VASCULITIS Vasculitis is a heterogeneous group of disorders

- Slides: 58
VASCULITIS
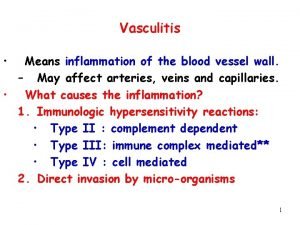
• Vasculitis is a heterogeneous group of disorders linked by the primary finding of inflammation within blood vessel walls. At least 20 forms of systemic vasculitis are recognized currently. • Vasculitides are classified first by the size of blood vessel involved—small (capillaries and postcapillary venules), medium (muscular arteries and arterioles), or large (the aorta and its major branches).
• Additional considerations in classification include patient demographics, organ tropism, presence or absence of granulomatous inflammation, participation (or not) of immune complexes, finding of autoantibodies, and detection of infections associated with some vasculitides. • Associations between genes and vasculitis have been recognized increasingly in recent years. There also has been progress in the area of geneenvironment interactions.
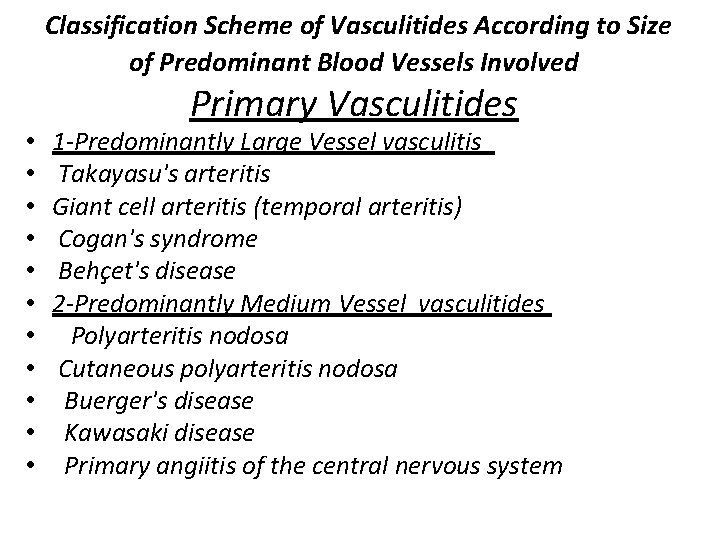
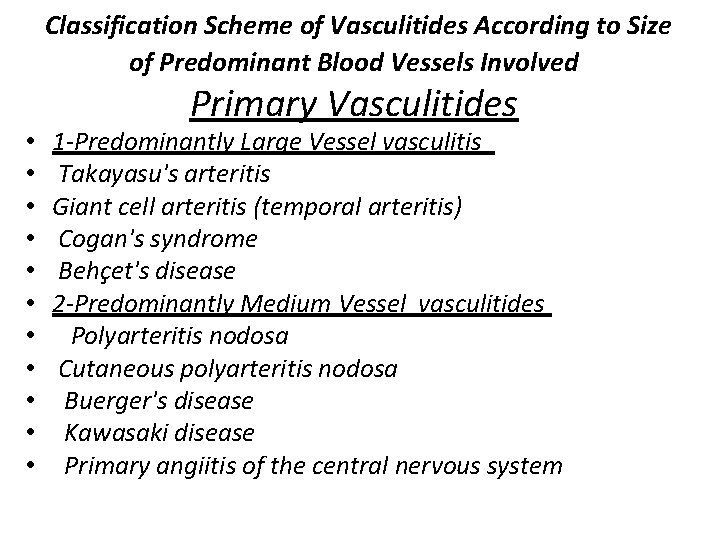
Classification Scheme of Vasculitides According to Size of Predominant Blood Vessels Involved • • • Primary Vasculitides 1 -Predominantly Large Vessel vasculitis Takayasu's arteritis Giant cell arteritis (temporal arteritis) Cogan's syndrome Behçet's disease 2 -Predominantly Medium Vessel vasculitides Polyarteritis nodosa Cutaneous polyarteritis nodosa Buerger's disease Kawasaki disease Primary angiitis of the central nervous system
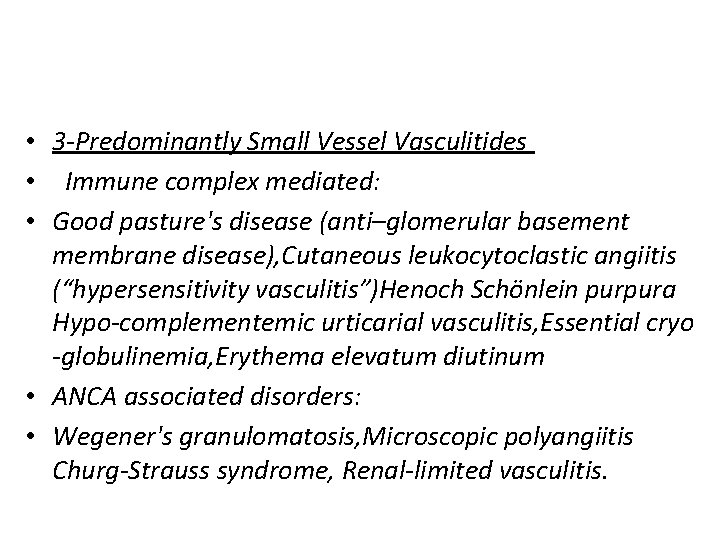
• 3 -Predominantly Small Vessel Vasculitides • Immune complex mediated: • Good pasture's disease (anti–glomerular basement membrane disease), Cutaneous leukocytoclastic angiitis (“hypersensitivity vasculitis”)Henoch Schönlein purpura Hypo-complementemic urticarial vasculitis, Essential cryo -globulinemia, Erythema elevatum diutinum • ANCA associated disorders: • Wegener's granulomatosis, Microscopic polyangiitis Churg-Strauss syndrome, Renal-limited vasculitis.
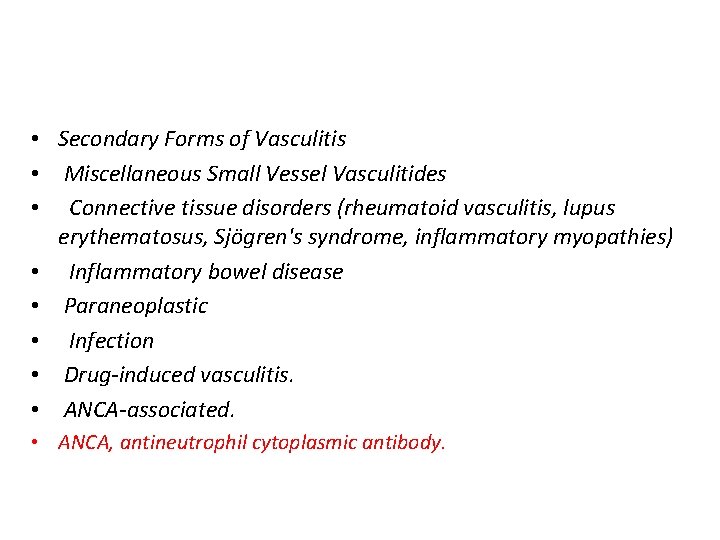
• Secondary Forms of Vasculitis • Miscellaneous Small Vessel Vasculitides • Connective tissue disorders (rheumatoid vasculitis, lupus erythematosus, Sjögren's syndrome, inflammatory myopathies) • Inflammatory bowel disease • Paraneoplastic • Infection • Drug-induced vasculitis. • ANCA-associated. • ANCA, antineutrophil cytoplasmic antibody.
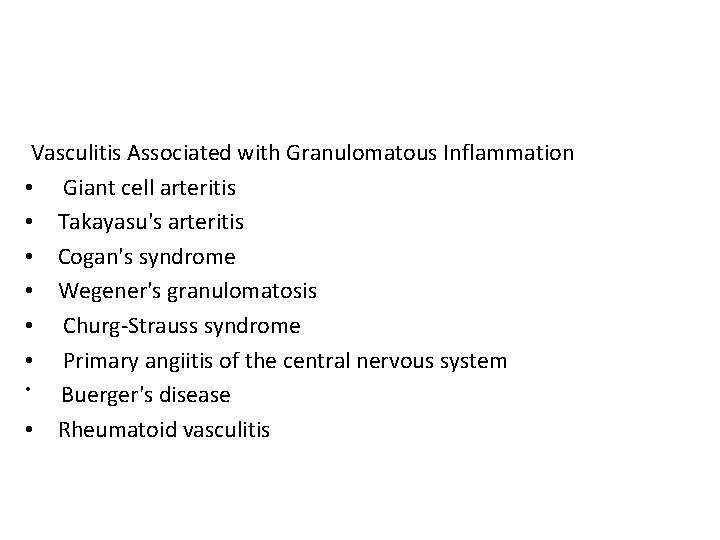
Vasculitis Associated with Granulomatous Inflammation • Giant cell arteritis • Takayasu's arteritis • Cogan's syndrome • Wegener's granulomatosis • Churg-Strauss syndrome • Primary angiitis of the central nervous system • Buerger's disease • Rheumatoid vasculitis
Epidemiology • AGE & GENDER • Age is an important consideration in the epidemiology of vasculitis. Of patients with Kawasaki disease, 80% are younger than age 5 years. In contrast, giant cell arteritis virtually never occurs in patients younger than age 50, and the mean age of patients with that disease is 72. • Age also may affect disease severity and outcome. In Henoch-Schönlein purpura, most cases in children (who comprise 90% of all cases) have self-limited courses, resolving within several weeks. In adults, Henoch. Schönlein purpura may have a higher likelihood of chronicity and a greater likelihood of a poor renal outcome.
• The distribution of gender varies across many forms of vasculitis. Buerger's disease is the only form of vasculitis with a striking male predominance. The predilection of this disease for men may be explained by the greater prevalence of smoking among men in most societies. • In contrast, Takayasu's arteritis has an overwhelming tendency to occur in women (a 9: 1 female-to-male ratio), a fact that presently has no explanation
• GENES • Although genetic risk factors are undoubtedly important in the susceptibility to some forms of vasculitis, familial cases are rare (with the exception of giant cell arteritis ). The rarity of familial cases in vasculitis indicates that the genetics of these disorders are polygenic and complex. The strongest link between any single gene and vasculitis is the association of HLA-B 51 with Behçet's disease. In Behçet's disease, 80% of Asian patients have the HLA-B 51 gene. • HLA-B 51 increases disease severity. Patients with this gene are more likely to have posterior uveitis, central nervous system involvement, or other severe manifestations.
• Reports of familial aggregation in giant cell arteritis are common. Genetic studies have indicated roles for HLA class II alleles such as HLA-DRB 1∗ 0401 and HLA-DRB 1∗ 0101, albeit the specific associations have varied from study to study. Other work indicates that certain tumor necrosis factor microsatellite polymorphisms may contribute to disease susceptibility
• ENVIRONMENT • Several environmental and occupational exposures have been linked to the development of vasculitis. The strongest environmental exposure, now linked convincingly to Buerger's disease and to rheumatoid vasculitis, is cigarette smoking. Buerger's disease does not occur in the absence of cigarette smoking. The relationship between smoking and Buerger's disease is usually one of primary exposure (usually heavy), but cases related to second-hand smoke have been alleged. • Associations have been reported, but not confirmed, between exposure to inhaled silica dust and some types of pauci-immune vasculitis
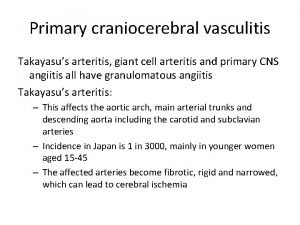
TAKAYASUS ARTERITIS • Takayasu's arteritis (TA), also known as pulseless disease or occlusive thromboaortopathy, is a form of vasculitis of unknown cause that chiefly affects the aorta and its major branches, most frequently in young women. • American College of Rheumatology Classification Criteria for Takayasu's Arteritis : • Onset before age 40 yr • Limb claudication • Decreased brachial artery pulse • Unequal arm blood pressure (>10 mm Hg) • Subclavian or aortic bruit • Angiographic evidence of narrowing or occlusion of aorta or its primary branches, or large limb arteritis
• CAUSE AND PATHOGENESIS • The geographic clustering of cases has suggested that genetics and environmental factors participate in the pathogenesis of TA. The young age of onset and the female predominance in TA have invited speculation about the influence of female hormones in promoting an autoimmune disease process. • Clinical Features of Takayasu's Arteritis • Feature At Presentation : Vascular Bruit , Claudication (upper extremity) Claudication (lower extremity) , Hypertension , Unequal arm blood pressures Carotidynia , Aortic regurgitation , Central nervous system Lightheadedness Visual abnormality Stroke • Musculoskeletal : Chest wall pain, Joint pain, Myalgia. • Constitutional : Malaise , Fever , Weight loss. • Cardiac: Aortic regurgitation , Angina , Congestive heart failure.
Investigation • At presentation, the ESR is more frequently elevated (80%) than the CRP (≈50%). Mild anemia and hypergammaglobulinemia are common. The white blood cell count is usually normal or slightly elevated. The platelet count is elevated in one third of patients and may exceed 500, 000/μL in those with active disease. • The serum creatinine and urinalysis are usually normal. Any renal abnormalities are usually secondary to hypertension; unlike antineutrophil cytoplasmic antibody–associated vasculitis, TA rarely causes glomerulonephritis.
• Imaging Studies • Vascular abnormalities in TA can be imaged by conventional angiography, MRI, MRA, CT angiography, or ultrasonography. • Each imaging technique has advantages and disadvantages The earliest detectable abnormality in TA is thickening of the vessel wall from inflammation. MRI, ultrasonography, and to a lesser degree CT can detect this early vessel wall thickening. • stenoses, occlusions, and aneurysms that characterize the latter stages of TA Also, can be detected by imging only conventional angiography allows the direct measurement of central arterial blood pressure, which may be otherwise unobtainable in patients with stenotic lesions affecting all four extremities.

• Although MRA does not provide the same level of detail as conventional angiography, it comes close. Because MRA is not invasive and does not involve ionizing radiation, it has become the preferred imaging method for following patients with TA.
Diagnosis • As previously noted, the ACR has established classification criteria for the diagnosis of TA In clinical practice, the diagnosis of TA is almost always secured by an imaging procedure that demonstrates the characteristic abnormalities of the aorta and its major branches • Rarely, the diagnosis is first suggested when a pathologist finds granulomatous inflammation in a section of aorta or other larger artery that was removed or biopsied during a vascular surgery procedure • a few patients with TA present chiefly with FUO. Most of these patients have other, albeit subtle, manifestations of TA such as bruits, diminished pulses, unequal arm blood pressures, or aortic regurgitation. In other patients with more striking vascular abnormalities
• the physician may be lured into focusing on familiar and dramatic abnormalities such as anemia or thrombocytopenia. • Thus, instead of ordering an imaging test that would explain the patient's unequal and low blood pressure in her left arm, the physician mistakenly diverts the patient to a hematologist, gastroenterologist, or oncologist for additional blood tests and procedures that further delay the diagnosis.
TREATMENT • Medical Therapy • Corticosteroids are the cornerstone of treatment of active TA Prednisone, at a dose of 0. 5 to 1 mg/kg per day, is indicated for the treatment of active disease. Criteria for active disease include new onset or worsening of two or more of the following: • (1) fever or other systemic features (in the absence of other cause), • (2) elevated ESR • (3) symptoms or signs of vascular ischemia or inflammation (e. g claudication, absent pulse, carotidynia). • (4) typical angiographic lesions. Although about 85% of TA patients present with active disease, about 15% do not The initial dose of prednisone is continued for 4 to 12 weeks before commencing a gradual taper,
• Relapses can be treated by increasing the prednisone dose or adding an immunosuppressive agent. • weekly oral methotrexate (started at 0. 3 mg/kg per week, with the initial dose not to exceed 15 mg/wk) is a moderately effective corticosteroid-sparing drug. • other corticosteroid-sparing drugs include azathioprine (2 mg/kg per day), mycophenolate mofetil (2000 mg/day), and cyclophosphamide (2 mg/kg per day • Surgical treatment by revascularization procedure
Wegeners granulomatosis • WG is a granulomatous necrotizing vasculitis characterized by a predilection to affect the upper and lower respiratory tracts and, in most cases, the kidneys. • WG affects both sexes equally, occurs in patients of all ages. • The cause of WG is unknown. Sporadic efforts have been made to identify a genetic predisposition to WG, and a higher prevalence of human leukocyte antigen (HLA)-DR 1 and HLA -DQw 7 has been reported among a small number of patients with WG. However, larger studies failed to identify any unique genetic markers • Although the association of PR 3 -ANCA antibodies and WG is now well established, the pathogenic role of these antibodies remains unclear.
• Clinical studies have documented that PR 3 -ANCA antibodies are highly specific for WG (90% to 97%). They are almost always present in active, generalized WG • Evidence of T cell involvement in WG is less direct than that supporting the pathogenic effect of ANCA. Biopsies of various tissues reveal the presence of polymorphonuclear and mononuclear infiltrates, the latter consisting of plasma cells, monocytes, and T cells, with a predominance of CD 4+ cells.
CLINICAL FEATURES • As stated earlier, WG is characterized by a predilection for the upper and lower respiratory tracts and the kidneys. • Relatively mild forms of WG without renal involvement have been described. The course of illness may be indolent or rapidly progressive • Upper airway disease is the most common presenting feature of WG. Otologic manifestations is an important part of clinical manifestations • Serous otitis media is the most common ear problem. It may be complicated by the presence of a suppurative infection in up to 25% of cases.
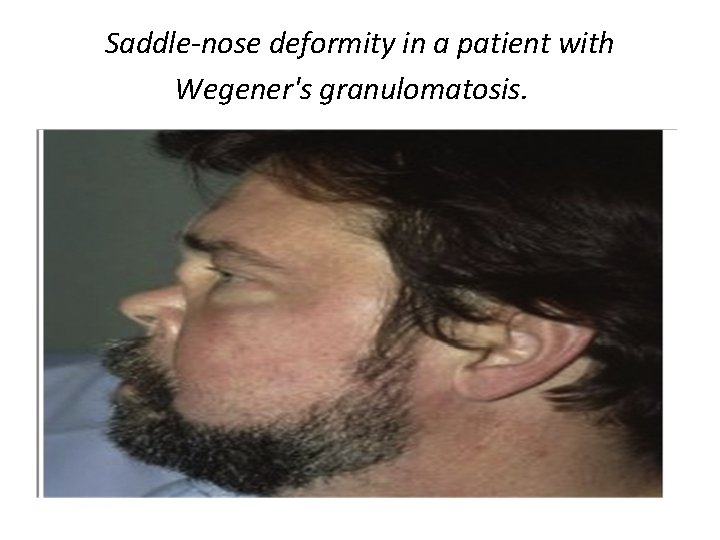
• Significant degrees of hearing loss (mostly conductive) may occure in patients wit WG. Inner ear manifestations include sensori-neural hearing loss and rarely vertigo. • Nasal disease is a prominent presenting feature in patients wit WG. • Symptoms and signs of nasal involvement in WG include mucosal swelling with nasal destruction, crusted nasal ulcers and septal perforations, serosanguineous discharge, epistaxis and external saddle-nose deformity.
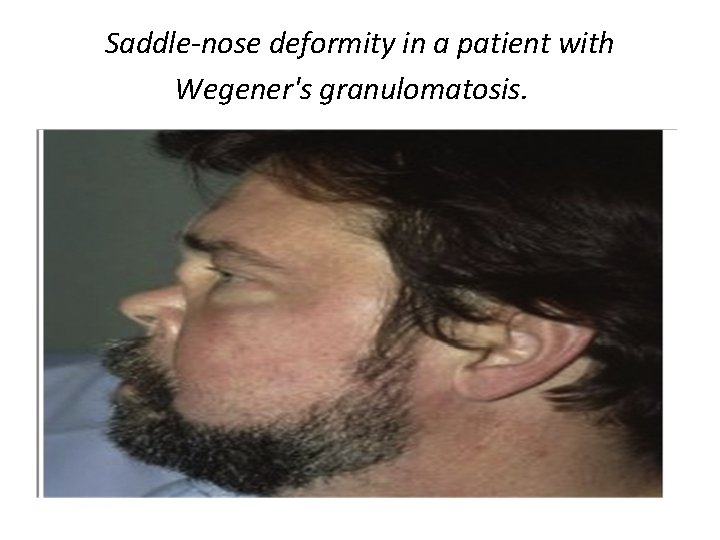
Saddle-nose deformity in a patient with Wegener's granulomatosis.
• • Sinusitis is present at initial presentation. Most patients with sinus or nasal disease eventually develop a secondary infection of these tissues; Staphylococcus aureus is the predominant organism identified from cultures. • Although laryngo-tracheal disease in WG may be asymptomatic, the clinical presentation can range from subtle hoarseness to strider and lifethreatening upper airway obstruction.
• Pulmonary Manifestations • Pulmonary involvement is one of the cardinal features of WG. Cough, hemoptysis, and pleuritis are the most common pulmonary symptoms. • The most common radiographic findings include pulmonary infiltrates. The pulmonary infiltrates in WG may be quite fleeting, appearing and resolving in some cases before the institution of therapy. • Persistent, diffuse interstitial infiltrates are rare (<1%) and should suggest other diagnoses.
• Pulmonary nodules in WG are usually multiple and bilateral and often cavitate (50%). CT of the chest may reveal infiltrates and nodules. • In patients presenting with pulmonary symptoms, it is imperative to make every effort to exclude the presence of infection in a timely fashion, because pneumonia in an immuno-compromised host can result in up to 50% mortality.
• Renal Manifestations • The presence or absence of renal disease defines the subsets of generalized and limited WG, respectively. • in patients thought to have limited WG and dictates the need for careful and close monitoring of renal status in all patients. • Extrarenal manifestations often precede renal disease. Once present, renal disease may progress from asymptomatic and mild to fulminant glomerulonephritis within days or weeks, resulting in end-stage renal failure. • If untreated, mean survival time for this subset of patients is about 5 months.
Ocular Manifestations • Ocular manifestations reportedly occur in patients with WG and may be part of the initial presentation. Any compartment of the eye can be affected. • Keratitis, conjunctivitis, scleritis, episcleritis, nasolacrimal duct obstruction, uveitis, retro-orbital pseudotumor with proptosis , retinal vessel occlusion, and optic neuritis have all been described. • Vision loss may occur in as many as 8% of patients. Although most ocular findings are nonspecific, proptosis is a diagnostically helpful finding , but it is a poor prognostic sign; about half of patients with proptosis in one series lost vision due to optic nerve ischemia
• The cutaneous manifestations of WG include ulcers, palpable purpura, subcutaneous nodules, papules, and vesicles. Although cutaneous lesions rarely dominate the clinical picture, they do tend to parallel disease activity in other organs. • Musculoskeletal Manifestations Although most patients experience only arthralgias and myalgias, arthritis is observed in up to 28% of patients. • When synovitis is present, several patterns can be observed, including monarticular disease, migratory oligoarthritis, and symmetric or asymmetric polyarthritis of small and large joints. Symmetric polyarthritis of small and large joints may be mistaken for RA.
• Multiple neurologic complications may occur. Peripheral neuropathy is the most common single neurologic manifestation of WG. • Mononeuritis multiplex is the most frequent clinical pattern followed by a distal and symmetric polyneuropathy. • cerebral vasculitis, pituitary involvement, cerebral hemorrhage or thrombosis, and cranial neuropathies can all occur. Cerebrovascular events, may include cerebral or brainstem infarction, subdural hematoma, and subarachnoid hemorrhage. • Diffuse meningeal and periventricular white matter disease, presumably reflecting CNS vasculitis, has been reported in patients presenting with diffuse and focal CNS symptoms.
TREATMENT • Glucocorticoids • In WG, glucocorticoids are most commonly used in combination with cytotoxic agents. Although palliation of limited, indolent disease may be achieved with glucocorticoids alone, disease progression and relapses usually occur. • Cyclophosphamide • Combination therapy with daily oral cyclophosphamide and glucocorticoid has been considered the standard therapy for WG. Oral cyclophosphamide is generally initiated at doses of 2 mg/kg per day. • Azathioprine • for the maintenance of remission in patients with WG and MPA. • Methotrexate • Low-dose methotrexate (MTX), such as 0. 05 to 0. 3 mg/kg per week, has been used to treat a variety of autoimmune diseases • Intravenous Immunoglobulin • Tumor Necrosis Factor Inhibitors
CHURG-STRAUSS SYNDROME • characterized by three histopathologic features: necrotizing vasculitis, infiltration by eosinophils, and extravascular granulomas. • diagnosis be based on clinical and pathologic grounds requiring three criteria: asthma, peak eosinophil count greater than 1500 cells/m. L, and systemic vasculitis involving two or more organs • The cause of CSS is unknown, but its association with allergy and atopic disorders is a dominant factor. Nearly 70% of patients have a history of allergic rhinitis, often associated with nasal polyposis; the association with asthma, usually adult onset, is part of most case definitions. • Both peripheral blood and tissue eosinophilia is a major constituent of the syndrome, and the majority of patients tested have elevated Ig. E levels.
• CSS has been reported to occur in asthmatics following the use of either lipoxygenase inhibitors or cysteinyl leukotriene receptor type 1 antagonists, • thereby raising the concern that leukotriene inhibition might function as a causative factor. • Alternative explanations include an unmasking effect when these drugs are provided to a population with severe airway disease, followed by steroid tapering. • simple unmasking effect is unlikely, however, in patients who were not on steroids or did not taper the dose of steroids before the onset of CSS.
CLINICAL FEATURES • CSS is thought by some observers to be characterized by three distinct phases. A prodrome, dominated by allergic features, is common in patients ultimately diagnosed with CSS. • Allergic rhinitis and asthma often precede the diagnosis of vasculitis by 3 to 7 years. • ANCA may influence the expression of the disease in certain organs. ANCA positivity, for example, is associated with a higher incidence of renal disease (particularly rapidly progressive glomerulonephritis), alveolar hemorrhage, mononeuritis multiplex, and purpura. • In contrast, ANCA-negative patients were more likely to suffer from cardiomyopathy, nonhemorrhagic pulmonary infiltrates, nasal polyposis, and eosinophilic gastritis or enteritis.
• Pulmonary Manifestations Pulmonary infiltrates may occur in the prodromal phase, vasculitic phase, or both, and their appearance is generally nonspecific. • Their radiographic appearance is variable, but lobar, interstitial, and nodular patterns have all been described, with most abnormalities being fleeting in nature. • Pleural effusions were reported in 27% of patients in one series and are typically rich in eosinophils. Pulmonary hemorrhage is a grave complication and may occur with or without renal involvement.
• Neurologic Manifestations Peripheral neurologic involvement often dominates the clinical picture and has been reported in the majority of patients It was found in 62% of patients in one series. • The pattern of involvement may be that of mononeuritis multiplex or symmetric or asymmetric polyneuropathy. Less commonly, cranial neuropathy is observed. • CNS involvement is uncommon and tends to dominate in the latter stages of the illness. Collectively, involvement of the peripheral nervous system is so common that in any patient with asthma who develops neurologic symptoms, CSS should be considered.
• Renal Manifestations Kidney involvement is less common in CSS than in MPA or WG and, when present, is rarely the cause of death. • CSS shares the same renal lesion (necrotizing crescentic pauci-immune glomerulonephritis) with the other ANCA-associated diseases. A noteworthy feature of CSS is its propensity to involve the lower urinary tract, including the prostate gland. • We have seen extremely high levels of prostatespecific antigen in the setting of active CSS normalize during successful treatment. Such lower urinary tract involvement may lead to obstruction.
• LABORATORY TESTS • Peripheral eosinophilia at levels in excess of 1500 cells/mm 3 often occurs in the prodromal stages of CSS, associated with rhinitis and asthma. • Occasionally, patients have been described without significant blood eosinophilia but with prominent tissue eosinophilia. • There is no definite correlation between eosinophilia and disease activity, for eosinophils often rapidly decrease on initiation of glucocorticoid therapy. • ANCAs have been reported in about 40% of patients , the majority of which are MPO-ANCA. A negative ANCA test should not dissuade the clinician from the diagnosis of CSS if there is a high probability.
TREATMENT • Therapeutic trials are limited, but they have demonstrated that both glucocorticoid alone and glucocorticoid combined with cyclophosphamide are efficacious. • it appears reasonable to treat patients with limited disease with glucocorticoid alone and reserve combined therapy for those with immediately lifethreatening or major organ–threatening disease. • Patients who should be considered for combined therapy are those with severe disease The principles of such therapy are similar to those outlined for the treatment of WG.
POLYARTERITIS NODOSA • Polyarteritis nodosa (PAN) is a necrotizing vasculitis of mediumsized arteries. Immune deposits are minimal or absent. Test results for antineutrophil cytoplasmic antibodies (ANCAs) are typically negative. • Patients with classic PAN can be any age, including children, but the peak onset is in the fifth or sixth decade • PATHOLOGY • PAN is a patchy disease, with areas of impressive necrosis and inflammation interspersed with unaffected vessels There is a propensity for aneurysm formation, especially in the mesenteric circulation. Other target organs include the kidney, the peripheral nerves, and the heart. There is strong correlation between the amount of fibrinoid necrosis and the number of neutrophils in the vessel wall and surrounding tissues. • Probably the most popular biopsy site today is the sural nerve.
• SYSTEMS INVOLVED IN POLYARTERITIS NODOSA • Cutaneous manifestations occur in one third of patients, usually seen as areas of palpable purpura, sometimes with ulceration • Hypertension, owing to arteritis in the renal circulation, is present in approximately one third of cases and is occasionally severe • The term mononeuritis multiplex is applied to the widespread development of neuropathy involving large, mixed motor and sensory nerves • Frequently affected nerves include the peroneal, median, ulnar, and sural nerves. The nerve injury is due to ischemia and eventual infarction. • Abdominal pain, owing to mesenteric vasculitis, is usually dull and constant, but it is often worsened by eating
• The liver is frequently involved at autopsy, but clinical involvement is uncommon • The testicle also is a frequent site of involvement in autopsy series, and testicular pain is occasionally seen • Kidney involvement usually manifests only as hypertension, often with mild-to-moderate azotemia. There is no glomerulitis, and the urinalysis usually shows only moderate proteinuria with modest hematuria, or the sediment may be entirely normal.
THERAPY • Treatment consists of prednisone, 1 mg/kg/day in divided doses, and, in most cases, an additional agent, usually a cytotoxic drug. • Cyclophosphamide has been the drug of choice • Alternatives to cyclophosphamide are chlorambucil, azathioprine, methotrexate, dapsone, cyclosporine, plasma exchange, and others. • The use of high-dose intravenous methylprednisolone (≤ 1 g/day) is recommended occasionally in cases of fulminant vasculitis
Giant cell arteritis • GCA is the most common form of systemic vasculitis in adults. The disease affects primarily the extracranial branches of the carotid artery in patients older than 50 years. The most feared complication of GCA is irreversible loss of vision • Classic Manifestations • The most common manifestations of GCA are constitutional symptoms, headache, visual symptoms, jaw claudication, and PMR. Almost all patients experience one or more constitutional symptoms, including fatigue, weight loss, malaise, and fever.
• Relationship between Polymyalgia Rheumatica and Giant Cell Arteritis. There is abundant evidence that PMR and GCA are related and should be considered different manifestations of a common disease process. • The associations with age, ethnicity, geographic region, and HLA class II alleles are the same in both disorders. Moreover, both disorders involve overproduction of many of the same inflammatory cytokines. Between 30% and 50% of patients with GCA develop PMR. • Approximately 10% to 15% of patients who appear to have only PMR have positive temporal artery biopsies. • In the absence of symptoms of GCA (e. g. , headache, jaw claudication, visual symptoms, high fever), PMR by itself does not appear to cause vision loss and responds to low doses of glucocorticoids.
• LABORATORY STUDIES • Except for the findings on arterial biopsy, laboratory results in PMR and GCA are similar A mild to moderate normochromic anemia is usually present in both diseases during their active phases. • Leukocyte and differential counts are generally normal. A markedly elevated ESR and C- reactive protein (CRP) level are characteristic of both. • An ESR higher than 100 mm/hr (Westergren method) is common, but untreated biopsy-proven cases of GCA may be associated with normal or nearly normal levels.
• Rare individuals appear to be unable to develop an elevated ESR during any inflammatory process, including active GCA. • The ESR is also liable to be relatively low or normal in patients who have been receiving corticosteroids for another condition. Thus, a normal ESR does not exclude GCA, especially in a patient with otherwise classic symptoms and findings. • Platelet counts are often increased.
• Treatment for Giant Cell Arteritis • An initial dose of prednisone 40 to 60 mg/day or equivalent is adequate in nearly all cases. • Dividing the dose for the first 1 to 2 weeks may accelerate the rate of improvement. • If the patient does not respond promptly, the dose should be increased. • Initiating treatment with intravenous methylprednisolone (15 mg/kg of ideal weight per day) for 3 days allowed more rapid tapering of oral corticosteroids and increased the likelihood of achieving a sustained remission.
• High-dose, intravenous-pulse methylprednisolone (1000 mg/day) for 3 days has also been tried in patients with recent loss of vision. Unfortunately, the loss remains permanent in the vast majority of patients • The occlusive nature of the vasculitis argues against any role of acute thrombolytic therapy in the treatment of blindness.
Behcets • CLINICAL FEATURES • APHTHAE • Oral aphthae are often the initial feature of Behçet's disease and constitute a requisite diagnostic feature. • Aphthae tend to be painful and shallow, and they heal without scarring over 1 to 3 weeks. Genital ulcers typically occur on the scrotum and penis in males and on the vulva or vaginal mucosa in females. These aphthae are similar in appearance to oral lesions, but they have a greater tendency to scar and may recur less frequently.
• CUTANEOUS LESIONS • Several cutaneous manifestations of Behçet's disease have been described: erythema nodosum , pyoderma gangrenosum , cutaneous small vessel vasculitis, and pustular vasculitic lesions Specimens from all these lesions demonstrate a neutrophilic vascular reaction on histopathologic analysis. Acneiform or pseudofolliculitis lesions. • OPHTHALMIC FEATURES • anterior and posterior uveitis, retinal vasculitis, and hypopyon, with secondary glaucoma, cataract formation, decreased visual acuity, and synechiae formation.
• ARTHRITIS • The arthritis of Behçet's disease is typically a nonerosive, inflammatory, symmetric or asymmetric oligoarthritis, The most commonly involved joints are the knees, wrists, ankles, and elbows. some time patients with Behçet's disease had a sacroiliitis. However, HLA-B 27–positive patients were not excluded from their series, and occult IBD was not excluded, • OTHER SYSTEMIC MANIFESTATIONS • Central nervous system involvement is most commonly characterized by brainstem or corticospinal tract syndromes (neuro-Behçet's syndrome), venous sinus thrombosis.
• gastrointestinal lesions resembling orogenital aphthae. These occur most commonly in the ileocecal region and in the ascending colon, transverse colon, or esophagus. • Large aphthae may lead to perforation • Pulmonary abnormalities are uncommon in Behçet's disease. Pulmonary artery aneurysms occur most frequently, followed by other complications secondary to vasculitis affecting the small pulmonary vessels. • Aneurysm, thrombosis, hemorrhage • Renal manifestations vary from minimal changes to proliferative glomerulonephritis and rapidly progressive crescentic glomerulonephritis. • The pathogenesis likely involves immune complex deposition.
Revised International Criteria for Behçet’s. Disease Oral aphthosis 1 point Skin manifestations (pseudofolliculitis, skin aphthosis) 1 point Vascular lesions (phlebitis, large vein thrombosis, aneurysm, arterial thrombosis) 1 point Positive pathergy test 1 point Genital aphthosis 2 points Ocular lesions 2 points *Diagnosis of Adamantiades-Behçet’s disease is made with a score of 3 points. • Modified from International Team for the Revision of International Criteria for Behçet’s Disease: Clinical manifestations of Behçet’s disease. • • •
• TREATMENT • Therapeutic options should be based on the degree of systemic involvement. • Mucocutaneous Disease Only : Topical, intralesional, or aerosolized corticosteroids’, Topical sucralfate , Local anesthetics Topical tacrolimus, Colchicine (0. 6 -1. 8 mg/day) , Dapsone (50 -150 mg/day) Combinations of these agents • Severe Mucocutaneous Disease Thalidomide (50 -150 mg/day) Methotrexate (2. 5 -25 mg/wk) Prednisone, Interferon-α (3 million-9 million U/wk) • Systemic Disease Prednisone; Azathioprine (50 -200 mg bid) Chlorambucil (4 -6 mg/day); Cyclophosphamide ; Cyclosporine Mycophenolate mofetil (1 -1. 5 g bid); Intravenous immunoglobulin Anti–TNF-α agents (adalimumab, etanercept, infliximab)
 V
V Vasculitis
Vasculitis Polyarteritis nodosa
Polyarteritis nodosa Perforacion septal
Perforacion septal Vasculitis
Vasculitis Dr donna braham ardenne road
Dr donna braham ardenne road Vasculitis
Vasculitis Takayasu arteritis
Takayasu arteritis Vasculitis
Vasculitis Anca p
Anca p Takayasu arteritis
Takayasu arteritis Ramona raya
Ramona raya Vasculitis
Vasculitis Sle vasculitis
Sle vasculitis Birmingham vasculitis activity score
Birmingham vasculitis activity score Inflexible personality
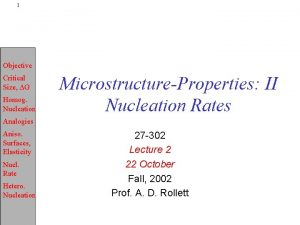
Inflexible personality Heterogeneous nucleation
Heterogeneous nucleation Heterogeneous distributed database
Heterogeneous distributed database Maple syrup homogeneous or heterogeneous
Maple syrup homogeneous or heterogeneous Homogeneous mixture juice
Homogeneous mixture juice Is a mud puddle homogeneous or heterogeneous
Is a mud puddle homogeneous or heterogeneous Vinegar homogeneous mixture
Vinegar homogeneous mixture What are lipids
What are lipids Element molecule compound mixture worksheet
Element molecule compound mixture worksheet Heterogeneous nucleation equation
Heterogeneous nucleation equation Heterogeneous data integration
Heterogeneous data integration Heterogenous audience
Heterogenous audience Heterogeneous vs homogeneous groups
Heterogeneous vs homogeneous groups Pictures of mixtures
Pictures of mixtures Heterogeneous market
Heterogeneous market Heterogeneous architecture presentation
Heterogeneous architecture presentation Heterogeneous mixture
Heterogeneous mixture Substances and mixtures
Substances and mixtures Homogeneous vs heterogeneous distributed database
Homogeneous vs heterogeneous distributed database Chapter 14 mixtures and solutions answer key
Chapter 14 mixtures and solutions answer key A heterogeneous mixture of intermediate sized particles
A heterogeneous mixture of intermediate sized particles Is mouthwash a homogeneous mixture
Is mouthwash a homogeneous mixture Heterogeneous
Heterogeneous Homogeneous vs heterogeneous
Homogeneous vs heterogeneous Is cake batter homogeneous or heterogeneous
Is cake batter homogeneous or heterogeneous Heterogeneous hypoechoic lesion in liver
Heterogeneous hypoechoic lesion in liver Is raisin bran a heterogeneous mixture
Is raisin bran a heterogeneous mixture Different types of mixtures
Different types of mixtures Heterogeneous computing
Heterogeneous computing Types of mixtures
Types of mixtures Tap water homogeneous or heterogeneous
Tap water homogeneous or heterogeneous Indiana jane and the investigation of matter answer key
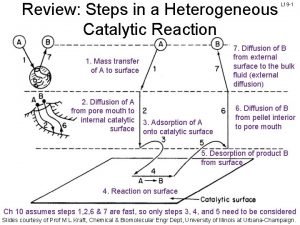
Indiana jane and the investigation of matter answer key 7 steps of heterogeneous catalysis
7 steps of heterogeneous catalysis Why blood is heterogeneous mixture
Why blood is heterogeneous mixture Homogeneous mixture and heterogeneous mixture class 9
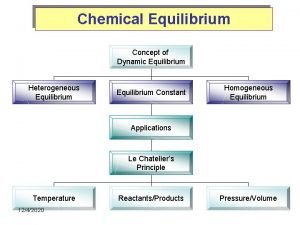
Homogeneous mixture and heterogeneous mixture class 9 Heterogeneous equilibrium
Heterogeneous equilibrium Foods that are heterogeneous mixtures
Foods that are heterogeneous mixtures Heterogeneous team
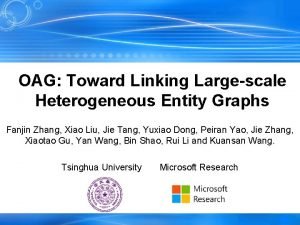
Heterogeneous team Oag: toward linking large-scale heterogeneous entity graphs
Oag: toward linking large-scale heterogeneous entity graphs Pure or mixture
Pure or mixture Is a pizza a heterogeneous mixture
Is a pizza a heterogeneous mixture Is chunky peanut butter homogeneous or heterogeneous
Is chunky peanut butter homogeneous or heterogeneous Heterogeneous transfer learning
Heterogeneous transfer learning Heterogeneous class
Heterogeneous class