CUTANEOUS LEISHMANIASIS Anam Saghir 12 10007 Cutaneous Leishmaniasis



- Slides: 18
CUTANEOUS LEISHMANIASIS Anam Saghir 12 -10007
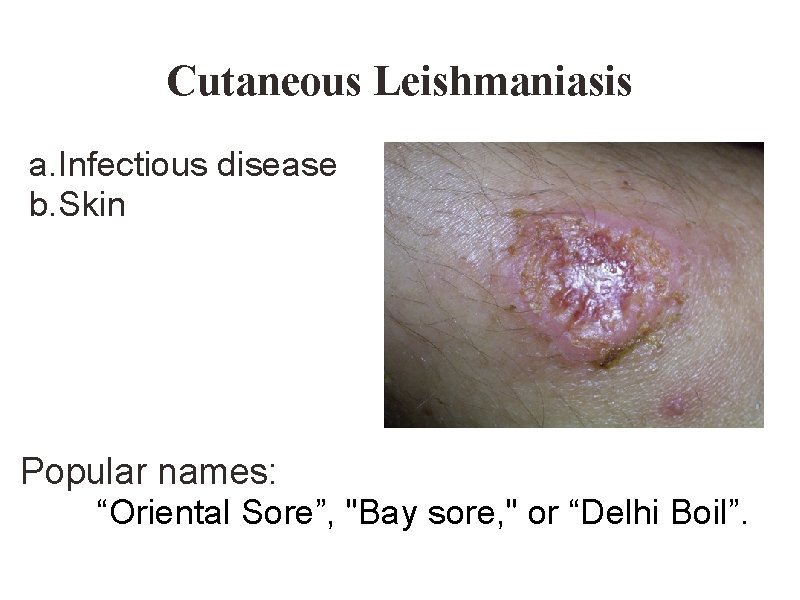
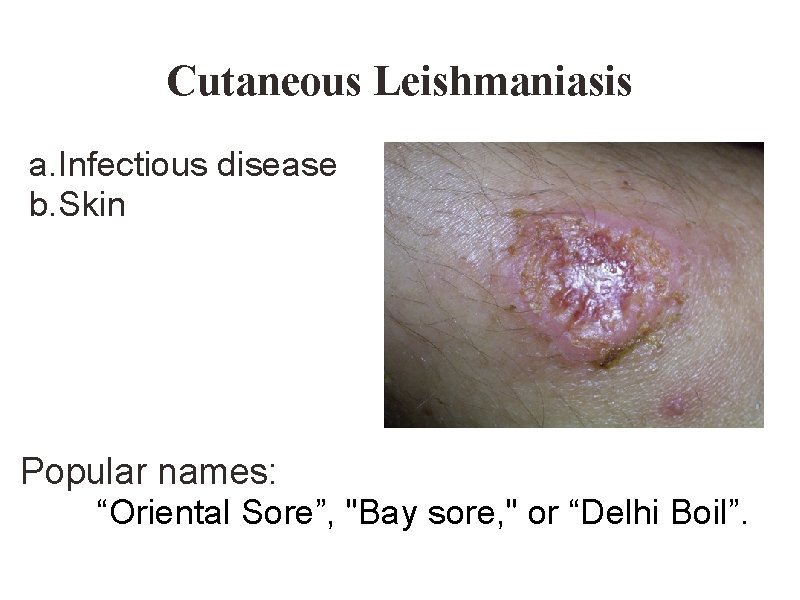
Cutaneous Leishmaniasis a. Infectious disease b. Skin Popular names: “Oriental Sore”, "Bay sore, " or “Delhi Boil”.
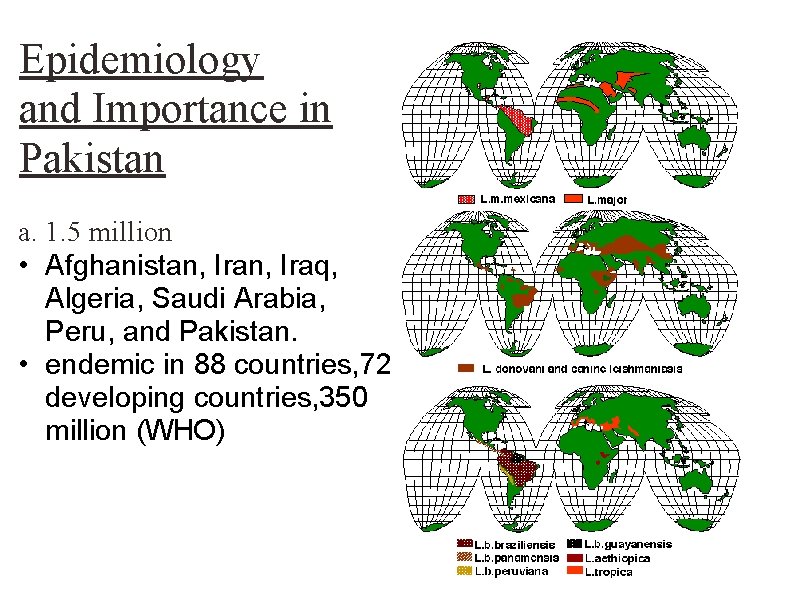
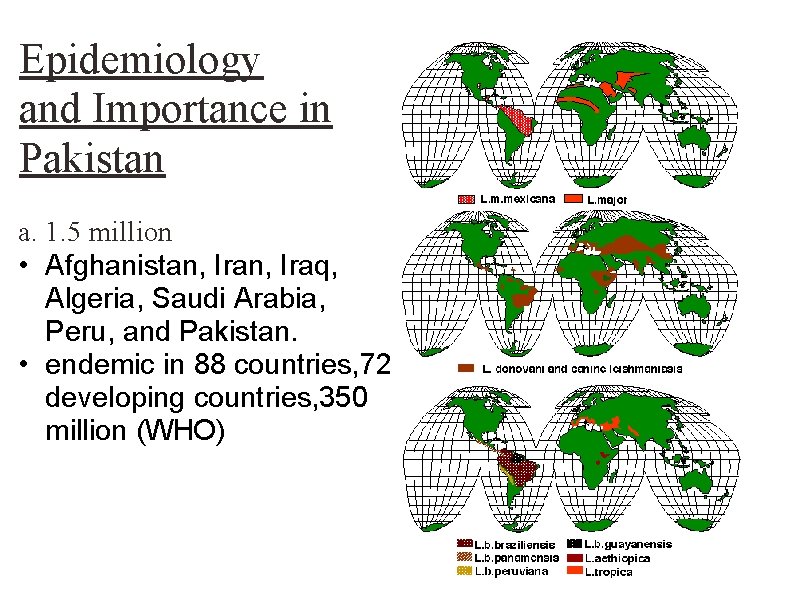
Epidemiology and Importance in Pakistan a. 1. 5 million • Afghanistan, Iraq, Algeria, Saudi Arabia, Peru, and Pakistan. • endemic in 88 countries, 72 developing countries, 350 million (WHO)
a. Hindukush and Karakoram sub mountain range (Chitral, Dir and Gilgit) b. Himalayan sub mountain range (Mansehra, Abbottabad, Rawalpindi) c. Kirthar and Suleman sub mountain range (Lasbela, Khuzdar, D. G. Khan, Rajanpur, Jacobabad, Larkana) d. Toba Kakar sub mountain range (Quetta, Qila Abdullah, Pishin, Qila Saifullah) KPK and FATA
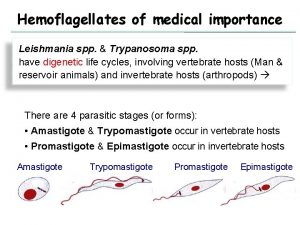
Causative Organism protozoa of genus Leishmania Leishman and Donovan (1903) 20 species----- human infecions

Cutaneous leishmaniasis causing organism Leishmania tropica major Leishmania tropica minor Leishmania aethiopica Leishmania mexicana
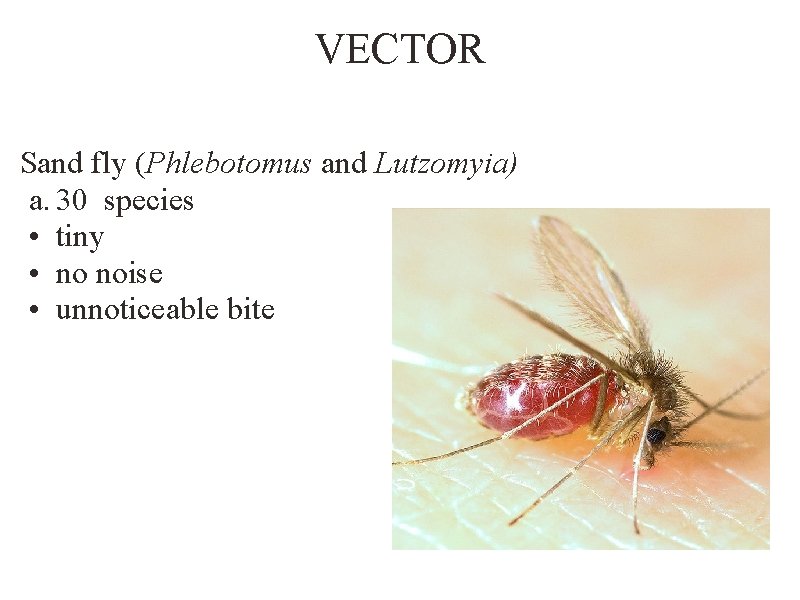
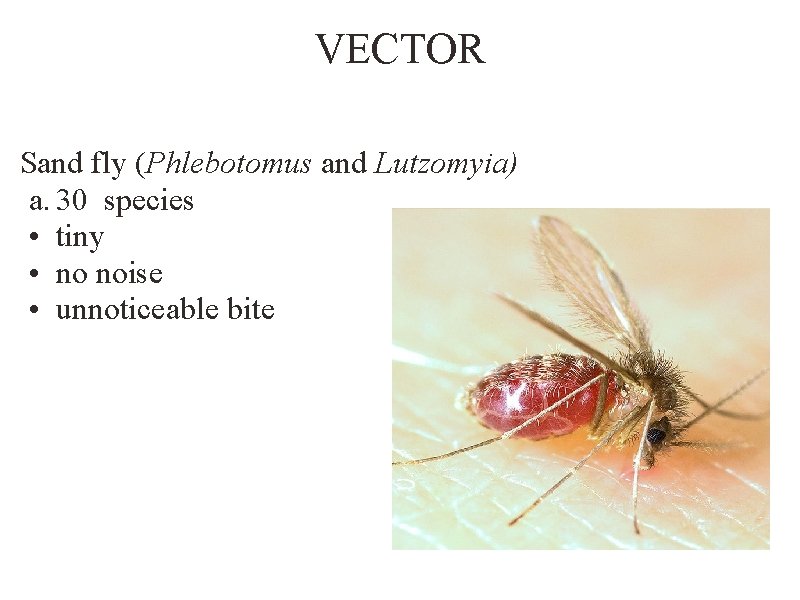
VECTOR Sand fly (Phlebotomus and Lutzomyia) a. 30 species • tiny • no noise • unnoticeable bite

a. lesions (a small reddish blue sore ) b. Size and appearance
PATEINTS RESPONSES 1. ANERGIC RESPONSE: a. formation of small papule b. nodular plaque c. no ulcer formation 2. HYPERSENSTIVE RESPONSE: a. papule appears • raised borders and ulcer in the centre • 3 -4 months • secondary infection • healing 90% • hyperpigmented and irregular scar
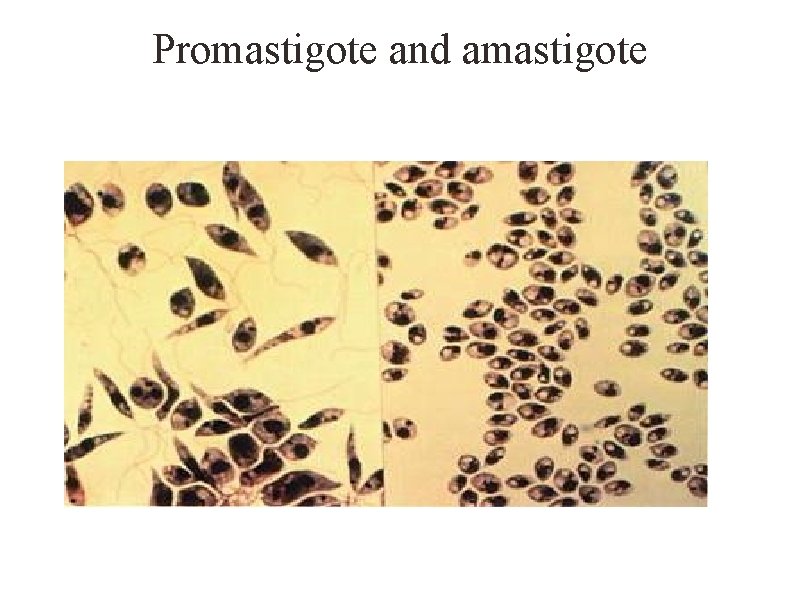
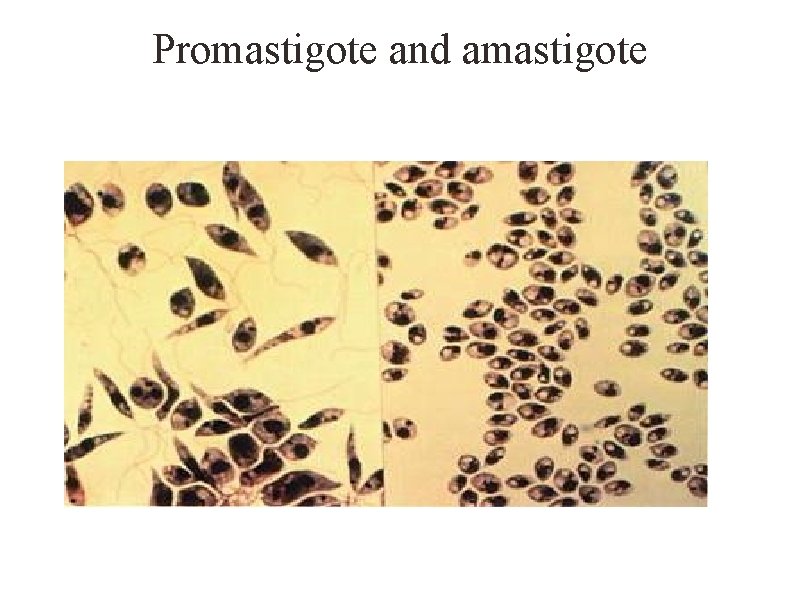
Promastigote and amastigote
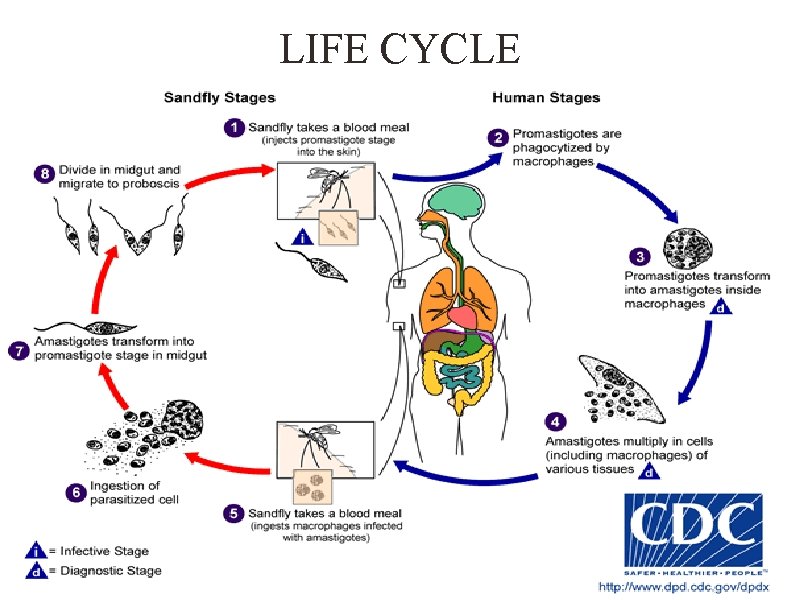
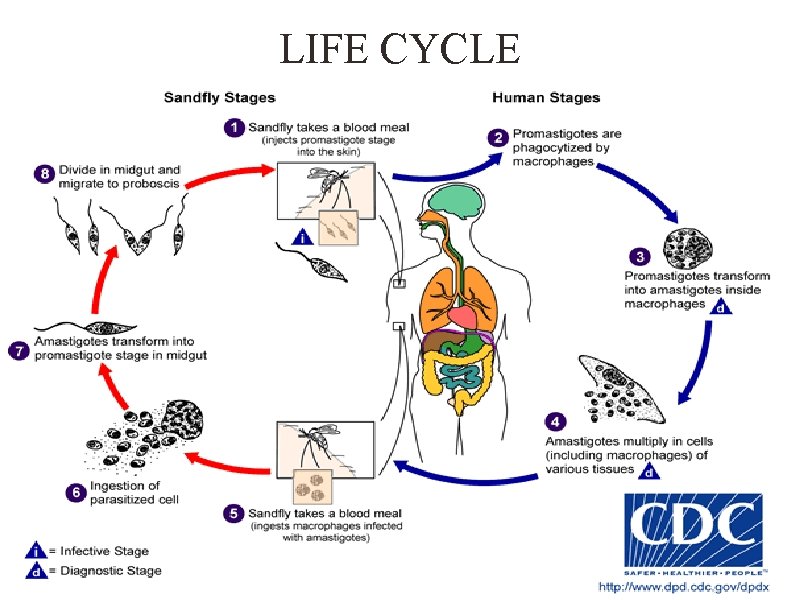
LIFE CYCLE
DIAGNOSTIC TEST Clinical diagnosis: a. history of origin specifying the endemic area of residence at the time of development of symptoms • morphology of the lesions • character of the lesions parasitalogical, immunological and molecular tests
PARASITLOGICAL TEST a. direct microscopic examination b. culture c. hamster inoculation
Skin biopsy specimen 1. Skin biopsy 2. Excision biopsy 3. Incisional biopsy 4. Shave / tangential biopsy 5. Punch biopsy 6. Curettings 7. Fine Needle Aspiration touch prepations, smears, histopathology, cultures in different media (NMN, BHI, EMTM etc. , )
SLIT SKIN SMEAR: a. margin of the lesion contains amastigotes b. area is punctred c. syringe is injected d. aspirated is taken e. examined microscopically or cultured CUTANEOUS SCRAPPING: a. proper cleaning and drying • centre and margins of ulcered lesions • multiple slides • +VE or -VE

MOLECULAR AND IMMUNOLOGICAL TESTS: IMMUNOLOGICAL TEST: a. Montenegro skin test • ELISA • Indirect Fluorescence Antibody Test (IFAT) • Direct Agglutination Test (DAT) MOLECULAR TEST: a. PCR • DNA hybridization • kinetoplast DNA
TREATMENT a. No treatment – self-healing lesions b. Medical: a. b. c. Pentavalent antimony (Pentostam), Amphotericin B Topical paromomycin c. Surgical: a. b. c. Cryosurgery Excision Curettage
PREVENTION a. usage of insect repellents such as DEET b. cover the exposed skin c. staying on higher floors of buildings in the evening or at night d. usage of fans e. insecticidal sprays f. Insecticide-treated bed nets, sheets and window curtains g. pumping of insecticides in rodent burrows to kill rodents h. treatment can also be considered a preventive measure Vaccines. . . .