Sepsis Affects 1 million Americansyear 3 rd leading
















- Slides: 68

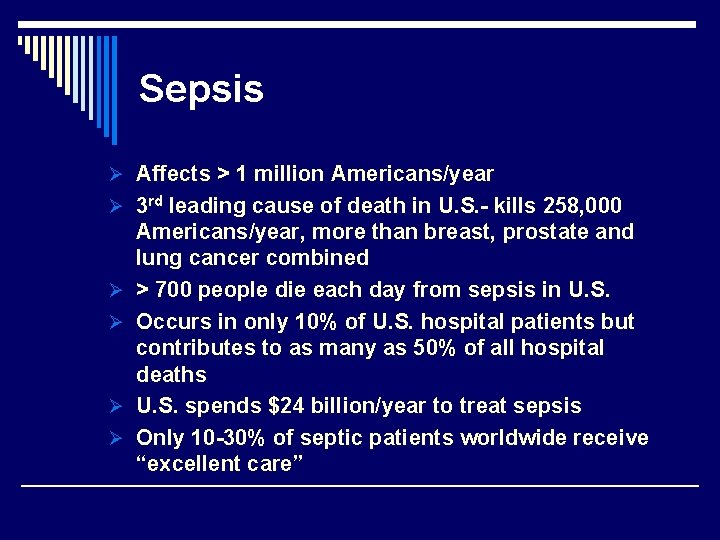
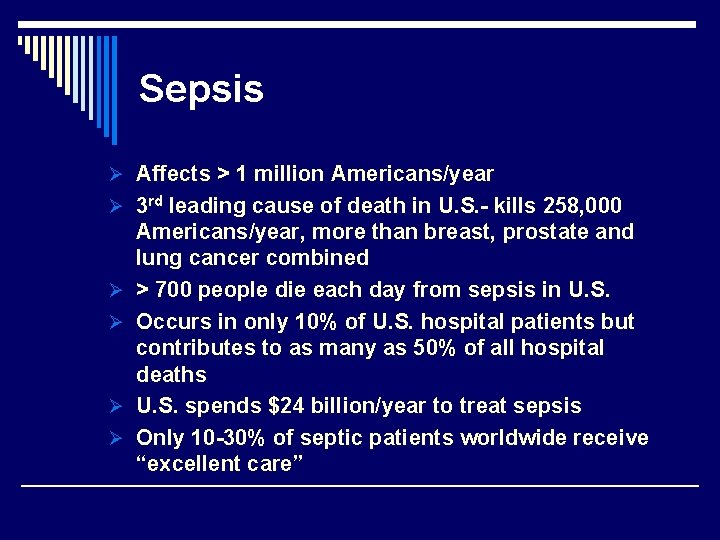
Sepsis Ø Affects > 1 million Americans/year Ø 3 rd leading cause of death in U. S. - kills 258, 000 Ø Ø Americans/year, more than breast, prostate and lung cancer combined > 700 people die each day from sepsis in U. S. Occurs in only 10% of U. S. hospital patients but contributes to as many as 50% of all hospital deaths U. S. spends $24 billion/year to treat sepsis Only 10 -30% of septic patients worldwide receive “excellent care”
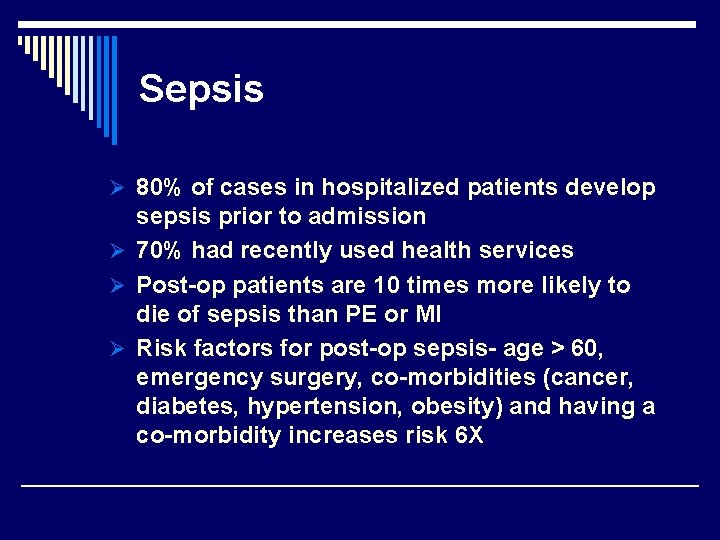
Sepsis Ø 80% of cases in hospitalized patients develop sepsis prior to admission Ø 70% had recently used health services Ø Post-op patients are 10 times more likely to die of sepsis than PE or MI Ø Risk factors for post-op sepsis- age > 60, emergency surgery, co-morbidities (cancer, diabetes, hypertension, obesity) and having a co-morbidity increases risk 6 X
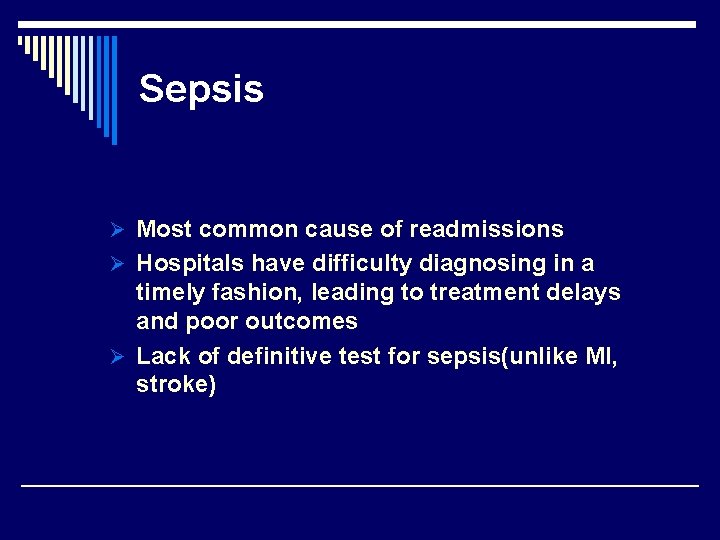
Sepsis Ø Most common cause of readmissions Ø Hospitals have difficulty diagnosing in a timely fashion, leading to treatment delays and poor outcomes Ø Lack of definitive test for sepsis(unlike MI, stroke)
Sepsis definitions

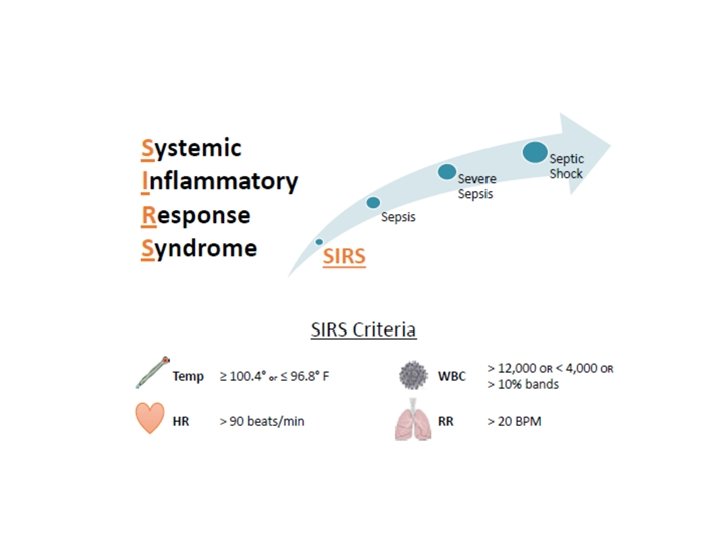
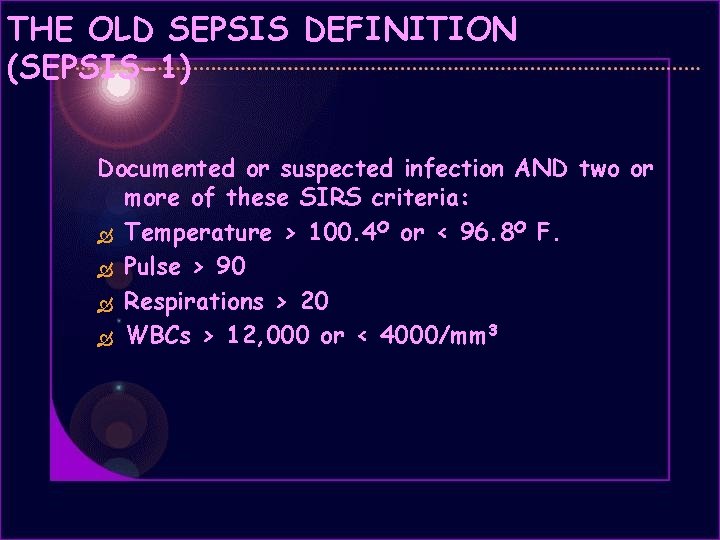
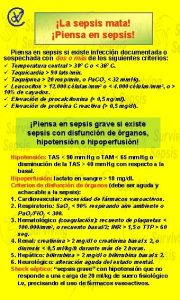
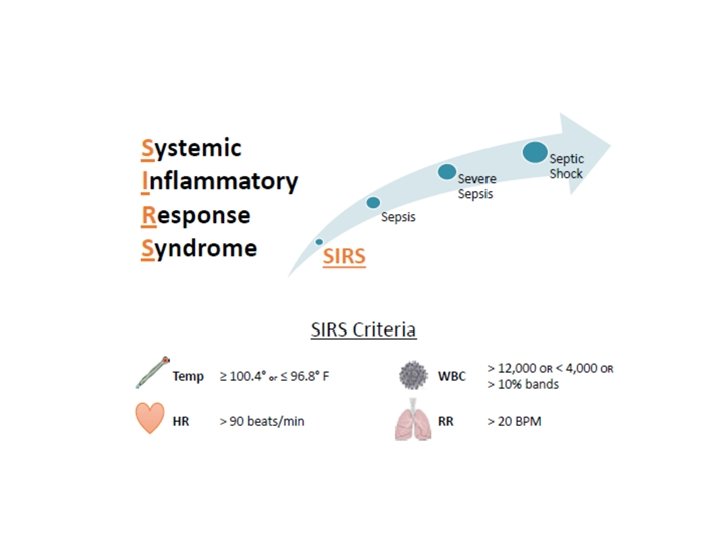
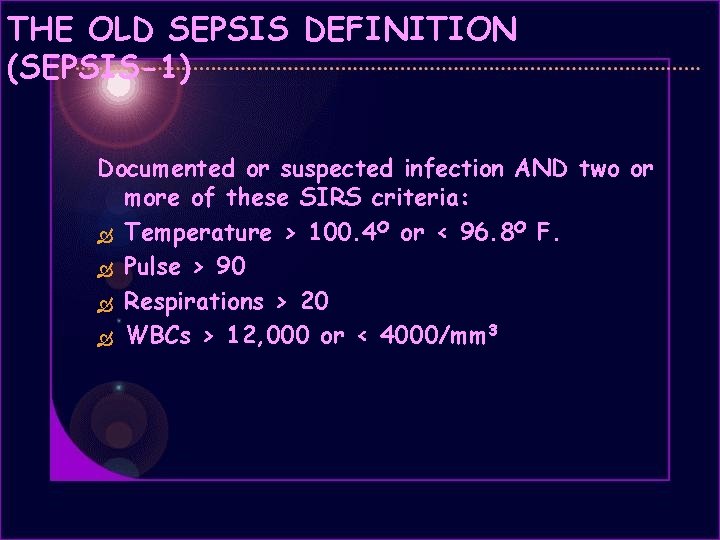
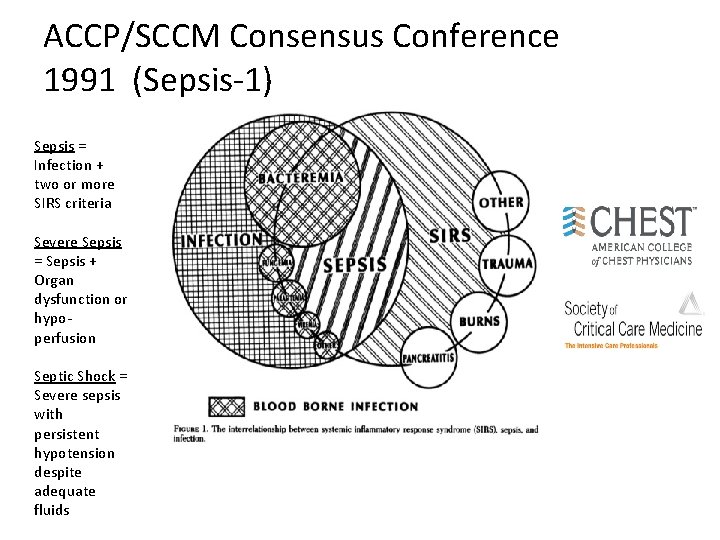
THE OLD SEPSIS DEFINITION (SEPSIS-1) Documented or suspected infection AND two or more of these SIRS criteria: Temperature > 100. 4 O or < 96. 8 O F. Pulse > 90 Respirations > 20 WBCs > 12, 000 or < 4000/mm 3
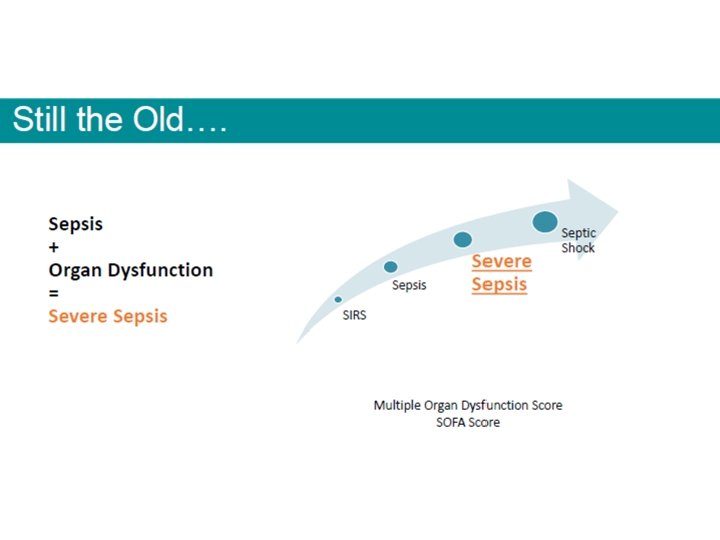

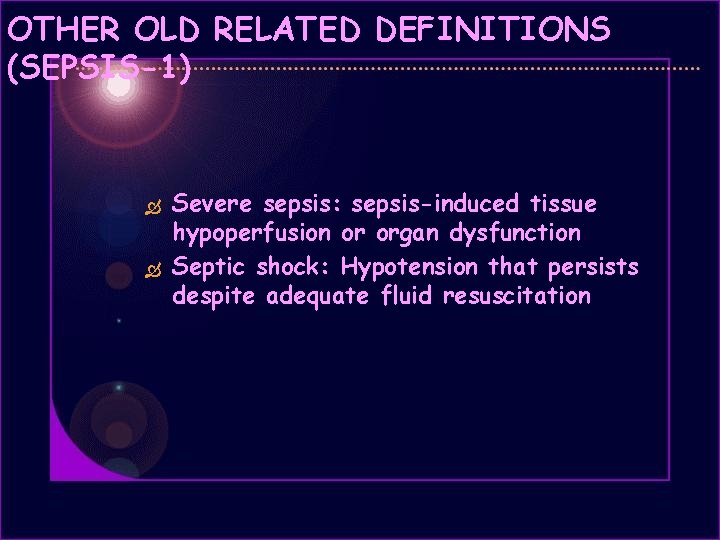
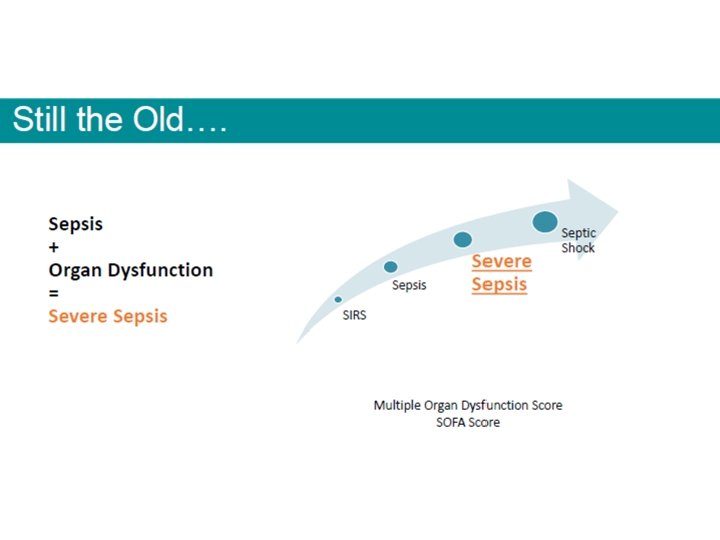
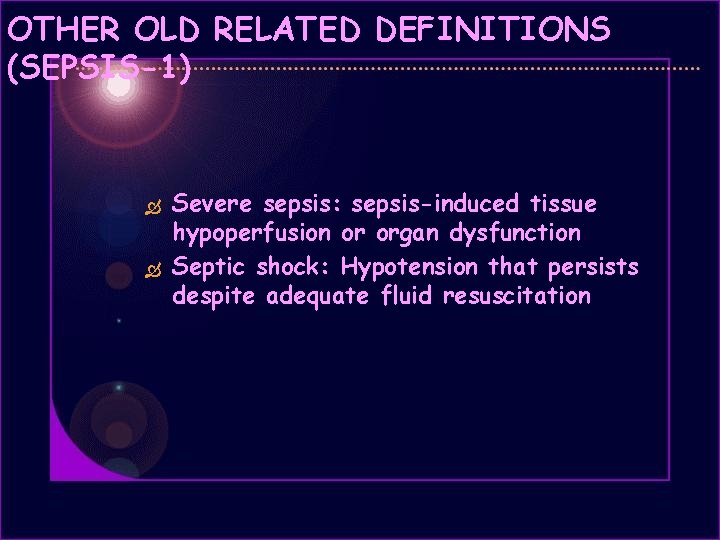
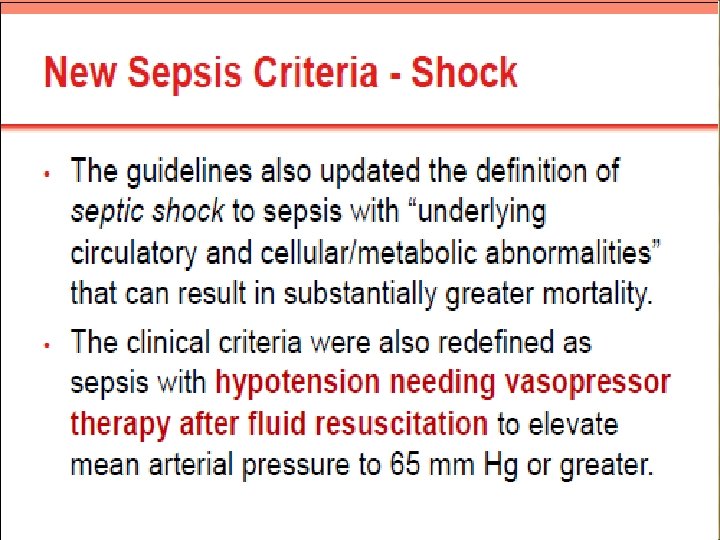
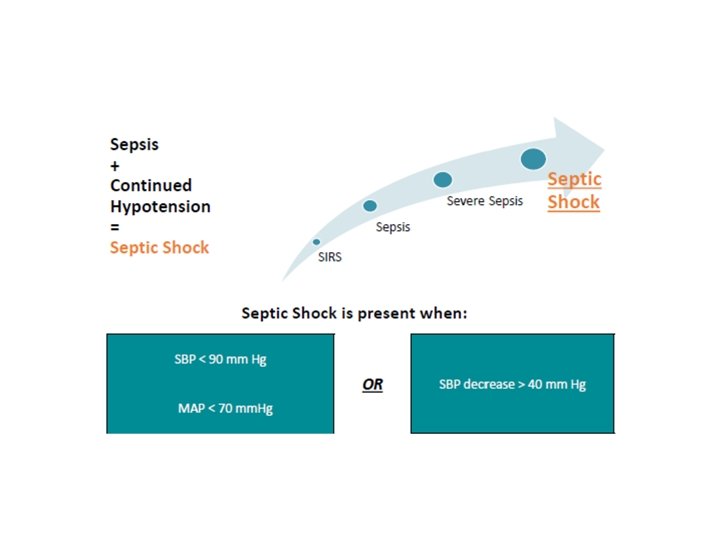
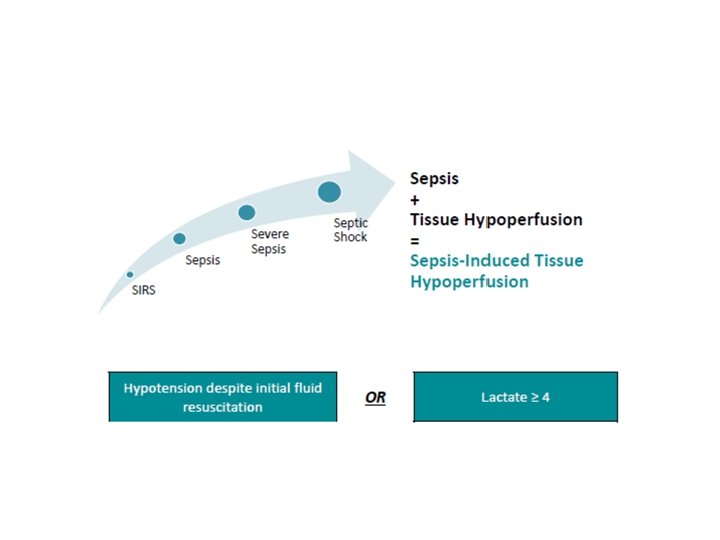
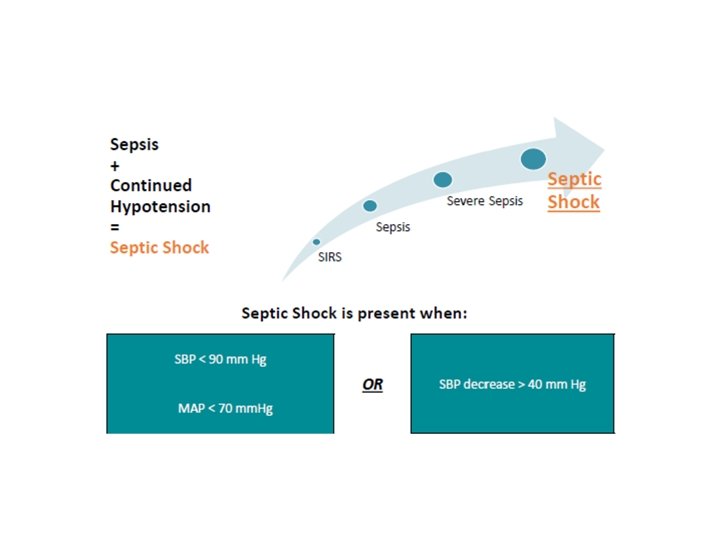
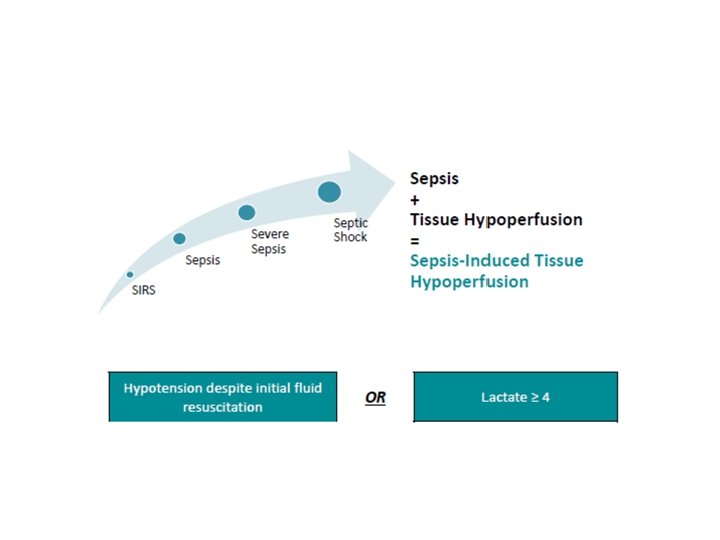
OTHER OLD RELATED DEFINITIONS (SEPSIS-1) Severe sepsis: sepsis-induced tissue hypoperfusion or organ dysfunction Septic shock: Hypotension that persists despite adequate fluid resuscitation
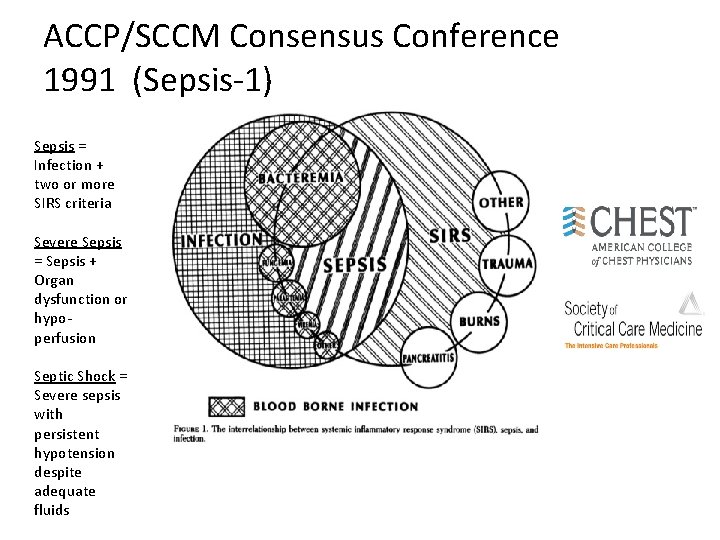
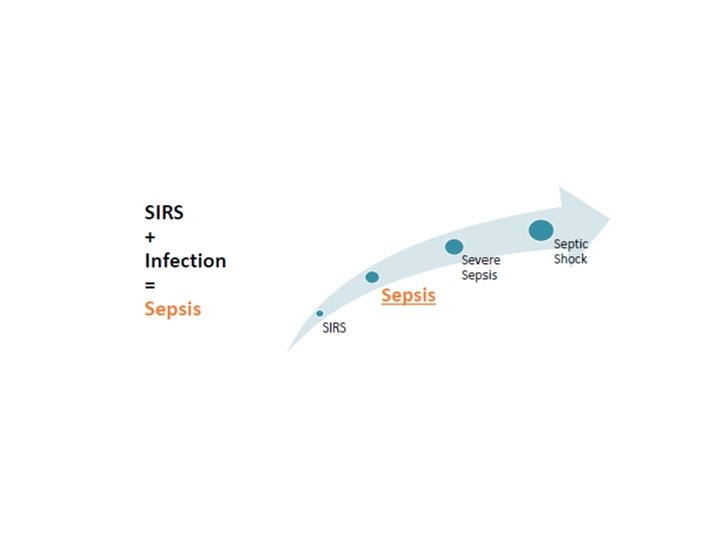
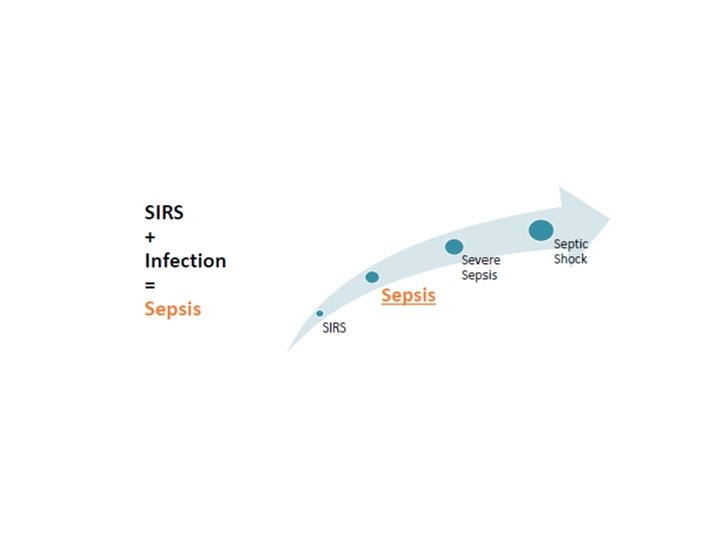
ACCP/SCCM Consensus Conference 1991 (Sepsis-1) Sepsis = Infection + two or more SIRS criteria Severe Sepsis = Sepsis + Organ dysfunction or hypoperfusion Septic Shock = Severe sepsis with persistent hypotension despite adequate fluids
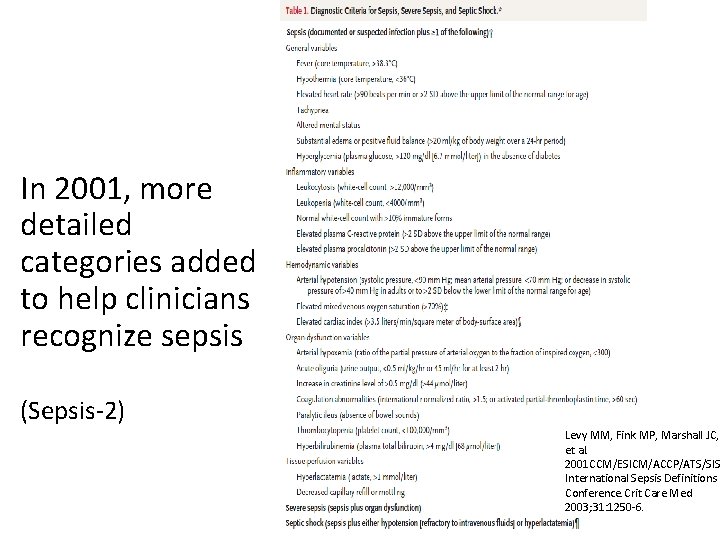
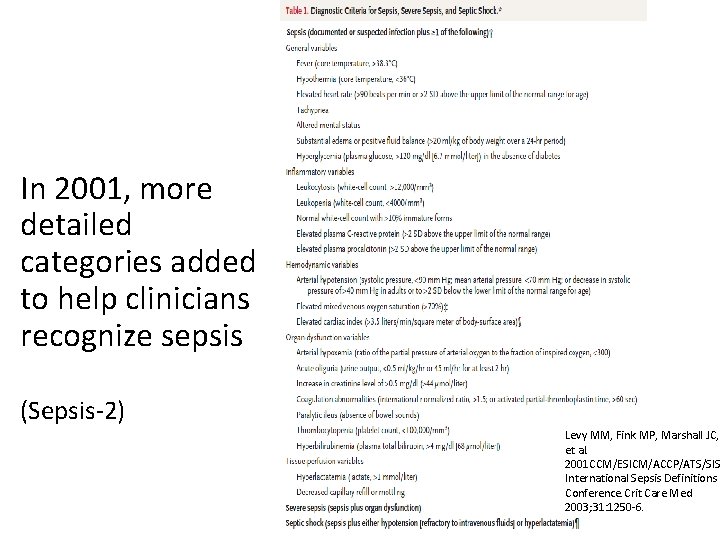
In 2001, more detailed categories added to help clinicians recognize sepsis (Sepsis-2) Levy MM, Fink MP, Marshall JC, et al. 2001 CCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 2003; 31: 1250 -6.
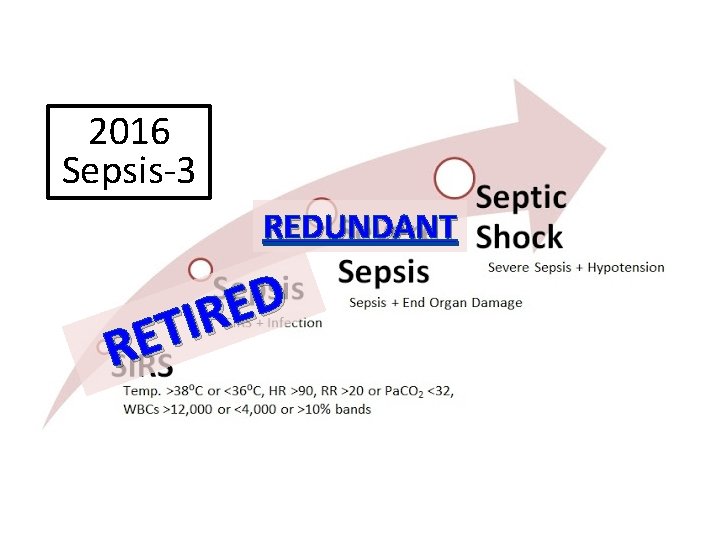
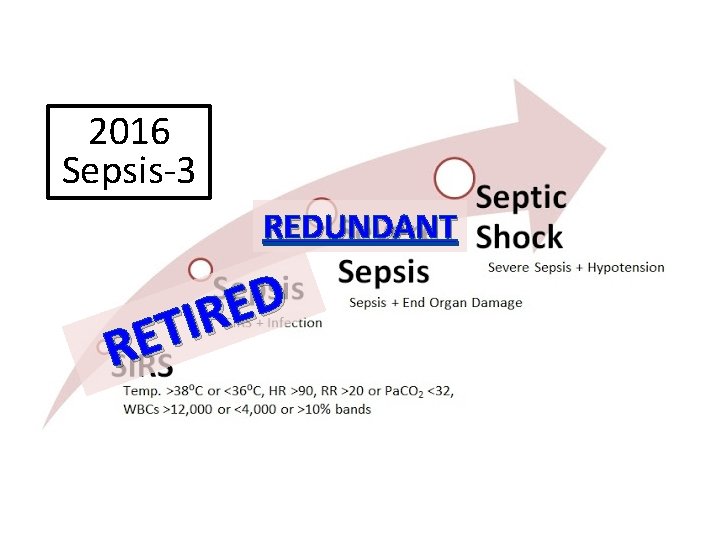
2016 Sepsis-3 REDUNDANT D E R I T E R

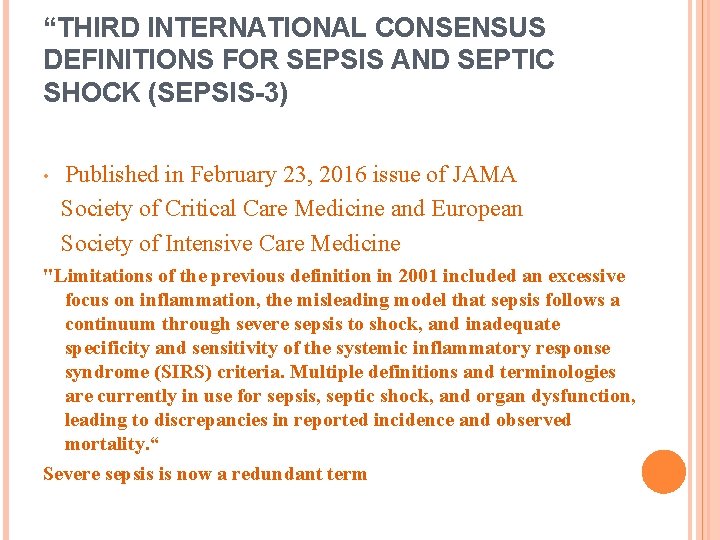
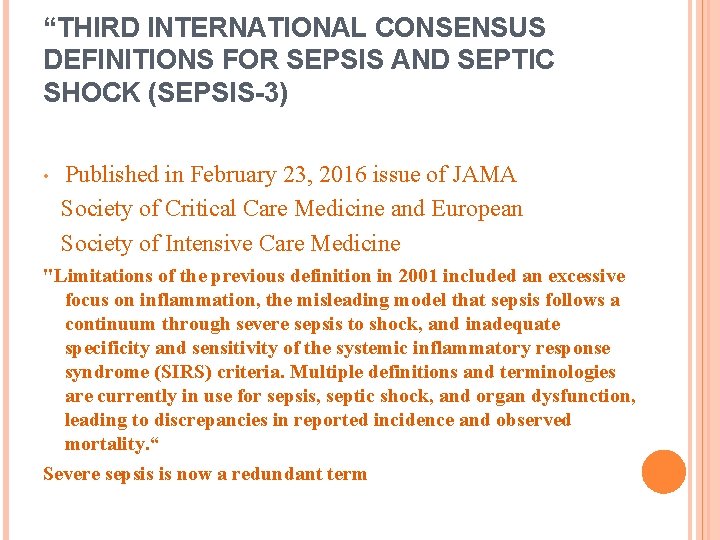
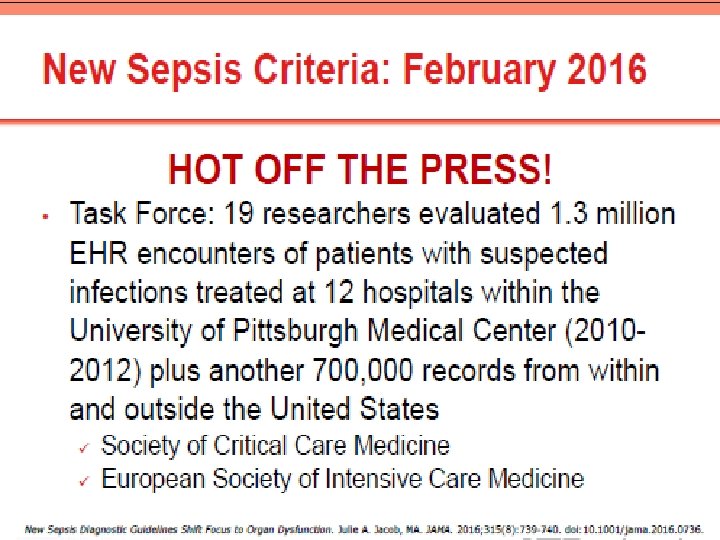
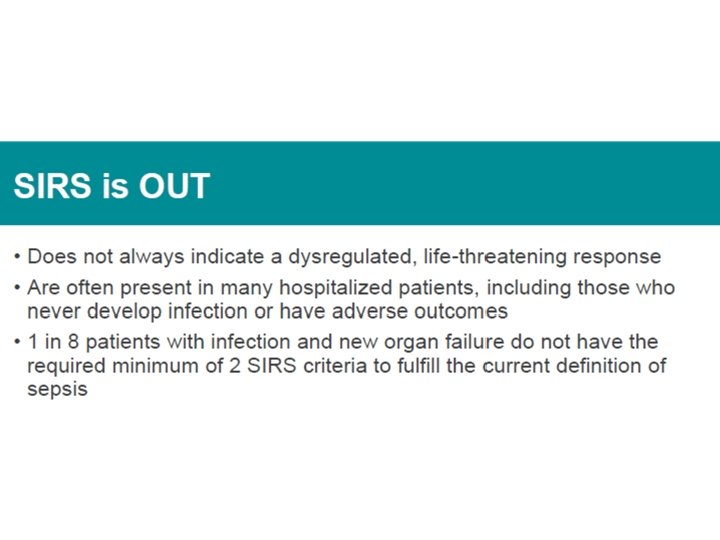
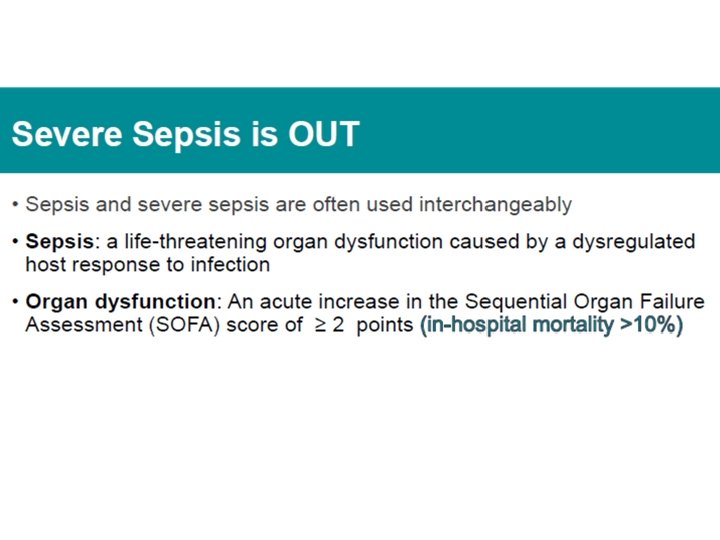
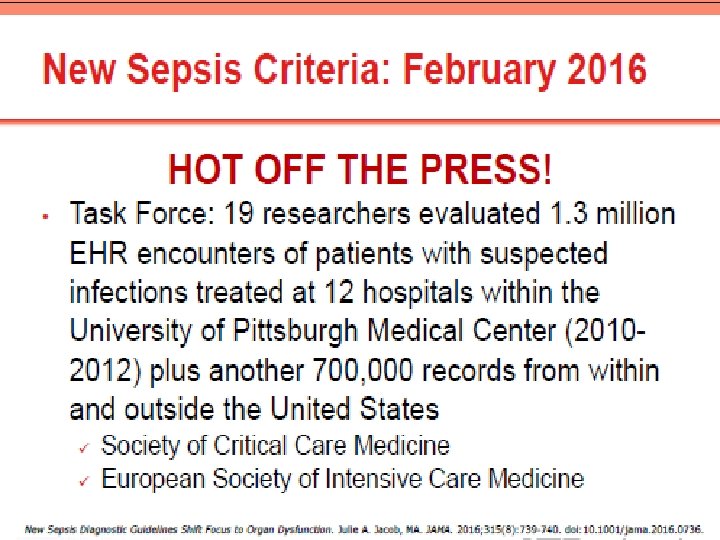
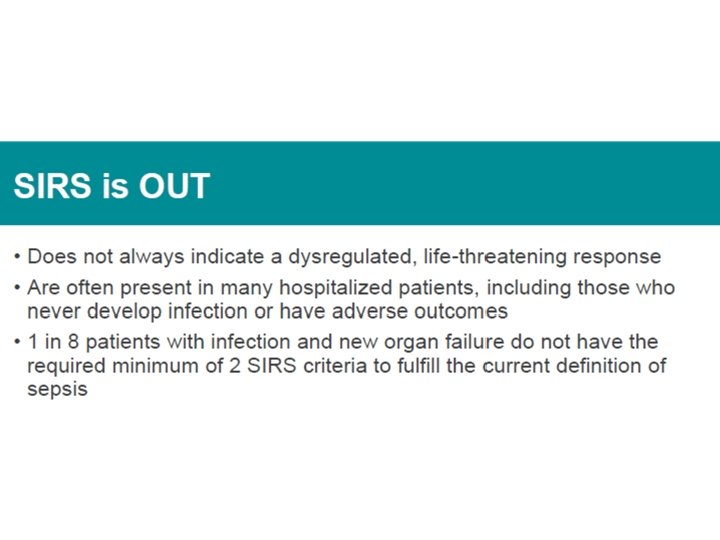
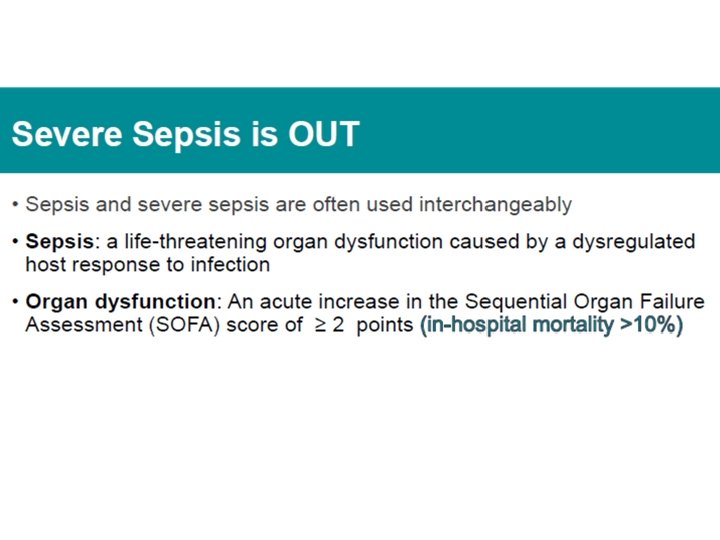
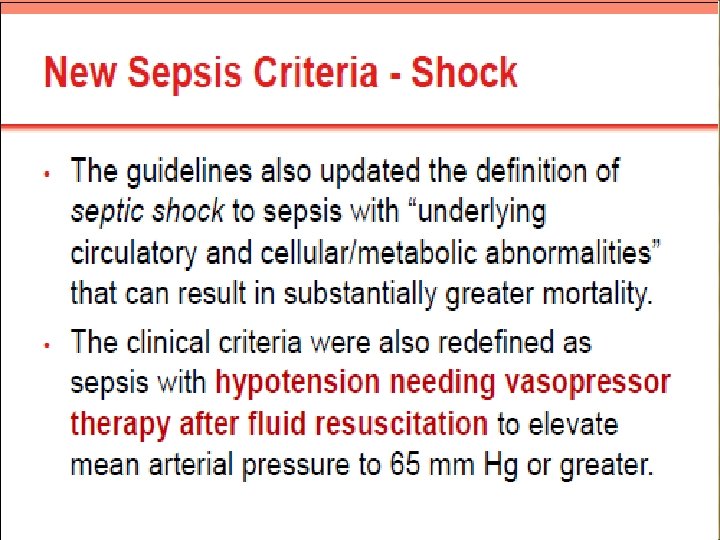
“THIRD INTERNATIONAL CONSENSUS DEFINITIONS FOR SEPSIS AND SEPTIC SHOCK (SEPSIS-3) • Published in February 23, 2016 issue of JAMA Society of Critical Care Medicine and European Society of Intensive Care Medicine "Limitations of the previous definition in 2001 included an excessive focus on inflammation, the misleading model that sepsis follows a continuum through severe sepsis to shock, and inadequate specificity and sensitivity of the systemic inflammatory response syndrome (SIRS) criteria. Multiple definitions and terminologies are currently in use for sepsis, septic shock, and organ dysfunction, leading to discrepancies in reported incidence and observed mortality. “ Severe sepsis is now a redundant term



Treatment Guidelines

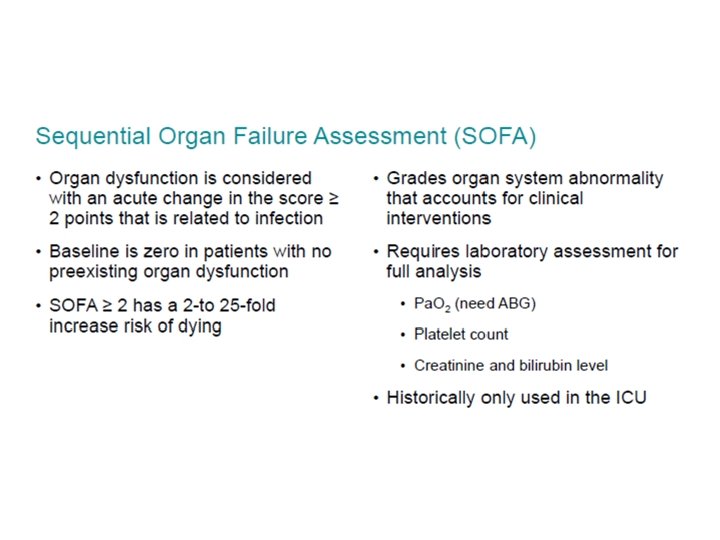

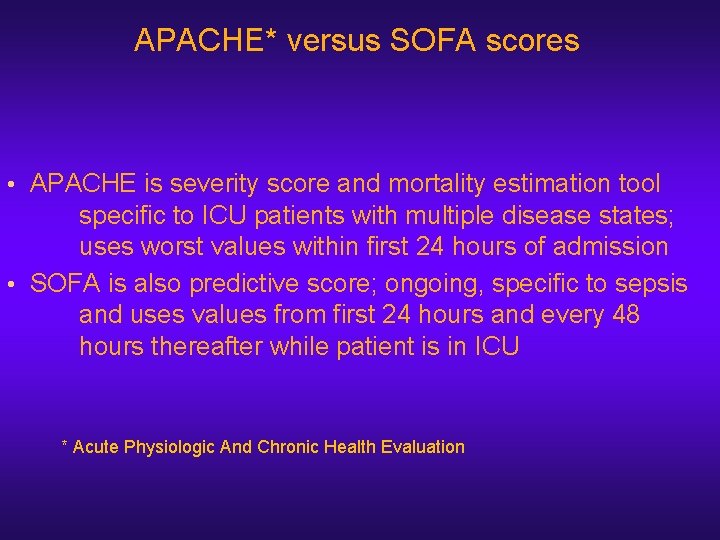
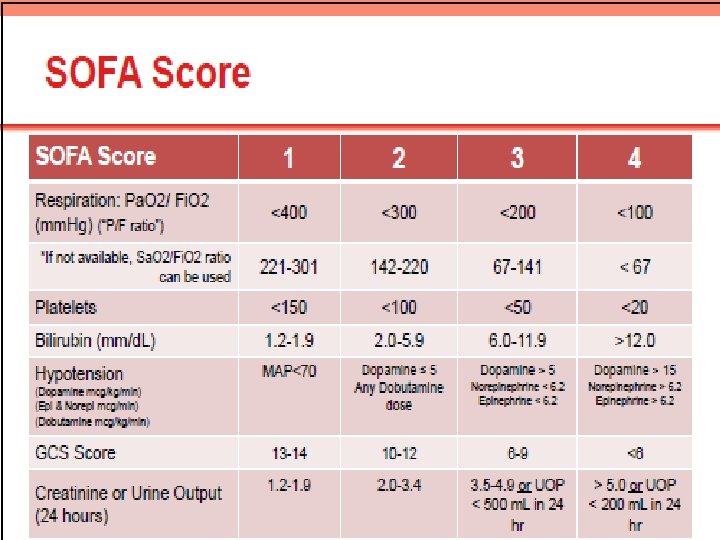
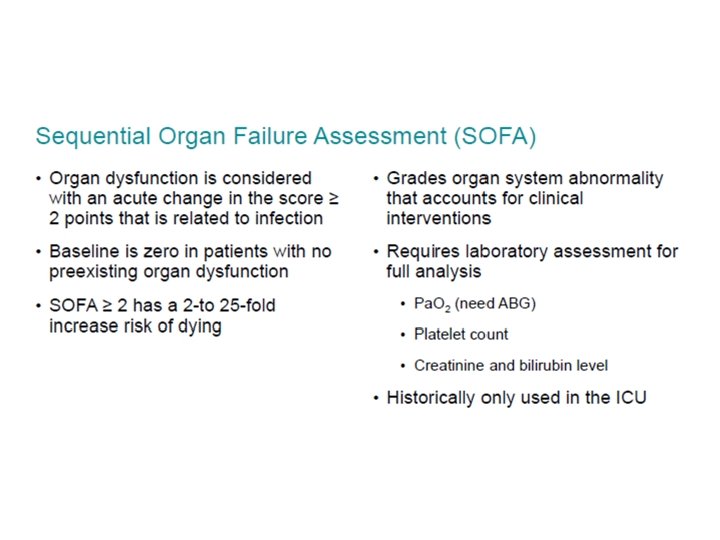
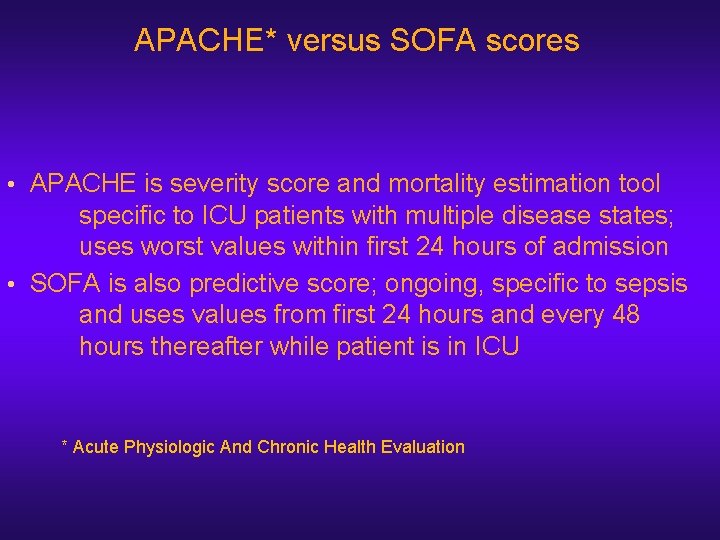
APACHE* versus SOFA scores • APACHE is severity score and mortality estimation tool specific to ICU patients with multiple disease states; uses worst values within first 24 hours of admission • SOFA is also predictive score; ongoing, specific to sepsis and uses values from first 24 hours and every 48 hours thereafter while patient is in ICU * Acute Physiologic And Chronic Health Evaluation
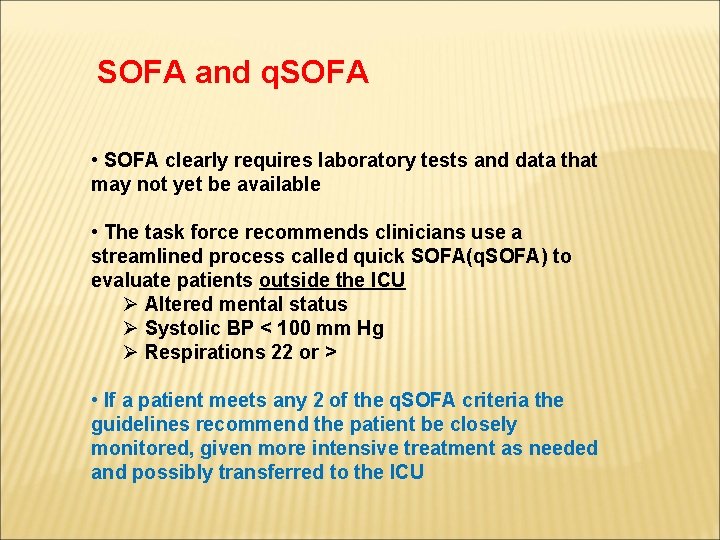
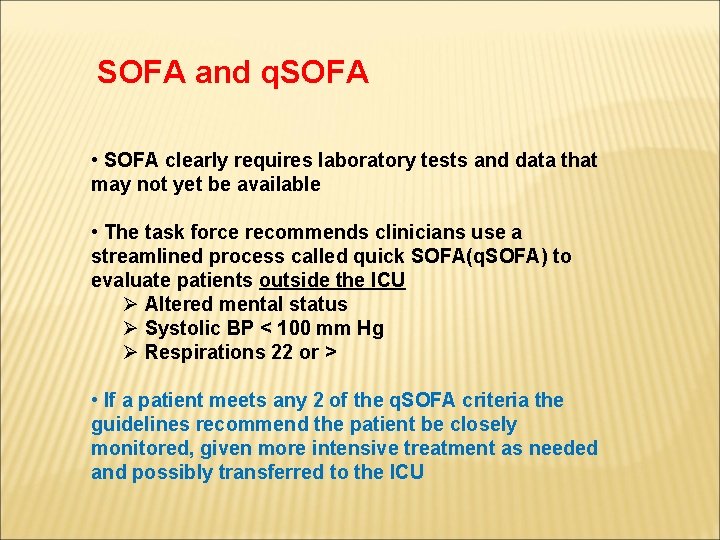
SOFA and q. SOFA • SOFA clearly requires laboratory tests and data that may not yet be available • The task force recommends clinicians use a streamlined process called quick SOFA(q. SOFA) to evaluate patients outside the ICU Ø Altered mental status Ø Systolic BP < 100 mm Hg Ø Respirations 22 or > • If a patient meets any 2 of the q. SOFA criteria the guidelines recommend the patient be closely monitored, given more intensive treatment as needed and possibly transferred to the ICU

IF YOU THINK THE PROBLEMS WE CREATE ARE BAD, JUST WAIT UNTIL YOU SEE OUR SOLUTIONS.
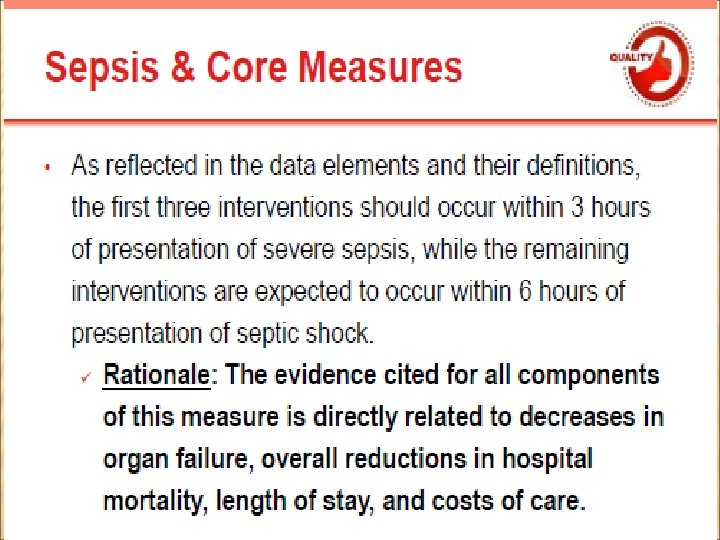
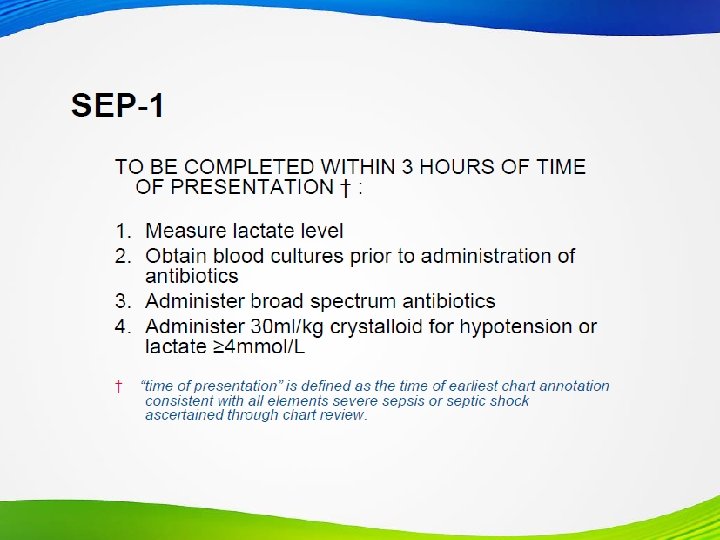
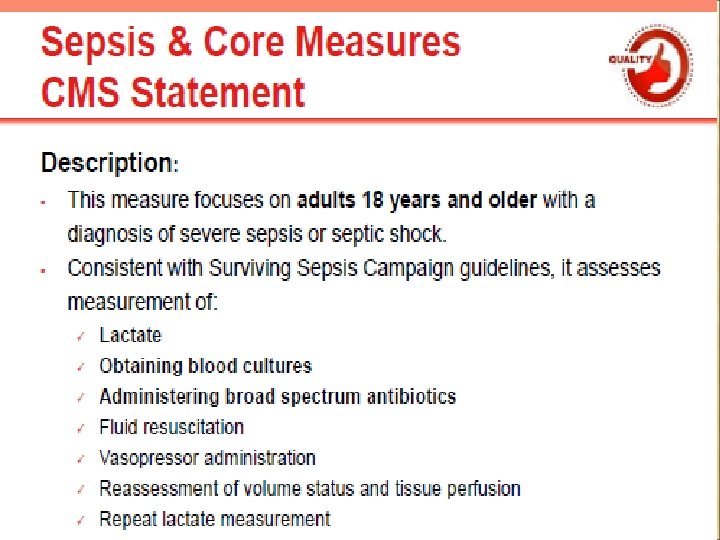
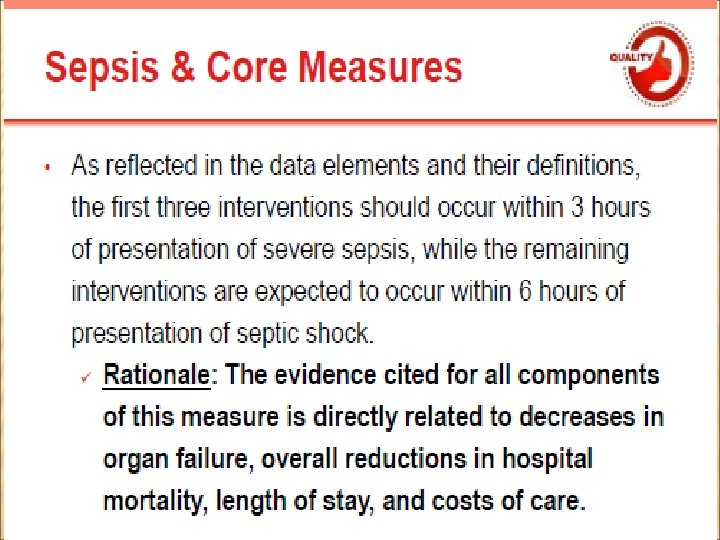
CMS Sepsis Core Measure



Caveats for CDI/Coding- The Past n n n CDI versus coding wars. Physicians often waited until patient was very ill to call the condition sepsis. Some hospitals convinced physicians to document SIRS-positive patients as septic even though they were only in a rule-out phase. Many of those patients ended up not having sepsis but were coded as sepsis anyway even in physician indicates “rule out sepsis” in discharge summary.
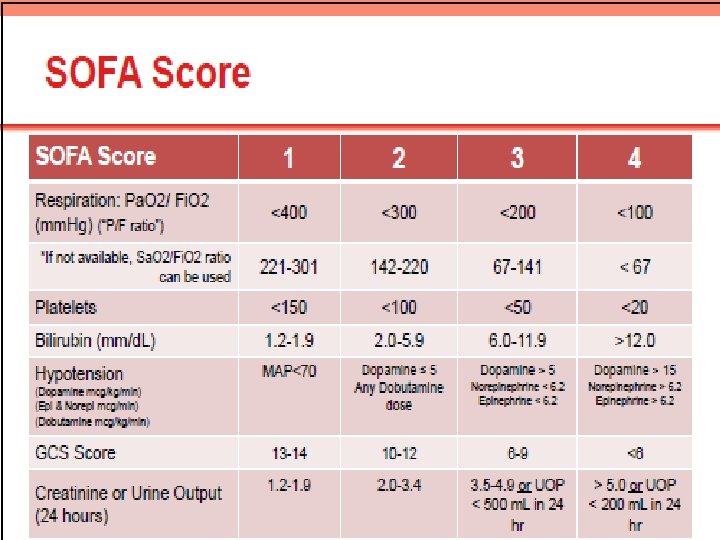
Caveats for CDI/Coding-The Present n n n If physicians write sepsis in the chart now using the new definition, it will correspond with the old definition's state of severe sepsis. Some coders may not code severe sepsis unless the physician explicitly writes 'severe. ' This may lead to discrepancies in coding practice. The SIRS criteria came out about 15 years ago, and even today CDI specialists query providers regarding SIRS has fairly easy to remember criteria versus those of SOFA, which has six different criteria with scores ranging from 0 to 4.
Caveats for CDI/Coding-The Future n n As more physicians embrace the new criteria, the effect on coding will be fewer reported cases of sepsis, but a greater percentage of those will be reported as severe sepsis. Hospital administrators will need to be aware that a shift in severity of illness or case mix index data may correspond to the new sepsis definition rather than to coding errors. Now, some physicians will embrace the sepsis-3 definition while others will continue their pattern of diagnosis based on the sepsis-2 definition. Furthermore, since there will be inconsistencies in coding, that will cause billing and reporting problems. It will be difficult to compare sepsis rates from hospital to hospital and over time until there is uniformity across the country.
Caveats for CDI/Coding-The Future n n Once new updated guidelines from CMS are provided and implemented, CDI and coding will need to be educated on what those new rules and regulations are. Query questions will need to be updated based on those guidelines as will physicians. Hospitals will need to set a standard for validating sepsis, determine a start date to adopt the new definitions, ascertain how documentation flow will evolve and work collaboratively among physician leadership, the CDI team, and HIM to develop facility-specific definitions and establish an in-house query policy for sepsis.
Caveats for CDI/Coding n n Inpatient quality reporting must follow specifications and guidelines for each quality measure based on predetermined bundles. If the new definition is what everyone is reporting, then quality measures and reporting will have to adjust as well. Guidance is needed from those quality programs. Abstractors will need to know what sepsis criteria to follow when reviewing documentation on hospital adherence to these measures. The National Quality Forum measure is very clear: Hospitals will still have to expend energy according to the sepsis-2 definition and report to CMS. What will change is increased confusion for hospitals that grapple with two definitions. Physicians may use the new definitions, but the hospitals will use the old ones to report to CMS. They will have to go back to physicians to query what they meant in the record, which will be onerous and challenging for some facilities.
Caveats for CDI/Coding n n n Sepsis-3 states that patients with an infection meeting their sepsis criteria should be coded as R 65. 20 (severe sepsis) but this is impossible since this code in ICD-10 -CM can only be assigned if physician documents “severe sepsis” not sepsis alone or if documents that acute organ dysfunction is associated with sepsis ICD-10 -CM still has multitude of codes for sepsis without organ dysfunction (A 40 -A 41) Must code what physician documents regardless of clinical criteria used to arrive at that diagnosis

Caveats for CDI/Coding n n n For severe sepsis, “use additional code to identify specific acute organ dysfunction”; however, if no organ dysfunction is documented or coded, RAC may severe sepsis code is invalid Any coding of R 65. 20 or R 65. 21 subjects record to sepsis core measure eligibility New 2016 definitions do not currently align with CMS sepsis core measure and unknown when this will occur SIRS due to infection was built into ICD-9 in 2001 but can’t be coded as sepsis in ICD-10 -CM Continue to code sepsis, severe sepsis and septic shock using most current version of ICD-10 -CM
*Better intelligence
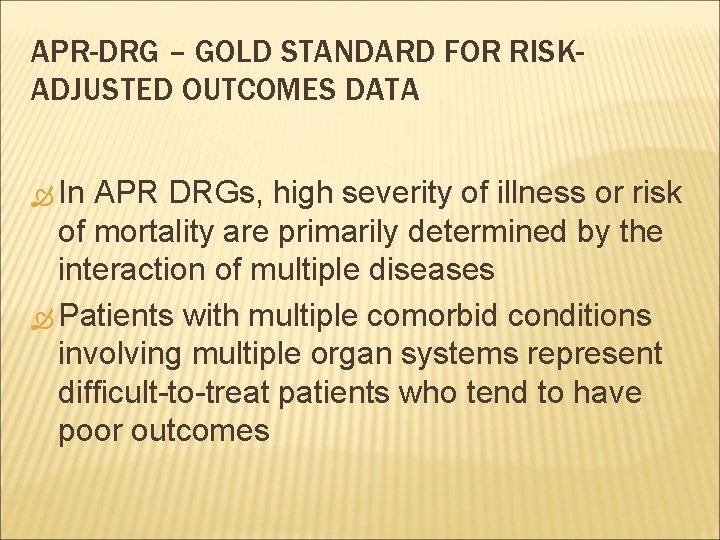
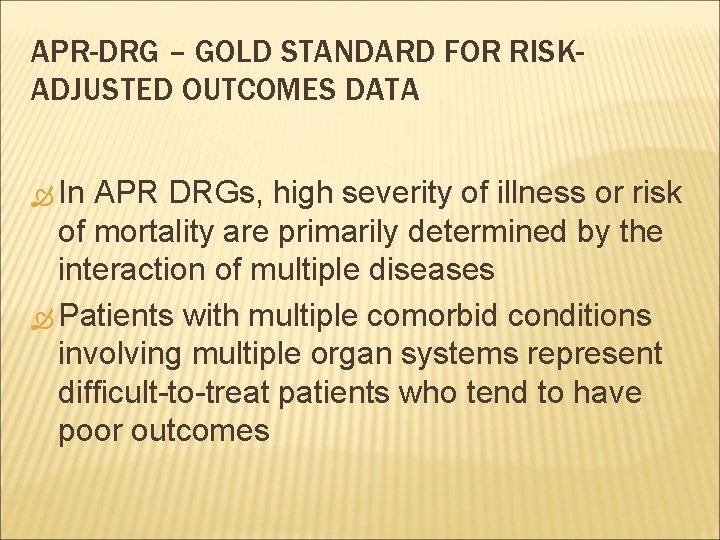
APR-DRG – GOLD STANDARD FOR RISKADJUSTED OUTCOMES DATA In APR DRGs, high severity of illness or risk of mortality are primarily determined by the interaction of multiple diseases Patients with multiple comorbid conditions involving multiple organ systems represent difficult-to-treat patients who tend to have poor outcomes
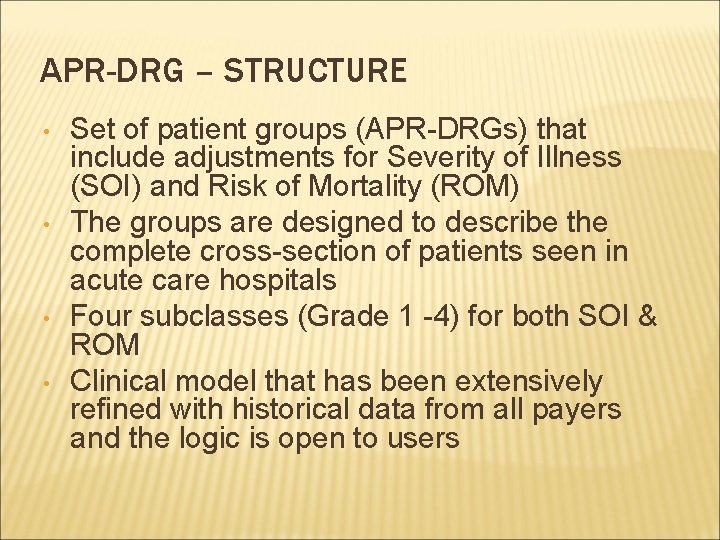
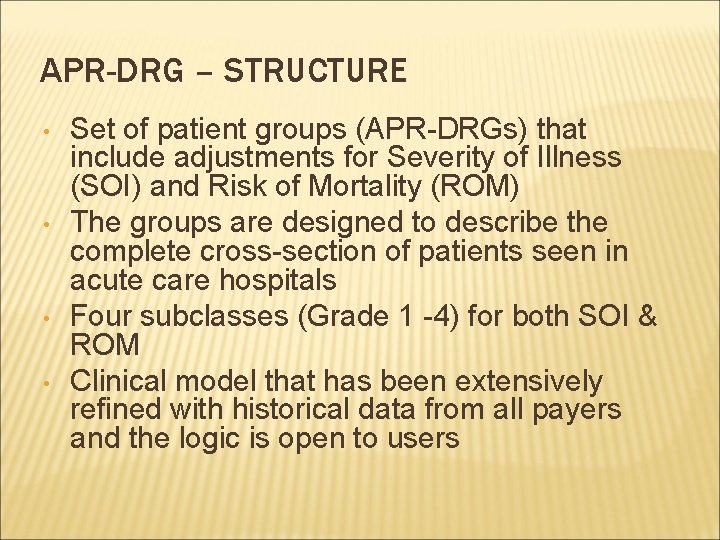
APR-DRG – STRUCTURE • • Set of patient groups (APR-DRGs) that include adjustments for Severity of Illness (SOI) and Risk of Mortality (ROM) The groups are designed to describe the complete cross-section of patients seen in acute care hospitals Four subclasses (Grade 1 -4) for both SOI & ROM Clinical model that has been extensively refined with historical data from all payers and the logic is open to users
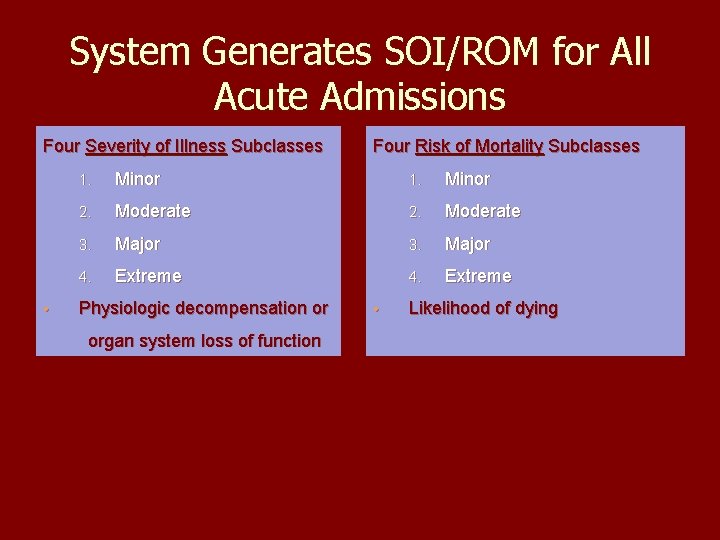
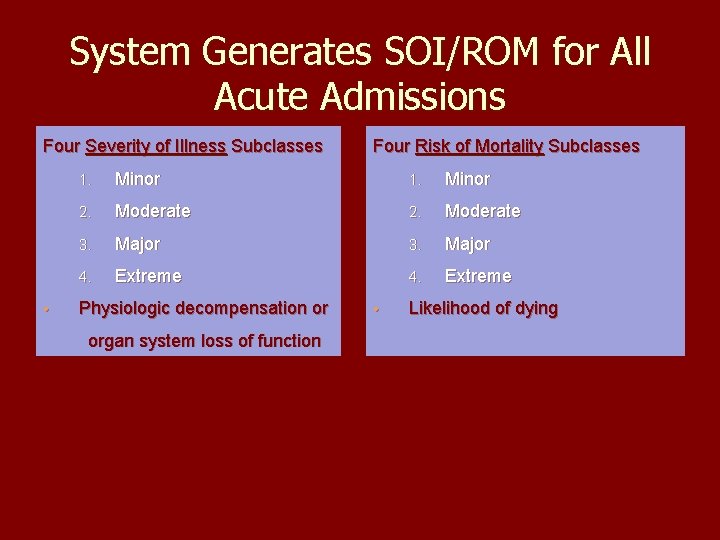
System Generates SOI/ROM for All Acute Admissions Four Severity of Illness Subclasses • Four Risk of Mortality Subclasses 1. Minor 2. Moderate 3. Major 4. Extreme Physiologic decompensation or organ system loss of function • Likelihood of dying
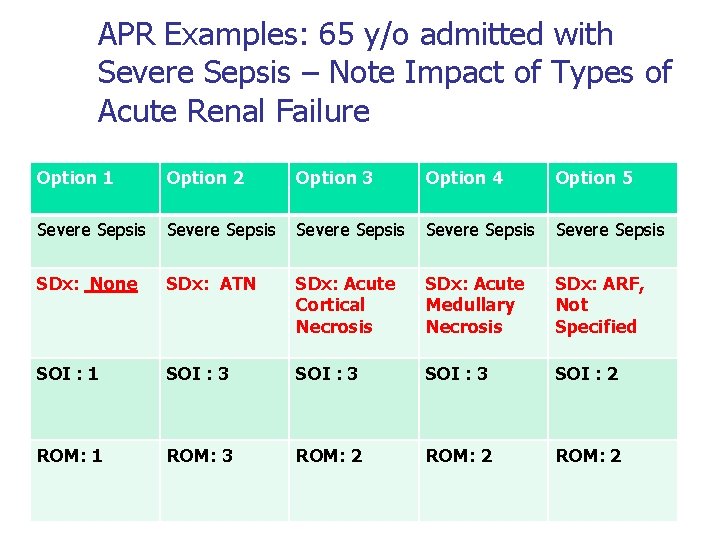
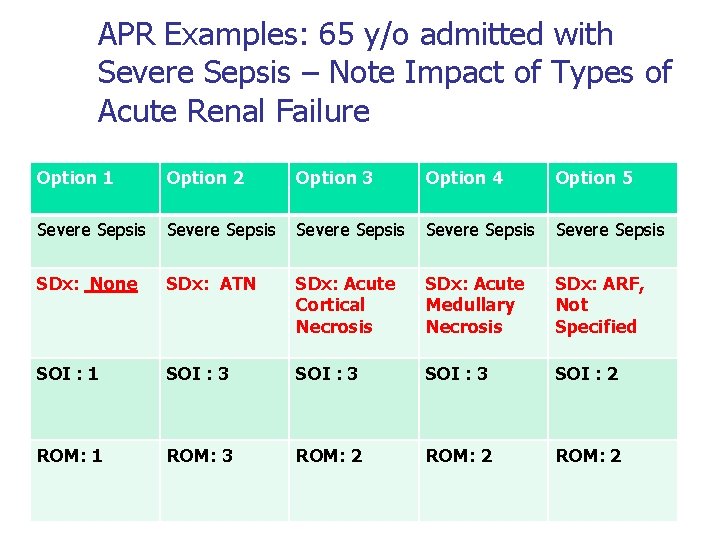
APR Examples: 65 y/o admitted with Severe Sepsis – Note Impact of Types of Acute Renal Failure Option 1 Option 2 Option 3 Option 4 Option 5 Severe Sepsis Severe Sepsis SDx: None SDx: ATN SDx: Acute Cortical Necrosis SDx: Acute Medullary Necrosis SDx: ARF, Not Specified SOI : 1 SOI : 3 SOI : 2 ROM: 1 ROM: 3 ROM: 2
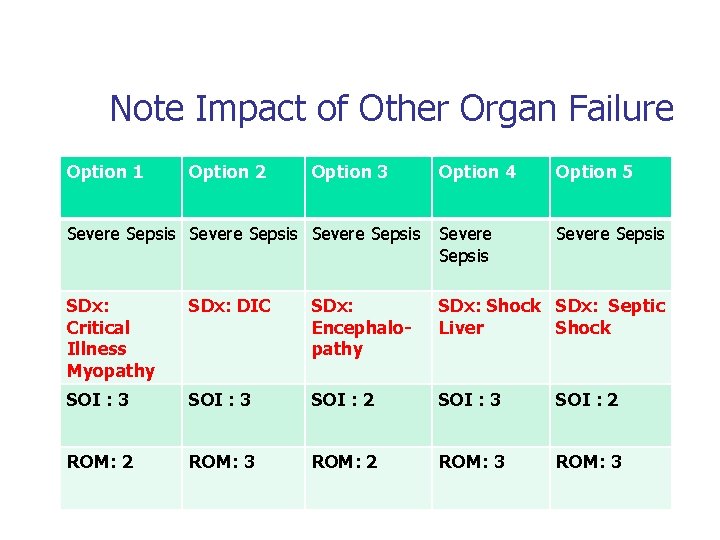
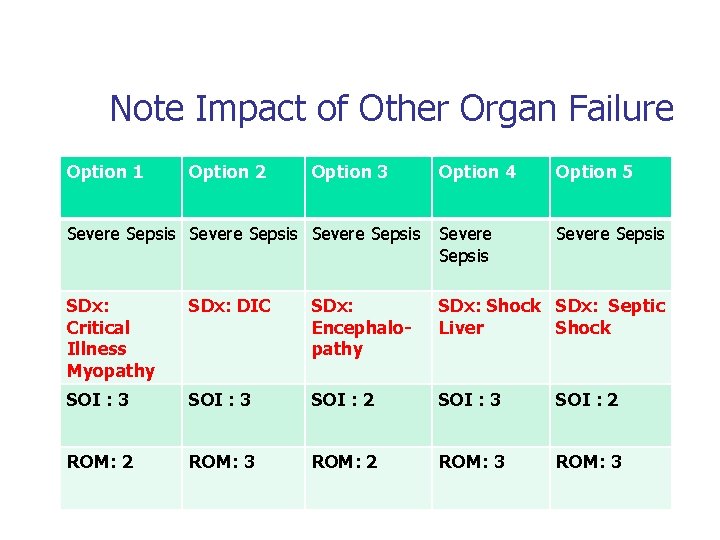
Note Impact of Other Organ Failure Option 1 Option 2 Option 3 Option 4 Option 5 Severe Sepsis Severe Sepsis SDx: Critical Illness Myopathy SDx: DIC SDx: Encephalopathy SDx: Shock SDx: Septic Liver Shock SOI : 3 SOI : 2 ROM: 3 ROM: 2 ROM: 3
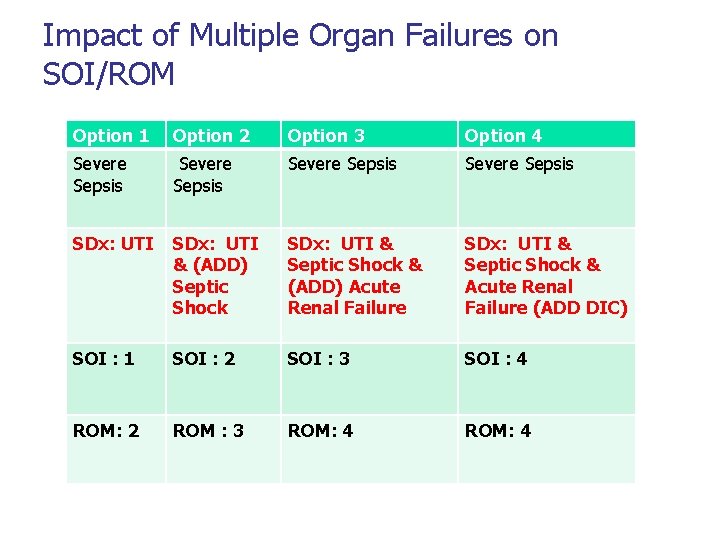
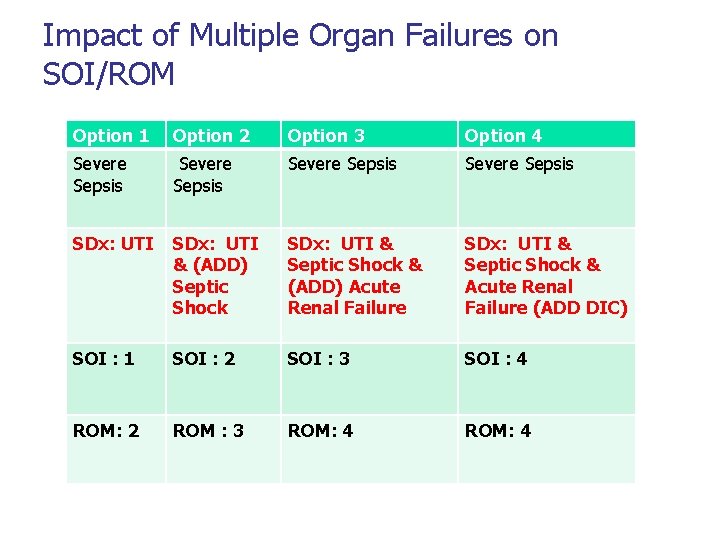
Impact of Multiple Organ Failures on SOI/ROM Option 1 Option 2 Option 3 Option 4 Severe Sepsis SDx: UTI & (ADD) Septic Shock SDx: UTI & Septic Shock & (ADD) Acute Renal Failure SDx: UTI & Septic Shock & Acute Renal Failure (ADD DIC) SOI : 1 SOI : 2 SOI : 3 SOI : 4 ROM: 2 ROM : 3 ROM: 4
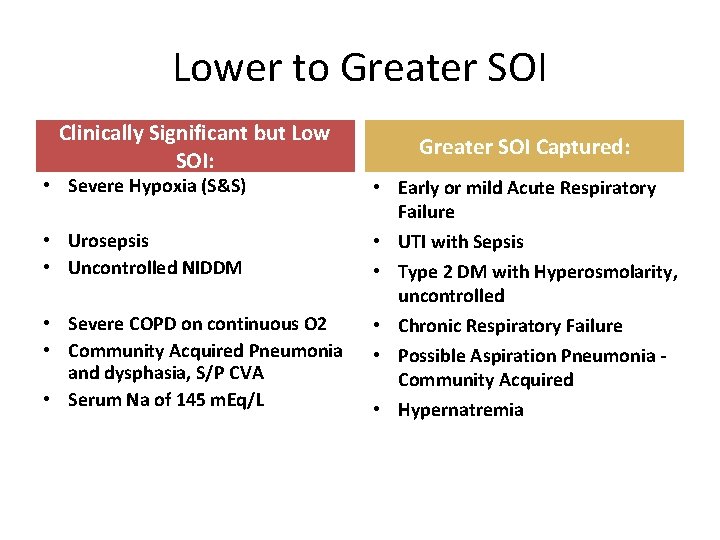
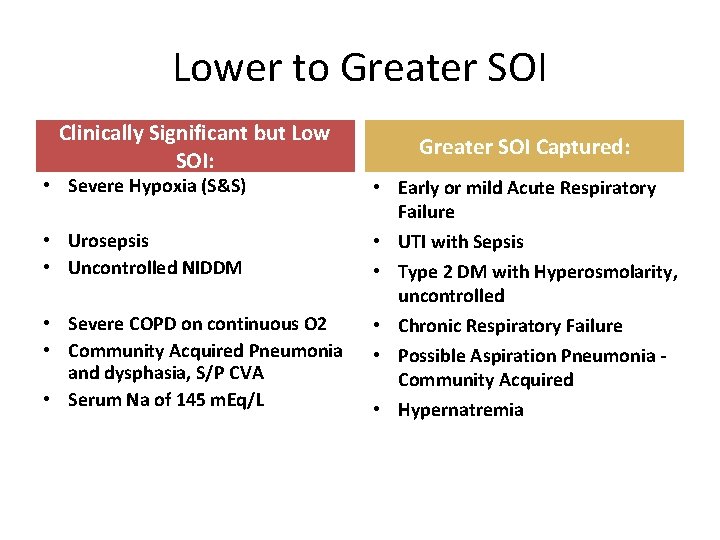
Lower to Greater SOI Clinically Significant but Low SOI: • Severe Hypoxia (S&S) • Urosepsis • Uncontrolled NIDDM • Severe COPD on continuous O 2 • Community Acquired Pneumonia and dysphasia, S/P CVA • Serum Na of 145 m. Eq/L Greater SOI Captured: • Early or mild Acute Respiratory Failure • UTI with Sepsis • Type 2 DM with Hyperosmolarity, uncontrolled • Chronic Respiratory Failure • Possible Aspiration Pneumonia Community Acquired • Hypernatremia
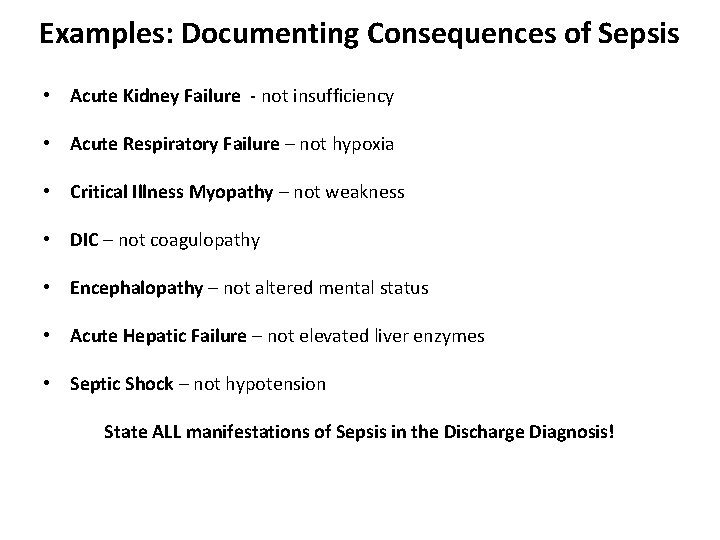
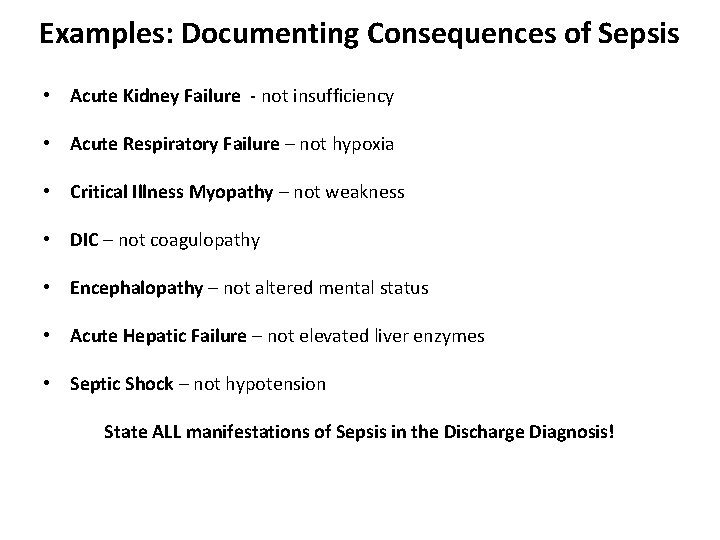
Examples: Documenting Consequences of Sepsis • Acute Kidney Failure - not insufficiency • Acute Respiratory Failure – not hypoxia • Critical Illness Myopathy – not weakness • DIC – not coagulopathy • Encephalopathy – not altered mental status • Acute Hepatic Failure – not elevated liver enzymes • Septic Shock – not hypotension State ALL manifestations of Sepsis in the Discharge Diagnosis!
Query? ? • A coder or other concurrent reviewer may ‘query’ a clinician regarding Severe Sepsis if certain conditions are present and the condition is not stated (or, sepsis IS stated, but not ‘supported’ by clinical indicators) • AHIMA released “Guidelines for Achieving a Compliant Query Practice, ” in the February 2013 edition of the Journal of AHIMA. The document, created in collaboration with ACDIS volunteers and approved by the ACDIS Advisory Board, states that coding (or CDI) staff should query the physician if a diagnosis is not supported by clinical indicator(s) in the medical record
Data Mining • Ensure all expired cases with low scores (2 or less) are reviewed systematically by clinician and coder prior to final coding • Review APR/DRG 720 for ROM/SOI Scores – Review cases with code assignment for 995. 92 : Severe Sepsis – with a ROM of ‘ 2’ or less (995. 92, Severe Sepsis) implies an organ failure – the ROM could be greater than ‘ 2’ when certain organ failure or combinations is/are reported with Severe Sepsis • Review cases with major infections that ARE NOT coded to Sepsis – Did these meet the SIRS Criteria and are not coded to Sepsis? – Examples, patients with Pneumonia, SBP, cholangitis – focus on those with high charges and/or extended LOS (GMLOS per MS-DRG Methodology)

Your Vital Roles Public reporting-Healthgrades, Leapfrog, CMS • PEPPER* • RAC audits • VBP- core measures • MD- could support higher than expected mortality and readmission rates • * Program for Evaluating Payment Patterns Electronic Report
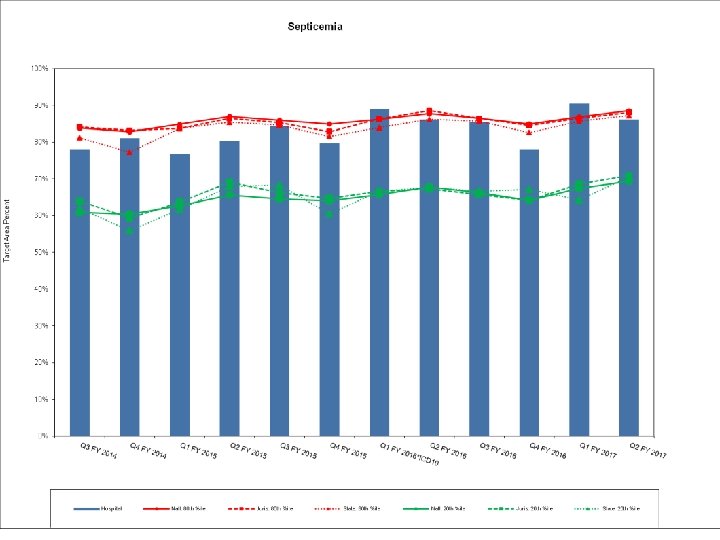
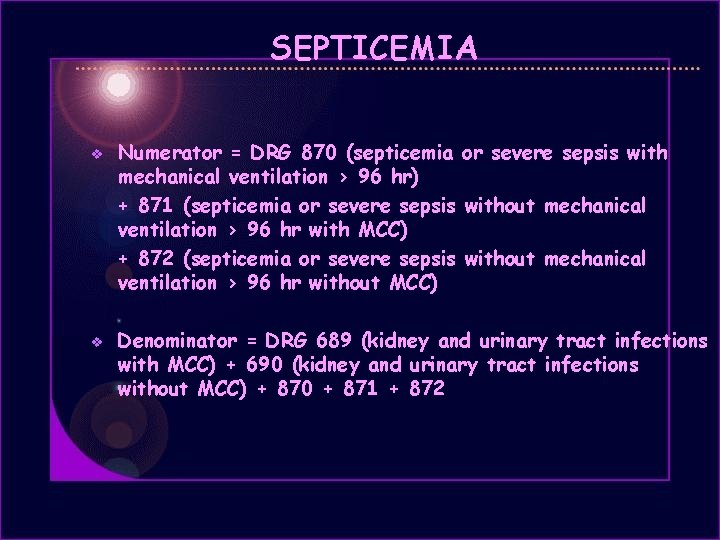
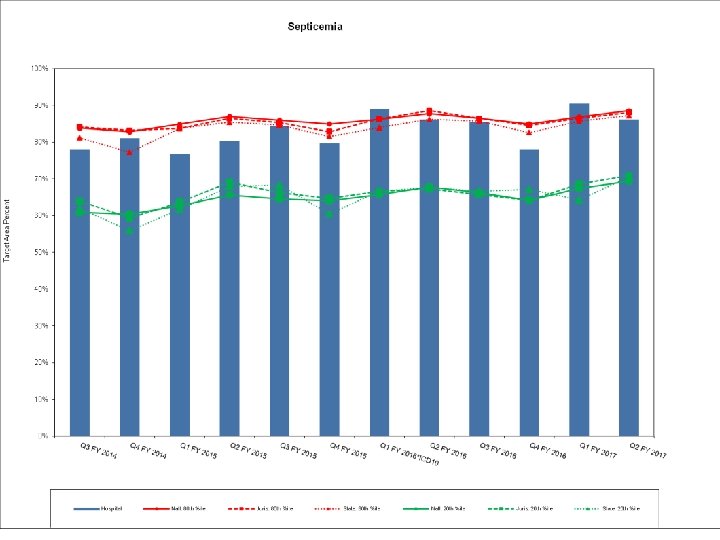
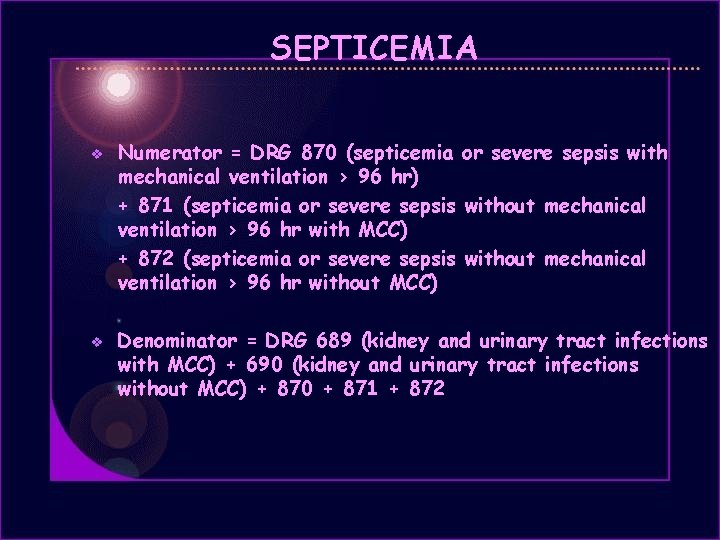
SEPTICEMIA v v Numerator = DRG 870 (septicemia or severe sepsis with mechanical ventilation > 96 hr) + 871 (septicemia or severe sepsis without mechanical ventilation > 96 hr with MCC) + 872 (septicemia or severe sepsis without mechanical ventilation > 96 hr without MCC) Denominator = DRG 689 (kidney and urinary tract infections with MCC) + 690 (kidney and urinary tract infections without MCC) + 870 + 871 + 872

Your Vital Roles Important to correctly and appropriately identify sepsis ü Research ü Accuracy ü Treatment ü Outcomes ü Core measures • BUT inappropriately querying for sepsis may incorrectly establish this diagnosis for the patient and lead to potentially deleterious results for your hospital •
Questions ? William C. Templeton, III, MD Chief Medical Officer Clark Memorial Hospital Jeffersonville, IN William. templeton@clarkmemorial. org
 Quick sofa
Quick sofa Thinking affects our language, which then affects our:
Thinking affects our language, which then affects our: Bobbin leading principle
Bobbin leading principle Surviving sepsis definition
Surviving sepsis definition Neonatal sepsis
Neonatal sepsis Sepsis bundle
Sepsis bundle Neonatal sepsis
Neonatal sepsis Bjarni geir viðarsson
Bjarni geir viðarsson Quick sofa
Quick sofa Stages of sepsis
Stages of sepsis Sepsis
Sepsis Gdp sepsis decision support tool
Gdp sepsis decision support tool Sepsis care near palo alto
Sepsis care near palo alto Sepsis pp respiratorio
Sepsis pp respiratorio Give 3 take 3 sepsis
Give 3 take 3 sepsis Nelson nec
Nelson nec Driver diagram template
Driver diagram template Prevention of puerperal sepsis
Prevention of puerperal sepsis Sofa score chart
Sofa score chart Puerperal sepsis definition
Puerperal sepsis definition Sepsis dietary management
Sepsis dietary management Guido marcangeli
Guido marcangeli Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Template
Template Hypotensis
Hypotensis Sepsis hour 1 bundle
Sepsis hour 1 bundle Sepsis
Sepsis What causes sepsis
What causes sepsis Sepsis
Sepsis Hemodynamics
Hemodynamics Maternal sepsis
Maternal sepsis Nanda hipertension
Nanda hipertension Riesgo de sepsis nanda
Riesgo de sepsis nanda Dental sepsis
Dental sepsis Sepsis definition
Sepsis definition Dr alex sepsis
Dr alex sepsis La hora dorada de la sepsis
La hora dorada de la sepsis Accefluid
Accefluid What affects basicity
What affects basicity Perception checking process
Perception checking process Factors affecting projectile trajectory
Factors affecting projectile trajectory Sumber:shutterstock.com
Sumber:shutterstock.com How does electrolytes affect the chemical equilibria?
How does electrolytes affect the chemical equilibria? A factor that affects tertiary activity
A factor that affects tertiary activity How technology affects managerial communication
How technology affects managerial communication How anxiety affects eyewitness testimony
How anxiety affects eyewitness testimony How perception affects communication
How perception affects communication How eating healthy affects your body
How eating healthy affects your body The noise that affects pcm
The noise that affects pcm Which of the following sets of maps would help explain
Which of the following sets of maps would help explain 8 elements of poetry
8 elements of poetry This affects us
This affects us What affects rate of weathering
What affects rate of weathering Culture is affects biology
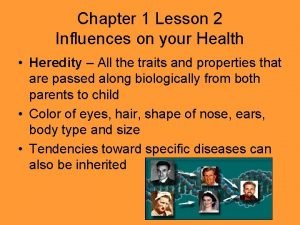
Culture is affects biology Chapter 1 lesson 2 what affects your health
Chapter 1 lesson 2 what affects your health Chapter 1 lesson 2 what affects your health
Chapter 1 lesson 2 what affects your health A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes A bacterial std that usually affects mucous membranes
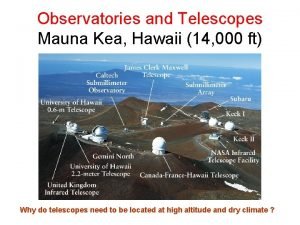
A bacterial std that usually affects mucous membranes Chromatic aberration affects reflector telescopes
Chromatic aberration affects reflector telescopes What emotion affects drivers the most
What emotion affects drivers the most Chapter 1 lesson 2 what affects your health
Chapter 1 lesson 2 what affects your health A teacher affects eternity meaning
A teacher affects eternity meaning Discuss how modifiers influence/affect human acts.
Discuss how modifiers influence/affect human acts. How culture affects decision making
How culture affects decision making This affects us
This affects us Waves means
Waves means Ux affects seo
Ux affects seo What affects rate of weathering
What affects rate of weathering What factor affects the speed of sound wave?
What factor affects the speed of sound wave?