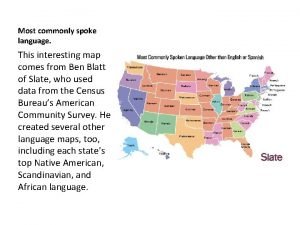
Hysterectomy Introduction Hysterectomy is the most commonly performed



- Slides: 70
Hysterectomy
Introduction • Hysterectomy is the most commonly performed gynecological surgical procedure § 600, 000 hysterectomies are performed yearly (US) § 90% done for benign conditions • Abdominal hysterectomy was more common than vaginal hysterectomy (65% vs. 35%) • Proportion of vaginal hysterectomies performed with laparoscopic assistance doubled (from 13% to 28%)
Indications • Leiomyomata • Pelvic pain • Pelvic relaxation • Abnormal uterine bleeding • Malignant and premalignant disease “In the absence of a life-threatening emergency (eg, uterine hemorrhage), the decision to proceed with hysterectomy is made mutually by the woman and her physician based upon her functional impairment, childbearing plans, response to medical therapy, discussion of alternatives, and perception that the risks of the procedure are outweighed by the expected benefits. ” Up. To. Date, March 17, 2007
Alternatives: Depend on underlying disorder • Uterine artery embolization and myomectomy may be used to treat symptomatic leiomyoma • Pain control services may be able to return patients with intractable pelvic pain to a functional status without surgery • Endometrial ablation may be an effective therapy for menorrhagia • Gn. RH analogs can help reduce discomfort associated with endometriosis • Endometrial hyperplasia can sometimes be treated medically with progestins • Conization may be adequate therapy for some women with high grade CIN/CIS
Hysterectomy Complete removal of fundus/cervix • TAH • TVH • LAVH • TLH
Hysterectomy Subtotal or supracervical hysterectomy • Result in cyclic vaginal bleeding in 7 -11% of patients • May require future resection • No difference in the rates of incontinence, constipation or measures of sexual function • Length of surgery and amount of blood lost during surgery were reduced during subtotal hysterectomy compared to total hysterectomy § No difference in transfusion rates
Hysterectomy Subtotal/supracervical hysterectomy • There was no difference in the rates of other complications, recovery from surgery, or readmission rates • Absolute contraindication to subtotal hysterectomy § presence of a malignant or premalignant condition of the uterine corpus or cervix • Extensive endometriosis is a relative contraindication § persistence of dyspareunia if the cervix is retained
Abdominal vs. Vaginal Hysterectomy • Historically, TAH has been designated as the appropriate route for more serious conditions § Abdominopelvic exploration § Procedures deemed too difficult to perform through the vagina • These traditional indications for laparotomy have been challenged
Abdominal vs. Vaginal Hysterectomy Uterine mobility • Prospective study • All patients without prolapse undergoing hysterectomy for benign conditions were included • There were 97 abdominal and 175 vaginal procedures, with no significant differences in patient characteristics • The frequency of complications was low and similar in both groups Varma, R, Tahseen, S, Lokugamage, AU, Kunde, D. Vaginal route as the norm when planning hysterectomy for benign conditions: change in practice. Obstet Gynecol 2001; 97: 613.
Abdominal vs. Vaginal Hysterectomy Uterine size • Prospective study evaluated vaginal hysterectomy outcome in 204 consecutive women with a myomatous uterus weighing 280 to 2000 g. • Vaginal morcellation was performed in all cases § no patient had uterovaginal prolapse • Four patients underwent conversion to a laparoscopic procedure for the completion of the hysterectomy § two of these ultimately required laparotomy • Adnexectomy was successfully performed vaginally in 91% of patients in whom it was indicated • Traditional uterine weight criteria for exclusion of the vaginal approach may not be valid Sizzi, O, Paparella, P, Bonito, C, et al. Laparoscopic assistance after vaginal hysterectomy and unsuccessful access to the ovaries or failed uterine mobilization: changing trends. JSLS 2004; 8: 339.
Abdominal vs. Vaginal Hysterectomy Prior cesarean delivery - concerns about scarring • Retrospective review compared vaginal hysterectomy outcome of 220 women with prior cesarean deliver (one or more) to 200 patients with no previous pelvic surgery • Only 3 of the 220 patients had inadvertent urological trauma intraoperatively • Factors favoring a successful vaginal approach were only one previous cesarean, a freely mobile uterus, previous vaginal delivery, uterus not exceeding 10 -12 weeks size, and absence of adnexal pathology • Infection following the previous cesarean was an unfavorable prognostic factor due to an increased risk of dense adhesions between the bladder and cervix Sheth, SS, Malpani, AN. Vaginal hysterectomy following previous cesarean section. Int J Gynaecol Obstet 1995; 50: 165.
Abdominal vs. Vaginal Hysterectomy Nulliparity • Vaginal hysterectomy outcome in 52 nulliparous and 293 primiparous or multiparous women was compared prospectively • The mean operative time was significantly longer in nulliparous patients (95 vs. 80 minutes) • Vaginal hysterectomy was successfully performed in 50/52 of the nulliparous and 292/293 of the parous patients • This suggests that nulliparous women can be considered candidates for vaginal hysterectomy Agostini, A, Bretelle, F, Cravello, L, et al. Vaginal hysterectomy in nulliparous women without prolapse: a prospective comparative study. BJOG 2003; 110: 515.
Abdominal vs. Vaginal Hysterectomy Need for oophorectomy • Multiple clinical trials have shown that as many as 95% of ovaries can be removed vaginally, with or without laparoscopic assistance* Obesity • Exposure of the operative field can be difficult in obese women, whether an abdominal or vagina route is taken • Vaginal approach is suggested for obese women requiring hysterectomy § associated with lower postoperative morbidity than abdominal hysterectomy** *Davies, A, O'Connor, H, Magos, AL. A prospective study to evaluate oophorectomy at the time of vaginal hysterectomy. Br J Obstet Gynaecol 1996; 103: 915. **Isik-Akbay, EF, Harmanli, OH, Panganamamula, UR, et al. Hysterectomy in obese women: a comparison of abdominal and vaginal routes. Obstet Gynecol 2004; 104: 710.
Abdominal Hysterectomy • Patient Preparation § For patients at risk, thromboembolism prophylaxis is begun preoperatively, or pneumatic compression boots are applied in the OR § Prophylactic antibiotic agent should be given as a single dose 30 minutes prior to the incision • Incision choice - transverse or vertical § Need for exploration of the upper abdomen § Size of the uterus § Presence of prior incisions § Desired cosmetic results
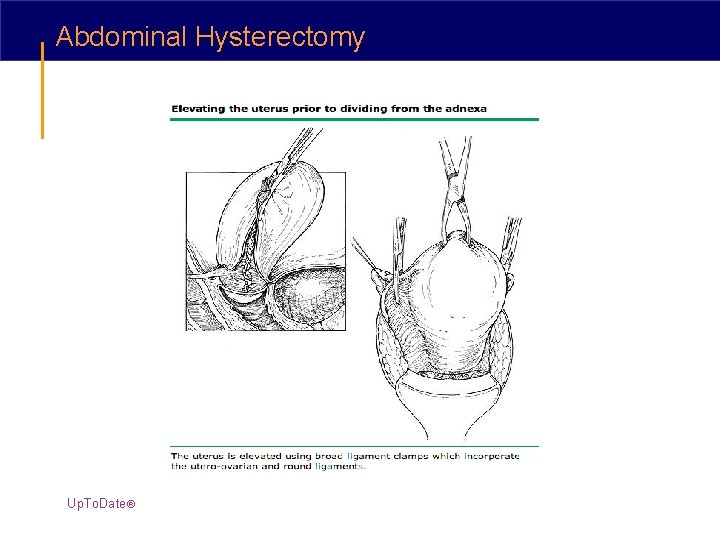
Abdominal Hysterectomy - the Procedure • The peritoneal cavity is entered and the upper abdomen and pelvis explored § unexpected pathology § confirm suspected pathological findings § cytologic sampling of peritoneal fluid or peritoneal washings if indicated • Exposure - When positioning retractors, it is important to avoid placing the lateral blades over the femoral nerves since this can lead to a peripheral neuropathy § O'Connor-O'Sullivan § Balfour § Bookwalter
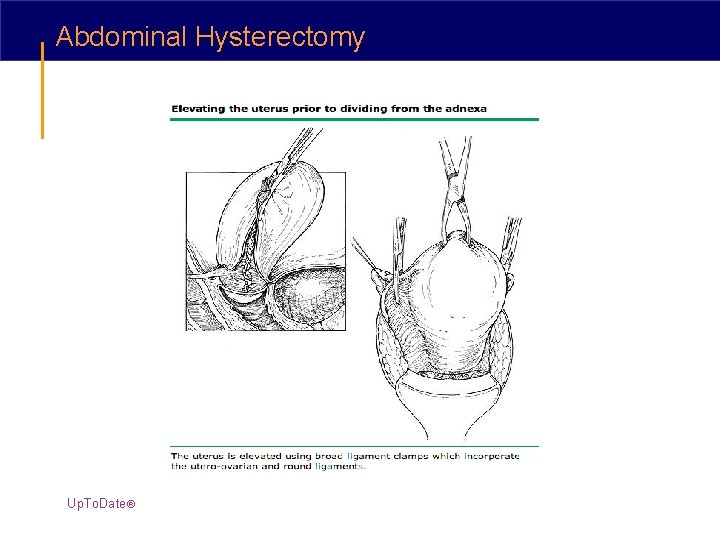
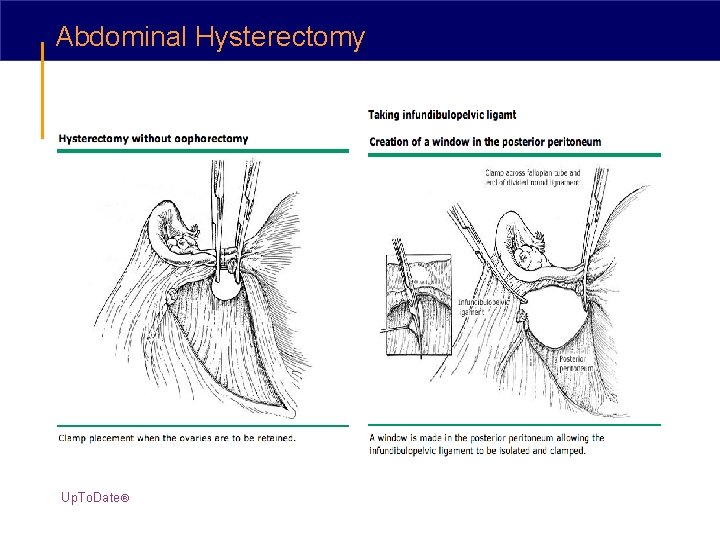
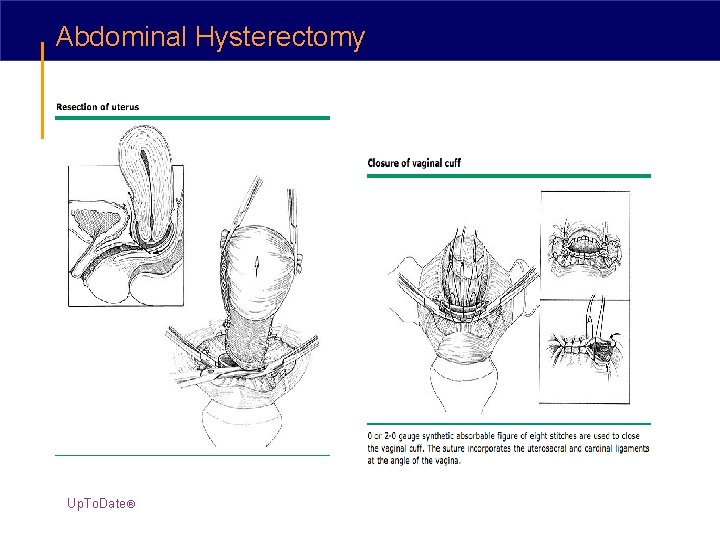
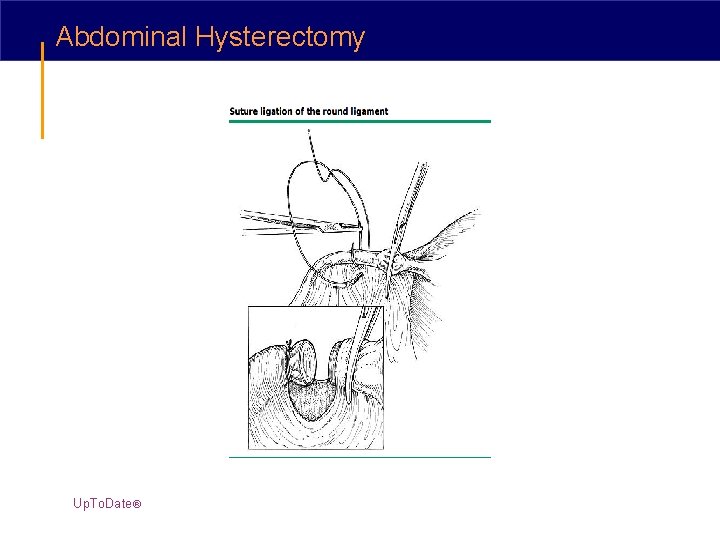
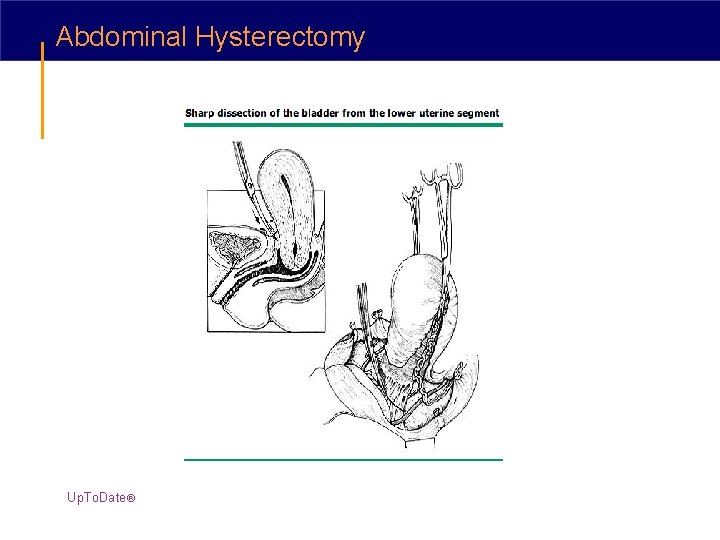
Abdominal Hysterectomy Up. To. Date®
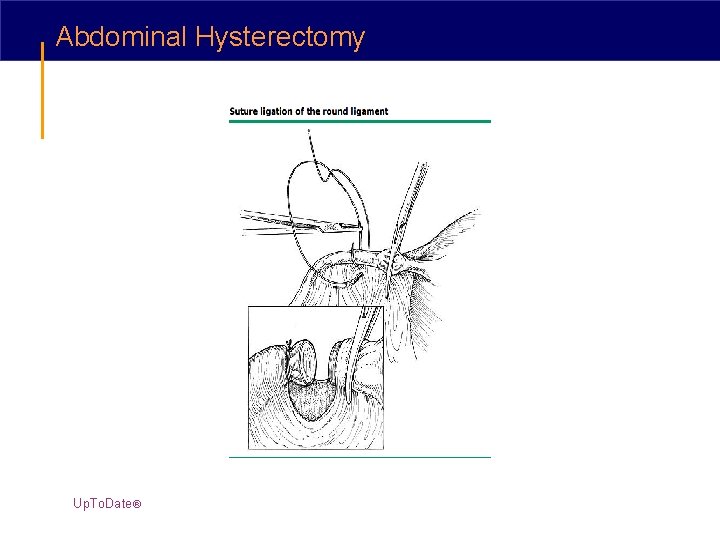
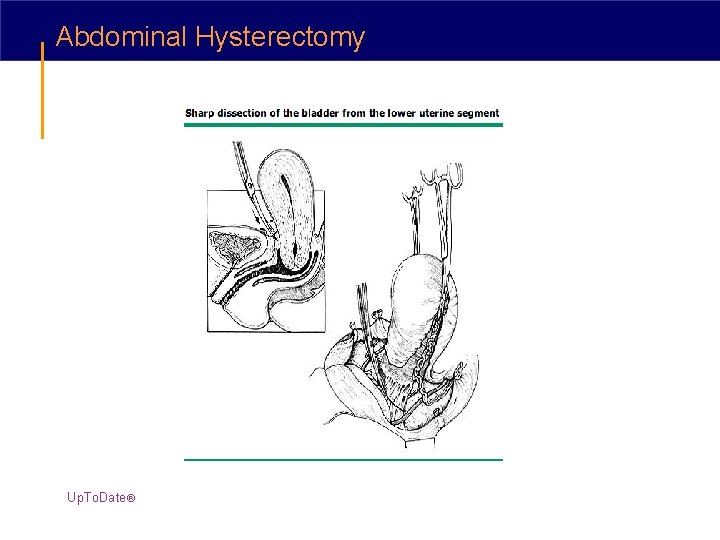
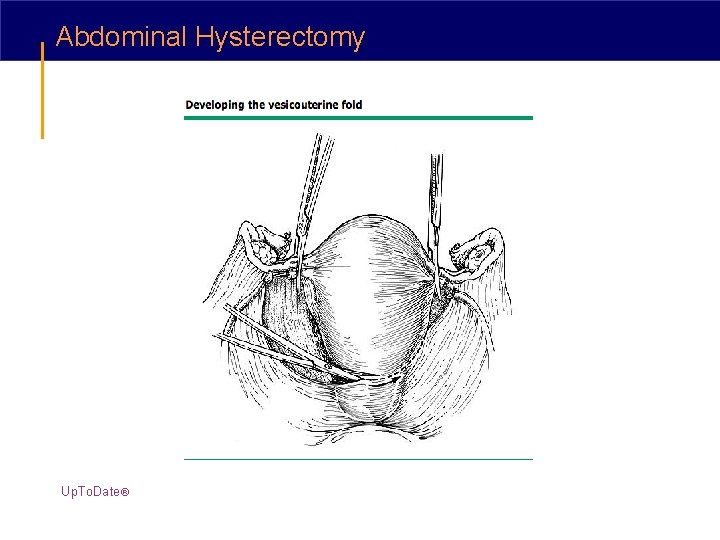
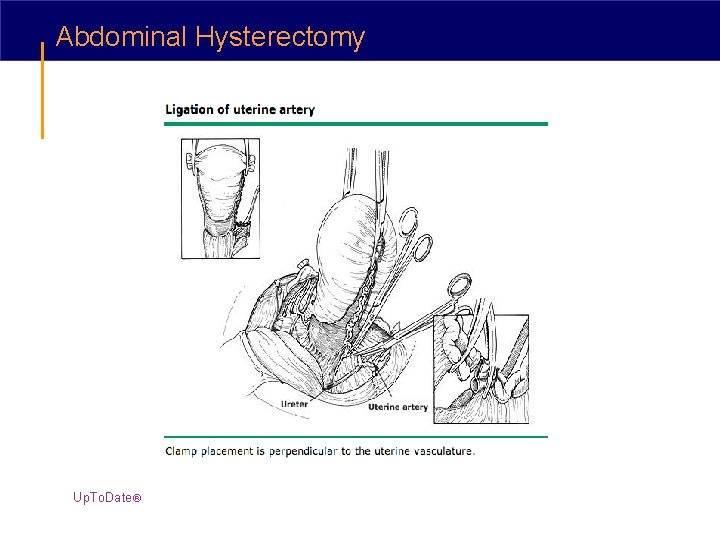
Abdominal Hysterectomy Up. To. Date®
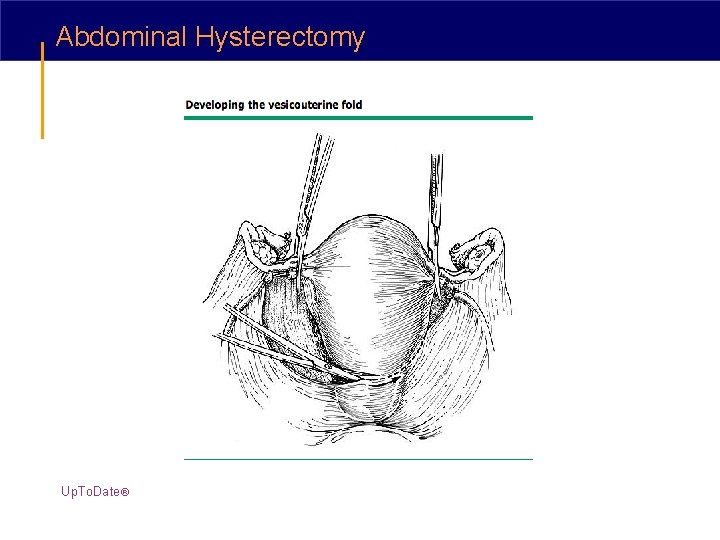
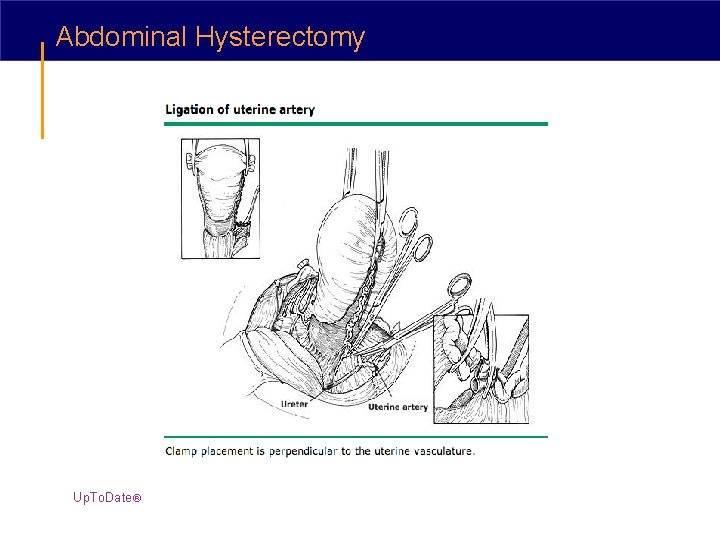
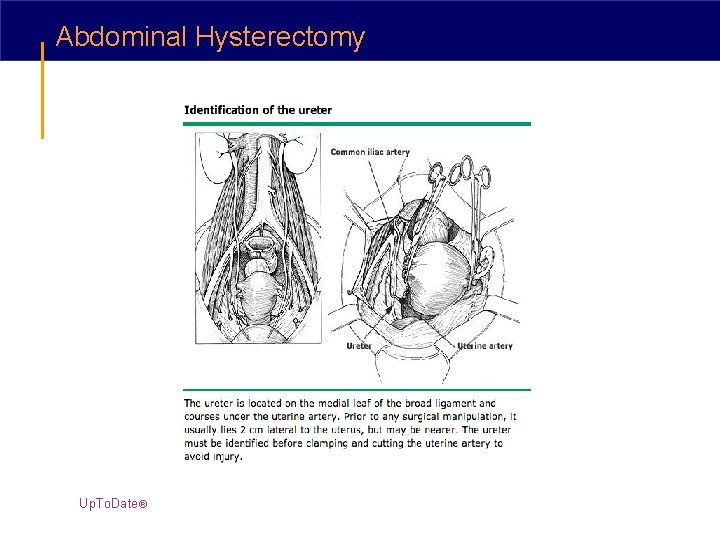
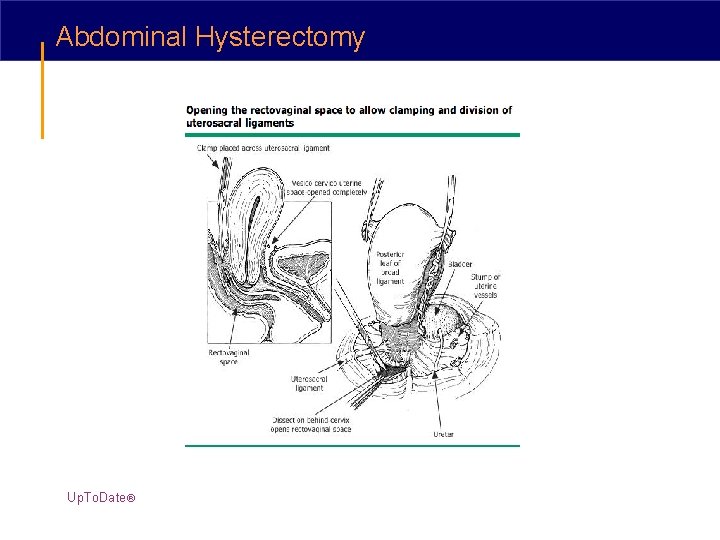
Abdominal Hysterectomy Up. To. Date®
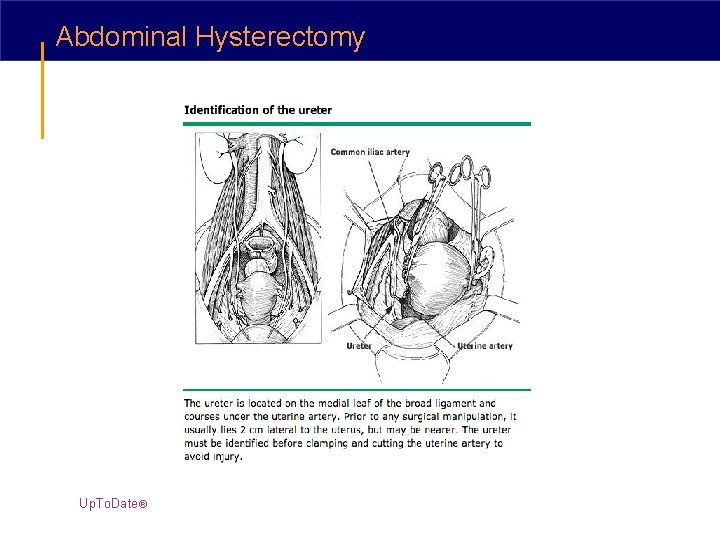
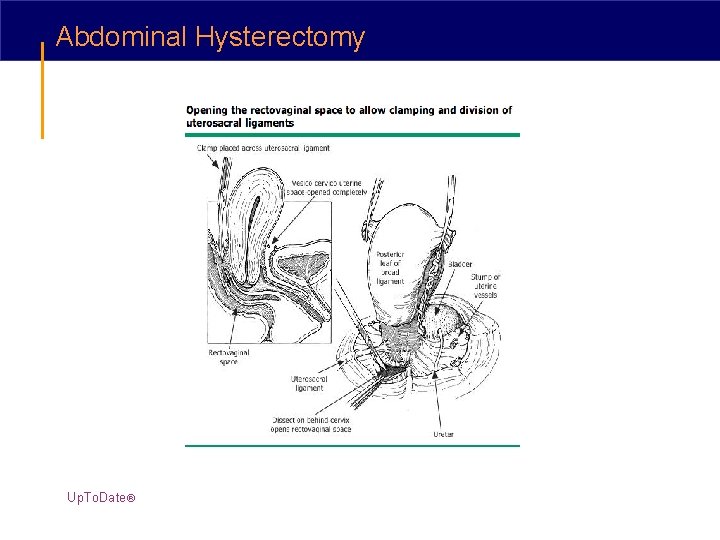
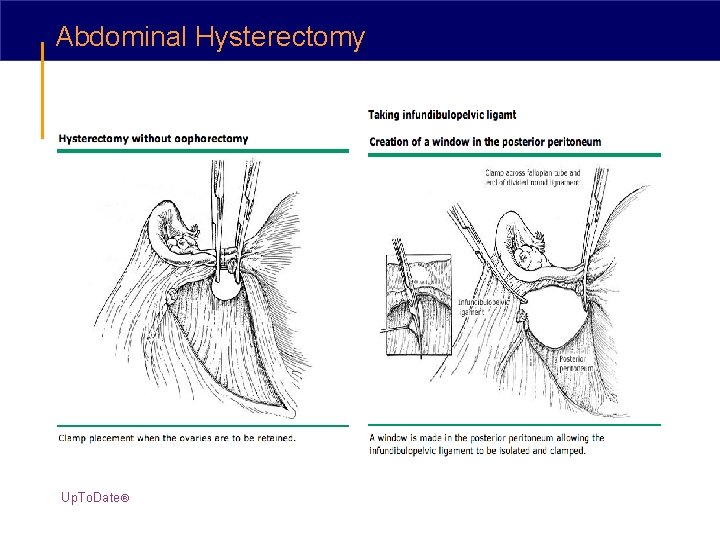
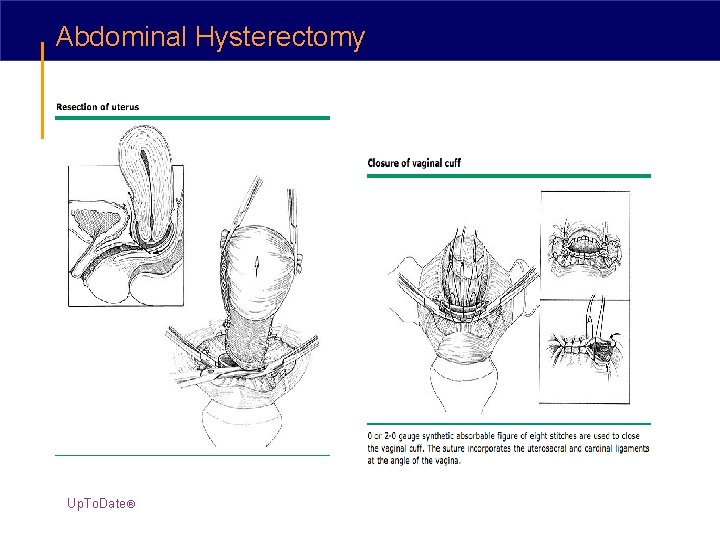
Abdominal Hysterectomy Up. To. Date®
Abdominal Hysterectomy Up. To. Date®
Abdominal Hysterectomy Up. To. Date®
Abdominal Hysterectomy Up. To. Date®
Abdominal Hysterectomy Up. To. Date®
Abdominal Hysterectomy Up. To. Date®
Abdominal Hysterectomy - the Procedure Post-Op care • Not necessary to leave a bladder catheter in place postoperatively • IV fluids for the first 24 hours to ensure that the patient remains well hydrated • Early feeding of a regular diet can stimulate the bowel and decrease the length of hospitalization* • Deep breathing to prevent atelectasis • Ambulation is encouraged • Intermittent compression boots • Adequate control of postoperative pain *Fanning, J, Andrews, S. Early postoperative feeding after major gynecologic surgery: Evidence-based scientific medicine. Am J Obstet Gynecol 2001; 185: 1.
Post-op Abdominal Hysterectomy • Walking and stair climbing are encouraged • Tub baths or showers are OK • Avoid heavy lifting (>20 pounds of weight from the floor) for 4 -6 weeks to minimize stress on the healing fascia • Vaginal intercourse is also discouraged 4 -6 weeks to allow the vaginal cuff to heal completely • Driving should be avoided until full mobility returns and opioid analgesia is no longer required • May return to work as soon as she has regained sufficient stamina and mobility
Vaginal Hysterectomy • A prophylactic antibiotic agent should be given as a single dose 30 minutes prior to the first incision for vaginal hysterectomy § cefazolin, cefoxitin, and cefuroxime § Metronidazole (500 mg IV) may be used in patients with cephalosporin allergies • A course of appropriate preoperative antibiotics in women with bacterial vaginosis can reduce the frequency of cuff infection

Vaginal Hysterectomy • Patient positioning - dorsal lithotomy • Bimanual pelvic examination is performed § assess uterine mobility and descent § confirm that no unsuspected adnexal pathology is found • A bladder catheter may be inserted § some surgeons believe that a distended bladder helps with recognition of a bladder injury and thus do not use a catheter
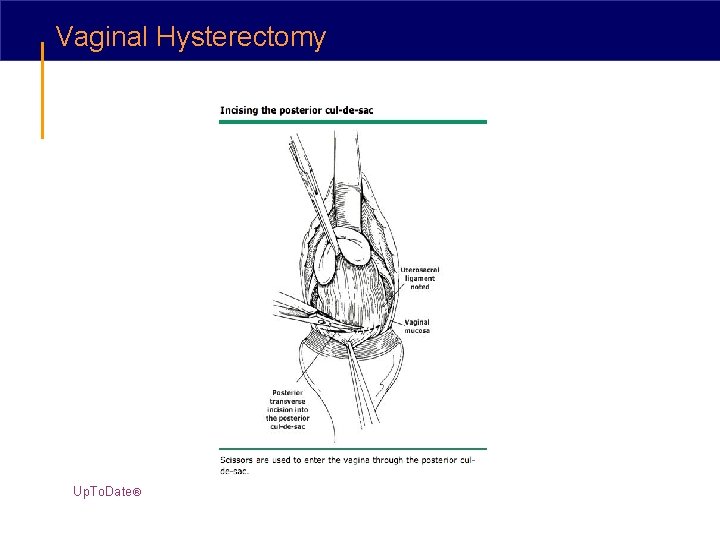
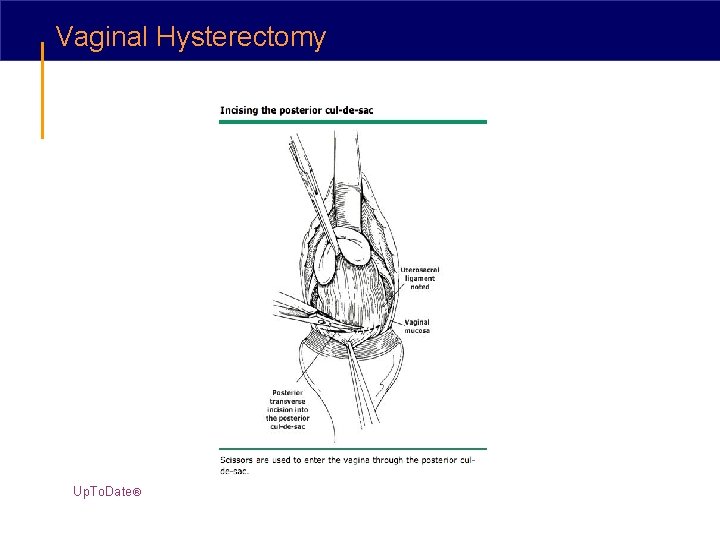
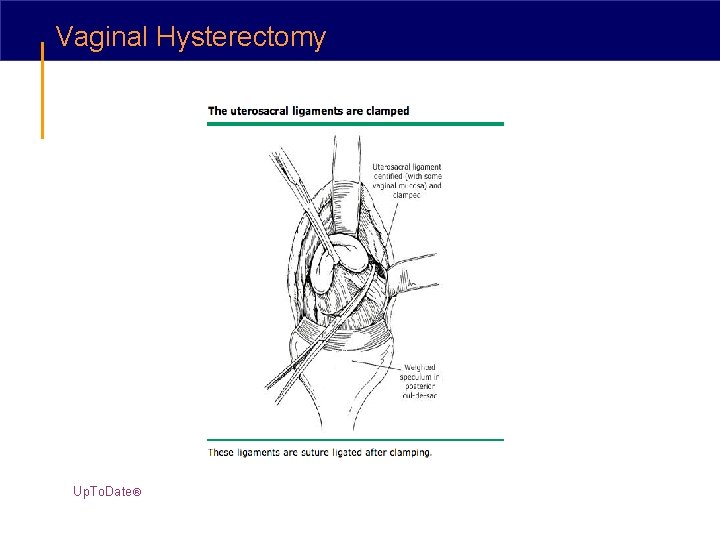
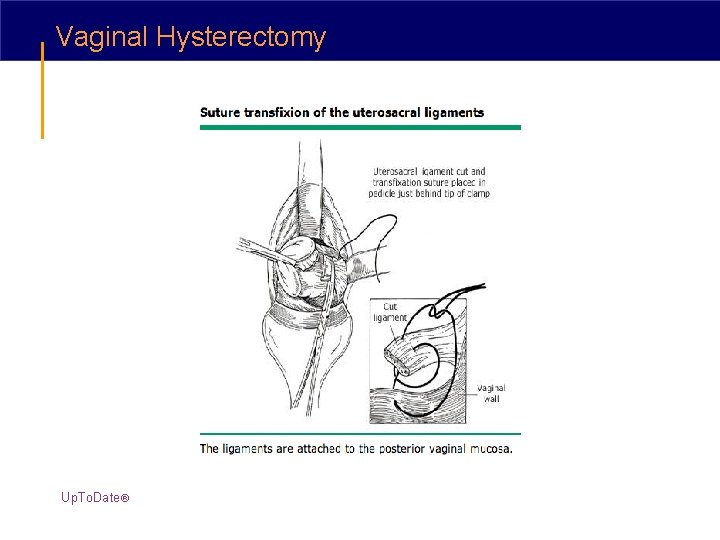
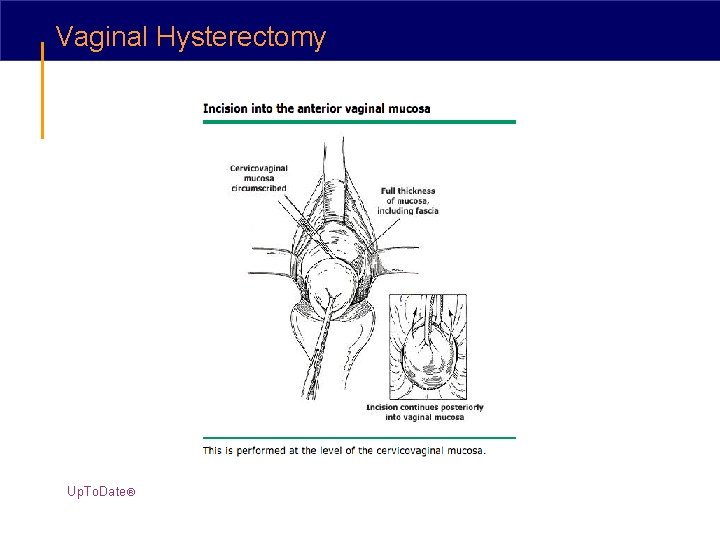
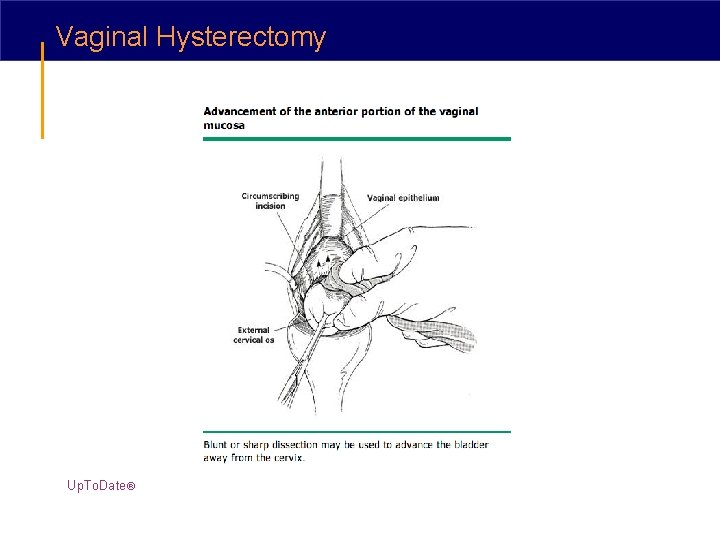
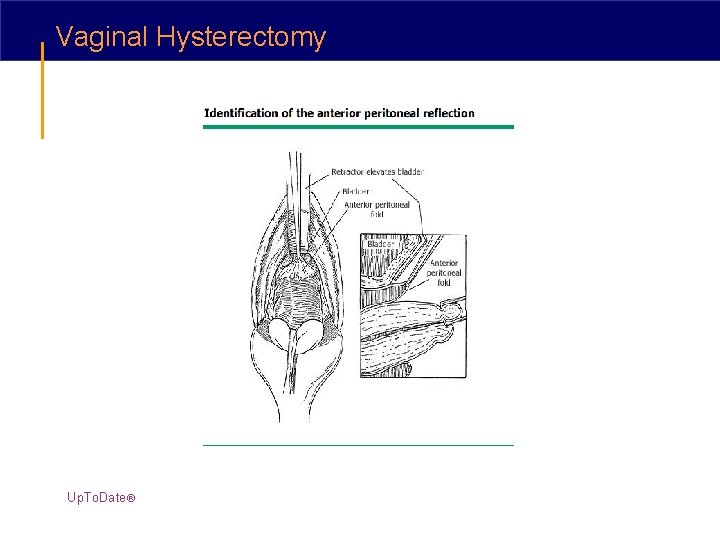
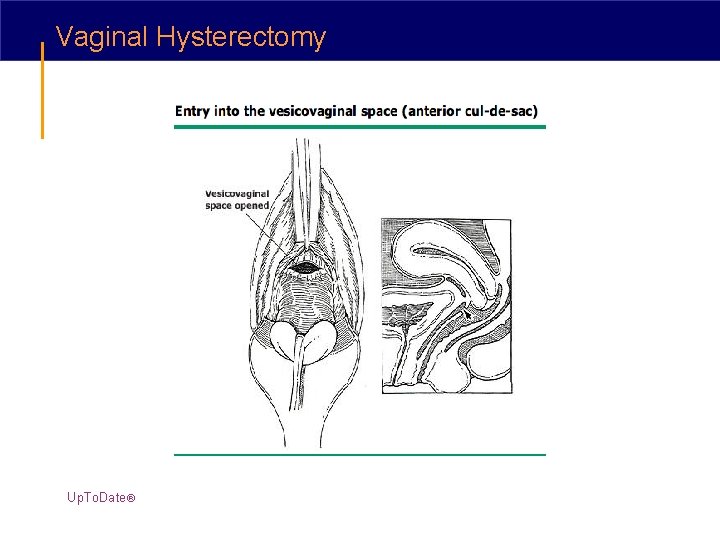
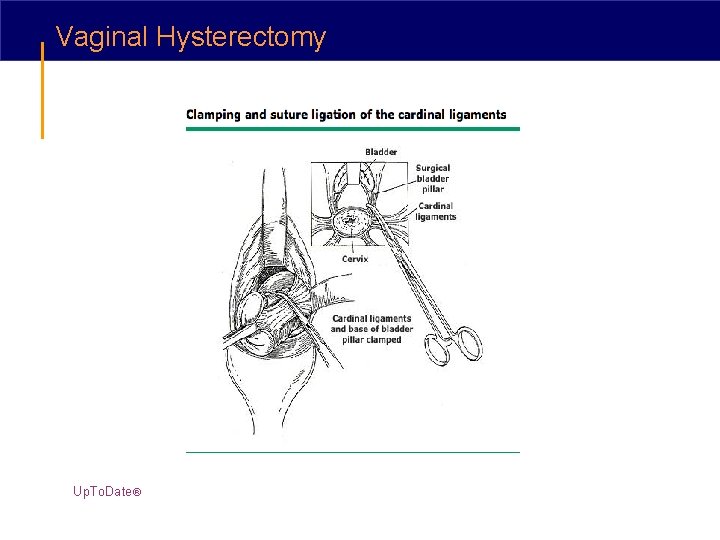
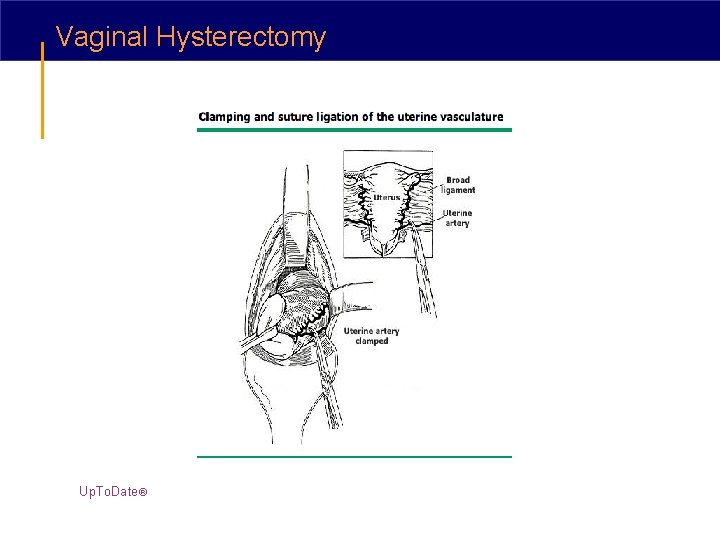
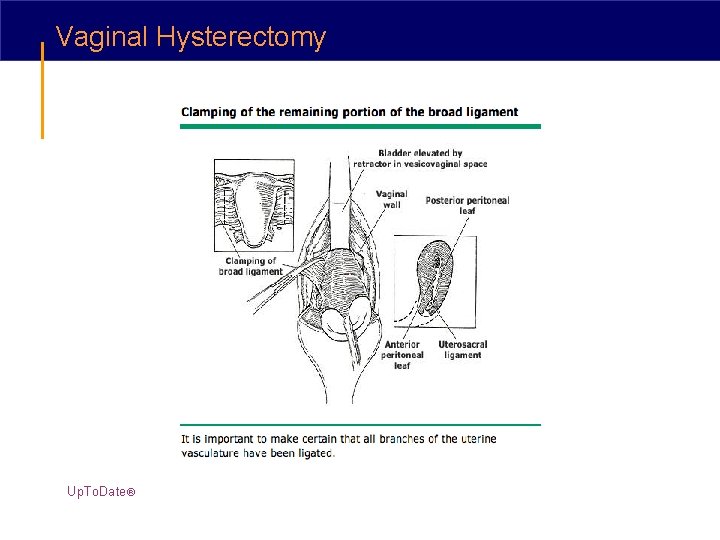
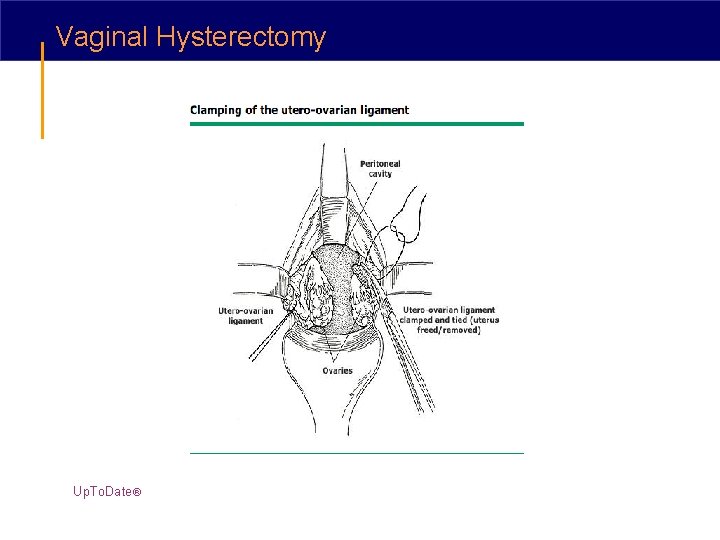
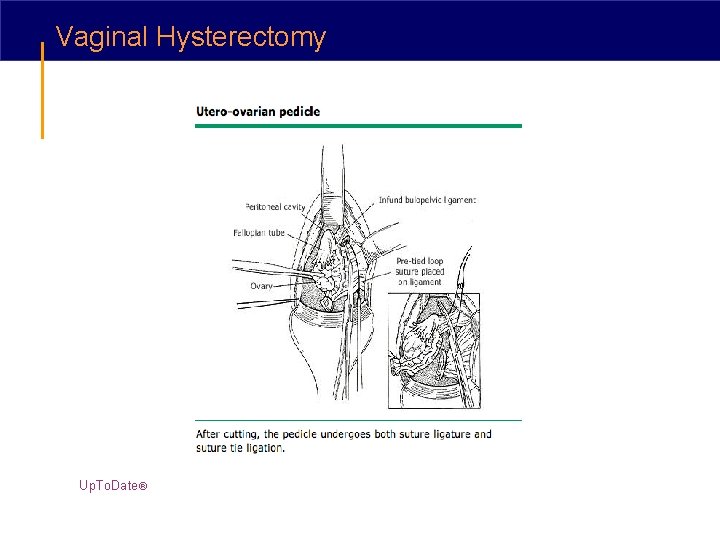
Vaginal Hysterectomy Up. To. Date®
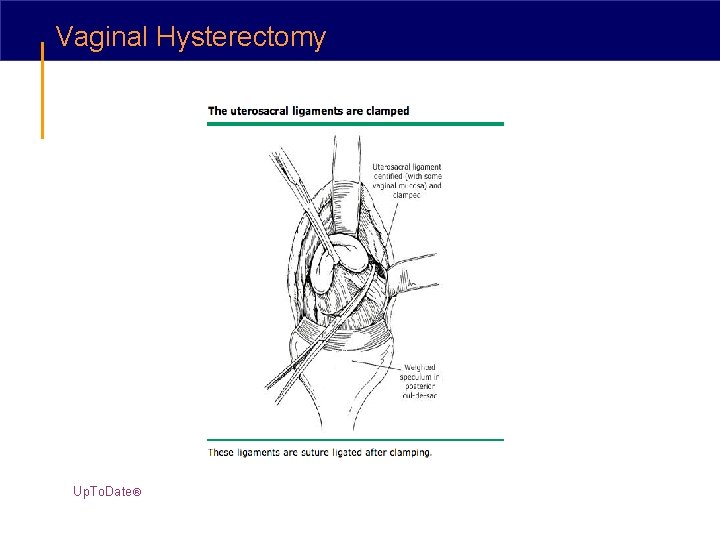
Vaginal Hysterectomy Up. To. Date®
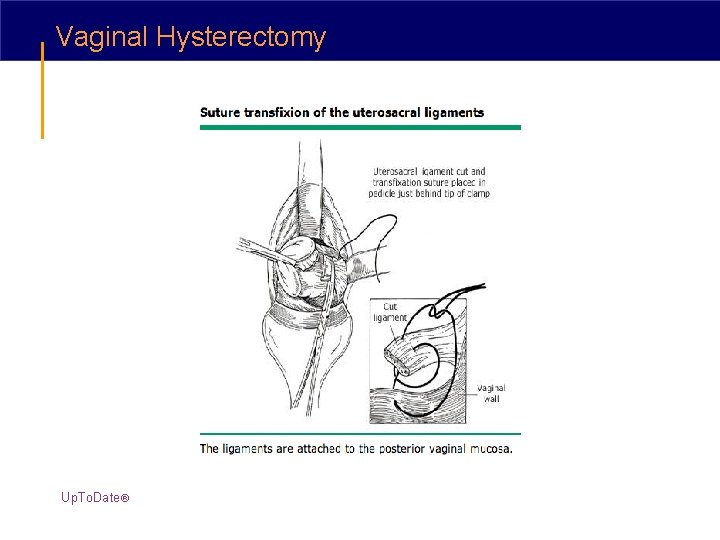
Vaginal Hysterectomy Up. To. Date®
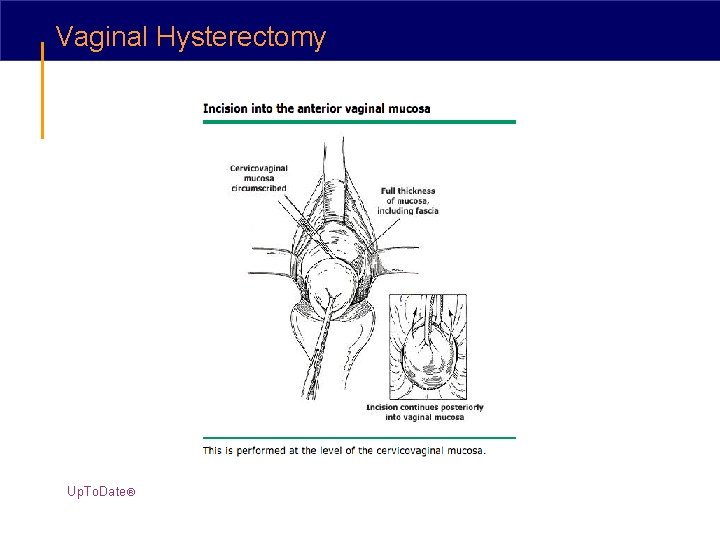
Vaginal Hysterectomy Up. To. Date®
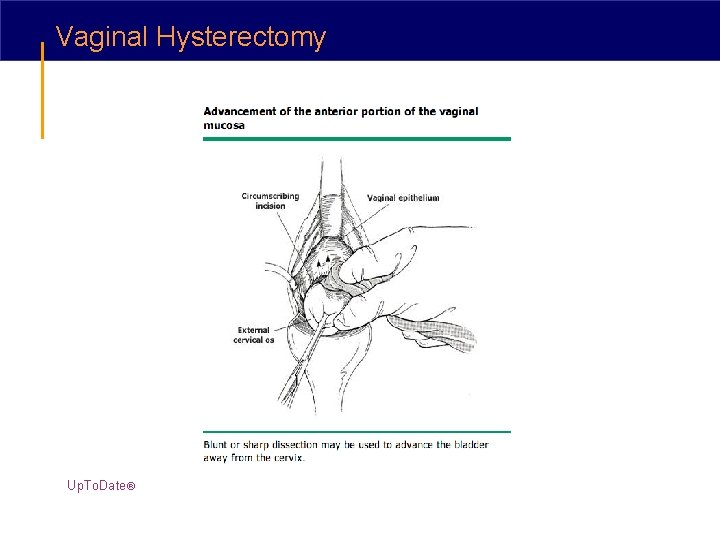
Vaginal Hysterectomy Up. To. Date®
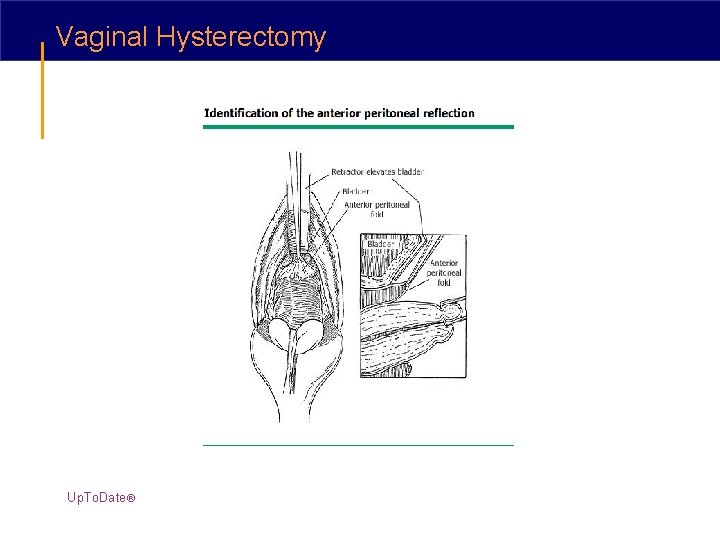
Vaginal Hysterectomy Up. To. Date®
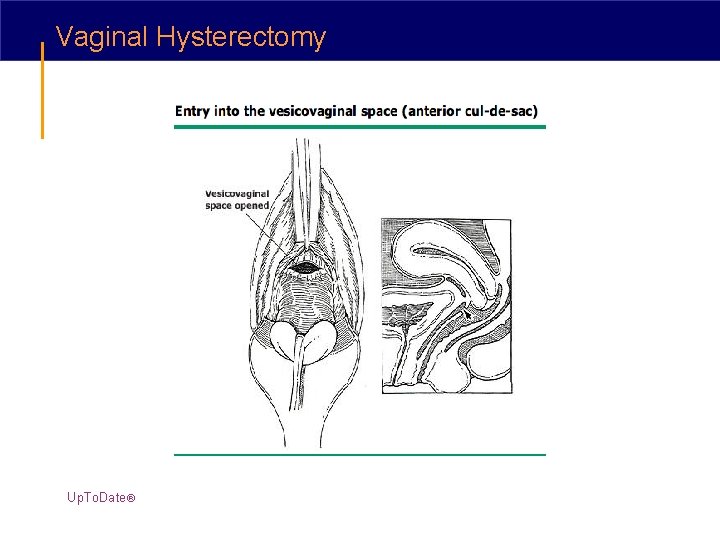
Vaginal Hysterectomy Up. To. Date®
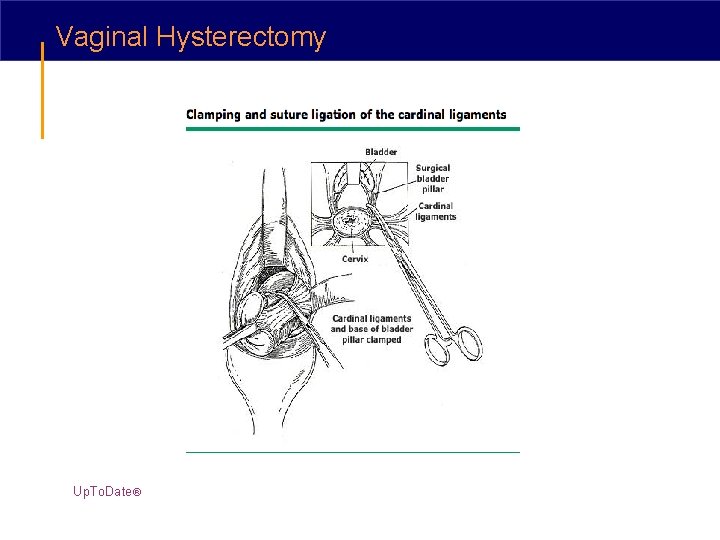
Vaginal Hysterectomy Up. To. Date®
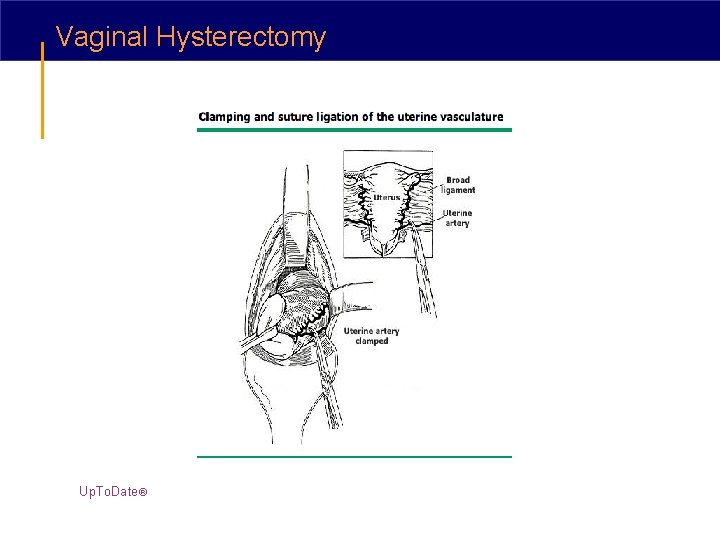
Vaginal Hysterectomy Up. To. Date®
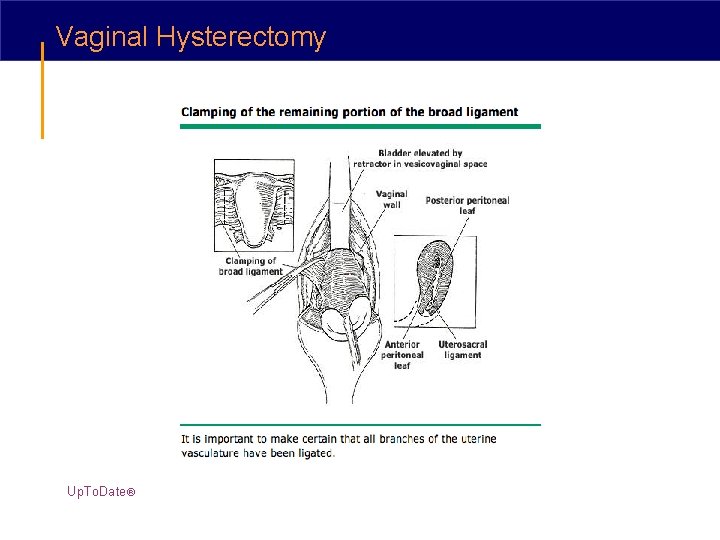
Vaginal Hysterectomy Up. To. Date®

Vaginal Hysterectomy Up. To. Date®
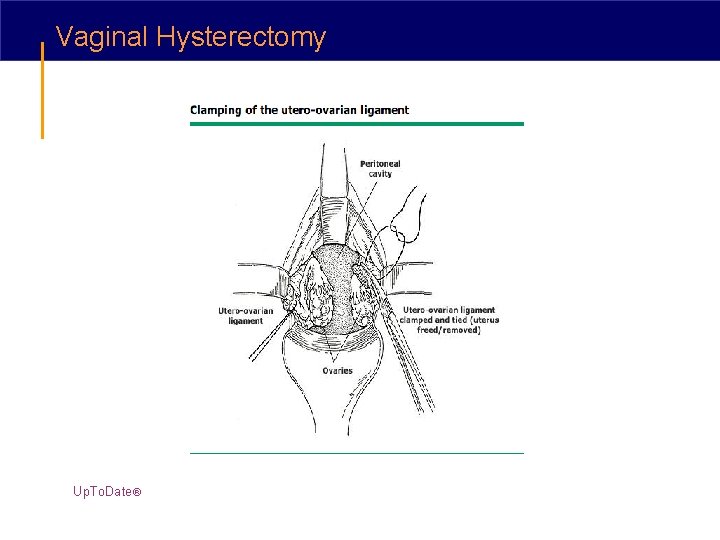
Vaginal Hysterectomy Up. To. Date®
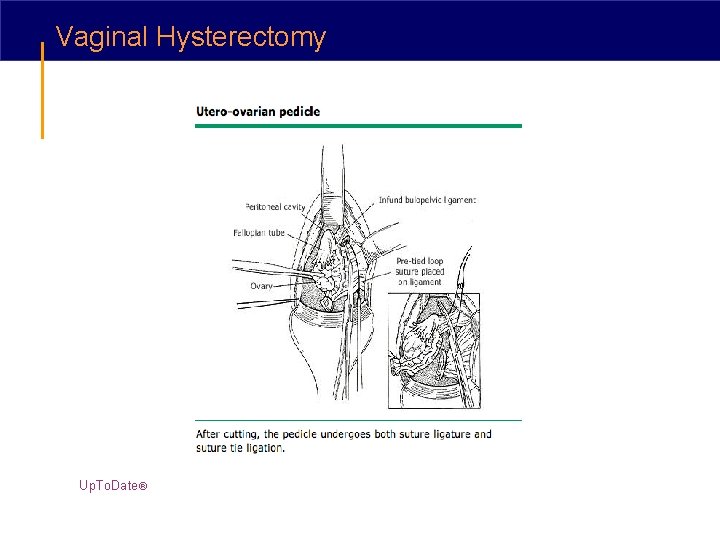
Vaginal Hysterectomy Up. To. Date®
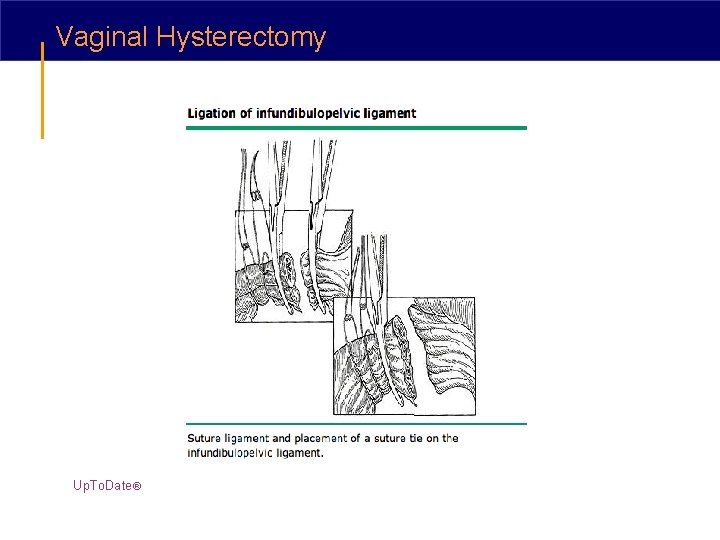
Vaginal Hysterectomy Up. To. Date®
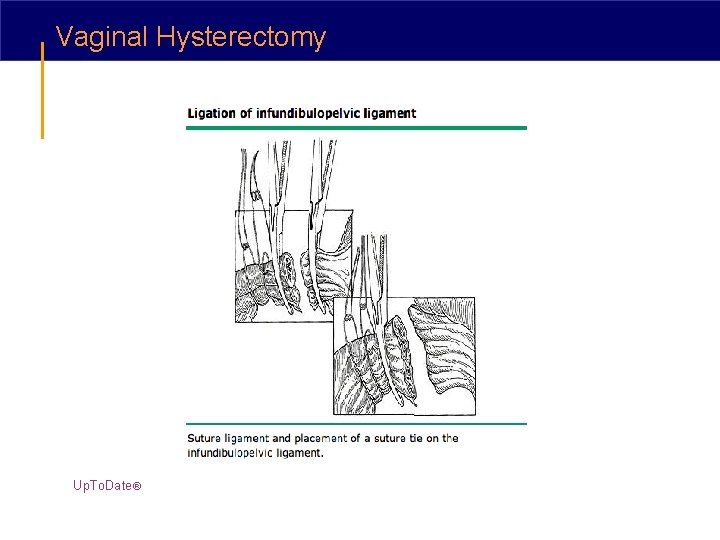
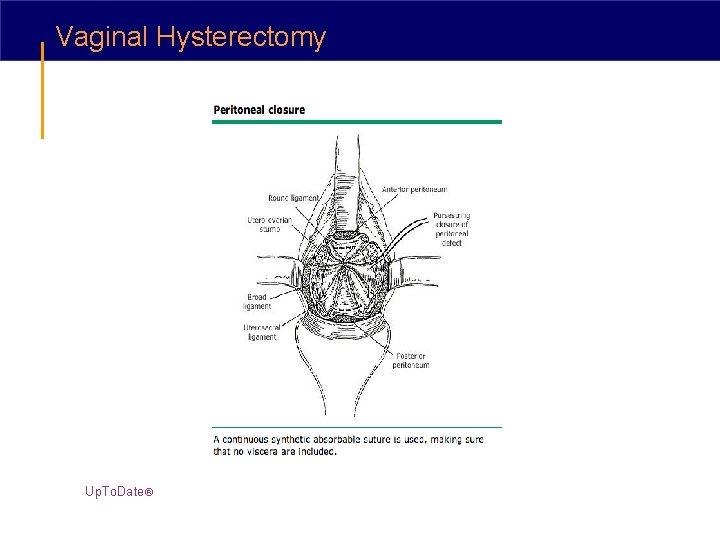
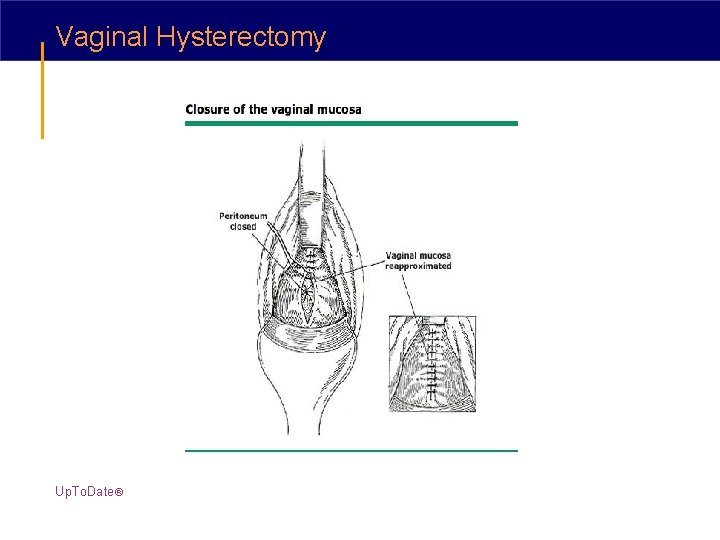
Vaginal Hysterectomy Up. To. Date®
Vaginal Hysterectomy Up. To. Date®
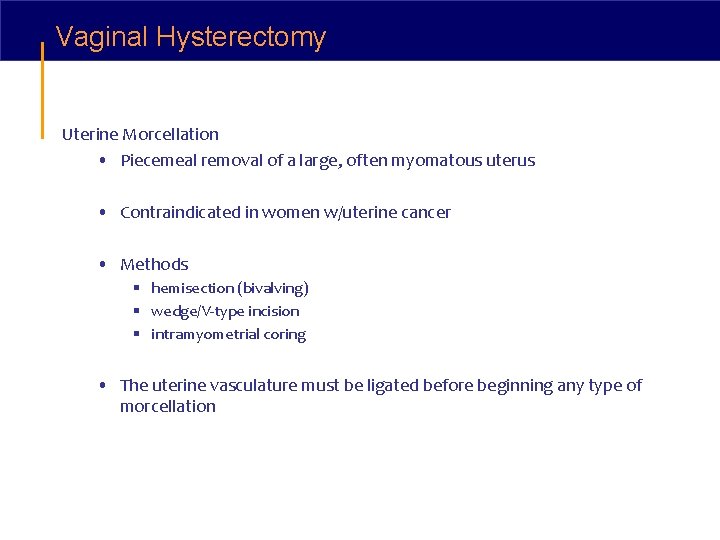
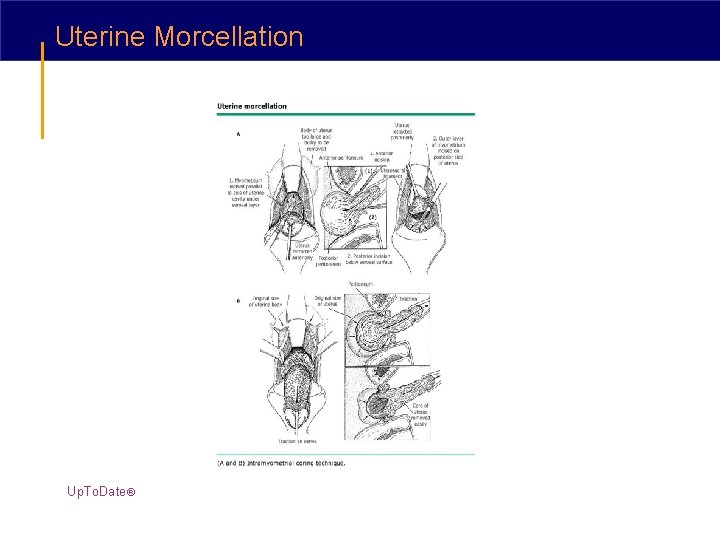
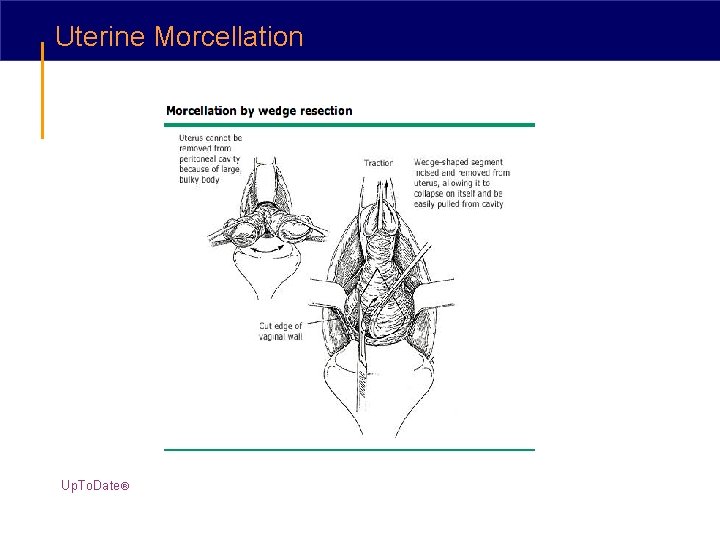
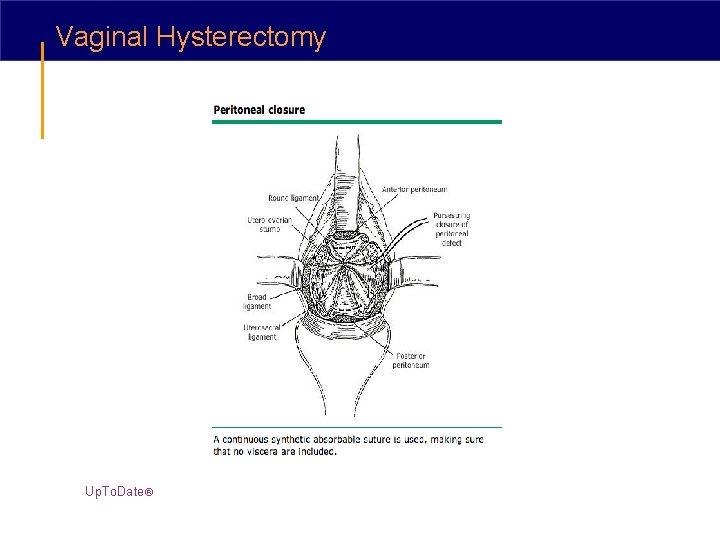
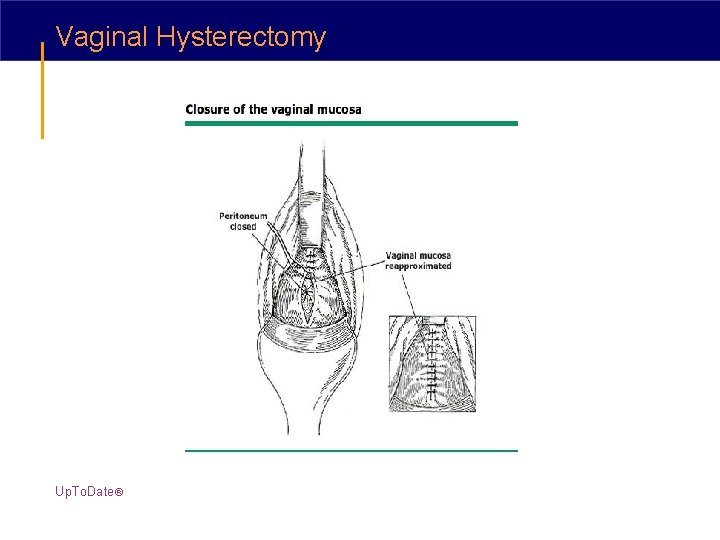
Vaginal Hysterectomy Uterine Morcellation • Piecemeal removal of a large, often myomatous uterus • Contraindicated in women w/uterine cancer • Methods § hemisection (bivalving) § wedge/V-type incision § intramyometrial coring • The uterine vasculature must be ligated before beginning any type of morcellation
Morellation is Safe • Morbidity is less than that encountered from an abdominal hysterectomy* • A rare problem in excision of a myoma is loss of the specimen into the peritoneal cavity due to clamp slippage § After completing removal of the uterus, the patient's head can be elevated and lavage of the peritoneal cavity will bring the errant fibroid into the pelvis • Uterine volume may be reduced preoperatively by administration of a Gn. RH *Taylor, SM, Romero, AA, Kammerer-Doak, DN, et al. Abdominal hysterectomy for the enlarged myomatous uterus compared with vaginal hysterectomy with morcellation. Am J Obstet Gynecol 2003; 189: 1579.
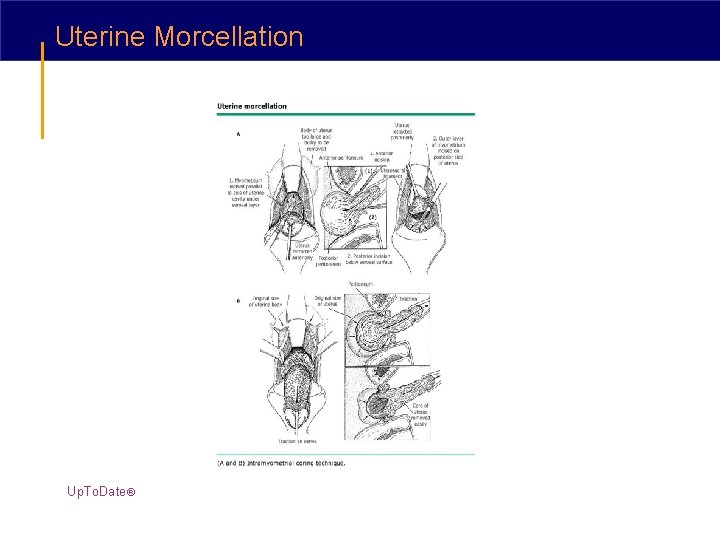
Uterine Morcellation Up. To. Date®
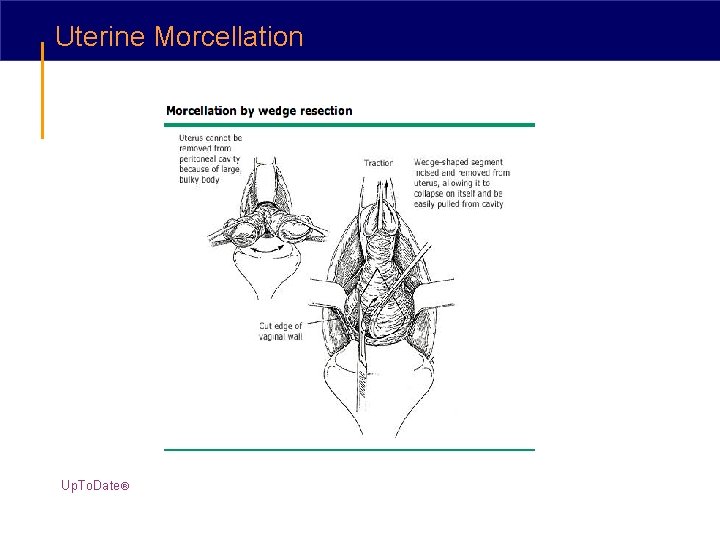
Uterine Morcellation Up. To. Date®
Poor uterine descensus • Decide whether to proceed with a vaginal approach or convert the procedure to an abdominal approach • If the problem relates to introital narrowing § midline or mediolateral episiotomy can be performed • If the problem stems from an enlarged uterus § morcellation can be begun after the uterine arteries have been ligated • Lack of descent resulting from extensive adhesive disease usually requires an abdominal incision or packing the vagina and accessing the pelvis by means of laparoscopy
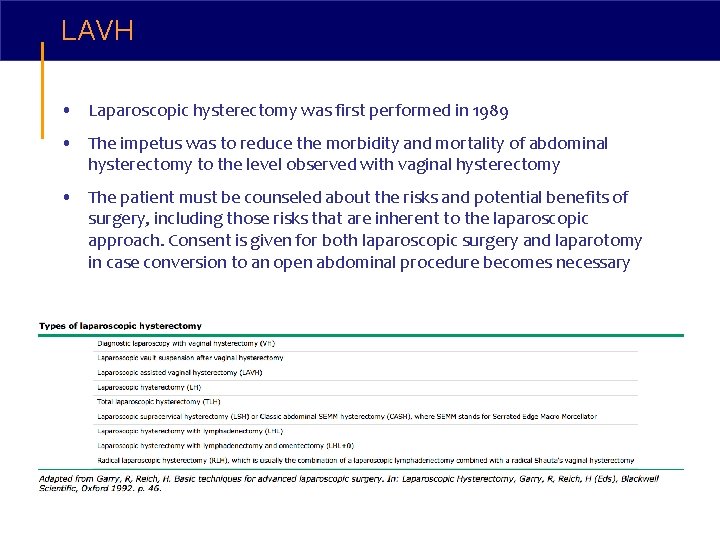
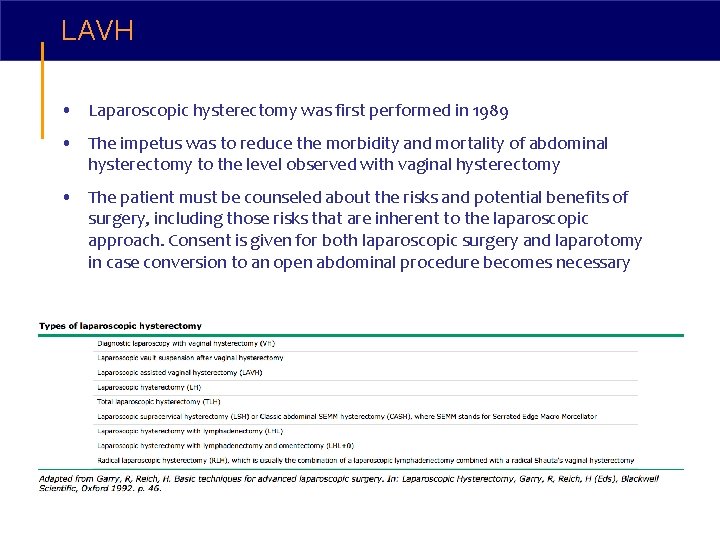
LAVH • Laparoscopic hysterectomy was first performed in 1989 • The impetus was to reduce the morbidity and mortality of abdominal hysterectomy to the level observed with vaginal hysterectomy • The patient must be counseled about the risks and potential benefits of surgery, including those risks that are inherent to the laparoscopic approach. Consent is given for both laparoscopic surgery and laparotomy in case conversion to an open abdominal procedure becomes necessary
LAVH • ACOG has listed the following as potential indications for laparoscopic assistance to facilitate hysterectomy via the vaginal approach: § Need for adhesiolysis § Need for treatment of endometriosis § Need for management of large leiomyoma(s) to facilitate uterine extraction § Need for ligation of the infundibulopelvic ligaments to facilitate oophorectomy ACOG Committee Opinion #311: Laparoscopically Assisted Vaginal Hysterectomy. Obstet Gynecol 2005; 105: 929.
LAVH • Laparoscopically performed portion of LAVH is limited to adhesiolysis, excision of endometriosis and division of the upper vascular pedicles and parametria § the remainder of the procedure is performed vaginally • At the completion of the vaginal procedure the abdomen is reinsufflated § helps the surgeon assess hemostasis
TLH • The entire procedure is performed laparoscopically § uterus is extracted vaginally, or removed abdominally using morcellation techniques • After the uterus is removed, the vaginal cuff is closed using laparoscopic suturing techniques MORCELLATION IS NOT PERFORMED IF UTERINE CANCER IS SUSPECTED
LSH is performed in an identical fashion to TLH • after occluding the ascending uterine vascular pedicles • cervix is amputated in a coring fashion § beginning at the level of the internal os, down into the endocervical canal
Robot-assisted Lap Hyst • Superior laparoscopic magnification of an image is achieved with robotic systems - surgical precision • Rotational movement of the robotic hands facilitates manipulation of tissues and suturing • “Tasks like adhesiolysis, suturing, and knot tying were enhanced with the robotic suturing system”* • “Robot-assisted laparoscopic hysterectomy appeared to provide a tool for overcoming surgical limitations seen with conventional laparoscopy”** *Beste, TM, Nelson, KH, Daucher, JA. Total laparoscopic hysterectomy utilizing a robotic surgical system. JSLS 2005; 9: 13. **Advincula, AP, Reynolds, RK. The use of robot-assisted laparoscopic hysterectomy in the patient with a scarred or obliterated anterior cul-de-sac. JSLS 2005; 9: 287.
Tools of the Trade for Scope & Hyst • Sutures • Electrosurgery • Bipolar cautery • Laser • Harmonic scalpel • Argon Beam Coagulator • Stapling device • Vessel Sealing device • Uterine manipulator • Vaginal fornix delineation tool • Pneumo-occluder
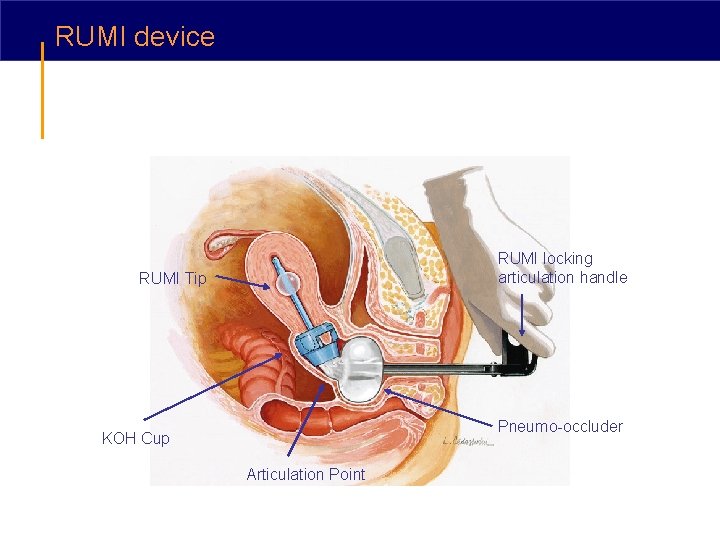
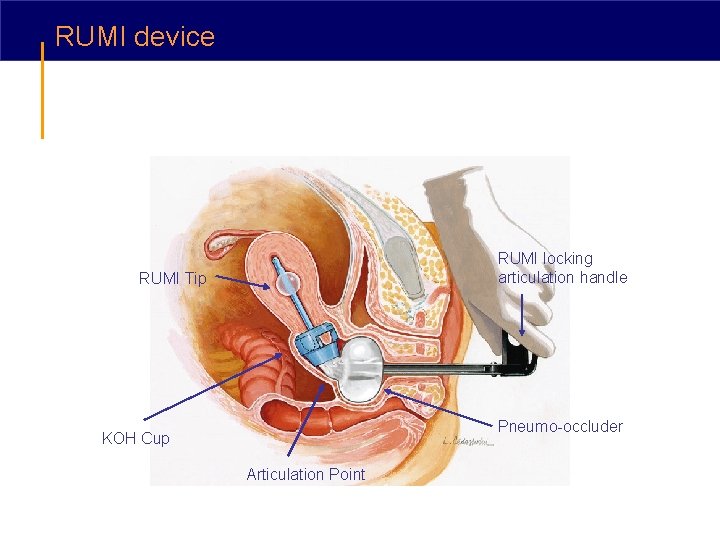
RUMI device RUMI locking articulation handle RUMI Tip Pneumo-occluder KOH Cup Articulation Point
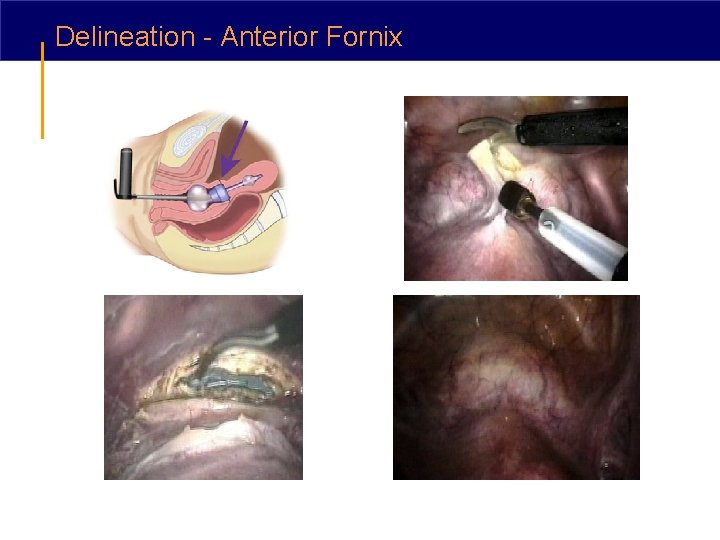
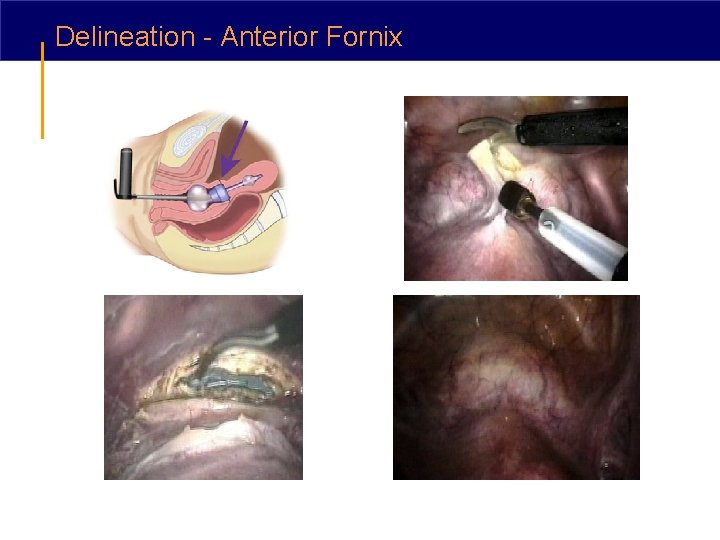
Delineation - Anterior Fornix
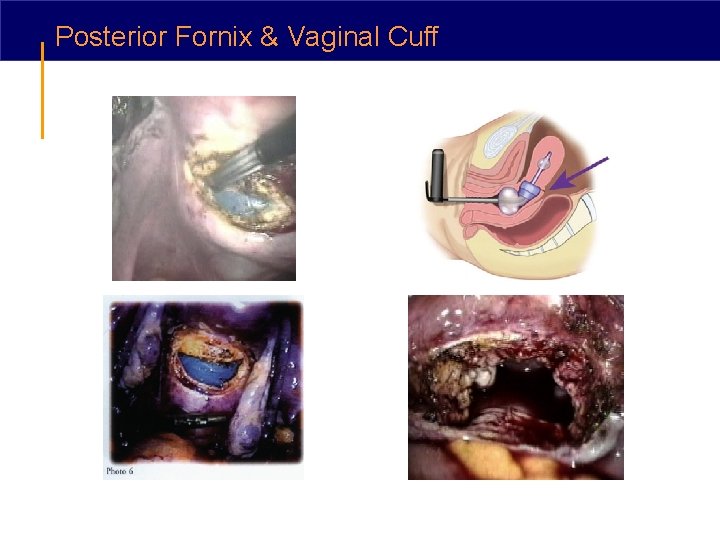
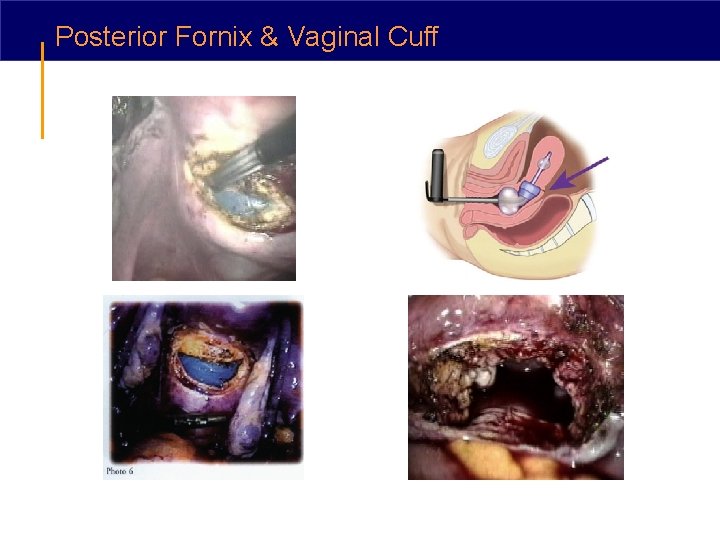
Posterior Fornix & Vaginal Cuff

Video clip of TLH using Rumi/KOH
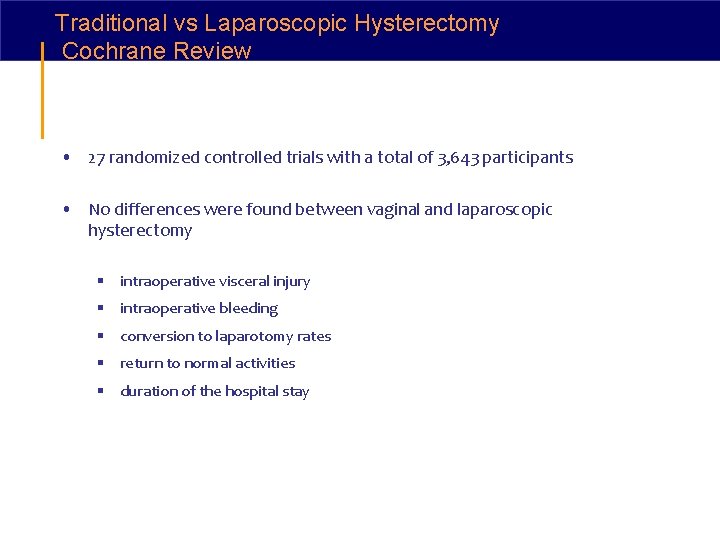
Traditional vs Laparoscopic Hysterectomy Cochrane Review • 27 randomized controlled trials with a total of 3, 643 participants • No differences were found between vaginal and laparoscopic hysterectomy § intraoperative visceral injury § intraoperative bleeding § conversion to laparotomy rates § return to normal activities § duration of the hospital stay
Traditional vs Laparoscopic Hysterectomy Cochrane Review No significant differences were found in: • occurrences of pelvic hematoma • vaginal cuff infection • urinary tract infection • chest infection • thromboembolic events • fistula formation • urinary dysfunction • sexual dysfunction • patient satisfaction
Traditional vs Laparoscopic Hysterectomy Cochrane Review • Return to normal activities was slower after the abdominal hysterectomy compared to laparoscopic and vaginal hysterectomy • Total laparoscopic hysterectomy was associated with the longest operation time, LAVH was comparable with abdominal hysterectomy, and vaginal hysterectomy was the fastest • The laparoscopic approach was associated with less risk of wound or other infections and less blood loss then abdominal hysterectomy
Traditional vs Laparoscopic Hysterectomy Cochrane Review • Urinary tract injuries (bladder plus ureteral injuries) appeared to be more likely in patients undergoing laparoscopic hysterectomy • No differences were found between TLH and LAVH, with the exception of surgical time
e. VALuate Study Multicenter randomized controlled trials that evaluated the relative roles of vaginal, abdominal and laparoscopic hysterectomy in routine gynecological practice • 2 parallel multicenter randomized trials all with benign disease § Arm 1: 292 women assigned to abdominal hysterectomy and 584 women assigned to laparoscopic hysterectomy § Arm 2: 168 women assigned to vaginal hysterectomy and 336 assigned to laparoscopic hysterectomy
e. VALuate study Multicenter randomized controlled trials that evaluated the relative roles of vaginal abdominal and laparoscopic hysterectomy in routine gynecological practice • Women were excluded if they had § 2 nd or 3 rd degree prolapse § uterus greater than 12 week size § medical disorder precluding laparoscopic surgery § required bladder or pelvic support surgery
e. VALuate Study Multicenter randomized controlled trials that evaluated the relative roles of vaginal, abdominal and laparoscopic hysterectomy in routine gynecological practice • Major composite surgical complications occurred more frequently in laparoscopic than abdominal hysterectomy (11% vs. 6%) • Rate of minor complications was similar (25% - 27%) • Laparoscopic hysterectomy took longer than abdominal or vaginal hysterectomy (median time of 84 vs. 50 minutes, and 72 vs. 39 minutes)
Cost Analysis • Cost analysis found that laparoscopic hysterectomy was not cost effective relative to vaginal hysterectomy* • Observational studies have documented cost effectiveness of laparoscopic hysterectomy as compared to abdominal hysterectomy **’*** *Sculpher, M, Manca, A, Abbott, J, et al. Cost effectiveness analysis of laparoscopic hysterectomy compared with standard hysterectomy: results from a randomised trial. BMJ 2004; 328: 134. **Demco, L, Garry, R, Johns, DA, et al. Hysterectomy. Panel discussion at the 22 nd annual meeting of the American Association of Gynecologic Laparoscopists (AAGL), San Francisco, November 12, 1993. J Am Assoc Gynecol Laparosc 1994; 1: 287 ***Lenihan, JP Jr, Kovanda, C, Cammarano, C. Comparison of laparoscopic-assisted vaginal hysterectomy with traditional hysterectomy for cost-effectiveness to employers. Am J Obstet Gynecol 2004; 190: 1714.
Summary • Based upon review of all available data, both laparoscopic assisted vaginal hysterectomy and vaginal hysterectomy are more cost-effective than abdominal hysterectomy • When vaginal hysterectomy is contraindicated or predicted to be difficult, the laparoscopic approach should be considered
Summary Laparoscopic hysterectomy was associated with § less postoperative pain than abdominal hysterectomy § shorter length of hospitalization (3 vs. 4 days) § quicker recovery § better quality of life at 6 weeks postoperatively • Laparoscopic techniques are applicable to a larger number of pathologies and situations than vaginal hysterectomy • Gynecologic surgeons need to learn and apply laparoscopic techniques when considering hysterectomy
 Most common site of ureteric injury during hysterectomy
Most common site of ureteric injury during hysterectomy What are optical storage devices are most commonly known as
What are optical storage devices are most commonly known as Water thief appliance
Water thief appliance A depressant drug drivers ed
A depressant drug drivers ed Most commonly used system
Most commonly used system Guerin bending process.
Guerin bending process. Extrafascial hysterectomy indications
Extrafascial hysterectomy indications Cesarean hysterectomy steps
Cesarean hysterectomy steps Disadvantages of laparoscopic hysterectomy
Disadvantages of laparoscopic hysterectomy Hysterectomy
Hysterectomy Cutting plane line symbol
Cutting plane line symbol Section 17-3 note taking guide answer key
Section 17-3 note taking guide answer key Commonly damaged areas of a vehicle during hoisting
Commonly damaged areas of a vehicle during hoisting Signing naturally 5:9 answers
Signing naturally 5:9 answers Potassium hydroxide relaxer
Potassium hydroxide relaxer Altered cognition in older adults is commonly attributed to
Altered cognition in older adults is commonly attributed to List three of the commonly used assembly constraints
List three of the commonly used assembly constraints History is a lie agreed upon
History is a lie agreed upon Computer graphics models are now commonly used for making
Computer graphics models are now commonly used for making Virtual memory is commonly implemented by
Virtual memory is commonly implemented by Multinational financial management an overview
Multinational financial management an overview Methods are commonly used to
Methods are commonly used to A commonly cited hazard for stairways and/or ladders is:
A commonly cited hazard for stairways and/or ladders is: The circle graphs are commonly called
The circle graphs are commonly called Open center curls
Open center curls Agaricus is commonly known as ......
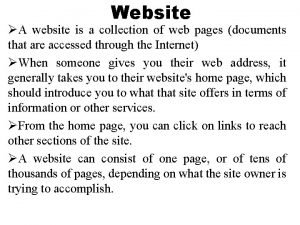
Agaricus is commonly known as ...... A web page is a collection of website
A web page is a collection of website Advantages of multi plate clutch
Advantages of multi plate clutch Sodium hydroxide relaxers are commonly called
Sodium hydroxide relaxers are commonly called A commonly cited hazard for stairways and or ladders is
A commonly cited hazard for stairways and or ladders is Commonly confused words paragraph
Commonly confused words paragraph To vs too
To vs too Development of a truncated cylinder
Development of a truncated cylinder Abused children commonly exhibit
Abused children commonly exhibit Narrative paragraph چیست
Narrative paragraph چیست Commonly confused words jeopardy
Commonly confused words jeopardy A pneumatic drill is commonly used
A pneumatic drill is commonly used What are poriferans
What are poriferans Homophone of week
Homophone of week Financial difficulties are commonly caused by overspending
Financial difficulties are commonly caused by overspending Commonly misused homonyms
Commonly misused homonyms Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Glasgow thang điểm
Glasgow thang điểm Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Các môn thể thao bắt đầu bằng tiếng nhảy
Các môn thể thao bắt đầu bằng tiếng nhảy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Phép trừ bù
Phép trừ bù Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V. c c
V. c c Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết