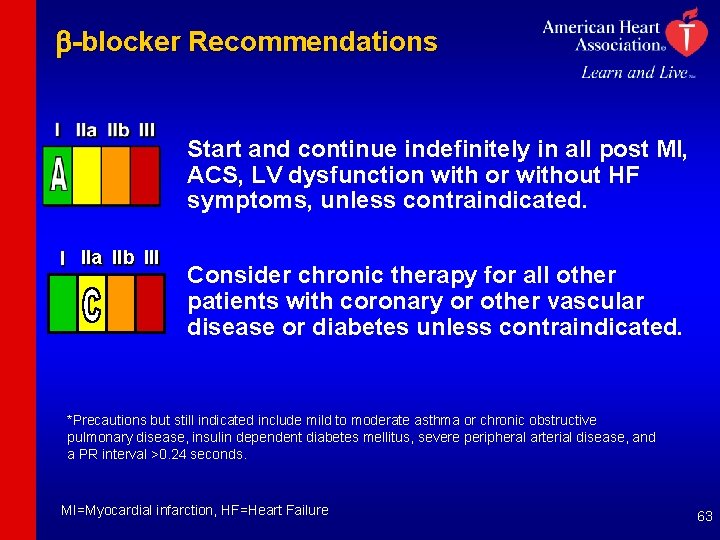
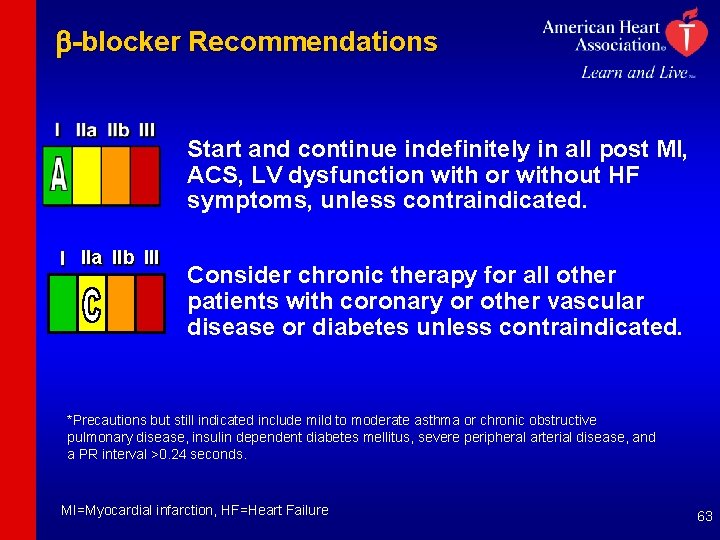
b-blocker Recommendations Start and continue indefinitely in all post MI, ACS, LV dysfunction with or without HF symptoms, unless contraindicated. I IIa IIb III Consider chronic therapy for all other patients with coronary or other vascular disease or diabetes unless contraindicated. *Precautions but still indicated include mild to moderate asthma or chronic obstructive pulmonary disease, insulin dependent diabetes mellitus, severe peripheral arterial disease, and a PR interval >0. 24 seconds. MI=Myocardial infarction, HF=Heart Failure 63
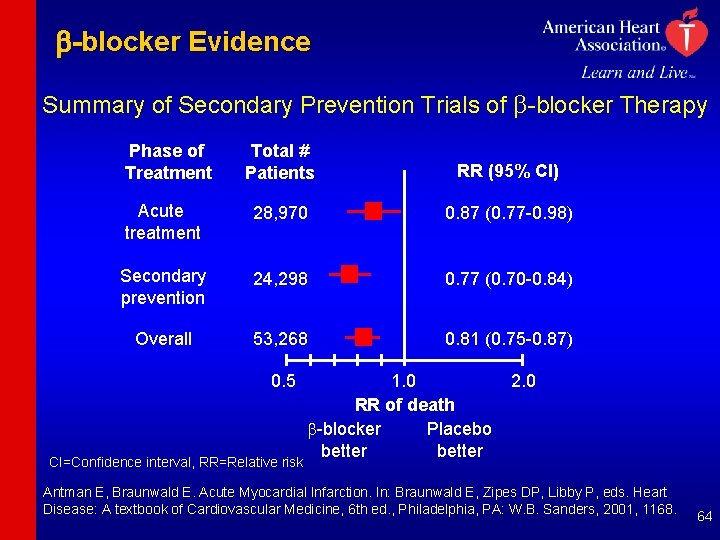
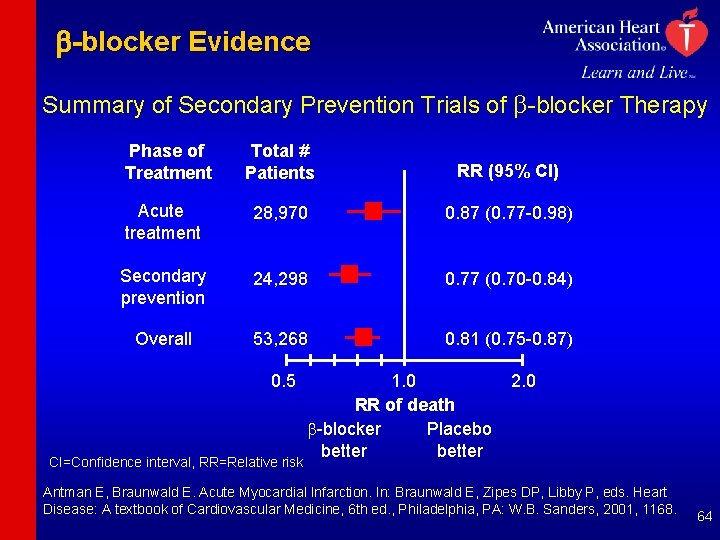
b-blocker Evidence Summary of Secondary Prevention Trials of b-blocker Therapy Phase of Treatment Total # Patients RR (95% CI) Acute treatment 28, 970 0. 87 (0. 77 -0. 98) Secondary prevention 24, 298 0. 77 (0. 70 -0. 84) Overall 53, 268 0. 81 (0. 75 -0. 87) 0. 5 CI=Confidence interval, RR=Relative risk 1. 0 RR of death b-blocker Placebo better 2. 0 Antman E, Braunwald E. Acute Myocardial Infarction. In: Braunwald E, Zipes DP, Libby P, eds. Heart Disease: A textbook of Cardiovascular Medicine, 6 th ed. , Philadelphia, PA: W. B. Sanders, 2001, 1168. 64
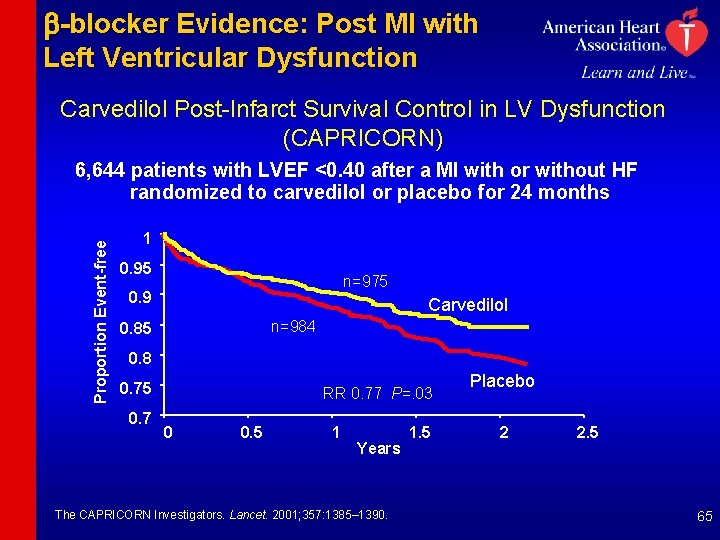
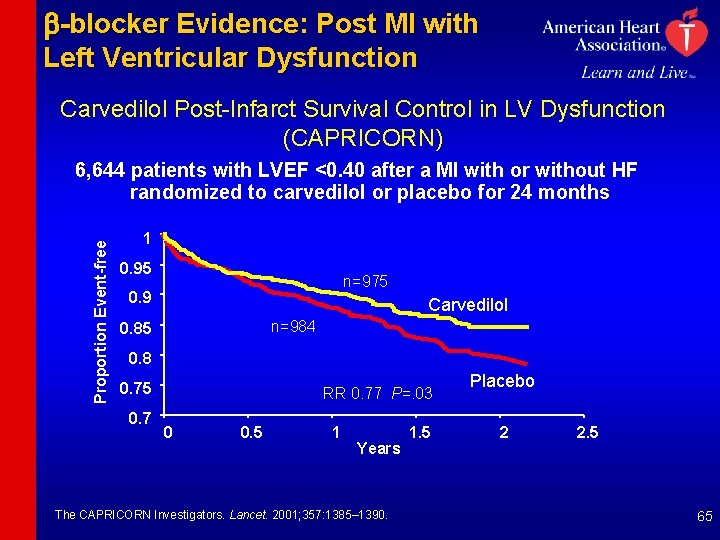
b-blocker Evidence: Post MI with Left Ventricular Dysfunction Carvedilol Post-Infarct Survival Control in LV Dysfunction (CAPRICORN) Proportion Event-free 6, 644 patients with LVEF <0. 40 after a MI with or without HF randomized to carvedilol or placebo for 24 months 1 0. 95 n=975 0. 9 Carvedilol n=984 0. 85 0. 8 0. 75 0. 7 RR 0. 77 P=. 03 0 0. 5 1 Years The CAPRICORN Investigators. Lancet. 2001; 357: 1385– 1390. 1. 5 Placebo 2 2. 5 65
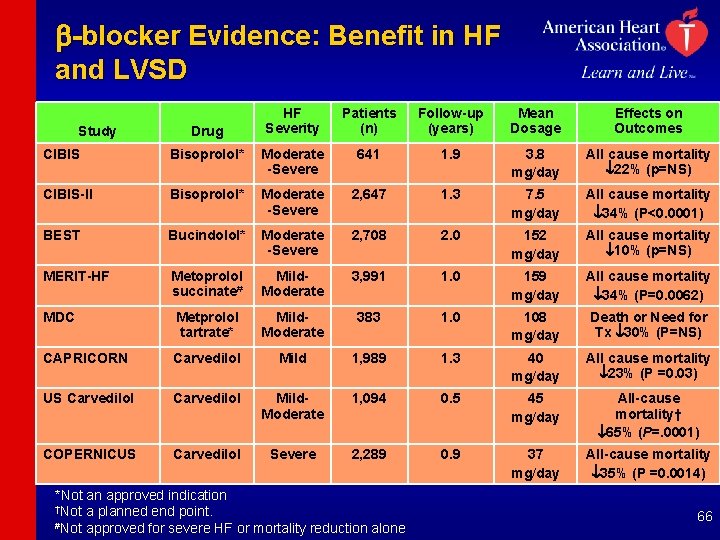
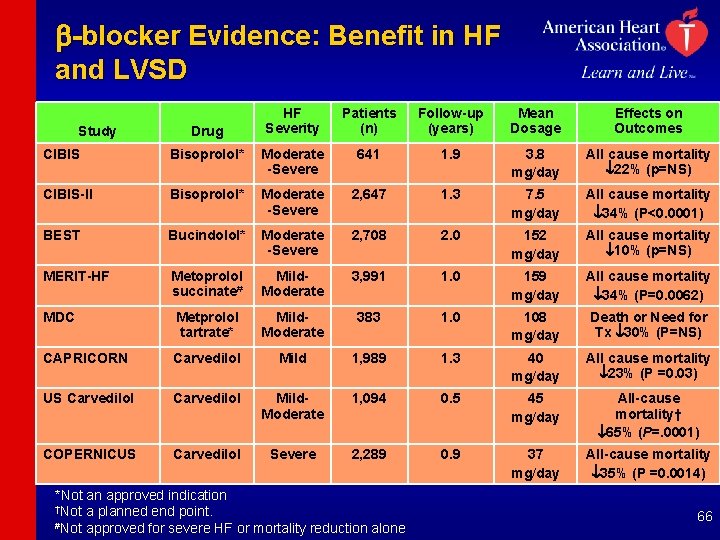
b-blocker Evidence: Benefit in HF and LVSD Study Drug HF Severity Patients (n) Follow-up (years) Mean Dosage Effects on Outcomes CIBIS Bisoprolol* Moderate -Severe 641 1. 9 3. 8 mg/day All cause mortality 22% (p=NS) CIBIS-II Bisoprolol* Moderate -Severe 2, 647 1. 3 7. 5 mg/day All cause mortality 34% (P<0. 0001) BEST Bucindolol* Moderate -Severe 2, 708 2. 0 152 mg/day All cause mortality 10% (p=NS) MERIT-HF Metoprolol succinate# Mild. Moderate 3, 991 1. 0 159 mg/day All cause mortality 34% (P=0. 0062) MDC Metprolol tartrate* Mild. Moderate 383 1. 0 108 mg/day Death or Need for Tx 30% (P=NS) CAPRICORN Carvedilol Mild 1, 989 1. 3 40 mg/day All cause mortality 23% (P =0. 03) US Carvedilol Mild. Moderate 1, 094 0. 5 45 mg/day All-cause mortality† 65% (P=. 0001) COPERNICUS Carvedilol Severe 2, 289 0. 9 37 mg/day All-cause mortality 35% (P =0. 0014) *Not an approved indication †Not a planned end point. #Not approved for severe HF or mortality reduction alone 66
Influenza Vaccination Patients with cardiovascular disease should have influenza vaccination 67
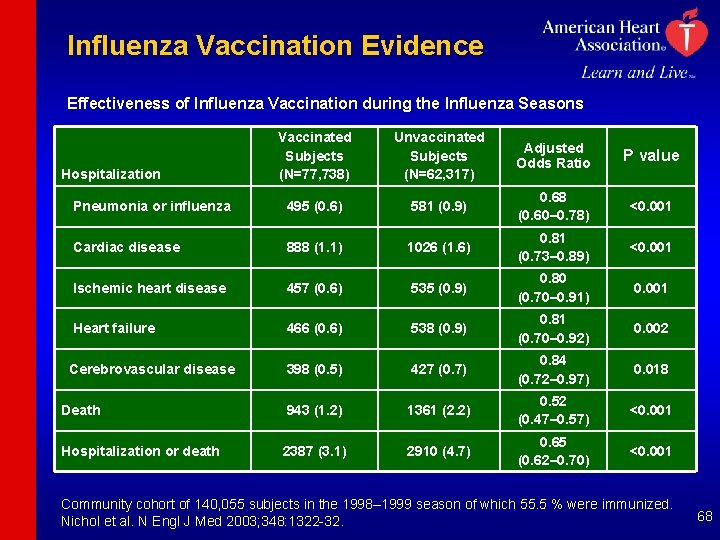
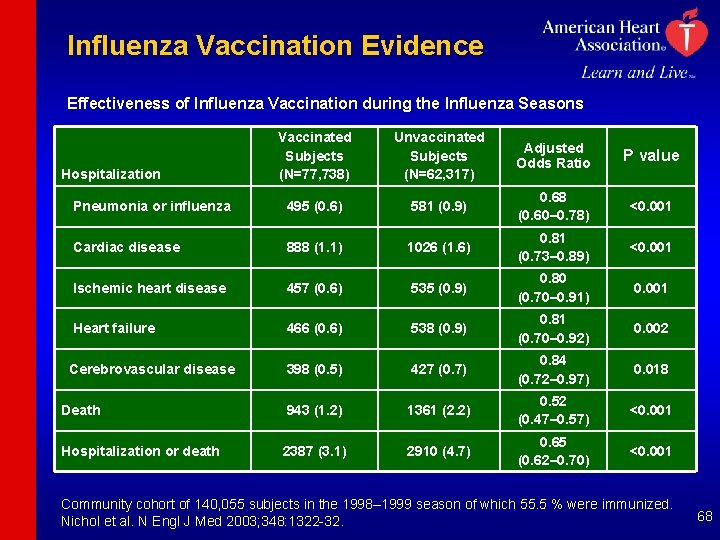
Influenza Vaccination Evidence Effectiveness of Influenza Vaccination during the Influenza Seasons Vaccinated Subjects (N=77, 738) Unvaccinated Subjects (N=62, 317) Adjusted Odds Ratio P value Pneumonia or influenza 495 (0. 6) 581 (0. 9) 0. 68 (0. 60– 0. 78) <0. 001 Cardiac disease 888 (1. 1) 1026 (1. 6) 0. 81 (0. 73– 0. 89) <0. 001 Ischemic heart disease 457 (0. 6) 535 (0. 9) 0. 80 (0. 70– 0. 91) 0. 001 Heart failure 466 (0. 6) 538 (0. 9) 0. 81 (0. 70– 0. 92) 0. 002 Cerebrovascular disease 398 (0. 5) 427 (0. 7) 0. 84 (0. 72– 0. 97) 0. 018 Death 943 (1. 2) 1361 (2. 2) 0. 52 (0. 47– 0. 57) <0. 001 Hospitalization or death 2387 (3. 1) 2910 (4. 7) 0. 65 (0. 62– 0. 70) <0. 001 Hospitalization Community cohort of 140, 055 subjects in the 1998– 1999 season of which 55. 5 % were immunized. Nichol et al. N Engl J Med 2003; 348: 1322 -32. 68
The Need to Implement Secondary Prevention Multiple studies of the use of these recommended therapies in appropriate patients continue to show that many patients in whom therapies are indicated are not receiving them in actual clinical practice. The AHA and ACC urge that in all medical care settings where these patients are managed that programs to provide practitioners with useful reminder clues based on the guidelines, and continuously assess the success achieved in providing these therapies to the patients who can benefit from them be implemented. Encourage that the AHA’s Get With the Guidelines and/or ACC’s Guidelines Applied to Practice Programs be instituted to identify appropriate patients for therapy 69
AHA GWTG Program GWTG is a national initiative of the AHA to improve guidelines adherence in patients hospitalized with cardiovascular disease. GWTG uses collaborative learning sessions, conference calls, e-mail and staff support to assist hospital teams improve acute and secondary prevention care systems. A web-based Patient Management Tool is used for point of care data collection and decision support, on-demand reporting, communication and patient education. 70
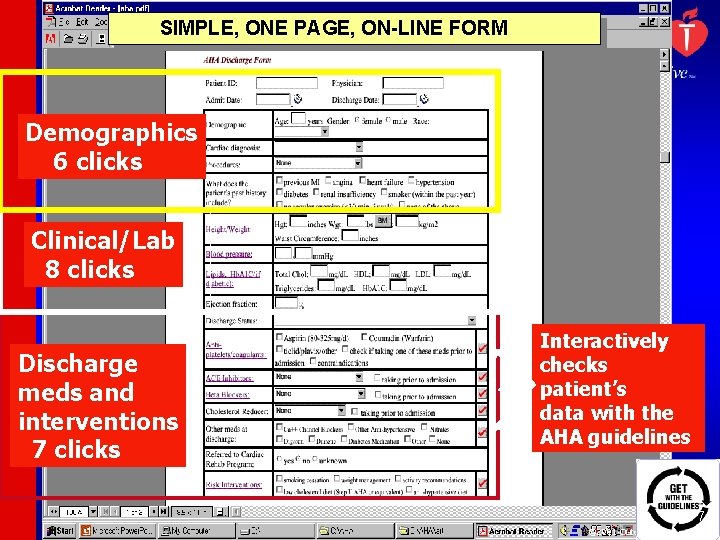
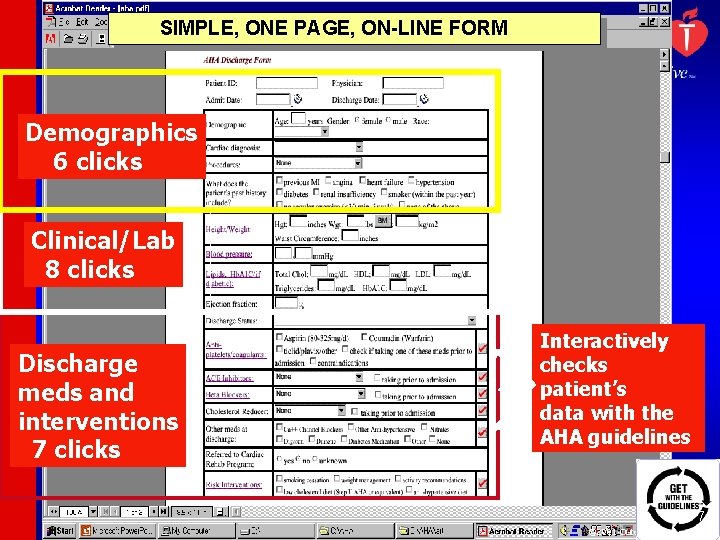
SIMPLE, ONE PAGE, ON-LINE FORM Demographics 6 clicks Clinical/Lab 8 clicks Discharge meds and interventions 7 clicks Interactively checks patient’s data with the AHA guidelines 71 © 2001 Outcome Sciences, Inc.
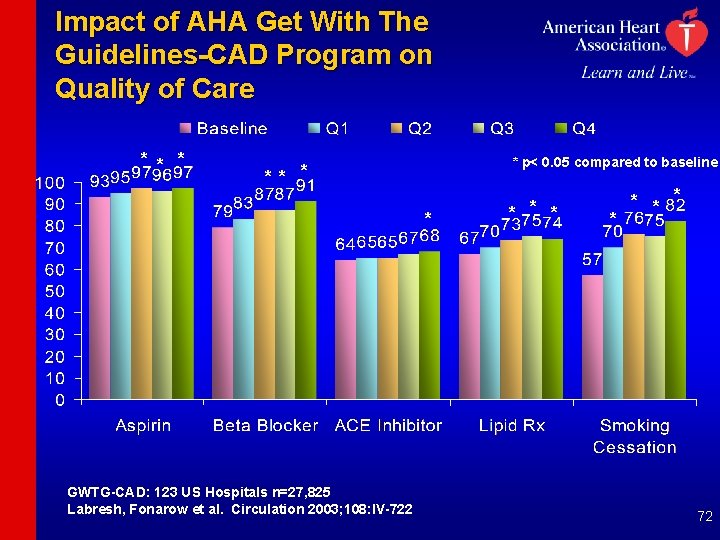
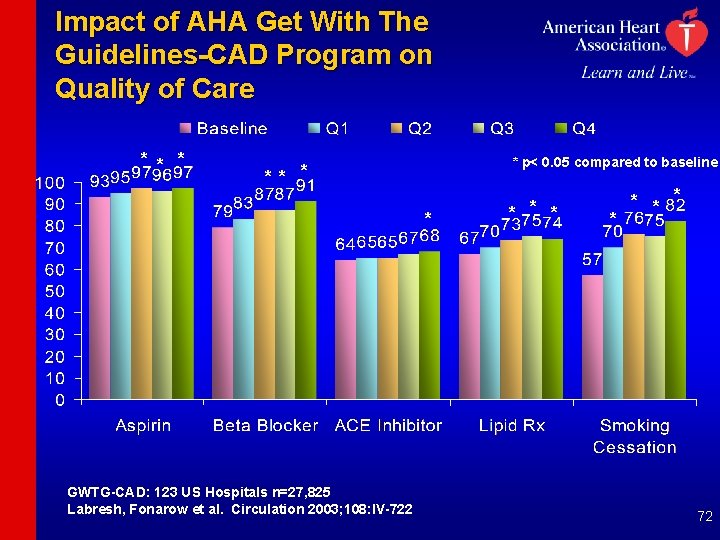
Impact of AHA Get With The Guidelines-CAD Program on Quality of Care * * p< 0. 05 compared to baseline ** * * GWTG-CAD: 123 US Hospitals n=27, 825 Labresh, Fonarow et al. Circulation 2003; 108: IV-722 * * * * 72
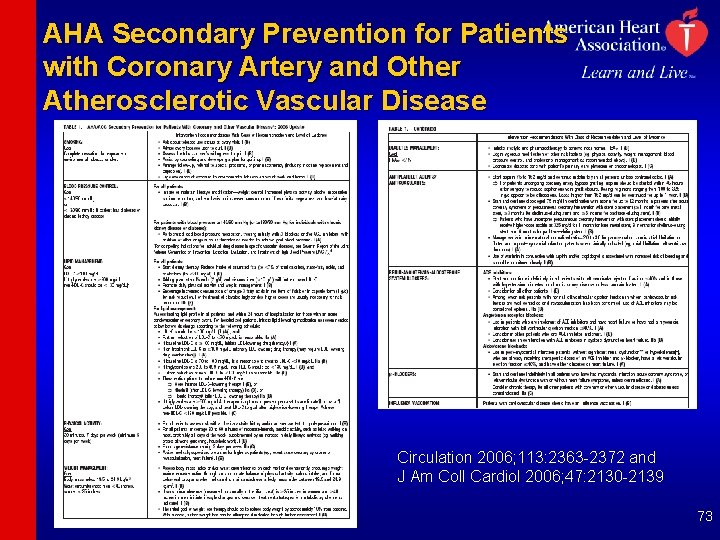
AHA Secondary Prevention for Patients with Coronary Artery and Other Atherosclerotic Vascular Disease Circulation 2006; 113: 2363 -2372 and J Am Coll Cardiol 2006; 47: 2130 -2139 73
Secondary Prevention Conclusions • Evidence confirms that aggressive comprehensive risk factor management improves survival, reduces recurrent events and the need for interventional procedures, and improves the quality of life for these patients. • Every effort should be made to ensure that patients are treated with evidence-based, guideline recommended, life-prolonging therapies in the absence of contraindications or intolerance. 74

75
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Prevention of vte in nonorthopedic surgical patients
Prevention of vte in nonorthopedic surgical patients Secondary prevention
Secondary prevention Secondary prevention
Secondary prevention Specific protection contoh
Specific protection contoh Secondary prevention
Secondary prevention Secondary prevention vte
Secondary prevention vte Secondary prevention
Secondary prevention Nursing management of liver abscess
Nursing management of liver abscess Factors of care that patients can expect to receive
Factors of care that patients can expect to receive Pico questions
Pico questions Write about admission procedure
Write about admission procedure Leadership rounding
Leadership rounding Medicare improvements for patients and providers act
Medicare improvements for patients and providers act Some patients shout in pain while ______ an injection.
Some patients shout in pain while ______ an injection. 10 patients' rights
10 patients' rights Ethical issues in treating lgbt patients
Ethical issues in treating lgbt patients Life expectancy of sickle cell patients
Life expectancy of sickle cell patients Dealing with challenging patients
Dealing with challenging patients Management of patients with neurologic trauma
Management of patients with neurologic trauma Wheeled ambulance stretcher
Wheeled ambulance stretcher Define inadequate
Define inadequate Patients rights charter
Patients rights charter Safe patient handling algorithms
Safe patient handling algorithms Cva
Cva Module 70 introduction to therapy
Module 70 introduction to therapy Jack in the box
Jack in the box Andreas leischker
Andreas leischker Ridge parallelism
Ridge parallelism What is lateral position in nursing
What is lateral position in nursing Semi fowler's position
Semi fowler's position Chapter 36 patients with special challenges
Chapter 36 patients with special challenges Ems lifting techniques
Ems lifting techniques Personal hygiene fundamentals of nursing
Personal hygiene fundamentals of nursing Rostering patients
Rostering patients 13 malaysian safety goals
13 malaysian safety goals Rocking chair therapy for dementia patients
Rocking chair therapy for dementia patients Moving and handling dementia patients
Moving and handling dementia patients Emergency move vs rapid extrication
Emergency move vs rapid extrication Chapter 58 care of patients with liver problems
Chapter 58 care of patients with liver problems Type 2 diabetes diet sheet
Type 2 diabetes diet sheet Nursing care of male patients with genitourinary disorders
Nursing care of male patients with genitourinary disorders Diamond carry ems
Diamond carry ems Periodontal therapy in female patients
Periodontal therapy in female patients How does nurse ratched manipulate the patients
How does nurse ratched manipulate the patients Nursing interventions for stroke patients
Nursing interventions for stroke patients Nurse with ocd
Nurse with ocd Shampoo caps for bedridden patients
Shampoo caps for bedridden patients Diet chart for icu patients
Diet chart for icu patients Nursing diagnosis cataract nursing care plan
Nursing diagnosis cataract nursing care plan Broadmoor inmates
Broadmoor inmates Leader rounding
Leader rounding Lippincott williams & wilkins
Lippincott williams & wilkins Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Lek med former i förskolan
Lek med former i förskolan Bris för vuxna
Bris för vuxna Mat för idrottare
Mat för idrottare Ledarskapsteorier
Ledarskapsteorier Offentlig förvaltning
Offentlig förvaltning Ellika andolf
Ellika andolf Datorkunskap för nybörjare
Datorkunskap för nybörjare Antika plagg
Antika plagg Kontinuitetshantering i praktiken
Kontinuitetshantering i praktiken Steg för steg rita
Steg för steg rita Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Claes martinsson
Claes martinsson Sju principer för tillitsbaserad styrning
Sju principer för tillitsbaserad styrning Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Dikter som rimmar
Dikter som rimmar Tidbok för yrkesförare
Tidbok för yrkesförare Datumr
Datumr Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden Borstål, egenskaper
Borstål, egenskaper Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Jätte råtta
Jätte råtta