ESTROGENS AND CARDIOVASCULAR DISEASES WALID SAGHIR M D

- Slides: 28
ESTROGENS AND CARDIOVASCULAR DISEASES WALID SAGHIR M. D. , FACS, FICS DEPARTMENT OF OB-GYN LEBANESE UNIVERSITY FACULTY OF MEDICAL SCIENCES BEIRUT-LEBANON
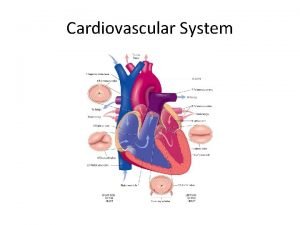
Cardiovascular Disease in Women Cardiovascular disease is the most common cause of death in the United States It includes Coronary heart disease Cerebral vascular disease Hypertension and Peripheral vascular disease Most cardiovascular disease results from atherosclerosis in major vessels.
PLAN Estrogens and coronary heart disease Estrogens and blood pressure Estrogens and VTE
WHAT IS ESTROGEN • Hormone that comprises a group of compounds, including estrone, estradiol and estriol. • Main sex hormone in women and is essential to the menstrual cycle. • Contributes to the development of secondary sex characteristics, which are the defining differences between men and women that don’t relate to the reproductive system. • Manufactured mostly in the ovaries by developing egg follicles.
MEDICAL USE Used in oral contraceptive pills in association with progesterone to prevent pregnancy. Used in estrogen replacement therapy for menopausal women.
EFFECTS ON LIPID PROFILE Contribute to increasing high density lipoprotein (HDL), which is considered the “good” cholesterol. Lower the low density lipoprotein (LDL) which is the “bad” cholesterol
The Women’s Health Initiative (WHI) was organized by the U. S. National Institutes of Health in 1992 to study the health of postmenopausal women and was scheduled to be completed in 2007. From 1993 to 1998 the WHI enrolled 161, 809 women aged 50 to 79 in 40 clinical centers.
The Women’s Health Initiative One of the randomized trials of postmenopausal HT an estrogen-only arm (daily 0. 625 mg conjugated estrogens), randomized 10, 739 hysterectomized women to treatment or placebo.
The Women’s Health Initiative One of the randomized trials of postmenopausal HT an estrogen-only arm (daily 0. 625 mg conjugated estrogens), randomized 10, 739 hysterectomized women to treatment or placebo. One of the randomized trials of postmenopausal HT, the combined estrogen-progestin arm (daily 0. 625 mg conjugated estrogen and 2. 5 mg medroxyprogesterone acetate) randomized 16, 608 women to either treatment or placebo.
The Women’s Health Initiative On July 9, 2002 the Data and Safety Monitoring Board decided 1 - to discontinue the trial arm administering daily estrogen-progestin after about 5 years of follow-up because of statistically significant increase in invasive breast cancer and an increase in cardiovascular events 2 - to continue the trial arm with daily unopposed estrogen in hysterectomized women.
The Women’s Health Initiative On March 2, 2004, the National Heart, Lung, and Blood Institute of the US National Institute of Health canceled the estrogen-only arm of the WHI after an average of 6. 8 years of follow-up because of an increased risk of stroke and probable dementia or cognitive impairment with no increase or decrease in CHD.
EFFECTS OF ESTROGENS ON CARDIO-VASCULAR SYSTEM PUBLISHED IN FINAL EDITED FORM AS: CLIN OBSTET GYNECOL. 2008 SEPTEMBER ; 51(3): 564– 580. DOI: 10. 1097/GRF. 0 B 013 E 318181 D E 86
ESTROGEN CARDIOPROTECTIVE HYPOTHESIS Randomized controlled trials demonstrated 3 salient points: 1 – Hormone therapy reduces total mortality while potentially reducing coronary heart disease in younger but not in older postmenopausal women 2 – Duration of HT is important in expressing the benefits on total mortality and CHD 3 – Risks of HT are rare especially in younger postmenopausal women and comparable to other primary prevention therapies for CHD.
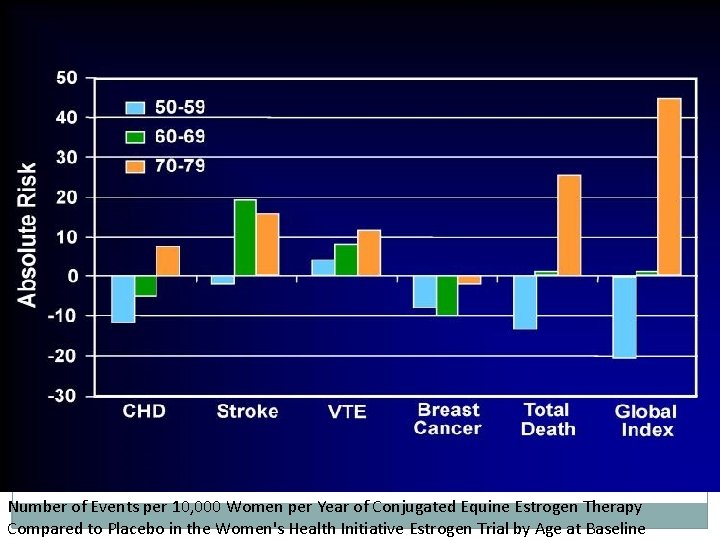
Cardioprotective Effect of HT According to Age and Timing of initiation In the WHI-estrogen alone trial, hysterectomized women randomized to daily conjugated equine estrogen 0. 625 mg (CEE) therapy within 10 years of menopause had a 52% reduction in CHD events and those randomized between 10 -20 years after menopause had a 4% reduction in CHD events and those randomized more than 20 years after menopause had a 12% increased risk of CHD, all relative to placebo treated women.
Cardioprotective Effect of HT According to Age and Timing of initiation However, several categories of CHD events (nonfatal myocardial infarction, coronary death, confirmed angina and coronary artery revascularization) were significantly reduced 34 -45% in the CEE treated group relative to the placebo treated group in women who were 50 -59 years old when randomized but not in the women in the 60 -69 or 70 -79 year old age ranges.
Reduction of Total Mortality by HT According to Age of Initiation In the WHI-E trial, women who were randomized to CEE therapy between the ages of 50 -59 years had a 29% reduction in total mortality, those randomized between the ages of 60 -69 years had a 2% increased risk of total mortality and those randomized between the ages of 70 -79 years had a 20% increased risk of total mortality, all relative to placebo treated women

Atheroprotective Effect of HT According to Stage of Atherosclerosis �women randomized to HT showed a reduction in the progression of common carotid artery intima-media thickness (CCA-IMT) compared with placebo after 2 years of treatment. �Age and/or time since menopause likely serve as chronological markers for vascular age (stage of atherosclerosis) which is the ultimate determinate as to whether HT will be cardioprotective since human and animal studies indicate that an underlying healthy endothelium is required for HT to be atheroprotective.
Duration of HT and Cardioprotection After 5 years of estrogen alone use, the risk for CHD in both the WHI-E trial (HR, 0. 80; 95% CI, 0. 571. 12) and the WHI observational study of estrogen users (HR, 0. 73; 95% CI, 0. 61 -0. 84) was reduced relative to nonusers. The WHI trials along with observational studies suggest that this duration-dependent lowering of CHD risk may predominantly manifest in women initiating HT in close proximity to menopause (within 6 years) or before 60 years of age.
CONCLUSION The totality of data indicate that the effect of postmenopausal HT on total mortality and CHD is modified by the timing of initiation (age and time since menopause) and the duration of therapy (>6 years of use). The absolute risks associated with HT are rare (less than 1 additional event per 1, 000 women) and even rarer in women who initiate HT below age 60 years or within 5 years of menopause.
CONCLUSION The cardiovascular results over the last few years support an emerging theme. The theme is: Healthy endothelium is needed to respond to estrogen. Experimental evidence in the monkey indicates that the beneficial effects of HT are progressively diminished with increasing atherosclerosis. In postmenopausal women, the vasodilatory effects of estrogen dissipate with increasing age. By the time, the endothelium is involved with atherosclerosis, it is too late for estrogen to exert a beneficial effect.
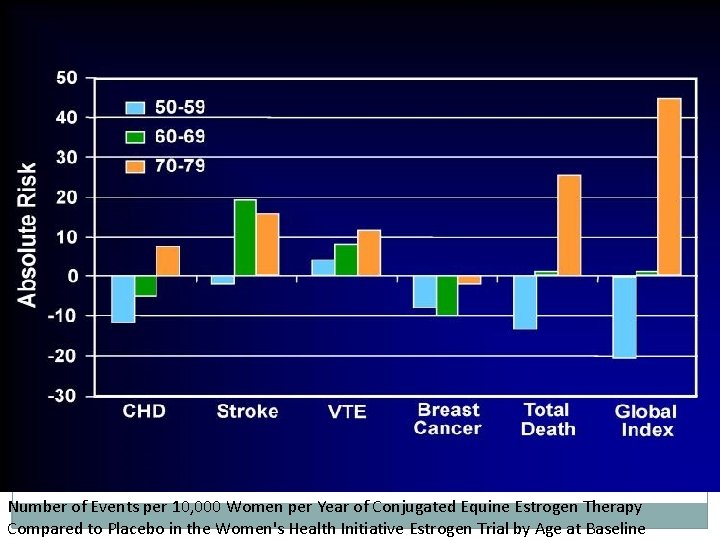
Number of Events per 10, 000 Women per Year of Conjugated Equine Estrogen Therapy Compared to Placebo in the Women's Health Initiative Estrogen Trial by Age at Baseline
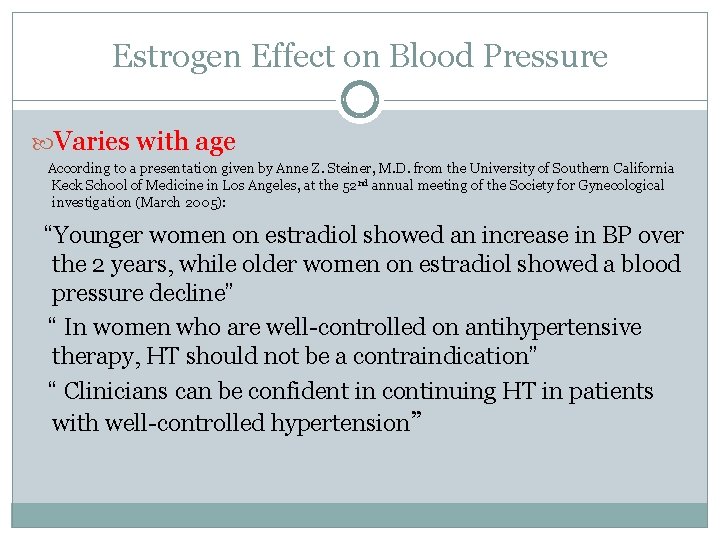
Estrogen Effect on Blood Pressure Varies with age According to a presentation given by Anne Z. Steiner, M. D. from the University of Southern California Keck School of Medicine in Los Angeles, at the 52 nd annual meeting of the Society for Gynecological investigation (March 2005): “Younger women on estradiol showed an increase in BP over the 2 years, while older women on estradiol showed a blood pressure decline” “ In women who are well-controlled on antihypertensive therapy, HT should not be a contraindication” “ Clinicians can be confident in continuing HT in patients with well-controlled hypertension”
VENOUS THROMBOSIS �The evidence is mounting that route of delivery and possibly type and dose of HT are important factors, particularly for venous thromboembolism (VTE) �Recent studies suggest that VTE risk may be lower with transdermal than oral estrogen and with estrogen alone than with combined therapy. � Neither micronized progesterone nor pregnane derivatives (including medroxyprogesterone acetate) were associated with VTE, whereas norpregnane derivatives were associated with a 4 -fold increase in odds of VTE.
Results from multiple studies indicate that postmenopausal HT increases the risk of venous thromboembolism about 2 -fold only to new hormone starters, mostly in the first year or two of treatment (WHI). VTE is a risk that is reduced with the use of statins and low-dose aspirin although it is not known whether statin and aspirin use would completely protect against the increased risk associated with HT.
CONCLUSION �The possible beneficial actions of estrogens on cardiovascular disease include all of the following: 1 – A favorable impact on lipoprotein profile (decrease total Chol. And LDL-Chol. and increase in HDL-Chol. ) 2 – A direct antiatherosclerotic effect in arteries 3 – Augmentation of vasodilating and antiplatelet aggregation factors, especially nitric oxide and prostacyclin. 4 – Direct inotropic actions on the heart 5 – Improvement of peripheral glucose metabolism with a subsequent decrease in circulating insulin levels. 6 – Inhibition of lipoprotein oxidation.
TAKE-HOME MESSAGE There continues to be good reason (a combination of biologic data and uniform agreement in a large number of observational studies) to believe that appropriately timed therapy can have a beneficial role in the primary prevention of coronary heart disease.
THANK YOU
 Dr walid saghir
Dr walid saghir Secretes estrogens and progesterone
Secretes estrogens and progesterone Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Jamal saghir
Jamal saghir Walid asaad
Walid asaad Udc real estate
Udc real estate Complications of hydrocephalus
Complications of hydrocephalus Walid radwan
Walid radwan Far point
Far point Walid radwan
Walid radwan Walid radwan
Walid radwan Walid radwan
Walid radwan Diadynamic
Diadynamic Walid abou jaoude
Walid abou jaoude Walid radwan
Walid radwan Walid radwan
Walid radwan Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Modern lifestyle and hypokinetic diseases
Modern lifestyle and hypokinetic diseases Is athlete's foot communicable or noncommunicable
Is athlete's foot communicable or noncommunicable Section 19-3 diseases caused by bacteria and viruses
Section 19-3 diseases caused by bacteria and viruses Retention hyperkeratosis dermnet
Retention hyperkeratosis dermnet Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Milady nail diseases and disorders
Milady nail diseases and disorders Elsevier
Elsevier