PRIMARY AND SECONDARY PREVENTION OF CARDIOVASCULAR DISEASES David
- Slides: 38
PRIMARY AND SECONDARY PREVENTION OF CARDIOVASCULAR DISEASES David R. Musselman, M. D. , F. A. C. C. , F. A. C. P North Texas Heart Center, P. A.
Primary and Secondary Prevention n Primary prevention – preventive measures in patients without diagnosed cardiovascular disease n Secondary prevention – preventive measures in patients with diagnosis of cardiovascular disease n Diabetes mellitus = Cardiovascular disease diagnosis
3 Interventions Types 1. Therapeutic interventions for secondary prevention for patients with known cardiovascular disease (ex. pharmacological interventions) n 2. Identification of high-risk individuals for primary prevention through mass screening or case finding (lipid profiles, BP screening) n 3. General recommendations disseminated throughout the population for primary prevention (ex. dietary and exercise recommendations) n * Implementation requires a practical systematic approach to prioritizing interventions and allocating resources (interventions vary dramatically in cost, both individually and to society) n
Introduction Framingham Heart Study gave modern medicine the term “Risk Factor”-Kannel et al 1961 n Risk Factor-parameter that can predict a future cardiovascular event n Risk prediction-what matters most is the predictive value of the risk factor, the feasibility of assessing it, and the cost of assessment n 4 categories of risk factors n – – predisposing factors risk-modifying behaviors metabolic risk factors disease markers
4 Types Risk Factors n Predisposing factors – Age, gender, family history, genetics n Risk-modifying behaviors – Smoking, atherogenic diet, alcohol intake, sedentary lifestyle n Metabolic risk factors – Dyslipidemia, HTN, obesity, DM, metabolic syndrome n Disease markers – Calcium score, catheterization results, stress test results, LVH, personal history of vascular disease, inflammatory state
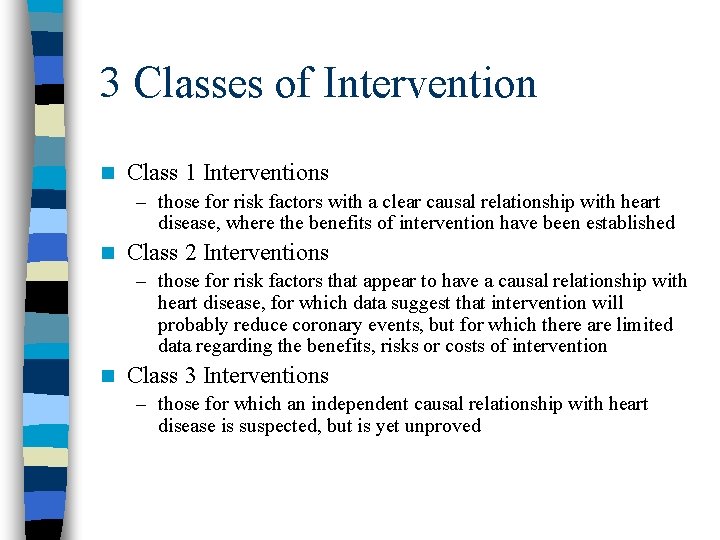
3 Classes of Intervention n Class 1 Interventions – those for risk factors with a clear causal relationship with heart disease, where the benefits of intervention have been established n Class 2 Interventions – those for risk factors that appear to have a causal relationship with heart disease, for which data suggest that intervention will probably reduce coronary events, but for which there are limited data regarding the benefits, risks or costs of intervention n Class 3 Interventions – those for which an independent causal relationship with heart disease is suspected, but is yet unproved
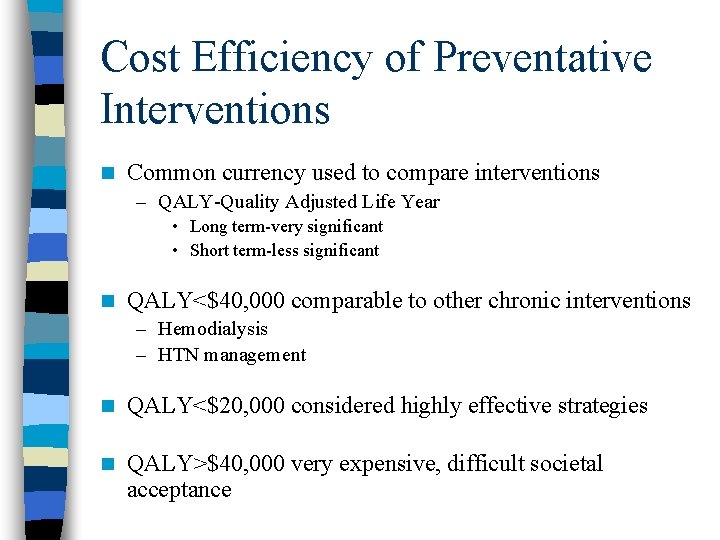
Cost Efficiency of Preventative Interventions n Common currency used to compare interventions – QALY-Quality Adjusted Life Year • Long term-very significant • Short term-less significant n QALY<$40, 000 comparable to other chronic interventions – Hemodialysis – HTN management n QALY<$20, 000 considered highly effective strategies n QALY>$40, 000 very expensive, difficult societal acceptance
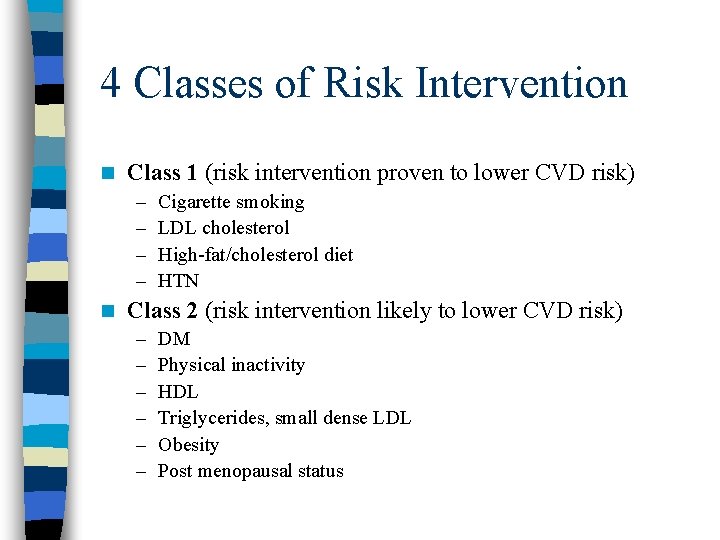
4 Classes of Risk Intervention n Class 1 (risk intervention proven to lower CVD risk) – – n Cigarette smoking LDL cholesterol High-fat/cholesterol diet HTN Class 2 (risk intervention likely to lower CVD risk) – – – DM Physical inactivity HDL Triglycerides, small dense LDL Obesity Post menopausal status
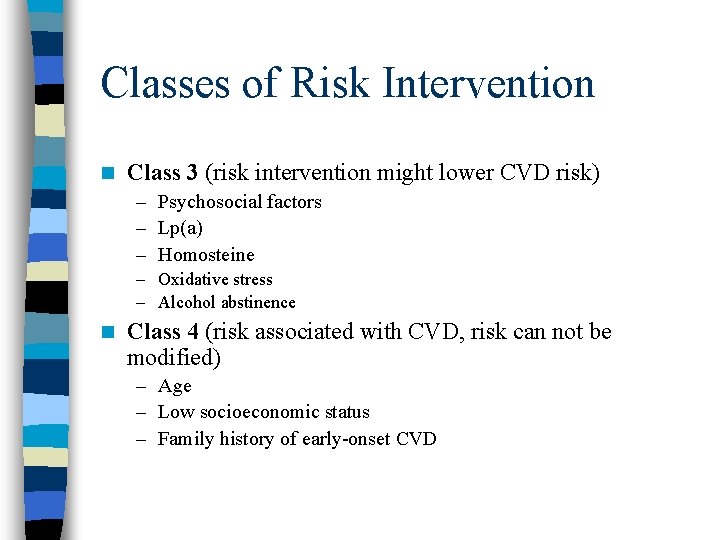
Classes of Risk Intervention n Class 3 (risk intervention might lower CVD risk) – Psychosocial factors – Lp(a) – Homosteine – Oxidative stress – Alcohol abstinence n Class 4 (risk associated with CVD, risk can not be modified) – Age – Low socioeconomic status – Family history of early-onset CVD
Smoking Cessation-Class 1 n Prevalence – increased in the first half of the 20 th century and has been declining since 1963 n Prevalence by gender – Men 25% – Women 21% n Prevalence – greater in African Americans – greater with less education – greater with lower income
Smoking Cessation-Incidence n Smoking doubles incidence of CHD and increases CHD mortality by 50% n Risk increases with number of cigarettes smoked and with age n Smoking causes 440, 000 excess deaths in USA per year, 6 million years of lost life n Smoking rates are rising rapidly in developing countries
Smoking Cessation-Benefits n Smokers who quit reduce risk by 50% (most in the first few months) n After cessation, risk approaches baseline in 5 -15 years n Smoking cessation is highly cost effective – programs cost less than continued smoking – $1100 -$4500 per QALY n Often repeat intervention is needed
Smoking Cessation-Treatment n Counseling and behavioral therapies (6 -18% effective) – Problem solving and skills training – Social support within treatment – Social support outside treatment n Pharmacological therapies (20 -40% effective) – Bupropion (Wellbutrin) – Supplemental nicotine • Gum • Patch • Nasal spray • Lozenge Smoking reduction in not acceptable therapy n Time of cardiac event is opportune time for intervention n
Hypertension-Class 1 n Prevalence – Increases with age (9% at age 19 -24 years, 75 % age>75 years) – African Americans>Whites – Men>Women n Associated risk – The shape of the CVD risk curve with BP is linear – Increment of 20 mm. Hg SBP or 10 mm. Hg DBP doubles risk of CVD n Benefit of intervention – Many randomized trials confirmed the protective effect of treating mild to moderate HTN – 10 mm. Hg decrease in SBP, sustained of 10 years, prevents 1 CVD death in 10 people treated – ALLHAT demonstrated efficacy of thiazide diuretics compared with other agents
Hypertension-Treatment n Treatment Guidelines – Routine BP screening of all adults – JNC-7 Goals • 140/90 for lower risk patients • 130/80 for those with CVD, DM or kidney disease • All patients with BP >120/80 should receive life- style modifications • ALLHAT-Thiazide diuretic should be the first-step antihypertensive therapy n Compelling indications of Individual antihypertensive drug classes • • • CHF-Diuretic, BB, ACE-I, ARB, CCB, AA MI-BB, ACE-I, AA High CVD risk-Diuretic, BB, ACE-I, CCB DM-Diuretic, BB, ACE-I, ARB, CCB Kidney disease-ARB, CCB CVA-Diuretic, ACE-I
Hypertension-Challenges and Costs n Challenges – HTN increasing in the developing world – 40% of those with HTN do not know they have the disease – 1/3 of patients being treated do not reach goal n Cost Efficacy-Detection and management of HTN are highly cost effective – In secondary prevention, using diuretics and BB’s cost is <$10, 000/QALY – In primary prevention, cost $10, 000 -$20, 000/QALY in moderate to severe HTN – Cost may be>$100, 000/QALY with more expensive antihypertensive agents
Hypercholesterolema-Class 1 n Prevalence – Cholesterol levels have been declining since the 1960’s in USA – 1/2 of Americans have cholesterol level >200 mg/dl – 18% have cholesterol levels >240 mg/dl n Associated Risk • 10% increase in total cholesterol is associated with a 20 -30% increase in CVD risk • Elevations early in life are associated with increases in risk
Hypercholesterolema-Benefit of intervention n Clear benefits of treatment have been demonstrated in multiple studies – Patients with established CAD – Patients with CAD, vascular disease or DM with average cholesterol levels – Elderly patients at risk for CAD – Patients following MI of CABG – Patients with several risk factors for CAD • Large Meta-analysis of statin therapy (31, 000 patients) – Duration 5. 4 years – Average reduction of 20% in total cholesterol, 28% in LDL, and 13 % in placebo – Risk reduction 31% in CVD events, 21% all-cause mortality reduction n Long-term compliance is important for successful intervention
Hypercholesterolema-Cost efficiency n Cost efficiency of non-pharmacological interventions is unclear n Pharmacological intervention is clearly cost-effective in secondary prevention – 4 -S Trial -$5, 400/QALY for men, $10, 500/QALY for women – Cost decreases as lipid levels increase – In primary prevention statins fail to reach a cost effective ratio (>$50, 000/QALY) – Calculations are highly sensitive to drug cost – Hopefully drug costs will decrease in the future
Hypercholesterolema-Treatment All CVD patients should be screened n In primary prevention, age of screening is controversial (20 -45 years) n n NCEP (National Cholesterol Education Program)/ATP(Adult Treatment Panel) – ATPIII-Different targets on calculated Framingham risk score • Existing CVD (DM or PVD)-LDL <100 mg/dl • Without CVD – <2 risk factors : LDL<130 mg/dl – Low risk patients : LDL<160 mg/dl n Dietary recommendations – – n 25 -35% fat (<7% saturated) Complex carbohydrates, 50 -60% calories Protein 15% calories High dietary fiber Exercise
Hypercholesterolema-Treatment n Benefits of statins in addition to lipid lowering – – n Anti-proliferative effects Anti-oxidant effects Plaque-stabilizing effects Change in lipid content of plaque New NCEP guidelines-”Lower is better” – Lower LDL goal to <70 mg/dl (CVD of equivalent) – Lower LDL goal to <100 mg/dl (>2 risk factors) – There does not appear to be an LDL below which risk does not fall
HDL and Triglycerides-Class 1 Low HDL and high triglycerides tend to coincide and may occur with or without high LDL levels n Associated risk n – HDL-independent risk factor, 1 mg/dl decrease causes 3 -4% increase in CVD risk – LDL/HDL ratio highly predictive, 1 U decrease in ratio reduces risk by 50% n Benefits of intervention – Gemfibrozil: VA-HIT-22% risk reduction in patients with HDL <40 mg/dl – Niacin therapy n Recommendations – Full fasting lipid profile – Diet and exercise in primary prevention – Pharmacological therapy in secondary prevention
Antiplatlet Agents-Secondary Prevention, Class 1 n ASA in existing CVD reduces subsequent risk by 25% n Unless contraindicated, ASA should be used by most patients n Clopidigril and ticlopidine should be considered for patients with ASA allergy or intolerance n Cost – ASA $11, 000/QALY – Clopidigril $130, 000/QALY
Antiplatlet Agents-Primary prevention n 5 large primary prevention trials of low-dose ASA – Meta-analysis-small benefit in men – Concern regarding increased risk of hemorrhagic stroke – Data on women is limited n Breakpoint – Use low-dose ASA if 10 -year risk of CVD is >6% in men – Ongoing Women’s Health Study addressing risk-benefit ratio in primary prevention
Beta-blockers-Class 1 n Many trials have demonstrated long-term efficacy of BB after MI in mortality reduction – About 25% reduction over long term Many trials have also shown reduction in recurrent CVD events n Greater efficacy of BB with increased beta-blockade as assessed by heart rate reduction n BB effective in CHF, especially carvedilol n BB are highly cost-effective ($11, 000/QALY) n
ACE-I’s and ARB’s-Class 1 n Benefits of ACE-I is large after MI – 7% mortality reduction at 30 days with normal LVEF – 26% mortality reduction at 30 days with low LVEF n HOPE Trial demonstrated 22% reduction in major clinical events in low risk patients without CVD, DM or CHF n CHARM-Use of candesartin in patients with CHF prevents – 1 death per 63 patients treated – 1 hospitalization per 23 patients treated – 1 new case of DM per 71 patients treated
Diabetes mellitus and metabolic syndrome-Class 2 n Prevalence – – n 6% of US population 90% of DM is Type 2 1/3 of people with disease are unaware of its presence Incidence increases with increasing BMI Associated risk – Very powerful risk factor for CVD – CVD causes 69% of deaths in DM patients – 7 -8 fold increase in CVD risk, compared with age-matched population without DM
Obesity-Class 2 Prevalence-2/3 of US population has BMI>25, considered over weight or obese n Early obesity is considered a strong marker of CVD risk n – Whether excess weight is an independent risk factor for CVD is unclear because of other risk factors and metabolic disorders associated with obesity Abdominal adiposity associated with greater risk (waist circumference 35” in women, 40” in men) n No randomized trial of weight reduction, as an isolated intervention, to evaluate benefits of lowering risk of CVD n However, even modest weight loss improves lipids, glycemic control, BP and sleep apnea n
Obesity-Class 2 Little consensus on ideal approach to weight reduction n Failure rates are exceedingly high n Cost effectiveness data are unavailable n A multi-factorial approach seem most effective n – – – n Dietary counseling Behavioral modification Increased physical activity Psychosocial support Pharmacological therapy and bariatric surgery Recommendations for intervention – All patients with BMI>30 – CVD patients or >2 risk factors with BMI>25
Physical inactivity-Class 2 n Prevalence – 75% or Americans do not meet the current recommendations of 30 minutes of leisure-time physical activity on most days of the week – One-third do not engage in any physical exercise – Exercise for children has declined and sedentary activities has dramatically increased Data from 40 observational studies demonstrate an inverse doseresponse relationship between volume of physical activity and allcause mortality n Energy expenditure of 1000 kcal/week reduces all-cause mortality by 30% n CVD risk in sedentary individuals is doubled compared with physically active individuals, when controlled for other CVD risk factors n
Physical inactivity-Class 2 n Activity can be as simple as brisk walking n Mortality reduction benefits are also present in the elderly who initiate new exercise programs n Exercise also reduced the risk of stroke and new onset DM n However, there is no large-scale randomized trials of physical activity in primary prevention n In secondary prevention, regular exercise reduces mortality by 25% n Exercise clearly has beneficial effects on other CVD risk factors (increase HDL, reduce LDL, lower BP, increase insulin sensitivity) n Recommendations: 30 -60 minutes of moderate activity on most days of the week (primary and secondary prevention)
Anticoagulants-Class 2 n Role is uncertain as the results of randomized trials is inconsistent n In meta-analyses, high and medium-intensity oral anticoagulation reduced MI and stroke rates, but increased bleeding complications n Low intensity anticoagulation does not appear to confer benefit over ASA alone
Postmenopausal estrogen therapy -Class 3 n Before age 45, CVD is rare in women. After age 60 CVD is the leading cause of death. The gap in CVD rates between men and women narrows after menopause (and oophorectomy) n After menopause, LDL rises, HDL falls, insulin resistance increases, vascular function decline and there adverse changes in coagulation n Physiological effects of supplemental are consistent with a cardioprotective effect
Postmenopausal estrogen therapy -Class 3 n Meta-analyses of 40 cohort studies suggested a 50% reduction in CVD risk. This was true for primary and secondary prevention n Data from 7 randomized trials not only failed to support a benefit of hormone therapy, but actually demonstrated an increased CVD risk n HERS Trial (secondary prevention)-no CVD benefit n Hormone therapy is no longer recommended to prevent CVD
Psychosocial factors-Class 3 n Depression, chronic hostility, social isolation, lack of social support have been consistently linked with CVD n Data on intervention is limited and confounded by difficulty in measurement and inconsistent definitions n One meta-analysis of 37 studies demonstrated a 29% reduction in recurrent MI and 34% in total mortality with reduction in psychosocial stressors n SADHART and ENRICHD studies, pharmacologic treatment of depression after MI, reduced second MI rates, CHF, recurrent angina and CVD death rates
Dietary Factors-Class 3 n Observational factors have suggested that a number of dietary factors may increase CVD risk n Ni-Hon-San Study-Japanese immigrants to Hawaii and California n Observational studies – – – n Diet high fruit and vegetables-lower CVD risk High fat and trans-fat diets-higher CVD risk Diet high in simple carbohydrates-higher CVD risk Low fiber diets-higher CVD risk Diets high in omega-3 fatty acids-lower CVD risk “Mediterranean diet”-lower CVD risk (secondary prevention study) Specific foods and nutrients – – Whole grains, fiber, fish oils, soy protein, folate, vitamin B 6, Vitamin E, coenzyme Q 10 observational studies suggest lower rates of CVD risk Vitamin E-in randomized trials, little effect on CVD risk, possibly a detrimental effect
Novel biochemical markers-Class 3 n CRP-only marker to add prognostic information over and above Framingham risk scoring n CRP best used as an adjunct to risk prediction among those at intermediate risk n EBCT-very expensive n Homocysteine-predicts risk, however data on treatment efficacy (folate, B 6. and B 12) is lacking n Other markers – – Lp(a) Interleukin-6 Phospholipase A 2 Factor V Leiden
Multiple Risk Factor Intervention Programs n Measure the impact of several risk factors simultaneouslyanalogous to clinical practice n WHO Trial (World Health Organization Trial)-substantial CVD risk reduction with multi-risk-factor approach n In general data is lacking
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 What are deficiency
What are deficiency Contoh tertiary prevention
Contoh tertiary prevention Recurvte
Recurvte Secondary prevention
Secondary prevention Secondary prevention
Secondary prevention Secondary prevention
Secondary prevention Secondary prevention
Secondary prevention Health education activities
Health education activities Primary prevention examples
Primary prevention examples Primary prevention of poliomyelitis
Primary prevention of poliomyelitis Anatomy and physiology unit 7 cardiovascular system
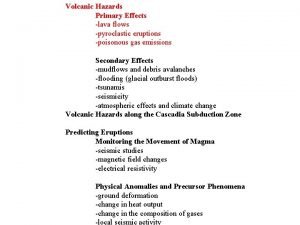
Anatomy and physiology unit 7 cardiovascular system Primary and secondary effects of a tectonic hazard
Primary and secondary effects of a tectonic hazard Secondary stakeholders
Secondary stakeholders Pink
Pink Pinotubo
Pinotubo Use case primary and secondary actors
Use case primary and secondary actors Pengertian include dan extend
Pengertian include dan extend Introduction to transformer
Introduction to transformer Thyroid storm tsh levels
Thyroid storm tsh levels Primary and secondary retroperitoneal organs
Primary and secondary retroperitoneal organs Difference between primary and secondary succesion
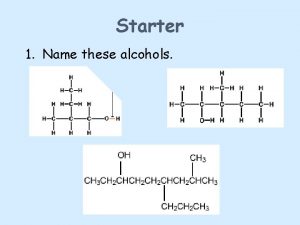
Difference between primary and secondary succesion Ketone to tertiary alcohol
Ketone to tertiary alcohol Purpose of project planning
Purpose of project planning Secondary socializing agents
Secondary socializing agents Primary and secondary deviance
Primary and secondary deviance Bronchiole
Bronchiole Setline planting in gujarat
Setline planting in gujarat Primary secondary and tertiary sources
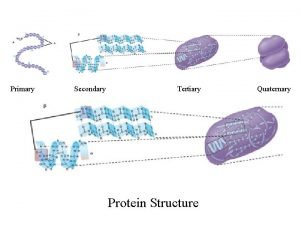
Primary secondary and tertiary sources Secondary and tertiary structure
Secondary and tertiary structure Secondary sources
Secondary sources Secondary light sources
Secondary light sources Secondary reinforcer definition
Secondary reinforcer definition Symport
Symport Primary needs and secondary needs
Primary needs and secondary needs Pustule
Pustule Pith
Pith Membrane structures that function in active transport
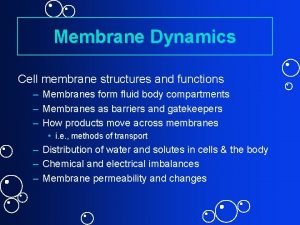
Membrane structures that function in active transport