CUTANEOUS VASCULITIS Oktay Takapan MD Vasculitis A term


- Slides: 34
CUTANEOUS VASCULITIS Oktay Taşkapan, MD
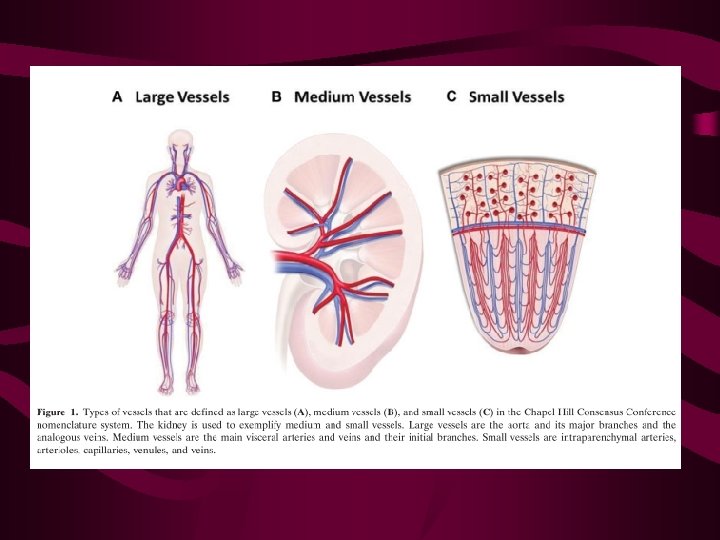
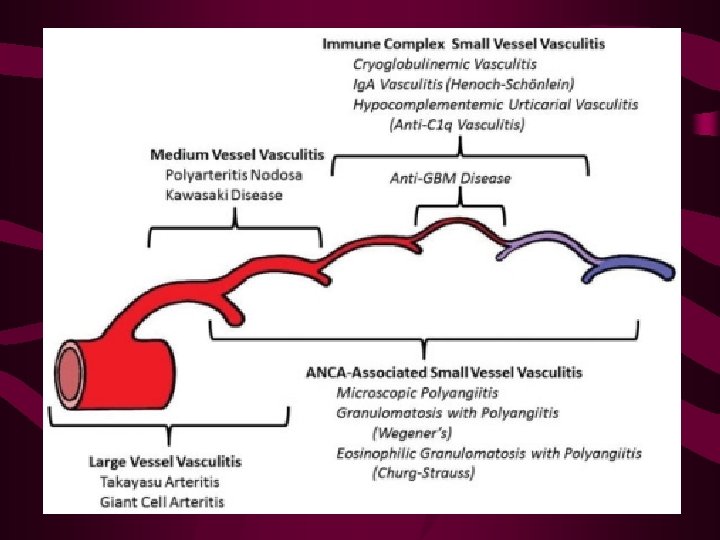
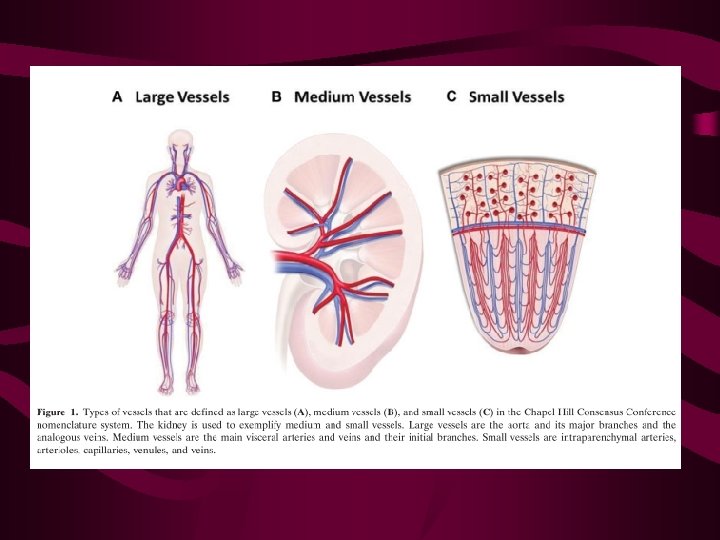
Vasculitis • A term applied to inflammation and necrosis of blood vessels • Vasculitis may be local or systemic, and may be primary or secondary to another disease process • Small vessels (such as capillaries, arterioles and venules), medium-sized vessels (such as visceral vasculature, including renal, coronary or hepatic arteries) and large vessels (the aorta and its great vessels) may be affected • Many vasculitides have a cutaneous component.
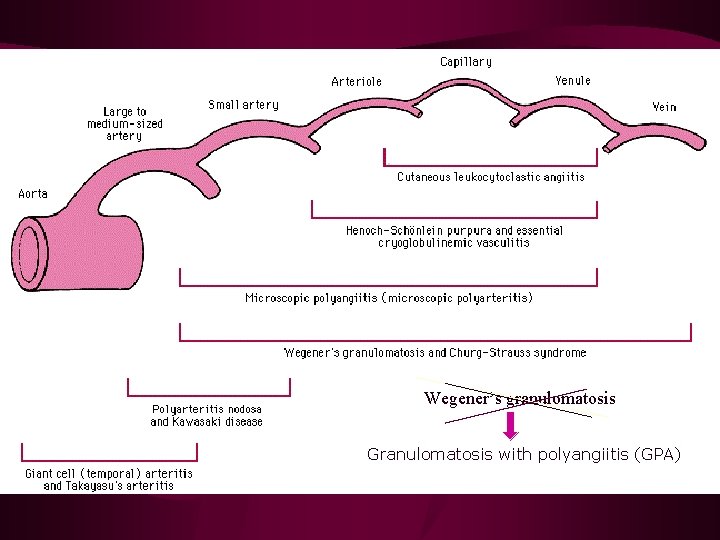
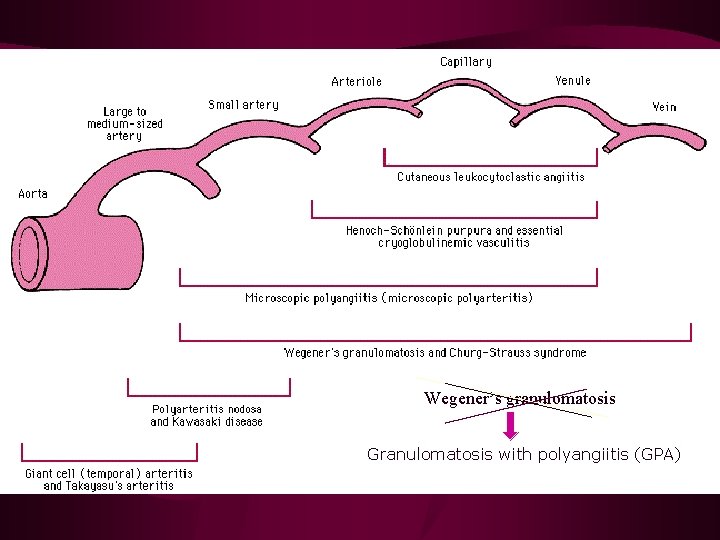
Wegener’s granulomatosis Granulomatosis with polyangiitis (GPA)
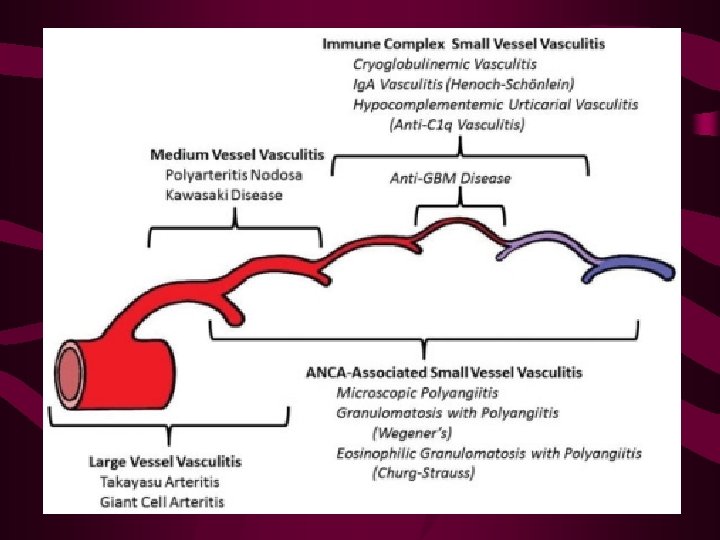
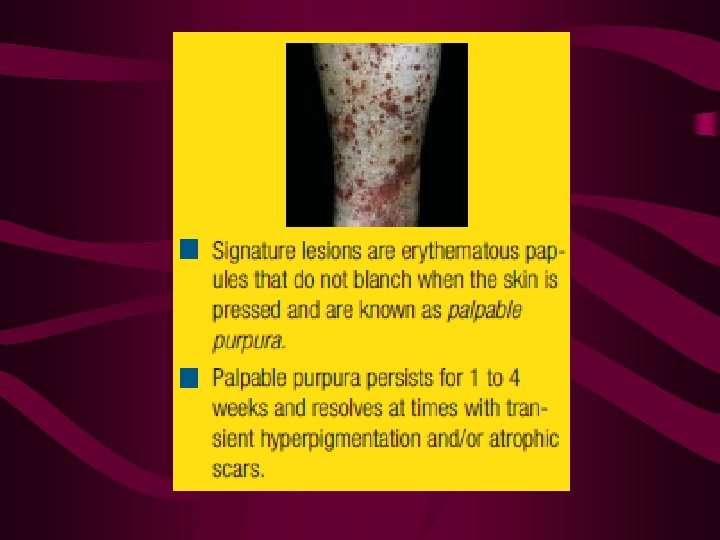
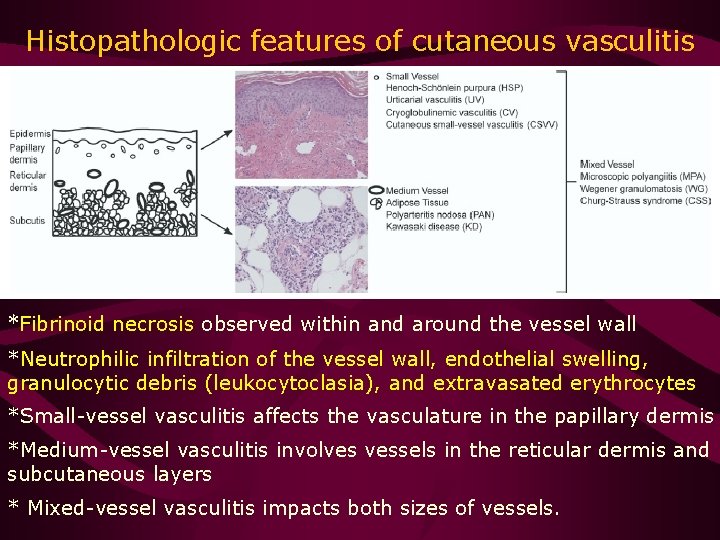
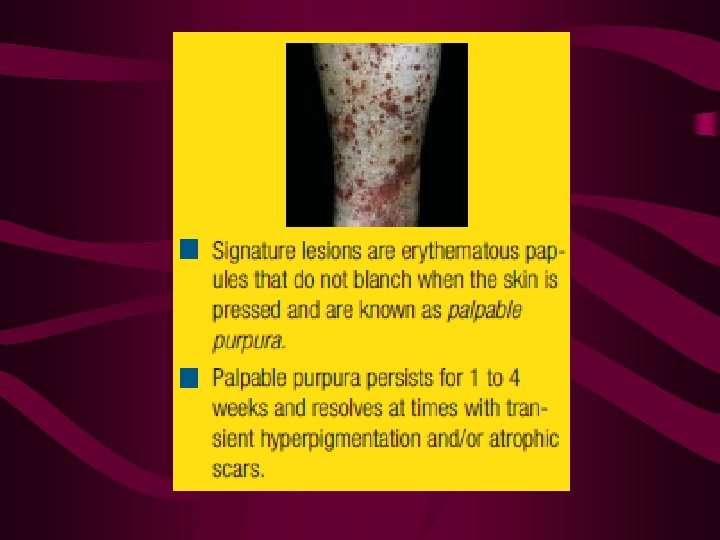
Small-vessel vasculitides • Small-vessel vasculitides: Henoch–Schönlein purpura (HSP), urticarial vasculitis (UV), cryoglobulinemic vasculitis (CV), and cutaneous small vessel vasculitis (CSVV), commonly referred to as cutaneous leukocytoclastic angiitis • The inflammation involves capillaries, postcapillary venules, and nonmuscular arterioles that reside in the superficial papillary dermis • Palpable purpura is the hallmark cutaneous finding of small-vessel vasculitis • Petechiae, vesicles, pustules, urticaria, and splinter hemorrhages may also be seen
Medium-vessel vasculitis • Arterioles with smooth muscle walls that are found within the deeper reticular dermis • PAN and Kawasaki disease (KD) are the predominant medium-vessel vasculitides • Cutaneous findings such as livedo reticularis, subcutaneous nodules, ulcers, digital infarcts, and papulonecrotic lesions are consistent with mediumvessel vasculitis.
Mixed-vessel vasculitis • It can involve both small and medium vessels • More diverse cutaneous findings than observed in either small- or medium-vessel vasculitis alone • Microscopic polyangiitis (MPA), Wegener granulomatosis (WG), and Churg–Strauss syndrome (CSS)
Large-vessel vasculitis • Takayasu arteritis or giant-cell (temporal) arteritis involve arteries not found within cutaneous tissues • Primarily with nondermatologic findings such as limb or jaw claudication, bruits, pulse defects, and new onset of headache

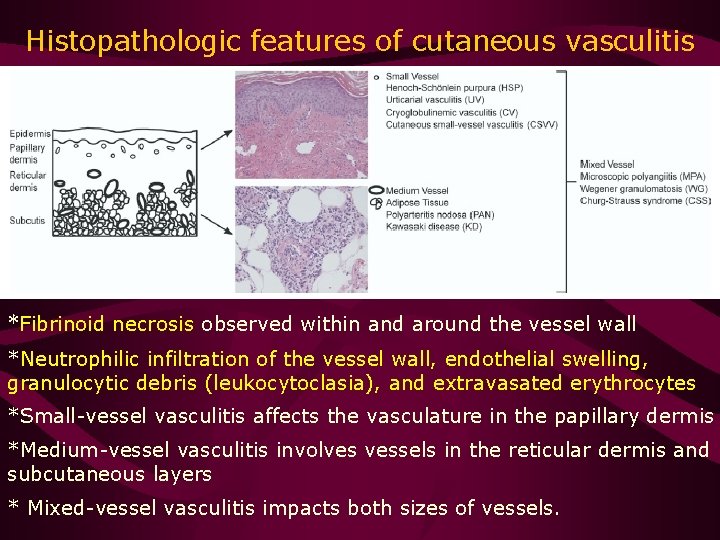
Histopathologic features of cutaneous vasculitis *Fibrinoid necrosis observed within and around the vessel wall *Neutrophilic infiltration of the vessel wall, endothelial swelling, granulocytic debris (leukocytoclasia), and extravasated erythrocytes *Small-vessel vasculitis affects the vasculature in the papillary dermis *Medium-vessel vasculitis involves vessels in the reticular dermis and subcutaneous layers * Mixed-vessel vasculitis impacts both sizes of vessels.
Dermatologic manifestations of cutaneous vasculitis • Palpable purpura: Symmetrically in dependent regions Postinflammatory hyperpigmentation • Asymptomatic, pruritic, or cause a burning sensation • Urticarial lesions may also suggest small-vessel vasculitis (UV) • Patients with UV frequently report a burning sensation • Simple urticaria usually starts regressing within 4 hours • Persistence of urticarial lesions for greater than 24 hours raises clinical suspicion of vasculitis • UV usually resolves with residual hyperpigmentation or ecchymoses • Biopsy allows distinction between urticaria and UV
Dermatologic manifestations of cutaneous vasculitis • Papulonecrotic lesions are characteristic findings of mixed vasculitides such as WG and CSS • Necrotic papules favor extensor surfaces • Medium-vessel vasculitis: Nodules, ulcers, LR, and digital infarctions • Nodules are typically painful and erythematous and tend to ulcerate
Dermatologic manifestations of cutaneous vasculitis • Vasculitic nodules also occur frequently on the lower extremities • Ulcers indicate intense inflammation within the vessel walls • LR occurs when blood flow through muscular arterioles supplying the skin is interrupted
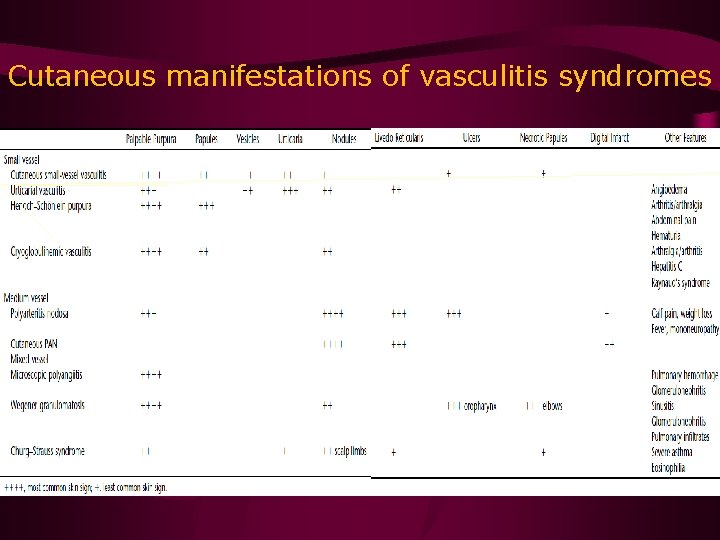
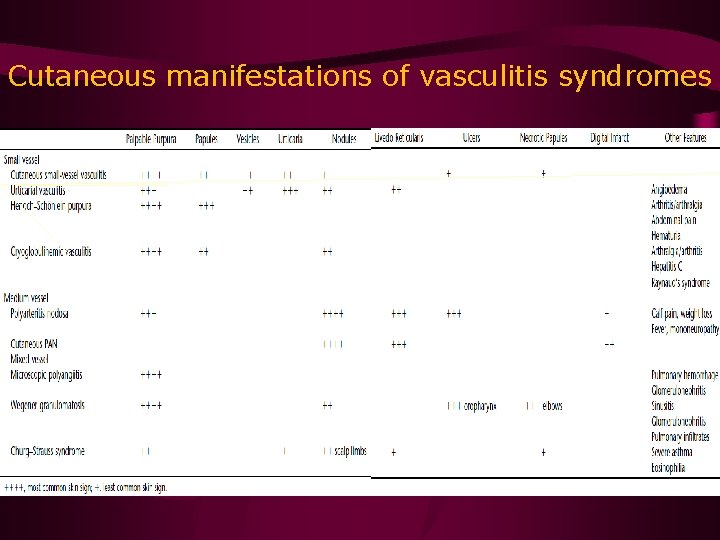
Cutaneous manifestations of vasculitis syndromes
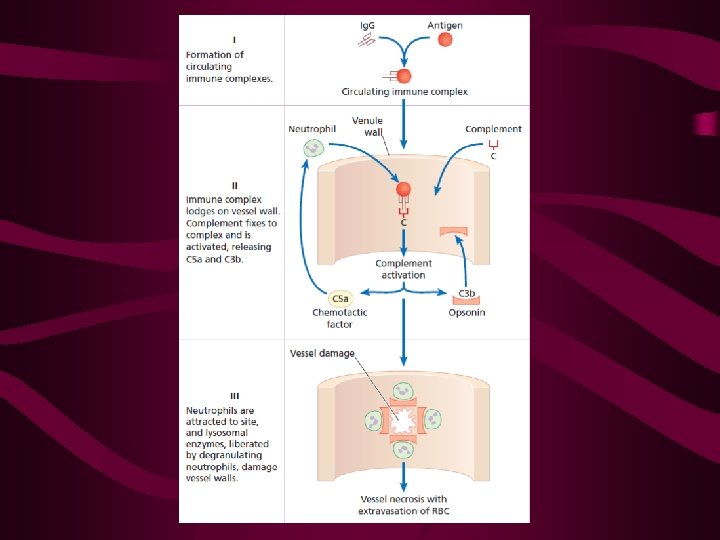
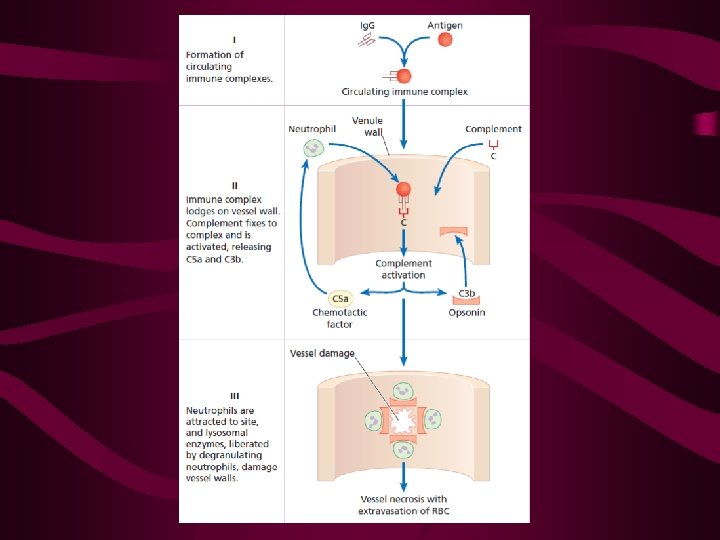
Pathophysiology of cutaneous vasculitis • Primary (idiopathic) process or the result of a secondary manifestation such as a drug reaction, infection, autoimmune disease, or malignancy • Penicillins, sulfonamides, allopurinol, thiazides, quinolones, propylthiouracil, and hydantoins • Viral hepatitis and subspecies of Neisseria, Rickettsia, and Streptococcus can trigger fibrinoid necrosis • Autoimmune disorders such as connective tissue diseases and systemic vasculitides present with CV • Harbinger for malignancies (lymphoma and leukemia) • Type II and III immune-mediated reactions are the most common pathogenic mechanisms underlying cutaneous vasculitis
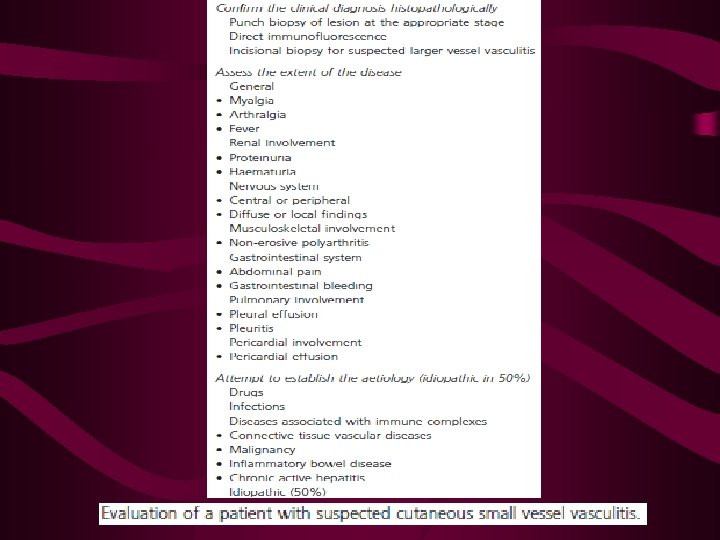
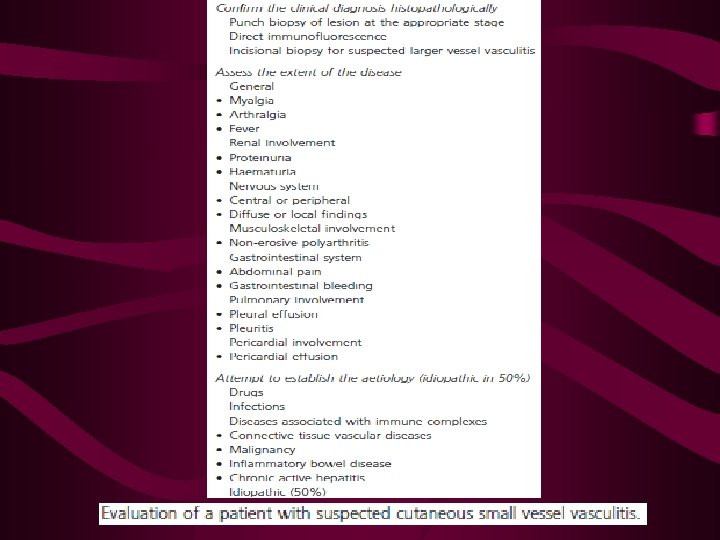
Diagnostic evaluation of cutaneous vasculitis • A thorough history and physical examination • The history: Chronicity of the symptoms, medications, allergies, family history of cancer, and past medical history including adult-onset asthma, connective tissue disorders, malignancy, and infections • Constitutional symptoms: Fever, night sweats, weight loss, and fatigue • Associated symptoms: Photosensitivity, hemoptysis, recurrent sinusitis, cough, dyspnea, wheezing, abdominal pain, diarrhea, melena, hematuria, arthralgias, paresthesias, muscle weakness, and testicular pain.
• The preliminary panel: WBC with cell differential, ESR, serum chemistry profile (blood urea nitrogen, creatinine), liver function tests, blood culture, and urine analysis. • Other relevant tests: Viral hepatitis serologies, ANAs, RF, C 3, C 4, ANCA, and cryoglobulins • Chest radiographs and WBC are adequate screening tools for malignancy unless other warning signs are present • CT scan may be needed for more thorough examination of the lungs and URT • Skin biopsy provides diagnostic confirmation of CV and should be performed in all suspected cases • Direct immunofluorescence (DIF)
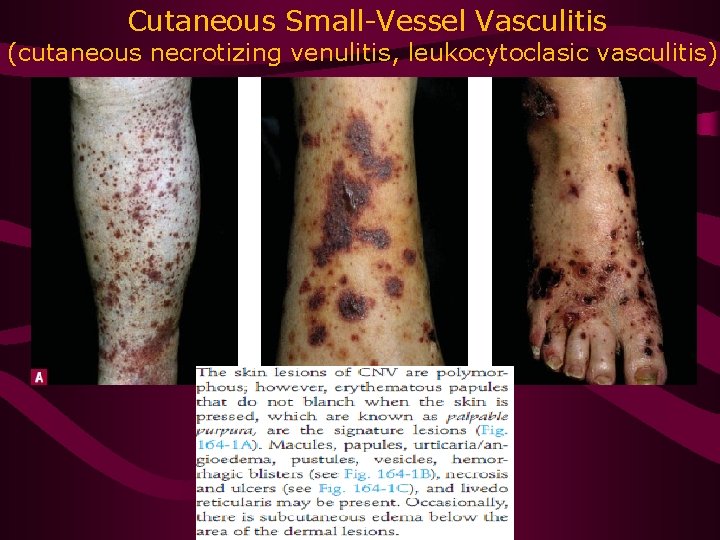
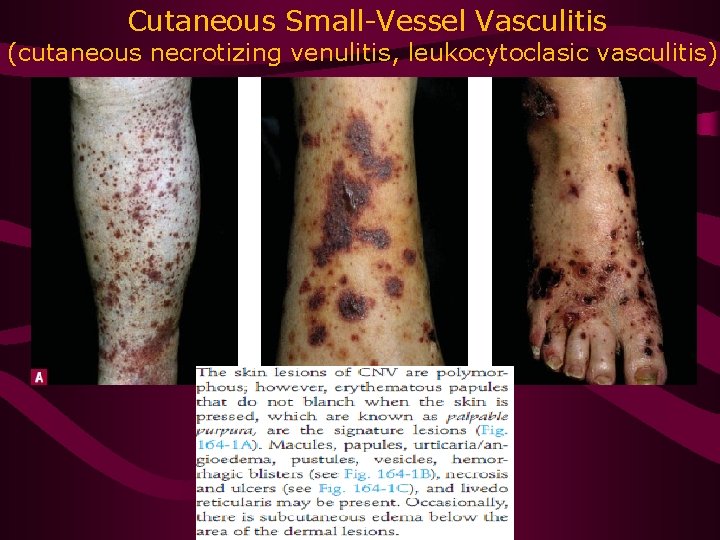
Cutaneous Small-Vessel Vasculitis (cutaneous necrotizing venulitis, leukocytoclasic vasculitis)
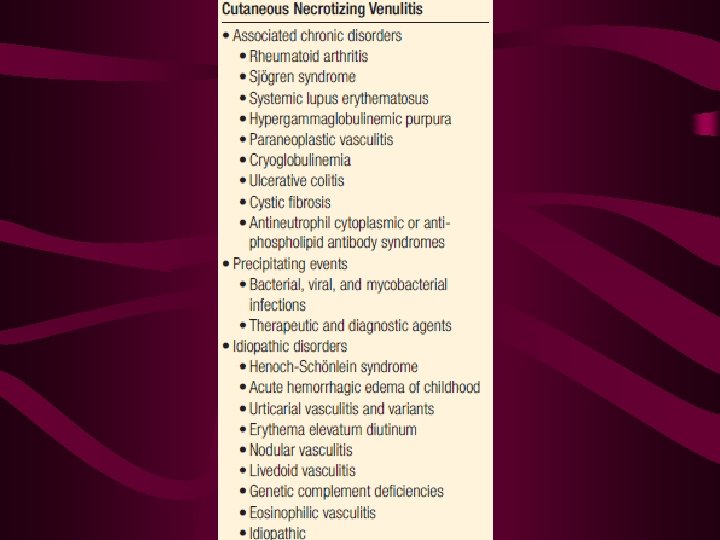
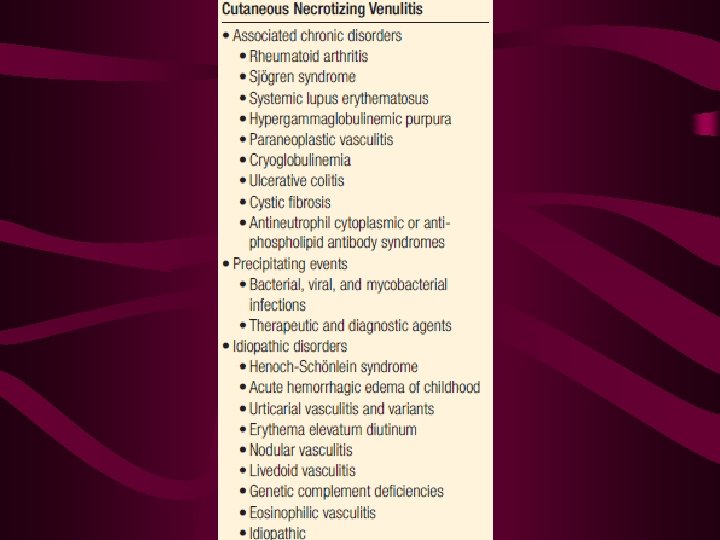
Cutaneous small-vessel vasculitis • CSVV is vasculitis confined to cutaneous tissues that primarily involves the postcapillary venules • It may occur in the presence of underlying systemic disease or as an idiopathic entity • Commonly associated conditions: Connective tissue diseases (SLE, Sjogren’s syndrome, RA) and infections (viral, bacterial, rickettsial, mycobacterial) • Recurrence occurs in approximately 10% of patients, who typically exhibit arthralgias, cryoglobulinemia, and the absence of fever

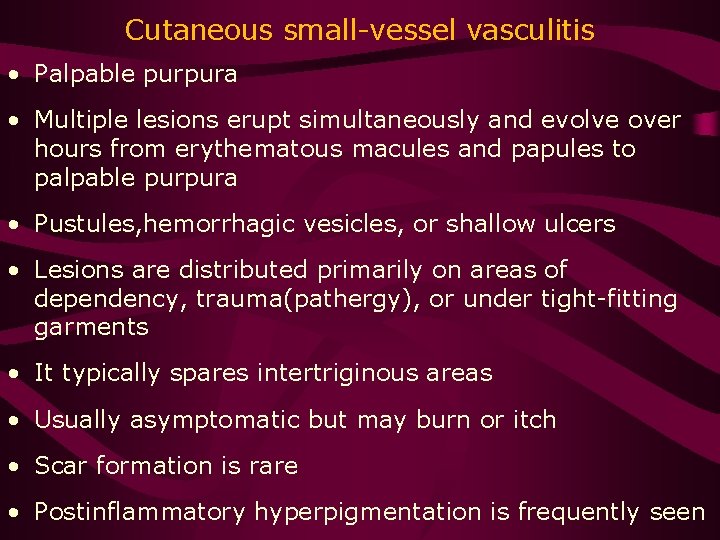
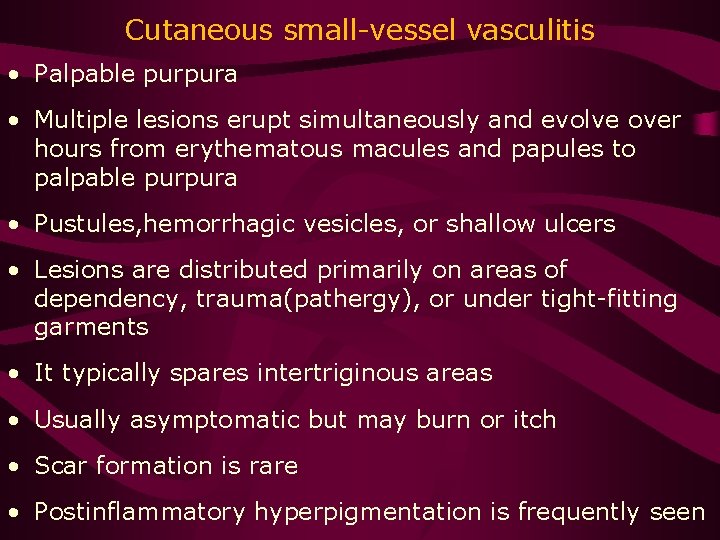
Cutaneous small-vessel vasculitis • Palpable purpura • Multiple lesions erupt simultaneously and evolve over hours from erythematous macules and papules to palpable purpura • Pustules, hemorrhagic vesicles, or shallow ulcers • Lesions are distributed primarily on areas of dependency, trauma(pathergy), or under tight-fitting garments • It typically spares intertriginous areas • Usually asymptomatic but may burn or itch • Scar formation is rare • Postinflammatory hyperpigmentation is frequently seen
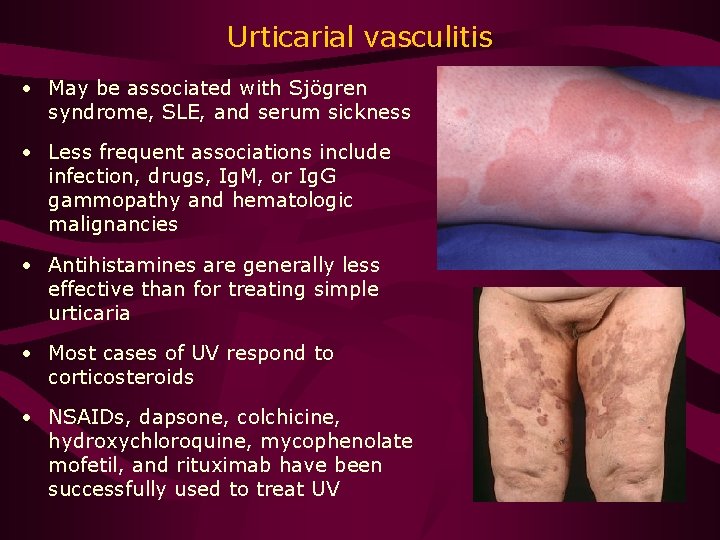
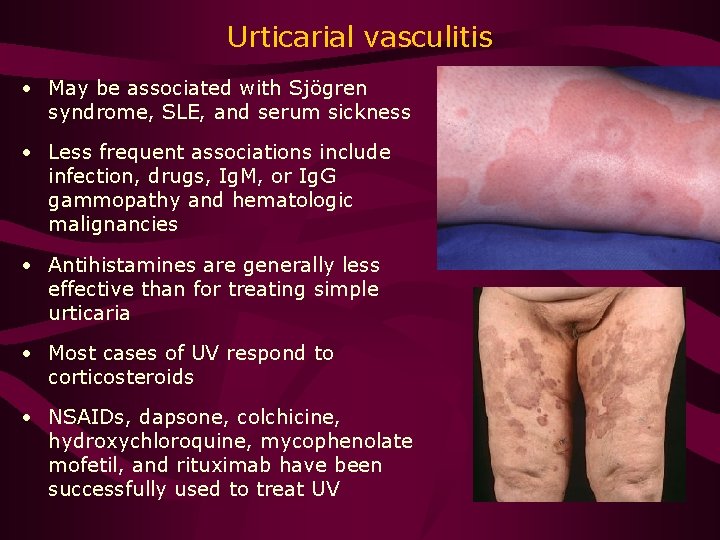
Urticarial vasculitis • May be associated with Sjögren syndrome, SLE, and serum sickness • Less frequent associations include infection, drugs, Ig. M, or Ig. G gammopathy and hematologic malignancies • Antihistamines are generally less effective than for treating simple urticaria • Most cases of UV respond to corticosteroids • NSAIDs, dapsone, colchicine, hydroxychloroquine, mycophenolate mofetil, and rituximab have been successfully used to treat UV
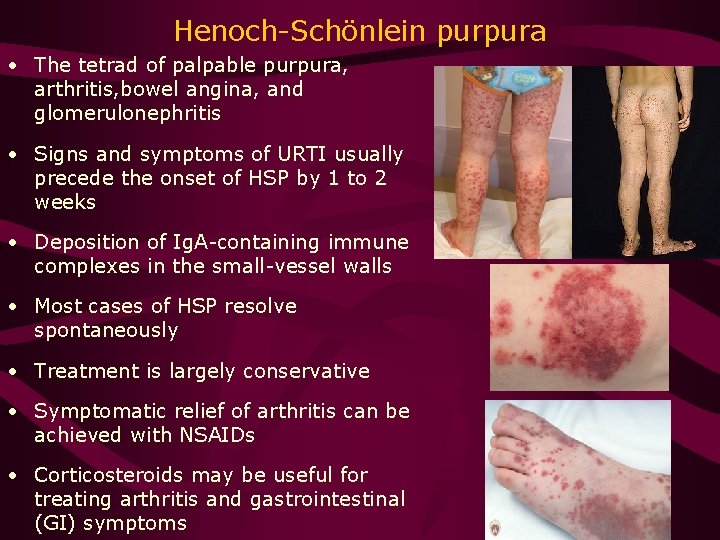
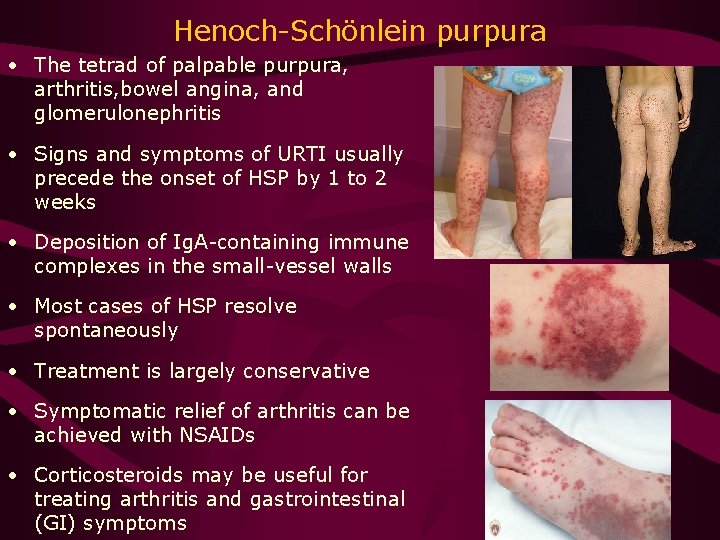
Henoch-Schönlein purpura • The tetrad of palpable purpura, arthritis, bowel angina, and glomerulonephritis • Signs and symptoms of URTI usually precede the onset of HSP by 1 to 2 weeks • Deposition of Ig. A-containing immune complexes in the small-vessel walls • Most cases of HSP resolve spontaneously • Treatment is largely conservative • Symptomatic relief of arthritis can be achieved with NSAIDs • Corticosteroids may be useful for treating arthritis and gastrointestinal (GI) symptoms
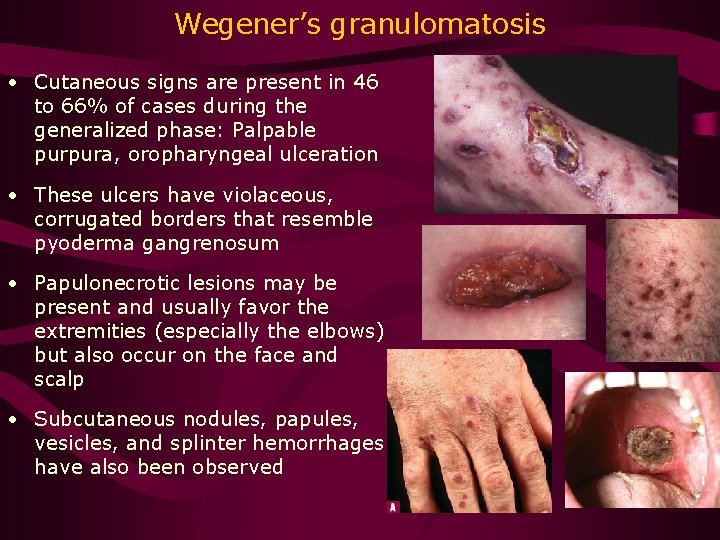
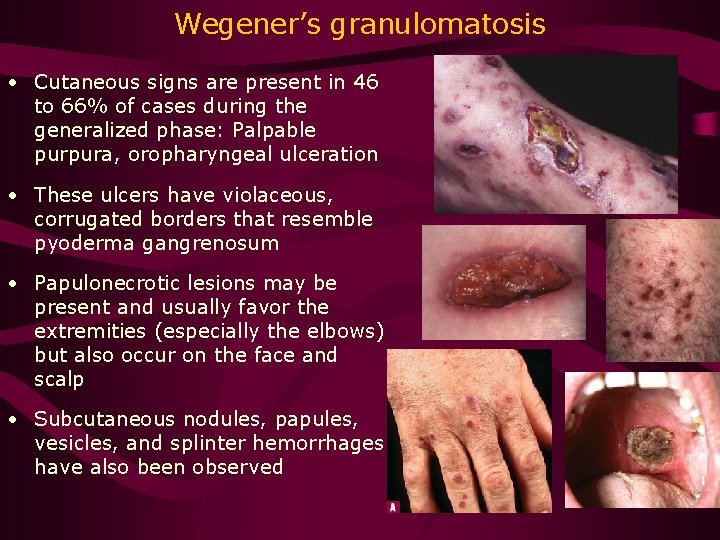
Wegener’s granulomatosis • Cutaneous signs are present in 46 to 66% of cases during the generalized phase: Palpable purpura, oropharyngeal ulceration • These ulcers have violaceous, corrugated borders that resemble pyoderma gangrenosum • Papulonecrotic lesions may be present and usually favor the extremities (especially the elbows) but also occur on the face and scalp • Subcutaneous nodules, papules, vesicles, and splinter hemorrhages have also been observed
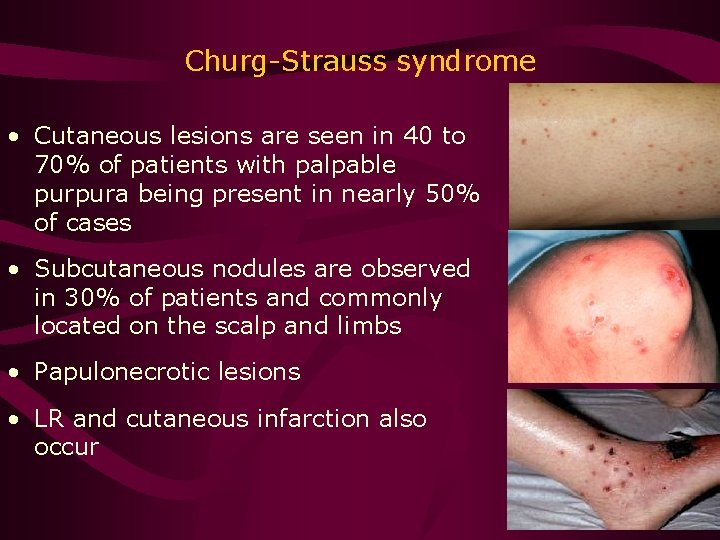
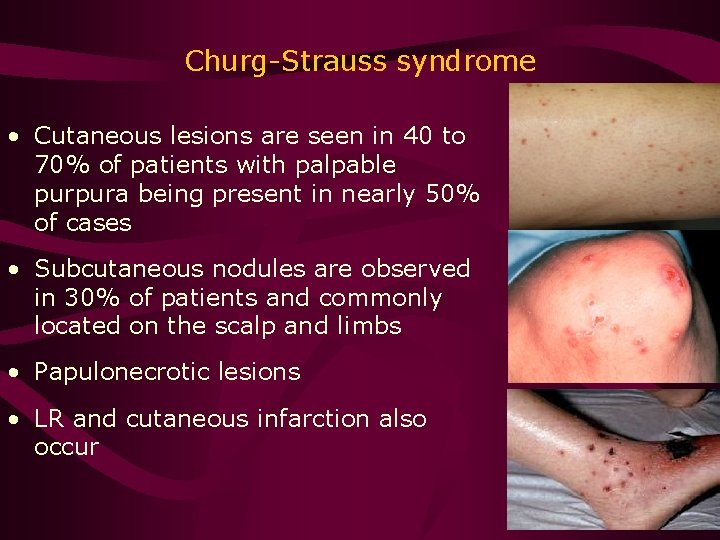
Churg-Strauss syndrome • Cutaneous lesions are seen in 40 to 70% of patients with palpable purpura being present in nearly 50% of cases • Subcutaneous nodules are observed in 30% of patients and commonly located on the scalp and limbs • Papulonecrotic lesions • LR and cutaneous infarction also occur
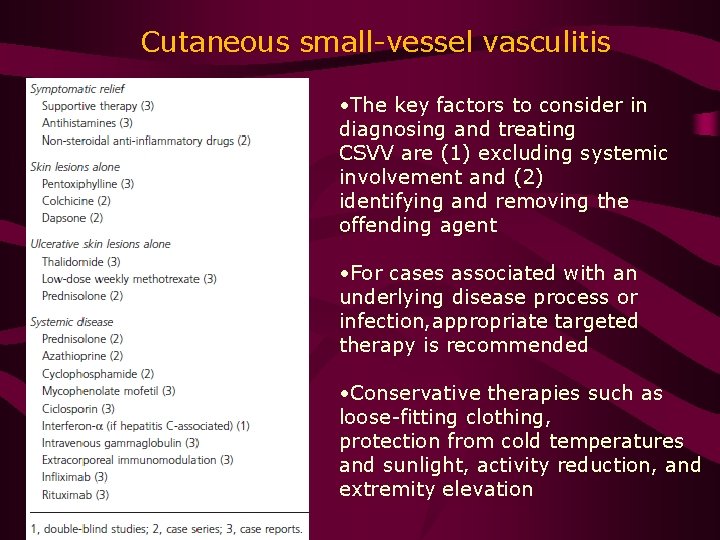
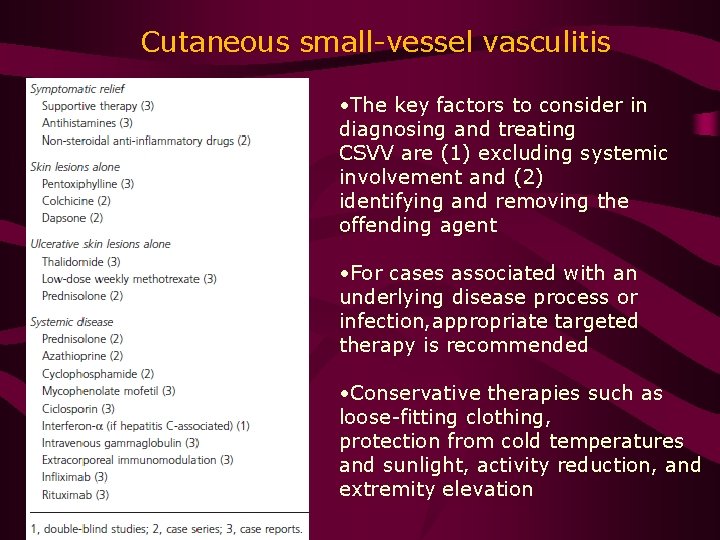
Cutaneous small-vessel vasculitis • The key factors to consider in diagnosing and treating CSVV are (1) excluding systemic involvement and (2) identifying and removing the offending agent • For cases associated with an underlying disease process or infection, appropriate targeted therapy is recommended • Conservative therapies such as loose-fitting clothing, protection from cold temperatures and sunlight, activity reduction, and extremity elevation
Epilogue • Cutaneous vasculitis presents in a wide variety of conditions with different degrees of systemic involvement • It is crucial to obtain a careful history, physical examination, and necessary diagnostic tests to distinguish self-limited conditions confined to the skin from those with systemic involvement and serious sequelae • Patients with cutaneous vasculitis typically follow 1 of 3 types of clinical courses in order of decreasing incidence: (1) a singular, self-limited episode triggered by prolonged exercise, allergy, drug, chemical, or infectious agent; (2) a relapsing, remitting cycle; or (3) a chronic, progressive course • Close interaction between the rheumatologist and the dermatologist may be critical in analyzing the fine details. Familiarity with the key clinical details of these various systemic illnesses is much more important than the serologic tests.