EARLY DETECTION OF SEPSIS IN THE ED SEPSIS


- Slides: 35
EARLY DETECTION OF SEPSIS IN THE ED SEPSIS SYMPOSIUM OCTOBER 31 ST 2018 TARYN KENNEDY MD
DISCLOSURES • I have nothing to disclose. .
DEFINITIONS: • Is it sepsis, severe sepsis or septic shock? ? • What does “early” mean and why is it important? • Why the ED? • 18 million estimated new cases of sepsis world wide a year • In US 65. 5 per 100, 000 persons. • 10 -50% mortality. • Costs ~17 billion /year
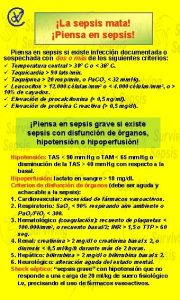
SEPSIS DEFINITIONS: A DISEASE CONTINUUM • Infection: invasion of a normally sterile tissue by an organism resulting in infectious pathology • SIRS: (Systemic inflammatory response syndrome), any > 2 of temp≥ 38. 3 or ≤ 36, HR > 90/min, RR >20/min, WCC ≥ 12, 000, ≤ 4, 000, or >10% bands. Present in many hospitalized patients i. e. pancreatitis, vasculitis, burns, post op. • Sepsis: ≥ 2 SIRS + new or worsening infection. Systemic response to local infection (1991 definition updated 2003 but not materially changed) • Severe sepsis: sepsis + new or acute onset organ failure • Septic shock: Severe sepsis + hypotension SBP<90, MAP<65, SBP<40 mm. Hg from baseline OR lactic acid ≥ 4 mmol. (intravascular depletion, peripheral vasodilation, myocardial depression increased metabolism with imbalance between delivery and demand) • And then came along the 3 rd international consensus on Sepsis….
2016 SCCM/ESICM • Defined sepsis as a life-threatening organ dysfunction caused by a dysregulated host response to infection (previously severe sepsis) • Clinical suspicion derived from signs and symptoms of infection with supporting radiography, microbiology data and response to therapy. • Organ failure: Pa. O 2/Fi. O 2 ratio, platelets <100, 000, BR >1. 5, Creat. >2, GCS < 12, INR >1. 5 a. PPT >60 sec, hypotension/vasopressor requirement • Septic shock is vasodilatory or distributive shock. Circulatory, cellular and metabolic abnormalities that are associated with greater risk of mortality.
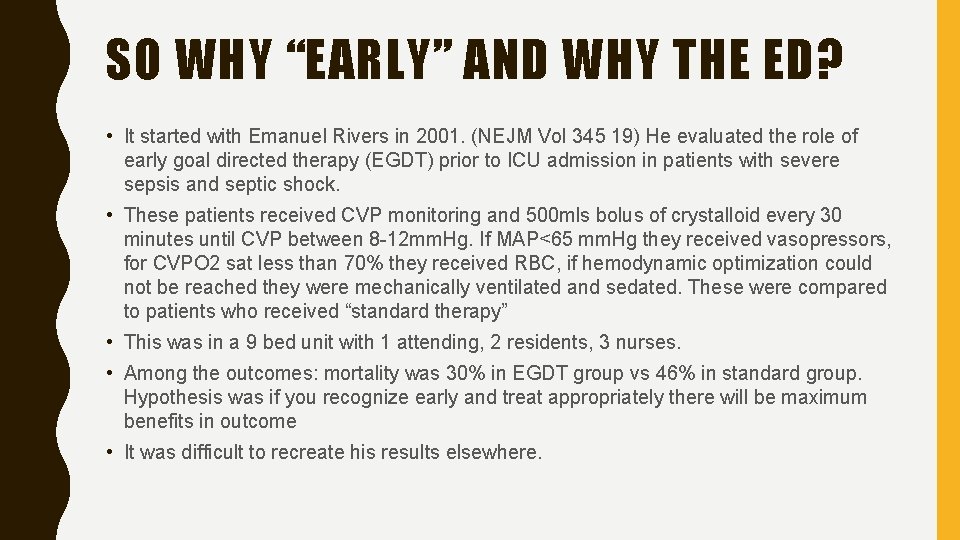
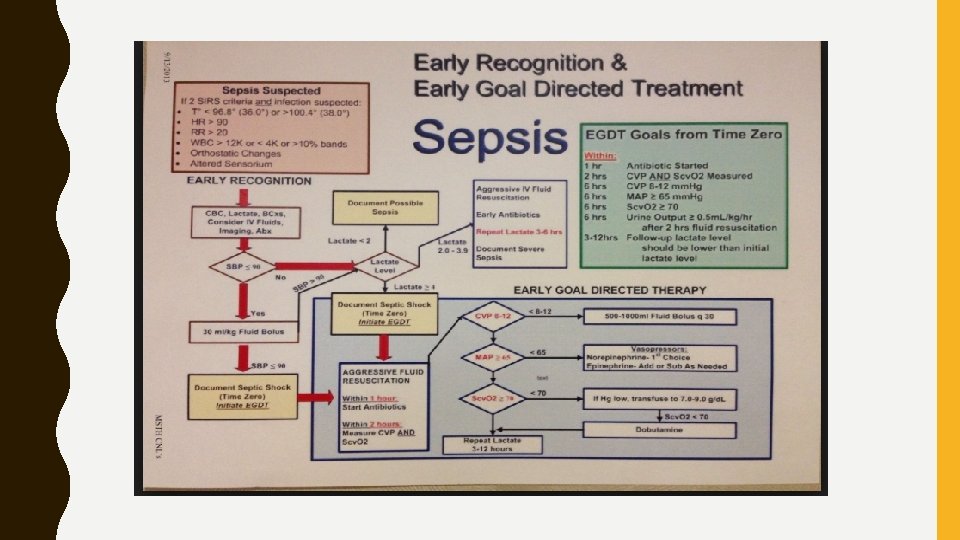
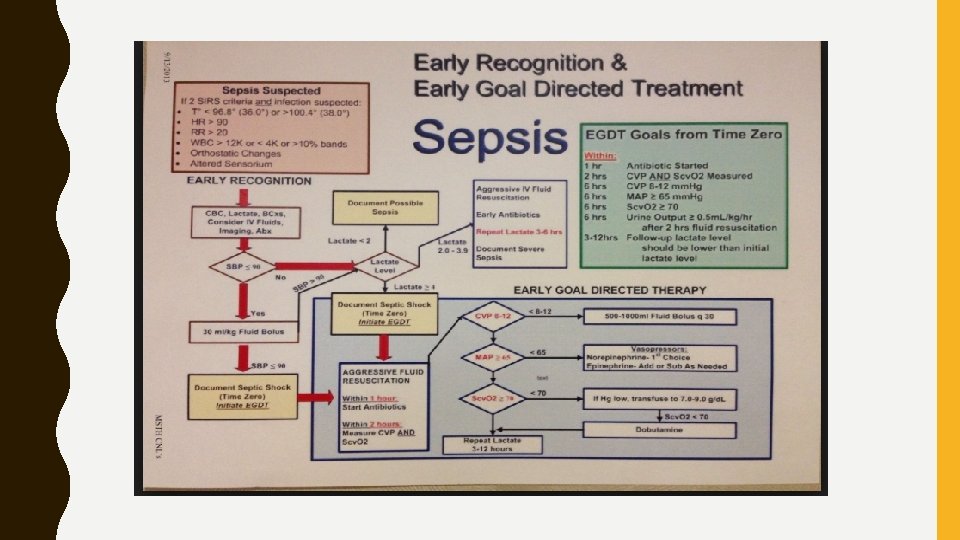
SO WHY “EARLY” AND WHY THE ED? • It started with Emanuel Rivers in 2001. (NEJM Vol 345 19) He evaluated the role of early goal directed therapy (EGDT) prior to ICU admission in patients with severe sepsis and septic shock. • These patients received CVP monitoring and 500 mls bolus of crystalloid every 30 minutes until CVP between 8 -12 mm. Hg. If MAP<65 mm. Hg they received vasopressors, for CVPO 2 sat less than 70% they received RBC, if hemodynamic optimization could not be reached they were mechanically ventilated and sedated. These were compared to patients who received “standard therapy” • This was in a 9 bed unit with 1 attending, 2 residents, 3 nurses. • Among the outcomes: mortality was 30% in EGDT group vs 46% in standard group. Hypothesis was if you recognize early and treat appropriately there will be maximum benefits in outcome • It was difficult to recreate his results elsewhere.
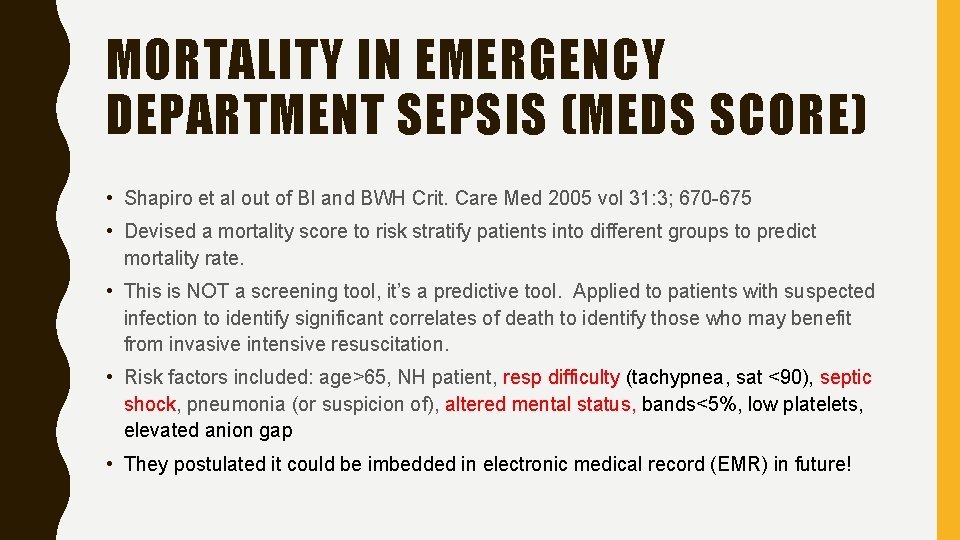
MORTALITY IN EMERGENCY DEPARTMENT SEPSIS (MEDS SCORE) • Shapiro et al out of BI and BWH Crit. Care Med 2005 vol 31: 3; 670 -675 • Devised a mortality score to risk stratify patients into different groups to predict mortality rate. • This is NOT a screening tool, it’s a predictive tool. Applied to patients with suspected infection to identify significant correlates of death to identify those who may benefit from invasive intensive resuscitation. • Risk factors included: age>65, NH patient, resp difficulty (tachypnea, sat <90), septic shock, pneumonia (or suspicion of), altered mental status, bands<5%, low platelets, elevated anion gap • They postulated it could be imbedded in electronic medical record (EMR) in future!
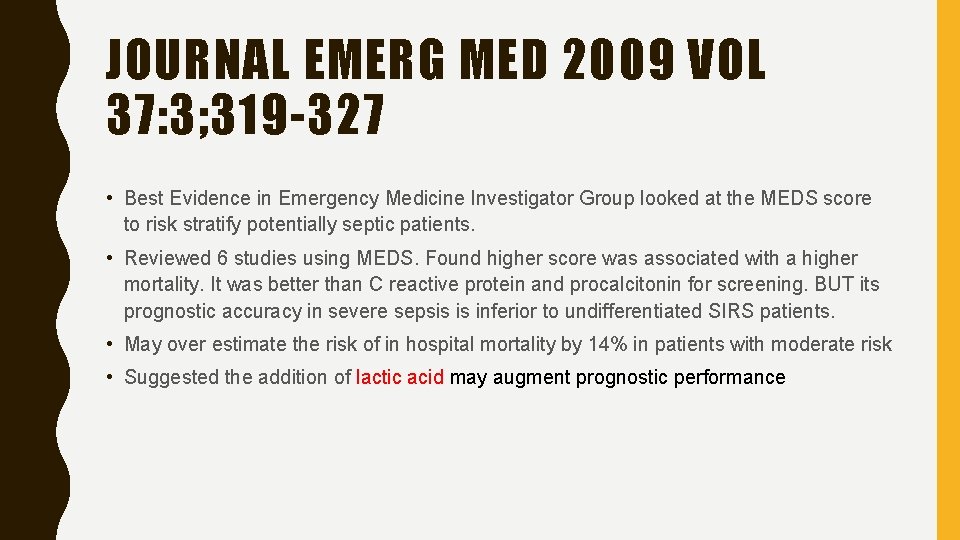
JOURNAL EMERG MED 2009 VOL 37: 3; 319 -327 • Best Evidence in Emergency Medicine Investigator Group looked at the MEDS score to risk stratify potentially septic patients. • Reviewed 6 studies using MEDS. Found higher score was associated with a higher mortality. It was better than C reactive protein and procalcitonin for screening. BUT its prognostic accuracy in severe sepsis is inferior to undifferentiated SIRS patients. • May over estimate the risk of in hospital mortality by 14% in patients with moderate risk • Suggested the addition of lactic acid may augment prognostic performance
CAN WE IDENTIFY SEPTIC SHOCK BY ECHO? • Jones and Kline in Carolinas Medical Center Shock 2005 vol 24; : 6: 513 -517 • Patients in the ED with hypotension, hyperdynamic LV function (EF>55%) was specific for sepsis as a cause of shock. 33% sensitive 94% specific • The study population was patients with undifferentiated hypotension AFTER H&P and labs • Was more specific than temp/WCC • All patients were suspected as having infection • Trying to identify septic shock patients early, recognizing their high mortality rate with a view to administration of early antibiotics and goal directed therapy.
BARRIERS TO IMPLEMENTATION OF PROTOCOL BASED SEPSIS RESUSCITATION IN ED • Crit. Care Med 2007 Vol 35; 11 2525 -2532 Carlboni, Rubenfeld et al • Identified challenges included : lack of available nursing staff • Inability to monitor CVP in ED • Challenge of identifying septic patients in ED
SO HOW DO WE FIND THESE PATIENTS…… • We need a screening tool…… • We need to be able to differentiate infection vs sepsis vs severe sepsis vs septic shock as mortality rate can be significantly different in each group • We need to know what interventions make a difference in that mortality rate. If we could risk stratify the patients could we get them the level of care they need in a timely fashion and would it make a difference?
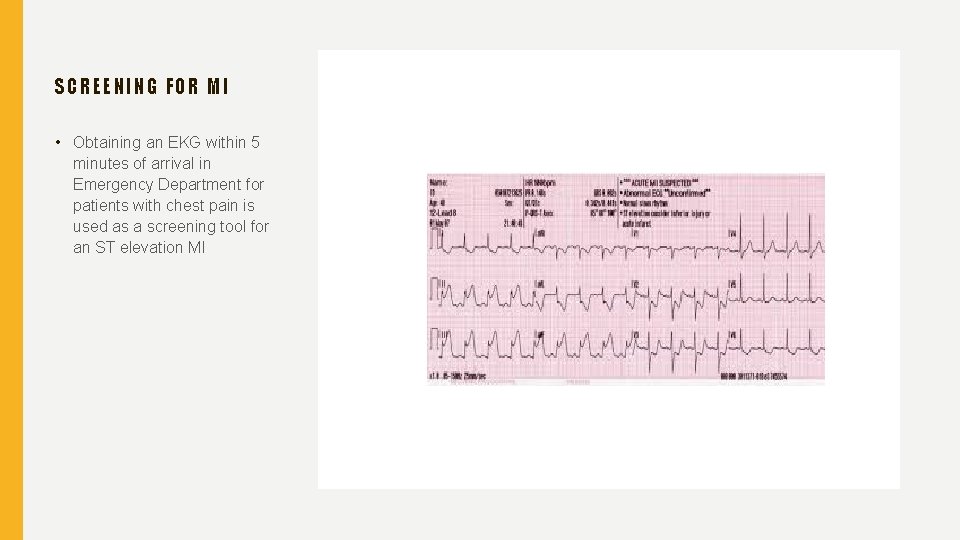
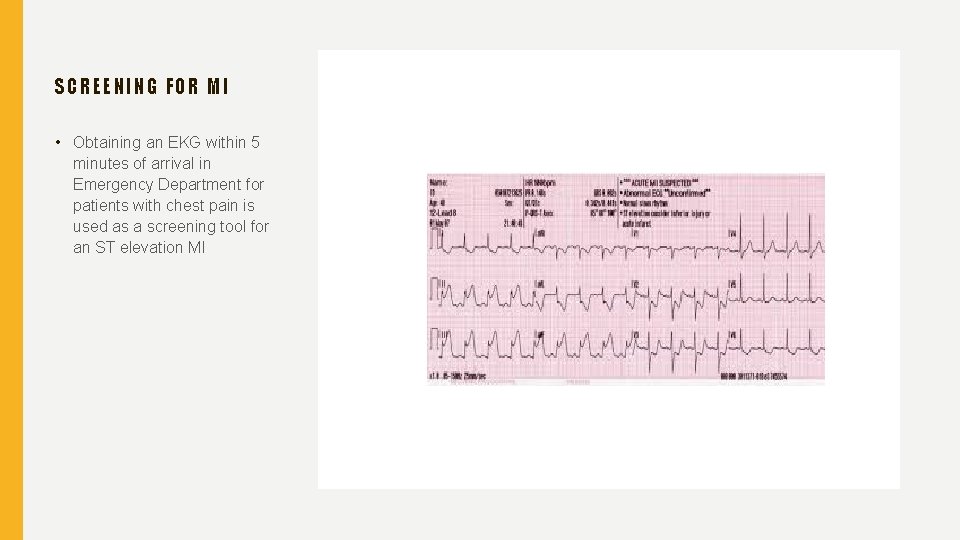
SCREENIN G FOR MI • Obtaining an EKG within 5 minutes of arrival in Emergency Department for patients with chest pain is used as a screening tool for an ST elevation MI

SCREENING FOR STROKE… • Looking for facial droop • Weakness one side of body • Abnormal speech
RISK FACTORS FOR SEPSIS • ICU admission • Bacteremia • >65 years old • Immunosuppression • Diabetes/obesity • Cancer • Previous hospitalization • Genetic factors
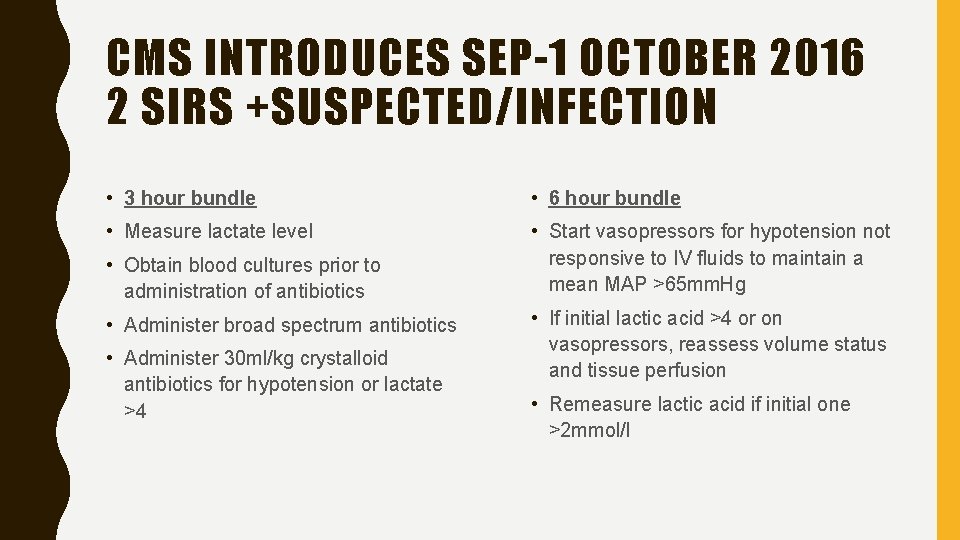
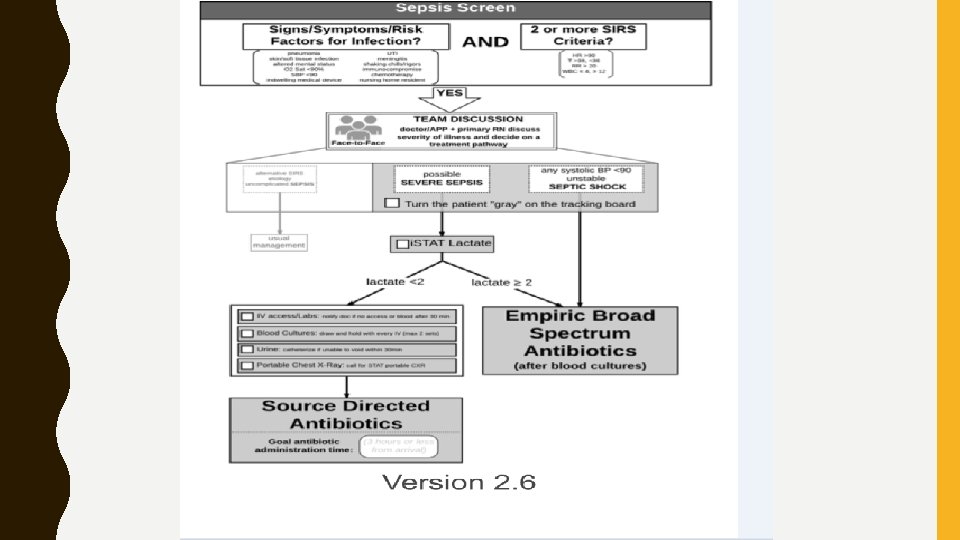
CMS INTRODUCES SEP-1 OCTOBER 2016 2 SIRS +SUSPECTED/INFECTION • 3 hour bundle • 6 hour bundle • Measure lactate level • Start vasopressors for hypotension not responsive to IV fluids to maintain a mean MAP >65 mm. Hg • Obtain blood cultures prior to administration of antibiotics • Administer broad spectrum antibiotics • Administer 30 ml/kg crystalloid antibiotics for hypotension or lactate >4 • If initial lactic acid >4 or on vasopressors, reassess volume status and tissue perfusion • Remeasure lactic acid if initial one >2 mmol/l
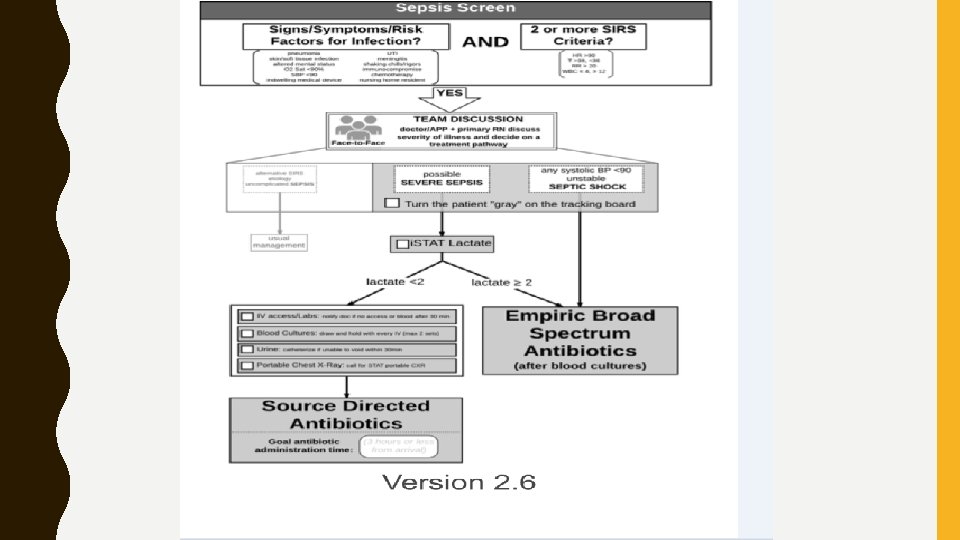
PURPOSE: TO HELP MEET THE CHALLENGE OF SEPSIS AND IMPROVE THE MANAGEMENT, DIAGNOSIS AND TREATMENT OF EVIDENCE BASED EARLY SEPSIS RECOGNITION USE OF AN ALGORITHM FOR EARLY DETECTION AND TREATMENT TO FACILITATE CONSISTENT IMPLEMENTATION ADEQUATE OXYGEN DELIVERY AND RESP SUPPORT, IV FLUID RESUSCITATION, MEDICATIONS TO SUPPORT CARDIAC OUTPUT AGGRESSIVELY AND EARLY ANTIBIOTIC ADMINISTRATION IMPLEMENTED IN AN EXPEDITIOUS MANNER.
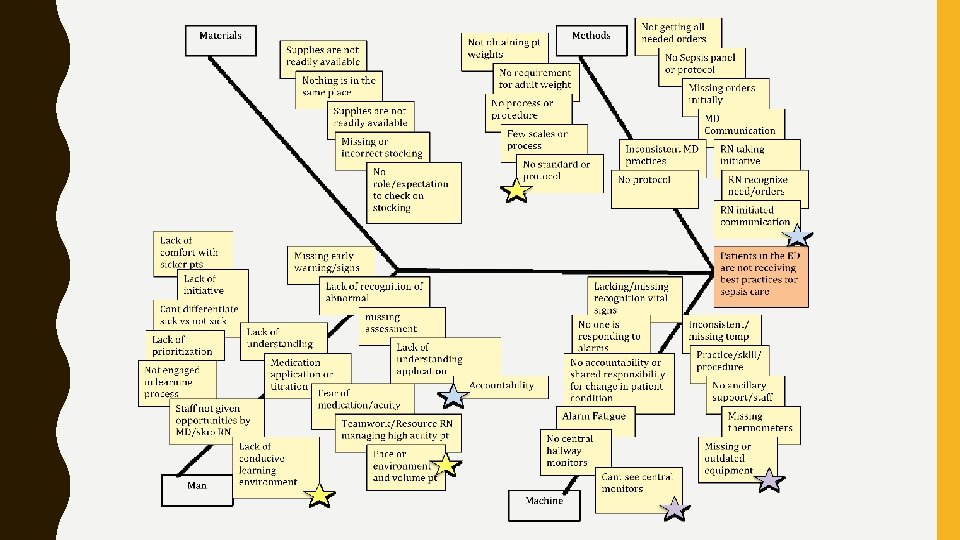
SOUNDS EASY, NOT SO MUCH IN PRACTICE…… • Still don’t have an easy screening tool for this patient population (procalcitonin? ? ) • Need a constellation of data to make the diagnosis. May be made empirically, retrospectively or in response to antibiotics • Need to educate all ED providers on sepsis and bundles • When does the time line start, how do you know where you are on the timeline? • People not used to ordering lactic acids in this population • Timing in chart/EHR may not reflect reality • Need a prompt to reorder the lactic acid, cannot “reflex” it as no sample in lab • Compliance varies and does compliance decrease mortality? ?

IT TAKES A TEAM AND THE TEAM STARTS WITH THE TRIAGE NURSE…. .
SCREENING ALL PATIENTS AT TRIAGE • With what? • Signs and symptoms suggestive of infection i. e. cough and dyspnea • 2+ SIRS criteria sensitive but not specific • q. SOFA: a modified version of Sequential (sepsis related)Organ Failure Assessment score. Identifies those potentially at risk of dying from sepsis. Not a screening tool – Score ≥ 2 assoc. poor outcomes – RR > 22 – Systolic BP <100 mm. Hg – Altered mentation
QSOFA • Weingart and Singer Annals of Emergency Medicine 2017 69: 475 -479 • q. SOFA ≥ predicts mortality in adult ED patients with and without infection. It is associated with inpatient mortality, admission, ICU admission, and hospital LOS • Its predictive validity is greater than SO or SIRS for inpatient mortality in patients outside the ICU
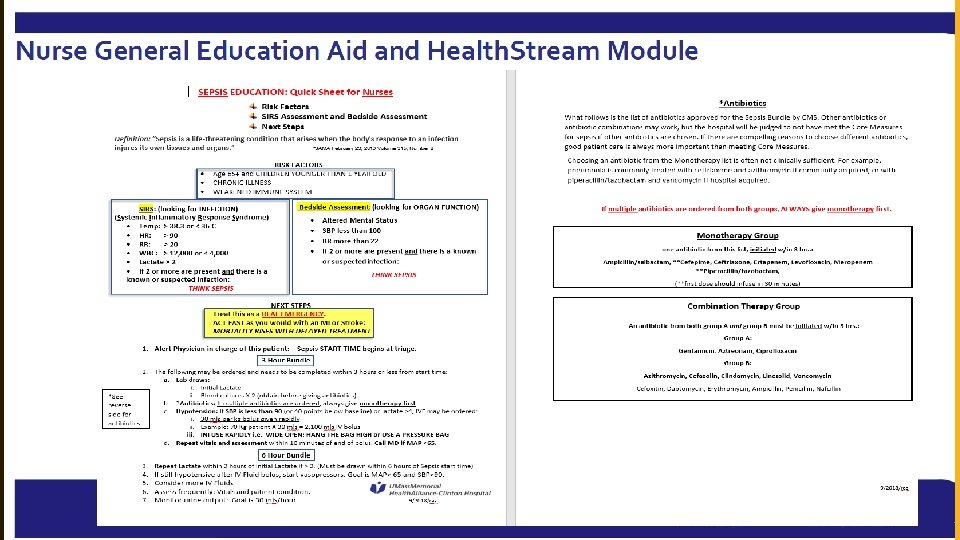
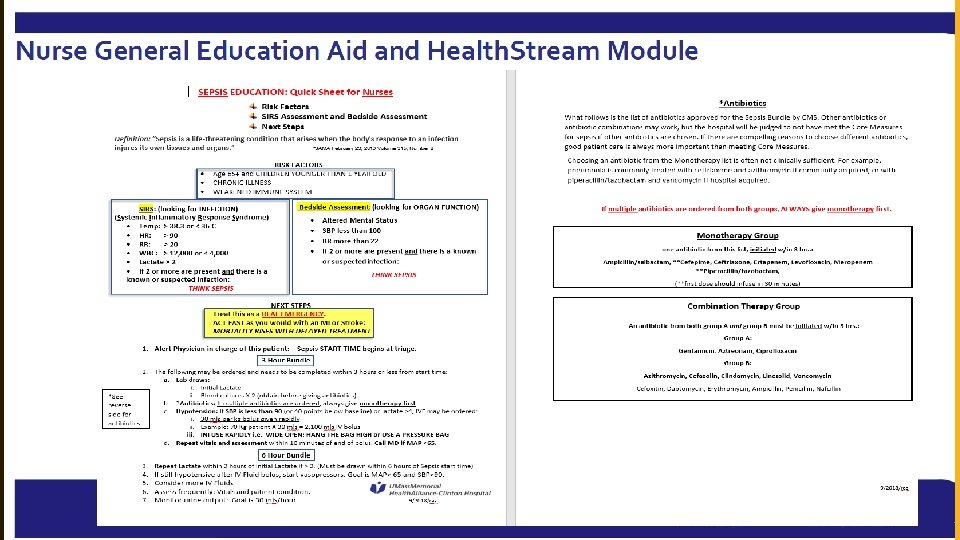
SON CHAE KIM ET AL • Journal of Emergency Nursing 2015 41: 2; 130 -137 • Impact of nurse initiated ED sepsis protocol on compliance with sepsis bundles, time to initial antibiotic administration and in patient mortality. • Retrospective chart review of severe sepsis/septic shock patients before and after implementation of the protocol. • Compliance with serum lactic acid and blood cultures 100% post implementation • Compliance with medical interventions requiring multiple health caregivers suboptimal. 25% did not get antibiotics in a timely fashion, 1/5 th didn’t get appropriate fluids. • Poor interdisciplinary collaboration and poor sepsis knowledge identified as barriers
GREGG A HALL ET AL UNIVERSITY SOUTH CAROLINA • American Journal of Emergency Medicine 2016 vol 34 1 -9 T • Triage Sepsis Alert and Sepsis protocol lowers times to fluids and antibiotics in ED. • Protocol emphasizing rapid mobilization of resources, standard order sets, early broad spectrum antibiotics and fluid resuscitation • Use of BPA in EHR in triage • Did decrease the time to antibiotics and IV fluids
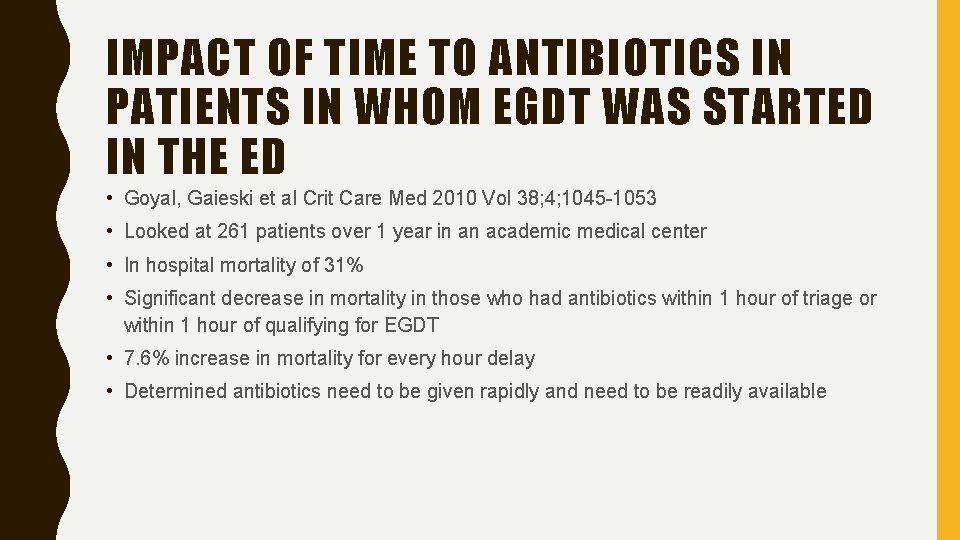
IMPACT OF TIME TO ANTIBIOTICS IN PATIENTS IN WHOM EGDT WAS STARTED IN THE ED • Goyal, Gaieski et al Crit Care Med 2010 Vol 38; 4; 1045 -1053 • Looked at 261 patients over 1 year in an academic medical center • In hospital mortality of 31% • Significant decrease in mortality in those who had antibiotics within 1 hour of triage or within 1 hour of qualifying for EGDT • 7. 6% increase in mortality for every hour delay • Determined antibiotics need to be given rapidly and need to be readily available
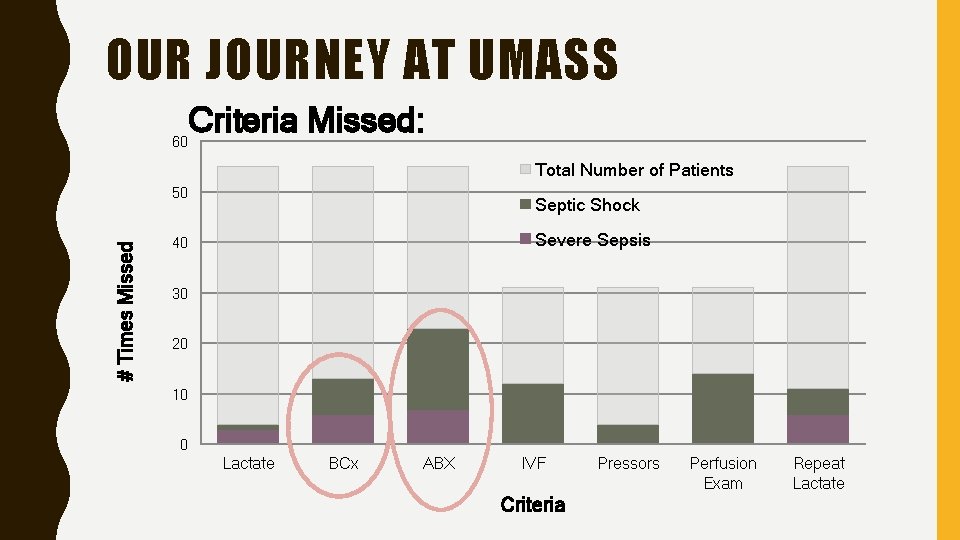
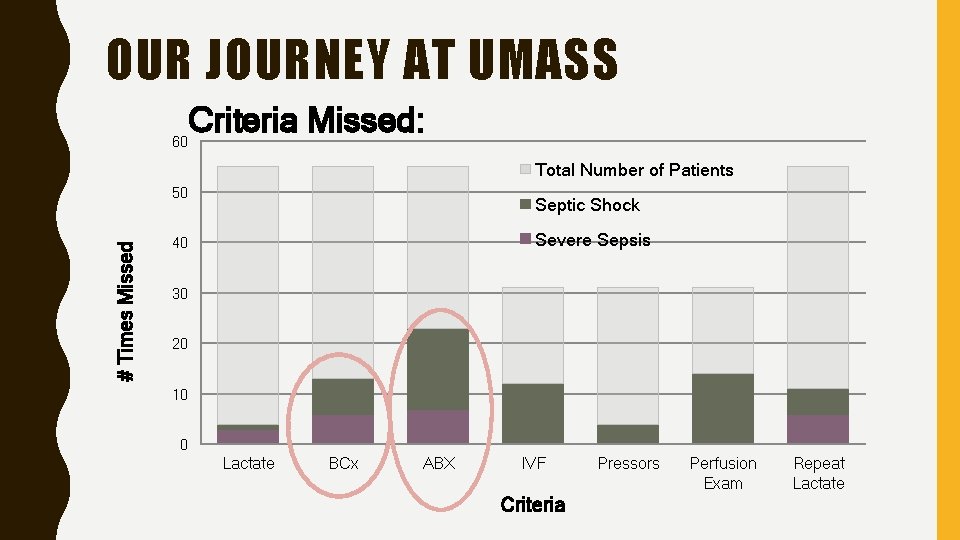
OUR JOURNEY AT UMASS Criteria Missed: 60 Total Number of Patients # Times Missed 50 Septic Shock Severe Sepsis 40 30 20 10 0 Lactate BCx ABX IVF Criteria Pressors Perfusion Exam Repeat Lactate
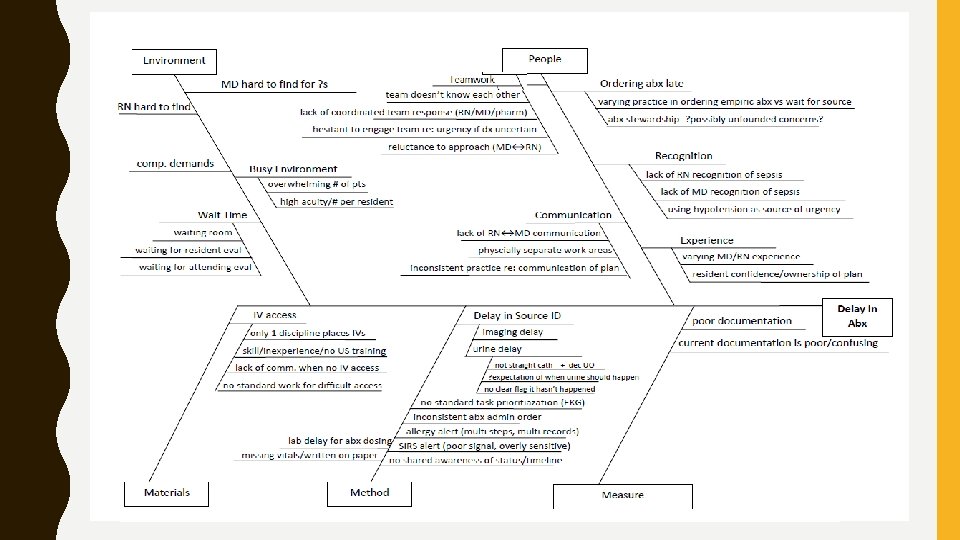
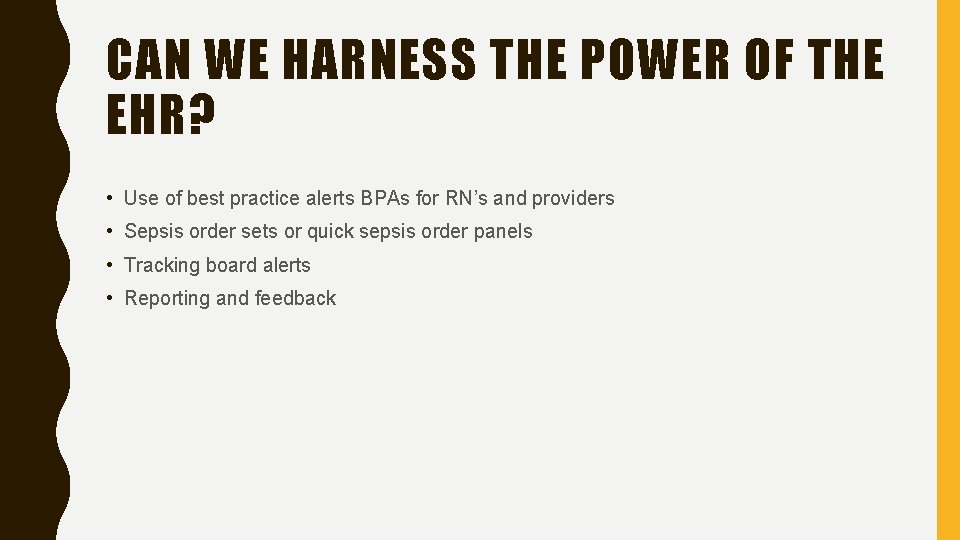
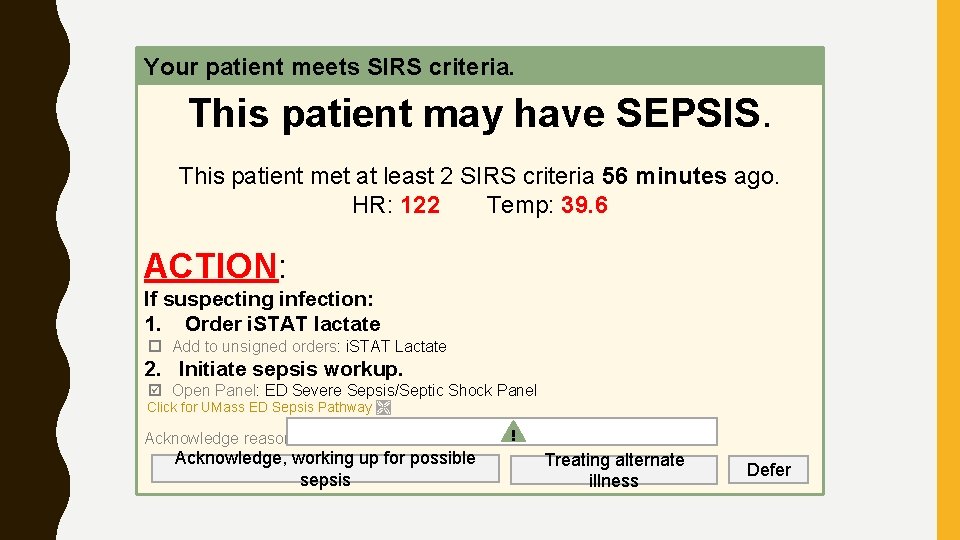
CAN WE HARNESS THE POWER OF THE EHR? • Use of best practice alerts BPAs for RN’s and providers • Sepsis order sets or quick sepsis order panels • Tracking board alerts • Reporting and feedback
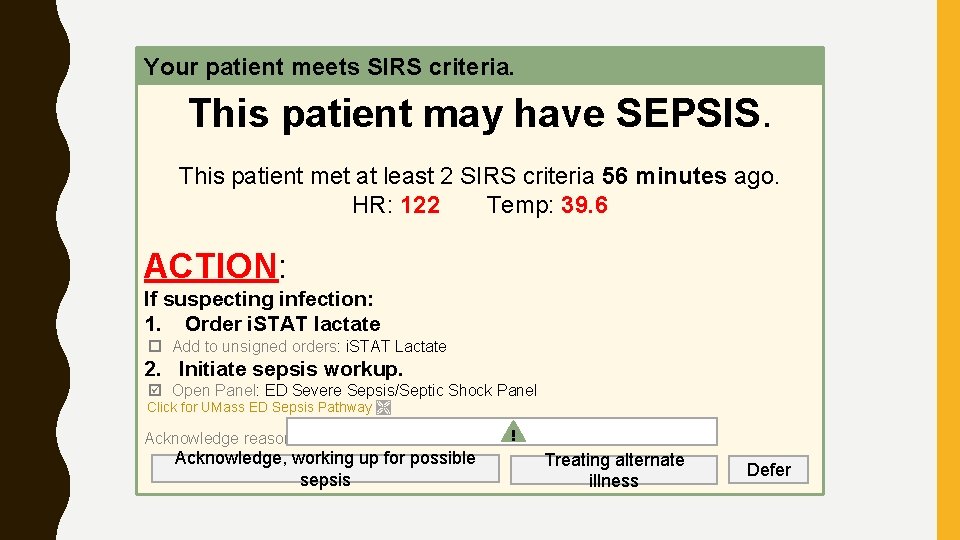
Your patient meets SIRS criteria. This patient may have SEPSIS. This patient met at least 2 SIRS criteria 56 minutes ago. HR: 122 Temp: 39. 6 ACTION: If suspecting infection: 1. Order i. STAT lactate Add to unsigned orders: i. STAT Lactate 2. Initiate sepsis workup. Open Panel: ED Severe Sepsis/Septic Shock Panel Click for UMass ED Sepsis Pathway Acknowledge reason: Acknowledge, working up for possible sepsis ! Treating alternate illness Defer
SUMMARY • There is currently no simple screening tool • Need to have heightened awareness and suspicion • Use of protocols improves adherence to bundles • Time to appropriate antibiotics is important • A team approach is vital • We need to work with the EHR to make life easier, give real time reports that are actionable • Our care of our patients with sepsis will continue to evolve, research and education is very important
SURVIVING SEPSIS CAMPAIGN RESOURCES
CDC CLINICAL RESOURCES
 Q sofa
Q sofa National breast and cervical cancer early detection program
National breast and cervical cancer early detection program Early kick detection
Early kick detection National breast and cervical cancer early detection program
National breast and cervical cancer early detection program Early cpr and early defibrillation can: *
Early cpr and early defibrillation can: * Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Surviving sepsis definition
Surviving sepsis definition Sepsis bundle
Sepsis bundle Skingar
Skingar Quick sofa
Quick sofa Sepsis
Sepsis Stages of sepsis
Stages of sepsis Criterios de gibbs
Criterios de gibbs Hod vasundhara
Hod vasundhara Maternal sepsis
Maternal sepsis Sepsis pp respiratorio
Sepsis pp respiratorio Give 3 take 3 sepsis
Give 3 take 3 sepsis Sepsis neonatal temprana y tardía
Sepsis neonatal temprana y tardía Driver diagram example
Driver diagram example Puerperal sepsis definition
Puerperal sepsis definition Hora dorada en medicina
Hora dorada en medicina Sepsis dietary management
Sepsis dietary management Indication for exploratory laparotomy
Indication for exploratory laparotomy Template
Template Sepsis
Sepsis Neonatal sepsis
Neonatal sepsis Qsofa
Qsofa Sepsis hour 1 bundle
Sepsis hour 1 bundle Gdp sepsis decision support tool
Gdp sepsis decision support tool Sepsis
Sepsis Sepsis care near palo alto
Sepsis care near palo alto Hemodynamics
Hemodynamics Hoja de balance hidrico en enfermeria
Hoja de balance hidrico en enfermeria Emanms
Emanms Sepsis
Sepsis Prevention of puerperal sepsis
Prevention of puerperal sepsis