The Utility of FlexEx Radiographs after Negative CT





- Slides: 39
The Utility of Flex-Ex Radiographs after Negative CT in Blunt Trauma SARAH LUCEY, PGY 3 GRAND ROUNDS FEBRUARY 4, 2016
Objectives �Assess the diagnostic information that FE radiographs add after a negative cervical spine CT scan �Examine the diagnostic accuracy of FE radiographs �Review the updated guidelines from the Eastern Association for the Surgery of Trauma (EAST) for cervical spine collar clearance
Cervical Spine Injury �Incidence in adult blunt trauma: 2 -6% Pure ligamentous injury: 0. 2 -0. 6% �Ligamentous injury can be missed in up to 8% of cases �Accurate detection is essential as it can result in sequelae including radiculopathy, quadriplegia, and death in up to 29% of missed diagnoses
Case � 35 year old man presents to the ED s/p MVA. He was a restrained driver traveling 35 mph when he spun out and struck the median. He denies loss of consciousness and complains of “pain all over. ” He denies alcohol or drug use. On exam, vital signs are stable, and he has a GCS of 15. He has no obvious deformities. He presents in a hard cervical collar and has diffuse midline tenderness, however normal neuro exam. Can we clear the cervical spine? What should be done next?
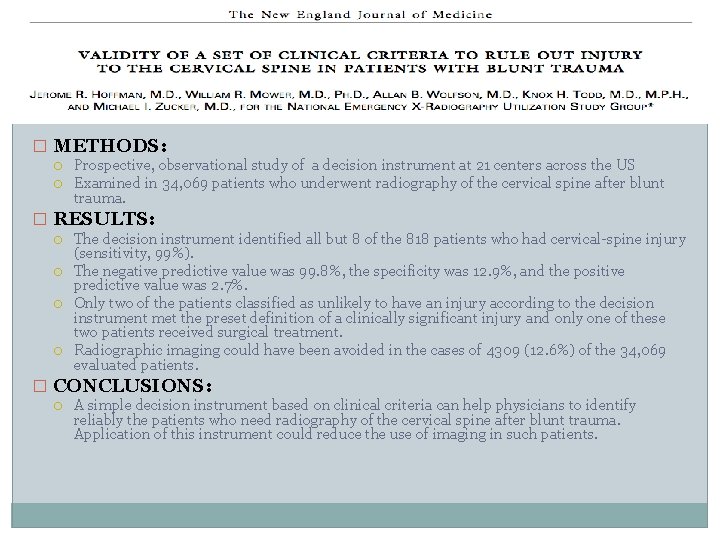
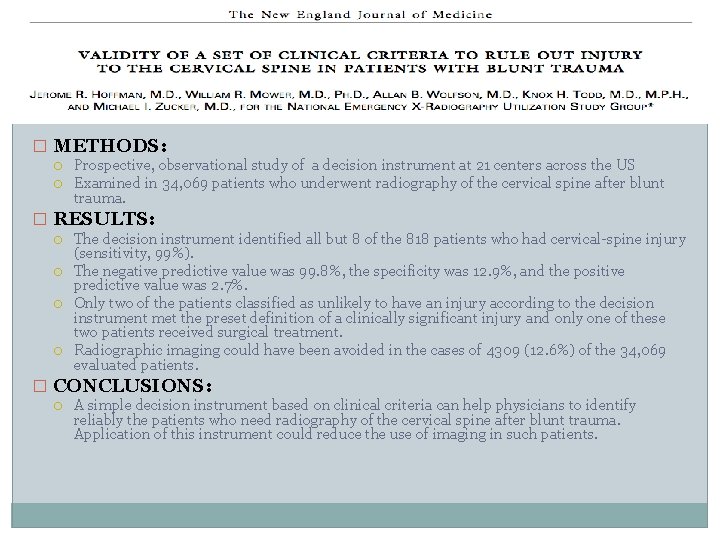
� METHODS: Prospective, observational study of a decision instrument at 21 centers across the US Examined in 34, 069 patients who underwent radiography of the cervical spine after blunt trauma. � RESULTS: The decision instrument identified all but 8 of the 818 patients who had cervical-spine injury (sensitivity, 99%). The negative predictive value was 99. 8%, the specificity was 12. 9%, and the positive predictive value was 2. 7%. Only two of the patients classified as unlikely to have an injury according to the decision instrument met the preset definition of a clinically significant injury and only one of these two patients received surgical treatment. Radiographic imaging could have been avoided in the cases of 4309 (12. 6%) of the 34, 069 evaluated patients. � CONCLUSIONS: A simple decision instrument based on clinical criteria can help physicians to identify reliably the patients who need radiography of the cervical spine after blunt trauma. Application of this instrument could reduce the use of imaging in such patients.
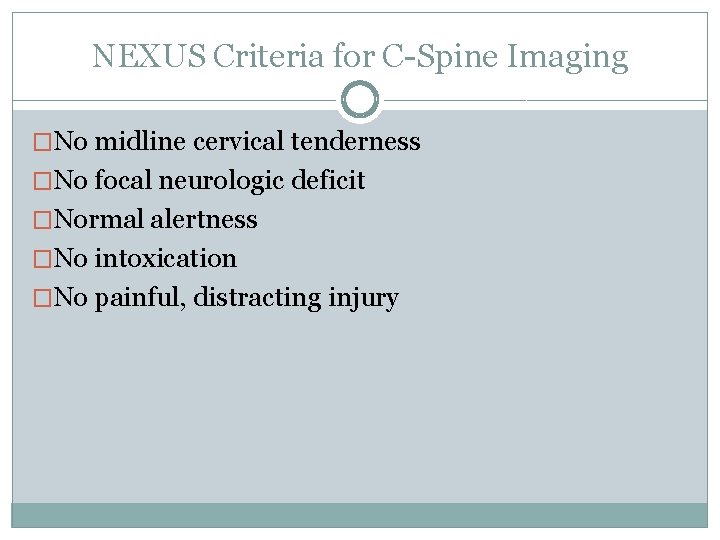
NEXUS Criteria for C-Spine Imaging �No midline cervical tenderness �No focal neurologic deficit �Normal alertness �No intoxication �No painful, distracting injury
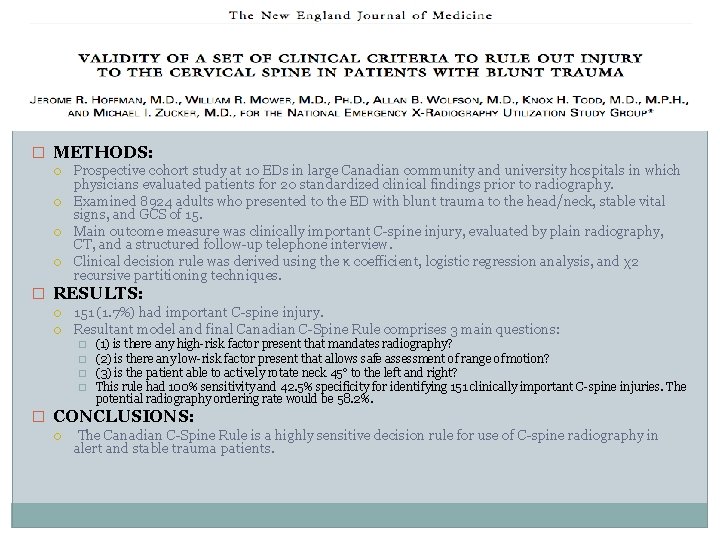
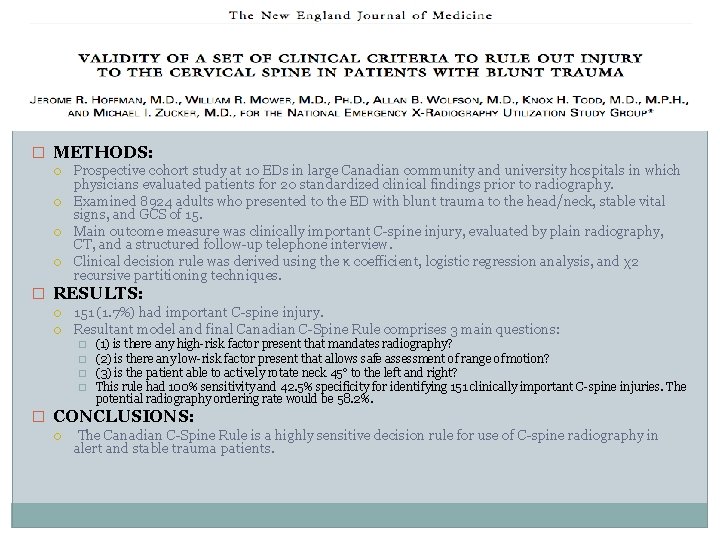
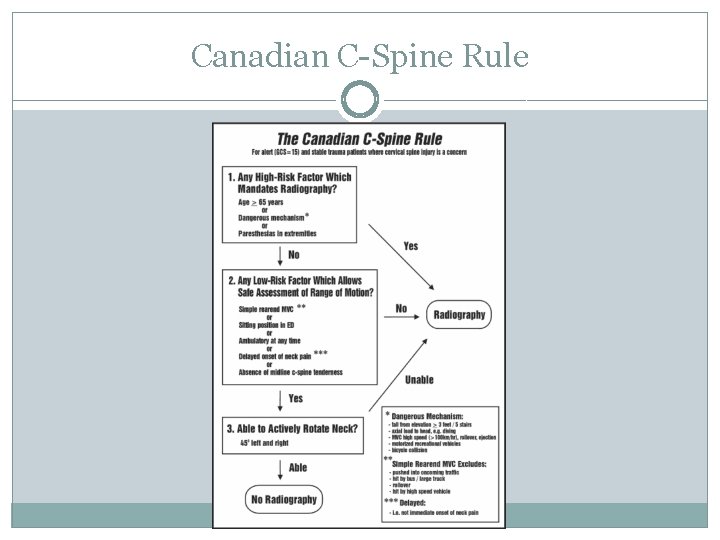
� METHODS: Prospective cohort study at 10 EDs in large Canadian community and university hospitals in which physicians evaluated patients for 20 standardized clinical findings prior to radiography. Examined 8924 adults who presented to the ED with blunt trauma to the head/neck, stable vital signs, and GCS of 15. Main outcome measure was clinically important C-spine injury, evaluated by plain radiography, CT, and a structured follow-up telephone interview. Clinical decision rule was derived using the κ coefficient, logistic regression analysis, and χ2 recursive partitioning techniques. � RESULTS: 151 (1. 7%) had important C-spine injury. Resultant model and final Canadian C-Spine Rule comprises 3 main questions: � � (1) is there any high-risk factor present that mandates radiography? (2) is there any low-risk factor present that allows safe assessment of range of motion? (3) is the patient able to actively rotate neck 45° to the left and right? This rule had 100% sensitivity and 42. 5% specificity for identifying 151 clinically important C-spine injuries. The potential radiography ordering rate would be 58. 2%. � CONCLUSIONS: The Canadian C-Spine Rule is a highly sensitive decision rule for use of C-spine radiography in alert and stable trauma patients.
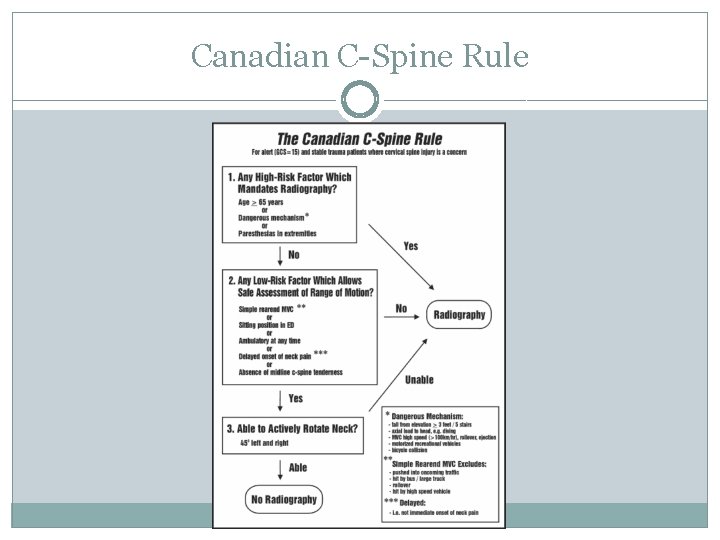
Canadian C-Spine Rule
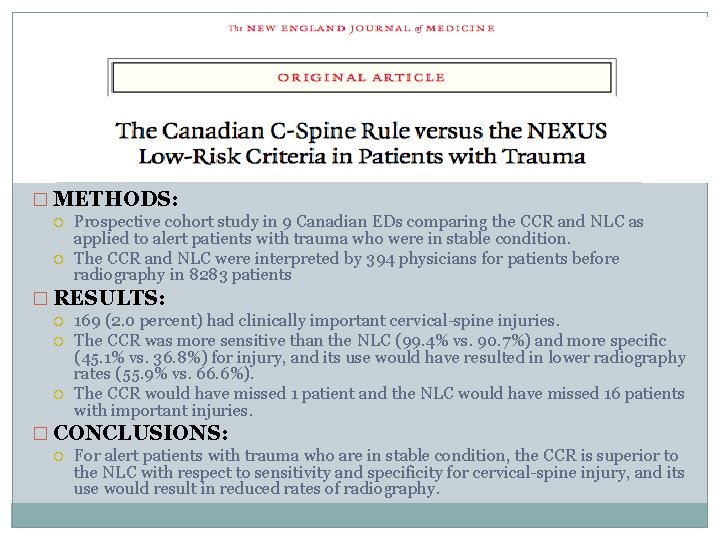
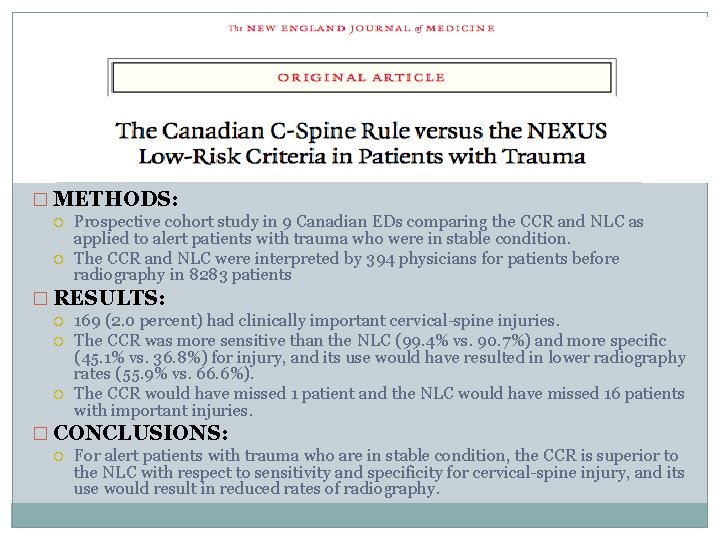
� METHODS: Prospective cohort study in 9 Canadian EDs comparing the CCR and NLC as applied to alert patients with trauma who were in stable condition. The CCR and NLC were interpreted by 394 physicians for patients before radiography in 8283 patients � RESULTS: 169 (2. 0 percent) had clinically important cervical-spine injuries. The CCR was more sensitive than the NLC (99. 4% vs. 90. 7%) and more specific (45. 1% vs. 36. 8%) for injury, and its use would have resulted in lower radiography rates (55. 9% vs. 66. 6%). The CCR would have missed 1 patient and the NLC would have missed 16 patients with important injuries. � CONCLUSIONS: For alert patients with trauma who are in stable condition, the CCR is superior to the NLC with respect to sensitivity and specificity for cervical-spine injury, and its use would result in reduced rates of radiography.
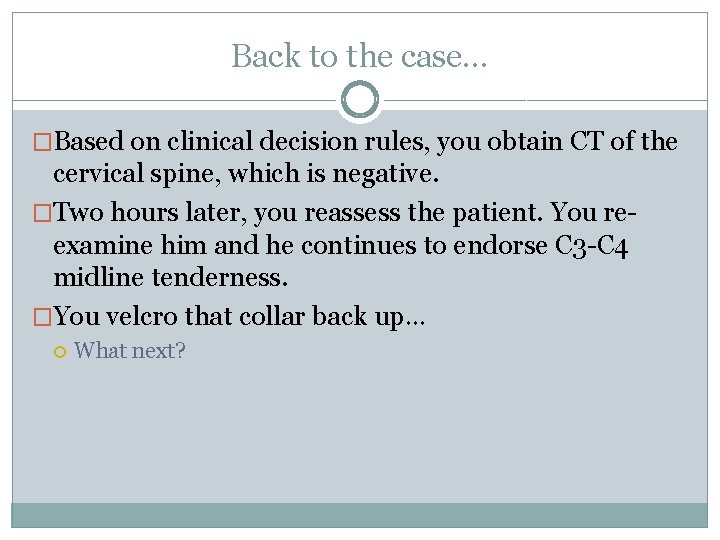
Back to the case… �Based on clinical decision rules, you obtain CT of the cervical spine, which is negative. �Two hours later, you reassess the patient. You reexamine him and he continues to endorse C 3 -C 4 midline tenderness. �You velcro that collar back up… What next?

Flexion-Extension Radiography (FE)
�To have a ligament injury that renders the spine unstable in the absence of a fracture: Hyper-flexion Injury � Tear of all posterior ligaments (costotransverse and posterior longitudinal ligaments) Hyper-extension Injury � Tear of all anterior ligaments and the capsular ligaments of the facet joints �Mechanism High-speed MVA, fall from height onto flexed neck, football injury �Clinical findings Significant tenderness Reluctance to flex the neck or lift head off the bed

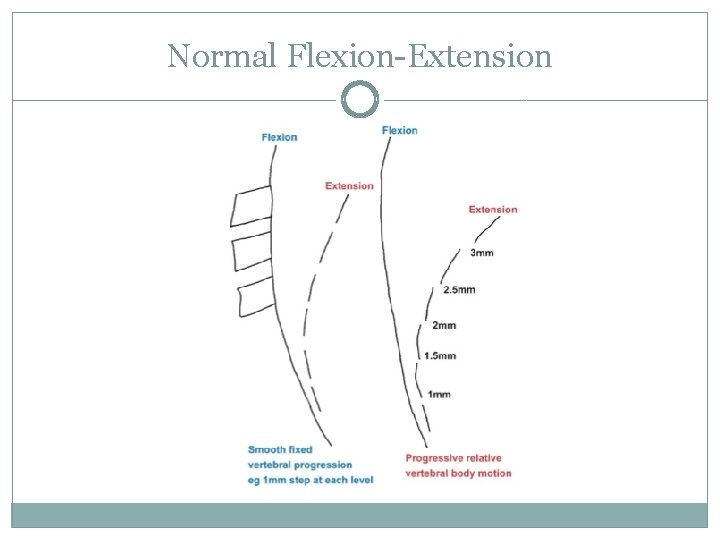
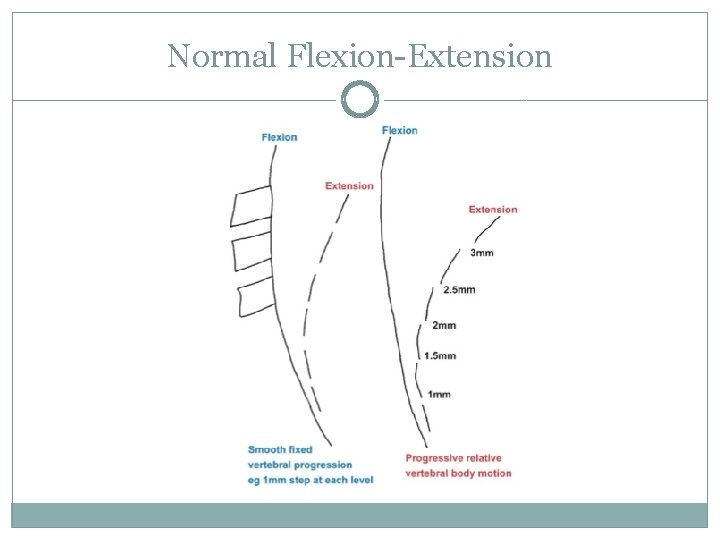
Normal Flexion-Extension
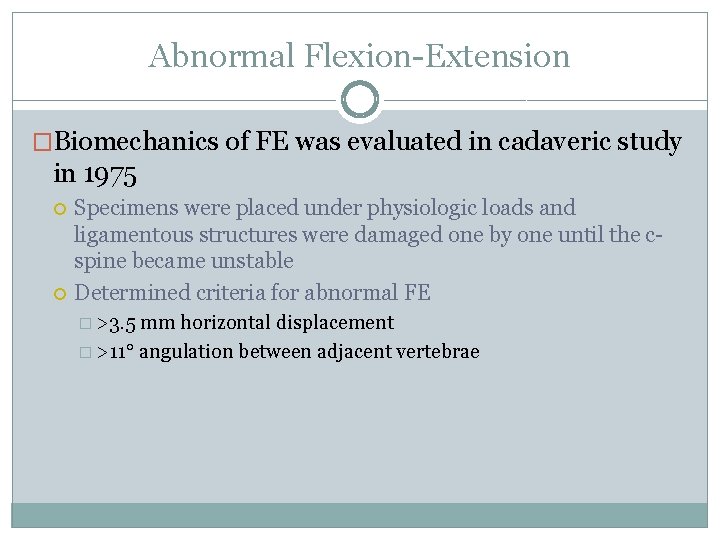
Abnormal Flexion-Extension �Biomechanics of FE was evaluated in cadaveric study in 1975 Specimens were placed under physiologic loads and ligamentous structures were damaged one by one until the cspine became unstable Determined criteria for abnormal FE � >3. 5 mm horizontal displacement � >11° angulation between adjacent vertebrae

Review of Literature
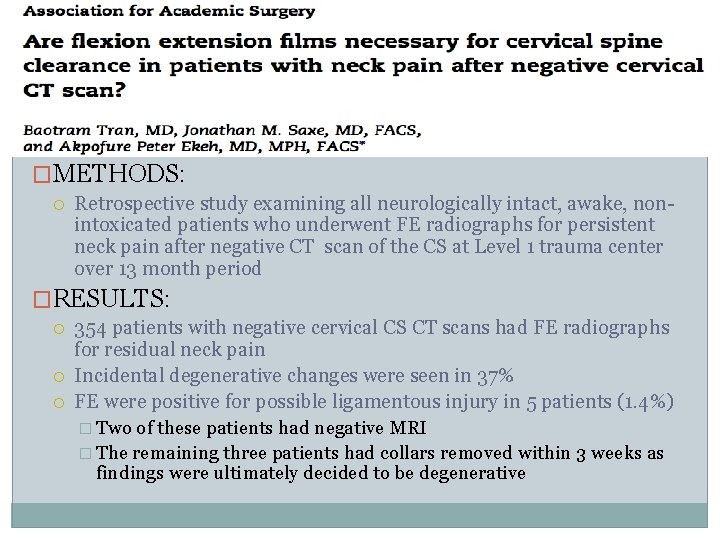
�METHODS: Retrospective study examining all neurologically intact, awake, nonintoxicated patients who underwent FE radiographs for persistent neck pain after negative CT scan of the CS at Level 1 trauma center over 13 month period �RESULTS: 354 patients with negative cervical CS CT scans had FE radiographs for residual neck pain Incidental degenerative changes were seen in 37% FE were positive for possible ligamentous injury in 5 patients (1. 4%) � Two of these patients had negative MRI � The remaining three patients had collars removed within 3 weeks as findings were ultimately decided to be degenerative
�CONCLUSIONS: In the current era where cervical CT has universally supplanted initial plain films, FE radiographs appear to be of little value in the evaluation of persistent neck pain Use of FE radiographs should be excluded from cervical spine clearance protocols in neurologically intact, awake patients
� METHODS: Retrospective chart review of 2 years duration at Level 1 trauma center examining all patients sustaining blunt trauma who were evaluated with both a CT as well as FE radiographs Exclusion criteria: penetrating injuries, neurologic symptoms, age <18 years old � RESULTS: Flexion and extension cervical radiographs were obtained in 379 patients after negative CT 8 F/E radiographs were positive Follow-up MRI was negative for ligamentous injury in all cases For the diagnosis of ligamentous injury, CT and FE had a negative predictive value both of 100% and a positive predictive value of 32% and 38% respectively, indicating that FE adds no additional diagnostic value following CT
�CONCLUSIONS: No cases of a clinically relevant positive FE radiograph after a negative CT scan were identified. Follow-up FE radiographs are not efficacious when a negative CT has been performed in blunt trauma without neurologic findings.
�METHODS: Retrospective study performed at Level 1 trauma center, using data from trauma registry throughout 8 years for a total of 271 patients CT scanning was compared with FE radiography as the reference standard for the detection of ligamentous injury Total of 160 patients underwent CT scan followed by active FE radiography �RESULTS 7 true positive ligamentous injuries were found with CT as well as 5 false positives, 146 true negatives, and two false negatives (that were identified by FE radiographs) � Specificity of 97% and sensitivity of 78% for CT The two false negative patients had no change in management (one was mild subluxation and another the patient needed prolonged collar for vertebral fracture)
�RESULTS: Almost 30% of the FE radiographs performed were either incomplete, suggesting that a full view or excursion was not realized, or ambiguous, suggesting that the films themselves could not be properly interpreted to provide reliable information.
�CONCLUSIONS: FE radiographs do not facilitate treatment and may lead to increased cost and prolonged cervical collars. FE radiographs often incomplete and unreliable making it difficult to use them to base management decisions.
� METHODS: Retrospective chart review of all patients admitted to a Level I trauma center with a negative CT scan of the cervical spine and a subsequent cervical flexion-extension study for evaluation of potential cervical spine injury. All flexion-extension films were independently reviewed to determine adequacy as defined by C 7/T 1 visualization and 30° of change in the angle from flexion to extension. The independent reviews were compared to formal radiology readings and the influence of the flexion-extension studies on clinical decision making was also reviewed. � RESULTS: 1000 patients met inclusion criteria for the study Review of the flexion-extension radiographs revealed that 80% of the films either did not adequately demonstrate the C 7/T 1 junction or had less than 30° range of motion. Radiologists only reported 23% of FE to be inadequate compared with 80% found by the authors There were 25 abnormal FE studies, all considered false positive as none required an intervention One normal FE study determined to be false negative at follow-up, with initial negative MRI. Ultimately required surgical stabilization. Results of the flexion-extension views had minimal effects on clinical decision making.
�CONCLUSIONS: Adequate flexion extension films are difficult to obtain and are minimally helpful for clearance of the cervical spine in awake and alert trauma patients.

�METHODS: Retrospective review of C-spine clearance at a level 1 trauma center. A trauma radiology database was queried for those patients with both a cervical spine CT and flexion-extension radiography through 10 year period; a single radiologist trained in trauma and critical care examined all acute (within 7 days) flexion-extension radiographs for adequacy. � Visualization of the cervical spine from base of occiput to top of first thoracic vertebrae (T 1) � Greater than or equal to 30° of angulation in both flexion and extension
�RESULTS: 355 flexion-extension radiographs were examined The entire cervical spine was not visualized in 55% and deemed inadequate Insufficient range of motion was seen in 45% of those with adequate visualization of the cervical spine Overall adequacy rate of the flexion-extension radiographs was 5% �CONCLUSIONS: The majority of flexion-extension radiographs are inadequate and should not be included in the algorithm for removal of the cervical collar If used, adequacy must be verified and supplemental radiographic studies obtained
�OBJECTIVE Perform a systematic review and to develop evidence-based recommendations that may answer the following PICO question: � In the obtunded adult blunt trauma patient, should cervical collar removal be performed after a negative high-quality C-spine CT result alone or after a negative high-quality C-spine CT combined with adjunct imaging, to reduce peri-clearance events, such as new neurologic change, unstable C-spine injury, need for post-clearance imaging, false negative CT imaging results on re-review, pressure ulcers, and time to cervical collar clearance?
� METHODS Eligibility criteria Adult blunt trauma patients 16 years or older � C-spine CT with axial thickness of less than 3 mm � Obtunded (GCS <15, unconscious, intubated, altered mental status, unreliable exam, distracting injury, intoxication, or not meeting NEXUS guidelines) � Comparators � Each patient underwent a C-spine CT that was read as normal and was then retested with the comparator adjunct imaging and/or physical exam Outcomes Critical outcome New neurologic change resulting in paraplegia or quadriplegia after cervical collar removal and identification of an unstable injury � Secondary outcomes Stable C-spine injury, post-clearance imaging, false-negative CT imaging result on re-review, pressure ulcers, and time to cervical collar removal �
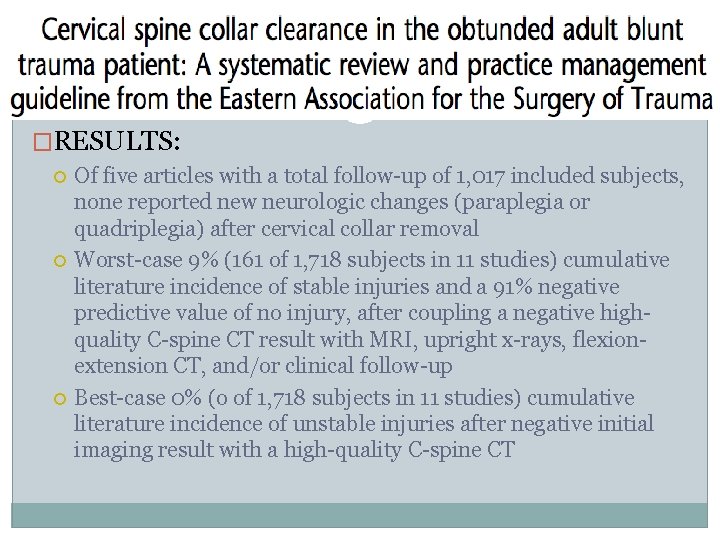
�RESULTS: Of five articles with a total follow-up of 1, 017 included subjects, none reported new neurologic changes (paraplegia or quadriplegia) after cervical collar removal Worst-case 9% (161 of 1, 718 subjects in 11 studies) cumulative literature incidence of stable injuries and a 91% negative predictive value of no injury, after coupling a negative highquality C-spine CT result with MRI, upright x-rays, flexionextension CT, and/or clinical follow-up Best-case 0% (o of 1, 718 subjects in 11 studies) cumulative literature incidence of unstable injuries after negative initial imaging result with a high-quality C-spine CT

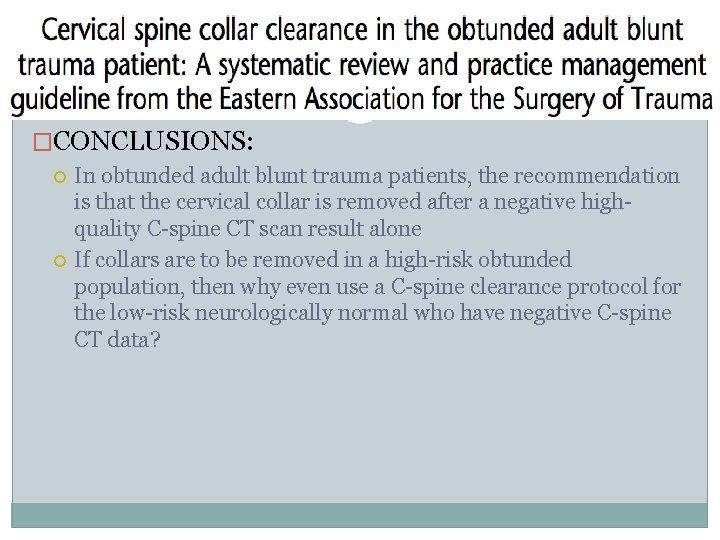
�CONCLUSIONS: In obtunded adult blunt trauma patients, the recommendation is that the cervical collar is removed after a negative highquality C-spine CT scan result alone If collars are to be removed in a high-risk obtunded population, then why even use a C-spine clearance protocol for the low-risk neurologically normal who have negative C-spine CT data?
Conclusions
�FE radiographs often lead to false-positive results, which could lead to additional unnecessary testing, immobilization, and hospitalization �The images in FE radiographs are often inadequate �There is no role for FE radiographs in the trauma patient who has a normal cervical spine CT
Questions?
References �Available upon request
 John 14:1-3
John 14:1-3 After me after me after me
After me after me after me Chapter 39 digital imaging film and radiographs
Chapter 39 digital imaging film and radiographs Faulty radiographs
Faulty radiographs Chapter 39 digital imaging film and radiographs
Chapter 39 digital imaging film and radiographs Machine that automates all film-processing stops
Machine that automates all film-processing stops Lower oblique occlusal radiograph
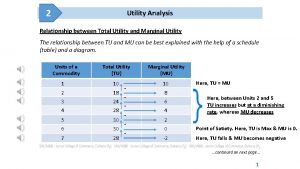
Lower oblique occlusal radiograph Relation between marginal utility and total utility
Relation between marginal utility and total utility Cardinal utility approach
Cardinal utility approach Inversion with negative adverbials exercises
Inversion with negative adverbials exercises Negative adverbial inversion
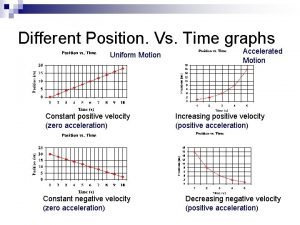
Negative adverbial inversion Negative velocity negative acceleration
Negative velocity negative acceleration Constant rightward velocity
Constant rightward velocity Same signs add and keep
Same signs add and keep 101012 bằng
101012 bằng Thể thơ truyền thống
Thể thơ truyền thống Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Cong thức tính động năng
Cong thức tính động năng Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phản ứng thế ankan
Phản ứng thế ankan Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu điện thế nghỉ
điện thế nghỉ Dot
Dot Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Chó sói
Chó sói Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Phối cảnh
Phối cảnh Một số thể thơ truyền thống
Một số thể thơ truyền thống Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Ng-html
Ng-html