Early Detection of Lung Cancer Dr Shanthi Paramothayan













- Slides: 74
Early Detection of Lung Cancer Dr. Shanthi Paramothayan Consultant Respiratory Physician St. Helier University Hospital 14 th June 2011
Aim and Objectives of this session n Aims and Objectives: Risk Factors: identify high risk patients u Clinical Presentation of lung cancer u Classification of lung cancers u Diagnosis including investigations u Staging of lung cancers u Management u
Benign Lung Tumours Hamartoma n Arterio-venous malformations (AVMs) n Carcinoid tumour n Granuloma n Patients often asymptomatic. Incidental finding on CXR (solitary pulmonary nodule) n Malignancy needs to be excluded n
Importance of Lung Cancer n n n n Incidence: 40, 000 new cases of lung cancer /year Leading cause of cancer death world wide Third commonest cause of death in UK 32, 000 deaths/year North South divide: higher prevalence in North Higher in lower socio economic groups with age Commoner in men but in women
Risk Factors for Lung Cancer n n n n Smoking (pack yrs), early onset worse u latent period of 30 years Passive smoking (early exposure) Asbestos u latent period of 30 -40 years Radiation Arsenic Coal tar Petroleum products Family History (genetic factors) Scar tissue
Poor Prognosis in Lung Cancer WHY? No significant improvement in mortality for many years
Poor Prognosis in Lung Cancer n Why? u No screening for lung cancer u Late presentation u Insufficient resources/emphasis towards Smoking Cessation u Poor surgical rates (10 -15% v 20% in USA) u Co-morbidity: limits treatment options How can we improve mortality in lung cancer in the 21 st Century?
What do you think……. ? Should cigarettes be banned? u What else can we do to stop smoking? u Should we screen for lung cancer? u How can we improve early referral for suspected lung cancer? u How can we improve referral for surgery – hence improve curative rates? u
Smoking Cessation Stop children/teenagers from starting to smoke: how? n Stop current smokers n Education n Political willingness: smoking ban n Resources: smoking cessation clinics n n Doctors: Advise strongly, refer to smoking cessation clinic, prescribe NRT
Screening For Lung Cancer How? CXR, CT thorax ? Mobile units n How Often? yearly? n In what population? Smokers? Family history? n False positives and false negatives n Cost effective? n
Case 1 50 year old Asian man n 30 pack year history of smoking n Strong family history of malignancy n Persistent cough for > 6 months n Frequent visits to GP: several course of antibiotics n Admitted to St. Helier Hospital with haemoptysis and weight loss n Cervical lymphadenopathy, clubbed n


Case 1 Tumour seen right upper lobe and right intermediate bronchus as Bronchoscopy n Poorly differentiated adenocarcinoma n Referred to RMH: Stage 4 disease, so palliative chemotherapy only n n Early chest X-ray and referral after onset of symptoms may have made a difference !
Case 2 40 year old woman, non smoker n Persistent productive cough despite several courses of antibiotics n CXR abnormality: not resolving after several weeks n Admitted to hospital with severe SOB and chest pain n Found to have extensive CXR changes and pericardial effusion n


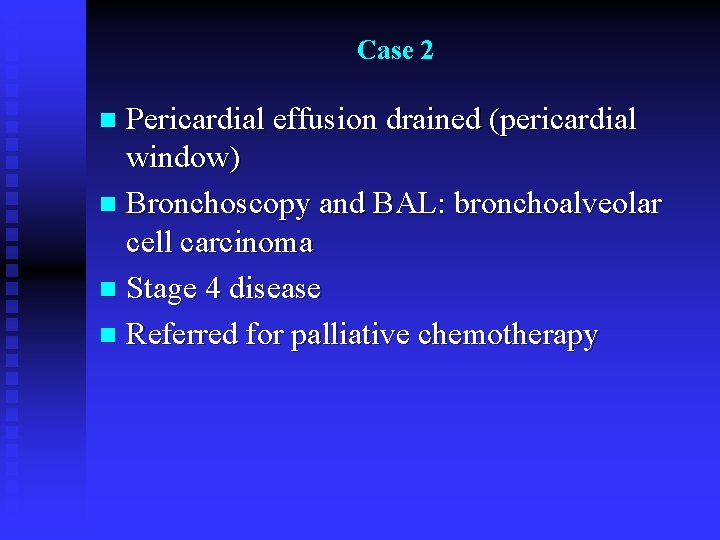
Case 2 Pericardial effusion drained (pericardial window) n Bronchoscopy and BAL: bronchoalveolar cell carcinoma n Stage 4 disease n Referred for palliative chemotherapy n
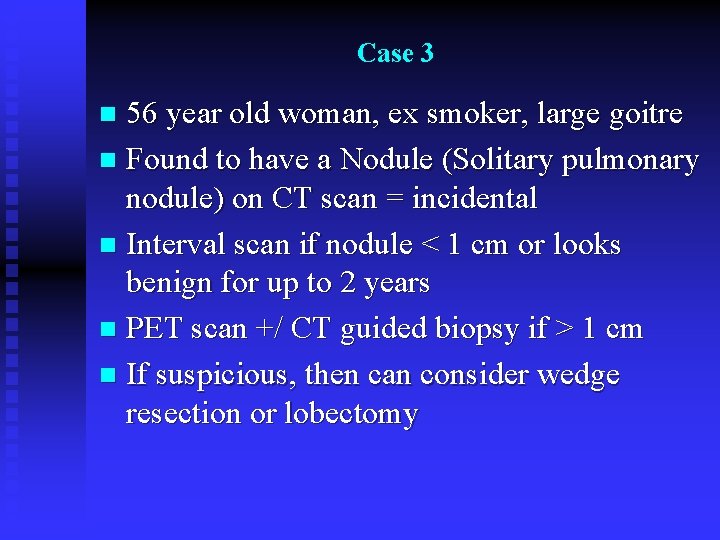
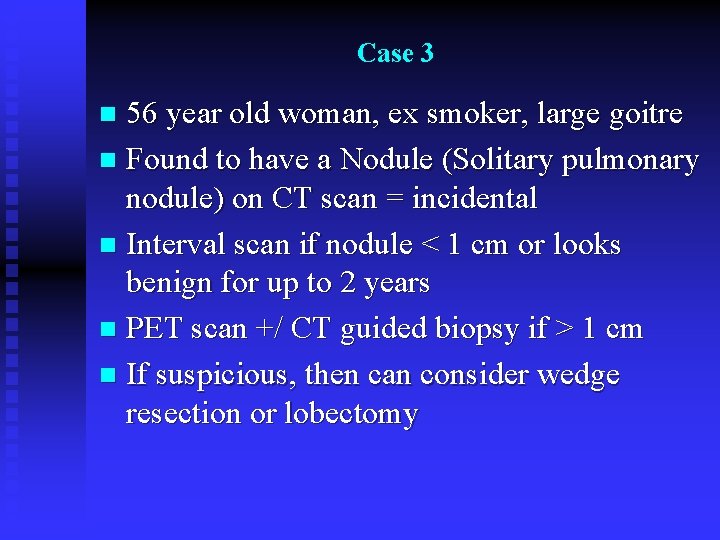
Case 3 56 year old woman, ex smoker, large goitre n Found to have a Nodule (Solitary pulmonary nodule) on CT scan = incidental n Interval scan if nodule < 1 cm or looks benign for up to 2 years n PET scan +/ CT guided biopsy if > 1 cm n If suspicious, then can consider wedge resection or lobectomy n

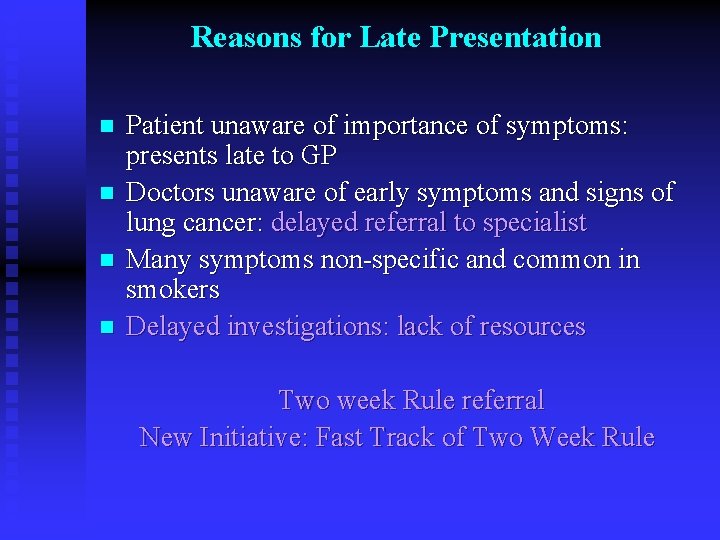
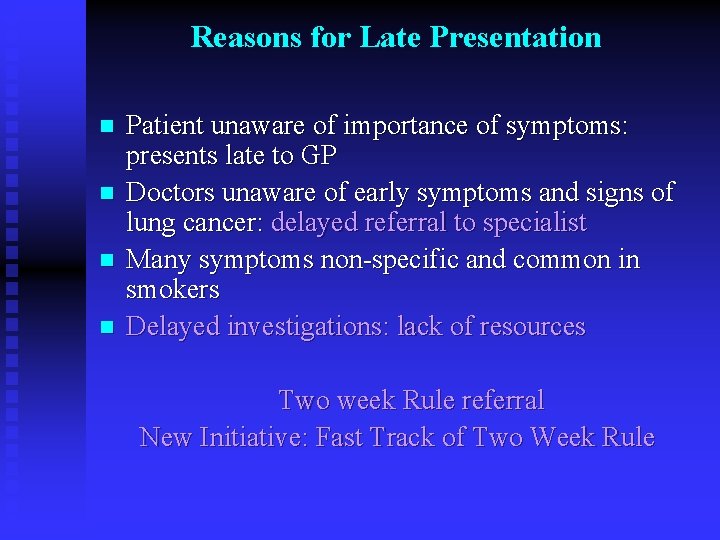
Reasons for Late Presentation n n Patient unaware of importance of symptoms: presents late to GP Doctors unaware of early symptoms and signs of lung cancer: delayed referral to specialist Many symptoms non-specific and common in smokers Delayed investigations: lack of resources Two week Rule referral New Initiative: Fast Track of Two Week Rule
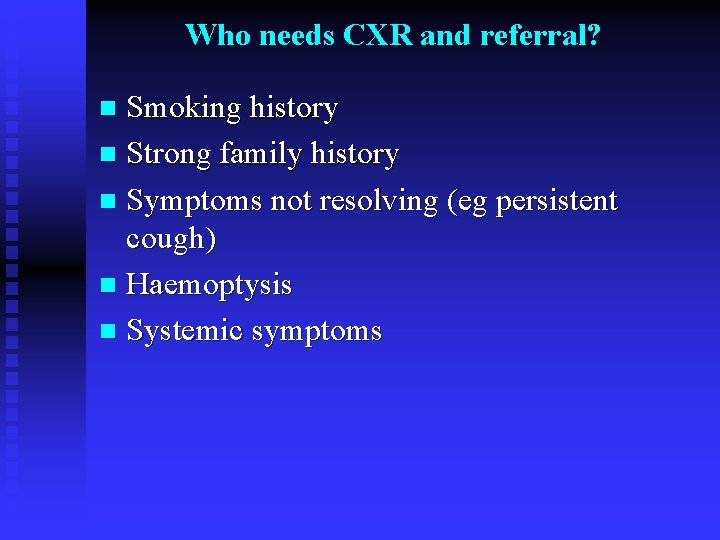
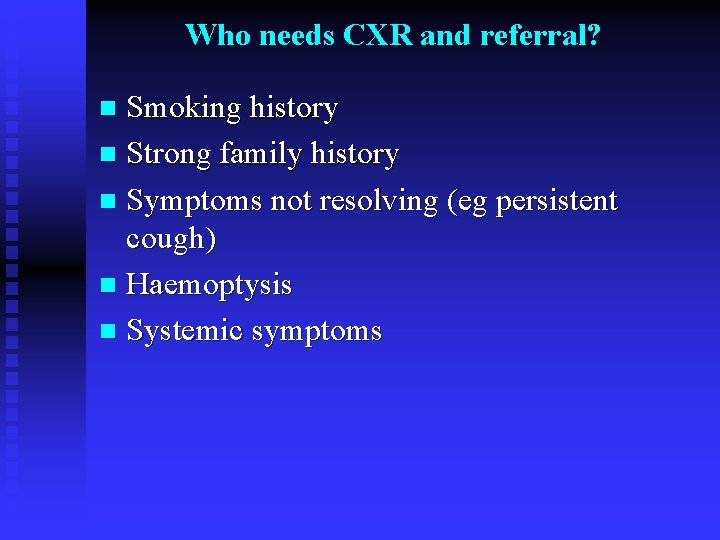
Who needs CXR and referral? Smoking history n Strong family history n Symptoms not resolving (eg persistent cough) n Haemoptysis n Systemic symptoms n
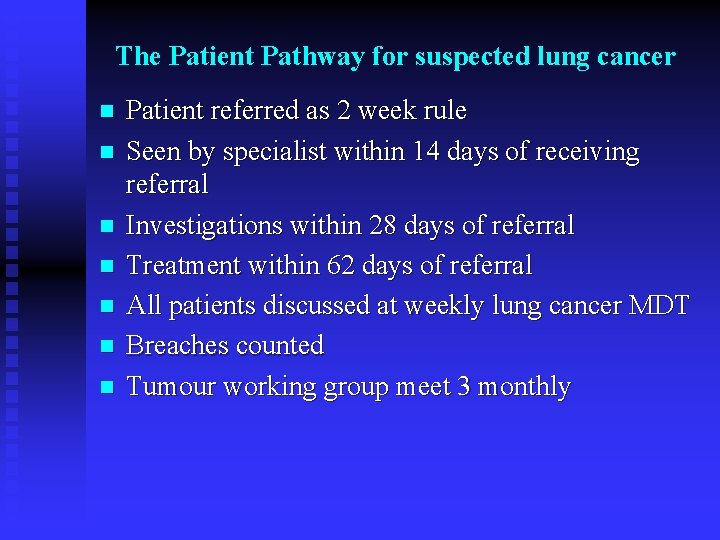
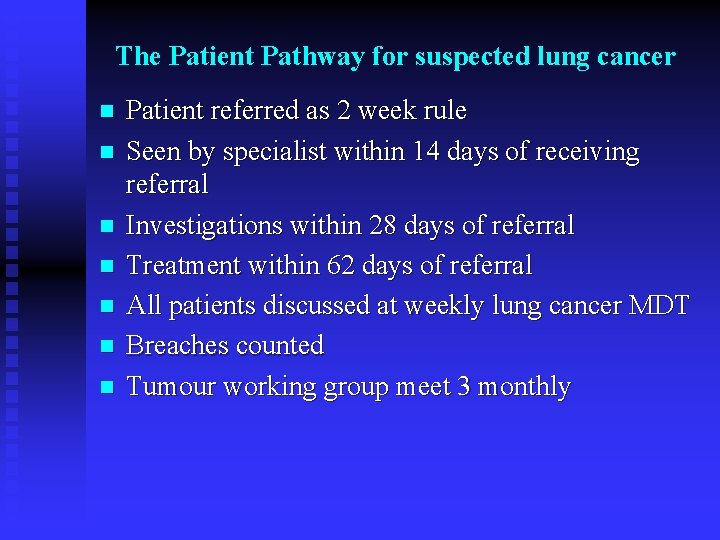
The Patient Pathway for suspected lung cancer n n n n Patient referred as 2 week rule Seen by specialist within 14 days of receiving referral Investigations within 28 days of referral Treatment within 62 days of referral All patients discussed at weekly lung cancer MDT Breaches counted Tumour working group meet 3 monthly
Reasons for poor surgical rates in UK n Late presentation n Co-morbidity: IHD, COPD
Clinical Presentation of Lung Cancer What is the commonest symptom? n What sort of patients should you be worried about? n Is there a problem with you getting CXR? n Do you have a problem referring patients to a respiratory consultant? n
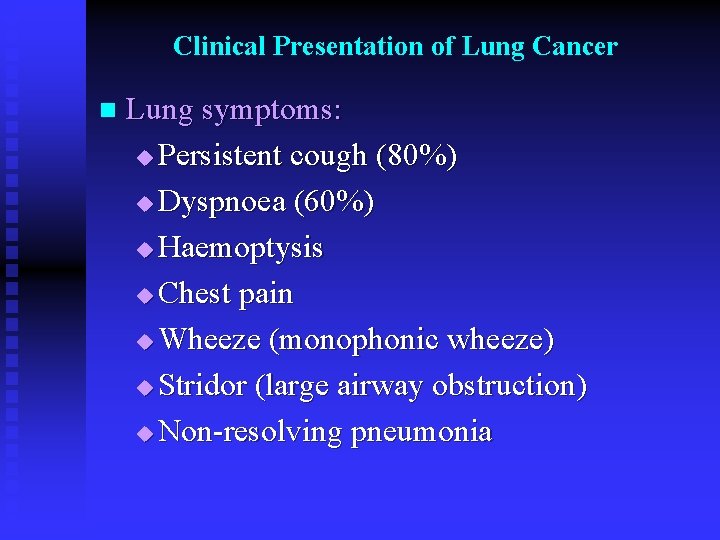
Clinical Presentation of Lung Cancer n Lung symptoms: u Persistent cough (80%) u Dyspnoea (60%) u Haemoptysis u Chest pain u Wheeze (monophonic wheeze) u Stridor (large airway obstruction) u Non-resolving pneumonia
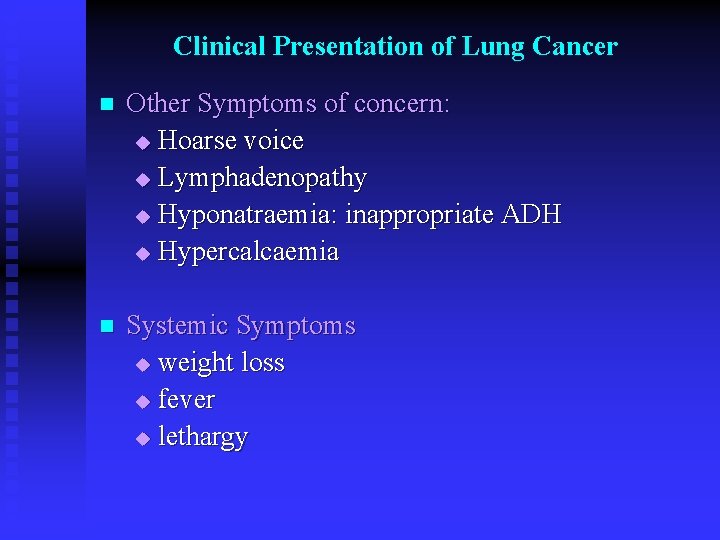
Clinical Presentation of Lung Cancer n Other Symptoms of concern: u Hoarse voice u Lymphadenopathy u Hyponatraemia: inappropriate ADH u Hypercalcaemia n Systemic Symptoms u weight loss u fever u lethargy
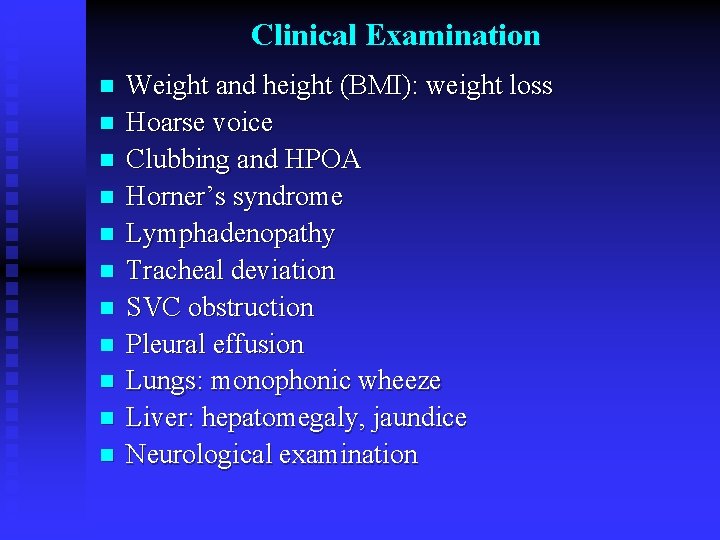
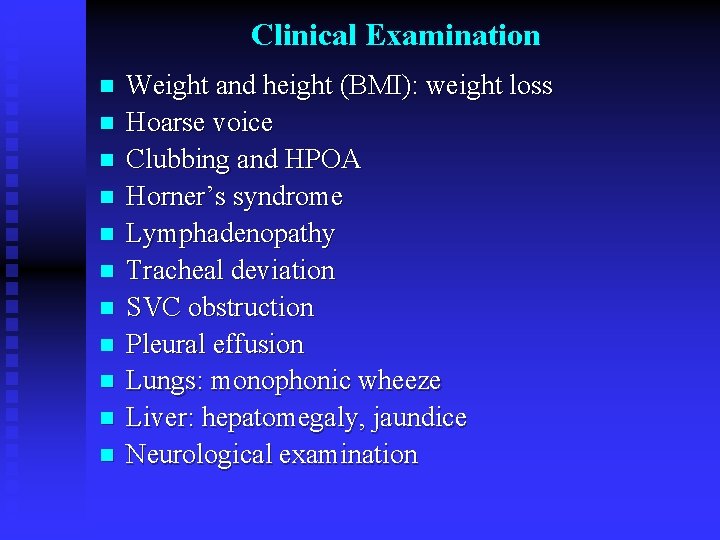
Clinical Examination n n Weight and height (BMI): weight loss Hoarse voice Clubbing and HPOA Horner’s syndrome Lymphadenopathy Tracheal deviation SVC obstruction Pleural effusion Lungs: monophonic wheeze Liver: hepatomegaly, jaundice Neurological examination
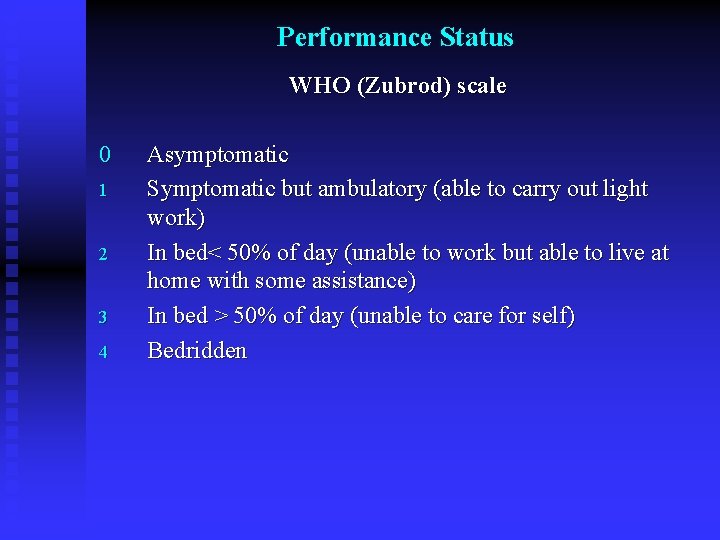
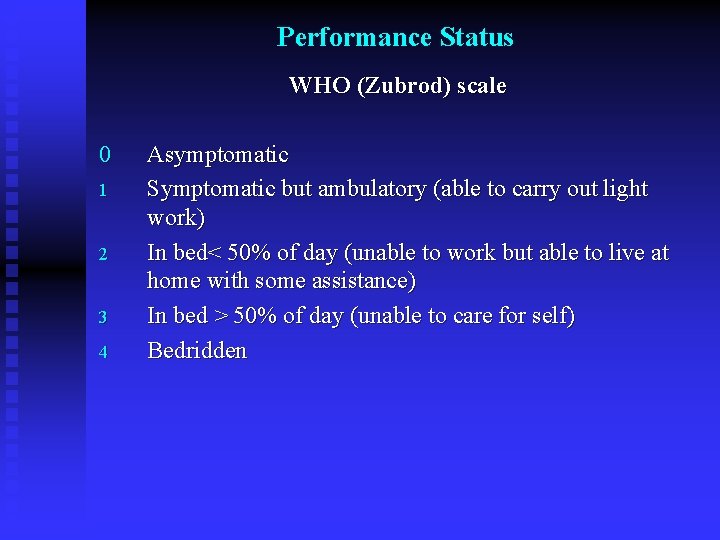
Performance Status WHO (Zubrod) scale 0 1 2 3 4 Asymptomatic Symptomatic but ambulatory (able to carry out light work) In bed< 50% of day (unable to work but able to live at home with some assistance) In bed > 50% of day (unable to care for self) Bedridden
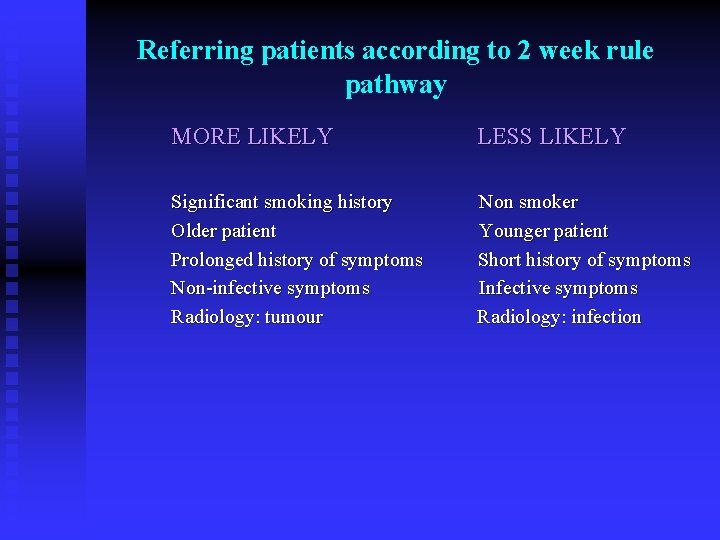
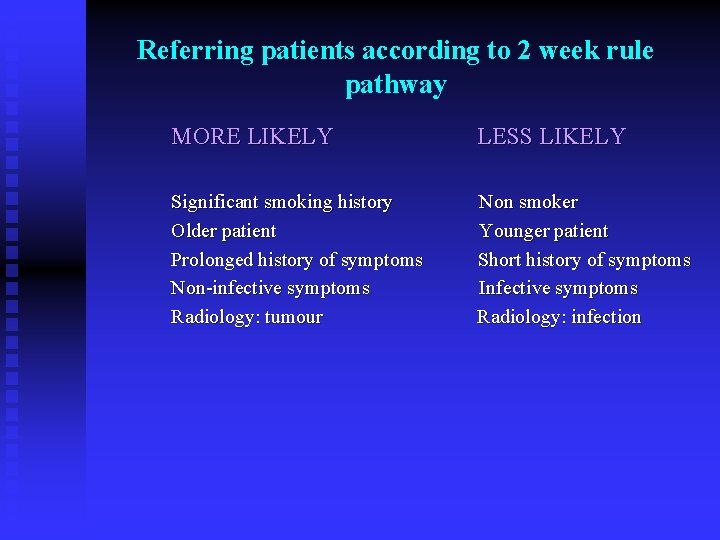
Referring patients according to 2 week rule pathway MORE LIKELY LESS LIKELY Significant smoking history Older patient Prolonged history of symptoms Non-infective symptoms Radiology: tumour Non smoker Younger patient Short history of symptoms Infective symptoms Radiology: infection
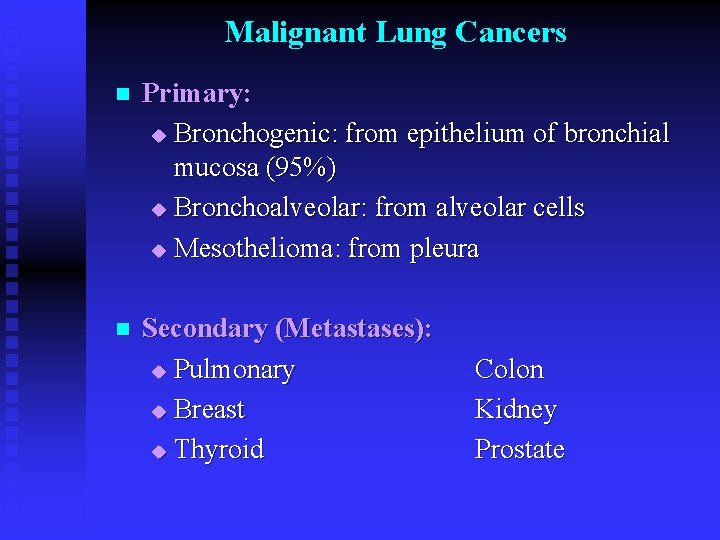
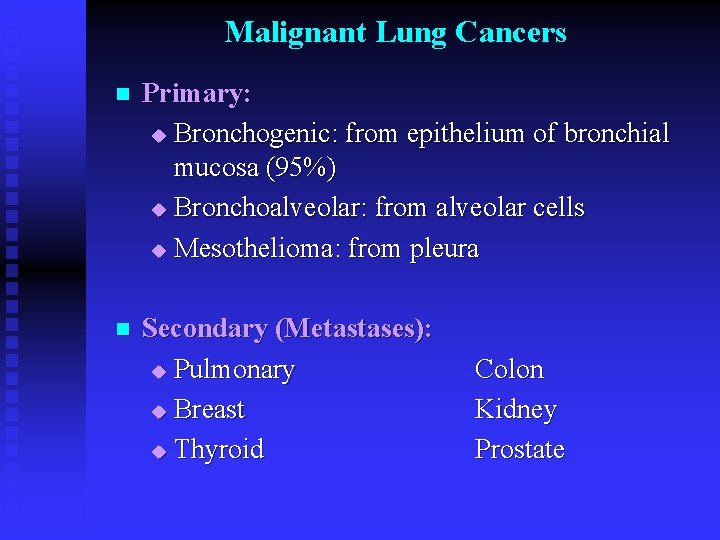
Malignant Lung Cancers n Primary: u Bronchogenic: from epithelium of bronchial mucosa (95%) u Bronchoalveolar: from alveolar cells u Mesothelioma: from pleura n Secondary (Metastases): u Pulmonary u Breast u Thyroid Colon Kidney Prostate
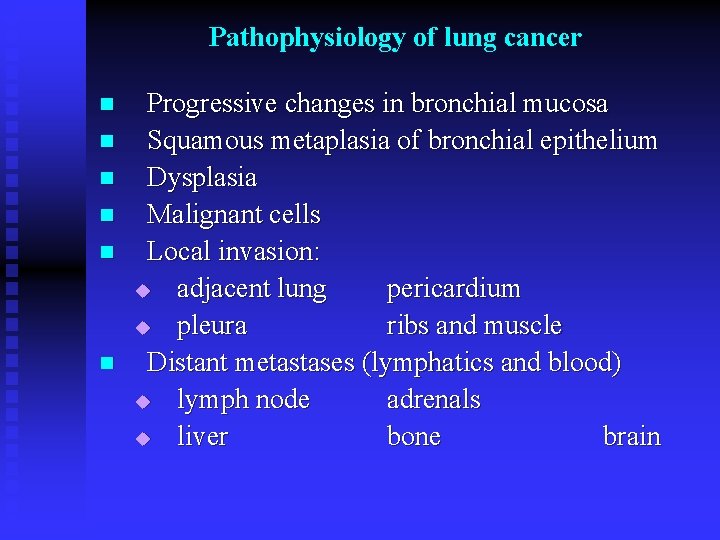
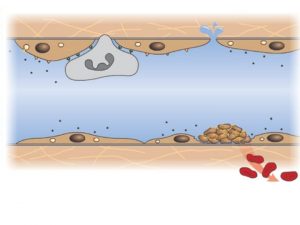
Pathophysiology of lung cancer n n n Progressive changes in bronchial mucosa Squamous metaplasia of bronchial epithelium Dysplasia Malignant cells Local invasion: u adjacent lung pericardium u pleura ribs and muscle Distant metastases (lymphatics and blood) u lymph node adrenals u liver bone brain
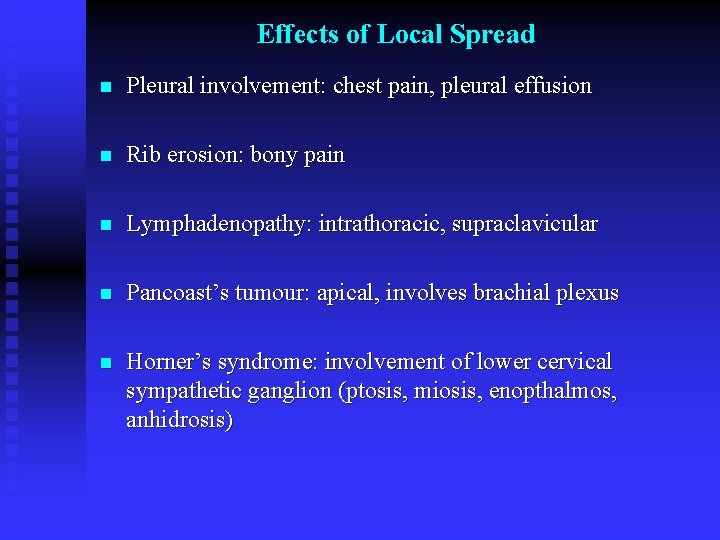
Effects of Local Spread n Pleural involvement: chest pain, pleural effusion n Rib erosion: bony pain n Lymphadenopathy: intrathoracic, supraclavicular n Pancoast’s tumour: apical, involves brachial plexus n Horner’s syndrome: involvement of lower cervical sympathetic ganglion (ptosis, miosis, enopthalmos, anhidrosis)
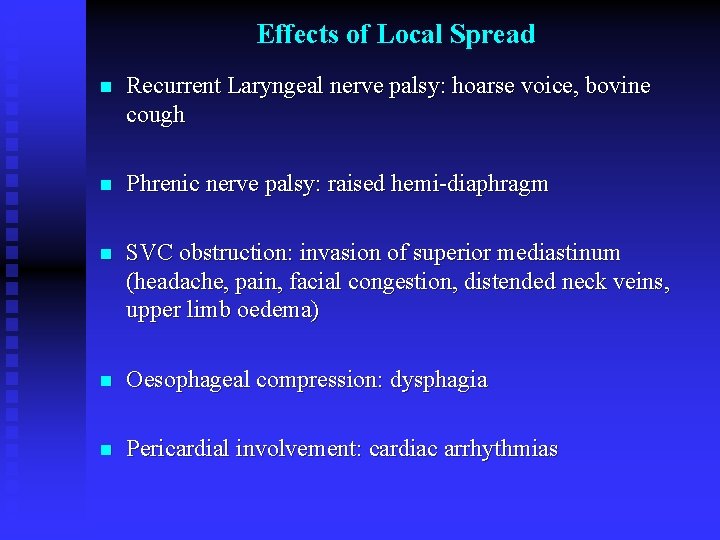
Effects of Local Spread n Recurrent Laryngeal nerve palsy: hoarse voice, bovine cough n Phrenic nerve palsy: raised hemi-diaphragm n SVC obstruction: invasion of superior mediastinum (headache, pain, facial congestion, distended neck veins, upper limb oedema) n Oesophageal compression: dysphagia n Pericardial involvement: cardiac arrhythmias
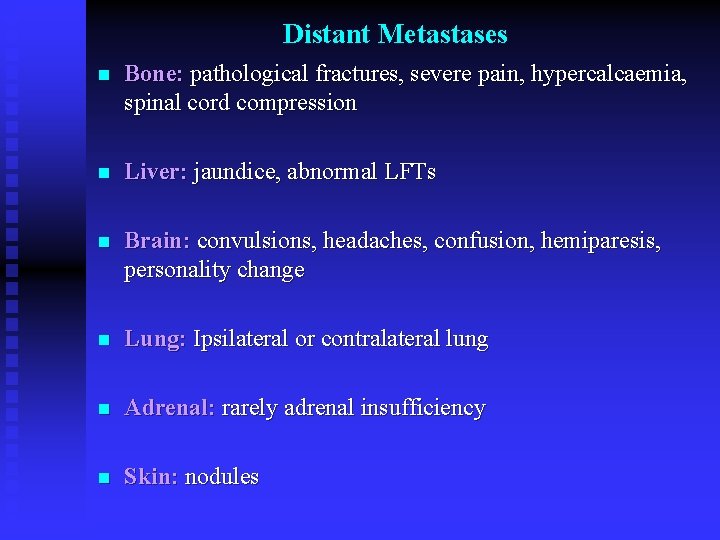
Distant Metastases n Bone: pathological fractures, severe pain, hypercalcaemia, spinal cord compression n Liver: jaundice, abnormal LFTs n Brain: convulsions, headaches, confusion, hemiparesis, personality change n Lung: Ipsilateral or contralateral lung n Adrenal: rarely adrenal insufficiency n Skin: nodules
Bronchogenic Lung Cancer n n Non small cell lung cancer (NSCLC): u Squamous cell carcinoma u Adenocarcinoma u Large cell (undifferentiated) Small cell lung cancer (SCLC)
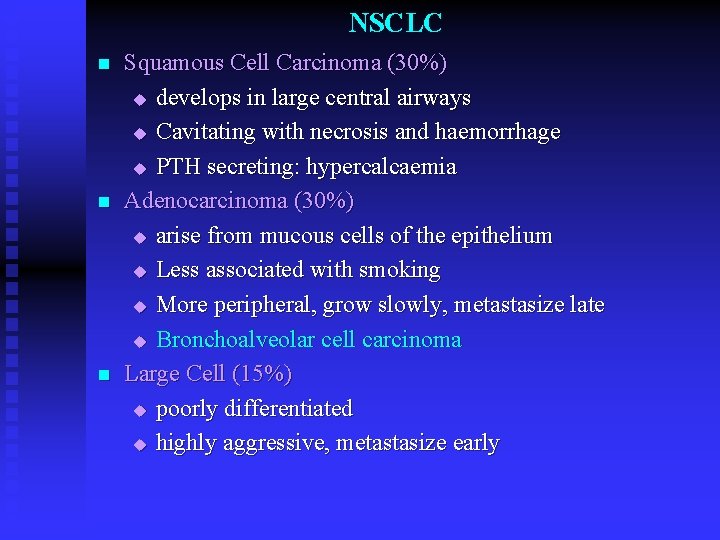
NSCLC n n n Squamous Cell Carcinoma (30%) u develops in large central airways u Cavitating with necrosis and haemorrhage u PTH secreting: hypercalcaemia Adenocarcinoma (30%) u arise from mucous cells of the epithelium u Less associated with smoking u More peripheral, grow slowly, metastasize late u Bronchoalveolar cell carcinoma Large Cell (15%) u poorly differentiated u highly aggressive, metastasize early
SCLC n n n Also known as “oat cell carcinoma” 25% of all lung cancers Arise from the Kulchitsky cells (endocrine cells): part of APUD Secrete polypeptide hormones Highly aggressive, grows rapidly and metastasizes early Very poor prognosis
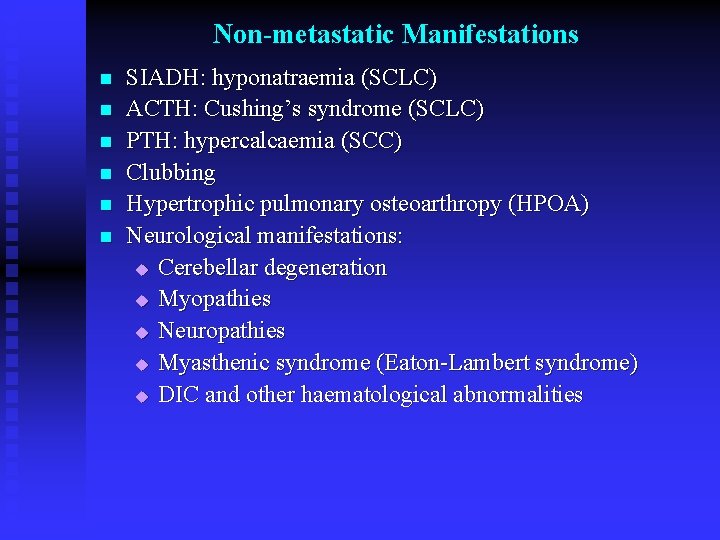
Non-metastatic Manifestations n n n SIADH: hyponatraemia (SCLC) ACTH: Cushing’s syndrome (SCLC) PTH: hypercalcaemia (SCC) Clubbing Hypertrophic pulmonary osteoarthropy (HPOA) Neurological manifestations: u Cerebellar degeneration u Myopathies u Neuropathies u Myasthenic syndrome (Eaton-Lambert syndrome) u DIC and other haematological abnormalities

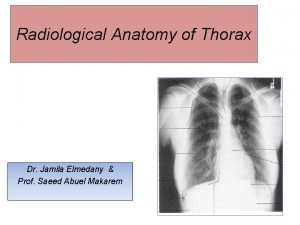
Investigations n Radiology: u CXR u Staging CT scan (thorax and abdomen) u Brain CT scan (neurological symptoms or signs) u MRI scan (nerve/rib involvement, sc compression) u Bone scan (bone pain, hypercalcaemia) u PET scan (staging)


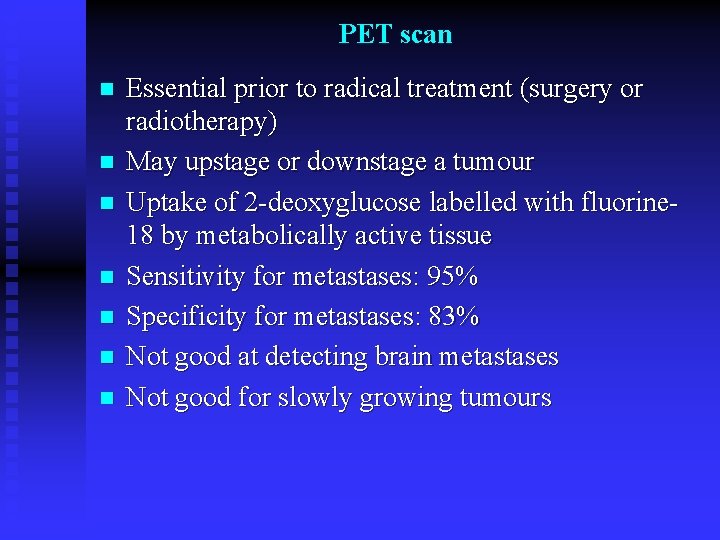
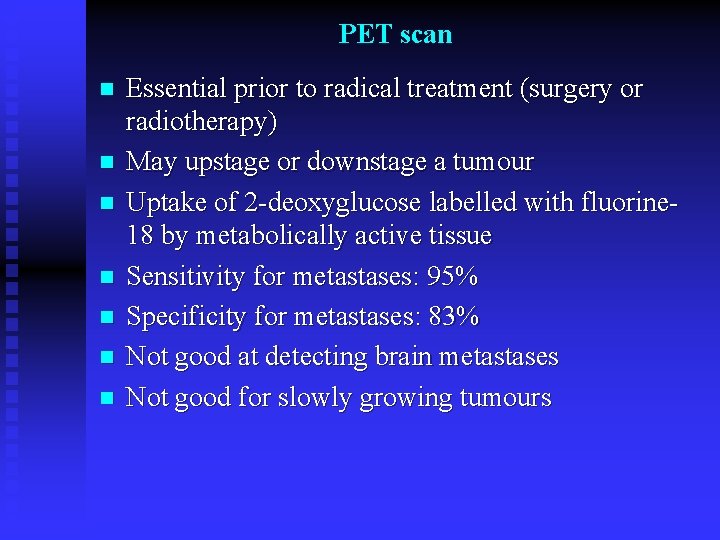
PET scan n n n Essential prior to radical treatment (surgery or radiotherapy) May upstage or downstage a tumour Uptake of 2 -deoxyglucose labelled with fluorine 18 by metabolically active tissue Sensitivity for metastases: 95% Specificity for metastases: 83% Not good at detecting brain metastases Not good for slowly growing tumours

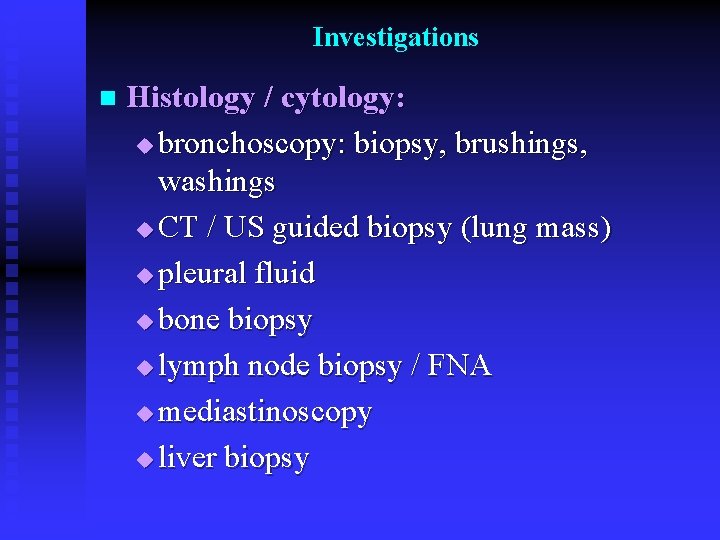
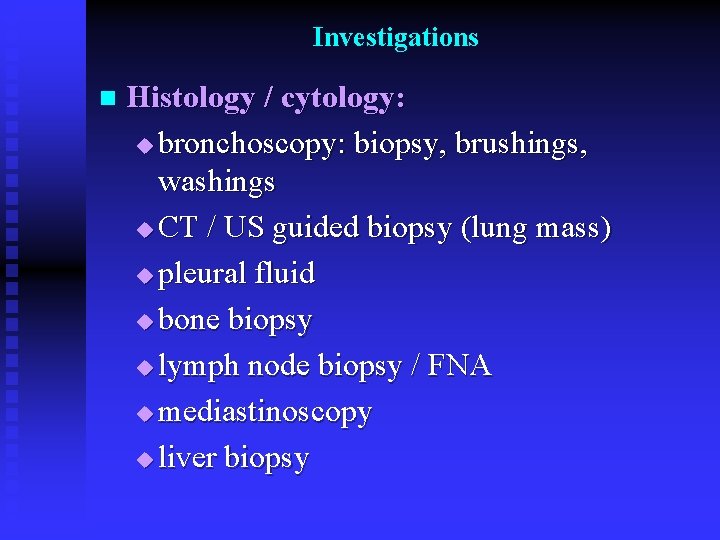
Investigations n Histology / cytology: u bronchoscopy: biopsy, brushings, washings u CT / US guided biopsy (lung mass) u pleural fluid u bone biopsy u lymph node biopsy / FNA u mediastinoscopy u liver biopsy

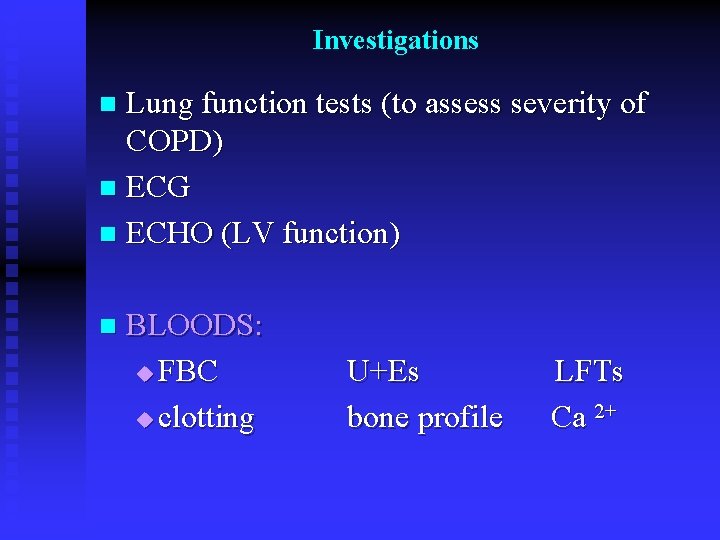
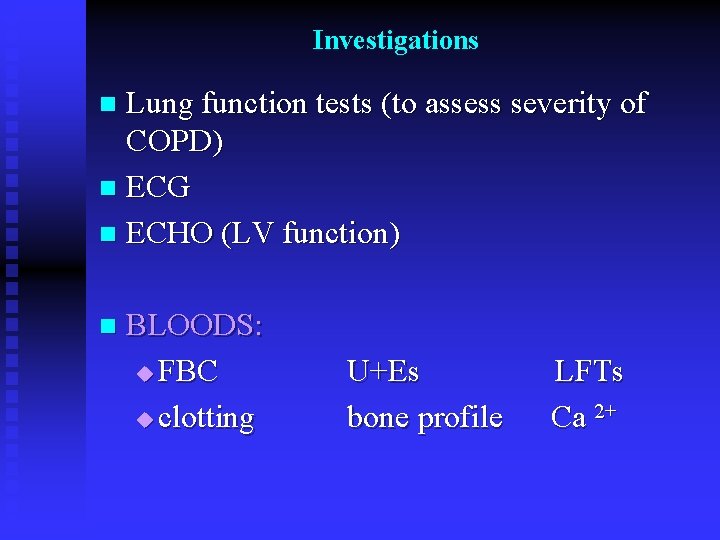
Investigations Lung function tests (to assess severity of COPD) n ECG n ECHO (LV function) n n BLOODS: u FBC u clotting U+Es bone profile LFTs Ca 2+
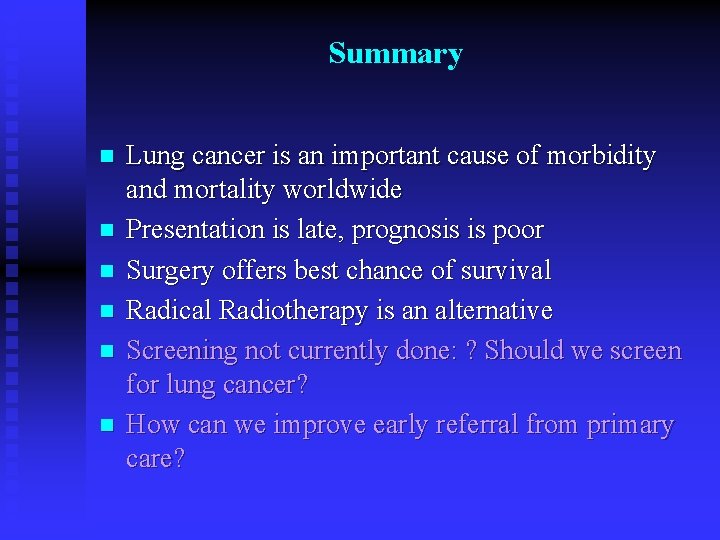
Summary n n n Lung cancer is an important cause of morbidity and mortality worldwide Presentation is late, prognosis is poor Surgery offers best chance of survival Radical Radiotherapy is an alternative Screening not currently done: ? Should we screen for lung cancer? How can we improve early referral from primary care?
Any Questions?
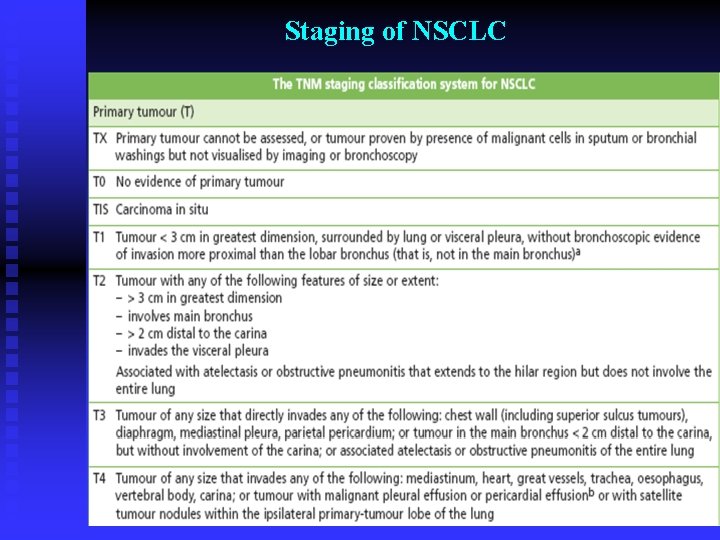
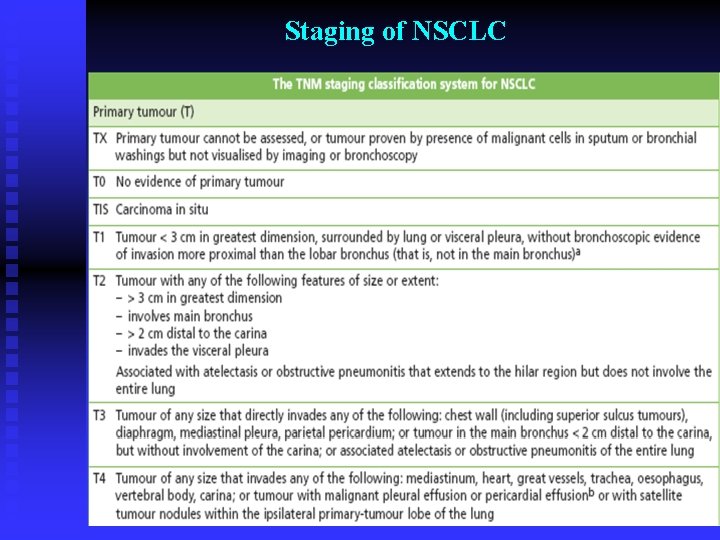
Staging of NSCLC
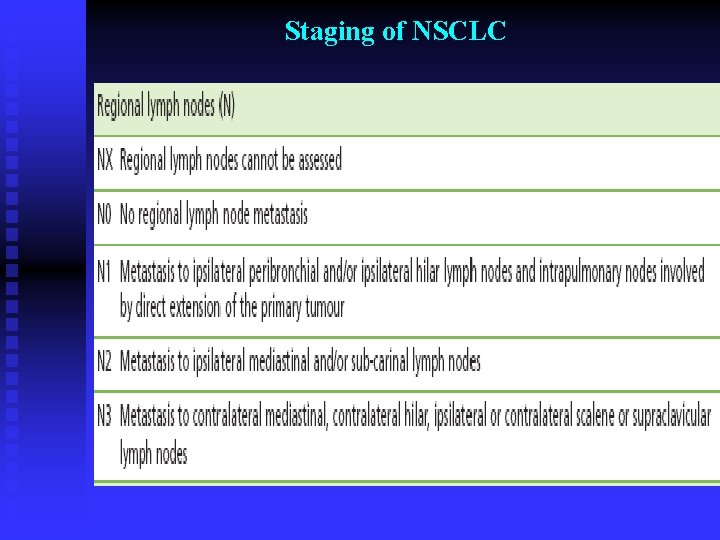
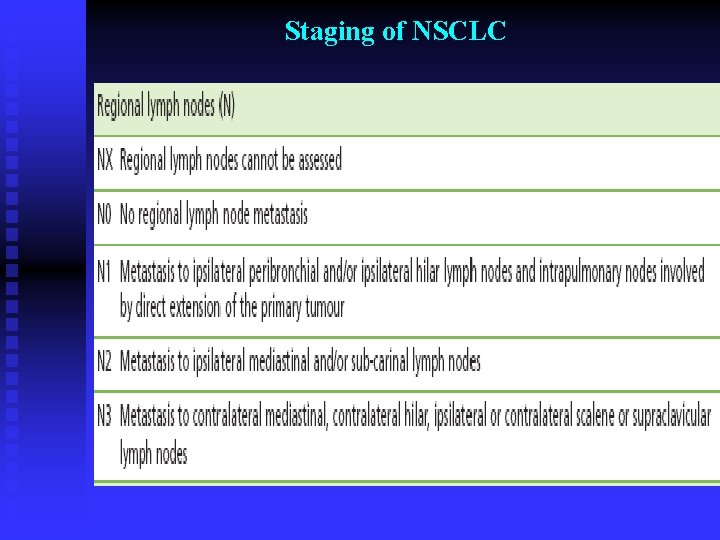
Staging of NSCLC
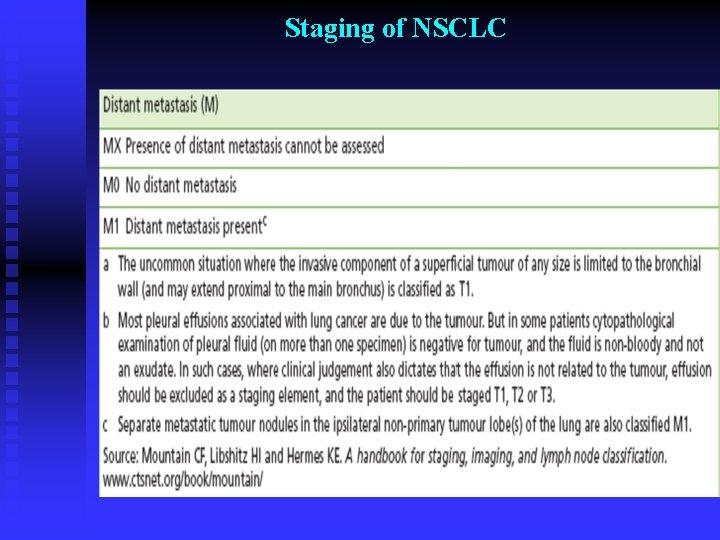
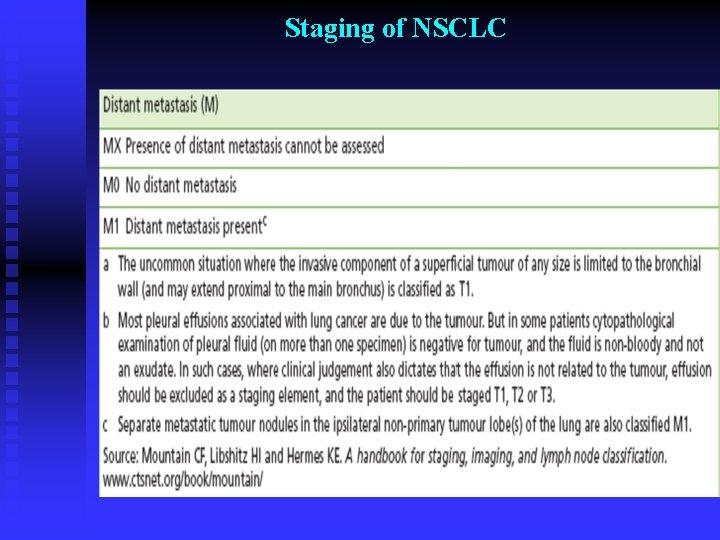
Staging of NSCLC

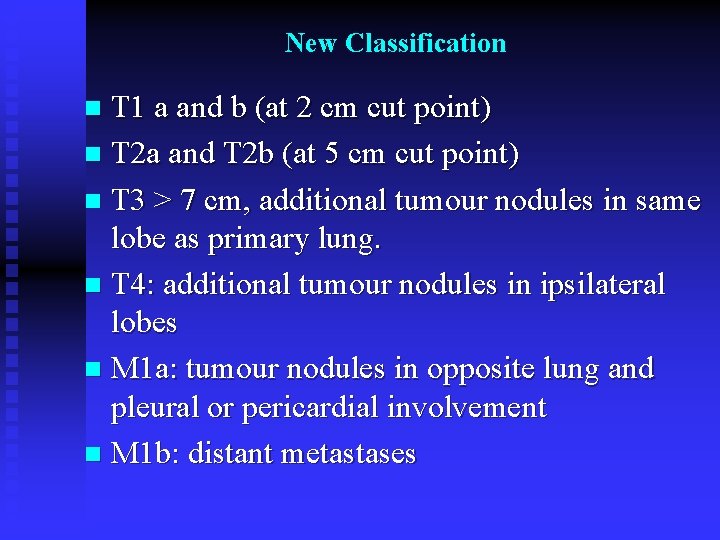
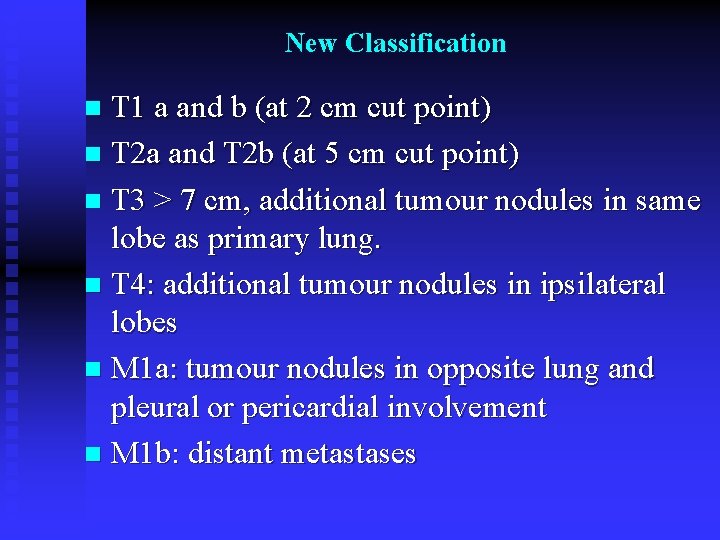
New Classification T 1 a and b (at 2 cm cut point) n T 2 a and T 2 b (at 5 cm cut point) n T 3 > 7 cm, additional tumour nodules in same lobe as primary lung. n T 4: additional tumour nodules in ipsilateral lobes n M 1 a: tumour nodules in opposite lung and pleural or pericardial involvement n M 1 b: distant metastases n
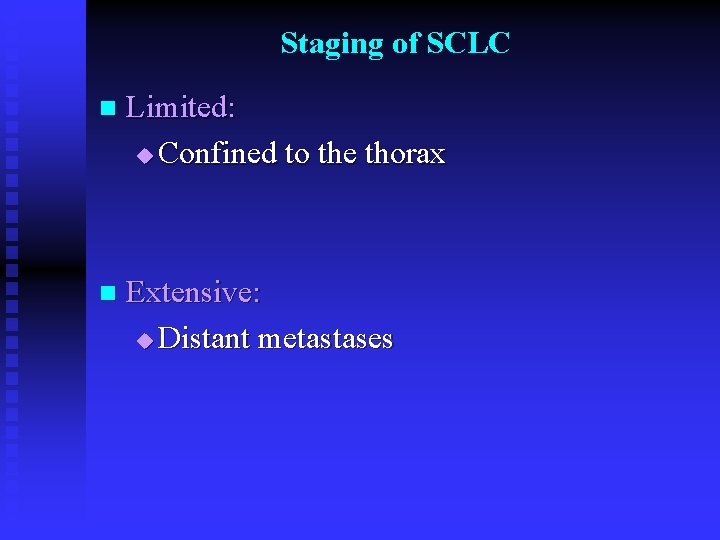
Staging of SCLC n Limited: u Confined to the thorax n Extensive: u Distant metastases
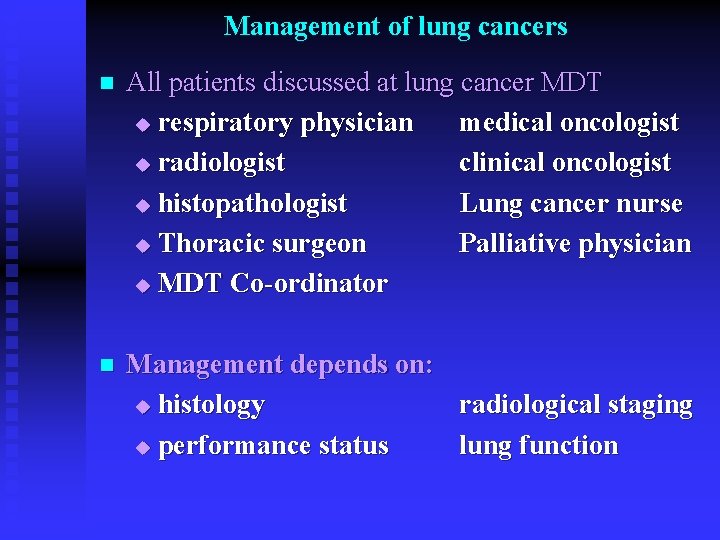
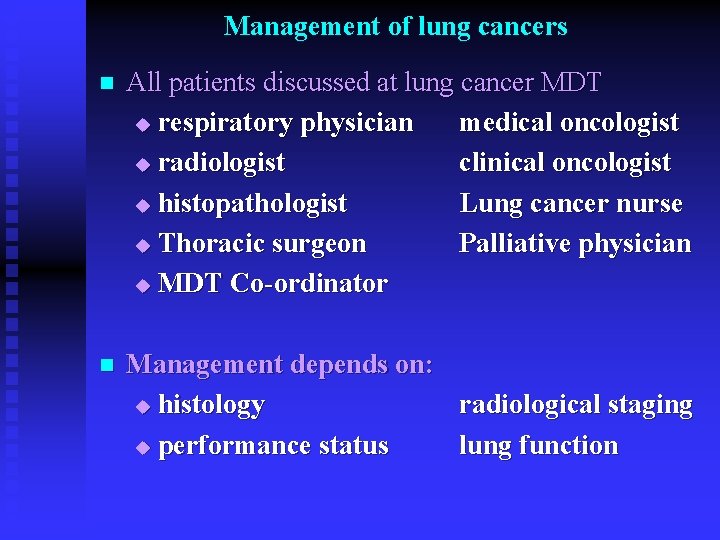
Management of lung cancers n All patients discussed at lung cancer MDT u respiratory physician medical oncologist u radiologist clinical oncologist u histopathologist Lung cancer nurse u Thoracic surgeon Palliative physician u MDT Co-ordinator n Management depends on: u histology radiological staging u performance status lung function
Management of NSCLC n Depends on: u Radiological Staging u Histology u Performance status u Lung function
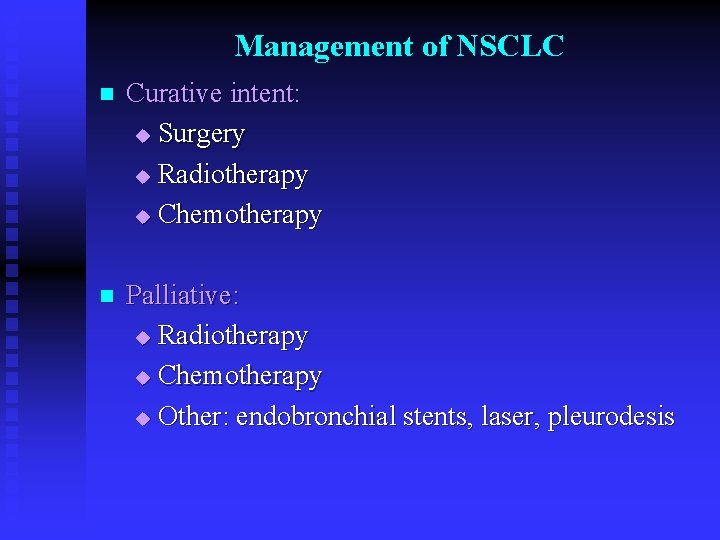
Management of NSCLC n Curative intent: u Surgery u Radiotherapy u Chemotherapy n Palliative: u Radiotherapy u Chemotherapy u Other: endobronchial stents, laser, pleurodesis
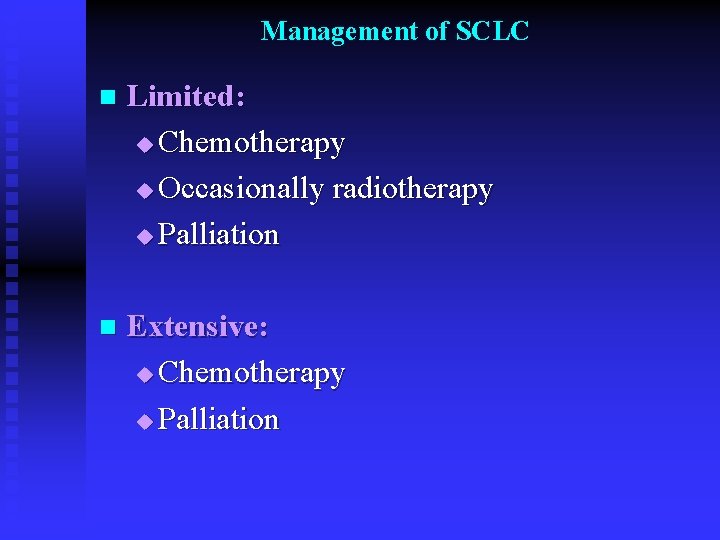
Management of SCLC n Limited: u Chemotherapy u Occasionally radiotherapy u Palliation n Extensive: u Chemotherapy u Palliation
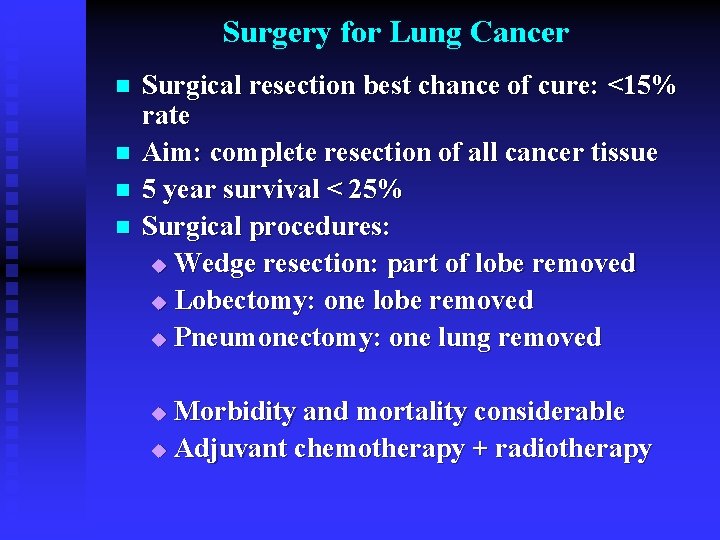
Surgery for Lung Cancer n n Surgical resection best chance of cure: <15% rate Aim: complete resection of all cancer tissue 5 year survival < 25% Surgical procedures: u Wedge resection: part of lobe removed u Lobectomy: one lobe removed u Pneumonectomy: one lung removed Morbidity and mortality considerable u Adjuvant chemotherapy + radiotherapy u
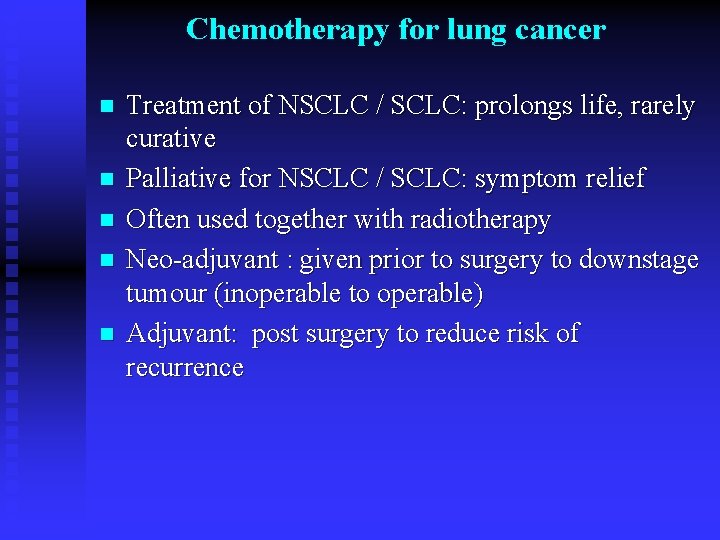
Chemotherapy for lung cancer n n n Treatment of NSCLC / SCLC: prolongs life, rarely curative Palliative for NSCLC / SCLC: symptom relief Often used together with radiotherapy Neo-adjuvant : given prior to surgery to downstage tumour (inoperable to operable) Adjuvant: post surgery to reduce risk of recurrence
Side Effects of Chemotherapy n Bone marrow : u Neutropenia thrombocytopenia anaemia n Immunosupression: u Infection sepsis n Other: u Nausea vomiting anorexia u Hair loss skin changes u Other symptoms related to specific agents
Radiotherapy for lung cancer n Radical: high dose, curative intent (CHART) n Palliative: low dose, symptom control u Pain at tumour site Bony metastases u Spinal cord compression n Prior to surgery: de-bulking, down-staging tumour n Combined modality: with chemotherapy n Post surgery: improve long term survival (27% 5 year survival)

Side effects of Radiotherapy n Lung: severe SOB u Pneumonitis u fibrosis n Heart n Oesophagus: u Dysphagia

Palliative Care n Palliative Care Team: Consultant u Community nurses u Occupational therapist u Inpatient care u Hospice u Nurses Social worker Physiotherapist Outpatient Home visits
Palliative Care n Symptom Control: Pain: pain ladder, opiates, syringe driver u Cough: opiates u SOB: O 2, morphine, diazepam u Secretions: hyoscine (pump u Constipation: laxatives u Decreased appetite: steroids u Depression: antidepressants u
Palliative Procedures n For relief of breathlessness: Endobronchial stents u Laser phototherapy u Drainage of pleural fluid u Medical or VATS pleurodesis u
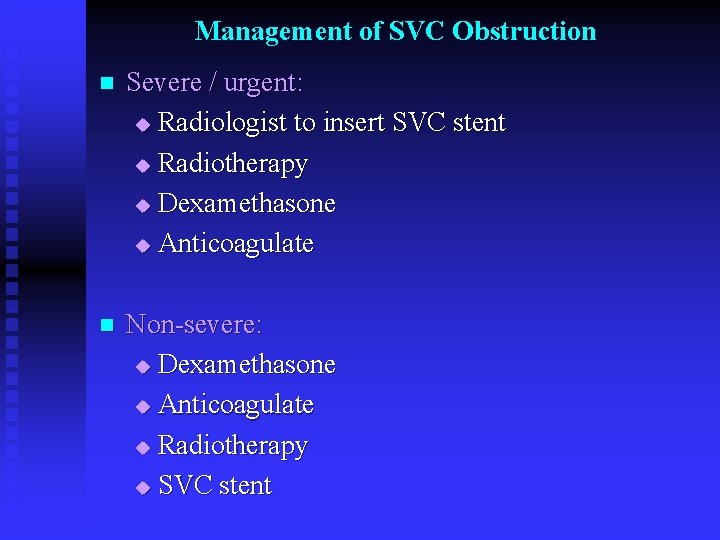
Management of SVC Obstruction n Severe / urgent: u Radiologist to insert SVC stent u Radiotherapy u Dexamethasone u Anticoagulate n Non-severe: u Dexamethasone u Anticoagulate u Radiotherapy u SVC stent
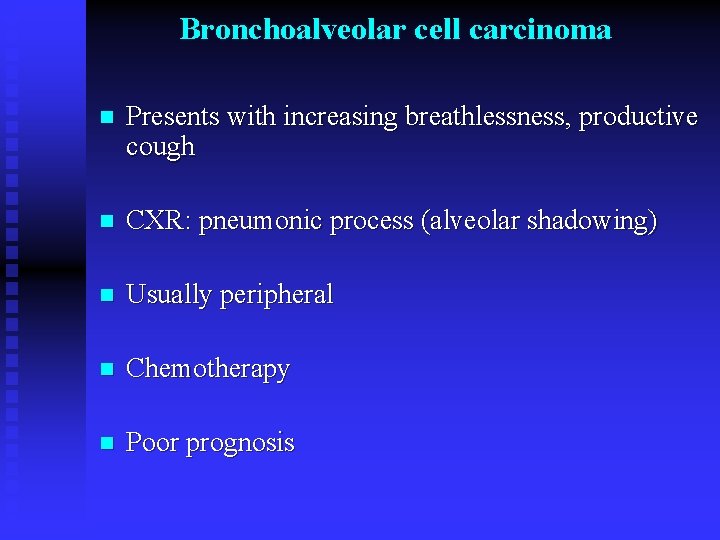
Bronchoalveolar cell carcinoma n Presents with increasing breathlessness, productive cough n CXR: pneumonic process (alveolar shadowing) n Usually peripheral n Chemotherapy n Poor prognosis
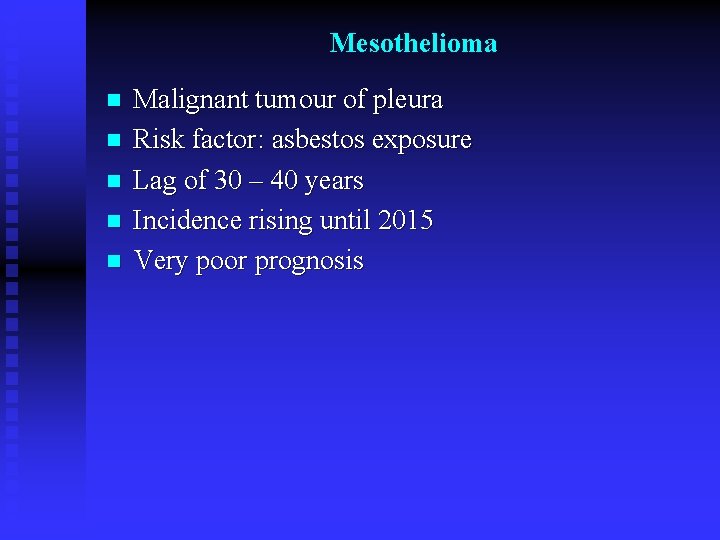
Mesothelioma n n n Malignant tumour of pleura Risk factor: asbestos exposure Lag of 30 – 40 years Incidence rising until 2015 Very poor prognosis
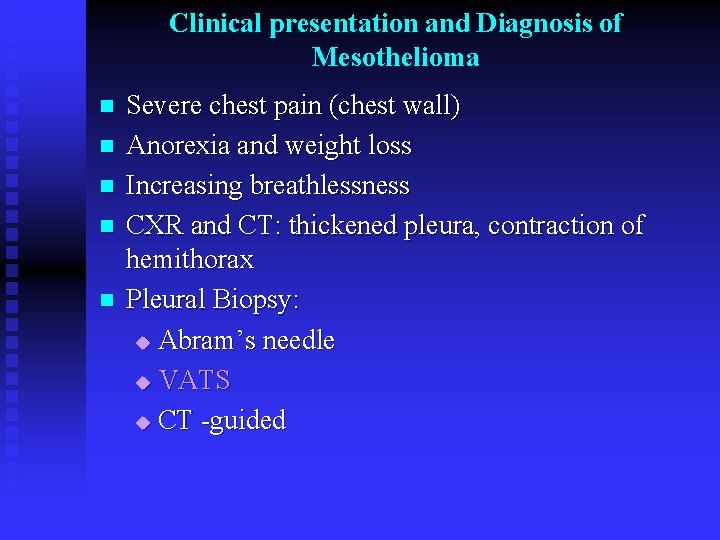
Clinical presentation and Diagnosis of Mesothelioma n n n Severe chest pain (chest wall) Anorexia and weight loss Increasing breathlessness CXR and CT: thickened pleura, contraction of hemithorax Pleural Biopsy: u Abram’s needle u VATS u CT -guided
Histopathology of mesothelioma n Epithelioid: better prognosis (18 months) n Sarcomatous: poor prognosis (6 months) n Mixed: intermediate prognosis (12 months)
Management of mesothelioma Surgery n Radiotherapy n Chemotherapy n Palliation n
Summary n n n n Lung cancer is an important cause of morbidity and mortality worldwide Presentation is late, prognosis is poor Surgery offers best chance of survival Screening not currently done: ? Should we screen for lung cancer? How can we improve early referral from primary care? Multidisciplinary approach essential Palliative care important
 Dr shanthi paramothayan
Dr shanthi paramothayan National breast and cervical cancer early detection program
National breast and cervical cancer early detection program National breast and cervical cancer early detection program
National breast and cervical cancer early detection program Shanti raghavan enable india
Shanti raghavan enable india Gesundheit central european lung cancer patient network
Gesundheit central european lung cancer patient network Dr. amy ford
Dr. amy ford Lung cancer location
Lung cancer location Optimal lung cancer pathway
Optimal lung cancer pathway Tnm stage lung cancer
Tnm stage lung cancer Lung cancer screening shared decision making tool
Lung cancer screening shared decision making tool Lifetime risk of lung cancer
Lifetime risk of lung cancer Siadh pathophysiology
Siadh pathophysiology Actual diagnosis
Actual diagnosis Ekd system
Ekd system Breast cancer anatomy and early warning signs
Breast cancer anatomy and early warning signs Early cpr and early defibrillation can: *
Early cpr and early defibrillation can: * Red infarct
Red infarct Lung dog
Lung dog Nb lung association
Nb lung association Right lung lateral view
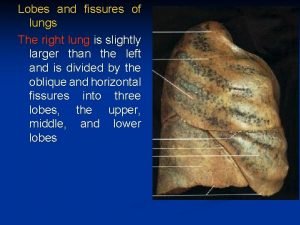
Right lung lateral view Right lung lateral view
Right lung lateral view Lung abscess classification
Lung abscess classification Bài thơ mưa làm lũng
Bài thơ mưa làm lũng 3 types of lung receptors
3 types of lung receptors Hypertranslucent lung meaning
Hypertranslucent lung meaning Weibel lung model
Weibel lung model Respiratory bud
Respiratory bud Hilum of lung
Hilum of lung Increase tactile fremitus
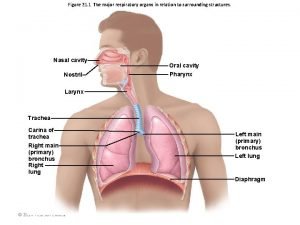
Increase tactile fremitus Carina respiratory system
Carina respiratory system Ca lung
Ca lung Cel mai lung psalm
Cel mai lung psalm Bony chest female
Bony chest female Lung surgery
Lung surgery Gây tê cơ vuông thắt lưng
Gây tê cơ vuông thắt lưng Tree in lung picture
Tree in lung picture Lung compliance
Lung compliance Lung layers
Lung layers Cvc lung histology diagram
Cvc lung histology diagram Acini
Acini Dynamic compliance formula
Dynamic compliance formula Restrictive lung disease
Restrictive lung disease Lung histology identification points
Lung histology identification points Lung lobe
Lung lobe Componentele sistemului respirator
Componentele sistemului respirator Collecting duct
Collecting duct Brochophony
Brochophony Spontaneous pneumothorax
Spontaneous pneumothorax Apex respiratory system
Apex respiratory system Percussion finger
Percussion finger Mặt hướng chạy xuất phát
Mặt hướng chạy xuất phát Lung tuberculosis
Lung tuberculosis Dlco判讀
Dlco判讀 Right middle lobe pneumonia
Right middle lobe pneumonia Caroline liqui lung
Caroline liqui lung Pneumonia
Pneumonia 3 types of lung receptors
3 types of lung receptors Atypical pneumonia
Atypical pneumonia Alveoli definition
Alveoli definition Surface anatomy of the breast
Surface anatomy of the breast Asthma pathophysiology
Asthma pathophysiology Sumptoms of blood clot in lung
Sumptoms of blood clot in lung Lung volume recruitment bag
Lung volume recruitment bag What is a restrictive lung disease
What is a restrictive lung disease Pleural cavity
Pleural cavity Lobes of lung
Lobes of lung Pleura parietal visceral
Pleura parietal visceral Dr paul healey
Dr paul healey Mediastinal surface
Mediastinal surface Right lung lateral view
Right lung lateral view Splanchnic mesoderm
Splanchnic mesoderm Heart vein
Heart vein Lungs 3 lobes
Lungs 3 lobes Identify the organ
Identify the organ Chest expansion test
Chest expansion test