esophagus Anatomy n n The esophagus is 25








- Slides: 56
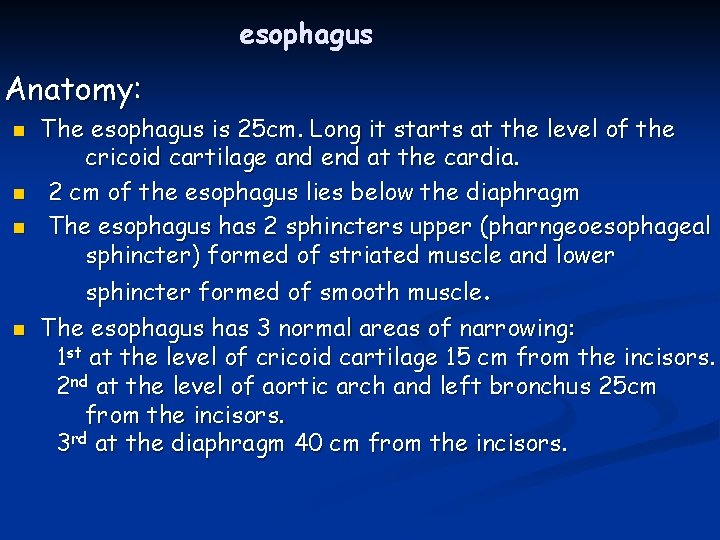
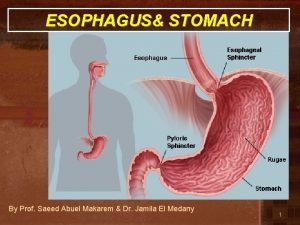
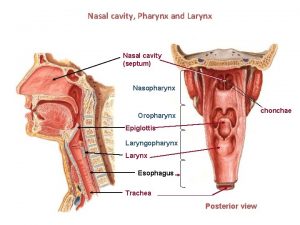
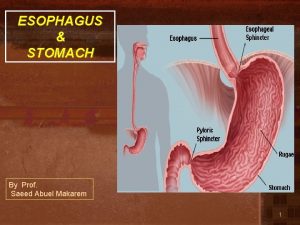
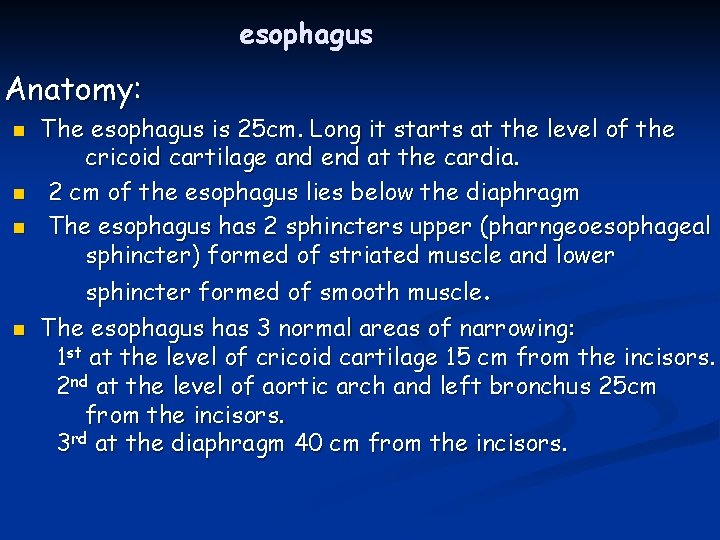
esophagus Anatomy: n n The esophagus is 25 cm. Long it starts at the level of the cricoid cartilage and end at the cardia. 2 cm of the esophagus lies below the diaphragm The esophagus has 2 sphincters upper (pharngeoesophageal sphincter) formed of striated muscle and lower sphincter formed of smooth muscle. The esophagus has 3 normal areas of narrowing: 1 st at the level of cricoid cartilage 15 cm from the incisors. 2 nd at the level of aortic arch and left bronchus 25 cm from the incisors. 3 rd at the diaphragm 40 cm from the incisors.

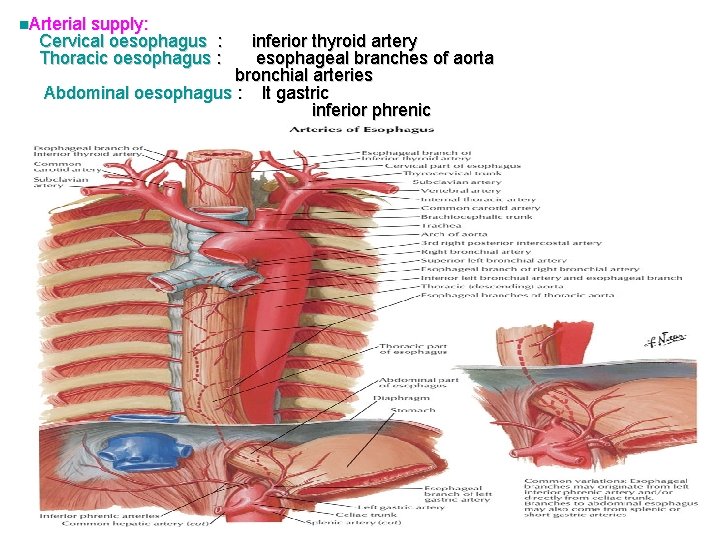
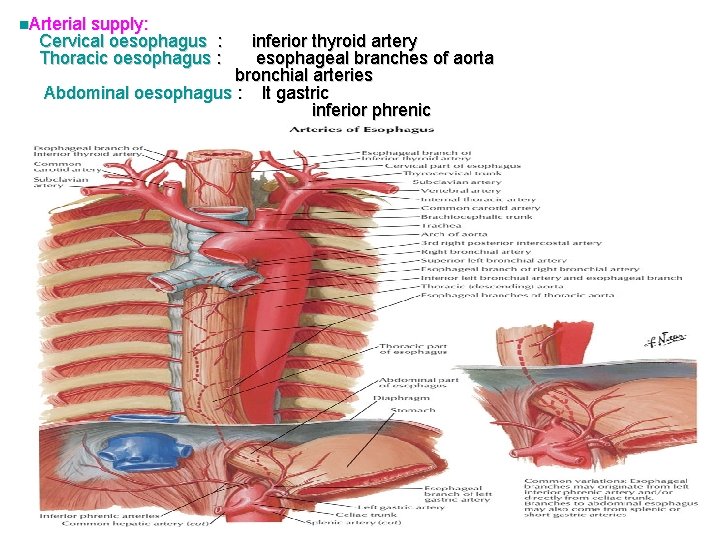
n. Arterial supply: Cervical oesophagus : Thoracic oesophagus : inferior thyroid artery esophageal branches of aorta bronchial arteries Abdominal oesophagus : lt gastric inferior phrenic
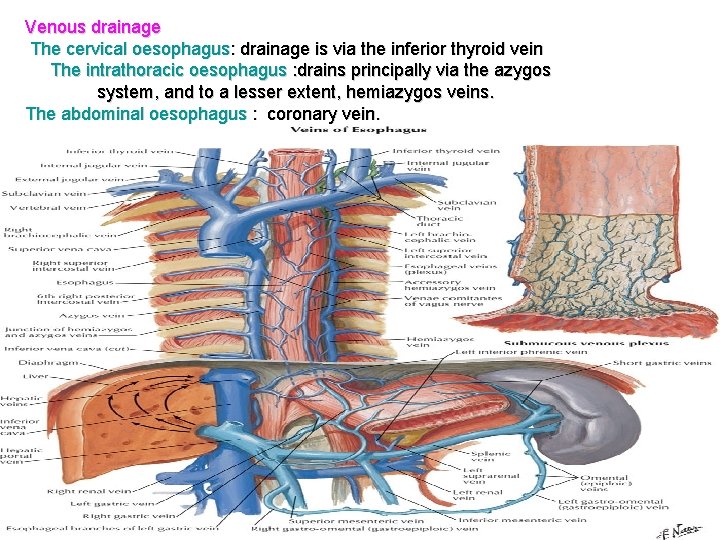
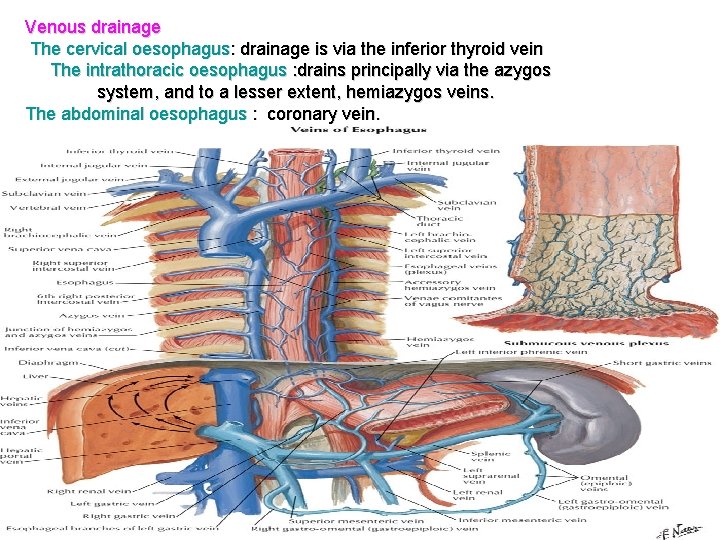
Venous drainage The cervical oesophagus: drainage is via the inferior thyroid vein The intrathoracic oesophagus : drains principally via the azygos system, and to a lesser extent, hemiazygos veins. The abdominal oesophagus : coronary vein.
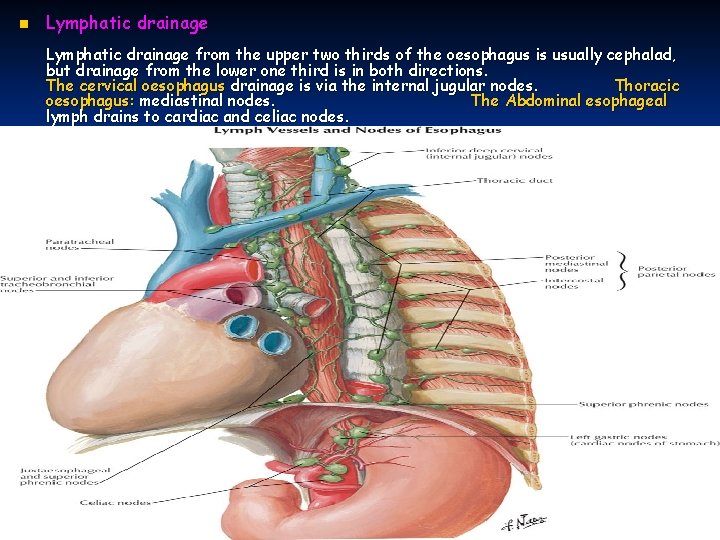
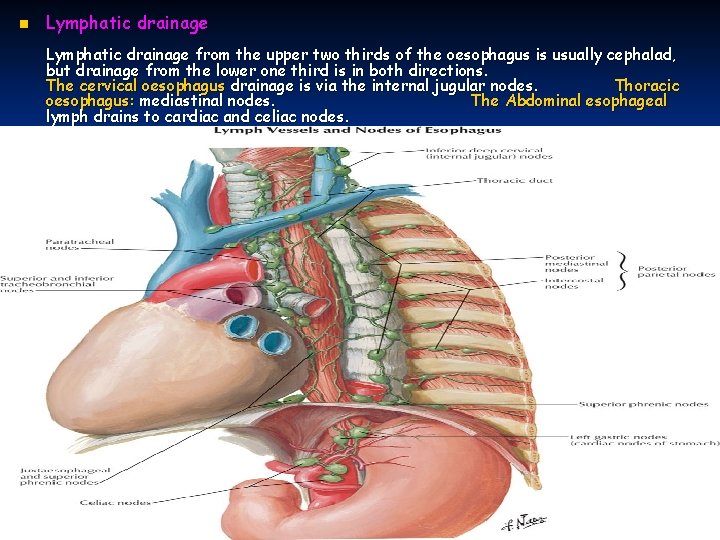
n Lymphatic drainage from the upper two thirds of the oesophagus is usually cephalad, but drainage from the lower one third is in both directions. The cervical oesophagus drainage is via the internal jugular nodes. Thoracic oesophagus: mediastinal nodes. The Abdominal esophageal lymph drains to cardiac and celiac nodes.

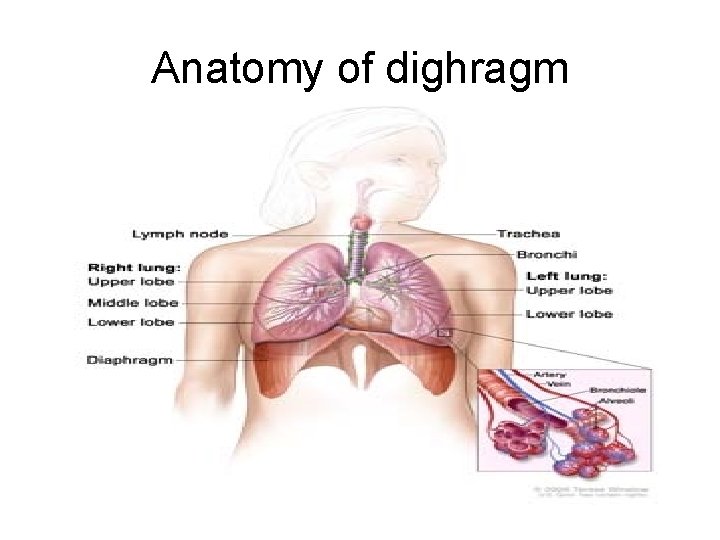
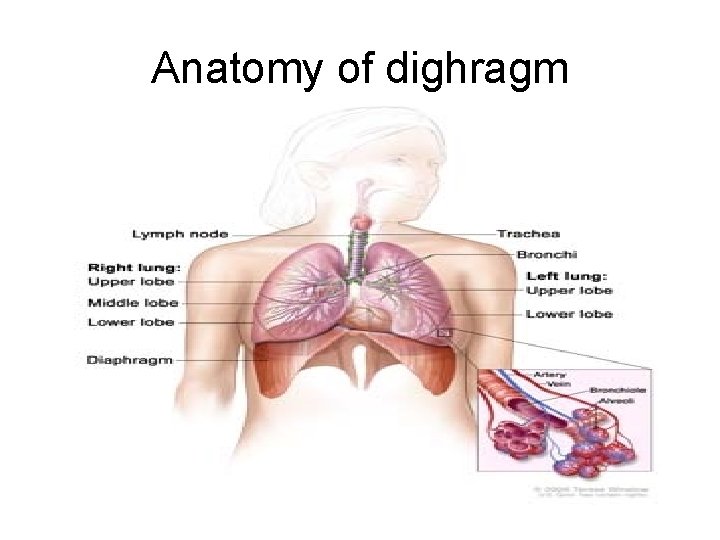
Anatomy of dighragm


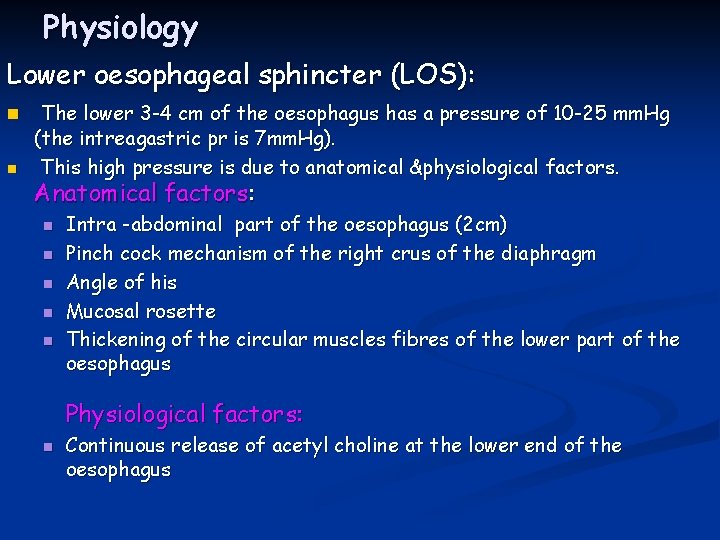
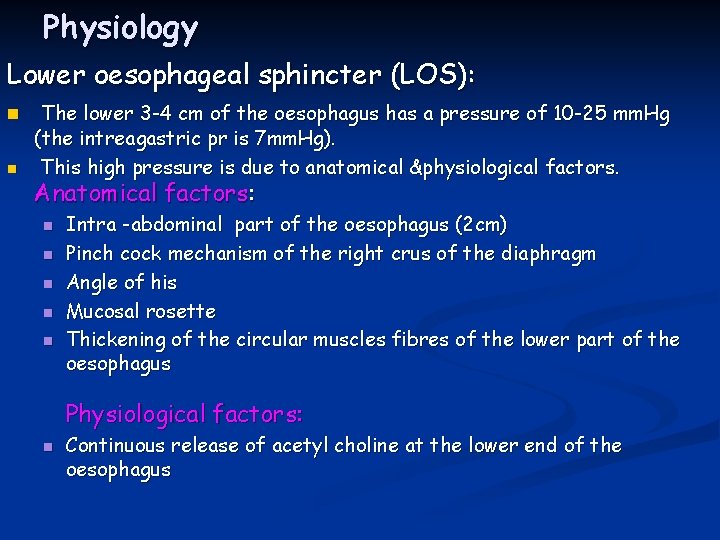
Physiology Lower oesophageal sphincter (LOS): n n The lower 3 -4 cm of the oesophagus has a pressure of 10 -25 mm. Hg (the intreagastric pr is 7 mm. Hg). This high pressure is due to anatomical &physiological factors. Anatomical factors: n n n Intra -abdominal part of the oesophagus (2 cm) Pinch cock mechanism of the right crus of the diaphragm Angle of his Mucosal rosette Thickening of the circular muscles fibres of the lower part of the oesophagus Physiological factors: n Continuous release of acetyl choline at the lower end of the oesophagus

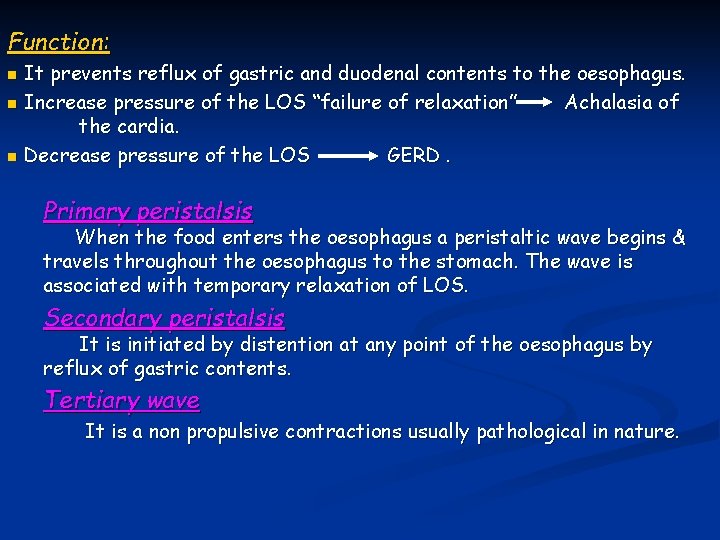
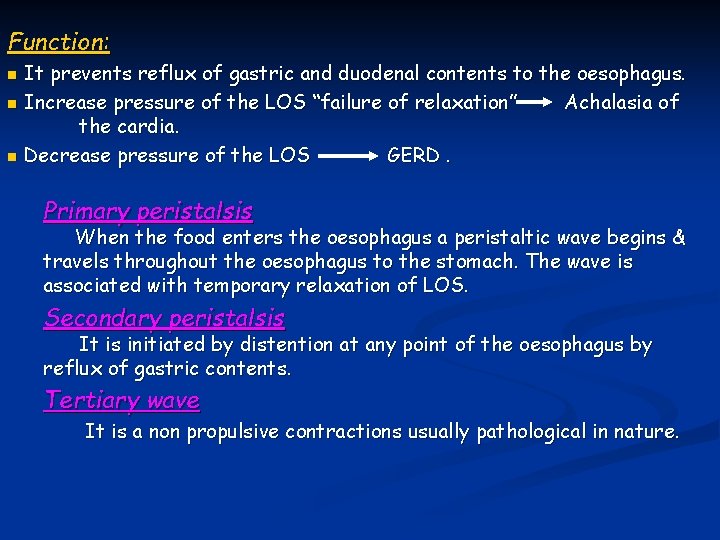
Function: It prevents reflux of gastric and duodenal contents to the oesophagus. n Increase pressure of the LOS “failure of relaxation” Achalasia of the cardia. n Decrease pressure of the LOS GERD. n Primary peristalsis When the food enters the oesophagus a peristaltic wave begins & travels throughout the oesophagus to the stomach. The wave is associated with temporary relaxation of LOS. Secondary peristalsis It is initiated by distention at any point of the oesophagus by reflux of gastric contents. Tertiary wave It is a non propulsive contractions usually pathological in nature.
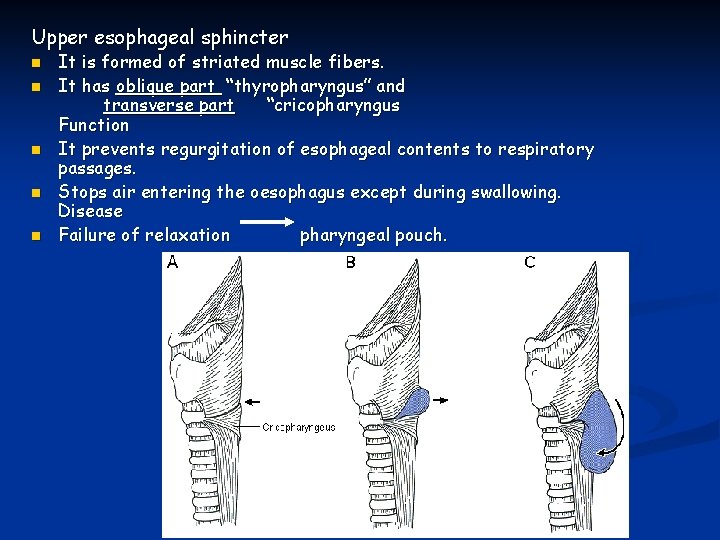
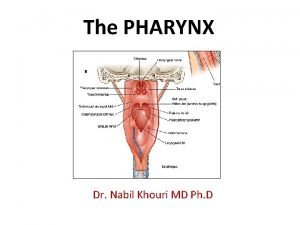
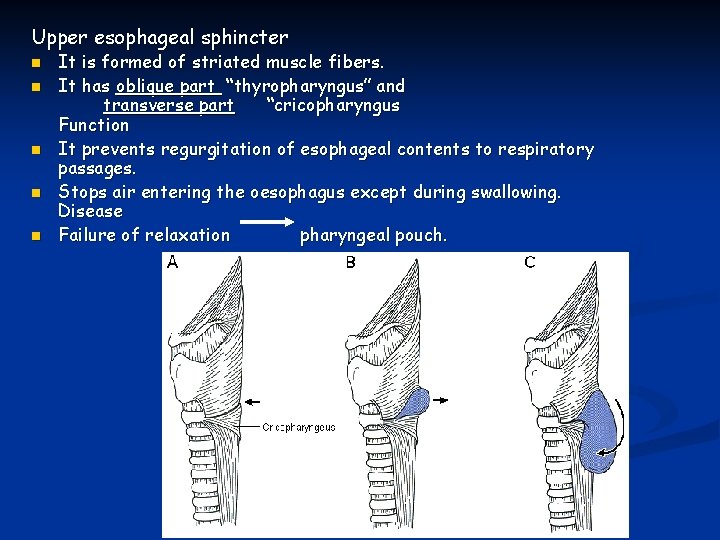
Upper esophageal sphincter n n n It is formed of striated muscle fibers. It has oblique part “thyropharyngus” and transverse part “cricopharyngus Function It prevents regurgitation of esophageal contents to respiratory passages. Stops air entering the oesophagus except during swallowing. Disease Failure of relaxation pharyngeal pouch.
Achalasia of the oesophagus Definition: incomplete or absent relaxation of the LOS with absent primary peristalsis of the body of the oesophagus associated with dilatation & hypertrophy of the circular muscle layer. Aetiology: Loss of ganglion cells of Auerbach’s plexus of unknown cause ( the inhibitory neurons are selectively affected). N. B Achalasia is similar to Chagas’ disease caused by Trypanosoma cruzi. Difference between Hirschsprung’s disease & Achalasia: the dilated part in Achalasia contains few ganglion cells but in Hirschsprung’s disease contains normal ganglion cells proximal to the constricted aganglionic segment. Clinical picture: Achalasia may affect any age but more common in middle age Dysphagia : intermittent , more to fluids (solids pass by their wt) Loss of weight: mild Regurgitation Aspiration pneumonia
Investigations: Br swallow Dilated tortuous oesophagus. Bird’s beak appearance Absence of gastric air bubble Endoscopy Dilatation of the oesophagus Food residues Biopsy ( there is increase incidence of carcinoma) Manometry Hypertensive LOS Absent 1 ry peristalsis. Complications Small mucosal ulceration Aspiration pneumonia Increase incidence of carcinoma
Treatment Medical : 1)Long-acting nitrates. 2)Calcium channel blockers. Invasive: 1) Forceful dilatation using inflatable bag. 2) Heller’s myotomy (through the abdomen or chest) using open or endoscopic surgery. 3) Endoscopic injection of Botulinum toxins into LOS to affect the cholinergic stimulatory neurons.

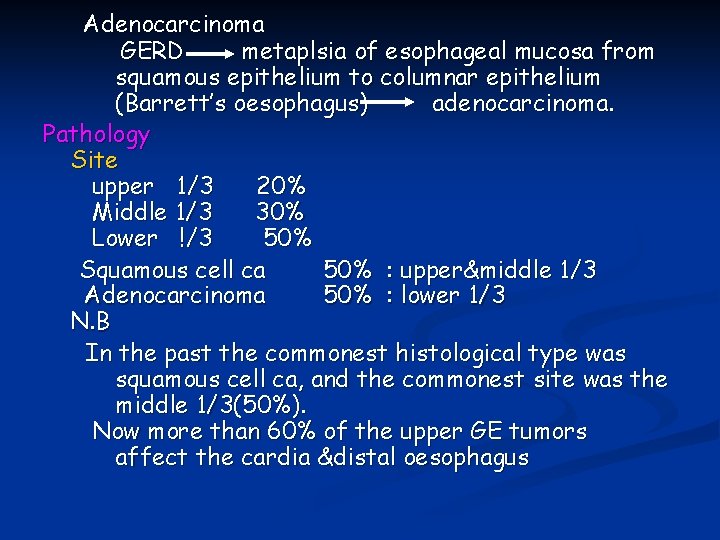
Carcinoma of the oesophagus Incidence Squamous cell ca of the oesophagus is rare disease. The incidence of adenocarcinoma of the oesophagus is increasing ( on top of Barrett’s oesophagus complicating GERD ) Aetiology Predisposing Factors Squamous cell ca: ▪Smoking ▪Alcohol ▪ High intake of nitrosamines derived from nitrates used in food preservation ▪ Achalasia ▪Post corrosive stricture ▪ Plummer Vinson syndrome
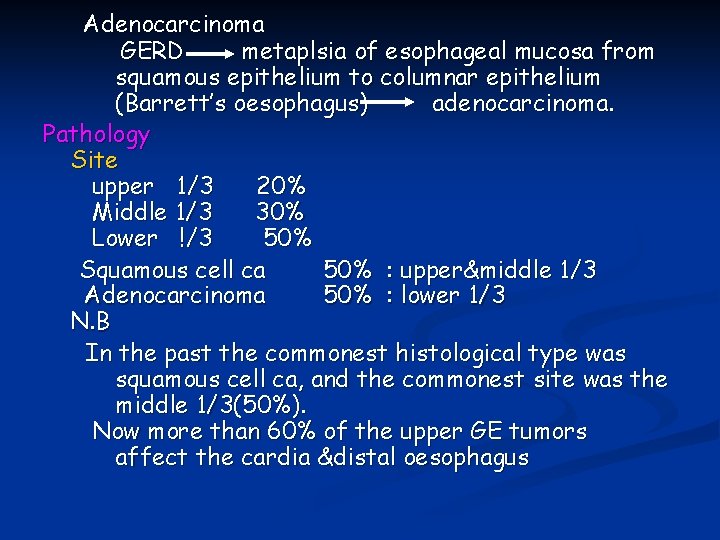
Adenocarcinoma GERD metaplsia of esophageal mucosa from squamous epithelium to columnar epithelium (Barrett’s oesophagus) adenocarcinoma. Pathology Site upper 1/3 20% Middle 1/3 30% Lower !/3 50% Squamous cell ca 50% : upper&middle 1/3 Adenocarcinoma 50% : lower 1/3 N. B In the past the commonest histological type was squamous cell ca, and the commonest site was the middle 1/3(50%). Now more than 60% of the upper GE tumors affect the cardia &distal oesophagus
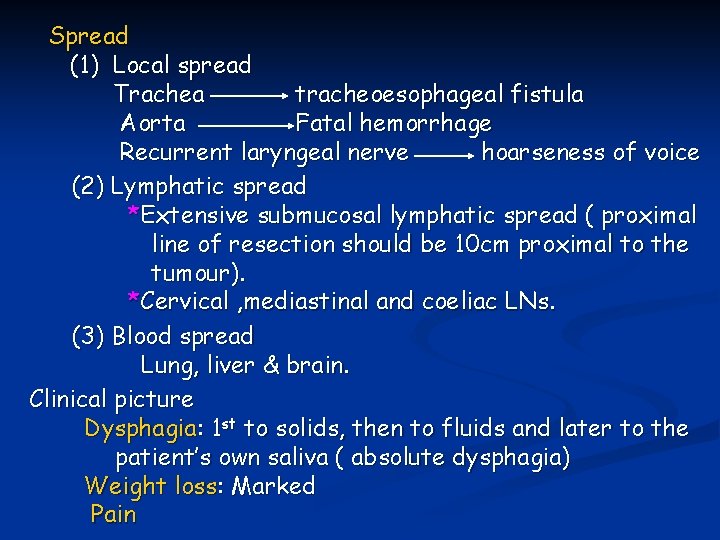
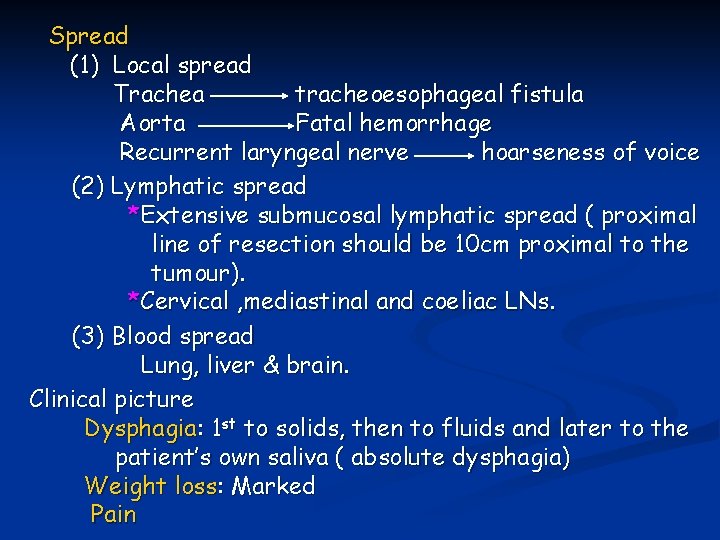
Spread (1) Local spread Trachea tracheoesophageal fistula Aorta Fatal hemorrhage Recurrent laryngeal nerve hoarseness of voice (2) Lymphatic spread *Extensive submucosal lymphatic spread ( proximal line of resection should be 10 cm proximal to the tumour). *Cervical , mediastinal and coeliac LNs. (3) Blood spread Lung, liver & brain. Clinical picture Dysphagia: 1 st to solids, then to fluids and later to the patient’s own saliva ( absolute dysphagia) Weight loss: Marked Pain
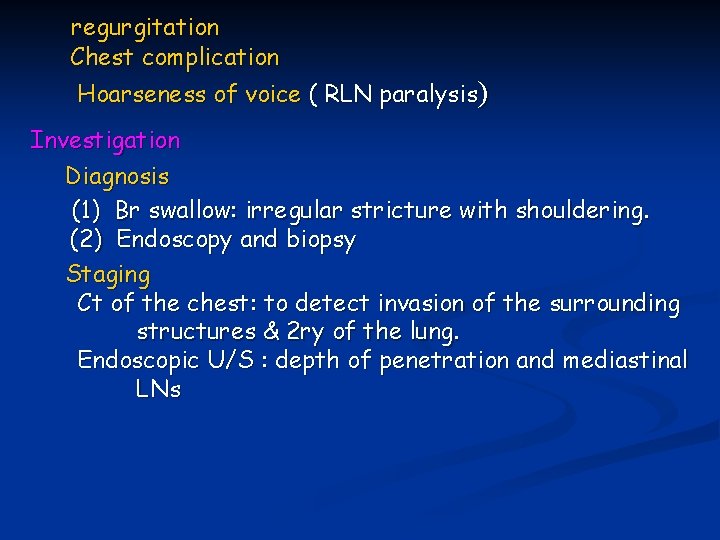
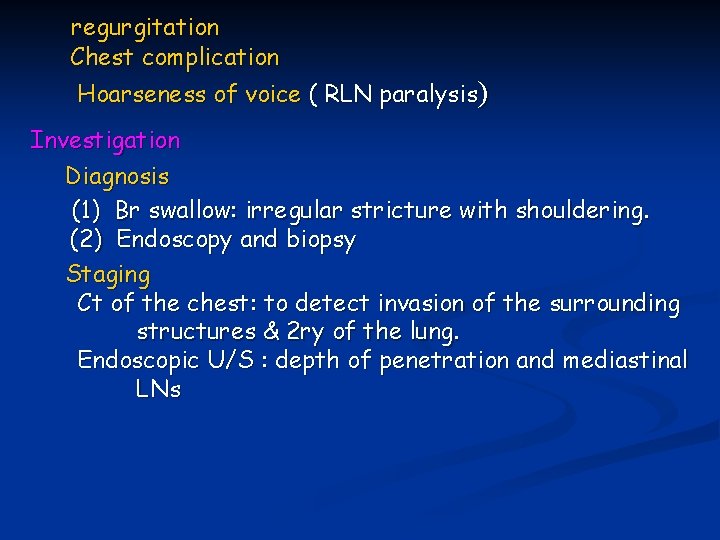
regurgitation Chest complication Hoarseness of voice ( RLN paralysis) Investigation Diagnosis (1) Br swallow: irregular stricture with shouldering. (2) Endoscopy and biopsy Staging Ct of the chest: to detect invasion of the surrounding structures & 2 ry of the lung. Endoscopic U/S : depth of penetration and mediastinal LNs
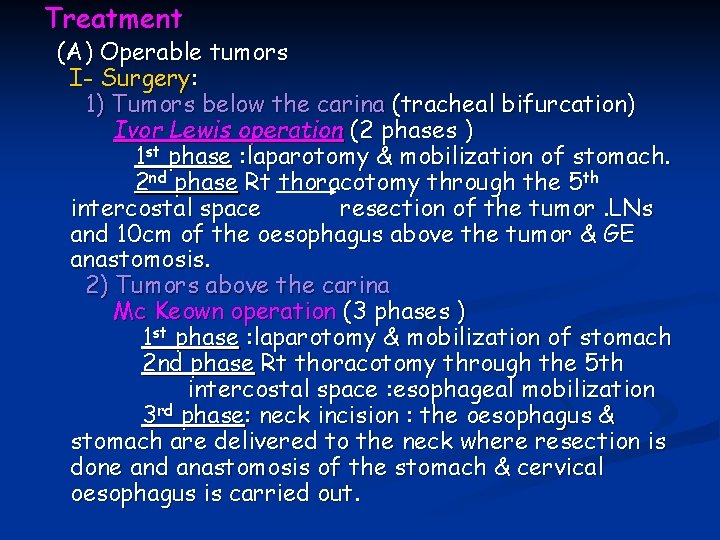
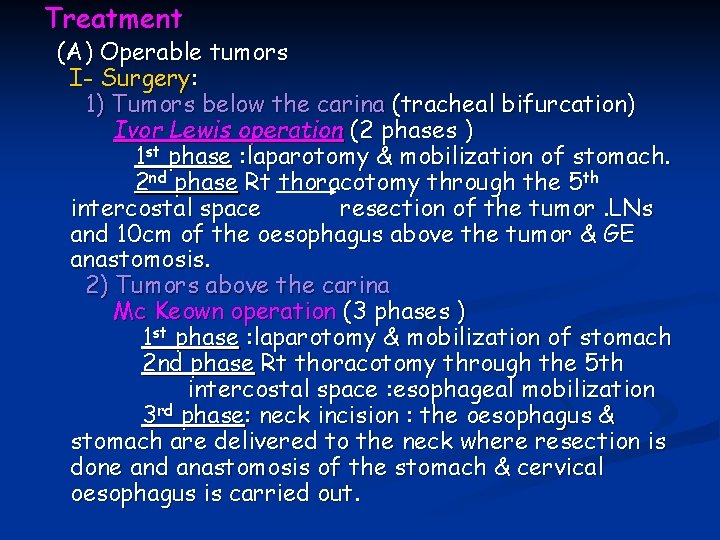
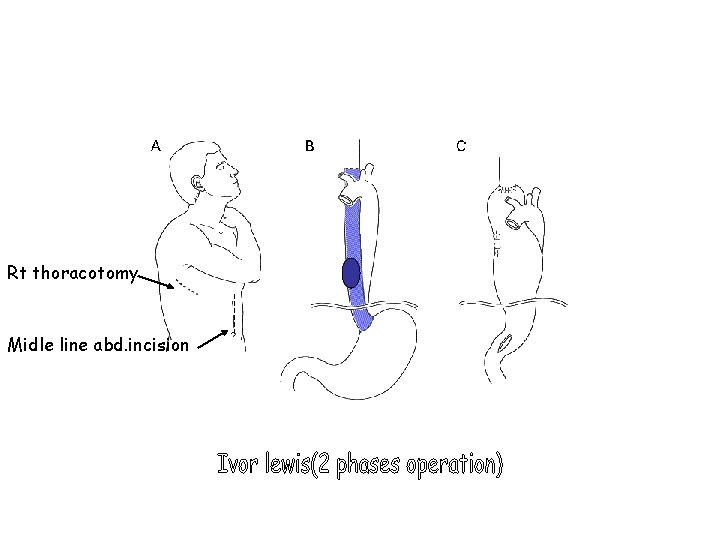
Treatment (A) Operable tumors I- Surgery: 1) Tumors below the carina (tracheal bifurcation) Ivor Lewis operation (2 phases ) 1 st phase : laparotomy & mobilization of stomach. 2 nd phase Rt thoracotomy through the 5 th intercostal space resection of the tumor. LNs and 10 cm of the oesophagus above the tumor & GE anastomosis. 2) Tumors above the carina Mc Keown operation (3 phases ) 1 st phase : laparotomy & mobilization of stomach 2 nd phase Rt thoracotomy through the 5 th intercostal space : esophageal mobilization 3 rd phase: neck incision : the oesophagus & stomach are delivered to the neck where resection is done and anastomosis of the stomach & cervical oesophagus is carried out.
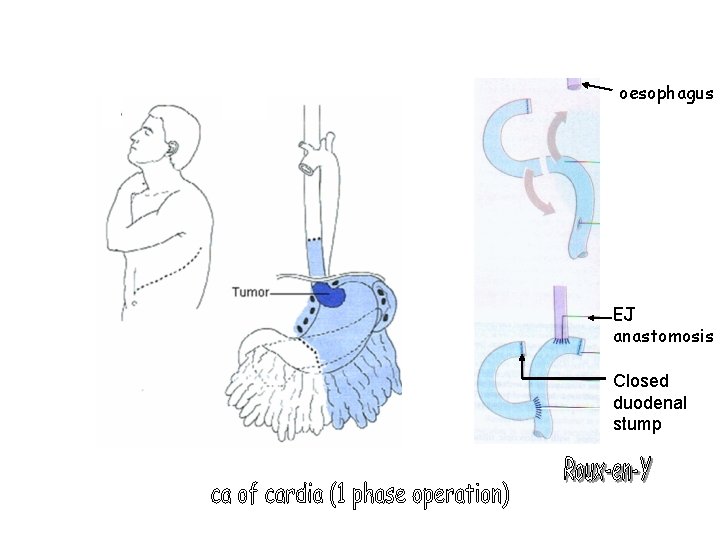
3) Tumours of the cardia (1 phase) lt thracoabdominal incision: the stomach & lower oesophagus are removed with -en-Y esophagojujenostomy Roux Other options Transhiatal esophagectomy Thoracotomy is avoided by mobilizing the oesophagus from the abdomen via the diaphragmatic hiatus and via the neck incision. Endopscopic removal through laparoscopy & thorascopy II-Adjuvant therapy Chemoradiotherapy
(B) Inoperable Tumors ( 60% of the patients) * Local spread( e. g tracheoesophageal fistula, RLN paralysis) * Distant spread * Bad general condition Options: n n Endoscopic Laser to core a channel through the tumor Intubations n n n Self expanding metal stents Traction stents e. g. Celestine stint Pulsion stents e. g. Soutter’ tube Radiotherapy for squamous cell ca. Chemotherapy : 5 FU
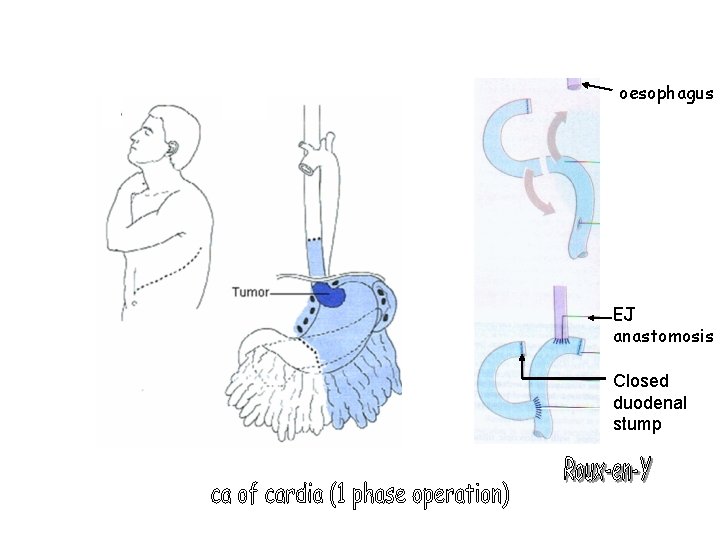
oesophagus EJ anastomosis Closed duodenal stump
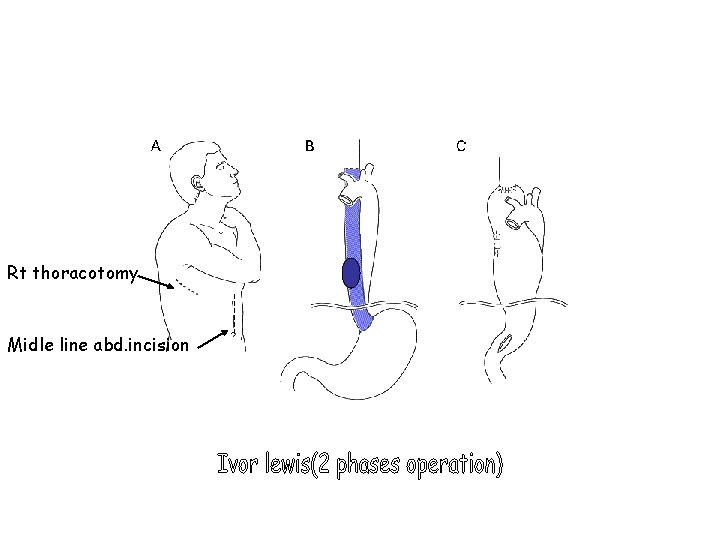
Rt thoracotomy Midle line abd. incision

Gastro-esophageal reflux disease GER is physiological; it only becomes pathological when it is excessive, resulting in symptoms or complication and is then called gastro-esophageal reflux disease GERD Defense Mechanisms against GER I- Lower esophageal sphincter There is high pressure zone at the lower 3 -4 cm of the oesophagus; due to n. Physiological factor continuous release of acetyl choline by the vagus nerve n. Anatomical Factors n. Intrabdominal part of the oesophagus n. Pinchcock action of right crus of diaphragm n. The mucosal rosette n. The GE mucosal fold: forms a flap valve
The mean pressure at this zone is about 25 mm. Hg. n The resting intragastric pressure is 7 mm. Hg n This pressure gradient (25 -7 mm. Hg) prevents reflux The pressure of LOS falls to equal gastric pressure on swallowing and also it is abolished for short periods during the day allowing physiological reflux to occur. II- Esophageal acid clearance Esophageal clearance depends on: n Volume of refluxed material n Salivary Secretion: rich in bicarbonate which neutralize the acid n Gravity n Esophageal motility swallow-induced primary peristalsis is the main mechanism for esophageal clearance. n
aided by secondary peristalsis in response to esophageal distension Propagation of peristalsis is the main factor which determines clearance Propagation is diminished or absent in achalasia, scleroderma and diffuse esophageal spasm.
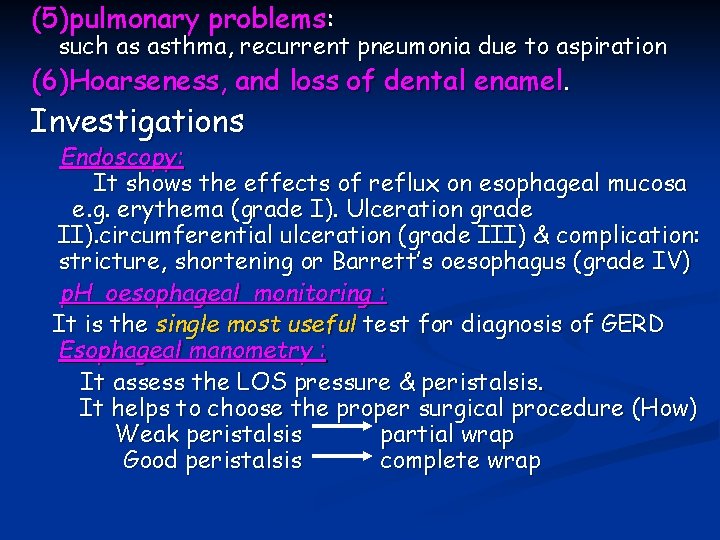
§Symptoms of GERD Typical symptoms : (1) Heartburn is the most common symptom associated with GERD. (2) Regurgitation is another common symptom of GERD exacerbated by lying flat or bending over It may lead to respiratory complications (Atypical symptom) Atypical symptoms: (3) Chest pain : Angina-like chest pain, sometimes called noncardiac chest pain, is frequently caused by GERD. (4)Dysphagia : due to edema associated with esophagitis associated motility disorder stricture
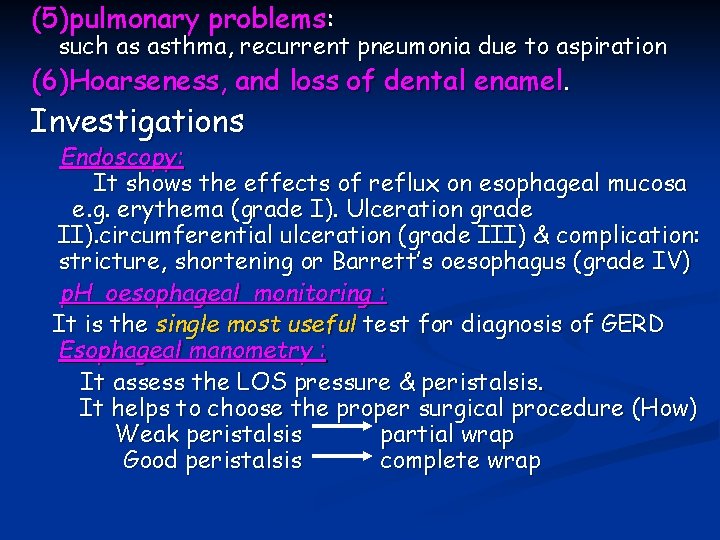
(5)pulmonary problems: such as asthma, recurrent pneumonia due to aspiration (6)Hoarseness, and loss of dental enamel. Investigations Endoscopy: It shows the effects of reflux on esophageal mucosa e. g. erythema (grade I). Ulceration grade II). circumferential ulceration (grade III) & complication: stricture, shortening or Barrett’s oesophagus (grade IV) p. H oesophageal monitoring : It is the single most useful test for diagnosis of GERD Esophageal manometry : It assess the LOS pressure & peristalsis. It helps to choose the proper surgical procedure (How) Weak peristalsis partial wrap Good peristalsis complete wrap
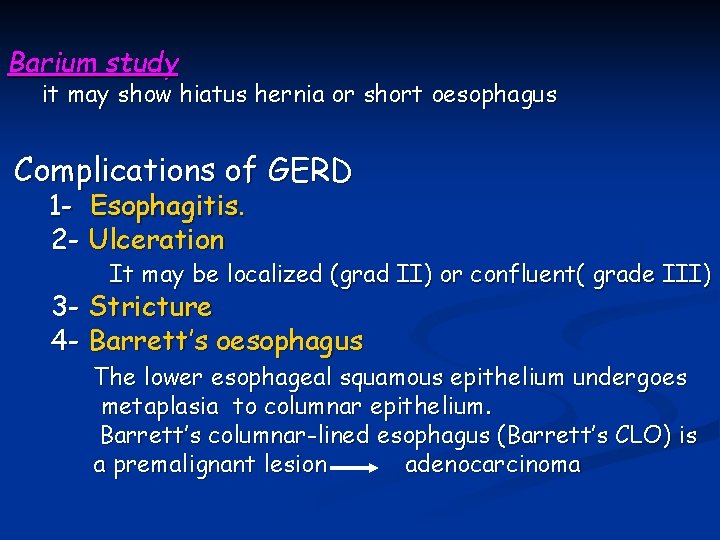
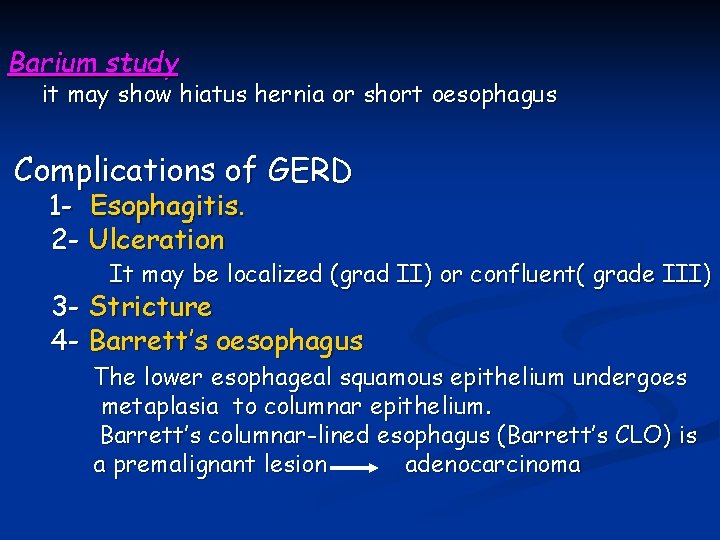
Barium study it may show hiatus hernia or short oesophagus Complications of GERD 1 - Esophagitis. 2 - Ulceration It may be localized (grad II) or confluent( grade III) 3 - Stricture 4 - Barrett’s oesophagus The lower esophageal squamous epithelium undergoes metaplasia to columnar epithelium. Barrett’s columnar-lined esophagus (Barrett’s CLO) is a premalignant lesion adenocarcinoma
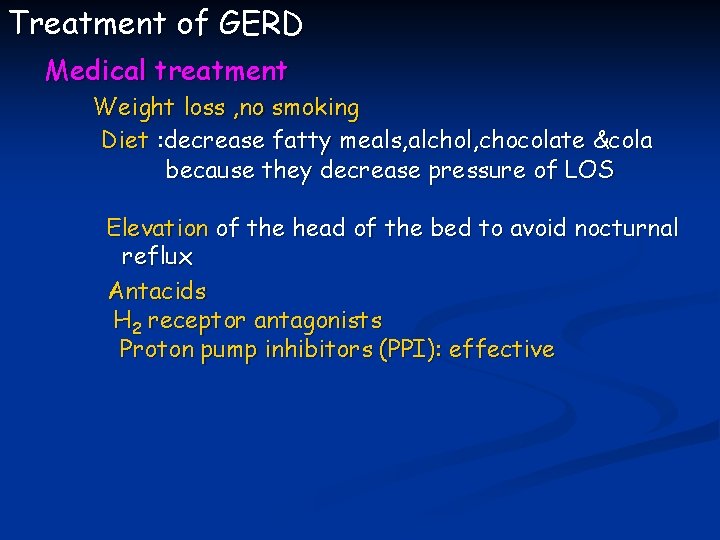
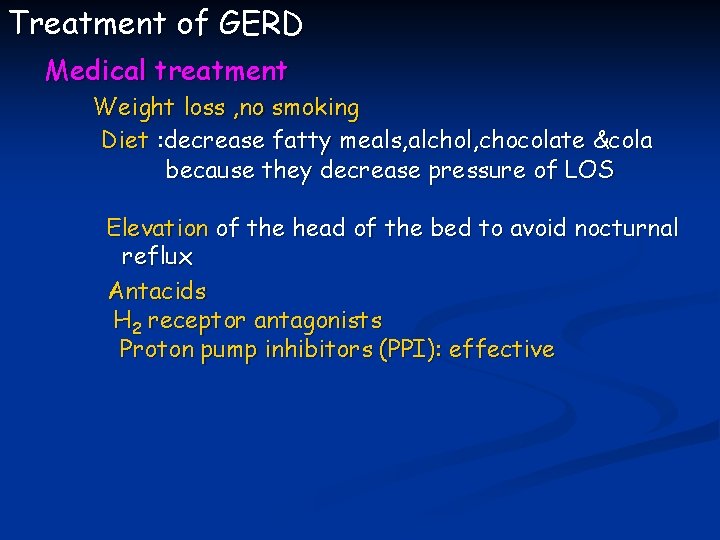
Treatment of GERD Medical treatment Weight loss , no smoking Diet : decrease fatty meals, alchol, chocolate &cola because they decrease pressure of LOS Elevation of the head of the bed to avoid nocturnal reflux Antacids H 2 receptor antagonists Proton pump inhibitors (PPI): effective
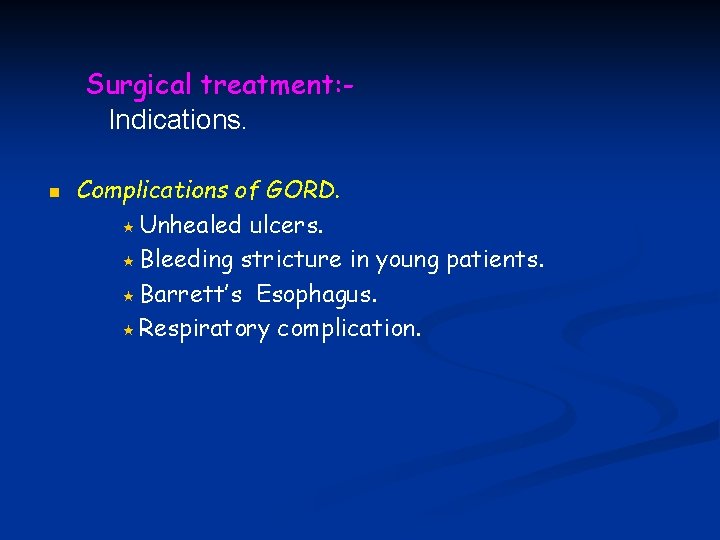
Surgical treatment: Indications. n Complications of GORD. « Unhealed ulcers. « Bleeding stricture in young patients. « Barrett’s Esophagus. « Respiratory complication.
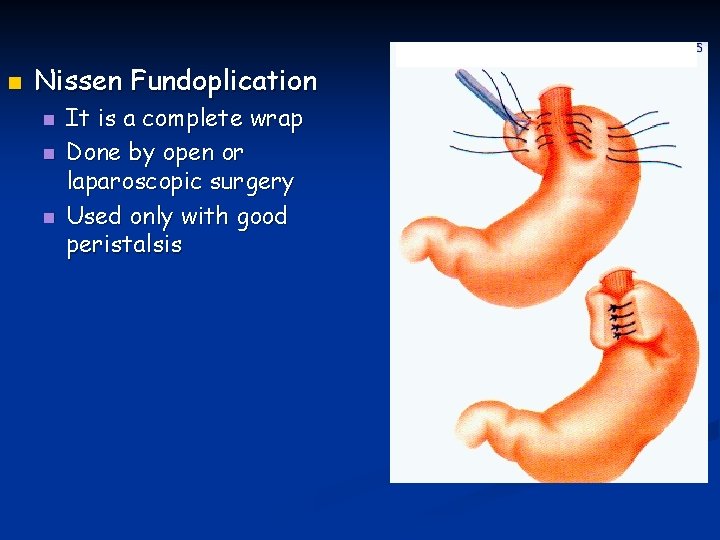
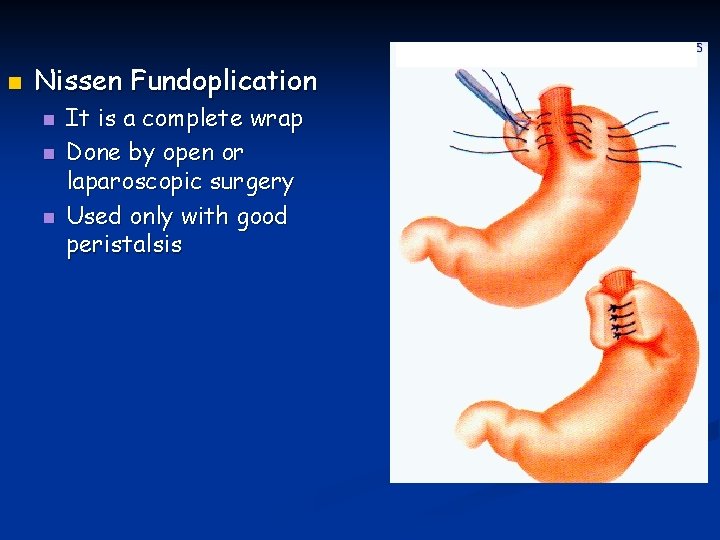
n Nissen Fundoplication n It is a complete wrap Done by open or laparoscopic surgery Used only with good peristalsis
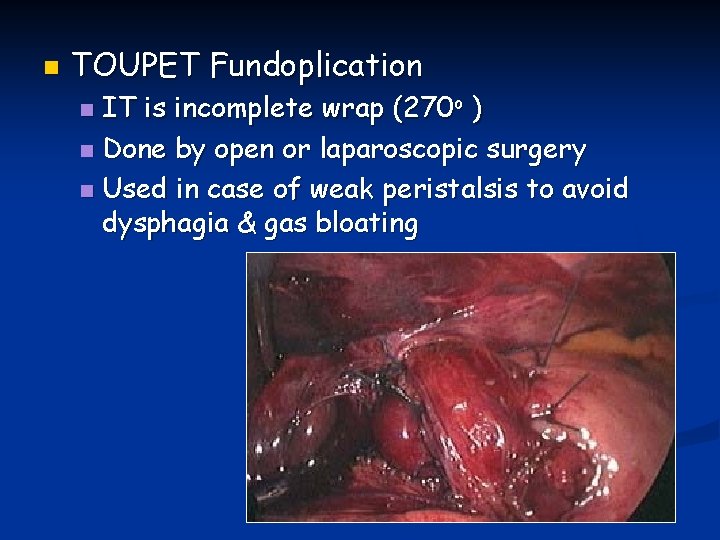
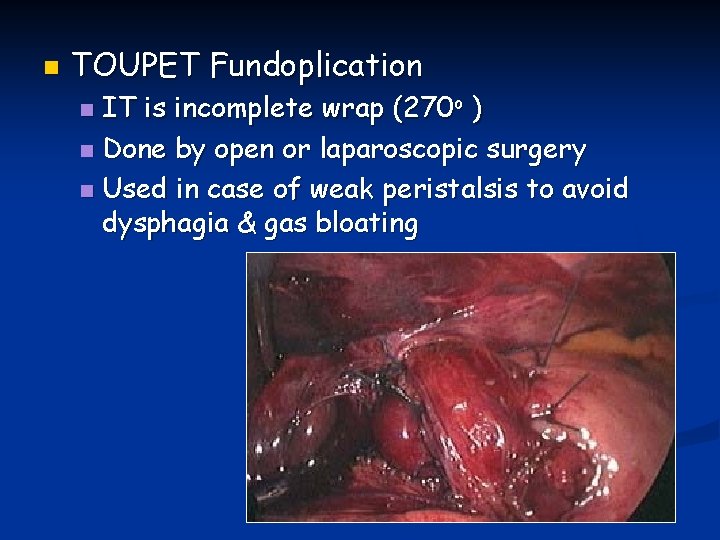
n TOUPET Fundoplication IT is incomplete wrap (270 o ) n Done by open or laparoscopic surgery n Used in case of weak peristalsis to avoid dysphagia & gas bloating n
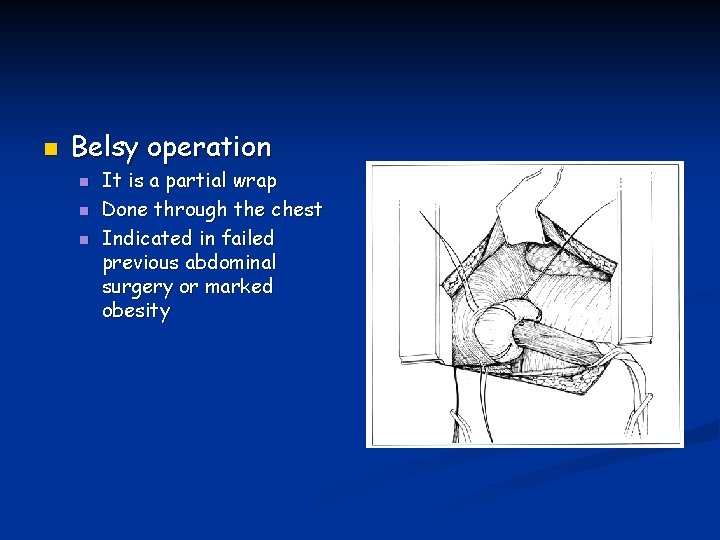
n Belsy operation n It is a partial wrap Done through the chest Indicated in failed previous abdominal surgery or marked obesity

Chemical injury of the esophagus n Target affected: n n Children (accidental ) Adult ( suicidal attempts, psychologically ill patients ) Agents: 1 -Strong acids "sulfuric acid” (certain odor and bad taste) It leads to coagulative necrosis and burn usually superficial. 2 -Alkalies (sodium hydroxide “lye”). It leads to liquifactive necrosis more deep effect perforation with high mortality rate
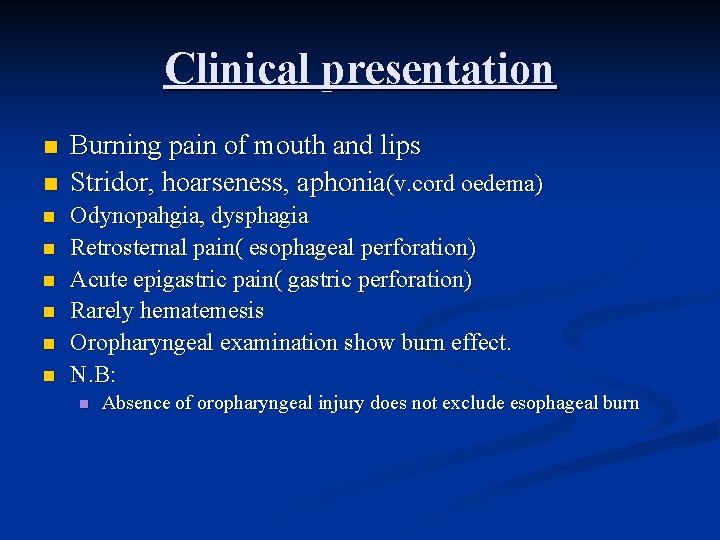
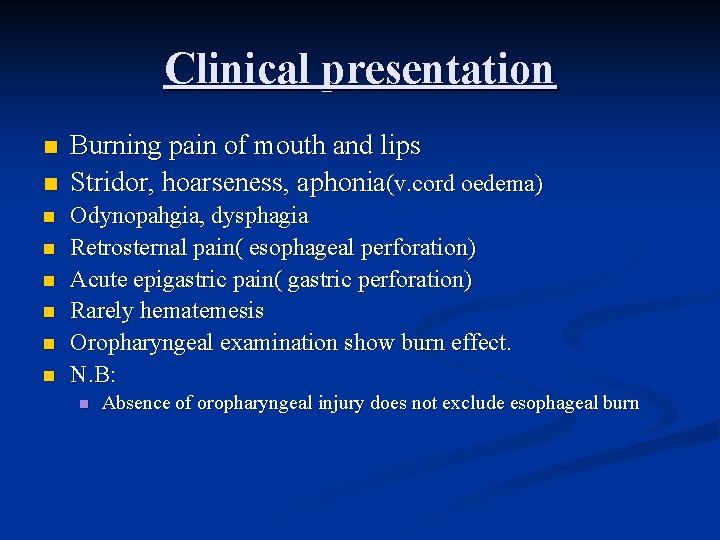
Clinical presentation n n n n Burning pain of mouth and lips Stridor, hoarseness, aphonia(v. cord oedema) Odynopahgia, dysphagia Retrosternal pain( esophageal perforation) Acute epigastric pain( gastric perforation) Rarely hematemesis Oropharyngeal examination show burn effect. N. B: n Absence of oropharyngeal injury does not exclude esophageal burn
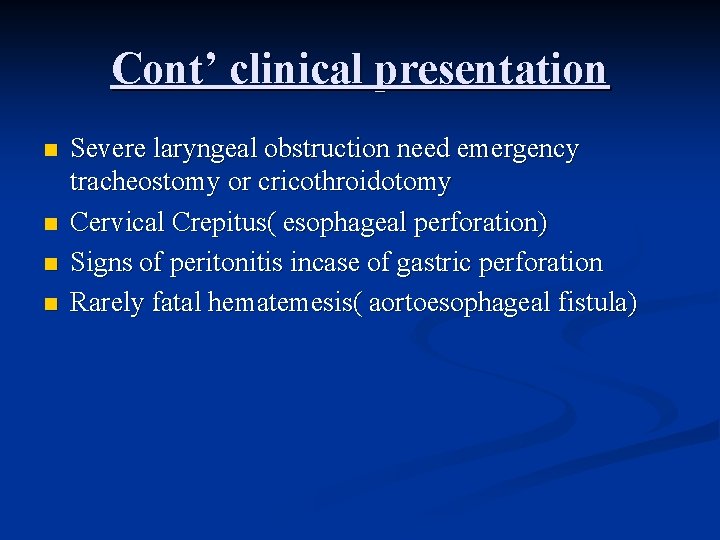
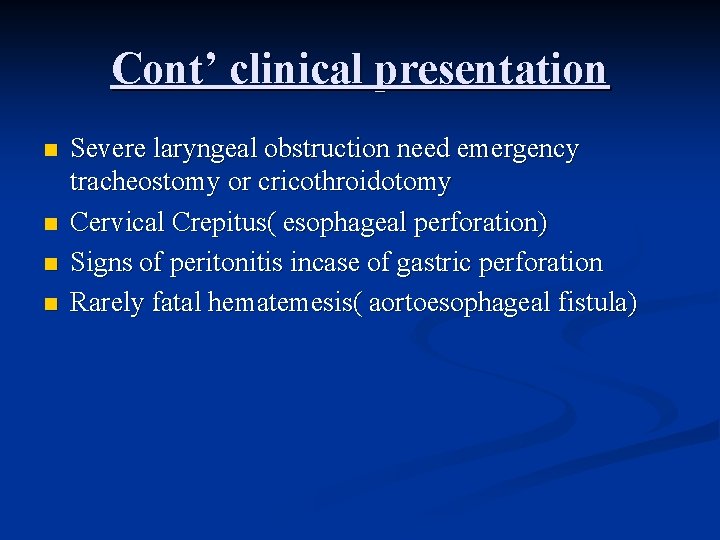
Cont’ clinical presentation n n Severe laryngeal obstruction need emergency tracheostomy or cricothroidotomy Cervical Crepitus( esophageal perforation) Signs of peritonitis incase of gastric perforation Rarely fatal hematemesis( aortoesophageal fistula)
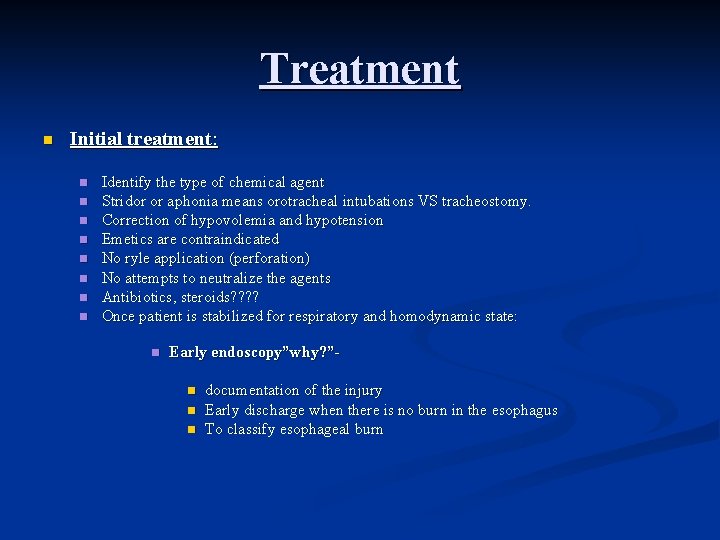
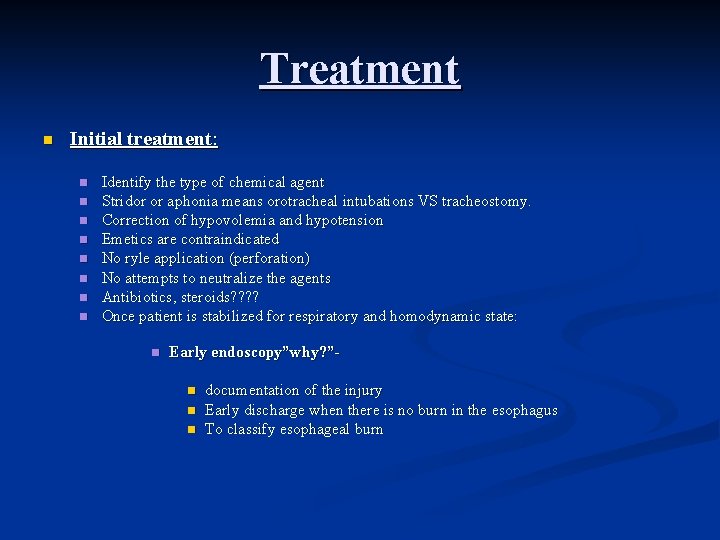
Treatment n Initial treatment: n n n n Identify the type of chemical agent Stridor or aphonia means orotracheal intubations VS tracheostomy. Correction of hypovolemia and hypotension Emetics are contraindicated No ryle application (perforation) No attempts to neutralize the agents Antibiotics, steroids? ? Once patient is stabilized for respiratory and homodynamic state: n Early endoscopy”why? ”n n n documentation of the injury Early discharge when there is no burn in the esophagus To classify esophageal burn
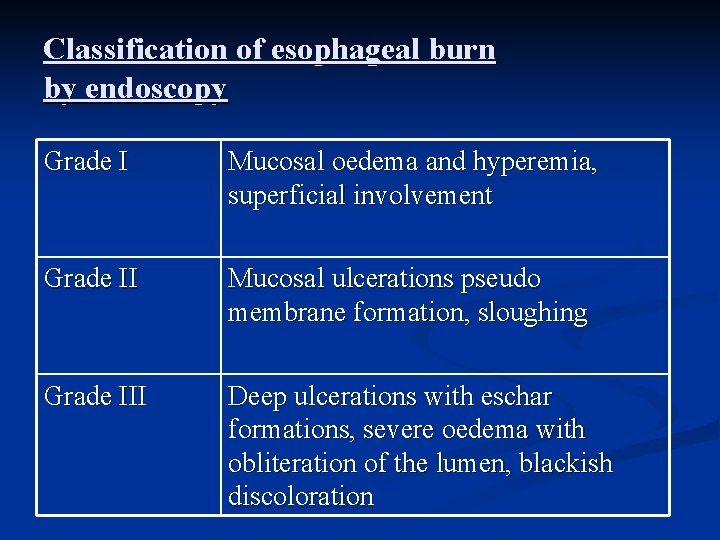
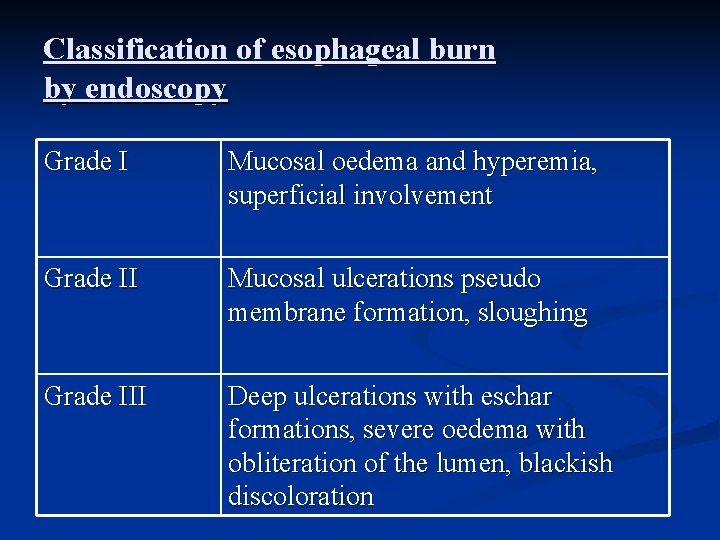
Classification of esophageal burn by endoscopy Grade I Mucosal oedema and hyperemia, superficial involvement Grade II Mucosal ulcerations pseudo membrane formation, sloughing Grade III Deep ulcerations with eschar formations, severe oedema with obliteration of the lumen, blackish discoloration
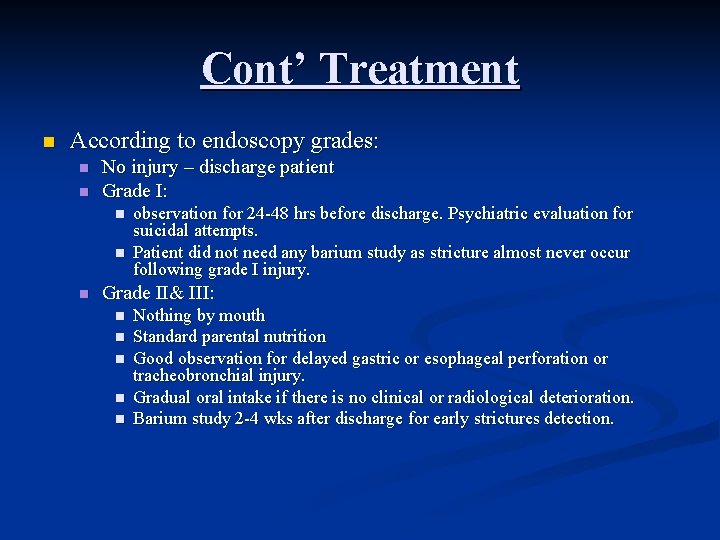
Cont’ Treatment n According to endoscopy grades: n n No injury – discharge patient Grade I: n n n observation for 24 -48 hrs before discharge. Psychiatric evaluation for suicidal attempts. Patient did not need any barium study as stricture almost never occur following grade I injury. Grade II& III: n n n Nothing by mouth Standard parental nutrition Good observation for delayed gastric or esophageal perforation or tracheobronchial injury. Gradual oral intake if there is no clinical or radiological deterioration. Barium study 2 -4 wks after discharge for early strictures detection.
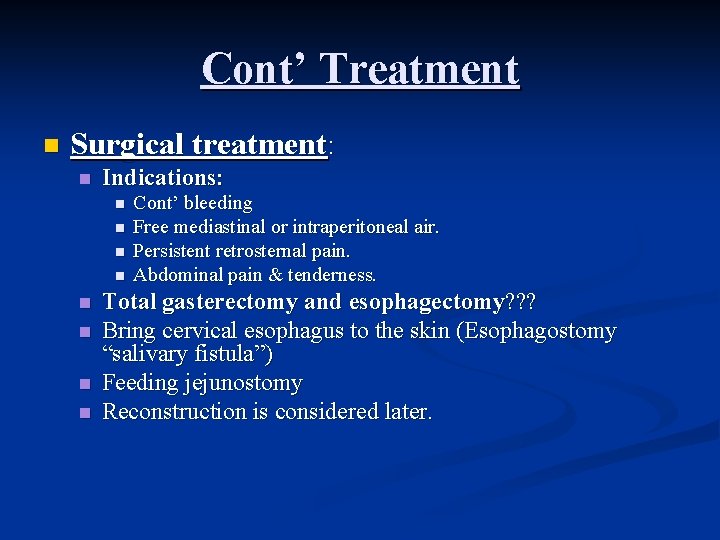
Cont’ Treatment n Surgical treatment: n Indications: n n n n Cont’ bleeding Free mediastinal or intraperitoneal air. Persistent retrosternal pain. Abdominal pain & tenderness. Total gasterectomy and esophagectomy? ? ? Bring cervical esophagus to the skin (Esophagostomy “salivary fistula”) Feeding jejunostomy Reconstruction is considered later.
Delayed complication Strictures n Esophageal carcinoma n
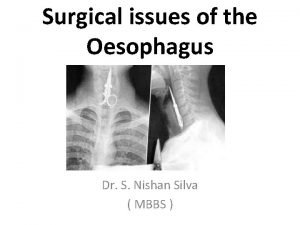
Esophageal perforation Serious condition necessitate prompt diagnosis and treatment
1 -Spontaneous perforation barotrauma “Boerhaave’s syndrome” n Etiology: n n Mechanism: n n Vomiting against closed glottis Esophageal burst due to increase intra esophageal pressure with its content into the mediastinum and pleural cavity Diagnosis: n Should be suspected if chest pain follow vomiting
2 - pathological perforation Perforation of ulcer (Barrett’s ulcer) or tumor of the esophagus. n If it erodes the aorta it will lead to fatal results n
3 - penetrating injuries n n n Perforation by knives and bullet are uncommon (small target surrounded by big organs). 4 -Foreign Bodies Perforation occur during endoscopic removal Foreign body has been left in the esophagus several days, it erodes.
5 - instrumental perforation “iatrogenic” The commonest cause of esophageal perforation. n Commonly rigid endoscopy n Unusual with flexible endoscopy n Dilatation of esophageal benign stricture n Balloon dilatation in achalsia n Insertion of tubes as a palliation of esophageal cancer n
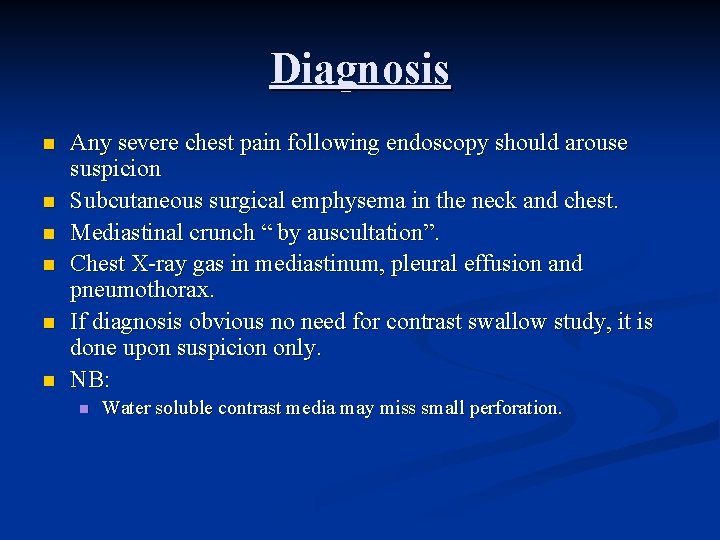
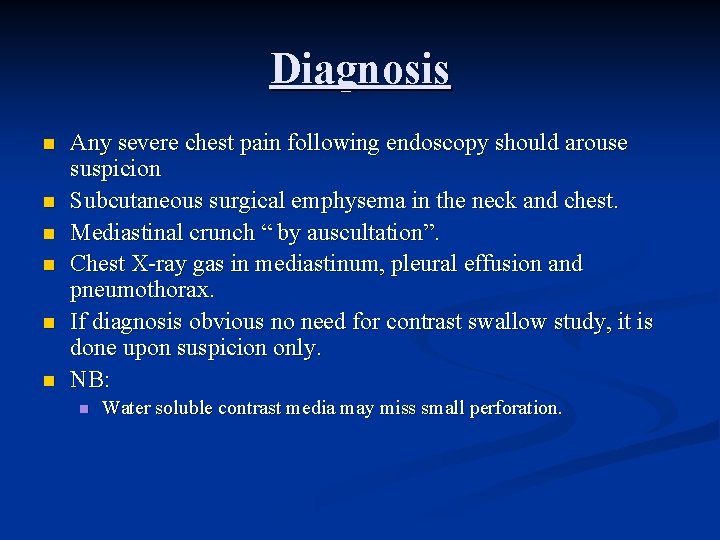
Diagnosis n n n Any severe chest pain following endoscopy should arouse suspicion Subcutaneous surgical emphysema in the neck and chest. Mediastinal crunch “ by auscultation”. Chest X-ray gas in mediastinum, pleural effusion and pneumothorax. If diagnosis obvious no need for contrast swallow study, it is done upon suspicion only. NB: n Water soluble contrast media may miss small perforation.
Treatment The management of esophageal perforation became controversial with strong opinion in favor of operative and non operative treatment. n This depend on the following table: n
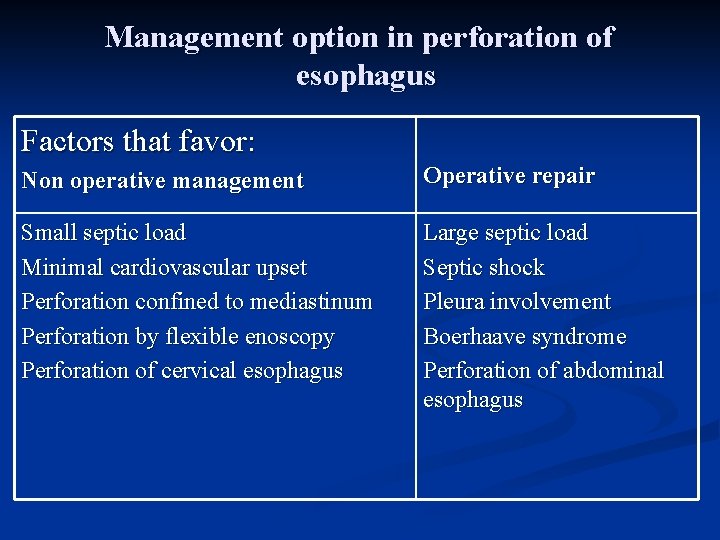
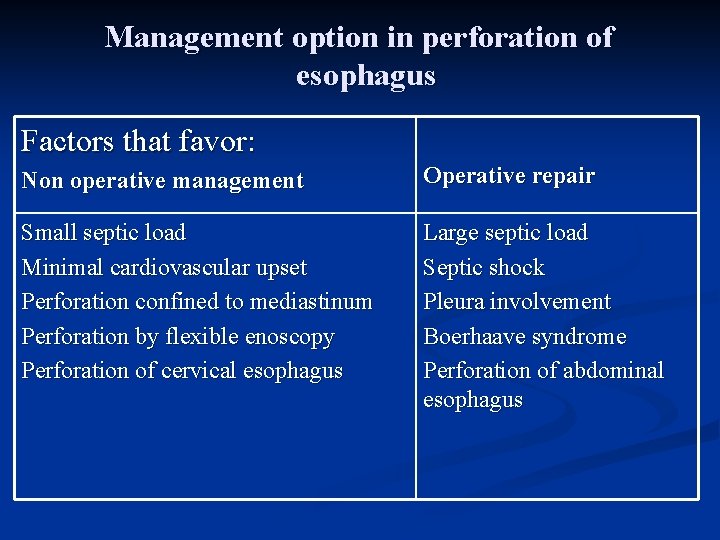
Management option in perforation of esophagus Factors that favor: Non operative management Operative repair Small septic load Minimal cardiovascular upset Perforation confined to mediastinum Perforation by flexible enoscopy Perforation of cervical esophagus Large septic load Septic shock Pleura involvement Boerhaave syndrome Perforation of abdominal esophagus
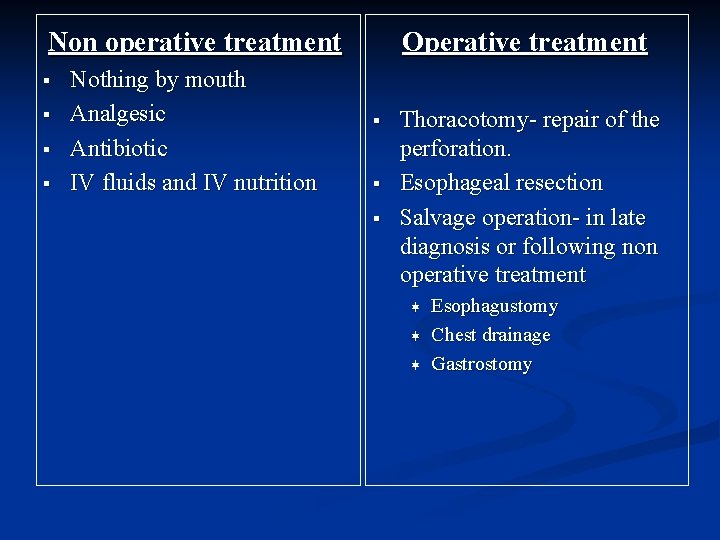
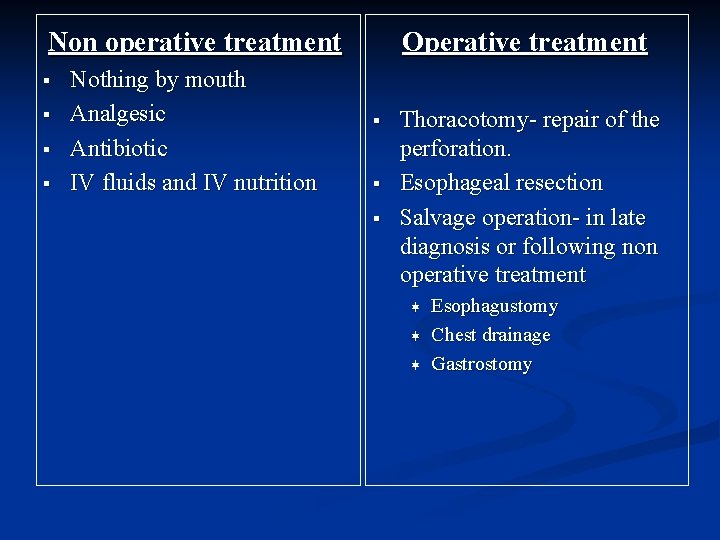
Non operative treatment § § Nothing by mouth Analgesic Antibiotic IV fluids and IV nutrition Operative treatment § § § Thoracotomy- repair of the perforation. Esophageal resection Salvage operation- in late diagnosis or following non operative treatment ¬ ¬ ¬ Esophagustomy Chest drainage Gastrostomy
 Peristaltic contraction
Peristaltic contraction Les in stomach
Les in stomach Abdominal part of esophagus
Abdominal part of esophagus Nutcracker esophagus
Nutcracker esophagus Pancreas anatomy cadaver
Pancreas anatomy cadaver Esophagus
Esophagus Esophagus
Esophagus Peristaltic movement in the esophagus
Peristaltic movement in the esophagus Esophagus stomach small intestine large intestine
Esophagus stomach small intestine large intestine Vitelline duct
Vitelline duct Mouth esophagus stomach intestines
Mouth esophagus stomach intestines Barrett's esophagus
Barrett's esophagus Cardiac in stomach
Cardiac in stomach Rugae in stomach
Rugae in stomach What is this a picture of
What is this a picture of Dr haris manzoor qadri
Dr haris manzoor qadri 4 muscles of pharynx
4 muscles of pharynx Parts of the abdomen
Parts of the abdomen Stomach arteries
Stomach arteries Pvt tim hall
Pvt tim hall Umich
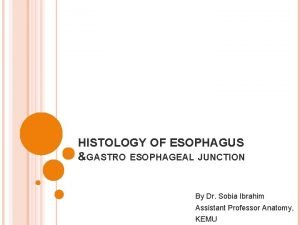
Umich Histology of esophagus
Histology of esophagus Pharynx to esophagus
Pharynx to esophagus Mallory wiess tear
Mallory wiess tear Scleroderma
Scleroderma Varus esophagus
Varus esophagus Stomach location
Stomach location Internal anatomy of a squid
Internal anatomy of a squid Turban epiglottis meaning
Turban epiglottis meaning Esophagus frog function
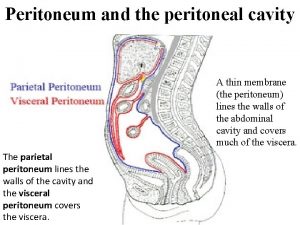
Esophagus frog function Visceral and parietal peritoneum
Visceral and parietal peritoneum Esophagus stomach junction histology
Esophagus stomach junction histology Esophagus wall
Esophagus wall Tư thế ngồi viết
Tư thế ngồi viết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thẻ vin
Thẻ vin Bổ thể
Bổ thể Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Tư thế ngồi viết
Tư thế ngồi viết Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Thứ tự các dấu thăng giáng ở hóa biểu
Thứ tự các dấu thăng giáng ở hóa biểu Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Diễn thế sinh thái là
Diễn thế sinh thái là Công thức tính thế năng
Công thức tính thế năng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Phép trừ bù
Phép trừ bù Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Lời thề hippocrates
Lời thề hippocrates Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể đại từ thay thế
đại từ thay thế Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra