LIVER TUMOURS Dr Ramdasd Rai Prof Unit Chief

- Slides: 79
LIVER TUMOURS Dr. Ramdasd Rai Prof. & Unit Chief YMCH
BENIGN LIVER TUMOURS 1) Haemangiomas 2) Hepatic adenomas 3) Focal nodular hyperplasia
� � HAEMANGIOMAS These are the most common liver lesions � They consist of an abnormal plexus of vessels and their nature is usually apparent on ultrasound. � If diagnostic uncertainty exists, CT scanning with delayed contrast enhancement shows the characteristic appearance of slow contrast enhancement due to small vessel uptake in the haemangioma.
� Often, haemangiomas are multiple. � Lesions found incidentally require confirmation of their nature and no further treatment. � The management of ‘giant’ haemangiomas is more controversial. � Occasional reports of rupture of haemangiomas have led some to consider resection for the large lesions, especially if they appear to be symptomatic
� They have little if any malignant potential, and this is no indication for surgery. � Percutaneous biopsy of these lesions should be avoided as they are vascular lesions and may bleed profusely into the peritoneal cavity.
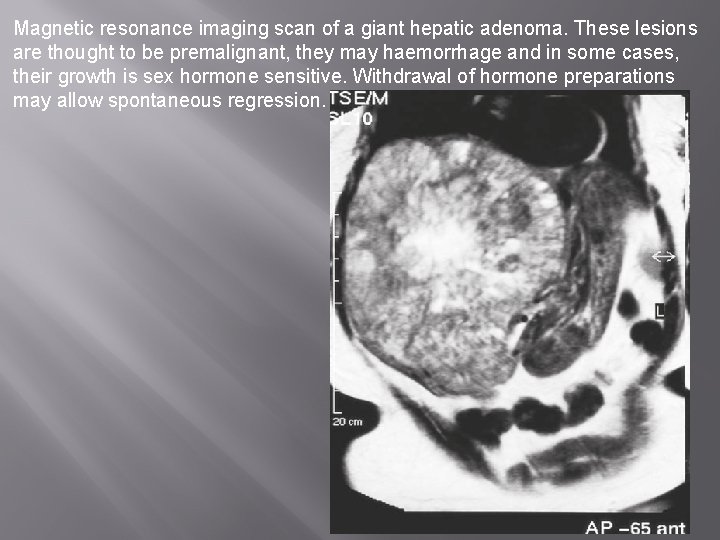
� � HEPATIC ADENOMAS Hepatic adenomas are rare benign liver tumours. � They occur mostly in women of child-bearing age. Imaging by CT or MRI demonstrates a well-circumscribed and vascular solid tumour. � They usually develop in an otherwise normal liver. Unfortunately, there are no characteristic radiological features to differentiate these lesions from HCC
� Arterial phase CT demonstrates a well-developed peripheral arterialisation of the tumour. Biopsy may be necessary for confirmation and characterisation of the nature of these lesions. � These tumours may bleed and are thought to have malignant potential, and resection is therefore the treatment of choice.
� An association with sex hormones (including the oral contraceptive pill) is well recognised, and regression of symptomatic adenomas on withdrawal of hormone stimulation is well documented.
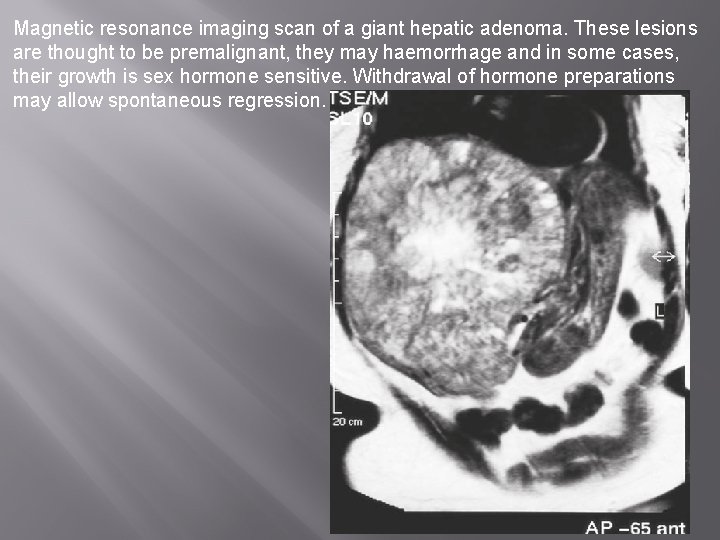
Magnetic resonance imaging scan of a giant hepatic adenoma. These lesions are thought to be premalignant, they may haemorrhage and in some cases, their growth is sex hormone sensitive. Withdrawal of hormone preparations may allow spontaneous regression.
FOCAL NODULAR HYPERPLASIA � This is an unusual benign condition of unknown aetiology in which there is a focal overgrowth of functioning liver tissue supported by fibrous stroma. � Patients are usually middle-aged females and there is no association with underlying liverdisease.
� Ultrasound shows a solid tumour mass but does not help in discrimination. � Contrast CT or/and MRI may show central scarring and evidence of a well-vascularised lesion. � Again, these appearances are not specific for focal nodular hyperplasia (FNH). � FNH contain both hepatocytes and Kupffer cells.
� MRI using liver-specific contrast agents, such as gadoxetic acid, which is taken up by hepatocytes and excreted in bile or superparamagnetic iron oxide which is taken up by Kupffer cells, may be useful in determining the hepatocellular origin of FNH and allowing differentiation of FNH from metastatic cancer.
� Similarly, a sulphur colloid liver scan may be useful, since Kupffer cells take up the colloid. � FNH do not have any malignant potential and, once the diagnosis is confirmed, they do not require any treatment.
PRIMARY MALIGNANT TUMOURS OF THE LIVER 1. Hepato-cellular carcinoma/Hepatoma/HCC (80%). 2. Cholangiocarcinoma (20%). 3. Hepatoblastoma in infants and children.
� � � � Hepatoblastoma occurs within 2 years of life. It is most common primary malignant tumour of liver in children. It is common in male child. CT scan shows vascular mass with speckled calcification. It is highly sensitive to chemotherapy (vincristine, doxorubicin, 5 FU). If it is resectable, it is the initial choice of therapy. Liver transplantation is also beneficial.
HEPATOCELLULAR CARCINOMA (HCC) � It is common in cirrhotics and hepatitis B and hepatitis C virus infection. � It is common in Mozambique. � Male to female ratio is 4: 1. � It is usually unicentric but occasionally can be multicentric. � Right lobe is commonly involved.
Aetiology � Aflatoxin B 1, a product of fungus aspergillus. � Hepatitis B and hepatitis C virus infection. � Alcoholic cirrhosis. � Clonarchis sinensis infestation. � Smoking. � Haemochromatosis. � Hepatic adenoma – potentially malignant.
� Environment related chemicals like DDT, nitrite and nitrate related food products; trichloroethylene (dry cleaning solvents), biphenyls, carbon tetrachloride, herbicides, solvents like dioxane. � Tannins, griseofulvin, bush tea (pyrrolizidine), rice toxins. � Anabolic steroids, polyvinyl chloride
Pathology � Gross � It is highly vascular with indistinct margin. Often it is well demarcated by fibrous tissue. � Haemorrhage and necrosis are common.
� Hanging type of tumour – tumour attached to normal liver by a small vascular stalk – always very well resectable. � Pushing type of tumour – large, well demarcated, displaces normal vasculature – resectable. � Infiltrative type of tumour – indistinct, infiltrative – often difficult to resect.
Histology � Well/moderate/poorly differentiated tumour. � Okudas classification – multifocal; indeterminate; spreading; expanding.
� Fibrolamellar Variant of HCC (FL HCC) It occurs in younger age group. � Incidence is equal in both sexes. � It does not show any elevated levels of serum AFP. � Tumour marker for this type is increase in serum vitamin. B 12 binding protein and increase in neurotensin levels. �
� It is not related to viral hepatitis or cirrhosis. � Left lobe is commonly involved. � It involves lymph nodes more commonly than HCC. � CT scan shows characteristic central scarring.
� Fibrous stromas with thin hyaline bands are typical. � Sheets of well differentiated hepatocytes are seen which are sandwiched between collagen and fibroblasts. � It is fairly resectable (50 -75%) with better prognosis than HCC.
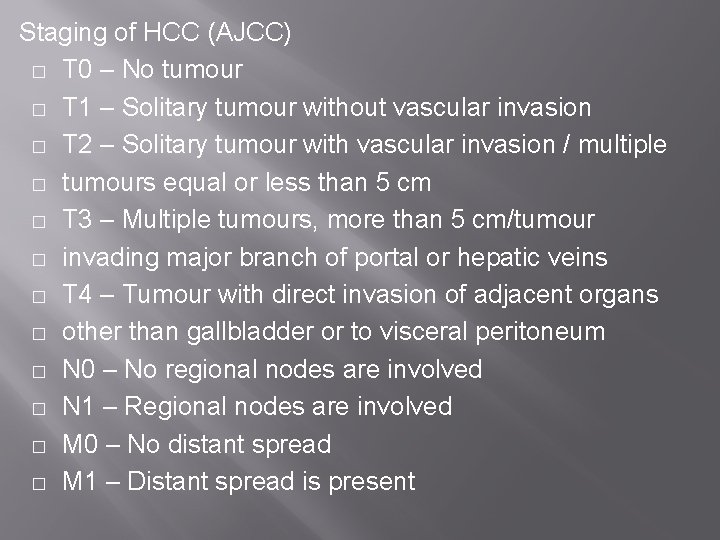
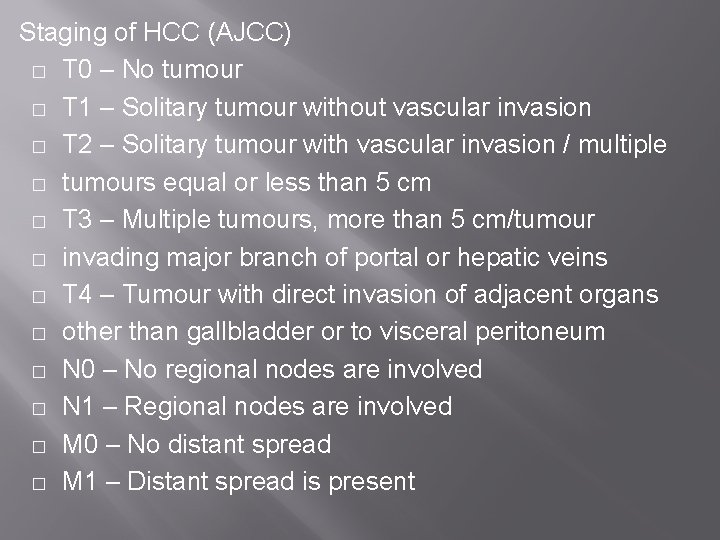
Staging of HCC (AJCC) � T 0 – No tumour � T 1 – Solitary tumour without vascular invasion � T 2 – Solitary tumour with vascular invasion / multiple � tumours equal or less than 5 cm � T 3 – Multiple tumours, more than 5 cm/tumour � invading major branch of portal or hepatic veins � T 4 – Tumour with direct invasion of adjacent organs � other than gallbladder or to visceral peritoneum � N 0 – No regional nodes are involved � N 1 – Regional nodes are involved � M 0 – No distant spread � M 1 – Distant spread is present
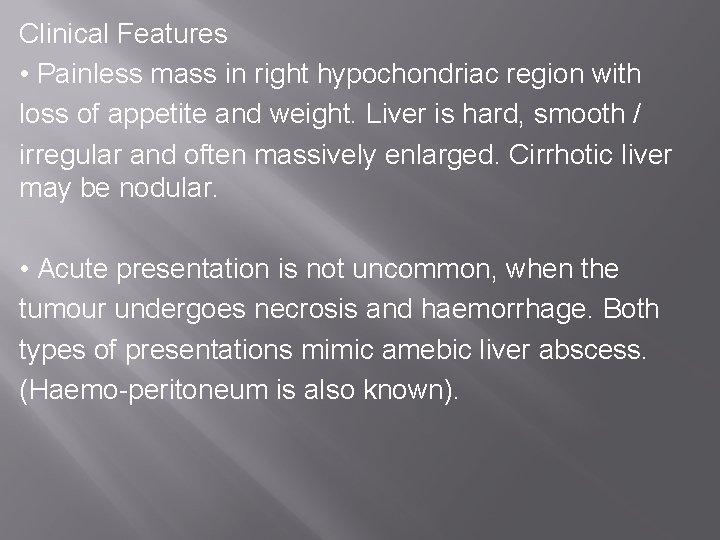
Clinical Features • Painless mass in right hypochondriac region with loss of appetite and weight. Liver is hard, smooth / irregular and often massively enlarged. Cirrhotic liver may be nodular. • Acute presentation is not uncommon, when the tumour undergoes necrosis and haemorrhage. Both types of presentations mimic amebic liver abscess. (Haemo-peritoneum is also known).
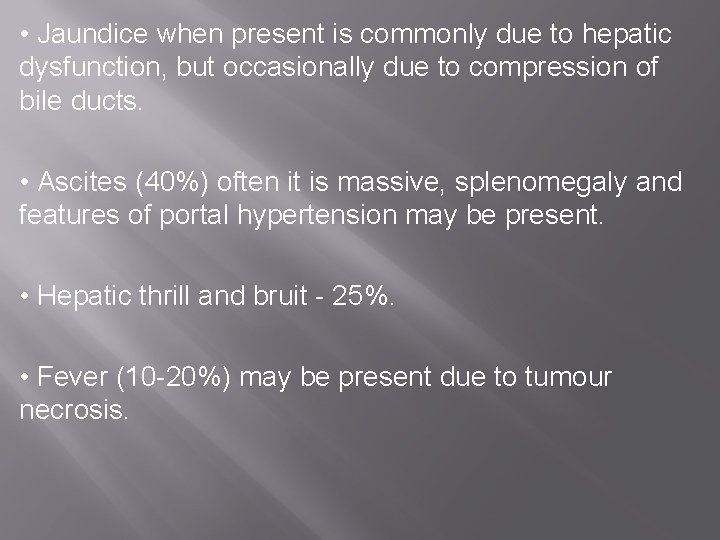
• Jaundice when present is commonly due to hepatic dysfunction, but occasionally due to compression of bile ducts. • Ascites (40%) often it is massive, splenomegaly and features of portal hypertension may be present. • Hepatic thrill and bruit - 25%. • Fever (10 -20%) may be present due to tumour necrosis.
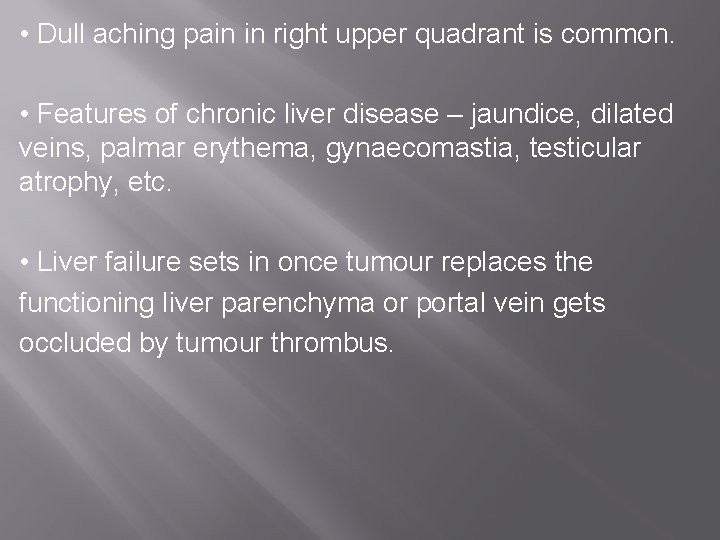
• Dull aching pain in right upper quadrant is common. • Features of chronic liver disease – jaundice, dilated veins, palmar erythema, gynaecomastia, testicular atrophy, etc. • Liver failure sets in once tumour replaces the functioning liver parenchyma or portal vein gets occluded by tumour thrombus.
� Gastrointestinal bleeding may be the presentation in 10% of cases due to portal hypertension or portal vein invasion by tumour. • Occasionally may present with para-neoplastic syndromes.
Spread of Tumour • Lymphatic spread: It can spread to other part of liver through lymphatics within the liver, to the lymph nodes in the porta hepatis and other abdominal lymph nodes later. Often spread occurs directly to cisterna chyli. • Blood spread: To lungs, bones and adrenals often can occur. • Direct infiltration: To diaphragm and neighbouring structures.
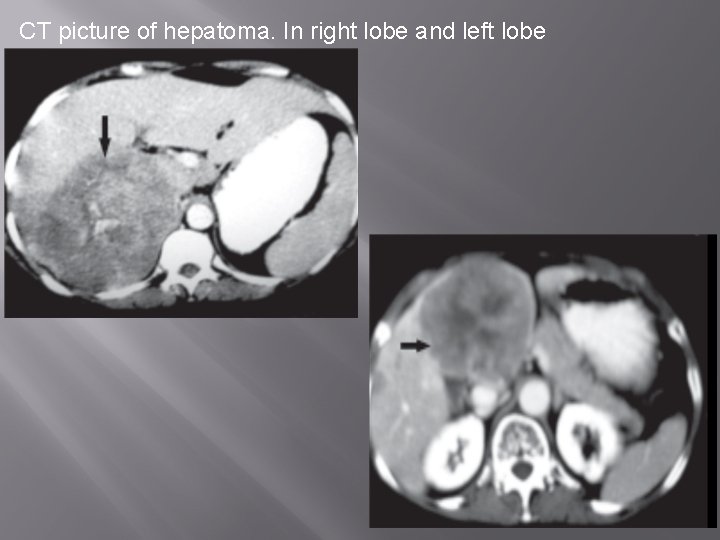
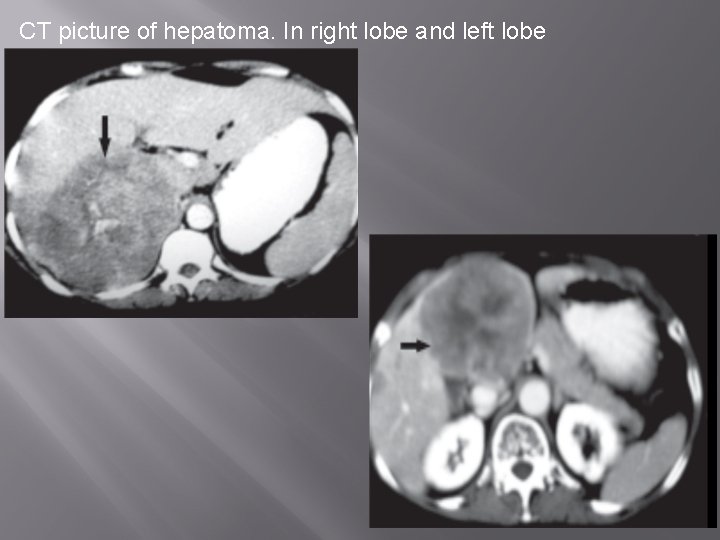
CT picture of hepatoma. In right lobe and left lobe
INVESTIGATIONS � U/S abdomen – very useful method. It shows hyper echoic mass; mosaic pattern with thin halo and lateral shadows. Extent, tumour thrombi extension can be made out. CT scan abdomen (CECT) more reliable and ideal (hypo dense, mosaic, vascular lesion with irregular margin). Reveals the size, location and extent, vascularity, portal vein invasion, nodal status, portal vein thrombosis. It helps to assess operability. �
� Tumour markers - α feto protein (AFP). AFP will be raised more than 100 IU; as high as 1000 IU is possible in HCC. PIVKA II is des γ carboxy prothrombin protein induced by vitamin K abnormality/ antagonists 2. It is increased in 80% of HCC patients. AFP is usually more than 400 IU in 70% of HCC patients. • Celiac angiography/CT angiography – It shows the vascularity of the tumour, tumour blush, arterial pattern of the liver and tumour; venous phase can show portal vein invasion or thrombosis and invasion/spread to IVC. Angiogram is essential while planning for hepatic resection
� Liver biopsy is done after controlling prothrombin time. � If it is elevated (by Inj vitamin K IM 10 mg for 5 days; FFP transfusion). � US / CT guided core liver biopsy is useful and mandatory before clinical trials. It is better than FNAC as it reveals tissue architecture. Problems with the core liver biopsy are spillage of tumour and bleeding (due to hypervascularity, associated thrombocytopenia and reduced liver dependent clotting factors like prothrombin). Such problems may be minimal in FNAC. Patients with high suspicious of HCC by clinical and imaging methods and who are appropriate for surgery may be taken up for surgery without a preoperative biopsy. In case of portal vein infiltration by tumour a portal vein biopsy may be done to exclude the patient for surgery or transplantation.
� Liver function tests like serum bilirubin, albumin, enzymes (alkaline phosphatase, transaminase, 5’ nucleotidase) including prothrombin time. � Contrast MRI/CT scan 1 -2 weeks following intrahepatic infusion of lipiodol (ethiodized oil emulsion 5 -15 ml) with contrast agent through hepatic artery is very useful. � MRI – T 2 weighted studies are useful for small HCC. � MR angiography is also done to see tumour thrombus in portal vein, hepatic vein and IVC.
� Ascitic tap when ascites is present for cytology. � Laparoscopic evaluation is useful for proper assessment of the tumour. � Investigations in relation to hepatitis B and hepatitis C virus infections. � Metastatic work up – HRCT of chest is essential
Treatment � Definitive Treatment � When limited to one lobe, hemihepatectomy is done. (Removal of 80% liver is compatible with life. There is no regenerative capacity in cirrhotic patients with poor coagulation status, portal hypertension, varices and ascites.
� In cirrhotic patients with HCC, total hepatectomy with orthotopic liver transplantation is required. Now it is found that even resection candidates will do better by transplantation than resection. But waiting period for transplantation is long. To bridge this waiting period for transplantation radiofrequency ablation, transarterial embolisation, ethanol/acetic acid injections are used.
� Note: Liver mass which is confirmed by CT/MRI and serum AFP is > 500 ng/dl is almost diagnostic and resection treatment can be started without tissue diagnosis
Indications for transplantation in HCC are – • Patient who is not a candidate for resection • Tumour less or equal to 5 cm • Tumour less than 3 in number • Tumour without portal/hepatic vein invasion • Tumour without extra hepatic spread
Palliative Treatment • Radiofrequency ablation (RFA): It is thermal ablation of the tumour by passing 18 G needle into the middle of the tumour and passing electric current of 500 k. Hz. � This creates frictional heat causing sphere of necrosis. � Maximum zone of necrosis which can be created is 7 cm for a 5 cm tumour. This causes adequate cyto destruction of the tumour. Tumour close to vessels and biliary tree, tumour more than 3 -5 cm and multicentric tumours are difficult to manage by radiofrequency ablation. One course ablation takes around 20 minutes. It can be done percutaneously under US or CT guidance or through laparoscopy. CONTD……
� Percutaneously it can be done on outpatient basis. It can be repeated several times. Tumour less than 3 cm, tumour deep in parenchyma, tumour away from hilum is ideal for radio ablation. � Per-cutaneous ethanol or acetic acid injection: (Rule of 3 is used here- indicated in HCC not >3 cm and not >3 nodules). Ethanol injection is minimally invasive, can be injected using fine needle, and is cheaper. Local recurrence is lower with acetic acid injection than ethanol. But radiofrequency ablation has got better result than ethanol / acetic acid injection. RFA is costly and not available in many centers.
� Intra-arterial chemotherapy using Adriamycin / cisplatin/mitomycin through gastroduodenal artery. It is often given along with lipiodol to make drugs to stay longer time in the liver tissue so that better results are achieved. This regional chemotherapy is much more successful in HCC. � Intra-arterial embolisation using gelfoam, microspheres, gelatin sponge, or chemoembolisation
� Microwave or cryo ablations similar to RFA. � As it is considered that tumour tissue exclusively gets its blood supply from hepatic artery, ligation of hepatic artery can be a good palliation (to achieve tumour necrosis) for HCC. Normal tissue will still have its blood supply from portal vein. � Transarterial I 131 lipiodol, Yttrium 90 microspheres.
Adjuvant Therapy. � Systemic chemotherapy using intravenous adriamycin (doxorubicin), cisplatin, carboplatin, mitomycin C, 5 fluorouracil. � Octreotide is used along with other chemotherapeutic agents. It decreases the size of the tumour. � Neoadjuvant (preoperative) chemotherapy also practiced to increase the operability/resectability of the tumour. � Newer treatments are tried using tamoxifen, interferons, EGFR antibody, interleukins, I 131 lipiodol, Yttrium 90 microspheres, etc.
Treatment strategies for HCC � Surgical resection � Liver transplantation � Radiofrequency ablation � Percutaneous ethanol/acetic acid injection � Transarterial embolisation/chemoembolisation � Microwave/cryoablation � Transarterial radiotherapy � Transarterial Yttrium 90 microspheres/I 131 lipiodol � Hepatic artery ligation � Adjuvant systemic chemotherapy � Immunotherapy/hormone therapy/growth factors
Simple cystic disease � Liver cysts are a common coincidental finding in patients undergoing abdominal ultrasound. � Radiological findings to suggest that a cyst is simple are that it is regular, thin walled and unilocular, with no surrounding tissue response and no variation in density within the cyst cavity. � If these criteria are confirmed and the cyst is asymptomatic, no further tests or treatment are required.
� Large cysts may be associated with symptoms of abdominal discomfort possibly related to stretching of the overlying liver capsule, acute pain associated with haemorrhage in the cyst, or may present as right upper quadrant abdominal mass. � Aspiration of the cyst contents under radiological guidance provides a sample for culture, microscopy and cytology and allows the symptomatic response to cyst drainage to be assessed.
� Aspiration alone is usually associated with cyst and symptom recurrence, in which case more definitive treatment is required. � Laparoscopic deroofing is the treatment of choice for large symptomatic cysts and is associated with good long-term symptomatic relief.
Polycystic liver disease � This is a congenital abnormality associated with cyst formation within the liver and often other abdominal organs, principally the pancreas and kidney. � Those associated with renal cysts may have autosomal dominant inheritance. � The cysts are often asymptomatic and incidental findings on ultrasound. They usually have no effect on organ function and require no specific treatment. � Massive polycystic disease of the liver is rare, but can give rise to discomfort or pain. This often responds to treatment with simple analgesics.
� Severe pain often indicates haemorrhage into a cyst, which may be confirmed by ultrasound or CT scan. � Cyst discomfort that is not adequately controlled by oral analgesics may be treated by open or laparoscopic fenestration of the liver cysts, although the results are less favourable than withsimple cysts. � Ultimately, massive polycystic liver disease may require liver transplantation
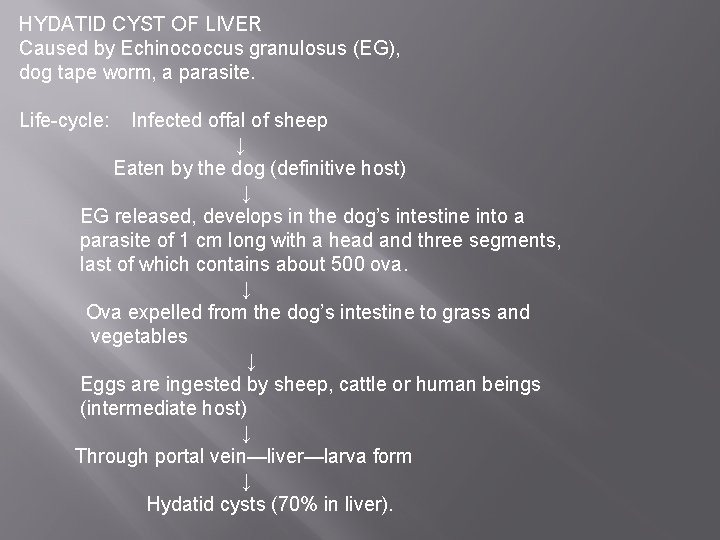
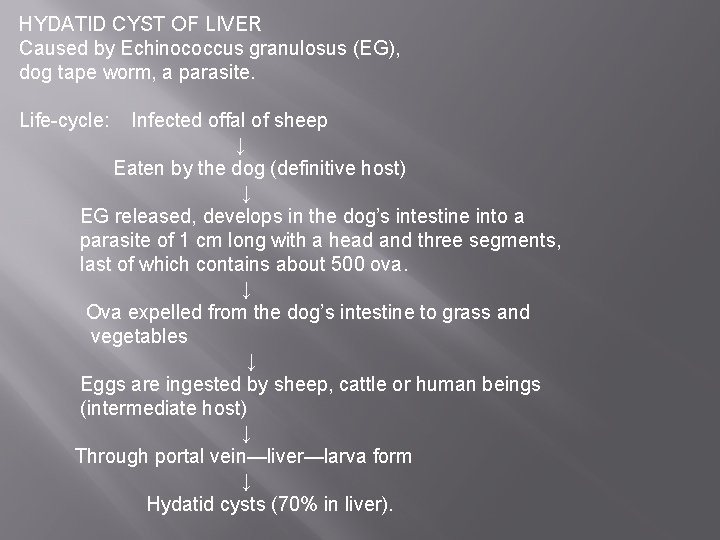
HYDATID CYST OF LIVER Caused by Echinococcus granulosus (EG), dog tape worm, a parasite. Life-cycle: Infected offal of sheep ↓ Eaten by the dog (definitive host) ↓ EG released, develops in the dog’s intestine into a parasite of 1 cm long with a head and three segments, last of which contains about 500 ova. ↓ Ova expelled from the dog’s intestine to grass and vegetables ↓ Eggs are ingested by sheep, cattle or human beings (intermediate host) ↓ Through portal vein—liver—larva form ↓ Hydatid cysts (70% in liver).
� It takes few years to evolve into a complete hydatid cyst. � Most commonly involved segment is segment VII – 27%. Commonly right lobe – 66%; both lobes in 16% and only left lobe is involved in 17%.
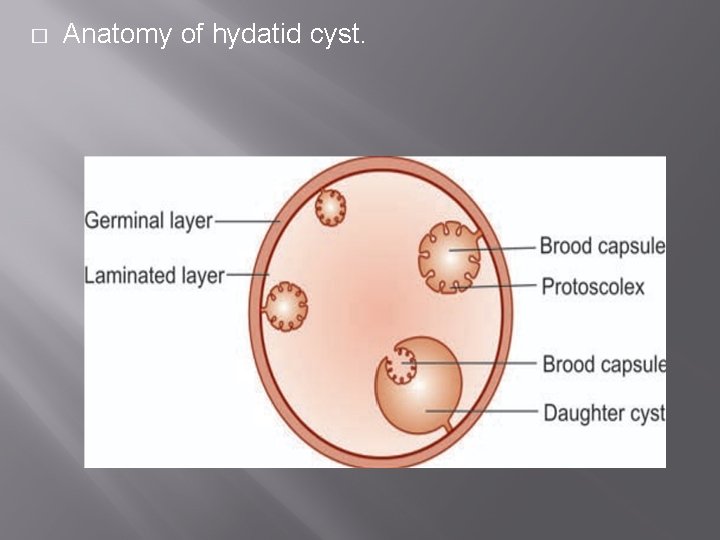
Pathology � It has got 3 layers 1. Adventitia (pseudocyst) is an inseparable fibrous tissue due to reaction of the liver to the parasite. 2. Laminated membrane (ectocyst), formed of the parasite itself is whitish, elastic, containing hydatid fluid, which can be peeled off readily from the adventitia 3. Germinal epithelium is the only living part, lining the cyst (endocyst). This layer secretes hydatid fluid, brood capsules with colices (heads of future worms).
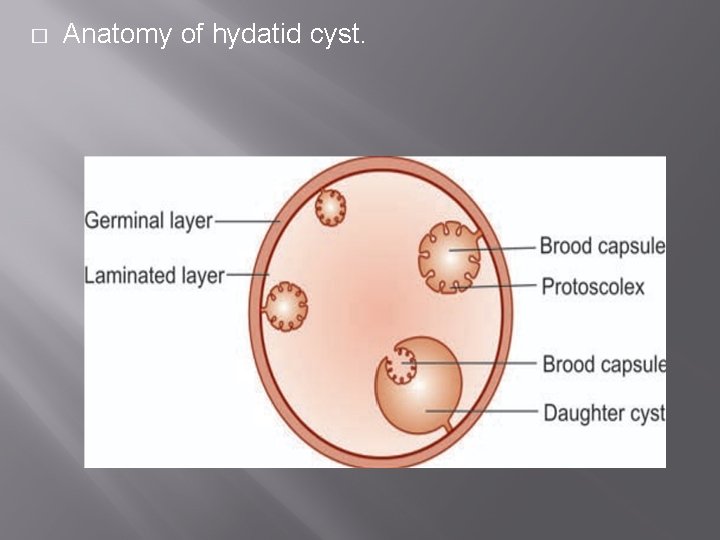
� Anatomy of hydatid cyst.
3. Germinal epithelium is the only living part, lining the cyst (endocyst). � This layer secretes hydatid fluid, brood capsules with scolices (heads of future worms). � Features of hydatid fluid • Clear • High specific gravity (1. 005 -1. 009) • Shows hooklets and scolices Once brood capsules disintegrate, it grows into daughter cysts.
Course of the Disease � The parasite may die and cyst eventually may get calcified. � Commonly cyst enlarges and is palpable per abdomen. � It may cause complications like jaundice due to pressure over biliary tree.
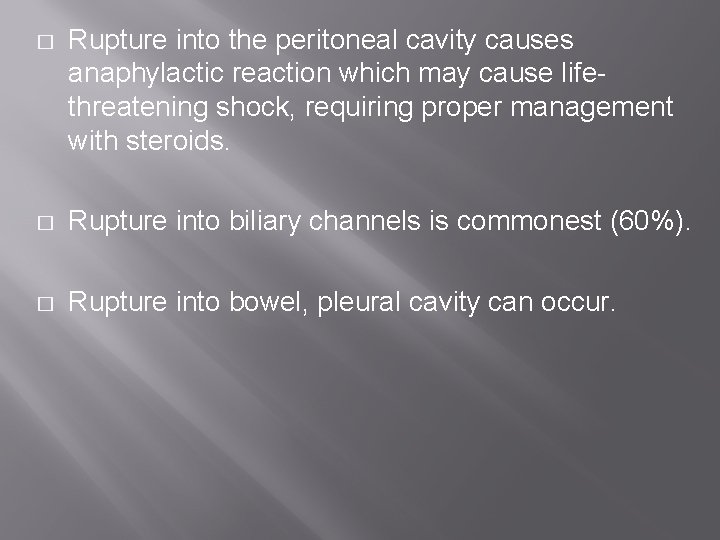
� Rupture into the peritoneal cavity causes anaphylactic reaction which may cause lifethreatening shock, requiring proper management with steroids. � Rupture into biliary channels is commonest (60%). � Rupture into bowel, pleural cavity can occur.
Secondary infection causing suppuration and septicaemia. � � Secondary cysts in the lung, spleen, mesentery, retroperitoneum and other organs can occur. � Hepatic dysfunction. � Disseminated abdominal hydatidosis can occur after silent rupture.
Clinical Features � Asymptomatic palpable liver with classical thrill (hydatid thrill) elicited by three-finger test. � Jaundice and pain. � Features of anaphylaxis. � Discomfort in right upper quadrant area; dyspepsia; hydatid cachexia in children; weight loss; fatigue; vomiting
� Occasionally splenomegaly, pleural effusion, cholangitis, allergic asthma, fever. � Camellotte sign: Following intrabiliary rupture, gas enters into cyst causing partial collapse of the cyst wall
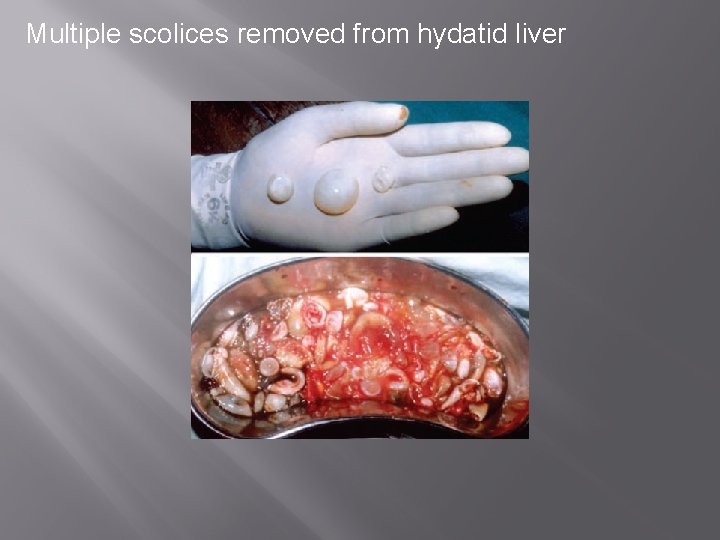
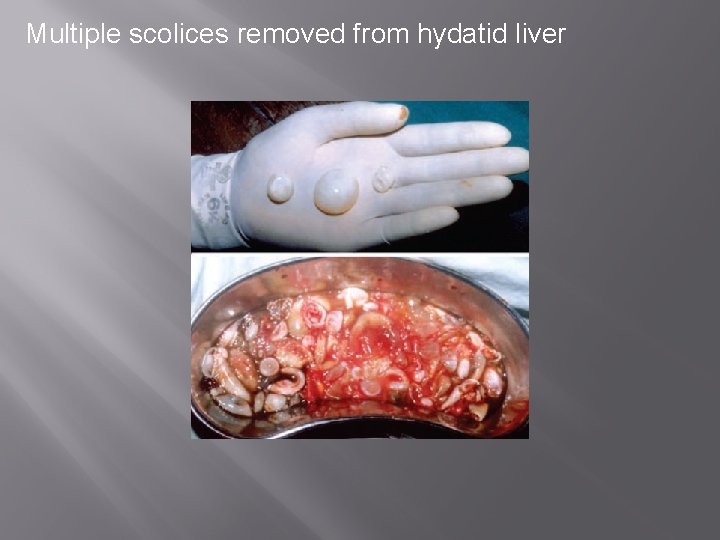
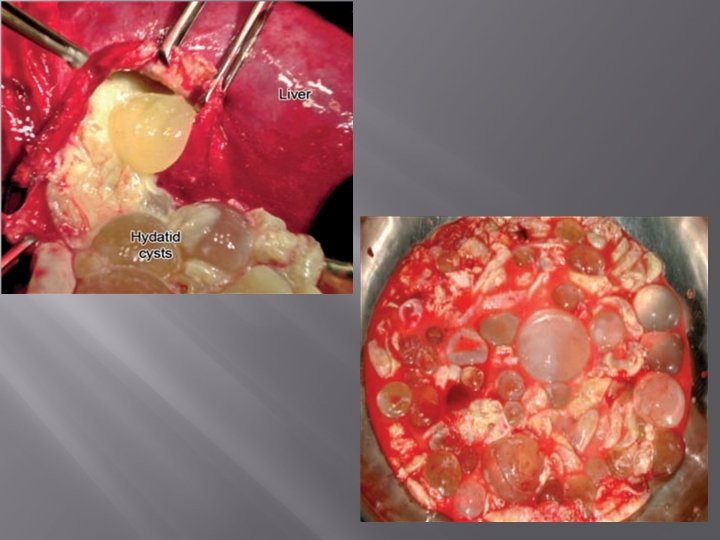
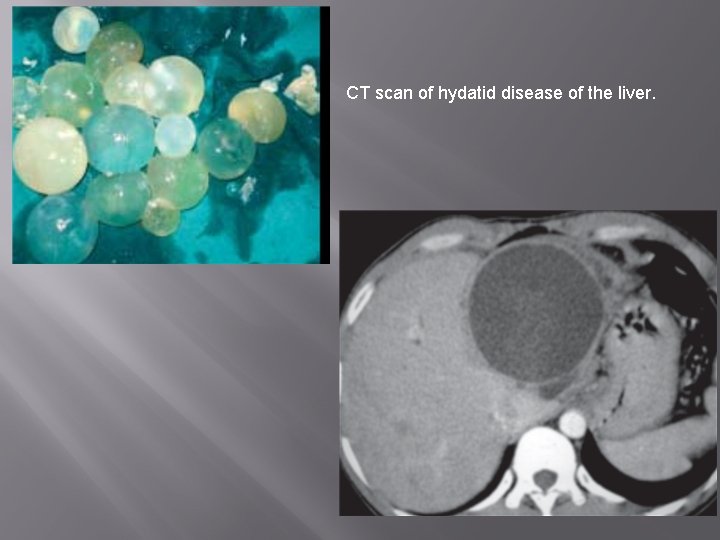
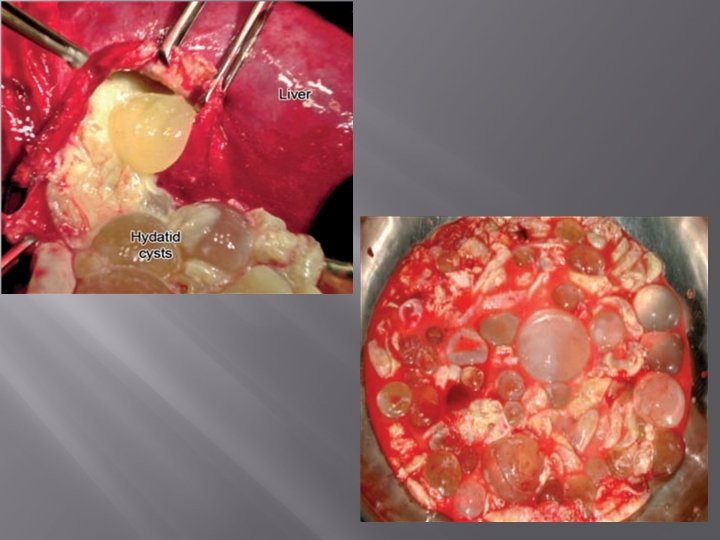
Multiple scolices removed from hydatid liver
Complications of hydatid � Anaphylaxis � Obstructive jaundice— ERCP sphincterotomy � may be needed � Infection � Calcification � Liver failure
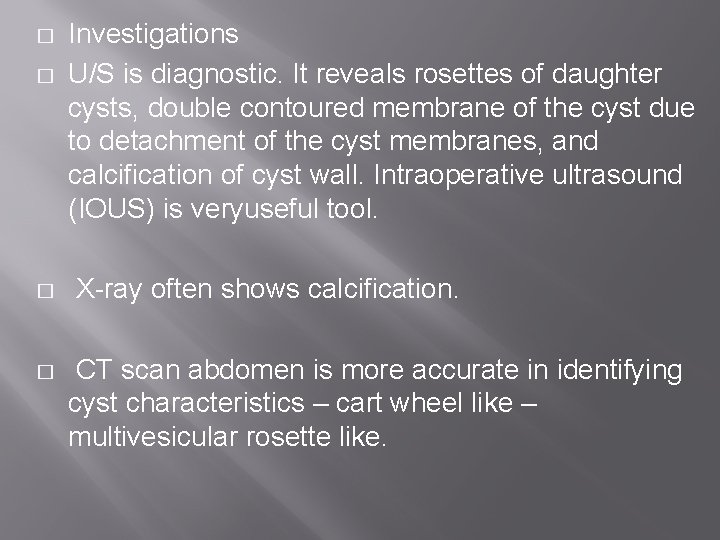
� � Investigations U/S is diagnostic. It reveals rosettes of daughter cysts, double contoured membrane of the cyst due to detachment of the cyst membranes, and calcification of cyst wall. Intraoperative ultrasound (IOUS) is veryuseful tool. X-ray often shows calcification. CT scan abdomen is more accurate in identifying cyst characteristics – cart wheel like – multivesicular rosette like.
� Primary serological tests ––ELISA; indirect haemagglutination test; latex agglutination test; immunofluorescence antibody test; immunoelectrophoresis. 80 -95% sensitivity for liver hydatid. � Secondary laboratory tests –Detection of precipitation line – arc 5; immunoblotting; polymerase chain reaction (PCR). More specific, very useful in extra hepatic hydatid disease and calcified non-fertile liver hydatid. � • Liver function tests.
� � Casoni‘s test (intradermal test – 75% sensitive); Complement fixation test – historical interest. � MRI when there is jaundice to visualise biliary tree and its relation to hydatid cyst; to find out cystobiliary communication; biliary hydatids in bile duct and hepatic ducts. � ERCP can also be done to find out the communications. Other method to find out the cysto-biliary communications is intraoperative cholangiogram. � � ERCP to find out biliary communications but not as useful as MRI.
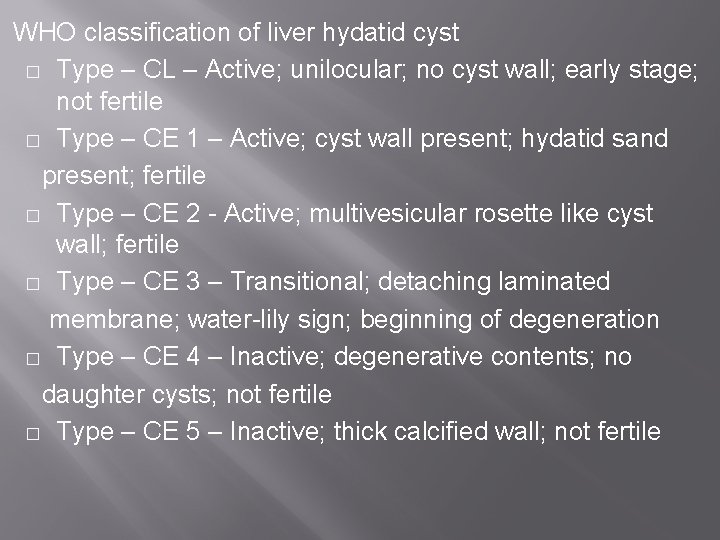
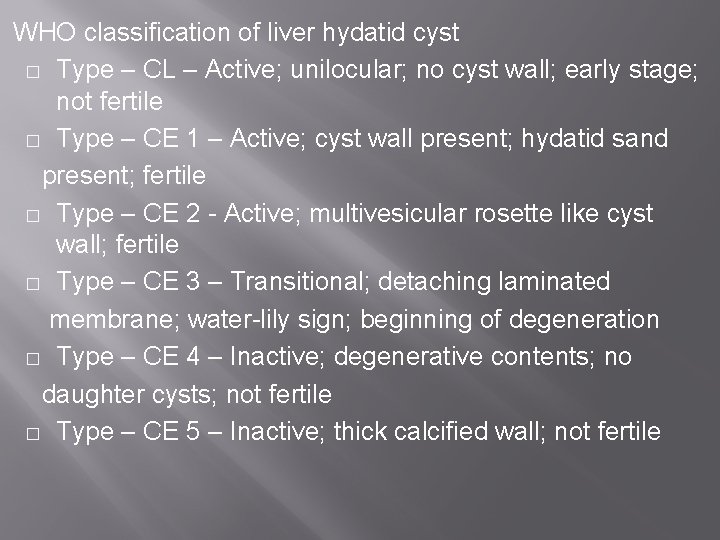
WHO classification of liver hydatid cyst � Type – CL – Active; unilocular; no cyst wall; early stage; not fertile � Type – CE 1 – Active; cyst wall present; hydatid sand present; fertile � Type – CE 2 - Active; multivesicular rosette like cyst wall; fertile � Type – CE 3 – Transitional; detaching laminated membrane; water-lily sign; beginning of degeneration � Type – CE 4 – Inactive; degenerative contents; no daughter cysts; not fertile � Type – CE 5 – Inactive; thick calcified wall; not fertile
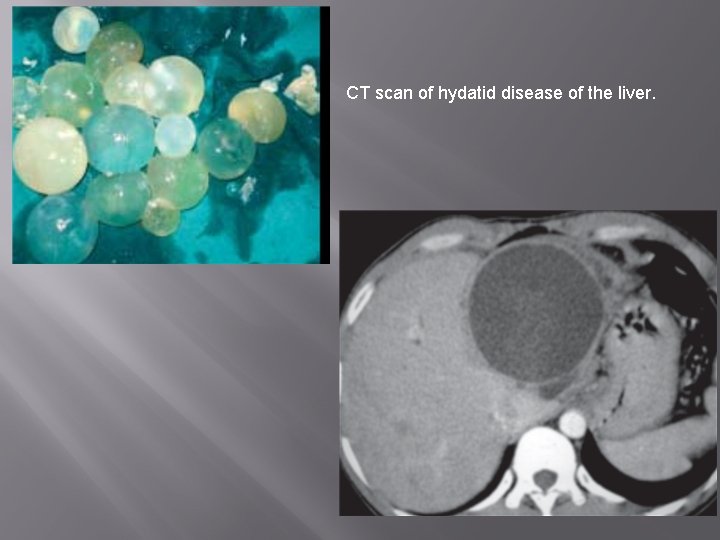
CT scan of hydatid disease of the liver.
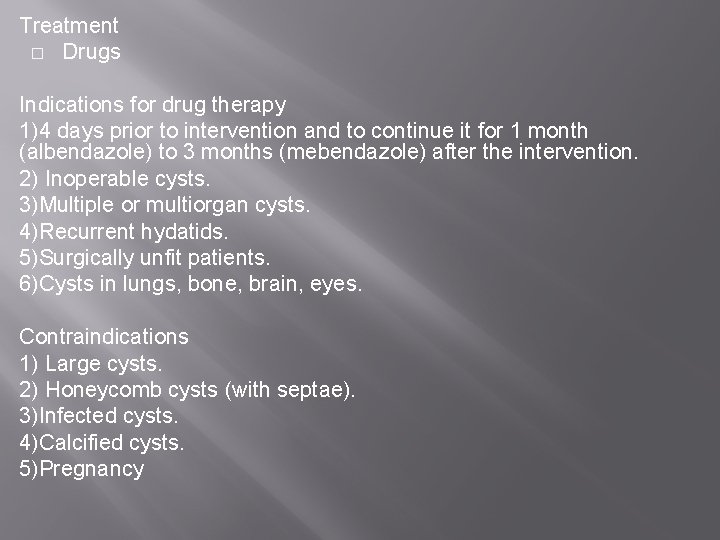
Treatment � Drugs Indications for drug therapy 1)4 days prior to intervention and to continue it for 1 month (albendazole) to 3 months (mebendazole) after the intervention. 2) Inoperable cysts. 3)Multiple or multiorgan cysts. 4)Recurrent hydatids. 5)Surgically unfit patients. 6)Cysts in lungs, bone, brain, eyes. Contraindications 1) Large cysts. 2) Honeycomb cysts (with septae). 3)Infected cysts. 4)Calcified cysts. 5)Pregnancy
PAIR – (Puncture – Aspiration – Injection. Reaspiration) Indications for PAIR • Inoperable patients • Patients who refuse surgery • CL, CE 1, CE 2 and CE 3 types /Gharbi type 1 and 2 • Relapse cysts • Infected cysts • In pregnant women; children less than 3 years • Cysts more than 5 cm in trolled by antibiotics different liver segments
Contraindications for PAIR � Inaccessible cysts � Cysts with multiple septae – honeycomb cysts � Hyperechogenic cysts � Communicating cysts to bile duct � Calcified cysts � Cysts in the lung
Technique of PAIR � Done under US / CT guidance. � Under local anaesthesia cyst is punctured using a cholangiography 22 gauge needle through thickest route/part of cyst wall. � Cyst is entered through non-dependent wall and 50% of fluid is aspirated. All multiple/daughter cysts are aspirated. Radiopaque dye is injected to see if any communications are present.
� Scolicidal agents— 15 - 20% hypertonic saline is injected into the cyst. � After 20 minutes re aspiration is done. � A sclerosant– alcohol is injected. If cyst is 6 cm or more, a drainage catheter is placed for 24 hours for complete drainage and later alcohol sclerosant is injected � PAIR has gained wide acceptance as it is safe, less invasive, and easier to do, with low morbidity and mortality.
Surgery � The abdomen is opened, and the peritoneal cavity is packed with mops [black or coloured mops are used to identify white scolices clearly so as to pick up all and prevent any spillage]. � Fluid from the cyst is aspirated and scolicidal agents (cetrimide, chlorohexidine, alcohol, hypertonic saline (15%-20%), 10% povidone iodine or H 2 O 2 ) are injected into the cyst cavity (formalin should not be used). � Hypertonic saline should be left within the cavity for 15 -20 minutes to have effective scolicidal effect.
� Detection of cystobiliary communications is very crucial as it may cause caustic sclerosing cholangitis when scolicidal agent like formalin is used. � Communicating openings may be single or multiple. � Cyst more than 10 cm is likely to have cysto-biliary communications. � Often clinically features of communications may not be present. � Preoperatively there may be recurrent cholangitis; dilated bile duct.
� Factors important are – its size; number; site; involvement of hepatic/bile ducts; liver dysfunction. � Finding of bile stained cyst on table during aspiration is highly suggestive of communication. � White mops soaked with hypertonic saline are kept in the cyst cavity and gallbladder is gently squeezed to see for the bile staining of the mop in the cavity which confirms communication � Liver resection – only occasionally segmental or hemihepatectomy is done.
Malignant hydatid disease � It is a misnomer as it is a benign condition � It is caused by Echinococcus multilocularis (Alveolaris) � It presents with multiple small cysts in both lobes of the liver, all over � It is difficult to treat, and mimics clinically and prognosis-wise to malignancy, hence the name � They die of liver failure

THANK YOU