Gastroenteritis Gastroenteritis refers to infection in the stomach







- Slides: 39



Gastroenteritis • Gastroenteritis refers to infection in the stomach and intestines • Medically, gastroenteritis is defined as a diarrheal disease, an increase in bowel movement frequency with or without vomiting, fever, and abdominal pain. • Diarrheal diseases, are responsible for substantial morbidity and mortality worldwide 4
Types of GI • According to the duration of symptoms, it is described as acute, persistent, chronic, or recurrent. • Acute: 14 days or fewer than 14 days in duration. • Persistent: More than 14 but fewer than 30 days in duration. • Chronic: More than 30 days in duration. • Recurrent: Diarrhea that recurs after 7 days 5
• Young children, the elderly, and immunocompromised patients are at greatest risk for more severe disease and complications. • Poor sanitation, inadequate water supplies, and increasing globalization of food transport systems all predispose to the development of large epidemics of food- and waterborne outbreaks of gastrointestinal disease. 6
Etiology • A wide array of bacterial, protozoal, and viral pathogens is responsible for gastrointestinal tract infections. • The most common cause of acute infectious diarrhea are viruses (norovirus, rotavirus, adenovirus, and others). Stool cultures are positive in less than 5% of cases in most studies. • Other than norovirus, important causes of watery diarrhea include Clostridium perfringens, and enterotoxigenic Escherichia coli (ETEC). 7
Bacterial gastroenteritis • Bacterial causes are more responsible for severe cases of infectious diarrhea than other infectious etiologies. • Greater than or equal to four watery/loose stools per day for 3 or more days, a bacterial pathogen was identified in 87% of cases. • Among these severe bacterial causes, nontyphoidal Salmonella and Campylobacter spp are the most common causes. 8
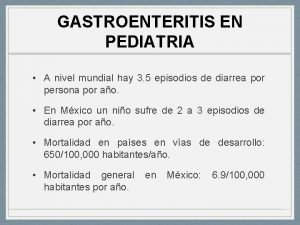
Epidemiology • Acute infectious diarrhea is a very common disease worldwide, • According to the WHO , 3 to 5 billion global cases of diarrheal disease are reported annually and are associated with an estimated 1. 5 to 2. 5 million deaths per year. • In children younger than 5 years, diarrheal disease is the second most common cause of death by infectious diseases. 9

Epidemiology The incidence rate per 100, 000 persons in 2019 was estimated by the Centers for CDC: Campylobacter - 19. 5 Salmonella - 18. 3 Shiga toxin-producing E. coli - 5. 9 Shigella - 4. 9 Vibrio - 1. 1 Yersinia - 0. 9 Listeria -0. 3 Iran 2017 : from 676 patients 42% Salmonella spp. , 40% Shigella spp. , 16% E. coli 10

• Diarrheal disease is most critical in developing countries, facilitated by • Unsafe water supplies, • Poor sanitation, • and nutritional deficiencies. • Traveler's diarrhea affects more than 50% of people traveling from developed to developing countries. 11
History and Physical Clinical manifestations • The most common history findings for a patient with gastroenteritis are as follows: • Nausea • Diarrhea (watery or bloody in dysentery) • Vomiting • Abdominal pain • Fever (suggests an invasive organism as the cause) 12
Diagnosis & Evaluation • Diagnostic approach to diarrheal illness is determined by the patient’s age and status, severity of disease, duration and type of illness, time of year, and geographic location. • For most patients no testing is necessary if the presentation is consistent with a viral cause and of mild to moderate severity. • The Infectious Disease Society of America (IDSA), based on low quality of evidence, recommends that those with fever, bloody, or severe diarrhea should be evaluated for treatable enteropathogens, such as Salmonella, Shigella, and Campylobacter • Fecal testing using culture or culture-independent methods is indicated for severe, bloody, febrile, dysenteric, nosocomial, or persistent diarrheal illnesses ﺍﻧﺠﻤﻦ ﺑیﻤﺎﺭیﻬﺎی ﻋﻔﻮﻧی آﻤﺮیکﺎ 13
Diagnosis & Evaluation • Initial evaluation requires good history taking and physical exam, particularly food and medical history, an assessment of duration, frequency, current volume status, and any other alarming signs and symptoms of the patient. • The potential number of bacteria associated with GI is now estimated to approach or exceed 40 individual species. • In contrast to this, both routine traditional and more contemporary molecular methods may screen for only 4 or 5 organisms 14
• Many cases of acute bacterial gastroenteritis may not require any testing to determine a specific etiology, but in a case of severe volume depletion, a serum electrolyte panel should be indicated to check for any electrolyte derangements. • The future role of bacterial stool cultures may be diminished by the emergence of nonculture diagnostic test methods for enteric pathogens. • Blood cultures should be collected for those with signs of sepsis, the immunosuppressed, infants <3 months of age, or those with a febrile illness of unclear cause. 15
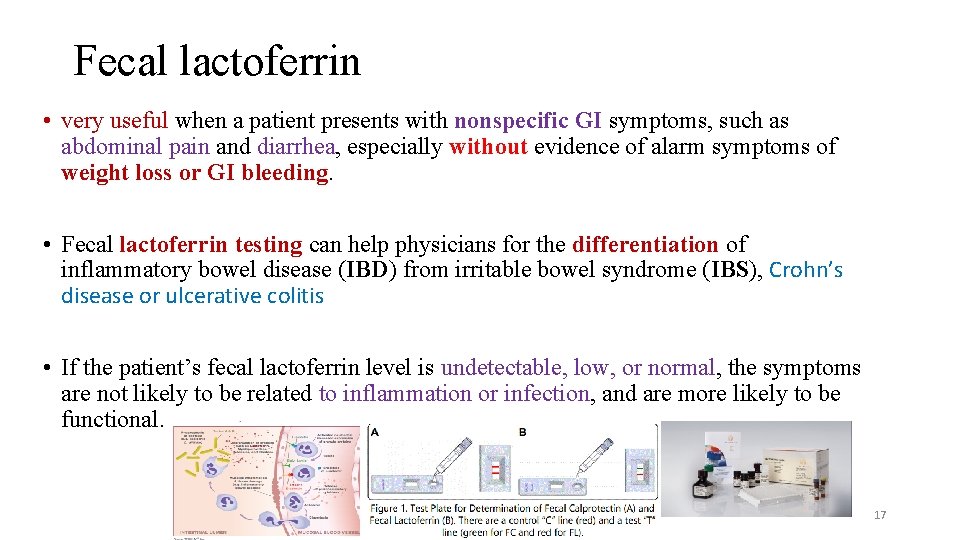
Nonculture diagnostic test methods • Stool nonmicrobiologic diagnostic tests have historically been considered in evaluating persons with suspected gastrointestinal infections, but the IDSA in their 2017 guideline recommends against testing for fecal leukocytes and lactoferrin, based on moderate evidence of lack of benefit. • The amount of lactoferrin released by neutrophils has been shown to correlate with the severity of inflammation in the gastrointestinal (GI) tract. 16
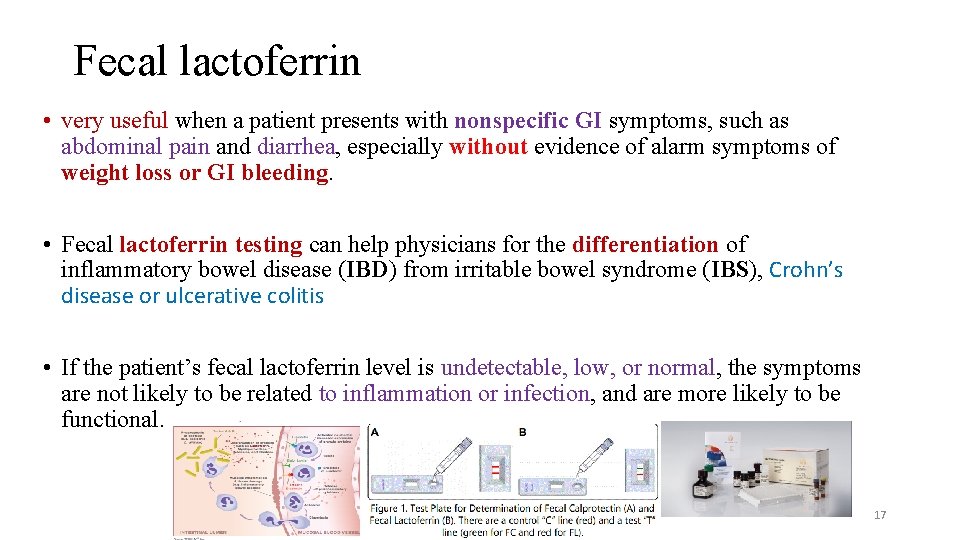
Fecal lactoferrin • very useful when a patient presents with nonspecific GI symptoms, such as abdominal pain and diarrhea, especially without evidence of alarm symptoms of weight loss or GI bleeding. • Fecal lactoferrin testing can help physicians for the differentiation of inflammatory bowel disease (IBD) from irritable bowel syndrome (IBS), Crohn’s disease or ulcerative colitis • If the patient’s fecal lactoferrin level is undetectable, low, or normal, the symptoms are not likely to be related to inflammation or infection, and are more likely to be functional. 17
Fecal leukocytes • This type of diarrhea may be a symptom of an bacterial infections such as: • Shigella, Clostridium difficile, campylobacter, or salmonella. 18
• A complete blood count cannot distinguish between bacterial etiologies but helps in suggesting severe disease or potential complications, for example, a high white blood count indicates invasive bacteria or pseudomembranous colitis • Hemoglobin and platelet counts, electrolytes, and blood urea nitrogen and creatinine is recommended to detect hematologic and renal function abnormalities that are early manifestations of HUS • low platelets counts indicate the development of the hemolytic-uremic syndrome. 19
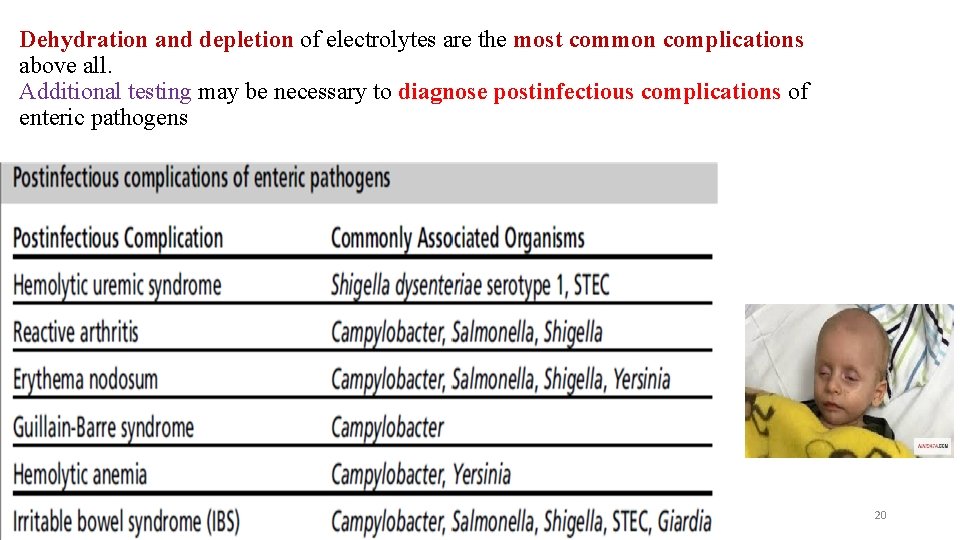
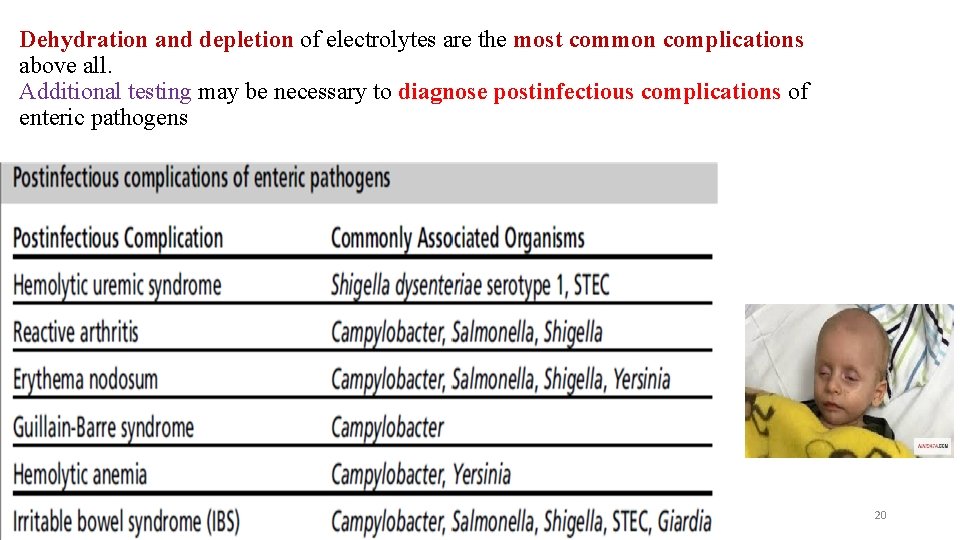
Dehydration and depletion of electrolytes are the most common complications above all. Additional testing may be necessary to diagnose postinfectious complications of enteric pathogens 20

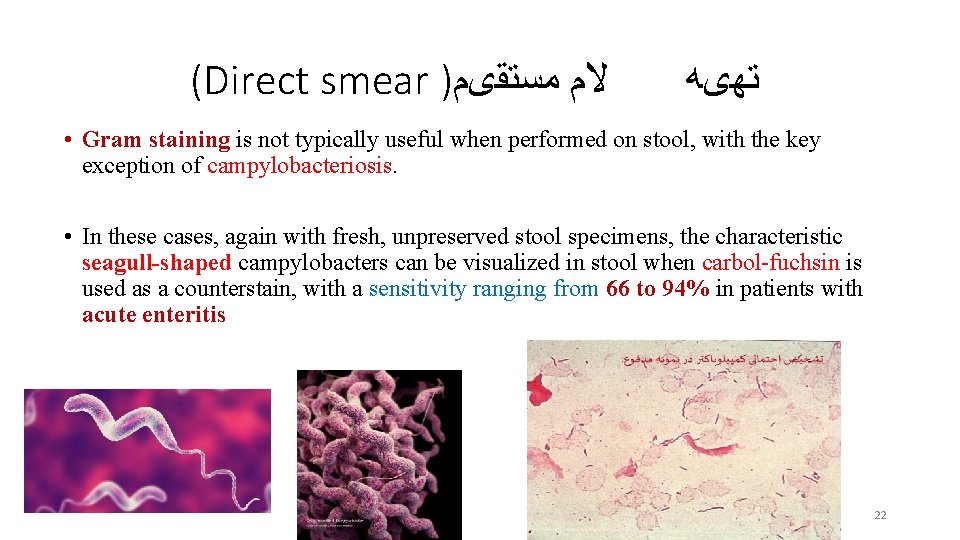
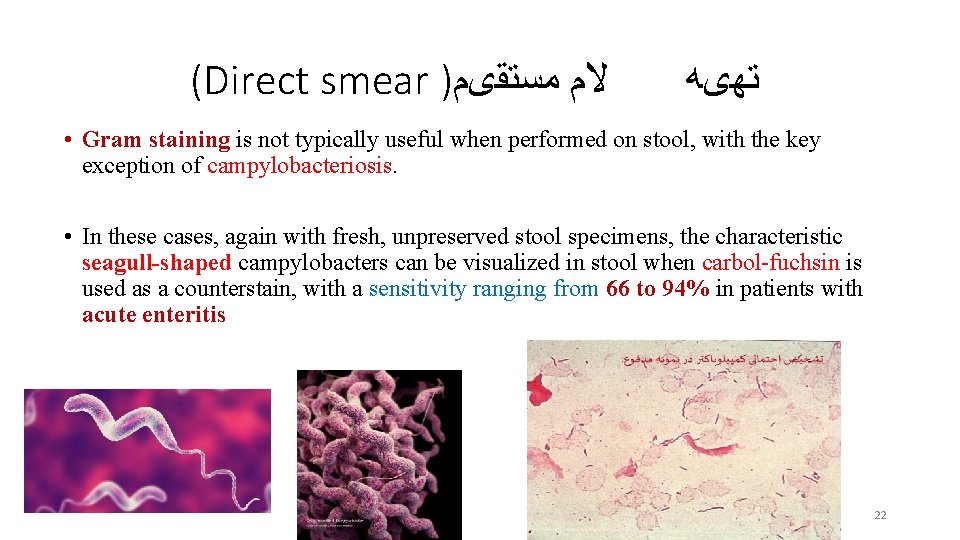
(Direct smear ) ﻣﺴﺘﻘیﻢ ﻻﻡ ﺗﻬیﻪ • Gram staining is not typically useful when performed on stool, with the key exception of campylobacteriosis. • In these cases, again with fresh, unpreserved stool specimens, the characteristic seagull-shaped campylobacters can be visualized in stool when carbol-fuchsin is used as a counterstain, with a sensitivity ranging from 66 to 94% in patients with acute enteritis 22
Standard laboratory methods • Include culture for bacteria, nucleic acid amplification and immunoassays for viruses and microscopy or enzyme immunoassays for parasites as well as culture for amoeba. • a reference method is selected that identifies the true infectious cause and provides a standard with which to assess alternative tests, assessing their test sensitivity and specificity. 23
Culture or culture-independent methods • laboratory is required to determine what organisms, methods, and screening parameters are included as part of the routine enteric pathogen culture or cultureindependent method. • Most laboratories will have the ability to culture for Salmonella, Shigella, and for Campylobacter and for Shiga toxin–producing Escherichia coli 24
Specimen collection • In studies of adult patients who submitted >1 specimen, the enteric pathogen was detected in the first sample 87%– 94% of the time, with the second specimen bringing the positive rate up to 98%. • In pediatric patients, the first specimen detects 98% of the enteric pathogens. • Thus, one sample for children and a second for selected adult patients may be considered. 25
• Rectal swabs are less sensitive than stool specimens when culture methods are employed and are not recommended for culture from adults, • but in symptomatic pediatric patients, rectal swabs and stool culture are equivalent in the ability to detect fecal pathogens. 26
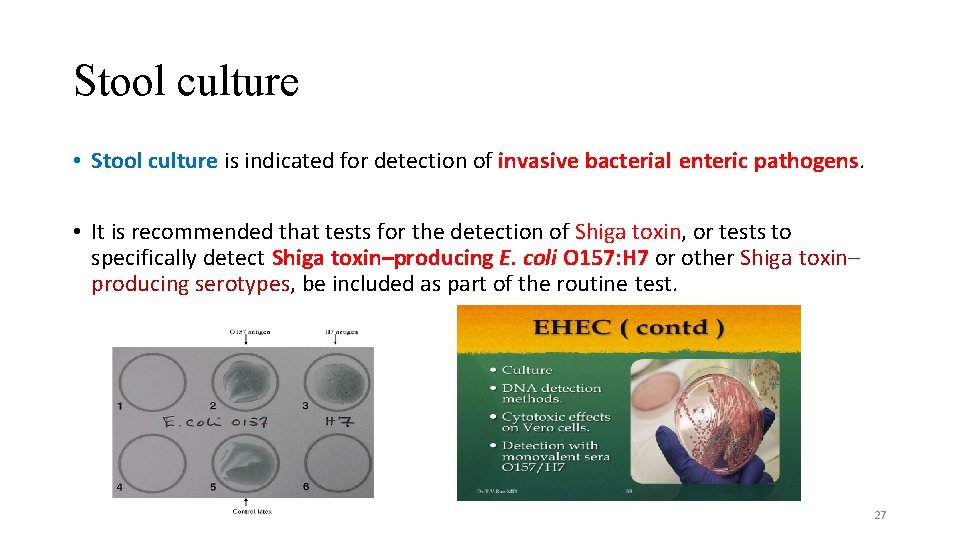
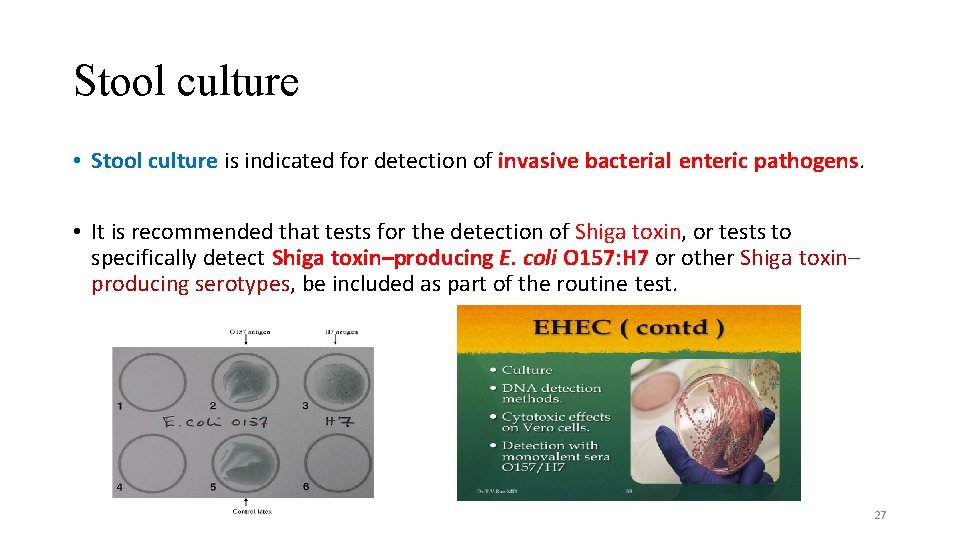
Stool culture • Stool culture is indicated for detection of invasive bacterial enteric pathogens. • It is recommended that tests for the detection of Shiga toxin, or tests to specifically detect Shiga toxin–producing E. coli O 157: H 7 or other Shiga toxin– producing serotypes, be included as part of the routine test. 27

• Screening of stool for toxin-producing E. coli is recommended for all pediatric patients. 28
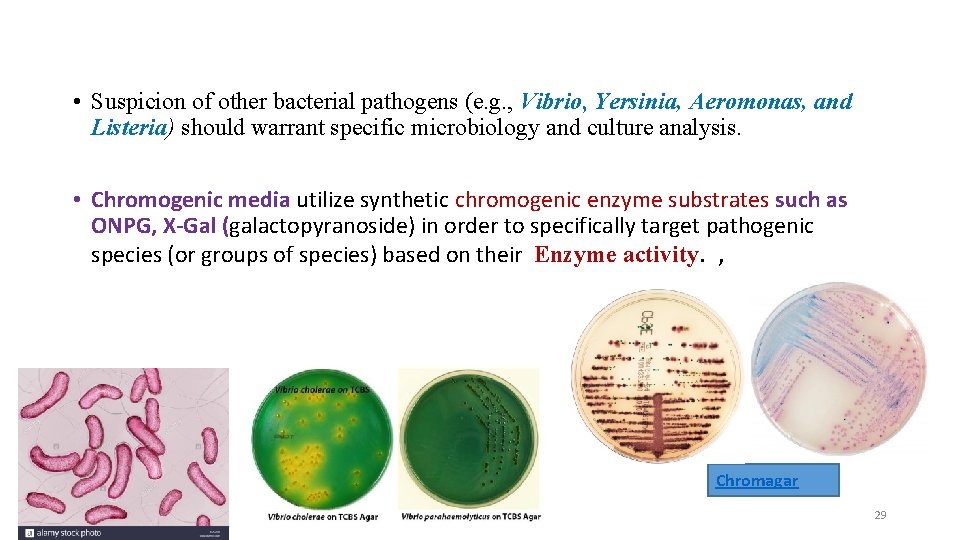
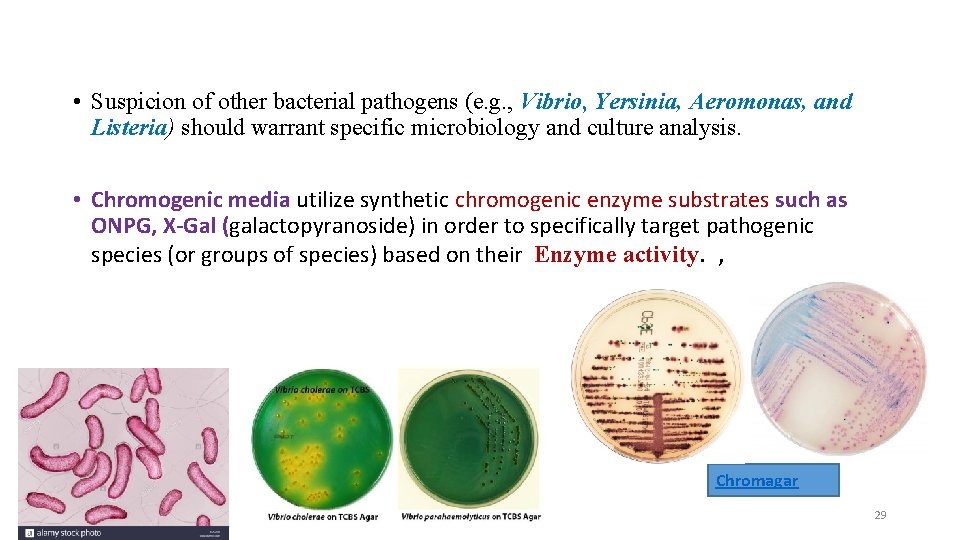
• Suspicion of other bacterial pathogens (e. g. , Vibrio, Yersinia, Aeromonas, and Listeria) should warrant specific microbiology and culture analysis. • Chromogenic media utilize synthetic chromogenic enzyme substrates such as ONPG, X-Gal (galactopyranoside) in order to specifically target pathogenic species (or groups of species) based on their Enzyme activity. , Chromagar 29
• In case of bloody diarrhea, additional testing for Shiga toxin and leukocytes in stool for EHEC should be ordered in addition to stool culture. • In case of persistent diarrhea, the practitioner should send stool samples for ova and parasite testing 30
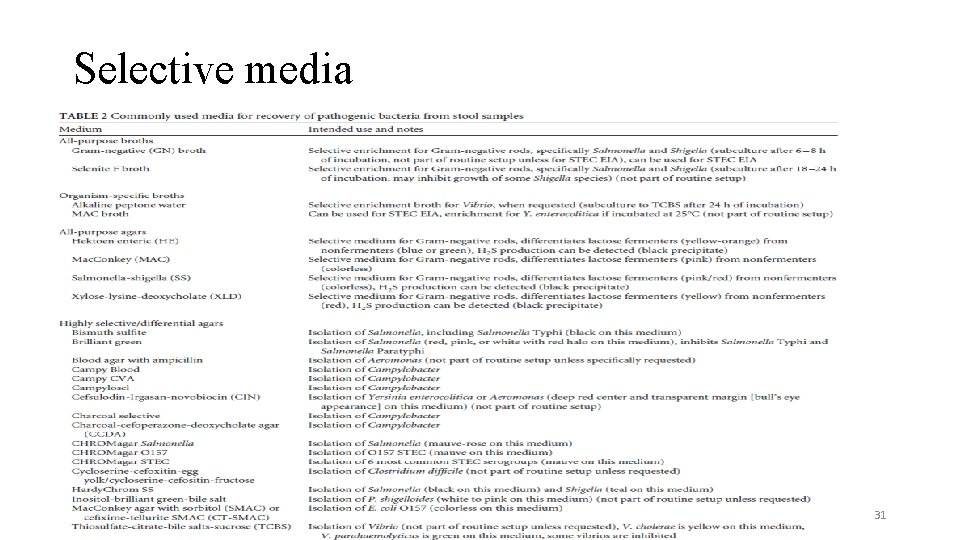
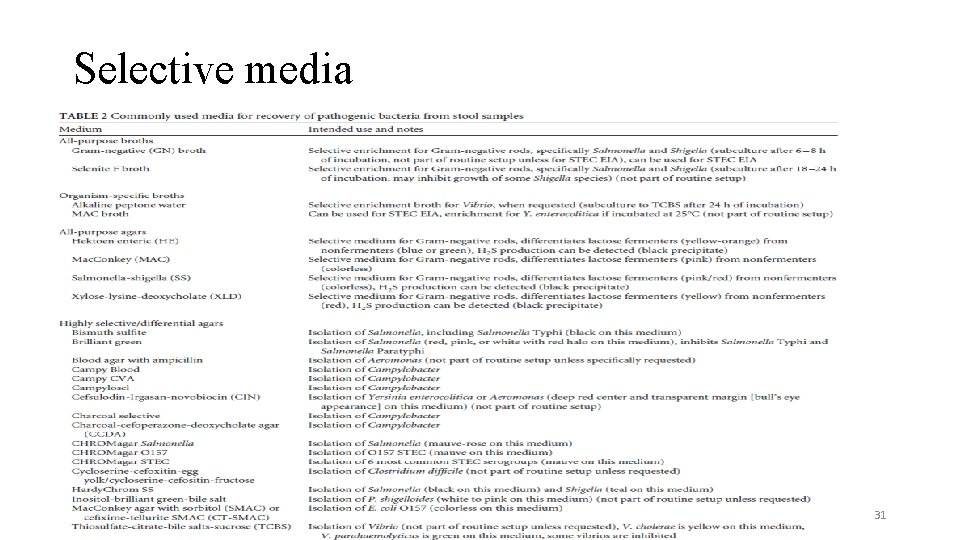
Selective media 31
Culture independent methods • Stool culture often fails to detect the causative agent and, when necessary, cultureindependent methods are recommended as adjunct methods. • for Clostridium difficile and, although available, may not be routinely employed for other bacterial and viral causes of gastrointestinal infections • Multiple stool specimens are rarely indicated for the detection of stool pathogens. 32
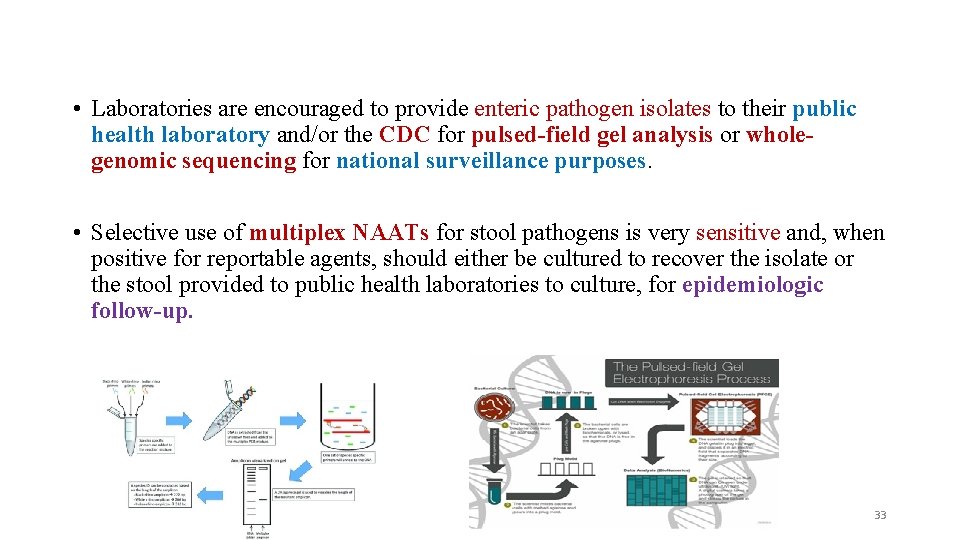
• Laboratories are encouraged to provide enteric pathogen isolates to their public health laboratory and/or the CDC for pulsed-field gel analysis or wholegenomic sequencing for national surveillance purposes. • Selective use of multiplex NAATs for stool pathogens is very sensitive and, when positive for reportable agents, should either be cultured to recover the isolate or the stool provided to public health laboratories to culture, for epidemiologic follow-up. 33
Culture-Independent Methods • Nucleic acid amplification assays vary from singleplex to highly multiplexed assays. • Culture independent methods can detect pathogens in as little as 1– 5 hours compared to the 24– 96 hours often required for culture. • more sensitive than culture and have resulted in much higher rates of detection. • Highly multiplexed assays allow for the detection of mixed infections, where the importance of each pathogen is unclear, and they may allow for the detection of pathogens, such as Enteroaggregative E. coli or sapovirus, where the indication for therapy is unclear. • Culture-independent methods should not be used as test of cure as they will detect both viable and nonviable organisms. 34
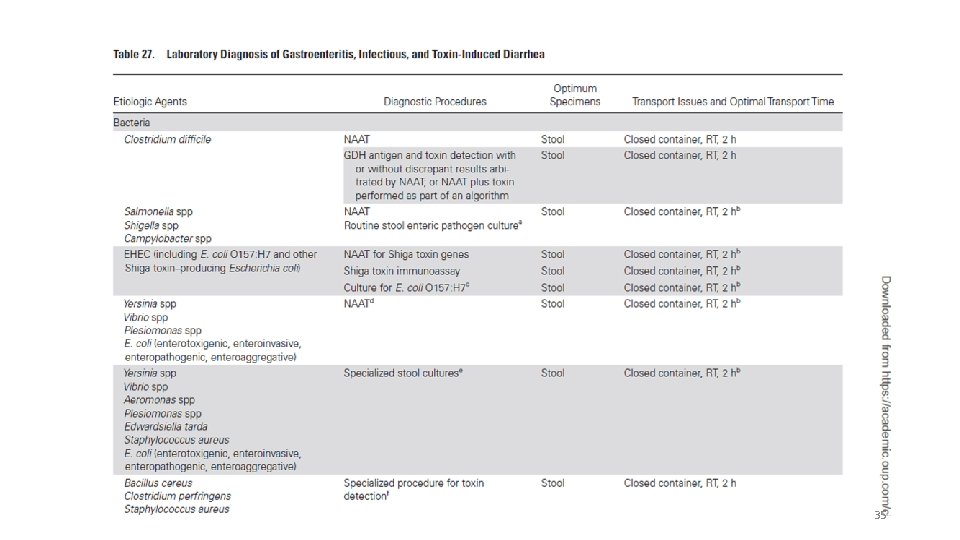
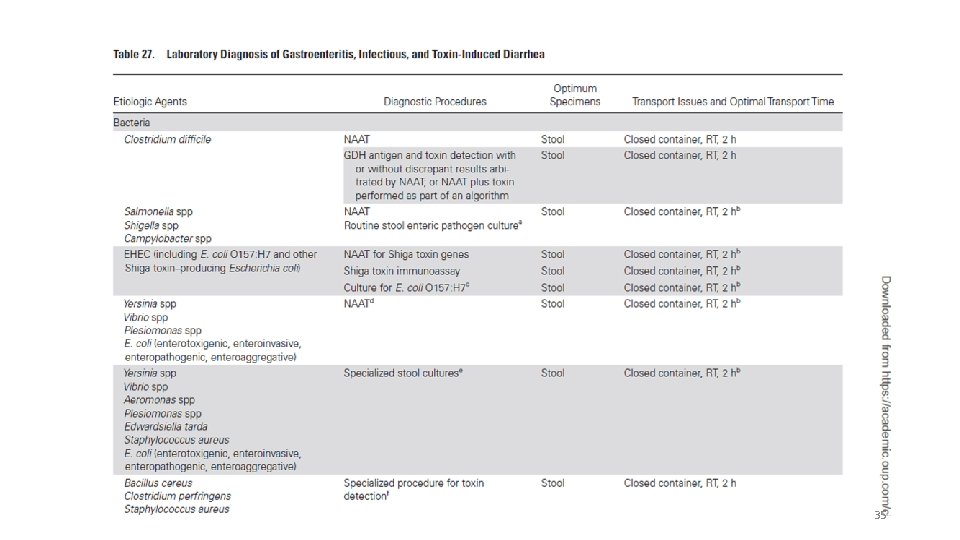
35
Differential Diagnosis • Differential diagnosis of acute bacterial gastroenteritis includes other causes of gastroenteritis such as viral and parasitic gastroenteritis. • Common foodborne illnesses also should be considered in differentials. • Other diseases that can cause watery diarrhea are Crohn disease, pseudomembranous colitis, microscopic colitis, acute HIV infection, irritable bowel disease, and lactose intolerance. • Bloody diarrheal disease other than dysentery includes ulcerative colitis. • Celiac disease and malabsorption syndromes also cause diarrhea. 36
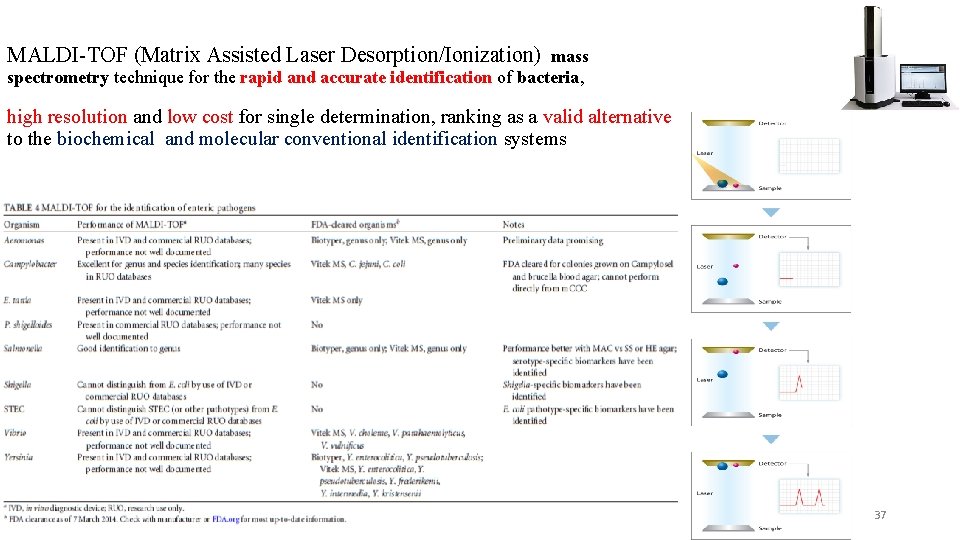
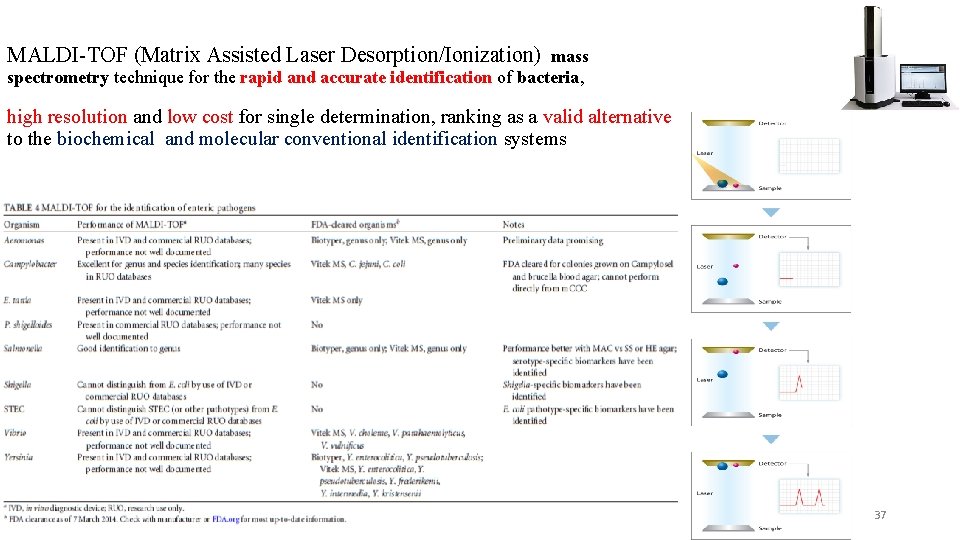
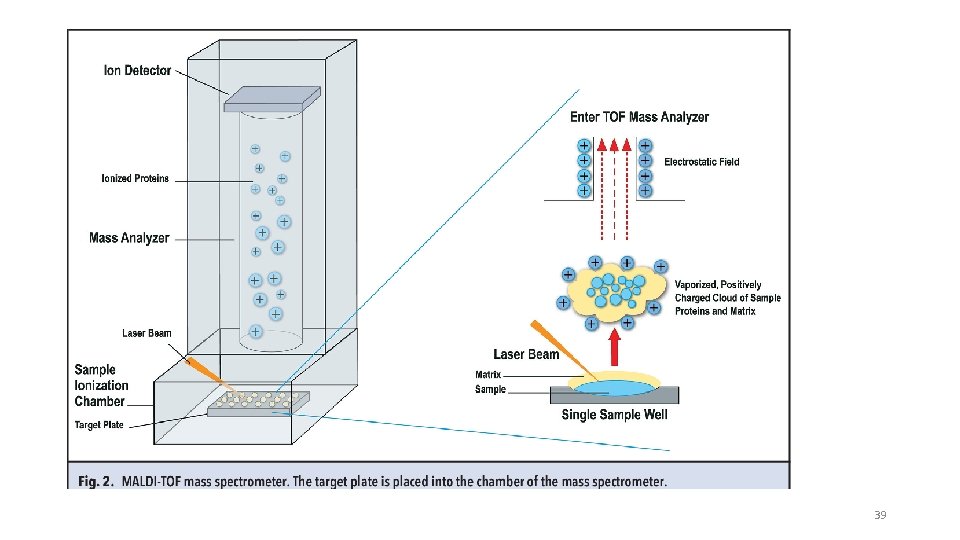
MALDI-TOF (Matrix Assisted Laser Desorption/Ionization) mass spectrometry technique for the rapid and accurate identification of bacteria, high resolution and low cost for single determination, ranking as a valid alternative to the biochemical and molecular conventional identification systems 37
38
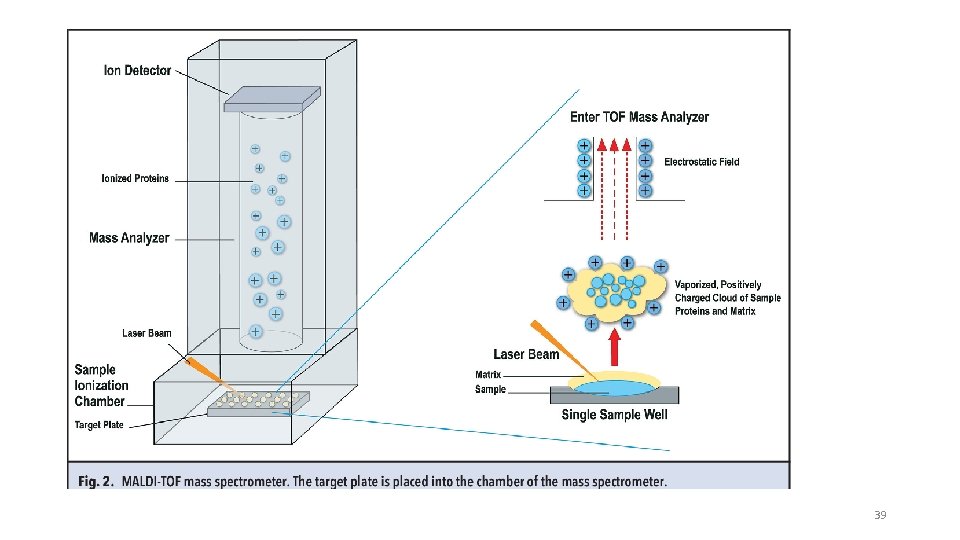
39
 Sengstaken-blakemore tube guidelines
Sengstaken-blakemore tube guidelines Akutni gastroenteritis
Akutni gastroenteritis Acute gastroenteritis
Acute gastroenteritis Gastroenteritis bacterial
Gastroenteritis bacterial Elements of a medical term are the:
Elements of a medical term are the: Gastroenteritis at a university in texas
Gastroenteritis at a university in texas Kontaktisolation
Kontaktisolation Shigellosis causative agent
Shigellosis causative agent Komorditet
Komorditet Dha mcq
Dha mcq Rotatest
Rotatest Gastroenteritis prefix and suffix
Gastroenteritis prefix and suffix Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể độ dài liên kết
độ dài liên kết Kể tên các môn thể thao
Kể tên các môn thể thao Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi điện thế nghỉ
điện thế nghỉ Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Chó sói
Chó sói Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Các số nguyên tố
Các số nguyên tố Lời thề hippocrates
Lời thề hippocrates Fecboak
Fecboak Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Tư thế ngồi viết
Tư thế ngồi viết Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Tư thế worms-breton
Tư thế worms-breton Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Thẻ vin
Thẻ vin