PLANNING ORGANISATION OF RCH SERVICES FOR 1 LAKH











- Slides: 59

PLANNING &ORGANISATION OF RCH SERVICES FOR 1 LAKH POPULATION IN A RURAL AREA Dr. I. Selvaraj
I am very grateful to The Super course, as my view is disseminated to global audience through my Power point presentations in different topics. I hope you might have enjoyed. This power point presentation is prepared based on RCH PHASE-II Programme. Those who have gone through my earlier presentations on RCH-PHASE-I , RCH-PHASE-II &Modified RCHPHASE-II will be benefited. My aim of this presentation is to help the developing countries to strengthen their activities in their areas so that our ultimate goal of population stabilization will be achieved. My vision is always to disseminate the knowledge of community medicine to all my public health colleagues without any monetary gain. I hope you will all enjoy & gain a lot. Please send me the feedback. Thanking you Dr. I. selvaraj, I. R. M. S B. Sc. , M. B. B. S. , D. I. H. , PGCH&FW(NIHFW) (M. D Community Medicine, Sree Ramachandra Medical college &RI) D. P. H. , (MADRAS MEDICAL COLLEGE, Recognized by MCI) Senior Divisional Medical officer (Selection Grade Officer) On Study Leave INDIAN RAILWAYS
Reproductive health can be defined as a state in which people have the ability to reproduce and regulate their fertility, women are able to go through pregnancy and child birth safely, the outcome of pregnancy is successful in terms of maternal and infant survival and well being, and couples are able to have sexual relations free of the fear of pregnancy and of contracting diseases.
• Right of the men & women to be informed • To have access to safe, effective, affordable, & acceptable methods of fertility regulation of their choice • Right of access to appropriate health care services • To enable women to go safely through pregnancy and childbirth • To provide couples with best chance of having a healthy infant
The first phase of the programme was started on 1997 with an aim to bring down the birth rate below 21 per 1000 population, to reduce the infant mortality rate below 60 per 1000 live birth and to bring down the maternal mortality rate <400/1, 000 lakh. 80% institutional delivery, 100% antenatal care and 100% immunization of children were other targeted aims of the RCH programme.

The 5 year RCH phase II is launched in Tamil. Nadu on 2005 with a vision to bring about outcomes as envisioned in the Millennium Development Goals, the National Population Policy 2000 (NPP 2000), the Tenth Plan, the National Health Policy 2002 and Vision 2020 India, minimizing the regional variations in the areas of RCH and population stabilization through an integrated, focused, participatory programme meeting the unmet needs of the target population, and provision of assured, equitable, responsive quality services.
VISION To bring about outcomes as envisioned in the 1. Millennium Development Goals 2. The National Population Policy 2000 Goals 3. The Tenth Plan Goals 4. The National Health Policy 2002 5. and Vision 2020 India
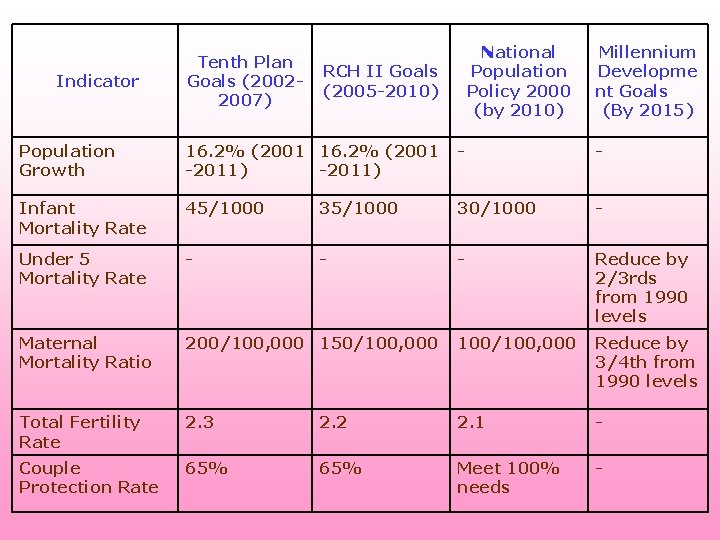
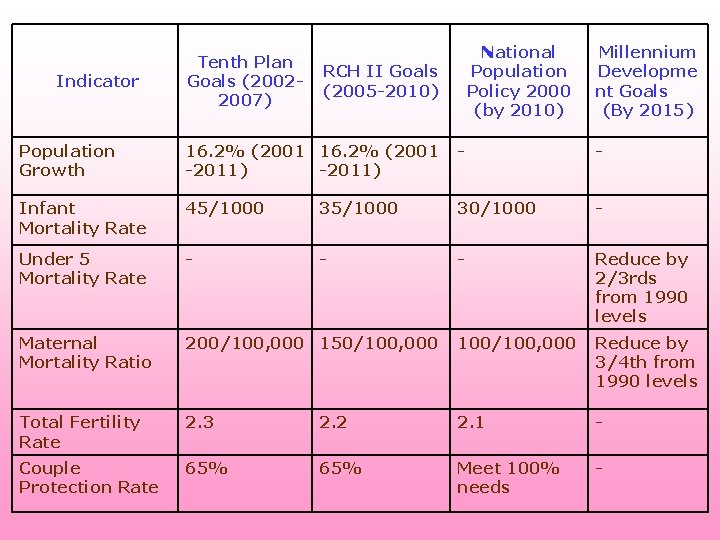
Indicator Tenth Plan Goals (20022007) National Population Policy 2000 (by 2010) RCH II Goals (2005 -2010) Millennium Developme nt Goals (By 2015) Population Growth 16. 2% (2001 -2011) - - Infant Mortality Rate 45/1000 30/1000 - Under 5 Mortality Rate - - - Reduce by 2/3 rds from 1990 levels Maternal Mortality Ratio 200/100, 000 150/100, 000 100/100, 000 Reduce by 3/4 th from 1990 levels Total Fertility Rate 2. 3 2. 2 2. 1 - Couple Protection Rate 65% Meet 100% needs -
• Immediate objective: 1. To Improve routine immunization coverage 2. To reduce the unmet need for contraception • Medium term objective: To bring the Total fertility Rate to replacement level by 2010 • The long term objective: Population stabilization by 2045
Target: • Total fertility rate to the replacement level by 2010 • To achieve the indicators of Health for All, Millenium. Development. Goal, National. Healthpolicy 2002, &10 th Five year plan Goal Program: Comprehensive R. C. H services Plan : High quality, integrated, decentralized, Need based and holistic approach, CNAMA Monitoring & Evaluation: R. C. H indicators/Feedback data
Strategy 1. Reduction of Maternal Morbidity And Mortality 2. 3. 2. Reduction of Infant Morbidity And Mortality 4. 3. Reduction of Under 5 Morbidity And Mortality 5. 4. Promotion of Adolescent Health 6. 5. Control of Reproductive Tract Infections and Sexually Transmitted Infections.

Programme strategy • • • Decentralized participatory planning CNAMA Good quality care Upgraded facilities Improved training Target free approach Absence of incentives Making services gender sensitive Male participation in family planning Involvement of Panchayat raj Multi sectoral approach Client satisfiaction
CNAA APPROACH • It refers to need assessment and planning for services with the involvement of community. • It is based on the felt need of the community and relevant to the community. • Enable the clients to meet their Goals • Client centered, Demand driven, Bottom-up, Decentralized • Full range of integrated high quality RCH services • Participatory planning • Target free approach • performance monitoring by Quality of care, Client satisfaction, coverage measures • Accountable to the client, community

There about 50 comprehensive R. C. H services to be effectively carried out for the entire population: • M. C. H Services • Nutritional Services • Management of childhood diseases • Referral Services • Fertility Services • Population control and sexuality educational Services • R. T. I / S. T. I Control Services • Health education regarding gender issues • Formal and Non-formal education about public health • Forty Plus Care etc. ,

RCH PACKAGE OF SERVICES
For Mothers 1. All pregnancies to be registered by health workers. 2. Pregnant women must be given two doses of tetanus toxoid immunizations. 3. Pregnant women must be given iron folic acid tablets for prevention and treatment of anemia. 4. Pregnant women must be given three antenatal checkups, which include checking their blood pressure and ruling out complications. 5. Deliveries by trained personnel in safe and hygienic surroundings should be encouraged. 6. Institutional deliveries should be encouraged for women having complications. 7. Referrals should be made to first referral units for management of obstetric emergencies. 8. Three postnatal checkups should be given to mothers after the delivery. 9. Spacing of at least three years between children must be encouraged
For New born & Children 1. Essential newborn care like keeping the baby warm, checking the baby's weight and giving the baby mother's first milk is important. The premature babies or low birth weight babies need special care. Babies with any complications should be refereed to the nearest health center. 2. Exclusive breast-feeding must be encouraged for the first three months. Weaning or starting the baby on semisolid food should start in the fourth month. 3. BCG, DPT, Polio and Measles immunizations should be administered to every child meticulously to prevent death and disabilities. 4. Vitamin A prophylactic for children is necessary to prevent blindness. 5. Parents must be informed about oral rehydration therapy and correct management of diarrhea. The availability of ORS packets in the villages should be ensured. 6. Acute respiratory infection in children should be detected early. They can be treated by cotrimoxazole tablets. Acute cases should be refereed to health center. 7. Treatment of Anemia.
ELIGIBLE COUPLES 1. Promoting use of contraceptive methods among eligible couples is important to prevent unwanted pregnancies. Couples should be able to choose from various contraceptive methods including condoms, Oral pills, IUDs, male and female sterilization. 2. Safe services for medical termination of pregnancies should be encouraged for women desiring abortions.
OTHER NEW SERVICES 1. A large number of people suffer in silence due to reproductive tract infections (RTIs) and sexually transmitted diseases (STDs). RTIs and STDs can make people infertile. If a pregnant woman has RTIs or STDs, it can affect the health of her child. People suffering from such infections should be referred to the health center. 2. Adolescents are parents of tomorrow. It is important to prepare them for the future by counseling them on family life and reproductive health. This can be a sensitive topic, as it has not been addressed before. Therefore, the involvement of parents, Anganwadi workers, and Mahila Swasthya Sanghs should be ensured
NEW STRATEGY OF RCH PHASE 1. To constitute empowered action group 2. Training of dais 3. To conduct RCH camps & organize RCH out reach scheme 4. Training of MBBS doctors in Life saving anesthetic skills for emergency obstetric care at FRUs. 5. Strengthening of core strategy of the existing PHCs and CHCs, and provision of 30 -50 bedded CHC (community health centre) per lakh population for improved curative care to a normative standard (Indian Public Health Standards defining personnel, equipment and management standards) 6. All Community health centers & 50% of the Primary health centers are to be made functional for providing 24 Hrs. delivery services 7. Primary Health Centers are proposed to be taken up for improving access to Essential Obstetric and New Born Care services round the clock. Cont……
8. Improving quality of antenatal, neonatal and postnatal care by providing increased number of antenatal checkups, fixed day antenatal clinics, linking visits of neonates with postnatal care, empowering the VHNs in performing obstetric first aid and newborn care. 9. Improvement of the referral networking systems by establishing emergency helpline 10. Regular conduct of blood donation camps for the continued availability of blood in the blood banks. 11. Universalizing the concept of birth companionship during the process of labor in all health facilities conducting deliveries. 12. Operationalisation of maternal death audit to address the issues that have led to maternal deaths
• Janani Suraksha Yojna (National Maternity Benefit Scheme) is envisaged as a package of services, geared at reducing maternal mortality, neonatal mortality, and female feticide and gender disparity. • “Vandematram” scheme -launched on 9 th Feb. 2004 in all the districts of the country with the active collaboration of the professional bodies. The aim of the scheme is to reduce the maternal mortality and morbidity of the pregnant and expectant mothers by involving and utilizing the vast resources of specialists/trained workforce available in the private sector. • A new initiative in National Rural Health Mission (20052012) is accountability. Every village/large habitat will have a female Accredited Social Health Activist (ASHA), accountable to the Panchayat. She will act as the interface between the community and the public healthcare system.
INFANT AND CHILD HEALTH 1. Reduction of Neo-natal deaths, infant deaths and child deaths by providing continuous health care and strengthening of newborn care infrastructure facilities. 2. Organizing counseling sessions for the mothers. 3. Implementing integrated management of neonatal and childhood illness 4. Operational sing infant death/stillbirth verbal autopsy. 5. Addressing the issue of female infanticide and foeticide 6 Gadchiroli model to take care of home based neonatal care 7. Kangaroo mother care to take care of low birth weight infants
FAMILY WELFARE 1. Higher order births will be targeted for intensified intervention 2. Social marketing programme has to be developed for condom and other health commodities, promotion of IUD insertions, familiarizing the concept of one-stop Family Welfare Centre. 3. Increasing access to safe abortion services by popularizing manual vacuum aspiration (MVA) technique. 4. Establishment of one-stop family welfare services at Comprehensive Emergency Obstetric and New Born Care (CEMONC) Centres. 5. Popularizing No Scalpel Vasectomy. 6. Availability of a wide range of contraceptive methods MCH and other services
7. Availability of a wide range of contraceptive methods MCH and other services 8. Accessibility, complete and accurate information about contraceptive methods, including their health risks and benefits 9. Safe and affordable services, along with high quality supplies 10. Well-trained service providers with skills in inter-personal communication and counseling 11. Appropriate follow-up care 12. Regular monitoring and evaluation of performance 13. A paradigm shift from individualized vertical interventions to a more holistic and integrated life cycle approach giving more focused attention to the reproductive health care.
OTHER INNOVATIVE REFORMS: 1. Improved drug procurement & supply systems to tackle the problem of inadequate and irregular supplies 2. Improved supply of cross-matched blood in first referral units thereby decreasing the inter-institutional transfers for transfusion 3. Regular conduct of blood donation camps for the continued availability of blood in the blood banks. 4. Systematic reporting and auditing of maternal & infant deaths 5. For monitoring purposes, standardized systematic reporting of services rendered at primary care level, using simple, manually completed, computer readable forms 6. Ensuring block and district level inter-sectoral coordination for ICDS 7. Improvement of the referral networking systems by establishing emergency help line 8. Each community health center should have one additional post of public health manager and public health nurse
Strengthening of IEC activities. These activities should cover the following messages: • Ideal age at marriage, Ideal age to produce a child, small family norm, Avoidance of higher order births, spacing, contraceptive acceptance, importance of female literacy, anemia control, monitoring the weight gain of mothers and growth monitoring of babies, breast feeding and importance of colostrums, diarrhea management, oral rehydration therapy, eradication of female infanticide and foeticide, upholding the image of girl child and women, safe delivery, institutional delivery, immunizations and nutrition. Propagation of messages through films, video spots, dramas, street plays and booklets have to be undertaken. Electronic media such as T. V. and radio have to be utilized. Audio-visual aids will be provided in medical institutions and publication of booklet on IEC activities.

Quality care Factors determining good quality care • Service delivery • Promoting informed choice • Need based service delivery • Providing follow up care • Interpersonal communication • Friendly and cooperative attitude of health worker Spending time with clients Caring of clients privacy and dignity • Social aspects • Gender sensitive service provision • Male participation • Increase Women role in the programme
ADOLESCENT HEALTH. a) Focusing adolescents as receivers and providers of knowledge and function as link volunteers in the community. b) Utilising the services of trained adolescents for propagating Indian System of Medicines. c) Broadcasting and Telecasting of programme by AIR/TV focusing adolescent, gender and health related subjects. d) Formation of co-ordination committee at the district level and monitoring committee at the State level for overseeing the AIR/TV programme.
Reproductive tract infections / Sexually transmitted infections / Cancer control. a) Establishment of Reproductive Tract Infection / Sexually Transmitted Infection, early Cancer detection clinics. b) Strengthening RCH outreach services. c) RTI/STD clinic in selected primary health centers
Infrastructure strengthening for service delivery a) Construction of HSC buildings where HSCs are currently functioning in rented premises b) Rebuilding HSCs which are unfit for occupation. c) Taking up of repairs/renovation and provision of water supply/electrical works to PHCs/HSCs. d) Need-based supply of equipment/furniture to the HSCs and PHCs as per the standard list including gas connections. e) Provision of Cell phones to HSCs where large number of deliveries take place. f) Provision of telephones to PHCs
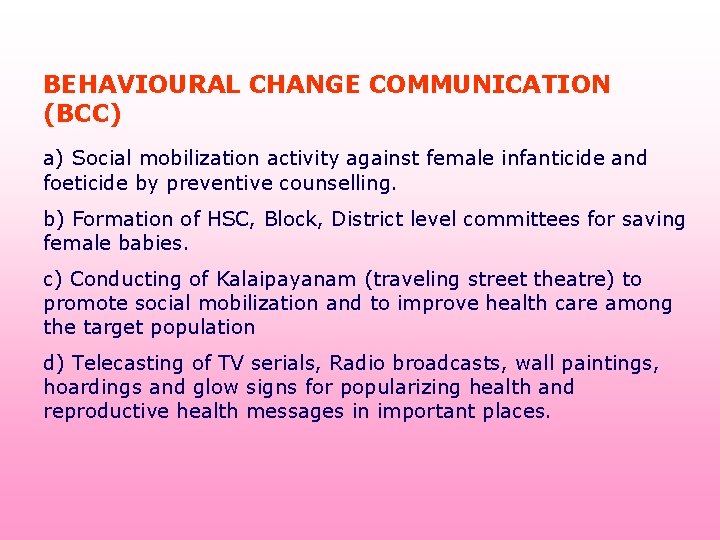
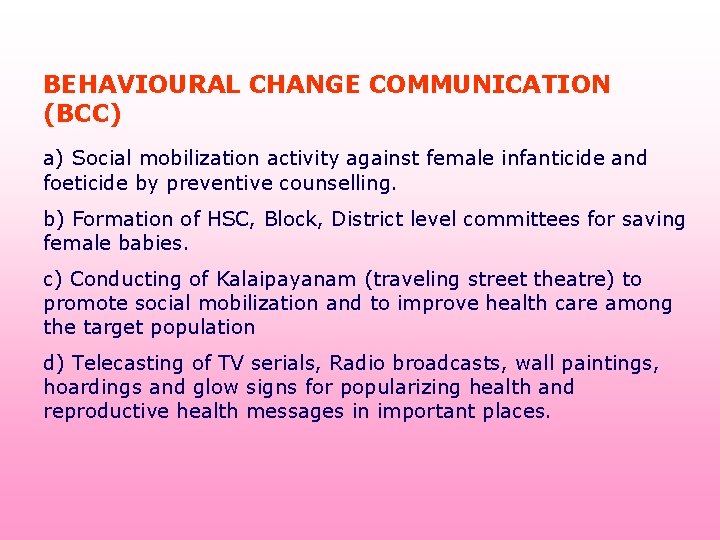
BEHAVIOURAL CHANGE COMMUNICATION (BCC) a) Social mobilization activity against female infanticide and foeticide by preventive counselling. b) Formation of HSC, Block, District level committees for saving female babies. c) Conducting of Kalaipayanam (traveling street theatre) to promote social mobilization and to improve health care among the target population d) Telecasting of TV serials, Radio broadcasts, wall paintings, hoardings and glow signs for popularizing health and reproductive health messages in important places.

Packages of services at sub-centre Immunization, Antenatal, Natal and Postnatal care, prevention of malnutrition and common childhood diseases, family planning services and counselling. They also provide elementary drugs for minor ailments such as ARI, diarrhea, fever, worm infestation etc. and carryout community needs assessment.

PACKAGES OF SERVICES AT FRU • Vacuum Extractions • Administration of Anesthesia • Blood Transfusion • Caesarean Section • Manual Removal of Placenta • Carry out Suction Curettage for Incomplete Abortion • Insert Intrauterine Devices • Sterilization Operation
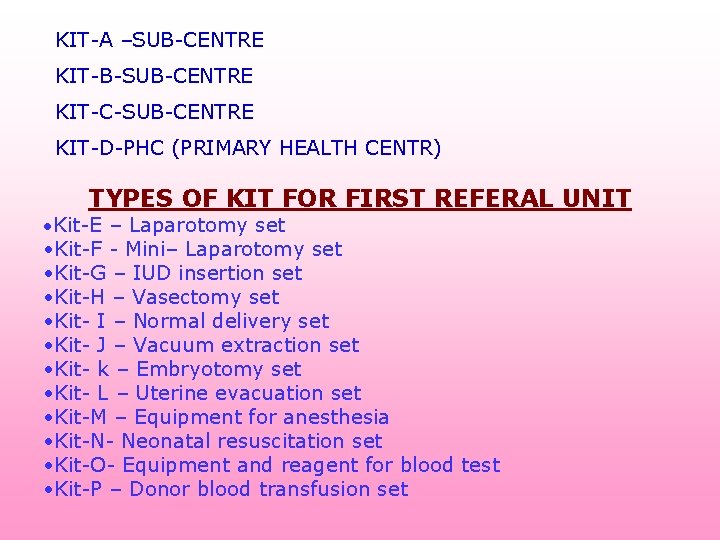
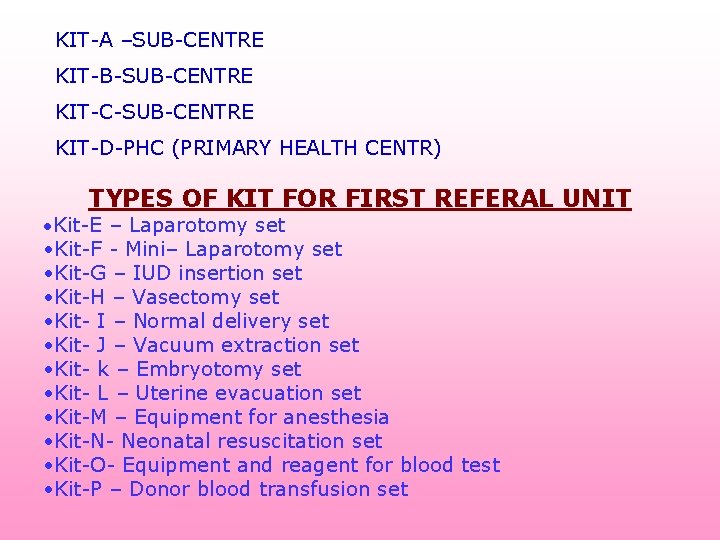
KIT-A –SUB-CENTRE KIT-B-SUB-CENTRE KIT-C-SUB-CENTRE KIT-D-PHC (PRIMARY HEALTH CENTR) TYPES OF KIT FOR FIRST REFERAL UNIT • Kit-E – Laparotomy set • Kit-F - Mini– Laparotomy set • Kit-G – IUD insertion set • Kit-H – Vasectomy set • Kit- I – Normal delivery set • Kit- J – Vacuum extraction set • Kit- k – Embryotomy set • Kit- L – Uterine evacuation set • Kit-M – Equipment for anesthesia • Kit-N- Neonatal resuscitation set • Kit-O- Equipment and reagent for blood test • Kit-P – Donor blood transfusion set
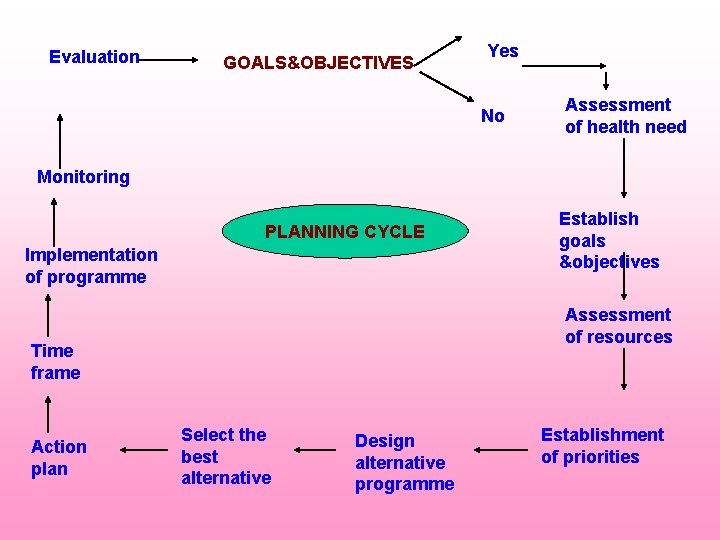
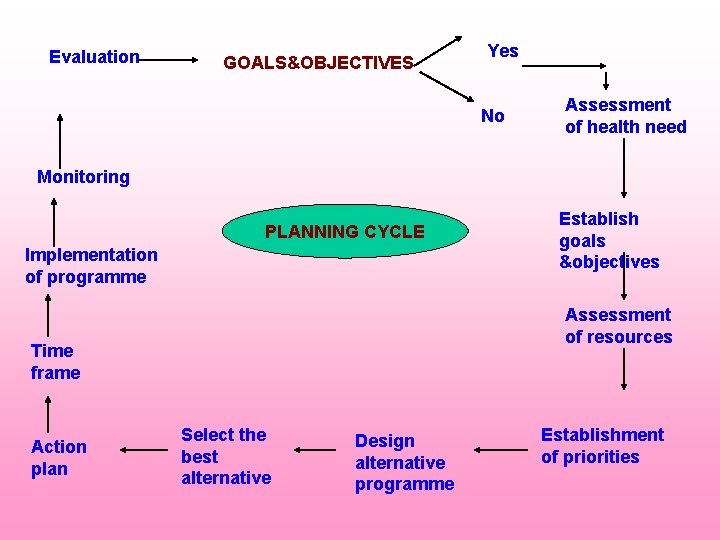
Evaluation GOALS&OBJECTIVES Yes No Assessment of health need Monitoring PLANNING CYCLE Implementation of programme Assessment of resources Time frame Action plan Establish goals &objectives Select the best alternative Design alternative programme Establishment of priorities
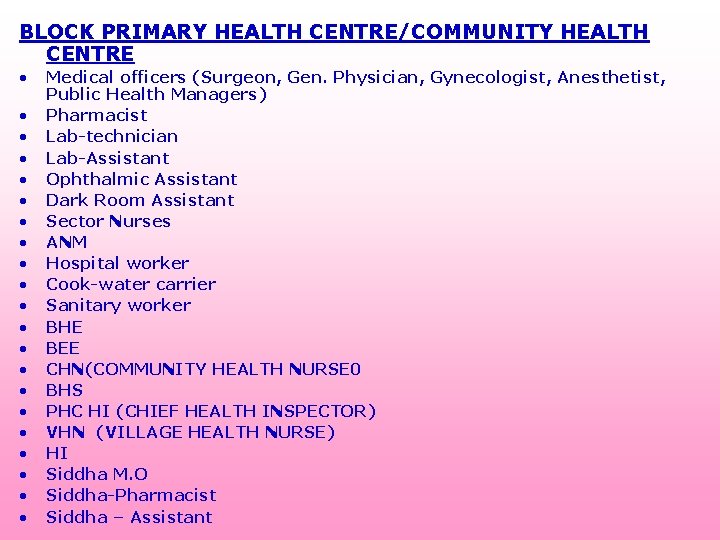
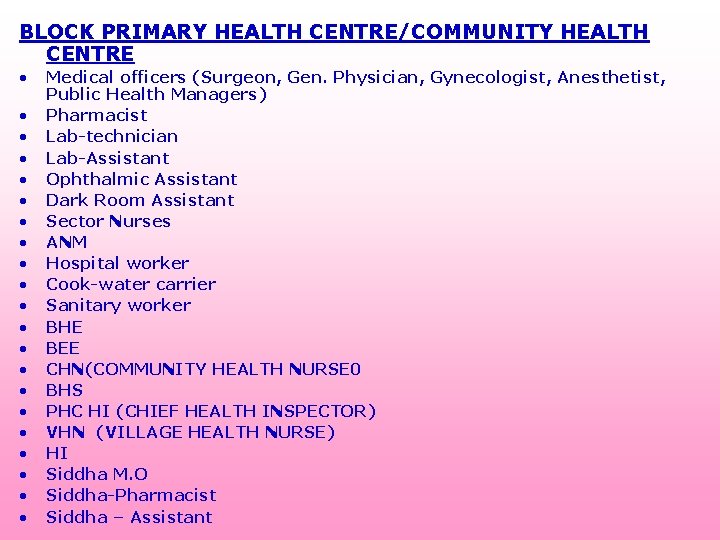
BLOCK PRIMARY HEALTH CENTRE/COMMUNITY HEALTH CENTRE • • • • • • Medical officers (Surgeon, Gen. Physician, Gynecologist, Anesthetist, Public Health Managers) Pharmacist Lab-technician Lab-Assistant Ophthalmic Assistant Dark Room Assistant Sector Nurses ANM Hospital worker Cook-water carrier Sanitary worker BHE BEE CHN(COMMUNITY HEALTH NURSE 0 BHS PHC HI (CHIEF HEALTH INSPECTOR) VHN (VILLAGE HEALTH NURSE) HI Siddha M. O Siddha-Pharmacist Siddha – Assistant
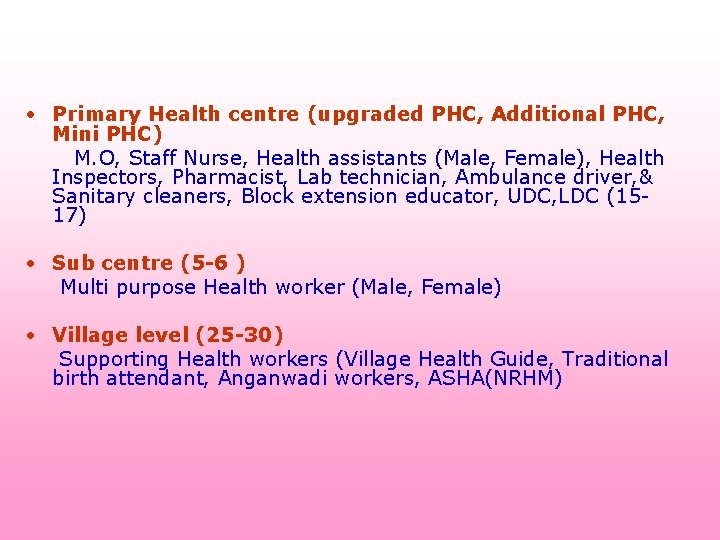
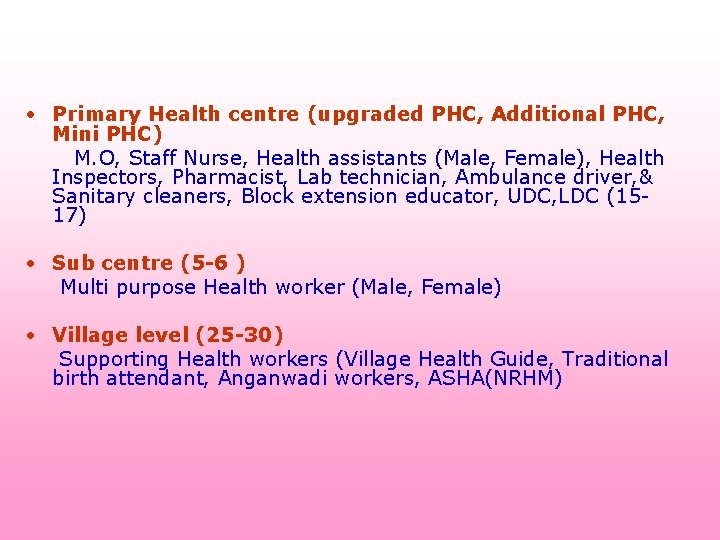
• Primary Health centre (upgraded PHC, Additional PHC, Mini PHC) M. O, Staff Nurse, Health assistants (Male, Female), Health Inspectors, Pharmacist, Lab technician, Ambulance driver, & Sanitary cleaners, Block extension educator, UDC, LDC (1517) • Sub centre (5 -6 ) Multi purpose Health worker (Male, Female) • Village level (25 -30) Supporting Health workers (Village Health Guide, Traditional birth attendant, Anganwadi workers, ASHA(NRHM)
INDICATORS OF MONITORING &EVALUATION RCH-II PROGRAMME 1. The public health managers have to monitor the programme. 2. They have to evaluate the effectiveness of the programme with the following indicators.
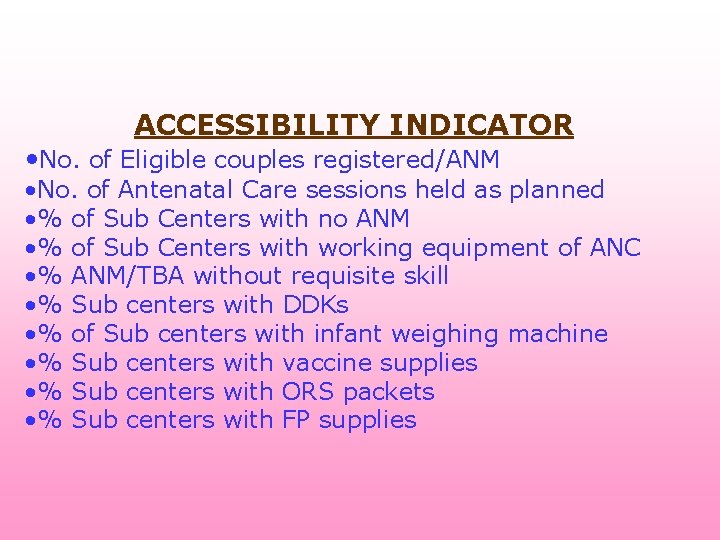
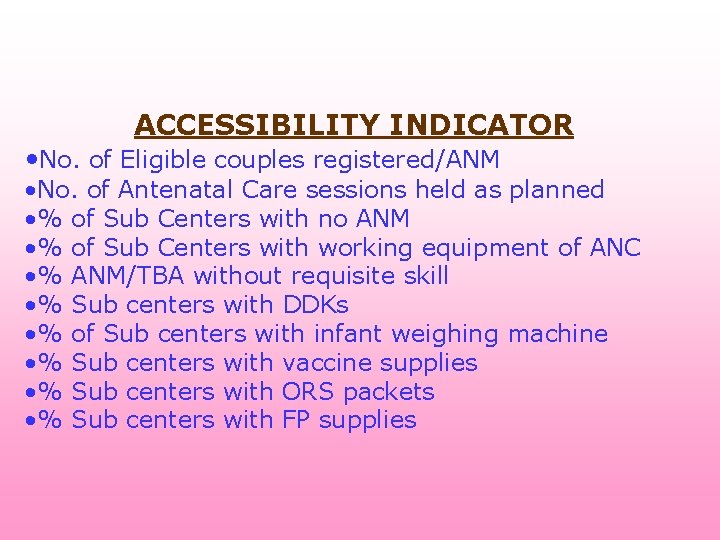
ACCESSIBILITY INDICATOR • No. of Eligible couples registered/ANM • No. of Antenatal Care sessions held as planned • % of Sub Centers with no ANM • % of Sub Centers with working equipment of ANC • % ANM/TBA without requisite skill • % Sub centers with DDKs • % of Sub centers with infant weighing machine • % Sub centers with vaccine supplies • % Sub centers with ORS packets • % Sub centers with FP supplies

QUALITY INDICATOR • % Pregnancy registered before 12 weeks • % ANC with 5 visits • % ANC receiving all RCH services • % High-risk cases referred • % High-risk cases followed up • % Deliveries by ANM/TBA • %PNC with 3 PNC visits • % PNC receiving all counselling • % PNC complications referred • % Eligible couple offered FP choices • % Women screened for RTI/STDs • % Eligible couple counselled for prevention of RTI/STDs • % ADD given ORS • % ARI treated • % Children fully immunized
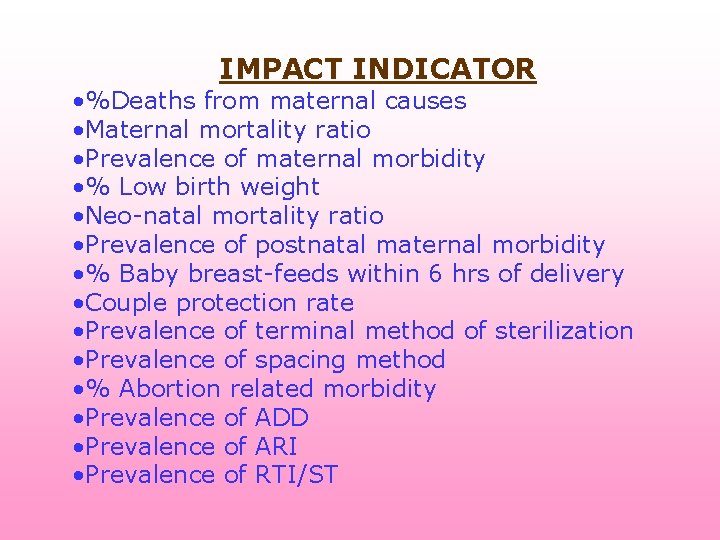
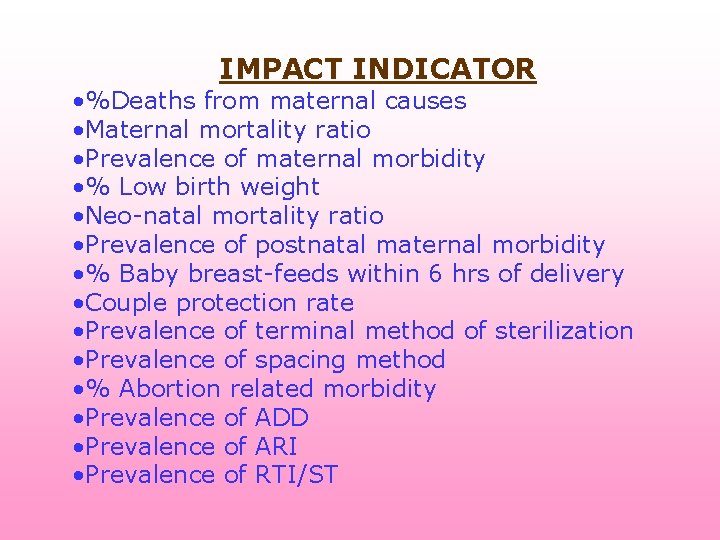
IMPACT INDICATOR • %Deaths from maternal causes • Maternal mortality ratio • Prevalence of maternal morbidity • % Low birth weight • Neo-natal mortality ratio • Prevalence of postnatal maternal morbidity • % Baby breast-feeds within 6 hrs of delivery • Couple protection rate • Prevalence of terminal method of sterilization • Prevalence of spacing method • % Abortion related morbidity • Prevalence of ADD • Prevalence of ARI • Prevalence of RTI/ST
HEALTH MANAGEMENT INFORMATION SYSTEMS Introduction of IT-enabled HMIS for planning and monitoring health services at the State/District /Block levels
TRAINING a) Skill upgradation training with focus on improving/upgrading the skills of health care providers. b) Integrated skill training for peripheral health functionaries such as VHNs, SHNs, medical officers and health inspectors. c) Improving managerial and communication skills of health staff.
SUB CENTRE ACTION PLAN • • • To collect the C. B. R from C. D. M. O’S office Survey the population of the area Estimate the No of eligible beneficiaries Estimate the no of Infants Estimate the no of Live births Estimate the no of <5 years children Estimate the no of Antenatal registration Estimate the no of High risk pregnancies Estimate the no of anemic pregnant women Estimate the no of high risk newborns Estimate the no of <3 years children
CALCULATION OF VACCINE REQUIREMENT • Population of the area • Birth rate • Infant mortality rate
• • No of beneficiaries No of doses of each vaccine Wastage & Multiplication factor Number of sessions
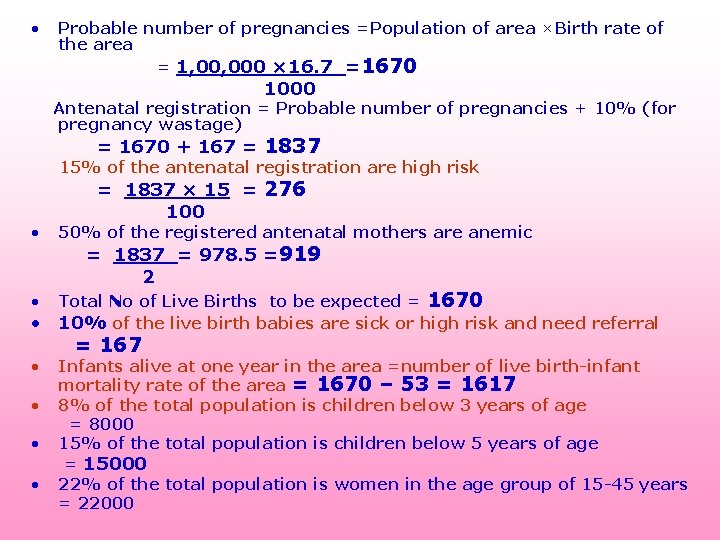
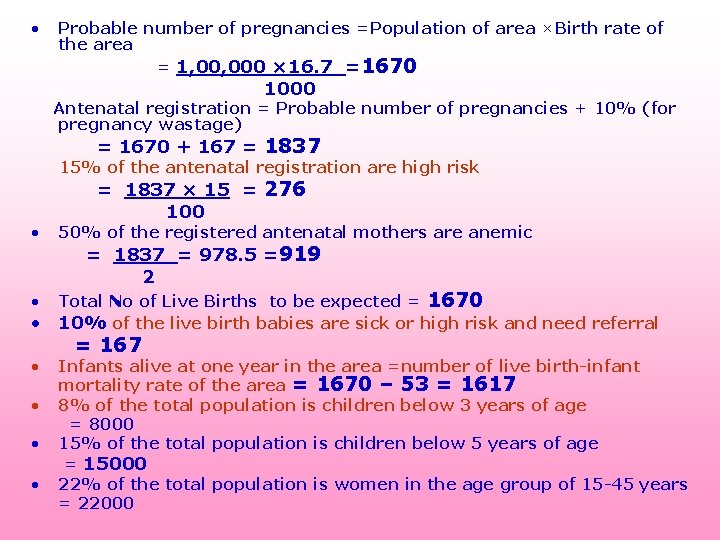
• Probable number of pregnancies =Population of area ×Birth rate of the area = 1, 000 × 16. 7 =1670 1000 Antenatal registration = Probable number of pregnancies + 10% (for pregnancy wastage) = 1670 + 167 = 1837 15% of the antenatal registration are high risk = 1837 × 15 = 276 100 • 50% of the registered antenatal mothers are anemic = 1837 = 978. 5 =919 2 Total No of Live Births to be expected = 1670 • 10% of the live birth babies are sick or high risk and need referral = 167 • Infants alive at one year in the area =number of live birth-infant mortality rate of the area = 1670 – 53 = 1617 • 8% of the total population is children below 3 years of age = 8000 • 15% of the total population is children below 5 years of age = 15000 • 22% of the total population is women in the age group of 15 -45 years = 22000 •

• The number of pregnant women = Population × Birth rate • The number of infants = Population × Birth rate ×(1 IMR) Annual Vaccine Requirement = No of eligible ×No of doses × Proposed coverage ×Multiplication factor based on VAR (DPT, DT, TT, OPV ) Multiplication factor=1. 33 ( BCG, Measles) Multiplication factor =2
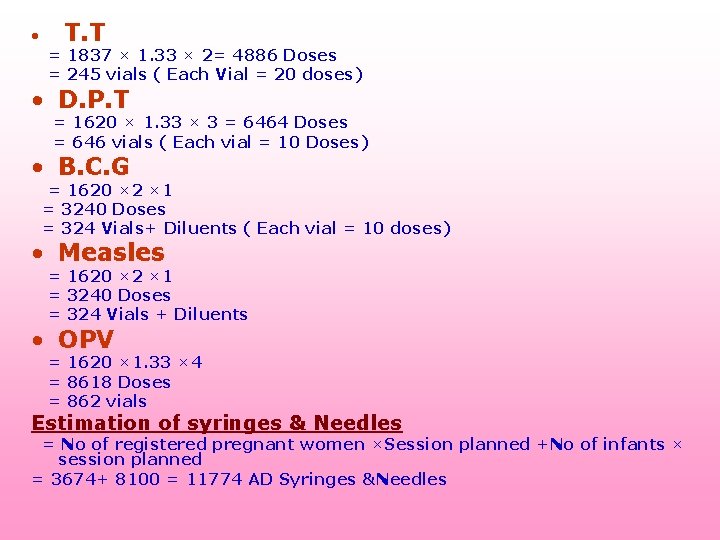
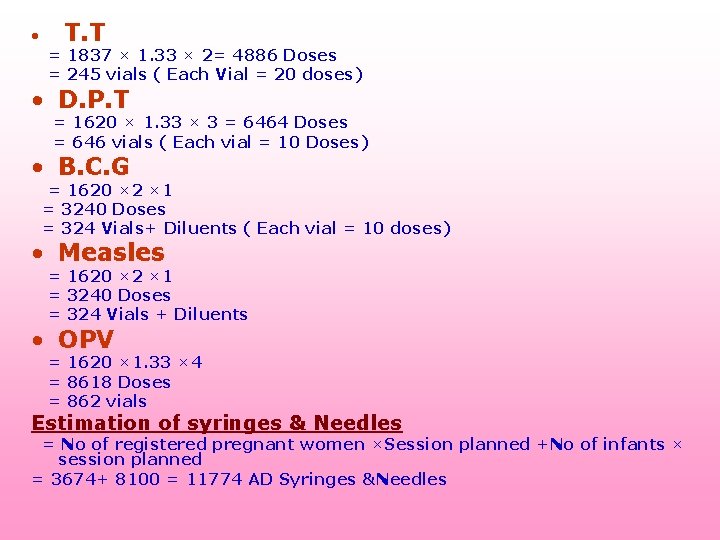
• T. T = 1837 × 1. 33 × 2= 4886 Doses = 245 vials ( Each Vial = 20 doses) • D. P. T = 1620 × 1. 33 × 3 = 6464 Doses = 646 vials ( Each vial = 10 Doses) • B. C. G = 1620 × 2 × 1 = 3240 Doses = 324 Vials+ Diluents ( Each vial = 10 doses) • Measles = 1620 × 2 × 1 = 3240 Doses = 324 Vials + Diluents • OPV = 1620 × 1. 33 × 4 = 8618 Doses = 862 vials Estimation of syringes & Needles = No of registered pregnant women ×Session planned +No of infants × session planned = 3674+ 8100 = 11774 AD Syringes &Needles
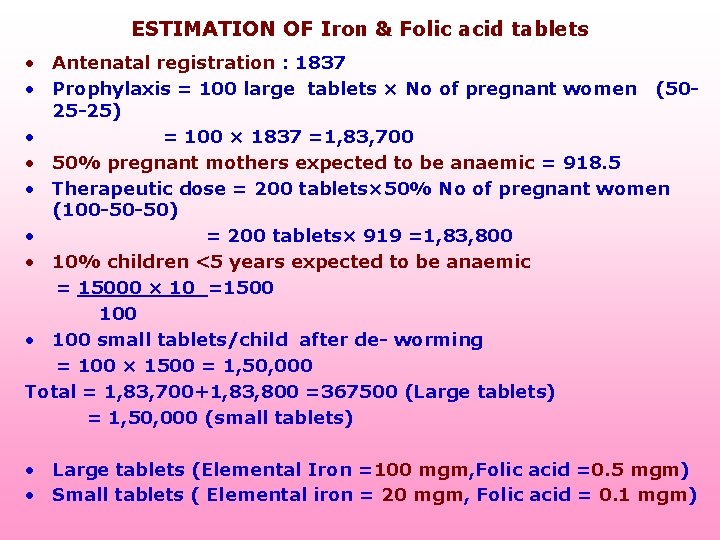
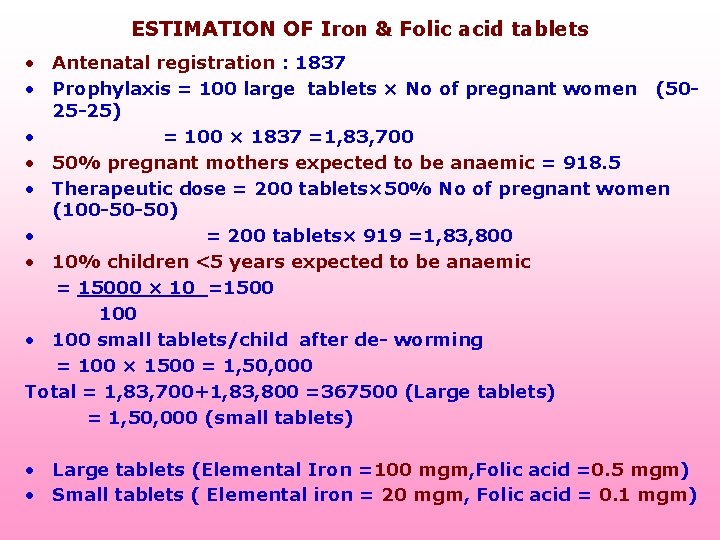
ESTIMATION OF Iron & Folic acid tablets • Antenatal registration : 1837 • Prophylaxis = 100 large tablets × No of pregnant women (5025 -25) • = 100 × 1837 =1, 83, 700 • 50% pregnant mothers expected to be anaemic = 918. 5 • Therapeutic dose = 200 tablets× 50% No of pregnant women (100 -50 -50) • = 200 tablets× 919 =1, 83, 800 • 10% children <5 years expected to be anaemic = 15000 × 10 =1500 100 • 100 small tablets/child after de- worming = 100 × 1500 = 1, 50, 000 Total = 1, 83, 700+1, 83, 800 =367500 (Large tablets) = 1, 50, 000 (small tablets) • Large tablets (Elemental Iron =100 mgm, Folic acid =0. 5 mgm) • Small tablets ( Elemental iron = 20 mgm, Folic acid = 0. 1 mgm)
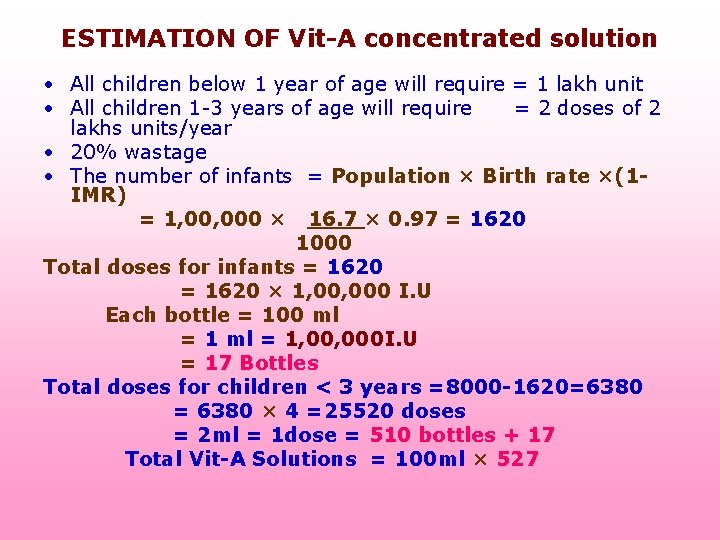
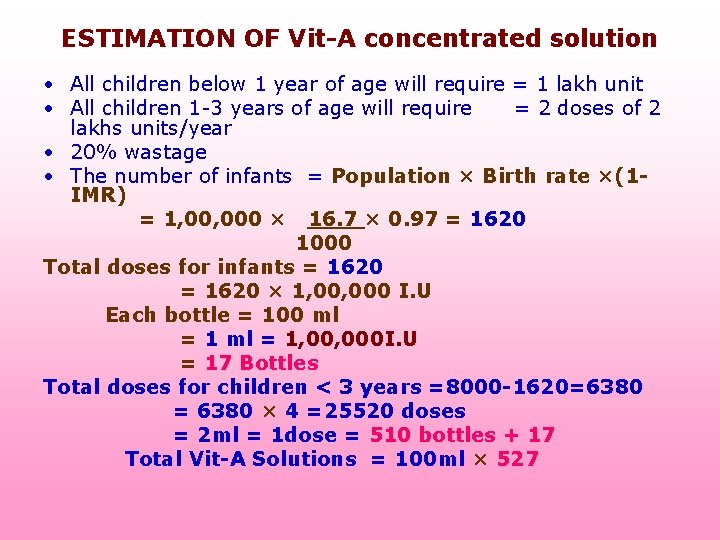
ESTIMATION OF Vit-A concentrated solution • All children below 1 year of age will require = 1 lakh unit • All children 1 -3 years of age will require = 2 doses of 2 lakhs units/year • 20% wastage • The number of infants = Population × Birth rate ×(1 IMR) = 1, 000 × 16. 7 × 0. 97 = 1620 1000 Total doses for infants = 1620 = 1620 × 1, 000 I. U Each bottle = 100 ml = 1 ml = 1, 000 I. U = 17 Bottles Total doses for children < 3 years =8000 -1620=6380 = 6380 × 4 =25520 doses = 2 ml = 1 dose = 510 bottles + 17 Total Vit-A Solutions = 100 ml × 527
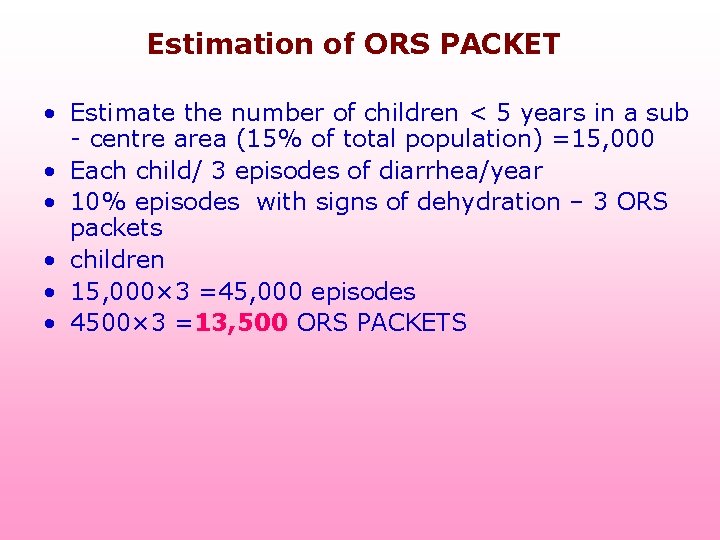
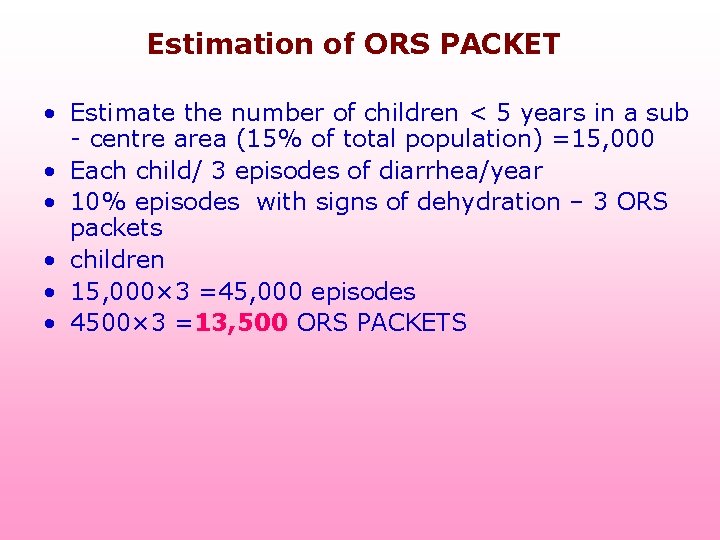
Estimation of ORS PACKET • Estimate the number of children < 5 years in a sub - centre area (15% of total population) =15, 000 • Each child/ 3 episodes of diarrhea/year • 10% episodes with signs of dehydration – 3 ORS packets • children • 15, 000× 3 =45, 000 episodes • 4500× 3 =13, 500 ORS PACKETS
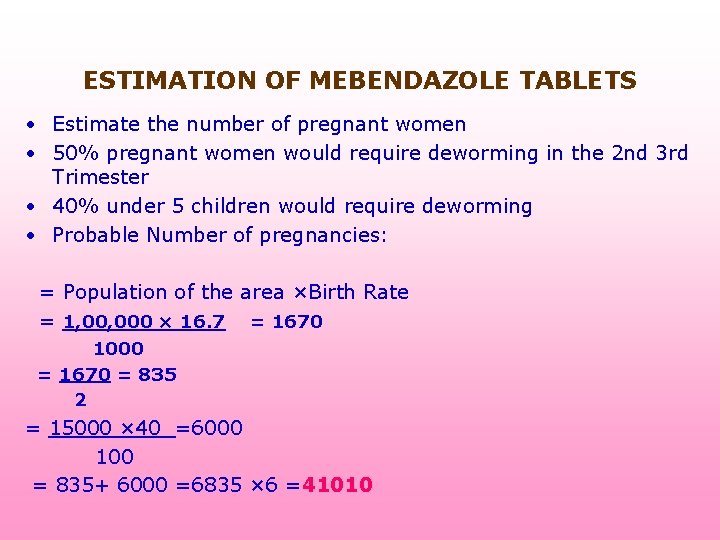
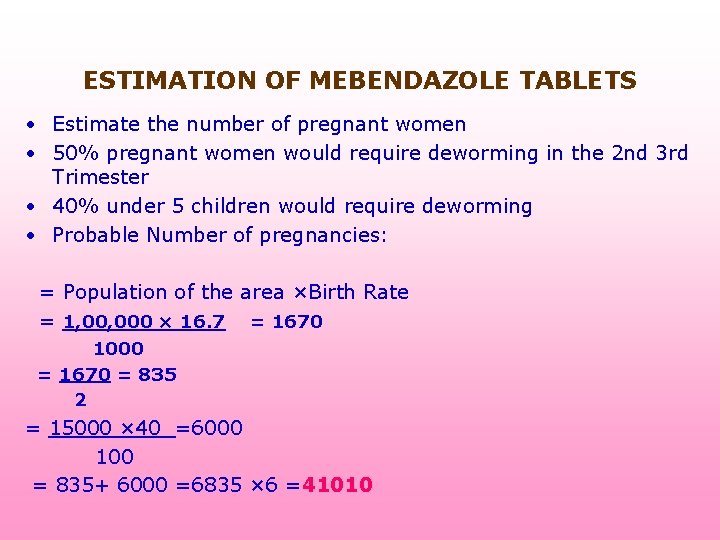
ESTIMATION OF MEBENDAZOLE TABLETS • Estimate the number of pregnant women • 50% pregnant women would require deworming in the 2 nd 3 rd Trimester • 40% under 5 children would require deworming • Probable Number of pregnancies: = Population of the area ×Birth Rate = 1, 000 × 16. 7 = 1670 1000 = 1670 = 835 2 = 15000 × 40 =6000 100 = 835+ 6000 =6835 × 6 =41010
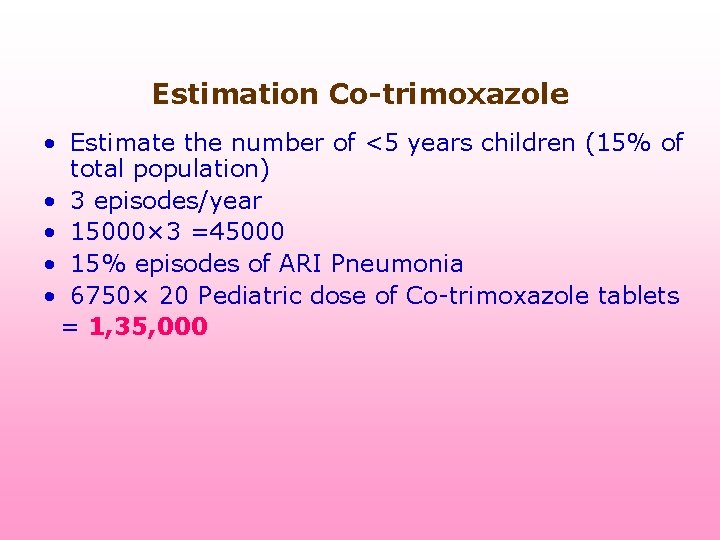
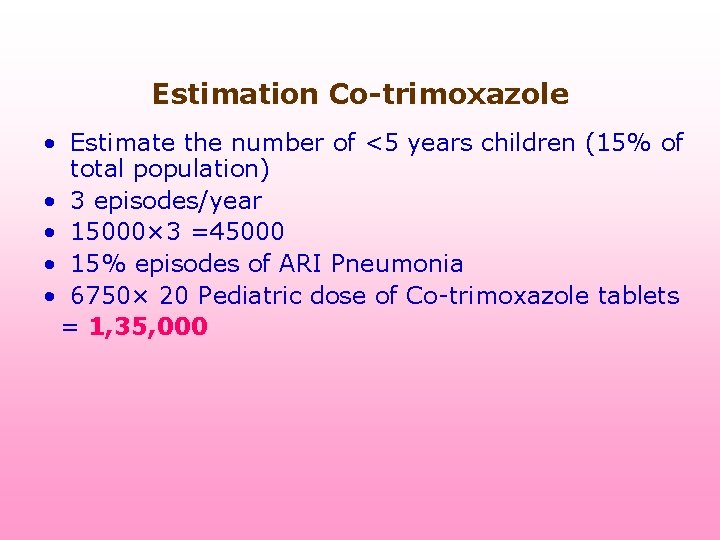
Estimation Co-trimoxazole • Estimate the number of <5 years children (15% of total population) • 3 episodes/year • 15000× 3 =45000 • 15% episodes of ARI Pneumonia • 6750× 20 Pediatric dose of Co-trimoxazole tablets = 1, 35, 000
COLD BOXES • 5 Litres – One month supply of PHC • 20 Litres – One month supply of Health centre for 1 lakh population • 5 days • VACCINE CARRIER • 16 -20 VIALS (20 NUMBERS) • 2 days • Day carrier • 6 -8 vials • 8 hrs Sphygmomanometer & stethoscope One for each sub center One weighing scale for adult & on spring balance for babies in each sub centre
CONCLUSION: Public health experts should be an essential part of the executive management team and will have to play a key role in our country by identifying the major problems in the RCH programme such as the absence of links between communities, subcentres and referral facilities; shortages of equipment and trained staff at referral facility; and a lack of emergency transport to adequately meet the needs of pregnant women particularly for obstetrical emergencies. Allocation of resources should be linked to states performance as well as to population size. They have to identify the new indicators for performance, and allocation of resources based on the felt need of the on priority. Active participation of Community with involvement and support of women’s self help groups, village health nurse, anganwadi workers, asha activist etc. , will be very effective in improving women accessibility to different components of RCH services and increasing sensitivity to women’s needs. The private sectors role in improving women’s health is very helpful. We have to find out a mechanism to involve them through appropriate rules ®ulations to provide the RCH Phase-II programme to the community. World Health Day slogan 2005 “Make Every Mother and Child Count” reflects that health of women and children should be given higher priority at all levels of health care system. Every one is accountable for health of mothers & children. The World Health Day slogan 2006 “Working together for health” reflects the involvement of health care workers to provide quality health care services to the community. The fulfillment objective of Phase-II RCH programme is the joint effort of community and service providers.
REFERENCES: • National Health programs of India by J. KISHORE • Text book of Preventive & Social Medicine 19 th edition • ISSN 0019 -557 X, VOL. XXXXIX No. 3 JULY-SEPTEMBER, 2005 • Country fact file on Maternal, Newborn and Child Health situation in India Centre for Community Medicine*All India Institute of Medical Sciences New Delhi – 110029 • www. tn. gov. in/spc/tenthplan/CH_5. PDF • Public Health in South-East Asia in the 21 st Century

THANKING YOU
 1 crore in numbers
1 crore in numbers Tenue type 1 rch
Tenue type 1 rch Role of nurse in rch phase 2
Role of nurse in rch phase 2 Rch programme launched in india
Rch programme launched in india Define rch in community
Define rch in community Rch anmol
Rch anmol Rch phase 2
Rch phase 2 Anmol
Anmol Role of nurse in rch phase 2
Role of nurse in rch phase 2 Epilepsy
Epilepsy Rchportal
Rchportal Herpesvirus
Herpesvirus Fracture
Fracture Kontinuitetshantering
Kontinuitetshantering Novell typiska drag
Novell typiska drag Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Ekologiskt fotavtryck
Ekologiskt fotavtryck Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Underlag för särskild löneskatt på pensionskostnader
Underlag för särskild löneskatt på pensionskostnader Tidböcker
Tidböcker A gastrica
A gastrica Förklara densitet för barn
Förklara densitet för barn Datorkunskap för nybörjare
Datorkunskap för nybörjare Stig kerman
Stig kerman Debattartikel mall
Debattartikel mall Magnetsjukhus
Magnetsjukhus Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Formel för lufttryck
Formel för lufttryck Publik sektor
Publik sektor I gullregnens månad
I gullregnens månad Presentera för publik crossboss
Presentera för publik crossboss Jiddisch
Jiddisch Bat mitza
Bat mitza Treserva lathund
Treserva lathund Fimbrietratt
Fimbrietratt Bästa kameran för astrofoto
Bästa kameran för astrofoto Centrum för kunskap och säkerhet
Centrum för kunskap och säkerhet Programskede byggprocessen
Programskede byggprocessen Bra mat för unga idrottare
Bra mat för unga idrottare Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Rutin för avvikelsehantering
Rutin för avvikelsehantering Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Tack för att ni har lyssnat
Tack för att ni har lyssnat Referat mall
Referat mall Redogör för vad psykologi är
Redogör för vad psykologi är Stål för stötfångarsystem
Stål för stötfångarsystem Tack för att ni har lyssnat
Tack för att ni har lyssnat Borra hål för knoppar
Borra hål för knoppar Orubbliga rättigheter
Orubbliga rättigheter Stickprovsvariansen
Stickprovsvariansen Tack för att ni har lyssnat
Tack för att ni har lyssnat Steg för steg rita
Steg för steg rita Informationskartläggning
Informationskartläggning Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Blomman för dagen drog
Blomman för dagen drog Mästar lärling modellen
Mästar lärling modellen Egg för emanuel
Egg för emanuel